Evidence for Sports Massage Benefit
Sport/Fitness and Rehabilitation Outcomes
General Massage Benefits and Safety
Fluid Movement—Blood and Lymph
Research Related to Massage, Tissue Healing, and Musculoskeletal Pain
After completing this chapter, the student will be able to perform the following:
1 Understand and describe massage outcomes based on known and theoretical physiologic mechanisms.
2 List and describe four general outcomes for the athlete/fitness and physical rehabilitation population.
3 Explain evidence that indicates that massage is a supportive and safe intervention.
4 Describe the potential for adverse effects from massage application.
This chapter will present research evidence for the benefits of massage therapy and will expose the inaccurate information. Massage outcome potential will be explained, and evidence related to benefit presented. First we will look at the evidence for massage in general, which is the foundation of massage for athletes. Then we will look at athletic and fitness massage research specifically, as well as evidence for adjunct methods such as hydrotherapy, Kinesio taping, and so forth.
Massage and bodywork can be described as a manual application to the body that influences multiple body responses. Research has shown that massage has validity in influencing body structure and function. It is the body’s ability to respond and to adapt to the stimuli and mechanical forces applied during massage that achieves the desired benefits.
As massage research continues to evolve, our understanding of why the methods provide benefit continues to increase. In addition, research has validated many of the outcomes that in the past were based on opinion and experience. At the same time, the increase in quality research has exposed misconceptions and has confirmed or refuted previous thinking. Three claims of massage benefit that were considered important when working with athletes—improved circulation, removal of lactic acid, and increased muscle strength after massage—have proved to be false. Research has also changed our understanding of training protocols and concepts of recovery. Our understanding of stretching has improved, as has our ability to determine whether it supports or harms performance or has no demonstrable effect. Even the use of ice and cold applications for recovery is under scrutiny. If you want to work effectively with this population and be respected by other professionals who work with athletes, it is necessary to remain current with the research by conducting ongoing searches in databases such as PubMed. This chapter references research primarily from 2005 until today. However, important findings will occur after publication. Some of these findings may even challenge the information presented here. That is okay. A professional remains open to change and to new information. Unfortunately, some aspects of massage delivery and outcome remain in the “it seems to works but we don’t know why” category. When this is the situation, it is necessary to be cautious when making claims that cannot be validated. However, just because a scientific explanation cannot be found for the benefit of a particular approach does not mean it should be discarded and not used. Instead, careful examination of the approach should determine the potential for harm. If concern for harm and detriment is minimal, the method can be incorporated into massage with explanation and intention. For example, the anatomy and physiology interphase for energy-based bodywork methods remains elusive. Compassionate intentional presence and near and/or light touch have little potential for harm. Therefore, respectful integration of an energy-based bodywork method into massage application can be justified. To enhance understanding of the overlap of massage/bodywork in the context of sport and fitness, a very mechanistic approach is presented in this text. However, it is important to remember that touch is a multidimensional experience, encompassing the body/mind/spirit experience of both client and therapist and the interplay of these three realms in the therapeutic relationship.
Typically, the application of massage and bodywork is described in terms of methods and modalities instead of physiologic response. To better understand the relationship of massage application to scientifically based evidence and to the synergistic interface with sport performance, it is necessary to move beyond the classic description of massage in terms such as effleurage or gliding strokes, petrissage or kneading, compression, friction, vibration, rocking, shaking (oscillation), tapotement or percussion, and joint movement. Bodywork methods such as reflexology, shiatsu, Rolfing, Trager, and so forth also do not describe the mechanisms of benefits and outcomes. Instead, to support future research, massage application needs to be described by the type of mechanical force applied, what stimulus the mechanical force causes to specific receptors, tissue type, or physiologic function. Variations in depth of pressure, drag on the tissue, speed of application, direction of movement, frequency of application, duration of application, and rhythm allow for extensive application options based on treatment plan outcomes.
Evidence for Massage
The terms bodywork and massage encompass a huge array of methods and philosophies. This chapter does not intend to teach the application of these methods and styles because excellent instructional texts already exist (see the recommended reading list at the end of the book). The focus of this chapter is to describe the underlying theme of all methods and their relationship to sport and fitness goals, measurable outcomes, and physiologic pleasurable mechanisms, as well as research currently being conducted to support these results (Bialosky et al., 2009). Additionally, logical explanations will be presented for some massage results even though research has not totally proved the response correlation. Many different types of scientific research methods are available. Some provide better evidence than others. Also, some evidence is based on clinical experience and expert opinion. The massage therapy profession is now being challenged to function in an evidence-based and informed manner (Box 3-1).
How the Body Responds to Massage
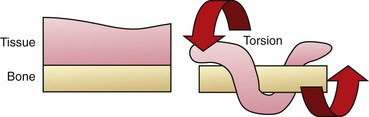
Massage effects appear to be determined by a combination of reflexive and mechanical responses to forces imposed on the body by massage (Box 3-2) (Figures 3-1 and 3-2).
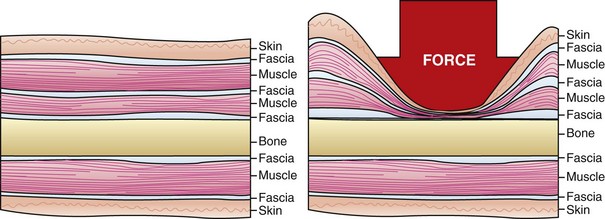
FIGURE 3-1 Massage applications systematically generate force through each tissue layer. This figure provides a graphic representation of force applied, which would begin with light superficial application, progressing with increased pressure to the deepest layer. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 3, St Louis, 2004, Mosby.)

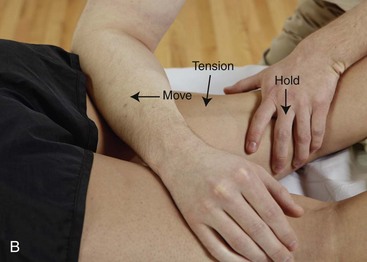








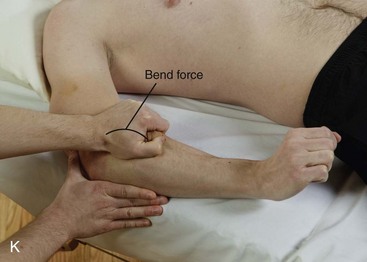
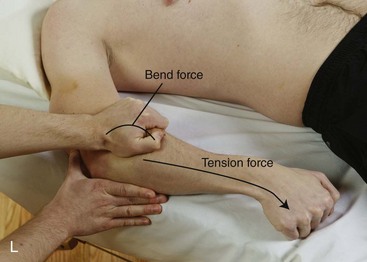

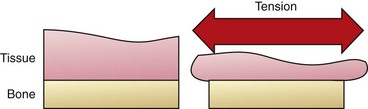
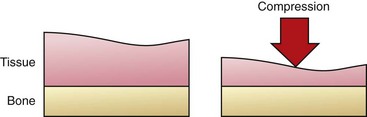
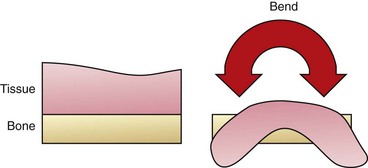
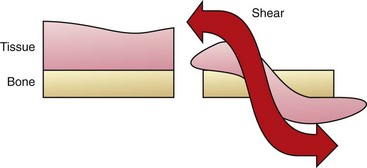
FIGURE 3-2 Examples of mechanical force loading during massage.
A, Tension loading occurs when tissue is elongated. Gliding massage methods and stretching can create tension forces in tissues.
B, Tension forces occur as tissues are stretched.
C, Compression loading occurs when force moves into tissues at a 90-degree angle. In this example, a forearm is used to create compression force in tissues of the shoulder with the client in a side-lying position.
D, Forearm used to compress calf with client in side-lying position.
E, Bending loading. In this example, the hands are used to bend tissues of the calf around the thumbs.
F, Using force compression to displace tissues of the calf, creating a bending force.
G, Example of shear loading. The tissues of the calf are pushed down.
H, Then the same tissues as in part G are pulled up. The back-and-forth movement creates the shear force.
I, Torsion forces twist tissue around a fixed point. In this example, thigh tissues are twisted around the femur.
J, Rotational or torsion forces in massage are generated by kneading. Move tissues by pushing one hand forward and around the fixed point while pulling the other hand back and around.
K, Example of combined loading when two or more mechanical forces are generated. Bending force caused by grasping and lifting.
L, Then client creates the tension force and the wrist is moved.
M, In this example of combined loading, compressive force is created as the therapist presses down on arm tissues and then moves the forearm back and forth to add torsion, bend, and shear forces.
Reflex response results from stimulation of the nervous system to activate feedback loops with the therapeutic intent of adjusting neuromuscular, neurotransmitter, endocrine, or autonomic nervous system (ANS) homeostatic mechanisms. For example, light stimulation of the skin usually results in a tickle or itch response and is arousing and stimulating. Our current understanding is that the effects of massage occur through the interrelationships of the central nervous system (CNS) and the peripheral nervous system (and their reflex patterns and multiple pathways), the ANS, and neuroendocrine control. Current consensus is that massage produces effects through a combination of neural, chemical, mechanical, and psychological factors that are important in supporting athletic performance and a fitness lifestyle.
In general terms, the total sensory input to the CNS affects overall tension throughout the body. This is why nonphysical emotional and mental stress can lead to physical symptoms such as headaches, digestive problems, and muscular discomfort. Massage works on many levels, which aim to reduce the symptoms that cause negative sensory input and to increase positive sensory input. This accounts for the general well-being that clients usually feel after treatment.
Massage can affect the nervous system in several ways. It stimulates nerve receptors in the tissues that control tissue tension. On a sensory level, the responses of mechanoreceptors to touch, pressure, warmth, and so on are stimulated. Generally, a reflex effect leads to further relaxation of the tissues and a reduction in pain.
Tension in the soft tissues can cause overactivity in the sympathetic nervous system. By releasing this tension, massage can restore balance and stimulate the parasympathetic system, resulting in a positive effect on minor and sometimes major medical conditions, such as high blood pressure, migraine, insomnia, and digestive disorders.
Mechanical responses to massage most often result from tissue deformation and the response of the intricate facial system. Structure can be thought of as anatomy, and function as physiology. Some massage applications can shift structure, primarily through influence on the connective tissues of the body. Massage always has a physiologic result because of required adaptation to the presence of the massage practitioner, the sensory stimulation of various touch receptors, and the client’s perception of the therapeutic interaction. Therefore, massage can achieve primarily physiologic responses of the body, and massage results cannot be isolated as strictly structural outcomes. This is an important concept in understanding the synergistic and multidisciplinary use of various methods to support the athlete.
It is reasonable that massage application is likely to influence the adaptive, restorative, and healing capacities of the body. Anatomic and physiologic outcomes include the following:
• Local tissue repair, as with a sprain or contusion
• Connective tissue normalization that affects elasticity, stiffness, and strength, as when pliability of scar tissue or overall flexibility is improved
• Shifts in pressure gradients to influence body fluid movement
• Neuromuscular function interfacing with the muscle length-tension relationship; force couples; motor tone of muscles; concentric, eccentric, and isometric functions; and contraction patterns of muscles working together to support efficient movement
• Mood and pain modulation through shifts in ANS function, yielding neurochemical and neuroendocrine responses
• Increased immune response to support systemic health and healing
Each of these common outcomes for massage supports rehabilitation, fitness, and performance recovery.
Sport/Fitness and Rehabilitation Outcomes
2. List and describe four general outcomes for the athlete/fitness and physical rehabilitation population.
Research often attempts to answer the question, “Does this (medicine, surgery, exercise, machine, food, and so forth) affect this outcome?” Before the evidence is explored, the outcomes need to be defined. The main outcomes of massage for sport and fitness are increased body stamina, stability, mobility, flexibility, and agility; reduced soft tissue tension and binding; normalized fluid (blood and lymph) movement; management of pain; reduction of suffering; support of healing mechanisms; alteration of mood; improved physical and mental performance; and experiences of pleasure. All of these outcomes can be appropriately applied to athlete care or rehabilitation after pathology, especially within the context of a multidisciplinary system.
These outcomes can be classified as four goal patterns for sport and fitness:
The question is, “Is the evidence that supports massage as an intervention to achieve these outcomes as good as or better than that for other types of interventions, and can massage be supportive in conjunction with other approaches to care?”
Performance Enhancement/Recovery
As was previously discussed, fitness and performance are not the same. Optimal performance is most often achieved when fitness is attended to first. Performance motivation and activity exceed fitness requirements by pushing the body to achieve activities that are outside the fitness parameters. Performance therefore becomes a strain on the system. Balancing fitness and performance is tricky with athletes. It is important for those whose goals are fitness oriented to not exceed the beneficial physical outcomes by getting caught up in performance demands that lead to increased strain on adaptive capacity.
Continual performance demand interferes with fitness and compromises health. Normal function and performance are not the same. A person who is learning to walk again after an accident exerts effort and has similar physical manifestations and demands on the body as an athlete does when seeking to decrease his or her 40-yard dash time. However, one is seeking to regain normal function, and the other is striving for peak performance. Performance is more than normal function.
The sports massage therapist needs to consider how the massage application supports the following client goals:
• Achieve normal function through rehabilitation and conditioning
• Reduce the negative effects that performance demand places on the body in excess of normal function
All people who engage in exercise may strive for excellence at some performance level. The elderly person who is beginning a cardiac rehabilitation program, the professional athlete striving for success in competition, and the child learning to walk—anyone who uses the body in a precise way—are all concerned about the ability to carry out an action with skill. Their motivations may vary but the desired outcome is the same—increased proficiency when performing the activity. Physical performance involves training, practice, and demand on the body. When desired performance levels are achieved and practiced, they become automatic.
Performance enhancement requires increasing demand on the body through practice. Maintaining performance involves attention to demand on the body and reinforcement. Each individual has a range of peak performance with the triad of body/mind/spirit function in his or her optimal range. As discussed in Chapter 8, this is called “the zone.” Peak performance is difficult to maintain for extended periods of time. Recovery is necessary to restore depleted energy and regenerate damaged soft tissue. Most athletes train at levels below peak performance with the desired outcome of reaching that peak during competition. This process is compromised if ongoing competition is extended over periods of time. This is common among professional athletes, especially in team sports such as baseball, basketball, football, hockey, and soccer.
Massage application can support performance by facilitating recovery and removing impediments to training.
Condition Management
The goal of condition management is to manage ongoing strain that is not going to change. Examples of such strain include inherent joint laxity, previous injury, emotional demands, and playing schedule. Maintaining the status quo is a common outcome for competing athletes, especially toward the end of a playing season.
Rehabilitation/Therapeutic Change
Injury is a common consequence of physical activity. Anyone who has worked with competing athletes knows the importance of injury prevention and of effective, accelerated injury recovery. Most athletes practice or compete when injured at one time or another. When injury is involved, performance is compromised. It takes more energy, accommodation, and compensation to perform when injured. Specifically, rehabilitation is the return to normal function, and for the athlete, this means return to peak performance (i.e., to function above normal).
Massage in this area is complex and requires the most training. Unit Three of this text deals specifically with injury. The specific massage application for injury is integrated into the general massage protocol.
Palliative Care
Palliative care includes comfort, support, nurturance, and pleasure, which are essential in the care of the athlete. Attention to warm environment, atmosphere, and ambience is part of the caring experience. Patience, flexibility, and commitment are included in the process. Competing athletes are tired, disappointed, and in pain much of the time. Periods of exhilaration and disappointment occur within complex life experiences. The losing athlete needs more support than the winning one. The older athlete needs more care than the young one. When exercising for fitness, weight loss, and rehabilitation, similar stresses occur. Reducing suffering and offering pleasurable sensation are invaluable in reducing the psychological and physical responses to these stresses.
In both training and rehabilitation, plateaus are reached. The satisfaction of seeing ongoing changes is diminished, and palliative care may be able to support the athlete during these periods. Diminished performance due to fatigue and other pressures can be comforted temporarily by nurturing touch. Sometimes there is just too much aching and pain to endure any longer; in this case, palliative massage is the most beneficial technique.
An example is seen in the case of rookie football players in the second week of training camp. They are tired, stressed, sore, and a bit difficult. Their adaptive capacity is maxed out at the moment, and yet they are driven to perform. The best massage approach is palliative care, not performance enhancement.
In the next section, we will consider whether research findings and clinical evidence support the benefit of massage for these outcomes.
General Massage Benefits and Safety
Benefits and safety are the most important factors to consider for any client population. In the sport and fitness world, we have the ability to use research evidence to justify general massage as the foundational approach for this population.
Research findings are mixed regarding the efficacy of massage. Generally, massage as the primary treatment for various conditions was not found to be a definitive treatment on its own, but studies were supportive of many other interventions used in enhancing effects or managing side effects of other treatments. This means that typically massage would be a beneficial part of a fitness program but should not be expected to provide optimal outcomes when it is the only therapeutic intervention used.
The “why massage works” remains elusive, but recurring findings suggest possible physiologic mechanisms for massage benefit. One study by Field and her associates (2005) is particularly relevant for this text because it deals with serotonin, which is associated with body pain modulation mechanisms. In other studies, Diego et al. (2004, 2009) speaks to how massage needs to be applied with sufficient nonpainful compressive force to stimulate an anti-arousal response, and that massage that is considered light tends to stimulate the sympathetic ANS response (Field et al., 2010).
Pressure Depth
Pressure-based massage produces different physiologic changes than are produced by light touch (Sefton et al., 2011; Rapaport et al., 2010). Application of moderate pressure massage appears necessary to influence hypothalamic-pituitary-adrenal function (Rapaport et al., 2010; Field et al., 2010) and diastolic blood pressure (Moraska et al., 2010). Light or moderate pressure massage (or a combination) may reduce the sensitivity of spinal nociceptive reflexes (Sefton et al., 2011; Roberts, 2011).
Light pressure gliding stroke–based massage has been shown to lower heart rate and systolic blood pressure and to decrease the deterioration of natural killer cell activity; however, no effects were identified for cortisol levels and diastolic blood pressure (Hillier et al., 2010; Billhult et al., 2009). Pressure levels used during massage are an important concept for athletes seeking restorative benefits from massage. It appears that moderate to light pressure can affect generalized restorative function, and deep aggressive massage application is not necessary to achieve these benefits.
The study “Massage Reduces Pain Perception and Hyperalgesia in Experimental Muscle Pain: A Randomized, Controlled Trial” (Frey Law et al., 2008) suggests that massage is capable of reducing myalgia symptoms by approximately 25% to 50% (extent of effect varies with the assessment technique used to measure pain). The purpose of this study was to determine the effects of massage on pressure pain thresholds (PPTs) and perceived pain. Researchers used delayed-onset muscle soreness (DOMS) as a model of myalgia (muscle pain). This condition is a major issue for athletes and those attempting to integrate an exercise program into their lifestyle.
The way Frey Law and associates conducted the research was to randomly assign participants to a no treatment control, superficial touch, or deep tissue massage group. A specific type of wrist exercise was performed at visit 1 to cause DOMS 48 hours later at visit 2. Pain, assessed using a visual analog scale (VAS), and pressure needed to cause pain were measured at baseline, after exercise, before treatment, and after treatment.
Results of the study showed that deep massage decreased pain (48.4% DOMS reversal) during muscle stretch. Mechanical hyperalgesia (increased pain response to pressure) was reduced (27.5% reversal) in both the deep massage and superficial touch groups when compared with the control group. The control group did not receive any massage and experienced an increased pain perception of 38.4%. Resting pain did not vary between treatment groups.
If we analyze the Frey et al. study, we can consider that both deep and light pressure massage reduced the sensation of pain, and deep pressure massage helped reduce pain when accompanied by stretching of sore muscles. However, the sensation of pain when there was no activity was not reduced by massage. Now if we think about how this information is used during massage practice, it might be seen as follows.
Example
A client just increased the intensity of his conditioning program and is sore and achy. The client feels stiff, and it hurts to stretch. Based on information provided in the study, massage would likely be most beneficial if a variety of pressures were used, and deeper pressure massage should target those areas that hurt when the client stretches. It might be important to explain to the client that he may still feel achy, but he should be able to move better.
Adverse Effect
Massage is not always the best technique for managing symptoms. According to Hanley et al. (2003), despite very strong patient preference for therapeutic massage, it did not show any benefit over a relaxation tape used to control postsurgery pain. Massage was effective in reducing anxiety but was no more effective than relaxing in a quiet room (Sherman et al., 2010).
Although these studies indicate that massage is effective for anxiety management, it is no more effective than other relaxation interventions. Key, however, is that people liked massage, which is an important factor in compliance with treatment. Muller-Oerlinghausen et al. (2004) concluded that slow-stroke massage is suitable as an intervention for depression, along with other treatment, and is readily accepted by very ill patients. A reduction in distress has been noted among oncology patients in response to massage, regardless of gender, age, ethnicity, or cancer type.
The athletic population often undergoes surgery to repair muscle skeletal injury. During the healing and rehabilitation process, it is common for depression and anxiety to occur based on the change in daily life schedule, as well as concern for future performance ability. Massage and other forms of relaxation intervention can be helpful.
Potential for Harm
When any treatment is assessed, safety is a primary concern (i.e., do no harm). If harm is possible, then the benefits of receiving massage must exceed the potential for harm. A summary of a review of massage safety by Ernst et al. (2006) concludes that massage is generally safe. Massage is not entirely risk free, and we need to be aware of potential harm. However, serious adverse effects are rare. Most adverse effects resulting from massage were associated with aggressive types of massage or massage delivered by untrained individuals. Also, these effects were associated most often with massage techniques other than “Swedish” (classic) massage. These findings are extremely important for those working with athletes. In general, over the years, “sport massage” has incorporated aggressive methods.
Another situation in which adverse effects may occur is when massage interferes with various types of implants such as stents, ports, prostheses, and so forth. Haskal (2008), in the Journal of Vascular and Interventional Radiology, reported a case where a stent placed in the lower limb as treatment for peripheral artery disease migrated to the right atrium after 3 years. Open heart surgery was required to remove the embedded stent fragments. The mechanism attributed with dislodging and moving the stent was deep tissue massage of the thigh. Although this outcome is rare, it is important to pay attention to adverse effects caused by massage. Athletes may have had various surgeries to repair injuries. Often various stabilizing devices such as pins and screws are used. Care needs to be taken to avoid compressing tissues into these areas to prevent potential damage to tissues as they are pushed into the stabilizing devices. Also, the “deep tissue” approach is often used with athletes without considering the potential for damage. Moderate to heavy pressure applied with a small contact such as at the tip of the elbow or with a massage implement such as a hand-held pressure device is more likely to cause tissue damage than pressure applied with a broad contact such as the forearm. Aggressive stretching procedures provide other opportunities for structural damage.
Benefits of stretching in general are being questioned (see later in chapter). A physiologic and safe range of motion has been determined for joints. Any stretching beyond this motion increases the potential for harm. In a cross-sectional study of 100 clients, 10% of massage clients experienced some minor discomfort after the massage session; however, 23% experienced unexpected, nonmusculoskeletal positive side effects. Most negative symptoms started within 12 hours after the massage and lasted for no longer than 36 hours. Most of the positive benefits began to be noted immediately after massage and lasted longer than 48 hours. No major side effects occurred during this study (Cambron et al., 2007). Soreness after massage can affect performance for an athlete. Based on findings of this study, it may be prudent for the athlete to avoid massage a day and a half before competition; however, because the benefits last for at least 2 days, the athlete should still experience positive results from massage.
Key Points
The studies in this section are beginning to provide evidence that massage may do the following:
• May play a role in reducing detrimental stress-related symptoms
• May appear to manage some muscle-type pain
• May likely improve perception of quality of life for those who enjoy massage
More important, massage therapy is typically safe when provided in a conservative and general manner with sufficient nonpainful pressure.
Neuroendocrine Regulation
Neuroendocrine substances carry messages that regulate physiologic functions. Neuroendocrine regulation is a continuous, ever-changing chemical mix that fluctuates with each external and internal demand on the body to respond, adapt, or maintain a functional degree of homeostasis. The immune system produces and responds to these communication substances. Substances that make up this “chemical soup” remain the same, but the proportion and ratio change with each regulating function or message transmission. The “flavor” of the soup, which is determined by the ratio of the chemical mix, affects such factors as mood, attentiveness, arousal, passiveness, vigilance, calm, ability to sleep, receptivity to touch, response to touch, anger, pessimism, optimism, connectedness, loneliness, depression, desire, hunger, love, and commitment.
Mood
Massage therapy appears to have a beneficial effect on anxiety levels; this is important for the management of performance anxiety experienced by many athletes. The therapeutic relationship established between massage therapist and client is similar to that seen in psychotherapy, a treatment that relies on communication and the therapeutic relationship to produce effects. It is possible that massage effects are related to the therapeutic relationship (Moyer et al., 2004). Excessive sympathetic output causes most of the stress-related diseases and dysfunctions, including headache, gastrointestinal difficulties, high blood pressure, anxiety, muscle tension and aches, and sexual dysfunction.
Long-term stress (i.e., stress that cannot be resolved by fleeing or fighting) may trigger the release of cortisol, a cortisone manufactured by the body. Long-term high blood levels of cortisol cause side effects similar to those of the drug cortisone, including fluid retention, hypertension, muscle weakness, osteoporosis, breakdown of connective tissue, peptic ulcer, impaired wound healing, vertigo, headache, reduced ability to deal with stress, hypersensitivity, weight gain, nausea, fatigue, and psychological disturbances.
Because of its generalized effect on the ANS and associated functions, massage can cause changes in mood and excitement levels and can induce the relaxation/restoration response. Massage seems to be a gentle modulator, producing feelings of general well-being and comfort. The pleasure aspect of massage supports these outcomes. This is especially important for sport recovery. The emotional arousal often found in rehabilitation situations is also favorably influenced.
Initially, massage stimulates sympathetic functions. The increase in autonomic, sympathetic arousal is followed by a decrease if the massage is slowed; arousal is sustained with sufficient pleasurable pressure lasting about 45 to 50 minutes. Pressure levels must be relatively deep but not painful. Slow, repetitive stroking, broad-based compression, rhythmic oscillation, and movement all initiate relaxation responses. Sufficient pressure applied with a compressive force to the tissues supports serotonin functions and vagal nerve tone. Compression and a fast-paced massage style stimulate sympathetic responses and may lift depression temporarily.
Pain Modulation
Point holding, such as acupressure or reflexology, releases the body’s own painkillers and mood-altering chemicals from the entire endorphin class. These chemicals stimulate the parasympathetic responses of relaxation, restoration, and contentment. These methods of massage depend on the creation of moderate, controlled pain to relieve pain. It takes a larger pain or stress stimulus to generate the endorphin response than the perception of existing pain. When release of substance P triggers pain, enkephalins are released and suppress the pain signal. A negative feedback system activates the release of serotonin and endogenous opiates, which inhibit pain. Therapeutic massage methods can be used to create a controlled, noxious (pain) stimulation that triggers this cycle. Clients often refer to this noxious stimulation as “good pain.”
Altering the muscles so that they are more or less tense, or changing the consistency of the connective tissue, affects the ANS through the feedback loop, which in turn affects the powerful body/mind phenomenon.
Research now indicates that most problems in behavior, mood, and perception of stress and pain, as well as other so-called mental/emotional dysfunction, are caused by dysregulation or failure of certain biochemical agents. These behaviors, symptoms, and emotional and physical states often are the result of normal chemical mixes that occur at inappropriate times. Athletes are particularly sensitive to neurochemical influences. Highs and lows, wins and losses, pain, and so forth place increased demands on the system.
The effects of neurotransmitters released during massage may explain and validate the use of sensory stimulation methods for treating chronic pain, anxiety, and depression. Much of the research on massage, especially that done at the Touch Research Institute of the University of Miami School of Medicine, revolves around shifts in the proportion and ratio of the composition of the body’s “chemical soup” brought about by massage.
Neuroendocrine Chemicals
Neuroendocrine chemicals potentially influenced by massage include the following:
Dopamine
Dopamine influences motor activity that involves movement (especially learned, fine movement such as handwriting), conscious selection (the ability to focus attention), and mood (in terms of inspiration, possibly intuition, joy, and enthusiasm). Dopamine is involved in pleasure states, seeking behavior, and the internal record system. Low levels of dopamine result in opposite effects such as lack of motor control, clumsiness, inability to focus attention, and boredom. Massage seems to increase the available level of dopamine in the body; this may explain the pleasure and satisfaction experienced during and after massage. The importance of optimal dopamine levels for the athlete is evident.
Serotonin
Serotonin allows a person to maintain context-appropriate behavior; that is, to do the appropriate thing at the appropriate time. It regulates mood in terms of appropriate emotions, attention to thoughts, and calming, quieting, comforting effects; it also subdues irritability and regulates drive states so that the urge to talk, touch, and be involved in power struggles can be suppressed. Serotonin is involved in satiety; adequate levels reduce the sense of hunger and craving such as for food or sex. It also modulates the sleep/wake cycle. A low serotonin level has been implicated in depression, eating disorders, pain disorders, and obsessive-compulsive disorders. A balancing effect has been noted between dopamine and serotonin, much like agonist and antagonist muscles. Athletic competition supports dopamine dominance, but recovery time is serotonin-dependent. Aggressive and impulsive behavior of athletes may be related to imbalances in this area. Massage seems to increase the available level of serotonin. Massage may support the optimal ratio of serotonin and dopamine, especially when used to aid recovery after competition. Care needs to be taken before competition to not disrupt the delicate balance of these neurotransmitters.
Epinephrine/Adrenaline and Norepinephrine/Noradrenaline
The terms epinephrine/adrenaline and norepinephrine/noradrenaline are used interchangeably in scientific texts. Epinephrine activates arousal mechanisms in the body, whereas norepinephrine functions more in the brain. These are the activation, arousal, alertness, and alarm chemicals of the fight-or-flight response and of all sympathetic arousal functions and behaviors. Athletic competition supports the release of these chemicals. If the levels of these chemicals are too high, or if they are released at an inappropriate time, a person may feel as if something very important is demanding his or her attention or may react with the basic survival drive of fight or flight (hypervigilance and hyperactivity). The person might have a disturbed sleep pattern, particularly in terms of lack of rapid eye movement (REM) sleep, which is restorative sleep. The individual with low levels of epinephrine and norepinephrine is sluggish, drowsy, fatigued, and underaroused.
Massage seems to have a regulating effect on epinephrine and norepinephrine through stimulation or inhibition of the sympathetic and parasympathetic nervous systems. This generalized balancing function of massage seems to recalibrate the appropriate adrenaline and noradrenaline levels. Depending on the response of the ANS, massage can just as easily wake a person up and relieve fatigue as it can calm down a person who is anxious and pacing the floor.
It should be noted that initially, touch stimulates the sympathetic nervous system, whereas it seems to take 15 minutes or so of sustained stimulation to begin to engage the parasympathetic functions. Therefore, it makes sense that a 15-minute chair massage tends to increase production of epinephrine and norepinephrine, which can help athletes become more attentive, whereas a 1-hour slow, rhythmic massage engages the parasympathetic functions, reducing epinephrine and norepinephrine levels and encouraging a good night’s sleep, necessary for recovery and healing.
Enkephalins, Endorphins, and Dynorphins
Enkephalins, endorphins, and dynorphins are mood lifters that support satiety and modulate pain. Massage may increase available levels of these chemicals secondary to the introduction of non-harmful pain stimuli. The massage effect is delayed until chemical levels rise to an inhibitory level. It usually takes about 15 minutes for blood levels of enkephalins, endorphins, and dynorphins to begin to rise. Appropriate availability of these pain-modulating chemicals is essential for athletes.
Oxytocin
The hormone oxytocin has been implicated in pair or couple bonding, parental bonding, feelings of attachment, and caretaking, along with its more clinical functions during pregnancy, delivery, and lactation. Massage tends to increase the available level of oxytocin, which could explain the connected and intimate feeling of massage.
Because athletes tend to be single-minded and hyperfocused, the oxytocin influence can support dependence on the therapist. If the massage routine is disrupted, the athlete’s performance can be affected. In this sense, commitment and consistency by the therapist working with competing athletes are essential.
Cortisol
Cortisol and other glucocorticoids are stress hormones produced by the adrenal glands during prolonged stress. Elevated levels of these hormones indicate increased sympathetic arousal. Cortisol and other glucocorticoids have been implicated in many stress-related symptoms and diseases, including suppressed immunity states, sleep disturbances, and increases in the level of substance P. Athletes and those in extensive physical rehabilitation programs are particularly susceptible to increased and sustained cortisol levels. Massage may influence levels of cortisol secondary to the increase in parasympathetic activation.
Growth Hormone
Growth hormone promotes cell division and in adults has been implicated in the functions of tissue repair and regeneration. This hormone is necessary for healing and is most active during sleep. Massage increases the availability of growth hormone indirectly through increased vagal stimulation, predisposing to parasympathetic dominance, encouraging sleep, and reducing the level of cortisol. Again, especially in competing athletes, recovery is a primary goal, and optimal levels of growth hormone are necessary.
Endocannabinoids
Endocannabinoid chemicals are produced in the body; compounds in the cannabis plant produce similar responses, just as morphine creates similar effects as endogenous endorphins. The endocannabinoid system plays an important role in regulating a variety of physiologic processes, including appetite control, energy balance, pain perception, and immune responses. The endocannabinoid (eCB) system is involved in modulation of pain and inflammation. The endocannabinoid system has recently been implicated in the regulation of bone metabolism and may help to reverse bone demineralization (Rossi et al., 2009; Bab et al., 2009).
As of this writing, the research data are insufficient to allow definitive statements regarding the treatment effects of massage therapy on cortisol and other stress-related substances. Although multiple research studies have found significant improvements in stress perception following massage therapy, available studies do not present a high enough level of evidence to allow definitive statements about the effects that massage therapy has on the physiologic functions associated with stress (Moraska et al., 2010).
It is not clear if massage directly influences neurochemicals that influence mood and behavior, but research in touch is promising. For example, a study named “Influence of a ‘Warm Touch’ Support Enhancement Intervention Among Married Couples on Ambulatory Blood Pressure, Oxytocin, Alpha Amylase, and Cortisol” (Holt-Lunstad et al., 2008) investigated whether a support intervention (warm touch enhancement) influences physiologic stress systems that are linked to important health outcomes. Findings indicated that physical and physiologic bonds occur with consistent warm touch. The compassionate touch of massage is a form of warm touch. Therefore, it is common for a bond to be formed between client and massage therapist. This bond between athlete and massage therapist can be exaggerated within the context of the therapeutic massage because of the intensity of the performance demand.
Serotonin is another important neurochemical related to stress levels. A study conducted in the Netherlands (Bakermans-Kranenburg and van Ijzendoorn, 2008) explored the relationship of oxytocin and serotonin to what they termed “sensitive parenting.” Animal studies suggest an important role of oxytocin in parenting and in social interactions with offspring. Evidence also indicates that the neurotransmitter serotonin may be important through its influence on mood and the release of oxytocin.
It is common to find a correlation between stress, anxiety, depression, and pain. This combination is common within the sport and fitness world. When a correlation is noted, a relationship between elements exists, but this does not mean that one of the elements causes the other. Therefore, although stress, anxiety, depression, and pain are commonly found together, it is not clear whether any one of these elements causes any of the others. Regardless, these four situations often respond to the same applications of massage. The following studies indicate that massage is helpful in management of these conditions. In 2002, a connection was made between pain perception and oxytocin using a massage-like intervention (Lund et al., 2002). A study of women giving birth indicates that oxytocin levels are increased using acupressure (Kashanian and Shahali, 2009).
Other studies have found that massage did not necessarily influence oxytocin levels. Recall that oxytocin is related to feelings of connectedness and bonding. Although most of the oxytocin studies involve touch, as massage therapists we can at least intelligently speculate that massage would produce similar responses because massage is a pleasurable touch.
Still other studies have found that (1) arginine vasopressin and/or cortisol levels changed after massage, indicating reduced stress response (Bello et al., 2008; Garner et al., 2008; Mackereth et al., 2009; Stringer et al., 2008; Lindgren et al., 2010), and that (2) the cortisol reduction response to massage is small if it occurs at all and may not equate to the reported physiologic changes (Noto et al., 2010; Moyer et al., 2011).
It can be summarized that therapeutic massage may, through the influence on the autonomic nervous system and the use of not harmful pain stimuli, help balance blood levels of serotonin, dopamine, endocannabinoids, and endorphins, which, in turn, facilitates the production of natural killer cells in the immune system and regulates mood. Oxytocin tends to increase supporting feelings of connectedness. These responses indicate that it would be beneficial to include massage as part of the total treatment program for athletes as well as in fitness programs.
Somatic Influence
The effects of massage can be processed through the somatic division of the peripheral nervous system. The somatic division controls movement and muscle contraction and relaxation patterns, as well as muscle and motor tone. Muscle tone is a mixture of tension in the connective tissue elements of the muscle and intermuscular fluid pressure. An example of muscle tone dysfunction is delayed-onset muscle soreness. Muscle tone is influenced more by mechanical massage applications as previously discussed. Motor tone is produced by motor neuron excitability and is influenced by reflexive massage application, which inhibits motor neuron activity. The most common reason for an increase in motor tone is the increase in sympathetic arousal and in sustained sympathetic dominance. Another cause is proactive muscle guarding after injury and nervous system damage. Both situations are common in athletes.
The usual outcome of reflexive massage is inhibitory and anti-arousal. Anti-arousal massage (relaxation massage) may influence motor tone activity in the same way that pharmaceutical muscle relaxers do, because the main reason for motor tone difficulties is sympathetic arousal.
In working with the neuromuscular mechanism in massage, the basic premises are as follows:
• Substitute a different neurologic signal stimulation to support a normal muscle resting length.
• Influence muscle and motor tone by lengthening and stretching muscles and connective tissue.
Dysfunction of soft tissue (muscle and connective tissue) without proprioceptive hyperactivity or hypoactivity is uncommon. It is believed that proprioceptive hyperactivity causes tense or spastic muscles and hypoactivity of opposing muscle groups. The main proprioceptors influenced by massage are the spindle cell and the Golgi tendon receptor. Mechanoreceptors of the skin are also influenced by stretching, compression, rubbing, and vibration of the skin. Stimulation of joint mechanoreceptors affects adjacent muscles, and the stimulation of the skin overlying muscle and joint structures has beneficial effects on these owing to shared innervations.
Deep broad-based massage has a minimal and short-term inhibitory effect on motor tone of muscle. It is used primarily to support a muscle reeducation process such as therapeutic exercise, or to temporarily reduce motor tone so that muscle activation sequences (firing patterns) can be reset. Inhibiting motor tone allows more mechanical methods to address tissue shortening without causing muscle spasm.
Active movements of the body, using techniques such as active assisted joint movement, and the application of active muscle contraction and release, as used during muscle energy methods of tense and relax, reciprocal inhibition, and combined methods of strain/counterstrain, do seem to improve motor function through interaction with proprioceptive function.
Vestibular Apparatus and Cerebellum
The vestibular apparatus is a complex system composed of sensors in the inner ear (vestibular labyrinth), upper neck (cervical proprioception), eyes (visual motion and three-dimensional orientation), and body (somatic proprioception) processed in several areas of the brain (brainstem, cerebellum, parietal and temporal cortices). Reflex activity affects the eyes (eurogeni-ocular reflexes), the neck (vestibulocolic reflexes), and balance (vestibulospinal reflexes) by sending and receiving information at the same time about how we are oriented to the environment around us. As an example, many amusement park rides create disorienting sensations in the vestibular apparatus that contribute to the effects of the ride.
The vestibular apparatus and the cerebellum are interrelated. Output from the cerebellum goes to the motor cortex and the brainstem. Stimulating the cerebellum by altering the motor tone of muscles, the position of the body, and vestibular balance stimulates the hypothalamus to adjust ANS functions to restore homeostasis. Reflex response time seems to be quicker in athletes than in nonathletes. Most athletes are extremely sensitive in this area.
The massage techniques that most strongly affect the vestibular apparatus and therefore the cerebellum are those that produce rhythmic oscillation, including rocking during the application of massage. Rocking produces movement at the neck and head that influences the sense of equilibrium. Rocking stimulates inner ear balance mechanisms, including the vestibular nuclear complex and the labyrinthine righting reflexes, to keep the head level. Stimulation of these reflexes produces a body-wide effect involving stimulation of muscle contraction patterns.
Massage can alter body positional sense and the position of the eyes in response to postural change. It initiates specific movement patterns that change sensory input from muscles, tendons, joints, and skin and stimulate various vestibular reflexes. This feedback information, which adjusts and coordinates movement, is relayed directly to the motor cortex and the cerebellum, allowing the body to integrate sensory data and adjust to a more efficient postural balance. If massage application involves vestibular influences, short-term nausea and dizziness can occur while the mechanisms rebalance. Using massage to restore appropriate muscle activation firing pattern sequences and gait reflexes is valuable. Influencing the balance of the various force couples within the body can shift the relationship of the eyes, neck, hips, and so forth and influences positional balance, mobility, and agility.
Hyperstimulation Analgesia
In 1965, Melzack and Wall proposed the gate control theory. Although some aspects of the original theory have been modified over the past 40 years, the basic premise remains viable. According to this theory, a gating mechanism functions at the level of the spinal cord. Pain impulses pass through a “gate” to reach the lateral spinothalamic system. Pain impulses are transmitted by large-diameter and small-diameter nerve fibers. Stimulation (e.g., rubbing, massaging) of large-diameter fibers prevents small-diameter fibers from transmitting signals and helps suppress the sensation of pain, especially sharp or visceral pain. Various massage methods, including pressure, positioning, and lengthening, provide this stimulation at sufficient intensity to activate the gating mechanism and produce hyperstimulation analgesia. Pain sensation may be reduced through manual analgesia by stimulating the sensory gating achieved when multiple sensations are processed at the same time. The reflexology (foot massage) benefit seems to be mediated by hyperstimulation analgesia.
Tactile stimulation produced by massage travels through the large-diameter fibers. These fibers also carry a faster signal. In essence, massage sensations win the race to the brain, and pain sensations are blocked because the gate is closed. Stimulating techniques such as percussion or vibration of painful areas to activate “stimulation-produced analgesia,” or hyperstimulation analgesia, also are effective. Pain management for those involved with sport and fitness is essential. Therefore, these methods are beneficial.
Counterirritation
Counterirritation is a superficial irritation that masks some irritation of deeper structures. Counterirritation may be explained by the gate control theory. Inhibition in central sensory pathways, produced by rubbing or oscillating (shaking) an area, may explain counterirritation.
All methods of massage can be used to produce counterirritation. Any massage method that introduces a controlled sensory stimulation intense enough to be interpreted by the client as a “good pain” signal will work to create counterirritation.
Massage therapy in many forms stimulates the skin over an area of discomfort. Techniques that create friction for the skin and underlying tissue to cause reddening of the skin are effective. Many sport therapeutic ointments contain cooling and warming agents and mildly caustic substances (capsicum) and are useful for muscle and joint pain. This is also a form of counterirritation.
Nerve Impingement
A nerve that is compressed or squeezed is a nerve impingement. Tissues that can bind include skin, fascia, muscles, ligaments, joint structures, and bones. An increase in fluid in an area can also result in nerve impingement. Shortened muscles and connective tissues (fascia) often impinge on major and minor nerves, causing discomfort. Tissues that are long and taut can also impinge on a nerve.
The specific nerve root, trunk, or division affected determines the condition such as thoracic outlet syndrome, sciatica, or carpal tunnel syndrome. Therapeutic massage techniques work in many ways to reduce pressure on nerves. The main ways include the following:
• Reflexively changing the tension pattern and lengthening the short muscles
• Mechanically stretching and softening connective tissue
• Interrupting the pain-spasm-pain cycle caused by protective muscle spasm that occurs in response to pain
• Supporting the effectiveness of therapeutic exercise to shift posture and function
• Supporting the use of medications such as antispasmodics, analgesics, antiinflammatories, and circulation enhancers such as vasodilators.
Connective Tissue Influences
The mechanical behavior of soft issue in response to tissue loading is related to the property of connective tissue viscoelasticity, as described in the anatomy and physiology review in Unit One. Connective tissue is a biological material that contains a combination of stiff and elastic fibers embedding a gel medium. Connective tissue, the structural component of the body, is the most abundant body tissue. Its functions include support, structure, space, stabilization, and scar formation. It assumes many forms and shapes, from fluid blood to dense bone. The pliability of connective tissue, which is based on its water-binding components, is significantly affected by connective tissue massage. Connective tissue is adaptive and is responsive to a variety of influences, such as injury, immobilization, overuse (increased demand), and underuse (decreased demand).
The basic connective tissue massage approach consists of mechanically softening the tissue by introducing various mechanical forces that result in pressure, pulling, movement, and stretch on the tissues; this allows them to rehydrate and become more pliable. The process is similar to softening gelatin by warming it. If you want connective tissue to stay soft, water must be added. This is one reason why it is important for the client to drink water before and after the massage.
Stretching, pulling, or pressure on the connective tissue is a little different from that seen with neuromuscular methods. Neuromuscular techniques usually flow in the direction of the fibers to affect the proprioceptive mechanism and create a quick response. Connective tissue approaches are slow and sustained, usually against or across the fibers. Connective tissue stretching is elongated or telescoped at the point of the tissue movement barrier.
Another aspect of connective tissue massage application is the generation of healing potentials through creation of controlled therapeutic inflammation.
The most specific localized example of this type of application is the cross-fiber friction concept of Dr. James Cyriax. This method is effective, especially around joints, where the tendons and ligaments become bound down to underlying or adjacent tissue. Deep transverse friction is always a specific rehabilitation intervention. It introduces therapeutic inflammation through creation of a specific and controlled acute reinjury of the tissues. Frictioning can last as long as 15 minutes to create controlled reinjury of the tissue, which introduces a small amount of inflammation and traumatic hyperemia to the area. The result consists of restructuring of the connective tissue, increased circulation to the area, and temporary analgesia.
Proper rehabilitation after friction massage is essential for the friction technique to be effective and produce a mobile scar or rehealing of the tissue. The area must be contracted painlessly with no strain placed on the tissue. This is done by fixing the joint in a position in which the muscle is relaxed, and then having the client contract the muscle as far as it will go. This is sometimes called a broadening contraction (Figure 3-3). The exercise is performed as 5 to 10 repetitions, 3 to 4 times a day.
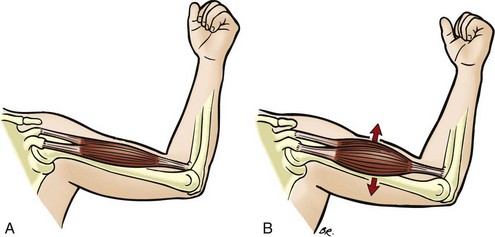
FIGURE 3-3 Broadening contraction.
(From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 3, St Louis, 2004, Mosby.)
Myofascial System
Day et al. (2009) consider the myofascial system to be a three-dimensional continuum, meaning that we cannot really separate muscle or any other type of tissue from the surrounding fascia or the body as a whole (i.e., there is no such thing as an individual muscle). Dr. Carla Stecco and Dr. Antonio Stecco have carried out extensive research into the anatomy and histology of the fascia via dissection of unembalmed cadavers, providing a biomechanical model that assists in deciphering the role of fascia in musculoskeletal disorders. Everything moves within the body, and parts need to slide over and around other parts of the body. Slippery fluid secreted by the body allows structures to slide. In muscle or myofascia, part of the fascia is anchored to bone (or another structure), and part is free to slide. If tissues cannot slide as they are supposed to, inflammation and reduced range of motion and strength can occur. Fascia is formed by crimped/wavy collagen fibers and elastic fibers arranged in distinct layers, and within each layer the fibers are aligned in a different direction. These fibers are embedded in a gelatin-like structure called ground substance. Fascia can be stretched because of the wavy nature of the fiber structure and the elastic fibers, which allows fascia to return to its original resting state. Subcutaneous fascia (tissue containing body fat located under the skin but on top of muscle) forms a very elastic sliding membrane essential for thermal regulation, metabolic exchanges, and protection of vessels and nerves. Deep fascia is more stiff and thin (think “duct tape”) than subcutaneous fascia. Deep fascia surrounds and compartmentalizes the muscles and forms the structures that attach soft tissues to bone. This type of fascia also forms a complex latticework of connective tissue, resembling struts, cross-beams, and guy wires, which help to maintain the structural integrity and function of the body. Another important fascia process is the ability of fibers and the tissue layer to slide relative to each other. According to Medline, the lubricating substance, called mucopolysaccharide, acts as both a lubricant (allowing the fibers to easily slide over one another) and a glue (holding fibers of the tissue together into bundles). Remember that connective tissues are made up of tendons, ligaments, and the fascial sheaths that envelop, or bind down, muscles into separate groups. These fascial sheaths, or fasciae, are named according to where they are located within the muscles:
• Endomysium: innermost fascial sheath, which envelops individual muscle fibers
• Perimysium: fascial sheath that binds groups of muscle fibers into individual fascicles (bundles). In addition, the perimysium provides slip planes between muscle bundles necessary for shape and directional changes, and one structure slides upon another. Thin layers of adipocytes (fat cells) are found between fascial layers separating adjacent structures, allowing single layers to slide over those below, beside, and above it (Purslow, 2010).
• Epimysium: outermost fascial sheath, which binds entire fascicles
Tom Myers (Anatomy Trains) for many years has described that the overall concept in myofascial anatomy is to trace grains and lines of the muscle and fascia while searching for straps, slings, and tensional lines, which extend farther than in a solitary muscle. Privileged to train directly with Ida Rolf (Rolfing), Tom Myers developed the Anatomy Trains concept, which is now validated by the researchers mentioned. An alternate name is emerging—myokinetic chain (Stecco, 2004).
It is likely that innervated fascia is maintained in a taut resting state called fascial tone, which refers to the different muscular fibers that pull on it (think “trampoline”). Fascial tone provides stability, supports tensegrity, and therefore becomes a mechanism of force transmission and potentially a communication network somewhat like a spider web. A spider can feel the vibrations and pulls and tugs on its web, alerting it that something has touched the web. The endomysium appears to be involved with transmission of contractile forces from adjacent muscle fibers within fascicles to prevent overstretching. The perimysium and the epimysium transmit mechanical forces through interconnected fascial units (myokinetic chains). Myofascial tissues connect muscles mechanically to neighboring muscular and nonmuscular structures (Yucesoy, 2010).
Free nerve endings and receptors within the fascial tissue sense any variation in the shape of the fascia and therefore any movement of the body, whenever it occurs (Stecco et al., 2007). Deep fascia is designed to sense and assist in organizing movements and plays a proprioceptive role. At the same time, the larger nerve fibers are often surrounded by loose connective tissue, which isolates the nerve from the traction to which the fascia is subjected.
Whenever a body part moves in any given direction, a myofascial, tensional rearrangement is evident within the corresponding fascia. Sensory nerve receptors embedded within the fascia are stimulated, producing accurate directional information that is sent to the central nervous system. Changes (too loose/too tight/twisted) in the gliding of the fascia will cause altered movement and tissue adaptation.
Robert Schleip directs the Fascia Research Project at Ulm University, Germany, and serves as Research Director of the European Rolfing Association. Schleip (2003) indicates that fascia is embedded with sensory receptors called mechanoreceptors. The presence of these receptors makes fascia a sensory organ with free nerve endings that respond to mechanical force stimulation. Massage is a form of mechanical force stimulation. Schleip et al. (2006) indicate that when connective tissues are out of balance, resulting in soft tissue strain, mechanoreceptors in the fascia can trigger changes in the autonomic nervous system.
Mechanical Stimulation and Interfascial Water
The European Fascia Group (Schleip et al., 2006) found that when fascia is stretched, water is squeezed out, causing complex and dynamic water changes. Water in our bodies has different physical properties from ordinary water because of the presence of proteins and other biomolecules in the water. Research is now providing insight into the behavior of water that interacts with protein in the human body. Proteins change the properties of water to perform particular tasks in different parts of our cells.
In response to mechanical stimuli, smooth muscle–like contraction and relaxation responses of the whole tissue occur, creating squeezing and refilling effects in the semiliquid ground substance. Sommer and Zhu (2008) note that interfascial water plays a key part in what is termed protein folding, the process necessary for cells to form their characteristic shapes, and that nanocrystals are a part of this process, and that these are influenced by light. “In the course of a systematic exploration of interfascial water layers on solids, we discovered microtornadoes, found [as] a complementary explanation [of] the surface conductivity on hydrogenated diamond, and arrived at a practical method to repair elastin degeneration using light.”
Pollack, a leading researcher in this field, and associates have shown that water at times can demonstrate a tendency to behave in a crystalline manner (2010). He has discussed interfascial water in living cells known as vicinal (crystalline) water. Interfascial water exhibits structural organizations that differ from those of common bulk water. Vicinal water seems to be influenced by structural properties that characterize the cell.
Several years ago, Klinger et al. (2004) showed that the water content of fascia partially determines its stiffness, and that stretching or compression of fascia (as occurs during almost all manual therapies) causes water to be extruded (as with squeezing of a sponge), making the tissues more pliable and supple. After a while, the water is taken up again, and stiffness returns, but in the meantime, structures can be mobilized and stretched more effectively and comfortably than when they were densely packed with water.
Klinger et al. (2004) measured wet and dry fresh human fascia and found that during an isometric stretch, water is extruded, refilling during a subsequent rest period. As water extrudes during stretching, temporary relaxation occurs in the longitudinal arrangement of collagen fibers. If the strain is moderate, and no microinjuries occur, water soaks back into the tissue until it swells, becoming stiffer than before.
Research suggests that tissue response to manual therapy may relate to the sponge-like squeezing and refilling effects noted in the semiliquid ground substance of connective tissue.
Muscle energy technique–like contractions and stretches almost certainly have similar effects on the water content of connective tissue, as do myofascial release methods and the multiple force-loading elements of massage.
According to Langevin et al. (2005), it is the dynamic, cytoskeleton-dependent responses of fibroblasts to changes in tissue length that have important implications for our understanding of normal movement and posture, as well as therapies using mechanical stimulation of connective tissue, including physical therapy, massage, and acupuncture.
Mechanical Stimulation Research Results:
• 80% of main trigger points lie on points located on a meridian (Wall & Melzack, 1990; Langevin & Yandow, 2002).
• Meridians may be fascial pathways; the fascial network represents one continuum from the internal cranial reciprocal tension membranes located inside the skull to the plantar fascia of the feet, similar to the interconnected pathway of meridians (Langevin & Yandow, 2002).
• Trigger points and acupuncture points may signify the same phenomenon (Kawakita et al., 2002).
• Acupuncture points and many effects of acupuncture seem related to the fact that most localized Ah shi points lie directly over areas of fascial cleavage (Langevin et al., 2001).
• Acupuncture points and most trigger points are structurally situated in connective tissue. The fascia network of the human body may be the physical substrate represented by the meridians of traditional Chinese medicine (TCM) (Bai et al., 2011).
• A cellular network of fibroblasts within loose connective tissue that occurs throughout the body may support yet unknown body-wide cellular signaling systems, which influence integrative functions at the level of the whole body (Langevin et al., 2004).
• Temporomandibular joint dysfunction may play an important role in the restriction of hip motion experienced by patients with complex regional pain syndrome, indicating a connectedness between these two regions of the body (Fischer et al., 2009).
Myofascial Trigger Points
Ongoing research is beginning to clarify our understanding of trigger points; however, the phenomenon remains unclear. Simons’ Integrated Hypothesis (2008) describes a complex process of trigger point formation and perpetuation. In the trigger point region, sensitized nociceptors lead to local and referred pain because of excessive acetylcholine (Ach) leakage at the motor endplate, which results in sarcomere shortening (Niddam et al., 2007). Motor dysfunction of the myofascial tissue forms a constant, discrete hardness, usually palpable as a nodule in a taut band within the belly of the muscle, and increased pain and acidic inflammation–related sensitizing biochemicals at the trigger point site (Shah & Gilliams, 2008; Shah et al., 2008). Tissue texture is altered, and compromised capillary circulation occurs. This leads to local hypoxia and/or tissue damage. A positive feedback loop occurs. Trigger points have been identified by sonograph and on magnetic resonance imaging (Kuan, 2009; Sikdar et al., 2009).
Latent points are trigger points that are not actively causing referred pain but that may interfere with motor function (Ge et al., 2008); if contributing to the ongoing symptom pattern, they should be addressed.
Research points toward a holistic role for the mechanical distribution of strain in the body that goes far beyond merely dealing with localized tissue pain. Creating an even tone across the bones and myofascial component and, further, across the entire fascial net can have profound implications for health—both cellular and general. The goal for massage is to support balance in the myofascial systems.
Classifications of fascial layering are artificial because the tensegric nature of fascia is seen as one large, interconnected, three-dimensional microscopic dynamic grid structure that connects everything with everything. Through the fascial system, if you pull on the little toe, you affect the nose, and if the structure of the nose is dysfunctional, it can pull anywhere in the body, including the little toe.
Although fascia generally orients itself vertically in the body, it will orient in any directional stress pattern. For example, scar tissue may redirect fascial structures, as can trauma, repetitive strain patterns, and immobility. This redirection of structural forces occurs as a result of compensation patterns. During physical assessment, the body appears “pulled” out of symmetry, or stuck.
Three or four transverse fascial planes are present in the body (depending on the resource you use). They are located at the cranial base, the cervical thoracic area, the diaphragm, and the lumbar and pelvic floor areas. Transverse planes are available for joints as well.
Myofascial/Connective Tissue Dysfunction
Myofascial/connective tissue dysfunction compromises the efficiency of the body, requiring an increase in energy expenditure to achieve functioning ability. Fatigue and pain often result. Fascial shortening and thickening restrict movement, and the easy undulations of body rhythms and entrainment mechanisms are disturbed. Twists and torsions of the fascia bind and restrict movement from the cellular level outward to joint mobility. This binding can be likened to ill-fitting clothing or, more graphically, “fascial wedgies.” The dysfunctions are difficult to diagnose medically, are not apparent with standard medical testing, and are a factor in many elusive chronic pain and fatigue patterns. They can disrupt athletic performance demands.
Healing of damage to body tissues requires the formation of connective tissue. In the first stages of healing, the inflammatory response is one trigger that generates the healing process. When the inflammatory response does not effectively resolve itself, more new tissue than is needed forms, and adhesions or fibrotic tissue develops. An adhesion is an attachment of connective tissue to structures not directly involved with the area of injury. Fibrosis is abnormal tissue formation, often in response to increased protein content in stagnant edematous tissue. Massage can be used to effect chronic inflammation, adhesion, and fibrotic tissue formation. Forces are applied to adhesions and fibrotic tissue, creating mild inflammation to stimulate connective tissue remodeling.
Connective tissue dysfunction usually is suspected as a factor in disorders older than 12 weeks, especially if the inflammatory response and the muscle tone patterns have not effectively resolved during normal healing.
Two basic massage approaches are used to address connective tissue dysfunction and, more important, to prevent dysfunction from occurring:
1. Some methods address the ground substance, which is thixotropic, meaning that the substance liquefies on agitation and reverts to a gel when standing. Ground substance is also a colloid. A colloid is a system of solids in a liquid medium that resists abrupt pressure but yields to slow, sustained pressure. (Think “silly putty” or “clay.”)
2. Other methods address fibers contained within the ground substance. These fibers may be collagenous (rope-like), elastic (rubber band—like), or reticular (mesh-like).
Methods that primarily affect the ground substance have a quality of slow, sustained pressure and agitation. Use of shearing, bending, and torsion forces and tension (tensile stretch) applied during massage adds energy to the matrix, softening it and encouraging rehydration. Most massage methods can soften the ground substance as long as the application is not abrupt.
Thermal influences from repeated loading and unloading create hysteresis, which is the process of energy loss due to friction when tissues are loaded and unloaded. On/off application of compression and oscillation methods that are intense enough to load tissues are often used. Heat will be produced during such a sequence, affecting the viscosity of the ground substance. The increase in pliability is due to the thixotropic nature of connective tissue ground substance through the introduction of energy by the application of forces, particularly shear and torsion, which cause a gel to become less viscous, because the tissue is hydrophilic and attracts water. Attention to these methods and outcomes is supportive of athletic massage goals.
Because of the water content of connective tissue, the balance of fluid flow, appropriate hydration, and principles of fluid dynamics in the body point to the importance of applying effective massage to address fluid movement in the body. Thermal or warming modalities support this process.
The fiber component of connective tissue is affected by methods that elongate fibers past the elastic range (i.e., past the normal give) into the plastic range (i.e., past the bind or point of restriction). For chronic conditions, an acute inflammatory response can be created by using massage to create minor rupture of collagen fibers, leaving free endpoints. These endpoints initiate an inflammatory response and synthesis of collagen by fibroblasts. The collagen is deposited to reunite the endpoints. The newly formed tissue has low tensile strength, is more susceptible to forces imposed, and can be encouraged to change structure, including increased or decreased tissue density, direction, and layering. Continued massage applications serve to influence tissue direction, length, and pliability, and to support effective healing. The positive therapeutic objective is to create therapeutic inflammation to encourage adaptation to controlled damage. Methods used to create the therapeutic inflammatory process are intense and may be interpreted as pain. The method used most often is friction (shear force).
Fascial restrictions can create abnormal strain patterns that can crowd or pull the osseous structures out of proper alignment. This results in compression of joints, producing pain and/or movement dysfunction. Neural and vascular structures can become entrapped in these restrictions, causing neurologic or ischemic conditions. Shortening of the myofascial fascicle can limit its functional length, reducing its strength, contractile potential, and deceleration capacity.
After injury, two separate processes may be occurring simultaneously: scar tissue development within traumatized tissues, and fibrosis in surrounding tissues caused by the presence of an inflammatory mediator. According to Langevin and Sherman (2007), fear of pain related to movement leads to a cycle of decreased movement, connective tissue remodeling, inflammation, and nervous system sensitization, which results in further decreased mobility. The mechanisms of a variety of treatments, such as massage, may reverse these abnormalities by applying mechanical forces to soft tissues (Chaitow & DeLany, 2002).
Based on a tensegrity principle (everything is connected, like a spider web), direct or indirect connections between fasciae seem to allow the transfer of tension over long distances. Massage applied to deform (change the shape) and stretch the soft tissue has an effect on the electrical and mechanical activities of other muscles not being massaged, but still indirectly connected to the massaged tissue. Massage therapy appears to influence muscle motor tone not only by massaging directly on the tissue, but also by indirectly affecting another distant soft tissue structure (Kassolik et al., 2009).
These concepts are useful for massage practitioners who work with athletes and other performers, in whom flexible and well-organized fasciae and myofascial relationships enhance performance and reduce the incidence of injury. Because the living tensegrity network is both a mechanical and a vibratory network, restrictions in one part have both structural and energetic consequences for the entire organism.
Various fascia-targeted techniques used in massage and other bodywork methods contain the same components. Any form of application that deforms (changes the shape of) tissue will affect fascia. All tissue compression, twisting, and stretching approaches may influence fascia. During massage, the therapist finds the area of tightness/bind where normal sliding of fascia does not occur, and some sort of mechanical force is applied to the area, allowing tissues to normalize by becoming more pliable, stimulating increased lubrication, changing water content, and sending signals to adjacent and distant areas of the body. It is likely that many more effects are waiting to be identified through the research process.
The more elastic connective tissue is present around a joint, the greater is the range of motion in that joint. Paoletti (2002), Stecco (2004), and Stecco et al. (2006) hypothesize that the deep fascia transmits forces between two adjacent joints and between synergic muscle groups, supporting the concepts of myokinetic chains.
The endocannabinoid (eCB) system, similar to the endorphin system, is involved in modulation of pain and inflammation. Endocannabinoid chemicals are produced in the body, and compounds in the cannabis plant causes similar responses, just as morphine creates effects similar to those produced by endogenous endorphins. The endocannabinoid system plays an important role in regulating a variety of physiologic processes, including appetite control, energy balance, pain perception, and immune responses. The endocannabinoid system has also been implicated in the regulation of bone metabolism (McPartland, 2008).
According to McPartland (2008), eCB reduces inflammation in myofascial tissues and plays a role in fascia reorganization. Evidence suggests that the eCB system may help resolve myofascial trigger points, and even may address pain that is resistant to treatment (Jhaveri et al., 2007); (Guindon & Hohmann, 2008). Studies of endogenous cannabinoids (endocannabinoids) have demonstrated that they are present in most tissues, and that in some pain states, such as neuropathic pain, levels of endocannabinoids are elevated at key sites involved in pain processing. Norrbrink and Lundeberg (2011) found massage to be effective in the management of neurogenic pain. This may become an important benefit if a connection is present between massage effects and the endocannabinoid system of the body. The eCB system is also influenced by exercise (Sparling et al., 2003).
Manipulation of fascial tissues by equiaxial stretching, which affects fibroblasts and myofibroblasts, has revealed that fascia, chondrocytes, and synoviocytes found in cartilage and joint membrane adipocytes in the superficial fascia and keratinocytes in the skin increased activity of the endocannabinoid system (McPartland, 2008). Because mechanical forces imposed on tissue by massage essentially manipulate the tissue in a similar manner as equiaxial stretching, it is logical to expect that massage would affect the endocannabinoid system by increasing the effects of this system. As with most massage therapy–related research, it is necessary to continue to study this area with a quality research design before definitive statements can be made, but the preliminary findings are exciting. Because management of pain and inflammation is a major goal of massage for athletes, it is logical to factor the effects of an unregulated endocannabinoid system into the goals for massage. Additionally, the immune system is supported, as is the appetite, which is important to the athlete.
Male and Female Hormone Effects on Connective Tissue
Connective tissue in the body is influenced by sex hormones. This information begins to explain why female athletes experience an increased frequency of ligament injuries. It appears that variation in estradiol and progesterone levels during the menstrual cycle influences ligament laxity and stiffness, and that estrogen receptors are found in tendon and ligament fibroblasts (Kjær & Hanse, 2008; Park et al., 2009; Moreno-Lorenzo et al., 2011).
Increased laxity may explain why anterior cruciate ligament (ACL) injury is so common in female athletes. Female hormone levels are related to increased knee joint laxity and decreased stiffness at ovulation.
Key Points
• Massage benefits may occur when we normalize tissues that are tense/tight/deformed/twisted/compressed by introducing mechanical forces (pulling, pressing, bending, twisting) into tissues of the body using massage, stretching, mobilizing, etc.
• The fascia is everywhere, connecting everything together so that the body functions as one integrated unit instead of as individual parts. We still do not know specifics about the massage application that best influences the fascia.
• Endocannabinoids are stimulated by some fascial methods. Focused tension (stretching) of the tissues currently appears to be the most effective mechanical force to influence fascia.
• We think that the force applied during massage needs to move the tissue until it binds, and at that point, just a bit more force is applied, holding it there.
• The current range reported for how long force should be applied is from 15 seconds to 3 minutes.
• Right now, we just do not know how often force needs to be applied, but expert opinions range from daily to weekly. These opinions may be more related to the way massage is practiced, following the “best to get a massage once a week” process.
• Manipulation of the fascia also affects the endocannabinoid system, which supports the premise of reduction of pain and inflammation.
• Connective tissue may be more lax or stiffer, which is determined by sex hormone levels.
Fluid Movement—blood and Lymph
The adult human body is approximately 70% water. This water, or fluid, is usually named for the tubes or compartments that contain it (e.g., lymph for lymph vessels). Fluids include blood in the vessels and heart, lymph in the lymph vessels, synovial fluid in the joint capsules and bursal sacs, cerebrospinal fluid in the nervous system, and interstitial fluid that surrounds all soft tissue cells. Water is found inside all cells (intracellular fluid) and is bound with glycoproteins in connective tissue ground substance. The ratio of water in connective tissue helps to determine its consistency. Just as elsewhere, water in the body moves in waves through the action of pumps, which include the heart, the respiratory diaphragm, the smooth muscle of the vascular and lymph systems, and the rhythmic movement of muscles and fascia. Water moves along paths of least resistance from high pressure to low pressure and flows downhill with gravity. Water moves at differing speeds according to other variables present, and its properties must be considered when massage methods are applied.
Circulation
Circulation may be affected by massage, but the research is sparse. Castro-Sánchez et al. (2009) found that connective tissue massage improves blood circulation in the lower limbs of type 2 diabetic patients at stage I or IIa and may be useful in slowing the progression of peripheral artery disease. A different study led by Castro-Sánchez (2009) indicated that a combined program of exercise and massage improves arterial blood pressure in persons with type 2 diabetes with peripheral arterial disease. Walton (2008) investigated myofascial release techniques in the treatment of primary Raynaud’s phenomenon and found that releasing restricted fascia using myofascial techniques may influence the duration and severity of vasospastic episodes experienced with this condition. Massage appears to cause an increase in peripheral blood flow in treated areas, as well as in adjacent not-massaged areas. Areas massaged and adjacent areas are significantly warmer for over 60 minutes owing to increased peripheral blood flow (Sefton et al., 2010).
Massage may reduce blood flow in tissues as well. It was found that massage (gliding and kneading specifically) may impair tissue recovery following strenuous exercise by mechanically blocking blood flow (Wiltshire et al., 2010).
Exercise and Lactic Acid
Another area of research involves exercise and lactic acid. Lactic acid does not actually exist as an acid in the body; it exists in another form called lactate. It is a myth that lactic acid is the cause of stiffness felt after a sporting event, such as a marathon, and that massage can flush it out. Another misconception is that lactate is responsible for acidifying the blood, thereby causing fatigue and that burning sensation during prolonged exercise. The truth is that lactate is actually an important fuel that is used by muscles during prolonged exercise (Messonnier et al., 2006). Lactate released from the muscle is converted in the liver to glucose, which then is used as an energy source. So rather than cause fatigue, it actually helps to delay possible lowering of blood glucose concentration—a condition called hypoglycemia.
Delayed-Onset Muscle Soreness
Postexercise stiffness, called delayed-onset muscle soreness (DOMS), is due most often to damage to the muscle and does not result from an accumulation of lactic acid or lactic acid crystals in the muscle. After unaccustomed exercise that results in DOMS, levels of an enzyme called creatine kinase increase, indicating that muscle damage has occurred. This type of tissue damage occurs in the form of tiny microscopic tears in the muscle. Hydroxyproline, an amino acid produced during the breakdown of collagen, is also present, indicating that connective tissue in and around muscle structures is also disrupted. This information shows that stiffness results from muscle damage and breakdown of connective tissue.
Inflammation occurs as part of the normal healing process. Signs of inflammation include heat, redness, swelling, and pain. One theory is that inflamed and swollen muscle fibers press on pain receptors (think “overfilled water balloon”) and alert the brain to register pain. Another theory suggests that cells called phagocytes that come to clean up the damaged tissue further damage the tissue, which leads to pain. Still another theory is based on the premise that free radicals (molecules that are highly reactive and harmful in the body) produced by inflammatory cells aggravate already existing damage, causing pain. Most likely, a combination of all of these factors contributes to the pain of DOMS. Use of massage applications to target lymphatic drainage may reduce the increase in fluid pressure in the tissue caused by the swelling aspect of the inflammatory response. If this does actually occur, a decrease in pain and stiffness should follow, but this hypothesis remains unproved.
Bakowski et al. (2008) and Zainuddin et al. (2005) indicate that massage was effective in alleviating DOMS by approximately 30% by reducing swelling. They found that massage treatment had significant effects on plasma creatine kinase activity, with a significantly lower peak value at 4 days post exercise. However, despite these changes, massage application had no effects on muscle function. In a different study, Bakowski et al. (2008) found that massage administered 30 minutes after exercise could have a beneficial influence on DOMS by reducing soreness but without influence on muscle swelling and range of motion. Massage applied too aggressively can actually interfere with the recovery process because of the potential for even more tissue damage, which then triggers the inflammatory response and more swelling.
Lymphatic Movement
It is even more difficult to justify massage for lymphatic movement. In lymphedema caused by damage or removal of collecting trunks, lymph is present only in the subepidermal (just under the skin) lymphatics, whereas the bulk of stagnant tissue fluid accumulates in the subcutaneous tissue and above and beneath muscular fascia. These findings should be useful for designing pneumatic rhythmic pumping devices that wrap around the edematous limb, leading to rational manual lymphatic drainage in terms of sites of massage and level of applied external pressures. Manual lymph drainage after treadmill exercise was associated with a faster decrease in serum levels of muscle enzymes. This may indicate improved regenerative processes related to structural damage of muscle cell integrity (Schillinger et al., 2006). Lacomba et al. (2010) reported that physiotherapy (exercise and manual lymph drain) could be an effective intervention in the prevention of secondary lymphedema for at least 1 year after surgery for breast cancer involving dissection of axillary lymph nodes.
Authors of the study titled “Systematic Review of Efficacy for Manual Lymphatic Drainage Techniques in Sports Medicine and Rehabilitation: An Evidence-Based Practice Approach” sum up the evidence for massage effects on lymph movement by commenting that manual lymphatic drainage techniques remain a clinical art founded upon hypotheses, theory, and preliminary evidence (Giampietro et al., 2009). Lymphatics supplying skeletal muscle are rhythmically compressed during movement and cardiac and respiratory functions. It is interesting to note that active muscle contraction is required to effect lymphatic movement. Passive tissue displacement does not support efficient lymphatic drainage; investigators have reported that respiratory activity promotes lymph formation, but mechanical ventilation does not (Negrini & Moriondo, 2011). These findings question whether manual forms of lymphatic drainage used when the client is passive are effective. Current research (Bongi et al., 2011; Castro-Sánchez et al., 2010; Lacomba et al., 2010; Duman et al., 2009) does support the effectiveness of manual movement of lymph. Kinesio taping (described in greater detail later in the chapter) shows promise for improving lymphatic movement (Białoszewski et al., 2009; Tsai et al., 2009).
Key Points
• Based on current research, it is difficult to confidently state that massage influences the movement of body fluids, even though research seems to support that massage affects the water content of fascia.
• The main component of body fluid is water. It seems reasonable to expect that mechanical forces applied during massage will at the very least affect the fluid in a particular area during the time the tissue is being massaged.
• Squeezing and compressing fluid in tissue (massage) should help the body move and process various body fluids, but more research is needed before we can confidently claim a specific massage effect on blood and lymphatic movement.
• Although it is appropriate to use methods that are thought to influence blood and lymph movement, as massage professionals, we need to disclose that the methods appear to be clinically effective, but that research remains unable to prove the outcomes.
Research Related to Massage, Tissue Healing, and Musculoskeletal Pain
Research provides varying levels of evidence for the benefits of massage therapy in different chronic pain conditions (Tsao, 2007). Existing research provides good support for the analgesic (reduced pain sensations) effects of massage for nonspecific low back pain, but only moderate support for such effects on shoulder pain and headache pain. Only modest, preliminary support has been found for use of massage in the treatment of mixed chronic pain conditions, neck pain, and carpal tunnel syndrome.
Studies suggest that cyclic stretching of fibroblasts contributes to antifibrotic processes of wound healing by reducing connective tissue growth factor (CTGF) production (Kanazawa et al., 2009). This finding may support the use of massage to manage scar tissue formation and promote pliability in scar tissue.
Ho et al. (2009) studied massage therapy (MT) for adhesive capsulitis (AC), shoulder impingement syndrome (SIS), and nonspecific shoulder pain/dysfunction. For SIS, no clear evidence suggests additional benefits of MT over other interventions. MT was not shown to be more effective than other conservative interventions for AC; however, massage and mobilization-with-movement methods may be useful in comparison with no treatment for short-term outcomes for shoulder dysfunction. In another study, it was determined that massage is safe and may provide clinical benefits for treating chronic neck pain, at least in the short term (Sherman et al., 2009).
Application of a single session of manual therapy (massage is a type of manual therapy) program produces a decrease in tension, anger status, and perceived pain and pressure pain thresholds in patients with chronic tension-type headache. In addition, an immediate increase in heart rate variability has been reported. Heart rate variability (HRV) is a physiologic phenomenon whereby the time interval between heartbeats varies. When people have greater heart rate variability, it is because a better balance between ongoing sympathetic and parasympathetic influences on the heart has been attained. Generally, people have greater heart rate variability when they are relaxed and when they are breathing in a regular or slow pattern (Toro-Velasco et al., 2009).
Arroyo-Morales et al. (2008) used electromyography (EMG) to evaluate and record electrical activity produced by skeletal muscles. They found that massage is beneficial when applied as a passive recovery technique after a high-intensity exercise protocol. This means that the muscles relax and a psychological state of relaxation occurs. However, this same response may cause short-term loss of muscle strength or a change in the muscle fiber tension-length relationship, leading to altered muscle function.
Vigorous exercise causes tiny tears in muscle fibers, resulting in an immune reaction that may lead to inflammation to repair injured cells. A small study performed by Justin D. Crane and associates (2012) found that massage applied to skeletal muscle that has been acutely damaged through exercise appears to be clinically beneficial in reducing inflammation and promoting mitochondrial biogenesis; mitochondria increase their ability to make adenosine triphosphate through this process. Researchers have screened tissues from massaged and unmassaged legs after exercise to compare their repair processes. Based on this study, it is known that massage affects the production of compounds called cytokines, which have a role in the inflammatory process. Massage also stimulates mitochondria inside cells that convert glucose into the energy essential for cell function and repair. According to research conducted by scientists from the Buck Institute for Research on Aging and from McMaster University in Hamilton, Ontario, massage dampened the expression of inflammatory cytokines within muscle cells, and the pain reduction associated with massage may involve the same mechanism as those targeted by conventional antiinflammatory drugs. This study also found that massage had no effect on muscle metabolites (glycogen, lactate), further dispelling the myth that massage removes lactic acid from muscle tissue.
Krzysztof Kassolik and associates (2009) conducted research to determine whether massage in one part of the body influences other parts of the body. They identified an electrical as well as a mechanical response of muscles connected indirectly by structural elements within the muscle being massaged. This finding affirms the results of studies discussed earlier regarding tensegrity.
Overall, it appears that a general, full-body massage can directly or indirectly influence many structures and functions to help the individual, including the athlete, in coping and restoring function. We may not be able to identify the results of individual specific applications because massage contains many different elements. Benefits can be derived from the quiet nurturing presence of the massage therapist, as well as from how long the massage lasts, the massage environment, unlimited variations in methods, pressure, and speed, and so forth. The well-performed, full-body massage is more like a tasty and nutritious cookie—ingredients all mixed together in the right proportions, baked at the correct temperature for the right amount of time, and served in a relaxing environment with time to enjoy the experience. It is important to remember that athletes need this approach as much as and maybe even more than others. Outcomes resulting from a massage application of this type serve as the foundation for recovery post physical (and mental) exertion.
Key Points
Research supports massage to manage anxiety related to pain and to mood alteration, as well as pain thresholds and perception of pain. These benefits are important for athletes and for all of us. This statement allows us to circle back to the initial topic in this section—“General Massage Benefits and Safety”—and to key points for that section. We can expand what we now know about massage somewhat. Massage
• Improves perception of quality of life.
• Changes the shape of fascia.
• May influence the entire body even if only one area is massaged.
• May help move fluids around.
• May affect cellular functions involved in inflammation and cell repair.
• Is safe when provided in a conservative and general manner with sufficient nonpainful pressure.
Sport-Specific Research
So far we have described the research that supports massage in providing health benefits for all individuals. As previously stated, these benefits serve as the foundation for massage for those involved in specific sport and fitness activity. In addition, questions specific to massage and athletes need to be addressed, such as these: When is massage best performed for the athlete? Are there any methods that should be avoided, and if so, when? What is the evidence for stretching in general and specifically as a massage therapy intervention? What evidence is available for adjunct methods that the massage therapist may use in conjunction with massage?
When Is Massage Best Given for Optimal Performance?
The research does not consistently support pre-event massage or massage before a physical exertion activity. Pre-event massage or massage applied within a few hours of physical activity appears to negatively affect muscle performance. Possible reasons include the following:
• Increased parasympathetic nervous system activity and a psychological state of relaxation
• Decreased afferent input with resultant decreased motor unit activation, resulting in transient loss of muscle strength or a change in the muscle fiber tension-length relationship (Arroyo-Morales et al., 2008; Arroyo-Morales et al., 2009; Arroyo-Morales et al., 2001).
Massage as a pre-performance preparation strategy seems to impair performance when compared with a traditional warm-up, although its combination with a normal active warm-up seems to have no greater benefit than active warm-up alone. Therefore, massage use before competition is questionable because it appears to play no effective role in improving performance or preventing injury. Massage appears to achieve the greatest benefit when used post activity after the cool-down (Fletcher, 2010; Goodwin et al., 2007; Weerapong et al., 2005). Massage appears to achieve the greatest benefit when used post activity (Goodwin et al., 2007; Weerapong et al., 2005).
Flexibility
Flexibility training, commonly referred to as stretching, has been thought to prevent injury and enhance sports performance. Research results on the effectiveness of stretching in preventing injury and promoting performance are mixed. A variety of researchers have found no benefit for pre-competition stretching (Molacek et al., 2010; Goldman & Jones, 2011; Kay & Blazevich, 2009; O’Sullivan et al., 2009; Franco et al., 2008; Witvrouw et al., 2004; Yeung & Yeung, 2001), and that it actually decreases the amount of force a muscle can produce (Behm et al., 2001; Cramer et al., 2004; Siatras et al., 2008). Winchester et al. (2009) reported that a single 30-second static stretch when held at the limit of toleration caused an inhibition in muscle strength, and that additional stretching reduced strength even further (McHugh & Cosgrave, 2010; McHugh & Nesse, 2008; Siatras et al., 2008). McHugh and Cosgrave reported that the general consensus is that stretching in addition to warm-up does not affect the incidence of overuse injuries (2010). Whether stretching is beneficial or detrimental may depend on the performance requirements. Athletes who require increased flexibility such as gymnasts or ballet dancers appear to benefit from pre-exercise stretching. However, for sports in which exaggerated range of motion is not required for performance such as cycling, running, tennis, and many others, no scientific data show a positive effect of stretching (Gremion, 2005). Muscle endurance may be diminished or may not be helped by stretching (Gomes et al., 2010; Winchester et al., 2009; Franco et al., 2008). Resistance-trained athletes do not appear to be influenced negatively and performance is not enhanced if static or proprioceptive neuromuscular facilitation (PNF) stretching is used when adequate rest is allowed before performance (Molacek et al., 2010).
The recommendation based on the research is that massage with or without stretching should be used after competition and during the recovery period.
When an increase in range of motion is beneficial, PNF stretching programs have been shown to be the most effective stretching technique for increasing range of motion (ROM); this can be explained by an increase in stretch tolerance (Mahieu et al., 2009; Sharman et al., 2009). The PNF method does show decreased muscle endurance. Strength and conditioning professionals may want to consider avoiding PNF stretching before activities requiring local muscular endurance performance (Gomes et al., 2010; Simão et al., 2010).
Trigger point therapies and a self-stretching protocol resulted in superior short-term outcomes as compared with a self-stretching program alone in the treatment of patients with plantar heel pain (Renan-Ordine et al., 2011). Other studies have not reported an advantage of one type of stretching method over another (Decoster et al., 2010).
Based on the research and on clinical experience, the following recommendations have been put forth for the various forms of stretching (specifically those described in Chapter 12). Avoid stretching combined with massage before competition. The athlete alone or with the help of an athletic trainer can use pre-competition stretching of muscle groups that are vulnerable to injury based on the history of the individual athlete and the demands of the sport (e.g., adductor strains for a hockey player with a history of groin and adductor muscle group shortening). When stretching is incorporated into postcompetition massage, recovery massage, and generalized care of the athlete, each jointed area should be assessed during the massage for available range of motion. Only areas that are hypomobile should be stretched, and the stretch should target restoration of normal joint function while not seeking to increase joint range beyond normal parameters. Stretching should not be used on joints that are hypermobile or that move beyond the normal physiologic range. If an athlete participates in a sport that mandates increased joint movement beyond normal parameters, stretching methods as presented in Chapter 12 should be used to support performance demands in a targeted application-based performance. For example, a baseball pitcher may require increased shoulder motion in the pitching arm.
Kinesio Taping
Kinesio taping is the use of a specially designed elastic tape that moves and recoils. This tape is applied using various patterns. Kinesio taping is theorized to be a sensory method that supports joint function by affecting muscle function, lymphatic flow and local circulation, and pain perception.
A variety of studies involving the effects of Kinesio taping have reported no benefit related to injury prevention (Briem et al., 2011) or to strength and function (Chang et al., 2010; Firth et al., 2010; Fu et al., 2008; Słupik et al., 2007). Some benefit may be derived from the use of Kinesio taping for shoulder impingement syndrome (Kaya et al., 2011; Hsu et al., 2009) and for whiplash (González-Iglesias et al., 2009). A few studies have found that the bioelectrical activity of muscle was increased for up to 48 hours, but that if the tape was then left in place, muscle tone decreased to previous levels, indicating no long-term benefit (Słupik et al., 2007). Range of motion may be increased for truck flexion (Yoshida & Kahanov, 2007), and some evidence suggests that Kinesio taping is supportive of lymphatic movement; however (Białoszewski et al., 2009; Tsai et al., 2009). Specific training in taping methods is recommended.
Magnetic Therapy
Use of magnets as an adjunct to other methods has little scientific support. However, magnetic healing has been part of healing traditions for eons. Currently, low-frequency pulsed electromagnetic fields have been shown to alleviate pain in arthritis by protecting and stimulating cartilage formation, supporting antiinflammatory actions of the body, and stimulating bone remodeling. This form of magnetic therapy could be developed as a viable alternative to arthritis therapy (Ganesan et al., 2009; Shupak et al., 2006). Evidence indicates that electromagnetic fields alleviate pain and accelerate recovery from soft tissue injury and can accelerate healing after bone fracture (Grote et al., 2007). Data suggest that low-frequency pulsed electromagnetic fields stimulate mood improvement in subjects with bipolar disorder and depression treatments (Robertson et al., 2004). Michael Rohan and colleagues (2004) ask, “But does this translate to the effects of using a magnet on an area for pain control?” Maybe.
Hyperbaric Oxygen Therapy
Athletes are using hyperbaric chambers to shorten healing time of injuries and to support recovery. Hyperbaric oxygen therapy (HBOT) is the therapeutic administration of 100% oxygen at environmental pressures greater than one atmosphere. A Cochrane systematic review (Bennett et al., 2005) did not find enough evidence from comparisons tested within randomized controlled trials to establish the effects of HBOT on ankle sprain or acute knee ligament injury, and on experimentally induced DOMS. Some evidence suggests that HBOT may increase interim pain in DOMS.
Key Points
• Research does not support massage immediately before competition for other than anxiety reduction.
• Research results on the effectiveness of stretching to prevent injury and to promote performance are mixed, and appear to lean toward little or no benefit, especially before competition.
• When an increase in range of motion is beneficial, proprioceptive neuromuscular facilitation (PNF) stretching programs have been shown to be the most effective stretching technique to increase range of motion (ROM); this can be explained by an increase in stretch tolerance.
• Only areas that are hypomobile should be stretched; the stretch should target restoration of normal joint function and should not seek to increase joint range beyond normal parameters.
• Stretching should not be used on joints that are hypermobile or that move beyond the normal physiologic range.
• Kinesio taping is the use of a specially designed elastic tape that moves and recoils and is theorized to be a sensory method that supports joint function by affecting muscle function, lymphatic flow, and local circulation, as well as pain perception.
• Evidence indicates that Kinesio taping is supportive of lymphatic movement.
• Low-frequency pulsed electromagnetic fields may alleviate pain, stimulating cartilage formation, supporting antiinflammatory action of the body, and stimulating bone remodeling.
• Hyperbaric oxygen therapy (HBOT) is the therapeutic administration of 100% oxygen at environmental pressures greater than one atmosphere. Benefits are mixed with small support for shortening of healing time.
Summary
It is necessary to work with the athletic population based on an evidence-informed platform. Increased valid research helps the massage therapist better understand what massage can do to support a variety of therapeutic outcomes for the sport and fitness population. Being aware of the research findings supports an ongoing multidisciplinary process with other health professionals involved in the performance and rehabilitation post-injury care of athletes. There remain many mysteries about the therapeutic interaction between massage therapist and client. Research is continuing to open avenues for understanding. Professionalism demands that the massage therapist remain current with the trends and validity of massage application and other adjunct methods such as magnets and Kinesio taping that affect this group of individuals. We also need to be prepared to accept the information provided by high-quality research even when findings conflict with prior learning and beliefs, and we must be sufficiently research literate to make decisions about the validity of the research that may influence our professional practice.
References
Arroyo-Morales, M, Fernández-Lao, C, Ariza-García, A, et al. Psychophysiological effects of preperformance massage before isokinetic exercise. J Strength Cond Res. 2001;25:481.
Arroyo-Morales, M, Olea, N, Martínez, MM, et al. Psychophysiological effects of massage-myofascial release after exercise: a randomized sham-control study. J Altern Complement Med. 2008;14:1223.
Arroyo-Morales, M, Olea, N, Ruíz, C, et al. Massage after exercise—responses of immunologic and endocrine markers: a randomized single-blind placebo-controlled study. J Strength Cond Res. 2009;23:638.
Bab, I, Zimmer, A, Melamed, E. Cannabinoids and the skeleton: from marijuana to reversal of bone loss (Bone Laboratory, the Hebrew University of Jerusalem, Jerusalem, Israel babi@cc.huji.ac.il). Ann Med. 2009;41:560.
Bai, Y, Wang, J, Wu, JP, et al. Review of evidence suggesting that the fascia network could be the anatomical basis for acupoints and meridians in the human body. Evid Based Complement Alternat Med. 2011 Apr 26. [Epub].
Bakermans-Kranenburg, MJ, van Ijzendoorn, MH. Oxytocin receptor (OXTR) and serotonin transporter (5-HTT) genes associated with observed parenting. Am Pain Soc. 2008;9:714.
Bakowski, P, Musielak, B, Sip, P, et al. Effects of massage on delayed-onset muscle soreness. Chir Narzadow Ruchu Ortop Pol. 2008;73:261.
Behm, DG, Button, DC, Butt, JC. Factors affecting force loss with prolonged stretching. Can J Appl Physiol. 2001;26:261.
Bello, D, White-Traut, R, Schwertz, D, et al. An exploratory study of neurohormonal responses of healthy men to massage. J Altern Complement Med. 2008;14:387.
Bennett, M, Best, TM, Babul, S, et al. Hyperbaric oxygen therapy for delayed onset muscle soreness and closed soft tissue injury. Cochrane Database Syst Rev. 2005;19:CD004713.
Bialosky, JE, Bishop, MD, Price, DD, et al. The mechanics of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14:531.
Białoszewski, D, Woźniak, W, Zarek, S. Clinical efficacy of kinesiology taping in reducing edema of the lower limbs in patients treated with the ilizarov method—preliminary report. Ortop Traumatol Rehabil. 2009;11:46.
Billhult, A, Lindholm, C, Gunnarsson, R, et al. The effect of massage on immune function and stress in women with breast cancer—a randomized controlled trial. Auton Neurosci. 2009;150:111.
Bongi, SM, Del Rosso, A, Passalacqua, M, et al. Manual lymph drainage improves upper limb oedema and hand function in patients with systemic sclerosis (SSC) in oedematous phase. Arthritis Care Res (Hoboken). 2011;63:1134.
Briem, K, Eythörsdöttir, H, Magnúsdóttir, RG, et al. Effects of Kinesio tape compared with non-elastic sports tape and the untaped ankle during a sudden inversion perturbation in male athletes. J Orthop Sports Phys Ther. 2011;41:328.
Cambron, JA, Dexheimer, J, Coe, P, et al. Side-effects of massage therapy: a cross-sectional study of 100 clients. J Altern Complement Med. 2007;13:793.
Castro-Sánchez, AM, Mataran-Penarrocha, GA, Aguilera-Manrique, G, et al. Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med. 2010 Dec 28. [Epub].
Castro-Sánchez, AM, Moreno-Lorenzo, C, Matarán-Peñarrocha, GA, et al. Connective tissue reflex massage for type 2 diabetic patients with peripheral arterial disease: randomized controlled trial. Evid Based Complement Alternat Med. 2009 Nov 23. [Epub].
Chaitow, L, DeLany, JW. Clinical applications of neuromuscular techniques, vol 2, The lower body. Edinburgh: Churchill Livingstone; 2002.
Chang, HY, Chou, KY, Lin, JJ, et al. Immediate effect of forearm Kinesio taping on maximal grip strength and force sense in healthy collegiate athletes. Phys Ther Sport. 2010;11:122.
Cramer, JT, Housk, TJ, Johnson, GO, et al. Acute effects of static stretching on peak torque in women. J Strength Cond Res. 2004;18:236.
Crane, JD, Ogborn, DI, Cupido, C, et al. Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage. Sci Transl Med. 2012;4:119.
Day, JA, Stecco, C, Stecco, A. Application of fascial manipulation technique in chronic shoulder pain—anatomical basis and clinical implications. J Bodyw Mov Ther. 2009;13:128.
Decoster, LC, Cleland, J, Altieri, C, et al. The effects of hamstring stretching on range of motion: a systematic literature review. J Orthop Sports Phys Ther. 2010;35:377.
Diego, MA, Field, T. Moderate pressure massage elicits a parasympathetic nervous system response. Int J Neurosci. 2009;119:630.
Diego, MA, Field, T, Sanders, C, et al. Massage therapy of moderate and light pressure and vibrator effects on EEG and heart rate. Int J Neurosci. 2004;114:31.
Duman, I, Ozdemir, A, Tan, AK, et al. The efficacy of manual lymphatic drainage therapy in the management of limb edema secondary to reflex sympathetic dystrophy. Rheumatol Int. 2009;29:759.
Ernst, E, Pittler, M, Wider, B. The desktop guide to complementary and alternative medicine: an evidence-based approach, ed 2. St Louis: Mosby; 2006.
Field, T, Diego, M, Hernandez-Reif, M. Preterm infant massage therapy research: a review. Infant Behav Dev. 2010;33:115.
Field, T, Hernandez-Reif, M, Diego, M, et al. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int J Neurosci. 2005;115:1397.
Firth, BL, Dingley, P, Davies, ER, et al. The effect of kinesiotape on function, pain, and motoneuronal excitability in healthy people and people with Achilles tendinopathy. Clin J Sport Med. 2010;20:416.
Fischer, MJ, Riedlinger, K, Gutenbrunner, C, et al. Influence of the temporomandibular joint on range of motion of the hip joint in patients with complex regional pain syndrome. J Manipulative Physiol Ther. 2009;32:364.
Fletcher, IM. The effects of precompetition massage on the kinematic parameters of 20-m sprint performance. J Strength Cond Res. 2010;24:1179.
Franco, BL, Signorelli, GR, Trajano, GS, et al. Acute effects of different stretching exercises on muscular endurance Program in Physical Therapy and Rehabilitation Science, The University of Iowa, Iowa City, Iowa. J Strength Cond Res. 2008;22:1832.
Frey Law, LA, Evans, S, Knudtson, J, et al. Massage reduces pain perception and hyperalgesia in experimental muscle pain: a randomized, controlled trial. J Pain. 2008;9:714.
Fu, TC, Wong, AM, Pei, YC, et al. Effect of Kinesio taping on muscle strength in athletes—a pilot study. J Sci Med Sport. 2008;11:198.
Ganesan, K, Gengadharan, AC, Balachandran, C, et al. Low frequency pulsed electromagnetic field—a viable alternative therapy for arthritis. Indian J Exp Biol. 2009;47:939.
Garner, B, Phillips, LJ, Schmidt, HM, et al. Pilot study evaluating the effect of massage therapy on stress, anxiety and aggression in a young adult psychiatric inpatient unit. Aust N Z J Psychiatry. 2008;42:414.
Ge, HY, Zhang, Y, Boudreau, S, et al. Induction of muscle cramps by nociceptive stimulation of latent myofascial trigger points. Exp Brain Res. 2008;187:623.
Giampietro, LV, Sayers, JM, McBrier, NM, et al. Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: an evidence-based practice approach. J Man Manipulative Ther. 2009;17(3):e80–e89.
Goldman, EF, Jones, DE. Interventions for preventing hamstring injuries: a systematic review. Physiotherapy. 2011;97:91.
Gomes, TM, Simão, R, Marques, MC, et al. Acute effects of two different stretching methods on local muscular endurance performance. J Strength Cond Res. 2010;25:745.
González-Iglesias, J, Fernández-de-Las-Peñas, C, Cleland, JA, et al. Short-term effects of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: a randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:515.
Goodwin, JE, Glaister, M, Howatson, G, et al. Effect of pre-performance lower-limb massage on thirty-meter sprint running. J Strength Cond Res. 2007;21:1028.
Gremion, G. Is stretching for sports performance still useful? A review of the literature. Rev Med Suisse. 2005;1:1830.
Grote, V, Lackner, H, Kelz, C, et al. Short-term effects of pulsed electromagnetic fields after physical exercise are dependent on autonomic tone before exposure. Eur J Appl Physiol. 2007;101:495.
Guindon, J, Hohmann, AG. Cannabinoid CB 2 receptors: a therapeutic target for the treatment of inflammatory and neuropathic pain. Br J Pharmacol. 2008;153:319.
Hanley, J, Stirling, P, Brown, C. Randomised controlled trial of therapeutic massage in the management of stress. Br J Gen Pract. 2003;53:20.
Haskal, ZJ. Massage-induced delayed venous stent migration. Vasc Interv Radiol. 2008;19:945.
Hillier, SL, Luw, Q, Morris, L, et al. Massage therapy for people with HIV/AIDS. Cochrane Database Syst Rev. 2010;20:CD007502.
Ho, CY, Sole, G, Munn, J. The effectiveness of manual therapy in the management of musculoskeletal disorders of the shoulder: a systematic review. Man Ther. 2009;14:463.
Holt-Lunstad, J, Birmingham, WA, Light, KC. Influence of a “warm touch” support enhancement intervention among married couples on ambulatory blood pressure, oxytocin, alpha amylase, and cortisol. Psychosom Med. 2008;70:976.
Hsu, YH, Chen, WY, Lin, HC, et al. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. J Electromyogr Kinesiol. 2009;19:1092.
Jhaveri, MD, Richardson, D, Chapman, V. Endocannabinoid metabolism and uptake: novel targets for neuropathic and inflammatory pain. Br J Pharmacol. 2007;152:624.
Kanazawa, Y, Nomura, J, Yoshimoto, S, et al. Cyclical cell stretching of skin-derived fibroblasts downregulates connective tissue growth factor (CTGF). Connect Tissue Res. 2009;50:323.
Kashanian, M, Shahali, S. Effects of acupressure at the Sanyinjiao point (SP6) on the process of active phase of labor in nulliparous women. J Matern Fetal Neonatal Med. 2009;15:1.
Kassolik, K, Jaskólska, A, Kisiel-Sajewicz, K, et al. Tensegrity principle in massage demonstrated by electro- and mechanomyography. J Bodyw Mov Ther. 2009;13:164.
Kawakita, K, Itoh, K, Okada, K. The polymodal receptor hypothesis of acupuncture and moxibustion, and its rational explanation of acupuncture points. International Congress Series: Acupuncture—is there a physiological basis?. 2002;1238:63.
Kay, AD, Blazevich, AJ. Moderate-duration static stretch reduces active and passive plantar flexor moment but not Achilles tendon stiffness or active muscle length. J Appl Physiol. 2009;106:1249.
Kaya, E, Zinnuroglu, M, Tugcu, I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clin Rheumatol. 2011;30:201.
Kjær, M, Hanse, M. The mystery of female connective tissue. J Appl Physiol. 2008;105:1026.
Klinger W, Schleip R, Zorn A: European Fascia Research Project Report, 5th World Congress Low Back and Pelvic Pain, November 2004, Melbourne, Australia.
Kuan, TS. Current studies on myofascial pain syndrome. Curr Pain Headache Rep. 2009;13:365.
Lacomba, MT, Yuste Sánchez, MJ, Zapico Goñi, A, et al. Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: randomised, single blinded, clinical trial. BMJ. 2010;340:5396.
Langevin, H, Churchill, D, Cipolla, M. Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. FASEB J. 2001;15:2275.
Langevin, HM, Bouffard, N, Churchill, D, et al. Dynamic fibroblast cytoskeletal response to subcutaneous tissue stretch ex vivo and in vivo. Am J Physiol Cell Physiol. 2005;288:C747.
Langevin, HM, Cornbrooks, CJ, Taatjes, DJ. Fibroblasts form a body-wide cellular network. Histochem Cell Biol. 2004;122:7.
Langevin, HM, Sherman, KJ. Pathophysiological model for chronic low back pain integrating connective tissue and nervous system mechanisms. Med Hypotheses. 2007;68:74.
Langevin, HM, Yandow, JA. Relationship of acupuncture points and meridians to connective tissue planes. Anat Rec. 2002;269:257.
Lindgren, L, Rundgren, S, Winsö, O, et al. Physiological responses to touch massage in healthy volunteers. Auton Neurosci. 2010;158:105.
Lund, I, Ge, Y, Yu, LC, et al. Repeated massage-like stimulation induces long-term effects on nociception: contribution of oxytocinergic mechanisms. Eur J Neurosci. 2002;16:330.
Mackereth, PA, Booth, K, Hillier, VF, et al. Reflexology and progressive muscle relaxation training for people with multiple sclerosis: a crossover trial. Complement Ther Clin Pract. 2009;15:14.
Mahieu, NN, Cools, A, De Wilde, B, et al. Effect of proprioceptive neuromuscular facilitation stretching on the plantar flexor muscle-tendon tissue properties. Scand J Med Sci Sports. 2009;19:553.
McHugh, M, Nesse, M. Effects of stretch on strength loss and pain after eccentric exercise. Med Sci Sports Exerc. 2008;40:566.
McHugh, MP, Cosgrave, CH. To stretch or not to stretch: the role of stretching in injury prevention and performance. Scand J Med Sci Sports. 2010;20:169.
McPartland, JM. The endocannabinoid system: an osteopathic perspective. J Am Osteopath Assoc. 2008;108:586.
Messonnier, L, Denis, C, Feasson, L, et al. An elevated sarcolemmal lactate (and proton) transport capacity is an advantage during muscle activity in healthy humans. Appl Physiol. 2006 Jul 27. [[Epub ahead of print]].
Molacek, ZD, Conley, DS, Evetovich, TK, et al. Effects of low- and high-volume stretching on bench press performance in collegiate football players. J Strength Cond Res. 2010;24:711.
Moraska, A, Pollini, RA, Boulanger, K, et al. Physiological adjustments to stress measures following massage therapy: a review of the literature. Evid Based Complement Alternat Med. 2010;7:409.
Moreno-Lorenzo, C, Matarán-Peñarrocha, GA, Aguilar-Ferrándiz, ME, et al. Effects of myofascial release techniques on pain, physical function, and postural stability in patients with fibromyalgia: a randomized controlled trial. Clin Rehabil. 2011;25:800.
Moyer, CA, Rounds, J, Hannum, JW. A meta-analysis of massage therapy research. Psychol Bull. 2004;130:3.
Moyer, CA, Seefeldt, L, Mann, ES, et al. Does massage therapy reduce cortisol? A comprehensive quantitative review. J Bodyw Mov Ther. 2011;15:3.
Muller-Oerlinghausen, B, Berg, C, Scherer, P, et al. Effects of slow-stroke massage as complementary treatment of depressed hospitalized patients. Dtsch Med Wochenschr. 2004;129:1363.
Negrini, D, Moriondo, A. Lymphatic anatomy and biomechanics. J Physiol. 2011;589(Pt 12):2927.
Niddam, DM, Chan, RC, Lee, SH, et al. Central modulation of pain evoked from myofascial trigger point. Clin J Pain. 2007;23:440.
Norrbrink, C, Lundeberg, T. Acupuncture and massage therapy for neuropathic pain following spinal cord injury: an exploratory study. Acupunct Med. 2011;29:108.
Noto, Y, Kudo, M, Hirota, K. Back massage therapy promotes psychological relaxation and an increase in salivary chromogranin A release. J Anesth. 2010;24:955.
O’Sullivan, K, Murray, E, Sainsbury, D. The effect of warm-up, static stretching and dynamic stretching on hamstring flexibility in previously injured subjects. BMC Musculoskelet Disord. 2009;10:37.
Paoletti, S. Les fascias: rôle des tissus dans la mécanique humaine. Vannes, France: Sully; 2002.
Park, SK, Stefanyshyn, DJ, Ramage, B, et al. Changing hormone levels during the menstrual cycle affect knee laxity and stiffness in healthy female subjects. Am J Sports Med. 2009;37:588.
Pollack, GH, Cameron, IL, Wheatley, DN. Water and the cell. New York: Springer; 2010. [p 65].
Purslow, PP. Muscle fascia and force transmission. J Bodywork Mov Ther. 2010;14:411.
Rapaport, MH, Schettler, P, Bresee, C. A preliminary study of the effects of a single session of Swedish massage on hypothalamic-pituitary-adrenal and immune function in normal individuals. J Altern Complement Med. 2010 Sep 1. [[Epub ahead of print]].
Renan-Ordine, R, Alburquerque-Sendín, F, de Souza, DP, et al. Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2011;41:43.
Roberts, L. Effects of patterns of pressure application on resting electromyography during massage. Intern J Ther Mass Bodyw. 2011;4:4.
Robertson, JA, Theberge, J, Weller, J, et al. Low-frequency pulsed electromagnetic field exposure can alter neuroprocessing in humans. Am J Psychiatry. 2004;161:93.
Rohan, M, Parow, A, Stoll, AL, et al. Low-field magnetic stimulation in bipolar depression using an MRI-based stimulator. Am J Psychiatry. 2004;161:93.
Rossi, F, Siniscalco, D, Luongo, L, et al. The endovanilloid/endocannabinoid system in human osteoclasts: possible involvement in bone formation and resorption (Department of Pediatrics, Second University of Naples, Naples, Italy). Bone. 2009;44:476.
Schillinger, A, Koenig, D, Haefele, C, et al. Effect of manual lymph drainage on the course of serum levels of muscle enzymes after treadmill exercise. Am J Phys Med Rehabil. 2006;85:516.
Schleip, R, Zorn, A, Else, MJ, et al. The European Fascia Research Project Report. http://www.somatics.de/FasciaResearch/ReportIASIyearbook06.htm, 2006.
Schleip, R. Fascial plasticity—a new neurobiological explanation. J Bodyw Mov Ther. 2003;7:104.
Sefton, JM, Yarar, C, Berry, JW, et al. Therapeutic massage of the neck and shoulders produces changes in peripheral blood flow when assessed with dynamic infrared thermography. J Altern Complement Med. 2010;16:723.
Sefton, JM, Yarar, C, Carpenter, DM, et al. Physiological and clinical changes after therapeutic massage of the neck and shoulders. Man Ther. 2011;16:487.
Shah, JP, Danoff, JV, Desai, MJ, et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008;89:16.
Shah, JP, Gilliams, EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. 2008;12:371.
Sharman, MJ, Cresswell, AG, Riek, S. Proprioceptive neuromuscular facilitation stretching: mechanisms and clinical implications. Scand J Med Sci Sports. 2009;19:553.
Sherman, KJ, Cherkin, DC, Hawkes, RJ, et al. Randomized trial of therapeutic massage for chronic neck pain. Clin J Pain. 2009;25:233.
Sherman, KJ, Ludman, EJ, Cook, AJ, et al. Effectiveness of therapeutic massage for generalized anxiety disorder: a randomized controlled trial. Depress Anxiety. 2010;27:441.
Shupak, NM, McKay, JC, Nielson, WR, et al. Exposure to a specific pulsed low-frequency magnetic field: a double-blind placebo-controlled study of effects on pain ratings in rheumatoid arthritis and fibromyalgia patients. Pain Res Manag. 2006;11:85.
Siatras, TA, Mittas, VP, Mameletzi, DN, et al. The duration of the inhibitory effects with static stretching on quadriceps peak torque production. J Strength Cond Res. 2008;22:40.
Sikdar, S, Shah, JP, Gebreab, T, et al. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Arch Phys Med Rehabil. 2009;90:1829.
Simons, DG. New views of myofascial trigger points: etiology and diagnosis. Arch Phys Med Rehabil. 2008;89:157.
Słupik, A, Dwornik, M, Białoszewski, D, et al. Effect of Kinesio taping on bioelectrical activity of vastus medialis muscle: preliminary report. Ortop Traumatol Rehabil. 2007;9:644.
Sommer, AP, Zhu, D. From microtornadoes to facial rejuvenation: implication of interfacial water layers. Cryst Growth Des. 2008;8:3889.
Sparling, PB, Giuffrida, A, Piomelli, D, et al. Exercise activates the endocannabinoid system. Neuroreport. 2003;14:2209.
Stecco, C, Gagey, O, Belloni, A, et al. Anatomy of the deep fascia of the upper limb. Second part: study of innervations. Morphologie. 2007;91:38.
Stecco, C, Porzionato, A, Macchi, V, et al. Histological characteristics of the deep fascia of the upper limb. Ital J Anat Embryol. 2006;111:105.
Stecco, L. Fascial manipulation for musculoskeletal pain. Padova, Italy: Piccin; 2004.
Stringer, J, Swindell, R, Dennis, M. Massage in patients undergoing intensive chemotherapy reduces serum cortisol and prolactin. Psychooncology. 2008;17:1024.
Toro-Velasco, C, Arroyo-Morales, M, Fernández-de-Las-Peñas, C, et al. Short-term effects of manual therapy on heart rate variability, mood state, and pressure pain sensitivity in patients with chronic tension-type headache: a pilot study. J Manipulative Physiol Ther. 2009;32:527.
Tsai, HJ, Hung, HC, Yang, JL, et al. Could Kinesio tape replace the bandage in decongestive lymphatic therapy for breast-cancer-related lymphedema? A pilot study. Support Care Cancer. 2009;17:1353.
Tsao, JCI. Effectiveness of massage therapy for chronic, non-malignant pain: a review. Evid Based Complement Alternat Med. 2007;4:165.
U.S. Preventive Services Task Force Ratings. Grade definitions: guide to clinical preventive services, ed 3. Periodic updates, Rockville, Md: Agency for Healthcare Research and Quality; 2000. [2003].
Wall, P, Melzack, R. Textbook of pain, ed 2. Edinburgh: Churchill Livingstone; 1990.
Walton, A. Efficacy of myofascial release techniques in the treatment of primary Raynaud’s phenomenon. J Bodyw Mov Ther. 2008;12:274.
Weerapong, P, Hume, PA, Kolt, GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35:235.
Winchester, J, Nelson, A, Kokkem, J. A single 30-s stretch is sufficient to inhibit maximal voluntary strength. Res Q Exerc Sport. 2009;80:257. [[serial online]].
Wiltshire, EV, Poitras, V, Pak, M, et al. Massage impairs postexercise muscle blood flow and “lactic acid” removal. Med Sci Sport Exerc. 2010;42:1062.
Witvrouw, E, Mahieu, N, Danneels, L, et al. Stretching and injury prevention: an obscure relationship. Sports Med. 2004;34:443.
Yeung, EW, Yeung, SS. Interventions for preventing lower limb soft-tissue injuries in runners. Cochrane Database Syst Rev. 3, 2001. [CD001256].
Yoshida, A, Kahanov, L. The effect of Kinesio taping on lower trunk range of motions. Res Sports Med. 2007;15:103.
Yucesoy, CA. Epimuscular myofascial force transmission implies novel principles for muscular mechanics. Exerc Sport Sci Rev. 2010;38:128.
Zainuddin, Z, Newton, M, Sacco, P, et al. Effects of massage on delayed-onset muscle soreness, swelling, and recovery of muscle function. J Athl Train. 2005;40:174.
Visit the Evolve website to download and complete the following exercises.
1. List some research findings that support massage for relaxation. Example: Massage application is slow.
2. List some current commonly accepted effects of massage. Example: neural stimulation.
3. Name specific conditions in which massage has been found beneficial. Example: delayed onset of muscle soreness.
4. Describe the interaction of relaxation, improved breathing, and cardiorespiratory and vascular function, as well as changes in connective tissue pliability. Example: Massage produces feelings of well-being that reduce physical awareness.
5. Explain how massage can prevent injury. Example: increases tissue pliability.
6. List the four general outcomes discussed in this chapter and provide a case example of each. Example: Performance/recovery—Athlete is a 22-year-old female collegiate volleyball player. The team is poised to win the championship in its division. The coach has indicated that everyone has to “step up” performance and wants to see everyone’s personal performance plan.
7. Using each of your four case studies, identify the list of physiology mechanisms best targeted to achieve the client’s outcomes. Example: To support performance and recovery, the following would be targeted: Increase ground substance pliability and fluid movement using compression, torsion, and tension force application; reduce sympathetic dominance and support parasympathetic dominance through entrainment using rhythmic, rocking, and deep compression.