CHAPTER 93
Examination and Management of Scapular Dysfunction
ANGELA TATE PT, PhD AND PHILIP MCCLURE, PT, PhD, FAPTA
CRITICAL POINTS
▪ It is only in recent years that specific tests have been developed to assess the function of the scapula. The measurement properties of these tests are still being investigated.
▪ The scapula should be assessed with most upper quarter conditions, and the examination should include the scapula dyskinesis test, modified scapula assistance test, scapula reposition test, pectoralis minor length, thoracic kyphosis/flexibility, flexibility of posterior capsule of the glenohumeral joint, and muscle performance testing for the primary scapular stabilizers: lower trapezius, middle trapezius, and serratus anterior.
▪ One key principle in designing a scapular exercise program is to match the difficulty of the exercise with the patient’s level of motor control and strength. It is important to observe the patient posteriorly during an exercise to assure that he or she is able to maintain good scapular control.
Scapular dysfunction is a common clinical problem, and proper scapular motion and stability is considered to be crucial to normal function of the shoulder. The scapula is required to serve as a stable base for glenohumeral function but is also required to move through a substantial arc of motion. This motion is required to maintain optimal muscle length-tension relationships and glenohumeral joint alignment and stability during elevation of the arm.
The goals of this chapter are to: (1) describe normal and abnormal motion of the scapula, (2) discuss the relationship between scapular dyskinesis and shoulder pathology, (3) describe current examination techniques for identifying possible scapular pathology, and (4) describe intervention techniques for scapular pathology including enhancing muscle performance, stretching, bracing, and taping.
Normal Scapular Motion
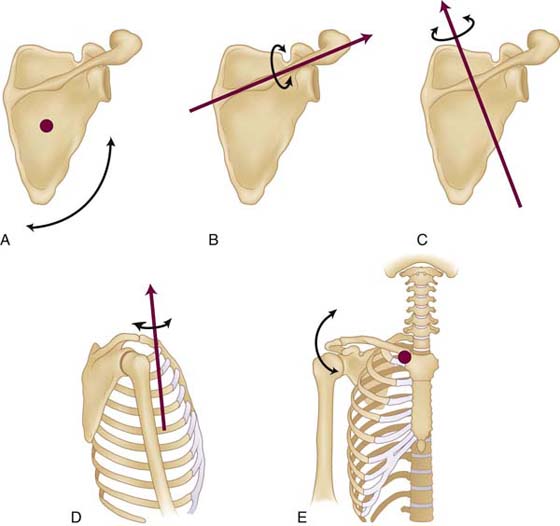
The basic anatomy of the shoulder girdle and the scapular muscles is covered in Chapter 4; therefore, this section will focus on describing scapular motion and the primary muscles and other factors controlling this motion. The terminology used to describe scapular motion is quite varied in the literature and no definitive standard has emerged, but we have promoted using scapular and clavicular angles to accurately describe scapular orientation and position, respectively. Three scapular rotations are typically used to describe scapular orientation,1,2 and these are depicted in Figure 93-1A–C. Upward/downward rotation of the scapula occurs around an axis that is perpendicular to the plane of the scapula. Anterior/posterior tilting (sometimes called tipping1) occurs around an axis through the spine of the scapula. Posterior tilting involves the inferior angle of the scapula moving anteriorly and the superior border moving posteriorly. Internal/external rotation occurs around a vertically oriented axis, and external rotation involves the lateral border of the scapula moving away from the thorax. More precise biomechanical definitions of these axis systems are available in original sources.3
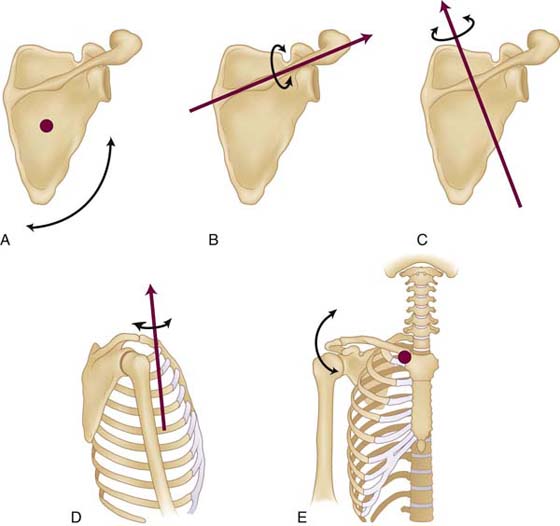
Figure 93-1 Scapular and clavicular rotations used to describe motion. A, Scapular upward/downward rotation. B, Scapular anterior/posterior tilting. C, Scapular internal/external rotation. D, Clavicular protraction/retraction. E, Clavicular elevation/depression.
Scapular position on the thorax has been described in various ways using terms that correspond to superior-inferior or medio-lateral translation of the scapula from its normal resting position between the second and seventh ribs. However, because the clavicle acts as a strut, the scapula remains at a fixed medio-lateral position relative to the thorax (assuming an intact acromioclavicular joint and clavicle). Therefore, the rotational motion of the clavicle around the sternoclavicular joint into protraction/retraction and elevation/depression can be used to describe scapular position in two degrees of freedom.4 The description of scapular position using these two clavicular angles can be likened to the identification of a point on the earth using two angles, longitude and latitude.4 As shown in Figure 93-1D and E, clavicular elevation and depression occur around an anterior-posterior axis through the sternoclavicular joint, and clavicular protraction and retraction occur around a vertical axis through the sternoclavicular joint. Therefore, the motions of “scapular elevation or depression” and “scapular protraction or retraction” really occur in conjunction with corresponding rotary motions at the sternoclavicular joint.
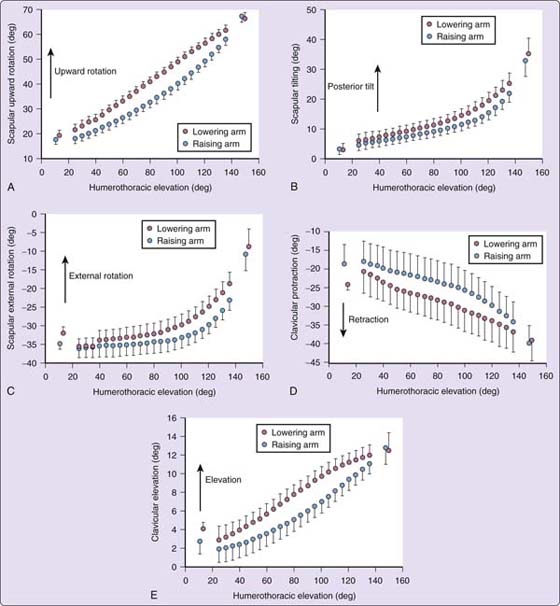
During elevation of the arm there is a consistent pattern of scapular upward rotation, posterior tilting, and external rotation, along with clavicular elevation and retraction. Figure 93-2 shows the normal pattern for each of these motions in healthy subjects derived using a sensor attached directly to the scapula via bone pins during arm raising and lowering in the scapular plane. This figure shows each of the scapular and clavicular rotations separately with humerothoracic motion plotted along the x-axis.
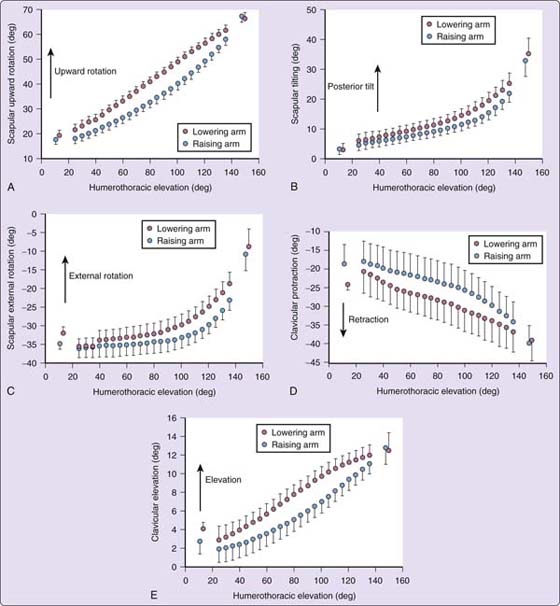
Figure 93-2 Humerothoracic elevation (in degrees) during various scapular movements of arm elevation. A, Scapular upward rotation. B, Scapular posterior tilting. C, Scapular external rotation. D, Clavicle retraction. E, Clavicle elevation.
As evidenced by Figure 93-2A, scapular upward rotation, there is a much greater contribution from the glenohumeral joint than the scapulothoracic joint in the early phase of elevation. After 90 degrees of arm elevation, the contribution from the glenohumeral joint and the scapulothoracic joint become almost equal. Scapular upward rotation is controlled primarily by a force couple between the upper and lower trapezius and the serratus anterior.5,6
Posterior tilting (Fig. 93-2B) and external rotation (Fig. 93-2C) motions are nonlinear, with the majority of these motions not occurring until after 90 degrees of arm elevation. While specific muscle activity associated with these motions has not been demonstrated directly, the lower fibers of the serratus anterior and lower trapezius are positioned to produce posterior tilting and the middle trapezius is positioned to produce external rotation. Weakness in these muscles following nerve injury has been clearly associated with scapular winging, which is attributable to excessive anterior tilting and scapular internal rotation.7
The clavicular retraction (Fig. 93-2D) observed suggests that the superior aspect of the scapula normally moves posteriorly during arm elevation while the scapula also moves superiorly as represented by clavicular elevation (Fig. 93-2E). These motions are attributable to all parts of the trapezius muscle.8
Abnormal Scapular Motion (Scapular Dyskinesis)
A commonly observed abnormal pattern of scapular motion (scapular dyskinesis) is the premature or excessive scapular elevation that appears as shrugging (Fig. 93-3). This pattern has been associated with rotator cuff pain,9 weakness,10,11 and fatigue.12 It has also been observed with loss of glenohumeral motion.13,14 Therefore, excessive or early elevation of the scapula is a sign of scapular compensation for a weak rotator cuff and/or a stiff glenohumeral joint capsule. This shrugging motion has been associated with increased upper trapezius activity.15,16 Abnormal eccentric control of scapular rotation during arm lowering may also occur. The normal pattern of scapular downward rotation during arm lowering is shown in Figure 93-2B and is quite linear. Clinically, this should appear as a smooth descent of the scapula during arm lowering. We have commonly observed that poor eccentric control of this scapular downward rotation appears as a rapid dumping of the scapula instead of smooth downward rotation (Fig. 93-4). We are unaware of experimental documentation of this kinematic abnormality.

Figure 93-3 Excessive scapular elevation “shrugging” associated with glenohumeral weakness or stiffness.

Figure 93-4 Excessive and poor eccentric control of scapular downward rotation on the left side during arm lowering known as “dumping”.
Another common form of scapular dyskinesis is scapular winging wherein either the inferior angle or medial border of the scapula become more prominent. Inferior angle prominence would be associated with anterior tilting of the scapula, while medial border prominence would be associated with excessive scapular internal rotation. We have documented these motion abnormalities in our laboratory on subjects with long thoracic nerve injuries (Fig. 93-5) affecting the serratus anterior muscle. Another source that may contribute to scapular winging is the action of the pectoralis minor muscle. If this muscle is tight or overactive, it has the ability to tilt the scapula forward, producing winging of the inferior angle as well as scapular depression (Fig. 93-6). Borstad has presented data suggesting that subjects with tight pectoralis minor muscles demonstrate greater anterior tilting and scapular internal rotation.17

Figure 93-5 Long thoracic nerve palsy and associated serratus anterior weakness producing scapular winging with anterior tilt and downward rotation on the left.

Figure 93-6 Pectoralis minor tightness or overactivity producing anterior tilting of the scapula during arm elevation, which produces the appearance of winging.
Is Scapular Dyskinesis Related to Shoulder Pathology?
Recognition of the biomechanical role of the scapula in normal shoulder function has led to several clinical studies attempting to associate abnormal scapular motion, “scapular dyskinesis,” with shoulder pathology such as shoulder impingement2,16,18,19,23 or instability.20 These studies have included several methods of capturing scapular motion including Moiré topography, electromechanical digitization, radiographic methods, MRI, and electromagnetic tracking devices. Results of studies assessing three-dimensional scapular motion in those with pathology have been inconsistent. Subjects with shoulder impingement have been found to demonstrate increased posterior tilting,21,22 decreased posterior tilting,2,6,23 decreased upward rotation,16,23 increased upward rotation,18,21 increased superior translation,2,21 and increased internal rotation.16,20 In addition to the variability of findings in these studies, the magnitude of differences between those with healthy shoulders and those with pathology is typically small, in the 3 to 5 degree range, and it is unclear whether these differences, although statistically significant, are really of clinical significance. Furthermore, in a recent study in overhead athletes, we failed to find an association between shoulder symptoms and abnormal scapular motion.24 Despite some authors claiming a strong relationship between abnormal scapular motion and shoulder pathology,25-27 the actual research evidence supporting this assertion is limited. Other clinical tests predicated on altering symptoms with manual scapula repositioning may hold promise in clarifying which patients truly have scapular dysfunction driving their symptoms.28-30
Specific Nerve Injuries
The spinal accessory and long thoracic nerves are two nerves commonly injured that lead to scapular muscle dysfunction, primary winging, and related shoulder disability. The spinal accessory nerve (cranial nerve XI) is derived from the ventral rami of C2, C3, and C4. It runs behind the sternocleidomastoid muscle and then emerges more superficially over the levator scapula to innervate the trapezius muscle. Due to its relatively superficial course, it is more susceptible to injury. Spinal accessory nerve injury has been reported to occur following blunt trauma, traction, lymph node biopsy in the posterior cervical triangle, and radical neck dissection.31 In the case of trapezius weakness, the shoulder appears depressed with the scapula translated laterally and the inferior angle rotated laterally. Winging will be most apparent with frontal plane abduction to 90 degrees.7
The long thoracic nerve originates from the ventral rami of the C5, C6, and C7 cervical nerves. The nerve passes around the middle scalene muscle then reaches the upper slip of the serratus anterior muscle and descends along its anterior surface. This nerve can be damaged from viral illness, repetitive trauma, stretching, or surgery. Long thoracic nerve injury produces weakness of the serratus anterior and results in primary winging most evident during sagittal plane elevation. The scapula is described as being superiorly elevated and medially translated, with the inferior pole medially rotated.
Friedenberg32 retrospectively reviewed 106 patients with either long thoracic or spinal accessory neuropathy with a mean follow-up of 48 months. They found that with conservative care 40/50 patients with long thoracic injury and 37/56 patients with spinal accessory neuropathy obtained a good outcome. A traumatic injury mechanism was associated with a poorer outcome, but electrodiagnostic findings were generally not predictive of outcome.32 With closed injuries, recovery is often spontaneous but may require up to one year. For patients in whom substantial weakness persists for longer than 6 months, procedures may be warranted. For more information on nerve injuries about the shoulder, see Chapter 57.
Examination
Evidence exists supporting the notion that altered scapular kinematics in a subset of persons may decrease the subacromial space, and that either this may therefore contribute to subacromial impingement or the altered kinematics may be a compensatory mechanism for the shoulder pathology.16,33,34 In light of this, clinicians need to be able to identify persons with scapular motion abnormalities. A scapular assessment measure should have clinical feasibility and acceptable reliability and validity. The measure should also assess dynamic, three-dimensional motion during concentric and eccentric loaded conditions, as would be present during athletics and occupational endeavors. Following is a description of existing clinical measures of scapular motion.
Two-Dimensional Tests
Lateral Scapula Slide Test and Modifications of Linear Tests
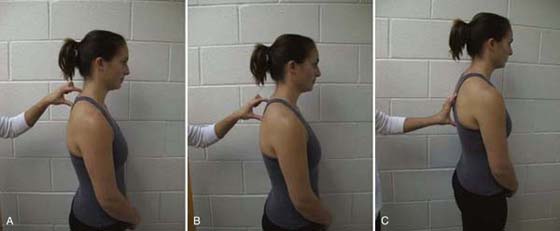
Kibler has described a measurement of scapular stability devised for use at static positions during arm elevation.35,36 The lateral scapular slide test involves taking a linear measure from the inferior angle of the scapula to the spinous process of the thoracic vertebrae and defines an “abnormality” threshold of 1.5 cm in side-to-side linear measurement difference in any of three test positions: with the arms resting at the sides, with the hands placed on the hips, and with the arms actively abducted to 90 degrees and internally rotated36 (Fig. 93-7A–C online). The reported reliability of this method was done on the actual linear measurements, not the difference in linear measures between sides at the different arm positions. Although Kibler cites a study reporting intertester reliability to be between 0.77 and 0.85, a replication of the original study found significant differences between the two testers on all Kibler measures.37 Odom et al.38 reported inter-rater intraclass correlation coefficients ranging from 0.52 to 0.66 for the measurement of scapula side-to-side differences for subjects with shoulder dysfunction and 0.75 to 0.80 for subjects without shoulder impairment. The standard error of measures sometimes exceeded the mean value of the difference. Based on these results, the value of the difference in side-to-side scapular distance measurements with this technique was not found to be reliable in determining the presence and amount of scapular asymmetry.

Figure 93-7 Lateral scapular slide test positions with linear measurement from inferior angle of scapula to thoracic spinous process A, with arms at the side; B, with hands on hips; C, with shoulders abducted to 90 degrees and internally rotated.
Other researchers have described modifications of the lateral scapular slide in the seated position,39 using overhead upper extremity positions,40 using string to measure linear distance, and additionally calculating normalized scapular abduction (the linear distance from T3 to the inferior angle of the acromion divided by the scapular size).41,42 The findings of these studies are inconsistent, but the use of a linear measure from the spinous process to a designated point on the scapula has inherent drawbacks irrespective of the reliability and validity issues. First, use of only a linear horizontal or oblique measure along the thorax does not address displacement of the scapula’s medial border or inferior angle away from the thoracic wall (winging). Additionally, in a study of 71 collegiate athletes who participated in one-arm-dominant sports, 52 of the 71 subjects exhibited a difference of at least 1.5 cm on one or more of the three positions assessed for the lateral scapular slide test.43 The calculated specificity of 26.8% in this study questions the usefulness of asymmetry as an indicator of pathology. In support of this finding, Nijs et al.44 report no association between the results of the lateral scapular slide and measures of pain and disability in a group of 29 patients diagnosed with a shoulder disorder.
SICK Scapula Rating Scale
Based on the concept of the SICK scapula (scapular malposition; inferior medial border prominence; coracoid pain and malposition; dyskinesis of scapular movement), linear measures of asymmetry have been described for use in throwers.26 With the arms by the side, three static measurements are taken: (1) infera, which is the difference between the vertical height of the superomedial angle of the inferior scapula in centimeters and that of the contralateral scapula; (2) lateral displacement, which is the difference of the horizontal distance of superomedial scapular angle from midline between the inferior scapula and the contralateral scapula; and (3) abduction, which is the difference between scapulas in angular measure of the medial scapular border from a midsagittal plumbline using a goniometer. Based on these static measurements as well as subjective complaints and other clinical examination findings, a 20-point rating scale has been devised for use as a measure of severity of symptoms. The authors acknowledge, however, that superficial landmarks have less than optimal reliability, but state that this scale is used as a qualitative measure of severity and progress assessment. A recent study performed on athletes performing repetitive overhead activities did support the assertion that static abnormalities with the arm at the side were associated with altered scapular kinematics found with dynamic movement, especially in the lower ranges of elevation.28
Visual Schemes
Although several authors45,46 recommend assessing the scapula visually and some even report statistics of abnormal scapula motion patterns,47,48 they either do not provide operational definitions or fail to substantiate their assessment methods with reliability or validity studies. Bak and Faunl48 observed scapulohumeral rhythm while standing behind competitive swimmers who were performing repeated abduction. They defined scapulothoracic instability as either scapular winging or asynchronous motion, but offer no reliability of their assessment measures. In 2004, Bulut and colleagues49 reported on the reliability of rating scapular position on 29 patients with shoulder pain. Two physical therapists rated scapula position as being either symmetrical or asymmetrical, and also described the scapula as either normal, inferior angle winging, or medial border winging. Winging was operationally defined as being able to place the finger under the respective location (inferior angle or medial border). Poor intertester reliability with κ coefficients ranging from –0.20 to 0.16 was reported for visual inspection of scapular position using this method, and rating occurred only with static shoulder position with the arms by the side.
Classification System Developed By Kibler et al
Rating during active arm elevation, operational definitions, and reliability measures are provided in a visual classification system reported by Kibler et al.,29 who define scapular dyskinesis as “the observable alterations in the position of the scapula and the patterns of scapular motion in relation to the thoracic cage.” They describe a system in which dyskinesis is categorized into three types: type I, inferior angle prominence; type II, medial border prominence; type III, translation of the scapula superiorly with prominence of the superior medial border. These categories correspond to abnormalities occurring about the three scapular axes, respectively: transverse, vertical, and perpendicular to the scapular plane. A type IV category designates normal, symmetrical scapular motion. A reliability study was undertaken using this system29 in which subjects performed frontal and scapular plane elevation while being videotaped from behind. Tapes were reviewed and rated by two physicians and two physical therapists. κ coefficients were used to measure agreement. Inter-rater reliability was 0.42 between the physical therapists and 0.31 between the physicians. Intratester reliability was 0.5. Although these values are not high enough to support the use of their system as described, the authors suggest that with refinement, reliable visual analysis of scapular dysfunction may be possible.
Scapula Dyskinesis Test
We have recently developed a visually based test to identify abnormal motion called the scapular dyskinesis test (SDT) that has demonstrated validity24 and has satisfactory reliability.50 The SDT involves viewing the exposed posterior thorax during elevation of the upper extremities in both the sagittal plane (flexion) and coronal plane (abduction) while grasping 3- to 5-pound (1.4–2.3 kg) dumbbells. Motion patterns are rated as normal, “obvious,” or “subtle” dyskinesis using the operational definitions in Box 93-1.
Box 93-1 Scapula Dyskinesis Test Operational Definitions and Rating Scale
DEFINITIONS OF TERMS
Normal scapulohumeral rhythm: Scapula is stable with minimal motion during initial 30 to 60 degrees of humerothoracic elevation, then smoothly and continuously upwardly rotates during elevation and smoothly and continuously downwardly rotates during humeral lowering with no evidence of winging.
Scapular dyskinesis: Either or both of the following motion abnormalities
Dysrhythmia: Scapula demonstrates premature or excessive elevation or protraction, non-smooth or stuttering motion during arm elevation or lowering, or rapid downward rotation during arm lowering.
Winging: There is posterior displacement of the medial border and/or inferior angle of the scapula away from the posterior thorax.
SCAPULAR DYSKINESIS RATING SCALE FOR EACH TEST MOVEMENT
N = Normal motion: no evidence of abnormality
S = Subtle abnormalities: mild/questionable evidence of abnormality, not consistently present
O = Obvious abnormalities: striking, clearly apparent abnormalities, evident on at least 3/5 trials (dysrhythmias or winging of 1 inch or greater displacement of scapula from thorax)
To determine the reliability of this system, 142 athletes competing in a collegiate sport that required repetitive overhead activity were recruited. This population was chosen due to the high incidence of shoulder pathology reported among athletes participating in sports requiring overhead arm use.52-55
To determine the reliability of this system, 142 athletes competing in a collegiate sport that required repetitive overhead activity were recruited. This population was chosen due to the high incidence of shoulder pathology reported among athletes participating in sports requiring overhead arm use.51-54 Each subject performed five repetitions of bilateral active weighted shoulder flexion (sagittal plane) and bilateral active weighted shoulder abduction (coronal plane) while they were videotaped from a posterior view. For subjects under 150 pounds (68 kg), 3-pound (1.4-kg) weights were held. For those weighing 150 pounds (68 kg) or greater, 5-pound (2.3 kg) weights were held. The test movements were based on previous pilot studies by these researchers55 and Johnson et al.56 that found that active movements with resistance resulted in abnormal scapular motion more often than static tests in subjects with shoulder pathology.
All examiners underwent standardized training via a self-instructional PowerPoint (Microscoft Corp.) presentation including operational definitions, photographs, and embedded video examples. Six raters (three separate pairs consisting of two athletic trainers and two pairs of experienced physical therapists) independently viewed randomly selected videotaped athletes and rated their shoulders as having obvious dyskinesis, subtle dyskinesis, or normal motion (Fig. 93-8A,B)

Figure 93-8 Subject performing flexion with 3-pound (1.4 kg) dumbbell. A, The scapular motion pattern was rated normal bilaterally. B, The scapular motion pattern was rated as having “obvious” dyskinesis on the left and “subtle” dyskinesis on the right.
We found moderate inter-rater reliability (average κ = 0.54 for video raters) in classifying scapular motion patterns as either normal, or having subtle or obvious dyskinesis, which is a higher κ value than reported using the Kibler method.29,57 Our system did not distinguish between subtypes of dyskinesis, as we observed that the subtypes described in the Kibler method often occurred simultaneously. The SDT also included loaded tasks, which can alter scapular kinematics.16,20,50-59 There is also evidence that muscular fatigue, which may occur with repetition, directly affects scapulohumeral rhythm and may result in compensatory increased rotation or destabilization of the scapula,60 so we feel that repetitive motion is necessary for proper evaluation.
To determine the validity of the SDT, athletes judged as having either “normal” motion or “obvious dyskinesis” underwent kinematic testing with an electromagnetic tracking system while performing weighted flexion and abduction, and the data from both groups were compared. Significant differences during arm elevation were found between the “normal” and “obvious dyskinesis” groups, with the latter group demonstrating less scapular upward rotation, less clavicular elevation, and greater clavicular protraction. These alterations have previously been associated with subacromial impingement. The suprahumeral structures, namely the rotator cuff, subacromial bursa, and long head of the biceps, probably undergo greater compression with reduced upward rotation. Kamkar and colleagues61 propose that upward rotation of scapula due to the serratus anterior activity is essential in preventing the humeral head from impinging on the acromion. The finding of less clavicular elevation in the dyskinesis group is consistent with the description of the SICK scapula syndrome, in which the scapula appears clinically as a “dropped” or lower scapula on the involved side in symptomatic throwing athletes.26 The scapulas in the dyskinesis group were more protracted than the normal group. Solem-Bertoft et al.33 found a reduction in the opening width of the subacromial space with the scapula in a protracted position compared with a retracted position using MRI. Our finding of greater protraction in those with dyskinesis may be relevant to the compression of structures within the subacromial space. The finding that shoulders visually judged as having dyskinesis have distinct alterations in three-dimensional scapular motion provides validity for the use of the SDT.
Under clinical conditions, use of the SDT is recommended using the test movements of repeated flexion and abduction, with the priority given to flexion if high irritability is encountered as this motion was more likely to evoke dyskinesis. To use this test, active elevation to at least 90 degrees is required. While these authors found that weighted shoulder was more provocative than if done without weights, there are some instances wherein using weights is not feasible due to pain or significant weakness.
Symptom Alteration Tests
The aim of symptom alteration tests is to infer that scapular pathology exists if an improvement in symptoms is found when applying manual forces to the scapula during provocation testing. The scapula assistance test described by Kibler36 is the application of a lateral and upward rotatory force to the medial border of the scapula during arm elevation to determine if symptoms of impingement were reduced or abolished. By assisting upward rotation, this test was reported to facilitate the action of the scapular rotators, primarily the serratus anterior–lower trapezius force couple, to elevate the arm and simultaneously assess the effect on pain. Reliability and validity have not been studied, but its concept provided the basis for further research regarding the potential identification of scapular pathology in those with shoulder pain.
Modified Scapula Assistance Test. Rabin30 described the modified scapula assistance test, in which posterior tilting was facilitated in addition to assisted upward rotation as described in the original scapula assistance test. This modification was based on several studies that found reduced posterior tilting in those with symptoms of shoulder impingement.2,16,34 The inter-rater reliability of the modified scapula assistance test was tested by two raters on 46 patients with shoulder pathology.30 Patients were asked to rate their pain using a typical 11-point verbal rating scale to describe their symptoms during arm elevation in the scapular and sagittal planes. Arm elevation and rating were then repeated while the tester applied a posterior tilting force with one hand by pulling back on the superior aspect of the scapula and concurrently using the heel of the hand to apply a lateral and upward rotary force to the inferior angle. A 2-point decrease in pain was considered clinically significant.62 κ values and percentage agreement for elevation in the scapular plane and sagittal plane were 0.53, 77% and 0.62, 91%, respectively, indicating moderate reliability and thus making it acceptable for clinical use. These authors recommend performing the test using the patient’s more painful arc of motion, in either the scapular or sagittal plane (Fig. 93-9).

Figure 93-9 Scapular assistance test. Clinician applies posterior tilting force through grasp on superior border of scapula and applies upward rotation force through inferior angle of scapula as subject elevates his arm.
Scapula Retraction Test. The scapula retraction test has been described as stabilization of the scapula in a retracted position on the thorax by manual application of force along the medial border of the scapula.63 Kibler et al.63 measured pain using a numeric rating scale, and elevation strength using a hand-held dynamometer during isometric shoulder elevation in the scapular plane with the scapula in its natural position and then manually retracted using the scapula reposition test. This was performed in a group of 20 patients diagnosed with shoulder pathology and in 10 asymptomatic controls. The researchers reported an increase in shoulder elevation strength using the scapula retraction test position compared to testing with the scapula in its natural “rest” position in 100% of their patients. No warm-up trials were reported, and the natural position was always tested first, so strength gains may have been due to a practice or testing-order effect instead of manual repositioning. In addition, this test was described using two examiners (one to apply the retraction and another to measure the strength using a dynamometer), which may be clinically impractical.28
Scapula Reposition Test. Smith et al.64 found decreased elevation strength with maximal scapular retraction, and these authors confirmed this finding during pilot testing. Therefore, we modified Kibler’s test63 by emphasizing posterior tilting and external rotation of the scapula but avoiding full retraction, and named it the scapula reposition test (SRT).28
The effect of the SRT on elevation strength and shoulder impingement was studied in 142 collegiate athletes who were engaged in sports requiring repetitive overhead movements.28 As part of the examination, three tests for impingement (Neer,65 Hawkins,66 and Jobe67) were performed as originally described with the scapula in its natural resting posture. If any of these tests were found to be positive for symptom provocation, the athlete was asked to rate his or her pain. Any pain-provoking test was then repeated with the scapula manually repositioned using the SRT. The SRT was performed by grasping the scapula with the fingers contacting the acromioclavicular joint anteriorly while remaining medial to the lateral acromial border. The palm and thenar eminence contact the spine of the scapula posteriorly, with the forearm obliquely angled toward the inferior angle of the scapula to provide additional support on the medial border (Fig. 93-10). This encourages scapular posterior tilting and external rotation (inferior angle and medial border moved anteriorly toward thorax) and approximates the scapula to a midposition on the thorax. As the SRT was applied, the impingement test(s) that originally provoked pain were repeated and the athlete again rated his or her pain.

Figure 93-10 Scapular reposition test. Clinician performing scapula reposition test by grasping the acromioclavicular joint superiorly and scapula posteriorly and then applying a posterior tilting and external rotation force to further approximate the scapula to the thorax. This is done during performance of the Jobe’s “empty can” test, and diminished pain or a significant increase in strength is considered a positive test result.
Isometric elevation strength in the Jobe’s test position (arm elevated to 90 degrees in the plane of the scapula and internally rotated by pointing the thumb down) was also measured using a hand-held dynamometer. Testing consisted of three repetitions of 5-second maximum isometric shoulder elevation contractions with the scapula in its natural position and also with the scapula manually repositioned using the SRT.
Almost half of the athletes had a reduction in pain during impingement testing with scapular repositioning, with a clinically significant strength gain in 26% of athletes with at least one positive shoulder impingement test, which amounted to about 10% strength increase with the SRT. Strength gains may have been facilitated simply by providing a more stable proximal fixation for the muscles such as the deltoid and rotator cuff used to perform shoulder elevation,25 or may have been the result of an improved length-tension relationship of the rotator cuff or scapular musculature secondary to an altered scapular position. A finding of increased shoulder elevation strength with scapular repositioning may provide a clinical test to identify the subset of those with shoulder pathology that may benefit from interventions designed to improve scapular musculature function.
In the clinical setting, we recommend asking for a pain rating (0–10) during resisted shoulder elevation in the Jobe’s “empty can” position with the shoulder elevated to 90 degrees in the plane of the scapula and maximally internally rotated. Manual resistance may be applied directly, or a hand-held dynamometer can be used for more objective strength assessment. The Jobe’s test should then be repeated using the SRT. A finding of a 2-point decrease in pain rating or a significant increase in strength using the SRT denotes a positive test and implies that suboptimal scapular orientation or position may be contributing to the patient’s symptoms, which suggests the need for interventions addressing the scapula.
Muscle Performance
Muscle performance is evaluated using a make test (subject uses maximal isometric force against stationary resistance) and graded as normal, reduced, or markedly reduced compared with the uninvolved extremity68 using the following operational definitions:
Normal (N): Strong, with equal resistance applied as compared bilaterally
Reduced (R): Mild to moderate deficit as compared bilaterally
Markedly Reduced (MR): Significant deficit as compared bilaterally (little to no resistance can be applied)
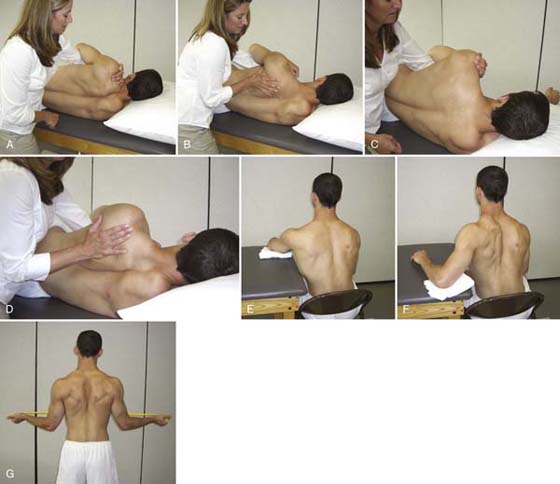
The muscles to be tested are the prime movers of the scapula, namely the serratus anterior and the lower and middle trapezius. The testing positions have been described by Kendall69 and verified electromyographically as eliciting maximal muscle activity.70,71
Middle Trapezius. The patient is prone and the shoulder is placed in a position of horizontal abduction and external rotation (thumb up) with scapula adducted toward midline. Pressure is applied against the forearm in a downward direction while the trunk is manually stabilized. Monitor the medial border of the scapula and grade on the ability to maintain scapular retraction (Fig. 93-11 online).

Figure 93-11 Manual muscle test position for the middle trapezius. Clinician applies an anteriorly directed force (toward the floor) while observing the ability of the middle trapezius to maintain retraction of the medial border of the scapula.
Lower Trapezius. The patient is prone and the arm is elevated overhead in line with the fibers of the lower trapezius with the scapula adducted. Downward resistance is applied proximal to the patient’s wrist, and the medial border of the scapula is monitored. Strength is graded based on the ability to maintain scapular retraction (Fig. 93-12 online).

Figure 93-12 Manual muscle test position for the lower trapezius. Clinician applies an anteriorly directed force (toward the floor) while observing the ability of the lower trapezius to maintain retraction of the medial border of the scapula.
Serratus Anterior. The patient is seated without back support, and the arm is flexed to 125 degrees in the sagittal plane. Resistance is applied proximal to the patient’s wrist in the direction of extending the shoulder. Monitor the inferior angle of the scapula, and grade based on ability of serratus to hold upward rotation (Fig. 93-13 online).

Figure 93-13 Manual muscle test position for the serratus anterior at 125 degrees shoulder elevation. Clinician applies an inferiorly directed force (toward the floor) while observing the ability of the serratus anterior to maintain upward rotation of the medial border of the scapula.
Posture
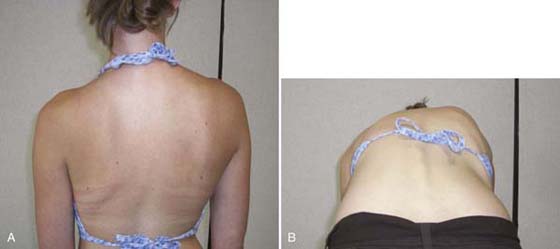
The relative height of the affected shoulder is observed from a posterior view. Although it has been stated that the dominant shoulder is often slightly lower than the nondominant shoulder,69 a significant reduction in shoulder height, especially if seen in combination with winging of the scapula, may be indicative of the SICK scapula syndrome in which the scapula appears lower on the involved side.26 Care should be taken to note if a scoliosis is present, which may produce the appearance of a dropped shoulder, which is unrelated to scapular pathology (Fig. 93-14A,B.) An “elevated scapula” has also been described as a type of impaired alignment in which the entire scapula and lateral portion of the clavicle are raised due to upper trapezius shortening.72 Superior translation of the scapula during arm elevation (see Fig. 93-3) was shown to be present in a sample of persons who had recovered from unilateral shoulder pathology (adhesive capsulitis, frozen shoulder, impingement, rotator cuff tendonitis/tear), and this could be altered by tactile and verbal cuing, which suggests a motor control issue instead of reduced muscle length in this population.13
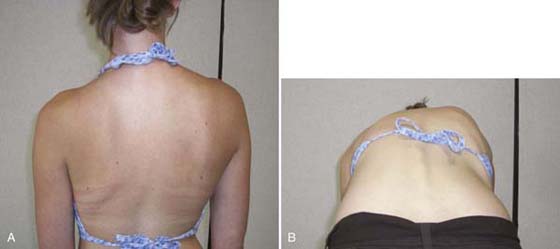
Figure 93-14 A, Asymmetry of shoulder heights is visible with the patient in erect standing position. B, With flexion a rib hump is present, confirming that the asymmetry is due to scoliosis rather than scapular pathology.
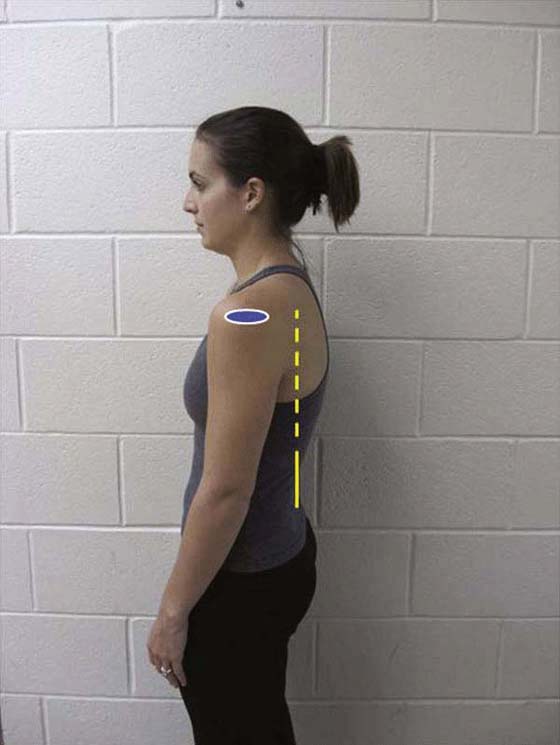
The patient should also be evaluated to determine if a forward head posture is present, as identified by the external auditory meatus being anterior to the lumbar spine. From the same sagittal view, shoulder protraction, defined as the acromion being anterior to the lumbar spine, should be noted (Fig. 93-15).69 Kyphosis is observed for the upper, middle, and lower thoracic areas while viewing the patient from the side. The following segmental groups should be assessed: C7 through T2 (cervicothoracic junction), T3 through T5, and T6 through T10. Each segmental group should be rated as having either a normal kyphosis (no deviation), diminished kyphosis (a flattening of the normal convexity), or excessive kyphosis (an increase in the normal convexity) (Fig. 93-16A–C online). A study of 80 subjects found that those with increased kyphosis and rounded shoulders were more likely to have interscapular pain, as were those with a forward head posture.73 κ values measuring inter-rater reliability for shoulder and thoracic postural observation measures as described have been reported between 0.58 and 0.9.74 In addition to spinal posture, intervertebral mobility of the cervical and thoracic spines should be assessed using spring testing (Fig. 93-17 online), and spinal flexibility should be assessed.74,75 McClure and colleagues21 failed to find a difference in thoracic resting posture between those with and without shoulder impingement syndrome, but flexibility, not static posture may be a primary issue, since mobility of the thoracic spine has been shown to vary significantly between those with healthy shoulders and those with shoulder pathology.76
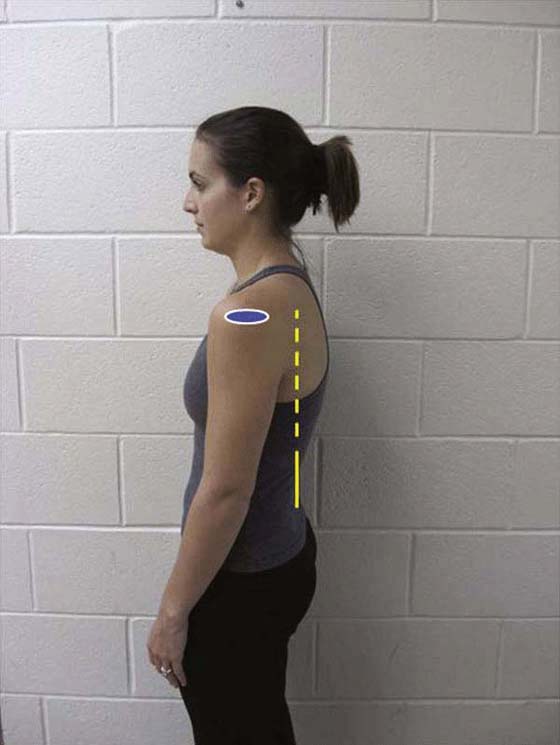
Figure 93-15 Shoulder protraction is present, indicated by acromion location anterior to apex of lumbar spine.
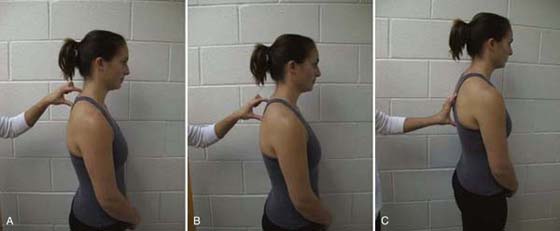
Figure 93-16 Assessment of kyphosis at (A) C7 through T2 (cervicothoracic junction), (B) T3 through T5, and (C) T6 through T10. Subject exhibits normal kyphosis at each of these segmental groups.

Figure 93-17 Assessment of intervertebral mobility using posterior-anterior glides.
Posterior Shoulder Tightness
Some authors have suggested that posterior shoulder tightness, reflected by limited glenohumeral internal rotation, is associated with scapular dysfunction.26,77 Burkhart et al.26 suggest that posterior capsular tightness may cause the scapula to rotate or protract excessively during follow-through of throwing or swinging, which involves a combination of adduction and internal rotation, and that scapular dyskinesis and tightness of the posterior capsule occur as part of a common syndrome in throwing athletes. They reported this finding in a group of symptomatic throwers, and it has been suggested that impingement of the posterior cuff may be exacerbated by scapular protraction. Borich et al.77 studied subjects involved in overhead sports with three-dimensional motion analysis and found that those with a glenohumeral internal rotation deficit had more anteriorly tilted scapulas during activities requiring arm elevation and internal rotation. Laudner et al.22 studied 11 throwing athletes diagnosed with pathologic internal impingement and compared them to asymptomatic throwers. Somewhat in contrast, they found increased clavicular elevation and increased posterior tilting in symptomatic throwers. Therefore, there does appear to be a connection between posterior shoulder tightness (limited glenohumeral internal rotation) and scapular dyskinesis; however, the precise nature of the altered scapular motion is unclear.
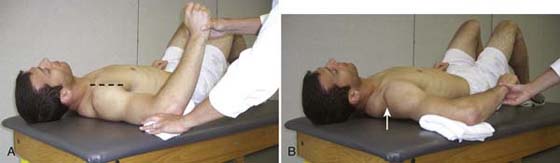
Multiple measures of posterior shoulder tightness have been reported including side-lying and seated horizontal adduction with the scapula blocked,78,79 seated horizontal adduction,80 supine internal rotation measured at 90 degrees abduction,81 and standing spinal level assessed with hand behind the back.82,83 Only modest correlations between spinal level and internal rotation at 90 degrees abduction were found (r = 0.44),84 indicating that measurements taken in these varied positions probably assess the flexibility of different portions of the posterior shoulder. Using spinal level with the hand behind the back assesses the posterior-superior capsule, while internal rotation at 90 degrees assesses the posterior-inferior capsule.85 Given this finding, we recommend that posterior shoulder tightness be assessed using both the standing spinal level and internal rotation at 90 degrees. When using the latter technique, it is critical to watch for the end of glenohumeral motion, which ends when the shoulder girdle lifts up, indicating compensatory scapulothoracic motion which may mask a glenohumeral internal rotation deficit (Fig. 93-18).
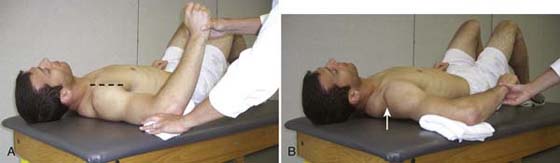
Figure 93-18 Position for goniometric ROM measurement of internal rotation as a measure of posterior capsule flexibility. A, End of glenohumeral internal rotation occurs when the shoulder begins to lift (beyond dashed line), signifying the end of glenohumeral motion. B, Incorrect positioning for goniometric internal rotation measurement allowing the scapula to lift from the plinth (arrow).
Pectoralis Minor Tightness
It has been theorized that a forward shoulder posture, defined as a change in the resting position of the scapula in the sagittal or transverse plane, may over time lead to adaptive shortening of the pectoralis minor muscle by approximating its attachment sites on the coracoid process and ribs 3, 4, and 5.69,86 Healthy subjects with a relatively shorter pectoralis minor resting length demonstrated increased internal rotation of the scapula during arm elevation and reduced posterior tilting at and above shoulder level than those with longer pectoralis minor lengths.17 As previously discussed, these alterations in scapular kinematics have been found in persons with subacromial impingement and are thought to decrease subacromial space, resulting in increased compression on the rotator cuff and long head of the biceps tendons.2,16,19 Recently, Borstad86 has provided research supporting a relationship between resting normalized pectoralis minor length, thoracic kyphosis, and scapular internal rotation, finding that those with a relatively short pectoralis minor demonstrated increased scapular internal rotation. Because this research supports a relationship between pectoral length and scapular kinematics, measurement of pectoralis minor length is recommended. The problem one encounters, however, is that the simple traditional measure reported to represent pectoral muscle length, using the distance from the posterolateral angle of the scapula to the table with the patient supine,87 has not been correlated with normalized pectoralis minor length and lacks diagnostic accuracy despite having excellent reported intrarater reliability.88 Taking a direct linear measure using either a measuring tape or vernier caliper between the medial inferior angle of the coracoid process and anterior inferior edge of rib 4 one finger-width lateral to the sternum was found to have acceptable intrarater reliability for clinical use (intraclass correlation coefficient ranged from 0.82 to 0.87 in 26 adults without a history of shoulder pathology) and was validated using comparison measures from an electromagnetic tracking device.89 Borstad89 describes palpation f these anatomic landmarks as follows: From the lateral concavity of the clavicle, palpate inferiorly in the deltopectoral groove for the medial inferior angle of the coracoid, then find the medial inferior aspect of rib 1 inferior to the sternoclavicular junction and count down to the anterior inferior edge of rib 4, one finger lateral to the sternum (Fig. 93-19) These authors have also used a PALM palpation meter (Performance Attainment Associates, St. Paul, MN) to obtain the pectoralis minor length using the same landmarks, as this device allows the clinician to circumvent other devices pressing into those with larger breast tissue. A pectoralis minor index can then be calculated by dividing the pectoralis minor length in centimeters by the person’s height in centimeters, and multiplying by 100.17 A pectoralis minor index of less than 7.44 has been reported to indicate a relatively short pectoralis minor.89

Figure 93-19 Linear measure of pectoralis minor length using tape measure from medial inferior angle of coracoid process to anterior inferior edge of rib 4 one finger-width lateral to the sternum.
Treatment
Since the etiology of scapular dysfunction appears to be multifactorial, the clinician should consider matching intervention strategies to the impairments identified during the examination process.
Muscle Strengthenin
There is strong evidence that shoulder strengthening exercise is an effective treatment for several conditions including shoulder impingement90 and shoulder instability.91 Most exercise programs for shoulder pathology should target both glenohumeral and scapulothoracic musculature, although the focus of this chapter is only scapular dysfunction.
One key principle in designing a scapular exercise program is to match the difficulty of the exercise with the patient’s level of motor control and strength. Therefore, it is important to visually observe the patient posteriorly during an exercise to assure he or she is able to maintain good scapular control. This concept is particularly important to patients who may have well-developed glenohumeral muscles (e.g., the deltoid) but poor scapular control. These patients may be able to grossly accomplish the arm motion required in the exercise but be unable to adequately control the scapula. This situation would produce excessive stress on the glenohumeral tissues and even reinforce poor motor control patterns.13 Another concept that often seems useful is to incorporate combined trunk and lower extremity movement to facilitate proper scapular motion. For example, hip and trunk extension can be combined to facilitate scapular retraction during arm extension or elevation.25,92
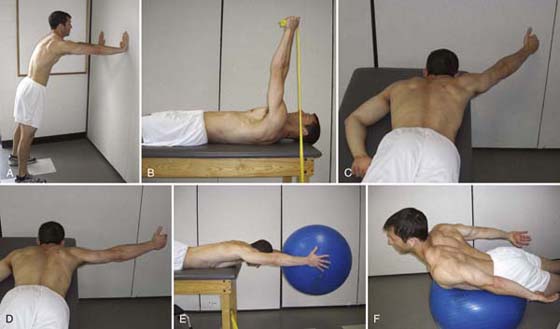
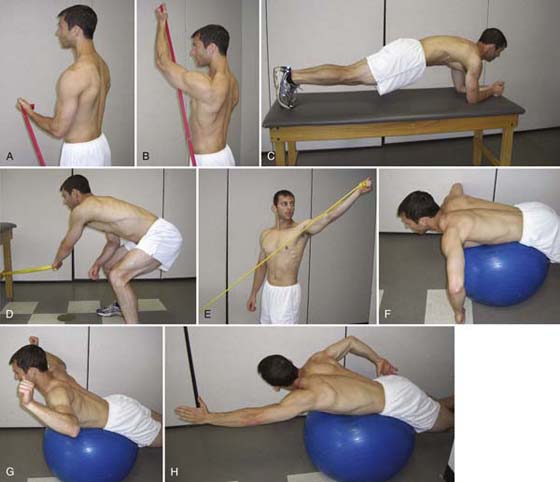
We present exercises as early (Fig. 93-20A–G online), middle (Fig. 93-21A–F online), or late (Fig. 93-22A–H online) phase. Exercises should be chosen and progressed based on the patient’s ability to control the scapula as well as consideration of the healing phase of any injured or repaired tissue. Obviously, the simple variables to alter are the load and repetitions, but the speed and complexity of the motion should also be progressed. In general, early-phase exercises should keep the shoulder in a protected midrange or nonprovocative position, while late-phase exercises will require end-range, more provocative positions.
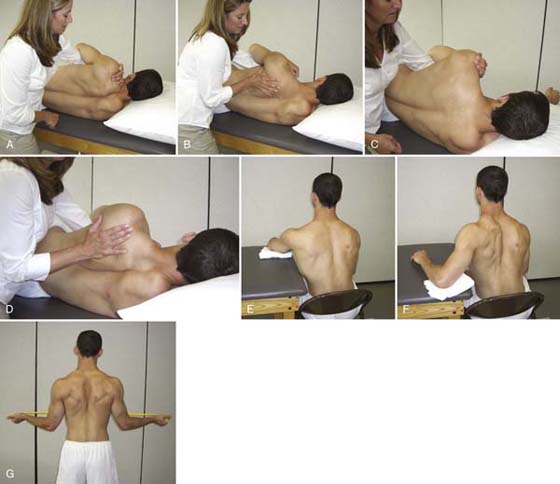
Figure 93-20 Early-phase exercises. Facilitating isolated scapula motion using tactile cuing on one side of the scapulothoracic articulation (A–D). A, Elevation; B, depression; C, protraction; D, retraction. E, Seated protraction with arm supported. F, Seated retraction with arm supported. G, Retraction with arms at side using elastic resistance.
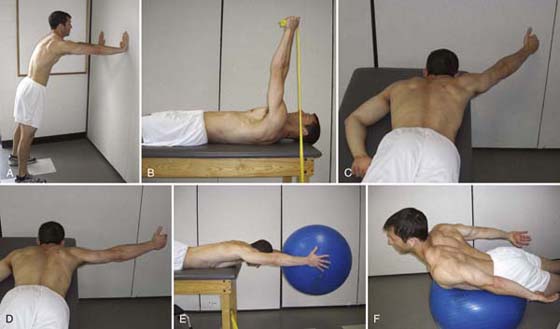
Figure 93-21 Middle-phase exercises. A, Wall with push-up plus for serratus anterior. B, Supine punch with theraband for serratus anterior. C, Prone “Y” exercise for lower trapezius with humeral external rotation (often done bilaterally). D, Prone “T” exercise for middle trapezius with humeral external rotation (often done bilaterally). E, Prone elevation holding ball encourages co-contraction with subscapularis and scapular retraction. F, Isolated thoracic extension on ball.
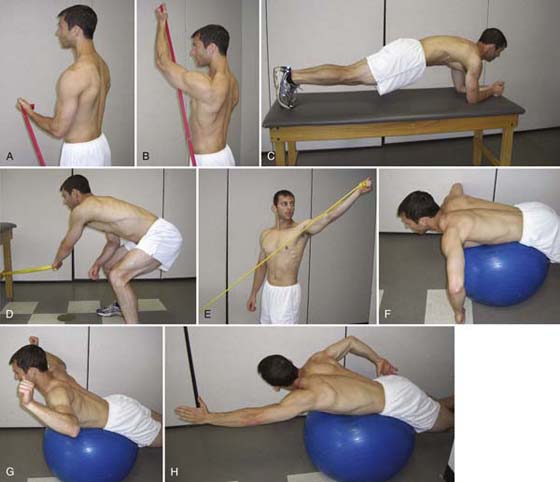
Figure 93-22 Late-phase exercises. A, Start position for flexion and external rotation for serratus anterior. B, End position for flexion and external rotation for serratus anterior. C, Prone plank position with protraction “plus” for serratus anterior. D, Start position for “lawnmower” exercise. E, End position for “lawnmower” exercise incorporating hip and spine extension, trunk rotation, shoulder elevation, external rotation, and retraction. F, Start position for “goalpost” exercise. G, End position for “goalpost” exercise incorporating thoracic extension, shoulder external rotation and retraction. H, “Swimmer” exercise incorporating thoracic extension and rotation with reciprocal arm motions.
Taping/Bracing
Although there are few studies addressing the efficacy of shoulder taping, two case studies of patients with clinical symptoms of shoulder impingement have described the use of scapular repositioning as a diagnostic tool that reduced patients’ symptoms.93,94 Subsequent use of scapular taping was effective in symptom reduction and was used as part of a comprehensive intervention program. Additional studies have investigated the effect of shoulder taping in healthy subjects,95,96 professional musicians,96 and in persons with subacromial impingement.96,98 Although taping did not produce significant electromyographic changes in the scapular muscles of those with healthy shoulders,99 it was successful in altering electromyographic activity of the scapular musculature in both symptomatic swimmers102 and professional violinists, half of whom were experiencing pain.97 Taping has been effective in reducing thoracic kyphosis96,100 as well as increasing shoulder elevation and pain-free elevation range of motion (ROM) in the sagittal plane and in the plane of the scapula.100 These findings are consistent with those of Kebaetse,101 who also reported increased shoulder elevation motion and a change in scapular position in the erect compared to the slouched postures. Concomitant with enhanced ROM was increased elevation force at 90 degrees in the erect-posture condition. This would logically lead one to believe that in symptomatic individuals with suboptimal scapulothoracic posture or motion, scapular taping may be an effective adjunct to enhance motor performance or reduce pain in a functional range of elevation. Taping has been described as “an adjunctive therapy to attempt to attain a more favorable scapular alignment and alleviate pain,”94 and proposed mechanisms of action include improved scapular alignment, providing a low load–long duration stretch to tight structures about the shoulder, increased subacromial space, reduced tension in the subacromial tissues,94 improved proprioception,102 and improvement of joint positional faults.103
If either postural correction or the SRT reduces symptoms, scapular taping should be considered in the patient who either has difficulty maintaining an optimal posture or requires a stretch to the anterior shoulder, or in those who are unable to exercise without pain. The following procedure is a modification of the postural taping technique described by Greig in 2007.100 The modification allows additional approximation force over the inferior angle of the scapula to the thorax. Taping may be applied unilaterally or bilaterally, although these authors recommend bilateral taping to enhance thoracic spine extension (Fig. 93-23). Box 93-2 provides directions for the bilateral taping method.

Figure 93-23 Scapular taping with cover roll stretch applied beneath Leukotape (ERP Group, Laval, QC, Canada).
Box 93-2 Directions for Bilateral Taping of the Scapula
• Patient should be seated and asked to “elongate the crown of the head toward the ceiling and gently draw shoulder blades down and together.”102
• A 2-inch-width cover roll stretch (Beiersdorf-Jobst Inc., Charlotte, North Carolina) should be used to protect the patient’s skin and will be applied without tension from the anterior aspect of acromion and acromioclavicular joint superiorly across the upper trapezius and angled toward the inferior angle of the scapula crossing the spine at approximately T8–T9 and ending on the contralateral thorax.
• Leukotape (Beiersdorf-Jobst Inc., Charlotte, North Carolina) should be anchored anteriorly and held firmly by the examiner’s thumb while the tape is firmly pulled superiorly and then diagonally across the inferior angle of the scapula to the contralateral thorax on top of the cover roll stretch. The tape should remain medial to the lateral border of the acromion proximally to maintain a more vertical orientation and avoid altering the position of the humerus relative to the glenoid.
• It is important to instruct another person on tape removal by gently lifting the edge of the tape and carefully pressing down on the skin to detach it. Patients should not remove their own tape.
The Spine and Scapula Stabilizing brace or S3 (Alignmed Inc., Santa Ana, CA) appears to work in a similar fashion as taping, but should provide improved wearing tolerance over extended time periods due to the lack of adhesive contact with the skin (Fig. 93-24A,B). An initial study104 of 15 subjects reported to have shoulder injuries with scapular dyskinesis and 15 healthy subjects assessed scapular kinematics using an electromagnetic tracking system during shoulder elevation with and without the S3 brace. Small (2–4 degrees) but statistically significant changes were found at rest and primarily during the early ranges of arm elevation. It is unknown whether the magnitude of reduced scapular internal rotation and increased posterior tilting detected while wearing the S3 are clinically significant. Although the S3 website references data report significant increases in internal and external rotation strength in the scapular plane while wearing the S3 as compared with not wearing the brace, no peer-reviewed studies are available at this time. Anecdotally, these authors have had favorable clinical experience using the S3 brace with patients, but further research should be done to determine widespread clinical efficacy.

Figure 93-24 Spine and Scapula Stabilizing Brace incorporates a mesh fitted vest and adjustable Velcro straps (S3) by Alignmed, Inc. A, Anterior view; B, posterior view.
Stretching
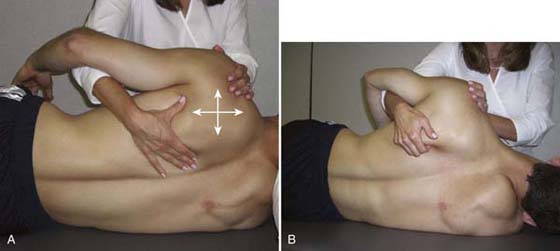
In patients with tight periscapular musculature or status post trauma or immobilization, limitations in scapulothoracic motion should be addressed using superior, inferior, medial, or lateral gliding or scapulothoracic distraction techniques (Fig. 93-25A,B). Facilitatory techniques may be used in the early phase of rehabilitation programs in conjunction with scapular mobilization to promote isolated active scapular motion (see Fig. 93-20A–D online).
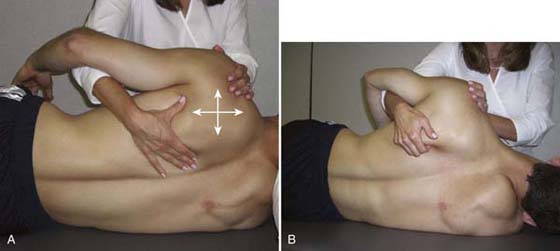
Figure 93-25 Scapulothoracic mobilization. A, Arrow indicates that scapula can be mobilized in superior, inferior, medial, and lateral directions. B, Scapulothoracic distraction.
In addressing any loss of glenohumeral mobility in a patient with upper extremity symptoms, particular attention should be given to tightness of the posterior shoulder musculature, as this may affect scapular kinematics,105,106 and adequate flexibility of the posterior capsule has been recommended before the initiation of a shoulder strengthening program. Several methods of self-stretching have been described, including: “cross-body stretch,” wherein the shoulder is elevated to approximately 90 degrees of flexion and pulled across the body into horizontal adduction with the opposite arm (Fig. 93-26)107; the “towel stretch,” wherein the glenohumeral joint is adducted, internally rotated, and extended while the hand now located behind the individual’s back is pulled up by the opposite hand using a towel107,108; a “sleeper stretch” that is accomplished by lying on the side to be stretched, elevating the humerus to 90 degrees on the support surface, then passively internally rotating the shoulder with the opposite arm (Fig. 93-27).26,109,110 A randomized study by McClure and colleagues84 found that in healthy subjects with limited internal rotation, the cross-body adduction method produced significant gains in internal rotation ROM after a 4-week intervention program of five 30-second stretches daily, whereas the sleeper stretch did not produce significant changes. For use in the clinic, manually assisted stretching techniques have been described in which the clinician manually stabilizes the scapula while the shoulder is passively adducted or internally rotated or performs anterior to posterior glides to stretch the posterior capsule (Fig. 93-28A,B).111 Postural exercises and mobilization techniques to facilitate cervical retraction and thoracic extension have also been described to improve shoulder elevation ROM96 (Fig. 93-29A–E online). Stretching of the pectoralis minor is also recommended so as to improve scapular kinematics during arm elevation, and Borstad and Ludewig have used an electromagnetic motion tracking system and found that the unilateral corner stretch was most effective in elongating the pectoralis minor followed by a manual stretch supine with a towel roll vertically placed over the thoracic spine (Fig. 93-29A online).112 As a modification of the latter technique, these authors have additionally stabilized the lower ribs while applying downward pressure over the coracoid process (Fig. 93-30A,B).

Figure 93-26 Cross-body stretch.

Figure 93-27 Sleeper stretch.

Figure 93-28 A, Manual horizontal adduction stretch with scapula blocked. B, Anterior-posterior glide to stretch the posterior capsule of the glenohumeral joint.

Figure 93-29 Exercises to promote cervical and thoracic extension. A, Cervical retraction with self-tactile cueing on sternum to promote thoracic extension. B, Cervical retraction with manual overpressure. C, Self thoracic extension over chair. D, Thoracic mobilization using posterior-anterior glide with contact of pisiforms adjacent to thoracic spinous process. E, Thoracic mobilization using posterior-anterior glide with contact of right pisiform on thoracic spinous process. Left fifth digit hooks over right index finger to apply overpressure. F, Upper thoracic manipulation using distraction technique.

Figure 93-30 A, Pectoralis minor corner stretch. B, Manual pectoralis minor stretch with ribs stabilized and posteriorly directed pressure over coracoid.
Summary
Scapular dysfunction is a common clinical problem with many upper quarter conditions, especially the shoulder. The scapula provides a stable base for glenohumeral function and upper extremity function. Therapists should examine for abnormalities in scapular motion and position to identify impairments in muscle performance and muscle length that create a suboptimal environment for scapular function. Recently, examination tools have been developed to assist therapists with their assessment of the scapula. Additional research is needed to establish the clinical utility of these examination techniques, but current evidence suggests some useful therapeutic strategies to help resolve scapular dysfunction. Box 93-3, available on the companion website, provides a review of the clinical guidelines presented in this chapter.
Box 93-3 Recommended Guidelines for Examination and Management of Scapular Dysfunction
EXAMINATION
Visual Classification using the Scapula Dyskinesis Test
• Active flexion with 3-pound [1.37 kg; persons weighing < 150 pounds (68 kg)] or 5-pound (2.3 kg; persons weighing > 150 pounds) dumbbells, if able
• Active abduction (coronal plane) with 3-pound or 5-pound dumbbells as above, if able
• Rate as having
• Normal motion
• Subtle dyskinesis (inconsistent winging or dysrhythmia)
• Obvious dyskinesis (obvious, consistent winging, or dysrhythmia)
Symptom Alteration Tests
• Modified scapula assistance test
• Perform active arm elevation (sagittal or scapular plane) with pain rating using numeric rating scale (0 to 10).
• Apply a posterior tilting force with one hand by pulling back on the superior aspect of the scapula, and concurrently use the heel of the hand to apply an upward rotary force to the inferior angle. Reassess elevation ROM and pain.
• Scapula reposition test
• Perform Jobe’s (empty can) test by isometrically resisting arm elevation in the scapular plane with the shoulder maximally internally rotated. Obtain pain rating using numeric rating scale (0–10).
• Lower arm and then reposition scapula using the scapula reposition test by grasping the scapula medial to the acromion with forearm providing additional support obliquely over thorax to encourage posterior tilting and external rotation. Perform Jobe’s test again to determine whether there is a decrease in pain or an increase in strength.
Muscle Performance
• Lower trapezius
• Middle trapezius
• Serratus anterior
Examination of Related Areas
• Pectoralis minor length
• Thoracic kyphosis/flexibility
• Posterior capsular flexibility of the glenohumeral joint
TREATMENT PRINCIPLES
Muscle Strengthening
• Difficulty is matched to patient’s motor control and strength based on direct visualization of scapular control.
• Progress from protected midrange positions with arm supported or low resistance to end-range positions against gravity and resistance.
• Incorporate related areas such as hip and trunk during functional exercises.
Taping and Bracing
• Consider this alternative in patients whose symptoms are reduced with either postural correction or the scapula reposition test.
Stretching
• Pectoralis minor
• Posterior glenohumeral joint
• Posterior gliding, cross-body adduction, sleeper stretch, towel stretch
• Cervical retraction-upper thoracic extension program
REFERENCES
1. Ludewig PM, Cook TM, Nawoczenski DA. Three-dimensional scapular orientation and muscle activity at selected positions of humeral elevation. J Orthop Sports Phys Ther. 1996;24(2):57–65.
2. Lukasiewicz AC, McClure P, Michener L, et al. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29(10):574–586.
3. Wu G, van der Helm FC, Veeger HE, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion–Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981–992.
4. McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10(3):269–277.
5. Bagg SD, Forrest WJ. Electromyographic study of the scapular rotators during arm abduction in the scapular plane. Am J Phys Med. 1986;65(3):111–124.
6. Kronberg M, Nemeth G, Broström L-Å. Muscle activity and coordination in the normal shoulder. Clin Orthop Rel Res. 1990 August;257:76–85.
7. Kuhn JE, Plancher KD, Hawkins RJ. Scapular winging. J Am Acad Orthop Surg. 1995;3(6):319–325.
8. Johnson G, Bogduk N, Nowitzke A, House D. Anatomy and actions of the trapezius muscle. Clin Biomech. 1994;9:44–50.
9. Scibek JS, Mell AG, Downie BK, et al. Shoulder kinematics in patients with full-thickness rotator cuff tears after a subacromial injection. J Shoulder Elbow Surg. 2008;17(1):172–181.
10. Paletta GA, Warner JJ, Warren RF, et al. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6:516–527.
11. Yamaguchi K, Sher JS, Andersen WK, et al. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9(1):6–11.
12. Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. J Electromyogr Kinesiol. 2006;16(3):224–235.
13. Babyar SR. Excessive scapular motion in individuals recovering from painful and stiff shoulders: causes and treatment strategies. Phys Ther. 1996;76(3):226–238. discussion 239-247
14. Jia X, Ji JH, Petersen SA, et al. Clinical evaluation of the shoulder shrug sign. Clin Orthop. 2008 Nov;466(11):2813–2819.
15. Kelly BT, Williams RJ, Cordasco FA, et al. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. J Shoulder Elbow Surg. 2005;14(2):165–171.
16. Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276–291.
17. Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35(4):227–238.
18. Graichen H, Stammberger T, Bonél H, et al. Three-dimensional analysis of shoulder girdle and supraspinatus motion patterns in patients with impingement syndrome. J Orthop Res. 2001;19(6):1192–1198.
19. Hebert LJ, Moffet H, McFadyen BJ, Dionne CE. Scapular behavior in shoulder impingement syndrome. Arch Phys Med Rehabil. 2002;83(1):60–69.
20. Warner JJ, Micheli LJ, Arslanian LE, et al. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moire topographic analysis. Clin Orthop. 1992;285:191–199.
21. McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86(8):1075–1090.
22. Laudner KG, Myers JB, Pasquale MR, et al. Scapular dysfunction in throwers with pathologic internal impingement. J Orthop Sports Phys Ther. 2006;36(7):485–494.
23. Endo K, Ikata T, Katoh S, Takeda Y. Radiographic assessment of scapular rotational tilt in chronic shoulder impingement syndrome. J Orthop Sci. 2001;6(1):3–10.
24. Tate AR, McClure P, Kareha S, et al. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165–173. Mar–Apr Mar–Apr
25. Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11(2):142–151.
26. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641–661.
27. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology, part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420.
28. Tate AR, McClure PW, Kareha S, Irwin D. Effect of the Scapula Reposition Test on shoulder impingement symptoms and elevation strength in overhead athletes. J Orthop Sports Phys Ther. 2008;38(1):4–11.
29. Kibler WB, Uhl TL, Maddux JW, et al. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11(6):550–556.
30. Rabin A, Irrgang JJ, Fitzgerald GK, Eubanks A. The intertester reliability of the Scapular Assistance Test. J Orthop Sports Phys Ther. 2006;36(9):653–660.
31. Wright TA. Accessory spinal nerve injury. Clin Orthop Relat Res. 1975 May;108:15–18.
32. Friedenberg SM, Zimprich T, Harper CM. The natural history of long thoracic and spinal accessory neuropathies. Muscle Nerve. 2002;25(4):535–539.
33. Solem-Bertoft E, Thuomas KA, Westerberg CE. The influence of scapular retraction and protraction on the width of the subacromial space. An MRI study. Clin Orthop Relat Res. 1993;296:99–103.
34. Graichen H, Bonel H, Stammberger T, et al. Three-dimensional analysis of the width of the subacromial space in healthy subjects and patients with impingement syndrome. AJR Am J Roentgenol. 1999;172(4):1081–1086.
35. Kibler WB. Role of the scapula in the overhead throwing motion. Contem Orthop. 1991;22:525–532.
36. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325–337.
37. Gibson MH, Goebel GV, Jordan TM, et al. A reliability study of measurement techniques to determine static scapular position. J Orthop Sports Phys Ther. 1995;21(2):100–106.
38. Odom CJ, Taylor AB, Hurd CE, Denegar CR. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the Lateral Scapular Slide Test: a reliability and validity study. Phys Ther. 2001;81(2):799–809.
39. T’Jonck L, Lysens R, Grasse G. Measurements of scapular position and rotation: a reliability study. Physiother Res Int. 1996;1(3):148–158.
40. Davies GJ, Dickoff-Hoffman S. Neuromuscular testing and rehabilitation of the shoulder complex. J Orthop Sports Phys Ther. 1993;18(2):449–458.
41. DiVeta J, Walker ML, Skibinski B. Relationship between performance of selected scapular muscles and scapular abduction in standing subjects. Phys Ther. 1990;70(8):470–476. discussion 476-479
42. Neiers L, Worrell TW. Assessment of Scapular Position. J Sports Rehab. 1993;2:20–25.
43. Koslow PA, Prosser LA, Strony GA, et al. Specificity of the lateral scapular slide test in asymptomatic competitive athletes. J Orthop Sports Phys Ther. 2003;33(6):331–336.
44. Nijs J, Roussel N, Vermeulen K, Souvereyns G. Scapular positioning in patients with shoulder pain: a study examining the reliability and clinical importance of 3 clinical tests. Arch Phys Med Rehabil. 2005;86(7):1349–1355.
45. Paine RM, Voight M. The role of the scapula. J Orthop Sports Phys Ther. 1993;18(1):386–391.
46. Ellen MI, Gilhool JJ, Rogers DP. Scapular instability. The scapulothoracic joint. Phys Med Rehabil Clin N Am. 2000;11(4):755–770.
47. Rupp S, Berninger K, Hopf T. Shoulder problems in high level swimmers–impingement, anterior instability, muscular imbalance? Int J Sports Med. 1995;16(8):557–562.
48. Bak K, Faunl P. Clinical findings in competitive swimmers with shoulder pain. Am J Sports Med. 1997;25(2):254–260.
49. Bulut I, Fitzgerald GK, Irrgang JJ. Reliability of measuring shoulder range of motion, strength and scapular position. J Orthop Sports Phys Ther. 2004;34:A14.
50. McClure P, Tate AR, Kareha S, et al. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009 Mar-Apr;44(2):160–164.
51. Lo YP, Hsu YC, Chan KM. Epidemiology of shoulder impingement in upper arm sports events. Br J Sports Med. 1990;24(3):173–177.
52. McMaster WC, Troup J. A survey of interfering shoulder pain in United States competitive swimmers. Am J Sports Med. 1993;21(1):67–70.
53. Soldatis JJ, Moseley JB, Etminan M. Shoulder symptoms in healthy athletes: a comparison of outcome scoring systems. J Shoulder Elbow Surg. 1997;6(3):265–271.
54. Wang HK, Cochrane T. A descriptive epidemiological study of shoulder injury in top level English male volleyball players. Int J Sports Med. 2001;22(2):159–163.
55. Tate A, McClure P, Neff N. Validity of a visual classification system for scapular motion. J Orth Sport Phys Ther. 2004;34:A42.
56. Johnson M. Development of a model to classify scapular motion: a pilot study. In: Pennsylvania Physical Therapy Association: Annual Conference. Pennsylvania: Seven Springs; 2001.
57. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174.
58. McQuade KJ, Smidt GL. Dynamic scapulohumeral rhythm: the effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther. 1998;27(2):125–133.
59. Doody SG, Freedman L, Waterland JC. Shoulder movements during abduction in the scapular plane. Arch Phys Med Rehabil. 1970;51:595–604.
60. McQuade KJ, Dawson J, Smidt GL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. J Orthop Sports Phys Ther. 1998;28(2):74–80.
61. Kamkar A, Irrgang JJ, Whitney SL. Nonoperative management of secondary shoulder impingement syndrome. J Orthop Sports Phys Ther. 1993;17(5):212–224.
62. Farrar JT, Young JP Jr, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158.
63. Kibler WB, Sciascia A, Dome D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med. 2006;34(10):1643–1647.
64. Smith J, Kotajarvi BR, Padgett DJ, Eischen JJ. Effect of scapular protraction and retraction on isometric shoulder elevation strength. Arch Phys Med Rehabil. 2002;83(3):367–370.
65. Neer CS 2nd, Welsh RP. The shoulder in sports. Orthop Clin North Am. 1977;8(3):583–591.
66. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8(3):151–158.
67. Jobe FW, Jobe CM. Painful athletic injuries of the shoulder. Clin Orthop. 1983 March;173:117–124.
68. Wainner RS, Fritz JM, Irrgang JJ, et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28(1):52–62.
69. Kendall F, McCreary EK, Provance PG. Muscles Testing and Function. Baltimore, MD: Williams and Wilkins; 1993.
70. Michener LA, Boardman ND, Pidcoe PE, Frith AM. Scapular muscle tests in subjects with shoulder pain and functional loss: reliability and construct validity. Phys Ther. 2005;85(11):1128–1138.
71. Ekstrom RA, Donatelli RA, Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003;33(5):247–258.
72. Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis, MO: Mosby; 2001.
73. Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther. 1992;72(6):425–431.
74. Cleland JA, Childs JD, Fritz JM, Whitman JM. Interrater reliability of the history and physical examination in patients with mechanical neck pain. Arch Phys Med Rehabil. 2006;87(10):1388–1395.
75. Maitland GD. Maitland’s Vertebral Manipulation. In: Maitland GD, Hengeveld E, Banks K, eds., et al. 6th ed Butterworth-Heinemann; 2001.
76. Meurer A, Grober J, Betz U, et al. [BWS-mobility in patients with an impingement syndrome compared to healthy subjects—an inclinometric study]. Z Orthop Ihre Grenzgeb. 2004;142(4):415–420.
77. Borich M, Bright JM, Lorello DJ, et al. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. J Orthop Sports Physi Ther. 2006;36(12):926–934.
78. Tyler TF, Roy T, Nicholas SJ, Gleim GW. Reliability and validity of a new method of measuring posterior shoulder tightness. J Orthop Sports Phys Ther. 1999;29:262–274.
79. Myers JB, Oyama S, Wassinger CA, et al. Reliability, precision, accuracy, and validity of posterior shoulder tightness assessment in overhead athletes. Am J Sports Med. 2007;35:1922–1930.
80. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352.
81. Awan R, Smith J, Boon AJ. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. 2002;83:1229–1234.
82. Mallon WJ, Herring CL, Sallay PI, et al. Use of vertebral levels to measure presumed internal rotation at the shoulder: a radiographic analysis. J Shoulder Elbow Surg. 1996 Jul-Aug;5(4):299–306.
83. Edwards TB, Bostick RD, Greene CC, et al. Interobserver and intraobserver reliability of the measurement of shoulder internal rotation by vertebral level. J Shoulder Elbow Surg. 2002 Jan-Feb;11(1):40–42.
84. McClure P, Balaicuis J, Heiland D, et al. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther. 2007;37(3):108–114.
85. Gerber C, Werner CM, Macy JC, et al. Effect of selective capsulorrhaphy on the passive range of motion of the glenohumeral joint. J Bone Joint Surg Am. 2003;85-A(1):48–55.
86. Borstad JD. Resting position variables at the shoulder: evidence to support a posture-impairment association. Phys Ther. 2006;86(4):549–557.
87. Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis, MO: Mosby; 2002.
88. Lewis JS, Valentine RE. The pectoralis minor length test: a study of the intra-rater reliability and diagnostic accuracy in subjects with and without shoulder symptoms. BMC Musculoskelet Disord. 2007;8:64.
89. Borstad JD. Measurement of pectoralis minor muscle length: validation and clinical application. J Orthop Sports Phys Ther. 2008;38(4):169–174.
90. Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. J Hand Ther. 2004;17(2):152–164.
91. Burkhead WZ Jr, Rockwood CA Jr. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74(6):890–896.
92. Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36(3):189–198.
93. Schmitt L, Snyder-Mackler L. Role of scapular stabilizers in etiology and treatment of impingement syndrome. J Orthop Sports Phys Ther. 1999;29(1):31–38.
94. Host HH. Scapular taping in the treatment of anterior shoulder impingement. Phys Ther. 1995;75(9):803–812.
95. Cools AM, Witvrouw EE, Danneels LA, Cambier DC. Does taping influence electromyographic muscle activity in the scapular rotators in healthy shoulders? Man Ther. 2002;7(3):154–162.
96. Lewis JS, Wright C, Green A. Subacromial impingement syndrome: the effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35(2):72–87.
97. Ackermann B, Adams R, Marshall E. The effect of scapula taping on electromyographic activity and musical performance in professional violinists. Aust J Physiother. 2002;48(3):197–203.
98. Smith MJ, Sparkes V. The immediate effect of scapular taping on electromyographic activity of the scapular rotators in swimmers with subacromial impingement symptoms. In: Physical Therapy in Sport International Conference: Enhancing Recovery and Performance in Sport. Birmingham, UK: Elsevier; 2006.
99. Cools AM, Witvrouw EE, Declercq GA, et al. Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med. 2003;31(4):542–549.
100. Greig AM, Bennell KL, Briggs AM, Hodges PW. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man Ther. 2008 Jun;13(3):249–257.
101. Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80(8):945–950.
102. Robbins S, Waked E, Rappel R. Ankle taping improves proprioception before and after exercise in young men. Br J Sports Med. 1995;29(4):242–247.
103. Mulligan B. Manual Therapy “NAGS”, “SNAGS”, “MWMS” etc. 5th ed Wellington, New Zealand: Plane View Press; 1995.
104. Uhl TL, Kibler WB, Tripp BL, et al. The effectiveness of a scapular brace on scapular kinematics. In: American Society of Shoulder and Elbow Therapists Annual Conference. Palm Beach, FL; 2005.
105. Maitland GD. Peripheral Manipulation. 2nd ed London: Butterworths; 1983.
106. Cook CE. Orthopedic Manual Therapy. Upper Saddle River, New Jersey: Pearson Education, Inc.; 2007.
107. Bandy WD, Sanders B. Therapeutic Exercise: Techniques for Intervention. Baltimore, MD: Lippincott Williams & Wilkins; 2001.
108. McClure PW, Bialker J, Neff N, et al. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther. 2004;84(9):832–848.
109. Weldon EJ 3rd, Richardson AB. Upper extremity overuse injuries in swimming. A discussion of swimmer’s shoulder. Clin Sports Med. 2001;20(3):423–438.
110. Bach HG, Goldberg BA. Posterior capsular contracture of the shoulder. J Am Acad Orthop Surg. 2006;14(5):265–277.
111. Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30(1):136–151.
112. Borstad JD, Ludewig PM. Comparison of three stretches for the pectoralis minor muscle. J Shoulder Elbow Surg. 2006;15(3):324–330.