2 HOMEOSTASIS
INTRODUCTION
The concept of homeostasis is essential to understanding how the human body is capable of maintaining normal function despite varying conditions and fluctuations in the environment. Homeostasis occurs continually. The body does not remain in a static state — it works towards a dynamic equilibrium, adjusting variables second by second. In a dynamic equilibrium, small changes are allowed to occur, but these changes are always corrected to keep the variables at normal levels.
HOMEOSTASIS
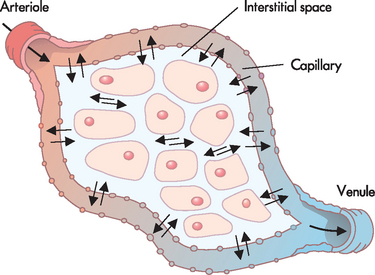
The underlying principle of how physiological variables in the body maintain a constant state, despite changes in the external environment, was the underpinning theme of how homeostasis arose. The term homeostasis was developed by the physiologist Walter Cannon and is defined as the body maintaining stable, constant conditions, despite changes in the environment.1 The term is derived from homeo (meaning similar) and stasis (meaning steady). Cannon deliberately chose the prefix homeo, rather than homo (meaning the same), as homeostasis does not require a variable to be maintained at one precise set point. Instead, the normal level for a particular variable is usually a range of values. This is known as the normal range (or reference range), so that slight increases or decreases in value may still be within normal levels. For example, the normal pH of blood is between 7.35 and 7.45 in a healthy individual (see Figure 2-1).
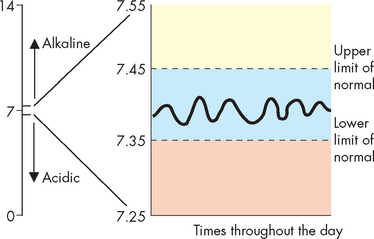
FIGURE 2-1 Homeostasis of blood pH.
Although the pH of the blood can undergo small changes, it must be maintained within the range 7.35 to 7.45. pH values outside this range indicate a disturbance to homeostasis.
An important feature about homeostasis is that when there is a tendency towards change from the normal level, the change does not actually deviate significantly from the normal level before it is corrected. In other words, as a result of constant monitoring and adjustments, small changes are corrected fairly quickly. Homeostasis operates by maintaining a stable internal environment by compensating automatically for changes in the surrounding environment. In order to understand how this works, we need to explore how a cell interacts with its local environment.
The cellular environment
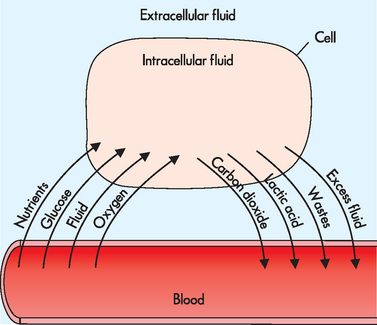
The smallest functional living component of the body is the cell. This small area is enclosed by a thin cell membrane that allows the essential substances inside the cell to be relatively separated from the surrounding environment. Nutrients and other required substances can enter the cell, while wastes and other substances produced by the cell can exit into the surrounding environment. In order for cells to maintain their normal structure and function, appropriate exchange with the extracellular environment is essential.
The human body is approximately 60% water — all components are dispersed in fluids. Both inside and outside the cells is a water-based environment (see Figure 2-2). Water can be found within cells, as well as in the blood (blood components travel through the watery plasma), brain fluid (cerebrospinal fluid) and other body fluids. The fluid inside the cells is known as the intracellular fluid, or cytoplasm. The fluid outside or between the cells — which is now known to be critical for maintaining the health of the cells — is known as the extracellular fluid. The extracellular fluid can be further subdivided into interstitial fluid between cells, and plasma or intravascular fluid within the bloodstream.
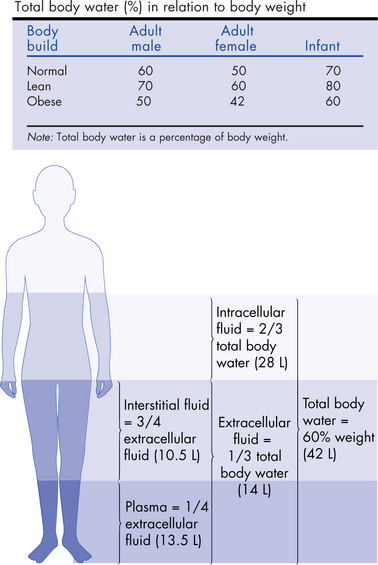
FIGURE 2-2 The composition of body fluid compartments in humans.
The shaded areas depict the approximate size of each compartment as a function of body weight. The figures indicate the relative sizes of the various fluid compartments and the approximate volumes of the compartments (in litres) in a 70-kg adult. In a normally built individual, the total body water content is roughly 60% of body weight. Because adipose tissue has a low concentration of water, the relative water-to-total body weight ratio is lower in obese individuals (and infants), as shown in the insert.
Source: Based on Goldman L. Cecil medicine. 23rd edn. Philadelphia: Saunders; 2008; and Verbalis JG. Body water as molality. In Wilkinson B, Jamison R (eds). Textbook of nephrology. London: Chapman & Hall. Reproduced with permission of Hodder Arnold.
In 1878 Claude Bernard described the extracellular fluid as the milieu intérieur — namely, the environment of the cell.2 Ongoing exchange between the cell and the extracellular fluid is vital for maintaining consistency of conditions inside the cell, which in turn is necessary for the cell to function normally. According to Bernard, the cell is able to maintain consistent conditions because it is located within the extracellular fluid — the extracellular fluid helps protect the cell from changes that occur in the environment outside the body. In fact, when Cannon developed the term homeostasis, he was expanding on this earlier work from Bernard regarding the importance of the local environment surrounding the cells.
Nutrients, oxygen, fluid and other valuable substances for fuelling cells are delivered to the cells by the bloodstream (see Figure 2-3). All body cells have a blood vessel located in close proximity, to allow this constant exchange. Substances travel out of the blood vessel, through the surrounding extracellular fluid and into the cell (see Figure 2-4). Cellular wastes such as carbon dioxide and lactic acid produced by the cell, as well as valuable substances produced by the cell, including hormones, travel to the bloodstream via the extracellular fluid.
Homeostasis at the cellular and local level
The condition, temperature, pressure and amount of nutrients and wastes travelling through the blood and extracellular fluid vary, even in a resting individual. These changes within the blood and extracellular fluid can impact on cells’ ability to maintain normal function. All cells need to have a stable environment to continue functioning normally, thus homeostasis is necessary.
When fluid levels inside the intracellular environment drop, the cell obtains additional fluid from the surrounding extracellular fluid (see Figure 2-5). Similarly, if oxygen levels in the cell are too low and carbon dioxide is allowed to accumulate, then exchange with the blood and extracellular fluid restores these levels in the cell back to normal (see Figure 2-6).
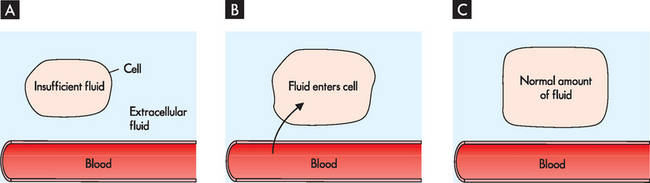
FIGURE 2-5 Homeostasis of cellular fluid levels.
A The cell has inadequate levels of fluid, so in B fluid enters the cell from the extracellular fluid. This leads to a normal amount of fluid in the cell in C, and homeostasis is restored.
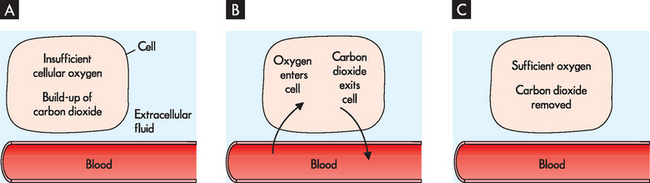
FIGURE 2-6 Homeostasis of oxygen and carbon dioxide levels within cells.
Insufficient levels of oxygen and excessive carbon dioxide in the cell A are corrected by oxygen entering the cell and carbon dioxide exiting the cell via the blood and extracellular fluid B, so that cellular homeostasis is restored C.
The levels of ions (or electrolytes) within the cell also need to be maintained in the appropriate range for normal cellular function. In particular, the relative proportions of the ions sodium, potassium and calcium are arguably the most critical, as these are required for neurons (nerve cells) to function — if neurons cannot function, this is fatal. The relative proportions of sodium, potassium and calcium between the intracellular and extracellular fluid is shown in Table 2-1. You need to become familiar with this table, as it forms a basis for understanding physiology and pathophysiology in the coming chapters, as well as being of key importance for electrolyte balance in the body. Figure 2-7 shows how sodium levels fluctuate in and around the cell during neuron signalling; importantly, sodium levels within the cell need to be restored to allow the neuron to continue functioning.
Table 2-1 RELATIVE PROPORTIONS OF THREE ESSENTIAL IONS (ELECTROLYTES)
| ION | INTRACELLULAR PROPORTION | EXTRACELLULAR PROPORTION |
|---|---|---|
| Sodium (Na+) | Low | High |
| Potassium (K+) | High | Low |
| Calcium (Ca2+) | Low | High |
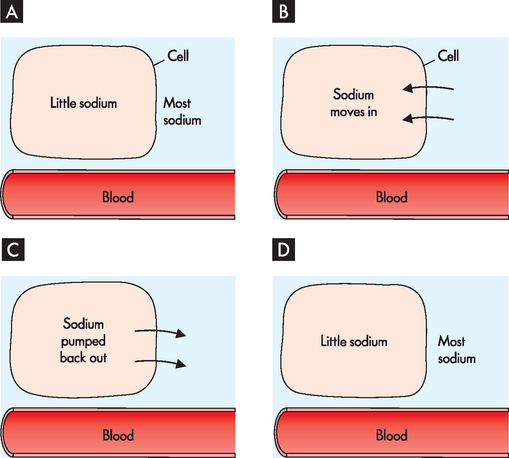
FIGURE 2-7 Homeostasis of sodium at the cellular level.
A When the neuron is at rest, most of the sodium is in the extracellular fluid. B During neuron signalling, sodium moves into the cell (across the cell membrane). C Towards the end of neuron signalling, an essential feature is the removal of the excess sodium from the cell. D Homeostasis is restored, with most sodium being returned to the extracellular fluid. If the sodium was not returned to the extracellular fluid, the neuron would not be able to send another signal.
Cells of the immune system function in their environment to maintain local homeostasis by destroying foreign substances such as bacteria (see Figure 2-8). This contributes to homeostasis of not just the cell, but also the local tissues. Other examples of local area homeostasis are wound healing after a small cut to the skin (see Figure 2-9) and blood clotting (see Figure 2-10). Although these are separate processes, a cut to the skin usually pierces a blood vessel, so both processes are generally working at the same time. These examples of homeostasis involve more than just one cell, but are still relatively localised.
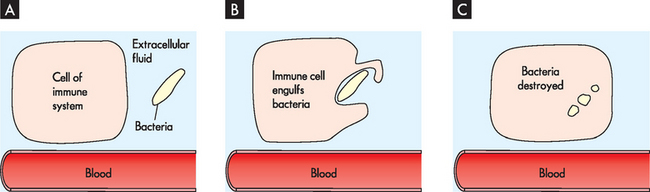
FIGURE 2-8 Homeostasis of the local area.
A Bacteria are identified as foreign by the immune cell. B The immune cell engulfs or consumes the bacteria and, once inside, the cell destroys the bacteria. C This destruction of the bacteria leads to homeostasis in the local environment.
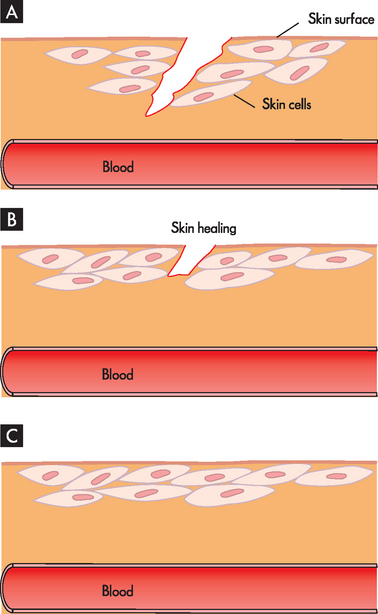
FIGURE 2-9 Homeostasis of the skin.
A A cut in the skin breaks the body’s protective cover, which may allow bacteria and harmful chemicals to enter the body. B This initiates a series of steps involved in wound healing. C The body’s protective covering is restored, resulting in homeostasis.
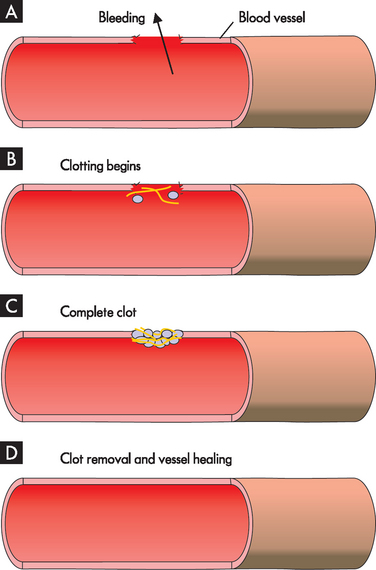
FIGURE 2-10 Homeostasis of the blood vessels.
A A break in the blood vessel allows blood to escape. B The process of blood clotting begins, which results in a complete clot C, so that no further blood loss occurs and homeostasis is maintained. The clot stays in place while the vessel heals. D When the vessel is healed, the clot is removed.
Homeostasis at the body level
Constancy within the cells leads to homeostasis in the whole body; each cell benefits from and contributes to homeostasis at the body level. Although each organ system has a distinct and unique role, the overarching function that is common to all systems is contributing to homeostasis at the body level. Coordination of homeostasis on such a large scale requires the involvement of the central nervous system (namely the brain and spinal cord), as well as the endocrine system (which uses hormones). In the next section, we explain how this regulation of essential processes maintains the harmony of all body systems.
REGULATION OF HOMEOSTASIS
Homeostasis of the whole body is achieved via the relationships between the different body systems (introduced in Chapter 1). Each system functions towards the overall health and wellbeing of the complete body.
As an example, valuable fuels from the digestion of food are found in abundance in the blood following a meal, but are less available in the hours afterwards. Glucose is one such fuel that is widely used by cells. A number of processes are involved in maintaining appropriate glucose levels in the bloodstream, so that consistent levels of glucose are available for cells. For instance, after a meal, when blood glucose levels rise, the pancreas secretes insulin (a hormone), returning blood glucose levels to normal and so maintaining homeostasis (see Figure 2-11).
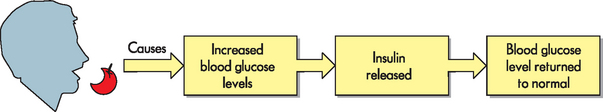
FIGURE 2-11 Blood glucose levels are maintained at a normal level after a meal by the pancreas releasing the hormone insulin.
The pain reflex is another important way that normal function is maintained. If your hand touches something that is sharp and painful, this is detected by nerves that go to your spinal cord, which results in an extremely fast response causing your hand to be moved away — the withdrawal reflex (see Figure 2-12). This reflex is extremely fast because it does not require processing of information by the brain — it can be controlled more quickly by the spinal cord. In this way, further damage to the hand is prevented.
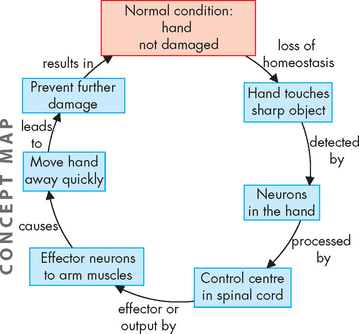
FIGURE 2-12 The pain reflex results in immediate removal of the hand from the source of pain to prevent further tissue damage.
Although slight fluctuations at the cellular level are usually restored locally, if homeostasis cannot be achieved by the cells, bloodstream and extracellular environment, responsibility shifts to the governing nervous system, which can coordinate additional responses if the fluctuations become too great. So, minor corrections can be restored locally, but larger corrections require the central nervous system (the brain and spinal cord) to regulate the processes of homeostasis. In most instances, it is the brain that is responsible for coordination of the critical functions of homeostasis. If a short-term response is required, this is coordinated quite efficiently by the nervous system itself. However, if a longer response is needed, the nervous system activates the endocrine system to assist in mediating the correction using hormones.
One way that the brain maintains homeostasis is by negative feedback pathways. There are three essential components of these feedback pathways:
Let us look at some common examples of negative feedback pathways, which will assist in your understanding of homeostasis. Levels of carbon dioxide in the body are regulated closely and corrected using negative feedback. As shown in Figure 2-13, the nervous system senses any increase in carbon dioxide, and the breathing rate is increased to exhale the excess carbon dioxide, thereby lowering carbon dioxide levels back to normal.
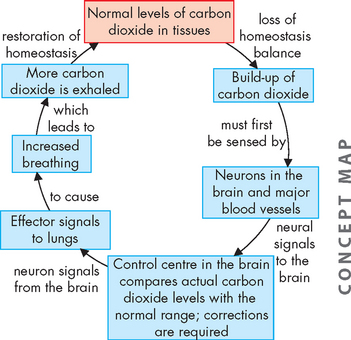
FIGURE 2-13 Negative feedback pathway to return carbon dioxide levels to normal.
The brain coordinates responses by the lungs to restore homeostasis — this is just one of several means of controlling levels of carbon dioxide in the body.
Fluid balance is critical for normal function of every cell (see Figure 2-14). Fluids are lost through the urine and sweat (as well as other areas). This loss is sensed by the brain, which triggers the thirst reflex and causes you to feel thirsty and have a drink. If you are unable to drink, other processes are initiated to limit dehydration, such as a decline in urine production to keep fluid within the body (which is achieved via hormone signals to the kidneys to retain the fluid in the blood rather than losing it in the urine). This demonstrates how body cells can maintain homeostasis of their intracellular fluid volume, despite substantial increases and decreases in water availability (due to inconsistent fluid intake).
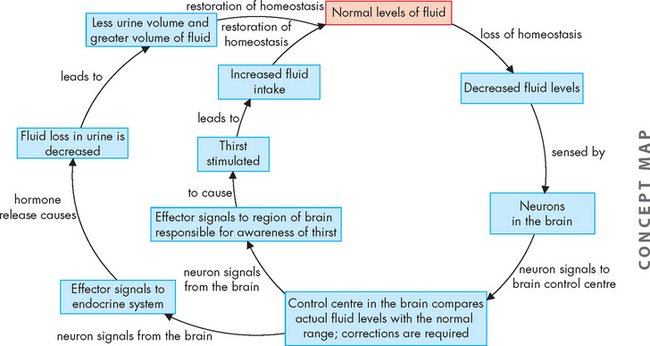
FIGURE 2-14 Negative feedback pathways to regulate fluid balance.
The pathways include a conscious awareness of thirst to stimulate fluid intake, as well as hormone signals to the kidneys to retain fluid in the blood rather than losing the fluid in the urine.
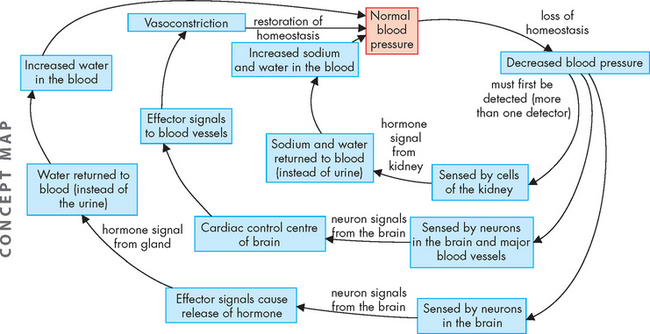
As noted previously, maintaining the appropriate sodium balance within the cells is vital for cell function. If sodium levels deviate too far from normal, this is sensed by the cells of the kidneys, which release a hormone to control the levels (see Figure 2-15). For example, low sodium levels are corrected by the kidneys returning sodium to the blood instead of losing it to the urine.
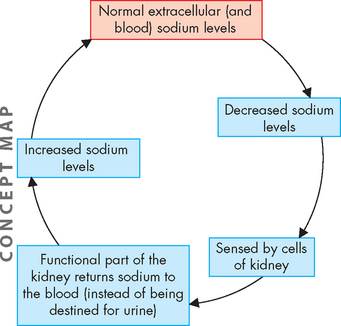
FIGURE 2-15 Homeostasis of sodium is achieved using the endocrine system to regulate kidney function.
This example is an oversimplification of the negative feedback pathway system, however, as in reality multiple sensor and effector pathways work simultaneously to correct the imbalance. In fact, for the most vital functions, more than one process is used to restore variables to normal. The following examples include multiple feedback arms to demonstrate the complexity of regulation.
Blood pressure is arguably the most important variable that needs to be controlled in the body. Adequate blood pressure is needed for blood flow, and hence the transport of all nutrients and wastes to and from regions such as the brain, heart and lungs — this essential function keeps these organs alive. The negative feedback pathways for low blood pressure actually show three loops (see Figure 2-16), which indicates that (at least) three different processes may be activated to keep blood pressure sufficient. In order to understand this negative feedback cycle, you need to be aware that when sodium is retained by the kidneys so that it remains in the blood instead of exiting the body in the urine, water is also retained. This leads to an increase in blood volume and a corresponding increase in blood pressure.
DISTURBANCES OF HOMEOSTASIS LEAD TO PATHOPHYSIOLOGY
When the body’s ability to compensate for changes and maintain homeostasis is exceeded, disorders and disease ensue. The original cause of a problem may be a source external to the body, such as use of drugs, or a source internal to the body, such as occurs with ageing. As another example, a local infection is a disturbance in homeostasis. The immune system will attempt to remove the infection to restore homeostasis, and treatments such as antibiotics may also be used to assist. In some cases, the infection may become so severe and widespread throughout the body that the person dies.
Throughout this textbook, as you learn about pathophysiology, think about what underlying processes of homeostasis have been altered. Remember that disturbances in homeostasis lead to disease, and possibly eventually death, when the body’s ability to compensate for change is exceeded.
Homeostasis
 Homeostasis is the ability to maintain stable conditions in the body, despite major changes in the environment. Homeostasis does not require a variable to be maintained at one precise set point: variables are usually controlled within a range of values known as the normal range.
Homeostasis is the ability to maintain stable conditions in the body, despite major changes in the environment. Homeostasis does not require a variable to be maintained at one precise set point: variables are usually controlled within a range of values known as the normal range. Slight changes in conditions are automatically corrected to maintain homeostasis. Such corrections are made continually.
Slight changes in conditions are automatically corrected to maintain homeostasis. Such corrections are made continually.In the first few days of semester you will form a study group with some classmates. This week, your group members will be helping each other to learn about homeostasis. Here are some general points for your group to discuss: