Physical and Chemical Injuries of the Oral Cavity
 . Injuries of Teeth Associated with Tooth Preparation
. Injuries of Teeth Associated with Tooth Preparation
 . Reaction To Rotary Instrumentation
. Reaction To Rotary Instrumentation
 . Effect of Restorative Materials
. Effect of Restorative Materials
 . Physical Injuries of the Teeth
. Physical Injuries of the Teeth
 . Physical Injuries of the Bone
. Physical Injuries of the Bone
 . Physical Injuries of Soft Tissues
. Physical Injuries of Soft Tissues
 . Nonallergic Reactions to Drugs and Chemicals used Systemically
. Nonallergic Reactions to Drugs and Chemicals used Systemically
Injuries of the oral cavity may be caused by physical or chemical causes. Physical injuries may be iatrogenic, self-inflicted, traumatic, or occupational. The most important iatrogenic cause is the repair of tooth affected by dental caries or other developmental defects and restoration of missing tooth. Iatrogenic cause also includes X radiation and laser radiation. Self-induced or factitious injuries are due to overzealous oral hygiene practices, caused by psychotic or neurotic condition, or habitual. Traumatic causes include a fall, fight, road traffic accidents, and sports injuries.
Although chemical injuries are caused by environmental elements such as toxic levels of chemicals in the water, air, or consumables, the restorative and endodontic materials used in the routine dental practice play an important role.
Injuries of Teeth Associated with Tooth Preparation
The teeth, particularly the dentin and pulp, may be injured not only by dental caries, but also from those procedures necessary for the repair of lesions involving dental hard tissues. Preparation of the teeth for receiving the restorations include cutting, grinding, and etching with acids etc. These physical and chemical methods of tooth preparation as well as the various medicaments and filling materials which are inserted into the prepared tooth, have their own effects.
Effect of Tooth Preparation
The effect upon the dental pulp of restorative procedure alone is difficult to assess except in the sound tooth, since the carious lesion itself produces demonstrable changes in both the dentin and the pulp. Even when a sound tooth is prepared for experimental purpose, care must be taken in observing the effects to separate those which are due solely to the tooth preparation from those which are due to the restorative materials applied.
Tooth preparation is usually done by rotary instruments such as tungsten carbide burs and diamond burs of different sizes and shapes. Lasers and air abrasion are also used alternatively. Pulpal responses to these various procedures depend on the heat generated by friction, cutting of odontoblastic processes and drying of dentinal tubules, thickness of remaining dentin, vibration, removal of minerals and exposure of the organic matrix of dentin, and formation of smear layer.
Reaction to Rotary Instrumentation
Stainless steel burs revolving at low speed were used in the past for cavity and crown preparation. As the hardness of the enamel is high, these burs could not abrade instead they cut or chip away the tooth material. Also a considerable amount of pressure is applied during the procedure, which results in excessive heat production and evaporation of the contents of the dentinal tubules. High speed rotary instrumentation with tungsten carbide and diamond burs has replaced the steel burs in recent years. Nevertheless stainless steel burs are used in procedures involving bone.
The reaction of the dental pulp to cutting of dentin with a dental bur has been studied by Fish in both dogs and monkeys. When dentin is injured, there is stasis of the contents of the dentinal tubules, which lose their fluid communication with the pulp because of the formation of secondary dentin. Involved dentinal tubules are occluded by the deposition of calcium which separates these sclerosed dentinal tubules physiologically from the rest of the tooth.
The cavities prepared by Fish in the teeth of dogs or monkeys were cut with steel burs which were kept wet to prevent the complication of heat-induced damage to the pulp. In some cases the cavities were then filled with copper oxyphosphate cement and in other instances they were left open and exposed to the oral fluids. The animals were sacrificed after varying periods of time, and sections of the filled teeth were prepared for microscopic study. Three general reactions to cavity preparation were noted: (1) the production of secondary dentin, (2) changes in the odontoblasts associated with injured tubules, and (3) general changes in the pulp. Fish carefully pointed out that the reaction of the tooth with the formation of a calcified barrier and secondary dentin production is always strictly confined to the pulp surface of the injured dentinal tubules. There is never overlap of uninjured tubules, and for this reason the changes may be regarded as a specific reaction to injury of the dentinal tubules.
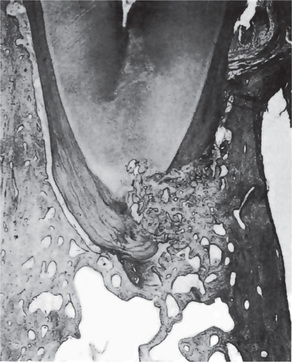
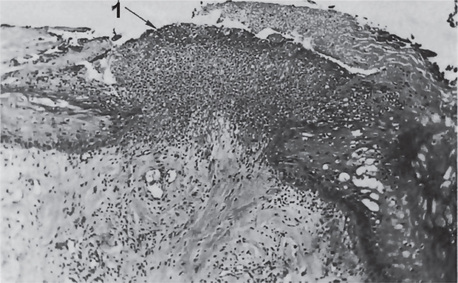
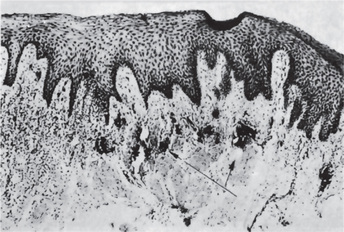
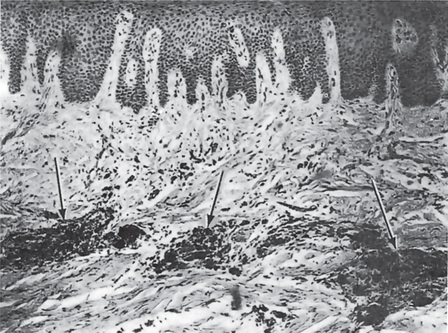
The pulp reaction to superficial injury of the dentin varies in degree of severity, depending partially upon the depth of the prepared cavity and partially upon the elapsed time between cutting the cavity and extraction of the tooth for study. In mild reactions the odontoblasts become distorted and reduced in number. Small vacuoles may appear between them, probably lymph exudate. Capillaries in the damaged area may be prominent. In more severe injuries, there may be complete disorganization of and hemorrhage in the odontoblastic layer (Fig. 12-1). The bulk of the pulp tissue away from the cut tubules may exhibit little or no reaction.
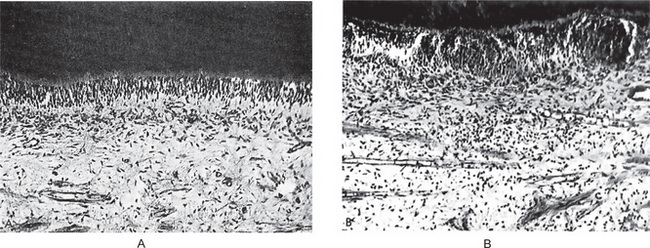
Figure 12-1 Effect on dental pulp of cavity preparation by steel bur.
Cavities were prepared in human teeth and filled with gutta-percha. A section of pulp from an intact normal tooth is shown in (A), while the injured area in the pulp six days after cavity preparation is seen in (B) Courtesy of Drs David F Mitchell and Jensen JH. J Am Dent Assoc, 55:57, 1957.
In more serious injuries there is a greater infiltration of the injured locus by polymorphonuclear leukocytes, which gradually become replaced by lymphocytes. The majority of the severe pulp injuries are probably associated with irritation brought about by the open cavities, with the sudden exposure of large numbers of open dentinal tubules to oral fluids and bacteria.
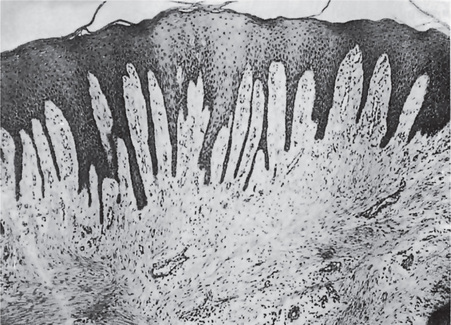
Even after such severe injuries the majority of damaged pulps undergo spontaneous healing or at least enter a quiescent phase and produce no signs or symptoms of persisting damage (Fig. 12-2). The factors responsible for this phenomenon, especially from the clinical aspect, are unknown.
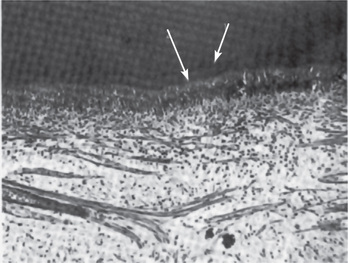
Figure 12-2 Effect of cavity preparation by steel bur on dental pulp.
A calciotraumatic line (1) and reparative dentin (2) are found beneath the cavity nine weeks after preparation Courtesy of Drs David F Mitchell, JH Jensen. J Am Dent Assoc, 55: 57, 1957.
It appears that dentin has a heat-dissipating action which reduces the temperature rise within the pulp to only a fraction of the actual temperature applied to the tooth. This is due to the low thermal conductivity of dentin, which acts as an effective insulating medium. Nevertheless the application of heat to a dental pulp already injured from a carious lesion of the dentin, but not an actual pulp exposure, may be sufficient to affect adversely the repair or healing of the pulp even though an apparently successful restoration is given to the tooth.
The preparation of tooth under the constant application of water to cool the cutting instrument and tooth will prevent many of the serious consequences due to heat, and this procedure is strongly recommended.
High-Speed Instrumentation
The development of high-speed dental engines and hand-pieces necessitated investigation of the possible effects which their use might have on pulp tissue, and numerous reports of such studies have been published.
Bernier and Knapp reported a study on high-speed instrumentation utilizing various speeds up to 100,000 rpm. They found evidence of mild pulpal damage, but, in addition, observed a new type of lesion which they termed the ‘rebound response’. This consisted variously in: (1) an alteration in ground substance, (2) edema, (3) fibrosis, (4) odontoblastic disruption, and (5) reduced predentin formation in a region directly across the pulp opposite the cavity site or at a distant pulpal site, and thought to be caused by waves of energy transmitted to the pulp focused into a certain region by the pulpal walls. The significance of this phenomenon is still not clear.
Swerdlow and Stanley in their study involving 450 human teeth found that speeds over 50,000 rpm with coolants were less injurious to the pulp than lower speeds. They concluded that the combination of high speed, controlled temperature, and light load produced minimal pathologic pulpal alteration. When heavy loads were used, even coolants did not minimize inflammatory responses. Extending this investigation to 13 operative techniques, Diamond and his coworkers found that the 300,000 rpm air-water spray—No. 35 carbide bur technique—provided all the cutting efficiency of a high-speed instrument without producing extended or burn lesions and caused the highest incidence of reparative dentin formation, a favorable protective reaction. A speed of 250,000 rpm with water coolant was reported by Nygaard-Ostby to produce even less pulpal reaction than the conventional (6,000 rpm) machine without water-spray. Caviedes-Bucheli and coworkers in their study found that substance P expression is increased in tooth where cavity preparation is done and concluded that it may have an important clinical significance in terms of inflammation and pain experience.
The practicability of use of accelerated hand-piece speeds has been accurately summarized by Stanley and Swerdlow, who stated: ‘In principle, high speed techniques approach the ideal but at the same time these methods can be easily abused… properly used, ultraspeed is an extremely safe and efficient method of reducing tooth structure’.
Effect of Air Abrasive Technique
In the air abrasive technique, aluminum oxide sprayed under pressure is used as an abrasive for the cavity preparation and surface treatment. The main drawback of this procedure is, it does not allow the operators’ stereognostic ability to control the depth of cutting. However Ferrazzano et al, based on their study in 60 mandibular third molar concluded that the macroscopic size and shape of cavities is connected to working distance, while working time is important to determine the depth of preparation. Also the abrasive dust is a potential health hazard to the operator and the patient. Nowadays it is used only to clean the pit and fissures prior to the application of sealants.
Effect of Ultrasonic Technique
The use of ultrasonic equipment for cutting cavities in teeth has been advocated because it involves less heat, noise, and vibration in contrast to rotary instruments. Essentially, the technique consists in the conversion of electrical energy into mechanical energy in the form of vibration of a tiny cutting tip, approximately 29,000 vibrations per second with an amplitude of about 0.0014 inch. Aluminum oxide abrasive in a liquid carrier is washed across this tip, and the vibration of the particles in turn results in a rapid reduction of tooth substance.
The effects of this technique, as used in cavity preparation, on the tooth and dental pulp have been evaluated by a number of investigators whose results are in essential agreement. Zach and Brown, Healey and his coworkers, and Lefkowitz among others have found that there are no remarkable differences in the reaction of the dental pulp to the preparation of cavities by the steel bur, the diamond stone or the ultrasonic instrument. This again emphasizes that only the dentinal injury itself is important, not how this injury is produced.
Mitchell and Jensen, studying the effect of steel bur and ultrasonic cavity preparation on the human tooth, also reported that no differences could be observed in the reaction of the pulp to these two techniques. Mild hyperemia, hemorrhage and a slight neutrophilic and lymphocytic infiltration of the pulp tissue immediately below the cut dentinal tubules were noted during the 6–12 day period following cavity preparation by either means. After several weeks the late reaction consisted in slight, irregular secondary dentin deposition and the formation of a ‘calciotraumatic’ line, a hematoxyphilic line between the regular dentin and the postoperative dentin apparently representing a disturbance in dentin formation at the time of the operative procedure.
Lasers
Laser is an acronym for Light Amplification by Stimulated Emission of Radiation. It is an electro-optical device which, upon stimulation, can convert jumbles of light waves into an intense, concentrated, uniform, narrow beam of monochromatic light with an energy source of great intensity and exceptional flexibility. The radiation may be continuous or modulated, or the emission may occur in short pulses. This high-intensity radiation can be focused on an extremely small area, approximately 1 micron in diameter, because of the small angle of divergence and coherency of the beam. Light photons of characteristic wavelengths are produced, amplified, and filtered to produce the laser beam. Carbon dioxide and neodymium:yttrium-aluminum-garnet (Nd:YAG) lasers are most commonly used. The main problem with laser cutting of hard dental tissues is the generation of heat and forbidden tactile control.
Lasers are used in dental practice to coalesce pits and fissures to eliminate retention sites for bacteria, to desensitize the exposed root surfaces, to make the hard tissue surfaces rough to promote bonding as an alternative to acid etching, to vaporize the carious tissue, to vaporize the organic tissues in the root canal in endodontic procedures, cavity preparation, restoration removal, treatment of dentinal sensitivity, caries prevention and bleaching.
Effects on Teeth
The effects of laser on teeth were first reported by Stern and Sognnaes, who found that exposure of intact enamel, caused a glass like fusion of the enamel, whereas dentin exposed to laser exhibited a definitive charred crater. Chalky spots, craters, or small holes in enamel may also be produced under other conditions. Scanning electron microscopic analysis showed the effects of laser on dentin vary from no effects to disruption of the smeared layer to actual melting and recrystallization of the dentin, depending on power level, duration of exposure, and color of the dentin. Although it has been shown that selective deep destruction of carious tooth substance can be accomplished, the practicality of its use in removing carious lesions is still questionable. Laser irradiation alters the dentin structure and produces surface layers that give the appearance of being more enamel-like. The laser-modified surface may be more resistant to demineralization; hence, many investigators are proposing continued development of the laser for caries prevention.
Open dentin surface exposed to laser results in melting and closure of the orifices of the dentin and this property is used to treat dentin hypersensitivity.
Bleaching of stained teeth has also been accomplished by lasing.
Effects on Pulp
The pulps of teeth in animals subjected to laser radiation have been described by Taylor and his associates as showing severe pathologic changes, including hemorrhagic necrosis with acute and chronic inflammatory cell infiltration. The odontoblastic layer also underwent coagulation necrosis, although the severity of the response varied with the amount of radiation.
Effect of Heat
The reaction of the dental pulp to heat is an important clinical problem because of the extraordinary amount of heat that may be generated by the revolving cutting and grinding instruments used in tooth preparation. Actually, temperatures over 700° F have been recorded on the cutting surfaces of stones and burs under abusive conditions.
Thermal change may be influenced by: (1) the size, shape, and composition of the bur or stone, (2) the speed of the bur or stone, (3) the amount and direction of pressure applied, (4) the amount of moisture in the field of operation, (5) the length of time that the bur or stone is in contact with the tooth, and (6) the type of tissue being cut, enamel or dentin. Of further significance is the heat generated during the setting of various restorative materials, particularly the direct resins. In in vitro experiments, Wolcott and his associates showed that the temperature at the dentin-resin junction may reach 212° F, and they recorded a temperature of 133° F in the pulp chamber.
Effect of Restorative Materials
The dentist has at his/her disposal a great many materials prepared commercially to restore the original contour of the tooth attacked by dental caries and other lesions of the tooth including trauma. The dentist must be familiar with the advantages and disadvantages of each material from the point of view of its physical and chemical properties and its ability to fulfil the purpose for which it is intended. In addition, he must be acquainted with the biologic effects of the restorative materials on the tooth, especially on the dental pulp.
A great many experimental studies have been carried out to investigate the effects of the different restorative materials on the dental pulp, and today such testing is routine before new restorative materials are released by ethical manufacturers for use by dentists. It should be obvious that a restorative material applied to a prepared tooth is in contact with more than just a mass of inert calcified material. The dentinal tubules, containing odontoblastic processes which have been freshly cut, form a series of passage ways leading directly to the pulp through which a fluid or soluble material may reach the pulp tissue. If this material is irritating, it may lead to serious injury. For this reason a comparison of the effects of the various common restorative materials is important.
Zinc Oxide and Eugenol
It is used routinely as a temporary filling material or root canal sealer. Eugenol of this cement fixes cells, depresses the cell respiration, and reduces the neural transmission in vitro. There is almost universal agreement that zinc oxide and eugenol is the least injurious of all filling materials to the dental pulp. Not only is there no irritation produced by this substance, but actually it exerts a palliative and sedative effect on the mildly damaged pulp, since it inhibits synthesis of prostaglandins and leukotrienes. It seems to be such a bland substance that it may lack even the necessary irritating properties requisite to the stimulation of secondary dentin formation. In view of these findings, zinc oxide and eugenol is the material of choice for use over injured pulps or as a base in deep cavity preparations.
Zinc Phosphate (Oxyphosphate) Cement
This particular cement is widely used in dentistry both as a protective base in deep cavities before the insertion of the restoration and also in cementing cast inlays, crowns, and other similar restorations. The majority of investigators have reported significant deleterious effects on the pulp when the material is placed in cavities, the actual injurious agent supposedly being the phosphoric acid.
Gurley and Van Huysen prepared cavities in teeth of young dogs and filled them with zinc phosphate cement. After approximately 1½ months they found hyperemia and inflammatory cell infiltration of the pulp with disarrangement of the odontoblastic layer. Secondary dentin had formed under the shallower cavities. The more severe pulpal reactions occurred under the deeper cavities.
Studies on human teeth, such as those by Manley, by Shroff, and by Kramer and McLean, show that hyperemia or hemorrhage with inflammatory cell infiltration of the pulp accompanied by reduction in the size and number of the odontoblasts occurs after placement of this cement in prepared cavities.
The studies generally indicate that zinc oxyphosphate cement is an irritant when placed in the base of a deep cavity, particularly in bulk, although the human pulp may be able to localize this reaction in most instances. When this cement is used in shallow cavities, it is relatively innocuous and reportedly serves a useful function in the stimulation of secondary dentin formation.
Polycarboxylate or polyacrylate cements have properties comparable to those of the phosphate cements, but have a low degree of pulpal irritation similar to that of the zinc oxide-eugenol cements.
Silver Amalgam
Silver amalgam is used as a filling material in dentistry. It is an innocuous material, particularly in shallow cavities. Beneath deep cavities filled with amalgam, Manley found a decrease in the number of odontoblasts, as well as mild inflammatory cell infiltration of the pulp. The complication of thermal shock transmitted by deep amalgam restorations is difficult to evaluate, but is a source of potential damage.
In contrast, Swerdlow and Stanley studied the pulpal responses in 73 intact human teeth with cavities prepared at speed of 20,000–300,000 rpm and filled with either amalgam or zinc oxide and eugenol. They reported that the amalgam increased the intensity of mild pulpal response to cavity preparation and that this appeared to be due, in part at least, to the mechanical aspects of amalgam condensation. Brännström studied the effect of amalgam restorations on pulp tissue, and concluded that any damage to the pulp was due to leakage around the restoration, not to the filling material itself. Dark colored metallic components of the silver alloy turn the dentin dark gray and tooth may appear discolored.
Amalgam restorations when in contact with gingiva cause inflammation because of corrosion products and dental plaque.
Relationship between oral lichenoid reactions and silver amalgam fillings is a matter of controversy. A number of studies have been published with respect to amalgam filling and lichenoid reactions. A Dunsche and coworkers suggest the removal of amalgam fillings in all patients with symptomatic oral lichenoid reactions associated with amalgam fillings if no cutaneous lichen planus is present.
Glass-ionomer
Glass-ionomer cement is considered as biocompatible and is widely used as filling and lining material and as a luting agent. It consists of fluoroaluminosilicate glass powder and polycarboxylic acid. Glass-ionomers are water-based, and the set materials are composed of an inorganic-organic complex with high molecular weight. In contrast to other cements, glass-ionomer has the advantages of chemically bonding to mineralized tissues and release of fluorides.
Glass-ionomer cement bonds to the dentin by chemical and mechanical means. The chemical bonding is based on the exchange of ions between carboxylic groups of the substrate and calcium ions derived from partially dissolved apatite crystallites. The mechanical interlocking is based on the demineralization of exposed dentin by polycarboxylic acid treatment. Collagen fibers can be exposed and an intermediate layer can be formed between glass-ionomer material and undemineralized dentin.
Biocompatibility of glass-ionomer cement is due to the weak nature of polyacrylic acid. Histologically there is minimal or absence of inflammation in pulp after a month. Pulpal pain may be present for a short period after the filling of cervical cavities, and is due to the increased dentin permeability after acid etching.
Self-polymerizing Acrylic Resin
Self-curing resins were extensively used as restorative materials, particularly in anterior teeth. There is evidence to indicate, however, that these resins may cause serious damage to the dental pulp. Still, not all investigations are in complete agreement.
Conventional Composite Resins
These are restorative materials developed chiefly because methyl methacrylate or unfilled acrylic resins have restrictive characteristics such as low hardness and strength, a high coefficient of thermal expansion and a lack of adhesion to tooth structure. The resin matrix is a compromise between epoxy and methacrylate resins. This resin is combined with a filler of dispersed particles of varying types in relatively high concentration. While most conventional composite resins are chemically activated, some are now marketed whose cure is based on light activation.
The biologic properties of the composite resins show the same irritational characteristics as the unfilled acrylic resins. For this reason, the same measures should be taken to protect the pulp from possible injury, especially when the cavity preparation is deep. A calcium hydroxide base is preferable to a zinc oxide and eugenol base because of the possible interaction of eugenol and resin.
Microfilled Composite Resins
These are a newer group of resins which contain the same resin matrix as the conventional composite resins but differ in that the size of the filler is much smaller than in the conventional resin. The biologic properties of the microfilled resins, including their irritational effects on the pulp, are comparable to those of the conventional composite resins. Thus, some pulpal protection is necessary under deep cavities.
The many experimental studies cited would indicate superficially that the majority of restorative materials used in dentistry today are dangerous because of the serious effects on the dental pulp which they often induce. It is true that many of these materials are potentially injurious. Nevertheless, literally millions of restorations with these substances are placed each year, and clinical experience has shown that, unless actual pulp exposure has occurred, the death rate of dental pulps directly attributable to the restorative material is extremely low. Even the occurrence of clinical symptoms of pulp injury is uncommon. Although this seems contradictory to experimental evidence, it should be appreciated that most cavities prepared by the dentist in which these materials are inserted are to repair a destructive carious lesion. The presence of this carious lesion, in contrast to the experimental cavities prepared in sound human and animal teeth, has usually induced the deposition of secondary dentin and has caused a certain amount of dentinal sclerosis, and these reactions offer considerable protection to the pulp. It is on this basis that the dentist is justified in continuing to use these filling materials. There is a need, however, for continued study of this general problem.
Effect of Cement Bases, Cavity Liners, Varnishes and Primers
A variety of materials commonly used in dental practice are inserted in a cavity preparation between the tooth and the restoration for the following purposes:
• To serve as a bacteriostatic agent.
• To provide thermal insulation, particularly under metallic restorations.
• To provide electrical insulation under metallic restorations.
• To prevent discoloration of tooth structure adjacent to certain types of restorative materials.
• To prevent the penetration of deleterious constituents of restorative materials into the dentin and pulp.
• To improve the marginal seal of certain restorative materials by preventing microleakage and the ingress of saliva and debris along the tooth-restoration interface.
These materials are generally classified as cement bases, cavity liners, cavity varnishes and cavity primers, and they are important because of their possible effects on the dental pulp.
Cement Bases
A cement base is a layer of cement commonly used beneath the dental restoration either to encourage recovery of the injured pulp or to protect the pulp against the injuries. Intermediary base materials that are commonly used under permanent restorations include zinc phosphate cement, zinc oxide-eugenol cement, and calcium hydroxide cement. Ideally, a cement base should be biologically compatible with the dental pulp and such is the case with zinc oxide-eugenol and calcium hydroxide. However, zinc phosphate cement, when placed against dentin, acts as an irritant to the dental pulp because of the acid content which varies between pH 3.5 and 6.6, as discussed previously.
Cavity Liners
Cavity liners are aqueous or volatile organic liquid suspensions or dispersions of zinc oxide or calcium hydroxide that can be applied in a relatively thin film to the surface of a cavity. They may also be solutions of resins in an organic solvent to which has been added calcium hydroxide or zinc oxide, or aqueous suspensions of calcium hydroxide in methylcellulose. The cavity liner provides the beneficial effects of zinc oxide and calcium hydroxide as thin films in shallow cavities and, in addition, neutralizes the free acid of zinc phosphate and silicate cements. The cavity liners themselves have no effect on dental pulp and, in fact, actually form a chemical barrier to provide reliable protection for the pulp under certain deep restorations.
Stanley has compared the protective effect of reparative dentin with cavity liners and bases, and generally concluded that: (1) pulpal tissue beneath preoperatively formed reparative dentin is safe from most subsequent procedures; (2) cavity liners and/or bases, should be employed since the completeness of the reparative dentin barrier cannot be ascertained; (3) the unrestored tooth being utilized as an abutment lacks reparative dentin and is more subject to the damaging effects of chemical agents because of patent dentinal tubules; (4) although 2 mm of primary dentin between the floor of the cavity preparation and the dental pulp is usually a sufficient protective barrier, the condensation of amalgam or gold foil, as well as the chemical irritation of cements and self-curing resins, may render this thickness of protection insufficient; (5) age changes in the tooth, with the production of reparative dentin in the involved area, are of no recognizable benefit regarding pulp protection; (6) high-speed, water-cooled cutting techniques produce an average incidence of reparative dentin formation of under 20%; even less reparative dentin formation is produced if more than 1 mm of primary dentin remains beneath the cavity preparation; (7) if reparative dentin does not form within the first 50 days following a restorative procedure, then there will be none; (8) nearly 20 postoperative days are required for new odontoblasts to differentiate and produce reparative dentin, and it has been shown that an average of 100 productive days of matrix formation is required to produce a reparative dentin barrier of 0.15 mm; (9) final cementation of restorations need not be delayed in allowing time for reparative dentin to form, since the use of cavity-lining materials is a reasonable substitute; and (10) cavity varnish and calcium hydroxide lining materials appear capable of protecting pulp if used appropriately.
Cavity Varnishes
Cavity varnishes are solutions of one or more resins from natural gums, synthetic resins, and rosin in organic solvents. It is generally agreed that varnishes may be of aid in reducing postoperative sensitivity, but their film thickness is insufficient to provide thermal insulation. This film also acts as a semipermeable membrane so that certain types of ions penetrate it, while others do not. It has been found also that varnishes are effective in reducing the microleakage of fluids around the margins of restorations.
While cavity varnishes themselves appear to have no significant effect upon a dental pulp, neither do they have a sedative effect. Therefore, in deep restorations, it may be advisable to utilize calcium hydroxide or zinc oxide-eugenol cements first, and then apply the varnish over this base.
Effect of Cavity-sterilizing Agents
Cavity-sterilizing agents are frequently used as a final step in routine cavity preparation and also in an attempt to sterilize discolored, infected dentin in the base of deep carious lesions when this dentin cannot be completely removed without risk of pulp exposure. It has been suggested that cavity sterilization is unnecessary, since microorganisms persisting in the dentinal tubules after a restoration has been placed do not flourish but, rather die or exist in an inactive state. Furthermore, should the dentin be carious so near the pulp that exposure is feared were it all to be removed, the pulp tissue by this time would almost certainly have become infected, and attempts at sterilization would be worthless.
Physical Injuries of the Teeth
Bruxism: (‘Night-grinding’, bruxomania)
Bruxism is the habitual grinding or clenching of the teeth, either during sleep or as an unconscious habit during waking hours. This term is generally applied both to the clenching habit, during which pressure is exerted on the teeth and periodontium by the actual grinding or clamping of the teeth, and also to the repeated tapping of the teeth. Bruxism is one of the most common sleep disorders. The incidence of bruxism has been variously reported as between 5 and 20%.
Etiology
In a review of the subject by Nadler and Meklas, the causes of bruxism have been described as: (1) local, (2) systemic, (3) psychologic, and (4) occupational.
Local factors are generally associated with some form of mild occlusal disturbance which produces mild discomfort, and chronic, even though unrecognized, tension. It has been suggested that in many cases bruxism becomes a firm habit as a result of an unconscious attempt by the patient to establish a greater number of teeth in contact or to counteract a local irritating situation. In children the habit is frequently associated with the transition from the deciduous to the permanent dentition and may result from an unconscious attempt to place the individual tooth planes so that the musculature will be at rest.
Systemic factors have been proposed as etiologically significant, but the role of most of these is difficult to assess. Gastrointestinal disturbances, subclinical nutritional deficiencies, and allergy or endocrine disturbances have all been reported as causative factors. A hereditary background has been described in some cases.
Psychologic factors are believed by some investigators to be the most common cause of bruxism. High levels of anxiety, stress, and emotional tension may be expressed through a number of nervous habits, one of which may be bruxism. Thus, when a person suffers from fear, rage, rejection, or a variety of other emotions which he/she is unable to express, these become hidden in the subconscious but are expressed periodically by numerous means. It has been observed that bruxism is common in mental institutions. Bruxism is a manifestation of nervous tension in children also and may be related to chronic biting or chewing of toys. Polysomnographic studies suggested that sleep bruxism episodes are part of sleep arousal response. The sleep arousal response is nothing but sudden change in the depth of sleep. Besides the sleep bruxism appears to be a disturbance in the dopaminergic system.
Occupations of certain types favor the development of this habit. Athletes engaged in physical activities often develop bruxism, although the exact reason for this is uncertain. Occupations, in which the work must be unusually precise, such as that of the watchmaker, are prone to cause bruxism. Voluntary bruxism is also recognized in those persons who habitually chew gum, tobacco, or objects such as toothpicks or pencils. Although voluntary, this too is a nervous reaction and may lead eventually to involuntary or subconscious bruxism.
Clinical Features
The person who engages in bruxism performs the typical grinding or clenching motions during sleep or subconsciously when awake. These may be associated with a grinding or grating noise. The symptomatic effects of this habit have been reviewed by Glaros and Rao, who have divided them into six major categories: (1) effects on the dentition, (2) effects on the periodontium, (3) effects on the masticatory muscles, (4) effects on the temporomandibular joint, (5) head pain, and (6) psychologic and behavioral effects.
When the habit is firmly established, severe wearing or attrition of the teeth may occur, not only occlusal wear, but also interproximal wear which produces sensitivity. On both surfaces actual facets may be worn in the teeth. As the bruxism continues, there may be loss of integrity of the periodontal structures, resulting in loosening or drifting of teeth or even gingival recession with alveolar bone loss. Temporomandibular joint disturbances are also reported to occur as a result of the traumatic injury of continuous tooth impact without normal periods of rest. Hypertrophy of the masticatory muscles, particularly the masseter muscle, may interfere with maintenance of the rest position, cause trismus, and alter occlusion and the opening and closing pattern of the jaws.
Finally, while it has been suggested that bruxism may give rise to facial pain and headache as well as psychologic and behavioral effects, these are very difficult manifestations to evaluate and correlate.
Treatment and Prognosis
If the underlying cause of the bruxism is an emotional one, the nervous factor must be corrected if the disease is to be cured. Removable splints to be worn at night may be constructed to immobilize the jaws or to guide the movement so that periodontal damage is minimal. Recently Botulinum toxin (Botox) has been very successful in treating the grinding and clenching of bruxism. Botox when injected into the masseter muscle, weakens the muscle enough to stop the grinding and clenching, but not so much as to interfere with chewing or facial expressions. RC DiFrancesco and coworkers suggest that there is a positive correlation between sleep-disordered breathing and bruxism and stated that there was an important improvement of bruxism after adenotonsillectomy based on their study of 69 children. If the disease is left untreated, severe periodontal and/or temporomandibular disturbances may result.
Fractures of Teeth
Tooth fracture is a common injury which may arise in a variety of situations, the most frequent of which is sudden severe trauma. This is usually a fall, a blow, an automobile accident or any of a large number of incidents in which children especially are frequently involved. Some cases of fracture occur when a tooth is weakened as by a large restoration, leaving thin walls or unsupported cusps which give way under the stress of mastication. A similar weakening and subsequent fracture occurs also in cases of internal resorption of teeth. Teeth which have had root canal therapy are often described as being somewhat brittle and susceptible to fracture.
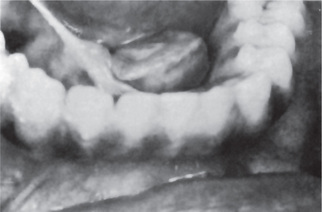
Clinical Features
Although fracture of teeth may occur at any age, children are especially prone to sustain this type of injury. The prevalence of tooth fracture is difficult to assess or evaluate, particularly since minor chipping of teeth is common. As might be expected, boys are more frequently involved than girls. There is a definite predilection for involvement of maxillary teeth, with between 75 and 90% of fractures occurring there (Fig. 12-3).
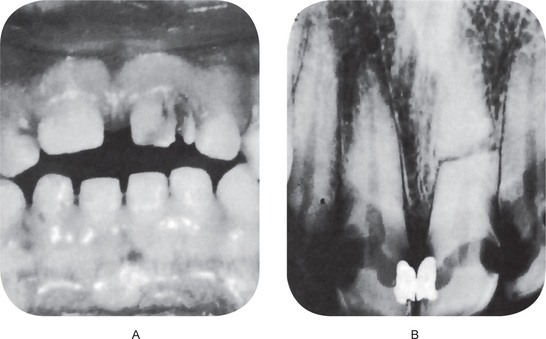
Figure 12-3 Fractured teeth after traumatic injury.
(A) Fracture of crown with pulp exposure. (B) Root fracture.
There are several classifications of fractured teeth, the simplest being only whether or not the fracture line involves the pulp. A more detailed classification is that of Ellis, who divides all traumatized anterior teeth (for these constitute the vast majority of such injuries) into nine classes:
Class 1: Simple fracture of the crown, involving little or no dentin.
Class 2: Extensive fracture of the crown, involving considerable dentin but not the dental pulp.
Class 3: Extensive fracture of the crown, involving considerable dentin and exposing the dental pulp.
Class 4: The traumatized tooth becomes nonvital, with or without loss of crown structure.
Class 5: Teeth lost as a result of trauma.
Class 6: Fracture of the root, with or without loss of crown structure.
Class 7: Displacement of a tooth, without fracture of crown or root.
Class 8: Fracture of the crown en masse and its replacement.
The clinical manifestation as well as the treatment and prognosis of the fractured tooth depend chiefly upon whether the dental pulp is pierced by the fracture and whether the crown or the root of the tooth is involved. If there is crown fracture without pulp involvement, vitality of the tooth is usually maintained, although there may be mild pulp hyperemia even when the overlying dentin is relatively thick. If the dentin over the pulp is exceedingly thin, bacteria may penetrate the dentinal tubules, infect the pulp and produce pulpitis, leading to death of the pulp. When vitality is maintained, usually a layer of secondary dentin is deposited over the involved dentinal tubules. The tooth may be sore and slightly loose because of the traumatic injury, but severe pain is usually absent.
A fractured tooth crown which exposes the pulp is a more serious problem, but pulp exposure does not necessarily imply that death of the pulp will occur. In some cases the exposure can be capped by calcium hydroxide, and a dentinal bridge will form as a part of the healing reaction. Pulpotomy or pulpectomy may often be necessary; however, since the pulp becomes infected almost immediately after the injury.
Root fractures are somewhat uncommon in young children, since their tooth roots are not completely formed and the teeth have some resilience in their sockets. It occurs in patients between the ages of 10 and 20 years and most are traumatic in origin. Root fractures involve mostly the middle third of the root and are horizontal. When fracture does occur, the tooth is loose and sore and there may be displacement of the coronal portion of the tooth. Most of the time tooth becomes nonvital after fracture. Some teeth may be repaired by forming a layer of reparative dentin along the pulp wall and cementum on the outer surface, or form granulation tissue between the fractured segments. Few may remain vital with resorption of the sharp edges of the fractured fragments.
In certain situations where the injury is sufficient to cause root fracture, fragments of cementum may be severed from dentin and is called cemental tear.
Histologic Features
Healing in such cases may be of several types. The most satisfactory form of healing is the union of the two fragments by calcified tissue, and this is analogous to the healing of a bony fracture. The clot between the root fragments is organized, and this connective tissue is subsequently the site of new cementum or bone formation. There is nearly always some resorption of the ends of the fragments, but these resorption lacunae ultimately are repaired. If the apposition between the two fragments is not close, the union is by connective tissue alone. It appears likely that the repair process can be organized from connective tissue cells in both the pulp and the periodontal ligament.
Cracked Tooth Syndrome
Cracked tooth syndrome (CTS) is characterized by sharp pain on chewing without any obvious reason, which is actually caused by a ‘hidden’ crack of the tooth. These are incomplete fractures that are too small to be seen on radiographs. The typical symptom is sharp fleeting pain when releasing biting pressure on an object. This is because when biting down, the segments are usually moving apart and thereby reduce the pressure in the nerves of the pulp. When the bite is released, the ‘segments’ snap back together sharply increasing the pressure causing pain. The pain is often inconsistent, and frequently hard to reproduce. Causes of CTS include attrition, bruxism, trauma, accidental bitting on a hard object, presence of large restoration, and improper endodontic treatment. The American Association of Endodontists have classified five specific variations of cracked teeth; craze line, fractured cusp, cracked tooth, split tooth, and vertical root fracture.
Treatment and Prognosis
The site, direction, and size of the crack or fracture dictates the choice of the treatment. It ranges from stabilization with a stainless steel band or crown to endodontic treatment and restoration. If untreated, CTS can lead to severe pain, possible pulpal necrosis and periapical abscess. Unfortunately, management of CTS is not always successful. In some cases, such as in vertical root fractures (split root) in single rooted teeth, the only treatment option is tooth extraction.
Abrasion
Wearing away of tooth substance due to mechanical means is known as abrasion. The most common cause is the faulty brushing techniques. Habits such as opening the hairpin constantly using anterior teeth, holding bobby pins, and holding pipe also produce a characteristic form of abrasion. This is described in Chapter 13 on Regressive Alterations of the Teeth.
Abuse of the teeth such as opening of beer or other bottles using teeth causes chipping away of enamel in incisors, canine and premolars.
Injuries to the Supporting Structures of the Tooth
Concussion is produced by injury which is not strong enough to cause serious, visible damage to the tooth and the periodontal structures. On clinical examination tooth may not be mobile or displaced from its original position. Crown appears normal and patient may not feel any difference in occlusion. Pulp gives normal response to vitality test. But the characteristic feature is the increased sensitivity of the tooth to percussion from any direction.
Treatment consists of selective grinding of the tooth to eliminate occlusal forces.
Subluxation refers to abnormal loosening of tooth without displacement due to sudden trauma. Tooth is mobile on palpation and sensitive to percussion and occlusal forces. Rupture of the periodontal tissue is usually evident by bleeding at the gingival marginal crevice. In time tooth becomes nonvital due to severance of apical blood supply.
Avulsion is dislocation of the tooth from its socket due to traumatic injury. It can be partial or total. Partial avulsion includes intrusion, extrusion, or facial, lingual or palatal, or lateral displacement.
Avulsion is usually accompanied by fracture of the alveolar bone. Partial avulsion is managed by reposition of the tooth and stabilization with splints. Completely avulsed tooth can be replanted in its socket. The prognosis of the replantation will be good if the extraoral time is minimal and the avulsed tooth is kept in a suitable medium during transportation. Nevertheless many of the replanted teeth undergo ankylosis to the alveolar bone.
Tooth Ankylosis
Fusion between the tooth and bone, termed ankylosis is an uncommon phenomenon in the deciduous dentition and even more rare in permanent teeth. The condition of deciduous tooth ankylosis (submerged tooth) has been described in Chapter 1 on Developmental Disturbances of Oral and Paraoral Structures.
Ankylosis ensues when partial root resorption is followed by repair with either cementum or bone that unites the tooth root with the alveolar bone. It must not be inferred that root resorption invariably leads to ankylosis. Actually, it is an uncommon sequela, and the cause for this sporadic happening is unknown. Ankylosis does occur rather frequently after a traumatic injury to a tooth, particularly occlusal trauma, but it is also seen as a result of periapical inflammation subsequent to pulp infection. Periapical inflammation is a well-recognized cause of root resorption. Ankylosis sometimes also follows root canal therapy if the apical periodontal ligament is irritated or seriously damaged. Resorption and ankylosis is more common in replanted teeth.
Clinical Features
Ankylosis of the permanent tooth seldom manifests clinical symptoms unless there is a concomitant pulp infection which may be the underlying cause. If there is an extensive area of the root surface involved, the tooth may give a dull, muffled sound on percussion rather than the normal sharp sound. The fact that this condition exists may become apparent only at the time of extraction of the tooth, when considerable difficulty will be encountered, sometimes necessitating surgical removal.
Radiographic Features
If the area of ankylosis is of sufficient size, it may be visible on the radiograph. There is loss of the normal thin radiolucent line surrounding the root that represents the periodontal ligament, with a mild sclerosis of the bone and apparent blending of the bone with the tooth root.
Histologic Features
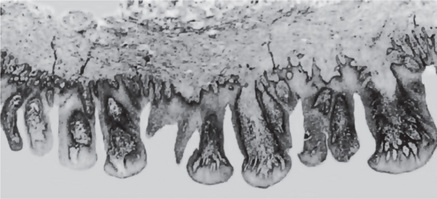
Microscopic examination reveals an area of root resorption which has been repaired by a calcified material, bone or cementum, which is continuous with the alveolar bone. The periodontal ligament is completely obliterated in the area of the ankylosis (Fig. 12-4).
Physical Injuries of the Bone
The most common physical injury involving the bone is fracture.
Fractures of Jaws
Fractures of the craniofacial complex occur commonly due to automobile, industrial, and sports accidents, and fights. Fracture can occur more easily in bones, which are already weakened by certain developmental and systemic disorders. Fracture may be simple, greenstick, compound, or comminuted. In simple fracture, the bone is broken completely; the overlying structures are intact and are not exposed to exterior. Greenstick fracture common in children is characterized by break of bone in one side and bend on the other side. In compound fractures external wound is associated with the break and is common in road traffic accidents. Bone is crushed or splintered in comminuted fractures and may or may not be exposed to the exterior.
Mandible is more prone for fractures, since chin is a prominent feature of the face. Fractures of the jaw are more common in males.
Fractures of the Maxilla
Maxillary fractures are more serious, than the mandibular fractures. Causes include road traffic accidents, blow, fall, and industrial accidents. Direction, force, and the location of the impact determine the extent of fracture.
Classification
Le Fort I or horizontal fracture, also known as floating fracture is characterized by separation of body of the maxilla from the base of the skull, below the level of zygomatic process.
Le Fort II or pyramidal fracture is characterized by vertical fractures through the facial aspects of the maxilla and extend upward to the nasal and ethmoid bones and usually extends through the maxillary sinus.
Le Fort III or transverse fracture is a high level fracture that extends across the orbits through the base of the nose and ethmoid region to the zygomatic arch. Bony orbit is fractured and the lateral rim is separated at the zygomaticofrontal suture. Zygomatic arch is fractured.
Displacement, anterior open bite, swollen face, reddish eye due to subconjunctival hemorrhage, and nasal hemorrhage are the common features. If the skull is involved, history of unconsciousness, cerebrospinal fluid rhinorrhea, cranial nerve involvement are characteristic.
Fractures of the Mandible
Most common causes of mandibular fractures are road traffic accidents and physical violence. Fractures of the mandible most commonly involve angle of the mandible, which is followed by condyle, molar region, mental region, and symphysis. Displacement of the mandible depends on the direction of the line of fracture, muscle pull, and the direction of force.
Traumatic Cyst: (Solitary bone cyst, hemorrhagic cyst, extravasation cyst, unicameral bone cyst, simple bone cyst, idiopathic bone cavity)
The traumatic cyst is a pseudo cyst (lacks an epithelial lining) and an uncommon lesion comprises about 1% of all jaw cysts. It occurs in other bones of the skeleton as well.
Etiology
The etiology of the solitary bone cyst is unknown, although a number of theories have been proposed and at least one, the trauma—hemorrhage theory has been rather widely accepted. Howe and also Sieverink have carried out extensive reviews of the literature and pointed out the wide acceptance of the theory of origin from intramedullary hemorrhage following traumatic injury. Hemorrhage occurring within the medullary spaces of bone after trauma heals in most cases by organization of the clot and eventual formation of connective tissue and new bone. According to the traumatic theory, the clot breaks down and leaves an empty cavity within the bone. Steady expansion of the lesion occurs secondary to altered or obstructed lymphatic or venous drainage. This expansion tends to cease when the cyst-like lesion reaches the cortical layer of bone, so that expansion of the involved bone is not a common finding in the solitary bone cyst.
It is not at all unusual; however, for the patient to be unable to recall any traumatic injury to the jaw. This may indicate that an injury so mild that the patient would not be aware of it or remember it, is sufficient to cause this lesion to develop. In the series reported by Howe, only slightly over 50% of the patients gave a history of trauma, the time lag between injury and discovery of the lesion varying from one month to 20 years.
Other theories of origin, reviewed by Whinery, have included:
• Cystic degeneration of primary bone tumors.
• A result of faulty calcium metabolism such as that induced by parathyroid disease.
• Ischemic necrosis of fatty marrow.
• The end result of a low-grade chronic infection.
• A result of osteoclasis resulting from a disturbed circulation caused by trauma creating an unequal balance of osteoclasis and repair of bone.
Clinical Features
The traumatic cyst occurs most frequently in young persons, the median age being 18 years in a series of 45 cases reviewed and reported by Gardner and Stoller. According to Howe, over 75% of cases occur in the second decade of life. There is no definite sex predilection although many series have shown the males being affected more commonly than females. Although it has been stated that the posterior portion of the mandible is more commonly involved than the anterior, numerous cases have been reported in the incisor region, since in the young person this area contains hemopoietic marrow. The maxilla has been known to develop the solitary bone cyst, but only on extremely rare occasions. In some cases enlargement of the mandible has been observed, but often the lesion is discovered during routine radiographic examination of the patient. In the majority of cases the pulps of the teeth in the involved area are vital, and this is important to ascertain, because the vital teeth should not be sacrificed. The presenting complaint may be swelling or rarely pain.
When the cavity is opened surgically, it is found to contain either a small amount of sero-sanguinous fluid, shreds of necrotic blood clot, fragments of fibrous connective tissue, or nothing. The dentist is frequently astonished to open into an empty space in bone and find that it has no clinically demonstrable membrane. It was reported by Toller in one case that the hydrostatic intracystic pressure was exceptionally low and comparable with capillary pressure, quite unlike that in other cysts of the jaw.
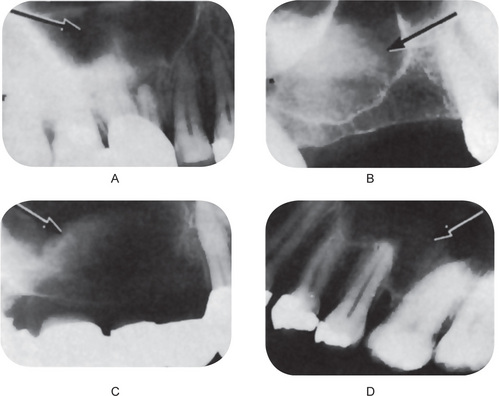
Radiographic Features
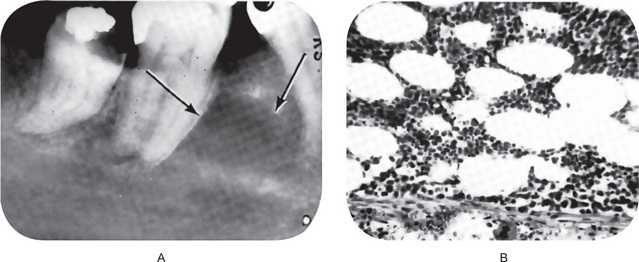
Radiographic examination usually reveals a rather smoothly outlined radiolucent area of variable size, sometimes with a thin sclerotic border, depending upon the duration of the lesion. Some traumatic cysts may measure only a centimeter in diameter (Fig. 12-5), whereas others may be so large that they involve most of the molar area of the body of the mandible as well as part of the ramus. When the radiolucency appears to involve the roots of the teeth, the cavity may have a lobulated or scalloped appearance extending between the roots of these teeth (Fig. 12-6). Seldom is there any displacement of teeth and, in many cases, the lamina dura appears intact. Rodrigues and Estrela reported a case of traumatic bone cyst in upper premolar-molar region, mimicking a large periapical lesion.
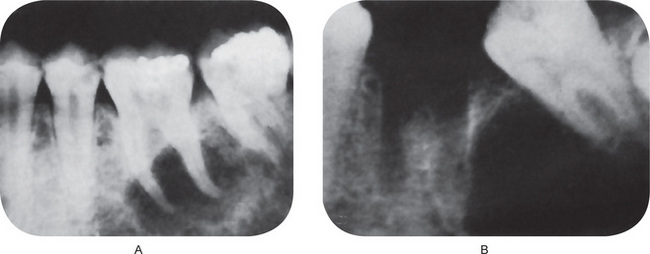
Figure 12-5 Traumatic bone cyst.
The radiolucent area in both cases was entirely empty and devoid of any lining. The molar teeth were vital.
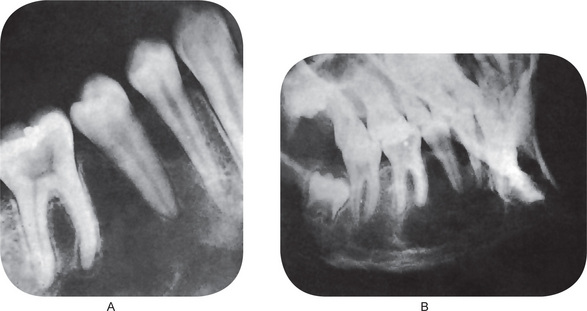
Figure 12-6 Traumatic bone cyst.
This large empty space in bone extended between the roots of the teeth. Periapical film (A) and lateral jaw film (B).
Care must be taken to differentiate the small solitary traumatic cyst occurring in the molar area and appearing as a round or ovoid radiolucent area associated with vital teeth from the lingual salivary gland depression of the mandible (q.v.) which has a similar radiographic appearance. However, the latter lesion is usually located below the mandibular canal, whereas the traumatic cyst usually lies above it.
Histologic Features
Histologic examination of the solitary bone cyst may reveal a thin connective tissue membrane lining the cavity, but no other significant features. Sometimes no such membrane is demonstrable. Waldron had the opportunity to study a solitary bone cyst in toto in a resected mandible. His case exhibited a thin connective tissue membrane and, in addition, an extensive osteophytic reaction on the outer surface of the cortical plate (Fig. 12-7). There may be presence of few red blood cells, blood pigments, or giant cells adhering to the bone surface.
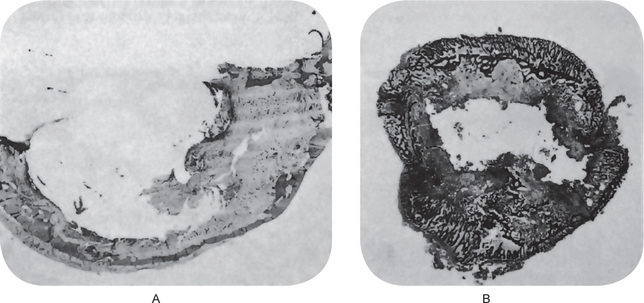
Figure 12-7 Traumatic bone cyst.
Traumatic cyst of mandible (A) and fibula (B). Only a thin shell of the cortical plates of the jaw remains with limited peripheral osteophyte reaction. The fibula shows a similar empty central cavity and thinning of the cortex, although osteophyte reaction is pronounced A, Courtesy of Dr Charles A Waldron and B, of Dr William C Sprague.
Treatment and Prognosis
Since the definitive diagnosis of the solitary bone cyst cannot be established without surgical exploration, the dentist usually opens into the cavity, attempts to enucleate a lining and, in the course of manipulation, reestablishes bleeding into the lesion. If the cavity is then closed, it has been found that healing and filling of the space by bone occur in most cases in 6–12 months. Seldom is a second surgical procedure necessary. If the space is a large one, bone chips have been used to aid in filling the defect with good results.
The extreme rarity of these lesions in older patients would suggest that not only may they be self-limiting, but at least some are capable of complete and spontaneous remission.
Focal Osteoporotic Bone-marrow Defect of the Jaw
The focal osteoporotic bone-marrow defect of the jaw is an uncommon lesion producing a focal radiolucency away from normal hematopoietic marrow. Hematopoietic marrow occurs normally in the jaws at the angle of the mandible, the maxillary tuberosity and occasionally other areas. It is well recognized that bone marrow may be stimulated in response to unusual demands for increased blood cell production and that this hyperplastic marrow may extend between adjacent trabeculae of bone, producing radiographically obvious osteoporosis and even thinning of the cortex. Other views regarding its pathogenesis include abnormal healing following tooth extraction since these lesions are most common in extracted sites, and persistence of remnants of fetal marrow.
Clinical Features
In the three reported series of cases, approximately 75% of the focal osteoporotic bone-marrow defects of the jaws occurred in women, and they involved the mandible in approximately 85% of the cases. In nearly every instance the lesions were asymptomatic and discovered only during routine radiographic examination.
Radiographic Features
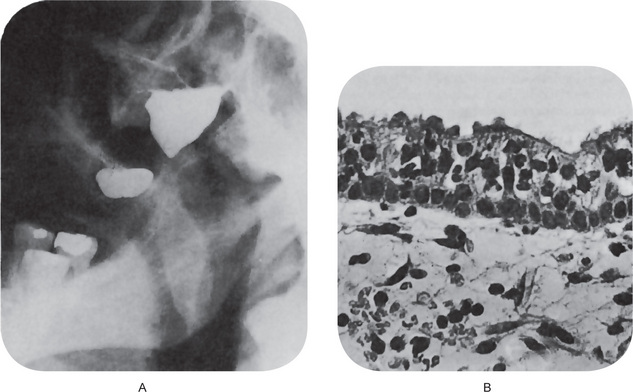
This lesion, which has a predilection for the mandibular molar area, generally appears as a radiolucency of variable size, a few millimeters to a centimeter or more, with a poorly defined periphery indicative of lack of reactivity of adjacent hone (Fig. 12-8A).
Histologic Features
The tissue removed from these defects consists of either normal red marrow, fatty marrow or a combination of the two (Fig. 12-8B). Megakaryocytes and small lymphoid aggregates may be present. The trabeculae of bone usually present in the sections are long, thin, irregular, and devoid of an osteoblastic layer.
Treatment
The radiographic appearance of these lesions is not sufficiently characteristic to permit diagnosis with certainty, and for this reason they must be investigated surgically to rule out osteomyelitis, traumatic bone cyst, and other odontogenic tumors. Once the diagnosis has been established, no additional treatment is necessary.
Surgical Ciliated Cyst of Maxilla: (Sinus mucocele)
The surgical ciliated cyst of the maxilla was originally reported by Gregory and Shafer. This cyst develops either after surgical entry into the maxillary sinus, usually a Caldwell-Luc operation or due to the obstruction of ostium. Basically, it is an implantation type of cyst in which epithelium of the maxillary sinus becomes entrapped along the line of surgical entry into the sinus and subsequently proliferates to form a true cystic cavity, anatomically separated from the sinus.
Clinical Features
The majority of patients with this type of lesion are middle-aged or older and present with a complaint of a nonspecific, poorly localized pain, tenderness, or discomfort in the maxilla. Extraoral or intraoral swelling is also frequently evident. Careful questioning of the patient usually reveals a history of some type of surgical procedure involving the maxilla and maxillary sinus, frequently 10–20 years previously. When content of the mucocele is infected, the lesion is called mucopyocele. Interestingly, it has been emphasized by Ohba and his associates among others that this lesion is more common in Japan than in America or Europe, possibly because of the higher incidence of maxillary sinusitis in Japan. Yamamoto and Takagi in their study involving 60 cases reported that postoperative maxillary cyst accounted for 19.5% of all oral cystic lesions.
Radiographic Features Radiographic examination shows a well-defined unilocular radiolucent area closely related to the maxillary sinus, often appearing to encroach upon the sinus but anatomically separate from it, as may be demonstrated by injection of the sinus with a radiopaque material. A filling defect of the cyst can then be seen (Fig. 12-9A).
Histologic Features
The surgical cyst is lined by pseudostratified ciliated columnar epithelium identical with that of the maxillary sinus (Fig. 12-9B). If infection or inflammation is present, squamous metaplasia may be found. The wall of the cyst is composed of fibrous connective tissue with or without inflammatory cell infiltration.
Effects of Orthodontic Tooth Movement
The science of orthodontics is based upon the ability of teeth to be moved through bone, without their subsequent extrusion or loss, by the application of pressure or tension under appropriate and controlled circumstances. Although the exact biologic mechanism responsible for this phenomenon is unknown, it is generally agreed that bone under pressure responds by resorbing, whereas the application of tension results in deposition of new bone. The periodontal ligament transfers the pressure or tension applied through orthodontic appliances.
Sandstedt applied force to the maxillary incisors of a dog, moving them lingually by means of a labial arch wire, and described the histologic findings of bone resorption, with numerous associated osteoclasts, on the pressure side of the teeth and formation of new bone on the tension side. He noted no tooth resorption, although necrosis or at least hyalinization of the periodontal ligament was found in the areas of pressure.
Tipping Movement
The exact movements which a tooth will undergo and the exact position it will assume after the application of orthodontic force will depend upon the degree and direction of the force and the position of the fulcrum around which the force acts. The general statement can be made, however, that pressure upon a tooth results in the resorption of bone in the direction of the application of force and compensatory new bone formation on the opposite side of the tooth, the tension side (Fig. 12-10).
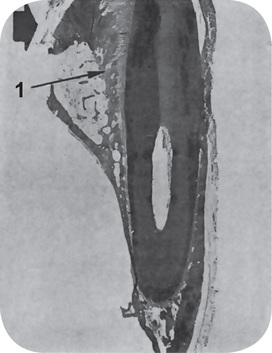
Figure 12-10 Tipping tooth movement.
Force was applied to this dog’s tooth in the direction of the arrow, and even at this magnification, widening of the periodontal ligament space (1) is noted.
The initial reaction on the pressure side is a compression of the periodontal ligament which, if excessive and prolonged, may result in ischemia with hyalinization and/or actual necrosis of tissue (Fig. 12-11B). On the opposite side under excessive force there may be actual tearing of the periodontal fibers and small capillaries with hemorrhage into the area. With reasonable forces, the periodontal ligament on the tension side of the tooth demonstrates stretching and widening of the periodontal space. Within a matter of hours or at the most a few days, large numbers of osteoclasts make their appearance along the surface of the bone under pressure, and resorption begins. This continues until the force of the pressure has been entirely dissipated.
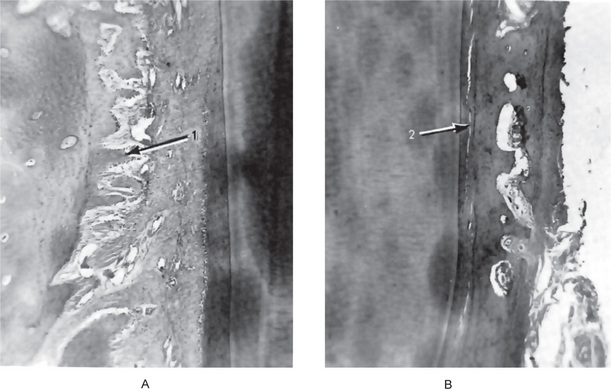
Figure 12-11 Tipping tooth movement.
There is widening of the periodontal ligament with formation of new spicules of bone (1) on the tension side of the tooth (A) and compression of the periodontal ligament (2) on the pressure side (B).
New trabeculae of bone on the tension side become evident early and appear as thin, elongated spicules arranged parallel to the periodontal fibers and confluent with them at their bony attachment (Fig. 12-11A). These spicules show evident osteoblastic activity along the sides and the end adjacent to the tooth, but usually there is intense osteoclastic activity at the ends of the spicules away from the tooth. As stabilization occurs, the alveolar bone gradually assumes its compact pattern that existed before movement occurred.
A secondary but most important occurrence is the deposition of new spicules of bone on the outer surface of the labial plate in instances of pressure in the labial direction. This serves to maintain the thickness of the already thin labial plate and prevent its perforation by the tooth. It is not entirely certain why resorption of even compact bone occurs before resorption of cementum and the tooth root. It is known that resorption of calcified tissues is favored by increased local vascularity, and the hypothesis has been advanced in explanation that the bone of the alveolus is in a more vascular environment than the cementum when orthodontic pressure is applied, particularly since ischemia of the periodontal ligament adjacent to the cementum is the usual situation.
It is generally recognized that the teeth of young persons respond much more rapidly and with less applied force to orthodontic movements than do the teeth of older adults. Although differences do exist in the chemical constitution of bone at varying ages, the difference in orthodontic response is probably due to variation in general tissue reactivity and local vascularity. Although bone retains the ability to undergo resorption throughout life, the degree of the stimulus needed to evoke this response shows dramatic differences between the various age groups.
Extrusive Movement
Extrusion of a tooth by an orthodontic appliance is similar to normal tooth eruption. The tissue changes induced by this form of movement consist apposition of new bone spicules at the alveolar crest and at the fundus of the alveolus arranged in a direction parallel to the direction of force. The direction of the spicules then is parallel to the long axis of the tooth and tends to increase the height of the alveolar crest. The normal width of the apical periodontal ligament is maintained by the new bony spicules here formed in the same direction. The relation between the tooth and the alveolus tends to remain constant.
Intrusive or Depressive Movement
The application of orthodontic force in such a manner as to cause depression of a tooth results in tissue changes that are the opposite of those found during extrusion, or elongation. In tooth depression, resorption of bone occurs at the apical area and around the alveolar margin. New bone formation is actually minimal.
Tissue Reactions during Retention Period
Discontinuance of the active phase of orthodontic force signals the beginning of alterations in the bone characteristic of the retention period. During this period there is gradual reformation of the normal dense pattern of the alveolar bone by apposition of bone around the bony spicules until they meet, fuse, and gradually remodel. The studies of Oppenbeim indicated that this reformation is slower around teeth held in position during the retention period by a retaining appliance as compared to teeth which remained free during this time. In any event, the final remodeling and the attainment of absolute bone-tooth equilibrium following orthodontic movements involve an extremely slow process, and a breakdown in this process is probably one of the most important contributing factors in cases of orthodontic failure due to relapse during the retention period.
Effect of Deciduous Tooth Movement upon Permanent Tooth Germs
Breitner and Tischler based on their study in young monkeys found that when a deciduous tooth was moved, the associated permanent tooth germ followed this movement.
Whenever a deciduous tooth was moved away from a tooth germ, the permanent tooth germ quickly followed. If a deciduous tooth was moved toward a permanent tooth germ, this germ moved in the same direction as the deciduous tooth.
These studies offered suggestive evidence that the form of the permanent dental arch may be modified by altering the deciduous arch through orthodontic treatment of the deciduous dentition.
Physical Injuries of Soft Tissues
Linea Alba
Linea Alba is a white line seen on the buccal mucosa extending from the commissures posteriorly at the level of the occlusal plane (Fig. 12-12). It is caused by the physical irritation and pressure exerted by the posterior teeth. It is usually bilateral and is more pronounced in persons who have clenching habit or bruxism. Histologically hyperkeratosis and intracellular edema of the epithelium is seen.
Toothbrush Trauma
This injury occurs to the gingiva and is produced by the toothbrush. It appears as white, reddish, or ulcerative lesions or linear superficial erosions, involving marginal and attached gingiva of maxillary canine and premolar region. They may be mistaken for vesiculobullous or infectious lesions if the history is not elicited properly. Severe form of toothbrush injury is characterized by clefting of the gingival margin and gingival recession. In more severe form there will be notching of the tooth and loss of alveolar bone. Presenting complaints are pain and burning sensation.
The above mentioned injury is caused by faulty brushing technique or rabid practice of cleanliness. But B Saravanan reported a case of penetrated injury of the buccal mucosa caused by toothbrush in middle-aged man due to a freak accident and reviewed literature with respect to such similar injuries (Fig. 12-13).

Figure 12-13 Penetrated injury caused by tooth brush. Courtesy to Dr B Saravanan, Tamilnadu Government Dental College, Chennai and Dr Devaki Saravanan, Meenakshi Ammal Dental College, Chennai.
Tooth pick injury is another form of factitial injury occurs as a result of overzealous oral hygiene practice. In contrast to toothbrush injury this involves the interdental gingiva.
Histologic Features
Microscopically there is focal ulceration with formation of granulation tissue with diffuse chronic inflammatory cell infiltration. Epithelium shows hyerkeratosis and acanthosis adjacent to the ulcers.
Treatment consists of medications to relieve the symptoms and teaching proper brushing technique.
Traumatic Ulcer: (Decubitus ulcer)
The traumatic ulcer of the oral mucous membranes is a lesion that is caused by some form of trauma. This may be an injury such as biting the mucosa, denture irritation, toothbrush injury, exposure of the mucous membrane to a sharp tooth or carious lesion, or it may be injury to the mucosa by some other external irritant.
The ‘cotton roll injury’, an iatrogenic injury, is a common reaction when the dry cotton roll placed by the dentist is roughly removed and the mucosa adhering to it is torn (Fig. 12-14). The traumatic ulcer often occurs in such sites as the lateral border of the tongue, usually after injury in which the patient severely bites the tongue (Figs. 12-15, 12-16). These ulcers are also seen, however, on the buccal mucosa, on the lips, and occasionally on the palate. Although in most instances of injury to the oral mucous membrane, healing is rapid and uneventful, occasional injuries persist for a long time without healing. This is particularly true in case of the traumatic ulcer of the tongue, which may bear considerable clinical resemblance to carcinoma and which sometimes is repeatedly biopsied in an attempt to establish a diagnosis of neoplasm. It is interesting; however, that many times the traumatic ulcer which has persisted for a matter of weeks or even months without healing will heal promptly after a minor surgical procedure such as an incisional biopsy.
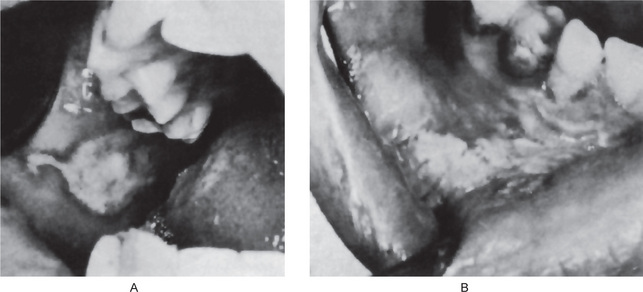
Figure 12-14 Iatrogenic injuries.
The lesion on the buccal mucosa (A) is a burn produced by a hand-piece used injudiciously by a dentist. The lesion in the mucobuccal fold (B) represents macerated mucosa torn by a cotton roll which had dried and adhered to the surface and was removed carelessly by a dentist A, Courtesy of Dr Stephen F Dachi.
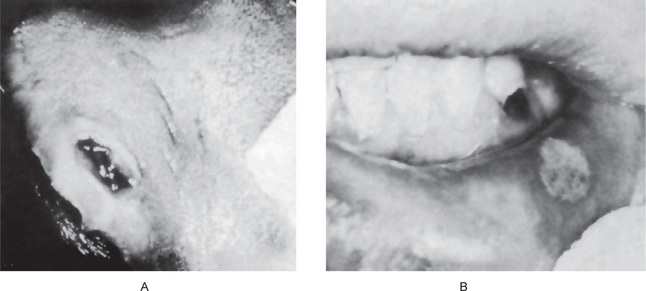
Figure 12-15 Traumatic ulcer.
The ulcer of the tongue (A) occurred during an epileptic seizure as a result of the patient’s biting himself. The ulcer of the lip (B) resulted from injury of the lip by rubbing against the large gingival carious lesion on the cuspid. The ulcer healed promptly after restoration of the carious lesion. A, Courtesy of Dr Stephen F Dachi.
Traumatic Ulcerative Granuloma with Stromal Eosinophilia: (Eosinophilic ulceration, traumatic granuloma)
The term traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) was suggested by Elzay in 1993 to delineate the eosinophilic ulcerations from more aggressive lesions, such as the eosinophilic granuloma of histiocytosis X. TUGSE is a reactive, benign, asymptomatic, self-limiting lesion of the oral mucosa. Cinically it may mimic squamous cell carcinoma at times. Its etiology remains obscure and may be associated with trauma. Although trauma might have an etiologic role, the pathogenesis of eosinophilic ulcer of the oral mucosa is probably T cell mediated as suggested by el-Mofty et al, who reported 38 cases of TUGSE. Trauma may be due to malposed teeth, or a partial denture. In infants the erupting teeth sometimes causes sublingual ulcerations and is referred to as Riga-Fede disease.
Riga-Fede disease occurs in infants between one week and one year of life. Lesions are usually observed on the anteroventral surface of the tongue, caused by contact with the erupting mandibular incisors. These associated teeth are usually natal or neonatal teeth.
Atypical eosinophilic ulcerations (atypical histiocytic granuloma) a rare lesion and exhibits sequential ulceration, necrosis, and self-regression. They are not associated with trauma and are believed to represent the oral counterpart of a T-cell cutaneous lymphoproliferative disorder.
Clinical Features
Eosinophilic ulcerations may occur at any age with a significant male predilection. Though common in anteroventral and dorsal surfaces of the tongue, these lesions may also be observed in other sites such as gingiva, palate, and mucobuccal fold. The ulcerations usually persist weeks to months and resemble traumatic ulcers. The center of the lesion is covered by a removable yellow fibropurulent membrane with erythematous borders.
Histologic Features
Eosinophilic ulcerations are similar to simple traumatic ulcerations in histologic pattern and are characterized by a dense and deeply infiltrative lymphoproliferation, showing epitheliotropism and massive eosinophilia. Presence of sheets of lymphocytes and histiocytes along with hyperplasia of the vascular connective tissue causes elevation of the surface ulceration.
Ulceration resulting from trauma permits the ingress of microorganisms, toxins, and foreign proteins into the connective tissue. These substances, in predisposed persons induce a severe inflammatory response resulting from an exaggerated mast cell-eosinophil reaction similar to that noticed in the pathogenesis of bronchial asthma. Degranulation of the mast cells leads to release of eosinophil chemotactic factor of anaphylaxis.
Treatment and Prognosis
Treatment of eosinophilic ulcerations is similar to simple traumatic ulcerations. Even large eosinophilic ulcerations heal rapidly after a biopsy. Though extraction of the involved teeth solves the problem in Riga-Fede disease, the teeth should be retained if they are stable.
Factitial Injuries
Factitial injuries are self-induced injuries. These may be habitual, accidental, or may have psychogenic background. As such, these overlap with a number of physical and chemical injuries to be discussed in this section.
Lip-biting and Cheek-biting
Also referred as morsicatio labiorum and morsicatio buccarum these injuries are habitual or psychogenic. It involves holding, biting, and tearing of the epithelium of the lip, buccal mucosa, or tongue, chewing of the cheek or stripping of the epithelium using fingers or creating negative pressure by sucking the lips and cheeks (Fig. 12-17). Most commonly seen in patients who are under psychologic stress.
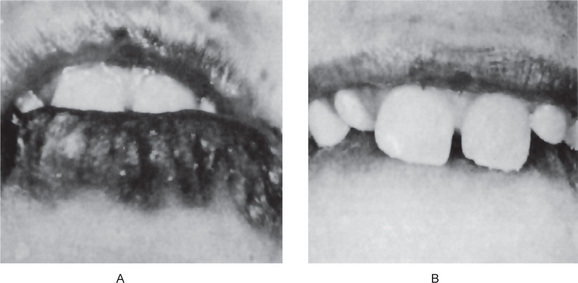
Figure 12-17 Factitial injury
Severe maceration of the lip had occurred as a result of a biting habit Courtesy of Dr Ralph E McDonald.
Gingiva may also be involved by factitial injury. This habitual gingival injury is inflicted by the patient using fingernails in which the patient presses the attached gingiva with his/her nails or force the free gingival margin apically.
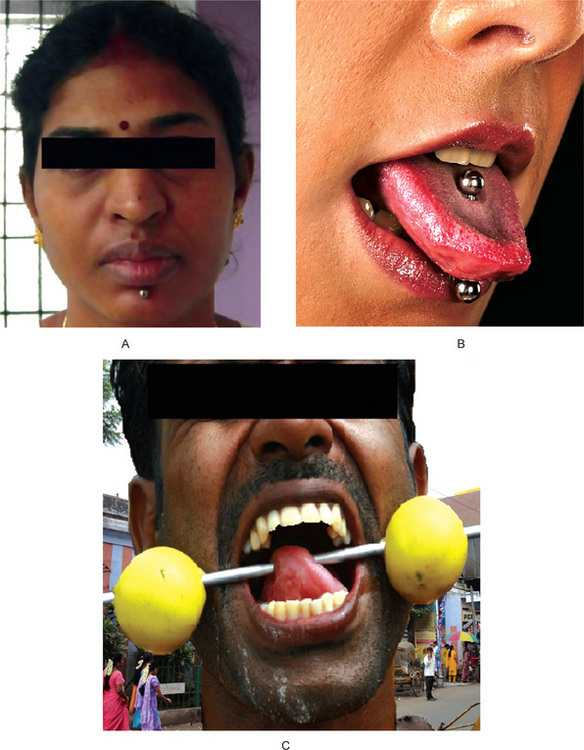
Clinical Features
The lesions are usually bilateral and seen along the occlusal line and also on the vestibular surface of the lips. The mucosa appears white and shredded, with areas of redness. Ulceration is common. This condition is more prevalent in females. Factitial gingival injury is characterized by vertical clefting in the free gingiva, exposure of the root, and gingival ulcers.
Denture Injuries
The oral mucosa is subject to a variety of injuries as a result of the wearing of artificial dentures. These may he manifested specifically as: (1) traumatic ulcer, (2) generalized inflammation, (3) inflammatory hyperplasia, (4) papillary hyperplasia of palate, and (5) denture base (acrylic or vulcanite) intolerance or allergy.
Traumatic Ulcer: (Sore spots)
The traumatic ulcer caused by denture irritation is the same type of ulcer that may be produced by a variety of other physical injuries.
Clinical Features
The denture ulcer, one or more, commonly develops within a day or two after the insertion of a new denture. This may be a result of overextension of the flanges, sequestration of spicules of bone under the denture or a roughened or ‘high’ spot on the fitting surface of the denture.
These ulcers are small, painful, irregularly shaped lesions usually covered by a delicate gray necrotic membrane and surrounded by an inflammatory halo. If treatment is not instituted, there sometimes may be beginning of proliferation of tissue around the periphery of the lesion on an inflammatory basis.
Histologic Features
The traumatic ulcer is a nonspecific ulcer and microscopically shows loss of continuity of surface epithelium with a fibrinous exudate covering the exposed connective tissue (Fig. 12-19). The epithelium bordering the ulcer usually demonstrates proliferative activity. There is infiltration of polymorphonuclear leukocytes in the connective tissue, particularly beneath the area of ulceration, although in chronic lesions these may be replaced by lymphocytes and plasma cells. Capillary dilatation and proliferation may also be evident. Fibroblastic activity is sometimes prominent, and macrophages may be present in moderate numbers.
The treatment for the traumatic denture ulcer consists in correction of the underlying cause: relief of the flange, removal of a tiny sequestrum, or relief of high spots. When this is accomplished, the ulcer usually heals promptly.
Generalized Inflammation: (Denture sore mouth, denture stomatitis)
The ‘denture sore mouth’ is an uncommon condition occurring in patients who may or may not have a new set of dentures. The condition is not due to a true allergy, since patch testing with the denture material gives negative results. Some cases appear to be due to an infection with Candida albicans, although the typical white patches of thrush (q.v.) do not usually develop, according to Calm and Bartels. Lehner has classified the condition as chronic atrophic candidiasis. Newton has suggested that denture sore mouth may be related to the ‘sweat retention syndrome’ in which keratin plug formation of the sweat glands or accessory salivary glands forces sweat or saliva into the adjacent tissues with subsequent inflammation. This concept has not been accepted widely, however Budtz-Jørgensen and Bertram demonstrated that yeast like fungi of C. albicans type could be cultivated from 90% of patients with denture stomatitis, but from only 40% of patients with dentures but without stomatitis. They also showed that poor denture cleanliness was associated with severe inflammation.
Renner and his associates emphasized that this condition is a multifaceted disease entity in which parasitism by C. albicans may be an extremely important factor often in association with other major contributions from denture trauma and continual denture wearing, poor oral hygiene habits and possibly dietary and systemic alterations.
Clinical Features
The mucosa beneath the denture becomes extremely red, swollen, smooth or granular and painful. Multiple pinpoint foci of hyperemia, usually involving the maxilla, frequently occur. A severe burning sensation is common. The redness of the mucosa is rather sharply outlined and restricted to the tissue actually in contact with the denture.
Treatment of this condition may not be successful. However, Budtz-Jørgensen and Bertram have reported significant therapeutic effects on denture stomatitis by antifungal therapy. Nystatin tablets 500,000 units, were allowed to dissolve in the mouth three times a day for 14 days. Bergendal and Isacsson reported similar results by treating denture stomatitis with nystatin powder placed on the fitting surface of the denture three times a day for 14 days. In addition, when the dentures fit poorly, construction of new appliances and instruction on hygienic care of the dentures aid in correcting the situation. If new dentures are not constructed, the old dentures must be sterilized daily by soaking in a nystatin solution overnight during the treatment period. Rebasing dentures with soft-tissue conditioners is also reported of benefit in addition to nystatin.
Inflammatory (Fibrous) Hyperplasia: (Denture injury tumor, euplis fissuratum, redundant tissue)
One of the most common tissue reactions to a chronically ill-fitting denture is the occurrence of hyperplasia of tissue along the denture borders. Such hyperplasia of oral mucosa is not restricted to this location but occurs in many areas where chronic irritation of any type exists, such as on the gingiva, buccal mucosa, and angle of the month.
Clinical Features
Inflammatory fibrous hyperplasia as a result of denture injury is characterized by the development of elongated rolls of tissue in the mucolabial or mucobuccal fold area into which the denture flange conveniently fits (Figs. 12-20, 12-21). This proliferation of tissue is usually slow in developing and probably is as much a result of the resorption of the alveolar ridge as of the trauma of the loose dentures.
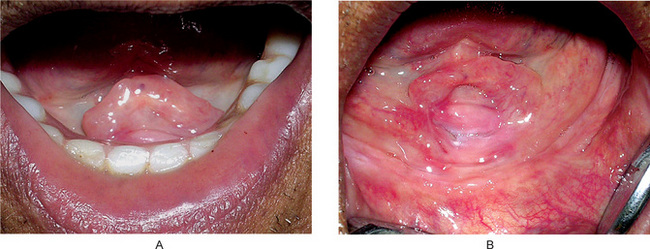
Figure 12-20 Inflammatory hyperplasia.
The redundant tissue forming at the border of the poorly fitting denture Courtesy of Drs Poonja LS, G Sriram, and Vaishali Natu, Nair Hospital Dental College, Mumbai.
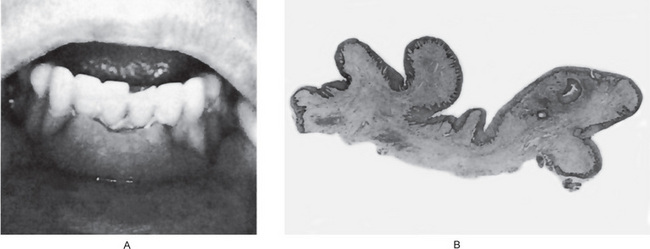
Figure 12-21 Inflammatory hyperplasia.
Some cases of redundant tissue exhibit extremely large rolls of fibrous tissue around the denture B, Courtesy of Dr Grant Van Huysen.
This excess fold of tissue is not usually highly inflamed clinically, although there may be irritation or even ulceration in the base of the fold into which the denture flange fits. The lesion is firm to palpation.
Histologic Features
The hyperplastic mass of tissue is composed of an excessive bulk of fibrous connective tissue covered by a layer of stratified squamous epithelium which may be of normal thickness or show acanthosis (Fig. 12-21). Pseudoepitheliomatous hyperplasia is often found. Hyper-keratosis is frequently present. The connective tissue is composed chiefly of coarse bundles of collagen fibers with few fibroblasts or blood vessels unless there is an active inflammatory reaction present. Such a reaction is frequently seen, however, in the base of the fissure adjoining the denture flange, especially if the tissue is superficially ulcerated.
One additional histologic finding often seen in the surface epithelium of inflammatory fibrous hyperplasia is mucopolysaccharide keratin dystrophy, also referred to as ‘plasma pooling’, first described by Toto. Its occurrence is not confined to inflammatory hyperplasia but may also be found in oral epithelium under a wide variety of other conditions, especially those involving irritated epithelium. This mucopolysaccharide keratin dystrophy consists histologically of homogeneous, eosinophilic pools of material in the superficial spinous layer of epithelium, where it appears to have replaced individual cells. Its significance is not known.
Treatment and Prognosis
Inflammatory fibrous hyper-plasia should he surgically excised, and either new dentures constructed or the old dentures rebased to provide adequate retention. If the denture is replaced or repaired, the lesion should not recur. Complete regression, even after construction of new dentures, will not occur, although subsidence of the inflammatory reaction may produce some clinical improvement of the condition.
Inflammatory Papillary Hyperplasia: (Palatal papillomatosis)
Papillary hyperplasia is an unusual condition involving the mucosa of the palate. It is of unknown etiology but may be considered a form of inflammatory hyperplasia associated in most instances with ill-fitting dentures, which permit frictional irritation and a poor state of oral hygiene. Often there is associated chronic hyperplastic candidiasis, which may be a contributing factor. Since many persons who have what might be described as poor-fitting dentures never acquire papillomatosis; however, there must be some as yet unidentified predisposing factors present in those persons who develop the lesion.
Clinical Features
Papillary hyperplasia occurs predominantly in edentulous patients with dentures, but is seen on rare occasions in patients with a full complement of teeth and no prosthetic appliance. In a series of 5,892 dental patients, Guernsey reported an incidence of 2.9% in denture wearers but only 0.2% in nondenture wearers. However, Bhaskar and his associates have stated that approximately 20% of all patients who wear dentures 24 hours a day show papillary hyperplasia, while among all denture wearers, the prevalence is 10%. Ettinger, studying the etiology and incidence of papillary hyperplasia, reported a similar occurrence of 97 affected patients, or 13.9%, in a series of 700 denture wearers. He concluded that constant wearing of the denture was one of the most important factors associated with the condition. When an appliance is present, the site of the lesion corresponds to the denture base, sometimes only to the relief chamber. It may arise at any age in the adult and has no definite sex predilection.
The lesion presents itself as numerous, closely arranged, red, edematous papillary projections, often involving nearly all of the hard palate and imparting to it a warty appearance. The lesions may extend onto the alveolar mucosa, and mandibular alveolar mucosa involvement occasionally occurs. The individual papillae are seldom over a millimeter or two in diameter. The tissue exhibits varying degrees of inflammation, but ulceration is rare (Fig. 12-22).

Figure 12-22 Papillary hyperplasia of palate in dentulous and edentulous patients.
The many small projections are confined to the palatal area and may be free of inflammation Courtesy of Dr Sujatha G, Department of Oral Pathology, and Dr Srinivasa Prasad T, Department of Oral and Maxillofacial Surgery, Meenakshi Ammal Dental College, Chennai.
Histologic Features
The microscopic section of papillomatosis shows numerous, small vertical projections each composed of parakeratotic or sometimes orthokeratotic stratified squamous epithelium and a central core of connective tissue (Fig. 12-23). Pseudoepitheliomatous hyperplasia, in varying degrees, is seen in the vast majority of cases; this is sometimes so severe as to be interpreted by the inexperienced pathologists as epidermoid carcinoma. However, most authorities now agree that true epithelial dysplasia and malignant transformation do not occur in palatal papillomatosis. Relatively severe inflammatory cell infiltration is nearly always present in the connective tissue, as is chronic sialadenitis in the accessory palatal glands. In the latter instance, metaplastic changes in acinar and ductal epithelium may mimic neoplastic transformation.
Treatment and Prognosis
There is no well recognized and accepted course of therapy for this condition. Discontinuing the use of the ill-fitting dentures or construction of new dentures without surgical removal of the excess tissue will generally result in regression of the edema and inflammation, but the papillary hyperplasia persists. Preferably, surgical excision of the lesion prior to new denture construction will return the mouth to a normal state. The use of a tissue conditioner to rebase an old denture often results in some improvement of the lesion, but seldom complete regression unless it is in an early stage.
Denture Base Intolerance or Allergy
Plasticizers of the soft liners are cytotoxic and affect many cellular metabolic reactions in vitro. Studies in animal exhibited significant epithelial changes. A true allergy to denture base material is extremely rare. Occasional cases have been reported, and studies have suggested that these were due to sensitivity to the monomer, both regular and self-curing types.
Mucous Retention Phenomenon: (Mucocele, mucous retention cyst)
The mucous retention phenomenon, which is generally conceded to be of traumatic origin, is a lesion involving salivary glands and their ducts.
Etiology and Pathogenesis
The mucous retention phenomenon is a common lesion. Many authorities formerly believed that this type of lesion resulted from obstruction of the duct of a minor or accessory salivary gland, but experimental investigations on mice by Bhaskar and his associates and on rats by Standish and Shafer failed to produce the mucous retention phenomenon by ligation of the submaxillary and sublingual gland ducts. The studies of Bhaskar and coworkers have shown instead that if the salivary duct was severed so that a continuous pooling of saliva occurred in the tissues, a well-demarcated cavity developed which was histologically identical with the natural mucocele.
These investigations appear to indicate that traumatic severance of a salivary duct, such as that produced by biting the lips or cheek or pinching the lip by extraction forceps, precedes the development of the retention phenomenon. It is also possible that a chronic partial obstruction of a salivary duct, in contrast to the acute total obstruction experimentally produced by ligation in mice and rats, may be of etiologic importance. Such a partial obstruction could result from a small piece of intraductal calculus or even from contraction of developing scar connective tissue around a duct after a traumatic injury. Occasional cases of calculus in the ducts of accessory salivary glands, or sialolithiasis (q.v.), have been reported, but are rather uncommon. Thus, mucoceles often have been classified as: (1) an extravasation mucocele, or (2) a retention mucocele (or true retention cyst). The extravasation type is far more common than the retention type.
Clinical Features
The retention phenomenon involving accessory salivary gland structures occurs most frequently on the lower lip, but may also occur on the palate, cheek, tongue (involving the glands of Blandin-Nuhn), and floor of the mouth. In the series of cases reported by Standish and Shafer, nearly 45% of the 97 mucoceles occurred on the lower lip. No cases were found in their series on the upper lip. In addition, there was no predilection for any age group, the lesions being rather equally divided among all decades of life, from lesions present at birth to the ninth decade. An equal distribution in occurrence between males and females was also noted in their study. In a study of 125 cases of mucocele, Robinson and Hjørting-Hansen reported similar findings except for the age predilection. They found that nearly 65% of their cases occurred within the first three decades of life. Ramanathan and his coworkers, in their series of 250 cases of mucoceles, found that nearly 85% occurred in the same time span.
Clinically, the lesion may lie fairly deep in the tissue or be exceptionally superficial and depending upon the location, will present a variable clinical appearance (Fig. 12-24). The superficial lesion appears as a raised, circumscribed vesicle, several millimeters to a centimeter or more in diameter, with a bluish, translucent cast. The deeper lesion is manifested also as a swelling but because of the thickness of the overlying tissue, the color and surface appearance are those of normal mucosa.

Figure 12-24 Retention cyst.
The typical lesion appears as a small vesicle on the lip (A) and floor of the mouth (B). Courtesy of Dr Spencer Lilly D, Meenakshi Ammal Dental College, Chennai.
It is interesting and significant that the mucous retention phenomenon is restricted almost entirely to the lower lip, seldom found on the upper lip, while accessory salivary gland neoplasms of the lips are almost universally found on the upper lip and only rarely on the lower lip. This could imply that trauma plays no role in the development of salivary gland tumors in this location.
The mucous retention phenomenon often arises within a few days, reaches a certain size and may persist as such for months unless treated. If the contents of the cyst are liberated, they usually are found to consist of a thick, mucinous material. Some lesions regress and enlarge periodically and may disappear after traumatic injury which results in their evacuation. They almost invariably recur, however.
Histologic Features
The majority of mucoceles, being of the extravasation type, consist of a circumscribed cavity in the connective tissue and submucosa, producing an obvious elevation of the mucosa with thinning of the epithelium as though it were stretched (Fig. 12-25). The cavity itself is not lined by epithelium and is, therefore, not a true cyst. Instead, its wall is made up of a lining of compressed fibrous connective tissue and fibroblasts. Sometimes these cells may be mistaken for flattened epithelial cells. Not uncommonly the connective tissue wall is essentially granulation tissue, but in any event it usually shows infiltration by abundant numbers of polymorphonuclear leukocytes, lymphocytes, and plasma cells. The lumen of the cyst like cavity is filled with an eosinophilic coagulum containing variable numbers of cells, chiefly leukocytes and mononuclear phagocytes.
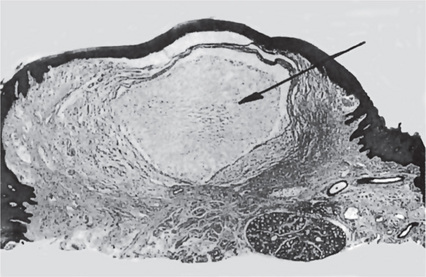
Figure 12-25 Mucous retention phenomenon.
The photomicrograph shows the circumscribed lesion containing mucoid material.
Occasional mucoceles demonstrate an intact, flattened epithelial lining. It is probable that this simply represents the portion of the excretory duct bordering the line of severance, if severance is actually the manner in which these lesions develop. The flattened epithelial lining has been referred to as epithelium of the ‘feeder duct’. In other instances, the epithelium-lined mucocele represents a lesion of the retention type.
The salivary gland, acini which lie adjacent to the area of the mucocele and are associated with the involved duct often show alterations. These may consist of interstitial inflammation or sialadenitis, dilatation of intralobular and interlobular ducts with collection of mucus, and breakdown of individual acinar mucous cells resulting in the formation of tiny areas of pooled mucus.
Treatment and Prognosis
Treatment of the mucous retention phenomenon is excision. If the lesion is simply incised, its contents will be evacuated, but it will be rapidly filled again as soon as the incision heals. There is occasional recurrence after excision, but this possibility is less likely if the associated salivary gland acini are removed also.
Ranula
The ranula is a form of mucocele but larger, which specifically occurs in the floor of the mouth in association with the ducts of the submaxillary or sublingual gland. The etiology and pathogenesis appear to be essentially the same as for the mucous retention phenomenon involving accessory glands, although some workers believe that it may arise through duct blockage or through the development of a ductal aneurysm.
Clinical Features
This lesion, which is rare compared to the usual mucocele, develops as a slowly enlarging painless mass on one side of the floor of the mouth (Fig. 12-26).The tongue may be elevated and when it is large it may hide the salivary gland. Since the lesion is usually a deep-seated one, the overlying mucosa is normal in appearance. If the lesion is superficial, the mucosa may have a translucent bluish color. A rare, plunging, suprahyoid type which has herniated through the mylohyoid muscle is also described. A thorough review of the literature on the plunging or cervical ranula has been reported by van den Akker and his associates, who also described four typical cases.
Histologic Features
The microscopic appearance is similar to that of the smaller mucocele except that a definite epithelial lining is sometimes present. Because of this finding, most investigators consider the ranula to be a true retention cyst, probably occurring as a partial blockade phenomenon, although a salivary duct stone is often not demonstrable.
Retention Cyst of Maxillary Sinus: (Secretory cyst of maxillary antrum, mucocele of maxillary sinus, mucosal cyst of maxillary sinus)
The retention cyst of the maxillary sinus is an uncommon variant of the mucous retention phenomenon most frequently encountered as an incidental finding in dental radiographs. It should be recognized; however because of the possibility of confusing it with a variety of other lesions occurring in the same location.
This lesion appears to represent a retention phenomenon of the mucous glands associated with the lining of the maxillary sinus. The cause of development of the cyst-like lesion is unknown, although traumatic injury associated with tooth extraction may be of etiologic significance. In some cases; however, the lesion develops in dentulous areas with no history of a surgical procedure. Other suggested causative factors include sinusitis, allergy and sinus infection, but these are without firm support.
Clinical Features
Most retention cysts of the maxillary sinus are completely asymptomatic and are discovered only during routine radiographic examination of the jaws. Occasionally, discomfort in the cheek or maxilla may be present. Pain and soreness of the face and teeth and numbness of the upper lip were described by Wright in about 10% of his series of 78 cases. Buccal expansion of the maxillary antrum has also been reported. There is no clear-cut age or sex predilection for occurrence of the lesion. Additional series of cases have been reported by Casamassimo and Lilly (73 cases in 4,546 patients, or 1.6%), Myall and his coworkers (73 cases in 1,469 patients, or 5.1%), and Halstead (45 cases in 2,325 patients, or 1.9%).
Radiographic Features
In the dental periapical radiograph, the lesion appears as a well-defined, homogeneous, dome-shaped or hemispheric radiopacity, varying in size from a tiny lesion to one completely filling the antrum, arising from the floor of the antrum and superimposed on it (Fig. 12-27). This radiopacity appears as a soft tissue mass rather than a calcified area, so that medial and lateral landmarks can generally be visualized through the lesion. In some instances the lesion appears more radiolucent than radiopaque. In the various reported series, between 10 and 20% of the cases have occurred bilaterally.
Histologic Features
Some of these retention cysts are analogous to the mucous retention phenomenon in as much as they consist of the accumulation of fluid within connective tissue spaces and have no definite lining. This type has sometimes been referred to as a non-secretory cyst. In other instances the lesion may be lined by a respiratory type of epithelium, and this has sometimes been described as the secretory type of antral cyst. In either case inflammatory cell infiltration in the connective tissue wall of the specimen is common.
Treatment
The majority of these cysts either persist unchanged or disappear spontaneously within a relatively short period, and for this reason it has been suggested that no treatment is necessary.
Differential Diagnosis
Care must he taken to differentiate this lesion from apical periodontal cysts of teeth in close association with the maxillary sinus, from fibro-osteomas of this area, and especially from the surgical ciliated cyst of the maxilla. Although etiologically different from the last lesion, the antral mucocele may be related to it pathogenetically.
Sialolithiasis: (Salivary duct stone, salivary duct calculus)
A stone in the salivary ducts or glands is called sialolithiasis. They are formed by deposition of calcium salts around a central nidus which may consist of altered salivary mucins, desquamated epithelial cells, bacteria, foreign bodies, or products of bacterial decomposition. It is the most common cause of salivary gland obstruction. The etiology is unclear and it can be complete or partial and may show recurrence.
Clinical Features
Many patients with sialolithiasis involving a duct of a major salivary gland complain of moderately severe pain, particularly just before, during and after meals, owing to psychic stimulation of salivary flow, associated with swelling of the salivary gland. The occlusion of the duct prevents the free flow of saliva, and this stagnation or accumulation of saliva under pressure produces the pain and swelling. In some instances this swelling is diffused and simulates a cellulitis. Occasionally the stone presents no remarkable symptoms, and the only evidence may be a firm mass palpable in the duct or gland. In some cases large numbers of individual small stones may be found occluding the duct system.
Stones, particularly in the more peripheral portion of the duct, may often be palpated if they are of sufficient size. They may also be demonstrated on the dental radiograph when appropriately located, particularly by the use of sialography (Fig. 12-28A). However 20% of the parotid and 40% of the submandibular stones are not radiopaque. Sialography is the retrograde injection of a radiopaque material into the duct system of a salivary gland and the study of its distribution by radiographs.
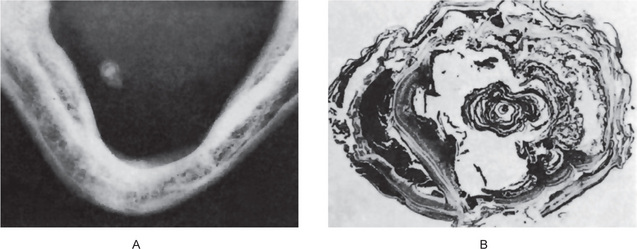
Figure 12-28 Sialolithiasis.
(A) A piece of calculus in the submandibular gland duct is shown in the occlusal radiograph. (B) The laminated structure of the stone is obvious in the photomicrograph.
Sialolithiasis may occur at any age, but is most common in middle-aged adults. Wakely reported that the occurrence of sialolithiasis in a large group of cases shows the following distribution: submandibular gland and duct, 64%; parotid gland and duct, 20%; and sublingual gland and duct, 16%. In a series of 180 cases reported by Levy and his associates, the gland distribution was 80%, 19%, and 1%, respectively. The common involvement of the submandibular gland and duct is thought to be due to the tenacity of the submandibular saliva, which, because of its high mucin content, adheres to any foreign particle. The submandibular duct is also long and irregular in its course.
Sialolithiasis involving ducts of the minor or intraoral accessory salivary glands sometimes is also seen. The majority of these sialoliths are found in the upper lip, with only slightly fewer in the buccal mucosa, together accounting for nearly 90% of all cases. Occasional cases are reported in the buccal sulcus, lower lip, palate, and tongue. They usually present as solitary, firm, freely movable, small masses or nodules, and may or may not be symptomatic.
Chemical and Physical Features
The sialolith may be round, ovoid, or elongated. It may measure just a few millimeters or 2 cm or more in diameter. The involved duct may contain a single stone or many stones. The surface of the calculi is rough, which may cause the duct lining to undergo squamous metaplasia. They are usually yellow and occasionally white or yellowish-brown in colour. It consists mainly of calcium phosphates and smaller amounts of calcium carbonates, organic materials, and water. Submandibular stones tend to be larger than those of the parotid or other minor glands.
Histologic Features
Microscopically the calcified mass exhibits concentric laminations (Fig 12-28B) around a central nidus of amorphous debris. The lamellated structure of the calculi is the result of successive deposition of inorganic and organic material. Periductal inflammation is also seen. The ductal obstruction frequently is associated with an acute or chronic sialadenitis of the feeding gland.
Treatment and Prognosis
Small calculi may sometimes be removed by manipulation or increasing the salivation by sucking a lemon, leading to expulsion of the stone. An intravenous antibiotic is given for bacterial infection due to persistent obstruction of the duct. The larger stones almost always require surgical removal. If they are present near or in the substance of the gland itself, particularly if multiple, surgical extirpation of the gland may be necessary. Piezoelectric shock wave lithotropsy may be an alternative to surgical removal. The solitary sialolith does not usually recur, although occasional cases have presented chronic multiple recurrences.
Maxillary Antrolithiasis: (Antral rhinolith)
Maxillary antrolithiasis is a relatively rare condition which is defined as a complete or partial calcific encrustation of an antral foreign body, either endogenous or exogenous, which serves as a nidus. An endogenous nidus may consist of a dental structure such as a root tip or may simply be a fragment of soft tissue, bone, blood, or mucus. Exogenous nidi are uncommon, but may consist of such materials as snuff paper.
Clinical Features
The antrolith may occur at any age in either sex. There may be a complete absence of symptoms, although some cases are marked by pain, sinusitis, nasal obstruction, and/or foul discharge, and epistaxis. Some cases, according to Blaschke and Brady, are discovered accidentally during radiographic examination in which an opaque mass is evident in the sinus. At times Aspergillus species served as a central fungus nidus associated with long-standing sinusitis, and poor sinus drainage resulting in the formation of a sinus stone.
Rhinolithiasis
Rhinoliths are calcareous concretions occurring in the nasal cavity. This uncommon lesion is formed by calcification of intranasal endogenous or exogenous foreign material. Although nasal foreign bodies are more frequently seen in children, they have been reported in patients of all ages. Rhinolith may be present for years and frequently gives rise to odorous discharge, symptoms of nasal obstruction, sinusitis, epiphora, as well as pain and epistaxis. At least one case of an antrorhinolith, a ‘stone’ partially in the nasal passage and partially in the antrum, has also been reported. Pinto et al, reported a case of rhinolith in a 54-year-old woman causing palatal perforation.
Radiation Injuries
The general term ‘radiation’ is applied to two different forms of energy: (1) that derived from electromagnetic radiation, and (2) that derived from particle radiation. Electromagnetic radiation consists of a continuous spectrum of varying wavelengths ranging from long electrical and radiowaves down through infra-red, visible light, ultraviolet light, X-rays and gamma rays. Particle radiation is generated through spontaneous decay of various natural and artificial radioactive materials; Particles may also be generated by accelerating deuterons, electrons, and so forth, in devices such as the cyclotron and betatron.
Certain natural radioactive elements such as radium and thorium give off radiant energy spontaneously in their decay process. A portion of this is electromagnetic or gamma (γ) rays, but most of the radiation consists of alpha (α) and beta (β) particles. Alpha particles, which are helium nuclei in rapid motion, have little ability to penetrate tissues and thus give up their energy in a very short distance. Beta particles, which are negatively charged electrons in rapid motion, have a greater penetrating power than alpha particles, but lose their energy in a few millimeters of tissue. Alpha and beta particles actually have little use in medical therapy and are important chiefly as hazards. Radioactive isotopes of most of the known elements have been prepared. The half-life of these isotopes ranges from a fraction of a second to centuries. The majority of the isotopes produce only beta radiation, although some produce alpha particles and gamma rays. In recent years many of these radioactive isotopes have found use in medicine as tracer substances, therapeutic agents and diagnostic agents, as well as in many areas of research.
These different types of radiant energy or radiation are sometimes spoken of as ‘ionizing radiation’. This term refers to rays which carry enough energy to produce ionization in materials which absorb them, including living tissues.
Radiation injuries are caused by ionizing effects of energized particles on cells. In the process of radiation therapy, which is commonly used in the treatment of head and neck malignancies, normal tissues in and around the field of radiation is also damaged to certain extent.
General Effects of Radiation on Tissue
The exact means by which radiation exerts its effect on cells and tissues is unknown. Most investigators believe that it is related to the mechanism of ionization, localized injuries being produced in single cells. The cellular injury has been postulated to be due to a number of possible factors. These include:
• Toxic effect of protein breakdown products
• Inactivation of enzyme systems
There is great variation in the radio-sensitivity of different types of living cells despite the fact that it is possible to kill any living thing with sufficiently large doses of radiation (Table 12-1). In general, embryonic, immature or poorly differentiated cells are more easily injured than differentiated cells of the same type. Once these cells are injured, however, they usually show greater recovery properties, although there are many exceptions to this rule. Significantly, all cells show increased vulnerability to radiation injury at the time of mitotic division. Furthermore, if cells are irradiated during the resting phase, mitosis is delayed or inhibited.
Latent tissue injury is one of the most unusual phenomena related to X-ray or gamma radiation and refers to residual tissue damage after the initial radiation reaction has subsided. Although frequently no residual injury can be detected by ordinary means, the tissues will retain for years an increased susceptibility to injury if again radiated. Furthermore, repeated exposure to small doses of radiation, no one of which is sufficient to evoke a perceptible reaction, may in the aggregate produce serious latent damage. Thus the biologic effects of radiation are cumulative, but show incomplete summation.
Effects of Radiation on Oral and Paraoral Tissues
Radiation effects are dependent upon a great number of factors such as the source of the radiation, the total amount of radiation administered, the period of time over which the radiation was administered (fractionation), the type of filtration used and the total area of tissue irradiated. The changes to be described here are those frequently seen after delivery of local therapeutic doses of X-ray radiation in the treatment of neoplasms about the head and neck. They are in no way related to the use of the diagnostic X-ray machine. No attempt will be made to describe the effect of total body radiation, such as those occurring after detonation of the various nuclear bombs, because of the lack of significant clinical application of such information.
However, adult patients with acute leukemia in relapse, whose disease has become refractory to all known chemo-therapeutic drugs, may receive bone marrow transplantation following total body radiation in an attempt to prolong their lives. The oral changes in 35 patients following 850–950 rads of total body X-ray radiation were detailed by Dreizen and his associates in 1979. Almost every patient exhibited bilateral parotitis, partial xerostomia, and oral mucositis following total body radiation. The parotitis resembled mumps that resolved spontaneously in 24–48 hours. Saliva production during the first week after radiation was noticeably reduced in amount and was thicker, ropier, and more mucoid than usual. The mucositis, which lasted two to three weeks, began as swelling, soreness, and whitening of the oral mucosa. Within 48–72 hours, the lips, tongue, and/or entire oral cavity showed an intense reddening of the oral mucosa. Pain and denudation accompanied the mucositis. After two or three weeks there was a whitening of the oral mucosa, which has been attributed to impaired mitotic activity and prolonged retention of the superficial epithelial cells, leading to an abnormally high degree of keratinization. Palliation of the transient radiation mucositis was achieved with warm salt water or sodium bicarbonate mouthrinses.
Evidence is accumulating that cobalt-60 radiation therapy, as contrasted with conventional orthovoltage radiation, may have significant skin- and bone-sparing qualities. Thus, this technique may reduce the incidence of radiation complications so frequently seen in the past.
Effects on Skin
The effects of heavy therapeutic doses of X-ray radiation on the skin are well documented, although variable among patients. Erythema is the earliest visible reaction and begins within a few days after irradiation. The original erythema fades quickly, only to reappear within two to four weeks. The secondary erythema fades slowly; often leaving the skin permanently pigmented a light tan shade. After heavy irradiation the secondary erythema may be accompanied by edema with desquamation of epithelial cells resulting in denudation of the surface. Re-epithelialization occurs in 10–14 days. These early effects are caused by direct injury of the radiated cells and tissues, while the later effects are brought about chiefly by changes in the vascular bed and in the intercellular material.
Alterations in the sebaceous gland activity, evidenced by a reduction in secretion with dryness of the skin, may occur within a week after the beginning of irradiation. The hair follicles are also sensitive to this type of radiation, and epilation, either temporary or permanent, may be produced. The sweat glands are similarly disturbed so that their absence of secretion contributes to the dryness and scaling of the skin.
Eventually the epithelium becomes thin and atrophic, and the superficial blood vessels become telangiectatic or occluded. The telangiectasia may persist for months or even years as evidence of the effect of X-rays. Other evidence of vascular damage includes thickening of the intima and, in some cases, thrombosis. Some veins and arteries show subintimal fibrosis with thickening of the wall at the expense of the lumen. Endophlebitis and phlebosclerosis may be particularly evident.
Effects on Oral Mucosa
The changes occurring in the oral mucosa after X-ray radiation are essentially the same as those in the skin and are related to the dose and the duration of therapy. The erythema may develop at a somewhat lower dose of X-ray, and the mucositis which occurs after therapeutic radiation is evoked somewhat earlier than the analogous dermatitis (Fig. 12-29).
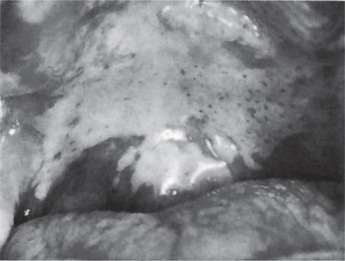
Figure 12-29 Radiation mucositis of palate.
The seven-day postradiation reaction consisted of a yellowish-white necrotic exudate, which disappeared within an additional 14 days.
Dreizen and his coworkers studied the effects of radiotherapy for oral cancer on the oral mucosa. They found that the mucosa in the path of radiation first appeared hyperemic and edematous. As treatment continued, the mucosa became denuded, ulcerated, and covered with a fibrinous exudate. Great discomfort, which was intensified by contact with coarse or highly seasoned foods, was commonly present. The mucositis persisted throughout radiotherapy and for several weeks thereafter. Unless secondary infection occurred, spontaneous remission followed termination of the radiation therapy. In many patients, a lidocaine mouthrinse before mealtimes was necessary to produce topical anesthesia so that eating was possible. When pain and dysphasia could not be controlled with local anesthetics and analgesics, nasogastric tube feeding was necessary.
Patients undergoing radiotherapy for oral cancer also quickly lost their sense of taste, probably because of damage to the microvilli and outer surface of the taste cells. The effect was usually transitory, and taste acuity was restored within 60–120 days after completion of the radiotherapy.
Effects on Salivary Glands
Xerostomia, or dryness of the mouth, is one of the earliest and most universal of complaints of patients receiving therapeutic radiation about the head and neck. Alterations in the salivary glands, characterized by diminution or even complete loss of secretion, may occur within a week or two after the beginning of radiation. It is interesting that the morphologic changes do not particularly mirror the physiologic changes which occur. There is some obvious damage of the acinar cells, chiefly a decrease in the number of secretory granules present, with congestion, edema, and inflammatory cell infiltration of the interstitial connective tissue. There are no remarkable changes in the ducts of the salivary glands.
One interesting feature of acute post radiation sialadenitis is the elevation of serum and urinary amylase, the source of this amylase being the salivary glands. This is one of the few biochemical changes that occur early and consistently following irradiation. Kashima and his associates have discussed this finding, as well as other clinical and histopathologic features of post radiation sialadenitis, concluding that direct exposure of the salivary glands is necessary to provoke this change and that the serum amylase response is related to the dose of irradiation.
The loss of secretion may be a permanent sequelae of the radiation, or there may be a gradual return of salivation, usually only after many months.
Effects on Teeth
Erupted teeth are often affected in patients who have received X-ray radiation about the head and neck, but the damage may not appear for several years after the radiation. The most common manifestation of the injury is a peculiar destruction of tooth substance, resembling dental caries and sometimes called ‘radiation caries’, which often begins at the cervical area of the teeth. The lesion resembles a demineralization more than it does true caries because of its pattern or the manner in which it sweeps across the tooth, sometimes causing amputation of the tooth crown at its neck. Teeth often seem brittle, and pieces of the enamel may fracture away from the tooth (Fig. 12-30).
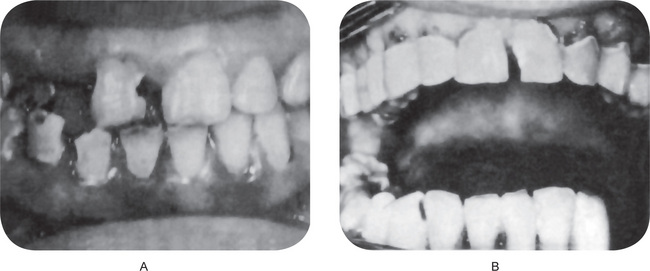
Figure 12-30 Radiation caries.
(A) The salivary glands on the side showing the caries were radiated during the course of treatment of an intraoral neoplasm; the radiation produced a xerostomia on that side and the ultimate caries. (B) The typical destruction of tooth substance at the cervical margins of the teeth is well illustrated. B, Courtesy of Dr Charles A Waldron.
The primary cause of the condition lies in alterations of the saliva induced by either direct or indirect radiation of the salivary glands. Although physical and chemical changes in the saliva following salivary gland irradiation have been postulated, there is no evidence for such changes other than the direct observation that the saliva often becomes somewhat thicker and more tenacious after irradiation. The xerostomia of varying degrees certainly favors the collection of debris on the teeth and ensuing caries. Radiation induced xerostomia in humans produced pronounced shifts in the oral microbial population, with cariogenic microorganisms gaining prominence at the expense of noncariogenic ones. These changes occurred prior to the onset of clinical caries and were irrespective of the use of a topical fluoride gel as a caries preventive measure.
Close cooperation between the radiotherapist, the dentist, and the patient is essential in promoting oral care for these patients. As Dreizen and his associates pointed out, xerostomia also deprives the teeth of an important natural defense against dental decay. There is a sharp decrease in the total daily output of caries-protective salivary electrolytes and immunoproteins. Patients with xerostomia change their eating habits to include frequent, nondetergent, and high carbohydrate meals. The microbial, chemical, immunologic, and dietary changes produce an enormous increase in the caries challenge.
Regardless of the patient’s previous caries history, the development of xerostomia is inevitably followed by rampant dental decay unless stringent protective steps are taken. Cariogenesis is so greatly accelerated that frank lesions may appear within three months after radiotherapy. However, the ravages of dental decay in the radiated patient can be almost completely prevented with one daily application of a 1% sodium fluoride gel containing a red, plaque-disclosing dye. This protocol was developed by Daly and Drane in 1972. The gel is applied for at least five minutes by means of custom fabricated flexible plastic carriers. When the carriers are removed and the gel is rinsed off, the plaque is stained red and can be removed by brushing and flossing. To be maximally effective, the program must be instituted at the beginning of radiotherapy and continued every day. Such a regimen can also arrest caries caused by xerostomia in previously unprotected patients. Because of the ever-present risk of caries in xerostomic patients, only diligent, lifelong cooperation will assure prevention.
Developing teeth are also particularly sensitive to X-ray radiation. Leist and Smith demonstrated that irradiation of developing teeth in rats resulted in a disorganization of the odontoblasts and the formation of atypical dentin. Ameloblasts appear to be considerably more resistant to radiation than odontoblasts, although Burstone demonstrated in mice that, after sufficient radiation there was cessation of ameloblastic histogenesis and metaplasia of ameloblasts to a less differentiated type of cell. Similar interference with tooth formation in rats has been reported by English and his coworkers.
Radiation of developing teeth in human beings sometimes occurs, and if it is at a sufficiently young age, manifestations of the injury may be obvious. Such radiation is usually administered for the treatment of a tumor about the head and neck, frequently a hemangioma. Depending upon the age of the patient at the time of the irradiation, there may be complete cessation of odontogenesis resulting in anodontia in the involved area or simply a stunting of the teeth (Fig. 12-31) have been cited by Carl and Wood.
Effects on Bone
Bone itself is relatively resistant to X-ray radiation, although osteoblasts are sensitive. If the radiation has been sufficiently intense, the normal balance between bone formation and bone resorption is disturbed; general bone vitality is decreased, and localized osteoporosis may result.
The greatest clinical significance of bone which has been irradiated lies in the inability of this bone to react in the normal fashion to infection. This is related, at least in part, to the damage of the vascular bed with subsequent disturbance of the typical inflammatory response. There is little actual danger to the patient except in a situation in which infection may enter the bone with little difficulty and spread widely. This may occur in the maxilla and mandible.
An experimental study of the effects of radiation on extraction wound healing in rats has been reported by Stein and coworkers. They found that when radiation shortly followed tooth extraction, there was retardation of surface closure of the wound, leaving an open pathway for tissue infection. The healing response was poor and slow. As the interval between tooth extraction and radiation was increased, impairment of healing decreased. In general, the longer the interval between tooth extraction and initiation of radiation, the less possibility is there of healing complications.
Osteoradionecrosis
This pathologic process sometimes follows heavy radiation of bone. It is an acute form of osteomyelitis caused by damage to the intraosseous blood vessels and is characterized by a chronic, painful infection, and necrosis accompanied by late sequestration and sometimes permanent deformity.
Histologically, there is destruction of osteocytes, absence of osteoblasts, and lack of new bone or osteoid formation. The walls of the regional blood vessels are thickened by fibrous connective tissue. They are also the seat of endarteritis and periarteritis. The loose connective tissue which usually replaces the bone marrow is infiltrated by lymphocytes, plasma cells, and macrophages. The devitalized bone may undergo sequestration, although there is no clear line of demarcation between vital and nonvital bone. The necrotic process may extend throughout the radiated bone. Although the exact pathogenesis is not completely understood, it is generally agreed that there are three factors involved: radiation, trauma, and infection.
The mandible is affected by osteoradionecrosis far more frequently than the maxilla. The cause for this is unknown, but may be related to the difference in blood supply between the two bones. After the infection has gained entry to the bone, following traumatic injury, extraction, pulp infection, or even severe periodontitis, there is a relatively diffuse spread of the process. There is minimal localization of the infection, and there may be necrosis of a considerable amount of bone, periosteum, and overlying mucosa (Fig. 12-32). Sequestration eventually occurs, but this may be delayed for many months or several years, during which time the patient usually suffers intense pain. The occurrence of osteoradionecrosis is unpredictable, and it may arise even without gross infection or trauma.

Figure 12-32 Osteoradionecrosis.
This lesion followed heavy X-ray irradiation for epidermoid carcinoma in this area Courtesy of Dr Anitha Balan, Department of Oral Medicine and Radiology, Government Dental College, Thiruvananthapuram.
Because patients that ultimately developed osteoradio-necrosis of the jaws seemed to have many characteristics in common, Daly and Drane were able to formulate a bone necrosis profile. The more factors present, the greater the chance of necrosis. Factors leading to osteoradionecrosis were listed as: (1) irradiation of an area of previous surgery before adequate healing had taken place, (2) irradiation of lesions in close proximity to bone, (3) a high dose of irradiation with or without proper fractionation, (4) use of a combination of external radiation and intraoral implants, (5) poor oral hygiene and continued use of irritants, (6) poor patient cooperation in managing irradiated tissues or fulfilling home care programs, (7) surgery in the irradiated area, (8) indiscriminate use of prosthetic appliances following radiation therapy, (9) failure to prevent trauma to irradiated bony areas, and (10) presence of numerous physical and nutritional problems prior to therapy. Patients are most vulnerable to osteoradionecrosis of the jaws in the two years following radiotherapy.
Laser Radiation
Applications of lasers to biology and medicine began shortly after 1960, while the laser effects on tissues and materials related to dentistry began shortly thereafter. Effects of laser on tooth and pulp were discussed already.
Electrical Burns
Electrical burns of the oral cavity are seen with an unpleasant frequency in children. This unfortunate injury has been discussed in detail by Gormley and his associates, who also reported 22 cases. They invariably result from an accident in which the child chews on an electrical cord, breaks the insulation and contacts the bare wire or sucks on the socket end of an extension cord.
The resulting burn of the lips, and sometimes of the gingiva and tongue, usually causes destruction and necrosis of a considerable amount of tissue (Fig. 12-33). Developing tooth germs or buds are often destroyed in the accident with permanent cosmetic disfigurement. This type of wound heals relatively slowly.
Cervicofacial Emphysema
Emphysema is a swelling due to the presence of gas or air in the interstices of the connective tissue. There have been numerous cases of emphysema reported involving the cervicofacial and even mediastinal areas following a variety of dental and oral procedures—e.g. tooth extraction; blowing of compressed air into a root canal during endodontic treatment, or into a periodontal pocket; blowing of air from a high- speed air-rotor machine following middle-face fractures; or spontaneously as a result of the patient’s breathing actions following some type of surgical procedure, with a break in the tissue permitting air to enter connective tissue spaces.
An analogous problem termed pneumoparotid can arise due to entrapment of air in the parotid duct, leading to enlargement of parotid gland caused by air insufflation. This can be occupational (such as in wind instrument players), self-induced, or accidental. Although the Stenson’s duct is protected by contraction of the buccinator muscle and numerous redundant mucosal folds, air enters the parotid ductal system due to dramatic increases in intraoral pressures.
Clinical Features
The emphysema manifests itself as a unilateral swelling of the tissues of the face and/or neck which occurs very rapidly and is generally somewhat painful, particularly during the first few days (Fig. 12-34). Not infrequently, the patient will complain of a ‘bubbling’ sensation when palpating this tissue and of difficulty in breathing. The facial enlargement is often confused with an angioedema, but it can be differentiated by identifying crepitus within the swelling. Spread into the mediastinum results in dysphagia, or dyspnea. In mediastinal involvement crepitus synchronous with the heartbeat (Hamman’s crunch) is heard on cardiac auscultation.

Figure 12-34 Cervicofacial emphysema.
The swelling of the facial soft tissues occurred within a few hours following a dental extraction.
Pneumoparotid appears as a unilateral enlargement of the parotid with demonstration of crepitus on palpation. Frothy air-filled saliva is produced by the parotid duct rather than the clear, water-like secretion.
Treatment and Prognosis
Unfortunately, venous air embolism is an unusual but often fatal complication of this condition. For example, Longenecker has reported that, of six cases of venous air embolism occurring during head and neck surgery, five terminated fatally. If the entrance of air into the venous circulation can be recognized promptly, resuscitation may prevent death. A second complicating factor is the possibility of bacterial infection in the emphysematous connective tissue, microorganisms being carried into the tissues with the air. In such instances, broad-spectrum antibiotic coverage is recommended. Aside from this, there is no particular treatment indicated and the condition will generally resolve within a week.
The treatment for pneumoparotid consists mainly of altering the inciting event to prevent air from entering the parotid duct. Acute symptoms can be treated with antibiotics, hydration, massages, sialagogues, and compresses.
Anesthetic Necrosis
At times, administration of a local anesthetic agent can cause ulceration and necrosis at the site of injection. This necrosis is thought to result from localized ischemia, although the exact cause is unknown. The possible causes include epinephrine content in local anesthetic solution, administration of excess solution in tissue firmly bound to bone, or subperiosteal injection.
Anesthetic necrosis usually appears several days after the procedure and most commonly appears on the hard palate as a well-circumscribed area of ulceration.
Human Bite: (Morsus humanus)
The human bite is a potentially serious injury which may occur in a variety of situations including quarrels, children’s play, child abuse, mental derangements, and sexual assaults or related activities. While the bite may involve any part of the body, the extremities are most frequently involved and, according to a series of approximately 900 cases of human bite injuries reported by Boyce in 1942, about 8% involved the head and neck region. Laskin and Donohue have reported 14 cases, all involving the lips, while Freeman et al, investigated 778 bitemarks and reported that females were bitten more often than males, males were bitten on the arm more than females, and females were bitten on the breast more often than males. Saiju and Georgescu have reported a rare case of human bite on the eyebrow.
There is great potential for serious infections as well as for marked disfigurement from the human bite. The infections are usually of mixed types of microorganisms and can be difficult to treat, especially since patients frequently delay seeking treatment for several days after the incident because of the embarrassing circumstances involved. There is a major risk of transmission of diseases such as syphilis, hepatitis, and HIV infection through biting.
The human bite also has assumed a very important role in forensic medicine and forensic dentistry, especially in murder, rape, or assault cases in which legal identification of the guilty party has been made through a set of characteristic tooth imprints in bite marks on a breast, neck, or other involved area.
Oral Trauma Related to Sexual Practices
Changes in sexual activities and increasing sexual liberalism in recent years have contributed to the recognition of intraoral lesions that have become relatively common and of diagnostic importance.
The lesion consists of palatal erythema, petechiae, and ecchymoses following fellatio, or oral intercourse, apparently as a result of the physical trauma to the area and/or the negative pressure occurring at the site from irrumation. There are usually multiple lesions, which are most often found at the junction of the hard and soft palate. They heal without treatment within seven to ten days. Typical examples have been reported by Schlesinger and his associates and by Giansanti and his coworkers. Horizontal ulceration of the lingual frenum arises from the act of cunnilingus and they also heal within a week without treatment.
The differential diagnosis is extremely important, since identical lesions at the same site may occur also in infectious mononucleosis, thrombocytopenic purpura or a variety of similar dyscrasias including leukemia in which a secondary thrombocytopenia may exist, and diseases of capillary fragility, among others.
Chemical Injuries of Oral Cavity
The oral cavity frequently manifests a serious reaction to a wide variety of drugs and chemicals, although the mechanism of this reaction may be dissimilar in different cases. In some instances the tissue reaction is that of a local response to a severe irritant or even a caustic used injudiciously. In other cases the drug or chemical is administered systemically, but manifests an oral reaction of a particular type. One of the most common reactions to drugs or chemicals is the allergic phenomenon, the two main types that are of dental interest being: (1) drug allergy, or stomatitis medicamentosa, and (2) contact stomatitis, or stomatitis venenata. Angioneurotic edema is still another allergic phenomenon which will be considered separately.
Nonallergic Reaction to Drugs and Chemicals used Locally
The materials used locally which induce a nonallergic reaction are chiefly irritants or caustics, many of which are used by the dentist in various therapeutic or technical procedures. Some of these substances also constitute occupational hazards, but these will be considered separately.
Aspirin (Acetylsalicylic Acid)
Aspirin tablets are used mistakenly by many people as a local obtundent, especially for the relief of toothache. It is also available in a powder form. Although effective if used systemically, they are particularly harmful to the oral mucosa if applied locally. The usual mode of local use is to place the tablet against the offending tooth, allowing the cheek or lip to hold it in position, and to let it dissolve slowly. Within a few minutes a burning sensation of the mucosa will be noted, and the surface becomes blanched or whitened in appearance (Fig. 12-35). The caustic action of the drug causes separation and sloughing of the epithelium and frequently bleeding, especially if the area is traumatized. The healing of the painful ‘aspirin burn’ usually takes a week or more.
Endodontic Materials
Soft tissue damage resulting in deep spread of inflammation and necrosis may occur due to the usage of some endodontic materials or their injection into the hard tissue. For instance paraformaldehyde is used to devitalize the inflamed pulp. This caustic agent may leak from the pulp chamber into the surrounding tissues and causes necrosis of the gingiva and bone.
Sodium hypochlorite and hydrogen peroxide produces similar damage when injected beyond the apex.
Sodium hypochlorite (NaOCl) is commonly used as root canal irrigant. Due to its efficacy against pathogenic organisms and pulp digestion it is considered to be the medicament of choice. It is found to be sporicidal and virucidal and shows far greater tissue dissolving effects on necrotic than on vital tissues as well as the organic components of the smear layer. Although considered safe, it may cause severe tissue damage if come in contact with the tissues or extruded beyond the apex. On contact with vital tissue, it causes hemolysis, ulceration, facial nerve weakness, and necrosis, inhibits neutrophil migration, and damages endothelial cells and fibroblasts. Inadvertent injection of NaOCl solution into periapical tissues leads to emphysema, caused by oxygen liberation into the tissues, permanent facial and trigeminal nerve weakness and allergic reactions. Bowden, Ethunandan, and Brennan have reported a case of life-threatening airway obstruction secondary to hypochlorite extrusion during root canal treatment.
Gutta-percha is a biologically inert latex material used to obturate, or fill the empty space inside the root of a tooth during endodontic treatment. It is used along with zinc oxide eugenol to attain apical seal. Gutta-percha points extruded past. The apices result in infective periapical periodontitis caused by the transport of bacteria beyond the apex and an incomplete cleansing and foreign body reactions.
Hydrogen peroxide is used commonly in varying concentrations in many branches of dentistry. It is a caustic agent. Upon contact it burn tissues and release toxic free radicals, perhydroxyl anion, or both. It should be handled with care in high concentrations, since it is thermodynamically unstable and may explode if not refrigerated or stored in a dark container.
30–35% hydrogen peroxide (superoxal) is used along with heat (thermocatalytic) for bleaching. This thermocatalytic process damages the tooth by causing irritation to the cementum and periodontal ligament leading to cervical root resorption.
Sodium perborate has been widely used as a mouthwash, bleaching agent, and in dentifrices because of its supposed therapeutic effect on gingival disease. Clinical studies reveal, however, that the compound may produce an erythema of the oral mucosa which may even progress to sloughing of the tissues. In some instances the inflammation was aggravated, and edema and ulceration of mucosa frequently occurred. The lesions healed spontaneously with cessation of treatment.
Carbamide peroxide is used as a component in bleaching preparation. These preparations were reported to be associated with varying degrees of damage to the teeth and the surrounding structures if not used cautiously.
Phenol is widely used in dentistry as a cavity sterilizing agent as well as a cauterizing agent in various procedures. It is extremely caustic and if used carelessly may produce severe painful burns of the oral mucosa and skin which heal slowly (Fig. 12-36).
Silver nitrate is also used extensively in dentistry as a cavity sterilizing agent, topically as a caries-preventive agent and as a chemical cautery. Injudicious or overzealous use may produce painful burns of the oral mucous membranes.
Trichloroacetic acid used as a cauterizing agent, particularly to cauterize gingival tissue when preparing a proximal or gingival cavity, placing a band or taking an impression of a cavity. Because of its extremely caustic nature, this acid may cause serious injury to the mucosa or skin if it is used carelessly.
Volatile oils such as oil of cloves, oil of wintergreen, and eucalyptus oil are used in dentistry and can produce mild burns of the mucous membranes.
Miscellaneous Drugs and Chemicals
The various drugs and chemicals listed above constitute only an infinitesimal number of those substances which are of potential danger if used injudiciously in the oral cavity and are included for exemplary purposes only. Any strong acid, alkali, germicidal agent, strong counter-irritant, or even certain plant and animal irritants (Figs. 12-37, 12-38) may produce injury.
Nonallergic Reactions to Drugs and Chemicals Used Systemically
The systemic administration of various drugs and chemicals frequently evokes an oral reaction which is not on the basis of an allergy or sensitivity. This reaction is often a part of a generalized epidermal reaction, but other times it occurs as a specific phenomenon apparently due to the anatomic peculiarities of the oral cavity.
Arsenic in both organic and inorganic forms is sometimes used therapeutically and may produce symptoms of either acute or chronic poisoning. Many cases of arsenic poisoning occur as an occupational hazard because of the wide use of this metal in industry.
Oral Manifestations
These include intense inflammation of oral mucous membranes, and severe gingivitis. The tissues may be painful. Local contact with arsenic trioxide often produces ulceration. Systemic arsenic poisoning also produces excessive salivation.
Bisphosphonate a potent antiresorptive agent, used in the management of benign and malignant diseases involving excessive bone resorption, such as bone lesions of multiple myeloma and metastatic bone diseases. They act by blocking the dissolution of hydroxyapatite, inhibiting differentiation of bone marrow precursors into osteoclasts, and inhibiting the osteoclast function. It causes osteonecrosis in many patients. The incidence of bisphosphonate associated osteonecrosis has been increased recently, and most of the cases involve nitrogen-containing bisphosphonates, mainly pamidronate and zolendronate. Osteonecrosis of the jaw probably results from the inability of hypodynamic and hypovascular bone to meet an increased demand for repair and remodeling. According to some authors, the predilection for this location may be attributed to the fact that the jaws are the only bone structures submitted to continuous trauma and masticatory stress with exposure to the environment and to oral microorganisms. Dental extractions have been identified as a predisposing factor for osteonecrosis in many cases; but cases of ‘spontaneous’ exposures and necrosis of the alveolar bone have also been reported.
Hellstein et al, reported 28 suspected cases of osteonecrosis of the jaw and discussed the nomenclature, the clinical and radiographic findings, as well as the main modalities of therapy and prevention. They suggested the term bisphosphonate osteochemonecrosis or bis-phossy jaw, since the features of bisphosphonate-associated osteonecrosis are similar to those found in phossy jaw, the historical occupational osteonecrosis of the jaw caused by exposure to white phosphorus during the manufacture of matches.
Treatment and Prognosis
There is no effective treatment for this condition. Most of the lesions have not responded well to surgical intervention, antibiotic therapy, hyperbaric oxygen therapy, or to the topical use of mouthrinses. Current conservative approach is sequential removal of sequestrum. Removal of the bone sequestrum with minimal epithelial manipulation with topical and systemic antibiotics seem to be the treatment modality of choice.
Bismuth was formerly used widely in the treatment of syphilis, but it has been replaced in recent years by the antibiotics. The use of this metal is still common in treating certain dermatologic disorders as well as various other diseases, so that oral signs are still sometimes seen.
Oral Manifestations
Bismuth pigmentation of the oral mucosa, particularly of the gingiva and buccal mucosa, is the most common oral feature of bismuth therapy and is reported to occur in a high proportion of patients receiving preparations containing the metal.
The pigmentation appears as a ‘bismuth line’, a thin blue-black line in the marginal gingiva which is sometimes confined to the gingival papilla (Fig. 12-39). There may also be the same type of pigmentation of the buccal mucosa, the lips, the ventral surface of the tongue, or in any localized area of inflammation such as around partially erupted third molars or around the periphery of an ulcer as an anachoretic phenomenon (Fig. 12-40).
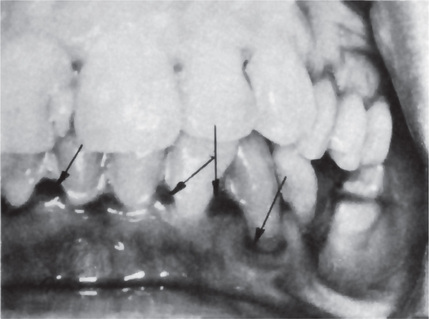
Figure 12-39 Bismuth pigmentation.
The gingiva shows the black line caused by the deposition of bismuth salts.
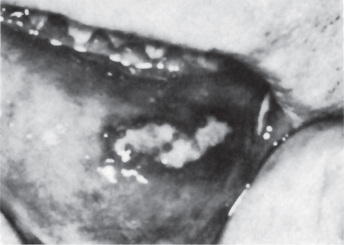
Figure 12-40 Bismuth pigmentation.
Deposition of bismuth around the periphery of this ulcer has produced a black ‘halo’ effect. Gingival pigmentation is also present.
This pigment represents precipitated granules of bismuth sulfide produced by the action of hydrogen sulfide on the bismuth compound in the tissues. The hydrogen sulfide is formed through bacterial degradation of organic material or food debris and is most common in sites of food retention. The bismuth line occurs in the majority of patients receiving prolonged bismuth treatment and is more frequent in unclean mouths. Patients receiving this metal also complain occasionally of a burning sensation of the mucosa and a metallic taste in the mouth.
Histologic Features
The granules of the sulfide are seen in the tissue section as small, irregular black collections of pigment, sometimes perivascular in location, but other times diffuse without apparent arrangement (Fig. 12-41). The material may be present in endothelial cells or in mononuclear phagocytes in the tissue, but it usually is in the intercellular tissue. It provokes no foreign body response and may be present even in the absence of inflammation.
Treatment and Prognosis
There is no specific treatment for the bismuth line. Once it is established, although it reportedly can be bleached by concentrated hydrogen peroxide. Its prevention by scrupulous oral hygiene during therapy is recommended. The prognosis of the condition is good. If untreated, the line will gradually disappear over a long period of time if use of the bismuth compound is discontinued.
Dilantin Sodium
Dilantin sodium (sodium diphenylhydantoinate) is an anticonvulsant drug, extensively used in the control of epileptic seizures. An unfortunate side effect of its use is fibrous hyperplasia of the gingiva. Most clinicians expect this hyperplasia to occur in less than half the cases, but if good oral hygiene is maintained, the incidence may be less than 10%. Why proliferation of fibrous tissue occurs in one case and not in another is not known, nor is it understood why dilantin stimulates overgrowth of gingival fibrous tissue, Nuki and Cooper have shown experimentally in cats that in the presence of local irritants in the form of orthodontic bands on the teeth and in the absence of brushing to remove plaque and debris, inflammation was produced and gingival enlargement occurred after diphenlhydantoin administration. However, when no bands were present and the teeth were brushed so that there was no irritation, the administration of the drug produced no gingival enlargement. In addition, studies of Shafer and his associates have shown stimulation of wound healing in experimental animals treated with dilantin, presumably as a result of stimulation of fibroblastic proliferation and increased collagen synthesis. In other studies Shafer has also shown remarkable stimulation of growth of human gingival fibroblasts in a tissue culture system after exposure to dilantin. Interestingly, this drug appeared to be cell-specific in his studies, since there was no similar stimulation of other types of cells.
Oral Manifestations
Gingival hyperplasia may begin as early as two weeks after dilantin therapy has been instituted, although usually it takes two to three months. The first change noted is a painless increase in the size of the gingiva, starting with the enlargement of one or two interdental papillae. The surface of the gingiva shows an increased stippling and finally a cauliflower, warty, or pebbled surface. As enlargement increases, the gingival tissue becomes lobulated, and clefts remain between each enlarged gingiva in many cases (Fig. 12-42). Palpation reveals that the tissue is dense, resilient and insensitive. It shows little tendency to bleed.

Figure 12-42 Dilantin induced hyperplasia of gingiva, demonstrating remarkable gingival enlargement. Courtesy of Dr Jayakumar ND, Saveetha Dental College, Chennai.
The hyperplasia of oral mucosa is almost entirely confined to the gingival tissues surrounding the teeth. In cases in which a patient is dentulous, but has a few edentulous areas, the gingival tissues around the teeth may show extreme hyperplasia, while the edentulous regions are generally normal in appearance. On rare occasions hyperplasia may occur in localities apart from the gingiva, such as the palate in patients wearing a prosthetic appliance, a probable source of chronic irritation (Fig. 12-43).
Histologic Features
Microscopic study of the gingival tissue reveals a suggestive but not pathognomonic appearance. The stratified squamous epithelium covering the tissue is thick and has a thin keratinized layer. The rete ridges are extremely long and thin, sometimes called ‘test-tube’ pegs, with considerable confluence, but mitotic figures are seldom seen. The bulk of the tissue is made up of large bundles of collagen fibers interspersed with fibroblasts and fibrocytes (Fig. 12-44). Vascularity is not a prominent feature of the lesion. If chronic inflammation is superimposed on this hyperplasia, plasma cells and leukocytes will be found.
Treatment and Prognosis
No treatment is necessary until the enlargement becomes esthetically objectionable. If the hyperplasia interferes with function, surgical excision is recommended, but the hyperplasia will often recur. Discontinuing use of the drug will result in a gradual diminution of the bulk of the gingiva. Most patients, however, prefer to continue use of the drug and suffer with the hyperplasia rather than resort to some other, less effective drug for the prevention of the epileptic seizures.
Cyclosporine
Cyclosporine is a selective immunosuppressant (suppress helper T cells), used primarily in organ transplant patients to overcome transplant rejection. It causes generalized gingival hyperplasia and perioral hyperesthesia. The mechanism for this phenomenon is not known.
Nifedipine
Nifedipine is a calcium channel blocker used in cardiovascular disorders. Calcium channel blockers interfere with the production of collagenase, through altered calcium influx into fibroblasts and collagen keeps accumulating without any degradation. Gingival enlargement begins after 1 to 3 months of taking these drugs. Gingiva is firm, nodular, and the clinical appearance is similar to that seen in dilantin and cyclosporine induced gingival hyperplasia.
Lead
Lead poisoning (plumbism) occurs chiefly as an occupational hazard today, but occasionally occurs because of some other accidental exposure of either an acute or chronic nature. In adults the chief means of poisoning is through inhalation of lead vapor or dust. In infants most cases result from ingestion by the child while chewing on wood painted with lead-containing paint. Many other unusual sources of lead may also result in poisoning. It appears that there have been increasing environmental levels of lead in recent years and that much of the increase is related to industry.
Clinical Features
Lead intoxication is manifested by serious gastrointestinal disturbances which include nausea, vomiting, colic, and constipation. A peripheral neuritis also develops which may produce the characteristic wrist-drop or foot-drop. Encephalitis may also occur. Blood changes are those of a hypochromic anemia with basophilic stippling of the red blood cells. Skeletal changes due to deposition of lead in growing bone occur in children and are demonstrable on the radiograph.
Oral Manifestations
The formation of a ‘lead line’ similar to the ‘bismuth line’ occurs in lead poisoning. This gray or bluish black line of sulfide pigmentation occurs in the gingiva, but is somewhat more diffuse than that of bismuth. It is also found occasionally in other areas of the oral cavity. Ulcerative stomatitis is an additional reported finding.
Excessive salivation and a metallic taste are also common complaints in this condition, as is swelling of the salivary glands. It is reported by Altshuller and his associates that lead is deposited in the deciduous teeth of children suffering from lead poisoning, and that those teeth may serve as an index of the body burden of lead.
Mercury
Mercury poisoning may be acute or chronic, but the systemic reactions in the acute form are so serious that the oral features need not be considered. Chronic mercurialism occurs after prolonged contact with mercurial compounds in a variety of situations, including therapeutic use of these compounds and as an occupational hazard. Intoxication from repeated exposure to mercury is still reported secondary to liquid mercury spills.
Clinical Features
Chronic mercurialism is characterized by gastric disturbances, diarrhea, excitability, insomnia, headache, and mental depression. The patients frequently have fine tremors of the fingers and limbs as well as of the lips and tongue. In addition, a desquamative dermatitis occurs in some persons. Nephritis is common in acute mercurial poisoning, but does not occur in severe form in the chronic type.
Oral Manifestations
The oral cavity suffers seriously in mercurialism and evidences numerous characteristic but not necessarily pathognomonic signs and symptoms. There is a remarkably increased flow of saliva (ptyalism), and a metallic taste in the mouth due to excretion of mercury in the saliva. The salivary glands may be swollen, and the tongue is also sometimes enlarged and painful. Hyperemia and swelling of the gingiva are occasionally seen.
Ulcerations on the gingiva, palate, and tongue are common. In severe cases pigmentation of the gingiva similar to the bismuth and lead lines may occur as a result of deposition of the dark sulfide compound. Loosening of the teeth, even leading to exfoliation, has been reported.
A toxic reaction from absorption of mercury in dental amalgam has heen reported on a number of occasions. Frykholm, after a thorough review of the literature and numerous studies on the absorption and excretion of mercury, concluded that the amount of estimated exposure to mercury from dental amalgam is not sufficient to cause mercury poisoning in the conventional sense. Nevertheless this exposure may suffice to bring about allergic manifestations in patients sensitive to the mercury, as in the case reported by Fernström and his associates.
Acrodynia: (Pink disease, Swift’s disease)
Acrodynia is an uncommon disease of unknown etiology, with striking cutaneous manifestations. Warkany and Hubbard established the cause of the disease as a mercurial toxicity reaction, either an actual mercury poisoning or, more likely, an idiosyncrasy to the metal. The source of the mercury is usually a teething powder, ammoniated mercury ointment, calomel lotion or bichloride of mercury disinfectant.
Clinical Features
Acrodynia occurs most frequently in young infants before the age of two years, although children are occasionally affected up to the age of five or six years. The skin, particularly of the hands, feet, nose, ears, and cheeks, becomes red or pink and has a cold, clammy feeling. The appearance has been described as resembling raw beef. The skin over the affected areas peels frequently during the course of the disease. The patients also have a maculopapular rash which is extremely pruritic. Severe sweating is an almost constant feature of acrodynia. Other features are a state of extreme irritability, photophobia with lacrimation, muscular weakness, tachycardia, hypertension, insomnia, gastrointestinal upset, and stomatitis. The children will frequently tear their hair out in patches (Fig. 12-45).
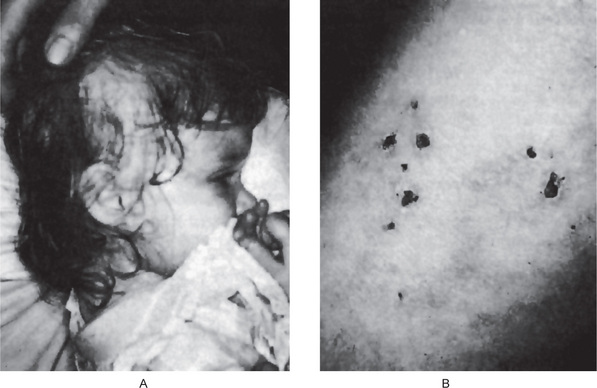
Figure 12-45 Acrodynia.
The child shows patchy loss of hair and numerous lesions of the skin, which are scabbed from the scratching due to the severe pruritus. Premature exfoliation of numerous deciduous teeth had also occurred Courtesy of Dr Nathaniel Rowe.
The excretion of mercury from the body appears to be a variable phenomenon. For this reason the recovery of unusual amounts of mercury from the urine is not always possible.
Oral Manifestations
Patients with acrodynia exhibit profuse salivation and often much ‘dribbling.’ The gingiva becomes extremely sensitive or painful and may exhibit ulcerations. Bruxism is a common finding and loosening and premature shedding of teeth often occurs; many times the child will extract loose teeth with his/her fingers. Mastication is difficult because of the pain.
Treatment and Prognosis
It is crucial to identify and remove the source of mercury. Immediate chelation therapy is the standard of care for a patient showing symptoms of severe mercury poisoning. The administration of dimercaprol, D-pencillamine, or DMSA, 2,3-dimercapto-1-propanesulfonic acid has proved successful in most cases unless the disease is of long duration. Some of the toxic effects of mercury are in some cases partially or wholly reversible. However, heavy or prolonged exposure can do irreversible damage, particularly in fetuses, infants, and young children.
Silver: (Argyria, argyrosis)
Chronic exposure to silver compounds may occur as an occupational hazard or as the result of therapeutic use of silver compounds such as silver arsphenamine or silver nitrate. It results in a permanent pigmentation of the skin and mucous membranes. Appearance of a slate-blue silver line along the gingival margins arising due to the deposition of metallic silver and silver sulfide pigments is one of the earliest signs of argyria. The pigmentation of the oral mucous membrane is diffusely dispersed throughout the oral cavity. The sclera and the nails are also pigmented. There are usually no other signs or symptoms, either local or systemic, associated with argyria.
Amalgam tattoo of oral mucous membrane is a relatively common finding in dental practice, generally occurring in one of four ways, according to Buchner and Hansen: (1) from condensation in gingiva during amalgam restorative work, (2) from particles entering mucosa lacerated by revolving instruments during removal of old amalgam restorations, (3) from broken pieces introduced into a socket or beneath periosteum during tooth extraction, or (4) from particles entering a surgical wound during root canal treatment with a retrograde amalgam filling.
Clinical Features
Amalgam tattoo appears as macules, or rarely, as slightly raised black, blue, or gray lesion. The most common locations for amalgam tattoos were gingiva, buccal mucosa, and alveolar mucosa. This tattoo has frequently been mistaken for a melanin-pigmented lesion, and in some cases biopsy is necessary to differentiate if the amalgam fragments are too small or diffuse to be visible on the dental radiograph. When the amalgam fragments are embedded within bone, they may be mistaken for a variety of other foreign bodies (Fig. 12-46).
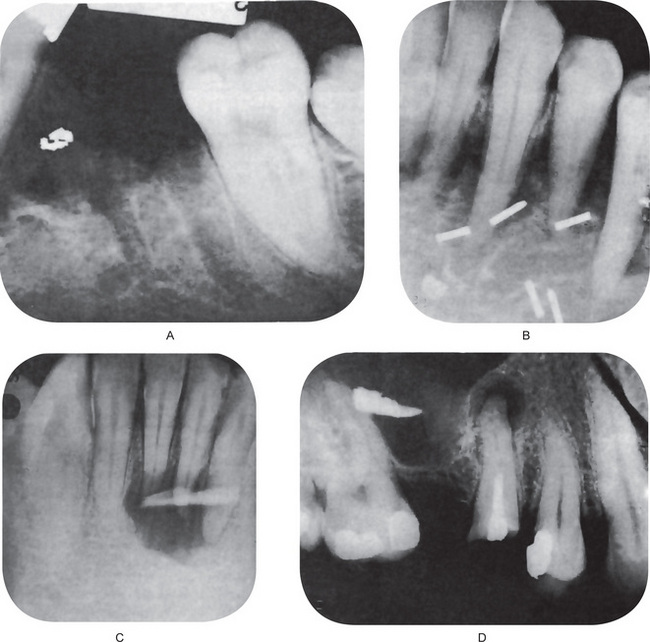
Figure 12-46 Amalgam in bone.
Dental amalgam in the bone (A) is compared to other foreign bodies seen occasionally such as radon seeds for radiation of a tumor (B), embedded glass after an automobile accident (C), and a bomb-shell fragment (D). B, Courtesy of Dr Henry M, Swenson C, Dr G Thaddeos Gregory, Dr Raymond Price.
Histologic Features
Microscopically, the dental amalgam fragments frequently show no tissue reaction to their presence, even no inflammatory response (Fig. 12-47). However, in 38% of the cases there was a chronic inflammatory response, usually manifesting as a foreign body granuloma with either foreign body giant cells or Langhans giant cells. In 17% of the cases there was a macrophagic reaction of some type, with or without a chronic inflammatory cell response.
The amalgam fragments appear as black or olive-brown granules or even as macroscopic pieces of material which can be seen plainly in the paraffin-embedded specimen as silver-gray flecks in the tissue. These granules are prominently arranged in a linear fashion along collagen fibers and around blood vessels. In addition, they are found around nerve sheaths and striated muscle fibers and along the basement membrane of mucosal epithelium.
Harrison and his associates have studied these tattoos by electron microscope and electron probe analysis and found that the original mercury-silver-tin amalgam undergoes eventual corrosion, leaving chiefly silver in the extracellular sites.
Tetracycline
Discoloration of either deciduous or permanent teeth may occur as a result of tetracycline deposition during prophylactic or therapeutic regimens instituted either in the pregnant female or postpartum in the infant. Tetracycline and its homologues have a selective affinity for deposition in bone and tooth substance, possibly through the formation of a complex with calcium ions in the surface of the microcrystals of hydroxyapatite.
The severity of the staining by tetracycline is determined by the stage of tooth development at the time of drug administration. Since tetracycline does cross the placental barrier, it may involve those deciduous teeth developing antepartum, although the discoloration itself depends upon the dosage, the length of time over which administration occurred, and the form of the tetracycline. Moffitt and his coworkers have emphasized that the critical period for tetracycline-induced discoloration in the deciduous dentition (the period of mineralization of the first millimeter of dentin nearest the dentinoenamel junction) is four months in utero to three months postpartum for maxillary and mandibular incisors and five months in utero to nine months postpartum for maxillary and mandibular canines. The period for permanent maxillary and mandibular incisors and canines is three to five months postpartum to about seven years of age. The age at which tetracycline administration occurred can easily be pinpointed by reference to a chart on the chronology of odontogenesis.
According to Grossman and his associates, the use of oxytetracycline, or possibly doxycycline, may diminish tooth discoloration if tetracycline therapy is indicated in the pregnant female or during the first six to seven years of life. After this age, the probability of discoloration need not be considered since the cosmetically important anterior teeth have completed their formation.
Significant discoloration of the teeth is also produced by minocycline hydrochloride, a semisynthetic derivative of tetracycline. Binding of minocycline to certain types of collagenous tissues like dentin, dental pulp, bone, and dermis, results in oxidation and produces the discoloration. The stained pulp is seen through the overlying translucent dentin and enamel.
Clinical Features
The teeth affected by tetracycline appear to have a yellowish or brownish-gray discoloration which is most pronounced at the time of eruption of the teeth. This discoloration gradually becomes more brownish after exposure to light. Oxytetracycline and tetracycline give a yellowish color, whereas chlortetracycline tends to cause a brownish-gray color. Tetracycline itself fluoresces under ultraviolet light and, accordingly, the teeth involved by its discoloration also fluoresce a bright yellow under ultraviolet light. However, in time this fluorescence gradually diminishes. It has been shown by Wallman and Hilton and by Zussman that the dentin is more heavily stained than the enamel.
Minocycline hydrochloride causes discoloration of the skin, nails, conjunctiva, bone, and teeth. Palate or anterior alveolar mucosa has a distinctive blue-gray appearance due to the black bone showing through the thin, translucent mucosa. The incisal edge of the fully erupted teeth reveal a blue-gray discoloration, with the middle one third being maximally involved and the exposed roots of the erupted teeth reveal dark green discoloration. The roots of developing teeth show a dark black color.
Cancer Chemotherapeutic Agents
A chemically very diverse group of drugs and agents has come into recent use for the treatment of certain malignant neoplasms. Their chief function is the destruction of malignant cells. Most of these cytotoxic agents exert their effect preferentially against cells in mitosis. Unfortunately, in addition to neoplastic cells, which undergo rapid division, certain normal cells including the cells of the oral and gastrointestinal mucosa, bone marrow, and skin also exhibit a similar degree of mitotic activity and are especially prone to manifest the toxic and damaging effects of the antineoplastic agents. Newer and experimental approaches like hematopoietic stem cell transplant (especially in treating myeloma, lymphoma, and leukemia) and isolated infusion of chemotherapy (to treat neoplasms in the liver and lung) are in use.
Clinical Features
Cancer chemotherapeutic agents are grouped into: (1) alkylating agents, (2) antimetabolites, (3) antitumor antibiotics, (4) plant alkaloids, (5) nitrosoureas, (6) enzymes, (7) hormonally active agents, and (8) miscellaneous compounds.
Because the major effect of these materials on cells and tissues is similar, regardless of each agent’s specific mechanisms of action, there are a few general manifestations of the group as a whole that can be emphasized. These are: (1) alopecia, due to arrest of mitosis of the rapidly germinating hair roots, (2) stomatitis, which may take a variety of forms, and (3) radiation recall or radiation sensitization, a reactivation of radiation reaction within the field of radiation following administration of certain of the antineoplastic agents.
Oral Manifestations
The most common oral reaction is mucosal erosion and ulceration, frequently diffuse and multiple, often related to the neutropenia produced by the drug but occasionally occurring in its absence. This may occur anywhere in the mouth but is most likely to be seen on the lips, tongue, and buccal mucosa. Hemorrhage is also a common manifestation resulting from the thromboeytopenia secondary to the drug therapy. These reactions do not occur following use of all cancer chemotherapeutic agents but are especially common with the alkylating, antimetabolite, and antitumor antibiotic groups.
Another oral finding in patients undergoing this type of therapy is the presence of any one of a variety of specific or nonspecific infections (commonly herpes simplex infection, candida infection, or infection by staphylococcal or streptococcal organisms), especially since many of these patients are also immunosuppressed. Finally, hyperpigmentation of oral mucosa has been reported occasionally, especially in patients receiving alkylating agents and antitumor antibiotics.
Occupational Injuries of the Oral Cavity
Occupational injuries of the oral cavity occur as a result of work or occupational activity. In recent years, industrial health programs have recognized the necessity of maintaining oral health and have stressed the need for special safety measures to prevent injuries to the oral and paraoral structures.
The inherent dangers in many occupations have been recognized and preventive measures have been taken to avoid injuries. Such remarkable advances have been made in the application of organic chemicals in industrial techniques that health officers, including the dentist, must constantly be alert against new hazards. Examples of occupational injuries are listed in Table 12-1.
The examination of the oral cavity in the study of occupational disease is of generally accepted importance, since local effects are recorded both in the teeth themselves and in the soft tissues. Dentin and enamel damage is usually permanent and is an indicator of past occupation. Saliva and blood stream transmit the systemic effects to the oral cavity. Prevention of these diseases must be the primary goal of our public health authorities, although early recognition and treatment of oral occupational diseases are important.
Occlusal Trauma
Occlusal forces can cause changes in the alveolar bone and periodontal connective tissue both in the presence and in the absence of periodontitis. Occlusion and local irritants are two factors in the etiology and pathogenesis of periodontal disease. Occlusal trauma and periodontal inflammation may act as co-destructive agents in periodontal disease. Excessive occlusal forces result in typical changes in periodontal tissues. These may be acute or chronic. Acute trauma occurs when biting on a hard food substance or a high point of a restoration. This causes acute inflammation of the periodontal ligament and results in pain, sensitivity to percussion, and slight mobility. If left untreated, it progresses to necrosis.
An acute traumatic force sufficient to produce traumatic injury to the periodontium also results in rather specific changes in the tooth attachment apparatus. For example, a force, which tips a tooth sharply to the buccal side, results in a crushing of the periodontal ligament fibers and perhaps that of the alveolar crest bone. The blood vessels in the involved area become thrombosed, and edema and extravasation of blood occur. On the opposite side of the tooth, there is often a tearing of the periodontal ligament, and sometimes cementum or bone is torn loose. Since the tooth rotates around a fulcrum point slightly apical to the midroot, the same changes may occur near the apex on the opposite side. These changes result in tenderness of the tooth for a few days, but if the forces are not grossly excessive, eventually the damaged alveolar crest bone will be resorbed. New periodontal fibers, cementum, and bone develop, and after a few weeks the tissues will return to normal, with the periodontal ligament space wider or the tooth reoriented in a new position.
When excessive forces occur in different and alternating directions, as may happen in cases of cusp interference, destruction of the supporting bone may occur around the entire periphery of the root, resulting in widening of the periodontal ligament space. This in turn, by interfering with mastication, favors collection of debris on teeth and predisposes to further periodontal disease.
Chronic occlusal trauma is relatively more common than acute forms. The most common cause is faulty occlusion. Physiological tooth wear, drifting, parafunctional habits like bruxism, clenching, and improper orthodontic tooth movement are the causes for chronic trauma.
In chronic trauma, the periodontal ligament gradually becomes denser, and the periodontal space widens. The alveolar bone also becomes denser and the teeth will show obvious ‘wear patterns’, with definite facets on the crowns of teeth.
Results of various types of trauma on the periodontium have been studied experimentally in laboratory animals. For example, Wentz and his colleagues subjected the premolar teeth of rhesus monkeys to excessive occlusal stresses, which tended to move the teeth buccally upon closure and lingually when the mouth was opened. Histologic studies after three days showed compression and pressure necrosis of the periodontal ligament, thrombosis of blood vessels, and the beginning of bone resorption at the buccal alveolar margin and lingual apical area (Figs. 12-48, 12-49A). Even though the excessive force was of three days duration, both areas showed undermining resorption of alveolar bone, while on the opposite sides of the root there was evidence of new bone formation on the endosteal surface of the alveolar bone. The characteristic cellular picture of inflammation was not present. After 14 days, the premolars used in the experiment were very loose. Histologic study revealed more extensive necrosis, undermining resorption of the bone and the adjoining root, and new bone formation on the opposite side of the root (Fig. 12-49B). After three, and later six months, involved teeth were still loose, but the traumatic tissue changes were no longer present. The periodontal ligament was lengthened, however, and the periodontal space was much wider (average 0.65 mm as compared to 0.19 mm in the control). New bone formation was noted on the buccal periosteal surface of the alveolar process. At no time was gingivitis or periodontitis noted. This experiment illustrates the extent of damage to the periodontium that can occur from excessive occlusal stresses. If the damage is not enough to cause exfoliation of the tooth, the periodontium is gradually adapted to withstand the added stress.
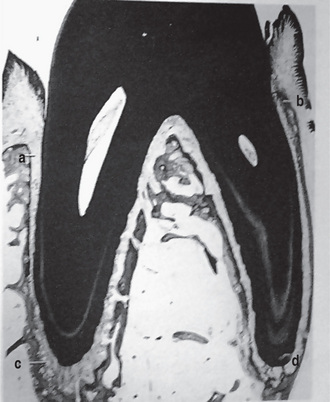
Figure 12-48 Periodontal traumatism.
A buccolingual section through the premolar of a rhesus monkey after excessive occlusal stresses had been applied for three days. Buccal alveolar margin (a), lingual alveolar margin (b), apex of mesiobuccal root (c), and apical area of lingual root (d). Note pressure necrosis at (a) and resorption of bone at (d). Courtesy of Dr Frank M Wentz: J Periodontol, 29: 117, 1958.
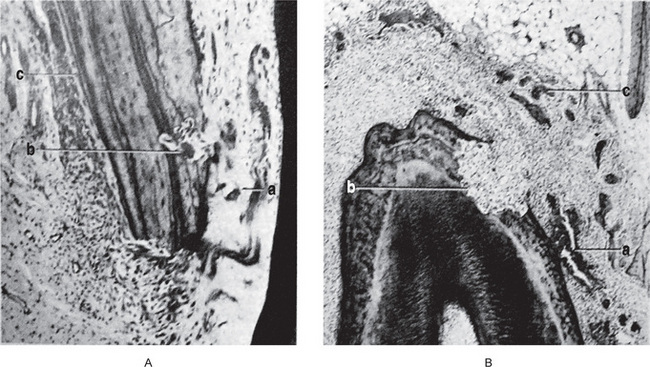
Figure 12-49 Periodontal traumatism.
A, Reaction of tissues after three days; high magnification of the pressure area (a) in Figure 12-48. Area of necrosis in the periodontal ligament (a), resorption of bone (b), and deposition of new bone (c). B, Reaction of tissues after 14 days; extensive necrosis near palatal root (a). Resorption has eliminated the area of compression (b, c). Courtesy of Dr Frank M Wentz: J Periodontol, 29: 117, 1958.
References
Adrian, R.M, Hood, A.F, Skarin, A.T. Mucocutaneous reactions to antineoplastic agents. 1980; 30:143.
Akers, L.H. Ulcerative stomatitis following therapeutic use of mercury and bismuth. J Am Dent Assoc. 1936; 23:781.
Albright, B.W, Taylor, C.G. Hereditary angioneurotic edema: report of a case. J Oral Surg. 1979; 37:888.
Altshuller, L.F, Halak, D.B, Landing, B.H, Kehoe, R.A. Deciduous teeth as an index of body burden of lead. J Pediatr. 1962; 60:224.
Anderson, GM, Practical Orthodontics. 9. CV Mosby, St Louis, 1960.
Andreasen, J.O. Etiology and pathogenesis of traumatic dental injuries: a clinical study of 1,298 cases. Scand J Dent Res. 1970; 78:329.
Andreasen, J.O. Fractures of the alveolar process of the jaw: a clinical and radiographic follow-up study. Scand J Dent Res. 1970; 78:263.
Andreasen, J.O. Luxation of permanent teeth due to trauma: a clinical and radiographic follow-up study of 189 injured teeth. Scand J Dent Res. 1970; 78:273.
André, Ferreira Leite, Paulo, Tadeu Figueiredo, Nilce, Santos Melo, Ana, Carolina AcevedoMarcelo Gusmão Paraíso Cavalcanti, Lílian, Marly Paula, Ana, Patrícia Paula, Eliete, Neves Silva Guerra. Bisphosphonate-associated osteonecrosis of the jaws: report of a case and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:14–21.
Andreasen, J.O, HjØrting-Hansen, E. Intraalveolar root fractures: radiographic and histologic study of 50 cases. J Oral Surg. 1967; 25:414.
Ball, J.S, Ferguson, A.W. Permanent discoloration of primary dentition by nitrofurantoin. Br Med J. 1962; 2:1103.
Barker, B.F, Jensen, J.L, Howell, F.V. Focal osteoporotic bone marrow defects of the jaws. Oral Surg. 1974; 38:404.
Barker, J.N. The sterilization of dentin. Aust J Dent. 1935; 39:156.
Bartels, H.A. Significance of yeastlike organisms in denture sore mouths. Am J Orthod. 1937; 23:90.
Baum, H.B. Occupational diseases of the mouth. Dent Cosmos. 1934; 76:247.
Beasley, J.D. Traumatic cyst of the jaws: report of 130 cases. J Am Dent Assoc. 1976; 92:145.
Bergendal, T, Isacsson, G. Effect of nystatin in the treatment of denture stomatitis. Scand J Dent Res. 1980; 88:446.
Bernier, J.L, Knapp, M.J. New pulpal response to high-speed dental instruments. Oral Surg. 1958; 11:167.
Bhaskar, S.N, Beasley, JD III, Cutright, D.E. Inflammatory papillary hyperplasia of the oral mucosa: report of 341 cases. J Am Dent Assoc. 1970; 81:949.
Bhaskar, S.N, Bolden, T.E, Weinmann, J.P. Experimental obstructive adenitis in the mouse. J Dent Res. 1956; 35:852.
Bhaskar, S.N. Pathogenesis of mucoceles. J Dent Res. 1956; 35:863.
Blaschke, D.D, Brady, F.A. The maxillary antrolith. Oral Surg. 1979; 48:187.
Bourgoyne, J.R. Sialolithiasis. Oral Surg. 1948; 1:719.
Bowden, J.R, Ethunandan, M, Brennan, P.A. Life-threatening airway obstruction secondary to hypochlorite extrusion during root canal treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:402–404.
Box, H.K. Red bone-marrow in human jaws. Bull No 20. Can Dent Res Fndn. 1933.
Box, H.K. Bone resorption in red marrow hyperplasias in human jaws. Bull No 21. Can Dent Res Fndn. 1936.
Boyce, F.F. Human bites. South Med J. 1942; 35:631.
Brännström, M. Reaction of the pulp to amalgam fillings. Odontol Revy. 1963; 14:244.
Brännström, M, Soremark, R. The penetration of 22 Na ions around amalgam restorations with and without cavity varnish. Odontol Revy. 1962; 13:331.
Breitner, C, Tischler, M. Über die Beeinflussung del’ Zahnkeime durch orthodontische Bewegung der’ Milchzahne Z. Stomatol. 1934; 32:1383.
Brown, L.R, Dreizen, S, Handler, S, Johnston, D.A. Effect of radiation-induced xerostomia on human oral microflora. J Dent Res. 1975; 54:740.
Brunner, H. Pathology of ranula. Oral Surg. 1949; 2:1591.
Budtz-JØrgensen, E. Denture stomatitis III. Histopathology of trauma- and candida-induced inflammatory lesions of the palatal mucosa. Acta Odontol Scand. 1970; 28:551.
Budtz-JØrgensen, E, Bertram, D. Denture stomatitis I. The etiology in relation to trauma and infection. Acta Odontol Scand. 1970; 28:71.
Budtz-JØrgensen, E. Denture stomatitis II. The effect of antifungal and prosthetic treatment. Acta Odontol Scand. 1970; 28:283.
Burstone, M.S. The effect of X-ray irradiation on the teeth and supporting structures of the mouse. J Dent Res. 1950; 29:220.
Burstone, M.S. Radiobiology of the oral tissues. J Am Dent Assoc. 1953; 47:630.
Cahn, L.R. The denture sore mouth. Ann Dent. 1936; 3:33.
Canizares, O. Contact dermatitis due to the acrylic materials used in artificial nails. Arch Dermatol. 1956; 74:141.
Carl, W, Schaaf, N.G, Chen, T.Y. Oral care of patients irradiated for cancer of the head and neck. Cancer. 1972; 30:448.
Carl, W, Wood, R. Effects of radiation on the developing dentition and supporting bone. J Am Dent Assoc. 1980; 101:646.
Carter, G.D, Goss, A.N. Bisphosphonates and avascular necrosis of the jaw: a possible association. Med J. 2005; 182:413–415. [Aug].
Casamassimo, P.S, Lilly, G.E. Mucosal cysts of the maxillary sinus: a clinical and radiographic study. Oral Surg. 1980; 50:282.
Caviedes-Bucheli, J, Correa-Ortíz, J.A, García, L.V, López-Torres, R, et al. The effect of cavity preparation on substance P expression in human dental pulp. J Endod. 2005; 31(12):857–859. [Dec].
Cawson, R.A. Denture sore mouth and angular cheilitis. Br Dent J. 1963; 115:441.
Claus, E.C, Orban, B. Fractured vital teeth. Oral Surg. 1953; 6:605.
Colby, R.A. Radiation effects on structures of the oral cavity: a review. J Am Dent Assoc. 1942; 29:1446.
Crawford, B.E, Weathers, D.R. Osteoporotic marrow defects of the jaws. J Oral Surg. 1970; 28:600.
Criep, LAllergy and Clinical Immunology. New York: Grune and Stratton, 1976.
Cruikshank, L.G. Dental disease and its relation to antisyphilitic treatment. Br J Vener Dis. 1938; 14:280.
Cuccia, A.M. Aetiology of sleep bruxism: a review of the literature. Recenti Prog Med. 2008; 99(6):322–328.
Curtis, A.C, Taylor, H, Jr. Allergic dermatoses of importance to the dentist. Am J Orthod Oral Surg. 1947; 33:201.
Cutright, D.E. Morphogenesis of inflammatory papillary hyperplasia. J Prosthet Dent. 1975; 33:380.
Daly, T.E, Drane, J.B. Management of dental problems in irradiated patients: refresher course. Radiological Society of North America. 1972.
Daly, T.E. Effects of prednisolone on the thermal sensitivity and pulpal reactions of silicate-restored teeth. J Prosthet Dent. 1964; 14:1124.
De Sermeño, R.F, Da, Silva LA, Herrera, H, Herrera, H, Silva, R.A, Leonardo, M. Tissue damage after sodium hypochlorite extrusion during root canal treatment.. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108(1):e46–9. [July].
Del Regato, J.A. Dental lesions observed after roentgen therapy in cancer of buccal cavity, pharynx and larynx. Am J Roentgenol. 1939; 42:404.
DiFrancesco, R.C, Junqueira, P.A, Trezza, P.M, De Faria, M.E, Frizzarini, R, Zerati, F.E. Improvement of bruxism after T & A surgery. Int J Pediatr Otorhinolaryngol. 2004; 68(4):441–445.
Dreizen, S, Daly, T.E, Drane, J.B, Brown, L.R. Oral complications of cancer radiotherapy. Postgrad Mede. 1977; 61:85.
Dreizen, S, McCredie, K.B, Dicke, K.A, Zander, A.R, et al. Oral complications of bone marrow transplantation in adults with acute leukemia. Postgrad Med. 1979; 66:187.
Dunsche, A, Kästel, I, Terheyden, H, Springer, I.N, Christophers, E, Brasch, J. Oral lichenoid reactions associated with amalgam: improvement after amalgam removal. Br J Dermatol. 2003; 148(1):70–76.
Ellis, RG, Davey, KW, The Classification and Treatment of Injuries to the Teeth of Children. 5. Year Book Publishers, Chicago, 1970.
Elzay, R.P. Traumatic ulcerative granuloma with stromal eosinophilia (Riga-Fede’s disease and traumatic eosinophilic granuloma. Oral Surg Oral Med Oral Pathol. 1983; 55(5):497–506. [May].
El-Mofty, S.K, Swanson, P.E, Wick, M.R, Miller, A.S. Eosinophilic ulcer of the oral mucosa. Report of 38 new cases with immunohistochemical observations. Oral Surg Oral Med Oral Pathol. 1993; 75(6):716–722. [Jun].
English, J.A, Schlack, C.A, Ellinger, F. Oral manifestations of ionizing radiation II: effect of 200 KV. X-ray on rat incisor teeth when administered locally to the head in the 1,500 R dose range. J Dent Res. 1954; 33:377.
Ennis, L.M, Berry, H.M, Phillips, J.EDental Roentgenology. Philadelphia: Lea and Febiger, 1967.
Esterberg, H.L, White, P.H. Sodium Dilantin gingival hyperplasia. J Am Dent Assoc. 1945; 32:16.
Ettinger, R.L. The etiology of inflammatory papillary hyperplasia. J Prosthet Dent. 1975; 34:254.
Evelyn, K.A. Medical applications of artificial radioactive isotopes. Can Med Assoc J. 1947; 56:547.
Fajardo, L.F, Berthrong, M. Radiation injury in surgical pathology Part III: salivary glands, pancreas and skin. Am J Surg Pathol. 1981; 5:279.
Ferrazzano, G.F, Iodice, G, Cantile, T, Ingenito, A. Scanning electron microscopic study of air abrasion effects on human dentine. Eur J Paediatr Dent. 2007; 8(3):113–118. [Sep].
Fernstrom, A.I.B, Frykholm, K.O, Huldt, S. Mercury allergy with eczematous dermatitis due to silver-amalgam fillings. Br Dent J. 1962; 113:204.
Fisher, A.A. Allergic sensitization of the skin and oral mucosa to acrylic denture materials. J Am Med Assoc. 1954; 156:238.
Fisher, A.K, Rashid, P.J. Inflammatory papillary hyperplasia of the palatal mucosa. Oral Surg. 1952; 5:191.
Frandsen, A.M. Effects of roentgen irradiation of the jaws on socket healing in young rats. Acta Odontol Scand. 1962; 20:307.
Frankel, M.A. Tetracycline antibiotics and tooth discoloration. J Dent Child. 1970; 37:117.
Freeman, A.J, Senn, D.R, Arendt, D.M. Seven hundred seventy eight bite marks: analysis by anatomic location, victim and biter demographics, type of crime, and legal disposition. J Forensic Sci. Nov, 2005; 50(6):1436–1443.
Frykholm, K.O. On mercury from dental amalgam: its toxic and allergic effects and some comments on occupational hygiene. Acta Odontol Scand. 15(Suppl 22), 1957.
Gao, S, Wang, Y, Liu, N, Li, S, Du, J. Eosinophilic ulcer of the oral mucosa: a clinicopathological analysis. Chin J Dent Res. 2000; 3(1):47–50. [May].
Gardner, A.F, Stoller, S.M, Steig, J.M. A study of the traumatic bone cyst of the jaw. Can Dent Assoc J. 1962; 28:151.
Gatot, A, Arbelle, J, Leiberman, A, Yani-Inbar, I. Effects of sodium hypochlorite on soft tissues after its inadvertent injection beyond the root apex. J Endod. 1991; 17:573–574.
Gelbke, H. The influence of pressure and tension on growing bone in experiments with animals. J Bone joint Surg. 1951; 33A:947.
Gher, M.E. Changing concepts. The effects of occlusion on periodontitis. Dent Clin North Am. 1998; 42(2):285–299.
Giansanti, J.S, Cramer, J.R, Weathers, D.R. Palatal erythema: another etiologic factor. Oral Surg. 1975; 40:379.
Glaros, A.G, Rao, S.M. Effects of bruxism: a review of the literature. J Prosthet Dent. 1977; 38:149.
Glickman, I, Bibby, B.G. Effect of sodium perborate upon the gingival mucosa: a controlled experiment. J Am Dent Assoc. 1944; 31:1201.
Glickman, I, Lewitus, M.P. Hyperplasia of the gingivae associated with Dilantin (sodium diphenylhydantoinate) therapy. J Am Dent Assoc. 1941; 28:199.
Going, R.E. Status report on cement bases, cavity liners, varnishes, primers, and cleansers. J Am Dent Assoc. 1972; 85:654.
Gonçales, E.S, Rubira-Bullen, I.F, Rubira, C.M, Miyazawa, M, et al. Eosinophilic ulcer of the oral mucosa versus squamous cell carcinoma. Quintessence Int. 2007; 38(8):677–680. [Sep].
Goldman, L, Gray, J.A, Goldman, J, Goldman, B, et al. Effect of laser beam impacts on teeth. J Am Dent Assoc. 1965; 70:601.
Gordon, N.C, Brown, S, Khosla, V.M, Hansen, L.S. Lead poisoning. Oral Surg. 1979; 47:500.
Gormley, M B, Marshall, J, Jarrett, W, Bromberg, B. Thermal trauma: a review of 22 electrical burns of the lip. J Oral Surg. 1972; 30:531.
Gottlieb, B. Some orthodontic problems in histologic illumination. Am J Orthod. 1946; 32:113.
Garcia-Pola, M.J, Garcia-Martin, J.M, Varela-Centelles, P, Bilbao-Alonso, A, et al. Oral and facial piercing: associated complications and clinical repercussion. Quintessence. 2008; 39(1):51–59. [Jan].
Greenberg, M.S. Intravenous bisphosphonates and osteonecrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:259–260.
Gregory, G.T, Shafer, W.G. Surgical ciliated cysts of the maxilla: report of cases. J Oral Surg. 1958; 16:251.
Grossman, E.R, Walchek, A, Freedman, H. Tetracyclines and permanent teeth: the relation between dose and tooth color. Pediatrics. 1971; 47:567.
Grossman, L.I. Pulp reactions to the insertion of selfcuring acrylic resin filling materials. J Am Dent Assoc. 1952; 46:265.
Guernsey, L.H. Reactive inflammatory papillary hyperplasia of the palate. Oral Surg. 1965; 26:814.
Halstead, C.L. Mucosal cysts of the maxillary sinus: report of 75 cases. J Am Dent Assoc. 1973; 87:1435.
Balto, H, Al-Nazhan, S. Accidental injection of sodium hypochlorite beyond the root apex. Saudi Dent J. 2002; 14(1):36–38.
Hansen, L.S, Sapone, J, Sproat, R.C. Traumatic bone cysts of jaws. Oral Surg. 1974; 37:899.
Hardwick, J.L. Sterilisation of carious dentin. Proc R Soc Med. 1949; 42:815.
Harrison, J.D. Salivary mucoceles. Oral Surg. 1975; 39:268.
Harrison, J.D, Garrett, J.R. Histological effects of ductal ligation of salivary glands of the cat. J Path. 1976; 118:245.
Harrison, J.D, Rowley, P.S.A, Peters, P.D. Amalgam tattoos: light and electron microscopy and electron-probe micro-analysis. J Pathol. 1977; 121:83.
Healey, H.G, Patterson, S.S, Van Huysen, G. Pulp reaction to ultrasonic cavity preparation. US Armed Forces Med J. 7, 1956.
Heft, M.W, Flynn, P.M. Hereditary angioedema: review of literature and dental treatment. J Am Dent Assoc. 1977; 95:986.
Hellstein, J.W, Marek, C.L, Pharm, B.S. Bisphosphonate osteochemonecrosis (bisphossy jaw): is this phossy jaw of the 21st century? J Oral Maxillofac Surg. 2005; 63:682–689.
Hellstein, J, Fielding, C. Bisphosphonate osteochemonecrosis: clinical findings and treatment theories may relate to a possible analogy with ‘phossy’ jaw. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:189–190. [(letter to the editor)].
Herzberg, B.L. Bone changes incident to orthodontic tooth movement in man. J Am Dent Assoc. 1932; 19:1777.
Hirshberg, A, Amariglio, N, Akrish, S, Yahalom, R, et al. Traumatic ulcerative granuloma with stromal eosinophilia: a reactive lesion of the oral mucosa. Am J Clin Pathol. Oct, 2006; 126(4):522–529.
HjØrting-Hansen, E, Holst, E. Morsicatio mucosae oris and suctio mucosae oris. Scand J Dent Res. 1970; 78:492.
Howe, G.L. Haemorrhagic cysts of the mandible-I, II. Br J Oral Surg. 77, 1965; 3:55.
Hurt, W.C. Mucous cysts. Oral Surg. 1950; 3:425.
Husein, A. Applications of lasers in dentistry: a review. Archives of Orofacial Sciences. 2006; 1:1–4.
Ivy, R.H. Hemorrhagic or traumatic cysts of the mandible. Surg Gynecol Obstet. 1937; 65:640.
Jensen, J.L, Howell, F.V, Rick, G.M, Correll, R.W. Minor salivary gland calculi. Oral Surg. 1979; 47:44.
Johnson, A.L, Appleton, J.L, Jr., Rittershofer, L.S. Tissue changes involved in tooth movement. Int J Orthod. 1926; 12:889.
Kaan, Orhan, Doruk, Kocyigit, Reha, Kisnisci, Candan, S Paksoy. Rhinolithiasis: an uncommon entity of the nasal cavity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:E28–32.
Kahler, W. The cracked tooth conundrum: terminology, classification, diagnosis, and management. Am J Dent. 2008; 21(5):275–282.
Kapferer, I, Benesch, T, Gregoric, N, Ulm, C, et al. Lip piercing: prevalence of associated gingival recession and contributing factors: a cross-sectional study. J Periodontal Res. Apr, 2007; 42(2):177–183.
Karges, M.A, Eversole, L R, Poindexter, B.J, Jr. Antrolith: report of case and review of Iiterature. J Oral Surg. 1971; 29:812.
Kashima, H.K, Kirkham, W.R, Andrews, J.R. Postirradiation sialadenitis: a study of the clinical features, histopathologic changes and serum enzyme variations following irradiation of human salivary glands. Am J Roentgenol Radium Ther Nucl Med. 1965; 94:271.
Kinerly, T, Jarabak, J.P, Phatak, N.M, Dement, J. Laser effect on tissue and material related to dentistry. J Am Dent Assoc. 1965; 70:593.
King, J.D. Experimental investigations of parodontal disease in the ferret and related lesions in man (2. Gingival hyperplasia due to epanutin therapy. 1947; 83:148.
Knapp, M.J, Bernier, J.L. The response of oral tissues to ultrasound. J Am Dent Assoc. 1959; 58:50.
Koenig, L.M, Molly, Carnes. Body Piercing-Medical Concerns with Cutting-Edge Fashion. Am J Dent. 2007; 20(5):340–344. [Oct].
Kronfeld, R. The process of repair following tooth fracture. J Dent Res. 1931; 11:247.
Kutscher, A.H, Zegarelli, E.V, Tovell, H.M.M, Hochberg, B. Discoloration of teeth induced by tetracycline. J Am Med Assoc. 1963; 184:586.
Lan, W.H, Liu, H.C. Treatment of dentin hypersensitivity by Nd:YAG laser. J Clin Laser Med Surg. 1996; 14(2):89–92.
Langeland, K. Tissue changes in the dental pulp. Odontol Tidskr. 1957; 65:239.
Lantz, B. Cervicofacial emphysema: a report of three cases with periodontal etiology. Odontol Rev. 1964; 15:279.
Laskin, D.M, Donohue, W.B. Treatment of human bites of the lip. J Oral Surg. 1958; 16:236.
Laskin, D.M, Robinson, I.B, Weinmann, J.P. Experimental production of sarcomas by methyl methacrylate implants. Proc Soc Exp Biol Med. 1954; 87:329.
Lawrence, E.A. Osteoradionecrosis of the mandible. Am J Roentgenol Radium Ther. 1946; 55:733.
Lea, W.A, Jr., Block, W.D, Cornish, H.H. The irritating and sensitizing capacity of epoxy resins. Am Med Assoc Arch Dermatol. 1958; 78:304.
Lee, J, Lorenzo, D, Rawlins, T, Cardo, V.A, Jr. Sodium hypochlorite extrusion: an atypical case of massive soft tissue necrosis. J Oral Maxillofacial Surg. 2011; 69(6):1776–1781. [June].
Lehner, T. Oral candidosis. Dent Practit. 1967; 17:209.
Leist, M. Uber die Einwirkung del’ Roentgenstrahlen und des Radiums auf Zahne und Kiefer. Strahlentherapie. 1927; 24:268.
Levin, Liran, Zadik, Yehuda. Oral piercing: complications and side effects. Am J Dent. Oct, 2007; 20(5):340–344. [Oct].
Levy, B.M, ReMine, W.H, Devine, K.D. Salivarv gland calculi: pain, swelling associated with eating. J Am Med A. 1962; 181:1115.
Levy, B.M, Rugh, R, Lunin, L, Chilton, N, et al. The effect of a single subacute X-ray exposure to the fetus on skeletal growth; a quantitative study. J Morphol. 1953; 93:561.
Labene, R.R, Fine, S. Interaction of laser radiation with oral hard tissues. J Prosthet Dent. 1966; 16:589.
Loeb, L. Effects of roentgen rays and radioactive substances on living cells and tissues. J Cancer Res. 1922; 7:229.
Longenecker, C.G. Venous air embolism during operations of the head and neck: report of a case. Plast Reconstr Surg. 1965; 36:619.
Low-Beer, B.V.A. Radiation therapy and dental medicine. Oral Surg. 1951; 4:739.
Lura, H.E. Tissue reactions of bone upon mechanical stresses. Am J Orthod. 1952; 38:453.
Lynch, M, Burket’s Oral Medicine. 7. JB Lippincott, Philadelphia, 1977.
Manley, E.B. Effect of filling materials on the human tooth pulp. Proc R Soc Med Sect Odontol. 1941; 34:693.
Manley, E.B. A review of pulp reactions to chemical irritations. Int Dent J. 1950; 1:36.
Medak, H, Sehour, I, Klauber, W.A. The effect of single doses of irradiation upon the eruption of the upper rat incisor. J Dent Res. 1950; 29:839.
Meklas, J.F. Bruxism: diagnosis and treatment. J Acad Gen Dent. 1971; 19:31.
Meyer, IOsteoradionecrosis of the Jaws. Chicago: Year Book Publishers, 1958.
Meyer, I, Shklar, G, Turner, J. Tissue healing and infection in experimental animals irradiated with cobalt-50 and orthovoltage. Oral Surg. 1966; 21:333.
Mezei, M.M, Tron, V.A, Stewart, W.D, Rivers, J.K. Eosinophilic ulcer of the oral mucosa. J Am Acad Dermatol. 1995; 33(5 Pt 1):734–740. [Nov].
Miglioratti, C.A, Schubert, M.M, Peterson, D.E, Seneda, L.M. Bisphosphonate-associated osteonecrosis of mandibular and maxillary bones: an emerging oral complication of supportive cancer therapy. Cancer. 2006; 104:83–93.
Miller, G. Fat embolism: a comprehensive review. J Oral Surg. 1975; 33:91.
Moffitt, J.M, Cooley, R.O, Olsen, N.H, Hefferren, J.J. Prediction of tetracycline-induced tooth discoloration. J Am Dent Assoc. 1974; 88:547.
Morrish, R.B, Jr., Chan, E, Silverman, S, Jr., Meyer, et al. Osteonecrosis in patients irradiated for head and neck carcinoma. Cancer. 1981; 47:1980.
Moyers, R.E. The periodontal membrane in orthodontia. J Am Dent Assoc. 1950; 40:22.
Myall, R.W.T, Eastep, P.B, Silver, J.G. Mucous retention cysts of the maxillary antrum. J Am Dent Assoc. 1974; 89:1338.
Nadler, S.C. Bruxism, a classification: critical review. J Am Dent Assoc. 1957; 54:615.
Nathanson, N.R, Quinn, T.W. Ranula: a review of the literature and report of three cases. Oral Surg. 1952; 5:250.
Needleman, H.L, Berkowitz, R.J. Electric trauma to the oral tissues of children. ASDC J Dent Child. 1974; 41:19.
Newton, A.V. Denture sore mouth: a possible aetiology. Br Dent J. 1962; 112:357.
Noble, W.H. Mediastinal emphysema resulting from extraction of an impacted mandibular third molar. J Am Dent Assoc. 1972; 84:368.
Nuki, K, Cooper, S.H. The role of inflammation in the pathogenesis of gingival enlargement during the administration of diphenylhydantoin sodium in cats. J Periodont Res. 1972; 7:102.
Nygaard-østby, B. Pulp reactions to direct filling resins. J Am Dent Assoc. 1955; 50:7.
Nygaard-østby, B. Clinical and experimental experience with Borden Airotor Nor Tannlaegeforen Tidskr. 1958; 68:124.
Ohba, T, Yang, R.C, Chen, C.Y, Uneoka, M. Postoperative maxillary cyst. Int J Oral Surg. 1980; 9:480.
Olech, E, Sicher, R.H, Weinmann, J.P. Traumatic mandibular bone cysts. Oral Surg. 1951; 4:1160.
Oman, C.R. Further report on use of ultrasonics in dentistry. Ann Dent. 1955; 14:1.
Oppenheim, A. Bone changes during tooth movement. Int J Orthod. 1930; 16:535.
Oppenheim, A. Human tissue response to orthodontic intervention of short and long duration. Am J Orthod Oral Surg. 1942; 28:263.
Oppenheim, A. Tissue changes, particularly of the bone incident to tooth movement. Am J Orthod. 1911–1912; 3:57–113.
Peck, S, Peck, H. Laser radiation: some specific dental effects and an evaluation of its potential in dentistry. J Prosthet Dent. 1967; 17:195.
Perkins, C.S, Meisner, J, Harrison, J.M. A complication of tongue piercing. Br Dent J. 1997; 22, 182(4):147–148. [Feb].
Peterson, L.J, Indresano, A.T, Marciani, R.D, Roser, S.M Principles of oral and maxillofacial surgery (. 1992;
Phillips, RW, Skinner’s Science of Dental Materials. 8. WB Saunders, Philadelphia, 1982.
Pilolli, G.P, Lucchese, A, Scivetti, M, Maiorano, E, et al. Traumatic ulcerative granuloma with stromal eosinophilia of the oral mucosa: histological and immunohistochemical analysis of three cases. Minerva Stomatol. 2007; 56(1–2):73–79. [Jan-Feb].
Pindborg, J.J. Clinical radiographic and histological aspects of intra-alveolar fractures of upper central incisors. Acta Odontol Scand. 1955–56; 13:41.
Pinto, L.S, Campagnoli, E.B, de Souza, Azevedo R, Lopes, M.A, et al. Rhinoliths causing palatal perforation: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104(6):42–46. [Oct 17].
Powers JM, Sakguchi RL. Craig’s Restorative Dental Materials (12th ed), CV Mosby St Louis
Poyton, H.G. The effects of radiation on teeth. Oral Surg. 1968; 26:639.
Pullon, P.A, Miller, A.S. Sialolithiasis of accessory salivary glands: review of 55 cases. J Oral Surg. 1972; 30:832.
Ramanathan, K, Ganesan, T.J, Raghavan, K.V. Salivary mucoceles-racial and histological variations. Med J Malaysia. 1977; 4:302.
Reitan, K. The initial tissue reactions incident to orthodontic tooth movement. Acta Odontol Scand, (Suppl. (6):1951.
Reitan, K. Tissue changes following experimental tooth movement as related to the time factor. Dent Record. 1953; 73:559.
Renner, R.P, Lee, M, Andors, L, McNamara, T.F. The role of C albicans in denture stomatitis. Oral Surg. 1979; 47:323.
Rhymes, R, Jr. Postextraction subcutaneous emphysema. Oral Surg. 1964; 17:271.
Rickles, N.H. Procaine allergy in dental patients: diagnosis and management; a preliminary report. Oral Surg. 1953; 6:375.
Roberts, H.W, Toth, J.M, Berzins, D.W, Charlton, D.G. Mineral trioxide aggregate material use in endodontic treatment: a review of the literature. Dental Materials. 2008; 24:149–164.
Robinson, HBG. Pulpal effects of operative dentistry. J Prosthet Dent. 1957; 7:282.
Robinson, L, Hjørting-Hansen, E. Pathologic changes associated with mucous retention cysts of minor salivary glands. Oral Surg. 1964; 18:191.
Rodrigues, C.D. Estrela C Traumatic bone cyst suggestive of large apical periodontitis. J Endod. 2008; 34(4):484–489. [Apr].
Ruggiero, S.L, Mehrotra, B, Rosenberg, T, Engroff, S.L. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 62(527–34), 2004.
Rycroft, R.J.G. Contact dermatitis from acrylic compounds. Br J Dermatol. 1977; 96:685.
Saiju, R, Georgescu, D. Involuntary human bite to the eyebrow. Kathmandu Univ Med J. 2008; 6(2):223–224. [Apr-Jun].
Samuels, H.S. Contact glossitis from autopolymerizing resin splint. US Armed Foces Med J. 1960; 11:1501.
Sandstedt, C. Einige Beitrage zur Theorie der Zahnregulierung. Nord Tandlakare Tidskr. 1905; 1904.
Sapp, P.J, Eversole, L.R, Wyosji, G.P Contemporary oral and maxillofacial patholog. 1997;
Saravanan, B. Toothbrush injury in an adult. Indian J Dent Res. 2010; 21:446–448.
Schlesinger, S.L, Borbotsina, J, O’Neill, L. Petechial hemorrhages of the soft palate secondary to fellatio. Oral Surg. 1975; 40:376.
Schour, I, Sarnat, B.G. Oral manifestations of occupational origin. J Am Med Assoc. 1942; 120:1197.
Schützmannsky, G. Unfallverletzungen an jugendlichen Zähnen. Dtsch Stomatol. 1963; 13:919.
Schwartz, A.M. Tissue changes incidental to orthodontic tooth movement. Int J Orthod. 1932; 18:331.
Schwartz, H.C. Rhinolithiasis: a disorder not to be approached transorally. J Am Dent Assoc. 1979; 98:228.
Segreto, V.A, Jerman, A.C, Shannon, L. Absorption and excretion of mercury in dental personnel: preliminary study. USAF School of Aerospace Medicine, Aerospace Medical Division (AFSC. 1968. [June].
Sewerin, I. A clinical and epidemiologic study of morsicatio buccarum/labiorum. Scand J Dent Res. 1971; 79:73.
Shafer, W.G. The effect of single and fractionated doses of selectively applied X-ray irradiation on the histologic structure of the major salivary glands of the rat. J Dent Res. 1953; 32:796.
Shafer, W.G. Effect of Dilantin sodium on various cell lines in tissue culture. Proc Soc Exp Biol Med. 1961; 108:694.
Shafer, W.G, Beatty, R.E, Davis, W.B. Effect of Dilantin sodium on tensile strength of healing wounds. Proc Soc Exp Biol Med. 1958; 98:348.
Shroff, F.R. Effects of filling materials on the dental pulp. New Zealand Dent J. 1947; 43:35. [42 99, 145, 1946].
Silverman, F.N, Cassady, H.A. Acrodynia following ingestion of mercurial ointment; late dental sequelae. New Eng J Med. 1952; 247:343.
Skillen, W.G, Reitan, K. Tissue changes following rotation of teeth in the dog. Angle Orthod. 1940; 10:140.
Smith, R.A. The effect of roentgen rays on the developing teeth of rats. J Am Dent Assoc. 1931; 18:111.
Southby, R. Pink disease with clinical approach to possible etiology. Med J. 1949; 2:801. [Aug].
Spiegel, L. Discoloration of skin and mucous membrane resembling argyria following use of bismuth and silver arsphenamine. Arch Dermatol Syph. 1931; 23:266.
Standish, S.M, Shafer, W.G. Serial histologic effects of rat submaxillary and sublingual salivary gland duct and blood vessel ligation. J Dent Res. 1957; 36:866.
Standish, S.M. Focal osteoporotic bone marrow defects of the jaws. J Oral Surg. 1962; 20:123.
Standish, S.M. The mucous retention phenomenon. J Oral Surg. 1959; 17:15.
Stanley, H.R, Jr. Methods and criteria in evaluation of dentin and pulp response. Int Dent J. 1970; 20:507.
Stanley, H.R. The protective effect of reparative dentin and how it compares to man-made liners. J Am Acad Gold Foil Oper. 1971; 14:29.
Stanley, H.R. Traumatic capacity of high-speed and ultrasonic dental instrumentation. J Am Dent Assoc. 1961; 63:749.
Stanley, H. R, Swerdlow, H. An approach to biologic variation in human pulpal studies. J Prosthet Dent. 1964; 14:365.
Stanley, H.R. Accelerated handpiece speeds: the potential abuse of high speed techniques. Dent Clin North Am. 1960; 4:621.
Stanley, H. R. Reaction of the human pulp to cavity preparation: results produced by eight different operative grinding technics. J Am Dent Assoc. 1959; 58:49.
Stein, M, Brady, L.W, Raventos, A. The effects of radiation on extraction-wound healing in the rat. Cancer. 1957; 10:1167.
Stern, R.H. The laser in dentistry: a review of the literature. J Dent Assoc S Afr. 1974; 29:173.
Stern, R.H, Sognnaes, R.F. Laser beam effect on dental hard tissues. J Dent Res. 1964; 43:873.
Stuteville, O.H. A summary review of tissue changes incident to tooth movement. Angle Orthod. 1938; 8:1.
Swerdlow, H, Stanley, H.R, Jr. Reaction of the human dental pulp to cavity preparation. II: at 150,000 rpm with an air-water spray. J Prosthet Dent. 1959; 9:121.
Swerdlow, H. Response of the human dental pulp to amalgam restorations. Oral Surg. 1962; 15:499.
Taylor, R.G, Shklar, G, Roeber, F. The effect of laser radiation on teeth, dental pulp, and oral mucosa of experimental animals. Oral Surg. 1965; 19:786.
Thoma, K.H. Papillomatosis of the palate. Oral Surg. 1952; 5:214.
Thomas, BOA. Penetration of phenol in tooth structure. J Dent Res. 1941; 20:435.
Toller, P.A. Radioactive isotope and other investigations in a case of haemorrhagic cyst of the mandible. Br J Oral Surg. 1964; 2:86.
Toto, P.D. Mucopolysaccharide keratin dystrophy of the oral epithelium. Oral Surg. 1966; 22:47.
Tsuzuki, M. Experimental studies on the biological action of hard roentgen rays. Am J Roentgenol. 1926; 16:134.
Turrell, AJW. Allergy to denture-base materials: fallacy or reality. Br Dent J. 1966; 120:415.
Ultrasonic Dental Research Group of Chicago: Using the ultrasonic dental unit in restorative technics, II1 Dent J 25: 770, 1956
Urist, M.R, Ibsen, K.H. Chemical reactivity of mineralized tissue with oxytetracycline. Arch Pathol. 1963; 76:484.
Van, Den Akker HP, Bays, R.A, Becker, A.E. Plunging or cervical ranula. J Maxillofac Surg. 1978; 6:286.
Van, Huysen G, Fly, W. Artificial dentures and the oral mucosa. J Prosthet Dent. 1954; 4:446.
Wakely, C. The surgery of the salivary glands. Ann R Coll Surg. 1948; 3:289.
Waldo, C.M, Rothblatt, J.M. Histologic response to tooth movement in the laboratory rat. J Dent Res. 1954; 33:481.
Waldron, C.A. Solitary (hemorrhagic) cyst of the mandible. Oral Surg. 1954; 7:88.
Wallman, I.S, Hilton, H.B. Teeth pigmented by tetracycline. Lancet. 1962; 1:827.
Walters, F.J, Fridl, J.W, Nelson, R.L, Trost, J.W Oral Manifestations of Occupational Origin: an Annotated Bibliograph. 1952;
Wank, G.S, Kroll, Y.J. Occlusal trauma. an evaluation of its relationship to periodontal prostheses. Dent Clin North Am. 1981; 25(3):511–532.
Warkany, J, Hubbard, D.M. Acrodynia and mercury. J Pediat. 1953; 42:365.
Warren, S. Effects of radiation of normal tissues. Arch Pathol. 1943; 35:121–304. [34: 443, 562, 749, 917, 1070, 1942].
Watson, W.L, Scarborough, J.E. Osteoradionecrosis in intraoral cancer. Am J Roentgenol Radium Ther. 1938; 40:524.
Weinstein, R.A, Stephen, R.J, Morof, A, Choukas, N.C. Human bites: review of the literature and report of case. J Oral Surg. 1973; 31:792.
Whinery, J.G. Progressive bone cavities of the mandible. Oral Surg. 1955; 8:903.
Williams, LIJ, Rowe and Williams’ maxillofacial injuries. 2. Churchill Livingston, New York, 1994.
Witkop, C.J, Jr., Wolf, R.O. Hypoplasia and intrinsic staining of enamel following tetracycline therapy. J Am Med Assoc. 1963; 185:1008.
Wolcott, R.B, Paffenbarger, G.C, Schoonover, J.C. Direct resinous filling materials: temperature rise during polymerization. J Am Dent Assoc. 1951; 42:253.
Wood, JFL. Mucosal reaction to cobalt-chromium alloy. Br Dent J. 1974; 136:423.
Wright, R.W. Round shadows in the maxillary sinuses. Laryngoscope. 1946; 56:455.
Wu, C.W, Tai, C.F, Wang, L.F, Tsai, K.B, et al. Aspergillosis: a nidus of maxillary antrolith. Am J Otolaryngol. 2005; 26(6):426–429. [Nov-Dec].
Yamamoto, H, Okabe, H, Ooya, K, Hanaoka, S, et al. Laser effect on vital oral tissues: a preliminary investigation. J Oral Path. 1973; 1:256.
Yamamoto, H, Takagi, M. Clinicopathologic study of the postoperative maxillary cyst Oral Surg Oral Med Oral Pathol. 1986; 62(5):544–548. [Nov].
Yu, C.H, minnena, B.J, Gold, W.L. Bacterial infections complicating tongue piercing. Can J infect Dis Med Microbiol. Spring. 2010; 21(1):e70–74.
Zach, L, Brown, G.N. Pulpal effect of ultrasonic cavity preparation: preliminary report. New York Dent J. 1956; 22:9.
Zander, H.A, Burrill, D.Y. Penetration of silver nitrate solution in dentin. J Dent Res. 1943; 22:85.
Zander, H.A, Smith, H.W. Penetration of silver nitrate into dentin. J Dent Res. 1945; 24:121.
Zhong, Y, Chasen, J, Yamanajka, R, et al. Extension and density of root fillings and postoperative apical radiolucencies in the Veterans Affairs Dental Longitudinal Study. J Endod. 2008; 34(7):798–803.
Ziskin, D.E, Stowe, L.R, Zegarelli, E.V. Dilantin hyperplastic gingivitis. Am J Orthod. 1941; 27:350.
Zivkovic, S, Brkanic, T, Dacic, D, Opacic, V, et al. Smear layer in enodontics. Serbian Dental J. 2005; 52:7–19.
Zussman, W.V. Tetracycline-induced fluorescence in dentin and enamel matrix. Lab Invest. 1966; 15:589.