Kinesiology
After completing this chapter, the student will be able to perform the following:
1 Apply principles of kinesiology to sports massage outcomes.
2 Describe the relationship of connective tissue to normal and abnormal movement.
5 Demonstrate normal and abnormal range of motion.
6 Describe two types of joint stability.
7 Identify joint capsule fibrosis.
8 Explain response to synovial membrane injury.
9 Describe the structure and function of cartilage.
10 Identify the location of bursae and explain bursitis.
11 Explain joint degeneration.
12 Demonstrate joint mobilization.
13 Describe the structure and function of the muscle organ.
14 Demonstrate three types of muscle actions resulting in five types of function.
15 Explain the muscle length-tension relationship.
16 Describe five reflexive muscle actions.
17 Define kinetic chain and multiplanar movement.
18 Explain and locate four muscular functional subsystems.
19 Explain full-body pronation and supination.
20 Define serial distortion patterns and synergistic dominance.
Kinesiology
Athletes move; therefore, the massage therapist who works with athletes needs to understand kinesiology. Kinesiology for the purposes of this text is the study of body movement and the factors that limit or enhance the capacity to move, which affects performance. Kinesiology is a multidisciplinary science encompassing anatomy, biomechanics, and physiology. An understanding of kinesiology will become an integral part of the assessment process for athletes, beginning with identifying fitness-based normal function as a foundation. This knowledge supports massage application during sport-specific training programs to develop optimal performance function. Finally, an understanding of kinesiology is necessary to identify pathologic movement, compensation caused by injury, and the effects that injury has on movement. This chapter targets functional relationships among bones, connective tissues, joints, fasciae, and muscles.
As mentioned in Chapter 1, it is expected that the fundamental elements of anatomy and physiology are in place, and that you, the reader, will take the next step toward understanding the real element of kinesiology, which is movement. Movement is a process for athletes. Athletic movement begins with a stable, strong, yet dynamic and flexible posture. Athletes are constantly balancing necessary stability and strength with flexibility and agility.
Kinesiology is the science of the study of movement and of active and passive structures involved, including bones, joints, muscle tissues, and all associated connective tissues. Elements of kinesiology include the following:
• Stability is required to provide a stable base for functioning. Usually, stability concerns are focused on proximal musculature in the trunk, shoulders, and hips to allow for movement of the extremities. Stability is required before there can be balance.
• Balance is the ability to execute complex patterns of movement with the right timing and sequencing. Balance is essential to motor function, as is the ability to maintain one’s center of gravity over the available base of support.
• Coordination is the efficient execution of a movement. Usually, coordination involves motor learning and practice.
• Endurance (lasting power) is based on efficiency and stamina.
• Agility is the ability to move and change direction and position of the body quickly and effectively while under control.
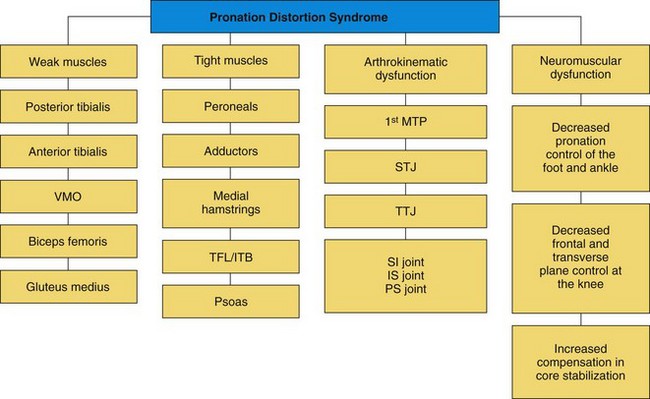
An important development in biomechanics research is the concept of the kinetic chain (also known as the kinetic link). This concept came out of mechanical engineering in the 1970s and was applied to biomechanics. The kinetic chain describes the body as a linked system of interdependent segments. By understanding their relationships to each other, we can maximize the effectiveness of massage application with an understanding of the importance of whole-body massage rather than isolated spot work. The diagram in Figure 4-1 illustrates the common areas of interrelated kinetic chain function. Follow the colored line to locate the interconnections.
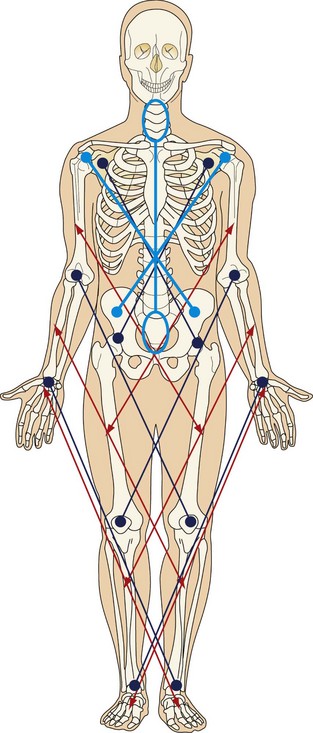
FIGURE 4-1 Areas of symmetry: arm-thigh; forearm-leg; hand-foot; shoulder-hip; elbow-knee; wrist-ankle; cervix-sacrum; shoulder girdle-pelvic girdle.
Beginning from the understanding that the body moves in an integrated fashion, let’s consider some of the individual elements, beginning with the integrative tissue—connective tissue.
Connective Tissue
Chapter 3 presented the research on fascia. Now we will review and explore the relevance of the connective tissue anatomy and physiology to massage therapy application.
Connective tissue is made up of ground substance and fibers. Connective tissue consists of hard and soft tissues. It forms the structure of the organs and blood vessels and binds joints together through ligaments and joint capsules. It transmits the pull of muscles through connective tissue surrounding the muscles and the tendons. It forms tensegretic tension lines that transverse the body in many directions.
Collagen
Collagen forms approximately 80% of tendons, ligaments, and joint capsules, and a large percentage of cartilage and bone, giving shape to the soft tissue. It forms the structural support of the skin, muscles, blood vessels, and nerve fibers. Normal stresses, in the form of exercise and activities of daily living, increase collagen synthesis and strengthen connective tissue. This is an important aspect of fitness, especially for the elderly.
Collagen stabilizes the joints through the ligaments, joint capsules, and periosteum by resisting the tension or pulling force transmitted through the joints by movement or gravity. Collagen transmits the pulling force of muscle contraction through the fascia within the muscle and the tendon attachment. The collagen fibers tend to orient to parallel and longitudinal alignment along the lines of mechanical stress imposed through loading of the tissue during activity. Normal gliding of collagen fibers is maintained by movement and lubrication from connective tissue ground substance.
Immobilization or lack of use decreases collagen production, leading to atrophy in the connective tissue and to osteoporosis in the bone. Without movement, collagen is laid down in a random orientation, with fibers packed close together and forming microadhesions. Adhesions are abnormal deposits of connective tissue between gliding surfaces (Figure 4-2). This atrophy with random orientation of fibers creates weakness in the tissue and instability of the associated joint. This condition is more common in those who are just beginning a fitness and performance regimen and increases injury potential. The aging process decreases the amount and quality of the collagen structure; therefore, exercise helps prevent age-related soft tissue dysfunction.
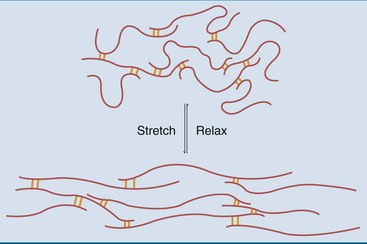
FIGURE 4-2 Adhesions are abnormal deposits of connective tissue between gliding surfaces. (From Meisenberg G: Principles of medical biochemistry, ed 3, St Louis, 2012, Saunders.)
Excessive mechanical and repetitive stress results in excessive deposits of collagen, causing abnormal cross-fiber links and adhesions. The fibers pack closer together, lubrication is decreased, and the water content of ground substance is reduced. This in turn decreases the ability of fibers and fascicles to slide relative to each other. This condition is often called fibrosis. Adhesions and fibrosis create a resistance to normal electrical flow. This decrease in electrical currents conducted in the connective tissues interferes with the normal repair and rejuvenation process.
Athletes are prone to excessive mechanical stress during practices and performance activity and to repetitive strain from the athlete’s specific activities, such as throwing, hitting, jumping, and running. Massage mechanically deforms the collagen fibers by introducing bind, shear, torsion, compression, and tension forces. Piezoelectricity is the ability of a tissue to generate electrical potentials in response to pressure of mechanical deformation. It is a property of most, if not all, living tissues. Piezoelectric potentials direct collagen fiber formation. Also, the negative charge in the soft tissue is increased, and this has a strong proliferative effect, stimulating the creation of new cells to repair an injured site.
Injury results in an acute inflammatory response. During the acute and subacute repair phases of the healing process, connective tissue fibers are laid down in a random orientation, instead of along normal lines of force. In essentially the same process of fibrotic change discussed earlier, the fibers pack closer together, forming abnormal cross-fiber links and adhesions. These adhesions can occur at every level of the soft tissue, including in the ligament or tendon adhering to the bone or between the fascicles, the fibers themselves, or individual muscle layers. In athletes, it is common to find first- and second-layer muscle adhesions, such as gastrocnemius/soleus and pectoralis major/pectoralis minor.
Because adhesions decrease tissue extensibility, the tissue becomes less elastic, thicker, and shorter. Clients often feel stiff in the area of adhered and fibrotic tissue.
Tendons
Tendons represent a continuation of connective tissue within the muscle. Tendons consist of long, spiraling bundles of parallel collagen fibers, oriented in a longitudinal pattern along the line of force stress; they are embedded in ground substance with a small number of fibroblasts. Tendons have a microscopic “crimp” or wave-like structure that acts like a spring, enabling them to withstand large internal forces. The junction where the muscle fibers end and the connective tissue that forms the tendon begins is called the musculotendinous junction. This area is vulnerable to injury.
Tendons may be cord-like, as in the Achilles tendon; may be seen as a flattened band of tissue, as in the rotator cuff; or may appear as a broad sheet of tissue called an aponeurosis, as in the attachment of the latissimus dorsi. They are surrounded by a loose connective tissue sheath. In areas of high pressure or friction, such as where tendons rub over the bones of the wrist and ankle, the tendon sheath is lined with a synovial layer to facilitate gliding. Tendon attaches to bone by weaving into the connective tissue covering of the bone called the periosteum. Tendons attach muscle to bone and transmit the force of muscle contraction to the bone, thereby producing motion of the joint. They also help to stabilize the joint and act as a sensory receptor through the Golgi tendon organs.
A strain is an injury to the tendon. It is a tearing of the collagen fibers at the musculotendinous junction, at the tenoperiosteal junction, or within the body of the tendon. Loss of normal motion in a tendon through injury or immobilization creates loss of collagen fibers and formation of adhesions between the tendon and surrounding structures, including the tendon sheath.
Ligaments
Ligaments attach bones at joints, help to stabilize joints, help to guide joint motion, prevent excessive motion, and act as sensory receptors. Ligaments are composed of dense, white, short bands of nearly parallel bundles of collagen fibers embedded in a matrix of ground substance and a small number of fibroblasts. They contain some elastic fibers and a “crimp” structure, giving them greater elasticity, and are pliable and flexible. All ligaments surrounding the joints contain proprioceptors, mechanoreceptors, and pain receptors that provide information about posture and movement, which plays an important role in joint function by directing joint movement.
Under normal conditions, when the joint moves, the ligament is stretched and the crimp in the tissue straightens out. The ligament returns to its normal length when the joint returns to a neutral position. If tension or force is slowly applied to a ligament consistently and is sustained, the tissue will assume the new length because of its viscous nature. This condition can lead to overstretched, or lax, ligaments and compromises stability of the joint. Because ligaments stabilize joints and act as neurosensory structures, injuries to ligaments can create dysfunction of the joint and surrounding soft tissue. A reflex connection exists between the ligaments of a joint and surrounding muscles; this connection affects the motor tone of muscles. In the case of lax ligaments, tone in muscles reflexively increases to provide joint stability. Ligaments function to transmit mechanical forces created by muscle contraction; they cross the joint, supporting integrated function.
The joint capsule and ligaments typically respond to an injury by becoming stretched, with resulting joint instability. These structures can also shorten, creating loss of a joint’s normal range of motion and joint stiffness. Immobilization causes ligaments to atrophy and weaken, changing the normal gliding motion of the joint. Ligaments can twist into abnormal positions. Irritation or injury of the ligaments usually causes a reflexive contraction or inhibition in the surrounding muscles. Muscle energy methods that address gait and firing pattern sequences can help restore normal function temporarily because the muscle is connected to the ligaments through a neurologic reflex. The condition will continue to occur because the instability of the joint is the underlying causal factor.
Injured ligaments can become thick and fibrous from increased collagen, abnormal cross-fiber links, and adhesions. This is especially common if inflammatory responses are slow to resolve or have remained chronic.
Massage applied to ligaments that have developed adhesions is performed across the direction of fibers to increase pliability and realign fiber structure. If ligaments are too lax, exercise rehabilitation can stimulate the production of new collagen and help restore normal integrity. Friction massage can be used to create small, controlled inflammation in the ligament structure to stimulate collagen production as well.
Periosteum
Periosteum is a dense, fibrous connective tissue sheath covering the bones. The outer layer consists of collagen fibers parallel to the bone and contains arteries, veins, lymphatics, and sensory nerves. The inner layer contains osteoblasts (cells that generate new bone formation). Repetitive stress can stimulate the inner layer of the periosteum to create bone outgrowths called spurs. This often occurs at the heel when the plantar fascia is short.
The periosteum weaves into ligaments and the joint capsule. Stretching of the periosteum provides mechanoreceptor information regarding joint function.
The periosteum also blends with the tendons, forming the tenoperiosteal junction, where the muscle pulls on the bone during joint movement. The sensory nerves in the periosteum are sensitive to tension forces. The periosteum also functions to transmit mechanical forces created by muscle contraction, supporting integrated function.
A common site of soft tissue injury is the tenoperiosteal junction. An acute tear or cumulative microtearing of the periosteum can cause the orientation of the collagen in the area to become random, leading to the development of abnormal cross-fiber links and adhesions. Massage can address this abnormal fibrotic developed at the tenoperiosteal junction. Friction is used to introduce small amounts of controlled inflammation. This results in an active acute healing process. When coupled with appropriate rehabilitation, more functional healing is the outcome.
Fascia
Fascia is a fibrous connective tissue arranged as sheets or tubes. Fascia can be thick and dense, or it can consist of thin, filmy membranes. Fascia is connected throughout the body, creating a unified form. You can conceptualize fascia as duct tape or plastic wrap (Figure 4-3). However, we must remember that we now know that fascia is not a passive tissue. Research shows that fascia responds to and sends nerve signals. Recent research (see Chapter 3) indicates that there may be a proprioceptive component, as well as an active contractile component, to fascia based on myofibroblast cells and sensory receptors embedded in the fascia. We now know that fascia tone is more than thickness or thinness of the tissue and is controlled through neuroendocrine mechanisms. The implications for massage therapists, particularly sports practitioners, are significant because our approach to connective tissue function and dysfunction would be expanded. Along with methods used to produce increased pliability, length and slide application of massage would include nervous system functions as well. It is important to understand that at the same time that massage application is introducing mechanical forces such as tension and torsion forces into the tissues to change the more passive elements of fascia (i.e., ground substance, fiber alignment), the nervous system is also being stimulated.
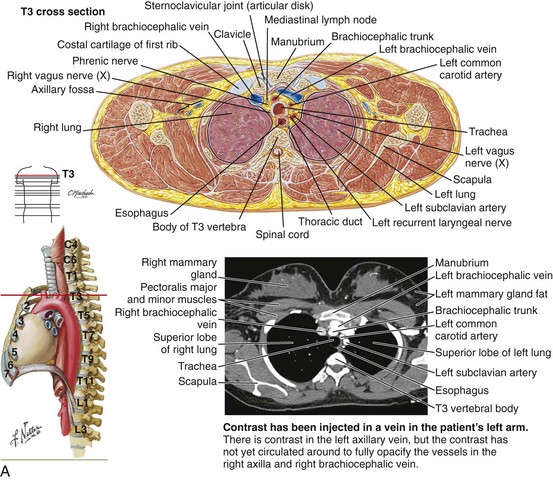
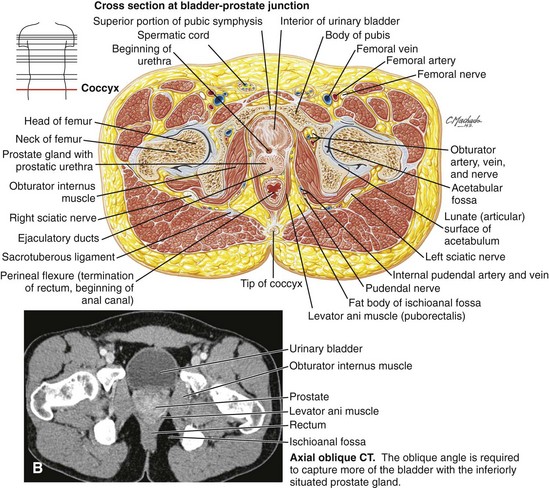
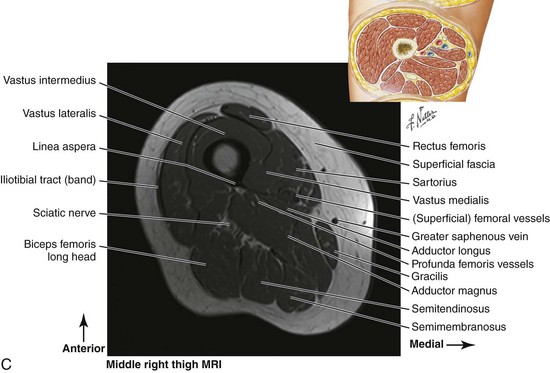
FIGURE 4-3 Fascia is connected throughout the body, creating a unified form. From head to foot, a continuum and unity are noted. A, Transverse view through thorax. B, Transverse view through hips and pelvis. C, Transverse view through thigh. (Netter illustration from www.netterimages.com. ©Elsevier Inc. All rights reserved.)
Fascia functions by connecting, unifying, and separating structure while acting as a communication network based on the interconnect tensegric structure. Muscle fibers are embedded in fascia, not just wrapped in it, and a single muscle structure becomes a unified functional unit consisting of multiple muscles in an intertwined chain of a variety of fascia wrappings, tendons, ligaments, joint capsule structures, and periosteum, which are located up and down, spiral around, and flow through the body. Through these interconnected structures, the forehead is connected to the bottoms of the feet, the left wrist connects to the right ankle (and vice versa), and the left shoulder is connected to the right hip and down through the knee. Tom Myers calls these chains myofascial meridians (Myers, 2008).
Information from the Stecco group describes the chains as myofascial units that function as uniting elements between unidirectional myofascial units (myofascial sequences), and as connecting elements between body joints through myofascial expansions and retinacula (myofascial spirals; Stecco at http://www.fascialmanipulation.com/englishhome32.html).
Functionally, muscle cells bundled together rarely transmit full contraction force directly via tendons into the skeleton. Instead, contractile or tensional forces caused by muscle action are distributed onto fascia sheets. These sheets transmit forces to synergistic and antagonistic muscles, affecting not only the target joint, but also distant sites within the myofascial unit.
For example, the muscles gluteus maximus and tensor fascia lata both insert into the dense fascia sheet along the lateral thigh, called the iliotibial tract, which is part of the fascial sleeve of the thigh, called the fascia lata. The latissimus dorsi on the opposite side weaves into the lumbar dorsal fascia, creating the connection to the opposite shoulder. This interconnected myofascial unit influences low back stability, shoulder motion, and stiffness of the lateral hamstrings and quadriceps, while stabilizing and guiding knee motion and finally stabilizing the foot though the plantar fascia and other connective tissue structures that support the arches of the foot and the elastic spring action of the foot during walking, running, and jumping. How then can we say that the quadriceps primarily extends the knee when the entire unit works together? An expanded understanding of fascia/muscle units challenges the typical study of muscles based on origin, insertion, and function. This being said, we can still benefit from studying the forms and function of the myofascial component of the body.
Superficial fascia lies under the dermis of the skin and is composed of loose, fatty connective tissues. Deep fascia is dense connective tissue that surrounds muscles and forms fascial compartments called septa, which contain muscles with similar functions. These compartments are well lubricated in the healthy state, allowing the muscles inside to move freely. At the same time, each layer is connected to the layer above and below by microscopic filaments with a wavy configuration that allow the sliding yet maintain connection and integrity between layers.
Fascia can tear, adhere, torque, shorten, or become lax, just as other connective tissue structures can, and it responds well to connective tissue massage methods, as described in Unit Two of this book.
Common sources of musculoskeletal pain are the deep somatic tissues, including periosteum, joint capsule, ligaments, tendons, muscles, and fascia. The most pain-sensitive tissues are the periosteum and the joint capsule. Tendons and ligaments are moderately sensitive, and muscle is less sensitive. This is an important awareness for massage therapists, who often are overly focused on muscle function as opposed to the total soft tissue system.
In general, mechanical forces applied during massage create heat within the tissues. This heat stimulates cellular activity and improves the lubrication of fibers by making the ground substance more fluid. Specific application of a massage approach to generate heat in the tissue can be used as a part of a warm-up activity. Strains and sprains of muscles, tendons, and ligaments are common in athletic activity and damage connective tissue. Fascial tone increases as part of protective guarding. With disuse and immobilization, the tissues become cool and the ground substance becomes thicker and more gel-like. Stiffness and aching, decreased circulation and nutrition, and decreased lubrication may result. Massage therapy can change the viscosity of ground substance from a gel to a more fluid state through the introduction of mechanical forces—that is, bend, shear, tension, compression, and torsion.
The active and passive tissue movement of massage stimulates the synthesis of ground substance and glycosaminoglycans (GAGs), promotes the circulation of blood and lymph, and supports ground substance pliability, creating greater lubrication to the tissue. Tissue movement also facilitates transport of nutrients and promotes the exchange of waste products.
Massage changes the shape of the fascia, which triggers response from the myofibroblasts; they contract similarly to smooth muscle cells and draw together, pulling the fascia taut and increasing stiffness.
Effectively focused massage can do the following:
• Stimulate fibroblasts to repair the injured collagen
• Introduce mechanical forces to realign the collagen fibers to their normal parallel alignment
• Introduce mechanical forces to separate tissue layers to support sliding
• Heat the tissue, affecting the fluidity of the ground substance
• Stimulate fluid distribution throughout tissue layering to promote normal tissue gliding
• Lengthen shortened tissue and increase ground substance pliability
• Create controlled focused inflammation to increase collagen proliferation, especially in lax structures. Proper rehabilitation must be combined with this approach for a beneficial outcome. Otherwise, the result can be increased adherence and scar tissue formation.
• Influence fascia tone related to myofibroblast contraction by changing the shape of tissue and altering autonomic nervous system function.
Joints
A joint, or articulation, is the junction between two or more bones of the skeleton that allows movement. Depending on joint type, the movement can be very small, as in cranial sutures and most evident in infants, or large, as in the ball and socket joint of the shoulder. The focus of this text will be on the synovial or freely movable joints of the body. Joint movement depends on the shape of the bones and articular surfaces where the bones meet, how ligaments cross the joint, and what type of movement is produced by muscles crossing the joint.
Simply, contraction of muscles crossing the joint causes the joint to move throughout its range of motion. Each specific joint has a normal range of motion that is expressed in degrees (Box 4-1). However, we now know that it is not that simple. The pulling forces created by contracting muscle cells are embedded in connected functional units unified by spans of connective tissue structures that are individually called fascia, aponeuroses, tendons, ligaments, and so forth. More than individual muscles, joint movements are caused by the distribution of force throughout these tissues.
Limited range of motion refers to a joint that has reduced ability to move. The reduced motion may signify a mechanical problem within specific joint structures; more often, it reflects some sort of binding within the myofascial continuum. Although limited joint function can be caused by diseases such as osteoarthritis and other types of arthritis, in the athlete, limits typically begin with changes in soft tissue, which ultimately can deteriorate, resulting in the pain, swelling, and stiffness associated with osteoarthritis and eventually degenerative joint disease.
Reflex control of muscles surrounding the joint is called the arthrokinematic reflex. The CNS (central nervous system) creates contraction or relaxation of the muscles to protect the joint. The arthrokinematic reflex coordinates agonists, antagonists, and synergists around the joint, as well as in other jointed areas, for gross movements and fine muscular control. Proper function of these reflex mechanisms is extremely important in posture, coordination, and balance; direction and speed of movement; position of the joint and body; and pain in the joint.
Irritation of pain receptors and mechanoreceptors typically causes the flexors of the joint to be facilitated and become short, tight, and hypertonic, whereas the extensors of the joint become inhibited or weak and long.
Irritation of joint receptors can lead to abnormalities in posture, muscle coordination, control of movement, balance, and awareness of body position. This is a major issue for athletes. Assessment and treatment of gait patterns and firing patterns and use of massage, including muscle energy methods, can support normal reflex functions (see Chapter 10).
Joint Stability
For a joint to perform a full and painless range of motion, it must first be stable. A rule to follow is stability before mobility, mobility before agility. Otherwise, abnormal forces move through the joint, leading to excessive wear and tear on articular surfaces. Joint stability is determined by
• The shape of the bones that make up the joint. This is form stability.
• Passive stability provided by the ligaments and joint capsule. This is also form stability.
• Dynamic stability provided by the muscles to produce stability. This is force stability.
If instability in the joint is caused by the form (bones, ligaments), then soft tissue methods will be only palliative. However, if force instability occurs in the joint as a result of muscle dysfunction, exercise and massage can be valuable (Figure 4-4).
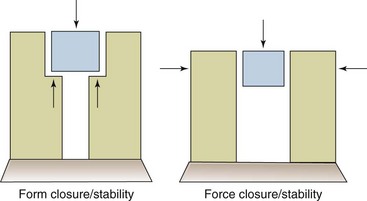
FIGURE 4-4 Form and force stability.
•Form closure/stability is dependent on the shape of the bones of the joint and the way everything fits together.
• Force closure/stability is the action of muscle contraction to stabilize the joint.
• Excessive form stability results in a stuck or fixed joint.
• Excessive force stability can result in excess form stability by jamming the joint surfaces.
• Decreased form stability results in increased muscle contraction to produce force stability.
• Decreased force stability results in strain on the joint capsule. (From Fritz S: Mosby’s essentials of therapeutic massage, ed 4, St Louis, 2013, Mosby.)
It is important that muscle structures that cross a joint are balanced with appropriate contraction ability; otherwise, forces on the joint will create uneven stresses, leading to dysfunction and eventual degeneration of the cartilage.
When a joint is in the close-packed position, the capsule and the ligaments are tightest. In the least-packed position, the joint is most open, and the capsule and the ligaments are somewhat lax. Generally, extension closes and flexion opens the joint surfaces. Midrange of the joint is typically the least-packed position and is most vulnerable to joint injury (Tables 4-1 and 4-2).
TABLE 4-1
Least-Packed Positions of Joints
| Joint(s) | Position |
| Spine | Midway between flexion and extension |
| Temporomandibular | Mouth slightly open |
| Glenohumeral | 55° abduction, 30° horizontal adduction |
| Acromioclavicular | Arm resting by side in normal physiologic position |
| Sternoclavicular | Arm resting by side in normal physiologic position |
| Elbow | 70° flexion, 10° supination |
| Radiohumeral | Full extension and full supination |
| Proximal radioulnar | 70° flexion, 35° supination |
| Distal radioulnar | 10° supination |
| Wrist | Neutral with slight ulnar deviation |
| Carpometacarpal | Midway between abduction/adduction and flexion/extension |
| Thumb | Slight flexion |
| Interphalangeal | Slight flexion |
| Hip | 30° flexion, 30° abduction and slight lateral rotation |
| Knee | 25° flexion |
| Ankle | 10° plantar flexion, midway between maximum inversion and eversion |
| Subtalar | Midway between extremes of range of motion |
| Midtarsal | Midway between extremes of range of motion |
| Tarsometatarsal | Midway between extremes of range of motion |
| Metatarsophalangeal | Neutral |
| Interphalangeal | Slight flexion |
From Magee DJ: Orthopedic physical assessment, ed 4, Philadelphia, 2002, Saunders.
TABLE 4-2
Close-Packed Positions of Joints
| Joint(s) | Position |
| Spine | Extension |
| Temporomandibular | Clenched teeth |
| Glenohumeral | Abduction and lateral rotation |
| Acromioclavicular | Arm abducted to 30° |
| Sternoclavicular | Maximum shoulder elevation |
| Elbow | Extension |
| Radiohumeral | Elbow flexed 90°, forearm supinated 5° |
| Proximal radioulnar | 5° supination |
| Distal radioulnar | 5° supination |
| Wrist | Extension with ulnar deviation |
| Carpometacarpal | Full flexion |
| Thumb | Full opposition |
| Interphalangeal | Full extension and medial rotation* |
| Hip | Full extension and lateral rotation of femur |
| Knee | Maximum extension |
| Ankle | 10° plantar flexion, midway between maximum inversion and eversion |
| Subtalar | Supination |
| Midtarsal | Supination |
| Tarsometatarsal | Supination |
| Metatarsophalangeal | Full extension |
| Interphalangeal | Full extension |
*Some authors include abduction.
From Magee DJ: Orthopedic physical assessment, ed 4, Philadelphia, 2002, Saunders.
John Mennell introduced the concept of joint play, which describes movements in a joint that can be produced passively but not voluntarily. In most joint positions, a joint has some “play” in it that is essential for normal joint function. (See joint play methods for assessment and correction of joint play dysfunction in Unit Two.)
Joint Capsule Pathology
Fibrosis or thickening of the outer layer of the joint capsule is caused by acute inflammation, irritation, inflammation caused by imbalanced stresses on the joint, and/or immobilization. A tight, fibrotic joint capsule results in compression of certain areas of the cartilage and degeneration of the joint surfaces.
The capsule and supporting ligaments may be stretched because of injury or excessive stretching during activity such as dancing and gymnastics. If loss of adequate motion results from immobilization, the fibrous layer of the joint capsule atrophies, and joint instability results.
The synovial membrane can become injured or dysfunctional because of acute trauma to the joint, cumulative stresses from chronic irritation caused by imbalanced forces on the joint, or immobilization. Although arthroscopic surgery may be performed to vastly improve results in a variety of joint injury treatments, the surgical procedure itself can involve trauma to the joint capsule when surgical instruments are inserted into the joint. Joint swelling occurs during inflammation. The swelling typically causes abnormal muscle function in controlling the joint. Immobilization, on the other hand, thickens the synovial fluid and causes an eventual decrease in the amount of synovial fluid. This leads to adhesions between capsule and articular cartilage, tendon sheaths, and bursae, contributing to stiffness and joint degeneration.
A fibrotic joint capsule is addressed by using massage to introduce mechanical forces into the tissue to increase pliability. The fibrotic capsule is treated with manual pressure into the structures of the capsule itself. Massage strokes are applied in all directions, addressing the irregular alignment of the collagen. Active and passive movement and stretching are used to reduce intraarticular adhesions.
A capsule that is too loose needs exercise rehabilitation to help lay down new collagen fibers and proprioception exercises to help restore neurologic function. Appropriate friction massage can stimulate an acute inflammatory response that stimulates collagen formation, although results may take a long time to manifest.
For an acute, swollen joint capsule with fluid accumulating inside the capsule, treat with gentle rhythmic compression and decompression of the joint and lymphatic drain to pump excess fluid out of the capsule. Pain-free, passive range of motion is used in the flexion/extension plane to act as a mechanical pump.
If too little fluid is found in the joint, passive and active movement may help stimulate the synovial membrane, increasing synovial fluid and thereby assisting lubrication and nutrition. An artificial joint fluid can be injected into the joint space and can support movement with reduced pain.
Fluid can also accumulate outside the capsule and around the knee. Common causes of this condition include patellar tendonitis. Irritation or injury to the capsule can create muscle contractions designed to protect the joint. This is called guarding. During the subacute healing phase, the guarding response begins to resolve. General massage in the area can support return to normal. If the guarding does not resolve, more specific methods such as muscle energy techniques to support focused stretching can be used to restore normal resting length and tone.
Cartilage
Cartilage is the tough but flexible tissue that covers the ends of bones at a joint. Healthy cartilage allows movement by permitting bone ends to glide over each other. It protects bones by preventing them from rubbing against each other. Injured, inflamed, or damaged cartilage can cause symptoms such as pain and limited movement. It can also lead to joint damage and deformity. Osteoarthritis results from breakdown of cartilage.
Cartilage is elastic and porous and has the capacity to absorb and bind synovial fluid. Intermittent compression and decompression creates a pumping action, which causes the movement of synovial fluid into and out of the cartilage, which is self-lubricating as long as the joint moves. Normal joint movements open and close the joint surfaces, compress and decompress the cartilage, and tighten and loosen the joint capsule and ligaments, all of which supports joint lubrication and nutrition.
Fibrocartilage consists of white fibrous connective tissue arranged in dense bundles or layered sheets. Fibrocartilage has great tensile strength combined with considerable elasticity. It functions to deepen a joint space, such as the labrum of the hip and shoulder, the menisci of the knee, and the intervertebral discs of the spine. It lines bone grooves for tendons, as in the bicipital groove for the long head of the biceps brachii. Common sport injuries include various types of fibrocartilage damage, often when these structures become pinched or torn. A common knee injury is a torn meniscus.
Synovial joints generate compression and decompression through movement, intermittent contraction of the muscles, and twisting and untwisting of the joint capsule. Massage application that includes passive and active forms of joint movement introduces compression and decompression and supports joint health.
Athletes are particularly prone to cartilage damage. An arthritic joint is a joint with degeneration of the cartilage (Figure 4-5). Damage to articular cartilage may be caused by acute trauma or cumulative stresses. These stresses are often the result of imbalances in the muscles surrounding the joint, a tight joint capsule, or a loose joint capsule. A tight capsule creates a high-contact area in the cartilage and decreased lubrication. A loose capsule allows inappropriate joint laxity and rubbing of the bone surfaces, damaging the cartilage on the bone ends. All muscles around the joint shorten to increase stability. Flexor, adductor, and internal rotator muscles are larger and therefore will create an uneven pull on the joint structures because the extensors, abductors, and external rotators cannot exert enough force to counterbalance. Imbalanced muscles that move the joint create excessive pressure on the cartilage. The cartilage degenerates, beginning with fracturing of the collagen fibers and depletion of the ground substance.
FIGURE 4-5 Arthritic degeneration of cartilage. (Netter illustration from www.netterimages.com. ©Elsevier Inc. All rights reserved.)
Recent studies show that cartilage cells can create new cartilage. The joint must be moved to stimulate the synthesis of chondrocytes and the secretion of synovial fluid. Compressing and decompressing the joint capsule pumps synovial fluid into and out of the cartilage, rehydrating the cartilage. In addition to appropriate exercise, massage including muscle energy methods supports joint health using the following methods: contract/relax/antagonist contract, pulsed muscle, or a combination of these methods. Both active and passive movements of the joint, as well as compression and decompression (traction), promote fluid exchange.
Bursa
A bursa, a synovia-filled sac lined with a synovial membrane, is found in areas of increased friction. The function of bursae is to secrete synovial fluid, which decreases friction in the area.
Bursitis typically is caused by excessive friction of the muscles and connective tissues (tendons and fascia) that overlie the bursa. Massage can lengthen structures that are rubbing and can drain excessive fluid from the area through lymphatic drain methods. For example, lengthening the supraspinatus muscle/tendon can relieve pressure placed on the subacromial/subdeltoid bursa, which is sandwiched between the supraspinatus and the acromion process.
Joint Degeneration
One common cause of joint degeneration is loss of normal function of the joint. This altered function can occur as a result of prior trauma or cumulative stress on the joint and is common in athletic performance.
Most conditions called arthritis are in fact noninflammatory and should be referred to as arthrosis, meaning “joint degeneration.” The terms osteoarthritis and degenerative joint disease are typically used interchangeably to describe chronic degeneration of a joint, although osteoarthritis may be used to describe an inflammatory condition, and the markers of inflammation (i.e., heat, redness, pain, and swelling) will be present. Arthrosis occurs when joint structures can no longer create an inflammatory response. Many athletes will develop arthritis and arthrosis.
Appropriate massage addresses adhesions and tightening of the joint capsule or ligaments, sustained contraction of the muscle surrounding the joint, muscle imbalances across a joint, and irregular firing patterns of the muscles moving the joint.
Short and tight muscles must be lengthened and relaxed, and muscles that are weak and inhibited need to be reeducated and exercised to regain their normal strength. Muscle activation firing pattern sequences need to be normalized (all discussed in future chapters).
Joint mobilization is any active or passive attempt to increase movement at a joint. Joint mobilization within the normal range of motion is within the scope of practice for the massage therapist. The movement must not be forcefully abrupt or painful.
Goals of joint mobilization are as follows:
• Restore the normal joint play.
• Promote joint repair and regeneration.
• Stimulate normal lubrication by stimulating synovial membranes to promote rehydration of articular cartilage.
Joint manipulation can be valuable. The chiropractor, physical therapist, or other specialist can manipulate the joint structure.
Muscle
A skeletal muscle is the organ of the muscular system composed of skeletal muscle tissue, nerves, blood and lymph vessels, and connective tissue. When we think of a muscle, we typically think of the muscle organ. The hamstrings, triceps, and fibularis all are examples of the muscle organ. You can isolate an individual muscle organ through dissection that artificially cuts the functional muscle units apart. Anatomic and physiologic understanding of the muscular system is changing primarily because of expansion of understanding of the fascia muscle connection and how the entire bone, joint, muscle, and associated connective tissues act as an interconnected functional unit. However, this understanding is not currently reflected in how we describe muscular function, and the terminology is confusing. The accuracy of saying that the gluteus maximus extends the hip and attaches to the external surface of the ala of the ilium, including the iliac crest, dorsal surfaces of the sacrum and coccyx, and the sacrotuberous ligament, with distal attachments at the iliotibial tract and the gluteal tuberosity of the femur, can be challenged.
For instance, the gluteus maximus acting alone could not complete the hip extension action or the proximal attachment limit to the iliac crest, sacrum, and coccyx. More correctly, to describe hip extension and attachments, we need to include the bones and joint structures involved, the local and distant fascial network, synergistic and antagonistic functions of other muscles, and associated movements, including coordination between upper and lower limbs, innervation and reflex patterns, circulation to and from the structures, and more. This understanding does not mean that we do not need to understand the location and function of individual muscles (more correctly, muscle organs, composed of muscle tissue, connective tissue, and nerve tissue that contract to produce a particular movement). To read and write, we need to understand the individual letters; however, meaning occurs only when letters are united into words that are united into sentences and eventually into an expression of a thought or the telling of a story.
Muscle tissue is composed of sheets or bundles of cells that contract to produce movement or to increase tension. Simply, muscle cells contain filaments made of the proteins actin and myosin, which lie parallel to each other. When muscle tissue is signaled to contract, actin and myosin filaments slide past each other in an overlapping pattern. Muscle tissues aligned to produce a similar pull direction are wrapped in fascia. All these units are wrapped and then wrapped again until a large grouping forms what we think of as a muscle (more correctly a muscle organ). Muscles are then bound together by fascia into compartments of muscles that produce similar movement within a plane of function (Figure 4-6).
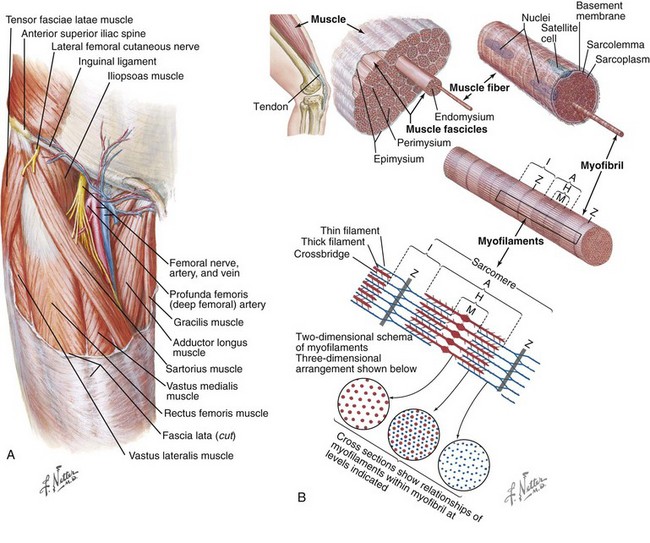
FIGURE 4-6 The muscle organ. A, Muscles bound with fascia. (From Cochard L, et al: Netter’s introduction to imaging, St Louis, 2012, Saunders.) B, Organization of skeletal muscle. Skeletal muscle is composed of fascicles, which in turn comprise multinucleated muscle fibers. These fibers are composed of smaller myofibrils, which contain sarcomeres, the site at which sliding of actin and myosin filaments produces contraction. The organization of sarcomeres within the skeletal muscle produces its striated appearance. The Z line marks the boundary between two sarcomeres. The I band contains only the actin thin filaments, which extend from the Z line toward the center of the sarcomere. Myosin thick filaments are found in the dark A band. At the H zone, no overlap is noted between actin and myosin. The M line is at the center of the sarcomere and is the site at which the thick filaments are linked with each other. (Netter illustration from www.netterimages.com. ©Elsevier Inc. All rights reserved.)
All of these connective tissue layers are lubricated in the healthy state. Muscle layers and bound units operating in different functional planes should slide over each other in relationship to each other; when this does not happen, function is altered. This commonly occurs in athletes and as part of the aging process.
Muscles are dynamic stabilizers of the joints because they actively hold the joints in a stable position for posture and movement. Muscles sense joint movement and body position.
Muscles are connected to nerves in the skin and to nerves in the capsule and ligaments of neighboring joints through neurologic reflexes. If the skin or joint is irritated or injured, the muscle may go into a reflexive spasm or into inhibition. Muscles have pain receptors that fire with chemical or mechanical irritation.
Muscles act as a musculovenous pump because the contracting skeletal muscle compresses the veins and moves blood toward the heart. A similar process assists lymphatic movement.
Muscle Function Types
Muscles exert a pull when the actin/myosin is stimulated to contract. Three types of muscle actions are known, all involving contraction:
1. Isometric—In an isometric contraction, the muscle contracts, but its constant length is maintained. The main outcome is stabilization.
2. Concentric—Concentric contraction is the shortening of muscle fibers while the muscle contracts. The main outcome is movement/acceleration.
3. Eccentric—Eccentric function is the moving apart of proximal and distal attachments while muscle fibers contract, yet the entire structure lengthens. The main outcome is control of movement and deceleration.
Muscles that contract concentrically to perform a certain movement are called agonists. This action is called acceleration, and the muscle is called the prime mover. For example, the biceps muscle is an agonist for elbow flexion. Muscles that perform the opposite movements of the agonists are called the antagonists; they provide control through deceleration during eccentric function. The triceps is the antagonist for the biceps because the triceps extends the elbow. The muscle that works with another muscle to accomplish a particular motion is called a synergist. Stabilizers typically are acting more with isometric function to hold a body part immobile while another body part is moving.
In most normal activities, proximal joints are stabilized by muscle contractions during movement of more distal joints. A neutralizer helps counteract unwanted motions that a muscle can perform, so a specific motion can occur.
Typically, when the agonist is working concentrically, the antagonist is functioning eccentrically. Sherrington’s law of reciprocal inhibition states that there is a neurologic inhibition of the antagonist when the agonist is working. When we contract the biceps to flex the elbow, the triceps is being neurologically inhibited, which allows it to lengthen during elbow flexion. Co-contraction is an exception to this rule. Co-contraction occurs when the agonist and the antagonist are working together. For example, when you make a fist, the flexors and extensors of the wrist are co-contracting to keep the wrist in a position that ensures the greatest strength of the fingers. Co-contraction also occurs during the protective guarding response.
Human movement seldom involves pure forms of isolated concentric, eccentric, or isometric actions because the body segments are periodically subjected to impact forces, as in running or jumping, or because some external force such as gravity causes the muscle to lengthen. In many situations, the muscles first act eccentrically, with a concentric action following immediately, mixed in with isometric stability function.
Muscle Length-Tension Relationship
A muscle develops its maximum strength or tension at its resting length or just short of its resting length because the actin and myosin filaments have the maximum ability to slide. When a muscle is excessively shortened or lengthened, it loses its ability to perform a strong contraction. This is called the length-tension relationship (Figure 4-7). A muscle can develop only moderate tension in the lengthened position and minimum tension in the shortened position. Often athletes overtrain, thinking it will make them stronger, but what really happens is that the length-tension relationship is disturbed and strength is decreased. Massage can effectively normalize this situation.
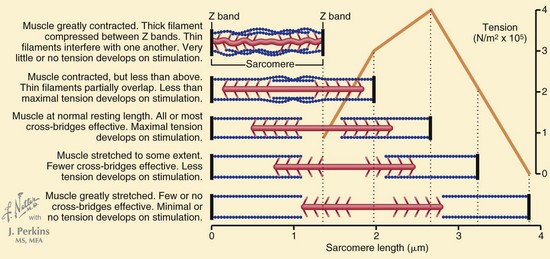
FIGURE 4-7 A length-tension relationship is seen, whereby greater resting sarcomere length (stretch of the muscle before contraction) is associated with greater force of contraction, up to NORMAL resting length. (Netter illustration from www.netterimages.com. ©Elsevier Inc. All rights reserved.)
Reflexive Muscle Action
Protective coordinated reflexive muscle action is an important consideration when massage is provided; it is influenced by the following reflexive actions:
• Withdrawal reflexes, such as pulling away from a hot stove, involve instantaneous muscle contraction.
• Righting reflexes, such as tonic neck reflex and oculopelvic reflexes from the eyes, ears, ligaments, and joint capsules, communicate with the muscle and stimulate instantaneous contraction for protection of the joint and associated soft tissue; they also support upright posture.
• Arthrokinematic reflexes are unconscious muscle contractions of muscles surrounding a joint that are caused by irritation in the joint.
• Splinting, guarding, and involuntary muscle contraction can be caused by a muscle injury.
• Emotional or psychological stress creates excessive and sustained muscle tension.
• Viscerosomatic reflexes occur when an irritation or inflammation in a visceral organ causes a muscle spasm.
Muscles have properties and are able to function in multiple ways to meet various tasks such as maintaining balance. Most daily activities require the coordination of complex neuromuscular interactions. Sometimes muscles are required to function for long periods without fatiguing; at other times, muscles must provide maximal effort for only a few seconds. As described, muscles have three major actions: isometric, concentric, and eccentric. Muscles must be able to shorten and lengthen to provide range of motion at joints, yet they must generate enough power to move a load at each end of the range. Muscles must be able to hold a static position to provide stability. The nervous system accomplishes fine control of muscle contraction over a wide range of lengths, tensions, speeds, and loads. When giving a massage, we have to assess for these functions. Massage application depends on accurate functional assessment.
We can observe as a muscle contracts through its range of motion. When a muscle moves a joint, its ability to stabilize is decreased, and vice versa. Muscles that span a long distance, such as the biceps brachii of the arm, are most efficient in supplying movement through a longer range of motion. Other muscles are more effective at stabilizing the joint than moving it. The coracobrachialis of the shoulder joint is a good example; its line of pull is mostly vertical and close to the axis of the shoulder joint. Therefore, the coracobrachialis has a short range of motion, which makes this muscle more effective at stabilizing than flexing the shoulder joint. Opposing muscle groups generate parallel forces to provide stability; this is achieved through co-contraction.
When considering the effect of the massage outcome, it is important to consider the function of the structure addressed. For example, it may be important to lengthen and stretch a muscle that spans a distance and is primarily a mover muscle. A muscle that functions primarily as a stabilizer may develop trigger points to help keep the muscle short and to support the stabilizing function necessary for balance. Because the trigger point is assisting stabilization of a joint, it is important during the massage to address the trigger point while not interfering with the stabilization function of the muscles.
Kinetic Chain
As mentioned, muscles do not function independently; instead, a body-wide interactive network is involved. This network is called the kinetic chain (Figure 4-8). The kinetic chain influences training, conditioning, rehabilitation, and massage application. It consists of the muscular/fascia system (functional anatomy), the articular joint system (functional biomechanics), and the neural/chemical system (motor behavior).
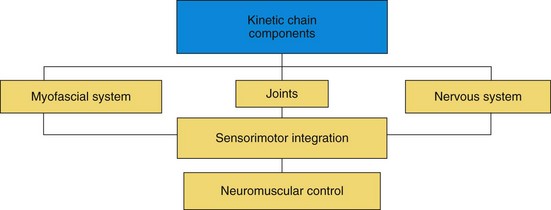
FIGURE 4-8 Kinetic chain components. (Modified from Fritz S: Mosby’s essential sciences for therapeutic massage: anatomy, physiology, biomechanics, and pathology, ed 2, St Louis, 2004, Mosby.)
Each of these systems works interdependently to allow structural and functional efficiency. If any of these systems does not work efficiently, compensations and adaptation occur in the other systems. These compensations and adaptation lead to tissue overload, decreased performance, and predictable patterns of injury.
Normal or maximally efficient function is an effectively integrated, multiplanar (frontal, sagittal, transverse) movement process that involves acceleration, deceleration, and stabilization of muscle and fascial tissue and joint structures. Many strength and conditioning programs involve only uniplanar force movement. Very little time is spent on core stabilization, neuromuscular stabilization, and eccentric training in all three planes of motion (sagittal, frontal, and transverse) (Figure 4-9). This situation predisposes an athlete to neuromuscular dysfunction. The massage professional can manage or assist in reversal of the dysfunctional patterns that occur from these types of exercise and training regimens. Conditioning programs and fitness protocols need to follow a sequence. Stability must develop before effective mobility. The core is considered the lumbar-pelvic-hip complex, thoracic spine, and cervical spine. The core operates as an integrated functional unit to dynamically stabilize the body during functional movements. The stabilization system has to function optimally to effectively utilize the strength and power in the prime movers. Many low back pain and hamstring problems are directly related to problems with core stability.
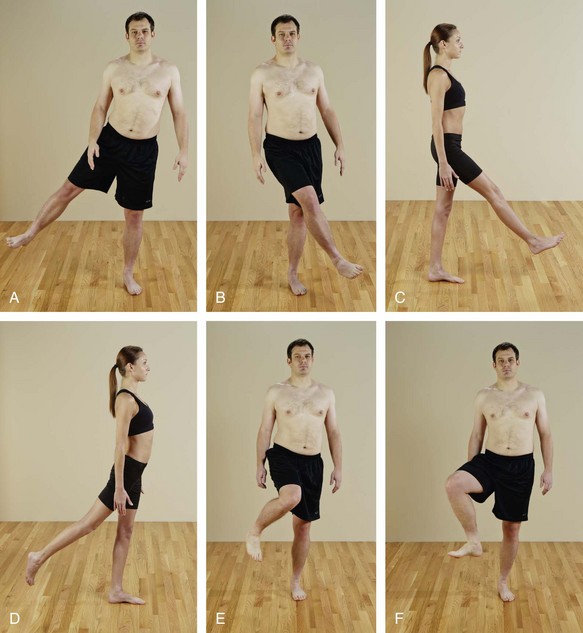
FIGURE 4-9 Examples of multiplanar movement. Example: hip joint. A, Frontal plane—abduction. B, Frontal plane—adduction. C, Sagittal plane—flexion. D, Sagittal plane—extension. Transverse movement. E, Internal rotation. F, External rotation.
Many types of strength are known, including maximal strength, absolute strength, relative strength, strength endurance (stamina), speed strength, stabilization strength, and functional strength.
During movement, muscles must eccentrically function to decelerate gravity, ground reaction forces, and momentum, before concentric contraction causes acceleration to produce movement. Stabilization strength, core strength, and neuromuscular efficiency control the time between the eccentric function and the preceding concentric contraction. Therefore, eccentric neuromuscular control and stabilization strength exercises should begin to make up a larger portion of any fitness program. Because eccentric movement has a greater potential to result in delayed-onset muscle soreness, the massage application needs to effectively manage this response to exercise and training and must ensure that compliance and performance are sustained. Functional movement patterns involve acceleration, stabilization, and deceleration, which occur at every joint.
Muscles must adjust to gravity, momentum, ground reaction forces, and forces created by other functioning muscles. During functional movement, the transversus abdominis, internal oblique, multifidus, and deep erector spinae muscles stabilize the lumbar-pelvic-hip complex, whereas the prime movers perform the actual functional activities.
Muscles function synergistically in groups called force couples to produce force, reduce force, and dynamically stabilize the kinetic chain. Force couples are integrated muscle groups that provide neuromuscular control during functional movements.
When movement of the body is viewed as an integrated functional system, muscles can be classified as local or global. Muscles that cross one joint are considered local muscles and form the inner unit. Global muscles cross multiple joints and form the outer unit.
The local musculature and connective tissue (inner unit) structurally consists of soft tissue that is predominantly involved in joint support or stabilization. The joint support system of the core (lumbar-pelvic-hip complex) consists of muscles that may originate from or insert into the lumbar spine, including the transversus abdominis, lumbar, multifidus, and internal oblique muscles, the diaphragm, and the muscles of the pelvic floor.
Local musculature also forms peripheral joint support systems of the shoulder, pelvic girdles, and limbs that consist of muscles that are not movement-specific but provide stability to allow movement of a joint. They also have attachments to the joint’s passive elements, such as ligaments and capsules, which makes them ideal for increasing joint stability. A common example of a peripheral joint support system (local muscles/inner unit) is the rotator cuff of the glenohumeral joint, which provides dynamic stabilization for the humeral head in relation to the glenoid fossa during movement. Other joint support systems include the posterior fibers of the gluteus medius and the external rotators of the hip, which perform pelvic-femoral stabilization, and the vastus medialis oblique muscles, which provide patellar stabilization at the knee.
The global muscles (outer unit) cross multiple joints and are predominantly responsible for movement. This group consists of more superficial muscles. The outer unit muscles are predominantly larger and are associated with movement of the trunk and limbs and equalize external loads placed upon the body. Major ones include the rectus abdominis, external oblique, erector spinae, gluteus maximus, latissimus dorsi, adductors, hamstrings, quadriceps, and biceps and triceps brachii. They also are important because they work together in complementary patterns to transfer and absorb forces from the upper and lower extremities to the pelvis.
The outer unit musculature has been broken down and described as force couples working in four subsystems. As described by Mike Clark (2000), these subsystems include the deep longitudinal, posterior oblique, anterior oblique, and lateral. Tom Myers (2008) describes similar patterns as myofascial unit meridians. Regardless, these muscle/fascial groups operate as an integrated functional unit because the central nervous system processes patterns of movement, not isolated muscles, and massage needs to address the system, not individual muscles.
Deep Longitudinal Subsystem
The major soft tissue components of the deep longitudinal subsystem are the erector spinae and biceps femoris muscles, thoracolumbar fascia, and sacrotuberous ligament. The long head of the biceps femoris attaches to the sacrotuberous ligament at the ischium. The sacrotuberous ligament in turn attaches from the ischium to the sacrum. The erector spinae attaches from the sacrum and ilium up to the ribs and cervical spine. Activation of the biceps femoris increases tension in the sacrotuberous ligament, which transmits force across the sacrum, stabilizing the sacroiliac joint, and allows force transference up through the erector spinae to the upper body. The functional interaction provides one pathway of force transmission longitudinally from the trunk to the ground. This muscle and fascia system functions mostly in the sagittal plane.
This transfer of force is necessary for normal gait. Prior to heel strike, the biceps femoris activates to eccentrically decelerate hip flexion and knee extension. Just after heel strike, the biceps femoris is further loaded through the lower leg via inferior movement of the fibula. This tension from the lower leg, up through the biceps femoris, into the sacrotuberous ligament and up the erector spinae, creates a force that assists in stabilizing the sacroiliac joint.
Another group of muscles acting as a force couple consists of the superficial erector spinae, psoas, transversus abdominis, lumbar, multifidus, and internal obliques and the muscles of the diaphragm and pelvic floor. Dysfunction of any structure can lead to sacroiliac joint instability and low back pain. Weakening of the gluteus maximus (often inhibited by the psoas and other related muscles) and structures of the deep longitudinal subsystem and/or latissimus dorsi may also lead to increased tension in the hamstring, thereby causing recurring hamstring strains.
Dysfunction in any of these structures can lead to sacroiliac joint instability and low back pain. These areas need to be addressed as one functional unit, not as individual muscles.
Posterior Oblique Subsystem
The muscles and fascia of the posterior oblique subsystem function in the transverse plane. Major muscles are the latissimus dorsi and gluteus maximus. When the contralateral gluteus maximus and latissimus dorsi muscles contract, this creates a stabilizing force for the sacroiliac joint.
Just before heel strike, the latissimus dorsi and the contralateral gluteus maximus are eccentrically loaded. At heel strike, each muscle accelerates its respective limb and creates tension in the thoracolumbar fascia. This tension creates a force couple that assists in maintaining the stability of the sacroiliac joint.
The posterior oblique subsystem is important for other rotation activities such as swinging a golf club or a baseball bat and throwing a ball.
Anterior Oblique Subsystem
The anterior oblique subsystem functions in a transverse plane orientation very similarly to the posterior oblique subsystem but on the front of the body. Functional muscles include the internal and external oblique muscles, the adductor complex muscle, and the hip external rotators. These muscles function as an aid in stability and rotation of the pelvis, as well as contributing to leg swing. The pelvis must rotate in the transverse plane to create a swinging motion for the legs. This rotation comes in part from the posterior muscle and anterior muscle groups. The fiber arrangements of the muscles involved—latissimus dorsi, gluteus maximus, internal and external obliques, adductors, and hip rotators—indicate this type of function. Oblique and adductor complexes produce rotational and flexion movements and stabilize the lumbar-pelvic-hip complex.
Lateral Subsystem
The lateral subsystem, which is composed of the gluteus medius, tensor fasciae latae, adductor complex, and quadratus lumborum muscles, creates frontal plane stability. This system is responsible for pelvic femoral stability, as during single leg functional movements when walking or climbing stairs. The ipsilateral gluteus medius, tensor fasciae latae, and adductors combine with the contralateral quadratus lumborum to control the pelvis and the femur in the frontal plane.
Dysfunction in the lateral subsystem increases pronation (flexion, internal rotation, and adduction) of the knee, hip, and/or feet during walking, squats, and lunges, or when climbing stairs.
Kinetic Chain Influences
19. Explain full-body pronation and supination.
20. Define serial distortion patterns and synergistic dominance.
When in a closed kinetic chain, full body pronation is multiplanar (frontal, sagittal, and transverse) synchronized joint motion that occurs with eccentric muscle function. Supination is multiplanar (frontal, sagittal, and transverse) synchronized joint motion that occurs with concentric muscle function (Box 4-2). This means that for one joint pattern to move effectively, all involved joints have to move. Movement can be initiated at any joint in the pattern, and restriction of any joint in the pattern will restrict motion or increase motion in interconnected joints.
To briefly describe functional biomechanics, the gait cycle is reviewed here. During walking or other locomotor activities such as running, motion at the subtalar joint is linked to the transverse plane rotations of the bone segments of the entire lower extremity. During the initial contact phase of the gait cycle, the subtalar joint pronates, which creates internal rotation of the tibia, femur, and pelvis. At midstance, the subtalar joint supinates, which creates external rotation of the tibia, femur, and pelvis. Poor control of pronation decreases the ability to eccentrically decelerate multisegmental motion and can lead to muscle imbalance, joint dysfunction, and injury. Poor production of supination decreases the ability of the kinetic chain to concentrically produce appropriate force during functional activities and can lead to synergistic dominance. During functional movement patterns, almost every muscle has the same synergistic function: to eccentrically decelerate pronation or to concentrically accelerate supination. The CNS recruits the appropriate muscles in an optimal muscle activator firing pattern sequence during specific movement patterns.
Joint arthrokinematics refers to roll, slide, glide, and translation movements that occur between two articular partners. Joint play is defined as the involuntary movement that occurs between articular surfaces that are separate from the range of motion of a joint produced by muscles. It is an essential component of joint motion and must occur for normal functioning of the joint. Predictable patterns of joint arthrokinematics occur during normal movement patterns. Optimum length-tension and force couple relationships ensure maintenance of normal joint kinematics.
Optimal posture enables the development of high levels of functional strength and neuromuscular efficiency. Functional strength is the ability of the neuromuscular system to perform dynamic eccentric, isometric, and concentric actions efficiently in a multiplanar environment. This process allows the appropriate motor program (muscle activator sequence) to be chosen to perform an activity, thus ensuring that the right muscle contracts at the right joint, with the right amount of force, and at the right time. If any component of the kinetic chain is dysfunctional (such as short muscle, weak muscle, joint dysfunction), neuromuscular control is altered. This decreases force production, force reduction, and stabilization. If the kinetic chain is out of alignment, the individual will have decreased structural efficiency, functional efficiency, and performance. For example, if one muscle is tight (altered length-tension relationships), the force couples around that particular joint are altered. If the force couples are altered, the normal arthrokinematics is altered.
Arthrokinematic inhibition is the neuromuscular phenomenon that occurs when a joint dysfunction inhibits the muscles that surround the joint. For example, a sacroiliac joint dysfunction causes arthrokinematic inhibition of the deep stabilization mechanism of the lumbo-pelvic-hip complex (transversus abdominis, internal oblique, multifidus, and lumbar transversospinalis). All of these neuromuscular phenomena occur secondary to postural dysfunction.
Development of Kinetic Chain–related Muscle Imbalances
Muscle imbalances are caused by postural stress, pattern overload, repetitive movement, lack of core stability, and lack of neuromuscular efficiency. Kinetic chain dysfunction typically results in predictable patterns. Although each individual will display the pattern somewhat differently, the following information provides a conceptual way of understanding integrated function and dysfunction. These dysfunctional patterns can be called serial distortion patterns and synergistic dominance.
Vladimir Janda discovered that muscles react to pain or excessive stress in predictable patterns. He found that certain muscles tend to become overactive, short, and tight, and describes these muscles as having a postural or stabilizing function. He found that other muscles tend to become inhibited and weak, and noticed that most of these muscles were concerned with movement rather than stability. Muscles of the body can be classified on the basis of which muscles have primarily a stabilizing role, and which muscles have primarily movement roles. Many terms are used to describe these muscle functions. Two more accurate terms that have been suggested for these groups are tightness-prone stabilizer (postural) and inhibition-prone mover (phasic). These categorizations are controversial because most muscles can function in both roles (Box 4-3). Tonic/postural/stabilizing muscles play a primary role in maintenance of posture and joint stability. The primary role of the phasic/mover muscles is quick movement. Tonic/postural/stabilizing muscles react to stress by becoming short and tight, and phasic/mover muscles react to stress by becoming inhibited and weak.
The phasic/mover muscle group is characterized as being prone to developing tightness; it is readily activated during most functional movements and is overactive in fatigue situations or during new movement patterns. The stabilization group is prone to weakness and inhibition, is less activated in most functional movement patterns, and fatigues easily during dynamic activities. If the phasic/mover group is prone to tightness and overuse, this can cause reciprocal inhibition of its functional antagonists. This inhibition leads to poor neuromuscular efficiency and further postural dysfunction. Furthermore, if the stabilization group is prone to weakness, synergistic dominance (discussed later) can result.
An important difference between the two muscle groups is that a small reduction in strength of an inhibition-prone muscle initiates a disproportionately larger contraction of the antagonist tightness-prone muscle. Because work and recreational activities favor tightness-prone muscles getting stronger, tighter, and shorter as inhibition-prone muscles become weaker and more inhibited, unless fitness programs are balanced, dysfunctional patterns are exacerbated, and the length-tension relationship becomes important. Some muscles, such as the quadratus lumborum and scalenes, can react with tightness or weakness.
In addition to the causes of muscle dysfunction listed previously, muscle injury, training protocols, reduced recovery time, chronic pain, and inflammation create disturbances in normal muscle function and may stimulate a neurologically based tightness or weakness in a muscle. In a force couple relationship, muscles work together to produce movement or dynamic force joint stability. Serial distortion patterns in the kinetic chain disrupt force couple relationships.
A serial distortion pattern is the state in which the functional and structural integrity of the kinetic chain is altered and in which compensations and adaptations occur (Figure 4-10). These distortion patterns can be described as follows:
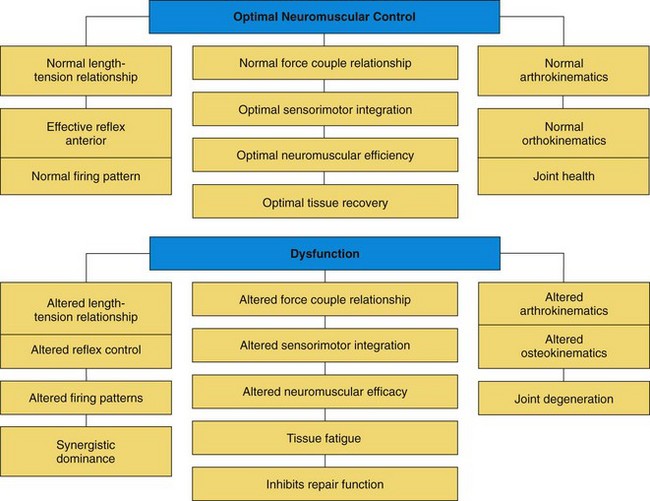
FIGURE 4-10 Overview of neuromuscular control. (Data from Chaitow L, DeLany JW: Clinical applications of neuromuscular techniques, vol 1, The upper body, Edinburgh, 2001, Churchill Livingstone.)
• Upper crossed syndrome (Figure 4-11)
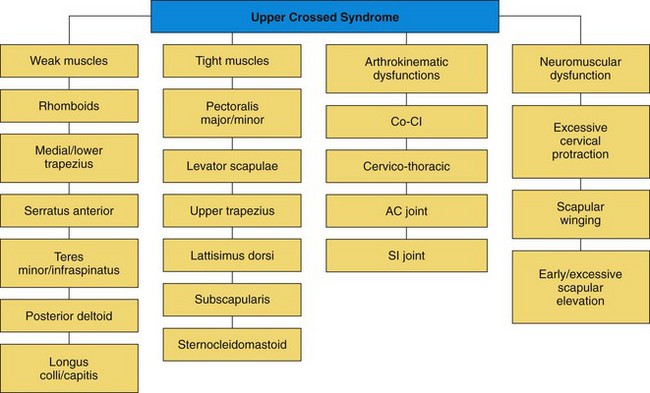
FIGURE 4-11 Upper crossed syndrome flow chart. (Data from Chaitow L, DeLany JW: Clinical applications of neuromuscular techniques, vol 1, The upper body, Edinburgh, 2001, Churchill Livingstone.)
• Lower crossed syndrome (Figure 4-12)
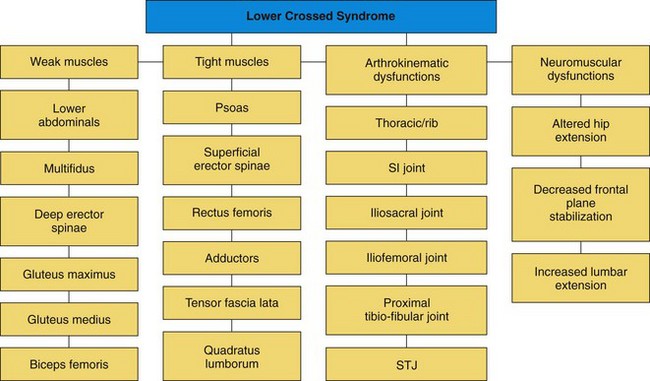
FIGURE 4-12 Lower crossed syndrome flow chart. (Data from Chaitow L, DeLany JW: Clinical applications of neuromuscular techniques, vol 1, The upper body, Edinburgh, 2001, Churchill Livingstone.)
• Pronation distortion syndrome (Figure 4-13)
A short, tight muscle is held in a sustained contraction. The muscle is constantly working, consumes more oxygen and energy, and generates more waste products than a muscle at rest. Circulation is decreased because the muscle is not performing its normal function as a pump, which can lead to ischemia and may cause the pain receptors to fire. Sustained tension in the muscle pulls on its attachments to the periosteum, joint capsule, and ligaments, creating increased pressure, uneven forces, and excessive wear in the joint. Short, tight muscles often compress nerves between muscles or through a muscle; this is a form of impingement syndrome.
Long weak muscles are unable to support joint stability and contribute to poor posture, excessive tension and compression, and abnormal joint movements. Muscle activator firing pattern sequences and gait reflexes are disturbed.
Inhibited muscles interfere with vascular and lymphatic movement.
Massage application as described in this book is particularly effective in dealing with these conditions and supports other professional treatments. Massage lengthens short tight muscles, normalizes firing patterns, and increases tissue pliability. These benefits support therapeutic exercise to treat long weak and inhibited muscles. In other words, treatment involves massage and stretching of short tight muscles and exercise for long weak muscles.
Reciprocal inhibition is the process whereby a short muscle with increased tone, the psoas for example, causes decreased neural stimulus in its functional antagonist, the gluteus maximus. This process results in decreased force production by the prime mover and leads to compensation by the synergists, a process called synergistic dominance. This process leads to altered movement patterns and is assessed and treated with muscle activator firing pattern sequences. Synergistic dominance often occurs as the result of improper training, including overtraining, and fatigue. Athletes may complain of heavy or labored movement if synergistic dominance is occurring.
As an example of synergistic dominance, if a client has a weak gluteus medius, then synergists (tensor fasciae latae, adductor complex, and quadratus lumborum) become dominant to compensate for the weakness. This alters normal joint alignment, which further alters normal length-tension relationships around the joint where the muscles attach. The combination of poor posture and muscle imbalances causing reciprocal inhibition and synergistic dominance leads to altered joint alignment. Altered joint alignment is the result of muscle shortening and muscle weakness. Altered arthrokinematics (joint movement) is further altered secondary to altered force couple relationships. If synergists are dominant, normal joint movements are altered because muscles are firing out of sequence. This is a continuous and cyclic process. Muscle shortening, muscle weakness, joint dysfunction, and decreased neuromuscular efficiency can all initiate this dysfunctional pattern.
Consider the knee as one of the most used and abused joints in athletic activity. An injury to the knee typically causes the joint to be held in sustained flexion during the acute phase. This position is the least-packed joint position, can accommodate increased fluid, and is the most comfortable. This position pulls the soft tissue on the medial and lateral aspects of the knee into an abnormal posterior alignment with the posterior short and anterior long. This misalignment creates abnormal torsion in the skin, muscles, tendons, and ligaments of the medial and lateral aspects of the knee, shortening of structures at the back of the knee, and weakening of the medial quadriceps, particularly the vastus medialis oblique at the distal end of this muscle. Increased torsion causes a decreased flow of fluids in the area, leading to a decreased ability for repair and the tendency for tissue layers to stick together and form adhesions. The sustained position eventually becomes fibrotic, and the knee ends up stuck in flexion and unable to fully extend. At the very least, performance is diminished. Compromised patterns body-wide will begin to occur, and reinjury is likely. Also, compensation patterns in other parts of the body become prone to injury, including a tendency for tissue layers to stick together and for adhesions to develop. So what is the next step? No recipe has been defined; clinical reasoning is essential and revolves around the following.
Key Points
• Apply therapeutic massage with an intelligent focus.
• Normalize soft tissue structures by increasing pliability and separation of the tissue layers.
Massage can potentially do the following:
• Create a mechanical force—tension, bind, shear, or torsion—on the fibers to encourage relaxation
• Reintroduce controlled acute inflammation to signal regeneration of connective tissue structures
• Create a piezoelectric effect (mechanical energy is transformed into electrical energy). The piezoelectric effect increases cellular activity, tissue repair, and alignment.
• Normalize fluid movement, rhythmic cycles of joint compression and decompression (traction), rocking, and specific methods such as lymphatic drain to restore the natural rhythmic movement of the body’s fluids
• Normalize autonomic nervous system, neurotransmitter, and endocrine functions. Deliberate use of stimulation or inhibition and pressure levels encourages appropriate neurochemical function.
Summary
Massage targets both connective tissue and the neuromuscular aspect of muscle tissue function because tension in a muscle and its fascia is created by both active and passive elements. Passive elements include collagen fibers and ground substance, which are influenced by introduction of various mechanical forces through massage. Because muscle contains ground substance, it demonstrates viscous behavior. It becomes thicker and stiff when it is stretched quickly, is cold, or is immobilized. It becomes more fluid-like when it is stretched slowly or when it is heated. Active components include the contractile proteins actin and myosin and the nerves’ massage interactions with the neurochemical stimulus.
The most important signs of impaired muscle function are the following:
• Increased muscle motor tone: occurs when muscles are held in a sustained contraction
• Muscle inhibition: a muscle may be functionally weak, which creates joint instability and causes others to become hypertonic in compensation
• Muscle imbalance: this change in function in the muscles crossing a joint occurs when certain muscles react to stress by getting shorter and tight and others become longer and weak. This is an important factor in chronic pain syndromes because this imbalance alters the movement pattern of the joint.
• Joint dysfunction: muscle dysfunction creates an uneven distribution of forces on the weight-bearing surfaces of the joint.
• Abnormal muscle firing pattern sequences: muscle dysfunction is often expressed by improper contraction sequences.
The reader is strongly encouraged to maintain active study of anatomy and physiology. Unit Two discusses this information in relation to massage benefits, assessment, and treatment plan development. Unit Three explores the related issues of sport pathology and uses this base to build treatment plans.
Visit the Evolve website to download and complete the following exercises.
1. Using the index, locate and summarize various contents in this book related to connective tissue and function. Include concepts of assessment, treatment outcomes, contraindications, and benefits (list page numbers).
2. Using the index locate and summarize content in this book related to joint function. Include concepts of assessment, treatment outcomes, contraindications, and benefits (list page numbers).
3. Using the index, locate and summarize the content in this book related to muscular function. Include concepts of assessment, treatment outcomes, contraindications, and benefits (list page numbers).