Chapter 32 Drugs Affecting Hearing, Taste and Smell
Knowledge of the anatomy of the ear (external, middle and inner ear) and related physiology (mechanisms of hearing and balance) is necessary to understand the clinical use of medications in treating ear disorders. People with ear disorders may have ear pain, vertigo, deafness and difficulty with communication. The pharmacological agents used to treat common ear disorders are limited (mainly antimicrobial and anti-inflammatory agents); however, many systemic agents can affect the ear adversely, causing ototoxicity. The other special senses, taste and smell, may also be impaired by drugs. This chapter reviews these agents.
Key abbreviations
Key background: anatomy, physiology and pathology of the ear
Anatomy and physiology
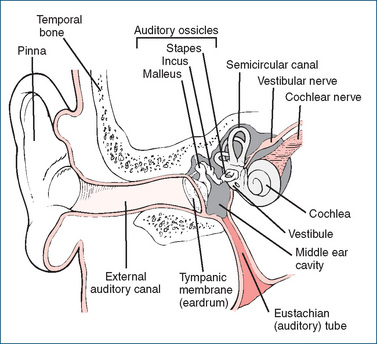
THE ear consists of three sections: the external ear, middle ear and inner ear (Figure 32-1). The external ear has two divisions: the outer ear, or pinna, and the external auditory canal (external acoustic meatus). The canal leads to the eardrum, or tympanic membrane, a thin transparent partition of tissue between the canal and the middle ear. The function of the external ear is to receive and transmit auditory sounds to the eardrum and to protect it from damage. The tympanic membrane in turn transmits sound to the bones of the middle ear and protects it from foreign substances.
The middle ear is an air-filled cavity in the temporal bone that contains three small bones called the auditory ossicles:1 the malleus (hammer), incus (anvil) and stapes (stirrup). The tip of the malleus is attached to the surface of the tympanic membrane. Its head is attached to the incus, which in turn is attached to the stapes. The ossicles amplify (about tenfold) and transmit vibrations from sound waves to the inner ear. The middle ear is also directly connected to the nasopharynx by the eustachian (auditory, or pharnygotympanic) tube. The eustachian tube is usually collapsed except when the person swallows, chews, yawns or moves the jaw. This tube allows for the equalisation of the air pressure in the inner ear with atmospheric pressure to prevent the tympanic membrane from rupturing. On airline flights, ear pain due to pressure changes is relieved by way of the eustachian tube by chewing, yawning or swallowing.
The inner ear, also referred to as the labyrinth because of its convoluted series of canals, has two main divisions. The bony labyrinth consists of the vestibule, cochlea and semicircular canals, and the membranous labyrinth consists of a series of sacs and tubes within the bony labyrinth. The cochlea, through which pass fibres of the cochlear division of the acoustic nerve, is the primary organ of hearing, while the vestibular apparatus is vital to maintaining equilibrium and balance. The inner ear transduces vibrations from sound waves, via movements of the hair cells in the cochlea, into electrical signals in the vestibulocochlear (acoustic) nerve. Action potentials generated are then transmitted along complex neuronal pathways to the acoustic areas in the temporal lobes of the cerebral cortex, where they are interpreted as sounds of varying pitch and loudness.
Common ear disorders
The most common ear disorders include infections of the ear (bacterial or fungal), earwax accumulation, various other painful or inflammatory conditions, deafness and problems with balance. Many ear disorders are minor and self-limiting or easily treated. Persistent pain or ear problems should be professionally evaluated because some untreated disorders can lead to hearing loss.
External ear disorders
External ear disorders usually involve trauma and subsequent infections, such as from lacerations or scratches to the skin of the ear canal, or from infected water entering the canal (see Clinical Interest Box 32-1). These are often minor and heal with time. If the injury results in bleeding and perhaps a haematoma, referral to a doctor may be necessary. Localised infections of the hair follicles may result in boils (furuncles associated with Staphylococcus aureus). Patients with recurring boils that do not respond to good hygiene and topical compresses may require surgical drainage and systemic antibiotics.
Clinical interest Box 32-1 Swimmer’s ear
Swimmer’s ear is an infection of the ear canal (otitis externa) related to aquatic activities such as swimming, bathing or showering. It is often associated with water retained in the outer ear canal (the external acoustic meatus) after swimming or hair-washing, or with overzealous use of cotton swabs or other implements to clean or dry the ear.
Bacteria may be introduced with water (especially if chlorination of pools is inadequate) and multiply in the warm moist environment of the ear canal. Debris can be generated, the canal lining invaded by microorganisms and symptoms of otitis externa appear (pain, swelling, sensation of fullness in the ear, impaired hearing).
Prevention is assisted by excluding moisture from the canal (e.g. with ear plugs) and by desiccation and acidification of the canal with drying ear-drops containing acetic acid and/or isopropyl alcohol, propylene glycol or glycerol, and an astringent agent such as aluminium acetate. A homemade version of commercial ear-drops, recommended by a Melbourne ear, nose and throat specialist, can be readily made by mixing 1 volume (e.g. 5 mL) of methylated spirits with 2 volumes (10 mL) white vinegar; as ear-drops do not need to be sterile, these can be homemade provided attention is paid to cleanliness of the vessels used.
Treatment is by gentle removal of debris, and drying by use of ear-drops (as above) then gentle insertion of a small plug of tissue to ‘wick’ the liquid out; if infection develops it may require topical antibiotics and anti-inflammatory agents.
Dermatitis of the ear, itching, local redness, weeping and drainage must be evaluated individually, as the causes can vary, from inflammation induced by seborrhoea, psoriasis or contact dermatitis, to head trauma producing ear discharge. Self-medication should be discouraged when infection is suspected, in the presence of known injuries of the ear or whenever effusion, pain and dizziness are present.
Middle ear disorders
Otitis media
Middle ear disorders should not be treated with overthe-counter (OTC) medications because prescription-only treatment such as antibiotics may be required. The most commonly reported problem is middle ear inflammation, otitis media (OM), occurring in children with viral upper respiratory tract infections, and it is one of the most common infections of childhood, especially between 6 and 12 months of age. OM can occur with or without perforation, effusion and suppuration (pus). Common bacterial pathogens are Streptococcus pneumoniae and Haemophilus influenzae. Pain, fever, malaise, pressure, a sensation of fullness in the ear and hearing loss are common symptoms.
It is usually a mild condition that resolves without treatment; parents may need reassurance during a ‘watchful waiting’ period. Analgesia may be required (e.g. ibuprofen or paracetamol), but systemic decongestants and antihistamines have no proven efficacy. Systemic antibiotics (amoxycillin, cefuroxime or cefaclor) may be required, especially in immunocompromised patients and in Aboriginal and Torres Strait Islander children. Ear-drops containing benzocaine (a local anaesthetic) and phenazone (a topical non-steroidal anti-inflammatory agent) may be used to relieve pain (see below under OTC otic preparations, and review by Morris and Leach [2009])
Persistent effusion of fluid in the middle ear (glue ear) with pain and hearing loss may resolve after some weeks or may require relief by drainage with a ventilating tube (grommet). Chronic suppurative OM, in which the eardrum has become ruptured and purulent exudate (pus) appears in the external canal, can cause hearing loss, and may require surgical removal of the pus and treatment with topical combination ear-drops containing an antiinflammatory agent (dexamethasone) and antibiotics (framycetin plus gramicidin [see Drug Monograph 32-1] or ciprofloxacin).
Drug monograph 32-1 Antibiotic–corticosteroid ear-drops and ointments
Combination ear-drops or ear ointments typically contain a corticosteroid (e.g. triamcinolone 0.1% or dexamethasone 0.05%) and two or three antibiotics (e.g. framycetin 0.5%, neomycin 0.25%, gramicidin 0.005%, bacitracin 400 IU/g or nystatin 100,000 U/g). Antimicrobial agents acting by different mechanisms (e.g. inhibiting protein synthesis, altering cell membrane permeability, antifungal actions) are usefully combined in ‘triple antibiotic’ formulations. The corticosteroid also has mild vasoconstrictor actions.
INDICATIONS These preparations are used as anti-inflammatory and antimicrobial agents to treat ear infections with sensitive organisms, such as otitis externa of bacterial or fungal origin, or chronic suppurative otitis media.
PHARMACOKINETICS The antibiotic components are not usually absorbed through intact skin. Corticosteroids and neomycin may be absorbed, particularly if the skin is inflamed, and can cause mild systemic effects. If absorb ed, they are subject to normal elimination proces ses of metabolism and excretion (in urine and bile).
ADVERSE DRUG REACTIONS Prolonged use can lead to hypersensitivity reactions, skin irritations and contact dermatitis; corticosteroids can cause delayed healing and secondary infections, especially fungal infections.
DRUG INTERACTIONS As the drugs are not well absorbed through the skin, few interactions should occur.
WARNINGS AND CONTRAINDICATIONS Aminoglycosides (including framycetin and neomycin) are used only with caution if the eardrum is perforated or ventilated (with a grommet), as serious inner ear damage and hearing loss can occur. They should be ceased immediately the infection resolves. Patients are advised to stop using the medication and contact their doctor if aural symptoms (tinnitus, hearing loss or dizziness) appear. They are contraindicated in viral or tubercular infections.
There is a risk of fungal overgrowth if antibiotic–corticosteroid preparations are used for more than 7 days. Use in children should be limited to the minimal effective duration. Due to the aminoglycoside present, the ear-drops are rated Pregnancy Category D.
DOSAGE AND ADMINISTRATION Before otic admin istration, ear wax and debris should be gently removed. Dosage of ear-drops is usually 2–3 drops, 2–4 times daily. Cream or ointment is applied and the ear gently massaged 2–3 times daily.
Acute tympanic membrane perforation from foreign objects or from water sports (such as diving or water skiing) may result in pain at the time of injury that subsides, diminished hearing acuity, tinnitus (a ringing or buzzing sound in the ears), nausea, vertigo and OM or mastoiditis. A physician’s examination is vital when a perforated tympanic membrane is suspected.
Inner ear disorders
Loss of hearing, especially unilateral hearing loss, may result from viral infection of the inner ear. Untreated external and middle ear infections may also affect the hearing and balance functioning of the inner ear.
Vertigo
 Vertigo, the sensation that the environment or the body is rotating, can be so severe as to cause the sufferer to fall over. Acute episodes usually settle within 1–2 days. There are numerous causes, and the drug treatment varies accordingly: otological vertigo due to inner ear disorders is treated with ‘vestibular blocking agents’, which may include anticholinergics, betahistine, antiemetics and benzodiazepines, whereas vertigo associated with migraine or strokes is treated with calcium channel antagonists, tricyclic antidepressants and (-blockers.
Vertigo, the sensation that the environment or the body is rotating, can be so severe as to cause the sufferer to fall over. Acute episodes usually settle within 1–2 days. There are numerous causes, and the drug treatment varies accordingly: otological vertigo due to inner ear disorders is treated with ‘vestibular blocking agents’, which may include anticholinergics, betahistine, antiemetics and benzodiazepines, whereas vertigo associated with migraine or strokes is treated with calcium channel antagonists, tricyclic antidepressants and (-blockers.
A new type of treatment for the vertigo and other balance disorders associated with Ménière’s disease is that of trans-tympanic perfusion (i.e. administration through the eardrum, by means of a sustained delivery system) of the corticosteroid dexamethasone or the antibiotic gentamicin (see ‘Otic administration’, below).
Other causes of ear disorders
Hearing deficits may be caused by genetic diseases or slowly progressive diseases such as otosclerosis or Ménière’s disease (see Clinical Interest Box 32-2). Some drugs can cause ototoxicity as an adverse effect, which results in impaired hearing. These will be discussed later in this chapter.
Clinical interest Box 32-2 Ménière’s disease
Ménière’s disease (named after the French physician Prosper Ménière, 1799–1862) is a progressive, episodic inner ear disease caused by an increase in pressure and spontaneous bursts of activity within the labyrinth (the semicircular canals and the cochlea that make up the vestibular system). It involves recurrent attacks of vertigo, nausea, tinnitus and variable hearing loss. The vertigo can be so severe that the person cannot stand or walk unaided, and the vomiting so severe that it precludes eating or drinking. The hearing loss is usually progressive.
The motion sickness and dizziness are thought to be caused by a disparity in the proprioceptive information being received from the two sides of the head. This also occurs in motion sickness, for example when viewing outside stationary objects from within a moving vehicle, or when watching waves from a rolling ship. The aquaporins (water channels) and vasopressin receptors involved in homeostasis of water in organs such as the kidney and ear are thought to play a crucial role in fluid homeostasis of endolymph in the inner ear. There are other causes of vertigo, both peripheral (rubella, mumps, acoustic neuroma, otitis media) and central (migraine, epilepsy, multiple sclerosis).
As well as drug treatments, the distressing vertigo may also be helped by various manoeuvres in which the head is moved through different planes to attempt to remove fluid in the canals. Sometimes the only effective treatment is surgical: vestibular nerve section or removal of the balance mechanisms (labyrinthectomy) on the affected side; this also removes the sense of hearing from that side, causing partial deafness.
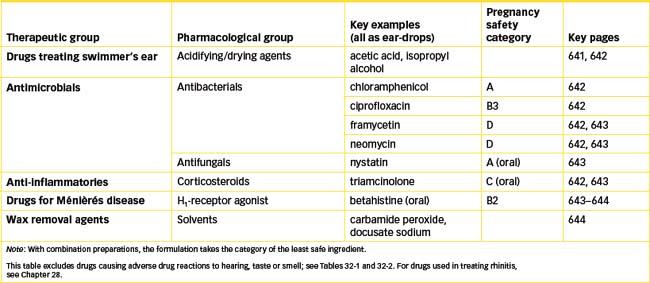
Drugs affecting the ear
A wide variety of both single and combination products is used to treat impacted cerumen (wax), inflammation, bacterial or fungal infections, ear pain and other minor or superficial problems associated primarily with the external ear canal. More serious problems, such as an earache secondary to an upper respiratory tract infection, ear discharge or drainage, persistent or recurrent OM or ear pain caused by recent injury or head trauma, require prescribed drugs such as antimicrobial drops, corticosteroid anti-inflammatory agents and local anaesthetics, given by the otic or systemic routes.
Otic administration
Otic administration
Drugs are administered to the ear for local effects only and are not absorbed systemically (as they potentially can be from the eye). Traditional formulations for otic administration are ear-drops and ear ointments. Pharmaceutical aspects of these are basically similar to the requirements for eye-drops and eye ointments; however, there is not the same strict importance attached to sterility of preparations, as ear-drops and ointments cannot penetrate the middle or inner ear unless the eardrum is perforated, and the tissues of the ear are well vascularised. Some drops are formulated for either eye or ear use.
Ear-drops and sprays are commonly formulated with the active drug(s) dissolved in aqueous solvents such as isopropyl alcohol, saline solutions, glycerol, benzyl alcohol, polyethylene glycol or propylene glycol; or in oily solvents such as arachis (peanut) oil. Acetic acid is often used in ear-drops to return the ear canal to a mildly acidic environment after swimming or bathing. Pharmacists are sometimes requested to dispense extemporaneous preparations (compounded as a one-off formulation in the dispensary), such as ear-drops with saline, aluminium acetate or sodium bicarbonate, in the solvents listed above.
Intracochlear drug delivery
Treatment of disorders of the inner ear that cause auditory or vestibular dysfunction is enhanced if the drug can be delivered to the inner ear. Two new methods of drug delivery are being developed (see review by Borkholder [2008]).
Trans-tympanic injections
Injections of drug can be made through the tympanic membrane (eardrum) into the middle ear, from where it can diffuse into the inner ear via thin membranous ‘windows’. This route is being used for administration of aminoglycoside antibiotics, such as gentamicin and corticosteroids, for treatment of Ménière’s disease and sudden sensorineural hearing loss. The aminoglycoside antibiotics are known to cause hearing loss, and it is thought that the trans-tympanic administration of gentamicin has its effect by damaging hair cells and thus reducing vestibular function; the dose must be carefully judged so that hearing is not completely lost.
Diffusion through the window membranes
Drug formulated in matrices can be administered into the middle ear to the oval or round window membrane, from where it can readily diffuse into the vestibule and semicircular canals or cochlea, respectively. Drugs in minute nanoparticles can diffuse through membranes (see Clinical Interest Box 42-4), and this method is being studied as a possible route for gene therapy, to regenerate functions of the inner ear.
Antimicrobial ear formulations
Antimicrobial ear formulations are used topically to treat infections of the external auditory canal (otitis externa). For serious middle or inner ear infections, systemic antibiotics are indicated. Antibiotics preferred for topical use are those that are not used systemically (because of systemic toxicity or adverse pharmacokinetics), such as the antibacterials chloramphenicol, ciprofloxacin, framycetin, neomycin, gramicidin and bacitracin, and the antifungals nystatin and clioquinol. (These antimicrobial drugs are covered in detail in Unit 14.) Antimicrobial ear-drops are also formulated in combination with a corticosteroid (see Drug Monograph 32-1).
Antibacterial antibiotics
Chloramphenicol, a broad-spectrum bacteriostatic antibiotic, is frequently used to treat external ear infections (otitis externa) and OM caused by Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, Enterobacter aerogenes, Haemophilus influenzae and other susceptible organisms. It is available as 5 mg/mL (0.5%) ear-drops. Potential adverse effects include burning, redness, rash, swelling or other signs of topical irritation that were not present before the start of therapy. The medication should be discontinued if this hypersensitivity reaction occurs. The usual dosage for adults and children is 4 drops inserted in the ear canal four times a day. (There is no risk of aplastic anaemia from topical use of chloramphenicol in the ear or eye.)
The aminoglycoside antibiotics (such as framycetin 0.5% and neomycin 0.35%) are also used in ear-drops, but it must be noted that these drugs themselves are liable to cause ototoxicity. Framycetin (a component of neomycin, and also known as neomycin B) is formulated as drops (5 mg/mL), ear ointment (5 mg/g) and also in combina tion preparations with other antibiotics and with corticosteroids.
The fluoroquinoline antibiotic ciprofloxacin is now available as ear-drops (0.3%) and is not ototoxic so is preferable in patients with a perforated tympanic membrane (eardrum) or a patent grommet. Ciprofloxacin ear-drops are indicated for chronic suppurative OM infections
Corticosteroid ear preparations
Corticosteroid anti-inflammatory agents used in the ear include triamcinolone, flumethasone, dexamethasone and hydrocortisone; they are usually formulated combined with antimicrobials (see Drug Monograph 32-1). The corticosteroid is included for its anti-inflammatory, antipruritic and antiallergic effects, while the antibiotic treats external ear canal infections and mastoidectomy cavity infections. Note, however, that corticosteroids have immunosuppressant actions and hence predispose to infections. Corticosteroids applied intranasally have also been used in otitis media with effusion (glue ear), but without general success.
Drug treatment of Ménière’s disease
There is no simple cure for Ménière’s disease (Clinical Interest Box 32-2); many drugs have been tried.
Betahistine
The main drug used for long-term treatment is betahistine, an orally-administered centrally-acting histamine analogue. It has H1 agonist activity, partial agonist/antagonist activity at H3 receptors and no affinity for H2 receptors. It is a vasodilator that probably acts by increasing blood flow to the labyrinth and brain stem. It may take several weeks for effects to become apparent. Adverse effects can include GIT disturbances and hypotension. It is contraindicated in conditions in which histamine is an aetiological factor, such as asthma, peptic ulcer and urticaria, and in pregnancy. Current research suggests that betahistine may be useful as an anti-obesity agent (see review by Barak [2008]).
Other drugs
Other drugs commonly tried include an anticholinergic antihistamine, such as promethazine or diphenhydra mine, and a diuretic (hydrochlorothiazide) to reduce fluid load. Corticosteroids help reduce any inflammation. Other treatment in the acute phase is with ‘labyrinthine seda tion’, using phenothiazine antipsychotics such as prochlorperazine or a benzodiazepine. A new treatment method is trans-tympanic administration of a corticosteroid for antiinflammatory effect, or of gentamicin for its ototoxic effect (‘chemical labyrinthectomy’) to reduce vestibular function. Between attacks, restricted intake of salt, sugar, cigarettes, alcohol, chocolate and caf feine and other CNS stimulants may be prophylactic.
OTC otic preparations
As with eye conditions, people often self-medicate when they realise they have ear problems. Although most OTC otic preparations are considered safe and effective, patients should be advised to see a doctor if symptoms do not improve within 2–3 days of using these preparations or if an adverse reaction occurs. Typical OTC products are described below.
Antiseptics and emollients
OTC otic preparations often contain acetic or boric acid, benzalkonium chloride, aluminium acetate (Burow’s solution), isopropyl alcohol or propylene glycol (propylene glycol also enhances the acidity of acetic acid), sodium bicarbonate and isotonic saline. Glycerol, mineral oil and olive oil are used as emollients to help relieve itching and burning in the ear, and hydroxyquinoline sulfate is present in a formulation for earache relief.
Analgesics
Ear-drops for relief of ear pain associated with OM may contain a non-steroidal anti-inflammatory drug (such as phenazone) and a local anaesthetic (benzocaine). There are precautions if the patient has symptoms like fever, dizziness, hearing loss or tinnitus, and the drops are contraindicated in perforated ear drums, ear discharge or known hypersensitivity to any ingredient. As the drops are administered topically, adverse systemic effects or drug interactions are unlikely. As benzocaine is an ester-type local anaesthetic, frequent use can cause contact dermatitis. If pain persists beyond 24 hours, medical assistance should be sought.
Wax removers
Cerumen (ear wax) consists mainly of keratin, long-chain fatty acids, alcohols, squalene and cholesterol; it has lubricating and protective functions. It normally gradually dries out and is naturally expelled from the ear, and should not be removed with hard implements. Accumulations of cerumen can be softened and its removal encouraged (‘ear toilet’) with the topical application of ear-drops containing oil-based or aqueous solutions.
Ingredients include oils (almond, arachis (peanut), olive, eucalyptus, apricot), glycerol, chlorbutol, sodium bicarbonate, sodium chloride, dichlorobenzenes and docusate sodium (a surfactant also used systemically as a laxative agent). Carbamide peroxide (urea hydrogen peroxide) is an antibacterial agent that releases oxygen to help remove wax.
Drug-induced ototoxicity
Mechanisms and manifestations
Many medications reportedly cause ototoxicity in humans. The ototoxicity may affect the person’s hearing (auditory or cochlear function), balance (vestibular function) or both. The most common symptom reported is tinnitus, ‘ringing in the ears’. Ototoxicity is usually bilateral and may be reversible but can become irreversible if not recognised early enough to withdraw the offending medications.
Reactive oxygen and nitrogen species, including free radicals (see Chapter 28 under ‘Oxygen’), have been implicated in ototoxicity. Oxidative stress damages macromolecules such as DNA, proteins and lipids; oxidative damage to the sensory hair cells in the inner ear may be involved in the ototoxicity of aminoglycoside antibiotics, loop diuretics and cisplatin antineoplastic agents. Similar mechanisms of toxicity may explain how these same drug groups damage the cells of the proximal tubules in the kidneys. (Reduction of ototoxicity in animals by antioxidants and iron chelators supports this proposed mechanism.)
The patients most at risk of ototoxicity are the elderly, those with impaired renal function (due to impaired drug excretion processes, which are exacerbated by nephrotoxicity of the same drugs that cause ototoxicity), people working or living with high noise levels and those taking ototoxic agents in high doses or for prolonged duration.
Cochlear ototoxicity causes a progressive or continuing hearing loss. Loss of high tones occurs first, then progresses to affect lower tones. Because of this slow progression, most patients are unaware it is occurring. Vestibular toxicity may start with a severe headache of 1–2 days’ duration, followed by nausea, vomiting, dizziness, ataxia and difficulty with equilibrium. The person may feel as though the room is in motion (vertigo)
Tinnitus
 Tinnitus is a common distressing and enigmatic disorder; no clear aetiology or pathology is agreed, although exposure to noise and salicylate drugs have been implicated. It is very difficult to treat; attempts have been made with retraining therapy, cognitive behavioural therapy, devices that mask the perceived buzzing/ringing noises, electrical or vibration stimulation, surgery and hearing aids. Drug therapies tried include local lignocaine or botulinum toxin or systemic corticosteroids, antidepressants or benzodiazepines. Dietary supplements, complementary and alternative therapies, acupuncture and Ginkgo biloba extracts have proven to be little better than placebo. The most recent pharmacological treatment is with trans-tympanic perfusion of corticosteroids or gentamicin, as for vertigo.
Tinnitus is a common distressing and enigmatic disorder; no clear aetiology or pathology is agreed, although exposure to noise and salicylate drugs have been implicated. It is very difficult to treat; attempts have been made with retraining therapy, cognitive behavioural therapy, devices that mask the perceived buzzing/ringing noises, electrical or vibration stimulation, surgery and hearing aids. Drug therapies tried include local lignocaine or botulinum toxin or systemic corticosteroids, antidepressants or benzodiazepines. Dietary supplements, complementary and alternative therapies, acupuncture and Ginkgo biloba extracts have proven to be little better than placebo. The most recent pharmacological treatment is with trans-tympanic perfusion of corticosteroids or gentamicin, as for vertigo.
Drugs associated with ototoxicity
Although many drugs have been associated with toxic effects on the ears, most drug-induced ototoxicity is associated with the use of salicylate and other antiinflammatory agents, aminoglycoside antibiotics, cisplatin antineoplastic agents and loop diuretics. Table 32-1 lists important drugs reported to induce ototoxicity.
Table 32-1 Some drugs reported to cause ototoxicity
| DRUG | COMMENTS |
| Analgesics | |
| Aspirin and other non-steroidal antiinflammatory drugs (NSAIDs) | NSAIDs, especially in high doses, can cause tinnitus, vertigo and hearing loss. These adverse effects are generally reversible if drug use is reduced or discontinued, although some cases of irreversible hearing loss are documented. |
| Antibiotics | |
| Aminoglycosides | Incidence of ototoxicity is 1%–5% and may be irreversible; damage occurs to auditory and vestibular hair cells. |
| Clarithromycin | Hearing loss has been reported (usually reversible). It occurs more often in elderly women. |
| Erythromycin | Reversible hearing loss has been reported in people with liver and/or kidney impairment, in people 50 years of age and over and in people who received high doses (>4 g/day). IV erythromycin has resulted in irreversible ototoxicity. |
| Vancomycin | Hearing loss has been reported, especially in people with kidney impairment or those receiving another ototoxic medication concurrently. |
| Antineoplastic agents | |
| Platinum compounds | Ototoxicity with tinnitus, hearing loss and possible deafness has been reported. This effect is especially severe in children under 12 years. The effect is cumulative, therefore audiometric testing is recommended. |
| Vinca alkaloids | Tinnitus and, less frequently, hearing loss and vertigo have been reported. |
| Loop diuretics | |
| Bumetanide, ethacrynic acid, frusemide | Reversible and irreversible hearing loss have been reported, usually with too-rapid IV injection, high diuretic dosages or concurrent use with other ototoxic medications and in people with renal impairment; tinnitus and vertigo can also occur. |
For full listing see Lee et al (2005).
Aminoglycoside antibiotics
The aminoglycoside antibiotics are commonly used for treatment of Gram-negative bacterial infections and mycobacterial diseases because of their high efficacy and low cost. They can cause irreversible ototoxicity; streptomycin and gentamicin are primarily vestibulotoxic, producing dizziness, ataxia and nystagmus, while amikicin, neomycin and tobramycin are cochleotoxic, causing permanent hearing loss.
Mechanisms proposed for the ototoxic actions are inhibition of mitochondrial protein synthesis, free-radical cell damage and activation of N-methyl-D-aspartate (NMDA) receptors. Susceptibility to ototoxicity is doserelated and also sometimes idiosyncratic and genetically linked. Carriers of a mutation in the mitochondrial 12S ribosomal RNA gene are predisposed (see review by Selimoglu [2007])
Total aminoglycoside dosage of patients should be noted, and both ototoxicity and nephrotoxicity monitored in clinical usage. Once-daily administration may be useful in increasing efficacy and reducing toxicity. Prophylactic treatment with antioxidants has been trialled.
Salicylates and other anti-inflammatories
Salicylates such as aspirin and methyl salicylate have long been known to cause auditory toxicity, especially after high doses (>4 g/day aspirin). Tinnitus, loss of acoustic sensitivity and alterations of perceived sounds occur, particularly at high frequencies. The mechanisms of auditory changes and hearing loss are not well understood, but outer hair cells in the cochlea are known to be damaged. It is not known yet whether the very low antiplatelet doses of aspirin used long-term in prevention of ischaemia (75–100 mg/day) will have a cumulative effect on hearing.
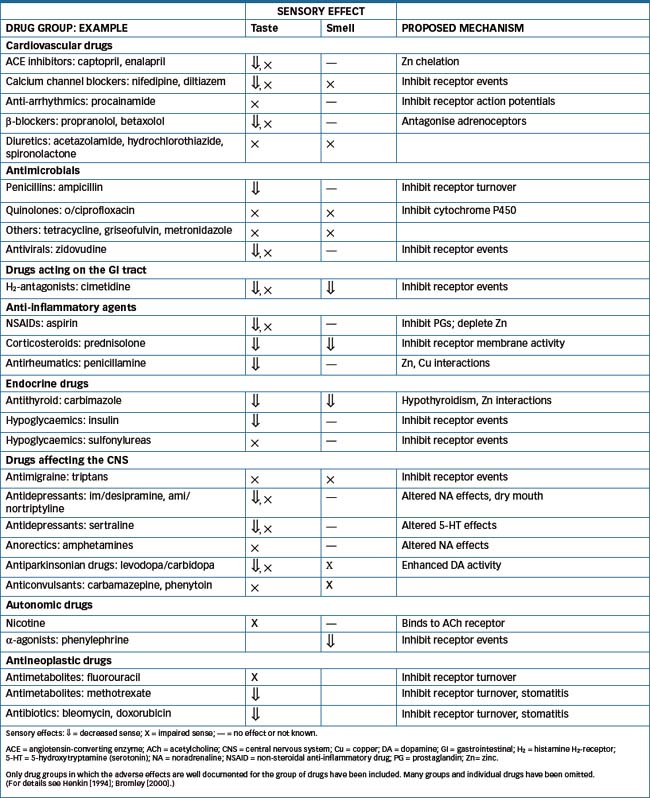
Key background: taste and smell
The senses of taste and smell aid in appreciation and normal digestion of foods, and help protect against toxins and pollutants. The sensations of taste and smell may be impaired in many situations (e.g. by ageing, radiation, dental treatment, poor oral hygiene, psychiatric and neurological disorders, tumours, trauma, epilepsy, migraine, hypothyroidism, infections and inflammation, renal failure and deficiencies of vitamin B or zinc). Dysfunctions of these senses are more common in the elderly and can significantly reduce quality of life. A great variety of drugs have been noted to cause alterations in taste and smell as an adverse effect; these are summarised in Table 32-2.
Gustation—the sense of taste
Gustation (the sense of taste) is a chemical sense closely linked to smell, but it is much less sensitive. Substances that have strong tastes, including alcohols, sugars, salts and acids, may have no smell. Molecules dissolved in saliva in the mouth are sensed by gustatory receptors on taste buds (specialised epithelial cells) located mainly on the back of the tongue and also elsewhere in the mouth, throat and oesophagus. The chemical contacts a gustatory ‘hair’ passing through a pore on the surface of the cell, stimulating receptors on the membrane and inducing action potentials in the primary afferent sensory neurons that make contact with the receptor cells. The chemical information is transduced into cellular signals via stimulation of G-proteincoupled membrane receptors, second messengers, enzymes and ion channels. Subsequent neurons in the taste pathway run via the pons and medulla to the thalamus, thence to the taste centre in the parietal lobe of the cerebral cortex, where the taste is perceived. Trace metals, especially zinc and copper, are involved at the active site of taste receptors, and zinc or copper deficiencies may cause loss or distortion of taste. Other common causes of taste disturbance are oral infections and appliances, dental procedures and exposure to toxic chemicals.
The gustatory receptors are sensitive to four main classes of taste: sour (acids), sweet (sugars, some alcohols, amino acids and lead salts), bitter (many alkaloids and acids) and salty (metal ions, especially sodium). A new taste recently described is called umami (Japanese for delicious), the taste elicited by glutamate in some meats and cheeses. The threshold for bitter tastes is the lowest: brucine is detectable at the level of about 0.4 parts per million. This sensitivity to bitter tastes may have developed as a protective func tion, as many potentially poisonous natural substances (including drugs such as quinine, strychnine, nicotine and cocaine) are very bitter.
Olfaction—the sense of smell
The receptors for olfaction (the sense of smell) are located in the olfactory epithelium at the top of the nasal cavity (see Figure 28-6). Specialised cilia projecting down from the dendrites of the olfactory receptor cells are stimulated by chemicals in the inhaled air and initiate an action potential in the olfactory neurons. These synapse within the olfactory bulb and form the olfactory tract of the first cranial nerve, passing eventually to the lateral olfactory area of the temporal lobe of the cortex and to other regions of the limbic system and to the hypothalamus. Chronic exposure to chemicals, especially metals, plastics, solvents and tobacco smoke, adversely affects olfaction.
Humans have a much greater sensitivity to smell than to taste. Vanillin can be smelt in the air at a concentration about one millionth of the concentration of brucine that can just be tasted. Consequently, there is a great range of different types of smells2 and a wide variation (1000-fold) in the thresholds at which different people can sense smells.
Anosmia (lack of sense of smell) can occur as a genetic trait, and different specific anosmias exist; for example, some people cannot smell naphthalene, others menthol, thymol, iodine or vanillin. Hyposmia, a mild general defect in olfaction, is a common symptom of colds and rhinitis (see Chapter 28), due to inflammation and obstruction of the nasal passages. Other common causes are head trauma, oral infections, wearing of dentures, dental procedures and Bell’s palsy. (Food often becoming tasteless during these conditions indicates that components of the flavour can no longer be smelled.) Hyperosmia occurs in cystic fibrosis, adrenal insufficiency and states of hysteria. In schizophrenia and epilepsy, olfactory hallucinations may occur. As with disorders of taste, there are few specific medical treatments for these olfactory dysfunctions; zinc supplements may be useful.
Drugs affecting taste and smell
Sweeteners
Sugars
Chemicals from many different classes may taste sweet—even salts of beryllium and lead. However, the most important sweet-tasting compounds are sugars, synthetic sweet-tasting com pounds such as aspartame and saccharin, and amino acids. The sweetest known sugar is (-D-fructose but its sweetness decreases with increasing concentration and at higher temperatures. In decreasing order of sweetness, other sugars rank as follows: sucrose (‘sugar’), glucose, galactose = mannose = lactose, maltose, raffinose. There are many other naturally-occurring sweet substances, including honey (see Clinical Interest Box 32-3) and plant extracts.
Clinical interest Box 32-3 ‘Isn’t it funny, how a bear likes honey?’
Honey is more than just a sweet-tasting spread—it is a viscous supersaturated sugar solution containing a complex mixture of carbohydrates, with small amounts of polyphenols, enzymes and other proteins, amino acids, minerals, vitamins, peroxide, trace elements and aroma compounds. It has a variety of nutritional and health effects, and has been claimed to have many useful pharmacological properties, including antibacterial, antioxidant, antiviral, antitumour, anti-inflammatory and antiplatelet actions.
Honey has been used since ancient times in medicine and recently has undergone a resurgence of popularity, particularly used in wound dressings and to enhance wound healing. There are new honey-based wound care products on the market; medical-grade honey has been sterilised (as honey can be a reservoir for microorganisms, despite its high osmotic pressure), has a standardised antibacterial activity and is free from plant toxins. In clinical trials, honey has been shown to improve healing times in mild to moderate superficial and partial thickness burns, but meta-analysis showed it did not significantly improve healing of leg ulcers.
Adapted from: Jull et al (2008) and Bogdanov et al (2008); and with apologies to AA Milne.
Artificial sweeteners
An artificial sweetener about 180 times sweeter than sucrose, and included in many pharmaceutical preparations, is aspartame, the methyl ester of the aspartic acid/phenylalanine dipeptide; it is contraindicated in people with phenylketonuria. Earlier sweeteners (saccharin and cyclamates) have been superseded due to potential risks of cancers. Newer sugar substitutes include acesulfame potassium, sucralose and sugar alcohols such as xylitol and mannitol. There is some debate about the usefulness of such substitutes: by providing sweet taste without kilojoules (or calories), they should lower energy intake of foods and drinks; however, some studies show that people using such sweeteners actually eat more, due to increased appetite for sweet foods.
Drugs impairing taste and smell
Loss or decrease of taste sensation (ageusia, hypogeusia) may occur as a result of neuronal damage or as an adverse effect of drugs. In some conditions, the sense of taste is distorted (dysgeusia), giving unexpected tastes sensed as metallic, bitter, burned or rotten. While these conditions cannot readily be treated medically, zinc supplements have been shown in some trials to be effective. Some drugs implicated in reducing or impairing the sense of taste are listed in Table 32-2; most commonly implicated are antihypertensives, antimicrobials and antidepressants.
In most cases, the mechanism by which the chemical sense is altered is poorly understood; doses at which the effects occur are very variable. The impaired sensation takes some days or weeks of chronic dosing to develop, and the impairment may persist for weeks or months. Patients who notice that ‘things are starting to smell different’ may need reassurance that this is an acknowledged adverse effect of the drug, which is usually reversible after stopping treatment.
Key points
 Knowledge of the anatomy and physiology of the ear is necessary for understanding the pathology of conditions affecting the senses of hearing and balance.
Knowledge of the anatomy and physiology of the ear is necessary for understanding the pathology of conditions affecting the senses of hearing and balance. Conditions affecting the external ear are generally simply treated with ear-drops that dry out and mildly acidify the ear canal. Antibiotic ear-drops are used to treat severe infections.
Conditions affecting the external ear are generally simply treated with ear-drops that dry out and mildly acidify the ear canal. Antibiotic ear-drops are used to treat severe infections. Infections and inflammation of the middle ear (otitis media) are treated with systemic analgesics and antibiotics. If the eardrum is ruptured, ear-drops containing antibiotics and anti-inflammatory agents are useful.
Infections and inflammation of the middle ear (otitis media) are treated with systemic analgesics and antibiotics. If the eardrum is ruptured, ear-drops containing antibiotics and anti-inflammatory agents are useful.Review exercises
References and further reading
Antibiotic Expert Group. Therapeutic Guidelines Antibiotic, version 13. Melbourne: Therapeutic Guidelines Limited; 2006.
Australian Medicines Handbook 2010. Adelaide: AMH, 2010.
Barak N. Betahistine: what’s new on the agenda? Expert Opinion on Investigative Drugs. 2008;17(5):795-804.
Bogdanov S., Jurendic T., Sieber R., Gallmann P. Honey for nutrition and health: a review. Journal of American College of Nutrition. 2008;27(6):677-689.
Borkholder D.A. State-of-the-art mechanisms of intracochlear drug delivery. Current Opinion in Otolaryngology and Head and Neck Surgery. 2008;16(5):472-477.
Bromley S.M. Smell and taste disorders: a primary care approach. American Family Physician. 2000;61(2):427-436. 438
Cazals Y. Auditory sensorineural alterations induced by salicylate. Progress in Neurobiology. 2000;62(6):583-631.
Coates H. Ear-drops and ototoxicity. Australian Prescriber. 2008;31(2):40-41.
Doty R.L., Shah M., Bromley S.M. Drug-induced taste disorders. Drug Safety. 2008;31(3):199-215.
Henkin R.I. Drug-induced taste and smell disorders: incidence, mechanisms and management related primarily to treatment of sensory receptor dysfunction. Drug Safety. 1994;11(5):318-377.
Jull A.B., Rodgers A., Walker N. Honey as a topical treatment for wounds. Cochrane Database of Systematic Reviews. 2008. (4): CD005083
Kuo C.-H., Pang L., Chang R. Vertigo: part 2 – management in general practice. Australian Family Physician. 2008;37(6):409-413.
Lee C.A., Mistry D., Uppal S., Coatesworth A.P. Otologic side effects of drugs. Journal of Laryngology and Otology. 2005;119(4):267-271.
Light J.P., Silverstein H. Transtympanic perfusion: indications and limitations. Current Opinion in Otolaryngology and Head and Neck Surgery. 2004;12(5):378-383.
McFerran D.J., Phillips J.S. Tinnitus. Journal of Laryngology & Otology. 2007;121:201-208.
Morris P.S., Leach A.J. Managing otitis media: an evidence-based approach. Australian Prescriber. 2009;32(6):155-159.
Sajjadi H., Paparella M.M. Ménière’s disease. The Lancet. 2008;372(9636):406-414.
Selimoglu E. Aminoglycoside-induced ototoxicity. Current Pharmaceutical Design. 2007;13(1):119-126.
Whitehouse C.R., Boullata J., McAuley L.A. The potential toxicity of artificial sweeteners. AAOHN Journal. 2008;56(6):251-259.
Growth hormone programme, PBS: www.healthyactive.gov.au/internet/main/publishing.nsf/Content/health-pbs-generalsupply-hghapplication
Ménière’s disease: www.menieresinfo.com/treatment.html
MIMS OnLine: http://0-mims.hcn.net.au
New Zealand Medicines and Medical Devices Safety Authority: www.medsafe.govt.nz
More weblinks at: http://evolve.elsevier.com/AU/Bryant/pharmacology