Principles of Manual Muscle Testing
MUSCLE TEST
THE GRADING SYSTEM
Grades for a manual muscle test are recorded as numerical scores ranging from zero (0), which represents no activity, to five (5), which represents a “normal” or best-possible response to the test or as great a response as can be evaluated by a manual muscle test. Because this text is based on tests of motions rather than tests of individual muscles, the grade represents the performance of all muscles in that motion. The 5 to 0 system of grading is the most commonly used convention.
Each numerical grade can be paired with a word that describes the test performance in qualitative terms. These qualitative terms, when written, are capitalized to indicate that they too represent a score. This does not mean that the test grades are quantitative in any manner.
OVERVIEW OF TEST PROCEDURES
The Break Test: Manual resistance is applied to a limb or other body part after it has completed its range of movement or after it has been placed at end range by the examiner. The term “resistance” is always used to denote a force that acts in opposition to a contracting muscle. Manual resistance should always be applied in the direction of the “line of pull” of the participating muscle or muscles. At the end of the available range, or at a point in the range where the muscle is most challenged, the patient is asked to hold the part at that point and not allow the examiner to “break” the hold with manual resistance. For example, a seated subject is asked to flex the elbow to its end range; when that position is reached, the examiner applies resistance at the wrist, trying to force the elbow to “break” its hold and move downward into extension. This is called a break test, and it is the procedure most commonly used in manual muscle testing today.
As a recommended alternative procedure, the examiner may choose to place the muscle group to be tested in the end or test position rather than have the patient actively move it there. In this procedure the examiner ensures correct positioning and stabilization for the test.
Active Resistance Test: An alternative to the break test is the application of manual resistance against an actively contracting muscle or muscle group (i.e., against the direction of the movement as if to prevent that movement). This may be called an “active resistance” test. During the motion, the examiner gradually increases the amount of manual resistance until it reaches the maximal level the subject can tolerate and motion ceases. This kind of manual muscle test requires considerable skill and experience to perform and is so often equivocal that its use is not recommended.
Application of Resistance: The principles of manual muscle testing presented here and in all published sources since 1921 follow the basic tenets of muscle length-tension relationships as well as those of joint mechanics.1,2 In the case of the biceps brachii, for example, when the elbow is straight, the biceps lever is short; leverage increases as the elbow flexes and becomes maximal (most efficient) at 90°, but as flexion continues beyond that point, the lever arm again decreases in length and efficiency.
In manual muscle testing, the application of external force (resistance) at the end of the range in onejoint muscles allows consistency of procedure rather than an attempt to select the estimated midrange position. In two-joint muscles (e.g., the medial or lateral hamstring muscles), the point of maximum resistance is generally at or near midrange.
The point on an extremity or part where the examiner should apply resistance is near the distal end of the segment to which the muscle attaches. There are two common exceptions to this rule: the hip abduc-tors and the scapular muscles. In testing the hip abductor muscles, resistance would be applied at the distal end of the femur just above the knee. The abductor muscles are so strong, however, that most examiners, in testing a patient with normal knee strength and joint integrity, will choose to apply resistance at the ankle. The longer lever provided by resistance at the ankle is a greater challenge for the abductors and is more indicative of the functional demands required in gait. It follows that when a patient cannot tolerate maximal resistance at the ankle, his muscle cannot be considered Grade 5. In the patient who has an unstable knee, resistance to the abductors of the hip should be applied at the distal femur just above the knee. When using the short lever, hip abductor strength must be graded no better than Grade 4 (Good) even when the muscle takes maximal resistance.
An example of testing with a short lever occurs in the patient with a transfemoral amputation, where the grade awarded, even when the patient can hold against maximal resistance, is Grade 4 (Good). This is done because of the loss of the weight of the leg and is particularly important when the examiner is evaluating the patient for a prosthesis. The muscular force available should not be overestimated in predicting the patient’s ability to use the prosthesis.
In testing the vertebroscapular muscles (e.g., rhomboids), the preferred point of resistance is on the arm rather than on the scapula where these muscles insert. The longer lever more closely reflects the functional demands that incorporate the weight of the arm. Other exceptions to the general rule of applying distal resistance include contraindications such as a painful condition or a healing wound in a place where resistance might otherwise be given.
The application of manual resistance to a part should never be sudden or uneven (jerky). The examiner should apply resistance somewhat slowly and gradually, allowing it to build to the maximum tolerable intensity. Critical to the manual test is the location of the resistance and its consistency over many tests. (The novice examiner should make a note of the point of resistance when a variation is used.) Resistance is applied at a 90° angle to the primary axis of the body part being tested.
The application of resistance permits an assessment of muscular strength when it is applied in the opposite direction to the muscular force or torque. The examiner also should understand that the weight of the limb plus the influence of gravity is part of test responses. When the muscle contracts in a parallel direction to the line of gravity, it is noted as “gravity minimal” (GM). It is suggested that the commonly used term “gravity eliminated” be avoided because, of course, that can never occur except in a zero-gravity environment. Thus strength is evaluated when weakened muscles are tested in a plane horizontal to the direction of gravity; the body part is supported on a smooth, flat surface in a way that friction force is minimal (Grades 2, 1, and 0). For stronger muscles that can complete a full range of motion in a direction against the pull of gravity (Grade 3), resistance is applied perpendicular to the line of gravity (Grades 4 and 5). Acceptable variations to antigravity and gravity-minimal positions are discussed in individual test sections.
The Examiner and the Value of the Muscle Test: The knowledge and skill of the examiner determine the accuracy and defensibility of a manual muscle test. Specific aspects of these qualities include the following:
• Knowledge of the location and anatomical features of the muscles in a test. In addition to knowing the muscle attachments, the examiner should be able to visualize the location of the tendon and its muscle in relationship to other tendons and muscles and other structures in the same area (e.g., the tendon of the extensor carpi radialis longus lies on the radial side of the tendon of the extensor carpi radialis brevis at the wrist).
• Knowledge of the direction of muscle fibers and their “line of pull” in each muscle.
• Knowledge of the function of the participating muscles (e.g., synergists, prime movers, accessories).
• Consistent use of a standardized method for each different test.
• Consistent use of proper positioning and stabilization techniques for each test procedure. Stabilization of the proximal segment of the joint being tested is achieved in several ways. These ways include patient position (via body weight), the use of a firm surface for testing, muscle activity by the patient, and manual fixation by the examiner.
• Ability to identify patterns of substitution in a given test and how they can be detected based on a knowledge of which other muscles can be substituted for the one(s) being tested.
• Ability to detect contractile activity during both contraction and relaxation, especially in minimally active muscle.
• Sensitivity to differences in contour and bulk of the muscles being tested in contrast to the contralateral side or to normal expectations based on such factors as body size, occupation, or leisure activities.
• Awareness of any deviation from normal values for range of motion and the presence of any joint laxity or deformity.
• Understanding that the muscle belly must not be grasped at any time during a manual muscle test except specifically to assess tenderness or pain and muscle mass.
• Ability to identify muscles with the same innervation, which will ensure a comprehensive muscle evaluation and accurate interpretation of test results (because weakness of one muscle in a myotome should require examination of all).
• Knowledge of the relationship of the diagnosis to the sequence and extent of the test (e.g., the patient with C7 complete tetraplegia will require definitive muscle testing of the upper extremity but only confirmatory tests in the lower extremities).
• Ability to modify test procedures when necessary while not compromising the test result and understanding the influence of the modification on the result.
• Knowledge of the effect of fatigue on the test results, especially muscles tested late in a long testing session, and a sensitivity to fatigue in certain diagnostic conditions such as myasthenia gravis or Eaton-Lambert syndrome.
The examiner also may inadvertently influence the test results and should be especially alert when testing in the following situations:
• The patient with open wounds or other conditions requiring gloves, which may blunt palpation skills.
• The patient who must be evaluated under difficult conditions, such as the patient in an intensive care unit with multiple tubes and monitors, the patient in traction, the patient in whom turning is contraindicated, the patient on a ventilator, and the patient in restraints.
The novice muscle tester must avoid the temptation to use shortcuts or “tricks of the trade” before mastering the basic procedures lest such shortcuts become an inexact personal standard. One such pitfall for the novice tester is to inaccurately assign a muscle grade from one test position that the patient could not perform successfully to a lower grade without actually testing in the position required for the lower grade.
For example, when testing trunk flexion, a patient partially clears the scapula from the surface with the hands clasped behind the head (the position for the Grade 5 test). The temptation may exist to assign a grade of 4 to this test, but this may “overrate” the true strength of trunk flexion unless the patient is actually tested with the arms across the chest to confirm Grade 4.
The good clinician never ignores a patient’s comments and must be a good listener, not just to questions but also to the words the patient uses and their meaning. This quality is the first essential of good communication and the means of encouraging understanding and respect between therapist and patient. The patient is the best guide to a successful muscle test.
Population Variation: Most of the research that reports muscle testing results is the result of studies done on normal adults, and on specific subpopulations such as athletes, sedentary persons, and the elderly. Children remain in their own category. With this wide variation, it is necessary to modify grading procedures but not testing technique. Some also believe that the assigned grade should be consistent with those used with the normal adult population standards, but this requires innate understanding that an 80-year-old woman will be further down the grade scale than a 30-year-old woman or that a husky football player may be “off the scale” in contrast to the nonathletic white-collar worker. A grade of 4 will be very different in a child of 10 years versus a teen of 18 years. Chapter 6 provides a different testing procedure for children before they reach school age.
Some muscles, such as the muscles of the face and head, cannot be evaluated by these standard methods; these are included with a different scale and criteria in Chapter 7.
Validity and Reliability from the Literature: Manual muscle testing is well embedded as a testing device in physical therapy, having first appeared during the poliomyelitis epidemic in New England before World War I. (See Brief History of Muscle Testing in Introduction.) Credit for development of the early procedures belongs primarily to Wilhelmine Wright3 (today she would be called a physical therapist), who worked with orthopedic surgeon Robert Lovett.4,5 The techniques she used to evaluate muscles are not radically different now, though they are refined and extended.
The first statistical measures systematically applied to manual muscle testing did not occur until after World War II when they were used to evaluate the presence and severity of paralytic poliomyelitis.6,7 The seminal gamma globulin field trials were conducted in 1952, followed by more elaborate field trials in 1955 and 1956 when controlled trials were used before and after Salk vaccine administration.8,9 These evaluations of the subjective manual muscle test results were quite positive and showed that they did, indeed, test muscular strength and torque (validity). The muscles that showed “weakness” were compared with functional tests (such as walking) of those muscles, though the correlation was much lower. These tests were done before the availability of instrumented dynamometers, but the validity was good enough to continue manual testing for almost 90 years after such testing began.
The analysis of the effectiveness of gamma globulin was planned and conducted in 1952.8 The test was modified for the 1953 gamma globulin trials in which muscles were grouped slightly differently. The muscles innervated by the cranial nerves were not overlooked because Gonnella described their involvement, albeit with somewhat different techniques.10
The results of these preliminary tests were impressive but did show the importance of using examiners who were experienced, as well as the importance of training examiners for the procedure to be used (standardization). The results revealed minor differences between experienced examiners, and wide variance between the new and experienced therapists. Many studies have followed the polio era ones, and in general, validity is high while reliability shows greater differences.11–16
Because manual muscle testing is subjective, the conventional acceptability for reliability is that among examiners and in successive tests with the same examiner, the results should be within one half of a grade (or within a plus or minus of the base grade).16 Others maintain that within the same grade is acceptable, pluses and minuses notwithstanding.17
Reliability is increased by adhering to the same procedure for each test (for one or several examiners), by providing clear instructions to the subject, and by having a quiet and comfortable environment for the test.
Some studies after the poliomyelitis years reported muscular strength grades as congruent 50 percent of the time; grades were within a plus or minus of the base grade 66 percent of the time; and 90 percent of the time they were identical within a full testing grade.12,13,15,19 These results were obtained with grouped data; between examiners, the agreement of grade assigned declined sharply.22–24
In muscles with grades below 3 (Fair) reliability declines.12,15,22,23 Other studies pointed out that differences in technique could account for their low reliability.22,23 The Grade 4 (Good) muscle presents considerable variance because Grade 4 can be so broad and can be interpreted differently by different examiners: in small muscle groups the relative strength of the examiner may not be capable of accurate discrimination between lumbricals and wrist flexors or extensors (e.g., a small female examiner testing the arm flexors of a large injured football lineman).
As stated earlier, reliability is affected by the experience of the examiners as was shown in the trials during the 1950s. In both the gamma globulin and the polio trials, the examiners all were experienced and also trained by the same instructors for the specific tests to be used in the trials.8,9 Because 38 physical therapists and a small number of physicians and nurses per-formed the muscle examinations across the country, reproducibility among examiners was a critical factor. This was indeed a definitive factor in the tests that proved the efficacy of the Salk vaccine.
When the instructors and trainees were compared in a variety of combinations, they agreed within a plus or minus grade 95 percent of the time and agreed completely 70 percent of the time. Blair reported similar results in 1957 after the Salk vaccine trials.9 In the same chronological period, Williams reported that two examiners agreed on the manual muscle testing grade 60 to 75 percent of the time.13 Iddings et al., in the early 1960s, reported intertester and intratester scores to be in agreement in 48 percent of tests and within a plus or minus in 91 percent of the tests.11 Surprisingly, in the Iddings study the test procedures used by the examiners were not homogeneous.
In later years (1980s and 1990s), investigators used statistical analyses to interpret data in studies that looked at examiner experience; comparison between test procedures and their standardization; influence of muscle weakness (e.g., Good tests and those below Fair) on the grade assigned; and the reliability of intertester versus intratester performance. In most testing, reliability was acceptable for these subjective tests.20–24
The issue of reliability of manual muscle testing has not disappeared, but neither has manual testing been replaced by instrumented dynamometers, which have their own issues that await resolution. More work is needed to assess the problems found in testing at the Grade 4 (Good) level and in solving the conundrums in grades below 3 (Fair). Examiners, especially novices, must be cautious about their test procedures and make vigorous attempts to standardize their methods.
Despite the multiple issues and problems with manual muscle testing, both reliability and validity are satisfactory for clinical use and can never be “perfect” because of the subjectivity of the measures.
Influence of the Patient on the Test: The intrusion of a living, breathing, feeling person into the neat test package may distort scoring for the unwary examiner. The following circumstances should be recognized:
• There may be variation in the assessment of the true effort expended by a patient in a given test (reflecting the patient’s desire to do well or to seem more impaired than is actually the case).
• The patient’s willingness to endure discomfort or pain may vary (e.g., the stoic, the complainer, the high competitor).
• The patient’s ability to understand the test requirements may be limited in some cases because of comprehension and language barriers.
• The motor skills required for the test may be beyond some patients, making it impossible for them to perform as requested.
• Lassitude and depression may cause the patient to be indifferent to the test and the examiner.
• Cultural, social, and gender issues may be associated with palpation and exposure of a body part for testing.
• The size and noncomparability between big and small muscles can cause considerable differences in grading, though not an individual variation (e.g., the gluteus medius versus a finger extensor). There is a huge variability in maximum torque between such muscles, and the examiner must use care not to assign a grade that is not consistent with muscle size and architecture.
CRITERIA FOR ASSIGNING A MUSCLE TEST GRADE
The grade given on a manual muscle test comprises both subjective and objective factors. Subjective factors include the examiner’s impression of the amount of resistance to give before the actual test and then the amount of resistance the patient actually tolerates during the test. Objective factors include the ability of the patient to complete a full range of motion or to hold the position once placed there, the ability to move the part against gravity, or an inability to move a part at all. All these factors require clinical judgment, which makes manual muscle testing an exquisite skill that requires considerable experience to master. An accurate test grade is important not only to establish a functional diagnosis but also to assess the patient’s longitudinal progress during the period of recovery and treatment.
The Grade 5 (Normal) Muscle: The wide range of “normal” muscle performance leads to a considerable underestimation of a muscle’s capability. If the examiner has no experience in examining persons who are free of disease or injury, it is unlikely that there will be any realistic judgment of what is Normal and how much normality can vary. Generally, a physical therapy student learns manual muscle testing by practicing on classmates, but this provides only minimal experience compared to what is needed to master the skill. It should be recognized, for example, that the average physical therapist cannot “break” knee extension in a reasonably fit young man, even by doing a handstand on his leg! This and similar observations were derived by objective comparisons of movement performance acquired by assessing the amount of resistance given and then testing the muscle group’s maximal capacity on an electronic dynamometer.15,28–30
The examiner should test normal muscles at every opportunity, especially when testing the contralateral limb in a patient with a unilateral problem. In almost every instance when the examiner cannot break the patient’s hold position, a grade of 5 (Normal) is assigned. This value must be accompanied by the ability to complete a full range of motion or maintain end-point range against maximal resistance.
The Grade 4 (Good) Muscle: The grade of 4 (Good) represents the true weakness in manual muscle testing procedures (pun intended). Sharrard counted alpha motor neurons in the spinal cords of poliomyelitis victims at the time of autopsy.27 He correlated the manual muscle test grades in the patient’s chart with the number of motor neurons remaining in the anterior horns. His data revealed that more than 50 percent of the pool of motor neurons to a muscle group were gone when the muscle test result had been recorded as Grade 4 (Good). Thus when the muscle can withstand considerable but less than “normal” resistance, it has already been deprived of at least half of its innervation.
Grade 4 is used to designate a muscle group that is able to complete a full range of motion against gravity and can tolerate strong resistance without breaking the test position. The Grade 4 muscle “gives” or “yields” to some extent at the end of its range with maximal resistance. When maximal resistance clearly results in a break, the muscle is assigned a grade of 4 (Good).
The Grade 3 (Fair) Muscle: The Grade 3 muscle test is based on an objective measure. The muscle or muscle group can complete a full range of motion against only the resistance of gravity. If a tested muscle can move through the full range against gravity but additional resistance, however mild, causes the motion to break, the muscle is assigned a grade of 3 (Fair).
Sharrard cited a residual autopsy motor neuron count of 15 percent in polio-paretic muscles that had been assessed as Grade 3, meaning that 85 percent of the innervating neurons had been destroyed.27
Direct force measurements have demonstrated that the force level of the Grade 3 muscle usually is low, so that a much greater span of functional loss exists between Grades 3 and 5 than between Grades 3 and 1. Beasley, in a study of children ages 10 to 12 years, reported the Grade 3 (Fair) in 36 muscle tests as no greater than 40 percent of normal (one motion), the rest being 30 percent or below a normal “strength” and the majority falling between 5 and 20 percent of a rated normal.26 A grade of 3 (Fair) may be said to represent a definite functional threshold for each movement tested, indicating that the muscle or muscles can achieve the minimal task of moving the part upward against gravity through its range of motion. Although this ability is significant for the upper extremity, it falls far short of the functional requirements of many lower extremity muscles used in walking, particularly such groups as the hip abductors and the plantar flexors. The examiner must be sure that muscles given a grade of 3 are not in the joint “locked” position during the test (e.g., locked elbow when testing elbow extension).
The Grade 2 (Poor) Muscle: The Grade 2 (Poor) muscle is one that can complete the full range of motion in a position that minimizes the force of gravity. This position often is described as the horizontal plane of motion.
The Grade 1 (Trace) Muscle: The Grade 1 (Trace) muscle means that the examiner can detect visually or by palpation some contractile activity in one or more of the muscles that participate in the movement being tested (provided that the muscle is superficial enough to be palpated). The examiner also may be able to see or feel a tendon pop up or tense as the patient tries to perform the movement. There is, however, no movement of the part as a result of this minimal contractile activity.
A Grade 1 muscle can be detected with the patient in almost any position. When a Grade 1 muscle is suspected, the examiner should passively move the part into the test position and ask the patient to hold the position and then relax; this will enable the examiner to palpate the muscle or tendon, or both, during the patient’s attempts to contract the muscle and also during relaxation.
The Grade 0 (Zero) Muscle: The Grade 0 (Zero) muscle is completely quiescent on palpation or visual inspection.
Plus (+) and Minus (–) Grades: Use of a plus (+) or minus (–) addition to a manual muscle test grade is discouraged except in three instances: Fair+, Poor-, and Poor–. Scalable gradations in other instances can be described in documentation as improved or deteriorated within a given test grade (such as Grade 4) without resorting to the use of plus or minus labels. The purpose of avoiding the use of plus or minus signs is to restrict the variety of manual muscle test grades to those that are meaningful and defendable.
The Grade 3+ (Fair+) Muscle: The Grade 3+ muscle can complete a full range of motion against gravity, and the patient can hold the end position against mild resistance. There are functional implications associated with this grade.
For example, the patient with weak wrist extensors at Grade 3 cannot use a wrist-hand orthosis (WHO) effectively, but a patient with a Grade 3+ muscle can use such a device. Likewise, the patient with only Grade 3 ankle dorsiflexion cannot use a shoe-insert type of ankle-foot orthosis functionally. The patient with Grade 3+ dorsiflexors can tolerate the added weight of the brace, which is comparable to the mild resistance used in the test.
The plus addition to Grade 3 is considered by many clinicians to represent not just strength but the additional endurance that is lacking in a simple Grade 3 muscle.
The Grade 2+ (Poor+) Muscle: The Grade 2+ is given when assessing the strength of the plantar flexors when either of the following two conditions exist. The first is when the patient, while weight bearing, can complete a partial heel rise using correct form (see test for plantar flexion). The second condition is when the test is performed non–weight bearing and the patient takes maximum resistance and completes the full available range. The 2+ Grade is clearly distinguished from Grade 2, which indicates that full range is completed with no resistance. A grade of 3 or better can be given to the plantar flexors only when the patient is weight bearing.
The Grade 2– (Poor–) Muscle: The Grade 2– (Poor–) muscle can complete partial range of motion in the horizontal plane, the gravityminimized position. The difference between Grade 2 and Grade 1 muscles represents such a broad functional difference that a minus sign is important in assessing even minor improvements in return of function. For example, the patient with infectious neuronitis (Landry-Guillain-Barré syndrome) who moves from muscle Grade 1 to Grade 2– demonstrates a quantum leap forward in terms of recovery and prognosis.
Available Range of Motion: When any condition limits joint range of motion, the patient can perform only within the range available. In this circumstance, the available range is the full range of motion for that patient at that time, even though it is not “normal.” This is the range used to assign a muscle testing grade.
For example, the normal knee extension range is 135° to 0°. A patient with a 20° knee flexion contracture is tested for knee extension strength. This patient’s maximal range into extension is −20°. If this range (in sitting) can be completed with maximal resistance, the grade assigned would be a 5 (Normal). If the patient cannot complete that range, the grade assigned MUST be less than 3 (Fair). The patient then should be repositioned in the side-lying position to ascertain the correct grade.
SCREENING TESTS
In the interests of time and cost-efficient care, it is rare-ly necessary to perform a muscle test for the entire body. Two exceptions among several are patients with Landry-Guillain-Barré syndrome and those with incomplete spinal cord injuries. To screen for areas that need definitive testing, the examiner can use a number of maneuvers to rule out parts that do not need testing. Observation of the patient before the examination will provide valuable clues to muscular weakness and performance deficits. For example, the examiner can do the following:
• Watch the patient as he or she enters the treatment area to detect gross abnormalities of gait.
• Watch the patient sit and rise from a chair, fill out admission or history forms, or remove street clothing.
• Ask the seemingly normal patient to walk on the toes and then on the heels.
PREPARING FOR THE MUSCLE TEST
The examiner and the patient must work in harmony if the test session is to be successful. This means that some basic principles and inviolable procedures should be second nature to the examiner.
1. The patient should be as free as possible from discomfort or pain for the duration of each test. It may be necessary to allow some patients to move or be positioned differently between tests.
2. The environment for testing should be quiet and nondistracting. The temperature should be comfortable for the partially disrobed subject.
3. The plinth or mat table for testing must be firm to help stabilize the part being tested. The ideal is a hard surface, minimally padded or not padded at all. The hard surface will not allow the trunk or limbs to “sink in.” Friction of the surface material should be kept to a minimum. When the patient is reasonably mobile a plinth is fine, but its width should not be so narrow that the patient is terrified of falling or sliding off. When the patient is severely paretic, a mat table is the more practical choice. The height of the table should be adjustable to allow the examiner to use proper leverage and body mechanics.
4. Patient position should be carefully organized so that position changes in a test sequence are minimized. The patient’s position must permit adequate stabilization of the part or parts being tested by virtue of body weight or with help provided by the examiner.
5. All materials needed for the test must be at hand. This is particularly important when the patient is anxious for any reason or is too weak to be safely left unattended.
Materials needed include the following:
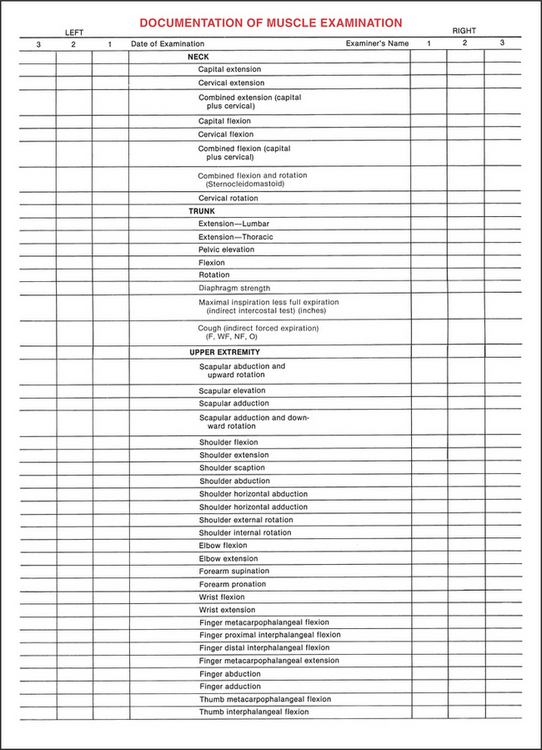
• Muscle test documentation forms (Figure 1-1)
• Pen, pencil, or computer terminal
• Pillows, towels, pads, and wedges for positioning
• Sheets or other draping linen
• Assistance for turning, moving, or stabilizing the patient
REFERENCES
1. LeVeau, B. Williams and Lissner’s Biomechanics of Human Motion, 3rd ed. Philadelphia: WB Saunders, 1992.
2. Soderberg, GL. Kinesiology: Application to Pathological Motion. Baltimore: Williams & Wilkins, 1997.
3. Wright, WG. Muscle training in the treatment of infantile paralysis. Boston Med Surg J. 1912;167:567–574.
4. Wright, WG. Muscle Function. New York: Hoeber, 1928.
5. Lovett, RW. Treatment of Infantile Paralysis, 2nd ed. Philadelphia: Blakiston’s, 1917.
6. Lovett, RW, Martin, EG. Certain aspects of infantile paralysis and a description of a method of muscle testing. JAMA. 1916;66:729–733.
7. Martin, EG, Lovett, RW. A method of testing muscular strength in infantile paralysis. JAMA. 1915;65:1512–1513.
8. Lilienfeld, AM, Jacobs, M, Willis, M. Study of the reproducibility of muscle testing and certain other aspects of muscle scoring. Phys Ther Rev. 1954;34:279–289.
9. Blair, L. Role of the physical therapist in the evaluation studies of the poliomyelitis vaccine field trials. Phys Ther Rev. 1957;37:437–447.
10. Gonnella, C, Harmon, G, Jacobs, M. The role of the physical therapist in the gamma globulin poliomyelitis prevention study. Phys Ther Rev. 1953;33:337–345.
11. Iddings, DM, Smith, LK, Spencer, WA. Muscle testing. Part 2. Reliability in clinical use. Phys Ther Rev. 1961;41:249–256.
12. Wintz, M. Variations in current manual muscle testing. Phys Ther Rev. 1959;39:466–475.
13. Williams, M. Manual muscle testing: Development and current use. Phys Ther Rev. 1956;36:797–805.
14. Beasley, WC. Influence of method on estimates of normal knee extensor force among normal and post-polio children. Phys Ther Rev. 1956;36:21–41.
15. Beasley, WC. Quantitative muscle testing: Principles and application to research and clinical services. Arch Phys Med Rehabil. 1961;42:398–425.
16. Lamb, R. Manual muscle testing. In: Rothstein JM, ed. Measurement in Physical Therapy. New York: Churchill-Livingstone, 1985.
17. Palmer, ML, Epler, ME. Fundamentals of Musculoskeletal Assessment Techniques, 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1998.
19. Daniels, L, Williams, M, Worthingham, CA. Muscle Testing: Techniques of Manual Examination, 5th ed. Philadelphia: WB Saunders, 1986.
20. Zimny, N, Kirk, C. A comparison of methods of manual muscle testing. Clin Manage Phys Ther. 1987;7:6–11.
21. Brandsma, JW, Schreuders, TAR, Birke, JA, et al. Manual muscle strength testing: Intraobserver and interobserver reliabilities for the intrinsic muscles of the hand. J Hand Ther. 1995;8:185–190.
22. Florence, JM, Pandya, S, King, WM, et al. Intrarater reliability of manual muscle test (Medical Research Council Scale) grades in Duchenne’s muscular dystrophy. Phys Ther. 1992;72:115–126.
23. Frese, F, Brown, M, Norton, BJ. Clinical reliability of manual muscle testing: Middle trapezius and gluteus medius muscles. Phys Ther. 1987;67:1072–1076.
24. Keyweg, RP, Van Der Meche, FGA, Schmitz, PIM. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome. Muscle Nerve. 1991;14:1103–1109.
26. Beasley WC. Normal and fair muscle systems: Quantitative standards for children 10 to 12 years of age. Presented at 39th Scientific Session of the American Congress of Rehabilitative Medicine, Cleveland, August 1961.
27. Sharrard, WJW. Muscle recovery in poliomyelitis. J Bone Joint Surg Br. 1955;37:63–69.
28. Williams, M, Stutzman, L. Strength variation through the range of motion. Phys Ther Rev. 1959;39:145–152.
29. Bohannon, RW. Test retest reliability of hand held dynamometry during single session of strength assessment. Phys Ther. 1986;66:206–209.
30. Bohannon, RW. Manual muscle test scores and dynamometer test scores of knee extension strength. Arch Phys Med Rehabil. 1986;67:390–392.
Bohannon, RW. Internal consistency of manual muscle testing scores. Percep Mot Skills. 1997;85:736–738.
Bohannon, RW. Measuring knee extensor muscle strength. Am J Phys Med Rehabil. 2001;80:13–18.
Bohannon, RW. Manual muscle testing: Does it meet the standards of an adequate screening test? Clin Rehabil. 2005;19:662–667.
Dvir, Z. Grade 4 in manual muscle testing: The problem with submaximal strength assessement. Clin Rehabil. 1997;11:36–41.
Great Lakes ALS Study Group. A comparison of muscle strength testing techniques in amyotrophic lateral sclerosis. Neurology. 2003;61:1503–1507.
Herbison, GJ, Issac, Z, Cohen, ME, et al. Strength post–spinal cord injury: Myometer vs manual muscle test. Spinal Cord. 1996;34:543–548.
Jepsen, J, Lawson, L, Larsen, A, Hagert, CG. Manual strength testing in 14 upper limb muscles: A study of inter-rater reliability. Acta Orthop Scand. 2004;75:442–448.
Li, RC, Jasiewicz, JM, Middleton, J, Condie, P, Barriskill, A, Hebnes, H, Purcell, B. The development, validity, and reliability of a manual muscle testing device with integrated limb position sensors. Arch Phys Med Rehabil. 2006;87:411–417.
Mulroy, SJ, Lassen, KD, Chambers, SH, Perry, J. The ability of male and female clinicians to effectively test knee extension strength using manual muscle testing. J Orthop Sports Phys Ther. 1997;26:192–199.
Perry, J, Weiss, WB, Burnfield, JM, Gronly, JK. The supine hip extensor manual muscle test: A reliability and validity study. Arch Phys Med Rehabil. 2004;85:1345–1350.
Phillips, BA, Lo, SK, Mastaglia, FL. Muscle force using “break” testing with a hand-held myometer in normal subjects aged 20 to 69 years. Arch Phys Med Rehabil. 2000;81:653–661.
Schwartz, S, Cohen, ME, Herbison, GJ, et al. Relationship between two measures of upper extremity strength: Manual muscle test compared to hand-held myometry. Arch Phys Med Rehabil. 1992;73:1063–1068.