CHAPTER 4 Uterine activity evaluation and management
Accurate assessment and management of uterine activity (UA) is crucial to maintain normal fetal oxygenation and acid-base status. Excessive uterine activity can result in an interruption of fetal oxygenation and has been linked to an increased incidence of fetal acidemia of all types.8,10,28,41,43 This chapter will focus on the evaluation of uterine activity in labor, including defining clinical parameters for both normal and excessive uterine activity. Additionally, the diagnosis and management of abnormal labor patterns will be reviewed, including specific issues regarding the use of oxytocin.
Assessment methods: palpation and electronic monitoring
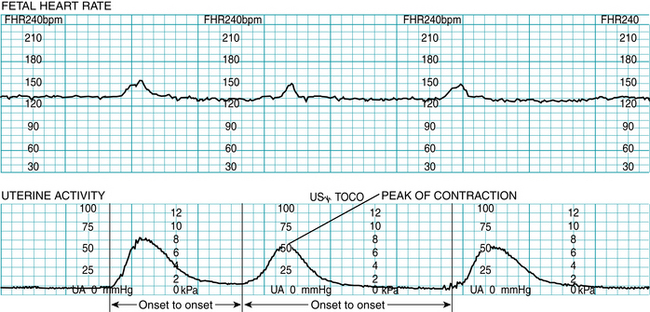
Uterine activity may be assessed by manual palpation or by electronic monitoring with either an external tocotransducer or an internal intrauterine pressure catheter (IUPC). A complete assessment of uterine activity includes the identification of contraction frequency, duration, strength or intensity, and resting tone. Differences in the accuracy of uterine activity evaluation are illustrated in Figure 4-1.
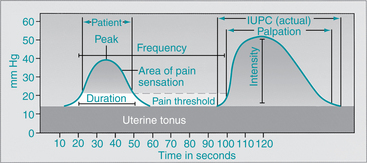
FIGURE 4-1 Comparison of relative sensitivities of assessing uterine contractions by internal monitoring (IUPC), manual palpation, and patient perception. Note that the woman does not usually perceive the contraction until the uterine pressure increases above the baseline uterine tonus. External monitor is variable.
(Modified from Dickason EJ, Silverman BL, Kaplan JA: Maternal-infant nursing care, ed 3, St. Louis, 1998, Mosby.)
Manual palpation
Manual palpation is the traditional method of monitoring contractions. This method can measure contraction frequency, duration, and relative strength. Palpation is a learned skill that is best performed with the fingertips to feel the uterus rise upward as the contraction develops. Mild, moderate, and strong are the terms used to describe the strength of uterine contractions as determined by the examiner’s hands during palpation and based on the degree of indentation of the abdomen.6,23 For learning and for the purpose of comparison, the degree of indentation corresponds to the palpation sensation when feeling the parts of the adult face, as described in the following chart:
| Contraction Strength | Palpation Sensation |
| Mild | Tense fundus but easy to indent (feels like touching finger to tip of nose) |
| Moderate | Firm fundus, difficult to indent with fingertips (feels like touching finger to chin) |
| Strong | Rigid, board-like fundus, almost impossible to indent (feels like touching finger to forehead) |
Palpation as the sole method of monitoring uterine activity is uncommon in the United States, where the majority of labors are monitored electronically. Palpation nevertheless remains an important clinical skill because it is used concomitantly with external electronic monitoring and may be used as an adjunct for confirmation of uterine activity during internal electronic monitoring.
Electronic monitoring of uterine activity
External uterine activity monitoring is achieved using a tocotransducer (to provide information about uterine contraction frequency and duration) combined with manual palpation (to evaluate relative strength). Electronic monitoring provides continuous data and a permanent record of uterine activity. The electronic display of a contraction depends on the depression of a pressure-sensing device placed on the maternal abdomen. Factors such as placement of the transducer, belt tightness, and maternal adipose tissue result in variations of depression and will affect the graphic representation on the fetal heart rate tracing (Figure 4-2). Thus the contractions may appear stronger (or less strong) than they truly are, making it imperative to assess strength of the uterine contraction by manual palpation when uterine activity is externally monitored.
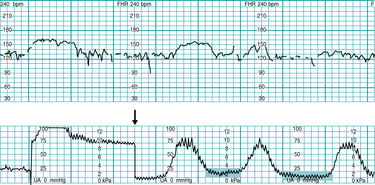
FIGURE 4-2 Adjustment of tocotransducer (arrow) to correct displacement following maternal position change. Note the tocotransducer picking up maternal breathing movements on the lower uterine activity panel as evidenced by jagged lines (highlighted).
(Courtesy Lisa A. Miller, CNM, JD.)
Internal uterine activity monitoring uses an intrauterine pressure catheter (IUPC) that measures actual intrauterine pressure in millimeters of mercury (mm Hg) during both contractile and acontractile (resting) periods. As demonstrated in Figure 4-1, the intrauterine pressure catheter allows clinicians to evaluate the frequency, duration, and strength of contractions in mm Hg with improved accuracy. The following chart contrasts the data obtained with these two modes of monitoring:
| External Mode - Tocotransducer | Internal Mode - Intrauterine Pressure Catheter |
| Frequency of Contractions | |
| Measured from the onset of one contraction to the onset of the next contraction | Measured from the onset of one contraction to the onset of the next contraction |
| Duration of Contractions | |
| Measured from contraction onset to offset | Measured from contraction onset to offset |
| Strength/Intensity of Contractions | |
| The abdomen must be palpated to assess the strength of the contraction based on the degree of indentation of the fundus. The more difficult it is to indent the fundus during palpation, the stronger the contraction. Strength of contractions using a toco is usually documented as mild, moderate, or strong to palpation. The tracing produced using a tocotransducer will reflect contraction strength relative to other contractions, i.e., stronger contractions will generally produce higher waveforms. | Intrauterine pressure is measured directly and recorded on the tracing in mmHg. Strength is usually documented as the numerical value at the peak of the contraction, e.g., 50 mm Hg, 70 mm Hg, etc. Intensity of contractions is technically a term used to identify the peak of the contraction less the resting tone, expressed in mm Hg. In clinical practice, the terms strength and intensity are often used interchangeably. |
| Resting Tone | |
| The abdomen must be palpated to assess resting tone based on whether the fundus palpates as soft or firm (rigid). During periods of palpated resting tone the external monitor is generally set/reset to a level of 10 on the uterine activity portion of the fetal monitoring tracing. | Resting tone is measured directly and reflected on the tracing based on the intrauterine pressure in mm Hg. Resting tone is recorded as the numerical value when the uterus is completely relaxed (acontractile), e.g., 10 mm Hg, 15 mm Hg, etc. |
Electronic display of uterine activity
Uterine activity is monitored and recorded on the lower section of the monitor strip (Figure 4-3). The range of the scale is from 0 to 100 mm Hg. There are five major vertical divisions of 20 mm Hg each, divided again into minor vertical representations of 10 mm Hg each. Some tracing paper manufactured in North America has four major vertical sections of 25 mm Hg each, with the smaller divisions representing 5 mm Hg pressure in the uterine activity section. For further information on instrumentation, please refer to Chapter 3.
Stages of normal labor
The first stage of labor begins with the onset of contractions and ends with complete dilation of the cervix. It is divided into two phases: latent and active. During the latent phase, irregular and infrequent uterine contractions are associated with gradual cervical softening, dilation, and effacement (thinning). During the active phase of labor, the rate of cervical dilation increases and the fetal presenting part descends. The progress of labor can be plotted on a partogram or cervicograph, providing a visual record of cervical dilation and descent of the presenting part over time (Figure 4-4). As the fetal presenting part descends and cervical dilation increases, the lines cross each other in an x pattern.
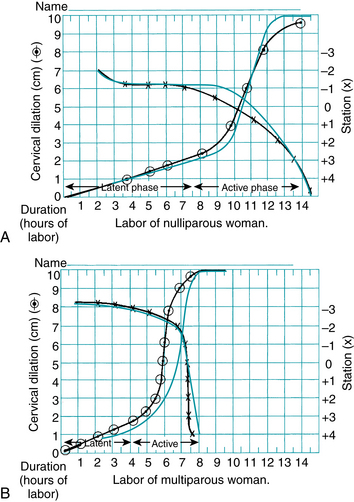
FIGURE 4-4 Partogram for assessment of patterns of cervical dilation and descent. Individual woman’s labor patterns (black) superimposed on preprinted labor graph for comparison. A. Labor of a nulliparous woman. B. Labor of a multiparous woman. The rate of cervical dilation is plotted with the circled plot points. A line drawn through these symbols depicts the slope of the curve. Station is plotted with Xs. A line drawn through the Xs reveals the pattern of descent.
(Modified from Lowdermilk DL, Perry SE, Cashion K, et al: Maternity & women’s health care, ed 10, St Louis, 2012, Mosby.)
Defining adequate uterine activity
Uterine activity in normal labor generally causes the progressive dilation and effacement of the cervix and descent of the fetal presenting part, resulting in spontaneous vaginal delivery. Much of the data defining the “normal” range of uterine activity was derived from the research of Caldeyro-Barcia and colleagues11-15 in the late 1950s and the 1960s. Using intra-amniotic pressure catheters, Caldeyro-Barcia and Poseiro12 evaluated uterine activity and coined the term Montevideo units (MVUs) as a method of measuring uterine activity. The original formula was calculated by multiplying the average intensity in mm Hg (peak of contraction less resting tone) times the frequency of uterine contractions in a 10-minute period. Thus, if there are 4 contractions in 10 minutes with an average intensity of 40 mm Hg, the Montevideo units for that period would be 4 × 40, or 160 Montevideo units. Over time, it became obvious that simple addition of the individual contraction intensities over 10 minutes resulted in essentially similar numbers to the multiplication method and since then the addition method has become common practice.6
Labor was found to begin clinically when Montevideo units rose to between 80 and 120, with contraction strength needing to reach at least 40 mm Hg.12,13 This would equate to two to three contractions with intensities of 40 mm Hg or more every 10 minutes for the initiation of labor. In normal labor, contractions increase in intensity and frequency as labor progresses through the first stage and into the second stage. Caldeyro-Barcia and colleagues12-14 found that uterine activity in the first stage of normal labors generally ranged between 100 and 250 Montevideo units, with contractions increasing in intensity from 25 to 50 mm Hg and in frequency from three to five over 10 minutes. In the second stage, Montevideo units can rise to 300 to 400,8,11-15 as contraction intensities may increase to 80 mm Hg or more and five or six contractions may be seen every 10 minutes.
Baseline uterine tone, also known as resting tone, averages 10 mm Hg during labor, rising from 8 to 12 mm Hg from the beginning of the first stage to the onset of the second stage. Resting tone is assessed during the time between contractions, known as relaxation time. Relaxation times are generally longer (60 seconds or more) in first stage labor and tend to shorten (45-60 seconds) during second stage. Contraction duration of 60 to 80 seconds remains relatively stable from active phase labor through the second stage.29 These findings provide a basis for logical definitions of “adequate” uterine activity when using internal pressure catheters for assessment of uterine contractions.
Caldeyro-Barcia and Poseiro also provided crucial information related to contraction assessment when using palpation, or palpation and a tocotransducer. They found that until the intensity (peak less baseline tonus) reaches 40 mm Hg, the wall of the uterus is easily indented by palpation.13 This correlates well with the premise that uterine contractions that palpate as moderate or stronger are likely to have peaks of 50 mm Hg or greater if they are measured by internal means, whereas palpated contractions identified as mild are likely to have peaks of less than 50 mm Hg if measured internally. These findings offer guidance for clinicians in identifying reasonable definitions of “adequate” uterine activity when using palpation (with or without a tocotransducer) for assessment of uterine contractions. Box 4-1 provides a summary of normal parameters of uterine activity in labor, while Figure 4-5 illustrates a variety of common uterine contraction patterns in normal labor.
BOX 4-1 Components of Uterine Activity During Labor
| Frequency | Contraction frequency overall generally ranges from 2 to 5 per 10 minutes during labor, with lower frequencies seen in the first stage of labor and higher frequencies seen during the second stage of labor. |
| Duration | Contraction duration remains fairly stable throughout first and second stages, ranging from 45-80 seconds, not generally exceeding 90 seconds. |
| Strength | Uterine contractions generally range from peaking at 40-70 mm Hg in first stage of labor and may rise to over 80 mm Hg in second stage. Contractions palpated as “mild” would likely peak at less than 50 mm Hg if measured internally, contractions palpated as “moderate” or greater would likely peak at 50 mm Hg or greater if measured internally. |
| Resting tone | Average resting tone during labor is 10 mm Hg; if using palpation, should palpate as “soft,” i.e., easily indented, no palpable resistance. |
| Relaxation time | Relaxation time is commonly 60 seconds or more in first stage, and 45 seconds or more in second stage. |
| Montevideo Units (MVUs) | Usually range from 100-250 MVUs in first stage, may rise to 300-400 in second stage. Contraction intensities of 40 mm Hg or more and MVUs of 80-120 are generally sufficient to initiate spontaneous labor. |
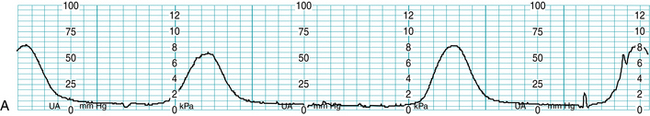
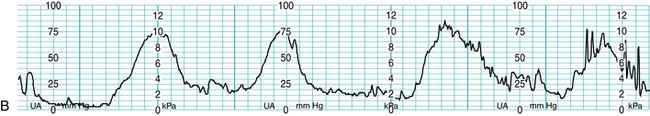
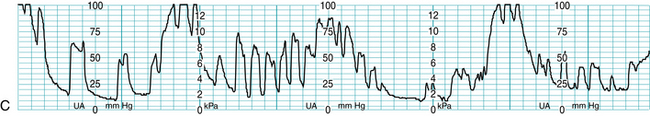
FIGURE 4-5 Examples of normal uterine activity during labor. A. Normal contraction pattern in latent phase labor. B. Normal contraction pattern in active phase labor; note that contractions are more frequent but there is still adequate relaxation time. C. Normal contraction pattern in second stage labor; note maternal pushing efforts.
(Courtesy Lisa A. Miller, CNM, JD.)
In summary, applying what is known about parameters of uterine activity during normal labor:
Defining excessive uterine activity
Historically, the lack of sound, standardized definitions for terminology related to excessive uterine activity has hindered effective communication and the development of consensus-based multidisciplinary guidelines. But recent literature provides an opportunity for clinicians to reach professional consensus. In 2008, the National Institute of Child Health and Human Development (NICHD) issued a workshop report on fetal monitoring that included summary terms for uterine activity.
The summary terms suggested by the NICHD are for the classification of uterine activity utilizing frequency of contractions averaged over a thirty-minute period:4,24
Normal: less than or equal to 5 contractions in 10 minutes
Tachysystole: greater than 5 contractions in 10 minutes
Tachysystole is to be further qualified by the presence or absence of fetal heart rate (FHR) decelerations and applies to spontaneous as well as stimulated labors. The workshop report stresses the importance of other parameters such as duration, intensity, and relaxation time in the evaluation of uterine activity, specifically stating that “frequency alone is a partial assessment of uterine activity.” 24 The report also suggests abandonment of previously used summary terms “hyperstimulation” and “hypercontractility.” While the NICHD workshop report is clearly important progress towards the standardization of terminology, standardized terminology alone does not provide clinicians with sufficient guidance for the safe and effective management of uterine activity in labor. Clinicians must be familiar with the normal physiology of uterine activity (described previously) as well as the relationship between excessive uterine activity and fetal acid-base status.
Excessive uterine activity has long been linked to untoward effects on fetal heart rate tracings.10,39 Peebles28 noted decreased fetal cerebral oxygen saturation with shorter contraction intervals. Bakker and colleagues8 found that fetal acidemia (umbilical artery pH ≤7.11) of all types (respiratory, metabolic, and mixed) was more prevalent in patients with excessive uterine activity during labor, both first and second stage. Specifically, a first stage average MVU value of 261 and relaxation time of 51 seconds was noted in the acidemic group, versus average MVU value of 236 and relaxation time of 63 seconds in the non-acidemic group. In second stage, an average MVU value of 442 and relaxation time of 36 seconds was noted in the acidemic group, versus average MVU value of 402 and relaxation time of 47 seconds in the non-acidemic group.8 Logic would therefore dictate that avoiding Montevideo unit values exceeding the previously discussed norm of 250 in the first stage of labor and 300 to 400 in the second stage could decrease the incidence of significant fetal acidemia at birth. And in cases of external monitoring, or any situation where MVU evaluation is not feasible, ensuring adequate relaxation times of 60 seconds or more in first stage and 45 seconds or more in second stage could also prevent fetal acidemia at birth.
In addition to evaluating frequency, strength, and relaxation time, it is important to understand that for the fetus to be able to maintain oxygenation, resting tone must also be normal. Hypertonus, or elevated resting tone is most commonly defined as uterine resting tone greater than 20-25 mmHg, or a uterus that does not return to soft if using palpation. The information in Box 4-2 can be used by clinicians and multidisciplinary committees to reach consensus on definitions for terms related to uterine activity as well as evidence-based guidelines for management of all types of excessive uterine activity. This information should serve as the starting point for the development of clear, physiologically sound, and clinically useful approaches to excessive uterine activity that include all parameters of uterine activity, versus focusing on frequency (tachysystole) alone.
BOX 4-2 Evaluation of Uterine Activity During Labor
Data from references 2, 3, 6, 8, 10-15, 18, 22, 28, 29, 38, 40, 43
| Preliminary Assumptions |
| Excessive Uterine Activity |
| Tachysystole |
| Hypertonus |
| Inadequate Relaxation Time |
| Excessive Contraction Duration (also Known as Tetanic Contractions or Uterine Tetany) |
Some clinicians contend that the management of excessive uterine activity should be based upon the presence or absence of FHR changes. This approach conflicts with what limited evidence exists regarding uterine activity and fetal oxygenation. Bakker and colleagues8 found no difference in the occurrence of late decelerations between the acidemic and non-acidemic fetuses, suggesting that the key to avoiding acidemia is not dependent upon the appearance of fetal heart rate changes, but rather the presence of excessive uterine activity itself. Simpson & James41 found that in the first stage of labor even 5 uterine contractions in 10 minutes (“normal” uterine activity by definition) over a 30-minute period resulted in a 20% decrease in fetal oxygen saturation as measured by fetal pulse oximetry. Both these studies make it clear that premising the management of uterine activity on frequency alone or basing the management of excessive uterine activity on FHR changes may lead to less than optimal fetal oxygenation and potentially the deterioration of fetal acid-base. Waiting to respond to excessive uterine activity until there are significant changes in fetal heart rate is not appropriate. Rather, to prevent fetal acidemia at birth, clinicians should focus on identifying and promoting normal (adequate) uterine activity and correcting underlying causes of any type of excessive uterine activity (Figure 4-6).
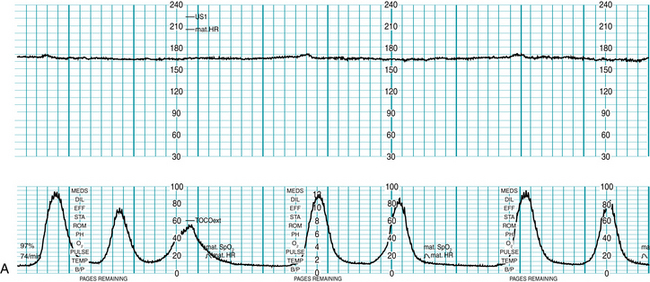
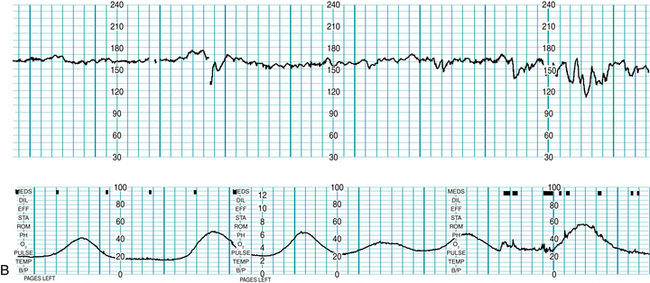
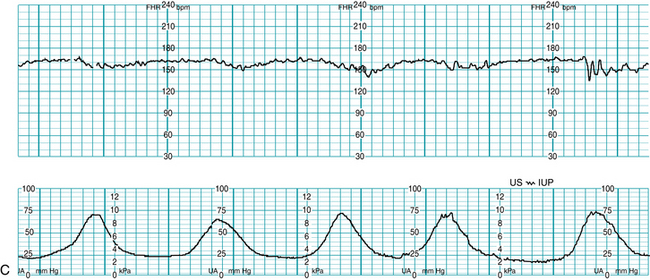
FIGURE 4-6 Examples of excessive uterine activity during labor. A. Tachysystole with coupling and tripling of contractions during oxytocin use. B. Tachysystole occurring spontaneously. C. Normal frequency of uterine contractions, but inadequate relaxation time between contractions for first stage labor; recommended relaxation time in first stage is 60 seconds, note possible FHR decelerations.
Common underlying causes of excessive uterine activity
Interventions to decrease excessive uterine activity
These interventions are specific to excessive uterine activity. Note that the management of fetal heart rate patterns is addressed in detail in Chapter 6. It is imperative that clinicians respond appropriately to fetal heart rate changes regardless of the nature of uterine activity, as uterine activity is only one of several causes of interrupted fetal oxygenation. However, fetal heart rate changes should not be a prerequisite for clinical response to excessive uterine activity. It cannot be overemphasized: excessive uterine activity should trigger clinician response whether or not fetal heart rate changes are observed.
Diagnosis and management of labor abnormalities
Labor abnormalities may be described by clinicians using a variety of expressions, such as “slow progress in labor,” “failure to progress,” “dystocia,” “dysfunctional labor,” or “cephalopelvic disproportion.”27 Up to 68% of unanticipated cesarean deliveries in patients with vertex presentation are reported to be due to dystocia, and given the number of repeat cesarean deliveries that follow a primary cesarean for dystocia, the diagnosis of dystocia may account for as many as 60% of all cesarean births.27
Strategies that have been shown to decrease the risk of dystocia include the following:25,27,36
While a detailed discussion of the diagnosis and management of dystocia is outside the scope of this book, a brief overview is warranted and can be helpful when interdisciplinary discussions arise regarding management of uterine activity, especially discussions regarding the utilization of oxytocin, the most common treatment for dystocia.
Latent phase abnormalities
Labor is defined as “the presence of uterine contractions of sufficient intensity, frequency, and duration to bring about demonstrable effacement and dilation of the cervix.”2 While most clinicians agree that active phase labor begins when cervical dilation reaches 3 to 4 cm, there is little consensus regarding the definition for latent phase labor.2,9,27,36 The most prevalent definition in clinical use is considering latent phase labor to begin with the onset of labor and end at the beginning of the active phase of first stage.27 Latent phase is considered prolonged if it is >20 hours in nulliparous patients and >14 hours in multiparous patients.27 Considerations for the management of prolonged latent phase labor are listed next.
Management strategies for latent phase disorders*
Active phase abnormalities
There are three main categories of active phase labor abnormalities:
ACOG recommends that oxytocin augmentation be considered for these disorders, stating that the goal “is to effect uterine activity sufficient to produce cervical change and fetal descent while avoiding uterine hyperstimulation and fetal compromise.”2 While traditionally the diagnosis of an arrest disorder required 2 hours without cervical change in the presence of a uterine contraction pattern that exceeded 200 Montevideo units,2 studies30,31,36 now suggest that 4 hours of uterine activity exceeding 200 Montevideo units (or 6 hours if the average uterine activity pattern was less than 200 Montevideo units) will result in up to a 92% vaginal delivery rate with no increased risk to the newborn. The suggested management approaches for active phase disorders are listed next.
Management strategies for active phase disorders*
Second stage abnormalities
Arrest of descent, failure of the fetus to rotate and descend, is the labor abnormality associated with the second stage. ACOG3 considers the second stage prolonged in the nullipara if it exceeds 3 hours when regional anesthesia is being utilized, 2 hours if not. In the multipara, a second stage with regional anesthesia that is longer than 2 hours is considered prolonged; in the absence of regional anesthesia, it is 1 hour. Contrary to some clinicians’ practices, these time frames are not mandates for delivery by cesarean section, but rather parameters for guiding assessment and intervention. Prolonged second stage should trigger clinical re-evaluation of the three Ps: powers, passenger, and passage.2 Evaluation of adequacy of uterine contractions, fetal position, and pelvic diameters may provide direction regarding interventions to facilitate rotation and descent.
Uterine activity and oxytocin use
Oxytocin, a frequent treatment choice for labor abnormalities, has been designated a high-alert medication20, and AWHONN has published new staffing recommendations for 1:1 nursing care during intrapartum oxytocin administration.7 Sadly, disagreements related to oxytocin management continue to be a source of conflict between nurses and physicians,42 and allegations related to oxytocin management are common in litigation.21 There are many sound, evidence-based protocols for the administration of oxytocin, ranging from high-dose, high-frequency to low-dose, low-frequency, and hybrids that combine aspects of both regimens. Because oxytocin usage can result in excessive uterine activity it is important to closely and accurately monitor uterine activity when administering oxytocin.
Several studies16,33-35 regarding the pharmacologic characteristics of oxytocin use in relation to dysfunctional labor and dystocia show that 40 minutes are needed to achieve maximum dose level. Reviews by Arias5 and Sanchez Ramos32 regarding oxytocin pharmokinetics conclude that lower doses and less frequent increases of oxytocin are preferable, as they allow time for a more physiologic approach and avoid the risk of tachysystole associated with higher doses and shorter dosing intervals. Simpson and Creehan38,40 suggest starting doses of 0.5 to 2 mU/min with increases every 30 to 60 minutes of 1 to 2 mU/min. This approach is in keeping with one of the primary tenets of pharmacology, which is use the lowest amount of drug needed to achieve the desired effect. However, it should be noted that a recent systematic review of high-dose versus low-dose oxytocin for labor augmentation showed a decrease in cesarean section rate as well as a decrease in labor duration in the high-dose group. The high-dose groups did have greater incidences of tachysystole, but no significant differences in neonatal outcomes. The authors noted some significant limitations of the review, including the fact that many of the reviewed trials were not blinded and decision criteria for cesarean section were not standardized.44 Clinicians should carefully consider all the data, as well as the differences in use of oxytocin for induction versus augmentation, when deciding on oxytocin management schemes. Suggestions for the safe and effective use of oxytocin in labor are summarized in Box 4-3.
BOX 4-3 Suggestions for Safe & Effective Oxytocin Usage
Data from References 2, 3, 21, 25-44.
Oxytocin dosage should be titrated to uterine activity, with a goal of attaining adequate or normal uterine activity. Coupling or tripling of uterine contractions (Figure 4-7) is a phenomenon that may be seen during oxytocin administration. Suggested treatment for this pattern is temporary discontinuation of oxytocin, lateral positioning of the mother, initiation of a fluid bolus, and a restart of oxytocin after 30 minutes or more.40
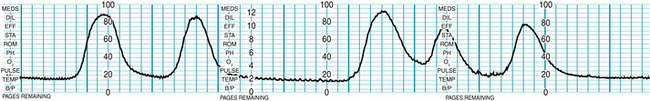
FIGURE 4-7 Oxytocin administration may result in coupling and tripling of uterine contractions. Treatment consists of discontinuation of oxytocin, maternal position change, and intravenous hydration.
(Courtesy Lisa A. Miller, CNM, JD.)
When administering oxytocin and utilizing internal monitoring during labor induction or augmentation, titration of oxytocin to establish uterine activity patterns reaching Montevideo units of 200 to 250 is an appropriate goal. When external monitoring and palpation are being used, palpable contractions of normal duration every 2.5 to 3 minutes should correlate well with adequate Montevideo units (Figure 4-8). If labor progress is not occurring with what appears to be adequate uterine activity to palpation, the proper clinical response is to consider internal monitoring to more accurately assess uterine activity and not to increase the oxytocin.
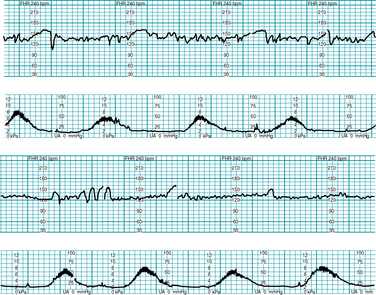
FIGURE 4-8 Example of adequate UA during oxytocin augmentation using external monitoring. Note adequate relaxation time between contractions. According to nursing documentation the contractions palpated were of moderate intensity.
Contraction frequency of less than every 2 minutes during oxytocin administration is a fairly common occurrence, and can lead to tachysystole, even when using low-dose, low-frequency protocols. Management must be based on clinical context and institutional protocol, but should be geared towards returning uterine activity to adequate and appropriate for the stage of labor. In other words, clinicians should not try to achieve second stage labor patterns in the latent or active phase of first stage labor, as this may interfere with fetal gas exchange. Continuous and ongoing evaluation of fetal status using a systematic approach can prevent fetal acidemia, improve outcomes, and also reduce medical-legal risk. Safety related to oxytocin use is achieved by avoidance of the injudicious use of oxytocin, adherence to evidence-based multidisciplinary guidelines regarding oxytocin administration, and appropriate and consistent team management of excessive uterine activity.
Summary
Excessive uterine activity is related to fetal acidemia at birth and should be avoided by careful monitoring and cautious use of labor stimulants when necessary. Parameters for normal, or adequate, uterine activity are easily defined based on the physiology of normal labor. Clinicians must reach consensus on definitions related to excessive uterine activity and recognize that the term tachysystole addresses only one aspect of uterine activity, that of frequency. Recognition of the importance of other parameters of uterine activity, such as strength, duration, resting tone, and relaxation time are equally important components of the evaluation of uterine activity during labor.
Understanding both the normal progress of labor and labor abnormalities is crucial to the promotion of improved outcomes for both mother and fetus. The availability of continuous labor support, patient education regarding appropriate admission criteria, and adequate hydration play key roles in minimizing labor abnormalities. An understanding of the pharmacologic characteristics of oxytocin, combined with a focus on attaining adequate uterine activity, leads to safe and effective use of this common labor medication.
The evaluation of uterine activity and fetal heart rate patterns is inextricably intertwined in the care and support of the laboring mother. Focus on uterine activity assessment and management has been inconsistent in clinical practice. As Bakker8 so aptly states, “contraction monitoring deserves full attention.” It is now clear that proper and careful assessment of uterine activity deserves consideration equal to that given to fetal heart rate pattern assessment.
1. American College of Obstetricians and Gynecologists: Clinical management guidelines for obstetricians-gynecologists: management of intrapartum fetal heart rate tracings. Practice Bulletin no. 116.. Obstet Gynecol. 2010;116:1232-1240
2. American College of Obstetricians and Gynecologists. Dystocia and augmentation of labor. Practice Bulletin no. 49. Washington DC: ACOG; December 2003. (reaffirmed September 2006)
3. American College of Obstetricians and Gynecologists. Induction of labor. Practice Bulletin no. 10. Washington, DC: ACOG; November 1999. (reaffirmed September 2006)
4. American College of Obstetricians and Gynecologists: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Practice Bulletin no. 106. Obstet Gynecol. 2009;114:192-202
5. Arias F. Pharmacology of oxytocin and prostaglandins. Clin Obstet Gynecol. 2000;43(3):455-468.
6. Association of Women’s Health, Obstetric and Neonatal Nurses: Fetal heart monitoring.principles and practices, principles and practices. Dubuque, IA; Kendall Hunt: 2009
7. Association of Women’s Health, Obstetric and Neonatal Nurses. Guidelines for professional registered nurse staffing for perinatal units. Washington, DC: AWHONN; 2010.
8. Bakker PCAM, Kurver PHJ, Kuik DJ, et al. Elevated uterine activity increases the risk of fetal acidosis at birth. Am J Obstet Gynecol. 2007;196(4):313-316.
9. Beckmann M. Predicting a failed induction. Aust N Z J Obstet Gynecol. 2007;47(5):394-398.
10. Caldeyro-Barcia R. Intrauterine fetal reanimation in acute intrapartum fetal distress. Early Hum Dev. 1992;29:27-33.
11. Caldeyro-Barcia R. Oxytocin in pregnancy and labour. Acta Endocrinol Suppl. 1960;34(Suppl 50)41-49. [Copenhagen]
12. Caldeyro-Barcia R, Poseiro JJ. Physiology of uterine contractions. Clin Obstet Gynecol. 1960;3:386-408.
13. Caldeyro-Barcia R, Poseiro JJ. Oxytocin and contractility of the pregnant human uterus. Ann NY Acad Sci. 1959;75:813-830.
14. Caldeyro-Barcia R, Sica-Blanco Y, Poseiro JJ, et al. A quantitative study of the action of synthetic oxytocin on the pregnant human uterus. J Pharmacol Exp Ther. 1957;121(1):18-31.
15. Caldeyro-Barcia R, Theobald G. Sensitivity of the pregnant human myometrium to oxytocin. Am J Obstet Gynecol. 1968;102(8):1181.
16. Crall HD, Mattison DR: Oxytocin pharmacodynamics: effect of long infusions on uterine activity. Gynecol Obstet Invest. 1991;31(1)17-22
17. Dowding DW, Cheyne HL, Hundley V: Complex interventions in midwifery care. reflections on the design and evaluation of an algorithm for the diagnosis of labor. Midwifery: 2010 doi:10.1016/j.midw.2009.11.01
18. Effer SB, Bértola RP, Vrettos A, et al. Quantitative study of the regularity of uterine contractile rhythm in labor. Am J Obstet Gynecol. 1969;105(6):909-915.
19. Hodnett ED, Gates S, Hofmeyr GJ, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev. 3, 2007. CD003766
20. Institute for Safe Medical Practices. High alert medications. Available at www.ismp.org, May 26, 2011. Accessed
21. Jonsson M, Nordén SL, Hanson U. Analysis of malpractice claims with a focus on oxytocin use in labour. Acta Obstet Gynecol Scand. 2007;86(3):315-319.
22. Krapohl AJ, Myers GG, Caldeyro-Barcia R: Uterine contractions in spontaneous labor: a quantitative study. Am J Obstet Gynecol. 1970;106(3)378-387
23. Lowdermilk DL, Perry SE, Cashion K, et al. Maternity & women’s health care, ed 10. St Louis: Mosby; 2012.
24. Macones GA, Hankins GD, Spong CY, et al: The 2008. National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. J Obstet Gynecol Neonatal Nurs. 2008;37:510-515 Obstet Gynecol 112(3):661–666, 2008
25. Mercer BM. Induction of labor in the nulliparous gravida with an unfavorable cervix. Obstet Gynecol. 2005;105(4):688-689.
26. Miller LA: Oxytocin, excessive uterine activity, and patient safety: time for a collaborative approach. J Perinat Neonatal Nurs. 2009;23(1)52-58
27. Ness A, Goldberg J, Berghella V. Abnormalities of the first and second stages of labor. Obstet Gynecol Clin North Am. 2005;32(2):201-220.
28. Peebles D, Spencer J, Edwards A, et al. Relation between frequency of uterine contractions and human fetal cerebral oxygenation saturation studied during labour by near infrared spectroscopy. Br J Obstet Gynaecol. 1994;101(1):44-48.
29. Pontonnier G, Puech F, Grandjean H, et al. Some physical and biochemical parameters during normal labour. Biol Neonate. 1975;26(3-4):159-173.
30. Rouse DJ, Owen J, Hauth JC: Criteria for failed labor induction: prospective evaluation of a standardized protocol. Obstet Gynecol. 2000;96(5 Pt 1)671-677
31. Rouse D, Owen J, Savage K, et al: Active phase labor arrest: revisiting the 2-hour minimum. Obstet Gynecol. 2001;98(4)550-554
32. Sanchez-Ramos L. Induction of labor. Obstet Gynecol Clin North Am. 2005;32(2):181-200.
33. Seitchik J. The management of functional dystocia in the first stage of labor. Clin Obstet Gynecol. 1987;30(1):42-49.
34. Seitchik J, Amico JA, Castillo M. Oxytocin augmentation of dysfunctional labor. V. An alternative oxytocin regimen. Am J Obstet Gynecol. 1985;151(6):757-761.
35. Seitchik J, Amico J, Robinson AG, et al. Oxytocin augmentation of dysfunctional labor. IV. Oxytocin pharmacokinetics. Am J Obstet Gynecol. 1984;150(3):225-228.
36. Shields S, Ratcliffe S, Fontaine P, et al. Dystocia in nulliparous women. Am Fam Physician. 2007;75(11):1671-1678.
37. Simon C, Grobman W. When has an induction failed. Obstet Gynecol. 2005;105(4):705-709.
38. Simpson KR. Cervical ripening and induction and augmentation of labor, ed 3. Washington DC: AWHONN; 2009. updated
39. Simpson KR: Intrauterine resuscitation during labor: review of current methods and supportive evidence. J Midwifery Womens Health. 2007;52(3)229-237
40. Simpson KR, Creehan PA. Perinatal nursing, ed 3. Philadelphia: Lippincott Williams & Wilkins; 2008.
41. Simpson KR, James DC. Effects of oxytocin-induced uterine hyperstimulation on fetal oxygen status and fetal heart rate patterns during labor. Am J Obstet Gynecol. 2008;199:34.e1-34.e5.
42. Simpson KR, James DC, Knox GE: Nurse-physician communication during labor and birth: implications for patient safety. J Obstet Gynecol Neonatal Nurs. 2006;35(4)547-556
43. Simpson KR, Miller LA. Assessment and optimization of uterine activity during labor. Clinical Obstet Gynecol. 2011;54(1):40-49.
44. Wei S, Luo Z, Qi H, et al: High-dose vs. low-dose oxytocin for labor augmentation: a systematic review. Am J Obstet Gynecol. 2010;203(4)296-304