Chapter 11 Imaging Abdominal Vascular Catastrophes
Abdominal vascular conditions demand special attention in diagnosis. First, despite highly variable presentations, they must be suspected by the clinician so that appropriate imaging can be performed. Routine abdominal imaging without vascular contrast agents can be normal in the presence of these life-threatening processes. Second, diagnostic imaging must be performed without delay, because these conditions are time sensitive and often fatal. Unfortunately, in many cases, the optimal test cannot be performed because of the patient’s hemodynamic condition, renal insufficiency, or contrast allergy. Even when the best available tests are performed, the sensitivity of diagnostic imaging for some key conditions is not perfect, so the emergency physician must remain vigilant for the possibility of a false-negative test result. We begin by defining the disease conditions and then briefly discuss their epidemiology and presentation. Although no formal clinical decision rules exist for these conditions, some risk stratification strategies can improve patient selection for diagnostic imaging. We also discuss the sensitivity and specificity of available imaging tests and interpretation of imaging findings.
Abdominal Vascular Catastrophes
Abdominal vascular catastrophes constitute a family of disorders sharing some key features but differing in details. Overall, these conditions primarily affect older patients, although rarely young patients with no apparent medical problems may be afflicted. Therefore vascular causes should always be considered in patients presenting with acute abdominal pain. According to Centers for Disease Control data, abdominal vascular diseases become an important cause of death by around age 50, with aortic aneurysm and dissection accounting for more than 13,000 U.S. deaths in 2006.1 Mesenteric ischemia may be more common than epidemiologic data suggest, because it may be misdiagnosed and may be a cause of death in elderly patients not undergoing premortem definitive diagnostic testing or autopsy. Here, we define each of these disease states, pointing out risk factors as well as some common misconceptions about the presentation that may prevent timely recognition.
General Approach to the Patient With Potential Abdominal Vascular Catastrophe
The clinical presentations of abdominal aortic aneurysm (AAA) rupture, abdominal aortic dissection, and mesenteric ischemia can overlap substantially, and a unified imaging approach to evaluate for all is best when any of the three is suspected. General resuscitation measures, preoperative preparation, and surgical consultation should occur simultaneously with imaging. Because perforation of a viscus with pneumoperitoneum can present with sudden abdominal pain simulating vascular catastrophes, an upright portable chest x-ray is a reasonable bedside screening examination (Figure 11-1, and CT for comparison Figure 11-2), although it provides no specific information about abdominal vascular disorders. Other plain radiographs should be minimized, because these provide little diagnostic information and can waste precious time. Rarely, frank pneumatosis intestinalis may be seen on plain radiographs (Figure 11-3), but more often x-rays may provide false reassurance or misdiagnosis of a more benign abdominal condition. Bedside imaging with ultrasound by the emergency physician to assess for AAA should occur at the time of initial physical examination (Figures 11-4 to 11-11). If AAA is not recognized by ultrasound, rapid computed tomography (CT) without oral contrast should be obtained in the stable patient. Intravenous (IV) contrast should be used when possible, as explained later. The presentation of vascular catastrophes can also overlap considerably with other important abdominal conditions, which are discussed in Chapter 9. Fortunately, CT without oral contrast provides substantial information about many other abdominal conditions.
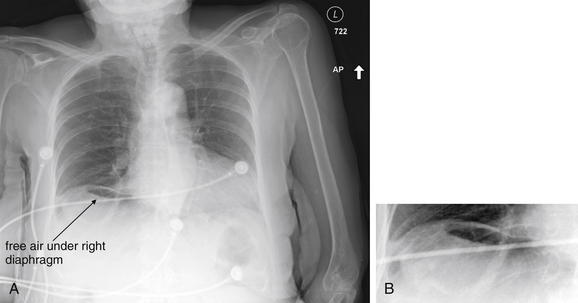
Figure 11-1 Pneumoperitoneum: X-ray.
A, AP upright chest x-ray. B, Close-up from A. This 88-year-old female presented with sudden onset of severe abdominal pain, diaphoresis, and nausea. A wide differential diagnosis, including cardiac ischemia and abdominal catastrophes such as mesenteric ischemia, was considered. Ironically, the chest x-ray shows free air, but the patient had already been transported for computed tomography (CT) before the chest image was visible on the picture archiving and communication system. When abdominal vascular catastrophes are considered, an upright chest x-ray is a reasonable bedside examination for the competing diagnosis of intestinal perforation, particularly in an unstable patient. Unless the patient is too unstable for CT, other plain films should generally be avoided, because they are insensitive and nonspecific and can waste precious time. Plain x-ray can be avoided entirely, because CT has the advantage of simultaneously assessing for vascular catastrophes and a multitude of other causes of abdominal pain, including free air. Compare the above x-ray with CT in Figure 11-2.
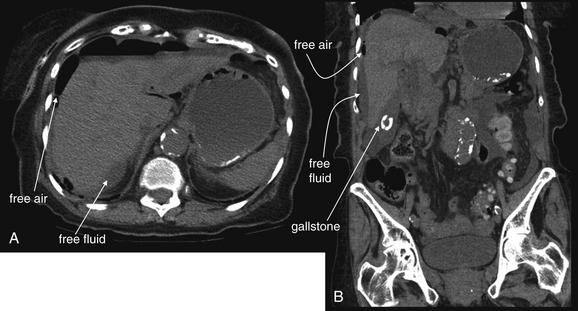
Figure 11-2 Pneumoperitoneum: CT without contrast.
Same patient as Figure 11-1.
The chest x-ray in Figure 11-1 showed free air, but the patient had already been transported for CT before the chest image was visible on the picture archiving and communication system (PACS). In the operating room, the patient was found to have a perforated duodenal ulcer.
A, Axial image on soft-tissue window shows free air (black) outlining the liver. Free fluid (gray) is also visible. B, A coronal view shows similar findings. An incidental gallstone is also seen.
Many forms of pathology can be detected without oral contrast, as described in Chapter 9.
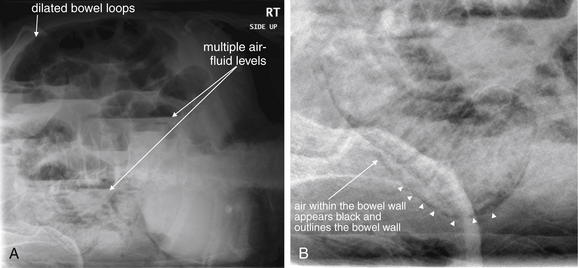
Figure 11-3 Mesenteric ischemia with pneumatosis: X-ray.
This 77-year-old male presented with abdominal distension and vomiting, along with aching abdominal pain, for 2 days. He was suspected of having bowel obstruction, and plain films were obtained. His initial white blood cell count was 8.6, with normal bicarbonate and no anion gap. Minutes after this x-ray, he arrested in the emergency department and could not be resuscitated.
A, Left lateral decubitus abdominal x-ray shows multiple air–fluid levels and dilated bowel loops, suggesting small-bowel obstruction. B, A closer look reveals mural pneumatosis. This patient may have had a closed loop obstruction leading to bowel ischemia or diffuse ischemia leading to ileus. Unfortunately, x-ray findings such as these occur after frank bowel necrosis, making them insensitive for early ischemia when intervention may be most beneficial. X-rays should generally not be obtained when bowel ischemia is suspected, because x-rays can be falsely reassuring and can waste precious time. Computed tomography with intravenous contrast is usually more definitive and should be performed as soon as possible. Delay for oral contrast is unnecessary and should be avoided when ischemic bowel is suspected.
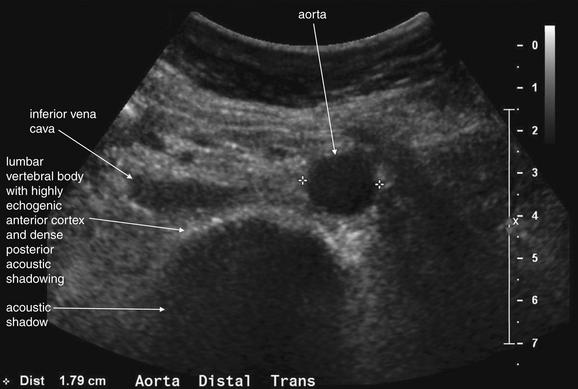
Figure 11-4 Normal aorta: Ultrasound.
Bedside ultrasound in the hands of emergency physicians has been shown to be sensitive for the presence of abdominal aortic aneurysm. Ultrasound is considered poorly sensitive for rupture. In the presence of symptoms suggestive of aortic rupture, identification of an aneurysm by bedside ultrasound should be acted upon as if diagnostic of rupture.
This ultrasound demonstrates a normal aorta, viewed in short-axis (transverse) cross section. The aorta should be examined in cross section from the xiphoid process to the umbilicus, the usual location of the aortic bifurcation to form the iliac arteries. The majority of aortic aneurysms are infrarenal, and this area should be examined in detail. If measurements are made only at the subxiphoid and umbilical levels, an aneurysm might be missed, because the aortic diameter may be quite normal proximal and distal to a sacular aneurysm.
Several features of the normal aorta should be recognized. First, the normal abdominal aorta lies just anterior and to the left side of the lumbar vertebral bodies. These are identified by their highly echogenic anterior surface (the bony cortex), which reflects sound waves and casts a dense posterior acoustic shadow. This should not be confused for an aortic aneurysm and is a reliable landmark for orientation. The normal aorta should be less than 3 cm in diameter and have a circular cross-sectional contour. The inferior vena cava (IVC) should lie just anterior to the lumbar vertebral bodies, on the right side. The IVC should be the same size or smaller than the aorta. Depending on the patient’s intravascular volume status, the IVC may be round or may have a flattened, elliptical shape. The IVC often varies in size and shape with respiration, but this should not be mistaken for the pulsatile aorta.
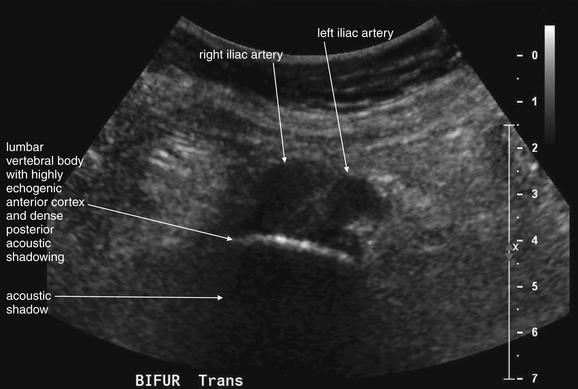
Figure 11-5 Normal ilioaortic bifurcation: Ultrasound.
Transverse (short axis) view. Around the level of the umbilicus, the aorta bifurcates to form the iliac arteries. Do not confuse these with the aorta and vena cava—a normal iliac artery diameter may occur with an aneurysm of the more proximal aorta. Be sure to examine the aorta from xiphoid process to the iliac bifurcation.

Figure 11-6 Normal abdominal aorta: Ultrasound.
Sagittal (long axis) view. Should the aorta be measured in long axis cross section? This is a standard measurement made by ultrasonographers, but be wary as an emergency ultrasonographer: this is a source of a potential pitfall. If the ultrasound probe slides to the patient’s right, the inferior vena cava (IVC), rather than the aorta, may be seen and measured. Though they do not look identical, the IVC might be mistaken for the aorta by a novice sonographer. Moreover, a long-axis view may not provide the maximal aortic diameter if the probe is positioned not in the midsagittal plane but, rather, slightly to the right or left of the midline diameter of the aorta. The diameter measured would then be a chord with a smaller length than the true diameter, underestimating the size of the aorta. See Figure 11-11 for an illustration.
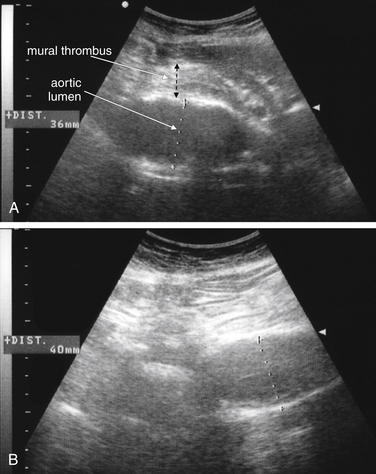
Figure 11-7 Large unruptured aortic aneurysm: Ultrasound.
In a patient suspected of ruptured abdominal aortic aneurysm, detection of an aortic aneurysm on ultrasound has a high correlation with rupture.
A, In this transverse (short-axis) image, the lumen of the aorta measures 36 mm, but the actual diameter is larger. Mural thrombus is visible, with a total aortic diameter of more than 50 mm.
B, A long-axis image, the patent lumen measures 40 mm, but care must be taken to look for mural thrombus.

Figure 11-8 Unruptured abdominal aortic aneurysm: Ultrasound.
A transverse view of the distal abdominal aorta. Again, adherent mural thrombus is present. This must be recognized to prevent undermeasurement of the aortic diameter.
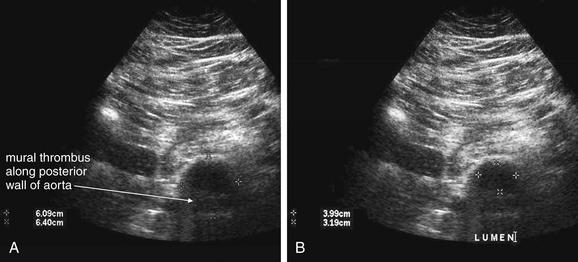
Figure 11-9 Abdominal aortic aneurysm (AAA): Ultrasound.
Ultrasound is sensitive for detection of AAA when the aorta can be visualized. An aneurysm is defined by a diameter 1.5 times the upper limit of normal. Because the normal aorta is 2 cm or less, any diameter exceeding 3 cm defines an aneurysm. As described in the earlier figure on ultrasound of the normal aorta, it is essential to examine the aorta in short-axis cross section from the xiphoid process to the iliac bifurcation, because an aneurysm may be present anywhere along this course and could be missed by measurements only at the subxiphoid and umbilical levels. This figure demonstrates another potential pitfall for the inexperienced emergency sonographer. Many aortic aneurysms have a mural thrombus that may eccentrically or concentrically surround the residual lumen. If the lumen alone is measured, it may appear to be of normal caliber, or smaller than the 5-cm size at which aneurysmal rupture becomes more likely. The complete diameter of the aorta, including both the residual lumen and the mural thrombus, must be measured to determine the true size of the aorta.
In this transverse view of the distal aorta, the aorta is 6 cm in diameter. A mural thrombus is present along the posterior wall of the aorta. The lumen measures between 3 and 4 cm. Although measurement of the lumen alone would allow recognition of aortic aneurysm, it would underestimate the size of the aorta. Look carefully for mural thrombus. A, Short-axis view. The full diameter, including the thrombus, is measured. B, Short-axis view. Only the lumen is measured, underestimating the aneurysm size.
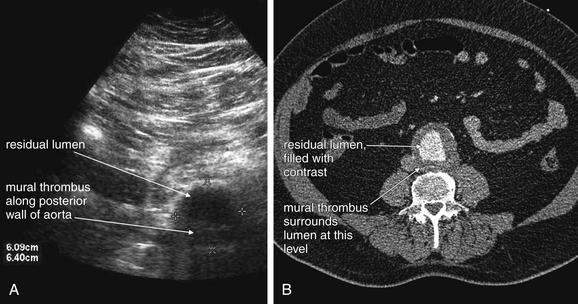
Figure 11-10 Abdominal aortic aneurysm: Ultrasound and CT with IV contrast, demonstrating mural thrombus.
This figure compares the ultrasound from Figure 11-9 (A) with the intravenous contrast–enhanced CT scan (B) performed in the same patient, which clearly demonstrates the eccentric mural thrombus. We explore CT findings in more detail in the next several figures.
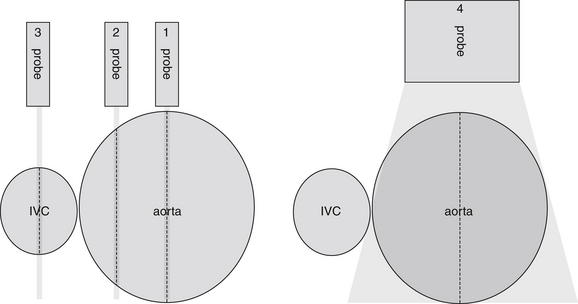
Figure 11-11 Abdominal aortic aneurysm: Ultrasound.
This diagram illustrates a pitfall of attempting to measure the aorta using a long-axis view. (1) If the ultrasound probe is positioned in the midline of the aorta in a sagittal plane, a true diameter will be measured, accurately indicating the maximum size of the aneurysm. (2) A probe moved to the patient’s right will measure a chord through the aorta, reflecting less than the maximum aortic diameter. (3) If the probe slides even farther to the right, the inferior vena cava (IVC) may be measured, giving a falsely reassuring value because the IVC is essentially always less than 3 cm in size. (4) Turning the probe 90 degrees to measure the aorta in short-axis cross section avoids this pitfall—though multiple cross sections from xiphoid process to the iliac bifurcation should be measured, because the aortic diameter may change drastically along its course.
Abdominal Aortic Aneurysm
AAA is defined as dilatation of the aorta to a size greater than 3 cm in the abdomen. Risk factors for AAA include advancing age, male gender, cigarette smoking, atherosclerotic disease, and family history of AAA.4 Diabetes, female gender, and black race are negatively associated with AAA.4 However, advancing age is the greatest risk factor, and no patient can be considered at no risk unless aortic imaging has been performed. Risk of acute aneurysm rupture increases with increasing aneurysm size, which correlates with increasing wall tension. Above a diameter of 5 cm in women and 6 cm in men, the risk of rupture dramatically increases.2-3 Lederle et al.3 reported the 1-year incidence of rupture was 9.4% for AAAs of 5.5 to 5.9 cm, 10.2% for AAAs of 6.0 to 6.9 cm, and 32.5% for AAAs 7 cm or greater. Brown et al.2 reported the rupture rate for aneurysms of 5.0 to 5.9 cm to be 1% per year in men and 3.9% per year in women. The rupture rate increased dramatically for both men and women with aneurysms of 6 cm or greater, reaching 14.1% and 22.3%, respectively. A rapid increase in the rate of aneurysm expansion also may predict rupture, although the mean difference in expansion rates between AAAs destined to rupture and those that do not rupture is small—an increase of less than 0.5 cm per year.2
The presentation of AAA rupture can be extremely variable. The classic presentation includes sudden abdominal and back pain, associated with hemodynamic collapse. This may be the most common presentation of AAA rupture, but the majority of patients who have AAA ruptures with immediate hemodynamic instability never reach an emergency physician’s care. Of those with AAA ruptures, 50% die before reaching a hospital,5 and the overall mortality is greater than 50%.6 In those patients surviving until hospital arrival, the clinical presentation is often more subtle. Fewer than half of those patients reaching the emergency department have the classic features of abdominal and back pain with hypotension.7 In one study of patients dying from AAA rupture, only 20% of patients presented with abdominal and back pain with hypotension.5 Hypotension with back or abdominal pain occurred in 60%.
Although a pulsatile abdominal mass is classically present, in several studies, the presence of a palpable pulsatile mass is unreliable. The sensitivity of abdominal palpation has been estimated from 15 studies of asymptomatic patients screened with ultrasound. For smaller AAAs, between 4.0 and 4.9 cm, the sensitivity of palpation is only around 50%, although these aneurysms have a low rate of rupture. The sensitivity of physical exam reaches 76% with an aortic diameter of 5 cm and greater, meaning that as many as one in four large AAAs in a size range at risk of acute rupture might be missed by palpation. The negative likelihood ratio for palpation in AAAs greater than 4.0 cm is only 0.51 with a 95% confidence interval (CI) of 0.38 to 0.67, making the absence of AAA by examination too unreliable for clinical use. The sensitivity of palpation is also compromised by increasing abdominal girth.8 The sensitivity of physical examination in the setting of acute rupture is not well studied. Marston et al.9 reported a pulsatile mass to be present in only about 60% of 152 patients with a ruptured AAA. In those patients who were initially misdiagnosed, only 26% had a pulsatile mass. It is possible that examination is even less sensitive once the AAA has ruptured. As a consequence, physical examination must never be used to rule out AAA rupture.
Historically, AAA rupture has been misdiagnosed initially in 30% to 60% of cases9-11 or diagnosed after substantial delay. Many patients present with surprising apparent hemodynamic stability and lack of anemia.10 Gaughan et al.11 found that initial hemodynamic stability was associated with delay in diagnosis, perhaps reflecting the supposition among physicians that AAA rupture would ubiquitously result in shock. Common alternative diagnoses in cases of actual ruptured AAAs include renal colic, urinary tract infection, spinal disease, diverticulitis, and gastrointestinal hemorrhage.9-12 Although these misdiagnoses may be less common today in an age of ubiquitous CT, the frequency of misdiagnosis in the past highlights the insensitivity of history and physical examination for the diagnosis. In one study of patients dying from AAA rupture within 2 hours of presentation, the median presenting systolic blood pressure was 110 mm Hg, the median presenting heart rate was 71 bpm, and the median presenting hemoglobin was 9.0 g/dL—all values that might be mistakenly interpreted as relatively reassuring.5 Remember that the median value is the 50th percentile, so half of patients had laboratory or vital sign values less ominous than those listed above. That these values occurred in patients who ultimately died within 2 hours of emergency department arrival emphasizes that seemingly reassuring vital signs and laboratory values offer little prognostic reassurance. This also stresses the urgency of rapid imaging, as diagnosis using CT with oral contrast can result in delays as great as 140 minutes.13 Although the time before diagnosis or death in some cases of AAA rupture can be greater than 24 hours, 12.5% of patients die within 2 hours of emergency department presentation without intervention.5 In any individual patient, the moment of hemodynamic collapse cannot be predicted, and all urgency should be taken in making the diagnosis. Patients who are hemodynamically unstable at the time of surgery have a higher 30-day mortality rate than those who are not, emphasizing the need to identify patients with AAA rupture before physiologic collapse.11
Imaging for Suspected Ruptured Abdominal Aortic Aneurysm
Because of the potential for rapid and sudden hemodynamic collapse, imaging for suspected AAA must be performed as rapidly as possible. Simultaneous with all diagnostic imaging should be patient resuscitation and surgical consultation. As we discuss in detail later, ultrasound is a sensitive modality for the presence of AAA, although it is insensitive for detecting aneurysm rupture.14 CT without any contrast, or with IV contrast if time allows, is usually definitive. X-rays play little role except in evaluating for other immediate surgical causes of abdominal pain such as free peritoneal air and should be avoided when possible to prevent dangerous delay.
Ultrasound for Abdominal Aortic Aneurysm
Ultrasound is considered highly sensitive for the detection of AAA. Multiple studies have investigated ultrasound in the hands of emergency physicians. In the context of acute abdominal pain, the presence of AAA on emergency physician–performed ultrasound has a very high positive predictive value, allowing rapid triage to operative care without further imaging.14-15 Ultrasound measurements of aortic diameter performed by emergency physicians correlate closely with measurements made using CT or MRI, differing by only around 4 mm.16-17 Knaut et al.17 reported that aortic measurements by emergency physicians closely estimated those from CT, differing by less than 1.5 cm at the superior mesenteric artery (SMA) and 1 cm at the aortic bifurcation in 95% of cases. Emergency physicians can perform the examination rapidly, in fewer than 5 minutes in most cases.17 The examination is simple to learn as well, with physicians becoming proficient after brief training.18 In one study of an abbreviated ultrasound examination performed in patients with suspected ruptured AAA, the sensitivity of ultrasound for detection of AAA is reported as 97%, with few indeterminate results in the hands of radiologists.14 Tayal et al.15 found that ultrasound performed by emergency physicians was 100% sensitive (95% CI = 89.5%-100%) with 98% specificity (95% CI = 92.8%-99.8%). In their study, 10 of 27 patients were taken to the operating room without further imaging following emergency physician ultrasound diagnosis of AAA.15 Costantino et al.16 similarly found that emergency medicine resident–performed ultrasound was 94% sensitive (95% CI = 86%-100%) and 100% specific (95% CI = 98%-100%).
The normal appearance of the aorta is simple to recognize on ultrasound (see Figures 11-4 to 11-6). The aorta occupies a uniform location anterior to the vertebral column, which serves as a reliable landmark. On transverse imaging, the aorta usually lies slightly left of the midline of the vertebral column. The inferior vena cava usually lies just to the patient’s right of the aorta. The anterior bony cortex of the vertebral body appears as a bright or highly echogenic curve, deep to the aorta. Deep to this curve, dense black acoustic shadowing occurs, making the remainder of the vertebral body invisible. Anticipation of this appearance of the vertebral body prevents mistaking the vertebral body for a large aortic aneurysm. The abdominal aorta should not exceed 2-3 cm. Aortic aneurysm is defined by a diameter exceeding 3 cm, although rupture is unlikely below 5 cm in women and 6 cm in men.2
Several pitfalls in the ultrasound evaluation of AAA should be considered. First, the reported sensitivity for AAA rupture is a stunning 4%, according to a single study published in Radiology in 1988.14 In this study, an abbreviated ultrasound examination was performed during the ongoing resuscitation of the patient, and only the periaortic region was examined for blood. Blood collecting in other abdominal areas such as Morison’s pouch might have been missed by the abbreviated exam. The retroperitoneum, where aortic hematoma might collect following a contained aortic rupture, is generally not well-evaluated with ultrasound. The sensitivity for AAA rupture today with modern ultrasound machines is unknown but must be assumed to be poor until proven otherwise. The second pitfall is undermeasurement of the aortic diameter because of the presence of circumferential mural thrombus (see Figures 11-7 to 11-10). Thrombus is common within aortic aneurysms and reduces the fluid-filled lumen visible on ultrasound. Although thrombus is usually visible on ultrasound, if it is not recognized, the fluid-filled channel may be measured without inclusion of the thrombus, underestimating the aneurysm size. A third pitfall is failure to image the abdominal aorta along its entire length from the xiphoid process to the umbilicus. Aortic aneurysms may occur anywhere along this length, although infrarenal aneurysms are most common. An additional pitfall is measuring the aorta in a longitudinal direction but failing to sample along the maximal diameter (see Figure 11-11). If a section of the aorta parallel to the long axis but not along the midpoint is measured instead, undermeasurement of the diameter may occur. Despite these concerns, in one study, longitudinal measurements correlated better with CT than did transverse measurements.19 Finally, failure to recognize a nondiagnostic ultrasound resulting from overlying bowel gas can result in a missed aneurysm.
Contrast-Enhanced Ultrasound
Several new studies suggest a possible solution to the poor sensitivity of ultrasound for the diagnosis of ruptured AAA. Contrast agents originally developed for echocardiography provide a means of visualizing both the aortic lumen and extravasation of blood. A variety of agents approved by the U.S. Food and Drug Administration are available. They shared a common feature of containing highly reflective microscopic bubbles that are extremely echogenic on ultrasound. Studies in the context of acute abdominal trauma and acute AAA rupture suggest improved sensitivity for extravasation of blood.20-21 Contrast agents can be injected at the bedside with a single hand bolus, followed by immediate performance of ultrasound. Catalano et al.22 reported the technique in the assessment of eight patients with ruptured AAA and visualized retroperitoneal hematoma and extravascular contrast leak in seven of the eight. The sensitivity has not been confirmed in larger series. Contrast-enhanced ultrasound has also been used to monitor aortic aneurysms for endoleak (discussed later in this chapter) following endovascular repair. In this setting, it has excellent sensitivity (100%) and specificity (93%) compared with multislice CT angiography. It outperforms color duplex ultrasound, which has a sensitivity of only 33.3% and specificity of 92.8%.23 Ultrasound contrast agents can be used in patients with renal insufficiency, severe iodinated contrast allergy, or hemodynamic instability preventing use of CT scan.
Computed Tomography for Ruptured Abdominal Aortic Aneurysm
CT scan without IV contrast can diagnose the presence of AAA and AAA rupture with high sensitivity and specificity (Figures 11-12 to 11-16).24-25 An AAA is defined by an aortic diameter 3 cm or greater, but ruptures are rare in aneurysms of this size. The aorta is readily identified as a circular structure in cross section, anterior to the spine. On unenhanced CT, high-density retroperitoneal hematoma can be seen in the perinephric retroperitoneal space, sometimes displacing the kidney anteriorly.26 Without IV contrast, blood shares the same density as the kidney and psoas muscle and can obscure the lower density fat plane that normally separates these two structures from one another and from the aorta. In addition, a high-attenuation crescent within the aortic wall or within mural thrombus predicts rupture.27-29 Without IV contrast, the crescent is considered to be “high attenuation” if its Hounsfield density exceeds that of unenhanced blood in the aortic lumen.28 If time allows, CT scan with IV contrast provides more anatomic definition to allow open surgical or endovascular intervention (Figures 11-17 and 11-18; see also Figures 11-13 and 11-14). IV contrast also identifies ongoing hemorrhage at the time of CT. Oral contrast should never be used when AAA rupture is suspected, because it introduces an unacceptably long delay before imaging.13
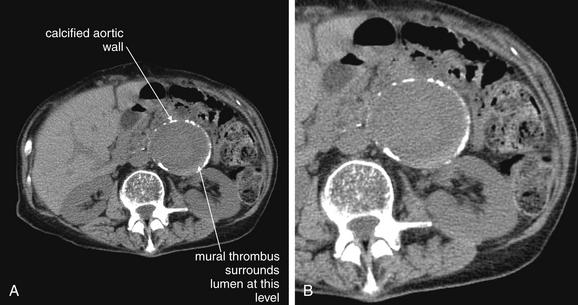
Figure 11-12 Unruptured abdominal aortic aneurysm (AAA): Noncontrast computed tomography (CT).
A, noncontrast CT viewed on soft-tissue windows, demonstrating a very large AAA. B, Close-up from A. Characteristic features include a calcified rim and adherent mural thrombus, which is faintly visible on this noncontrast CT as a crescent-shaped rim along the aortic wall. Intravenous (IV) contrast better delineates this in the next figure. This patient does not have an aortic rupture, although it is difficult to be certain of this viewing this noncontrast CT. Retroperitoneal fat (nearly black) bounds the aorta posteriorly and on the patient’s left, but the right and anterior margins of the aorta abut soft-tissue density, so a small amount of extraluminal bleeding could be missed on this scan. CT with IV contrast can evaluate for active bleeding, marked by contrast extravasation. In some cases, aortic rupture can be clearly identified on noncontrast CT. Examples of this are shown in Figures 11-15B and 11-16.
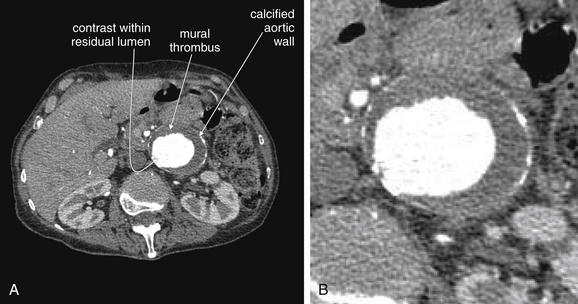
Figure 11-13 Unruptured abdominal aortic aneurysm: Computed tomography (CT) image enhanced by intravenous (IV) contrast.
A, An IV contrast–enhanced CT scan performed immediately after the noncontrast CT in the same patient as Figure 11-12. B, Close-up from A. Both A and B are viewed on soft-tissue windows. With the administration of IV contrast, the true lumen can be clearly differentiated from the adherent mural thrombus, which is nearly circumferential in this patient. Calcifications in the aortic wall are visible. The contrast remains bounded within the rounded aortic contour, ruling out active bleeding from rupture (which would demonstrate contrast extravasation outside of the aortic contour). Oral contrast is not needed for evaluation of the abdominal aorta.
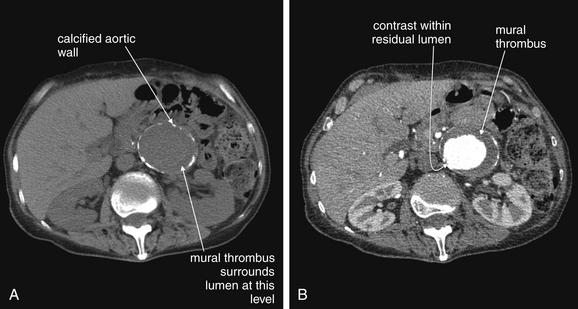
Figure 11-14 Unruptured abdominal aortic aneurysm (AAA): Comparison of noncontrast and intravenous (IV) contrast–enhanced computed tomography (CT).
Noncontrast (A) and IV contrast–enhanced (B) CT scans were performed in the same patient on the same day. These slices are through the same level and demonstrate the additional value of IV contrast in delineating the lumen and adherent mural thrombus, which is faintly visible on the noncontrast scan. This patient does not have active rupture, so contrast is not seen leaving the aorta. A, The presence of an AAA can be confirmed or ruled out without IV contrast. IV contrast assists in the detection of active hemorrhage.
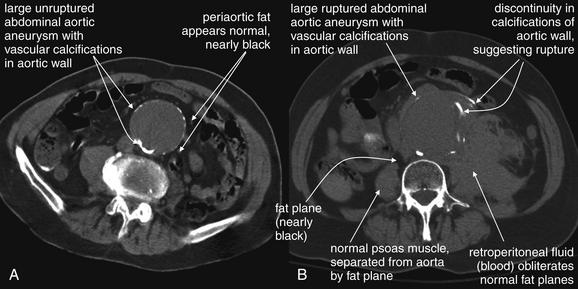
Figure 11-15 Unruptured and ruptured aortic aneurysms: CT without IV or oral contrast.
A, An unruptured but large abdominal aortic aneurysm (AAA), identified by CT without IV contrast. CT without any contrast allows accurate identification of an aortic aneurysm. By definition, an aneurysm has a diameter of 3 cm or greater, though rupture is relatively rare under 4-5 cm. Increasing size is accompanied by increased rupture risk. Typical features include wall calcifications. The surrounding fat should appear nearly black on CT soft-tissue windows. Without IV contrast, blood within the aorta is dark gray on CT soft-tissue windows.
B, A large ruptured AAA, identified on CT without IV contrast. Free peritoneal rupture has occurred, and blood is visible throughout the patient’s left abdomen. Blood without contrast appears gray on CT. In this case, the extravasating blood appears slightly hyperdense (brighter) relative to blood in the aorta, despite the absence of injected contrast. This is a well-described phenomenon in the radiology literature. Rupture of an aneurysm can be detected without any contrast. Blood in the retroperitoneum obscures normal fat planes, such as that separating the aorta and psoas muscle. A retroperitoneal hematoma may also displace the kidneys.
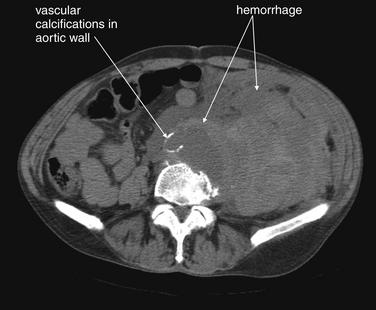
Figure 11-16 Ruptured aortic aneurysm: CT without intravenous or oral contrast.
Free peritoneal rupture has occurred, and blood is visible throughout the patient’s left abdomen.

Figure 11-17 Abdominal aortic aneurysm (AAA) rupture: CT with IV contrast.
A, Axial image. B, Coronal image. C, Sagittal image.
All images are viewed on CT soft-tissue windows. Administration of IV contrast allows recognition of active contrast extravasation—ongoing hemorrhage at the moment of CT. However, IV contrast is not generally needed for recognition of AAA rupture. In this patient, blood is seen throughout the abdomen and retroperitoneum. Blood that escaped from the aorta before the administration of IV contrast appears dark gray. Abdominal and retroperitoneal fat appears nearly black on CT soft-tissue windows. Injected contrast appears bright white. Adherent thrombus within the aorta appears dark gray, whereas white contrast material defines the patent lumen. Contrast outside of the aorta indicates active hemorrhage. Compare the patient’s right psoas muscle with the left. On the left, blood obscures the normal fat plane surrounding the psoas. The diagnosis of AAA rupture could have been made in this patient without any contrast. Multiplanar reconstructions with IV contrast are useful if the patient is sufficiently stable, because these allow sizing of endovascular grafts.
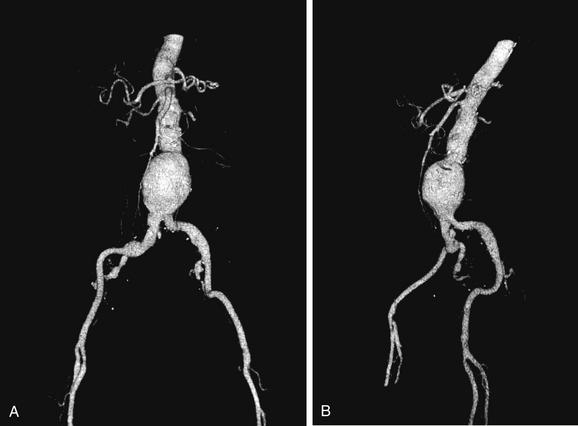
Figure 11-18 Abdominal aortic aneurysm (AAA): Three-dimensional CT reconstructions.
Three-dimensional reconstructions can be generated and rotated in space to visualize the aorta for preoperative planning. Measurements from these three-dimensional models and from two-dimensional axial, coronal, and sagittal plane reconstructions are used to size endovascular grafts. Three-dimensional modeling requires fine CT slice acquisition, around 1.25 mm per slice, for high-quality rendering. Multiple software packages allow three-dimensional modeling from standard CT datasets. Here, a sacular AAA is viewed from the front (A) and side (B).
Alternative Imaging Modalities for Abdominal Aortic Aneurysm Rupture
Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) can be used to diagnose AAA with excellent sensitivity and specificity, but the delay before imaging is unacceptably long in most institutions using this modality.30 Noncontrast CT should always be preferred over MRI, because it is highly sensitive and specific for AAA and AAA rupture. Catheter-based formal angiography can be used to diagnose AAA with or without rupture, although in most institutions this has been replaced by ultrasound or CT imaging for diagnostic purposes, as angiography is both time-consuming and invasive. Plain radiographs play virtually no role in the diagnosis of AAA and should be avoided whenever possible, because they may introduce unacceptable diagnostic delay. Rarely, the calcified outline of an aortic aneurysm may be seen on x-ray, but the sensitivity is unknown and plain x-ray should not be used for this diagnosis (Figure 11-19). An exception to this rule is in the unstable patient in whom a competing diagnosis such as perforation of a hollow viscus is being considered. In this case, an upright portable chest x-ray to assess for pneumoperitoneum can be rapidly performed (see Figure 11-1).
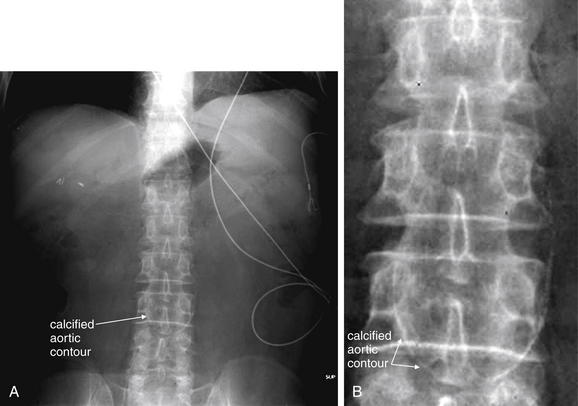
Figure 11-19 Abdominal aortic aneurysm (AAA): Plain radiograph.
X-rays should not be used to diagnose the presence of AAA, because the sensitivity is unknown and the ability to detect rupture is likely poor. Occasionally, x-ray obtained for other suspected diagnoses may reveal a calcified aortic contour. A, Supine abdominal x-ray. B, Close-up from A.
Angiography
Angiography is the historical gold standard for the diagnosis of AAA, aortic dissection, and mesenteric ischemia. Today, the wide availability of CT angiography has relegated catheter-based angiography to a purely therapeutic role following a diagnostic CT in most centers (discussed in more detail in Chapter 16). Angiography can be used for the treatment of even ruptured AAAs using endovascular stents.31 Because the stent must be sized carefully to prevent occlusion of branch vessels and to ensure that a leak does not occur at the margins of the stent, CT with IV contrast and multiplanar reconstructions is usually required (see Figures 11-17 and 11-18). Aortic dissection can also be diagnosed with angiography. Under angiographic guidance, stenting of dissections or fenestration of the intimal flap to restore blood flow to an occluded true lumen is sometimes used as a therapy. Angiography can be used to diagnose and treat mesenteric ischemia (see Figure 11-35 later in the chapter). Tissue plasminogen activator or similar thrombolytic agents can be infused through a catheter. Vascular stents can also be placed to restore blood flow. The urgency to restore bowel perfusion cannot be overemphasized. Surgical consultation should be performed even if interventional radiology is the intended initial therapeutic approach. Death from delay in reperfusion can occur; increased time to surgery is strongly associated with poor outcome.32
Imaging of Patients With Prior Endovascular Abdominal Aortic Aneurysm Repairs: Endoleaks
Following endovascular repair of AAAs, an endoleak may occur (Figures 11-20 and 11-21).33 An endoleak is defined as the continued flow of blood into the aneurysm sac. Endoleaks are graded as one of four types. Type 1 endoleaks occur immediately, at the time of placement of an endovascular graft, usually because of mis-sizing of the graft, such that the proximal or distal ends of the graft are not sealed against the aorta. This requires placement of a larger graft, because type 1 endoleak leaves the aneurysm sac subject to systemic vascular pressures with continued risk of acute rupture. Type 2 endoleaks result from retrograde flow of blood through collateral vessels into the aneurysm sac (see Figure 11-21). Common examples include filling of the aneurysm sac from lumbar perforating arteries. Type 2 endoleaks are often observed without treatment, because they do not subject the aneurysm sac to full systemic vascular pressures and are at relatively low risk of rupture. Type 2 endoleaks that do not resolve spontaneously can be treated with angiographic embolization. Type 3 endoleaks occur when a tear in the fabric of the graft occurs or if separation occurs between grafts consisting of multiple modules. This type of leak is relatively rare but leaves the aneurysm sac subject to systemic vascular pressures, requiring replacement of the graft because of continued risk of aneurysm rupture. Type 4 endoleaks occur from leaks through pores of the graft material and usually do not require repair.33
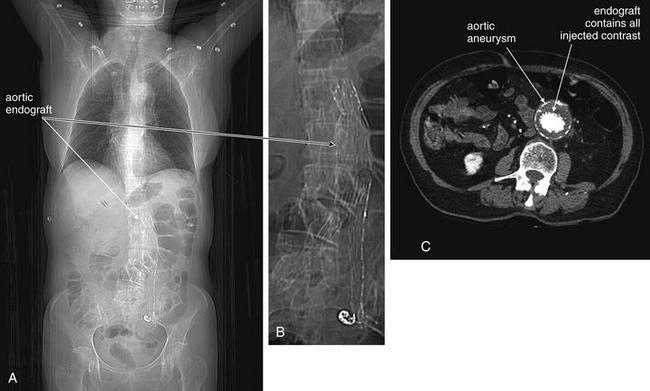
Figure 11-20 CT evaluation of patients with prior endovascular aortic aneurysm repair.
A, B, CT scout images showing the radiodense graft.
C, CT with intravenous (IV) contrast, showing contrast contained within the graft.
CT is useful for assessment of patients with prior endovascular aortic aneurysm repair. Although the graft material is visible without IV contrast, detection of a leak of blood within the aneurysm sac but outside of the graft material (an endoleak) requires IV contrast. Here, contrast appears contained within the graft material.
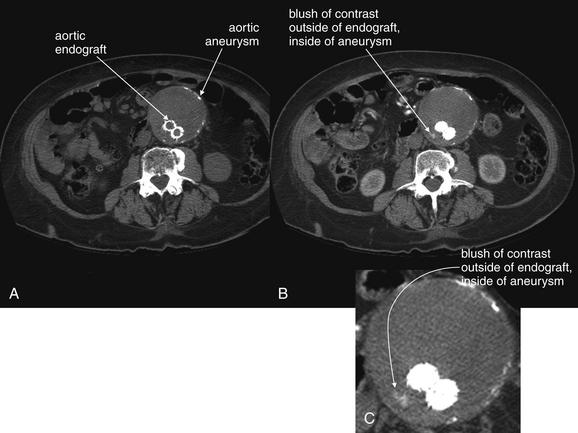
Figure 11-21 Type 2 endoleak following aortic aneurysm endovascular repair: CT without and with intravenous (IV) contrast.
A, A noncontrast CT shows the endograft within the aortic aneurysm but cannot detect an endoleak (leak of blood within the aneurysm sac, outside of the graft).
B, C, IV contrast–enhanced CT shows contrast outside of the graft but within the aneurysm sac—confirming an endoleak. Some slow leaks are not seen on arterial phase imaging but are visible on delayed images.
Definitive diagnosis of an endoleak can be made with IV contrast–enhanced CT (see Figures 11-20 and 11-21). Without IV contrast, the presence of an endoleak will go unrecognized on CT, because leaking blood will have a similar Hounsfield density to thrombus outside of the stent but contained within the aneurysm sac. With the addition of IV contrast, blood flow within the aneurysm sac outside of the stent is evident. Because retrograde filling of the aneurysm sac is often slow (e.g., with type 2 endoleaks described earlier), some endoleaks can be difficult to detect on arterial-phase CT with IV contrast. Additional delayed images (acquired approximately 5 minutes after initial contrast injection) may be required.34-35 Some authors have argued against the need for delayed phase images, because most endoleaks detected with this technique resolve spontaneously without intervention.36 Contrast-enhanced ultrasound can be used to assess for endoleak in patients with contraindications to IV contrast for CT. Contrast-enhanced ultrasound performs favorably compared with CT.23,37 MRI can also be used to assess for endoleaks, because graft materials are MRI compatible. Contraindications to gadolinium contrast are discussed elsewhere in this chapter.
Aortic Dissection
Dissection of the thoracic aorta presenting primarily with abdominal pain is rare, occurring in only 4.6% of cases in a large international registry.38 However, mortality is increased in these patients, resulting from a delay in diagnosis because of atypical presentation.38 Although type B aortic dissections (those affecting only the descending aorta) account for 37.5% of aortic dissections, only 1.3% of all aortic dissections affect solely the abdominal aorta.39 Risk factors for aortic dissection include collagen vascular diseases such as Marfan’s and Ehlers-Danlos syndrome, but these account for a minority of cases (2.9% of type B dissections) in the International Registry of Acute Aortic Dissection (IRAD), and a history hypertension is likely the greatest risk factor, occurring in 80%.40 Pregnancy and the postpartum state are also risk factors, likely as a consequence of increased collagenase production during this time. Use of stimulant drugs such as cocaine can also result in aortic dissection.41-42 Although the classic description of aortic dissection includes sudden tearing pain radiating to the back, the clinical presentation can be quite variable. Sudden pain is common (80% to 90%), as is migratory pain (25%).38-40 In the International Registry of Acute Aortic Dissection, among type B dissections presenting with primarily abdominal pain, tearing pain was described in 25%, sharp pain in 44%, pressure-like pain in 33%, and burning pain in 6%.38 The latter descriptors might mislead emergency physicians who are commonly taught to seek “tearing” pain as a clue to aortic dissection. The age distribution for aortic dissection is skewed toward older patients, with a mean age of 65 years and with 42% of type B dissections occurring in patients 70 years or older. Patients with a personal or family history of connective tissue diseases must be suspected of dissection at a younger age.
Unlike aortic aneurysm rupture, which frequently leads to hemodynamic instability, aortic dissection can present without any substantial derangement of hemodynamics. Although hypertension is a risk factor for the development of aortic dissection, patients may present with normotension (28%), hypertension (69%), or hypotension (3%).40 Initially, aortic dissection is a disease process involving only the intimal layer of the aorta. A tear in the intima develops, and blood typically undermines this layer, creating a flap that extends distally in the direction of blood flow. Proximal extension may also occur. Extension into branch vessels is the greatest threat, because it can disrupt perfusion to vital organs including the kidneys, mesentery, and bowel (21% in cases of abdominal aortic dissection); spinal perforating arteries (2.7%); and extremities (25% to 30%).39-40 Proximal dissection can result in disruption of the aortic valve with acute valvular insufficiency. Dissection into the pericardium can occur, resulting in pericardial tamponade.
In none of these former cases does blood loss external to the aorta occur, accounting for the frequent relative hemodynamic stability of patients with aortic dissection.38-40 This also accounts for the low sensitivity of chest x-ray for the diagnosis of thoracic aortic dissection and naturally for abdominal aortic dissection. In traumatic thoracic aortic injury, violation of all layers of the aorta may occur, leading to extravasation of blood and formation of a mediastinal hematoma, which can in turn lead to widening of the mediastinal silhouette on chest x-ray. In contrast, nontraumatic dissection may occur in an aorta of normal caliber and may be restricted to an intimal injury without formation of a mediastinal hematoma. This can result in a normal mediastinal silhouette on x-ray, occurring in as many as 20%, according to a large international registry.40 Luker et al.43 reported that only 25% of chest x-rays were prospectively interpreted as suggesting aortic pathology in cases of acute thoracic dissection.
Classic examination features such as pulse deficits are relatively rare in type B dissections, occurring in only about 20% to 30% of patients with type B thoracic or isolated abdominal aortic dissections.39-40 The classic finding of a differential blood pressure between upper extremities is of unknown sensitivity and specificity. In a study of asymptomatic emergency department patients with a prior history of hypertension, 18% of patients had differences in the blood pressures obtained in the upper extremities exceeding 10 mm Hg.44 This suggests that the finding is nonspecific, so its use as a screening tool would result in unnecessary diagnostic imaging in many patients. The sensitivity is also likely to be very low. If the intimal flap does not involve an extremity branch of the aorta, neither pulse deficits nor differential blood pressure might result. Reliance on this physical examination finding to prompt definitive imaging would result in failure to diagnose aortic dissection in many patients. Common features that should prompt evaluation for aortic dissection include sudden onset and migratory pain, which has been found to be a frequent, though not ubiquitous, feature. Abdominal pain in concert with back or chest pain is worrisome. The presence of unilateral neurologic features also can suggest stroke from dissection involving the carotid arteries. Vertebral artery dissection can result in posterior circulation symptoms. Ischemic peripheral neuropathy occurs in a small minority of patients (2.2%).40 Occlusion of spinal perforating arteries can result in neurologic deficits, including bilateral limb paralysis or sensory loss. Sometimes these symptoms can be transient, and they may be mistaken for patient malingering, sciatica, or spinal cord compression. Dissection of the mesenteric arteries can result in simultaneous mesenteric ischemia in as many as 5% of cases, and renal failure can result from dissection of the renal arteries in up to 13% (see Figures 11-25 and 11-26).40 Limb ischemia (7%) may also result from abdominal aortic dissection involving the iliac arteries.40
Screening for aortic dissection using D-dimer measurement has been advocated by some authors, who have reported sensitivity of 93% to 100%.45-52 A meta-analysis suggested a sensitivity of 94% (95% CI = 91%-98%).53 However, other authors have reported sensitivities of 88% to 92%, with false-negative results reported in patients with thrombosed false aortic lumens. Moreover, the small size of most published studies results in wide 95% confidence limits. The lower confidence limits of sensitivity reported are as low as 67% to 85% in some studies; for this reason, some authors continue to raise concerns that D-dimer testing is too unreliable for clinical use, given the high mortality of aortic dissection.54-55
Imaging for Aortic Dissection
Because the clinical presentation of AAA rupture and abdominal aortic dissection can overlap substantially, diagnostic imaging for aortic dissection should begin with bedside ultrasound to assess for AAA. Ultrasound can sometimes visualize the intimal flap of dissection (Figures 11-22 and 11-23). However, the sensitivity is relatively low, around 70% with use of B scan and color Doppler techniques. Contrast-enhanced ultrasound has been reported to be 97% sensitive compared with CT, although the technique is not widely used.56 CT without IV contrast cannot rule out aortic dissection, because the intimal flap typically shares the same density with blood in the true and false lumens (Figure 11-24). Rare case reports document aortic dissection on noncontrast CT, based on displacement of calcified atheromatous plaques or high attenuation clot within the false lumen, but the sensitivity of these findings is unknown and should not be relied upon.57 Administration of a rapid bolus of IV contrast should be considered critical to the diagnosis. Thus if a noncontrast CT is first performed to evaluate for AAA and is negative, CT with IV contrast must be performed if possible. With IV contrast, the intimal flap is highlighted as an unenhanced line separating the true and false lumens of the aorta (see Figure 11-24). A normal aorta is circular in cross section, filling uniformly with bright contrast. When an intimal flap is present, the circular cross section appears divided into two lumens. These may be unequal in size. Both lumens may enhance with contrast, or one or both lumens may be thrombosed and fail to enhance (Figure 11-25). In addition to initial arterial phase images, delayed images are usually obtained to assess the perfusion of organs such as the kidneys. Failure of the kidneys to enhance on delayed images indicates hypoperfusion related to the dissection and may require emergency surgery or intravascular techniques to fenestrate the dissection flap and restore blood flow (Figure 11-26).
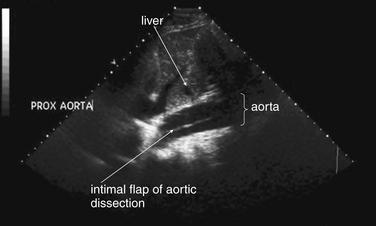
Figure 11-22 Abdominal aortic dissection: Ultrasound.
This sagittal or long-axis ultrasound demonstrates the intimal flap of an aortic dissection in the proximal abdominal aorta.
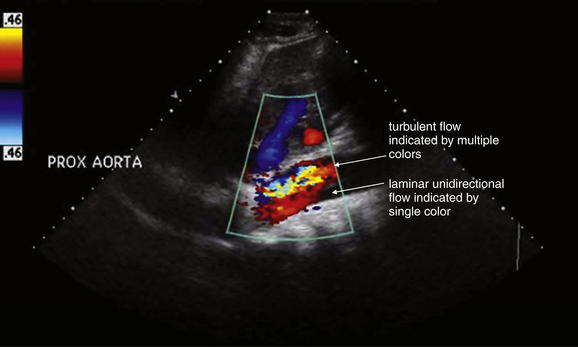
Figure 11-23 Abdominal aortic dissection: Ultrasound with Doppler flow.
Same patient as Figure 11-22. Ultrasound demonstrates the intimal flap of an aortic dissection in the proximal abdominal aorta. Color Doppler shows differential blood flow in the true and false lumens.
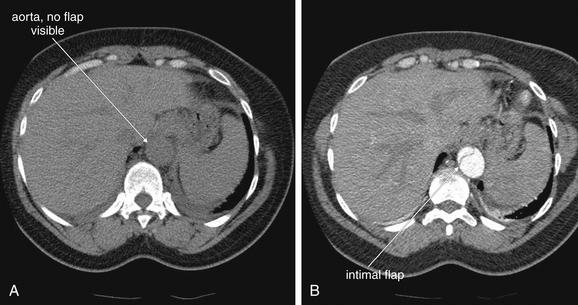
Figure 11-24 Aortic dissection involving the abdominal aorta: CT without and with intravenous (IV) contrast.
Soft-tissue windows. A, On CT without IV contrast, the intimal flap of dissection is not visible.
B, When IV contrast is administered, the intimal flap separating the true and false lumens of the aorta becomes visible. No oral contrast is needed to make this diagnosis.
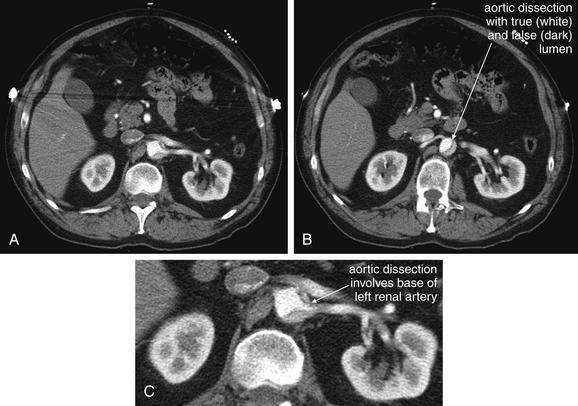
Figure 11-25 Aortic dissection: Stanford type B with involvement of the left renal artery.
CT with IV contrast, soft-tissue windows. A, B, Sequential images at the level of the renal artery. C, Close-up from A.
This patient has a dissection of the abdominal aorta. An intimal flap and false lumen appear to involve the origin of the left renal artery, although the kidney does enhance with contrast.
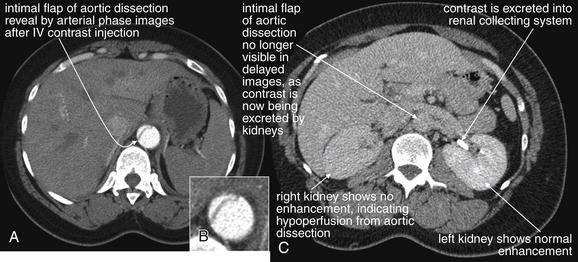
Figure 11-26 Aortic dissection with end-organ ischemia: Delayed phase, intravenous-contrasted CT images.
Aortic dissection involving the abdominal aorta can result in ischemia of end organs, including bowel and kidneys. A, Arterial phase images obtained immediately following contrast administration can reveal the dissection flap, including major branch vessel involvement. In this case, the initial scan was terminated inadvertently above the level of the renal arteries. B, Close-up from A showing intimal flap in detail. C, Delayed images can show evidence of hypoperfusion. In this case, the right kidney does not show normal enhancement, indicating hypoperfusion. The left kidney enhances and shows contrast in the renal collecting system, indicating normal perfusion.
MRI or MRA is also highly sensitive and specific for abdominal aortic disease, including aortic dissection.58-59 In patients with contraindications to iodinated contrast for CT, such as renal insufficiency or iodinated contrast allergy, MRI or MRA is a reasonable alternative if its performance can be timely. Typical MRI or MRA for aortic dissection requires approximately 25 minutes to complete, compared with fewer than 6 minutes for CT.60 This does not take into account the limited availability of MRI outside of normal business hours in many centers, with additional time often required for technicians to arrive. Three-dimensional MRA with injected gadolinium contrast is usually used to demonstrate the intimal flap.58-59 In patients with renal insufficiency at risk for gadolinium-associated complications (discussed at the end of this chapter), MRI without IV gadolinium can be performed to assess for aortic dissection. New sequences that require no contrast material perform favorably compared with gadolinium-enhanced MRA.58-61 These protocols include steady-state, two-dimensional, gradient–recall echo60; two-dimensional turbo spin echo; and two-dimensional, balanced, steady-state free precession.61
Mesenteric Ischemia
Mesenteric ischemia is not a single disease but a family of related disorders. These include acute and chronic occlusions of mesenteric arteries and acute, subacute, or even chronic occlusions of portal and mesenteric veins. Bowel ischemia can also be a consequence of small-bowel obstruction and intestinal volvulus. Vascular thrombosis most often afflicts patients at advanced age; however, rarely, conditions such as vasculitis, hypercoagulable states, or atrial fibrillation may underlie acute thrombosis in young patients.32 We review here the mechanism and the presentation for each of these disease states, recognizing that these diseases are rare enough that large studies with good methodology are generally lacking.
Acute Mesenteric Artery Occlusion
Acute mesenteric artery occlusion and ischemia can occur from in situ thrombosis or embolic events. Atrial fibrillation is likely the most common cause, accounting for 95% of cases in one prospective study.62 Dissection of mesenteric vessels can complicate aortic dissection or rarely may occur in isolation. The superior mesenteric artery (SMA) is the most commonly affected vessel in the setting of atrial fibrillation (see Figures 11-31 to 11-35).63 Occlusion of the SMA may be more common than previously believed. In a population-based study using autopsy results, the incidence was 8.6 per 100,000 person years, with a cause-specific mortality of 6 in 1000 deaths. Suspicion of intestinal ischemia before death was noted in only 33%, possibly reflecting a variable presentation not fitting the classically described signs and symptoms.64
Classically, acute mesenteric ischemia from arterial occlusion is characterized by sudden and severe abdominal pain without significant abdominal tenderness. This is often described as “pain out of proportion to exam.” This may be a misleading myth that could result in misdiagnosis or delayed diagnosis in many patients. In a retrospective review from Wake Forest University,65 63% of cases had a delay of greater than 24 hours from symptom onset until treatment, reflecting the difficulty of the diagnosis. Of 77 cases presenting with acute mesenteric ischemia, 64% were described in their initial emergency department record as having peritonitis–suggesting that exam findings were severe, not mild. In a second study of 43 patients with mesenteric ischemia, 48% had diffuse tenderness, and 52% had peritonitis by exam.66 One explanation is that these are late findings and patients often present after a delay of many hours from onset of ischemia. In any case, mesenteric ischemia should never be ruled out because the physical examination demonstrates too much tenderness.
Lab abnormalities associated with mesenteric ischemia include substantial leukocytosis, elevated anion gap, elevated lactate level, and hyperphosphatemia, but small studies on the topic limit the value of these findings in ruling out a potentially lethal process. Ritz et al.32 found that marked leukocytosis and elevated serum lactate occurred in 93% of patients with acute mesenteric ischemia and were prognostic of mortality. Lange and Jackel67 found serum lactate to be elevated in 100% of 20 patients with mesenteric ischemia, although the specificity was only 42%. Merle et al.68 found a serum lactate level of greater than 5 mmol/L to be associated with death within 72 hours. High inorganic phosphate levels have long been reported to be associated with mesenteric ischemia, based primarily on animal studies.69-72 Phosphate is believed to originate from sloughing intestinal mucosa. The sensitivity has not been studied in well-designed human trials but is inadequate for screening in case series. May and Berenson73 reported elevations in only 25% of cases of intestinal ischemia. Gorey and O’Sullivan74 reported hyperphosphatemia in only 15% of 65 patients with extensive intestinal ischemia, leukocytosis in 65%, and metabolic acidosis in 67%.
Pitfalls in laboratory screening can occur. Although marked leukocytosis can suggest acute mesenteric ischemia, this is likely a late finding that may occur after frank bowel necrosis has occurred, in which case patient prognosis is poor. Thus patients with normal white blood cell counts should not be dismissed as not having mesenteric ischemia. Patients with significant leukocytosis may be mistakenly suspected of infectious or inflammatory conditions of the abdomen, such as diverticulitis, abdominal abscess, or appendicitis. Although these patients undoubtedly would undergo additional observation or diagnostic imaging, the absolute time criticality of the diagnosis of ischemia might be missed. For example, observation of several hours in the case of SMA thrombosis can result in complete loss of the small bowel, with high morbidity and mortality.
When considering the screening sensitivity of laboratory tests, it is extremely important to remember the methodologic limitations of most studies on the subject, which are usually small, retrospective reviews. In addition, mesenteric ischemia is a spectrum of disease including partial and incomplete vascular occlusions. The elapsed time from the moment of vascular occlusion until emergency department presentation, as well as the degree of bowel hypoperfusion, may affect the sensitivity of laboratory testing and diagnostic imaging.
Imaging for Mesenteric Ischemia
In any patient with suspected acute mesenteric ischemia, immediate surgical consultation and definitive imaging must be performed. Plain radiographs play a limited role in the diagnosis. In retrospective reviews of patients ultimately diagnosed with mesenteric ischemia, plain films are both insensitive and nonspecific.75-76 In one study of 187 patients, 35% had normal plain films and 42% showed signs of small-bowel obstruction.32 Common plain film abnormalities in acute mesenteric ischemia include an appearance of intestinal ileus, which should come as little surprise given that intestinal motility would be expected to cease in the absence of intestinal blood flow (Figures 11-27 and 11-28; see Figure 11-3). Findings in one small study included air–fluid levels (84%), dilated bowel loops (48%), thickened and unchanging loops (20%), gastric distension and gasless abdomen (12%), and small-bowel pseudo-obstruction (8%).76 Findings of ileus may give false reassurance that no critical abnormality is present in the abdomen. The finding of intestinal pneumatosis is likely a relatively rare and late finding, occurring after the onset of intestinal necrosis (see Figures 11-3, 11-27, and 11-28). In one study, only 4% of patients with mesenteric ischemia had pneumatosis on x-ray.77 Although pneumatosis should prompt immediate surgical consultation, reliance on this finding likely results in diagnosis at such a late time that exceedingly high morbidity and mortality result.78 Ironically, in addition to being insensitive for mesenteric ischemia, pneumatosis is not specific for the diagnosis, occurring sometimes from a variety of less emergent causes (see Figures 11-43 and 11-46).78 As with other syndromes of acute abdominal pain, an upright portable chest x-ray is reasonable to detect pneumoperitoneum resulting from intestinal perforation (see Figure 11-1). A negative chest x-ray must be followed by immediate definitive imaging. Abdominal plain films should not be routinely obtained but should be considered in patients too unstable to undergo CT.
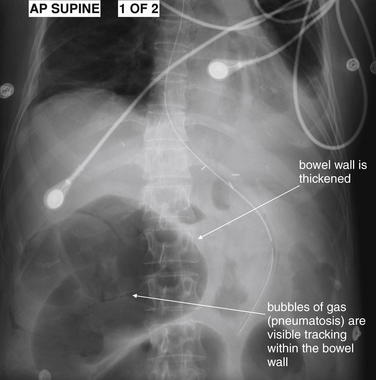
Figure 11-27 Bowel infarction (ischemic colitis with pneumatosis): X-ray.
This image depicts classic findings of mesenteric ischemia, including gross distension of bowel, bowel wall thickening, and frank pneumatosis.
Pneumatosis is a late finding, representing the penetration of gas-forming organisms into necrotic bowel wall. How can gas be recognized to be within the bowel wall? The gas is organized in a curved line—indicating that the gas is trapped within the bowel wall, not scattered at random as would be expected if gas were distributed in stool within the bowel. See magnified view, Figure 11-28.
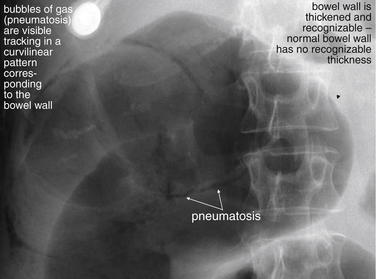
Figure 11-28 Bowel infarction (ischemic colitis with pneumatosis): X-ray.
Close-up from Figure 11-27. This image depicts classic findings of mesenteric ischemia, including gross distension of bowel, bowel wall thickening, and frank pneumatosis.
Computed Tomography for Mesenteric Ischemia
Definitive imaging for mesenteric ischemia is CT with IV contrast (Figures 11-29 to 11-34; see also Figures 11-36 to 11-43, 11-45, 11-46, and 11-48). Oral contrast is not necessary for the diagnosis and should be avoided because of substantial delay, more than 2 hours in some institutions, that can result.13 Because of the overlapping presentation of AAA rupture, aortic dissection, and mesenteric ischemia, an immediate CT scan with no contrast agents can be performed to assess for AAA. If this test is negative, immediate CT with IV contrast should be performed unless the patient has significant contraindications to iodinated contrast. As with aortic dissection, the extreme morbidity and mortality of mesenteric ischemia means that the risks and benefits of IV contrast must be carefully weighed. Because this is a time-critical diagnosis with a mortality as high as 60% to 70%,65-66 some patients with moderate or severe renal insufficiency or contrast allergies should receive immediate IV contrast after a discussion and informed consent from the patient or patient family. Contrast allergies and renal insufficiency are discussed in more detail later.
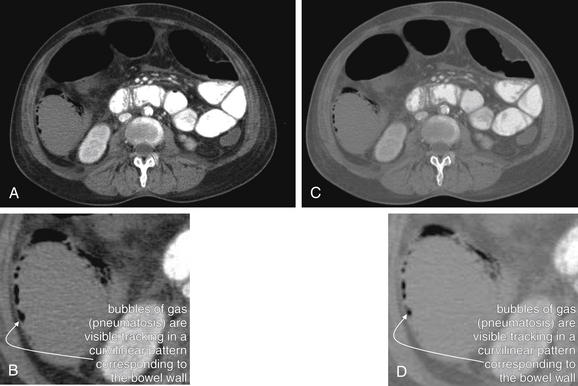
Figure 11-29 Bowel infarction (ischemic colitis with pneumatosis): CT with oral and IV contrast.
Same patient as in Figures 11-27 and 11-28.
A, A slice viewed on typical CT soft-tissue windows. B, Close-up from A. C, The same slice viewed on an intermediate window setting designed to highlight air. D, Close-up from C. Air is visible within the bowel wall, indicating a bowel segment with frank necrosis whose wall has been infiltrated with gas-forming organisms. This is a dire imaging finding that should prompt immediate surgical consultation. The mortality exceeds 70% for mesenteric ischemia.
Why choose different CT window settings? Standard soft-tissue windows render fat dark—nearly black. This is useful because it allows the identification of subtle fat stranding, which lightens the color of fat. But air can be less noticeable on this setting, because air (black) and fat (nearly black) have little contrast with each other. The window settings in C and D make fat a lighter gray, helping to differentiate it from gas.
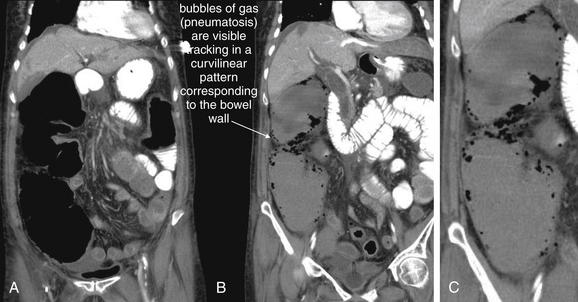
Figure 11-30 Bowel infarction (ischemic colitis with pneumatosis): CT with intravenous and oral contrast (soft-tissue windows).
Same patient as Figures 11-27 through 11-29.
This 61-year-old female presented with sepsis, lactic acidosis, and frank pneumatosis on x-ray caused by ischemic colitis. Unstable, on pressor medications, she underwent exploratory laparotomy, extensive lysis of adhesions, subtotal colectomy with end ileostomy, small-bowel resection with primary anastomosis, and splenectomy. Miraculously, she survived, given the severity of her illness on presentation. The operative findings suggested that her ischemia may have been caused by extensive adhesions rather than a single vascular obstruction.
Coronal reconstructions show massive dilatation of the large bowel, as well as frank pneumatosis. A, An anterior slice shows the bowel to be dilated and air filled (remember, the patient was supine during CT, so an anterior coronal plane represents the superior portion of the abdomen). B, A more posterior coronal plane shows a dilated, fluid-filled ascending colon with gas infiltrating its wall—pneumatosis. C, Close-up from B.
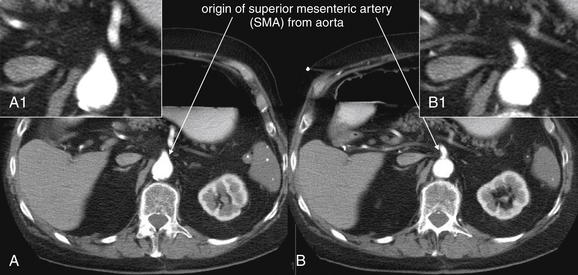
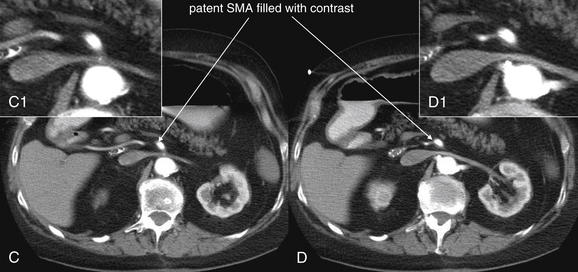
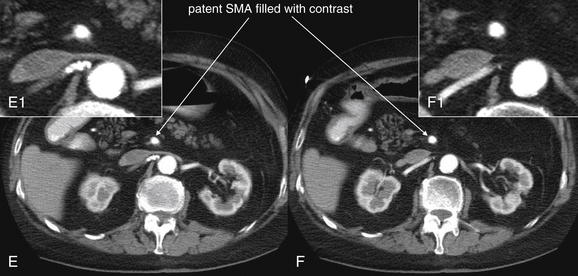
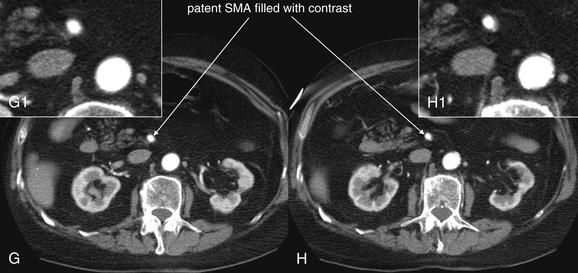
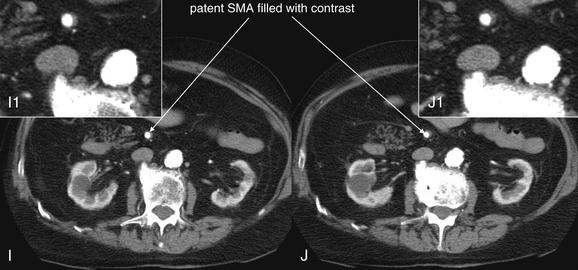
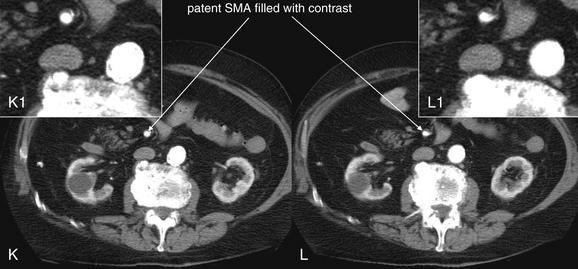
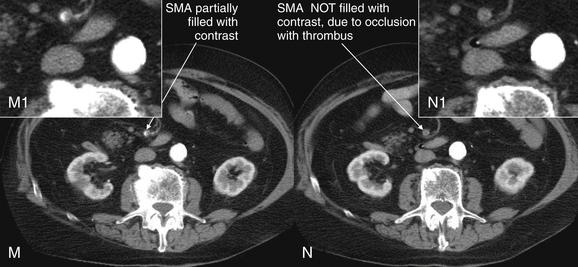
Figure 11-31 Superior mesenteric artery (SMA) occlusion: CT with intravenous (IV) contrast.
This 77-year-old male presented in atrial fibrillation with abdominal pain and bright red blood from his colostomy, beginning abruptly after dinner. He had recently been discontinued from warfarin therapy because of falls. Mesenteric ischemia from an embolic occlusion was suspected, given the abrupt onset, atrial fibrillation, gastrointestinal bleeding, and an elevated lactate level (twice the upper limit of normal). CT with IV and oral contrast was performed. The SMA was noted to be completely obstructed with thrombus approximately 6 cm distal to its origin. No secondary bowel findings of ischemia were noted, likely because of the rapidity with which CT was performed after the onset of symptoms. This series of axial views follows the SMA from its origin (A, cephalad slice) to the point of thrombus obstruction (N, caudad slice). Because the SMA tracks anteriorly and diagonally from cephalad to caudad, it is visible in short-axis cross section in most of the slices. Note the sudden change from a widely patent, contrast-filled SMA to a completely unopacified vessel. The finding is the same one that would be noted with an occlusive pulmonary embolism.
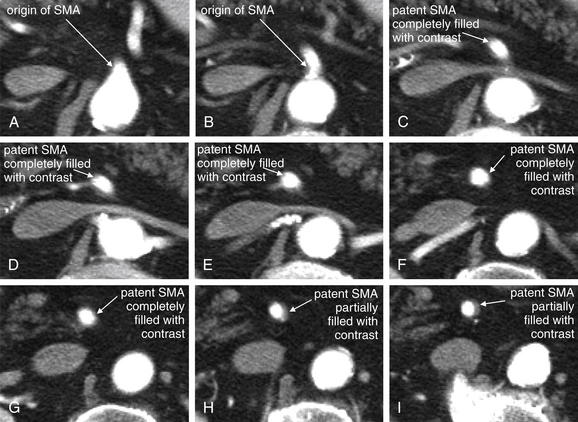
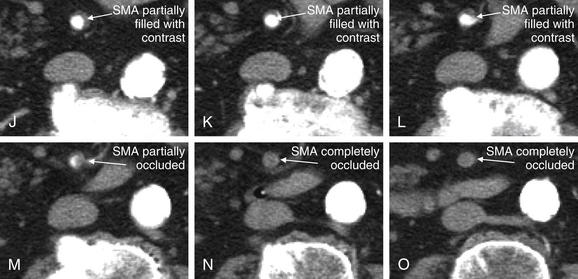
Figure 11-32 Superior mesenteric artery (SMA) occlusion: CT with IV contrast.
Same patient as Figure 11-31. This series of axial views (cropped to the region of interest) tracks the SMA from its origin (A) to the point of thrombosis (O).

Figure 11-33 Superior mesenteric artery (SMA) occlusion: CT with IV contrast.
Same patient as in Figures 11-31 and 11-32. This coronal CT captures the SMA at a point where it travels almost perfectly parallel to the coronal plane (A). The patent proximal portion is visible, and the abrupt thrombosed section is also seen. Compare with the angiogram in Figure 11-34. B, Close-up.
Was contrast needed for this diagnosis? Oral contrast played no role here. This patient had a normal CT with the exception of the SMA thrombus, with no secondary bowel findings. IV contrast was essential to the diagnosis, because the SMA thrombosis would not have been visible without a well-timed, high-quality bolus through a large-bore IV catheter.
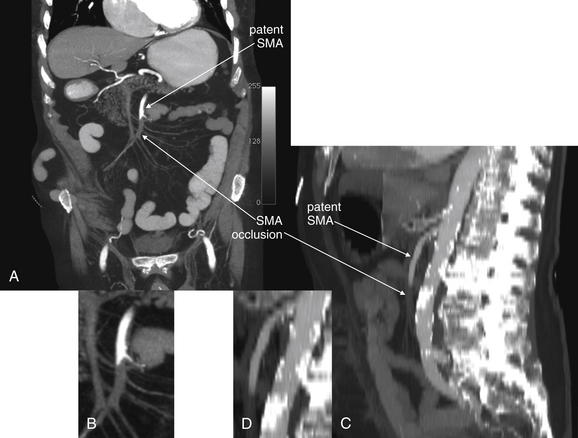
Figure 11-34 Superior mesenteric artery (SMA) occlusion: Computed tomography (CT) with intravenous contrast.
Same patient as in Figures 11-31 through 11-33. Maximal intensity projection (MIP) images show the thrombosed SMA section in more detail. MIP images are created after the CT scan is performed using the original CT dataset. They “thicken” the image slab, allowing tortuous anatomic structures that cross through multiple routine CT slices to be seen in a single image. Your radiologist can create these upon request to improve diagnostic capabilities. Your local institution may already be performing this postprocessing “behind the scenes.”
A, Coronal reconstruction and enlargement. B, Close-up from A.
C, Sagittal reconstruction and enlargement. D, Close-up from C.
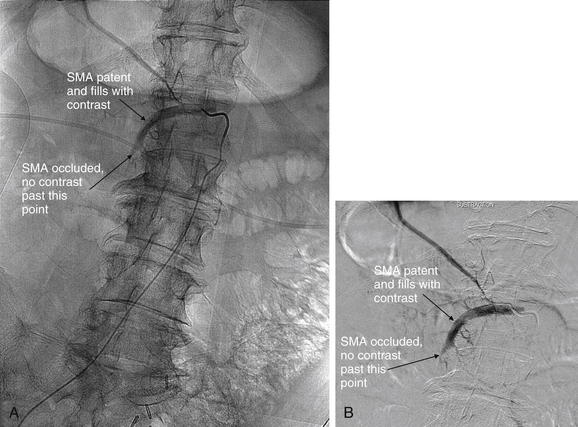
Figure 11-35 Superior mesenteric artery (SMA) occlusion: Angiogram.
Same patient as in Figures 11-31 through 11-34. A catheter has been inserted into the aorta through a femoral artery. The catheter tip has been positioned at the origin of the SMA, and contrast has been injected. The proximal SMA fills, but contrast does not fill the vessel beyond approximately 6 cm—indicating complete thrombotic occlusion. Compare with Figure 11-34, a coronal maximal intensity projection image created from computed tomography reconstruction.
A, Digital angiography. B, The same image using a digital subtraction technique, which digitally removes static portions of the image to allow better inspection of the dynamic contrast injection.
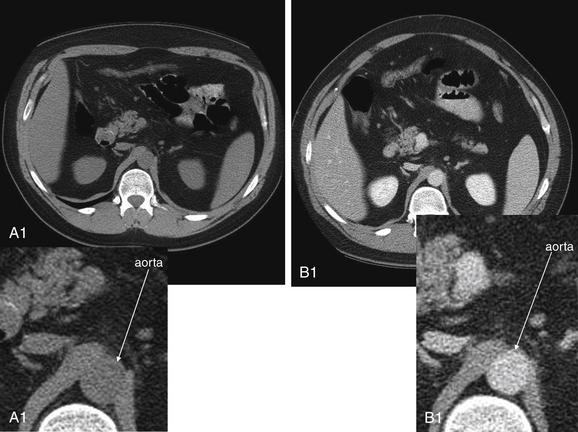
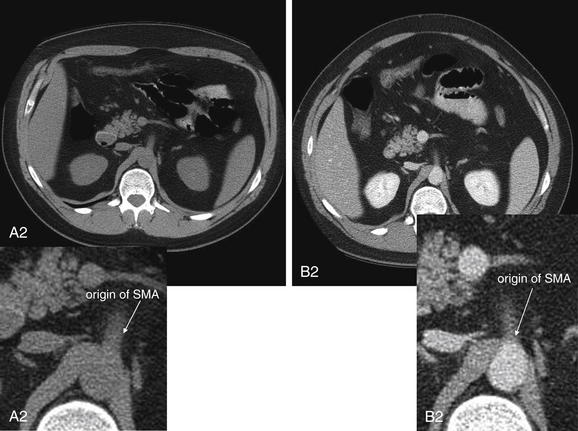
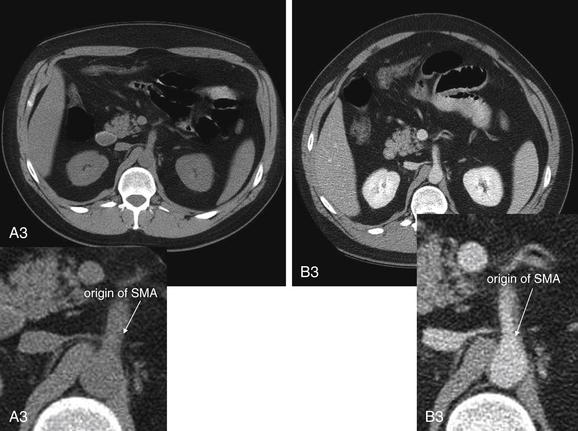
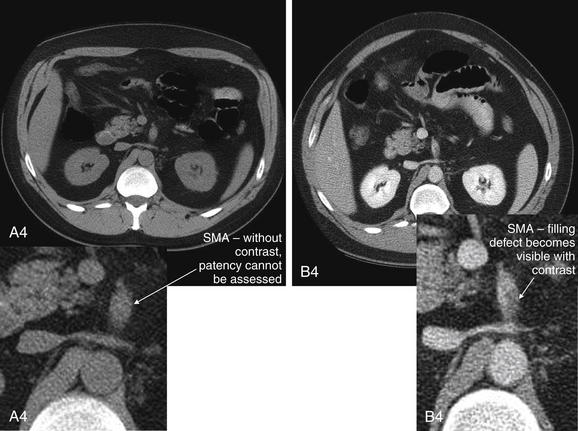
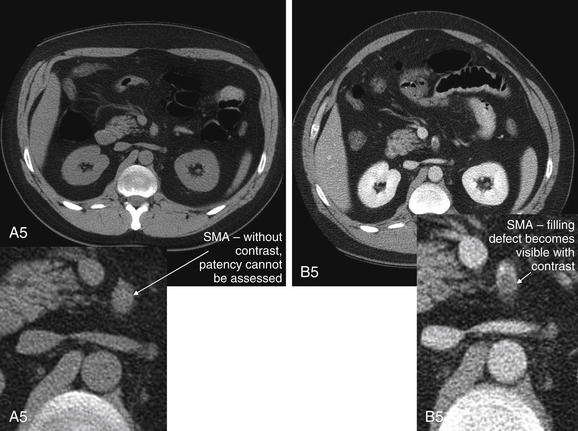
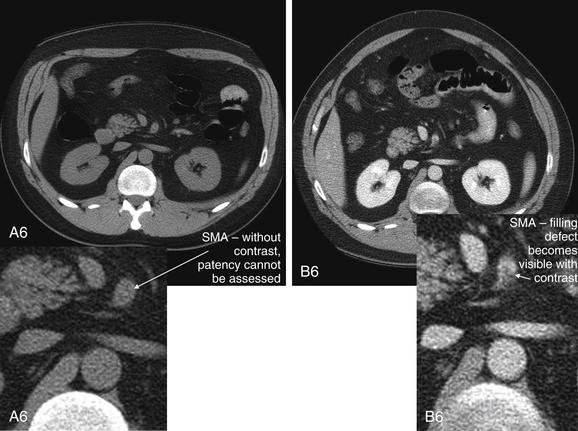
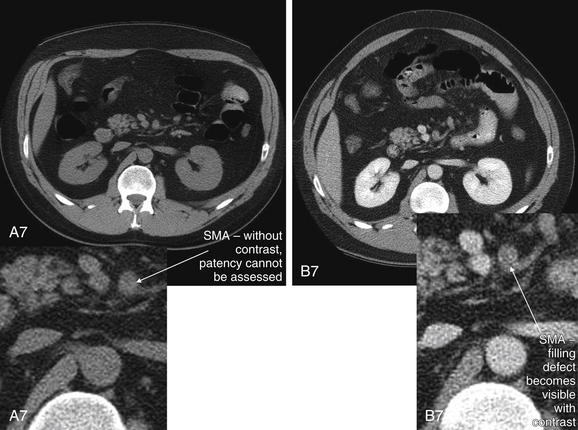
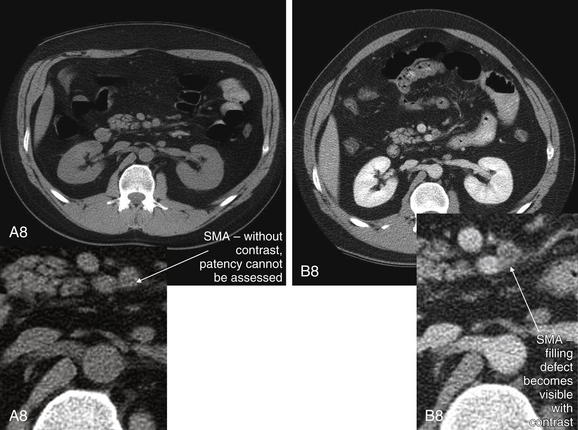
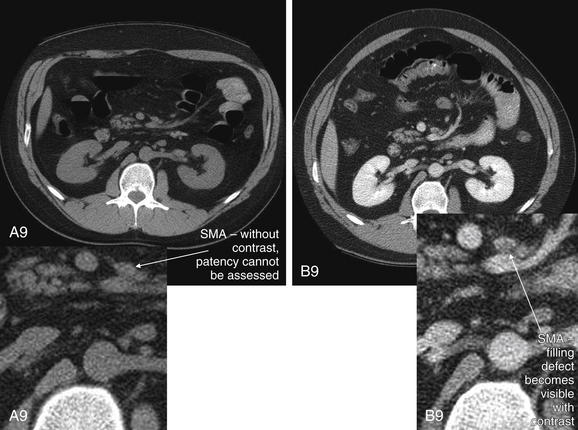
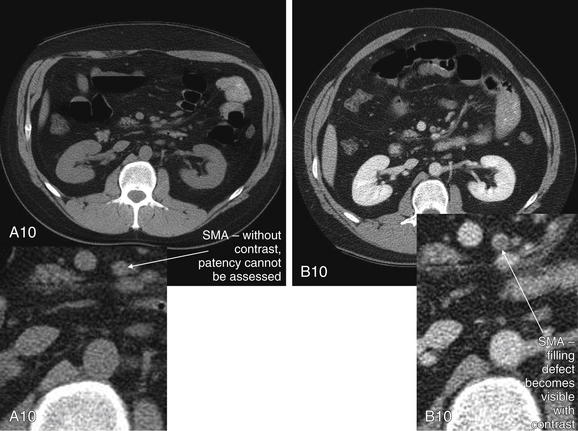
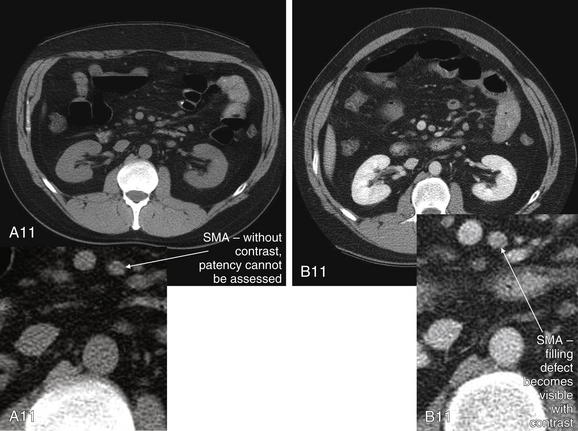
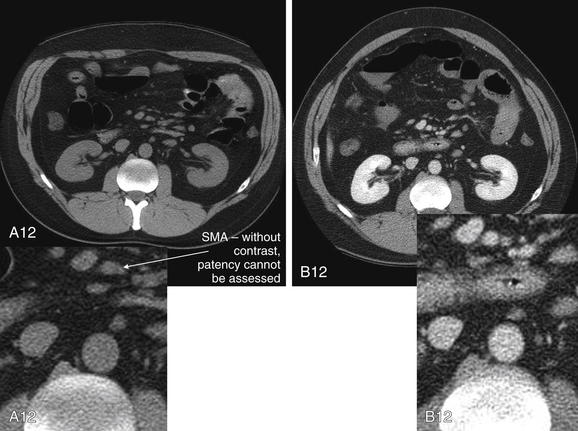
Figure 11-36 Mesenteric ischemia resulting from superior mesenteric artery (SMA) thrombosis: CT without and with contrast.
This 37-year-old male with no prior medical or surgical history presented with abdominal pain with nausea, vomiting, and diarrhea. He underwent noncontrast CT that was interpreted as normal—despite a white blood cell count of 24.5 x 109, an anion gap of 19 mEq/L, and a lactate level of 3.5 mmol/L. The emergency physicians then suspected mesenteric ischemia. CT with contrast was performed, revealing complete thrombosis of the SMA near its origin from the aorta. The two CT scans are displayed side by side to allow comparison of the images. A key point is the need for injected contrast to allow recognition of filling defects within vascular structures. When reviewing the images, compare the noncontrast CT (A) to the CT with intravenous (IV) contrast (B). Slices are numbered from cephaladmost (1) to caudadmost (12). Each slice is shown with an enlarged view centered on the vascular structures of interest. Track the SMA from its origin off the aorta. Without IV contrast, patency of the SMA cannot be assessed, because liquid blood and thrombus have nearly identical density and appear dark gray. With the addition of IV contrast, the patent lumen appears bright white, whereas the filling defect resulting from a thrombus appears dark gray.
Oral contrast is not needed for the diagnosis. In this patient, oral contrast was given but did not progress beyond the stomach—likely because of ileus in the face of bowel ischemia. Oral contrast results in unnecessary delay that can worsen the severe morbidity and mortality of mesenteric ischemia. Operatively, this patient was found to have SMA thrombosis with gangrene of the small intestine and right and transverse colon. He underwent resection of more than 200 cm of small bowel and was left dependent on total parenteral nutrition.
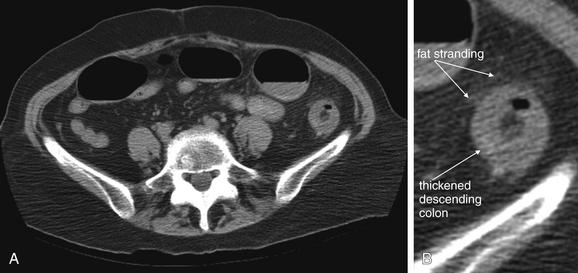
Figure 11-37 Ischemic colitis: CT without IV contrast.
CT soft-tissue windows. This 86-year-old female presented with abdominal pain, vomiting, altered mental status, and hypotension. The patient had an elevated lactate level of 5.7 mmol/L, although this could represent sepsis, rather than mesenteric ischemia. A, The patient did not receive IV contrast because of renal insufficiency (creatinine 2 mg/dL), so vascular structures are not well seen. Although the patient received oral contrast, none reached the distal bowel before CT scan. B, Close-up.
The descending colon shows circumferential wall thickening with a doughnut-like configuration, suggesting colitis, though the cause is not certain (ischemic or infectious). Some surrounding fat stranding is seen. Other images showed portal venous gas (Figure 11-38). The radiologist interpreted the CT scan as suggestive of ischemic colitis.
Because of a concurrent non–ST-elevation myocardial infarction (NSTEMI), the patient was treated solely with fluid resuscitation and antibiotics. She survived the illness. Was the CT diagnosis correct? Was the portal venous gas real, or was it misrecognized air in biliary ducts? These questions remain unanswered. Perhaps this was a case of infectious colitis.
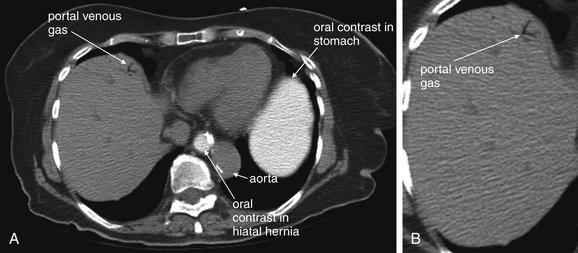
Figure 11-38 Portal venous gas in setting of ischemic colitis: CT without IV contrast.
Same patient as in Figure 11-370. A, Portal venous gas does not require any contrast for identification. This patient had an elevated creatinine and received no IV contrast. She did receive oral contrast, but this did not contribute to the diagnosis. B, Close-up.
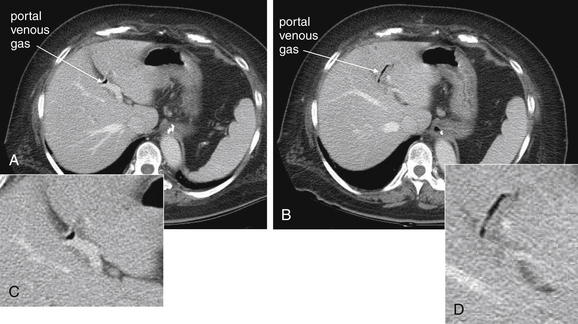
Figure 11-39 Portal venous gas and possible ischemic colitis.
CT with IV contrast, soft-tissue windows. This 65-year-old female presented with nausea and epigastric pain. CT with intravenous contrast was performed and showed concerning findings, including thickening of the entire ascending colon, pneumatosis of the colon, and portal venous gas. Laparoscopy was performed because of concern for ischemic colitis—but after inspection of the entire bowel, no resection was performed. The patient was treated for likely infectious colitis. Stool cultures, Clostridium difficile testing, and fecal leukocyte testing were all negative. She recovered uneventfully. Look carefully at these images, which demonstrate portal venous gas. A collection of gas is seen at a branch point in the portal vein (A) and extending to the patient’s left portal vein (B). C, Close-up from A. D, Close-up from B.
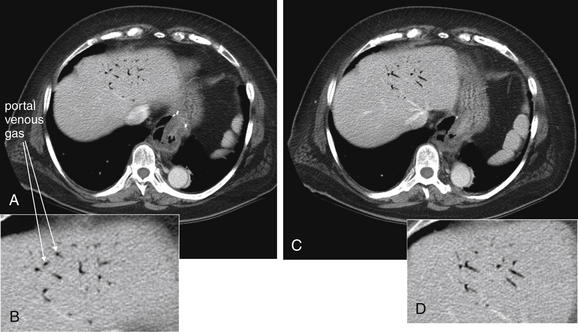
Figure 11-40 Portal venous gas and possible ischemic colitis.
Same patient as Figure 11-39. Gas has spread through the portal system. Normally, this is an ominous sign, possibly indicating mesenteric ischemia. Remarkably, this patient had a nontherapeutic laparoscopy and recovered with fluids and antibiotic therapy. These images do not readily distinguish portal vein gas from gas in the biliary tree, which can have a similar appearance. However, Figure 11-39 showed gas more proximally in the portal vein, so these gas collections presumably are present in peripheral portal vein branches, not bile ducts A and C, two adjacent axial CT images through the cephalad portion of the liver, viewed on soft-tissue windows. IV contrast has been administered. B, Close-up from A. D, Close-up from C.
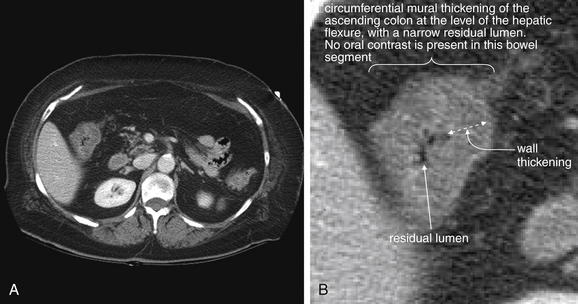
Figure 11-41 Thickening of right colon and ischemic colitis: CT with intravenous contrast only.
Same patient as Figures 11-39 and 11-40. Did this patient have ischemic or infectious colitis? This is uncertain, but patients with her concerning constellation of CT findings should be pursued as possible mesenteric ischemia, because delay in treatment could be catastrophic. A, Axial CT viewed on soft-tissue windows. B, Close-up from A.
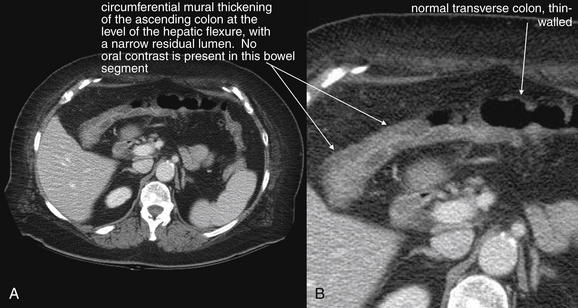
Figure 11-42 Thickening of right colon and ischemic colitis.
Same patient as Figures 11-39 through 11-41. As the ascending colon transitions to the transverse colon beyond the hepatic flexure, it relatively rapidly resumes a normal wall thickness. A, Axial CT with IV contrast viewed on soft-tissue windows. B, Close-up from A.
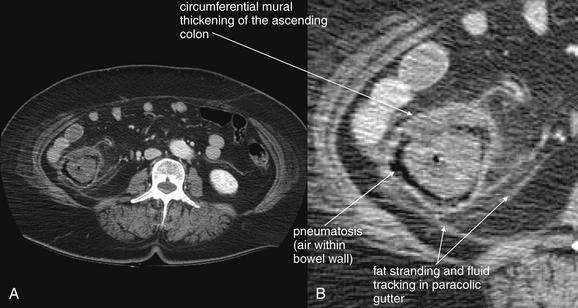
Figure 11-43 Thickening of right colon and ischemic colitis.
Same patient as Figures 11-39 through 11-42. A, Axial CT with IV and oral contrast. B, Close-up from A. Bowel wall thickening is accompanied by an even more concerning finding—pneumatosis (air within the bowel wall). Normally, this finding is associated with bowel wall necrosis, usually in the face of ischemia. Remarkably, this patient recovered without bowel resection or revascularization, but pneumatosis should be treated as a possible surgical indication because of the extreme mortality of untreated mesenteric ischemia. Bowel wall thickening and inflammatory stranding may be seen in infectious, inflammatory, or ischemic colitis. Yersina, Campylobacter, and Salmonella have been described as causing pneumatosis.
Remember that air appears black on all CT window settings. Fat also appears nearly black on soft-tissue window settings. When in doubt, inspect the same slice using lung or bone window settings, as fat appears gray on these window settings. In this case, a standard soft-tissue window setting has been adjusted slightly to make fat brighter in appearance, thereby making black gas more evident.
If the patient has an absolute contraindication to administration of iodinated contrast, noncontrast CT can be performed to assess for mesenteric ischemia. There are no large trials of this approach. Several letters to the editors of radiology journals have commented on the ability to diagnose mesenteric ischemia based on the presence of mural pneumatosis, thickening of the bowel wall, free air, and fat stranding surrounding regions of the small bowel corresponding to vascular territories (see Figures 11-37 and 11-45).79-81 It is likely that these findings occur relatively late in the presentation, so although their presence may be helpful, their absence does not rule out the possibility of acute mesenteric ischemia. A red flag for mesenteric ischemia is a normal noncontrast abdominal CT in the presence of significant abdominal pain or concerning laboratory findings, such as profound leukocytosis, anion gap, or elevated lactate (Figure 11-36).
When ordering CT for evaluation of mesenteric ischemia, it is important to communicate the diagnostic concern to the radiologist and CT technician so that the CT can be performed appropriately. Modern protocols specifically tailored for evaluation of mesenteric ischemia have been developed.63,82-84 These use thin-section imaging through the region of the celiac, superior and inferior mesenteric, and middle colic arteries, as well as a rapid contrast bolus to ensure proper opacification of these vessels. Some protocols use arterial phase imaging to evaluate for acute arterial occlusion, followed by delayed images obtained approximately 60 seconds later to evaluate contrast filling of the mesenteric veins and portal venous system.82 Kirkpatrick et al.82 reported high sensitivity (96%) and specificity (94%) in a small study of 62 patients. Zandrino et al.85 reported sensitivity of 92% and specificity of 100% using a similar protocol. However, because of the rarity of mesenteric arterial occlusion and resulting small studies, wide confidence intervals exist around these point estimates. In addition, no studies to date have evaluated the interobserver variability in recognizing these findings. In the setting of intestinal ischemia associated with small-bowel obstruction, the prospective sensitivity of CT for detecting ischemic changes is relatively low in clinical practice (15%),86 in contrast to high sensitivity of CT in a pure research setting, which has been reported as high as 96%.87 This may reflect the increased vigilance of radiologists when assessing specifically for ischemic changes in a research study.
What Are the CT Findings of Mesenteric Ischemia?
The CT findings of acute mesenteric ischemia include arterial vascular occlusion with an intravascular filling defect similar to that observed with pulmonary embolism (see Figures 11-31 to 11-34 and 11-36). The normal celiac, superior mesenteric, and inferior mesenteric arteries fill uniformly with injected contrast. At their origins from the aorta, these are relatively large vessels with predictable locations. Failure of these vessels to fill, or partial filling, is generally readily recognized, and CT images correlate closely with formal angiography (see Figure 11-35). More distal branches are smaller and more difficult to assess. Secondary findings like bowel wall thickening, regional fat stranding, free air, and mural pneumatosis can be seen in advanced cases. Hypoperfused bowel may also fail to enhance with IV contrast. The portal venous system should be inspected for gas, which can also indicate mesenteric ischemia (Figures 11-38 to 11-40).88
Primary findings of a filling defect in mesenteric arteries are highly specific (see Figures 11-31 to 11-34 and 11-36). Unfortunately, some secondary CT findings of mesenteric ischemia are nonspecific and can sometimes be confused with those of inflammatory bowel disease such as Crohn’s disease or ulcerative colitis. In addition, infectious causes such as infectious enteritis can cause bowel wall thickening and fat stranding, similar in appearance to ischemic changes (Figures 11-41 to 11-43; see also Figure 11-46). However, it is essential that the clinician consider ischemia and avoid delay in surgical consultation if the presentation remotely suggests an ischemic cause. If mesenteric ischemia is mistaken for a less dire condition such as inflammatory bowel disease, the outcome can be disastrous (see Figure 11-36).
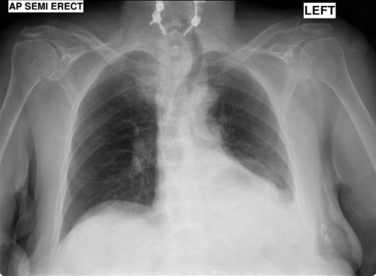
Figure 11-44 Mesenteric ischemia with free air: Nondiagnostic chest x-ray.
This 81-year-old female presented with diffuse abdominal pain and vomiting. Her electrocardiogram showed new atrial fibrillation, and her lactate level was elevated. A chest x-ray was performed and showed no pneumoperitoneum. Compare this x-ray with the CT in Figure 11-45.
How Sensitive Is Ultrasound for the Diagnosis of Mesenteric Ischemia? What Are the Ultrasound Findings?
Doppler ultrasound can be used to assess thrombosis or stenosis of the celiac artery and SMA. The proximal portions of these vessels at their origins from the aorta are readily seen on ultrasound. The examination can be technically difficult but is a reasonable initial approach in patients with contraindications to CT with IV contrast. In one prospective study of 100 patients, Moneta et al.89 reported that mesenteric duplex ultrasound was able to visualize 93% of superior mesenteric arteries and 83% of celiac arteries. Using a threshold of 70% or greater stenosis, duplex ultrasound was 92% sensitive and 96% specific for SMA stenosis and 87% sensitive and 80% specific for celiac stenosis. Danse et al.90 reported that Doppler ultrasound confirmed mesenteric ischemia in 8 of 21 patients (38%) and suggested ischemia in an additional 11 of 21 patients (52%)—although this study did not include blinding to other clinical data. More recently, Hata et al.19 assessed the performance of contrast-enhanced ultrasound for the diagnosis of bowel ischemia. In this study, patients with evidence of small-bowel dilatation were imaged using an injected ultrasound contrast agent. Rather than imaging blood vessels, the investigators assessed bowel wall for normal, diminished, or absent enhancement. The pooled sensitivity of diminished or absent enhancement was 85% (95% CI = 62%-97%), with a specificity of 100% (95% CI = 91%-100%). Contrast-enhanced ultrasound may gain a role in the assessment of unstable patients or those with contraindications to CT contrast agents.
How Sensitive Is Magnetic Resonance Imaging or Angiography for Mesenteric Ischemia?
MRI or MRA has excellent sensitivity and specificity for arterial mesenteric ischemia and for portal venous thrombosis.30,58,63,84 Gadolinium contrast is generally given.63,84 CT should be the first-line test because of higher spatial resolution and speed. Indications for MRI include nondiagnostic CT or contraindications for iodinated contrast, particularly severe allergy. Because mesenteric ischemia is extremely time dependent, no time should be wasted performing steroid prep for patients with iodinated contrast allergy (most protocols require 6 hours or more of delay); therefore, emergency MRI is sometimes required. Gadolinium is contraindicated in patients with renal insufficiency, as described later. In this circumstance, MRA can be performed without gadolinium contrast using special sequences as described earlier for aortic dissection—although the sensitivity of these sequences has not been extensively evaluated in mesenteric ischemia.
Variations in Mesenteric Ischemia
Ischemic Colitis
Ischemic colitis accounts for more than half of cases of intestinal ischemia, occurring in about 0.3% of acute hospital admissions. It particularly affects elderly patients with volume depletion and other medical illnesses. Ischemic colitis can also mimic infectious colitis such as Clostridium difficile colitis. Common features of ischemic colitis include hematochezia, abdominal pain, and diarrhea. Remarkably, many patients recover with IV fluid resuscitation and antibiotics. Nonetheless, morbidity is high, and mortality can occur in elderly patients with this condition. Emergent colectomy is sometimes required.91 Moreover, the presentation can be indistinguishable from SMA occlusion, so the same urgency of diagnostic evaluation is essential. Ischemic colitis has similar noncontrast CT findings, with thickening of the large-bowel wall, surrounding regional fat stranding, pneumatosis, and sometimes pneumoperitoneum (Figures 11-45 and 11-46; see also Figures 11-29, 11-30, and 11-37 to 11-43). CT with IV contrast should be used when possible, because this may reveal a filling defect in vessels supplying the affected large bowel.92 The findings are not specific and can mimic infectious colitis or inflammatory bowel disease.
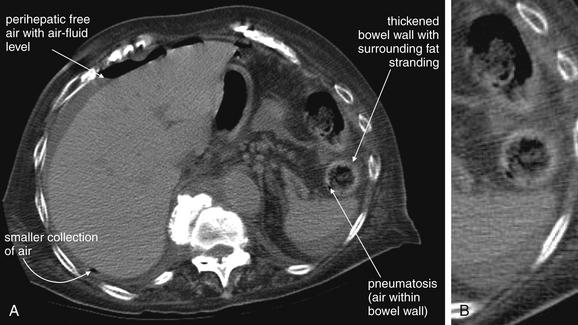
Figure 11-45 Ischemic colitis: CT without IV contrast.
A, Axial CT, viewed on soft-tissue windows. B, Close-up from A. Same patient as Figure 11-44. The patient’s presentation suggested mesenteric ischemia.
Because of the patient’s renal insufficiency, no IV contrast was given. Oral contrast was administered but did not progress beyond the small bowel before CT. This CT scan shows pneumoperitoneum, with a large amount of free air visible within a perihepatic fluid collection. Compare this with the chest x-ray in Figure 11-44, which showed no sign of pneumoperitoneum. Chest x-ray is relatively insensitive for pneumoperitoneum, whereas CT is exquisitely sensitive for this without any contrast agents. Also note the thickened descending colon with surrounding fat stranding. Pneumatosis is also visible in the wall of the descending colon, though no oral contrast has reached the colon. Laparotomy showed perforated ischemic colitis. The patient died of multiorgan failure and sepsis 4 days later.
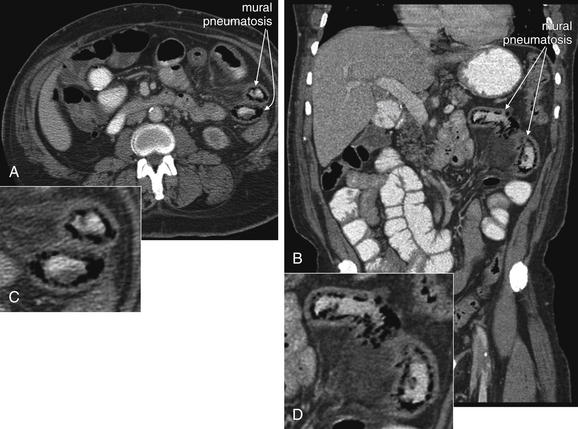
Figure 11-46 Pneumatosis: CT with oral and intravenous (IV) contrast.
This 56-year-old male with end-stage renal disease on hemodialysis, diabetes, and peripheral vascular disease presented with abdominal pain. He reported similar episodes managed with antibiotics.
His CT demonstrates pneumatosis intestinalis, concerning for ischemic bowel. Given his previous history, this patient was managed nonoperatively and improved with IV antibiotics (ciprofloxacin and metronidazole). CT findings of pneumatosis, though not specific for ischemic bowel, should prompt surgical consultation and consideration of surgical exploration. All panels are displayed with CT soft-tissue windows. Mesenteric ischemia has a mortality rate greater than 70%.
A, Axial view. B, Coronal view. C, Close-up from A. D, Close-up from B.
Chronic Mesenteric Ischemia
Chronic mesenteric ischemia has sometimes been called intestinal angina. Classically, the presentation is subacute or even chronic abdominal pain with a duration of weeks or even months. Patients develop weight loss and fear of eating, because they anticipate pain following a meal. Postprandial pain results from demand ischemia after a meal challenge. Pathologically, this is caused by stenosis of a mesenteric vessel, resulting in diminished blood flow. This is not unlike stable angina developing in a patient with coronary artery disease. The presentation can overlap substantially with other disease processes, including intra-abdominal malignancies with weight loss and chronic pain, chronic pancreatitis, and ulcer disease. The imaging workup is similar to acute mesenteric ischemia, with CT with IV contrast being the best test. CT is useful, because it can depict most other serious causes of abdominal pain, including malignancy, free air, appendicitis, diverticulitis, pancreatitis, and small-bowel obstruction. Ulcer disease is not well diagnosed by CT unless frank perforation has occurred, so a normal CT should not be considered to have eliminated the possibility. Because acute-on-chronic mesenteric ischemia can occur, a prodrome of several months of abdominal pain should not relieve the urgency to perform definitive imaging.
Portal Vein Thrombosis
The presentation of portal vein thrombosis is variable, likely because of the variety of underlying pathology that can result in the condition. Many patients develop portal vein thrombosis in the setting of other acute or chronic abdominal conditions, including malignancies or acute inflammatory and infectious conditions within the abdomen such as pancreatitis. Symptoms may reflect the underlying disease process more than the acute or chronic thrombosis of the portal vein. Primary portal vein thrombosis can occur, with abdominal pain being the predominant symptom. Hypercoagulable states can precipitate acute portal vein thrombosis. Portal vein thrombosis can be considered a type of deep venous thrombosis—“really deep vein thrombosis.” The peripartum state is also a risk factor, with risk persisting for as long as 2 months after delivery. The morbidity and mortality of portal vein thrombosis is high, partly reflecting the underlying causes. Many patients with this condition are older, with chronic comorbidities contributing to the morbidity and mortality of portal vein thrombosis. Significant thrombosis of the portal venous system can result in mesenteric or bowel infarction, and death. The treatment is systemic anticoagulation. Late complications include upper gastrointestinal bleeding caused by portal hypertension.93-95
Ultrasound of Portal Vein Thrombosis
Doppler ultrasound can reveal portal vein thrombosis. In cases of gross thrombosis of the portal vein, ultrasound without use of Doppler imaging can reveal a filling defect (Figure 11-47). The normal patent portal vein appears anechoic (black) on ultrasound. Clot within the portal vein can appear hypoechoic or anechoic acutely but usually becomes echogenic with time.96 Doppler imaging shows absence of flow in the portal vein. In cases of partial obstruction, some flow may be seen.
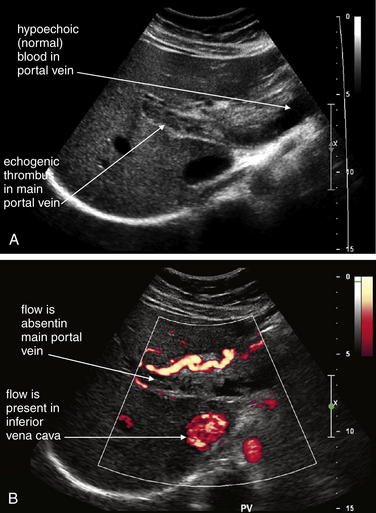
Figure 11-47 Portal vein thrombosis: Ultrasound.
This 22-year-old female, 2 months postpartum, presented with 1 week of right upper quadrant pain. Ultrasound was performed to evaluate for suspected cholecystitis or symptomatic cholelithiasis. Instead, portal vein thrombosis was discovered. The postpartum state is a risk factor for this condition. Hypercoagulable states and inflammatory or neoplastic abdominal conditions, including pancreatitis and abdominal malignancies, also can result in portal vein thrombosis.
A, Ultrasound grayscale image showing thrombus in the main portal vein.
B, Doppler ultrasound showing no flow within the portal vein.
Computed Tomography for Portal Vein Thrombosis
CT with IV contrast can be performed to diagnose portal vein thrombosis.97 Oral contrast is unnecessary and should not be used due to time delay. Ideally, CT should be performed with both arterial and portal venous phase images to rule out mesenteric arterial and venous thrombosis. This is accomplished by initiating CT scan early after contrast injection for arterial imaging. Additional CT images are then acquired after a delay of approximately 1 minute to allow filling of the portal venous system by the original injected contrast bolus. Portal venous thrombosis is marked by a failure of filling of the mesenteric and portal venous trees with IV contrast (Figure 11-48).97-99 The imaging findings are similar to those found in pulmonary embolism. Some contrast may be seen distal to the filling defect if thrombosis is incomplete. Signs of bowel ischemia may also be present, including bowel wall thickening and regional mesenteric fat stranding. Other diagnostic imaging findings include air in the portal venous system. Depending on the underlying cause, other findings may include acute pancreatitis, regional lymph nodes, or intra abdominal mass lesions.
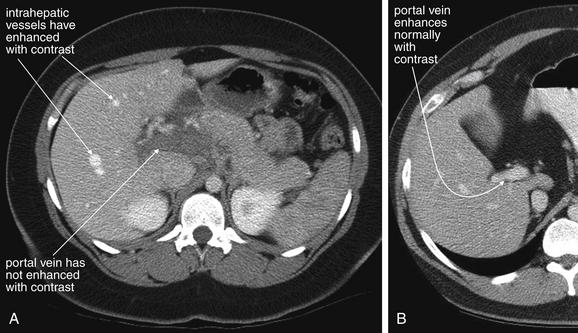
Figure 11-48 Portal vein thrombosis: CT with intravenous (IV) contrast.
A, Same patient as Figure 11-47, with thrombosis of the portal vein. Notice how other vessels, including the aorta and intrahepatic vessels, have enhanced with IV contrast. The portal vein remains dark in appearance, because it has not enhanced with contrast because of lack of blood flow. Compare with ultrasound in the prior figure. For the CT diagnosis of portal vein thrombosis, IV contrast must be used, and delayed images must be obtained approximately 1 minute after contrast injection. Images acquired earlier could show lack of enhancement of the portal vein—even when the vein is patent—if contrast has not yet reached the portal vein, falsely simulating thrombosis. B, CT image from another patient showing normal enhancement of the portal vein, ruling out thrombosis. An advantage of ultrasound over CT for this diagnosis is that ultrasound does not require contrast administration and does not involve radiation exposure. However, CT may show secondary complications of portal vein thrombosis such as bowel wall ischemic changes.
Bowel Ischemia Complicating Small-Bowel Obstruction
Bowel ischemia can complicate small-bowel obstruction. Frager et al.103 found that intestinal ischemia complicated 48% of cases of high-grade obstruction from adhesions or hernias undergoing surgery—although selection bias undoubtedly inflates this number above what would be observed in patients with lower grades of obstruction being managed medically. Several mechanisms may account for ischemia in the setting of bowel obstruction. Volvulus of a segment of intestine may occur, or tight adhesive bands may reduce blood flow within the wall of the intestine. The possibility of bowel ischemia is one of the key reasons for CT, regardless of the x-ray appearance, when small-bowel obstruction is suspected. For this indication, CT with IV contrast should be performed. Oral contrast is not necessary for the diagnosis of small-bowel obstruction or ischemia. Oral contrast may result in an unacceptable delay before imaging. Small-bowel obstruction is described in more detail in Chapter 9. Because a large vessel vascular occlusion is often not present, a filling defect should not be expected. A twisted vascular pedicle may be seen in some cases, with “whirling of the mesentery.” CT findings of small-bowel ischemia in the setting of small-bowel obstruction include thickening of bowel wall, stranding in surrounding fat, and decreased enhancement of a segment of the bowel following administration of IV contrast. Normally, the wall of well-perfused bowel enhances with IV contrast. When the blood supply is compromised, the bowel wall fails to enhance.104
In the pure research setting, CT has high sensitivity for the detection of ischemia complicating bowel obstruction. Mallo et al.105 performed a meta analysis suggesting a sensitivity for ischemia of 83% (range = 63% to 100%) and a specificity of 92% (range = 61% to 100%). However, these studies may inflate the actual sensitivity, because the interpreting radiologists are specifically attuned to the possibility of ischemia. In studies investigating the sensitivity of CT in the hands of clinical radiologists interpreting CT in the course of usual patient care, the sensitivity is far lower, only around 15%.86
What Is Contrast Nephropathy? Which Patients Are at Risk?
Contrast nephropathy is defined as a 25% increase in baseline serum creatinine or an absolute rise of 0.5 mg/dL following administration of parenteral iodinated contrast.106-107 It complicates 15% of contrast procedures, accounts for 10% of in-hospital renal failure, and affects more than 150,000 patients annually in the United States. Although a minority of these patients progress to permanent renal failure or require dialysis, contrast nephropathy is responsible for significant morbidity.106
Contrast nephropathy risk becomes significant at creatinine clearance rates below 60 mL per minute. Measured serum creatinine is a poor surrogate for creatinine clearance, because it is just one variable in the formula for creatinine clearance (Box 11-1), which is also affected by patient mass, age, gender, and race. In a study of 765 emergency department patients, of whom nearly 1 in 8 had a creatinine clearance rate of less than 60 mL per minute, a serum creatinine limit of 1.8 mg/dL missed 55% of at-risk patients.108 Even using a highly conservative limit of 1.0 mg/dL would have failed to identify 9% of at-risk patients—highlighting the importance of using creatinine clearance rather than measured serum creatinine.
How Can Contrast Nephropathy Be Prevented?
Multiple means of reducing the risk of contrast nephropathy have been investigated. Early work suggested a benefit to hydration with sodium bicarbonate,109 but a larger randomized, controlled trial showed no advantage over hydration with normal saline.110 N-acetyl cysteine has been shown in some trials to reduce the incidence of contrast nephropathy, but studies have not demonstrated improvements in patient-oriented outcomes such as need for dialysis.111 Most studies on N-acetyl cysteine focus on oral administration 24 hours before contrast administration and thus have no role in emergency department patients with suspected acute abdominal vascular catastrophes requiring immediate imaging. Only one study has investigated the use of IV N-acetyl cysteine 30 minutes before contrast administration and showed a small benefit.112
Low-osmolality and nonionic contrast agents have lower associated risks of contrast nephropathy than higher-osmolality and ionic contrast agents.113 Hydration with sodium chloride has been shown to reduce the risk of contrast nephropathy and should be used whenever possible, unless contraindicated by comorbidities such as heart failure or anuria.113-115 Reducing the volume of contrast administered is also beneficial.106
Reactions to Iodinated Contrast
A history of reaction to iodinated contrast is a relative contraindication to its administration. Reactions to iodinated contrast agents are likely not true allergies but are treated clinically like allergic reactions. Allergies to seafood are generally related to protein allergens, not iodine allergy; however, severe allergy to any allergen increases the risk of a contrast reaction. Consequently, iodinated contrast should be used with caution in patients with any history of severe allergic reaction. When abdominal vascular catastrophe is suspected, contrast allergies present a particular dilemma. Vascular catastrophes including AAA rupture, aortic dissection, and mesenteric ischemia are time dependent and life threatening, making delay for prophylactic treatment of allergy hazardous. The best strategy in this scenario is likely immediate noncontrast CT. As discussed in this chapter and in Chapter 9, noncontrast CT has been shown to be sensitive and specific for a range of key abdominal disorders, including AAA and AAA rupture, pneumoperitoneum, small-bowel obstruction, renal colic, appendicitis, diverticulitis, and pancreatitis. If noncontrast CT provides a definitive diagnosis, the patient can be spared the risk of injected iodinated contrast. If noncontrast CT is nondiagnostic, a tailored risk–benefit decision must be made for the individual patient, weighing the suspicion of acute vascular catastrophe against the severity of prior allergic or contrast reactions. Other diagnostic options, including laparotomy without definitive imaging, delayed CT to allow time for prophylactic steroid treatment, MRA, and Doppler or contrast-enhanced ultrasound, must be considered. However, given the
Box 11-1 Cockcroft-Gault Formula for Estimating Creatinine Clearance
A serum creatinine clearance (glomerular filtration) rate of less than 60 mL per minute predicts an increased risk of contrast nephropathy following administration of IV contrast. Other formulas exist. Online creatinine clearance calculators are available.
mortality and morbidity risk of vascular catastrophes, in some cases the decision to proceed with IV contrast administration must be made, with informed consent from the patient.
Several prophylactic steroid protocols have been endorsed by the American College of Radiology (ACR) in its Manual on Contrast Media (Box 11-2).116 Despite
Box 11-2 Emergency Prophylaxis Regimens to Attenuate or Prevent Reaction to Iodinated Contrast Media116
Lasser EC, Berry CC, Mishkin MM, et al. Pretreatment with corticosteroids to prevent adverse reactions to nonionic contrast media. AJR Am J Roentgenol 162:523-526, 1994.
∗ Diphenhydramine 50 mg intravenously 1 hour before contrast injection.
premedication, contrast reactions may occur. The evidence for benefit from premedication is relatively weak, based on small trials. The ACR recommends 6-hour pretreatment, with no study showing benefit from immediate steroid administration fewer than 3 hours before IV iodinated contrast.113 Unfortunately, such a delay is unacceptable if an abdominal vascular catastrophe is strongly suspected.
Magnetic Resonance Imaging and Gadolinium-Associated Fatal Nephrogenic Systemic Fibrosis
Gadolinium contrast used in MRI is strongly contraindicated in patients with renal insufficiency, because it has been recently associated with the development of fatal nephrogenic systemic fibrosis (NSF), discussed extensively in Chapter 15.117 The risks of NSF must be weighed against the risks of iodinated contrast for CT and a potentially fatal abdominal vascular catastrophe. Overall, the risk of NSF is very low after standard doses of gadolinium, occurring in none of more than 74,000 patients in one study.118 Higher doses of gadolinium were associated with an overall risk of 0.17%, with all cases occurring in patients with glomerular filtration rates less than 30 mL per minute. In chronic dialysis patients, the risk was 0.4%. Patients with acute renal failure not receiving dialysis were at high risk, between 8% and 19%—and thus represent a group where gadolinium should be avoided whenever possible.118 Dialysis patients and patients with acute renal failure should undergo dialysis immediately following MRI if possible to eliminate gadolinium.119 This is in distinction to the scenario with iodinated contrast for CT, in which dialysis patients are not at risk of renal injury from contrast, as complete kidney failure is already present. Dialysis is not urgently needed following iodinated contrast administration.
Summary
Abdominal vascular catastrophes must be considered early in the evaluation of patients with abdominal and back pain. Hemodynamic stability does not rule out a life-threatening vascular process, and imaging should be performed as quickly as possible before hemodynamic compromise. X-rays play little role and generally be should be avoided, with the occasional exception of upright chest x-ray to assess for free air. Ultrasound is a rapid and useful bedside screening modality for the presence of AAA. CT is the most rapid and definitive emergency department test for AAA rupture, aortic dissection, and mesenteric ischemia; oral contrast is not needed, though IV contrast is important to the diagnosis of aortic dissection, mesenteric ischemia, and active aortic aneurysm bleeding. Rarely, other modalities, including MRA, may be useful in stable patients with contraindications to CT.
1. Heron M., Hoyert D.L., Murphy S.L., et al. Deaths: Final data for 2006. Natl Vital Stat Rep. 2009;57:1-134.
2. Brown P.M., Zelt D.T., Sobolev B. The risk of rupture in untreated aneurysms: The impact of size, gender, and expansion rate. J Vasc Surg. 2003;37:280-284.
3. Lederle F.A., Johnson G.R., Wilson S.E., et al. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA. 2002;287:2968-2972.
4. Lederle F.A., Johnson G.R., Wilson S.E., et al. The aneurysm detection and management study screening program: Validation cohort and final results. Aneurysm Detection and Management Veterans Affairs Cooperative Study Investigators. Arch Intern Med. 2000;160:1425-1430.
5. Lloyd G.M., Bown M.J., Norwood M.G., et al. Feasibility of preoperative computer tomography in patients with ruptured abdominal aortic aneurysm: A time-to-death study in patients without operation. J Vasc Surg. 2004;39:788-791.
6. Rutledge R., Oller D.W., Meyer A.A., Johnson G.J.Jr. A statewide, population-based time-series analysis of the outcome of ruptured abdominal aortic aneurysm. Ann Surg. 1996;223:492-502. discussion 503-5
7. Kiell C.S., Ernst C.B. Advances in management of abdominal aortic aneurysm. Adv Surg. 1993;26:73-98.
8. Lederle F.A., Simel D.L. The rational clinical examination: Does this patient have abdominal aortic aneurysm? JAMA. 1999;281:77-82.
9. Marston W.A., Ahlquist R., Johnson G.Jr., Meyer A.A. Misdiagnosis of ruptured abdominal aortic aneurysms. J Vasc Surg. 1992;16:17-22.
10. Lederle F.A., Parenti C.M., Chute E.P. Ruptured abdominal aortic aneurysm: The internist as diagnostician. Am J Med. 1994;96:163-167.
11. Gaughan M., McIntosh D., Brown A., Laws D. Emergency abdominal aortic aneurysm presenting without haemodynamic shock is associated with misdiagnosis and delay in appropriate clinical management. Emerg Med J. 2009;26:334-339.
12. Eckford S.D., Gillatt D.A. Abdominal aortic aneurysms presenting as renal colic. Br J Urol. 1992;70:496-498.
13. Garra G., Singer A.J., Bamber D., et al. Pretreatment of patients requiring oral contrast abdominal computed tomography with antiemetics: A randomized controlled trial of efficacy. Ann Emerg Med. 2009;53:528-533.
14. Shuman W.P., Hastrup W.Jr., Kohler T.R., et al. Suspected leaking abdominal aortic aneurysm: Use of sonography in the emergency room. Radiology. 1988;168:117-119.
15. Tayal V.S., Graf C.D., Gibbs M.A. Prospective study of accuracy and outcome of emergency ultrasound for abdominal aortic aneurysm over two years. Acad Emerg Med. 2003;10:867-871.
16. Costantino T.G., Bruno E.C., Handly N., Dean A.J. Accuracy of emergency medicine ultrasound in the evaluation of abdominal aortic aneurysm. J Emerg Med. 2005;29:455-460.
17. Knaut A.L., Kendall J.L., Patten R., Ray C. Ultrasonographic measurement of aortic diameter by emergency physicians approximates results obtained by computed tomography. J Emerg Med. 2005;28:119-126.
18. Kuhn M., Bonnin R.L., Davey M.J., et al. Emergency department ultrasound scanning for abdominal aortic aneurysm: Accessible, accurate, and advantageous. Ann Emerg Med. 2000;36:219-223.
19. Hata J., Kamada T., Haruma K., Kusunoki H. Evaluation of bowel ischemia with contrast-enhanced US: Initial experience. Radiology. 2005;236:712-715.
20. Catalano O., Sandomenico F., Raso M.M., Siani A. Real-time, contrast-enhanced sonography: A new tool for detecting active bleeding. J Trauma. 2005;59:933-939.
21. Catalano O., Lobianco R., Sandomenico F., et al. Real-time, contrast-enhanced sonographic imaging in emergency radiology. Radiol Med. 2004;108:454-469.
22. Catalano O., Lobianco R., Cusati B., Siani A. Contrast-enhanced sonography for diagnosis of ruptured abdominal aortic aneurysm. AJR Am J Roentgenol. 2005;184:423-427.
23. Clevert D.A., Minaifar N., Weckbach S., et al. Color duplex ultrasound and contrast-enhanced ultrasound in comparison to MS-CT in the detection of endoleak following endovascular aneurysm repair. Clin Hemorheol Microcirc. 2008;39:121-132.
24. Seeger J.M., Kieffer R.W. Preoperative CT in symptomatic abdominal aortic aneurysms: Accuracy and efficacy. Am Surg. 1986;52:87-90.
25. Weinbaum F.I., Dubner S., Turner J.W., Pardes J.G. The accuracy of computed tomography in the diagnosis of retroperitoneal blood in the presence of abdominal aortic aneurysm. J Vasc Surg. 1987;6:11-16.
26. Rosen A., Korobkin M., Silverman P.M., et al. CT diagnosis of ruptured abdominal aortic aneurysm. AJR Am J Roentgenol. 1984;143:265-268.
27. Siegel C.L., Cohan R.H. CT of abdominal aortic aneurysms. AJR Am J Roentgenol. 1994;163:17-29.
28. Schwartz S.A., Taljanovic M.S., Smyth S., et al. CT findings of rupture, impending rupture, and contained rupture of abdominal aortic aneurysms. AJR Am J Roentgenol. 2007;188:W57-W62.
29. Mehard W.B., Heiken J.P., Sicard G.A. High-attenuating crescent in abdominal aortic aneurysm wall at CT: A sign of acute or impending rupture. Radiology. 1994;192:359-362.
30. Vosshenrich R., Fischer U. Contrast-enhanced MR angiography of abdominal vessels: Is there still a role for angiography? Eur Radiol. 2002;12:218-230.
31. Peppelenbosch N., Geelkerken R.H., Soong C., et al. Endograft treatment of ruptured abdominal aortic aneurysms using the Talent aortouniiliac system: An international multicenter study. J Vasc Surg. 2006;43:1111-1123. discussion 1123
32. Ritz J.P., Germer C.T., Buhr H.J. Prognostic factors for mesenteric infarction: Multivariate analysis of 187 patients with regard to patient age. Ann Vasc Surg. 2005;19:328-334.
33. Makaroun M., Zajko A., Sugimoto H., et al. Fate of endoleaks after endoluminal repair of abdominal aortic aneurysms with the EVT device. Eur J Vasc Endovasc Surg. 1999;18:185-190.
34. Iezzi R., Cotroneo A.R., Filippone A., et al. Multidetector-row computed tomography angiography in abdominal aortic aneurysm treated with endovascular repair: Evaluation of optimal timing of delayed phase imaging for the detection of low-flow endoleaks. J Comput Assist Tomogr. 2008;32:609-615.
35. Iezzi R., Cotroneo A.R., Filippone A., et al. Multidetector CT in abdominal aortic aneurysm treated with endovascular repair: Are unenhanced and delayed phase enhanced images effective for endoleak detection? Radiology. 2006;241:915-921.
36. Hong C., Heiken J.P., Sicard G.A., et al. Clinical significance of endoleak detected on follow-up CT after endovascular repair of abdominal aortic aneurysm. AJR Am J Roentgenol. 2008;191:808-813.
37. McWilliams R.G., Martin J., White D., et al. Detection of endoleak with enhanced ultrasound imaging: Comparison with biphasic computed tomography. J Endovasc Ther. 2002;9:170-179.
38. Upchurch G.R.Jr., Nienaber C., Fattori R., et al. Acute aortic dissection presenting with primarily abdominal pain: A rare manifestation of a deadly disease. Ann Vasc Surg. 2005;19:367-373.
39. Trimarchi S., Tsai T., Eagle K.A., et al. Acute abdominal aortic dissection: Insight from the International Registry of Acute Aortic Dissection (IRAD). J Vasc Surg. 2007;46:913-919.
40. Suzuki T., Mehta R.H., Ince H., et al. Clinical profiles and outcomes of acute type B aortic dissection in the current era: Lessons from the International Registry of Aortic Dissection (IRAD). Circulation. 2003;108(Suppl 1):II312-II317.
41. Singh S., Trivedi A., Adhikari T., et al. Cocaine-related acute aortic dissection: Patient demographics and clinical outcomes. Can J Cardiol. 2007;23:1131-1134.
42. Daniel J.C., Huynh T.T., Zhou W., et al. Acute aortic dissection associated with use of cocaine. J Vasc Surg. 2007;46:427-433.
43. Luker G.D., Glazer H.S., Eagar G., et al. Aortic dissection: Effect of prospective chest radiographic diagnosis on delay to definitive diagnosis. Radiology. 1994;193:813-819.
44. Pesola G.R., Pesola H.R., Lin M., et al. The normal difference in bilateral indirect blood pressure recordings in hypertensive individuals. Acad Emerg Med. 2002;9:342-345.
45. Ohlmann P., Faure A., Morel O., et al. Diagnostic and prognostic value of circulating D-dimers in patients with acute aortic dissection. Crit Care Med. 2006;34:1358-1364.
46. Sbarouni E., Georgiadou P., Marathias A., et al. D-dimer and BNP levels in acute aortic dissection. Int J Cardiol. 2007;122:170-172.
47. Weber T., Hogler S., Auer J., et al. D-dimer in acute aortic dissection. Chest. 2003;123:1375-1378.
48. Sodeck G., Domanovits H., Schillinger M., et al. D-dimer in ruling out acute aortic dissection: A systematic review and prospective cohort study. Eur Heart J. 2007;28:3067-3075.
49. Perez A., Abbet P., Drescher M.J. D-dimers in the emergency department evaluation of aortic dissection. Acad Emerg Med. 2004;11:397-400.
50. Akutsu K., Sato N., Yamamoto T., et al. A rapid bedside D-dimer assay (cardiac D-dimer) for screening of clinically suspected acute aortic dissection. Circ J. 2005;69:397-403.
51. Hazui H., Fukumoto H., Negoro N., et al. Simple and useful tests for discriminating between acute aortic dissection of the ascending aorta and acute myocardial infarction in the emergency setting. Circ J. 2005;69:677-682.
52. Eggebrecht H., Naber C.K., Bruch C., et al. Value of plasma fibrin D-dimers for detection of acute aortic dissection. J Am Coll Cardiol. 2004;44:804-809.
53. Marill K.A. Serum D-dimer is a sensitive test for the detection of acute aortic dissection: A pooled meta-analysis. J Emerg Med. 2008;34:367-376.
54. Sutherland A., Escano J., Coon T.P. D-dimer as the sole screening test for acute aortic dissection: A review of the literature. Ann Emerg Med. 2008;52:339-343.
55. VanderLinden C. Towards evidence based emergency medicine: Best BETs from the Manchester Royal Infirmary. Detection of acute thoracic aortic dissection with D-dimer. Emerg Med J. 2007;24:846-847.
56. Clevert D.A., Horng A., Jung E.M., et al. Contrast-enhanced ultrasound versus conventional ultrasound and MS-CT in the diagnosis of abdominal aortic dissection. Clin Hemorheol Microcirc. 2009;43:129-139.
57. Demos T.C., Posniak H.V., Churchill R.J. Detection of the intimal flap of aortic dissection on unenhanced CT images. AJR Am J Roentgenol. 1986;146:601-603.
58. Venkataraman S., Semelka R.C., Weeks S., et al. Assessment of aorto-iliac disease with magnetic resonance angiography using arterial phase 3-D gradient–echo and interstitial phase 2-D fat-suppressed spoiled gradient–echo sequences. J Magn Reson Imaging. 2003;17:43-53.
59. Liu Q., Lu J.P., Wang F., et al. Three-dimensional contrast-enhanced MR angiography of aortic dissection: A pictorial essay. Radiographics. 2007;27:1311-1321.
60. De Cicco M.L., Andreoli C., Casciani E., et al. Steady state evaluation of aortic dissections: A feasibility study. Radiol Med. 2005;110:523-531.
61. Gebker R., Gomaa O., Schnackenburg B., et al. Comparison of different MRI techniques for the assessment of thoracic aortic pathology: 3D contrast enhanced MR angiography, turbo spin echo and balanced steady state free precession. Int J Cardiovasc Imaging. 2007;23:747-756.
62. Acosta S., Bjorck M. Acute thrombo-embolic occlusion of the superior mesenteric artery: A prospective study in a well defined population. Eur J Vasc Endovasc Surg. 2003;26:179-183.
63. Shih M.C., Hagspiel K.D. CTA and MRA in mesenteric ischemia: I. Role in diagnosis and differential diagnosis. AJR Am J Roentgenol. 2007;188:452-461.
64. Acosta S., Ogren M., Sternby N.H., et al. Incidence of acute thrombo-embolic occlusion of the superior mesenteric artery: A population-based study. Eur J Vasc Endovasc Surg. 2004;27:145-150.
65. Edwards M.S., Cherr G.S., Craven T.E., et al. Acute occlusive mesenteric ischemia: Surgical management and outcomes. Ann Vasc Surg. 2003;17:72-79.
66. Deehan D.J., Heys S.D., Brittenden J., Eremin O. Mesenteric ischaemia: Prognostic factors and influence of delay upon outcome. J R Coll Surg Edinb. 1995;40:112-115.
67. Lange H., Jackel R. Usefulness of plasma lactate concentration in the diagnosis of acute abdominal disease. Eur J Surg. 1994;160:381-384.
68. Merle C., Lepouse C., De Garine A., et al. Surgery for mesenteric infarction: Prognostic factors associated with early death within 72 hours. J Cardiothorac Vasc Anesth. 2004;18:734-741.
69. Taylor B.M., Jamieson W.G., Durand D. Preinfarction diagnosis of acute mesenteric ischemia by simple measurement of inorganic phosphate in body fluids. Can J Surg. 1979;22:40-45.
70. Sodhi D., Arora N. Serum inorganic phosphate levels in experimental intestinal ischaemia. Indian J Med Sci. 1993;47:259-263.
71. Lores M.E., Canizares O., Rossello P.J. The significance of elevation of serum phosphate levels in experimental intestinal ischemia. Surg Gynecol Obstet. 1981;152:593-596.
72. Jamieson W.G., Lozon A., Durand D., Wall W. Changes in serum phosphate levels associated with intestinal infarction and necrosis. Surg Gynecol Obstet. 1975;140:19-21.
73. May L.D., Berenson M.M. Value of serum inorganic phosphate in the diagnosis of ischemic bowel disease. Am J Surg. 1983;146:266-268.
74. Gorey T.F., O’Sullivan M. Prognostic factors in extensive mesenteric ischaemia. Ann R Coll Surg Engl. 1988;70:191-194.
75. Wolf E.L., Sprayregen S., Bakal C.W. Radiology in intestinal ischemia: Plain film, contrast, and other imaging studies. Surg Clin North Am. 1992;72:107-124.
76. Grassi R., Pinto A., Romano L., et al. [Twenty-six consecutive patients with acute superior mesenteric infarction. Comparison of conventional radiology, ultrasonography, and computerized tomography]. Radiol Med (Torino). 1997;93:699-703.
77. Smerud M.J., Johnson C.D., Stephens D.H. Diagnosis of bowel infarction: A comparison of plain films and CT scans in 23 cases. AJR Am J Roentgenol. 1990;154:99-103.
78. Pear B.L. Pneumatosis intestinalis: A review. Radiology. 1998;207:13-19.
79. De Filippo M., Sverzellati N., Zompatori M. Unenhanced CT in patients with chronic renal failure with clinical suspicion of small-bowel infarct. AJR Am J Roentgenol. 192, 2009. W266
80. De Filippo M., Sagone C., Zompatori M. Unenhanced MDCT findings of acute bowel ischemia. AJR Am J Roentgenol. 190, 2008. W271
81. Kim A.Y. Reply to Unenhanced MDCT findings of acute bowel ischemia. AJR Am J Roentgenol. 190, 2008. W283
82. Kirkpatrick I.D., Kroeker M.A., Greenberg H.M. Biphasic CT with mesenteric CT angiography in the evaluation of acute mesenteric ischemia: Initial experience. Radiology. 2003;229:91-98.
83. Fleischmann D. Multiple detector-row CT angiography of the renal and mesenteric vessels. Eur J Radiol. 2003;45(Suppl 1):S79-S87.
84. Shih M.C., Angle J.F., Leung D.A., et al. CTA and MRA in mesenteric ischemia: II. Normal findings and complications after surgical and endovascular treatment. AJR Am J Roentgenol. 2007;188:462-471.
85. Zandrino F., Musante F., Gallesio I., Benzi L. Assessment of patients with acute mesenteric ischemia: Multislice computed tomography signs and clinical performance in a group of patients with surgical correlation. Minerva Gastroenterol Dietol. 2006;52:317-325.
86. Sheedy S.P., Earnest F.T., Fletcher J.G., et al. CT of small-bowel ischemia associated with obstruction in emergency department patients: Diagnostic performance evaluation. Radiology. 2006;241:729-736.
87. Zalcman M., Sy M., Donckier V., et al. Helical CT signs in the diagnosis of intestinal ischemia in small-bowel obstruction. AJR Am J Roentgenol. 2000;175:1601-1607.
88. Martinez J.L., Gonzalez-Acosta J. Portal venous gas: Report of three cases. Ann Hepatol. 2009;8:151-155.
89. Moneta G.L., Lee R.W., Yeager R.A., Taylor L.M.Jr., Porter J.M. Mesenteric duplex scanning: A blinded prospective study. J Vasc Surg. 1993;17:79-84. discussion 85-6
90. Danse E.M., Laterre P.F., Van Beers B.E., et al. Early diagnosis of acute intestinal ischaemia: Contribution of colour Doppler sonography. Acta Chir Belg. 1997;97:173-176.
91. Elder K., Lashner B.A., Al Solaiman F. Clinical approach to colonic ischemia. Cleve Clin J Med. 2009;76:401-409.
92. Taourel P., Aufort S., Merigeaud S., et al. Imaging of ischemic colitis. Radiol Clin North Am. 2008;46:909-924. vi
93. Chawla Y., Duseja A., Dhiman R.K. Review article: The modern management of portal vein thrombosis. Aliment Pharmacol Ther. 2009;30:881-894.
94. Primignani M. Portal vein thrombosis, revisited. Dig Liver Dis. 2009.
95. Plessier A., Darwish-Murad S., Hernandez-Guerra M., et al. Acute portal vein thrombosis unrelated to cirrhosis: A prospective multicenter follow-up study. Hepatology. 51(1), 2010. 210-218
96. Saad W.E., Lin E., Ormanoski M., et al. Noninvasive imaging of liver transplant complications. Tech Vasc Interv Radiol. 2007;10:191-206.
97. Lee H.K., Park S.J., Yi B.H., et al. Portal vein thrombosis: CT features. Abdom Imaging. 2008;33:72-79.
98. Agarwal A., Jain M. Multidetector CT portal venography in evaluation of portosystemic collateral vessels. J Med Imaging Radiat Oncol. 2008;52:4-9.
99. Rossi S., Ghittoni G., Ravetta V., et al. Contrast-enhanced ultrasonography and spiral computed tomography in the detection and characterization of portal vein thrombosis complicating hepatocellular carcinoma. Eur Radiol. 2008;18:1749-1756.
100. Smith C.S., Sheehy N., McEniff N., Keogan M.T. Magnetic resonance portal venography: Use of fast-acquisition true FISP imaging in the detection of portal vein thrombosis. Clin Radiol. 2007;62:1180-1188.
101. Wilson M.W., LaBerge J.M., Kerlan R.K., et al. MR portal venography: Preliminary results of fast acquisition without contrast material or breath holding. Acad Radiol. 2002;9:1179-1184.
102. Laissy J.P., Trillaud H., Douek P. MR angiography: Noninvasive vascular imaging of the abdomen. Abdom Imaging. 2002;27:488-506.
103. Frager D., Baer J.W., Medwid S.W., et al. Detection of intestinal ischemia in patients with acute small-bowel obstruction due to adhesions or hernia: Efficacy of CT. AJR Am J Roentgenol. 1996;166:67-71.
104. Frager D., Medwid S.W., Baer J.W., et al. CT of small-bowel obstruction: Value in establishing the diagnosis and determining the degree and cause. AJR Am J Roentgenol. 1994;162:37-41.
105. Mallo R.D., Salem L., Lalani T., Flum D.R. Computed tomography diagnosis of ischemia and complete obstruction in small bowel obstruction: A systematic review. J Gastrointest Surg. 2005;9:690-694.
106. Barrett B.J., Parfrey P.S. Clinical practice: Preventing nephropathy induced by contrast medium. N Engl J Med. 2006;354:379-386.
107. McCullough P.A., Adam A., Becker C.R., et al. Epidemiology and prognostic implications of contrast-induced nephropathy. Am J Cardiol. 2006;98:5K-13K.
108. Band R.A., Gaieski D.F., Mills A.M., et al. Discordance between serum creatinine and creatinine clearance for identification of ED patients with abdominal pain at risk for contrast-induced nephropathy. Am J Emerg Med. 2007;25:268-272.
109. Merten G.J., Burgess W.P., Gray L.V., et al. Prevention of contrast-induced nephropathy with sodium bicarbonate: A randomized controlled trial. JAMA. 2004;291:2328-2334.
110. Brar S.S., Shen A.Y., Jorgensen M.B., et al. Sodium bicarbonate vs sodium chloride for the prevention of contrast medium-induced nephropathy in patients undergoing coronary angiography: A randomized trial. JAMA. 2008;300:1038-1046.
111. Alonso A., Lau J., Jaber B.L., et al. Prevention of radiocontrast nephropathy with N-acetylcysteine in patients with chronic kidney disease: A meta-analysis of randomized, controlled trials. Am J Kidney Dis. 2004;43:1-9.
112. Baker C.S., Wragg A., Kumar S., et al. A rapid protocol for the prevention of contrast-induced renal dysfunction: The RAPPID study. J Am Coll Cardiol. 2003;41:2114-2118.
113. Morcos S.K., Thomsen H.S. Adverse reactions to iodinated contrast media. Eur Radiol. 2001;11:1267-1275.
114. Trivedi H.S., Moore H., Nasr S., et al. A randomized prospective trial to assess the role of saline hydration on the development of contrast nephrotoxicity. Nephron Clin Pract. 2003;93:C29-C34.
115. Krasuski R.A., Beard B.M., Geoghagan J.D., et al. Optimal timing of hydration to erase contrast-associated nephropathy: The OTHER CAN study. J Invasive Cardiol. 2003;15:699-702.
116. ACR Committee on Drugs and Contrast Media: Manual on Contrast Media, version 7. American College of Radiology, 2010. (Accessed at http://www.acr.org/SecondaryMainMenuCategories/quality_safety/contrast_manual/FullManual.aspx.)
117. Grobner T. Gadolinium: A specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant. 2006;21:1104-1108.
118. Prince M.R., Zhang H., Morris M., et al. Incidence of nephrogenic systemic fibrosis at two large medical centers. Radiology. 2008;248:807-816.
119. Kanal E., Barkovich A.J., Bell C., et al. ACR guidance document for safe MR practices. AJR Am J Roentgenol. 2007;2007(188):1447-1474.
120. Greenberger P.A., Patterson R. The prevention of immediate generalized reactions to radiocontrast media in high-risk patients. J Allergy Clin Immunol. 1991;87:867-872.
121. Greenberger P.A., Patterson R., Tapio C.M. Prophylaxis against repeated radiocontrast media reactions in 857 cases: Adverse experience with cimetidine and safety of beta-adrenergic antagonists. Arch Intern Med. 1985;145:2197-2200.