Chapter 7 Planning, implementing and evaluating nursing care
LEARNING OUTCOMES
Mastery of content will enable you to:
• Describe goal-setting.
• Discuss the process of selecting nursing interventions.
• Discuss the differences between independent and collaborative interventions.
• Describe the differences between care plans used in hospital and community healthcare settings.
• Discuss the differences between protocols and standing orders.
• Develop a care plan from a nursing assessment.
• Explain the relationship of implementation to the diagnostic process.
• Explain how evaluation involves critical thinking.
• Give examples of evaluation measures used to determine a client’s progress towards outcomes.
• Describe how evaluation can lead to revision or modification of a plan of care.
• Explain the interaction between evaluation and quality improvement.
Nursing assessment and the formulation of nursing diagnoses (Chapter 6) are essential to planning, implementation (the use of nursing interventions) and evaluation of nursing care. Planning involves creating client-centred goals and expected outcomes, and nursing interventions are selected to achieve the goals and outcomes of care. During planning, priorities are set in collaboration with the client, family and other members of the healthcare team. The process of planning nursing care is to first prioritise health problems, then set general goals, followed by specific client outcomes and then the selection of appropriate nursing interventions to achieve those outcomes. The appropriate selection of client outcomes will provide a base for evaluation of the care, given the client’s progress towards goals and the standard of care received.
Establishing priorities
Nursing work is complex and requires critical thinking to prioritise client problems and interventions. As a student it may be useful to apply a model or framework to help organise and guide your thinking. For example, the primary survey (ABCDE) approach provides a systematic method of assessment and prioritisation in acute care situations. Life-threatening problems are treated when encountered, before moving on to the next part of the assessment.
The hierarchy of human needs (Maslow, 1970) is another framework for prioritisation that arranges the basic human needs in levels of priority. In this model the first level is physiological: the need for air, water and food. The second level is safety and security needs, which involve physical and psychological security. The third level is love and belonging needs, including friendship, social relationships and sexual love. The fourth level encompasses esteem and self-esteem needs, which involve self-confidence, usefulness, achievement and self-worth. The final level is the need for self-actualisation, the state of fully achieving potential and having the ability to solve problems and cope realistically with life’s situations. Basic physiological and safety needs are usually the first priority. However, there may be situations where high priority must be given to the psychological, sociocultural, developmental or spiritual needs of the client.
Clients entering the healthcare system generally have unmet needs. For example, a person brought to an emergency department experiencing acute pneumonia has an unmet need for oxygenation, the most basic physiological need. An older woman living alone may be concerned about the safety of her home while hospitalised, and may have a need for psychological security from fear that her home will be burgled. You were introduced to Mr Brown and the assessment of his needs in Chapter 6, and it may be useful to review this scenario and consider the priorities of care at this point.
Priorities may be classified as high, intermediate or low depending on the urgency of the problem, the nature of the treatment indicated, and the interactions among the nursing diagnoses. Nursing diagnoses that, if untreated, could result in harm to the client or others have the highest priorities. For example, risk of violence, impaired gas exchange, decreased cardiac output and the risk of self-harm are high-priority needs. High priorities can occur in both the psychological and the physiological dimensions, and the nurse should avoid classifying only physiological nursing diagnoses as high priority. Intermediate-priority nursing diagnoses involve the non-urgent, non-life-threatening needs of the client. Low-priority nursing diagnoses are client needs that may not be directly related to a specific illness or prognosis.
Whenever possible, the client should be involved in setting priorities. In some situations, the client and nurse may assign different rankings to nursing diagnoses. If they place different values on healthcare needs and treatments, they can resolve these differences through open communication. However, when the client’s physiological and emotional needs are at stake, decisions concerning priority setting become more complex. At such times the nurse needs to work to the principles of person-centred care and find ways of working with the client and their family in finding the best way forward. When the nurse uses clinical judgment and diagnostic reasoning to assign priorities to nursing diagnoses, the needs of the client, the resources of the healthcare system and the limitations of time are considered (Carpenito-Moyet, 2008).
Critical thinking in establishing goals and expected outcomes
There are two main purposes for writing goals and expected outcomes:
1. to provide direction for individualised nursing interventions
2. to set standards for determining the effectiveness of the interventions.
Each goal and expected outcome statement must have a timeframe for evaluation. The time element depends on the nature of the problem, aetiology, overall condition of the client, and treatment setting.
Goals of care
Goals are defined as guideposts to the selection of nursing interventions and as criteria in the evaluation of those interventions. To create a plan of care, the nurse uses critical thinking skills to develop goals relevant to the client’s needs as evidenced by the assessment database and the nursing diagnoses. As the goals are developed, the nurse is simultaneously synthesising critical thinking, knowledge, experience, standards and attitudes that pertain to the client’s present healthcare needs.
The nurse’s knowledge base from scientific, sociobehavioural and nursing disciplines enables the planning of goals. For example, a client with pneumonia may have a nursing diagnosis of impaired gas exchange. The nurse’s knowledge of the pathophysiology of pneumonia and the normal respiratory anatomy and physiology, coupled with the knowledge of respiratory care principles, allows the nurse to establish the goal ‘client will achieve clear lung sounds to auscultation by 8th October’. Similarly, the nurse’s knowledge base suggests that indications of improved gas exchange will be effected in outcomes such as ‘return of oxygen saturation to > 95% on room air, absence of pulmonary secretions’. Finally, experience with other clients with pulmonary alterations allows the nurse to select interventions that were successful previously.
A client-centred goal is a specific, measurable objective designed to reflect the client’s highest possible level of wellness and independence in function. Client-centred goals require active involvement by the client. Goals should be realistic and based on client needs and resources.
For clients to participate in goal setting, they should be alert and have some degree of independence in completing activities of daily living (ADLs), problem solving and decision making. This is important, as the nurse and client are partners throughout the client’s care. If the client’s cognitive and physical impairments are so severe that they cannot actively participate in goal setting, the nursing team works with family or significant others and acts on the client’s behalf to develop client-centred goals. When developing goals, the nurse acts as an advocate for clients in developing nursing interventions to promote their return to health or to prevent further deterioration in their level of wellness or cognitive and physical function.
• CRITICAL THINKING
Can you think of other examples where the client may be unable or unwilling to participate in their care? What strategies could you use to overcome this?
Goals should not only meet the immediate needs of the client, but should also strive towards prevention and rehabilitation. Two types of goals, short-term goals and long-term goals, are developed for the client depending on the nature of the client’s need or problems and the nature of the nursing services provided.
Short-term goals
A short-term goal is one that is expected to be achieved in a short time, usually less than a week (Carpenito-Moyet, 2008). With the present healthcare system and shorter hospital stays, short-term goals are the direction for the immediate care plan. A short-term goal for a client with ineffective airway clearance, for example, may be ‘client’s lungs will remain clear’.
Long-term goals
A long-term goal is an objective that is expected to be achieved over a longer period of time, usually over weeks or months. Long-term goals may be more appropriate for problem resolution after discharge, especially from acute care settings (Carpenito-Moyet, 2008). Long-term goals are appropriate for clients in home care settings and those adapting to chronic illnesses that live in extended-care facilities, and for some clients in rehabilitation, mental health, ambulatory care and community nursing settings. For example, a long-term goal for a client with an ineffective airway clearance might be to remain free of upper respiratory infection for 6 months. These goals often focus on prevention, rehabilitation, discharge and health education. Failure to set long-term goals may prevent the client from receiving continuity of care.
Goal setting establishes the framework of the nursing care plan. Mr Brown was introduced in Chapter 6. It is now 1 day after Mr Brown had surgery for a bowel resection. His operative course had some complications. His blood loss was greater than anticipated, and his haemoglobin level is now 85 g/L. His fatigue has worsened, and his tolerance of routine postoperative leg exercises and ambulation is poor. Table 7-1 shows the progression from nursing diagnoses to goals and expected outcomes for Mr Brown. Through goals, the nurse is able to provide continuity of care and promote the best use of time and resources. Ultimately, the goal leads to the development of expected outcomes.
TABLE 7-1 EXAMPLES OF GOAL SETTING WITH EXPECTED OUTCOMES FOR MR BROWN
| NURSING DIAGNOSES |
GOALS |
EXPECTED OUTCOMES |
| Ineffective individual coping related to fear of negative prognosis |
Client will openly discuss diagnosis |
Client will ask pertinent questions about diagnosis by 5 July
Client will express fears by 5 July
Client will identify at least two strategies for dealing with fears by 6 July
|
| Ineffective airway clearance related to incisional pain |
Client’s lungs will remain clear throughout postoperative period |
Client will turn, cough and deep-breathe every hour
Client achieves incentive spirometer goal of 90% every 2 hours
Client pain level remains < 3 on a scale of 0–10
|
| Knowledge deficit regarding postoperative care at home related to inexperience |
Client will state four postoperative risks before discharge |
Client drinks 2–3 L of fluid every day by 5 July
Client will name three signs of wound infection by 5 July
Client will demonstrate aseptic wound care by 5 July
Client will state home activity restrictions by 5 July
|
| Altered peripheral tissue perfusion related to postoperative venous status and risk of thrombophlebitis |
Client will maintain adequate tissue perfusion by discharge |
Client performs active range of motion exercises every 2 hours while restricted to bed
Client’s toes remain warm, dry with capillary refill of < 2 seconds
Client increases ambulation by 15 metres every day
|
Expected outcomes
An expected outcome is the specific, step-by-step objective that leads to attainment of the goal and the resolution of the aetiology for the nursing diagnosis. An outcome is a measurable change of the client’s status in response to nursing care (Carpenito-Moyet, 2008). Client outcomes have been referred to as the ultimate definition of effectiveness and efficiency, and there is an increased emphasis on identifying and measuring the results of nursing interventions and practice. Outcomes are the desired responses of a client’s condition in the physiological, social, emotional, developmental or spiritual dimensions. This change in condition is documented through observable or measurable client responses (Scherb and Weydt, 2009).
The expected outcomes determine when a specific, client-centred goal has been met and later help in the evaluation of the response to nursing care and resolution of the nursing diagnosis (see Table 7-1). Expected outcomes provide a direction for nursing activities because they are projected before nursing actions are selected. They provide a projected timespan for goal attainment and an opportunity to state any additional resources that may be required to achieve the goal, including additional equipment, personnel or knowledge. The nurse uses expected outcomes as criteria to evaluate the effectiveness of nursing activities.
When writing expected outcomes, the nurse should ensure that the outcome statement is written in measurable behavioural terms. A useful mnemonic here is RUMBA: that is, outcome statements should be realistic (R), unambiguous (U), measureable (M), behavioural (B) and achievable (A). This allows the nurse to note specifically the behaviour expected for resolution of the client’s problem. The expected outcome statements should be written sequentially, with timeframes. This provides an order for the interventions, as well as a time reference for resolution of the problem.
In the current healthcare environment, much attention is given to measuring outcomes of nursing interventions (see Research highlight). It is important to reflect on the goals and expected outcomes of care to ensure that they are specific to the care-delivery setting, the client, the discipline delivering the care, and the underlying medical diagnosis.
Developing a plan of care must also incorporate the role of other healthcare disciplines, the family and community resources. In the planning of care, the nurse displays attitudes such as creativity and perseverance to develop a plan of care that is tailored to the client/family needs and has measurable outcomes.
Guidelines for writing goals and expected outcomes
Client-centred factors
Because nursing care is directed by nursing diagnoses, statements of goals and expected outcomes of care focus on the client and underlying diagnosis. These statements reflect expected client behaviour and responses as a result of nursing interventions.
Research focus
The value of systematic development and validation of an adherence promoting intervention for leg ulcer patients.
Research abstract
Exploring the perspectives of both nurses and clients during the development of an intervention increases the likelihood that the intervention is feasible and attuned to patients’ needs. An adherence-promoting intervention for leg ulcer clients was developed based on van Miegle’s model, which requires a systematic development using clients’ experiences and professionals’ views on good care. The model employs a cyclical process of trying out, evaluating, revising and reassessing the adapted intervention in clients. The study required an examination of current practice, including an extensive literature review, an intervention design, which combined cognitive, behavioural and affective elements and different actions, and a validation process.
The focus was on wearing compression stockings, performing leg exercises, physical activity and leg elevation.
Evidence-based practice
• Using a theoretical model enabled the development of a nursing intervention to promote adherence.
• Client involvement and an exploration of the client’s perspective are important to designing and refining a nursing intervention.
• Systematic development of nursing interventions is critical to the development of evidence-based nursing practice.
Reference
Van Hecke A, et al. Systematic development and validation of a nursing intervention: the case of lifestyle adherence promotion in patients with leg ulcers. J Adv Nurs. 2011;67:662–676.
Singular factors
Each goal and expected outcome statement should refer to only one behavioural response. This singularity provides a precise method of evaluating client response to the nursing action. For example, an incorrect outcome statement might read ‘client’s lungs will be clear on auscultation, and respiratory rate will be 20 per minute by 22 August’. If the lungs are clear but the respiratory rate is 28 per minute after nursing actions, it is difficult to determine whether the expected outcome has been achieved. By splitting the statement into two parts—‘lungs will be clear on auscultation by 22 August’ and ‘respiratory rate will be 20 per minute by 22 August’—the nurse can determine specifically the outcome that has been achieved.
Observable factors
Nursing is required to objectively demonstrate the effectiveness of nursing interventions on the client’s level of health. Observable changes can occur in physiological findings and in the client’s level of knowledge and behaviour. The results can be obtained by directly asking the client about the condition or by using assessment skills. Examples of outcomes involving assessment skills are ‘lungs will be clear on auscultation by 22 August’ and ‘purulent wound drainage will cease by 12 September’.
Measurable factors
Goals and expected outcomes are written to give the nurse a standard against which to measure the client’s response to nursing care. Examples are ‘body temperature will remain at 37.2°C’ and ‘apical pulse will remain between 60 and 100 beats per minute’. A goal or an outcome stated in measurable terms allows the nurse to objectively quantify changes in the client’s status.
Common mistakes are made when the nurse uses vague qualifiers such as ‘normal’, ‘stable’, ‘acceptable’ or ‘sufficient’ in the expected outcome statement. Terms specifically describing quality, quantity, frequency and weight allow the nurse to evaluate whether the expected outcome was achieved.
Time-limited factors
The timeframe for each goal and expected outcome indicates when the expected response should occur. Timeframes help the nurse and client determine that progress is being made at a reasonable rate. When the date of evaluation arrives, the nurse assesses the client to determine whether that particular expected outcome has been reached. If the outcome is not achieved, but it is still appropriate for the client’s care, another evaluation date is set.
Mutual factors
Mutual setting of goals and expected outcomes ensures that the client and nurse agree on the direction and time limits of care. Mutual goal setting can increase the client’s motivation and cooperation, because the nurse does not impose personal values on the client. However, using experience and acquired knowledge, the nurse may need to direct some of the goals and expected outcomes to keep the client physically and emotionally stable and safe. For example, a client may be refusing pain medication because of fear of addiction. The subsequent pain is preventing mobilisation and exercise, thus giving the potential for lung and bladder stasis and infection. The nurse remains alert to cues and will create goals and interventions to ensure the optimal outcome for the client.
Realistic factors
Short-term, realistic goals and expected outcomes can quickly provide the client and nurse with a sense of accomplishment. In turn, this sense of accomplishment can increase the client’s motivation and cooperation. When establishing realistic goals, the nurse, through assessment, must know:
1. the resources of the healthcare facility, family and client
2. the client’s physiological, emotional, cognitive and sociocultural potential, and
3. the economic cost and resources available to reach expected outcomes in a timely manner.
Establishing goals and expected outcomes without a thorough assessment of client, environment or resources can be frustrating to the client and nurse because the plan then contains unrealistic goals.
Expected outcomes measurement
It is imperative for nurses to measure the outcome of care. The International Council of Nurses (ICN) is contributing to the development of meaningful measurement language for the classification of nursing care activities. The International Classification for Nursing Practice (ICNP®) was commenced in 1989. National nurses’ associations such as the Royal College of Nursing, Australia contribute to the development of the system (Conrick, 2005).
Expected outcomes are the expected results of a goal-oriented process. They are statements of progressive, step-by-step responses or behaviours that the client needs to accomplish to achieve the goals of care provided. When outcomes are achieved, the related factors for a nursing diagnosis no longer exist. For example, for a nursing diagnosis of impaired skin integrity related to pressure of physical immobilisation, the client must achieve the goal of attaining intact skin in the area of injury. This will be accomplished by meeting the outcomes of ‘the skin lesion will be clean without drainage in 3 days’ and showing evidence of healing through ‘reduction in size (by 1 cm) and inflammation in 1 week’. If the outcomes are met, the nurse has successfully eliminated pressure over the skin and used therapies that have healed the skin lesion. Expected outcomes have short timeframes (depending on the healthcare setting) and include as few as one or two intervention sessions.
After a specified interval or when all interventions in the plan of care have been completed, the nurse evaluates the client’s ability to demonstrate the behaviour or response stated in the outcomes. Evaluation of each expected outcome and its place in the sequence of care is essential. Failure to evaluate each expected outcome results in an inability to determine where the sequence faltered. In other words, the nurse is not able to revise and redirect the plan of care at the most appropriate time. Achievement of clinically useful and measurable client outcomes sensitive to nursing interventions is needed to determine the effectiveness of planned interventions, and can improve the client’s level of health.
If the client achieves the expected outcomes, the nurse either continues the care plan or discontinues interventions because the goal of care is met. If evaluation determines that the expected outcomes were not met or only partially met, the nurse begins reassessment and revision of the care plan.
• CRITICAL THINKING
You are caring for a client who has just been admitted to the ward for a laparoscopic cholecystectomy. What actions would you undertake in order to develop goals and expected outcomes of care for this woman?
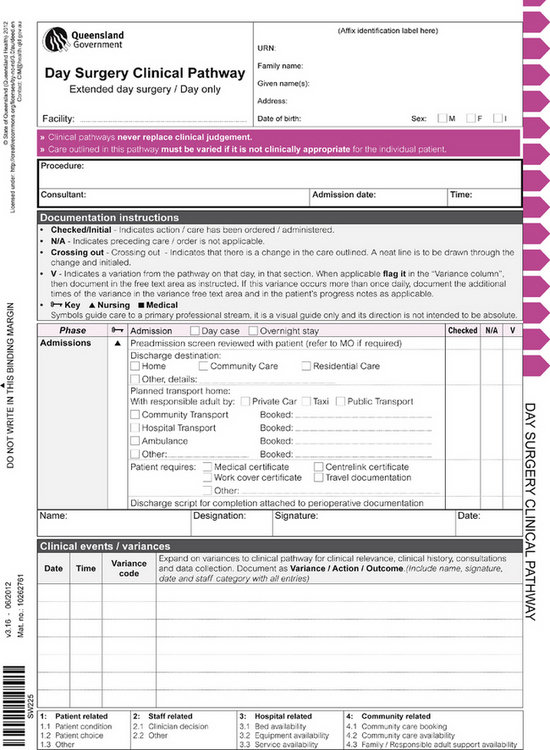
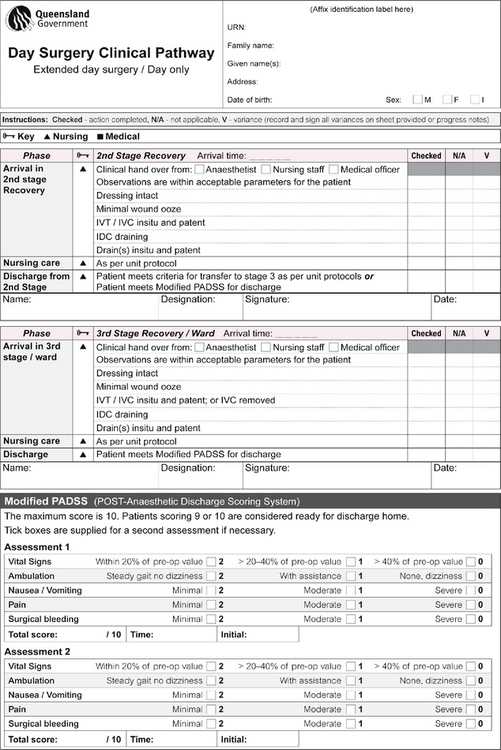
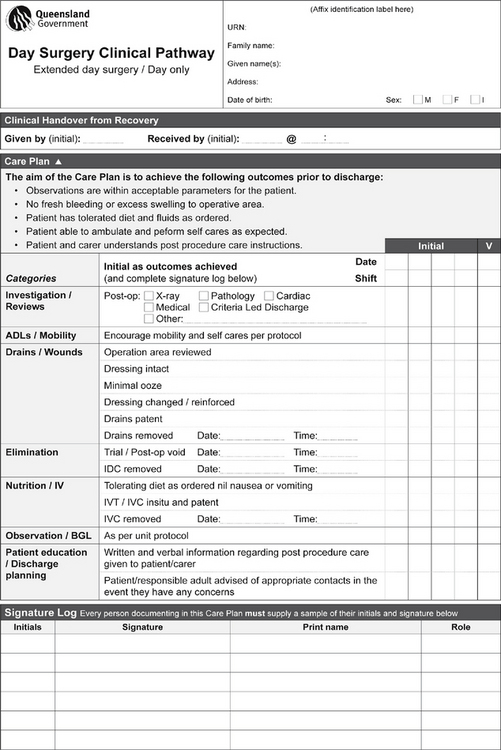
Planning nursing care
There are many ways to communicate a client’s nursing care. One is the nursing care plan, which includes the nursing diagnoses, goals, expected outcomes and specific nursing activities and strategies. In many settings, nursing care plans are integrated into multidisciplinary plans of care. The nursing component of a multidisciplinary plan is easily recognisable. A second way is critical pathways, often known as clinical pathways. Critical or clinical pathways are multidisciplinary treatment plans that prescribe interventions and the timeframe for achieving expected outcomes for selected clients over a projected length of stay. Many health institutions also utilise protocols and standing orders which are integrated into an individualised plan of care.
Purpose of care plans
The nursing care plan is a written guideline for client care. Written care plans document the client’s healthcare needs. In addition, the written care plan communicates to other nurses and healthcare professionals the client’s pertinent assessment data, a list of problems and therapies. A written care plan is designed to decrease the risk of incomplete, incorrect or inaccurate care.
The care plan is organised so that any nurse can quickly identify the nursing actions to be delivered. In hospitals, outpatient clinics and community-based settings, the client often receives care from more than one nurse, medical officer or allied health professional. The written nursing care plan makes possible the coordination of nursing care, subspecialty consultations and scheduling of diagnostic tests.
The care plan can also identify and coordinate resources, human, physical and financial, required to deliver nursing care. The nursing care plan enhances the continuity of nursing care by listing specific nursing actions necessary to achieve the goals of care. Written nursing care plans organise information exchanged by nurses in change-of-shift reports. Nurses focus these reports on nursing care and treatments delineated in care plans. At the end of shifts, nurses discuss care plans with the next caregivers. Thus all nurses are able to discuss current and pertinent information about the client’s care plan.
The written care plan also includes the long-term needs of the client. Incorporating the goals of the care plan into discharge planning is particularly important for a client who will be undergoing long-term rehabilitation in the community. A complete care plan enhances the continuity of nursing care between nurses in the hospital and in the community.
When developing an individualised care plan, the nurse involves the client and family. The family can help the client meet health goals. In addition, meeting some of the family’s needs may improve the client’s level of wellness.
The last items documented on the nursing care plan are the expected outcomes used in evaluation of care. Proper listing of the outcomes provides the nurse with objective statements that help determine whether the goals of care have been achieved. The complete care plan is the blueprint for nursing action. The nursing care plan is also an important legal document.
Care plans in various settings
The format of the nursing care plan varies from one healthcare setting to another. For example, in a hospital, a care plan may consist of columns for assessment, goals, interventions and expected outcomes. The nursing care plan developed for the client returning home is usually based solely on long-term health needs. In addition, the client, family and significant others are more involved and assume more responsibility for care because the client is receiving nursing care in the home.
In a community health setting, the care plan may be in a narrative form. Despite variations, the overall purpose of the care plan is to provide written guidelines so that the healthcare needs of the client and subsequent therapies are communicated to all healthcare team members. Sample care plans are included in the clinical chapters of this text. It is also a good learning resource to collect, with permission, sample care plans from clinical placement experiences.
Nursing students also frequently learn to write and use a nursing care plan as part of their education. The student care plan is essential for learning the problem-solving technique, the nursing process, skills of written communication and organisational skills needed for nursing care. Most importantly, by using the nursing care plan, students can apply the knowledge gained to a clinical situation.
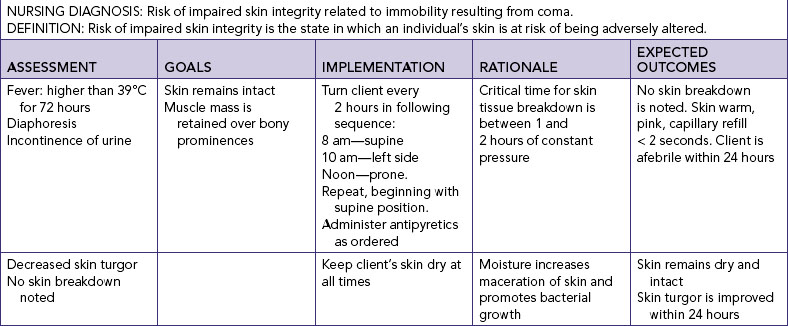
The student care plan is more elaborate than a care plan in a hospital or community healthcare agency because its purpose is to teach the process of planning care. To learn the care planning process, the student must progress in a step-by-step manner, beginning with assessment and ending with evaluation. Student care plans vary from one educational program to another, and between beginning and more advanced students. Some educational institutions model the student care plan on the care plan used in an affiliated healthcare agency. The only modification might be that the instructor requires the beginning student to include the scientific rationale for the nursing interventions selected (see Table 7-2).
Planning care for clients in community-based settings, such as clinics, community centres or clients’ homes, involves the same principles of nursing practice. However, in these settings the nurse must complete a more comprehensive community, home and family assessment. In this setting, the client/family unit is in equal partnership with healthcare professionals. Ultimately, the client/family must be able to independently provide the majority of healthcare. The nurse designs a plan to:
1. educate the client/family about the necessary care techniques
2. teach the client/family how to integrate care with family activities, and
3. allow the client/family to assume a greater percentage of care in graduated increments.
The plan is designed to include the nurse’s and the client’s/family’s evaluation of expected outcomes.
Writing the nursing care plan
The nursing diagnosis with the highest priority is the starting point for the nursing care plan, and is followed by other nursing diagnoses in order of assigned priority. The example in Table 7-2 shows how to write a care plan in a five-column format. In the assessment column (column 1), the nurse includes all data relevant to the corresponding nursing diagnosis. The previously developed goals are written in the next column (column 2). At this point, the nurse begins to translate the short- and long-term goals into action plans that anticipate the needs of the client, coordinate nursing care and select appropriate nursing interventions.
The nurse writes the action plan in the implementation column (column 3). Each nursing action is written to include information necessary to implement nursing care. It may help the beginning nurse to ask whether the stated interventions answer the following questions:
• What is the intervention?
• When should each intervention be implemented?
• How should each intervention be performed?
• What resources may be needed for the intervention?
• Who should be involved in each aspect of intervention?
In addition, the student nurse should understand the scientific rationale (column 4) for a specific intervention. Non-specific nursing interventions result in incomplete or inaccurate nursing care, lack of continuity among caregivers and poor use of resources.
Common omissions in writing nursing interventions include action, frequency, quantity, method or person to perform the action. These errors can occur if the nurse is unfamiliar with the planning process. Table 7-3 illustrates these types of errors by showing incorrect and correct statements of nursing interventions.
TABLE 7-3 COMMON ERRORS IN WRITING NURSING INTERVENTIONS
| TYPE OF ERROR |
INCORRECTLY STATED NURSING INTERVENTION |
CORRECTLY STATED NURSING INTERVENTION |
| Failure to precisely or completely indicate nursing actions |
Nurse assistant will turn client every 2 hours |
Nurse assistant will turn client every 2 hours, using the following schedule:
8 am—supine
10 am—left side
Noon—prone
2 pm—right side
Repeat sequence at 4 pm and at midnight
|
| Failure to indicate frequency |
Nurse assistant will observe client cough and deep-breathe |
Nurse assistant will observe client cough and deep-breathe at 10 am–2 pm–6 pm–10 pm |
| Failure to indicate quantity |
Primary nurse will provide hydrogen peroxide (H2O2) mouthwash to client every 2 hours while awake: 8-10-12-2-4-6-8-10 |
Primary nurse will provide 50 mL of H2O2 mouthwash to client every 2 hours while awake: 8-10-12-2-4-6-8-10 |
| Failure to indicate method |
Primary nurse will change client’s dressing once a shift: 6 am-2 pm-10 pm |
Primary nurse will replace client’s dressing, with Neosporin ointment to wound and two dry 10 cm × 10 cm dressings secured with hypoallergenic tape, once a shift: 2 pm–10 pm–6 am |
| Failure to indicate person to perform the action |
Irrigate nasogastric (NG) tube every 2 hours (even) round the clock with 30 mL of normal saline (NS) |
Primary nurse will irrigate NG tube every 2 hours (even) around the clock with 30 mL NS |
Column 5 of the nursing care plan contains the projected outcomes previously identified. Listing the outcomes on the care plan provides a written estimation of when the goal of care is to be achieved. The nurse can enter when outcomes are met, thus indicating when a particular nursing diagnosis is no longer relevant to the client’s plan of care.
Critical (or clinical) pathways
Critical pathways allow staff from all disciplines, such as nursing, medicine, pharmacy and social work, to develop integrated care plans for a projected length of stay or number of visits for clients with a specific case type (see example in Figure 7-1). For example, a pathway for a trans-urethral resection of the prostate (TURP) may recommend on a day-by-day basis the client’s activities, consults, procedures and discharge planning activities, and educational topics expected for the client’s progression through the process (see Chapter 37 for example; Johnson and Ellis, 1999). The nurse and other healthcare team members use the pathway to monitor a client’s progress and as a documentation tool.
The writing of a critical pathway is a lengthy process, involving all members of a multidisciplinary healthcare team. Often it takes many weeks of research and review for a team to agree on the components of a critical pathway. Once developed, critical pathways become a case management tool that delineates desired interventions and client outcomes within specific timeframes. To write and use a critical pathway, the nurse must understand each component of the nursing process. Critical pathways are multidisciplinary, outcome-based care plans.
Protocols and standing orders
A protocol is a written plan specifying the procedures to be followed during care of a client with a selected clinical condition or situation, such as care of a postoperative client. Nurses providing primary care for clients in an outpatient setting may follow treatment and diagnostic protocol. In such a setting, nurses assess the client and identify abnormalities. The protocol delineates the conditions that nurses are permitted to treat, such as controlled hypertension, and the types of treatment they are permitted to administer, such as immunisations.
A protocol can also be strictly within the framework of nursing, such as a protocol for admission and discharge, pain management, or initiating cardiopulmonary resuscitation. Protocols are also used in interdisciplinary settings for diagnostic testing and physical, occupational and speech therapies.
A standing order is a document containing orders for the conduct of routine therapies, monitoring guidelines and/or diagnostic procedures for specific clients with identified clinical problems. The orders direct the conduct of client care in various clinical settings. Standing orders are approved and signed by the medical officer in charge of care before their implementation. They are commonly found in critical care settings, where clients’ needs can change rapidly and require immediate attention. Such a standing order might specify a certain drug, such as lignocaine or propranolol, for an irregular heart rhythm. After assessing the client and identifying the irregular rhythm, the critical care nurse gives the specified medication without first notifying medical staff. Standing orders are also common in the community and remote health settings, in which the nurse encounters situations that do not permit immediate contact with a doctor.
Thus, standing orders and protocols give the nurse legal protection to intervene appropriately in the client’s best interest. Before implementing any therapy, including those in protocols and standing orders, the nurse must use sound judgment in determining whether the intervention is correct and appropriate. Second, the nurse implementing any intervention has the responsibility of obtaining correct theoretical knowledge and developing the clinical competency necessary to perform the intervention.
Critical thinking in designing nursing interventions
Nursing interventions, strategies or actions are selected after goals and expected outcomes are established. Nursing interventions are those actions designed to help the client move from the present level of health to that which is described in the goal and measured with the expected outcomes. A nursing intervention is defined as any treatment based on clinical judgment and knowledge that a nurse performs to enhance client outcomes.
The client may require intervention in the form of a wound dressing, treatment for the current condition, client–family education, treatment to prevent future health problems, or social, emotional or physical support. Interventions that promote culturally sensitive care increase the chances of attaining the goals and expected outcomes of nursing care. Implementation is a continuous process and interacts with the other components of the nursing process. As the nurse carries out interventions, the client’s condition can change or the client may respond to the interventions as expected.
When choosing suitable nursing interventions, the nurse uses critical thinking by applying attitudes and standards and synthesising information from the client’s assessment data, previous knowledge and experience to select interventions that will successfully meet established goals and expected outcomes for each diagnostic statement (Eizenberg, 2010). In addition, to initiate the intervention the nurse must:
1. know the scientific rationale for the intervention (see, for example, Table 7-2)
2. possess the necessary psychomotor and interpersonal skills, and
3. be able to function within a particular setting to use the available healthcare resources effectively.
Examples of specific clinical interventions and their scientific rationale are given throughout the clinical chapters of this text.
Types of interventions
Nurse-initiated interventions
Nurse-initiated interventions are the independent response of the nurse to the client’s healthcare needs and nursing diagnoses. This type of intervention is an autonomous action based on scientific rationale that is executed to benefit the client in a predicted way related to the nursing diagnosis and client-centred goals (Carpenito-Moyet, 2008). Nurse-initiated interventions involve aspects of professional nursing practice covered by licence and law. These interventions require no supervision or direction from others. For example, interventions for increasing a client’s knowledge about adequate nutrition or ADLs related to hygiene are independent nursing actions.
Nurse-initiated interventions do not require a medical prescription. According to the various state Acts and Regulations governing the conduct of nursing, actions pertaining to ADLs, health education, health promotion and counselling are within the domain of nursing practice. These Acts and Regulations delineate the legal scope of the practice of nursing within the boundaries of their jurisdiction.
Several factors make decision making more difficult when choosing among nurse-initiated (independent) nursing interventions. One factor is the absence of objective data concerning the probable effects or results of the interventions. Evidence-based literature on the effectiveness of nursing interventions is increasingly available through online databases such as the Cochrane Collaboration (see Chapter 8), but much work remains to be done. A second factor is that nurse-initiated interventions are often not mutually exclusive. For example, the nurse may need to include relaxation, massage and guided imagery techniques with prescribed analgesics for pain management. The nurse implements the care plan using the knowledge bases that were necessary for care planning and to complete the planned interventions most effectively. In addition, the nurse applies previous clinical experiences in using specific interventions. Thus, to each clinical situation the nurse brings an experiential base of what has worked and what did not work in certain situations. Before implementing a plan of care, the nurse is aware of both professional standards of practice and the agency’s standards. It is important to know what the guidelines are for frequency of procedures and to whom the procedures may be delegated. Attitudes of independent thinking and responsibility and authority enable the nurse to reflect on the care delivered. Creativity and self-discipline guide the nurse in reviewing, modifying and implementing activities.
Collaborative interventions
Collaborative interventions are therapies that require the knowledge, skill and expertise of multiple healthcare professionals. Nurses collaborate with other members of the healthcare team when the nurse has identified a client problem that cannot be solved by the RN alone. For example, nurses administer treatments prescribed by advanced practitioners, such as medication, implementing an invasive procedure or changing a dressing. It is not always within the legal practice of nursing for the nurse to prescribe and order these treatments, but nurses have ethical and legal obligations to assess all planned care. Nurses are not relieved of malpractice liability simply because they were administering treatment as prescribed. For example, when administering medications, the nurse is responsible for knowing the classification of the drug, its physiological action, normal dosage, side effects and nursing interventions related to its action or side effects. With an invasive procedure or dressing change, the nurse is responsible for knowing when the procedure is necessary, the clinical skills necessary to complete it, and its expected outcome and possible side effects. The nurse is also responsible for adequate preparation of the client and proper communication of the results.
When a specific diagnostic or laboratory test is prescribed, the nurse is responsible for knowing when the test is scheduled, preparing the client, and knowing the normal findings and nursing implications associated with it. When encountering collaborative interventions, the nurse does not automatically implement the therapy but must determine whether it is appropriate for the client. Every nurse encounters an inappropriate or incorrect order at some time. The nurse with a strong knowledge base recognises the error and seeks to correct it. The ability to recognise and query incorrect therapies is competent nursing practice, and it protects the client and members of the healthcare team. The nurse carrying out an incorrect or inappropriate intervention is as much in error as the person who wrote or transcribed the original order, and is liable for any complications resulting from the error.
Consider the clinical example of Mrs Joachim, a 72-year-old woman, who is a hemiplegic from a recent cerebrovascular accident (stroke) which has also severely affected her speech. She is unable to make herself understood, and is anxious and frustrated by her futile efforts. She is also at risk of problems related to impaired mobility, and she is unable to independently complete ADLs. In order for Mrs Joachim to maintain her present level of health, she requires multiple interventions, including nursing interventions to prevent pressure ulcer development, physiotherapy interventions to prevent musculoskeletal changes from immobility, speech therapy interventions for communication difficulties and occupational therapy interventions for eating and hygiene needs. Caring for this client requires the coordination of collaborative interventions from multiple healthcare professionals, all directed towards the long-term goal of maintaining her present level of health.
Consultation may occur at any step in the nursing process, but it is needed most often in the planning and intervention steps, when the nurse is more likely to identify a problem requiring additional knowledge, skills or resources. Consultation is a process in which the expertise of a specialist is sought to identify ways to handle problems in client management or the planning and implementation of programs. In clinical nursing, consultation is used to solve problems in the delivery of nursing care or the use of resources. Nurse consultants are most often approached for advice about difficult clinical problems. Nurses are consulted for their clinical expertise, client education skills or staff education skills. For example, a nurse encountering a client with a recent colostomy might request a consultation from an enterostomal therapist to determine the materials needed to clean the colostomy site and the specific techniques to use during the procedure. Consultation increases the nurse’s knowledge about the problem and helps in learning skills and obtaining the resources needed to solve the problem. After the consultation, the nurse may be able to resolve similar problems in the future. Consultation is also used when the exact problem remains unclear. A consultant objectively entering a situation can more clearly assess and identify the exact nature of the problem, whether it is to do with clients, personnel or equipment.
Selection of interventions
When selecting interventions for a client, the nurse thinks about six factors:
1. characteristics of the nursing diagnosis
2. expected outcomes
3. research base (nursing knowledge) for the interventions
4. feasibility of the interventions
5. acceptability to the client, and
6. competencies of the nurse (Carpenito-Moyet, 2008).
The nurse reviews standardised care plans, critical pathways, policy or procedure manuals, textbooks and nursing and related healthcare literature, and collaborates with other health professionals. The nurse also reviews previous experiences, client needs and priorities to select nursing interventions that have the best chance of achieving the expected outcomes. As the nurse gains experience, this deliberation process becomes more efficient and experience-based. Collaboration and consultation complete the selection of interventions. Through collaboration, the nurse is able to tap the best resources to tailor the nursing actions. During collaboration the nurse includes the client and/or family in selecting suitable interventions.
Critical thinking and the implementation process
The nurse must adequately and thoroughly prepare before implementing the care plan. This preparation ensures efficient, safe and effective nursing care. The implementation component of the nursing process has five steps:
1. reassessing the client
2. reviewing and revising the existing nursing care plan
3. organising resources and care delivery
4. anticipating and preventing complications, and
5. implementing nursing interventions.
Reviewing and revising the existing nursing care plan
Before beginning care, the nurse reviews the care plan and compares it with assessment data to validate the stated nursing diagnoses and determine whether the nursing interventions are the most appropriate for the clinical situation. If the client’s status has changed and the nursing diagnosis and related nursing interventions are no longer appropriate, the nursing care plan needs to be modified.
Modification of the existing written care plan includes several steps. First, data in the assessment column are revised to reflect the client’s current status. New data entered in the care plan should be dated to inform other members of the healthcare team of the time that the change occurred.
Second, nursing diagnoses are revised. Those that are no longer relevant are deleted, and new ones are added and dated. Because the client’s status and healthcare needs have changed, the priorities, goals and expected outcomes must also be revised. The revisions are also dated on the care plan.
Third, specific implementation methods are revised to correspond to the new nursing diagnoses and client goals. This revision reflects the client’s present status. In addition, revised implementation can include the client’s specific needs for healthcare resources, such as a specific form of dressing.
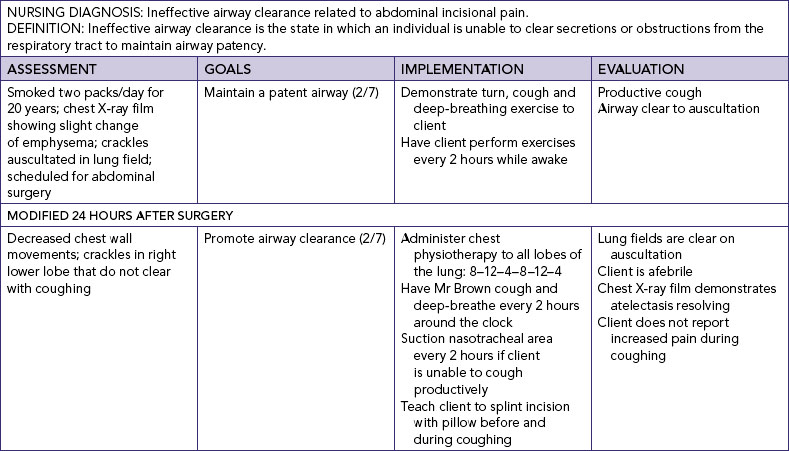
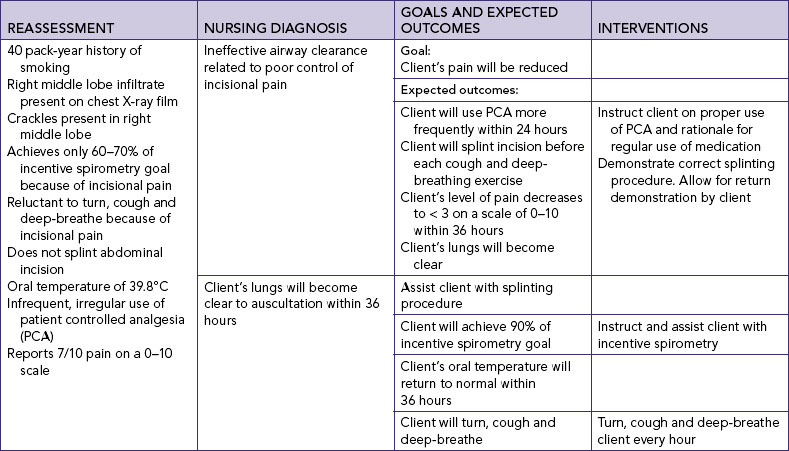
Finally, the nurse determines what methods of evaluation will be used. For example, a preoperative care plan was developed for Mr Brown. As he progressed through the postoperative period, his nursing needs changed. The nurse made modifications in the care plan for one nursing diagnosis: ineffective breathing pattern after surgery related to abdominal incisional pain. On the second postoperative day the nurse assessed the client and noted decreased chest wall movements, crackles that were auscultated in the right lower lobes and an elevated temperature (39°C). Mr Brown had a standing order for a chest X-ray examination, which was taken immediately and revealed a right lower lobe collapse. The nursing diagnosis was revised to read ineffective airway clearance related to abdominal incisional pain (Table 7-4). The nursing diagnostic label was revised because of the presence of right lower lobe crackles and decreased chest wall movement. The goal of maintaining a patent airway was still appropriate. Specific new nursing interventions were developed to help achieve a patent airway. Finally, the nurse determined the method of evaluation for the new clinical problem.
Organising resources and care delivery
A facility’s resources include equipment and skilled personnel. Organisation of equipment and personnel makes efficient, skilled client care possible. After a plan of care is determined, the nurse prepares the necessary supplies and decides on the time and provider of care. Preparation for care delivery also involves preparing the environment and client for nursing intervention.
Equipment
All necessary supplies should be gathered and put in a convenient location, usually where they will be used, before implementing the care plan. Extra supplies should be available in case of mishaps. By having extra sterile gloves, for example, the nurse anticipates the possibility of a break in aseptic technique. The nurse also arranges the supplies in the order in which they will be used.
Personnel
Before intervention, the nurse must consider the competencies of personnel available and the model of care delivery being used. Agency policies also help to clarify what interventions various levels of staff can perform. Nursing care delivery systems vary among facilities and must be considered when allocating resources. The system by which nursing is organised determines the way in which personnel are designated for client care delivery. The most common types of nursing delivery systems are functional, team, total client care, primary nursing and case management; review of these systems can be found in later chapters.
Depending on the system of healthcare delivery, the nurse who develops the care plan may not perform all of the nursing interventions. Some activities may be delegated to other members of the healthcare team and coordinated by the nurse. When delegating aspects of a client’s care to another staff member, the nurse assigning the tasks must ensure that each task is appropriately assigned and completed according to the standard of care.
Environment
Environmental factors influence the delivery and reception of care. The surroundings in which nursing activities occur should be safe and conducive to the implementation of the therapy. If the client has sensory deficits, physical disability or an alteration in level of consciousness, the environment must be arranged to prevent injury. Having special rooms, rearranging furniture and equipment, keeping rooms free of clutter and providing for additional personnel are examples of creating safe surroundings.
Privacy promotes relaxation when body parts are exposed. Reducing distractions enhances a client’s learning opportunities. Adequate space and lighting promotes efficiency when procedures are performed.
Client
Making sure the client is comfortable before initiating interventions enables the client to participate more fully. For example, if client alertness is needed, the dose of pain medication should be enough to relieve discomfort but not cause sedation. The nurse should also consider the client’s level of endurance, and plan only the amount of activity that the client can comfortably tolerate.
Awareness of the client’s psychosocial needs helps the nurse to create a favourable emotional climate. Some clients feel reassured by having a significant other present to lend encouragement and moral support. Other strategies include planning sufficient time or multiple opportunities for the client to work through and ventilate feelings and anxieties.
Anticipating and preventing complications
Risks to the client arise from both illness and treatment. The nurse must identify these risks, evaluate the relative benefit of the treatment versus the risk and initiate risk-prevention measures.
Many client conditions place the client at risk of additional complications. For example, the client with pre-existing left-sided paralysis following a stroke 2 years earlier is at risk of developing a pressure ulcer following surgery that limits mobility. Some nursing procedures also pose risks for the client. For instance, the client receiving enteric feeding through a nasogastric tube is at risk of aspiration. The nurse should elevate the head of the bed and have pharyngeal suction equipment at the bedside before initiating the feedings.
Identifying areas of assistance
Some nursing situations require the nurse to get help from additional personnel, knowledge and/or nursing skills. For example, a nurse assigned to care for an overweight, immobilised client may need additional personnel to help turn, transfer and position the client. The nurse needs to determine the number of additional personnel and when they are needed.
Some nursing situations require additional knowledge and skills, as well as additional personnel. A nurse needs additional knowledge when administering a new medication or implementing a new procedure. Such information can be obtained from a hospital’s procedure or policy manual. If the nurse is still uncertain about the new procedure, other members of the healthcare team can be consulted.
Because of the continual growth of healthcare professions and related technology, a nurse may lack the skills to perform a new procedure. When this occurs, information about the procedure is obtained from the literature and the agency’s procedure book, and another nurse who has completed the procedure correctly and safely can provide assistance and guidance. Asking for help occurs often in all types of nursing practice, and is a learning process that continues throughout educational experiences and into professional development.
Implementing nursing interventions
The nurse selects from the following nursing intervention methods to achieve the client care goals:
• Performing, assisting or directing the performance of ADLs, activities usually performed in the course of a normal day; they include walking, eating, dressing, bathing, brushing the teeth and grooming.
• Counselling and teaching the client and family. Counselling is an implementation method that helps the client use a problem-solving process to recognise and manage stress and to facilitate interpersonal relationships among the client, family and healthcare team. Teaching presents correct principles, procedures and techniques of healthcare to clients and informs clients about their health status.
• Providing direct care to achieve client-centred goals; the nurse initiates interventions to compensate for adverse reactions, uses preventive measures in providing care, applies correct techniques in administering care and preparing the client for special procedures and initiates life-saving measures in emergency situations. The specific knowledge and skills needed to carry out these nursing procedures are detailed in subsequent chapters.
• Delegating, supervising and evaluating the work of other staff members recording and exchanging information relevant to the client’s continued care.
Nursing practice includes cognitive, interpersonal and psychomotor (technical) skills. Each type of skill is needed to implement interventions. The nurse is responsible for knowing when one of these methods is preferred over another, and for having the necessary theoretical knowledge and psychomotor skills to implement each.
Achieving a client’s goals of care
The client’s healthcare goals can be achieved by:
1. providing an environment conducive to meeting such goals
2. adjusting care in accordance with the client’s expressed or implied needs
3. stimulating and motivating clients, thereby enabling them to achieve self-care and independence, and
4. encouraging clients to accept care or adhere to the treatment regimen.
For each nursing intervention, the nurse and client work together to meet the mutually developed goals. The nurse assumes a more active or more passive role depending on the intervention.
An early step in establishing an appropriate environment is to familiarise clients and families with the healthcare agency. If it is a hospital, clients need to be shown to their rooms and introduced to the healthcare team and other clients. Clients in clinics should be informed of clinic policies and procedures, shown the location of restrooms and cafeterias and introduced to the healthcare team. When clients receive care in the home, the nurse should take time to acquaint clients and their families with the purposes and expectations of the home visits.
Whether clients are in a hospital, outpatient clinic or community setting, the nurse takes measures to provide privacy. In an environment of privacy, clients may feel free to share concerns, ask questions about their diagnosis and treatment and resolve personal problems.
Nursing care and other therapeutic measures are designed to meet the client’s needs. As a further help in attaining healthcare goals, the nursing care plan should be flexible so that the client is not placed in a fixed routine. The degree of flexibility, however, depends on the nature of the need, the severity of the client’s disability or illness and the client’s dependence on nursing care. Clients with severe and chronic diseases are encouraged to increase their levels of self-care and independence. To avoid discouraging clients, it is best to progress gradually. The care plan is implemented so that clients successfully achieve one level of independence before attempting the next.
In the clinical example, each day includes achievable tasks for Mr Altmann. The tasks are sequenced for the following reasons:
1. each task was developed with the knowledge that Mr Altmann could successfully complete the activity
2. a sequence of successes will motivate Mr Altmann to continue with the plan, and
3. the sequence was designed to gradually increase Mr Altmann’s activity tolerance.
Clients with chronic diseases may need to adhere to many treatment regimens. Client adherence means that clients and families invest time in carrying out the required home treatments. For example, a client with chronic obstructive pulmonary disease (COPD) may need to spend several hours a day performing respiratory therapies designed to keep the airway open and maintain an acceptable level of wellness. Investments of time, money and personal resources for a long period can be discouraging. Nurses are able to intervene and help the client adhere to the treatment plan. Adequate discharge planning and education of the client and family help promote a smooth transition from one healthcare setting to another or to the home.
Mr Altmann is a 50-year-old executive, husband and father of three teenagers. He is recovering from an acute myocardial infarction (MI) and cardiac arrest. For the past 3 days, all of Mr Altmann’s hygiene needs have been met by the nursing staff. Mr Altmann has expressed doubts about ever getting his energy back and being able to care for himself. A student nurse assesses Mr Altmann and develops a nursing care plan. One of the client goals is complete self-care within 1 week. The following plan is developed, which is designed to achieve the overall goal of independence in various phases:
Day 1: Wash face, shave and comb hair
Day 2: Feed himself meals, wash face, shave and comb hair
Day 4: Perform grooming activities and feed himself
Day 6: Shower
Communicating nursing interventions
Nursing interventions are incorporated into the nursing care plan and client’s healthcare record. The care plan usually reflects proposed nursing interventions. After the interventions are completed, the client’s response to the treatment is recorded on the appropriate record. Documenting a brief description of pertinent assessment findings and the client’s response in the client’s healthcare record validates the need for a specific nursing intervention. Recording the time and the details of the intervention documents that the procedure was completed.
Unless communication is timely and accurate, caregivers may be uninformed, interventions may be needlessly duplicated, procedures may be delayed or tasks may be left undone. Clients can tell when members of the healthcare team communicate inconsistent messages, indicating that no one is in charge. Nurses commonly communicate orally when conferring with colleagues, changing shifts, transferring a client to another unit or discharging a client to another healthcare agency. Whether the nursing intervention is written or communicated orally, the language should be clear, concise and to the point.
Critical thinking skills and evaluation of care
Evaluation of care requires the nurse to think about client responses to nursing interventions and to determine their effectiveness in promoting the client’s wellbeing. Evaluation requires the nurse to have knowledge of the characteristics of improved care in all client domains, expected and unexpected outcomes of interventions from nursing and other disciplines, characteristics of improved family and group dynamics, and community resources. Previous client-care experiences add to the nurse’s knowledge base. Professional and regulatory standards of care, as well as agency standards, are applied when evaluating care. The nurse applies attitudes of critical thinking to objectively evaluate the existing care plan and to make appropriate modifications.
Evaluation is the step in the nursing process whereby the nurse continually redirects nursing care to best meet client needs. For example, when evaluating a client for a change in vital signs, the nurse applies knowledge of disease processes and physiological responses to interpret whether a change has indeed occurred and whether the change is desirable. For example, a client in acute pain may present with an increased heart rate and increased muscular tension. The nurse knows that this is a sympathetic nervous system response to painful stimuli. After administering a pain medication and repositioning the client, the nurse will return to evaluate whether vital signs have returned to either a more acceptable level or the client’s pre-pain baseline. Positive evaluations occur when established outcomes are achieved, leading the nurse to conclude that the medication dosage and nursing intervention effectively met the client’s goal of improved comfort. Negative evaluations or undesired results indicate that the intervention was not effective in minimising or resolving the problem or in avoiding a potential problem. As a result, the nurse must change the care plan and try different therapies or a different approach to administering existing therapies.
This sequence of evaluating and revising therapies continues until problems are appropriately resolved. The nurse must realise that evaluation is dynamic and ever-changing, depending on the client’s nursing diagnoses and condition; as problems change, so too may expected outcomes. A client whose health status continuously changes requires more frequent evaluation. In addition, priority diagnoses are often evaluated first. For example, a nurse evaluates a client’s acute pain before evaluating the status of a knowledge deficit.
Evaluation of goal achievement
The purpose of nursing care is to help the client resolve actual health problems, prevent the occurrence of potential problems and maintain a healthy state. Evaluation of the goals of care determines whether this was accomplished (Table 7-5). For example, during an initial assessment a postoperative client may report acute abdominal pain, rate the pain as 8 on a scale of 0–10 and grimace or hold the abdomen during attempts to move in bed. This baseline is used by the nurse to identify the nursing diagnosis of acute pain and establish the comfort–function goal of < 3/10 pain. The nurse’s evaluation determines whether the outcomes that reflect goal accomplishment were met. Did the interventions of positioning, proper and timely administration of analgesics and use of relaxation successfully reduce the client’s pain? To objectively evaluate the degree of success in achieving a goal, the nurse should use the following steps:
1. Examine the goal statement to identify the exact desired client behaviour or response.
2. Assess the client for the presence of that behaviour or response.
3. Compare the outcome criteria with the behaviour or response.
4. Judge the degree of agreement between outcome criteria and the behaviour or response.
5. If there is no agreement (or only partial agreement) between the outcome criteria and the behaviour or response, what are the barriers? Why did they not agree?
TABLE 7-5 EVALUATION MEASURES TO DETERMINE THE SUCCESS OF GOALS AND EXPECTED OUTCOMES
| GOALS |
EVALUATIVE MEASURES |
EXPECTED OUTCOMES |
| Client’s pressure ulcer will heal within 7 days |
Inspect colour, condition and location of pressure ulcer |
Erythema will be reduced in 2 days |
| Measure diameter of ulcer daily |
Diameter of ulcer will decrease in 5 days |
| Note odour and colour of drainage from ulcer |
Ulcer will have no drainage in 2 days
Skin overlying ulcer will be closed in 7 days
|
| Client will tolerate ambulation to end of hall by 20/11 |
Palpate client’s radial pulse before exercise |
Pulse will remain below 110 beats per minute during exercise |
| Palpate client’s radial pulse 10 minutes after exercise |
Pulse rate will return to resting baseline within 10 minutes of exercise |
| Assess respiratory rate during exercise |
Respiratory rate will remain within 2 breaths of client’s baseline rate |
| Observe client for dyspnoea or breathlessness during exercise |
Client will deny feeling of breathlessness |
| Client will have improved grief resolution by 15/1 |
Ask client about frequency of periods of crying, sadness |
Client reports decreased frequency of crying, sadness in 2 months |
| Review client’s sleeping log |
Client has periods of 6–7 hours of sleep without interruption within 10 days |
| Review client’s dietary intake |
Client has no weight loss in 1 month |
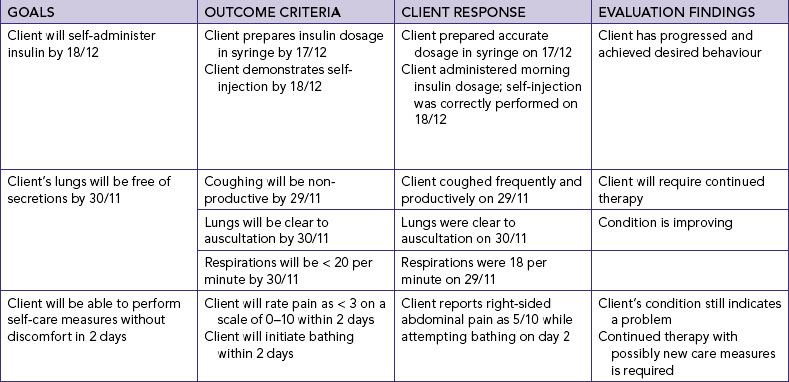
There are different degrees of goal attainment. If the client’s response matches or exceeds the outcome criteria, the goal is met. If the client’s behaviour begins to show changes but does not yet meet the criteria set, the goal is partially met. If there is no progress, the goal is not met (Table 7-6). A clearly defined goal with specific outcomes is easily measured.
The data collected during evaluation are analysed and compared with expected outcomes to determine whether changes in the client’s health status occurred (see Table 7-4). After caring for a client over a long period, the nurse is able to make comparisons of responses and behaviours. Previous experience coupled with a scientific knowledge base is key to critical thinking. Evaluation is also more exact after the nurse has seen more than one client with a similar type of problem. All members of the healthcare team should have a sense of the client’s progress. Each nurse summarises data continually to ensure that the client is progressing to a better level of health.
• CRITICAL THINKING
Following her laparoscopic cholecystectomy, the client’s recovery is delayed because she has developed a chest infection. What actions would you take to revise her plan of care and to evaluate her response to nursing interventions?
Unmet goals
As hospital stays become shorter, many clients are discharged before all goals are met and all nursing diagnoses are resolved. When preparing a client for discharge, the nurse evaluates the status of each nursing diagnosis and writes an evaluative statement identifying the client’s progress towards goal achievement and problem resolution. Appropriate revisions to the care plan are made for home or follow-up care (e.g. an extended-care facility). The nurse must clearly distinguish between goals that have been met and goals that require continued intervention.
When goals are not met, the nurse identifies the variables or factors that interfered with goal achievement. Usually a change in the client’s condition, needs or abilities makes alteration of the care plan necessary. For example, when teaching self-administration of insulin, the nurse discovers that the client has a literacy problem or a visual impairment that prevents the reading of insulin dosages on the syringe. As a result, original outcomes cannot be met. Thus the nurse uses new interventions and revises outcomes to meet the goal of care.
The evaluation of interventions examines two factors: the appropriateness of the interventions selected, and the correct application of the implementation process. The appropriateness of an intervention may be based on the standard of care for a client’s health problem. A standard of care is the minimum level of care accepted to ensure a high quality of care to clients. Standards of care define the types of therapies typically administered to clients with defined problems or needs.
During implementation, the nurse evaluates the client’s response during and immediately after intervention. Evaluation must be integrated with ongoing nursing care. If the response is favourable, implementation continues. Re-evaluation occurs when the intervention proves to be unsuccessful. The nurse then examines the other components of implementation, such as client and environment preparation, expected complications, or use of personal or technical skills during care delivery.
Changes in implementation should be guided by the nature of the client’s unfavourable response. Consulting with other nurses may yield suggestions for improving the approach to care delivery. Senior nurses are often excellent resources because of their experience. Simply changing the care plan is not enough. The nurse must implement the new plan and re-evaluate the client’s response to the nursing actions.
Evaluation is the final step of the nursing process, a systematic method for organising and delivering nursing care. Excluding evaluation from the nursing process prevents the nurse from appraising nursing practice and determining whether the outcomes of client care are beneficial. Regular evaluation ensures that a client’s care plan is current and appropriate.
KEY CONCEPTS
• During the planning component, client goals are determined and ranked in priority order, expected outcomes of nursing care are developed and a nursing care plan is written.
• Nursing care is planned and organised around specific nursing diagnoses, resulting in individualised care plans.
• Using expected outcomes, the nurse measures the effectiveness of the care plan.
• The care plan is a written guideline for care so that care can be given effectively and efficiently and is understood by all members of the healthcare team.
• The planning of individualised care requires involvement of the client and family.
• The care plan is a method for teaching students to transfer nursing knowledge into practice.
• Correctly written nursing interventions include actions, frequency, quantity, method and the person to perform the actions.
• Nurse-initiated or independent nursing interventions can solve the client’s problems without consultation or collaboration with medical or other healthcare professionals.
• Collaborative interventions require a prescription from an advanced practitioner, but always require nursing judgment or decision making.
• Implementation requires the nurse to reassess the client, review and modify the existing care plan, identify areas in which help is needed, implement nursing interventions and communicate nursing interventions to other healthcare team members.
• The care plan is modified as a client’s level of wellness and healthcare needs change.
• The implementation of nursing care may require additional knowledge, nursing skills and personnel.
• Teaching is used to present correct principles, procedures and techniques of healthcare to clients, inform clients about their health status and refer clients and families to appropriate resources.
• After implementation, the nurse writes in the client’s record a brief description of the nursing assessment, specific procedures and the client’s response to nursing care.
• Evaluation determines a client’s response to nursing actions and the extent to which goals of care have been met.
• The nurse compares the client’s response to nursing actions with expected outcomes established during planning.
• Evaluation enables the nurse to determine why the care plan was successful or unsuccessful.
• The nursing care plan is modified based on data obtained during evaluation.
REFERENCES
Carpenito-Moyet LJ. Nursing diagnoses: application to clinical practice, ed 12. Philadelphia: JB Lippincott, 2008.
Conrick M. The International Classification for Nursing Practice: a tool to support nursing practice? Collegian. 2005;12(3):9–13.
Eizenberg M. Implementation of evidence based nursing practice: nurses’ personal and professional factors. J Adv Nurs. 2010;67(1):33–42.
Johnson S, Ellis BW. The care pathway: a tool to enhance clinical governance, clinic pathways. Qual Health Care. 1999;7(3):134–144.
Maslow AH. Motivation and personality, ed 2. New York: Harper & Row, 1970.
McKinley C, McMurray A. Evidence-based management practice: reducing falls in hospital. Collegian. 2007;14(2):20–25.
Scherb C, Weydt A. Work complexity assessment, nursing interventions classification and nursing outcomes classification: making connections. Creative Nurs. 2009;15(1):6–22.
Van Hecke A, Verhaeghe S, Grypdonck M, et al. Systematic development and validation of a nursing intervention: the case of lifestyle adherence promotion in patients with leg ulcers. J Adv Nurs. 2011;67:662–676.