Chapter 21 NURSING MANAGEMENT: visual and auditory problems
1. Describe the types of refractive errors and appropriate corrections.
2. Outline the aetiology and multidisciplinary care of extraocular disorders.
3. Explain the pathophysiology, clinical manifestations, and nursing management and multidisciplinary care of the patient with selected intraocular disorders.
4. Apply clinical decision making in order to plan and implement appropriate nursing measures that promote optimal function of the eyes and ears.
5. Explain the general preoperative and postoperative care of the patient undergoing surgery of the eye or ear.
6. Outline the action and uses of drug therapy for treating problems of the eyes and ears.
7. Explain the pathophysiology, clinical manifestations, and nursing management and multidisciplinary care of common ear problems.
8. Compare the causes, management and rehabilitative potential of conductive and sensorineural hearing loss.
9. Explain the use, care and patient teaching related to assistive devices for eye and ear problems.
10. Describe the common causes and assistive measures for uncorrectable visual impairment and deafness.
11. Describe available measures to assist the patient in adapting psychologically to decreased vision and hearing.
Correctable refractive errors
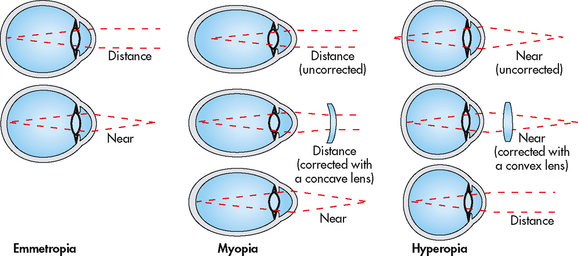
Uncorrected refractive error accounts for about half of all avoidable vision impairment cases and nearly a third of avoidable blindness cases throughout the world.1 This defect prevents light rays entering the eye from converging into a single focus on the retina. Defects arise from irregularities of the corneal curvature, the focusing power of the lens or the length of the eye. The major symptom is blurred vision. In some cases the patient may also complain of ocular discomfort, eye strain or headaches. Patient with refractive errors need to use corrective lenses to improve the focus of light rays on the retina (see Fig 21-1).
In the 2007–2008 Australian National Health Survey, 52% of those surveyed reported problems with their eyesight, including myopia (23%, nearsightedness) and hyperopia (26%, farsightedness).2 These figures are similar to previous prevalence estimates. Presbyopia, which is farsightedness resulting from a decrease in the accommodative ability of the eye as a result of ageing, is less common.
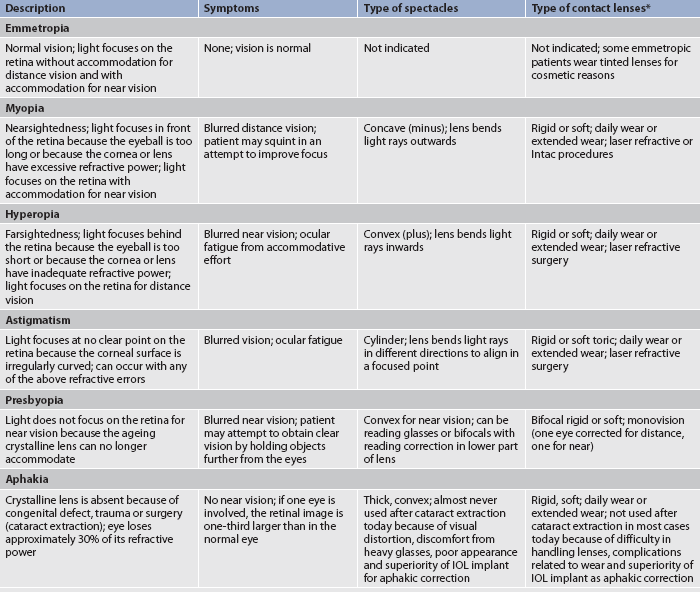
Table 21-1 summarises the types of refractive errors and the appropriate corrections. Contrary to common belief, uncorrected refractive errors do not worsen the error, nor do they cause further pathology. However, refractive errors in young children should be corrected because children may develop amblyopia (reduced vision in the affected eye) if their refractive error is uncorrected. An Australian study indicated that in the Blue Mountains region of New South Wales amblyopia was diagnosed in 3.2% of the population over 49 years of age, with causes being identified as anisometropia (27%) and strabismus (19%).3 No significant associations were found between amblyopia and gender or the eye affected (e.g. right or left).
MYOPIA
In myopia (nearsightedness) the light rays are focused in front of the retina. Myopia may occur because of excessive light refraction by the cornea or lens or because of an abnormally long eye. Myopia may also occur because of lens swelling, which occurs when blood glucose levels are elevated, as in uncontrolled diabetes. This type of myopia is transient and variable and fluctuates with the blood glucose level.4
HYPEROPIA
In hyperopia (farsightedness) the light rays focus behind the retina and the patient must use accommodation to focus the light rays on the retina for near and far objects. This type of refractive error occurs when the cornea or lens does not have adequate focusing power or when the eyeball is too short.
HEALTH DISPARITIES
• Most of the vision-impaired people in Australia and New Zealand are over 65 years of age.
• Indigenous Australian and Māori people are more prone to visual and hearing impairment than people living in urban areas.
• Indigenous Australians suffer blindness 10 times more frequently than non-Indigenous Australians.
• Blindness in Indigenous Australians is often related to trachoma, cataract or diabetes.
• Access to adequate healthcare may not be as readily available for Indigenous people of Australia and New Zealand, older people or people living in rural or remote Australia or New Zealand.
PRESBYOPIA
Presbyopia is the loss of accommodation associated with age. This condition generally appears at about age 45 years. As the eye ages, the crystalline lens becomes larger, firmer and less elastic. These changes, which progress with ageing, decrease the eye’s accommodative ability. People with presbyopia have difficulty focusing on near objects without some visual aid.5
ASTIGMATISM
Astigmatism is caused by an irregular corneal curvature. This irregularity causes the incoming light rays to be bent unequally. Consequently, the light rays do not come to a single point of focus on the retina. Astigmatism can occur in conjunction with any of the other refractive errors.
APHAKIA
Aphakia is defined as the absence of the crystalline lens. The lens may be absent congenitally or it may be removed during cataract surgery. A lens that is traumatically dislocated results in functional aphakia, although the lens remains in the eye. Since the lens accounts for approximately 30% of ocular refractive power, the absence of the lens results in a significant refractive error.6 Without the focusing ability of the lens, images are projected behind the retina.
NON-SURGICAL CORRECTIONS
Corrective glasses
Myopia, hyperopia, presbyopia, astigmatism and aphakia can be modified by using the appropriate corrective lens (see Table 21-1). Myopia requires a minus corrective lens (concave), whereas hyperopia, presbyopia and aphakia all require a plus corrective lens (convex). Glasses for presbyopia are often called reading glasses because they are usually worn for close work only. The presbyopic correction may also be combined with a correction for another refractive error, such as myopia or astigmatism. In these combined glasses the presbyopic correction is in the lower portion of bifocal or trifocal glasses. A newer type of correction for presbyopia, the no-line bifocal, is actually a multifocal lens that allows the patient to see clearly at any distance.
Aphakic glasses are very thick, making them heavy and unattractive to wear. The high degree of correction also causes images to be magnified about 25%. With the modern surgical procedures prevalent today, patients seldom wear aphakic glasses for correction because of the associated visual problems.
Contact lenses
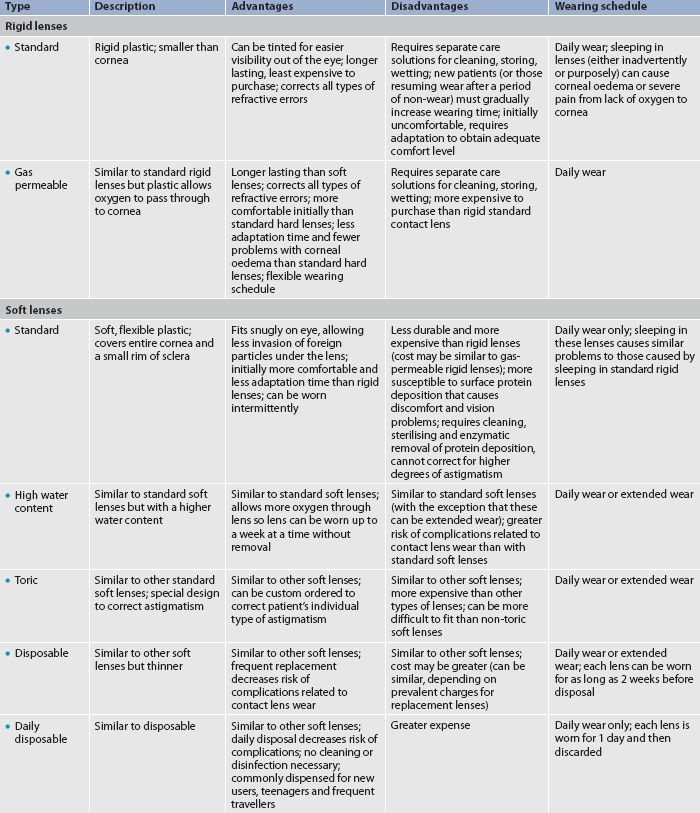
Contact lenses are another way to correct refractive errors. Contact lenses generally provide better vision than glasses because the patient has more normal peripheral vision without the distortion and obstruction of the glasses and their frames. Aphakic contact lenses magnify objects only approximately 7% and are visually superior to aphakic glasses.7 However, many older patients have difficulty handling and caring for contact lenses. Table 21-2 describes the various types of contact lenses and the advantages and disadvantages of each.
Lenses may be either rigid or flexible (soft lenses). Rigid contact lenses ride on the tear film layer of the cornea and are held in place by surface tension. Blinking causes the tear film to move under and over the contact lens, providing oxygen for the cornea. If the oxygen supply to the cornea is decreased, it becomes swollen, visual acuity decreases and the patient experiences severe discomfort.
Soft contact lenses do not ride on the corneal tear film layer so the cornea cannot receive oxygen from the tear film. Instead, the cornea receives oxygen through the soft contact lens, which is permeable to oxygen. Gas-permeable rigid contact lenses also allow oxygen to reach the cornea through the lens itself.
Altered or decreased tear formation can make wearing contact lenses difficult. Tear production can be decreased by antihistamines, decongestants, diuretics, oral contraceptives and hormones produced during pregnancy. Allergic conjunctivitis with itching, tearing and redness can also affect contact lens wear.
In general, the nurse must know whether the patient wears contact lenses, the pattern of wear (daily versus extended) and care practices. The nurse must be able to identify whether contact lenses are present and should know how to remove them in an emergency situation. Shining a light obliquely on the eyeball can help visualise a contact lens. A hard contact lens can be removed with a small suction cup designed for that purpose.
Patients should know the signs and symptoms of contact lens problems that must be managed by the eye care professional. They may remember these symptoms better if the nurse uses the mnemonic RSVP:
The nurse must stress the importance of removing contact lenses immediately if any of these problems occur.
SURGICAL THERAPY
Surgical procedures are designed to eliminate or reduce the need for glasses or contact lenses and correct refractive errors by changing the focus of the eye. Surgical management for refractive errors includes laser, intraocular lens (IOL) implant and thermal procedures.
Laser procedures
Laser-assisted in situ keratomileusis (LASIK) may be considered for patients with low to moderately high amounts of myopia, hyperopia and astigmatism. The procedure has two basic steps: first, using a laser or surgical blade, a thin flap is created in the cornea. Second, using ‘wave-front’ technology, the laser is programmed to use a map of the patient’s cornea to sculpt the cornea and correct the refractive error. The flap is then repositioned and adheres on its own without sutures in a few minutes.8,9
Photorefractive keratectomy (PRK) uses a laser to reshape the central corneal surface and is indicated for low to moderate amounts of myopia, hyperopia and astigmatism. It is a good option for a patient with insufficient corneal thickness for a LASIK flap. Although it is successful in treating lesser degrees of hyperopia, the unpredictability of the results for higher degrees of hyperopia make it an unacceptable recommendation of treatment at present.10 Evidence supports claims that LASIK creates earlier visual stability in patients with a high degree of myopia than does PRK.9 In PRK only the epithelium is removed and the laser sculpts the cornea to correct the refractive error. Laser-assisted epithelial keratomileusis (LASEK) is similar to PRK except that the epithelium is replaced after surgery.
Implants
Intracorneal ring segments (ICRs) are two semicircular pieces of plastic that are implanted between the layers of the cornea to treat mild forms of myopia. They are designed to change the shape of the cornea by adjusting the focusing power. ICRs can be removed and the cornea will usually return to its original shape within a few weeks.
Refractive intraocular lenses (refractive IOLs) are an option for patients with a high degree of myopia or hyperopia. Like cataract surgery, this involves the removal of the patient’s natural lens and implantation of an IOL, which is a small plastic lens designed to correct the patient’s refractive error. Since this requires entering the eye, the risk of complications is higher. New accommodating IOLs will correct both myopia and presbyopia.
Phakic intraocular lenses (phakic IOLs) are sometimes referred to as implantable contact lenses. They are implanted into the eye without removing the eye’s natural lens. They are used for patients with high degrees of myopia and hyperopia. Unlike refractive IOLs, the phakic IOL is placed in front of the eye’s natural lens. By leaving the natural lens in the eye, the ability of the eye to focus for reading vision is preserved.
Thermal procedures
Laser thermal keratoplasty (LTK) and conductive keratoplasty (CK) are procedures for patients with hyperopia or presbyopia. Using laser or high radiofrequency radiation, heat is applied to the peripheral area of the cornea to tighten it like a belt and make the central cornea steeper. Only the less dominant eye is treated and the desired effect is monovision. Monovision enables one eye to focus at close proximity and the other is left untreated or, if needed, treated to focus at a distance. A preoperative trial with contact lenses is a useful test to see whether a patient will adapt to the intended refractive outcome.
Uncorrectable vision impairment
The patient with correctable errors of vision is not functionally impaired. When no correction is possible, the patient’s visual impairment may be moderate or profound. It is estimated that 70–80% of blindness is preventable. In 2004, the prevalence of visual impairment was estimated at just under 500,000 Australians and this figure is set to increase to 800,000 by 2024 when the entire baby boomer generation has reached retirement age.11 In New Zealand there are approximately 12,000 blind or partially sighted people, and every year almost 1500 people become blind or experience serious loss of sight.12 It is highly probable that there is underreporting of significant visual impairment. This may be due to the ongoing nature of visual impairment for some people, whereas for others it may be an unwillingness to acknowledge the full extent of visual loss. The partially sighted individual may have significant visual abilities. It is important when working with visually impaired patients to understand that a person classified as blind may have some useful vision. Appropriate responses and interventions depend on the nurse’s understanding of each patient’s visual abilities.
LEVELS OF VISION IMPAIRMENT
Patients may be categorised by the level of visual loss.13 Low vision is a form of vision impairment that involves irreversible vision loss. Low vision is significantly reduced vision but not blindness. The World Health Organization (WHO) defines low vision in two ways. From an epidemiological perspective, it is defined by measures of visual acuity and/or visual field, as when visual acuity is less than 6/18 and equal to or better than 3/60 in the better eye with best correction.13,14 From a service provision perspective, low vision is defined in functional terms if a person has impairment of visual functioning even after treatment and/or standard refractive correction, and has a visual acuity of less than 6/18 to light perception, but uses, or is potentially able to use, vision for the planning and/or execution of a task.14 WHO estimates that there are 124 million people with low vision worldwide, 90% of whom live in developing countries.15
Legally blind is a term used in Australia to determine a person’s low vision level where there is no possibility of correcting vision through treatments such as surgery, laser or corrective glasses. Legally blind individuals can have some usable vision. The majority of people who are legally blind (i.e. have less than 6/60 vision in the better eye or a field of vision restricted to 20° in diameter or less, or a combination of both) will most likely be eligible to receive special benefits or services.13,14 They may use vision substitutes, such as guide dogs and canes for ambulation and Braille for reading. Vision enhancement techniques (see below) are not usually helpful. Total blindness is defined as no light perception and no usable vision.
Partially sighted individuals who are not legally blind have a corrected visual acuity greater than 6/60 in the better eye and greater than 20° of visual field, but the visual acuity is 6/15 or worse in the better eye. Patients who are partially sighted can benefit greatly from visual assistive technology. Assistive technology refers to all equipment and technology, both hardware and software, that assists people to access or participate in a particular activity or range of activities. Examples of assistive technologies can be found on Vision Australia’s website (see Resources on p 506).
 NURSING MANAGEMENT: VISION IMPAIRMENT
NURSING MANAGEMENT: VISION IMPAIRMENT
 Nursing assessment
Nursing assessment
Nursing assessment of the patient with vision impairment should involve assessment of the patient’s health promotion practices and history, the potential factors that may affect the sensory function and the extent of the impact on their lifestyle, as well as their expectations regarding the alterations they are experiencing. Appropriate assessment involves the nurse’s: (1) knowledge of the specific deficit and the relevant pathophysiology and effects, and communication principles used for patient–nurse interaction; (2) application of relevant standards of clarity, precision and depth during assessment; (3) experience in caring for patients with such impairments; and (4) attitude and ability to provide a competent level of care.4
It is important to determine how long the patient has had vision impairment because recent loss of vision has different implications for nursing care. The nurse should determine how the patient’s vision impairment affects normal functioning. This may be done by questioning the patient about the level of difficulty encountered when doing certain tasks. For example, the nurse may ask how much difficulty the patient has when reading a newspaper, writing a cheque, moving from one room to the next or watching television. Other questions can help the nurse determine the personal meaning that the patient attaches to the vision impairment. The nurse can ask how the vision loss has affected specific aspects of the patient’s life, whether the patient has lost a job or what activities the patient does not engage in because of the vision impairment. The patient may attach many negative meanings to the impairment because of societal views of blindness. For example, patients may view the impairment as punishment or view themselves as useless and burdensome. It is also important to determine the patient’s primary coping strategies and emotional reactions, and the availability and strength of support systems.
 Nursing diagnoses
Nursing diagnoses
Nursing diagnoses and identification of patient problems depend on the degree of vision impairment and how long it has been present. Nursing diagnoses for the vision-impaired patient include, but are not limited to, the following:
• disturbed sensory perception related to vision deficit
• risk of injury related to vision impairment and inability to see potential dangers
• self-care deficits related to vision impairment
• fear related to inability to see potential danger or accurately interpret environment
• anticipatory grieving related to loss of functional vision.
 Planning
Planning
When planning care, the nurse should work with the patient to choose strategies that will assist or enable the patient to remain functional within their own home as far as possible. The overall goals for the patient with recently impaired vision or the patient with impaired adjustment to longstanding vision impairment are that the patient will: (1) make a successful adjustment to the impairment; (2) verbalise feelings related to the loss; (3) identify personal strengths and external support systems; and (4) use appropriate coping strategies. If the patient has been functioning at an appropriate or acceptable level, the goal is to maintain the current level of function.
 Nursing implementation
Nursing implementation
 Health promotion
Health promotion
The nurse should encourage the partially sighted patient with preventable causes of further vision impairment to seek appropriate healthcare. For example, the patient with vision loss from glaucoma may prevent further visual impairment by complying with prescribed therapies and suggested ophthalmic evaluations.
 Acute intervention
Acute intervention
It is important to provide care that addresses the following major areas: environmental management, emotional support and family involvement. The nurse provides emotional support and direct care to the patient with recent visual impairment. Active listening and grief work facilitation are important components of nursing care for the recently visually impaired patient. The nurse should allow the patient to express anger and grief and should help the patient to identify their fears and successful coping strategies. The family is intimately involved in the experiences that follow vision loss. With the patient’s knowledge and permission, the nurse should include family members in discussions and encourage members to express their concerns.
Many people are uncomfortable around a blind or partially sighted individual because they are not sure what behaviours are appropriate. Sensitivity to the patient’s feelings without being overly solicitous or stifling the patient’s independence is vital in creating a therapeutic nursing presence. The nurse should always communicate in a normal conversational tone and manner with the patient, and should address the patient, not a family member or friend who may be with the patient. Common courtesy dictates introducing oneself and any other persons who approach the blind or partially sighted patient and saying goodbye on leaving. Making eye contact with the partially sighted patient accomplishes several objectives. It ensures that the nurse speaks while facing the patient so that the patient has no difficulty hearing the nurse. The nurse’s head position validates that the nurse is attentive to the patient. Also, establishing eye contact ensures that the nurse can observe the patient’s facial expressions and reactions.
The nurse should explain any activities or noises occurring in the patient’s immediate surroundings. Orientation to the environment lessens the patient’s anxiety or discomfort and facilitates independence. In orienting the partially sighted or blind patient to a new area, the nurse should identify one object as the focal point and describe the location of other objects in relation to it. For example, the nurse may say, ‘The bed is straight ahead, approximately 10 steps. The chair is to the left, and the nightstand is to the right, near the head of the bed. The bathroom is to the left of the foot of the bed.’
The nurse should assist the patient to each major object in the area, using the sighted-guide technique. When using this technique, the nurse stands slightly in front and to one side of the patient and offers an elbow for the patient to hold. The nurse serves as the sighted guide, walking slightly ahead of the patient with the patient holding the back of the nurse’s arm (see Fig 21-2). When using this technique in any situation, the nurse should describe the environment to help orient the patient. For example, the nurse may say, ‘We’re going through an open doorway and approaching two steps down. There is an obstacle on the left.’ To assist patients to sit, the nurse should place one of the patient’s hands on the back of the chair.
 Ambulatory and home care
Ambulatory and home care
Rehabilitation after partial or total loss of vision can foster independence, self-esteem and productivity. The nurse should know what services and devices are available for the partially sighted or blind patient and should be prepared to make appropriate referrals for those services and devices. A list of agencies that serve partially sighted or blind patients in Australia is available from Vision Australia (see Resources on page 506). In New Zealand, the Royal New Zealand Foundation of the Blind assists people to maintain independence and lifestyle after vision loss by teaching them the safest techniques for moving around (see Resources on p 506).12 Instructors in techniques of daily living teach clients how to undertake everyday tasks, such as cooking, eating, sorting laundry and getting money from an automatic teller machine. Other agencies are listed in the Resources on page 506.
Using Braille or audio books for reading and a cane or guide dog for ambulation are examples of vision substitution techniques. These are usually most appropriate for patients with no functional vision. For most patients who have some remaining vision, vision enhancement techniques can provide enough help for them to learn to ambulate, read printed material and accomplish activities of daily living.
 Optical devices for vision enhancement
Optical devices for vision enhancement
Telescopic lenses for near or far vision and magnifiers of various types can often enhance patients’ remaining vision enough for them to be able to perform many previously impossible tasks and activities. Most of these devices require some training and practice for successful use.16 Closed-circuit television can provide magnification up to 60 times, allowing some patients to read, write, use computers and do crafts. Although these systems are expensive and have limited portability, they are available in some public or university libraries.
 Non-optical methods for vision enhancement
Non-optical methods for vision enhancement
Approach magnification is a simple but sometimes overlooked technique for enhancing the patient’s residual vision. The nurse can recommend that the patient sit closer to the television or hold books closer to their eyes, which the patient may be reluctant to do unless encouraged. Contrast enhancement techniques include watching television in black and white, placing dark objects against a light background, or vice versa (e.g. a white plate on a black placemat), using a black felt-tip marker and using contrasting colours (e.g. a red stripe at the edge of steps or kerbs). Increased lighting can be provided by halogen lamps, direct sunlight or gooseneck lamps that can be aimed directly at the reading material or other near objects. Large type is often helpful, especially in conjunction with other optical or non-optical vision enhancements.
Gerontological considerations: visual impairment
The older patient is at an increased risk of vision loss because cataracts, glaucoma, diabetic retinopathy, macular degeneration and other potential causes of visual impairment are more common in older patients. This is particularly so for the Indigenous population of Australia. Older patients may have other deficits, such as cognitive impairment or limited mobility, which further affect the ability to function in usual ways. Societal devaluation of older people may compound the self-esteem or isolation issues associated with the older patient’s visual impairment. Financial resources may meet normal needs but can be inadequate in meeting increased demands associated with vision services or devices.
Older patients may become confused or disoriented when visually compromised. The combination of decreased vision and confusion increases the risk of falls, which have potentially serious consequences for the older adult. Decreased vision may compromise the older patient’s ability to function, causing concerns about maintaining independence and a decreased self-image. Decreased manual dexterity may make the instillation of prescribed eye drops difficult for some older adults.
 Evaluation
Evaluation
Evaluation of nursing interventions provides an opportunity for the nurse to reassess the signs and symptoms experienced by the patient, determine their ability to remain functional within their home, allow patients to demonstrate any newly acquired skills and review patient expectations using established expected outcomes and standards, such as evidence-based practice standards.
The overall expected outcomes are that the patient with severe vision impairment:
Eye trauma
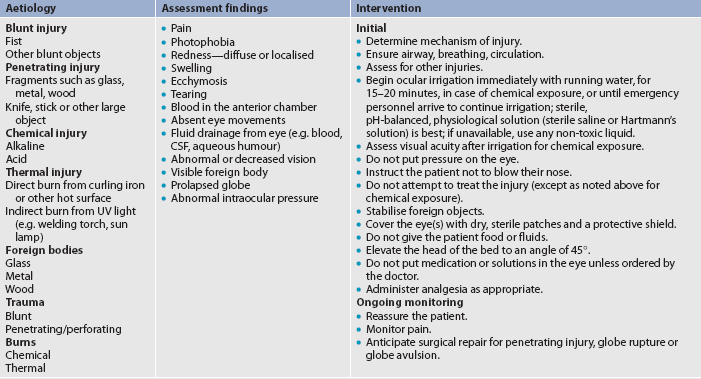
Although the eyes are well protected by the bony orbit and fat pads, everyday activities can result in ocular trauma. Ocular injuries can involve the ocular adnexa, the superficial structures or the deeper ocular structures. In Australia, eye injuries are a major cause of lost working days, with certain work areas being more at risk than others.17 Table 21-3 outlines the emergency management of the patient with an eye injury. Types of ocular trauma include blunt injuries, penetrating injuries and chemical exposure injuries. Causes of ocular injuries include car accidents, falls, sports and leisure activity injuries, assaults and accidents through work-related situations. Trauma is often a preventable cause of vision impairment. Many sports-related eye injuries could be prevented by wearing protective eyewear.18 The nurse’s role in individual and community education is extremely important in reducing the incidence of ocular trauma.
Inflammation and infection
One of the most common conditions encountered by the ophthalmologist is inflammation or infection of the external eye. Many external irritants or microorganisms affect the lids and conjunctiva and can involve the avascular cornea. It is a nursing responsibility to teach the patient appropriate interventions related to the specific disorder.
HORDEOLUM
A hordeolum (commonly called a stye) is an infection of the sebaceous glands in the lid margin. The most common bacterial infective agent is Staphylococcus aureus.19 A red, swollen, circumscribed and acutely tender area develops rapidly. The nurse should instruct the patient to apply warm, moist compresses at least four times a day until it improves. This may be the only treatment necessary. If there is a tendency for recurrence, the patient should perform lid scrubs daily. In addition, appropriate antibiotic ointments or drops may be indicated.
CHALAZION
A chalazion is a swelling arising from a blockage of one or more meibomian ducts. It may affect either the upper or the lower lid. When it becomes infected it is sometimes called an internal hordeolum. It may also occur as a response to the material released into the lid when a blocked gland ruptures. A chalazion appears as a swollen, non-painful, reddened area, usually on the upper lid. It may fluctuate in size during the course of the condition and may reoccur several times. Initial treatment is similar to that for a hordeolum. If warm, moist compresses are ineffective in causing spontaneous drainage, the ophthalmologist may surgically remove the chronic lesion (this is normally a surgical procedure) or may inject the chronic lesion with corticosteroids.
BLEPHARITIS
Blepharitis is a common term used for inflammation of the lids, lashes and meibomian glands and is among the most common of ocular disorders.20 It is usually chronic, with periods of exacerbation and remissions. It can be very difficult to treat. The pathology is complex and may involve abnormal lid-margin secretions and organisms, as well as a dysfunctional precorneal tear film.21 The general clinical features include sore eyelids; itchy, burning or gritty sensations; photophobia; and eyelids sticking together. Conjunctivitis may occur simultaneously.
The most common organisms seen in chronic blepharitis include Staphylococcus epidermidis, Staphylococcus aureus, Propionibacterium canes and Corynebacterium. Alterations in the secretions from the meibomian glands and changes to the orifices of the glands may occur in chronic blepharitis. Over time these changes result in instability and thinning of the tear film. This allows more of the aqueous component of tears to evaporate, ultimately leading to damage to the ocular surface and in dysfunctional tear syndrome. Treatment usually needs to be ongoing and is based on scrupulous eyelid hygiene, topical and systemic antibiotics and, in acute inflammatory periods, topical anti-inflammatory agents such as corticosteroids.21
CONJUNCTIVITIS
Conjunctivitis is an infection or inflammation of the conjunctiva and is one of the most common causes of red eyes. Conjunctival infections may be caused by bacterial or viral microorganisms. Conjunctival inflammation may result from exposure to allergens or chemical irritants (including cigarette smoke). The tarsal conjunctiva (lining the interior surface of the lids) may become inflamed as a result of a chronic foreign body in the eye, such as a contact lens or an ocular prosthesis.
Bacterial infections
Acute bacterial conjunctivitis is a common infection. Although it occurs in every age group, epidemics commonly occur in children because of their poor hygiene habits The most common causative microorganisms are staphylococcal species, Streptococcus pneumoniae and fungi.21 The patient with bacterial conjunctivitis may complain of gritty irritation, tearing, redness and a mucopurulent drainage. Although this typically occurs initially in one eye, it spreads rapidly to the unaffected eye. Visual acuity is usually normal. Careful hand-washing and using individual or disposable towels helps prevent spreading the condition. Although this condition is usually self-limiting and does not cause any serious damage, it is preferable to have it treated to shorten the course of the disease, thereby reducing the spread and likelihood of more widespread extraocular disease.
Viral infections
Conjunctival infections may be caused by many different viruses and are often associated with a viral upper respiratory tract infection. There are several forms of adenoviral infection—follicular conjunctivitis, pharyngoconjunctival fever, epidemic keratoconjunctivitis and, rarely, acute haemorrhagic conjunctivitis. It is extremely contagious, with transmission usually occurring through direct contact with infected persons or contaminated instruments. Particular adenovirus serotypes can cause epidemic keratoconjunctivitis, which is seen most commonly in older children and adults. The patient may complain of foreign body sensation, redness, oedema of the eyelids, itchiness and a watery discharge. Unless other ocular structures become involved, this condition is usually mild and self-limiting. Good hygiene practices decrease the spread of the virus. Treatment is usually palliative. Topical corticosteroids should be avoided because they may increase adenoviral replication. Antiviral drops are ineffective and therefore not indicated. Secondary bacterial infection is rare.22
Chlamydia infections
Adult inclusion conjunctivitis (AIC) is caused by the occulogenital type of Chlamydia trachomatis serotypes D–K. AIC is becoming more prevalent because of the increase in sexually transmitted Chlamydia infections. The patient complains of a mucopurulent ocular discharge, irritation, redness and lid swelling. Systemic symptoms may be present as well. For unknown reasons, AIC does not carry the long-term consequences of trachoma (a sight-threatening keratoconjunctivitis caused by a different type of the C. trachomatis bacterium). AIC also differs from trachoma in that it is common in economically developed countries, whereas trachoma is rarely seen except in developing countries.23
Trachoma is a major health problem in rural and remote Australia, where hot dry conditions exist with crowded living conditions.23 The condition is caused by the C. trachomatis organism, an intracellular bacterium causing keratoconjunctivitis. It is particularly common among Indigenous children. Even though it may appear mild, chronic infection can lead to loss of vision in middle age associated with persistent follicles on the inside of the eyelid, which may lead to scarring of the conjunctiva and the underlying eyelid. For this reason it is most important to detect the disease early and promote good public health practices.23,24 Optimal treatment involves the administration of a single dose of oral azithromycin, an erythromycin-like antibiotic. It is effective when used as a single dose, thereby overcoming the problems of compliance with previous treatment involving prolonged courses of tetracycline ointment or drops.25
Adults with AIC have a high risk of concurrent Chlamydia genital infection, as well as other sexually transmitted infections. Consequently, all patients should be referred for further evaluation and systemic antibiotic therapy. The nurse’s responsibility includes education about the ocular condition, as well as the sexual implications of the condition.
Allergic conjunctivitis
Conjunctivitis caused by exposure to some allergen can be mild and transitory, or it can be severe enough to cause significant swelling, sometimes ballooning the conjunctiva beyond the eyelids. The defining symptom of allergic conjunctivitis is itching. The patient may also complain of burning, redness and tearing. Acutely, the patient may have white or clear exudate. If the condition is chronic, the exudate is thicker and becomes mucopurulent. In addition to pollens, the patient may develop allergic conjunctivitis in response to animal fur, ocular solutions and medications, or even contact lenses. The nurse should instruct the patient to avoid the allergen if it is known. Artificial tears can be effective in diluting the allergen and washing it from the eye. Effective topical medications include antihistamines and corticosteroids.
KERATITIS
Keratitis is an inflammation or infection of the cornea that can be caused by a variety of microorganisms or by other factors. The condition may involve the conjunctiva and/or the cornea. When it involves both, the disorder is termed keratoconjunctivitis.
Bacterial infections
The intact cornea provides an effective defence against infection. However, when the epithelial layer is disrupted, the cornea can become infected by a variety of bacteria. Topical antibiotics are generally effective but eradicating the infection may require subconjunctival antibiotic injection or, in severe cases, intravenous (IV) antibiotics. Risk factors include mechanical or chemical corneal epithelial damage, wearing contact lens, debilitation, nutritional deficiencies, immunosuppressed states and contaminated products (e.g. lens care solutions and cases, topical medications, cosmetics).19
Viral infections
Herpes simplex virus (HSV) keratitis (ocular herpes) is the most frequently occurring infectious cause of corneal blindness in the Western hemisphere.26 It is a significant problem, especially with immunosuppressed patients. It may be caused by HSV-1 or HSV-2 (genital herpes), although HSV-2 ocular infection is much less common. The resulting corneal ulcer has a characteristic dendritic (tree-branching) appearance and it is often, although not always, preceded by infection of the conjunctiva or eyelids. Pain and photophobia are common. Up to 40% of patients with herpetic keratitis heal spontaneously. The spontaneous healing rate increases to 70% if the cornea is debrided to remove infected cells. Collaborative therapy includes aciclovir ointment and corneal debridement, if required. Corticosteroids are contraindicated because they contribute to a longer course, possible deeper ulceration of the cornea and systemic complications.
The varicella zoster virus (VZV) causes both chickenpox and herpes zoster ophthalmicus (HZO). HZO may occur by reactivation of an endogenous infection that has persisted in latent form after an earlier attack of varicella or by direct or indirect contact with a patient with chickenpox or herpes zoster. It occurs most frequently in older adults and immunosuppressed patients. Multidisciplinary care of the patient with acute HZO may include narcotic or non-narcotic analgesics for the pain, antiviral agents such as aciclovir to reduce viral replication, mydriatic agents to dilate the pupil and relieve pain, and topical antibiotics to combat secondary infection. The patient may apply warm compresses and povidone–iodine ointment to the affected skin (ointment should not be applied near the eye).
Epidemic keratoconjunctivitis (EKC) is the most serious ocular adenoviral disease. It is spread by direct contact, including sexual activity. In the medical setting, contaminated hands and instruments can be the source of spread. The patient may complain of tearing, redness, photophobia and foreign body sensation. In most patients, the disease involves only one eye. Treatment is primarily palliative and includes ice packs and dark glasses. In severe cases, therapy can include mild topical corticosteroids to relieve symptoms temporarily and topical antibiotic ointment.22 The nurse’s most important role is to teach the patient and family members good hygiene practices to avoid spreading the disease.
Other causes of keratitis
Keratitis may also be caused by fungi (most commonly by the Aspergillus, Candida and Fusarium species), especially in the case of ocular trauma in an outdoor setting where fungi are prevalent in the soil and moist organic matter. It is slow to develop over a number of weeks with patients complaining of increasing pain and decreased vision. The infection may take a long time to resolve with no guarantee of a good result. Several systemic anti-fungal antibiotics, such as fluconazole, can be used.
Acanthamoeba keratitis is caused by a parasite that is associated with contact lens wear.27 The parasite lives in fresh water and is most commonly seen in individuals wearing contact lenses in water, but it is also found in contaminated care solutions and cases. It was first described in 1974 and its incidence has increased significantly over the last 5 years, corresponding with the increase in contact lens wear. Homemade saline solution is particularly vulnerable to Acanthamoeba contamination. The nurse should instruct the patient who wears contact lenses about good lens care practices. In the past it has been difficult to treat; however, treatment is much more effective now. First-line treatment is with biguanides and debridement of the cornea. If this treatment is unsuccessful, the patient may require a keratoplasty (corneal transplant).
Exposure keratitis occurs when the patient cannot adequately close the eyelids. The patient with exophthalmos (protruding eyeball) from thyroid eye disease or masses posterior to the globe is susceptible to exposure keratitis.
Corneal ulcer
Tissue loss due to infection of the cornea produces a corneal ulcer (infectious keratitis). The infection can be due to bacteria, viruses, fungi or trauma (e.g. foreign body, abrasion or contact lens). Corneal ulcers are often very painful and patients may feel as if there is a foreign body in their eye. Other symptoms can include tearing, purulent or watery discharge, redness and photophobia. Treatment is generally aggressive to avoid permanent loss of vision. Antibiotic, antiviral or antifungal eye drops may be prescribed as frequently as every hour night and day for the first 48 hours. Corneal healing may be delayed by the constant irritation of blinking and exposure to the environment. In these cases a bandage contact lens can be used. These can be left in situ for varying periods and are often successful in aiding the healing process. An untreated corneal ulcer can result in corneal scarring and perforation (hole in the cornea). A corneal transplant may then be indicated.
 NURSING MANAGEMENT: INFLAMMATION AND INFECTION IN THE EYE
NURSING MANAGEMENT: INFLAMMATION AND INFECTION IN THE EYE
 Nursing assessment
Nursing assessment
The nurse should assess ocular changes (e.g. oedema, redness, decreasing visual acuity, feeling as if a foreign body is present or discomfort) and document the findings in the patient’s record. The nurse’s assessment should also consider the psychosocial aspects of the patient’s condition, especially when the patient has visual impairment associated with the condition.
 Nursing diagnoses
Nursing diagnoses
Nursing diagnoses for the patient with inflammation or infection of the external eye include, but are not limited to, the following:
 Planning
Planning
The overall goals are that the patient with inflammation or infection of the external eye will: (1) avoid spreading the infection; (2) maintain an acceptable level of comfort and functioning during the course of the specific ocular problem; (3) maintain or improve visual acuity; (4) comply with the prescribed therapy; and (5) promote appropriate health-seeking behaviours.
 Nursing implementation
Nursing implementation
 Health promotion
Health promotion
Careful asepsis and frequent, thorough hand-washing are essential to prevent spreading organisms from one eye to the other, to other patients, to family members and to the nurse. The nurse should dispose of any contaminated dressings in the identified contaminated waste container. The patient and family need information about avoiding sources of ocular irritation or infection and responding appropriately if an ocular problem occurs. Patients with infective disorders that may have a sexual mode of transmission or an associated sexually transmitted infection need specific information about those disorders. Patients also need information about the appropriate use and care of contact lenses and lens care products. The nurse should encourage the patient to follow the recommended regimens.
 Acute intervention
Acute intervention
The nurse may apply warm or cool compresses if indicated for the patient’s condition. Darkening the room and providing an appropriate analgesic are other comfort measures. If the patient’s visual acuity is decreased, the nurse may need to modify the patient’s environment or activities for safety.
The patient may require eye drops as frequently as every hour. If the patient receives two or more different drops, the nurse should stagger the eye drops to promote maximum absorption. For example, if two different eye drops are ordered hourly, the nurse should administer one drop on the hour and one drop on the half hour unless otherwise prescribed. The patient who needs frequent eye drop administration may experience sleep deprivation.
It is important that nurses know how to safely administer eye drops. The Australian Prescriber website has information on the correct use of eye drops (see Resources on p 506).
 Ambulatory and home care
Ambulatory and home care
The patient’s primary need in the home environment is for information about required care and how to accomplish that care. The nurse should provide the patient and family with information about proper hygiene techniques to prevent contamination and limit the spread of infectious disorders. The patient and family also need information about proper techniques for medication administration. If the patient’s vision is compromised, the nurse can provide suggestions for alternative ways to accomplish necessary daily activities and self-care. The patient who wears contact lenses and develops infections should discard all opened or used lens care products and cosmetics to decrease the risk of reinfection from contaminated products (a common problem and a probable source of infection for many patients).
Dry eye disorders
Complaints of dry eye are caused by a variety of ocular disorders characterised by decreased tear secretion or increased tear film evaporation. Keratoconjunctivitis sicca is caused by lacrimal gland dysfunction from an autoimmune mechanism. If the patient with keratoconjunctivitis sicca has associated dry mouth, the patient may have primary Sjögren’s syndrome (see Ch 64). If the patient has associated rheumatoid arthritis, scleroderma or systemic lupus erythematosus (SLE), the patient may have secondary Sjögren’s syndrome. The patient complains of a sandy or gritty sensation that typically worsens during the day and is better in the morning after eye closure with sleep. Treatment is directed at the underlying cause. With meibomian gland dysfunction, hot compresses and lid margin massage may be used. With decreased tear secretion, the patient may use artificial tears or ointments. These should be used sparingly because preservatives in the drops or overuse can cause further ocular irritation. In severe cases the ophthalmologist may temporarily or permanently surgically occlude the puncta, effectively providing the ocular surface with more available tears.
Strabismus
Strabismus is a condition in which the patient cannot consistently focus both eyes simultaneously on the same object. One eye may deviate in (esotropia), out (exotropia), up (hypertropia) or down (hypotropia). Strabismus in the adult may be caused by thyroid disease, neuromuscular problems of the eye muscles, entrapment of the extraocular muscles in orbital floor fractures, retinal detachment repair or cerebral lesions. In the adult, the primary complaint with strabismus is double vision.
Corneal disorders
CORNEAL SCARS AND OPACITIES
The cornea is an optically transparent tissue that allows light rays to enter the eye and focus on the retina, thus producing a visual image. Any wound causes the cornea to become abnormally hydrated and decreases the normal transparency. A bandage contact lens can be effective in correcting the irregular astigmatism that results from corneal scars. In other situations the treatment for corneal scars or opacities is a keratoplasty. The most commonly used corneal transplant procedure, the penetrating keratoplasty, treats the cornea as a single-layered tissue, while the lamellar keratoplasty specifically targets the diseased layers. This focused surgery spares normal anatomy and can improve clinical outcome. Endothelial lamellar transplantation avoids full-thickness wounds, which are responsible for the slow visual recovery and uncontrolled refractive results that often occur with penetrating keratoplasty. Anterior lamellar transplantation does not replace normal host endothelium, thereby avoiding the risks of endothelial rejection, late endothelial failure and the long-term usage of topical steroids.28
Prior to transplanting the donated corneas, donors are tested for human immunodeficiency virus (HIV) and hepatitis B and C. The tissue is preserved in a special nutritive solution and can be stored for up to a month if used for transplantation. Improved methods of tissue procurement and preservation, refined surgical techniques, postoperative topical corticosteroids and careful follow-up have decreased graft rejection rates.
KERATOCONUS
Keratoconus is a non-inflammatory, usually bilateral disease that is familial but has no exclusive inheritance pattern. It can be associated with Down syndrome, atopic dermatitis, Marfan’s syndrome, aniridia (congenital absence of the iris) and retinitis pigmentosa (hereditary disease characterised by bilateral primary degeneration of the retina beginning in childhood and progressing to blindness by middle age), but most cases of keratoconus are sporadic.
The anterior cornea thins and protrudes forwards, taking on a cone shape. Keratoconus usually appears during adolescence and slowly progresses between 20 and 60 years of age. The only symptom is blurred vision caused by the variable astigmatism associated with the altered corneal shape. The astigmatism may be corrected with glasses or rigid contact lenses. The cornea can perforate as central corneal thinning progresses. Penetrating keratoplasty is indicated when management of refractive error is unsatisfactory and before perforation in advanced cases. Current research in Australia is evaluating the use of riboflavin combined with UVA treatment to confirm the efficacy and safety profile for a new treatment for keratoconus.29
Cataracts
A cataract is an opacity within the crystalline lens. The patient may have a cataract in one eye or both eyes. If cataracts are present in both eyes, one may affect the patient’s vision more than the other. Cataracts are a major factor in preventable blindness and the leading cause of vision problems among people over 5 years of age.30 They are also the largest direct single eye cost condition in Australia. Surgery is the main treatment for cataracts and the patient may still need to wear glasses for distance and/or reading following surgery.
AETIOLOGY AND PATHOPHYSIOLOGY
It is now believed that the development of cataracts is a normal part of the ageing process. By about 70 years of age almost everyone will have some degree of cataract formation. Cataracts can, however, be associated with other factors.31 These include blunt or penetrating trauma, congenital factors such as maternal rubella, radiation or UV light exposure, certain drugs such as systemic corticosteroids or long-term topical corticosteroids and ocular inflammation. People with diabetes mellitus tend to develop cataracts at a younger age than do people without diabetes.
Cataract development is mediated by a number of factors. In degenerative cataract formation, it appears that altered metabolic processes within the lens cause an accumulation of water and alterations in the lens fibre structure. These changes affect lens transparency, causing vision changes.31
CLINICAL MANIFESTATIONS
The patient with cataracts may complain of a decrease in vision, abnormal colour perception and glare. Glare is due to light scatter caused by the lens opacities and may be significantly worse at night when the pupil dilates. The decline of vision is gradual but the rate of cataract development varies from patient to patient. Some patients may complain of a sudden loss of vision because they inadvertently cover their unaffected eye and the decreased acuity of the eye with cataracts becomes suddenly apparent. Secondary glaucoma can also occur if the enlarging lens causes increased intraocular pressure (IOP).
DIAGNOSTIC STUDIES
Diagnosis is based on decreased visual acuity or other complaints of vision changes. The opacity is directly observable by ophthalmoscopic or slit lamp microscopic examination. A totally opaque lens creates the appearance of a white pupil. Box 21-1 outlines other diagnostic studies that may be helpful in evaluating the visual impact of a cataract.
MULTIDISCIPLINARY CARE
Diagnostic studies
History and physical examination
Ophthalmoscopy (direct and indirect)
Glare testing, potential acuity testing in selected patients
Keratometry and A-scan ultrasound (if surgery is planned)
Other tests (e.g. visual field perimetry) may be indicated to differentiate visual loss due to cataract from visual loss due to other causes
COMPLEMENTARY & ALTERNATIVE THERAPIES
Clinical uses
Cataracts, myopia, glaucoma, macular degeneration, night blindness, retinopathy, varicose veins.
MULTIDISCIPLINARY CARE
The presence of a cataract does not necessarily indicate a need for surgery. For many patients the diagnosis is made long before they actually decide to have surgery. Non-surgical therapy may postpone the need for surgery. Multidisciplinary care for cataracts is presented in Box 21-1.
Non-surgical therapy
Currently, there is no available treatment other than surgical removal. If the cataract is not removed, the patient’s vision will continue to deteriorate. However, palliative measures alone may help the patient. Often, changing the patient’s eyewear prescription can improve the level of visual acuity, at least temporarily. Other vision aids include strong reading glasses or magnifiers of some type, which may help the patient with close vision. Increasing the amount of light to read or accomplish other near-vision tasks is another useful measure. Patients may be willing to adjust their lifestyle to accommodate for the decline in their vision. For example, if glare makes it difficult to drive at night, a patient may elect to drive only during daylight hours or to have a family member drive at night. Sometimes informing and reassuring the patient about the disease process makes the patient comfortable about choosing non-surgical measures, at least temporarily.
Surgical therapy
When palliative measures no longer provide an acceptable level of visual function, the patient is an appropriate candidate for surgery. The patient’s occupational needs and lifestyle changes are also factors affecting the decision to have surgery. In some instances, factors other than the patient’s vision needs may influence the need for surgery. Lens-induced problems, such as an increased IOP, may require lens removal. Opacities may prevent the ophthalmologist from obtaining a clear view of the retina in the patient with diabetic retinopathy or other sight-threatening pathology. In those cases the cataract may be removed to allow visualisation of the retina and adequate management of the problem.
Preoperative phase
The patient’s preoperative preparation should include an appropriate history and physical examination. Because almost all patients have local anaesthesia, many doctors and surgical facilities do not require an extensive preoperative physical assessment. However, most cataract patients are older adults who may have several medical problems that should be evaluated and controlled before surgery. Patients may need to discontinue any anticoagulation therapy for a few days preoperatively.
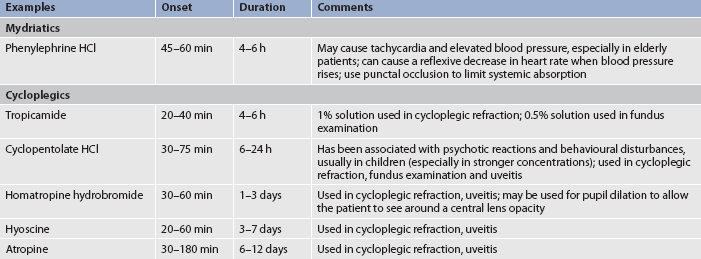
Almost all cataract patients are admitted to a day surgery facility on an outpatient basis. On the day of admission the patient should not have food or fluids for approximately 6–8 hours before surgery. The nurse will instil dilating drops to help maintain pupil dilation. One type of drug used for dilation is a mydriatic (vasoconstrictor), an α-adrenergic agonist (sympathomimetic) that produces pupillary dilation by contraction of the iris dilator muscle. Another type of drug is a cycloplegic, an anticholinergic agent that produces paralysis of ciliary muscles, and hence accommodation (cycloplegia), by blocking the effect of acetylcholine on the ciliary body muscles. Cycloplegics produce pupillary dilation (mydriasis) by blocking the effect of acetylcholine on the iris sphincter muscle. Examples of mydriatics and cycloplegics are listed in Table 21-4. The patient often receives preoperative antianxiety medication before the local anaesthesia injection.
Intraoperative phase
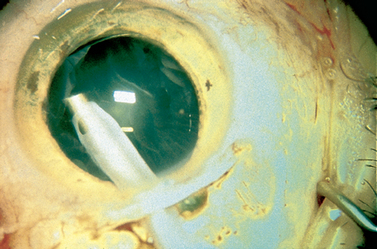
Cataract extraction is an intraocular procedure. Phacoemulsification is the most commonly used technique, in which the nucleus is fragmented by ultrasonic vibration and aspirated from inside the capsular bag (see Fig 21-3).32 An artificial IOL is then inserted into the lens capsule. The incision is usually approximately 3 mm, thereby not requiring sutures. Extracapsular extraction is less commonly performed, but is effective for those patients whose cataract is not suitable for phacoemulsification. A small incision is made, the anterior capsule is opened and the lens nucleus and cortex are removed, leaving the remaining capsular bag intact. The artificial IOL is inserted and fixed into position. The incision is then closed with sutures. Rarely, intracapsular extraction is performed in which the entire lens is removed with the capsule intact (this procedure may be necessary in instances of trauma). Almost all patients now have an IOL implanted at the time of cataract extraction surgery. Because most patients have a phacoemulsification procedure, the lens of choice is a posterior chamber lens that is implanted in the capsular bag behind the iris. At the end of the procedure, the patient receives injections of subconjunctival corticosteroid and antibiotic medications.33 Then an antibiotic and corticosteroid ointment is applied and the patient’s eye is covered with a patch and protective shield. The patch is usually worn overnight and removed during the first postoperative visit.
Postoperative phase
Unless complications occur, the patient is usually ready to go home within a few hours after the surgery as soon as the effects of sedative agents have dissipated. Postoperative medications usually include antibiotic and corticosteroid drops to prevent infection and decrease the postoperative inflammatory response. There is some evidence that postoperative activity restrictions and night-time eye shielding are unnecessary. However, many ophthalmologists still prefer that the patient avoid activities that increase the IOP, such as bending or stooping, coughing or lifting. Ophthalmologists may also recommend using an eye shield over the operative eye at night for protection.
The ophthalmologist will usually see the patient two to three times at increasing intervals throughout the 6–8 weeks following surgery. During each postoperative examination the surgeon will measure the patient’s visual acuity, check anterior chamber depth, assess corneal clarity and measure the IOP. A flat anterior chamber may cause adhesions of the iris and cornea. The cornea may become hazy or cloudy from intraoperative trauma to the endothelium. Even on the first postoperative day the patient’s uncorrected visual acuity in the operative eye may be good. However, it is not unusual or indicative of any problem if the patient’s visual acuity is reduced immediately after surgery. The postoperative eye drops are gradually reduced in frequency and finally discontinued when the eye has healed. The newest innovation is a multifocal IOL that corrects for both near and far vision. Regardless of the type of IOL used, however, patients may still need glasses to achieve their best visual acuity.
 NURSING MANAGEMENT: CATARACTS
NURSING MANAGEMENT: CATARACTS
 Nursing assessment
Nursing assessment
The nurse should assess the patient’s distance and near visual acuity. If the patient is going to have surgery, the nurse should especially note the visual acuity in the patient’s non-operated eye. With this information the nurse can determine how visually compromised the patient may be while the operative eye is patched and healing. In addition, the nurse should assess the psychosocial impact of the patient’s visual disability and the patient’s level of knowledge regarding the disease process and therapeutic options. Postoperatively, it is important to assess the patient’s level of comfort and ability to follow the postoperative regimen.
 Nursing diagnoses
Nursing diagnoses
Nursing diagnoses for the patient with a cataract include, but are not limited to, the following:
 Planning
Planning
Preoperatively, the overall goals are that the patient with a cataract will: (1) make informed decisions regarding therapeutic options; and (2) experience minimal anxiety. Postoperatively, the overall goals are that the patient with a cataract will: (1) understand and participate in postoperative therapy; (2) maintain an acceptable level of physical and emotional comfort; and (3) remain free of infection and other complications.
 Nursing implementation
Nursing implementation
 Health promotion
Health promotion
There are no proven measures to prevent cataract development. However, it is probably wise (and certainly does no harm) to suggest that the patient wear sunglasses, avoid extraneous or unnecessary radiation and maintain an appropriate intake of antioxidant vitamins (e.g. vitamins C and E) and good nutrition. The nurse can also provide information about vision enhancement techniques for the patient who chooses not to have surgery.
 Acute intervention
Acute intervention
Preoperatively, the patient with cataracts needs accurate information about the disease process and the treatment options, especially because cataract surgery is considered an elective procedure. For the patient who wants or needs to see better than is possible with medical interventions only, cataract surgery may not seem elective. However, in most cases there is no harm in not having surgery except that the patient has some degree of vision impairment. The nurse should be available to give the patient and the family information to help them make an informed decision about appropriate treatment.
Can nurses improve adherence to eyedrop therapy?
EVIDENCE-BASED PRACTICE
Clinical question
For patients with glaucoma (P), what interventions (I) increase adherence to eyedrop treatments (O)?
Critical appraisal and synthesis of evidence
• 8 RCTs (n = 690), 5 studies showed that interventions improved adherence
• Interventions were patient education programs, verbal/written information, follow-up support, prescription and medication chart reminders, rescheduling eyedrop therapy, simplification of dosing, eyedrop instillation training and counselling
• Adherence measured by patient interviews, questionnaires, patient diaries or electronic monitoring devices
Implications for nursing practice
• Where possible, simplify eyedrop regimens because they can be challenging to follow.
• Assess patient barriers to eyedrop administration. Provide initial instruction and reinforce correct use.
• Help patients to identify a reminder system for multiple daily eyedrops, such as setting timers or connecting drop administration to other daily routines.
• Teach carers to administer eyedrops for patients with impaired hand coordination.
P, patient population of interest; I, intervention or area of interest; O, outcome(s) of interest
For the patient who elects to have surgery, the nurse is able to provide information, support and reassurance about the surgical and postoperative experience that can reduce or alleviate the patient’s anxiety.
When administering topical medications for pupil dilation before surgery (see Table 21-4 for examples), note that patients with dark irises may need a larger dose. Photophobia is common; therefore, using dark glasses is helpful. These medications produce transient stinging and burning and may be contraindicated in patients with narrow-angle glaucoma, because angle-closure glaucoma may be produced. Mydriatic agents can produce significant cardiovascular effects. When administering mydriatics, punctal occlusion should be used, especially in older and susceptible patients. When using cycloplegic agents for inflammatory disorders such as uveitis or iritis, the desired effect is to place the iris and ciliary body at rest, thus increasing patient comfort.
Box 21-2 outlines patient and carer teaching following eye surgery. The nurse should inform patients that they will not have depth perception until their patch is removed (usually within 24 hours). This necessitates special considerations to avoid possible falls and other injuries. The patient with significant visual impairment in the non-operated eye requires more assistance while the operative eye is patched. Once the patch is removed (usually within 24 hours), most patients with visual impairment in the non-operated eye will have adequate vision for necessary activities because the implanted IOL provides immediate vision rehabilitation in the operated eye. Occasionally, it may take 1–2 weeks for the visual acuity in the operated eye to reach an adequate level for most visual needs. Such patients may need special assistance until their vision improves. The postoperative cataract patient usually experiences little or no pain. There may be some scratchiness in the operative eye. Mild analgesics are usually sufficient to relieve these problems. If the pain is intense or does not ease with analgesia, the patient should notify the surgeon because this may indicate haemorrhage, infection or increased IOP. The nurse should also instruct the patient to notify the surgeon if there is increased or purulent drainage, increased redness or any decrease in visual acuity.
PATIENT & FAMILY TEACHING GUIDE
The following information should be included in the teaching plan for the patient after eye surgery:
1. Proper hygiene and eye care techniques to ensure that medications, dressings and/or surgical wound are not contaminated during necessary eye care.
2. Signs and symptoms of infection and when and how to report these to allow for early recognition and treatment of possible infection.
3. Importance of complying with postoperative restrictions on head positioning, bending, coughing and Valsalva manoeuvre to optimise visual outcomes and prevent increased intraocular pressure.
4. How to instil eye medications using aseptic techniques and adherence with prescribed eye medication routine to prevent infection.
5. How to monitor pain and take medication prescribed for pain, and to report pain not relieved by medication.
6. Importance of continued follow-up as recommended to maximise potential visual outcomes.
Source: Lamb P, Simms-Eaton S. Core curriculum for ophthalmic nursing. 3rd edn. Dubuque, Iowa: Kendall-Hunt; 2004.
Gerontological considerations: cataracts
Most patients with cataracts are elderly. When older patients have impaired vision, even temporarily, they may experience a loss of independence, lack of control over their life and a significant change in self-perception. Societal devaluation of the older individual complicates these experiences. Older patients often need emotional support and encouragement, as well as specific suggestions to allow a maximum level of independent function. The nurse can assure the older patient that cataract surgery can be accomplished safely and comfortably with minimal sedation. The use of outpatient surgery for cataract surgery is particularly beneficial for older patients, who may become confused or disoriented during hospitalisation. Postoperatively, older patients may need to be reminded to ask for assistance when getting out of bed or at night and to sleep on the unaffected side in order to reduce the IOP.
 Ambulatory and home care
Ambulatory and home care
For patients with cataracts who have not had surgery, the nurse can suggest ways in which they may modify their activities or lifestyle to accommodate the visual deficit caused by the cataract. The nurse should also provide patients with accurate information about appropriate long-term eye care.
Patients with cataracts who have day surgery remain in the surgical facility for only a few hours. This shift in practice patterns has dramatically affected how the nurse provides the patient with postoperative care and teaching. The patient and the family are now responsible for almost all postoperative care. It is essential that the nurse give them written and verbal instructions before discharge. These teachings should include information about postoperative eye care, activity restrictions, medications, a follow-up visit schedule, and signs and symptoms of possible complications. The patient’s family should be included in the instruction because some patients may have difficulty with self-care activities, especially if the vision in the non-operated eye is poor. The nurse should provide an opportunity for the patient and family to perform return demonstrations of any necessary self-care activities.
Most patients experience little vision impairment following surgery. IOL implants provide immediate vision rehabilitation and many patients achieve a usable level of visual acuity within a few days following surgery. Also, the patient’s eye remains patched for only 24 hours and many patients have good vision in their non-operated eye.
A few patients may experience significant visual impairment postoperatively. These include patients who do not have an IOL implanted at the time of surgery, those who require several weeks to achieve a usable level of visual acuity following surgery and those with poor vision in their non-operated eye. For these patients the time between surgery and receiving aphakic glasses or contact lenses can be a period of significant visual disability. The nurse can suggest ways in which the patient and family can modify activities and the environment to maintain an adequate level of safe functioning. Suggestions may include getting assistance with steps, removing rugs and other potential obstacles, preparing meals for freezing before surgery or obtaining audio books for diversion until visual acuity improves.
Retinopathy
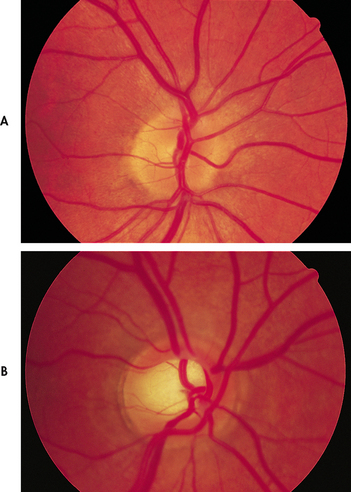
Retinopathy is a process of microvascular damage to the retina. It can develop slowly or rapidly and lead to blurred vision and progressive vision loss. In adults retinopathy is most often associated with diabetes mellitus and hypertension.
Diabetic retinopathy is the leading cause of visual disability and blindness in persons with longstanding diabetes. (Diabetes is discussed in Ch 48.) Non-proliferative retinopathy is the most common form of diabetic retinopathy and is characterised by capillary microaneuryms, retinal swelling and hard exudates. Macular oedema represents a worsening of the retinopathy as plasma leaks from macular blood vessels. This can lead to severe loss in central vision.34 As the disease advances, proliferative retinopathy may occur where new blood vessels grow. However, these blood vessels are abnormal, fragile and predisposed to leak, thus causing severe vision loss. Fluorescein angiography is used to detect diabetic macular oedema, which may be treated with laser photocoagulation.
Hypertensive retinopathy is caused by high blood pressure, creating blockages in retinal blood vessels. (Hypertension is discussed in Ch 32.) These changes may not initially affect a person’s vision. On a routine eye examination, retinal haemorrhages and macular swelling can be noted. Sustained, severe hypertension can cause sudden visual loss from swelling of the optic disc and nerve (papillo-oedema). Treatment, which may be an emergency, focuses on lowering the blood pressure. Signs of retinal damage may persist for weeks to months after the pressure has been reduced.35
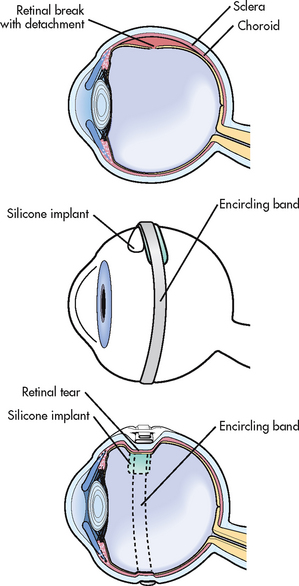
Retinal detachment
A retinal detachment is a separation of the sensory retina and the underlying pigment epithelium, with fluid accumulation between the two layers. The incidence of non-traumatic retinal detachment is approximately 1 in 10,000 people, including 29.1% of people with diabetic retinopathy.36 Retinopathy is reported as being positively associated with a longer reported duration of diabetes but is not significantly related to age, ethnicity, body mass index, glaucoma, myopia, alcohol intake, or tobacco or aspirin use.34 In Victoria in 2000, most people with retinal detachment received laser therapy.36 The number of people with retinal detachment increases when aphakic individuals are included because retinal detachment is more likely to occur in aphakic patients. If traumatic retinal detachments are included, the incidence is only slightly increased. In the patient with no other risk factors who has had a retinal detachment in one eye, the risk of detachment in the second eye is 2–25%. Almost all patients with untreated, symptomatic retinal detachment will lose some vision in the involved eye.
AETIOLOGY AND PATHOPHYSIOLOGY
There are many causes of retinal detachment. The most common cause is a retinal break. Retinal breaks are interruptions in the full thickness of the retinal tissue and they can be classified as tears or holes. Retinal holes are atrophic retinal breaks that occur spontaneously. Retinal tears can occur as the vitreous humour shrinks during ageing and pulls on the retina. The retina tears when the traction force exceeds the strength of the retina. Once there is a break in the retina, liquid vitreous can enter the subretinal space between the sensory layer and the retinal pigment epithelium layer, causing a rhegmatogenous retinal detachment. Less frequently, retinal detachment can occur when abnormal membranes mechanically pull on the retina. These are called tractional detachments. A third type of retinal detachment is the secondary or exudative detachment that occurs with conditions that allow fluid to accumulate in the subretinal space (e.g. choroidal tumours, intraocular inflammation). Risk factors for retinal detachment are listed in Box 21-3.
BOX 21-3 Risk factors for retinal detachment
High myopia
Premature, accelerated rate of vitreous humour detachment; increased incidence of lattice degeneration
Proliferative diabetic retinopathy
Vitreous humour remains attached to areas of neovascularisation as the normal process of vitreal contraction occurs
CLINICAL MANIFESTATIONS
Patients with a detaching retina describe symptoms that include photopsia (light flashes), floaters and a cobweb, hairnet or ring in the field of vision. Once the retina has detached, the patient describes a painless loss of peripheral or central vision, like a curtain coming across the field of vision. The area of visual loss corresponds to the area of detachment. If the detachment is in the superior nasal retina, the visual field loss will be in the inferior temporal area. If the detachment is small or develops slowly in the periphery, the patient may not be aware of a visual problem.
DIAGNOSTIC STUDIES
Visual acuity measurements should be the first diagnostic procedure with any complaint of vision loss (see Box 21-4). The retinal detachment can be directly visualised using direct and indirect ophthalmoscopy or slit lamp microscopy in conjunction with a special lens to view the far periphery of the retina. Ultrasound may be useful to identify a retinal detachment if the retina cannot be directly visualised (e.g. when the cornea, lens or vitreous humour is hazy or opaque).
MULTIDISCIPLINARY CARE
The ophthalmologist will carefully evaluate the patient with retinal breaks to determine whether prophylactic laser photocoagulation or cryopexy is necessary to avoid possible retinal detachment. Some retinal breaks are not likely to progress to detachment and the ophthalmologist will simply watch the patient, giving precise information about the warning signs and symptoms of impending detachment and instructing the patient to seek immediate evaluation if any of those signs or symptoms are recognised. The general ophthalmologist will usually refer the patient with retinal detachments to a retinal specialist. Treatment of retinal detachment has two objectives. The first is to seal any retinal breaks and the second is to relieve inward traction on the retina. Several techniques are used to accomplish these objectives.
Surgical therapy
Laser photocoagulation and cryopexy
These techniques seal retinal breaks by creating an inflammatory reaction that causes a chorioretinal adhesion or scar. Laser photocoagulation involves using an intense, precisely focused light beam, such as the argon laser, to create an inflammatory reaction. The light is directed at the area of the retinal break. This produces a scar that seals the edges of the hole or tear and prevents fluid from collecting in the subretinal space and causing a detachment. The ophthalmologist may use photocoagulation alone if there is a single small tear with no detachment in the periphery and minimal subretinal fluid. For retinal breaks accompanied by significant detachment, the surgeon may use photocoagulation intraoperatively in conjunction with scleral buckling. Tears or holes without accompanying retinal detachment may be treated prophylactically with laser photocoagulation if the ophthalmologist judges them to be at high risk of progressing to retinal detachment.37 When used alone, laser therapy is an outpatient procedure that usually requires only topical anaesthesia, and the patient generally experiences minimal adverse symptoms during or following the procedure.
An alternative method used to seal retinal breaks is cryopexy. This procedure involves using extreme cold to create the inflammatory reaction that produces the sealing scar. The ophthalmologist applies the cryoprobe instrument to the external globe in the area over the tear. This is usually done on an outpatient basis and under local anaesthesia. As with photocoagulation, cryotherapy may be used alone or during scleral buckling surgery. The patient may experience significant discomfort and eye pain following cryopexy. The nurse should encourage the patient to take the prescribed pain medication following the procedure.
Scleral buckling
Scleral buckling is an extraocular surgical procedure that involves indenting the globe so that the pigment epithelium, choroid and sclera move towards the detached retina. This not only helps seal retinal breaks but also helps relieve inward traction on the retina. The surgeon sutures a silicone implant against the sclera, causing the sclera to buckle inwards. The surgeon may place an encircling band over the implant if there are multiple retinal breaks, if the surgeon cannot locate suspected breaks or if there is widespread inward traction on the retina (see Fig 21-4). If present, subretinal fluid may be drained, by inserting a small-gauge needle, to facilitate contact between the retina and the buckled sclera. Scleral buckling is usually accomplished under local anaesthesia and the patient may be discharged on the first postoperative day.
Intraocular procedures
In addition to the extraocular procedures described, retinal surgeons may use one or more intraocular procedures in treating some retinal detachments. Pneumatic retinopexy is the intravitreal injection of a gas to form a temporary bubble in the vitreous humour, which closes retinal breaks and provides apposition of the separated retinal layers. As the intravitreal bubble is temporary, this technique is combined with laser photocoagulation or cryotherapy. The patient with an intravitreal bubble must position the head so that the bubble is in contact with the retinal break. It may be necessary for the patient to maintain this position as much as possible for up to several weeks.
Pars plana vitrectomy (surgical removal of the vitreous) is performed for rhegmatogenous retinal detachment and to relieve traction on the retina, which may occur in proliferative diabetic retinopathy. The surgery may also include removal of subretinal fluid, photocoagulation to seal the retinal breaks and insertion of an internal tamponade, such as gas, oil or, rarely, silicone oil to replace the vitreous.38 An external implant (e.g. scleral buckle) may also be used. In proliferative vitreoretinopathy (PVR), membranes develop in the vitreous cavity and on the retinal surface, exerting traction, which causes folds in the retina. Vitrectomy may be combined with membrane peeling to relieve traction in such cases.
Postoperative considerations in scleral buckling and intraocular procedures
Reattachment is successful in 90% of retinal detachments. Visual prognosis varies, depending on the extent, length and area of detachment. Postoperatively, the patient may be on bed rest and may require special positioning to maintain proper position of an intravitreal bubble. The head must be positioned so that the gas, air or oil is lying against the hole/detachment. If a macular hole has been repaired, it is especially important that the patient is positioned face down for up to a fortnight after surgery. The patient is allowed a brief period hourly to attend to nutritional and comfort needs. If gases have been used it is important that patients are informed that activities such as flying or anaesthetics can adversely affect the gases, causing further expansion and possible occlusion of the central retinal artery. To minimise the risk of an adverse event, a ‘bracelet’ stating the type of gas may be useful to remind the patient of potential complications and to inform other medical staff of the presence of gas. It is removed by the ophthalmologist when there is no evidence of gas in the vitreous cavity.38 Overnight hospitalisation varies according to the surgeon’s preference. The patient may need multiple topical medications, including antibiotics and anti-inflammatory agents. Atropine drops are commonly prescribed to prevent ciliary spasm. The patient should be advised that the prolonged action of these drops may cause photophobia and blurred vision. Activity recommendations also vary according to the surgeon’s preference, the extent of the detachment and the particular repair procedure.
In most cases retinal detachment is an urgent situation and the patient is confronted suddenly with the need for surgery. The patient needs emotional support, especially during the immediate preoperative period, when preparations for surgery produce additional anxiety. When the patient experiences postoperative pain, the nurse should administer prescribed pain medications and teach the patient to take the medication as necessary after being discharged. The patient may go home within a few hours of surgery or may remain in the hospital for several days, depending on the surgeon and the type of repair. Discharge planning and teaching are important, and the nurse should begin this process as early as possible because the patient may not remain hospitalised for long. Patient and family teaching following eye surgery is discussed in Box 21-2.
The level of activity restriction following retinal detachment surgery varies greatly. The nurse should verify the prescribed level of activity with each patient’s surgeon and help the patient plan for any necessary assistance related to activity restrictions. The nurse should teach the patient the signs and symptoms of retinal detachment because of the risk of retinal detachment in the other eye.
Age-related macular degeneration
Age-related macular degeneration (ARMD) is common in Australia.39 Loss of vision from ARMD occurs either as a result of choroidal neovascularisation with leaking vessels and exudate near the macula—the exudative or ‘wet’ form—or by slow atrophy of the retinal pigment epithelium and overlying receptors—non-exudative or ‘dry’ ARMD. Wet ARMD, even though much less common than dry ARMD, may cause rapid central vision loss. People with dry ARMD notice that reading and other close-vision tasks become more difficult. In this form, the macular cells have wasted or atrophied and simply do not function as well as previously. Patients report that ‘sometimes I see the image and sometimes it sort of blinks at me, like I have a short circuit’. For these patients ARMD is slowly progressive and usually can result in a final vision outcome of 6/60. Many patients retain reading and other abilities with low-vision assistive devices, and many can retain a driver’s licence to drive during daylight or at reduced speeds.
AETIOLOGY AND PATHOPHYSIOLOGY
The pathophysiological mechanism is thought to be abnormal accumulation of waste material in the retinal pigment epithelium. People with an ARMD-affected first-degree relative have a 50% lifetime risk of developing ARMD and vision loss, and tend to develop it earlier. Cigarette smokers have a four-fold risk of developing ARMD. Weaker links have been found with obesity, hypertension, macrovascular disease, raised cholesterol level, cumulative light exposure and cataract surgery.39
CLINICAL MANIFESTATIONS
The hallmark sign of ARMD is the appearance of drusen in the fundus, which are found on ophthalmoscopic evaluation. Drusen appear as yellowish exudates beneath the retinal pigment epithelium and represent localised or diffuse deposits of extracellular debris. The patient may complain of blurred vision, the presence of scotomas (blind spots in the central visual field) or metamorphopsia (distortion of vision).40
DIAGNOSTIC STUDIES
In addition to visual acuity measurement, the primary diagnostic procedure is ophthalmoscopy. The examiner looks for drusen and other fundus changes associated with ARMD. The Amsler grid test (see Table 20-5) may help define the involved area and provides a baseline for future comparison. Fundus photography and IV angiography with fluorescein and/or indocyanine green dyes may be helpful in further defining the extent and type of degenerative disease.
MULTIDISCIPLINARY CARE
Laser photocoagulation of the abnormal blood vessels when visual acuity is already compromised extensively has been the therapy of choice until recently. The laser seals leaking blood vessels in the retina and reduces the growth of new blood vessels. Vision often does not improve after treatment and may even deteriorate; however, the Macular Photocoagulation Study Group showed that treated patients lose less vision than untreated patients.40 At present this type of therapy is recommended for the treatment of well-demarcated lesions outside the fovea and those lesions that are sufficiently removed from the fovea so that treatment does not extend to the centre of the fovea, as the laser destroys the retinal pigment epithelium and photoreceptor cells where it is applied, leaving a blind spot at the scarred area.40
One of the first treatments for wet ARMD was photodynamic therapy (PDT), which used verteporfin intravenously and a non-thermal laser to activate the photosensitive drug molecules.40 Verteporfin is a photosensitising drug that becomes active when exposed to the low-level laser light wave. Until the drug is completely excreted by the body, it can be activated by exposure to sunlight or other high-intensity light, such as halogen. Therefore, patients are cautioned to avoid direct exposure to sunlight and other intense forms of light for 5 days after treatment. Patients leave the clinic completely covered because any exposure to skin by sunlight could activate the drug in that area, resulting in a thermal burn. This treatment now tends to be reserved for patients who are unable to have antivascular endothelial factor (anti-VEGF) therapy or who have had a poor result from it.
The loss of normal retinal pigment epithelium function can lead to local tissue hypoxia, which may result in oversecretion of several chemical factors. One of these factors is endothelial growth factor. This chemical, along with others, may cause new vessel growth (neovascularisation), the classic sign of wet ARMD. The anti-VEGF medication given to treat this is administered intravitreally every 4–6 weeks for 3 doses. The VEGF Inhibition Study in Ocular Neovasculisation (VISION) found that the earliest of these drugs, pegaptanib sodium, was at least as effective as PDT in slowing the progression of moderate to severe vision loss.41 The benefit of this medication over PDT is that it was also shown to be effective in patients with lesions previously untreatable with PDT. At present two other anti-VEGF drugs, bevacizumab and ranibizumab, are being used and early results show that they are effective in improving patients’ visual acuity.42
The role of high-dose vitamin therapy, especially vitamins C and E and beta-carotene, in slowing the progression of vision loss has been investigated in several studies, but there appears to be no definitive evidence as to whether the introduction of these dietary elements is justifiable in terms of preventing illness.39
The permanent loss of central vision associated with ARMD has significant psychosocial implications for nursing care. Nursing management of the patient with uncorrectable visual impairment is discussed on pages 472–474 and is appropriate for the patient with ARMD. It is especially important when caring for patients with ARMD to avoid giving the impression that nothing can be done about the problem. Although it is true that therapy will not recover lost vision, much can be done to augment the remaining vision. Just knowing that the healthcare provider has not abandoned them can give these patients a more positive outlook.
Glaucoma
Glaucoma is not one disease but rather a group of disorders with a diverse range of clinical and pathological features. The features common to all glaucomas are optic neuropathy, visual field abnormalities and progressive, irreversible blindness if untreated. Until recently it was thought that IOP was always increased in glaucoma. While this is not the case, it is thought that 60–70% of patients do have an IOP above average (more than 21 mmHg).43
Glaucoma may occur congenitally, as a primary disease, or secondary to other ocular or systemic conditions. IOP is regulated by the formation and reabsorption of aqueous humour. The presence of glaucoma is directly related to the balance or imbalance of this fluid. If elevated IOP is not recognised and treated, glaucomatous damage to the optic nerve and retinal cells results in atrophy and permanent vision loss. In Australia, New Zealand and the US, glaucoma is the second leading cause of permanent blindness. In the US, at least 2 million people have glaucoma and, of these, more than 50% are unaware of their condition. Another 5–10 million people have elevated IOP, placing them at an increased risk of developing the disease. The incidence of glaucoma increases with age. One in 50 Caucasians is affected. Blindness from glaucoma is largely preventable with early detection and appropriate treatment. Those at risk include people over the age of 40 with a family history of glaucoma who are extremely short-sighted, the aged, people of African origin, long-term steroid users and those with medical problems (e.g. hypertension, diabetes).43
AETIOLOGY AND PATHOPHYSIOLOGY
The aetiology of glaucoma is related in most types of glaucoma to the consequences of an elevated IOP. A proper balance between the rate of aqueous production (referred to as inflow) and the rate of aqueous reabsorption (referred to as outflow) is essential to maintain IOP within normal limits. IOP between 10 and 21 mmHg is considered normal. When the rate of inflow is greater than the rate of outflow, IOP can rise above the normal limits. If IOP remains elevated, permanent visual damage may occur. However, a raised IOP is not the only cause of damage to the optic nerve, given that 30–40% of patients with primary open-angle glaucoma have normal pressures. It is thought that the damage may be caused by ischaemia to the optic nerve.44
Primary open-angle glaucoma represents 90% of the cases of primary glaucoma. In primary open-angle glaucoma, the outflow of aqueous humour through the trabecular meshwork is impaired due to changes within this sieve-like structure.45 Primary angle-closure glaucoma represents the other 10% of cases of primary glaucoma. As the name implies, the mechanism reducing the outflow of aqueous humour is angle closure. Usually, this is caused by the lens bulging forwards as a result of an age-related process. Angle closure may also occur as a result of pupil dilation in the patient with anatomically narrow angles. Dilation causes peripheral iris bulging with the same outcome of covering the trabecular meshwork and blocking the outflow channels. An acute attack may be precipitated by situations during which the pupil remains in a partially dilated state long enough to cause an acute and significant rise in IOP. This may occur because of drug-induced mydriasis, emotional excitement or darkness. Drug-induced mydriasis may occur not only from topical ophthalmic preparations but also from many systemic medications (both prescription drugs and over-the-counter drugs). The nurse should check drug documentation before administering medications to the patient with angle-closure glaucoma and should instruct the patient not to take any mydriatic-producing medications.
In secondary glaucoma, increased IOP results from other ocular or systemic conditions that may block the outflow channels in some way. Secondary glaucoma may be associated with various inflammatory processes that block the outflow channels. Inflammatory processes may also damage the trabecular meshwork. Trauma, intraocular or periorbital neoplasms, iris neovascularisation (new blood vessel growth) and other ocular or systemic disorders may also be associated with secondary glaucoma.
CLINICAL MANIFESTATIONS
Primary open-angle glaucoma develops slowly and without symptoms. The patient reports no symptoms of pain or pressure and usually does not notice the gradual visual field loss until peripheral vision has been severely compromised. Eventually the patient with untreated glaucoma has ‘tunnel vision’ in which only a small centre field can be seen and all peripheral vision is absent.
Acute angle-closure glaucoma causes definite symptoms, including sudden, excruciating pain in or around the eye. This is often accompanied by nausea and vomiting. Visual symptoms include seeing coloured haloes around lights, blurred vision and ocular redness. The acute rise in IOP may also cause corneal oedema, giving the cornea a frosted appearance.
Manifestations of subacute or chronic angle-closure glaucoma appear more gradually. The patient who has had a previous, unrecognised episode of subacute angle-closure glaucoma may report a history of blurred vision, seeing coloured haloes around lights, ocular redness or eye or brow pain.
DIAGNOSTIC STUDIES
IOP is usually elevated in glaucoma. Normal IOP by applanation tonometry is 10–21 mmHg. In the patient with elevated pressure, the ophthalmologist will usually repeat the measurements over a period of time to verify the elevation. Although in some patients with open-angle glaucoma IOP may not be raised, for most patients it will be between 22 and 32 mmHg. In acute angle-closure glaucoma, IOP may be 50 mmHg or higher.
In open-angle glaucoma, slit lamp microscopy reveals a normal angle. In angle-closure glaucoma, the examiner may note a markedly narrow or flat anterior chamber angle, an oedematous cornea, a fixed and moderately dilated pupil, and ciliary injection. Gonioscopy allows better visualisation of the anterior chamber angle.
Measures of peripheral and central vision provide other diagnostic information. Whereas central acuity may remain 6/6 even in the presence of severe peripheral visual field loss, visual field perimetry may reveal subtle changes in the peripheral retina early in the disease process, long before actual scotomas develop. When visual field defects begin to appear, the initial scotoma is a small, football-shaped defect that gradually progresses to a nasal and superior field defect in chronic open-angle glaucoma. In acute angle-closure glaucoma, central visual acuity will be reduced if the patient has corneal oedema, and the visual fields may be markedly decreased.
As glaucoma progresses, optic disc cupping occurs. This is visible with direct or indirect ophthalmoscopy (see Fig 21-5). The optic disc becomes wider, deeper and paler (light grey or white). Optic disc cupping may be one of the first signs of chronic open-angle glaucoma. Optic disc photographs are useful for comparison over time to demonstrate an increase in the cup-to-disc ratio and progressive blanching.
MULTIDISCIPLINARY CARE
The primary focus of glaucoma therapy is to keep IOP low enough to prevent the patient from developing optic nerve damage. This damage is manifested by increasing visual field loss and progressive optic disc cupping. Specific therapies vary with the type of glaucoma. The diagnostic and multidisciplinary care of glaucoma is summarised in Box 21-5.
MULTIDISCIPLINARY CARE
Chronic open-angle glaucoma
Initial treatment in chronic open-angle glaucoma is with drugs (see Table 21-5). With all drug therapy, the patient must understand that continued treatment and supervision are necessary because the drugs control, but do not cure, the disease.
TABLE 21-5 Acute and chronic glaucoma
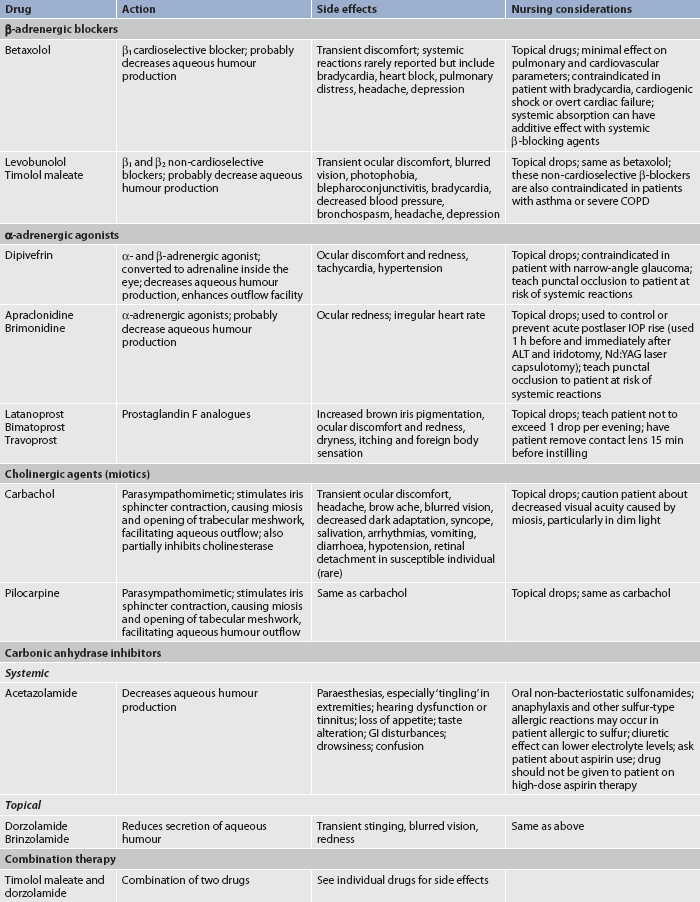
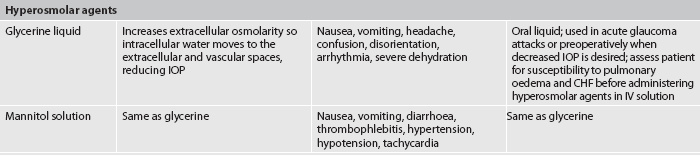
ALT, argon laser trabeculoplasty; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; GI, gastrointestinal; IOP, intraocular pressure; IV, intravenous.
Argon laser trabeculoplasty (ALT) is a therapeutic option to lower IOP when medications are not successful or when the patient either cannot or will not use the drug therapy as recommended. ALT is an outpatient procedure that requires only topical anaesthetic. The topical drops anaesthetise the cornea before the gonioscopy lens is applied, allowing visualisation of the treatment area. Approximately 50 laser spots are evenly spaced around the superior or inferior 180° of the trabecular meshwork. The laser stimulates scarring and contraction of the trabecular meshwork, opening the outflow channels. ALT reduces IOP in approximately 75% of cases. A second 180° area may be treated in a subsequent procedure. The patient uses topical corticosteroids for approximately 3–5 days following surgery. The most common complication is an acute postoperative IOP rise. Because the decrease in pressure is gradual, the patient continues taking the preoperative glaucoma medication. The ophthalmologist examines the patient 1 week after the procedure and again 4–6 weeks following surgery.
A filtering procedure, such as trabeculectomy, may be indicated if medical management and laser therapy are not successful. In this procedure the surgeon makes conjunctival and scleral flaps, removes part of the iris and trabecular meshwork, and closes the scleral flap loosely. Aqueous humour may now percolate out through the area of missing iris where it is trapped under the repaired conjunctiva and absorbed into the systemic circulation. The success rate of this filtering surgery is 75–85%. The subconjunctival application of mitomycin or 5-fluorouracil may increase the success rate by preventing scarring and subsequent closure of the opening created during surgery.
Cyclocryotherapy is another procedure that reduces IOP. The cryoprobe is touched to the sclera outside the ciliary body. This freezes parts of the ciliary body, causing local destruction of the ciliary tissue and decreasing the production of aqueous humour. The procedure may be repeated and can also be used in treating acute glaucoma.
An implant is another surgical option, usually reserved for the patient in whom filtration surgery has failed. It involves surgical placement of a small tube and reservoir to shunt aqueous humour from the anterior chamber to the implanted reservoir.
Acute angle-closure glaucoma
Acute angle-closure glaucoma is an ocular emergency that requires immediate intervention. Miotics and oral or IV hyperosmotic agents are usually successful in immediately lowering IOP (see Table 21-5). A laser peripheral iridotomy or surgical iridectomy is necessary for long-term treatment and prevention of subsequent episodes. These procedures allow the aqueous humour to flow through a newly created opening in the iris and into normal outflow channels. One of these procedures may also be performed on the other eye as a precaution because many patients often experience an acute attack in the other eye.
 NURSING MANAGEMENT: GLAUCOMA
NURSING MANAGEMENT: GLAUCOMA
 Nursing assessment
Nursing assessment
Glaucoma is a chronic condition requiring long-term management. The nurse must carefully assess the patient’s ability to understand and comply with the rationale and regimen of the prescribed therapy. In addition, the nurse should assess the patient’s psychological reaction to the diagnosis of a potentially sight-threatening chronic disorder. The patient’s family must be included in the assessment process because the chronic nature of this disorder affects the family in many ways. Some families may become the primary providers of necessary care, such as eyedrop administration or insulin injections, if the patient is unwilling or unable to accomplish these self-care activities. The nurse also assesses visual acuity, visual fields, IOP and fundus changes when appropriate.
 Nursing diagnoses
Nursing diagnoses
Nursing diagnoses for the patient with glaucoma include, but are not limited to, the following:
 Planning
Planning
The overall goals are that the patient with glaucoma will: (1) have no progression of visual impairment; (2) understand the disease process and rationale for therapy; (3) participate in all aspects of therapy (including medication administration and follow-up care); and (4) have no postoperative complications.
 Nursing implementation
Nursing implementation
 Health promotion
Health promotion
The nurse has an important role in teaching the patient and family about the risk of glaucoma. In addition, the nurse should stress the importance of early detection and treatment in preventing vision impairment. This knowledge should encourage the patient to seek appropriate ophthalmic healthcare. The patient should know that the incidence of glaucoma increases with age and that a comprehensive ophthalmic examination is invaluable in identifying persons with glaucoma or those at risk of developing glaucoma. The current recommendation is for an ophthalmic examination every 2–4 years for persons aged 40–64 years and every 1–2 years for persons aged 65 years and older. Indigenous Australians in every age category should have examinations more often because of the increased incidence and more aggressive course of glaucoma in these individuals.
 Acute intervention
Acute intervention
Acute nursing interventions are directed primarily towards the patient with acute angle-closure glaucoma and the surgical patient. The patient with acute angle-closure glaucoma requires immediate medication to lower IOP, which the nurse must administer in a timely and appropriate manner. The patient may also be ordered analgesia and/or an antiemetic. The patient may be uncomfortable and appropriate nursing comfort interventions include darkening the environment, applying cool compresses to the patient’s forehead and providing a quiet and private space for the patient. Most surgical procedures for glaucoma are outpatient procedures. The patient will need postoperative instructions and may require nursing comfort measures to relieve discomfort related to the procedure. Patient and family teaching following eye surgery is discussed in Box 21-2.
 Ambulatory and home care
Ambulatory and home care
Because of the chronic nature of glaucoma, the patient needs encouragement to follow the therapeutic regimen and follow-up recommendations prescribed by the ophthalmologist. The patient needs accurate information about the disease process and treatment options, including the rationale underlying each option. The patient also needs information about the purpose, frequency and technique for administration of prescribed anti-glaucoma agents. In addition to verbal instructions, all patients should receive written instructions that contain the same information. This should be sufficiently detailed to provide all the necessary information without being so extensive that the patient becomes overwhelmed. The patient may be encouraged to comply with the medication regimen if the nurse promotes consideration of the sight-saving nature of the drops. The nurse can further encourage compliance by helping the patient to identify the most convenient and appropriate times for medication administration or by advocating a change in therapy if the patient reports unacceptable side effects.
Gerontological considerations: glaucoma
Many older patients with glaucoma have systemic illnesses or take systemic medications that may affect their therapy. In particular, patients using a β-adrenergic blocking glaucoma agent may experience an additive effect if a systemic β-adrenergic blocking drug is also being taken. All β-adrenergic blocking glaucoma agents are contraindicated in patients with bradycardia, greater than first-degree heart block, cardiogenic shock and overt cardiac failure. The non-cardioselective β-adrenergic blocking glaucoma agents are also contraindicated in patients with severe chronic obstructive pulmonary disease (COPD) or asthma. The hyperosmolar agents may precipitate congestive heart failure (CHF) or pulmonary oedema in susceptible patients. Older patients on high-dose aspirin therapy for rheumatoid arthritis should not take carbonic anhydrase inhibitors. The β-adrenergic agonists can cause tachycardia or hypertension, which may have serious consequences in older patients. The nurse should teach the older patient to occlude the puncta to limit the systemic absorption of glaucoma medications.
Intraocular inflammation and infection
The term uveitis is used to describe inflammation of the uveal tract, retina, vitreous humour or optic nerve. It is classified according to which tissue is inflamed. This inflammation may be caused by bacteria, viruses, fungi or parasites. Cytomegalovirus retinitis (CMV retinitis) is an opportunistic infection that occurs in patients with acquired immunodeficiency syndrome (AIDS) and in other immunosuppressed patients. The aetiology of sterile intraocular inflammation includes autoimmune disorders, AIDS, malignancies or conditions associated with systemic diseases such as juvenile rheumatoid arthritis and inflammatory bowel disease. Pain and photophobia are common symptoms.
Endophthalmitis is an extensive intraocular inflammation of the posterior cavity, which contains vitreous humour. Bacteria, viruses, fungi or parasites can all induce this serious inflammatory response. The mechanism of infection may be endogenous, in which the infecting agent arrives at the eye through the bloodstream, or exogenous, in which the infecting agent is introduced through a surgical wound or a penetrating injury. Manifestations include ocular pain, photophobia, decreased visual acuity, headaches, upper lid oedema, reddened and swollen conjunctiva, and corneal oedema. Until recently the condition was devastating, with the majority of cases leading to significantly decreased vision, sometimes blindness, and to prevent it spreading through the entire eye, enucleation was performed. With aggressive treatment the prognosis has improved significantly. The current treatment involves administration of intravitreous antibiotics within an hour of presentation, with follow-up injections daily until improvement shows. If the infection is very severe on presentation, total removal of the vitreous humour and installation of antibiotics is required.
When all the layers of the eye (vitreous, retina, choroid and sclera) are involved in the inflammatory response, the patient has panophthalmitis. In the final stages of extensive cases, the scleral coat may undergo bacterial or inflammatory dissolution. Subsequent rupture of the globe spreads the infection into the orbit or eyelids.
Treatment of intraocular inflammation depends on the underlying cause. Intraocular infections require antimicrobial agents, which may be delivered topically, subconjunctivally, intravitreally, systemically or in some combination. Sterile inflammatory responses require anti-inflammatory agents such as corticosteroids. The site and severity of the sterile inflammatory response determine whether topical, subconjunctival or systemic corticosteroids are necessary. The patient with intraocular inflammation is usually uncomfortable and may be noticeably anxious and frightened. The patient may fear sudden and total loss of vision. In some cases this fear is realistic and the nurse should provide accurate information and emotional support to the patient and family. In severe cases enucleation may be necessary. When the patient has lost visual function or even the entire eye, the patient will grieve the loss. The nurse’s role includes helping the patient through the grieving process.
Enucleation
Enucleation is the removal of the eye. The primary indication for enucleation is a blind, painful eye. This may result from absolute glaucoma, infection or trauma. Enucleation may also be indicated in ocular malignancies, although many malignancies can be managed with cryotherapy, radiation and chemotherapy. An extremely rare indication is sympathetic ophthalmia, in which the untraumatised eye develops an inflammatory response following the primary eye trauma. In this situation the traumatised eye is enucleated. The surgical procedure includes severing the extraocular muscles close to their insertion on the globe, inserting an implant to maintain the intraorbital anatomy and suturing the ends of the extraocular muscles over the implant. The conjunctiva covers the joined muscles, and a clear conformer is placed over the conjunctiva until the permanent prosthesis is fitted. A pressure dressing helps prevent postoperative bleeding.
Postoperatively, the nurse observes the patient for signs of complications, including excessive bleeding or swelling, increased pain, displacement of the implant or temperature elevation. Patient teaching should include the instillation of topical ointments or drops and wound cleansing. The nurse should also instruct the patient in the method of inserting the conformer into the socket in case it falls out. The patient is often devastated by the loss of an eye, even when enucleation occurs following a lengthy period of painful blindness. The nurse should recognise and validate the patient’s emotional response and provide support to the patient and family.
Approximately 6 weeks following surgery the wound is sufficiently healed for the permanent prosthesis. The prosthesis is fitted by an ocularist and designed to match the remaining eye. The patient should learn how to remove, cleanse and insert the prosthesis. Special polishing is required periodically to remove dried protein secretions.
Ocular manifestations of systemic diseases
Many systemic diseases have significant ocular manifestations. Although it is not the purpose of this discussion to provide a full description of these disorders, it is important for the nurse to recognise that many systemic diseases have ocular symptoms. Conversely, ocular signs and symptoms may be the first finding or complaint in the patient with a systemic disease. One example is the patient with undiagnosed diabetes who seeks ophthalmic care for blurred vision. A careful history and examination of the patient can reveal that the underlying cause of the blurred vision is lens swelling caused by hyperglycaemia. Another example is the patient who seeks care for a conjunctival lesion. The ophthalmologist may be the first healthcare professional to make the diagnosis of AIDS, based on the presence of a conjunctival Kaposi’s sarcoma. Table 21-6 lists some systemic diseases and disorders and the associated ophthalmic manifestations.
TABLE 21-6 Ocular manifestations of systemic diseases or disorders
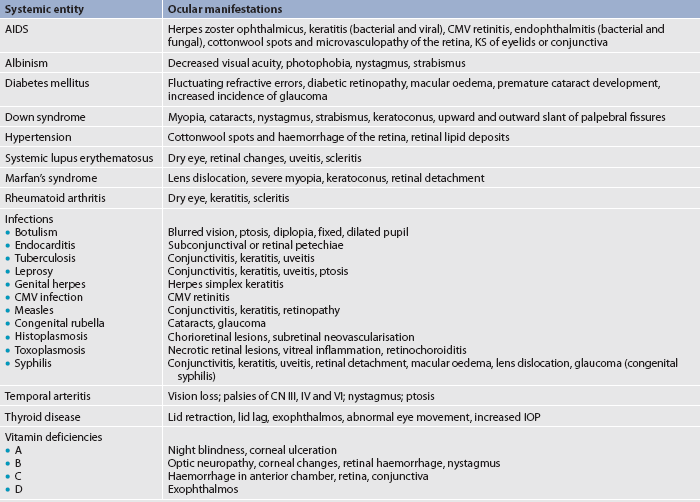
AIDS, acquired immunodeficiency syndrome; CMV, cytomegalovirus; CN, cranial nerve; KS, kaposi’s sarcoma; IOP, intraocular pressure.
AUDITORY PROBLEMS
Problems with the auditory system may include problems with the peripheral auditory system, as well as problems with hearing and the vestibular system. Conditions such as external otitis, otitis media and otosclerosis, as well as the effects of ageing, can all lead to hearing loss. The vestibular system is closely related to the auditory system and symptoms such as vertigo and dizziness may be difficult to distinguish from symptoms related to hearing loss and tinnitus.
Trauma
Trauma to the external ear can cause injury to the subcutaneous tissue, which may result in inflammation of the membrane (perichondritis) and the formation of a subperichondrial haematoma (see Fig 21-6). If the haematoma is not aspirated promptly, the ear may become deformed, resulting in a cauliflower ear. Antibiotics are given to prevent infection. Blows to the ear can also cause a conductive hearing loss if there is damage to the ossicles in the middle ear or if a perforation of the tympanic membrane results. It is important to obtain a careful history of the accident and to assess the hearing of a patient who has had a blow to the ear or to the side of the head.
External otitis
The skin of the external ear and canal is subject to the same problems as skin anywhere on the body. External otitis involves inflammation or infection of the epithelium of the auricle and ear canal. Frequent swimming may alter the flora of the external canal, resulting in an infection often referred to as swimmer’s ear. Trauma caused by picking the ear or, most commonly, the use of sharp objects, such as hairpins, frequently causes the initial break in the skin. Piercing of cartilage in the upper part of the auricle is at higher risk of infection than ear lobe piercing.46
AETIOLOGY
Infections or dermatitis, or both, may cause external otitis (see Fig 21-7). Bacteria or fungi may be the cause. The bacteria most commonly cultured are Pseudomonas aeruginosa followed by Klebsiella, Proteus, Escherichia coli and S. aureus. The most common fungi are Candida albicans and Aspergillus organisms.47 Fungi are often the causative agents of external otitis, especially in warm, moist climates. The warm, dark environment of the ear canal provides a good medium for the growth of microorganisms.
CLINICAL MANIFESTATIONS AND COMPLICATIONS
Pain (otalgia) is one of the first signs of external otitis. Even in mild cases, the patient may experience pain that is disproportionate to the infection. Pain is caused by the swelling of the bony ear canal as a result of the inflammatory process. Pain is especially noted on movement of the auricle or on application of pressure to the tragus (directly in front of the ear). Drainage from the ear may be serosanguineous or purulent. If it is the result of an infection caused by Pseudomonas, the drainage will be green and have a musty smell. Temperature elevations occur when there is extensive involvement of the tissue. The swelling of the ear canal can block hearing and cause dizziness.
 NURSING MANAGEMENT: EXTERNAL OTITIS
NURSING MANAGEMENT: EXTERNAL OTITIS
Diagnosis of external otitis is made by observation with the otoscope light using the largest speculum that the ear will accommodate without causing the patient unnecessary discomfort. The eardrum may be normal if it can be seen. Culture and sensitivity studies of the drainage may be done. It can be a very painful condition, so analgesics may be required to control the pain. After the ear canal is cleansed, a cotton wick impregnated with antibiotic and anti-inflammatory medication is placed in the canal. This will help reduce inflammation and the infection. Cotton wicks should be used with caution in young patients and confused or psychotic patients, who may push them further into the ear. Topical antibiotics include polymyxin B, neomycin and chloramphenicol. Nystatin is used for fungal infections. If the surrounding tissue is involved, systemic antibiotics are prescribed. Warm, moist compresses or heat may be applied. Improvement should occur in 48 hours, but 7–14 days are required for complete resolution.
Careful handling and disposal of material saturated with drainage are important. Otic drops (ear drops) should be administered at room temperature because cold drops can cause dizziness in the patient due to stimulation of the semicircular canals. The tip of the dropper should not touch the ear during administration to prevent contamination of the entire bottle of drops. The ear is positioned so that the drops can run down the canal. This position should be maintained for 2 minutes after ear drop administration to allow dispersion of drops. Multidisciplinary care of external otitis is shown in Box 21-6.
Cerumen and foreign bodies in the external ear canal
Impacted cerumen can cause discomfort and decreased hearing, which is often described as a hollow sensation. In the older person, the cerumen becomes dense and drier. Hair becomes thicker and coarser, entrapping the hard dry cerumen in the canal. Water that enters the canal during a shower or swimming may cause swelling of the cerumen, resulting in complete blockage of the canal. Symptoms of cerumen impaction are outlined in Box 21-7. Management involves irrigation of the canal with body temperature solutions. Special syringes can be used and vary from the simple bulb syringe to special irrigating equipment used in the healthcare provider’s surgery or clinic. The patient is placed in a sitting position with an emesis basin under the ear. The auricle is pulled up and back, and the flow of solution is directed to the top of the canal. It is important that the ear canal not be completely occluded with the syringe tip. Mild lubricant drops containing docusate sodium or arachis oil may be used (sometimes overnight) to soften the cerumen and irrigation may then be effective in removing the impacted cerumen. In Australia, ear syringing is increasingly being replaced by aural irrigation, where the doctor uses microsuction and microscopic instruments.
The list of objects that have been removed from patients’ ears is extensive and includes animate, inanimate (see Fig 21-8), vegetable and mineral objects. Attempts to remove an object occasionally result in pushing it further into the canal. An otolaryngologist should remove the object. Vegetable matter tends to swell and may create a secondary inflammation, making removal more difficult. Animate objects must be immobilised before removal. Mineral oil or lignocaine can be used to drown an insect, and it can then be removed with microscope guidance. Removal of impacted objects should be performed by the healthcare provider. The use of general anaesthesia or conscious sedation may be necessary depending on the level of patient cooperation.
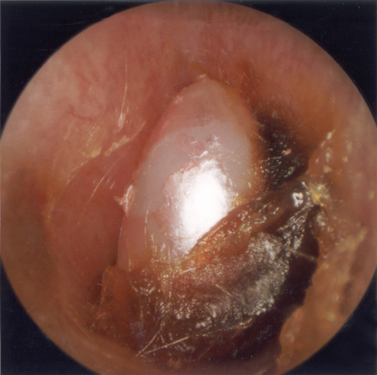
Figure 21-8 A bead in the external ear canal.
Source: Royal Victorian Eye & Ear Hospital, Medical Photography Department.
Patients should be instructed to keep objects out of their ears. Ears should be cleaned only with a washcloth and finger. Hairpins and cotton buds should especially be avoided. Penetration of the middle ear by a cotton bud can cause serious injury to the tympanic membrane and ossicles and may lead to facial paralysis as a result of nerve damage. The use of cotton buds can also impact cerumen against the tympanic membrane and impair hearing.
Malignancy of the external ear
Malignancies of the external ear (other than skin cancers) and canal are uncommon. The predominant signs include a chronic ulcer of the auricle and persistent drainage from the canal, much like that seen with external otitis. This drainage may be tinged with blood and does not diminish with treatment. Multidisciplinary care includes biopsy and other diagnostic studies, such as a computed tomography (CT) scan to determine invasion of the underlying tissue and bone. Treatment usually involves surgery. If the malignancy involves the ear canal and temporal bone, radical surgery of the middle and inner ear with resection of the facial nerve (cranial nerve [CN] VII), auditory nerve (CN VIII) and part of the temporal bone may be necessary.
As a result of long-term sun exposure, the ears are at increased risk of the development of cancer. The most common malignant neoplasms of the auricle are basal cell and squamous cell carcinomas. These skin cancers can be excised surgically or they may be serially excised using a special technique to examine the tissue microscopically to ensure that all residual cancer cells are resected. This procedure is known as Mohs’ micrographic technique (see Ch 23). These skin cancers are usually not life-threatening and the cure rate after resection is greater than 90% in most cases. Melanoma occurs rarely on the external ear. Cancer of the ear often results in cosmetic deformities that are difficult to reconstruct.
Acute otitis media
The most common problem of the middle ear is acute otitis media (see Fig 21-9), which is usually a childhood disease because in childhood the auditory tube that normally drains fluid and mucus from the middle ear is shorter and narrower and its position is flatter than in adulthood.48 In many Indigenous communities in Australia there are high rates of otitis media. Although most patients have mixed infections, bacteria are the predominant aetiological agents. Pain, fever, malaise, headaches and reduced hearing are signs and symptoms of acute otitis media.
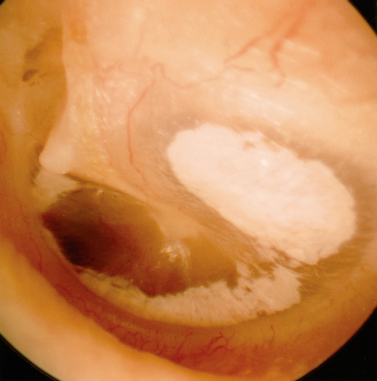
Figure 21-9 Acute otitis media.
Source: Royal Victorian Eye & Ear Hospital, Medical Photography Department.
Multidisciplinary care involves the use of antibiotics to eradicate the causative organism. The treatment of choice is a broad-spectrum antibiotic, oral amoxycillin 250–500 mg at 20–40 mg/kg/day for children administered 8 hourly for 7 days. Surgical intervention is generally reserved for patients who do not respond to medical treatment. A myringotomy involves an incision in the tympanum to release the increased pressure and exudate from the middle ear. A tympanostomy tube may be placed for short- or long-term use. Prompt treatment of an episode of acute otitis media generally prevents spontaneous perforation of the tympanic membrane. In adult patients for whom allergy may be a causative factor, antihistamines may also be prescribed. Since the advent of treatment with antibiotics, the incidence of severe and prolonged infections of the middle ear and mastoid has been greatly reduced.
 NURSING MANAGEMENT: ACUTE OTITIS MEDIA
NURSING MANAGEMENT: ACUTE OTITIS MEDIA
 Following tympanoplasty
Following tympanoplasty
Routine preoperative care is provided before tympanoplasty and includes teaching postoperative expectations. Postoperative concerns are the avoidance of complications such as disruption of the repair during the healing phase, facial nerve paralysis (rare) and increased pressure in the middle ear. The patient is instructed to avoid blowing the nose because this causes increased pressure in the eustachian tube and the middle ear cavity and could dislodge the tympanum graft. Coughing and sneezing can cause similar disruption and are to be avoided if possible. If the patient must cough or sneeze, leaving the mouth open will reduce the pressure. It is essential for the nurse to assist the client when ambulating for the first time. Dizziness and a loss of balance may cause the client to fall.
A cottonwool ball dressing is used for an endaural incision. If a postauricular incision is used and a drain is in place, a mastoid dressing is used. A 7.5 cm square dressing is cut to fit behind the ear and fluffs are applied over the ear to prevent the outer circular head dressing from placing pressure on the auricle. It is necessary to monitor the tightness of the dressing (to prevent tissue necrosis) and the amount and type of drainage postoperatively.
Chronic otitis media and mastoiditis
AETIOLOGY AND PATHOPHYSIOLOGY
Untreated or repeated attacks of acute otitis media may lead to a chronic condition. Chronic infection of the middle ear is more common in persons who experience episodes of acute otitis media in early childhood. Organisms involved in chronic otitis media include S. aureus, Streptococcus, Proteus mirabilis, P. aeruginosa and E. coli. As the mucous membrane is continuous, both the middle ear and the air cells of the mastoid can be involved in the chronic infectious process.
CLINICAL MANIFESTATIONS
Chronic otitis media is characterised by a purulent, mucoid or serous discharge accompanied by hearing loss and occasionally ear pain, nausea and episodes of dizziness or tinnitus (see Fig 21-10). The patient may complain of hearing loss that may be a result of destruction of the ossicles, a tympanic membrane perforation or the accumulation of fluid in the middle ear space. In severe cases the ear may be pushed away from the head by the swelling of the mastoid area. Occasionally, a facial palsy or an attack of vertigo may alert the patient to this condition. Chronic otitis media is usually painless but, if pain is present, it indicates that fluid has accumulated.
COMPLICATIONS
Untreated conditions can result in perforation of the tympanic membrane and the formation of a cholesteatoma (an accumulation of keratinising squamous epithelium in the middle ear). Its enlarging tumour-like behaviour may destroy the adjacent bones, including the ossicles. Unless removed surgically, a cholesteatoma can cause extensive damage to the structures of the middle ear, erode the bony protection of the facial nerve, create a labyrinthine fistula or even invade the dura, threatening the brain. Other complications of a cholesteatoma are facial palsy if it erodes the bony protection of the facial nerve, vertigo from the creation of a labyrinthine fistula and neurological deficits if it invades the dura.
DIAGNOSTIC STUDIES
Otoscopic examination may reveal a marginal or central perforation of the tympanic membrane (see Fig 21-11). Some tympanic membranes may be healed but have an area that is more flaccid and thinner, indicating a previous perforation. Culture and sensitivity tests are necessary to identify the organisms involved so that the appropriate antibiotic therapy can be prescribed. The audiogram may demonstrate no loss in hearing or a loss as great as 50–60 dB if the ossicles have been partially destroyed or disarticulated (separated). Sinus X-rays, magnetic resonance imaging (MRI) or a CT scan of the temporal bone may demonstrate bone destruction, the absence of ossicles or the presence of a mass, most likely a cholesteatoma.
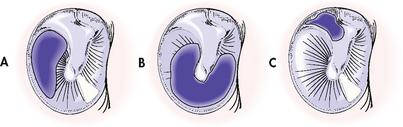
Figure 21-11 Three common tympanic perforations. A, Small central perforation (hearing is usually good). B, Large central perforation around the handle of the malleus (hearing is usually poor). C, Marginal perforation of Shrapnell’s membrane (hearing is usually good). Cholesteatomas commonly occur in patients with a marginal perforation and are always present with attic perforation.
MULTIDISCIPLINARY CARE
The aim of treatment is to clear the middle ear of infection (see Box 21-8). Systemic antibiotic therapy is initiated based on the culture and sensitivity results. In addition, the patient may need to undergo frequent evacuation of drainage and debris in an outpatient setting. Antibiotic ear drops and 2% acetic acid drops are also used to reduce infection. If there is a recurrence, the patient may need to be treated with parenteral antibiotics. In many cases of chronic otitis media, additional antibiotic therapy loses its effectiveness as the number of treatments increases.
MULTIDISCIPLINARY CARE
Surgical therapy
Often, chronic tympanic membrane perforations will not heal with conservative treatment and surgery is necessary. Surgery involving reconstruction of the tympanic membrane and/or the ossicular chain is called a tympanoplasty (see Box 21-9). Diseased tissue is removed, and the ossicles are examined and evaluated in reconstructing the conductive mechanism. This may be done with the use of partial or total ossicular prostheses in combination with a fascia graft to repair the perforation of the tympanic membrane. The incision may be endaural (within the ear canal) or postauricular (behind the auricle or ear), depending on the amount of involvement.
A mastoidectomy is often performed with a tympanoplasty to remove diseased tissue and the source of infection. A modified mastoidectomy attempts to preserve functioning by removing as little tissue as possible. Removal of tissue stops at the middle ear structures that appear capable of functioning in the conduction of sound.
Chronic otitis media with effusion
Chronic otitis media with effusion is an inflammation of the middle ear in which a collection of fluid is present in the middle ear space. The fluid may be thin, mucoid or purulent. This condition is commonly called serous otitis media, glue ear or secretory otitis media. It may occur at any age but is more frequent in children. The fluid usually collects because of a malfunction of the eustachian tube, which commonly follows upper respiratory tract and/or chronic sinus infections, barotrauma (caused by pressure change) or otitis media. If the eustachian tube does not open and allow equalisation of atmospheric pressure, negative pressure within the middle ear causes fluid transudation from the tissues. Allergic reaction of the mucosa, creating oedema, can also cause blockage of the eustachian tube and fluid within the ear. Overgrowth of nasopharyngeal lymphoid tissue and chronic sinusitis are additional factors that may contribute to middle ear effusion.
Complaints include a feeling of fullness of the ear, plugged feeling or popping, and decreased hearing. The patient does not experience pain, fever or discharge from the ear. Otoscopic examination may reveal a normal tympanic membrane or minimal dullness and retraction. Tympanometry and pneumatoscopy may demonstrate limited tympanic membrane motion, which is consistent with decreased hearing acuity.
Decongestants, antihistamines, corticosteroids and antibiotics have been used in the treatment of middle ear effusions. Exercises such as swallowing and gum chewing are used to open the eustachian tube. In addition, the patient may be taught the Valsalva manoeuvre, which forces air into the middle ear through the eustachian tube. If the effusion is not relieved after a period of time, a myringotomy is performed, usually under local or topical anaesthesia with an operating microscope. A ventilating tube is frequently used for patients who have recurrent otitis media with effusion or dysfunction of the eustachian tube. Patients who have a ventilating tube in the tympanic membrane must be instructed not to swim or get water in the ear for at least 6 weeks. Despite efforts to correct inadequate middle ear aeration, eustachian tube dysfunction may persist, causing collapse of the eardrum, conductive hearing loss and formation of a cholesteatoma. Adenoidectomy may also be done in conjunction with myringotomy to correct the underlying problem of middle ear aeration.
Otosclerosis
Otosclerosis, an autosomal dominant disease, is the fixation of the footplate of the stapes in the oval window. It is a common cause of conductive hearing loss in young adults, especially women, and may accelerate during pregnancy. Otosclerosis is bilateral in about 80% of patients. Spongy bone develops from the bony labyrinth, causing immobilisation of the footplate of the stapes, which reduces the transmission of vibrations to the inner ear fluids. Although hearing loss is typically bilateral, one ear may show greater hearing loss progression. The patient is often unaware of the problem until the loss becomes so severe that communication is difficult.
Otoscopic examination may reveal a reddish blush of the tympanum (Schwartz’s sign) caused by the vascular and bony changes within the middle ear. Tuning-fork tests help identify the conductive component of the hearing loss. On the Rinne test, bone conduction will be better than air conduction if hearing loss is greater than 25 dB. Weber’s test lateralises to the ear with the greater conductive hearing loss. An audiogram demonstrates good hearing by bone conduction but air conduction or an air–bone gap audiogram demonstrates poor hearing. Usually a difference of at least 20–25 dB between air- and bone-conduction levels of hearing is seen in otosclerosis.
MULTIDISCIPLINARY CARE
The hearing loss associated with otosclerosis may be stabilised by the use of sodium fluoride with vitamin D and calcium carbonate. These medications retard bone resorption and encourage the calcification of bony lesions. Amplification of sound by a hearing aid can be effective because the inner ear function is normal.
Stapedectomy is the surgical treatment for otosclerosis and is usually performed under local anaesthesia with sedation. The ear with poorer hearing is repaired first and the other ear may be operated on 6 months to a year later. (Multidisciplinary care of otosclerosis is shown in Box 21-10.) In stapedectomy, an endaural incision is made using the operating microscope for visualisation. Generally, the stapes superstructure is removed and a small hole is made in the footplate with a drill or laser. A prosthesis made of stainless steel, Teflon or other synthetic material completes the ossicular chain. Sound is then conducted with the prosthesis. The tympanum is rolled back into normal position and Gelfoam is placed on the flap. A cottonwool ball is placed in the ear canal and a dressing is used to cover the ear. During surgery the patient will often report an immediate improvement in hearing in the operative ear. As a result of the accumulation of blood and fluid in the middle ear, the hearing level decreases postoperatively, but then returns to near-normal levels. After implantation of a stapes prosthesis, 75–85% of patients experience a significant improvement in hearing.49
 NURSING MANAGEMENT: OTOSCLEROSIS
NURSING MANAGEMENT: OTOSCLEROSIS
Nursing management of the patient undergoing a stapedectomy is similar to that for the patient who has undergone a tympanoplasty. Postoperatively, the patient may experience dizziness, nausea and vomiting as a result of stimulation of the labyrinth intraoperatively. Some patients demonstrate nystagmus on lateral gaze because of disturbance of the perilymph. Care should be taken to decrease sudden movements by the patient that may bring on or exacerbate dizziness. Actions such as coughing, sneezing, lifting, bending and straining during bowel movements should also be minimised.
INNER EAR PROBLEMS
Three symptoms that indicate disease of the inner ear are sensorineural hearing loss, vertigo and tinnitus. Vertigo is a subjective feeling of usually rotary movement and is the result of a mismatch between three sensory systems: the vestibular, visual and somatosensory systems. It is not a well-defined disease entity, but rather a syndrome induced by stimulation of the sensory–motor system. It may be accompanied by nausea and vomiting. The objective sign of vertigo is nystagmus.50 Tinnitus is a common and difficult complaint to treat. It may be subjective—the false perception of sound in the absence of an acoustic stimulus—or objective, in which real sounds are heard. Meticulous history taking and physical examination are essential to diagnose the cause.
There is an overlap between manifestations of inner ear disease and central nervous system (CNS) disorders.
Ménière’s disease
Ménière’s disease is characterised by symptoms caused by inner ear disease, including episodic vertigo, tinnitus, fluctuating sensorineural hearing loss and aural fullness. This disease causes significant disability for the patient because of sudden, severe attacks of vertigo with nausea and vomiting. Symptoms usually begin between 30 and 60 years of age. In 40% of patients with Ménière’s disease, bilateral involvement is found.
Although the cause of the disease is unknown, it probably results from changes in the fluid pressures within the inner ear.51 Attacks of vertigo are sudden, with little or no warning. Attacks may be preceded by a sense of fullness in the ear, increasing tinnitus and a decrease in hearing acuity. The patient may experience the feeling of being pulled to the ground (drop attacks). However, only 7% of patients with Ménière’s disease report this symptom. Some patients report that they feel as if they are whirling in space. The duration of attacks may be hours or days, and attacks may occur several times a year. Autonomic symptoms include pallor, sweating, nausea and vomiting.
The clinical course of the disease is highly variable. Low-pitched tinnitus may be present continuously in the affected ear or it may be intensified during an attack. It is often described as a roar or sounds like the ocean. Hearing loss fluctuates and, with continued attacks, hearing recovery is often less complete with each episode, eventually leading to progressive permanent hearing loss.
 NURSING AND COLLABORATIVE MANAGEMENT: MÉNIÈRE’S DISEASE
NURSING AND COLLABORATIVE MANAGEMENT: MÉNIÈRE’S DISEASE
Multidisciplinary care of Ménière’s disease (see Box 21-11) includes diagnostic tests to rule out CNS disease. The audiogram demonstrates a mild low-frequency sensorineural hearing loss in the affected ear. Speech discrimination is often diminished in the affected ear. Vestibular tests are performed to determine whether dizziness is caused by inner ear disturbance. One such test is the caloric test, where the ear is irrigated with warm or cool water or air. This results in nystagmus or rapid eye movements, which assists the doctor in analysing inner ear function. Other tests include measurement of inner ear fluid pressure, an auditory brain stem response (ABR), a computerised test of the hearing nerves and brain pathways and, as these symptoms may be caused by other conditions such as tumours, a CT scan or MRI may be required.
MULTIDISCIPLINARY CARE
During the acute attack, antihistamines, anticholinergics and benzodiazepines can be used to decrease the abnormal sensation and lessen symptoms such as nausea and vomiting. Acute vertigo is treated symptomatically with bed rest, sedation and antiemetics or drugs for motion sickness administered orally, rectally or intravenously. The patient requires reassurance and counselling that the condition is not life-threatening.
Medical management between attacks may include vasodilation, diuretics and antihistamines. Diazepam or prochlorperazine may be used to reduce the dizziness. There is increasing evidence that dietary changes can reduce the frequency of Ménière’s disease episodes. The aim of these changes is to stabilise the body fluid levels to avoid the secondary fluctuations of fluid within the ear. These modifications include eating regular meals, having an adequate intake of low-salt, low-sugar fluids, and avoiding caffeine-containing foods and fluids, such as chocolate, coffee and tea. Caffeine is a stimulant that can make dizziness worse and tinnitus louder. Limiting alcohol to avoid headaches is suggested, as is avoiding smoking as the nicotine constricts blood vessels, thereby decreasing oxygen levels to the inner ear, making the symptoms worse. Approximately 75–85% of patients experience improvement with medical management and supportive therapy. The remainder of patients may, in time, require surgical intervention.
Frequent and incapacitating attacks, reduced quality of life and threatened unemployment are indications for surgical intervention. There are several surgical procedures that may be undertaken. The least invasive is the intratympanic application of gentamicin (also known as chemical labyrinthotomy), which causes partial ablation of the vestibular end organ. It results in a partial loss of balance function in the treated ear, controlling vertigo and usually preserving hearing. Following an initial period of adjustment to the new level of balance function, this treatment is well tolerated. Decompression of the endolymphatic sac and shunting are performed to reduce the pressure on the cochlear hair cells and to prevent further damage and hearing loss. If relief is not achieved, vestibular nerve resection may be performed.52 Recurrence of vertigo attacks following this surgery has been reported in patients followed up over a 10-year period. When involvement is unilateral, surgical ablation of the labyrinth, resulting in loss of the vestibular and hearing cochlear function, is performed. Labyrinthectomy with eighth cranial nerve section has the highest rates for control of vertigo attacks.
Nursing interventions are planned to minimise vertigo and provide for patient safety. During an acute attack the patient is kept in a quiet, darkened room in a comfortable position. The patient needs to be taught to avoid sudden head movements or position changes. Fluorescent or flickering lights or watching television may exacerbate symptoms and should be avoided. An emesis basin should be available because vomiting is common. To minimise the risk of falling, the nurse should keep the side rails up and the bed low in position when the patient is in bed. The patient should be instructed to call for assistance when getting out of bed. Medications and fluids are administered parenterally, and intake and output are monitored. When the attack subsides, the patient should be assisted with ambulation because unsteadiness may remain.
Similar nursing care is provided after surgical ablation of the labyrinth. The patient will have severe tinnitus and vertigo, which decrease during a period of days or weeks as the brain adjusts to the loss of vestibular input and postural stability is regained.
Labyrinthitis
Labyrinthitis is an inflammation of the inner ear, usually caused by either viral or bacterial infection, affecting the cochlear and/or vestibular portion of the labyrinth. An upper respiratory tract infection often precedes the onset of symptoms. The patient may be severely incapacitated for several days to weeks, with gradual resolution of vertigo and vestibular function. Return of hearing usually occurs with the return of vestibular function. A rare form of viral labyrinthitis is herpes zoster oticus, where there is reactivation of a latent varicella zoster virus infection many years after the primary infection. As well as vertigo, hearing loss and facial weakness, there will be deep burning auricular pain followed by the eruption of a vesicular rash in the external auditory canal. While the symptoms gradually resolve over a few weeks, permanent damage may occur.
Bacterial labyrinthitis may occur as a complication of meningitis or otitis media by direct invasion (suppurative labyrinthitis), or by direct invasion through the inner ear (serous labyrinthitis). Meningitis usually affects both ears, whereas otogenic infection causes unilateral symptoms. Profound hearing loss, vertigo, ataxia and nausea and vomiting are commonly seen. Management is directed at eradicating the underlying infection and preventing the spread of infection. Persistent vestibular symptoms and hearing loss often occur.53
Vestibular neuronitis is a disorder of the vestibular nerve associated with hearing loss. It causes vertigo, nausea, vomiting and nystagmus in an otherwise healthy adult. It may follow an upper respiratory tract infection. A viral infection may be the cause and the patient should recover after 7–10 days. Tinnitus is not present and hearing loss does not occur. Management is similar to that for bacterial labyrinthitis.
Benign paroxysmal positional vertigo
Benign paroxysmal positional vertigo (BPPV) is characterised by incapacitating vertigo and involuntary eye movements (nystagmus), usually lasting less than a minute. These usually occur with rapid changes in body position, such as rolling over in bed or straightening up after bending over. Hearing is not affected. It is caused by an accumulation in the inner ear of particles made up of calcium carbonate crystals. It may be secondary to head injury, infection or degeneration of the vestibular system with advanced age. Spontaneous resolution often occurs. If not, management consists of repositioning manoeuvres. The most commonly used technique is the Epley manoeuvre, which, through a series of head movements, causes the particles to be repositioned to an area in the inner ear where the vestibular nerve is not stimulated. As this treatment is almost always successful, surgery is considered only in the very few patients with prolonged BPPV who do not respond completely to physiotherapy.54
Acoustic neuroma
An acoustic neuroma (or vestibular schwannoma) is a benign tumour that occurs where the acoustic nerve (CN VIII) enters the internal auditory canal or the temporal bone from the brain. It is important that an early diagnosis be made because the tumour can compress the facial nerve and arteries within the internal auditory canal. Once the tumour has expanded and become an intracranial neoplasm, more extensive surgery is necessary, reducing the chances of preserving hearing and normal facial nerve function. It can expand into the cerebellopontine angle and involve other cranial nerves and the brain by compression.
Early symptoms are associated with CN VIII compression and destruction. They include unilateral, progressive, sensorineural hearing loss; unilateral tinnitus; and mild, intermittent vertigo. One of the earliest symptoms of an acoustic neuroma is reduced touch sensation in the posterior ear canal. Diagnostic tests include neurological, audiometric and vestibular tests and CT scans and MRI with gadolinium enhancement.
Surgery to remove small tumours is performed through the middle cranial fossa or retrolabyrinthine approach, which preserves hearing and vestibular function. A translabyrinthine approach is usually used for medium-sized tumours and when hearing is minimal. Although hearing is destroyed by this approach, advantages include good access to the tumour and preservation of the facial nerve. Retrosigmoid (suboccipital) or transotic approaches are used for large tumours (>3 cm). It is almost impossible to preserve hearing when the tumour is larger than 2 cm.
Hearing loss and deafness
Hearing disorders are considered to be a primary disability worldwide. Many older people have hearing impairment and it is one of the most common disabilities in Australia: more than 50% of people over 60 years of age complain of some degree of hearing loss.2 The majority of people lose their hearing as adults, but hearing loss from noisy environments (industrial deafness) is also being noticed in young adults aged 20–30 years. Routine screening for adults is advised in order to detect problems early. Often the patient is unaware of minimal hearing loss or may compensate by asking others to speak up or by showing irritability with those who do not speak up. More often it is the family and friends who are the first to notice a patient’s hearing loss.
TYPES OF HEARING LOSS
Conductive hearing loss
Conductive hearing loss occurs in the outer and middle ear and impairs the sound being conducted from the outer to the inner ear. It is caused by conditions interfering with air conduction, such as impacted cerumen and foreign bodies, middle ear disease, otosclerosis and stenosis of the external auditory canal. The audiogram demonstrates an air–bone gap of at least 15 dB. One of the most common causes of conductive hearing loss is otitis media with effusion.
An air–bone gap occurs when hearing sensitivity by bone conduction is significantly better than by air conduction. Patients may speak softly because they hear their own voice, which is conducted by bone, as being loud. These patients hear better in a noisy environment. A hearing aid is helpful for a patient with a 40–50 dB loss or more, although the device often is not necessary because of the excellent results of treatment of the underlying problem.
Sensorineural hearing loss
Sensorineural hearing loss is caused by impairment of function of the inner ear or its central connections. Congenital and hereditary factors, noise trauma over a period of time, ageing (presbycusis), Ménière’s disease and ototoxicity can cause sensorineural hearing loss. Systemic diseases, such as tuberculosis, syphilis, Lyme disease, CMV, HIV and Paget’s disease of the bone, can also cause sensorineural deafness. Immune diseases, diabetes mellitus, bacterial meningitis and trauma are additional causes of this type of hearing loss.
The two main problems associated with sensorineural loss are the ability to hear sound but not to understand speech, and the lack of understanding of the problem by others. The ability to hear high-pitched sounds diminishes with a sensorineural hearing loss. Consonants are high-pitched sounds that give intelligibility to speech. Words become difficult to distinguish and sound becomes muffled. An audiogram demonstrates a loss in decibel levels in the 4000 Hz range, which can progress to the 2000 Hz range. A hearing aid may help the patient who has a 30 dB loss or more by reducing the strain of trying to hear but the sounds will still be muffled. Presbycusis, which is degenerative change of the inner ear, is a major cause of sensorineural hearing loss in older adults. It is a progressive problem that results in many psychological and communication issues. The management of inner ear diseases such as Ménière’s disease can prevent further hearing loss. If ototoxic drugs are used, hearing should be monitored frequently during treatment. Causes of hearing loss are shown in Figure 21-12.
Mixed hearing loss
Mixed hearing loss is caused by a combination of conductive and sensorineural losses. Careful evaluation is needed before corrective surgery for conductive loss is planned because the sensorineural component of the hearing loss will still remain.
Central and functional hearing loss
Central hearing loss is caused by problems in the CNS from the auditory nucleus to the cortex. The patient is unable to understand or to put meaning to the incoming sound. Functional hearing loss may be caused by an emotional or a psychological factor. The patient does not seem to hear or respond to pure-tone subjective hearing tests but no organic cause can be identified. A careful history is helpful because there is usually a reference to deafness within the family. Psychological counselling may help. Referral to qualified hearing and speech services is indicated.
CLINICAL MANIFESTATIONS
Manifestations that indicate hearing loss include asking others to speak up, answering questions inappropriately, not responding when not looking at the speaker, straining to hear, cupping a hand around the ear, showing irritability with others who do not speak up and increasing sensitivity to slight increases in noise level. Often the patient is unaware of minimal hearing loss or may compensate by using these mannerisms. Family and friends who get tired of repeating or talking loudly are often the first to notice hearing loss.
Deafness is often called the ‘unseen handicap’ because it is not until conversation is initiated with a deaf adult that the difficulty in communication is realised. It is important that the health professional be aware of the need for thorough validation of the deaf person’s understanding of health teaching. Descriptive visual aids can be helpful.
Interference in communication and interaction with others can be the source of many problems for the patient and family. Often the patient refuses to admit or may be unaware of impaired hearing. Irritability is common because of the concentration with which the patient must listen to understand speech. The loss of clarity of speech in the patient with sensorineural hearing loss is most frustrating. The patient may hear what is said but not understand it. Withdrawal, suspicion, loss of self-esteem and insecurity are commonly associated with advancing hearing loss.
 NURSING AND COLLABORATIVE MANAGEMENT: HEARING LOSS AND DEAFNESS
NURSING AND COLLABORATIVE MANAGEMENT: HEARING LOSS AND DEAFNESS
 Health promotion
Health promotion
 Environmental noise control
Environmental noise control
Hearing loss can be caused by acute loud noise (acoustic trauma) or by chronic exposure to loud noise (noise-induced hearing loss). Acoustic trauma causes hearing loss from mechanical destruction of parts of the organ of Corti. Some recovery of function may occur in the first weeks after injury but the remaining loss is permanent. Noise-induced hearing loss is probably caused by high-intensity stimulation of the cochlea, resulting in mechanical damage to the hair cells and supporting cells in the organ of Corti.
Sensorineural hearing loss as a result of increased and prolonged environmental noise, such as amplified sound, is occurring in young adults at an increasing rate. Health teaching regarding avoidance of continued exposure to noise levels greater than 85–95 dB is essential. Table 21-7 describes the range of sounds audible to humans.
TABLE 21-7 Range of sounds audible to the human ear
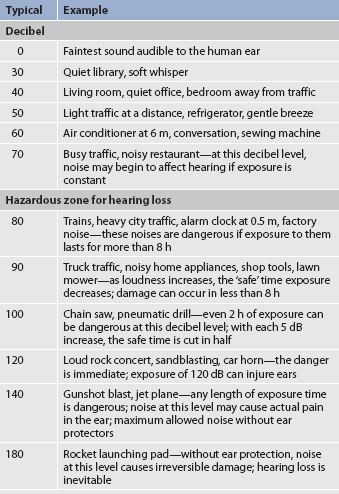
Source: Adapted from American Academy of Otolaryngology, 2009. Available at www.entnet.org.
In work environments known to have high noise levels (>85 dB), ear protection should be worn. Occupational Health and Safety (OHS) standards require ear protection for workers in environments where the noise levels exceed 85 dB consistently. A variety of protectors are available that are worn over the ears or in the ears to prevent hearing loss. Periodic audiometric screening should be part of the health maintenance policies of industry. This provides baseline data on hearing against which to measure subsequent hearing loss.
Nurses should participate in hearing conservation programs in work environments. A hearing conservation program should include noise exposure analysis, provision for control of noise exposure (hearing protectors), measurements of hearing, and employee–employer notification and education. Often a multidisciplinary team, including an industrial OHS nurse, engineer and audiometric technician, is responsible for such a program.
Ear protection should be worn during target shooting and other recreational pursuits with high noise levels. Young adults should be encouraged to keep amplified music at a reasonable level and limit their exposure time. Hearing loss caused by noise is not reversible.
 Immunisations
Immunisations
Childhood and adult immunisations, including measles, mumps and rubella (MMR) immunisation, should be promoted. Various viruses can cause deafness as a result of fetal damage and malformations affecting the ear. The period of greatest risk of birth defects due to rubella infection is during the first trimester. If infection occurs early in the second trimester, the result is often permanent hearing impairment.55 Women of childbearing age should be tested for immunity. A rubella antibody titre of 1:8 or greater shows that the individual has immunity to rubella. If the titre is less, immunisation with live vaccine should be given. The woman should avoid pregnancy for at least 3 months after being immunised. Immunisation must be delayed if the woman is pregnant. Women who are susceptible to rubella can be vaccinated safely during the postpartum period.
 Ototoxic drugs
Ototoxic drugs
The patient’s reaction to drugs that are known to cause ototoxicity should be monitored. Ototoxicity may affect a person’s hearing (auditory or cochlear function) or balance (vestibular function), or both. Ototoxic drugs are capable of damaging one or both branches of the auditory nerve (CN VIII) and the inner ear. Drugs commonly associated with ototoxicity include salicylates, analgesics, antimalarial drugs, loop diuretics, antineoplastic drugs and antibiotics (see Table 21-8). Patients who are receiving these drugs should be assessed for signs and symptoms associated with ototoxicity. The most common symptoms of drug-induced ototoxicity are tinnitus, sensorineural hearing loss and vestibular dysfunction. If these symptoms develop, immediate withdrawal of the drug may prevent further damage and may cause the symptoms to disappear.
 Assistive devices and techniques
Assistive devices and techniques
 Hearing aids
Hearing aids
It is important that the patient with a suspected hearing loss has a hearing assessment by a qualified audiologist, including examination and audiometric testing. If a hearing aid is indicated, it should be fitted by the audiologist or a speech and hearing specialist. Many types of hearing aids are available, each with advantages and disadvantages: completely-in-the-canal, in-the-canal, in-the-ear, behind-the-ear (see Fig 21-13) and implantable hearing aids. The conventional hearing aid serves as a simple amplifier. For the patient with bilateral hearing impairment, binaural hearing aids provide the best sound lateralisation and speech discrimination. Patients who are motivated and optimistic about using a hearing aid will be more successful users. The nurse must be prepared to give careful instruction on its use and maintenance and to assist the patient during the period of adjustment.
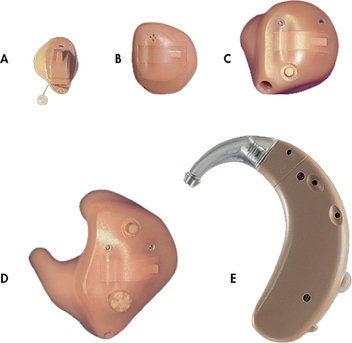
Figure 21-13 Hearing aids are classified into five basic types. A, TRIANO Micro CIC (completely-in-the-canal) hearing aid. B, TRIANO ITC (in-the-canal) hearing aid. C, TRIANO HS (half shell) hearing aid. D, TRIANO ITE (in-the-ear) hearing aid. E, TRIANO 3 BTE (behind-the-ear) hearing aid. The TRIANO product family, its fitting philosophy, and its range of accessories were intended to satisfy individuals of all ages, from infants through senior citizens, who have hearing loss.
Initially, use of the hearing aid should be restricted to quiet situations in the home. The patient must first adjust to voices (including the patient’s own) and household sounds. The patient should also experiment by increasing and decreasing the volume, as situations require. As adjustment to the increase in sounds and background noise occurs, the patient will be ready to try a different listening environment, such as a small party where several people will be talking simultaneously. Then the environment can be expanded to the outdoors. After adapting to controlled situations, the patient will be ready to encounter environments such as a shopping centre or supermarket. Adjustment to different environments occurs gradually, depending on the individual patient.
When the hearing aid is not being worn, it should be placed in a dry, cool area where it will not be inadvertently damaged or lost. The battery should be disconnected or removed. Battery life averages 1 week and patients should be advised to purchase only a month’s supply at a time. Ear moulds should be cleaned weekly or as needed. Toothpicks or pipe cleaners may be used to clear a clogged ear tip.
 Speech reading
Speech reading
Speech reading, commonly called lip reading, can be helpful in increasing communication. It allows for approximately 40% understanding of the spoken word. The patient is able to use visual cues associated with speech, such as gestures and facial expressions, to help clarify the spoken message. In speech reading, many words will look alike to the patient (e.g. rabbit and woman). If the patient wears glasses, the glasses should be used to facilitate speech reading. The nurse can help the patient by using and teaching verbal and non-verbal communication techniques, as described in Box 21-12. If a hearing aid is used, it should be readily available to the patient.
 Sign language
Sign language
Sign language is used as a form of communication for people with profound hearing impairment. It can involve gestures, finger spelling and facial changes such as eyebrow motion and lip/mouth movements. Sign language is not universal. For example, Auslan (Australian Sign Language; see Resources on p 506) is the language of the deaf community in Australia, and New Zealand Sign Language (NZSL; see Resources on p 506) is unique to New Zealand.
 Cochlear implant
Cochlear implant
The cochlear implant is used as a hearing device for the profoundly deaf. The system consists of a surgically implanted induction coil beneath the skin behind the ear and an electrode wire placed in the cochlea (see Fig 21-14). The implanted parts interface with an externally worn speech processor. The system stimulates auditory nerve fibres by means of an electric current so that signals reach the brainstem’s auditory nuclei and ultimately the auditory cortex. The implant is intended for patients whose sensorineural hearing loss is either congenital or acquired and for whom hearing aids are not helpful. The ideal candidate is one who has become deaf after acquiring speech and language. Adults who were born deaf or became deaf before learning to speak or understand language may have difficulty using a cochlear implant. This is because it is thought that some memory of sound is necessary in order to make sense of the signals passed to the brain by the implant. While there is still debate about when is it best to undertake implants, studies have suggested that cochlear implants fitted in children of 2–6 years of age have the best results.56
The implant offers the profoundly deaf the ability to hear environmental sounds, including speech, at comfortable loudness levels. Multichannel cochlear implants also serve as aids to speech production. Extensive training and rehabilitation are essential to receive maximum benefit from these implants. The positive aspects of a cochlear implant include providing sound to the person who has heard none, improving lip reading, monitoring the loudness of the person’s own speech, improving the sense of security and decreasing feelings of isolation. With continued research the cochlear implant may offer the possibility of aural rehabilitation for a wider range of hearing-impaired individuals.
 Assisted listening devices
Assisted listening devices
Numerous devices are now available to assist the hearing-impaired. Direct amplification devices, amplified telephone receivers, alerting systems that flash when activated by sound, an infrared system for amplifying the sound of the television, and a combination FM receiver and hearing aid are all aids that can be explored by the nurse based on patient needs.
Gerontological considerations: hearing loss
Presbycusis, which is hearing loss associated with ageing, includes the loss of peripheral auditory sensitivity, a decline in word recognition ability, and associated psychological and communication issues. Consonants (high-frequency sounds) are the letters by which spoken words are recognised and the ability of the older person with presbycusis to understand the spoken word is greatly affected. Vowels are heard but some consonants fall into the high-frequency range and cannot be differentiated. This may lead to confusion and embarrassment because of the difference between what was said and what was heard.
The cause of presbycusis is related to degenerative changes in the inner ear, such as loss of hair cells, reduction of blood supply, diminution of endolymph production, decreased basilar membrane flexibility and loss of neurons in the cochlear nuclei. Noise exposure is thought to be a common factor related to presbycusis. Table 21-9 describes the classification of specific causes and associated hearing changes of presbycusis. Often, more than one type of presbycusis may be present in the same person. The prognosis for hearing depends on the cause of the loss. Sound amplification with the appropriate device is often helpful in improving the understanding of speech. In other situations an audiological rehabilitation program can be valuable.
TABLE 21-9 Classification of presbycusis
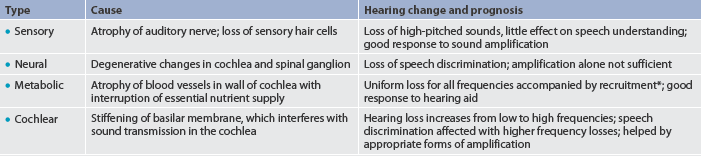
* Abnormally rapid increase in loudness as sound intensity increases.
Older adults are often reluctant to use a hearing aid for sound amplification. Reasons cited most often include cost, appearance, insufficient knowledge about hearing aids, amplification of competing noise and unrealistic expectations. Most hearing aids and batteries are small, and neuromuscular changes, such as stiff fingers, enlarged joints and decreased sensory perception, often make the care and handling of a hearing aid a difficult and frustrating experience for an older person. Some elderly people may also tend to accept their losses as part of getting older and believe there is no need for improvement.
CASE STUDY
Patient profile
Anne Richards, a 60-year-old Indigenous Australian woman with rheumatoid arthritis, returns to the clinic in North Queensland for follow-up care of primary open-angle glaucoma. Her current medical regimen includes topical timolol 0.25% twice daily and latanoprost 0.005% 1 drop at night. Her intraocular pressures are stable on this regimen.
Multidisciplinary care
CRITICAL THINKING QUESTIONS
1. Explain the aetiology of this patient’s new scotoma.
2. Why might ALT be an appropriate therapy in this case?
3. What is the purpose of the topical corticosteroid drops after the laser procedure?
4. What topics should the nurse discuss with this patient in discharge teaching?
5. What is the therapeutic goal of ALT?
6. Based on the assessment data, write one or more appropriate nursing diagnoses. Are there any collaborative problems?
1. What are the main coping strategies of the patient with severe visual impairment? How can the nurse best support these strategies?
2. What strategies are most effective in teaching patients about avoiding sources of ocular irritation?
3. What factors contribute to the decision-making process for a patient with cataracts who chooses surgery over continued palliative therapy?
4. Are there significant differences in outcomes for older patients when postoperative care following eye surgery includes visits by a home healthcare nurse?
5. How does family support significantly influence patient use of and adjustment to a hearing aid?
6. What motivates a patient to comply with the therapeutic regimen following a tympanoplasty?
1. Presbyopia occurs in older individuals because:
2. The most important nursing intervention in patients with epidemic keratoconjunctivitis is:
3. Patients with an eye inflammation or infection should be taught:
4. Rubella can cause hearing problems if:
5. In preparing patients for retinal detachment surgery, the nurse should:
6. The nurse should instruct patients with glaucoma that:
7. The nurse would suspect otosclerosis from assessment findings of hearing loss in:
8. The patient who has a sensorineural hearing loss:
9. The nurse teaches the patient with extended wear contact lenses that:
10. A nursing measure that is helpful in communicating with a hearing-impaired patient is to:
1 Cochrane G, du Toit R, Le Mesurier R. Management of refractive errors. BMJ. 2010;340:1711.
2 Australian Bureau of Statistics. National Health Survey: summary of results. Available at www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.02004-05?OpenDocument, 2007–2008. accessed 20 February 2011.
3 Attebo K, Mitchell P, Cumming R, et al. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998;105(1):154–159.
4 Thompson JM, McFarland GK, Hirsch JE, Tucker SM, eds. Mosby’s clinical nursing, 5th edn., St Louis: Mosby, 2002.
5 Marsden JM, Spence M. Optics in ophthalmic care. London: John Wiley & Sons, 2006.
6 Kanski JJ. Clinical ophthalmology: a systematic approach, 5th edn. New York: Butterworth–Heinemann, 2003.
7 Brandt JT, Nason FE. Community resources for the ophthalmic practice. Albert DM, Jakobiec FA, eds. Principles and practice of ophthalmology: clinical practice, 3rd edn., Vol 5. Philadelphia: WB Saunders, 2008.
8 Chalita MR, Krueger RR. Correlation of aberrations with visual acuity and symptoms. Ophthalmol Clin North Am. 2004;17:135–142.
9 LASIK for hyperopia, hyperopic astigmatism, and mixed astigmatism: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111:1604–1617.
10 Royal Australian and New Zealand College of Ophthalmologists. Excimer laser surgery. Available at www.ranzco.edu/aboutus/faq/excimer-laser-surgery/. accessed 20 February 2011.
11 Centre for Eye Research Australia. The economic impact and cost of vision loss in Australia. Available at www.cera.org.au/uploads/CERA_clearinsight_overview.pdf. accessed 20 February 2011
12 Royal New Zealand Foundation of the Blind. Available at www.rnzfb.org.nz accessed 20 February 2011.
13 World Health Organization. Available at www.who.int/blindness/causes/priority/en/print.html accessed 20 February 2011.
14 Centre for Eye Research Australia. Focus on low vision. Available at www.cera.org.au/uploads/CERA_FocusLowVision.pdf. accessed 20 February 2011.
15 World Health Organization. Vision 2020. Fact sheet. Available at http://whqlibdoc.who.int/fact_sheet/2004/FS_282.pdf. accessed 20 February 2011.
16 Rosenberg E, Sperrazza L. The visually impaired patient. Am Acad Fam Phys. 2008;77:1431.
17 Worksafe Western Australia. Safetyline. Available at www.commerce.wa.gov.au/WorkSafe/Content/Safety_Topics/Plant_and_machines/Additional_information/Eye_injuries.html. accessed 20 February 2011.
18 Bord S, Linden J. Trauma to the globe and orbit. Emerg Med Clin North Am. 2008;26:97.
19 McQueen L. Eyelid and lacrimal drainage system. In: Marsden JM, Spence M, eds. Optics in ophthalmic care. London: John Wiley & Sons, 2006.
20 Foulks American Academy of Ophthalmology, Ophthalmic News and Education Network. Blepharitis: preferred practice pattern guidelines. Available at www.aao.org/theeyeshaveit/red-eye/blepharitis.cfm, 2003. accessed 20 February 2011
21 Jackson WB. Blepharitis: current strategies for diagnosis and management. Can J Ophthalmol. 2008;43(2):170–179.
22 Boling E. A review of ocular infections for the primary care optometrist. Contemp Optom. 2005;3(11):1–6.
23 Taylor HR. Trachoma in Australia. Med J Aust. 2001;175:371–372.
24 Ejere H, Alhassan M, Rabiu M. Face washing for preventing active trachoma. Cochrane Database Syst Rev. (3):2004. CD003659.
25 Bryant B, Knights K, Salerno E. Pharmacology for health professionals. Sydney: Elsevier, 2003.
26 Pavan-Langston D. Viral disease of the cornea and external eye. Albert DM, Jakobiec FA, eds. Principles and practice of ophthalmology: clinical practice, 3rd edn., Vol 5. Philadelphia: WB Saunders, 2008.
27 Dart JK, Saw VPJ, Kilvington S. Acanthamoeba keratitis: diagnosis and treatment update, 2009. Am J Ophthalmol. 2009;148(4):487–499.
28 Talamo JH, Steinert RF. Keratorefractive surgery. Albert DM, Jakobiec FA, eds. Principles and practice of ophthalmology: clinical practice, 3rd edn., Vol 5. Philadelphia: WB Saunders, 2008.
29 Centre for Eye Research Australia. Keratoconus research. Available at www.cera.org.au/index.php?nodeId=48. accessed 20 February 2011.
30 New Vision Clinics. Small incision cataract surgery. Available at www.newvisionclinics.com.au/newvision/lasereyesurgery.asp?id=18&lvl=2&title=. accessed 20 February 2011.
31 Kirkwood B. Clinical assessment of patients with cataract. Insight. 2008;33:10.
32 Snellingen T, Evans JR, Ravilla T, Foster A. Surgical intervention for age-related cataract. Cochrane Database Syst Rev. (4):2006. CD001323.
33 DeCroos F, Afshari N. Perioperative antibiotics and antiinflammatory agents in cataract surgery. Curr Opin Ophthalmol. 2008;19:22.
34 Frank RN. Diabetic retinopathy. N Engl J Med. 2004;350:48–58.
35 Wegmann-Burns M, Gugger M, Goldblum D. Hypertensive retinopathy. Lancet. 2004;363:456.
36 McKay R, McCarty CA, Taylor HR. Diabetic retinopathy in Victoria, Australia: The Visual Impairment Project. Aust NZ J Publ Health. 2000;24:565–569.
37 Wilkinson C. Interventions for asymptomatic retinal breaks and lattice degeneration for preventing retinal detachment. Cochrane Database Syst Rev. (1):2005. CD003170.
38 Raynel S, Brochner O. The retina and vitreous. In: Marsden JM, Spence M, eds. Optics in ophthalmic care. London: John Wiley & Sons, 2006.
39 Constable JJ. Age-related macular degeneration and its possible prevention. Despite well publicised claims of the therapeutic value of dietary supplements and other new treatments, the evidence for their effectiveness is modest. Med J Aust. 2004;181:471–472.
40 Rosenthal B, Fletcher K, Rubin G, et al. Visual function and age-related macular degeneration. New York: Lighthouse International, 2003.
41 Singerman LJ, et al. Pegaptanib sodium for neovascular age-related macular degeneration: third-year safety results of the VEGF Inhibition Study in Ocular Neovascularisation (VISION) trial. Br J Ophthalmol. 2008;92:1606–1611.
42 Spaide RF, Laud K, Fine H, et al. Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age related-macular degeneration. Retina. 2006;26:383–390.
43 Kunimoto D, Kanitkar K, Makar M, et al. Wills eye manual: office and emergency room diagnosis and treatment of eye diseases, 5th edn. Philadelphia: Lippincott, 2008.
44 Craft J, Gordon C, Tiziani A. Understanding pathophysiology. Sydney: Elsevier, 2011.
45 Sharts-Hopko N, Glynn-Milley C. Primary open-angle glaucoma. Am J Nurs. 2009;109:40.
46 Keene WE, Markum AC, Samadpour M. Outbreak of Pseudomonas aeruginosa infections caused by commercial piercing of upper ear cartilage. JAMA. 2004;291:981–985.
47 Cantrell HF, Lombardy EE, Duncanson FP, et al. Declining susceptibility to neomycin and polymyxin B of pathogens recovered in otitis externa trials. South Med J. 2004;97:465–471.
48 Patton KT, Thibodeau GA. Anatomy and physiology, 7th edn. St Louis: Mosby, 2010.
49 Durko M, et al. Does the material of stapes prosthesis influence hearing improvement in stapes surgery? Retrospective analysis of 350 cases. Otolaryngol Pol. 2008;62:4.
50 Dieterich M. Dizziness. Neurologist. 2004;10(3):154–164.
51 Merchant SN, Adams JC, Nadol JB, Jr. Pathophysiology of Meniere’s syndrome: are symptoms caused by endolymphatic hydrops? Otol Neurotol. 2005;26:74–81.
52 Sajjadi H, Paparella M. Ménière’s disease. Lancet. 2008;372:406.
53 Boston ME. Inner ear, labyrinthitis. Available at www.emedicine.com/ent/topic226.htm. accessed 24 February 2011.
54 Bull PD. Diseases of the ear, nose and throat, 10th edn. Oxford: Blackwell Publishing, 2007.
55 Olds SB, London ML, Ladewig PA. Maternal newborn nursing, 7th edn. Upper Saddle River, NJ: Prentice Hall Health, 2003.
56 National Institute on Deafness and Other Communication Disorders. Cochlear implants. Available at www.nidcd.nih.gov/health/hearing/coch.html#c. accessed 24 February 2011.
Association for the Blind of WA (Inc.). www.abwa.asn.au
Auslan (Australian Sign Language). www.auslan.org.au
Australian Institute of Health & Welfare. www.aihw.gov.au
Australian Prescriber: correct use of eye drops. www.australianprescriber.com/magazine/31/1/16/7
Australian Safety and Compensation Council. www.ascc.gov.au
Better Hearing Australia. www.betterhearing.org.au
Blind Citizens Australia. www.bca.org.au
Council of Remote Area Nurses of Australia Inc. www.crana.org.au
Deaf Association of New Zealand. www.deaf.co.nz
Deafness Forum of Australia. www.deafnessforum.org.au
Department of Health and Ageing (Australia). www.health.gov.au
Fred Hollows Foundation. www.hollows.org
Glaucoma Australia. www.glaucoma.org.au
National Institute on Deafness and Other Communication Disorders. www.nidcd.nih.gov
New Zealand Ministry of Health. www.health.govt.nz
New Zealand Sign Language (NZSL). www.deaf.org.nz/resources/new-zealand-sign-language
Royal New Zealand Foundation of the Blind. www.rnzfb.org.nz
Royal Victorian Eye & Ear Hospital. www.eyeandear.org.au
Seeing Eye Dogs Australia. www.seda.org.au
Vision Australia. www.visionaustralia.org.au
Vision 2020 Australia. www.vision2020australia.org.au