Chapter Twenty-nine The complete health assessment
Nurses working at an advanced level of practice or those in specific contexts such as community health or regional and remote nursing may need to conduct a total or comprehensive health assessment. This chapter illustrates how to approach the complete health assessment. The following examination sequence is one suggested framework. It is intended to minimise the number of position changes for the patient and for you. With experience, you may wish to adapt this and arrange a sequence that feels natural for you. Perform all the steps listed here for a complete examination. You will learn to strike a balance between which steps you must retain to be thorough and which corners you may safely cut when time is pressing. Have all equipment prepared and accessible before the examination. Review Chapter 8 for the list of necessary equipment, the setting, the patient’s emotional state, your demeanour and the preparation of the patient considering their age.
| Sequence | Selected photos |
|---|---|
 |
|
 |
|
 |
|
| Ask the person to empty the bladder (save specimen, if needed), disrobe except for underpants and put on a gown. The person sits with legs dangling off side of the bed or table; you stand in front of the person. | |
 |
|
 |
|
 |
|
 |
|
 |
|
 |
|
 |
|
1. Inspect the posterior chest: configuration of the thoracic cage, skin characteristics and symmetry of shoulders and muscles. 2. Palpate: symmetrical expansion; lumps or tenderness. 3. Palpate length of spinous processes. 4. Percuss over all lung fields. |
 |
| Move around to face the patient; the patient remains sitting. For a female breast examination, ask permission to lift gown to drape on the shoulders, exposing the anterior chest; for a male, lower the gown to the lap. | |
 |
|
 |
|
Help the woman to lie supine with head at a flat to 30-degree angle. Stand at the person’s right side. Drape the gown up across shoulders and place an extra sheet across lower abdomen. 3. Palpate each breast, lifting the same side arm up over head. Include the tail of Spence and areola. |
|
 |
|
1. Inspect the praecordium for any pulsations or heave (lift). 2. Palpate the apical impulse and note the location. 3. Auscultate apical rate and rhythm. 4. Auscultate with the diaphragm of the stethoscope to study heart sounds, inching from the apex up to the base, or vice versa. 5. Turn the person over to left side while again auscultating apex with the bell. |
 |
| The person should be supine, with the bed or table flat; arrange drapes to expose the abdomen from the chest to the pubis. | |
 |
|
 |
|
 |
|
| Ask the person to sit up and to dangle the legs off the bed or table. Keep the gown on and the drape over the lap. | |
 |
|
 |
|
| Ask the person to stand with the gown on. Stand close to the person. |
 |
 |
|
 |
|
 |
|
 |
|
| Tell the patient you are finished with the examination and that you will leave the room as they get dressed. Return to discuss the examination and further plans and to answer any questions. Thank the person for their time. | |
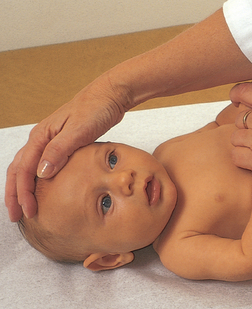
Review Chapter 8 for the steps on preparation and positioning and on developmental principles of the infant. The 1-minute and 5-minute Apgar results will give important data on the neonate’s immediate response to extrauterine life. The following sequence will expand these data. You may reorder this sequence as the infant’s sleep and wakefulness state or physical condition warrants. The infant is supine on a warming table or examination table with an overhead heating element. The infant may be nude except for a nappy over a boy. |
 |
 |
|
1. Inspect the skin condition over the chest and abdomen, chest configuration and nipples and breast tissue. 2. Note movement of the abdomen with respirations, and any chest retraction. 3. Palpate apical impulse and note its location. 4. Auscultate breath sounds, apical heart sounds and bowel sounds in the abdomen and in the chest. |
 |
 |
|
 |
|
| To open the neonate’s eyes, support the head and shoulders and gently lower the baby backwards, or ask the parent to hold the baby over their shoulder while you stand behind the parent. | |
 |
|
 |
|
 |
|
1. Inspect and manipulate, noting ROM, muscle tone and absence of scarf sign (elbow should not reach midline). 2. Count fingers, count palmar creases and note colour of hands and nail beds. 3. Place your thumbs in the infant’s palms to note the grasp re.ex, then wrap your hands around infant’s hands to pull up and note the head lag. |
 |
 |
|
| Lift the infant under the axillae, and hold the infant facing you at eye level. | |
1. Note shoulder muscle tone and the infant’s ability to stay in your hands without slipping. 2. Rotate the neonate slowly side to side; note the doll’s eye re.ex. 3. Turn the infant around so their back is to you; elicit the stepping reflex and the placing reflex against the edge of the examination table. |
 |
| Turn the infant over and hold them prone in your hands, or place the infant prone on the examination table. | |
 |
|
 |
|
Review the developmental considerations in preparing for an examination of the toddler and the young child in Chapter 8. A young child during this time is beset with independence and dependence needs on the parent, is aware of and fearful of a new environment, has a fear of invasive procedures, dislikes being restrained and may be attached to a security object. |
 |
1. Note child’s ability to amuse themself while the parent speaks. 2. Note parent and child interaction. 3. Note gross motor and fine motor skills as the child plays with toys. Gradually focus on and involve yourself with the child, at first in a ‘play’ period. 4. Evaluate developmental milestones by using a Denver II test: gait, jumping, hopping, building a tower and throwing a ball. 5. Evaluate posture while the child is sitting and standing. Evaluate alignment of the legs and feet while the child is walking. 6. Evaluate speech acquisition. |
 |
| Ask the parent to undress the child to the nappy or the underpants. Position the older infant and young child, 6 months to 2 or 3 years, in the parent’s lap. Move your chair to sit knee-to-knee with the parent. A 4- or 5-year-old child usually feels comfortable on the examination table. |
 |
1. Auscultate breath sounds and apical heart sounds, count respiratory rate, count heart rate and auscultate bowel sounds. 2. Inspect size, shape and configuration of chest cage. Assess respiratory movement. 3. Inspect pulsations on the praecordium. Note nipple and breast development. 4. Palpate apical impulse and note location, chest wall for thrills. |
 |
| The child should be sitting up in the parent’s lap or on the examination table, nappy or underpants in place. | |
 |
|
| The child should be sitting up in the parent’s lap or on the examination table, nappy or underpants in place. | |
 |
|
 |
|
1. Inspect the external structures. Note any palpebral slant. 2. With a penlight, test the corneal light and pupillary light reflexes. 3. Direct a moving penlight for cardinal positions of gaze. 4. If indicated, perform the cover test, covering the eye with your thumb in a young child, or use an index card. |
 |
 |
|
1. Inspect and palpate the auricle. Note any discharge from the auditory meatus. Check for any foreign body. 2. With an otoscope, inspect the ear canal and tympanic membrane. Gain cooperation through the use of a puppet, encouraging the child to handle the equipment or to look in the parent’s ear as you hold the otoscope. You may need to have the parent help restrain the child. |
 |
THE SCHOOL-AGE CHILD, THE ADOLESCENT AND THE ADULT OVER 65 YEARS The sequence of the examination for people in these age groups is the head-to-toe format described in the adult section. However, you should be aware of differences in approach and timing and special developmental considerations. Review Chapter 8 for a full discussion of these factors. |
 |
DOCUMENTATION AND CRITICAL THINKING
RECORDING THE DATA
Record the data from the history and physical examination as you conduct the assessment. The documentation of your findings should be systematic, comprehensive and detailed. This includes charting relevant normal or abnormal findings. On the other hand, a listing of every assessment parameter described in this text yields an unwieldy, unworkable record. One way to keep your record complete yet succinct is to study your writing style. Use short, clear phrases. Avoid redundant introductory phrases such as, ‘The patient states that …’
Use simple line drawings to describe your findings. You do not need artistic talent; draw a simple sketch of a tympanic membrane, breast, abdomen or cervix and mark your findings on it. A clear picture is worth many sentences of words.
Refer to the following example of a complete history and physical examination. Note that the subject is the same young woman introduced in Chapter 1 of this text.
HEALTH HISTORY
Ellen K is a 23-year-old, single, currently unemployed for 6 months.
Source. Ellen, seems reliable.
Reason for seeking care. ‘I’m coming in for alcohol treatment.’
History of present illness. First alcoholic drink, age 16. First intoxication, age 17, drinking one to two times per week, a 6-pack per occasion. Was attending high school classes every day, but grades slipped from A−/B+ average to C− average. At age 20, drinking two times per week, six to nine beers per occasion. At age 22, drinking two times per week, a 12-pack per occasion, and occasionally a 6-pack the next day to ‘help with the hangover’. During this year, experienced blackouts, failed attempts to cut down on drinking, being physically sick the morning after drinking and being unable to stop drinking once started. Also, incurred a ‘drink-driving’ offence which resulted in licence cancellation.
Childhood illnesses. Chickenpox at age 6. No measles, mumps, croup, pertussis.
Accidents. 1. Motor vehicle accident, age 12, father driving, Ellen thrown from car, right leg crushed. Hospitalised, surgery for leg pinning to repair multiple compound fracture. 2. Motor vehicle accident, age 21, head hit dashboard, no loss of consciousness, treated and released from hospital ED.
Hospitalisations. Age 12, surgery to repair right leg.
Obstetric history. No pregnancies.
Immunisations. Childhood immunisations up to date. Last tetanus ‘probably high school’.
Last examinations. Last dental examination 8 years ago; last vision test for driver’s licence age 18, never had ECG, chest x-ray study.
Allergies. No known allergies.
Current medications. Oral contraceptives, low-oestrogen type, 1/day, for 5 years. No other prescription or over-the-counter medications.
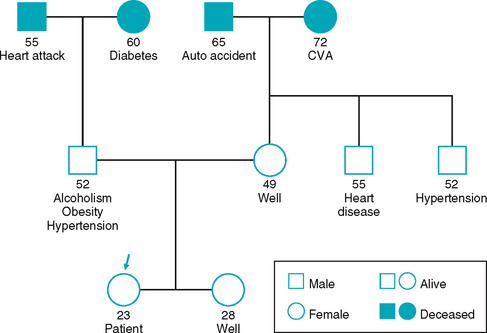
Ellen is second youngest child, parents divorced 8 years, father has chronic alcoholism. See family genogram below.
Health perception. Identifies alcohol as a health problem for herself, feels motivated for treatment. Never been interested in physical health and own body before, ‘Now I think it’s time I learned’. Expects healthcare providers to ‘Help me with my drinking. I don’t know beyond that’. Expects to stay at this place for 6 weeks, ‘Then, I don’t know what’.
General health. Reports usual health ‘OK’. No recent weight change, no fatigue, weakness, fever, sweats.
Sleep-Rest: bedtime 1 am. Sleeps 10–11 hours. No sleep aids.
Believes housing adequate, adequate heat and utilities, and neighbourhood safe. Believes home has no safety hazards. Uses seat belts. Identifies current stresses to be drinking, loss of driver’s licence, unemployment, financial worries. Considers her drinking to be problematic.
Typical day: arises midday, light chores or TV, spends day looking for work, running errands, with friends, bedtime at 1 am. No sustained physical exercise. Believes self able to perform all ADLs; limp poses no problem in bathing, dressing, cooking, household tasks, mobility. No mobility aids. Hobbies are listening to music, watching DVDs, going to pubs with friends, communicating with friends on Facebook. Currently lack of finances restricts social activities.
Describes family life growing up as chaotic. Father physically abusive towards mother and sexually abusive towards Ellen. Parents divorced because of father’s continual drinking. Few support systems currently. Estranged from mother, ‘didn’t believe me about my father’. Father estranged from entire family. Gets along ‘OK’ with sister. Relationship with boyfriend chaotic, has hit her twice in the past. Ellen has never pressed legal charges. No close women friends. Most friends are ‘drinking buddies’ at pub.
Cardiovascular function. No chest pain, palpitation, cyanosis, fatigue, dyspnoea with exertion, orthopnoea, paroxysmal nocturnal dyspnoea, oedema. No history of heart murmur, hypertension, coronary artery disease, or anaemia.
No pain, numbness or tingling, swelling in legs. No coldness, discolouration, varicose veins, infections, or ulcers. Legs are unequal in length as sequela of accident age 12. Self-care.
Respiratory function. No history of lung disease, no chest pain with breathing, wheezing, shortness of breath. Colds sometimes ‘go to my chest’, treats with over-the-counter cough medicine and paracetamol. Occasional early morning cough, nonproductive. Smokes cigarettes 2 PPD × 2 years, prior use 1 PPD × 4 years. Never tried to quit. Boyfriend smokes cigarettes.
No nasal discharge, has two to three colds per year, no sinus pain, nasal obstruction, epistaxis or allergy. No hoarseness or sore throat. Has tonsils.
Musculoskeletal function. No history of arthritis, gout. No joint pain, stiffness, swelling, deformity, limitation of motion. No muscle pain, or weakness. Bone trauma at age 12, has sequela of unequal leg lengths, right leg shorter, walks with limp. Self-care. No walking or running for sport or exercise ‘because of leg’. Uses lift pad in right shoe to equalise leg length.
Nutrition and metabolism. Appetite good with no recent change. No food intolerance, indigestion, pain in abdomen, nausea or vomiting. No history of ulcers, liver or gallbladder disease, jaundice, appendicitis or colitis. 24-hour recall: breakfast, none; lunch, sandwich, chips, diet cola drink; dinner, hamburger, chips, coffee; snacks, peanuts, potato chips. This menu is typical of most days. Eats lunch at home alone. Most dinners at fast food restaurants. Shares household grocery expenses and cooking chores with sister. No food intolerances.
Paternal grandmother has diabetes. No increase in hunger, thirst or urination; no problems with hot or cold environments; no change in skin, appetite or nervousness.
No mouth pain, bleeding gums, toothache, sores or lesions in mouth, or dysphagia. Self-care. Brushes teeth twice/day, no flossing.
No change in skin colour, pigmentation or naevi. No pruritus, rash, lesions. Has bruise now over right eye, struck by boyfriend 1 week ago. No history skin disease. Hair, no loss, change in texture. Nails, no change. Self-care. Stays in sun ‘as much as I can’. No use of sunscreen. No bleeding problems in skin, excessive bruising. Not aware of exposure to toxins, never had blood transfusion, never used needles to inject drugs.
Bowel function. Bowel movement 1/day, soft, brown (Bristol 4), no rectal bleeding or pain. Self-care. No use of vitamins, antacids, laxatives.
Urinary function. No dysuria, frequency, urgency, nocturia, hesitancy or straining. No pain in flank, groin, suprapubic region. Urine colour yellow, no history kidney disease.
Mental status. Graduated from high school. Trained ‘on-the-job’ as bartender, also worked in a supermarket. Unemployed now, ‘on the dole’, does not believe she has enough money for daily living. Lives with older sister. Raised as Presbyterian, believes in God, does not attend church. Believes self to be ‘honest, dependable’. Believes limitations are ‘smoking, weight, drinking’.
Neurological and sensory function. No unusually frequent or severe headaches, no head injury, dizziness, syncope, or vertigo. No neck pain, limitation of motion, lumps or swollen glands.
No history of seizure disorder, stroke, fainting. Has had blackouts with alcohol use. No weakness, tremor, paralysis, problems with coordination, difficulty speaking or swallowing. No numbness or tingling. Not aware of memory problem, nervousness or mood change, depression. Had counselling for sexual abuse in the past. Does not report any suicidal ideation or intent during adolescent years or now.
No difficulty with vision or double vision. No eye pain, inflammation, discharge, lesions. No history glaucoma or cataracts. Wears no corrective lenses.
No hearing loss or difficulty. No earaches, infections now or as child, no discharge, tinnitus or vertigo. Self-care. No exposure to environmental noise, cleans ears with washcloth.
Sexuality and reproductive function. Menarche age 11. Last menstrual period 18 April. Cycle usually q 28 days, duration 4 to 5 days, flow moderate, no dysmenorrhoea. No vaginal itching or discharge, sores or lesions.
In relationship now that includes intercourse. This boyfriend has been her only sexual partner for 2 years, had one other partner before that. Uses oral contraceptives, partner uses no condoms. Concerned that boyfriend may be having sex with other women but has not confronted him. Aware of no STI contact. Never been tested for HIV. History of sexual abuse by father from ages 12 to 16 years, abuse did not include intercourse. Ellen is unwilling to discuss further at this time.
No breast pain, lump, nipple discharge, rash, swelling or trauma. No history breast disease in self, mother or sister. No surgery. Self-care. Does not know about breast awareness.
PHYSICAL EXAMINATION
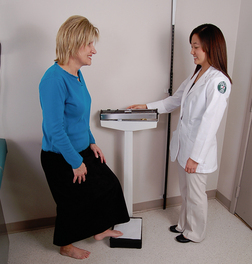
Height: 163 cm Weight: 68.6 kg
B/P: 142/100 right arm, sitting
Temp: 37°C. Pulse: 76, regular. Respirations: 16, unlaboured
General survey. Ellen K is a 23-year-old female, not currently under the influence of alcohol or other drugs, who articulates clearly, ambulates without difficulty and is in no distress.
Cardiovascular function. Colour tan-pink, no redness, cyanosis, lesions other than surgical scar. Scar right lower leg, anterior, 28 cm× 2 cm wide, well healed. No oedema, varicosities. No calf tenderness. All peripheral pulses present, 2+ and = bilaterally. Nail beds pink and firm with brisk capillary refill.
Apical impulse at 5th ics in left MCL. Normal heart sounds.
Respiratory function. Nose: no deformities or tenderness to palpation. Nares patent. Mucosa pink, no lesions. Septum midline, no perforation. No sinus tenderness.
Pharynx pink, no exudate. Tonsils 1+. Trachea midline.
Chest expansion symmetrical. Breath sounds diminished bilaterally. Expiratory wheeze in posterior chest at both bases, scattered crackles in posterior chest at both bases, that does not clear with coughing.
Musculoskeletal function. GALS screen: gait—limp on right side due to asymmetrical leg length, right leg 3 cm shorter than left. Arms, legs and spine normal. No pain on movement. Muscle strength, able to maintain flexion against resistance and without tenderness.
Mouth: mucosa and gingivae pink, no lesions or bleeding. Right lower 1st molar missing, multiple dark spots on most teeth, gums receding on lower incisors. Tongue symmetrical, protrudes midline, no tremor. Uvula rises midline on phonation. Gag reflex present. Temporomandibular joint no slipping or crepitation.
Skin, hair and nails: uniformly tan-pink in colour, warm, dry, intact, turgor good. No lesions, birthmarks, oedema. Resolving 2-cm yellow-green haematoma present over right eye, no swelling, ocular structures not involved. Hair, normal distribution and texture. No lesions, lumps, scaling, parasites, or tenderness on scalp. Nails, no clubbing, biting or discolourations.
Abdomen: flat, symmetrical. Skin smooth with no lesions, scars or striae. Bowel sounds present. Tympany predominates in all quadrants. Abdomen soft, no masses or tenderness.
Mental status. Appearance, behaviour, speech appropriate. Alert and oriented to person, place, time. Thought coherent. Remote and recent memories intact.
Neurological and sensory function. Face, symmetrical, no weakness, no involuntary movements. Neck supple with full ROM. Symmetrical, no masses or tenderness.
Motor: no atrophy, weakness or tremors. Gait has limp.
Eyes. Visual fields full by confrontation. EOMs intact, no nystagmus. No ptosis, lid lag, discharge or crusting. Corneal light reflex symmetrical, no strabismus. Conjunctivae clear. Sclera white, no lesion or redness. PERRLA.
Ears. Pinna no mass, lesions, scaling, discharge or tenderness to palpation. Canals clear. Tympanic membrane pearly grey, landmarks intact, no perforation. Whispered words heard bilaterally.
Sexuality and reproductive function. External genitalia has no lesion, discharge.
Breasts: symmetrical; no retraction, discharge or lesions. Contour and consistency firm and homogeneous. No masses or tenderness, no lymphadenopathy.
Patient problems/Nursing diagnoses
Alcohol abuse for referral to medial practitioner for further assessment
Ineffective airway clearance R/T tracheobronchial secretions and obstruction
Right orbital contusion (resolving)
Self-care deficit: oral hygiene R/T lack of motivation
Deficient knowledge about alcoholism disease process, treatment options, support systems
Deficient knowledge about ‘quit’ smoking techniques