Figure 34-1 Schematic of tendon matrix. HA, hyaluronic acid; HABP, hyaluron binding protein.
SIGNIFICANCE OF TENDON INJURIES
AUGMENTATION OF INTRINSIC TENDON HEALING WITH STEM CELLS
▪ Motion aids healing and reduces adhesions.
▪ There is no evidence that loading, in the absence of motion, is helpful, or that, once the tendon is moving, more loading helps healing.
▪ We do know that loading may lead to failure of the repair.
▪ Enough loading to initiate motion
▪ Not enough to risk the repair
▪ Slow healing: Cell-rich patch between tendon ends, with or without cytokines
Upper extremity injuries are common, representing approximately one third of all traumatic injuries. Tendon injuries are among the most severe upper extremity injuries. The number of tendon injuries is difficult to quantify because epidemiologic studies have not been done, but estimates suggest that roughly 40,000 inpatient tendon repairs are done each year in the United States.1 A much larger number of tendon surgeries are done on an outpatient basis. More importantly, these injuries occur almost exclusively in a young, working-age population and result in considerable disability. The typical tendon injury requires 3 to 4 months of rehabilitation, during which time the affected hand is unavailable for work use. Failure rates or residual impairment remain disturbingly high, in the 20% to 30% range in most series, despite ongoing attention to the problem. From 1976 to 1999, consistently between 7% and 8% of the articles in the Journal of Hand Surgery focused on tendon injuries.2 Despite this evident importance and ongoing interest, translation of research results into meaningful clinical improvements have been limited. By most accounts,3 the most significant improvement in tendon rehabilitation remains the institution of early passive motion therapy by Kleinert in the early 1970s.4 Since then, quality improvements have been incremental. Tendon rupture rates continue to be cited at an incidence of 5% to 10%. These failures require complex secondary tendon reconstruction surgeries.5-8 Better methods for improving intrinsic tendon healing and minimizing tendon adhesions are still needed so we can improve upon clinical outcomes, with the ultimate goal being the production of an adhesion-free tendon repair.
The extracellular matrix (ECM) is the principal component of tendon tissue and is responsible for its material properties.9-11 The major constituents of the ECM are type I collagen; proteoglycans, principally decorin, but also aggrecan in the gliding regions;12-15 fibronectin; and elastin. This matrix is synthesized by tendon cells, or tenocytes (Fig. 34-1). These cells are surrounded by the dense matrix; thus, although they are metabolically active, they do not participate much in the tendon-healing process. Instead, undifferentiated cells in the epitenon do the heavy lifting for tendon healing, and proliferating, migrating into the gap between the tendon ends, and finally uniting the cut tendon ends16,17 (Fig. 34-2). Unfortunately, this process presents a bit of a dilemma; if these same cells migrate away from the tendon, toward the tendon sheath, they form adhesions that restrict tendon motion. Often this is indeed the case, as the relatively ischemic tendon is surrounded by better vascularized tissue, which sends out vascular buds under the stimulation of vascular endothelial growth factor (VEGF).18-21
After tendon injury, the ECM undergoes significant changes due to synthesis of new elements, such as type III collagen, by the tenocytes,22-24 degradation of existing elements by various matrix metalloproteinases (MMP), and remodeling of the resulting combination, under the influence of cytokines such as transforming growth factor beta (TGF-β) as well as mechanical forces. Manipulation of these processes, to augment their action between the tendon ends while reducing them at the tendon’s gliding surface, is the goal of much research, as described later.
Various pharmacologic agents have been used in the past in an attempt to modify adhesion formation. Steroids, antihistamines, and β-aminoproprionitrile have not been shown to decrease scar formation clinically.25,26 Ibuprofen and indomethacin, however, have been found to have a small beneficial effect.27
The ideal pharmacologic agent should have no systemic side effects, should be limited to a single application, and should be directed at growth factor expression and ECM production. Such a drug may be 5-fluorouracil (5-FU), an antimetabolite used not only as a cancer chemotherapeutic agent but also to prevent adhesions in glaucoma filtration surgery. The exposure of a surgical field to 5-FU produces a focal inhibition of scarring. Blumenkranz and colleagues have found that 5-FU inhibits the proliferation of fibroblasts in cell cultures and reduces retinal scarring.28,29 Single exposures to 5-FU, for as short duration as 5 minutes, can have antiproliferative effects on fibroblasts for several days. The suppression of fibroblast proliferation has been observed for up to 36 hours without signs of cell death.30,31 This time frame may be adequate to inhibit tendon adhesions prior to beginning postoperative motion protocols. Reversible prolonged inhibition of fibroblast function is attributed to the drug’s inhibition of DNA and messenger RNA (mRNA) synthesis through thymidylate syntheses. More importantly, these effects appear to be focal to the site of application and titratable in terms of length of action.32-34 A 5-minute exposure to 5-FU has been shown to significantly decrease postoperative flexor tendon adhesions in chicken and rabbit models.35,36 This beneficial effect is felt to be due to the down-regulation of TGF-β and modulation of MMP-2 and MMP-9 production.37,38 The effect on surface lubrication is unknown. No adverse effect was noted on tendon healing in these studies. It is presumed therefore that the topical 5-FU does not penetrate to affect the cells below the tendon surface. Topical 5-FU may well have a role in improving the outcomes in selected cases of tenolysis.
Growth factors are the chemical signals that direct the migration and proliferation of the tendon fibroblast during the healing process. The role of growth factors has been examined extensively in cutaneous wounds and other soft tissue processes, yet we are only beginning to know the specifics involved in flexor tendon healing.11,39 The factors that appear to be involved include TGF-β, platelet-derived growth factor (PDGF), basic fibroblast growth factor (bFGF), insulin-like growth factor (IGF), epidermal growth factor (EGF), and VEGF.21,40,41 These same growth factors have also been shown to optimize tissue-engineered constructs used for tendon repair.21,40-44 Growth differentiation factor-5 (GDF-5), a member of the TGF-β superfamily, has also been shown to accelerate tendon healing in multiple animal models.45-47
TGF-β stimulates the formation of the ECM. It signals fibroblasts to produce collagen and fibronectin, decreases protease production, and increases the formation of integrins, which promote cellular adhesions and matrix assembly. In normal tissue, TGF-β becomes inactivated once wound healing is complete; however, it may remain active in tendon adhesion formation, continuing the cycle of matrix accumulation.48,49 Excessive expression of TGF-β is detrimental to many tissues, resulting in tissue fibrosis in the heart, kidney, and liver.49 Modulation of TGF-β has been reported to reduce the fibrotic process in glomerulonephritis, dermal wounds, and arthritis as well as decreasing peritendinous adhesions in a rabbit tendon model.49-52 TGF-β levels can remain elevated for up to 8 weeks after tendon injury.53,54
Neuropeptides may also play a role in tendon healing.55-58 During the early phases of healing, tendons exhibit nerve fiber ingrowth.55 This nerve ingrowth is associated with the temporal release of substance P (SP). SP promotes tendon regeneration through the stimulation and proliferation of fibroblasts.59-62 Further studies have found that tendon motion helps to modulate the release of SP.56 The injection of SP into the peritendinous region of ruptured rat tendons improves healing and increases tendon strength.63 Similarly, GDF-5 has a potential to stimulate bone marrow-derived stem cell (BMSC) proliferation and regulate BMSC differentiation to tenocytes.64 Recent experiments have shown a beneficial effect of GDF-5 on tendon healing as well.19,46,65
At one time, most flexor tendon injuries were treated with tendon grafts,66,67 but today primary repair is used almost exclusively, with grafts being used primarily to reconstruct otherwise unbridgeable tendon gaps. This is a good thing, since tendons in the hand are intrasynovial and have a specialized gliding surface, whereas most tendon grafts, such as the palmaris or plantaris, are extrasynovial and have no such specialized surface.68,69 The result is much more adhesion formation than would be the case if intrasynovial grafts were available. As noted later, in the future it may be possible to engineer such grafts to reduce friction and improve healing.
Healing of flexor tendons in zone 2 depends on the ability of the injured tendon to recruit fibroblasts and other cellular components to the site of injury.70 Normally these are circulating or locally derived undifferentiated (i.e., stem) cells that are recruited to the injury site by the expression of cytokines in the wound.18,21,71-73 Cytokine stimulation is also important in converting these undifferentiated cells into the tendon phenotype, characterized by the expression of markers such as tenomodulin and scleraxis.74,75 BMSC can also enter and participate in soft tissue healing.76-78 BMSCs delivered on collagen sponges improve healing in animal models of tendon repair,42,79 and stem cells from other origins have been shown to be effective in enhancing repair in several other tendon injury models.80-83 Current research is focused on optimizing the isolation and differentiation of stem cells into the tendon phenotype. In the future, it is likely that cells derived from the patient’s own bone marrow, fat, skin, or muscle will be used to augment tendon repair and to populate engineered tendon graft substitutes (Fig. 34-3). My colleagues and I are pursuing one such option in our laboratory now: a decellularized flexor digitorum profundus tendon allograft, reconstituted with stem cells from the patient’s own tissues and lubricated with an engineered surface containing hyaluronic acid (HA) (Fig. 34-4) and lubricin.84-87 Such a graft could be used to bridge flexor tendon defects and, finally, to replace like with like.
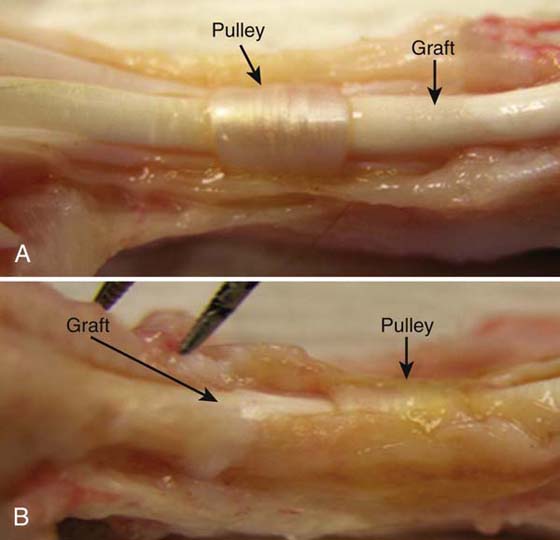
Figure 34-4 A, Graft treated with carbodiimide-derivatized hyaluronic acid at 6 weeks. Note marked reduction in adhesions. B, Tendon graft at 6 weeks. Note extensive adhesions. (Reprinted, with permission, from Zhao C, Sun YL, Amadio PC, et al. Surface treatment of flexor tendon autograft with carbodiimide-derivatized hyaluronic acid. An in vivo canine model. J Bone Joint Surg Am. 2006;88:2187, Fig. 8.)
In addition to collagen and structural proteoglycans, such as decorin, the tendon ECM also contains important lubricants for efficient flexor tendon motion (see Fig. 34-1). The synovial cells of the flexor tendon sheath secrete HA into the ECM, which may serve as a surface lubricant.88 HA, a polysaccharide, is found in all vertebrate tissues and body fluids. Various physiologic functions have been assigned to HA, including lubrication, water homeostasis, filtering effects, and regulation of plasma protein distribution.89 HA is found in increased amounts during the first week after tendon repair.90 After a tendon is treated with a hyaluronidase solution, which destroys HA, the gliding resistance between the tendon and pulley increases significantly.91 This suggests that HA on the surface of the flexor tendons may play a role in the surface lubrication of the tendon–pulley system. In vivo results have demonstrated that HA may inhibit the proliferation of rabbit synovial cells, thus preventing cell adhesion between the sheath and the tendon.92,93
Recent studies indicate that lubricin, a proteoglycan found in the superficial zone of articular cartilage, may play an important role in preventing cellular adhesions in addition to providing the lubrication necessary for normal joint function.94-97 Lubricin was originally isolated from articular cartilage.98 It has since been identified on the surface of tendons97,99-101 and plays an important role in tendon lubrication.85 However, lubricin also inhibits cellular adhesion and so has the undesirable effect of inhibiting tissue repair.102
The expression of lubricin is modulated by interleukin-1 (IL-1), tumor necrosis factor (TNF-α) and TGF-β.97 Little else is known about the expression or regulation of lubricin within digital flexor tendons, but its modulation may have a profound effect on the restoration of the flexor surface and the prevention of adhesions after tendon injury and repair (Fig. 34-5) and perhaps as a coating on a tissue-engineered tendon graft or tendon graft substitute, as discussed later.
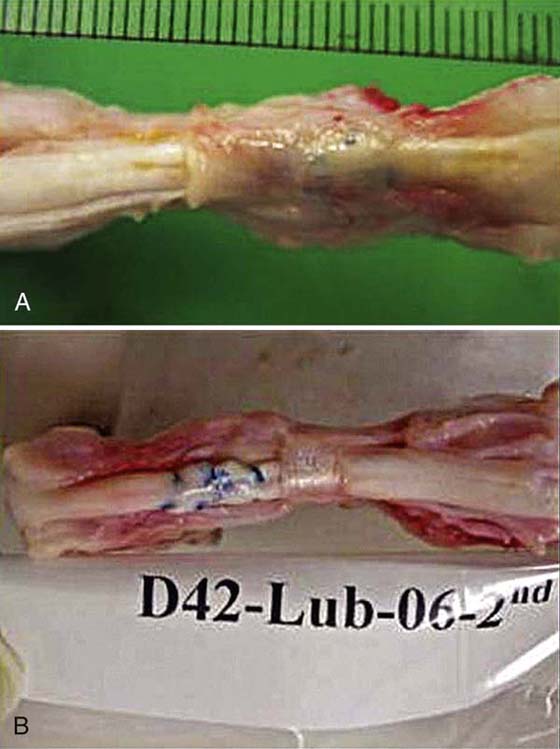
Figure 34-5 A, Tendon repair at 6 weeks. Note adhesions. B, Tendon repair treated with carbodiimide-derivatized lubricin, hyaluronic acid, and gelatin. Note marked reduction in adhesions.
The effect of HA on flexor tendon repair has been investigated in animal and clinical studies.103-107 Exogenously applied HA may prevent adhesion formation between the flexor tendon and surrounding tissue following tendon repair without affecting tendon healing,108-111 although in vivo results have been contradictory.93,106,112 As the half-life of HA in tissue is short, native HA is probably eliminated too rapidly to maintain a long-lasting physical barrier between opposing tissues.113 Moreover, abrasion during tendon gliding constantly threatens to physically remove HA from the tendon surface.114 Therefore, extending HA half-life and strengthening HA binding ability on the tendon surface are important to enhancing the clinical effect of exogenously administered HA.
The carbodiimide derivatization, a chemical modification of HA, has been developed recently for clinical use.115-117 This modification of HA decreases the water solubility of HA, increases its intermolecular binding strength, and therefore increases tissue residence time.118 Clinical studies of a proprietary form of this derivatized HA (Seprafilm or Seprafilm II, Genzyme Corp, Cambridge, MA, or Hyaloglide; ACP gel, Fidia Advanced Biopolymers, Abano Terme, Italy), fabricated as a cross-linked sheet to be inserted as a barrier between opposing surfaces where adhesion is undesirable, have shown that it can reduce postsurgical adhesions in gynecologic and abdominal surgery.118-121 A variation on this theme, by doing the cross-linking reaction in situ to fix the HA directly to the tendon surface, using collagen as an intermediary (carbodiimide derivatized HA, or cd-HA), has had promising preliminary results in animal studies in vitro and in vivo.122 The combination of HA and lubricin appears to have an additive effect.85 Recent work has also shown, though, that although physicochemical and pharmacologic interventions can reduce adhesion formation, in both tendon grafts and tendon repairs,122-124 there is a cost in terms of delayed or impaired tendon healing after tendon repair. Newer investigations are considering how to combine adhesion reduction and improved healing through the use of growth factors and stem cells.
Over the past 50 years, novel repair techniques have resulted in improved clinical outcomes following flexor tendon surgery.125-129 The details of clinical tendon repair are covered in Chapter 35, but this chapter focuses on the effect of repair constructs on tendon healing and tendon kinematics.
Despite these advances in repair technique, adhesions continue to occur, and results can be less than adequate, particularly when the injury occurs in zone 2, the so called no-man’s land, where the tendon resides within a fibro-osseous pulley system. Critical features related to tendon repair include a strong, minimally reactive repair that maintains strong tendon coaptation while permitting tendon gliding.130-134 Two major problems continue to occur within the clinical setting: gapping with rupture at the repair site and adhesion formation within the flexor sheath.70,135-137 Despite attempts at modifying rehabilitation, whether through increased levels of applied load or increased rates, tendon excursion methods have failed to increase early tendon core strength.138-141
The ideal tendon repair is strong, easy to perform, and does not interfere with either tendon healing or tendon gliding. Current methods are moderately strong and able to withstand the normal forces of light motion.142-147 However, some of these constructs, especially those with multiple loops or knots on the anterior tendon surface,133,148,149 also generate high-friction forces with movement and may abrade the pulley surface over time150 (Fig. 34-6). Newer suture designs have incorporated features such as fewer surface loops, loops on the lateral rather than anterior tendon surfaces, and knots inside the repair rather than on the surface; all these features help reduce friction while having little effect on breaking strength.151 Newer suture materials, such as FiberWire, a composite suture consisting of a monofilament polyethylene core surrounded by a braided polyester jacket (Arthrex, Naples FL), combine higher breaking strength, so that a smaller-diameter suture can be used, as well as providing low friction.146,152
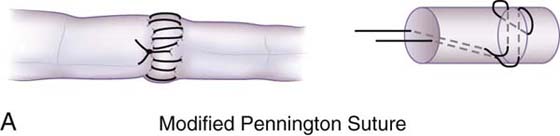
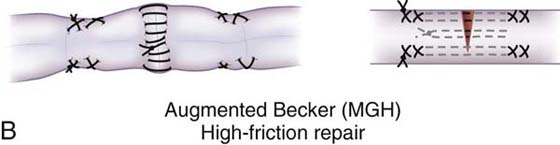
Figure 34-6 A, Modified Pennington suture. Low-friction, high-strength repair. [Modified, with permission, from Pennington DG. The locking loop tendon suture. Plast Reconstr Surg. 1979;63:(5)648-652; and Tanaka T, Amadio PC, Zhao C, et al. Gliding characteristics and gap formation for locking and grasping tendon repairs: A biomechanical study in a human cadaver model. J Hand Surg Am. 2004;29(1):6-14.] B, Augmented Becker Massachusetts General Hospital high-friction, high-strength repair. [Reproduced, with permission, from Amadio PC. Friction of the gliding surface. Implications for tendon surgery and rehabilitation. J Hand Ther. 2005;18(2):115, Figure 4.]
Animal studies over the past decade have shown convincingly that high-friction repairs result in abrasion of the tendon sheath (Fig. 34-7) and adhesion formation, even when factors such as rehabilitation method are optimized.150,153,154 Thus, the goal should be to use a high-strength, low-friction repair construct and a low-friction suture material. Most recently I have been using 3-0 Ethibond and a modified Pennington design, but the recent data noted earlier on FiberWire is certainly intriguing.
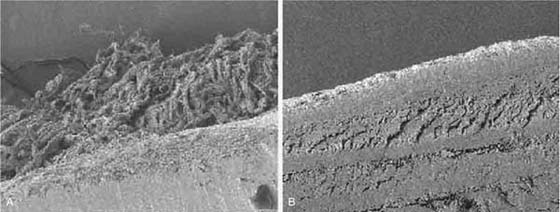
Figure 34-7 Scanning electron micrograph of tendon sheath in contact with A, high-friction Massachusetts General Hospital suture. B, Low-friction suture (modified Kessler technique). [Reproduced, with permission, from Zhao C, Amadio PC, Momose T, et al. Remodeling of the gliding surface after flexor tendon repair in a canine model in vivo. J Orthop Res. 2002;20(4):861, Fig. 6.]
Until the mid-1960s, most flexor tendon repairs were immobilized postoperatively for 3 weeks. This policy was based on the research of Mason and Allen,155 who had shown that canine flexor tendon repairs decreased in tensile strength for 3 weeks postoperatively. Subsequent clinical work by Verdan,156 Kleinert and Verdan,157 and Duran and associates158 showed that human flexor tendon repairs could be safely mobilized with a combination of active extension and passive flexion.
The use of early mobilization after tendon repair has resulted in improved outcomes.4,156,158-161 In animal models,153,162-167 earlier mobilization results in better final tendon gliding and tensile strength. More recently, the fine details of mobilization have been studied, specifically the effect of timing168-170 and the effect of differential motion of the wrist and finger joints on tendon loading and tendon gliding during the healing period.153,171,172 Active motion protocols have also been used, although, interestingly, the clinical results are not reliably better than passive protocols.5,125,173,174 Moreover, the addition of loading to motion in animal models has been shown to have little effect on the final result in terms of strength and motion.166,172,175 Thus, the available evidence suggests that motion, not load, is the critical factor.
Of course, there must be some load on the tendon if it is going to move; at the very least, the load must be sufficient to overcome the forces of friction. It is for this reason that low-friction repairs are important—they minimize the load needed to initiate movement. Friction, though, is not the only concern. The force needed to overcome joint stiffness and to flex traumatized, edematous tissues must also be considered, as well as the weight of the distal digit itself; often these latter forces far outweigh the frictional ones in magnitude, especially in injured digits. So, the minimum force needed to load the tendon is a combination of the frictional force and the force needed to move the joints and soft tissues. This combination is often called the “work of flexion” of the unloaded digit.169,176,177
One might imagine that the maximum load that could be applied is the load that represents the breaking strength of the tendon, but that would be incorrect: long before the tendon breaks, it begins to gap, and gapping also increases friction, setting up a vicious cycle that can lead to later rupture. So, really, the upper bound is not breaking strength but the force needed to create a gap, which is usually much less.161,178-187 The difference between the two forces—the unloaded work of flexion and the gapping force—represents the “safe zone” in which rehabilitation can occur151 (Fig. 34-8). Early on, this safe zone is bounded by strictly mechanical parameters related to the anatomy and biomechanics of the repair. Over time, though, the effects of tendon healing are added in; the general effect is usually to gradually widen the safe zone, enabling the rational use of a graded resistance program as outlined by Groth.188 The details of such programs are reviewed in Chapter 36.
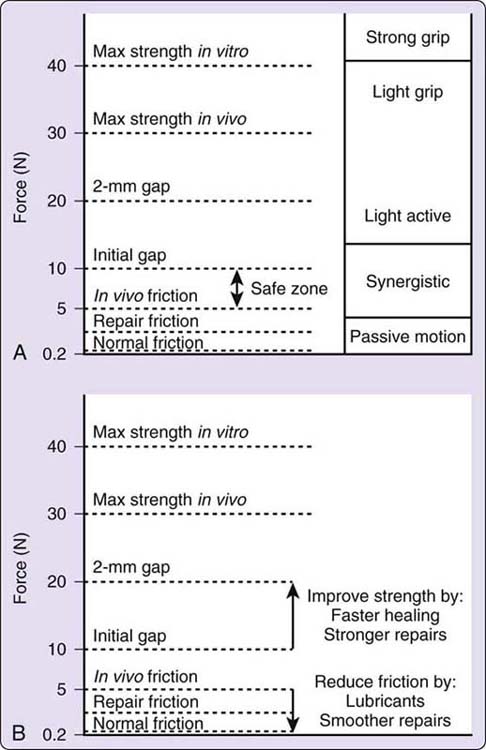
Figure 34-8 A, The “safe zone” concept [Reproduced, with permission, from Amadio PC. Friction of the gliding surface. Implications for tendon surgery and rehabilitation. J Hand Ther. 2005;18(2):115, Fig. 3.] B, Implications of tendon research on the safe zone.
Unfortunately, in some cases, early mobilization after tendon repair is not possible by any method. Common examples include situations with complex hand injury, in which motion might jeopardize bone, skin, nerve, or vascular integrity; patients who are uncooperative due to age or mental status; or situations where the tendon repair is deemed to be too tenuous to tolerate mobilization. In such cases, adhesions have been, up to now, inevitable. It is possible, though, that the application of a tissue-engineered, biocompatible adhesion barrier that is porous to nutrients might allow an immobilized tendon to heal without adhesions. We are currently pursuing research to address this issue, using cd-HA and lubricin, linked to collagen, as the proposed barrier, and hope to have an update in time for the next edition of this book!
In summary, considerable advances have been made in our understanding of tendon healing and both the biology and biomechanics of tendon repair and reconstruction. The “safe zone” concept provides a good framework for thinking about the interaction among friction, repair strength, healing, and loading. Early motion, using the least load possible, is the key to better results, but early motion alone is usually not sufficient to prevent adhesions, without posing an undue risk of repair rupture. Thus, the ideal tendon repair of the future will probably need to include a combination of three features. There will always be a need for better, low-friction repair techniques. Lubricants bound to the tendon surface would further reduce friction, lower the loading requirements, and block adhesions. Cell and cytokine “patches” at the repair site can speed healing and allow a faster widening of the safe zone, which should result in fewer complications. This combination approach would appear to offer the best path toward the ultimate goal of predictable restoration of normal function after tendon injury.
1. Kelsey JL. Upper Extremity Disorders: Frequency, Impact, and Cost. New York: Churchill Livingstone; 1997.
2. Newmeyer W. History of the Journal of Hand Surgery. J Hand Surg. 2000;25A:5–13.
3. Wilgis EF. Classic papers in hand surgery. [comment]. J Hand Surg Am. 2000;25(1):14–18.
4. Kleinert HE, Serafin D, Kutz JE, Atasoy E. Reimplantation of amputated digits and hands. Orthop Clin North Am. 1973;4(4):957–967.
5. Harris SB, Harris D, Foster AJ, Elliot D. The aetiology of acute rupture of flexor tendon repairs in zones 1 and 2 of the fingers during early mobilization. J Hand Surg Br. 1999;24(3):275–280.
6. Kitsis CK, Wade PJ, Krikler SJ, et al. Controlled active motion following primary flexor tendon repair: a prospective study over 9 years. J Hand Surg Br. 1998;23(3):344–349.
7. Elliot D, Moiemen NS, Flemming AF, et al. The rupture rate of acute flexor tendon repairs mobilized by the controlled active motion regimen. J Hand Surg Br. 1994;19(5):607–612.
8. Small JO, Brennen MD, Colville J. Early active mobilisation following flexor tendon repair in zone 2 [see comments]. J Hand Surg Br. 1989;14(4):383–391.
9. Guo Y, Pili R, Passaniti A. Regulation of prostate-specific antigen gene expression in LNCaP human prostatic carcinoma cells by growth, dihydrotestosterone, and extracellular matrix. Prostate. 1994;24(1):1–10.
10. Occleston NL, Daniels JT, Tarnuzzer RW, et al. Single exposures to antiproliferatives: long-term effects on ocular fibroblast wound-healing behavior. Invest Ophthalmol Vis Sci. 1997;38(10):1998–2007.
11. Beredjiklian PK. Biologic aspects of flexor tendon laceration and repair. J Bone Joint Surg Am. 2003;85-A(3):539–550.
12. Vogel KG, Keller EJ, Lenhoff RJ, et al. Proteoglycan synthesis by fibroblast cultures initiated from regions of adult bovine tendon subjected to different mechanical forces. Eur J Cell Biol. 1986;41(1):102–112.
13. Rees SG, Flannery CR, Little CB, et al. Catabolism of aggrecan, decorin and biglycan in tendon. Biochem J. 2000;350(Pt 1):181–188.
14. Caterson EJ, Nesti LJ, Albert T, et al. Application of mesenchymal stem cells in the regeneration of musculoskeletal tissues. Medgenmed Computer File. MedGenMed. 2001.E1.
15. Hae Yoon J, Brooks R, Kwan Kim Y, et al. Proteoglycans in chicken gastrocnemius tendons change with exercise. Arch Biochem Biophys. 2003.(412):279–286.
16. Kryger GS, Chang AK, Costa M, et al. A comparison of tenocytes and mesenchymal stem cells for use in flexor tendon tissue engineering. J Hand Surg Am. 2007;32(5):597–605.
17. Chen MY, Jeng L, Sun YL, et al. Contraction of collagen gels seeded with tendon cells. Biorheology. 2006;43(3-4):337–345.
18. Boyer MI, Watson JT, Lou J, et al. Quantitative variation in vascular endothelial growth factor mRNA expression during early flexor tendon healing: an investigation in a canine model. J Orthop Res. 2001;19(5):869–872.
19. Aspenberg P. Stimulation of tendon repair: mechanical loading, GDFs and platelets. A mini-review. Int Orthop. 2007;31(6):783–789.
20. Salo P, Bray R, Seerattan R, et al. Neuropeptides regulate expression of matrix molecule, growth factor and inflammatory mediator mRNA in explants of normal and healing medial collateral ligament. Regul Pept. 2007;142(1-2):1–6.
21. Tsubone T, Moran SL, Amadio PC, et al. Expression of growth factors in canine flexor tendon after laceration in vivo. Ann Plast Surg. 2004;53(4):393–397.
22. Chan D, Cole WG. Quantitation of type I and III collagens using electrophoresis of alpha chains and cyanogen bromide peptides. Anal Biochem. 1984;139(2):322–328.
23. Jozsa L, Reffy A, Balint JB. Polarization and electron microscopic studies on the collagen of intact and ruptured human tendons. Acta Histochem. 1984;74(2):209–215.
24. Kannus P, Jozsa L, Kvist M, et al. The effect of immobilization on myotendinous junction: an ultrastructural, histochemical and immunohistochemical study. Acta Physiol Scand. 1992;144(3):387–394.
25. Herzog M, Lindsay WK, McCain WG. Effect of beta-aminioproprionitrile on adhesions following digital flexor tendon repair in chickens. Surg Forum. 1970;21:509–511.
26. Kapetanos G. The effect of the local corticosteroids on the healing and biomechanical properties of the partially injured tendon. Clin Orthop Relat Res. 1982;163:170–179.
27. Kulick MI, Smith S, Hadler K. Oral ibuprofen: evaluation of its effect on peritendinous adhesions and the breaking strength of a tenorrhaphy. J Hand Surg Am. 1986;11(1):110–120.
28. Blumenkranz MS, Ophir A, Claflin AJ, Hajek A. Fluorouracil for the treatment of massive periretinal proliferation. Am J Ophthalmol. 1982;94(4):458–467.
29. Blumenkranz M, Hernandez E, Ophir A, Norton EW. 5-fluorouracil: new applications in complicated retinal detachment for an established antimetabolite. Ophthalmology. 1984;91(2):122–130.
30. Khaw PT, Grierson I, Hitchings RA, Rice NS. 5-fluorouracil and beyond. Br J Ophthalmol. 1991;75(10):577–578.
31. Khaw PT, Ward S, Porter A, et al. The long-term effects of 5-fluorouracil and sodium butyrate on human Tenon’s fibroblasts. Invest Ophthalmol Vis Sci. 1992;33(6):2043–2052.
32. Khaw PT, Sherwood MB, MacKay SL, et al. Five-minute treatments with fluorouracil, floxuridine, and mitomycin have long-term effects on human Tenon’s capsule fibroblasts. Arch Ophthalmol. 1992;110(8):1150–1154.
33. Khaw PT, Doyle JW, Sherwood MB, et al. Effects of intraoperative 5-fluorouracil or mitomycin C on glaucoma filtration surgery in the rabbit. Ophthalmology. 1993;100(3):367–372.
34. Doyle JW, Sherwood MB, Khaw PT, et al. Intraoperative 5-fluorouracil for filtration surgery in the rabbit. Invest Ophthalmol Vis Sci. 1993;34(12):3313–3319.
35. Moran SL, Ryna CK, Orlando GS, et al. Effects of 5-fluorouracil on flexor tendon repair. J Hand Surg Am. 2000;25(2):242–251.
36. Akali A, Khan U, Khaw PT, MacGrouther AD. Decrease in adhesion formation by a single application of 5-fluorouracil after flexor tendon injury. Plast Reconstr Surg. 1999;103(1):151–158.
37. Khan U, Occleston NL, Khaw PT, MacGrouther AD. Single exposures to 5-fluorouracil: a possible mode of targeted therapy to reduce contractile scarring in the injured tendon. Plast Reconstr Surg. 1997;99(2):465–471.
38. Ragoowansi R, Khan U, Brown RA, MacGrouther DA. Reduction in matrix metalloproteinase production by tendon and synovial fibroblasts after a single exposure to 5-fluorouracil. Br J Plast Surg. 2001;54(4):283–287.
39. Singer AJ, Clark RAF. Cutaneous wound healing. N Engl J Med. 1999;341(10):738–746.
40. Costa MA, Wu C, Pham BV, et al. Tissue engineering of flexor tendons: Optimization of tenocyte proliferation using growth factor supplementation. Tissue Eng. 2006;12:1937–1943.
41. Thomopoulos S, Zeagel M, Das R, et al. PDGF-BB released in tendon repair using a novel delivery system promotes cell proliferation and collagen remodeling. J Orthop Res. 2007;25:1358–1368.
42. Juncosa-Melvin N, Boivin JP, Gooch C, et al. The effects of autologous mesenchymal stem cells on the biomechanics and histology of gel-collagen sponge constructs used for rabbit patellar tendon repair. Tissue Eng. 2006;12:369–379.
43. Tang JB, Xu Y, Ding F, Wang XT. Tendon healing in vitro: promotion of collagen gene expression by βFGF with NF-kappaB gene activation. J Hand Surg. 2003;28:215–220.
44. Wang XT, Liu PY, Tang JB. Tendon healing in vitro: modification of tenocytes with exogenous vascular endothelial growth factor gene increases expression of transforming factor beta but minimally affects expression of collagen genes. J Hand Surg. 2005;30:222–229.
45. Aspenberg P, Forslund C. Enhanced tendon healing with GDF 5 and 6. Acta Orthop Scand. 1999;70(1):51–54.
46. Rickert M, Wang H, Wieloch P, et al. Adenovirus-mediated gene transfer of growth and differentiation factor-5 into tenocytes and the healing rat Achilles tendon. Connect Tissue Res. 2005;46(4-5):175–183.
47. Dines JS, Weber L, Razzano P, et al. The effect of growth differentiation factor-5–coated sutures on tendon repair in a rat model. J Shoulder Elbow Surg. 2007;16(5 Suppl):S215–S221.
48. Border WA, Lkuda S, Languino LR, et al. Suppression of experimental glomerulonephritis by antiserum against transforming growth factor B1. Nature. 1990;346:371–374.
49. Border WA, Noble NA. Transforming growth factor-B in tissue fibrosis. N Engl J Med. 1994;331:1286–1292.
50. Chang J, Thunder R, Most D, et al. Studies in flexor tendon wound healing: neutralizing antibody to TGF-beta1 increases postoperative range of motion. Plast Reconstr Surg. 2000;105:148–155.
51. Shah M, Foreman DM, Ferguson MN. Control of scaring in adult wounds by neutralizing antibody to transforming growth factor-B. Lancet. 1992;339:213–214.
52. Wahl SM, Allen JB, Costa GL. Reversal of acute and chronic synovial inflammation by anti-transforming growth factor-B. J Exp Med. 1993;177:225–230.
53. Chang J, Most D, Stelnicki E, et al. Gene expression of transforming growth factor beta-1 in rabbit zone II flexor tendon wound healing: Evidence for dual mechanisms of repair. Plast Reconstr Surg. 1997;100:937–944.
54. Natsu-ume T, Nakamura N, Shino K, et al. Temporal and spatial expression of transforming growth factor beta in the healing patellar ligament of the rat. J Orthop Res. 1997;15:837–843.
55. Ackermann PW, Ahmed M, Kreicbergs A. Early nerve regeneration after Achilles tendon rupture—a prerequisite for healing? J Orthop Res. 2002;20:849–856.
56. Bring DK, Kreicbergs A, Renström PA, Ackermann PW. Physical activity modulates nerve plasticity and stimulates repair after Achilles tendon rupture. J Orthop Res. 2007;25:164–172.
57. Schäffer M, Beiter T, Becker HD, Hunt TK. Neuropeptides: mediators of inflammation and tissue repair? Arch Surg. 1998;133:1107–1116.
58. Smith CA, Stauber F, Waters C, et al. Transforming growth factor-beta following skeletal muscle strain injury in rats. J Applied Physiol. 2007;102(2):755–761.
59. Ackermann PW, Li J, Lundeberg T, Kreicbergs A. Neuronal plasticity in relation to nociception and healing of rat Achilles tendon. J Orthop Res. 2003;21:432–441.
60. Brain SD. Sensory neuropeptides: their role in inflammation and wound healing. Immunopharmacology. 1997;37:133–152.
61. Burssens P, Steyaert A, Forsyth R, et al. Exogenously administered substance P and neutral endopeptidase inhibitors stimulate fibroblast proliferation, angiogenesis and collagen organization during Achilles tendon healing. [Erratum appears in Foot Ankle Int. 2007 Oct;28(10):table of contents. Note: De Paepe, Yves corrected to Depaepe, Yves]. Foot Ankle Int. 2005;26(10):832–839.
62. Nilsson J, von Euler AM, Dalsgaard CJ. Stimulation of connective tissue cell growth by substance P and substance k. Nature. 1985;315:61–63.
63. Steyaert AE, Burssens PJ, Vercruysse CW, et al. The effects of substance P on the biomechanic properties of ruptures rat Achilles’ tendon. Arch Phys Med Rehabil. 2006;87:254–258.
64. Nixon AJ, Goodrich LR, Scimeca MS, et al. Gene therapy in musculoskeletal repair. Ann NY Acad Sci. 2007;1117:310–327.
65. Dines JS, Weber L, Razzano P, et al. The effect of growth differentiation factor-5-coated sutures on tendon repair in a rat model. J Shoulder Elbow Surg. 2007;16(5 Suppl):S215–221.
66. White WL. Tendon grafts: A consideration of their source, procurement and suitability. Surg Clin North Am. 1960;40(2):403–413.
67. Boyes JH, Stark HH. Flexor-tendon grafts in the fingers and thumb. A study of factors influencing results in 1000 cases. J Bone Joint Surg Am. 1971;53(7):1332–1342.
68. Gelberman RH, Seiler JG 3rd, Rosenberg AE, et al. Intercalary flexor tendon grafts. A morphological study of intrasynovial and extrasynovial donor tendons. Scand J Plast Reconstr Surg Hand Surg. 1992;26(3):257–264.
69. Abrahamsson SO, Gelberman RH, Lohmander SL. Variations in cellular proliferation and matrix synthesis in intrasynovial and extrasynovial tendons: an in vitro study in dogs. J Hand Surg Am. 1994;19(2):259–265.
70. Gelberman RH. Flexor tendon physiology: tendon nutrition and cellular activity in injury and repair. Instructional Course Lectures. 1985;34:351–360.
71. Duffy FJ Jr, Seiler JG, Gelberman RH, Hergreuter CA. Growth factors and canine flexor tendon healing: initial studies in uninjured and repair models. J Hand Surg Am. 1995;20(4):645–649.
72. Tsuzaki M, Brigman BE, Yamamoto J, et al. Insulin-like growth factor-I is expressed by avian flexor tendon cells. J Orthop Res. 2000;18(4):546–556.
73. Ngo M, Pahm H, Longaker MT, Chang J. Differential expression of transforming growth factor-beta receptors in a rabbit zone II flexor tendon wound healing model. Plast Reconstr Surg. 2001;108(5):1260–1267.
74. Docheva D, Hunziker EB, Fässler R, Brandau O. Tenomodulin is necessary for tenocyte proliferation and tendon maturation. Mol Cell Biol. 2005;25(2):699–705.
75. Shukunami C, Takimoto A, Oro M, Hiraki Y. Scleraxis positively regulates the expression of tenomodulin, a differentiation marker of tenocytes. Dev Biol. 2006;298(1):234–247.
76. Fathke C, Wilson L, Hutter J, et al. Contribution of bone marrow-derived cells to skin: collagen deposition and wound repair. Stem Cells. 2004;22:812–822.
77. Krause DS, Theise ND, Collector MI, et al. Multi-organ, multi lineage engraftment by a single bone marrow -derived stem cell. Cell. 2001;105:369–377.
78. Tepper OM, Capla JM, Galiano RD, et al. Adult vasculogenesis occurs through in situ recruitment, proliferation, and tubulization of circulating bone marrow derived cells. Blood. 2005;105:1068–1077.
79. Butler DL, Juncosa-Melvin N, Boivin GP, et al. Functional tissue engineering of tendon repair: a multidisciplinary strategy using mesenchymal stem cells, bioscaffolds, and mechanical stimulation. J Orthop Res. 2008;26:1–9.
80. Cao Y, Liu Y, Liu W, et al. Bridging tendon defects using autologous tenocyte engineered tendon in a hen model. Plast Reconstr Surg. 2002;110:1280–1289.
81. Juncosa-Melvin N, Shearn JT, Boivin GP, et al. Effects of mechanical stimulation on the biomechanics and histology of stem cell collagen sponge constructs for rabbit patellar tendon repair. Tissue Eng. 2006;12:2291–2300.
82. Liu W, Chen B, Deng D, et al. Repair of tendon defects with dermal fibroblast engineered tendon in a porcine model. Tissue Eng. 2006;12:775–788.
83. Zantop T, Gilbert TW, Yoder MC, Badylak SF. Extracellular matrix scaffolds are repopulated by bone marrow derived cells in a mouse model of Achilles tendon reconstruction. J Orthop Res. 2006;24:1299–1309.
84. Zhao C, Sun YL, Amadio PC, et al. Surface treatment of flexor tendon autografts with carbodiimide-derivatized hyaluronic acid. An in vivo canine model. J Bone Joint Surg Am. 2006;88(10):2181–2191.
85. Taguchi M, Sun YL, Zhao C, et al. Lubricin surface modification improves extrasynovial tendon gliding in a canine model in vitro. J Bone Joint Surg Am. 2008;90(1):129–135.
86. Tanaka T, Sun YL, Zhao C, et al. Optimization of surface modifications of extrasynovial tendon to improve its gliding ability in a canine model in vitro. J Orthop Res. 2006;24(7):1555–1561.
87. Sun YL, Yang C, Amadio PC, et al. Reducing friction by chemically modifying the surface of extrasynovial tendon grafts. J Orthop Res. 2004;22(5):984–989.
88. Józsa L, Kannus P. Histopathological findings in spontaneous tendon ruptures. Scand J Med Sci Sports. 1997;7(2):113–118.
89. Fraser JR, Laurent TC, Laurent UBG. Hyaluronan: its nature, distribution, functions, and turnover. J Intern Med. 1997;242(1):27–33.
90. Kain CC, Manske PR, Reinsel TE, et al. Reconstruction of the digital pulley in the monkey using biologic and nonbiologic materials. J Orthop Res. 1988;6(6):871–877.
91. Uchiyama S, Amadio PC, Ishikawa J, An KN. Boundary lubrication between the tendon and the pulley in the finger. J Bone Joint Surg Am. 1997;79(2):213–218.
92. Goldberg RL, Toole BP. Hyaluronate inhibition of cell proliferation. Arthritis Rheum. 1987;30:769–778.
93. Wiig M, Abrahamsson SO, Lundborg G. Tendon repair–cellular activities in rabbit deep flexor tendons and surrounding synovial sheaths and the effects of hyaluronan: an experimental study in vivo and in vitro. J Hand Surg Am. 1997;22(5):818–825.
94. Jay GD. Characterization of a bovine synovial fluid lubricating factor. I. Chemical, surface activity and lubricating properties. Connect Tissue Res. 1992;28(1-2):71–88.
95. Marcelino J, Capten JD, Suwairi WM, et al. CACP, encoding a secreted proteoglycan, is mutated in camptodactyly-arthropathy-coxa vara-pericarditis syndrome. Nature Genet. 1999;23(3):319–322.
96. Flannery CR, Hughes CE, Schumacher BL, et al. Articular cartilage superficial zone protein (SZP) is homologous to megakaryocyte stimulating factor precursor and Is a multifunctional proteoglycan with potential growth-promoting, cytoprotective, and lubricating properties in cartilage metabolism. Biochem Biophys Res Commun. 1999;254(3):535–541.
97. Rees S, Davies JR, Tudor D, et al. Immunolocalisation and expression of proteoglycan 4 (cartilage superficial zone proteoglycan) in tendon. Matrix Biol. 2002;21:593–602.
98. Swann DA, Sotman S, Dixon M, Brooks C. The isolation and partial characterization of the major glycoprotein from articular lubricating fraction from bovine synovial fluid. Biochem J. 1977;161:473–485.
99. Jay GD, Tantravahi U, Britt DE, et al. Homology of lubricin and superficial zone protein (SZP): products of megakaryocyte stimulating factor (MSF) gene expression by human synovial fibroblasts and articular chondrocytes localized to chromosome 1q25. J Orthop Res. 2001;19(4):677–687.
100. Jay GD, Britt DE, Cha CJ. Lubricin is a product of megakaryocyte stimulating factor gene expression by human synovial fibroblasts. [Comment]. J Rheumatol. 2000;27(3):594–600.
101. Sun Y, Berger EJ, Zhao C, et al. Mapping lubricin in canine musculoskeletal tissues. Connect Tissue Res. 2006;47(4):215–221.
102. Schaefer DB, Wendt D, Moretti M, et al. Lubricin reduces cartilage—cartilage integration. Biorheology. 2004;41(3-4):503–508.
103. Amiel D, Ishizue K, Billings E Jr, et al. Hyaluronan in flexor tendon repair. J Hand Surg. 1989;14A:837–843.
104. St Onge R, Weiss C, Denlinger JL, Balazs EA. A preliminary assessment of Na-hyaluronate injection into “no man’s land” for primary flexor tendon repair. Clin Orthop Relat Res. 1980;146:269–275.
105. Meyers SA, Seaber AV, Glisson RR, Nunley JA. Effect of hyaluronic acid/chondroitin sulfate on healing of full-thickness tendon lacerations in rabbits. J Orthop Res. 1989;7(5):683–689.
106. Hagberg L. Exogenous hyaluronate as an adjunct in the prevention of adhesions after flexor tendon surgery: a controlled clinical trial. J Hand Surg Am. 1992;17(1):132–136.
107. Miller JA, Ferguson RL, Powers DL, et al. Efficacy of hyaluronic acid/nonsteroidal anti-inflammatory drug systems in preventing postsurgical tendon adhesions. J Biomed Mater Res. 1997;38:25–33.
108. Gaughan EM, Nixon AJ, Krook LP, et al. Effects of sodium hyaluronate on tendon healing and adhesion formation in horses. Am J Vet Res. 1991;52(5):764–773.
109. Salti NI, Tuel RJ, Mass DP. Effect of hyaluronic acid on rabbit profundus flexor tendon healing in vitro. J Surg Res. 1993;55(4):411–415.
110. Weiss C. The inhibition of flexor tendon adhesions. Bull Hosp Joint Dis Orthop Inst. 1986;46(2):193–194.
111. Weiss C, Suros JM, Michalow A, et al. The role of Na-hylan in reducing postsurgical tendon adhesions: Part 2. Bull Hosp Joint Dis Orthop Inst. 1987;47(1):31–39.
112. Foland JW, Trotter GW, Powers BE, et al. Effect of sodium hyaluronate in collagenase-induced superficial digital flexor tendinitis in horses. Am J Vet Res. 1992;53(12):2371–2376.
113. Band PA. The chemistry, biology, and medical application of hyaluronan and its derivatives. In: Laurent TC, ed. Hyaluronan Derivatives: Chemistry and Clinical Applications. London U.K.: Portland Press; 1998:33–42.
114. Momose T, Amadio PC, Sun YL, et al. Surface modification of extrasynovial tendon by chemically modified hyaluronic acid coating. J Biomed Mater Res. 2002;59(2):219–224.
115. Bulpitt P, Aeschlimann D. New strategy for chemical modification of hyaluronic acid: preparation of functionalized derivatives and their use in the formation of novel biocompatible hydrogels. J Biomed Mater Res. 1999;47(2):152–169.
116. Hanthamrongwit M, Reid WH, Grant MH. Chondroitin-6-sulphate incorporated into collagen gels for the growth of human keratinocytes: the effect of cross-linking agents and diamines. Biomaterials. 1996;17(8):775–780.
117. Kuo JW, Swann DA, Prestwich GD. Chemical modification of hyaluronic acid by carbodiimides. Bioconjug Chem. 1991;2(4):232–241.
118. Tzianabos AO, Cisneros RL, Gershkovitch J, et al. Effect of surgical adhesion reduction devices on the propagation of experimental intra-abdominal infection. Arch Surg. 1999;134(11):1254–1259.
119. Burns JW, Skinner K, Colt MJ, et al. A hyaluronate based gel for the prevention of postsurgical adhesions: evaluation in two animal species. Fertil Steril. 1996;66(5):814–821.
120. Leach RE, Burns JW, Dawe EJ, et al. Reduction of postsurgical adhesion formation in the rabbit uterine horn model with use of hyaluronate/carboxymethylcellulose gel. Fertil Steril. 1998;69(3):415–418.
121. Brunelli G, Longinotti C, Bertazzo C, et al. Adhesion reduction after knee surgery in a rabbit model by Hyaloglide, a hyaluronan derivative gel. J Orthop Res. 2005;23(6):1377–1382.
122. Zhao C, Sun YL, Amadio PC, et al. Surface treatment of flexor tendon autograft with carbodiimide-derivatized hyaluronic acid. An in vivo canine model. J Bone Joint Surg Am. 2006;88:2181–2191.
123. Tanaka T, Zhao C, Sun YL, et al. The effect of carbodiimide-derivatized hyaluronic acid and gelatin surface modification on peroneus longus tendon graft in a short-term canine model in vivo. J Hand Surg Am. 2007;32(6):876–881.
124. Zhao C, Amadio PC, Tanaka T, et al. Short-term assessment of optimal timing for postoperative rehabilitation after flexor digitorum profundus tendon repair in a canine model. J Hand Ther. 2005;18(3):322–329. quiz 329
125. Cetin A, Dinçer F, Keçik A, Cetin M. Rehabilitation of flexor tendon injuries by use of a combined regimen of modified Kleinert and modified Duran techniques. Am J Phys Med Rehabil. 2001;80(10):721–728.
126. Helm R. The management of flexor tendon injuries in zone II. Curr Orthop. 2002;16:434–444.
127. Elliot D. Primary flexor tendon repair—operative repair, pulley management and rehabilitation. J Hand Surg Br. 2002;27(6):507–513.
128. Golash A, Kay A, Warner JG, et al. Efficacy of ADCON-T/N after primary flexor tendon repair in zone II: a controlled clinical trial. J Hand Surg Br. 2003;28(2):113–115.
129. Miller B, Dodds SD, deMars A, et al. Flexor tendon repairs: the impact of fiberwire on grasping and locking core sutures. J Hand Surg Am. 2007;32(5):591–596.
130. Silfverskiold KL, Andersson CH. Two new methods of tendon repair: an in vitro evaluation of tensile strength and gap formation. J Hand Surg Am. 1993;18(1):58–65.
131. Aoki M, Manske PR, Pruitt DL, Larson BJ. Work of flexion after tendon repair with various suture methods. A human cadaveric study. J Hand Surg Br. 1995;20(3):310–313.
132. Zhao C, Amadio PC, Zobitz ME, An KN. Gliding characteristics of tendon repair in canine flexor digitorum profundus tendons. J Orthop Res. 2001;19(4):580–586.
133. Momose T, Amadio PC, Zhao C, et al. Evaluation of suture techniques with high breaking strength and low gliding resistance. Acta Orthop Scand. 2001;72(6):635–641.
134. Paillard PJ, Amadio PC, Zhao C, et al. Gliding resistance after FDP and FDS tendon repair in zone II: an in vitro study. Acta Orthop Scand. 2002;73(4):465–470.
135. Zhao C, Amadio PC, Paillard PJ, et al. Digital resistance and tendon strength during the first week after flexor digitorum profundus tendon repair in a canine model in vivo. J Bone Joint Surg Am. 2004;86-A(2):320–327.
136. Gelberman RH, Boyer MI, Brodt MD, et al. The effect of gap formation at the repair site on the strength and excursion of intrasynovial flexor tendons. An experimental study on the early stages of tendon-healing in dogs. J Bone J Surg Am. 1999;81:975–982.
137. Khan U, Kakar S, Akali A, et al. Modulation of the formation of adhesions during the healing of injured tendons. J Bone Joint Surg Br. 2000;82(7):1054–1058.
138. Boyer MI, Meunier MJ, Lescheid J, et al. The influence of cross-sectional area on the tensile properties of flexor tendons. J Hand Surg Am. 2001;26(5):828–832.
139. Lieber RL, Amiel D, Kaufman KR, et al. Relationship between joint motion and flexor tendon force in the canine forelimb. J Hand Surg. 1996;21A(6):957–962.
140. Lieber RL, Silva MJ, Amiel D, Gelberman RH. Wrist and digital joint motion produce unique flexor tendon force and excursion in the canine forelimb. J Biomech. 1999;32:175–181.
141. Silva M, Brodt MD, Boyer MI, et al. Effects of increased in vivo excursion on digital range of motion and tendon strength following flexor tendon repair. J Orthop Res. 1999;17:777–783.
142. McLarney E, Hoffman H, Wolfe SW. Biomechanical analysis of the cruciate four-strand flexor tendon repair. J Hand Surg Am. 1999;24(2):295–301.
143. Lin GT, An KN, Amadio PC, Cooney WP 3rd. Biomechanical studies of running suture for flexor tendon repair in dogs. J Hand Surg Am. 1988;13(4):553–558.
144. Taras JS, Raphael JS, Marczyk SC, Bauerle WB. Evaluation of suture caliber in flexor tendon repair. J Hand Surg Am. 2001;26(6):1100–1104.
145. Momose T, Amadio PC, Zhao C, et al. Suture techniques with high breaking strength and low gliding resistance: experiments in the dog flexor digitorum profundus tendon. Acta Orthop Scand. 2001;72(6):635–641.
146. Silva JM, Zhao C, An KN, et al. Gliding resistance and strength of composite sutures in human flexor digitorum profundus tendon repair: an in vitro biomechanical study. J Hand Surg Am. 2009;34(1):87–92.
147. Schuind F, Garcia-Elias M, Cooney WP 3rd, An KN. Flexor tendon forces in vivo measurements. J Hand Surg Am. 1992;17:291–298.
148. Momose T, Zhao C, An K, et al. Gliding resistance and breaking strength of suture techniques with knots inside the repair site. 46th Annual Meeting of Orthopaedic Research Society. Orlando, FL, 2000.
149. Momose T, Amadio PC, Zhao C, et al. The effect of knot location, suture material, and suture size on the gliding resistance of flexor tendons. J Biomed Mater Res. 2000;53(6):806–811.
150. Zhao C, Amadio PC, Mamose T, et al. Remodeling of the gliding surface after flexor tendon repair in a canine model in vivo. J Orthop Res. 2002;20(4):857–862.
151. Amadio PC, Amadio PC. Friction of the gliding surface. Implications for tendon surgery and rehabilitation. J Hand Ther. 2005;18(2):112–119.
152. Miller B, Dodds SD, deMars A, et al. Flexor tendon repairs: the impact of fiberwire on grasping and locking core sutures. J Hand Surg Am. 2007;32(5):591–596.
153. Zhao C, Amadio PC, Momose T, et al. Effect of synergistic wrist motion on adhesion formation after repair of partial flexor digitorum profundus tendon lacerations in a canine model in vivo. J Bone Joint Surg. 2002;84-A(1):78–84.
154. Zhao C, Amadio PC, Momose T, et al. The effect of suture technique on adhesion formation after flexor tendon repair for partial lacerations in a canine model. J Trauma. 2001;51(5):917–921.
155. Mason M, Allen H. The rate of healing of tendons. An experimental study of tensile strength. Ann Surg. 1941;113:424–459.
156. Verdan CE. Half a century of flexor-tendon surgery. Current status and changing philosophies. J Bone Joint Surg Am. 1972;54(3):472–4791.
157. Kleinert HE, Verdan C. Report of the Committee on Tendon Injuries (International Federation of Societies for Surgery of the Hand). J Hand Surg Am. 1983;8(5 Pt 2):794–798.
158. Duran RJ, Houser RG, Stover MG. Management of flexor tendon lacerations in zone 2 using controlled passive motion. In: Hunter JM, ed., et al. Rehabilitation of the Hand. St. Louis, MO: CV Mosby; 1978:217–224.
159. Lister GD, Kleinert HE, Kutz JE, Atasoy E. Primary flexor tendon repair followed by immediate controlled mobilization. J Hand Surg Am. 1977;2(6):441–451.
160. Strickland JW. Flexor tendon surgery. Part 1: Primary flexor tendon repair see comments]. J Hand Surg Br. 1989;14(3):261–272.
161. Silfverskiold KL, May EJ. Flexor tendon repair in zone II with a new suture technique and an early mobilization program combining passive and active flexion [see comments]. J Hand Surg Am. 1994;19(1):53–60.
162. Woo SL-Y, Gelberman RH, Cobb NG, et al. The importance of controlled passive mobilization in flexor tendon healing. Acta Orthop Scand. 1981;52:615–622.
163. Bishop AT, Cooney WP, Wood MB. Treatment of partial flexor tendon lacerations: the effect of tenorrhaphy and early protected mobilization. J Trauma. 1986;26(4):301–312.
164. Hitchcock TF, Light TR, Bunch WH, et al. The effect of immediate constrained digital motion on the strength of flexor tendon repairs in chickens. J Hand Surg. 1987;12A:590–595.
165. Gelberman RH, Woo SL, Amiel D, et al. Influences of flexor sheath continuity and early motion on tendon healing in dogs. J Hand Surg Am. 1990;15(1):69–77.
166. Nessler JP, Amadio PC, Berglund LJ, An KN. Healing of canine tendon in zones subjected to different mechanical forces. J Hand Surg Br. 1992;17(5):561–568.
167. Zhao CF, Amadio PC, Momose T, et al. The effect of synergistic motion on FDP excursion after tendon repair in a canine model in vivo. 46th Annual Meeting of Orthopaedic Research Society. Orlando, FL 2000.
168. Adolfsson L, Söderberg G, Larsson M, Karlander LE. The effects of a shortened postoperative mobilization programme after flexor tendon repair in zone 2. J Hand Surg Br. 1996;21(1):67–71.
169. Halikis MN, Mankse PR, Kubota H, Aoki M. Effect of immobilization, immediate mobilization, and delayed mobilization on the resistance to digital flexion using a tendon injury model. J Hand Surg Am. 1997;22(3):464–472.
170. Zhao C, Amadio PC, Paillard P, et al. Digital resistance and tendon strength during the first week after flexor digitorum profundus tendon repair in a canine model in vivo. J Bone Joint Surg Am. 2004;86A:320–327.
171. Sántha E, Szarvas J, Szabó L, Répásy E. [Active movement therapy after flexor tendon suture using a new dynamic control splint][Article in German]. Handchir Mikrochir Plast Chir. 1998;30(5):312–316.
172. Lieber R, Silva MJ, Amiel D, Gelbern RH. Wrist and digital joint motion produce unique flexor tendon force and excursion in the canine forelimb. J Biomech. 1999;32(2):175–181.
173. Cooney WP, Wiedman K, Malo D, Wood MB. Management of acute flexor tendon injury in the hand. Instr Course Lect. 1985;34:373–381.
174. Saldana MJ, Chow JA, Gerbin P 2nd, et al. Further experience in rehabilitation of zone II flexor tendon repair with dynamic traction splinting. Plast Reconstr Surg. 1991;87(3):543–546.
175. Amadio P, Berglund L, An KN. Effect of Weightbearing Stress on Healing of Biologically Distinct Zones of Canine Flexor Tendon. La Jolla, CA: First World Congress of Biomechanics; 1990.
176. Tanaka T, Amadio PC, Zhao C, et al. Gliding resistance versus work of flexion—two methods to assess flexor tendon repair. J Orthop Res. 2003;21:813–818.
177. Yang C, Zhao C, Amadio PC, et al. Total and intrasynovial work of flexion of human cadaver flexor digitorum profundus tendons after modified Kessler and MGH repair techniques. J Hand Surg Am. 2005;30(3):466–470.
178. Hotokezaka S, Manske PR. Differences between locking loops and grasping loops: effects on 2-strand core suture [see comments]. J Hand Surg Am. 1997;22(6):995–1003.
179. Sanders DW, Milne AD, Dobravec A, et al. Cyclic testing of flexor tendon repairs: an in vitro biomechanical study see comments]. J Hand Surg Am. 1997;22(6):1004–1010.
180. Mashadi ZB, Amis AA. Strength of the suture in the epitenon and within the tendon fibres: development of stronger peripheral suture technique. J Hand Surg Br. 1992;17(2):172–175.
181. Wade PJ, Wetherell RG, Amis AA. Flexor tendon repair: significant gain in strength from the Halsted peripheral suture technique. J Hand Surg Br. 1989;14(2):232–235.
182. Gelberman RH, Boyer MI, Brodt MD, et al. The effect of gap formation at the repair site on the strength and excursion of intrasynovial flexor tendons. An experimental study on the early stages of tendon-healing in dogs. J Bone Joint Surg Am. 1999;81(7):975–982.
183. Tang JB, Gu YT, Rice K, et al. Evaluation of four methods of flexor tendon repair for postoperative active mobilization. Plast Reconstr Surg. 2001;107(3):742–749.
184. Silva MJ, Boyer MI, Gelberman RH, et al. Repair site gap decreases the strength of repaired canine flexor tendons but does not decrease digital range of motion. in 45th Annual Meeting, Orthopaedic Research Society. 1999B. Anaheim, CA.
185. Tanaka T, Amadio PC, Zhao C, et al. Gliding characteristics and gap formation for locking and grasping tendon repairs: a biomechanical study in a human cadaver model. J Hand Surg Am. 2004;29:6–14.
186. Zhao C, Moran SL, Cha SS, et al. An analysis of factors associated with failure of tendon repair in the canine model. J Hand Surg Am. 2007;32(4):518–525.
187. Zhao C, Amadio PC, Tanaka T, et al. Effect of gap size on gliding resistance after flexor tendon repair. J Bone Joint Surg Am. 2004;86-A(11):2482–2488.
188. Groth GN. Pyramid of progressive force exercises to the injured flexor tendon. J Hand Ther. 2004;17(1):31–42.

* Disclosure: The author has, with others, applied for a patent relating to the tissue engineering of tendon surfaces to reduce friction, but has no financial or other relationships with any commercial entities related to the subject of this chapter.