Chapter 6 Extraspinal Techniques
Role of the peripheral joints
From the beginnings of chiropractic, practitioners have treated the nonspinal joints. D.D. Palmer1 described his treatment of the feet in 1910. Applying manual procedures to the peripheral joints is a skill that is taught in all accredited chiropractic programs.
The extremity joints are lever-hinge complexes that translate forces into motion, but in so doing, can also amplify forces negatively to the neuromusculoskeletal (NMS) system. The mechanical principles that determine what functions the body can perform are the same, regardless of the activity, whether it’s an athletic, recreational, occupational, or everyday task.
Understanding biomechanics (the application of mechanical laws to living structures) is paramount when confronted with a clinical dysfunctional process affecting the musculoskeletal system and, specifically, a peripheral joint. The joint, its ligamentous structures, and its capsule form the hinge for the bony lever to move about when a force from the muscles is provided. Proper joint function depends on the integrity of the soft tissues and the alignment of the bony joint surfaces.
By incorporating biomechanical principles in clinical practice, the chiropractor will better understand the nature and extent of the manipulable lesion, as well as the way the patient’s NMS system is influenced locally and globally. Moreover, mechanisms for the dysfunctional changes will become apparent, as will the extent and effect of the patient’s adaptational process.
Impairments involving the muscles, ligaments, and joints of the extremities can significantly reduce the quality or the ease of performing many important activities related to personal care, livelihood, and recreation. The rationale for treating peripheral joints includes correction of biomechanical problems and reflex-triggered functional syndromes.2 Biomechanical problems are characterized primarily by joint pain, but swelling and paresthesia may be present. These problems may be the result of trauma (sprains, strains, athletic injuries, or work injuries) or repetitive activities and postures (carpal tunnel syndrome, plantar fasciitis, or foot pronation). Reflex-triggered functional syndromes occur through a series of distortions affecting the kinetic chain. They are a result of mechanical deficiencies (short leg) or muscular insufficiencies or deformities (valgus or varus). These problems present as clinical findings associated with specific areas of the body, but the major dysfunctions are located somewhere else. For example, a patient may have acute or recurrent low back pain that appears to be localized to the sacroiliac joints, but treatment to the sacroiliac joints is ineffective. On further examination, a dysfunctional metatarsal joint is found that disturbs normal proprioceptive function, leading to sacroiliac changes.
As is the case with manual procedures applied to the spine, a detailed examination must be conducted to determine the necessity for care and the type of procedures to be applied to the peripheral joints. In addition to joint manipulation and adjustment to the peripheral joints, consideration should be given to the use of soft tissue procedures, hot and cold modalities, stretching exercises, rehabilitation, taping and supports, and orthotics.
It is necessary to assign a clear and specific name to each technique procedure for teaching and testing purposes. The adjustive techniques in this chapter have been given names that are based on the involved joint or region, patient position, contact used by the clinician, body part contacted, and any necessary additional information (e.g., push, pull, with distraction, etc.), as well as the induced joint movement. These names follow the patterns used by the U.S. National Board of Chiropractic Examiners and are designed to be helpful in the teaching and testing for competence of the procedures.
Temporomandibular joint
The weight of the head must be balanced and stabilized atop the spine. A biomechanical relationship exists between the forces developed in stabilization of the cervical spinal segments, tension in the deep cervical fascia, movements of the temporomandibular joints (TMJs), and activity of the hyoid bone muscles, as well as the structures of the shoulder girdle (Figure 6-1). More importantly, postural stresses, muscle tone, malocclusion of the teeth, and joint dysfunction have clinical relationships with neck pain, headache, orofacial pain, and abnormalities of chewing and swallowing. An association is formed between two of the body’s most complicated joint systems—the TMJ and the atlanto-occipital joint. Both of these joint systems should be evaluated in patients complaining of head and neck pain.
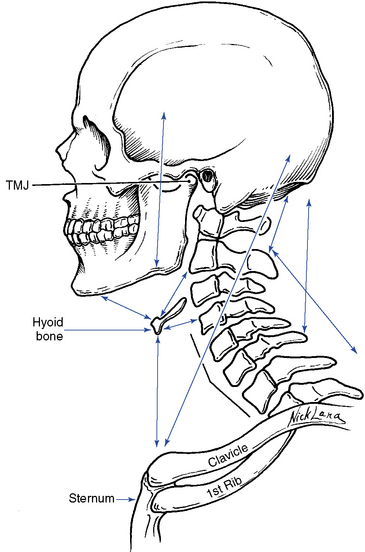
Figure 6-1 Biomechanical relationship necessary to stabilize the head and the cervical spine segments. Arrows indicate direction of muscle pull.
(Modified from Grieve G: Common vertebral joint problems, ed 2, Edinburgh, 1988, Churchill Livingstone.)
The craniomandibular complex is composed of the TMJ, the teeth, muscles of mastication, and the hyoid bone. The TMJ is one of the most active joints in the body, moving more than 2000 times per day in its functions of mastication, swallowing, respiration, and speech. The head is tethered to the body by the muscles that move the TMJ and the atlanto-occipital joint. Head posture depends on the tone of these muscles, thus developing an intimate association between movements of the head and mandible. Because of this relationship, a change in either cervical spine posture, head posture, or mandibular rest position can create a change in the others.
Functional anatomy
Osseous Structures
The mandible, the largest and strongest bone of the face, articulates with the temporal bones while accommodating the lower teeth (Figure 6-2). The body of the mandible runs horizontally and has two posterior rami. The rami are perpendicular to the body and form an inferior palpable angle. Each ramus has two processes: the coronoid process, serving as a point of attachment for muscles, and the condylar process, for articulation with the temporal bone via the intra-articular disc. Lines drawn through the axis of each condyle intersect just anterior to the foramen magnum, the significance of which is in visualizing a line of correction for manipulative procedures (Figure 6-3). The temporal bone has a concave mandibular fossa, with the convex articular eminence just anterior to it.
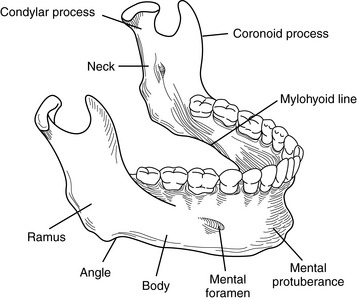
Figure 6-2 The osseous components of the mandible.
(Modified from Hertling D, Kessler RM: Management of common musculoskeletal disorders: Physical therapy principles and methods, ed 2, Philadelphia, 1990, JB Lippincott.)
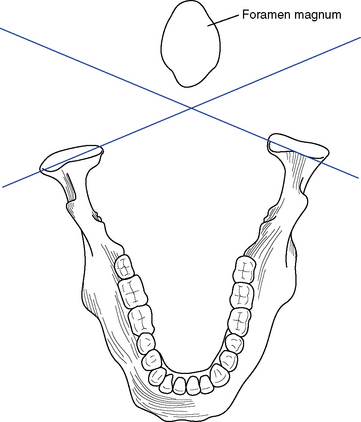
Figure 6-3 Line drawn through the axes of the mandibular condyles will intersect just anterior to the foramen magnum.
(Modified from Hertling D, Kessler RM: Management of common musculoskeletal disorders: Physical therapy principles and methods, ed 2, Philadelphia, 1990, JB Lippincott.)
Functionally, the mandibular fossa serves as a receptacle for the condyles when the joint is in a closed-packed position (teeth approximated). During opening, closing, protrusion, and retrusion, the convex surface of the condyle must move over the convex surface of the articular eminence (Figure 6-4). The existence of the intraarticular disc compensates functionally for the incongruity of the two opposing convex surfaces.3 The disc also separates the joint into an upper and lower portion or compartment, each with synovial linings. The outer edges of the disc are connected to the joint capsule.
Ligamentous Structures
Four ligaments serve as secondary stabilizers for the joint. They are the articular capsule, temporomandibular ligament, stylomandibular ligament, and sphenomandibular ligament (Figure 6-5). The primary function of the joint capsule is to enclose the joint, but because the disc is tethered to it, the joint capsule also causes the disc to move forward when the condyle moves forward. The temporomandibular ligament is the main suspensory ligament of the mandible during opening movements of the jaw. It also prevents excessive forward, backward, and lateral movements. The stylomandibular ligament prevents excessive anterior movement of the mandible and, as such, serves as a stop for the mandible in extreme opening. The sphenomandibular ligament functions as a suspensory ligament for the mandible during wide opening of the joint.
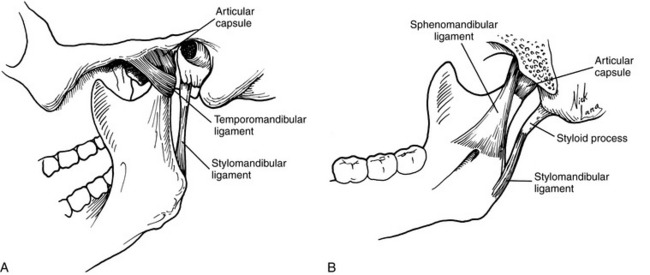
Figure 6-5 Lateral view of the left temporomandibular joint (TMJ) (A) and medial view of the right TMJ (B), showing the ligamentous structures.
A mandibular-malleolar ligament connecting the neck and anterior process of the malleus to the medioposterior aspect of the joint capsule has been reported. 4,5 The clinical significance of this structure lies in making an anatomic connection between the TMJ and the middle ear. The mandibular malleolar ligament passes through the petrotympanic fissure to connect the malleolus to the meniscus and the capsular ligament of the TMJ. The anterior tympanic artery, which is responsible for supplying blood to the tissue around the tympanic membrane, and the chorda tympani nerve, which gives pain sensation to the tongue, also travel through this fissure. Irritation to these structures can cause symptoms such as ear pain, tinnitus, vertigo, subjective hearing loss, hyperacusis, tongue pain, and muscle pain.
Musculature
The primary movers of the mandible in elevation are the temporalis, masseter, and medial pterygoid muscles (Table 6-1 and Figure 6-6). The posterior fibers of the temporalis also retract the mandible while maintaining the condyles posteriorly. The superficial fibers of the masseter protrude the jaw, and the deep fibers act as a retractor. The deep fibers also attach to the lateral aspect of the joint capsule. The medial pterygoid can protrude the mandible, as well as deviate the jaw laterally (Figure 6-7).
TABLE 6-1 Actions of the Muscles of the Temporomandibular Joint
| Action | Muscles |
|---|---|
| Mandibular elevation (closing) | Temporalis, masseter, and medial pterygoid |
| Mandibular depression (opening) | Lateral pterygoid, suprahyoid, and infrahyoid |
| Protrusion (anterior glide) | Superficial fibers of the masseter, medial pterygoid, and lateral pterygoid |
| Retrusion (posterior glide) | Temporalis and deep fibers of the masseter |
| Lateral glide | Medial pterygoid and lateral pterygoid |
| Hyoid elevation | Stylohyoid, mylohyoid, and digastrics |
| Hyoid depression | Infrahyoid |
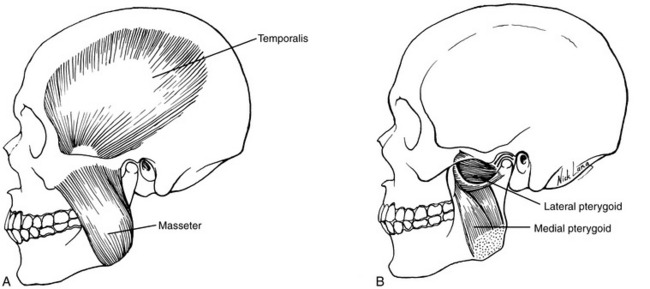
Figure 6-6 Intrinsic musculature of the mandible. A, Left temporalis and masseter, externally. B, Left medial and lateral pterygoid, with proximal mandible removed.
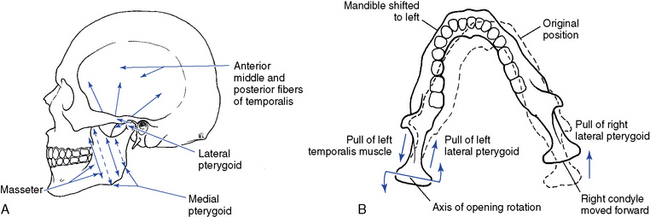
Figure 6-7 The directions of muscular pull in the temporomandibular joint. A, Opening, closing, and anterior glide. B, Left lateral deviation.
The major depressors of the mandible are the lateral pterygoid, suprahyoid, and infrahyoid muscles. The lateral pterygoid also attaches to the mandibular condyle and the intraarticular disc, thereby serving as a significant stabilizer of the joint. It is the primary muscle used in opening the mouth, but can also assist in lateral movements and protrusion. Of clinical importance is its frequency of involvement in cases of TMJ dysfunction.
The suprahyoid muscle group is composed of the digastric, stylohyoid, geniohyoid, and the mylohyoid muscles (Figure 6-8). The digastric muscle pulls the mandible downward and in a posterior direction. The stylohyoid muscle initiates and assists jaw opening, but also draws the hyoid bone upward and backward when the mandible is fixed. The geniohyoid muscle pulls the mandible downward and backward. The mylohyoid muscle elevates the floor of the mouth and assists in depressing the mandible when the hyoid is fixed or in elevating the hyoid when the mandible is fixed.
The prime function of the infrahyoid muscle group, composed of the sternohyoid, thyrohyoid, and omohyoid muscles, is to stabilize or depress the hyoid bone. This action then allows the suprahyoid muscles to act on the mandible.
Biomechanics
Posture and Alignment
In the normal relaxed and inactive state of the TMJ, referred to as the mandibular postural rest position, the teeth should not touch. Instead, there should be an intraocclusal space, termed the freeway space, of approximately 3 to 5 mm. This position is the result of the equilibrium between the muscle tone of the mandibular elevators and the force of gravity. Moreover, it is influenced by the state of the anterior and posterior neck muscles, head posture, and inherent elasticity of the mandibular muscles. This resting posture is decreased in people who brux, or clench, their teeth and is increased in mouth breathers. Disturbances in the resting position may affect the remodeling or reparative processes, leading to an unhealthy TMJ system.
The position of the mandible when the teeth are fully occluded is termed the intercuspal position and is directly influenced by the state of the dentition. In this position, the condylar location is also affected by the dentition, which may differ from that imposed by muscle action. Furthermore, the intercuspal position may have an effect on the mandibular resting posture by disturbing the balance of the musculature, which in turn can affect the head posture and cervical spine function. Therefore, the state of the dentition should not be ignored in patients who have chronic neck pain.
The TMJ undergoes the coupled motions of rotation and translation. Rotational movement of the condyle occurs about a transverse axis between the condyle and the intraarticular disc. This movement causes the first 12 to 15 mm of mandibular opening and closing. Translational movement of the condyle consists of a downward and forward gliding movement of the disc-condyle complex and depends on the synchronous movement of disc and condyle (Figure 6-9). Rotational movements occur mainly in the inferior (subdiscal) joint space, and translational movements occur mainly in the superior (supradiscal) joint space.
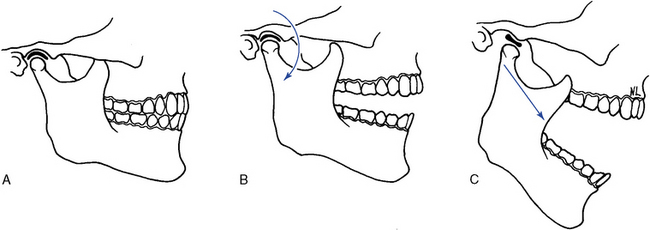
Figure 6-9 Mandibular movement is a complex relationship of rotational and translational movements. A, Closed position. B, Initial opening is rotational. C, Full opening requires forward translation with continued rotation.
Mandibular movement is a dynamic combination of opening, closing, anterior glide (protrusion), posterior glide (retrusion), and lateral glide. Mandibular opening involves the contraction of the lateral pterygoids and digastrics, with assistance from the suprahyoid and infrahyoid muscles. Indirectly, the posterior cervical muscles must contract to prevent neck flexion and permit the mandible to drop away from the cranium. The first few degrees of opening are rotational movements about a transverse axis. Then the condyle and disc complex must translate forward over the articular eminence, allowing condylar rotation to continue. The closing sequence is the reverse. The condyle and disc complex translate posteriorly with condylar rotation, which brings the joint to its resting position, or intercuspal position. The masseter, medial pterygoid, and temporalis muscles are responsible for this action. Table 6-2 lists the osteokinematic and arthrokinematic movements of the TMJ.
TABLE 6-2 Arthrokinematic and Osteokinematic Movements of the Temporomandibular Joint
| Osteokinematic Movements | Arthrokinematic Movements | |
|---|---|---|
| Mandibular elevation and depression | 40 to 60 mm of incisor separation | Combination of spin and glide occurring in the upper and lower joint compartments |
| Mandibular retraction and protrusion | 5 to 10 mm of incisor separation | Glide movement occurring in the upper joint compartment |
| Mandibular lateral deviation | 5 to 10 mm of incisor separation | Glide, spin, and angulation occurring mostly in the upper compartment but also in the lower joint space |
Lateral glide of the mandible involves a pivoting rotation of the condyle on the side to which the mandible is moving and a translation of the other condyle. For lateral glide to the right, the left lateral pterygoid and the anterior bellies of both the digastrics contract, causing the left condyle to move downward, forward, and medially. Meanwhile, contraction of the right temporalis and the right lateral pterygoid rotates the right condyle in the fossa and displaces the mandible to the right. Box 6-1 identifies the close-packed and loose-packed positions for the TMJ.
Evaluation
Problems affecting the TMJ can be broadly classified into developmental abnormalities, intracapsular diseases, and dysfunctional conditions (Box 6-2). Developmental abnormalities include hypoplasia, hyperplasia, impingements of the coronoid process, chondromas, and ossification of ligaments, such as the stylohyoid ligament (Eagle syndrome). The intracapsular diseases include degenerative arthritis, osteochondritis, rheumatoid arthritis, psoriatic arthritis, synovial chondromatosis, infections, steroid necrosis, gout, and metastatic tumors.6 Developmental abnormalities and intracapsular diseases must be ruled out by using appropriate evaluative procedures, including diagnostic imaging and clinical laboratory studies. The focus here is on the dysfunctional conditions affecting the TMJ, which are categorized as extracapsular (myofascial pain syndromes and muscular imbalance); capsular (sprain, hypomobility and hypermobility, and synovial folds); and intracapsular (disc displacement and disc adhesions).
BOX 6-2 Classification of Problems Affecting the Temporomandibular Joint
Inspect the face and jaw, looking for bony or soft tissue asymmetry, misalignment of the teeth, and evidence of swelling (Figure 6-10). Observe the jaw during opening and closing to identify excursional deviations and the presence of clicking7 8 9 (Figure 6-11). Ask the patient if the movements are painful. Normal opening should accommodate three of the patient’s fingers inserted between the incisors. If not, hypomobility resulting from joint dysfunction or a closed lock as a result of disc displacement should be suspected. If opening beyond three fingers occurs, hypermobility from capsular attenuation is likely (Figure 6-12).
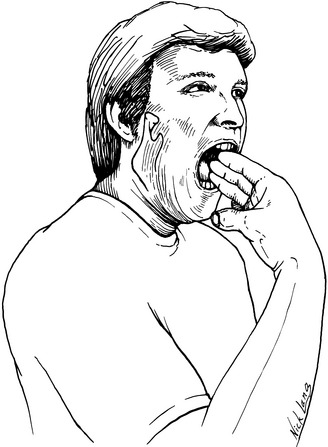
Figure 6-12 Generally, and only as a screen, three of the patient’s fingers should fit between the incisors when fully opened.
Palpate the joint by placing the fifth digit into the patient’s external auditory meatus with the palmar surface forward (Figure 6-13). Before placing the finger into the ear, push on the tragus to determine if the external ear canal is painful. The position of the condyles and intra-articular clicking can be felt from within the external canal. The lateral aspect of the joint and capsule can be palpated externally for position, pain, and movement disorders (Figure 6-14). Palpate the muscles to determine changes in tone, texture, and tenderness. The lateral pterygoid can be palpated intraorally by following the buccal mucosa to the medial aspect of the TMJ just proximal to the tonsils (Figures 6-15 and 6-16). According to investigations, the lateral pterygoid muscle is practically inaccessible for intraoral palpation because of topographic and anatomic reasons.10 11 12 13 Palpation of the lateral pterygoid muscle is also characterized by poor interexaminer agreement.10 In contrast to these reports, Stelzenmüller and associates14 reliably confirmed the palpation of the lateral pterygoid muscle, which was controlled by two imaging procedures and electromyography. All three of the procedures confirmed palpation. The difficulty in reliably identifying the muscle seems to be due to the fact that the medial pterygoid muscle must be passed before palpating the lateral pterygoid muscle.14 Note also the position and movement of the hyoid bone, as well as the state of the associated soft tissues.
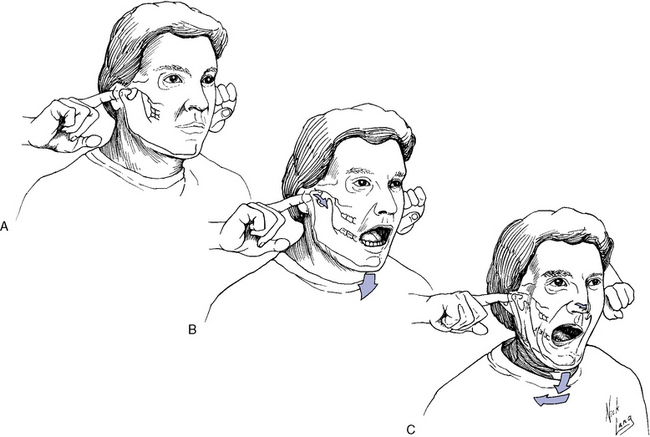
Figure 6-13 Intra-auricular palpation of the temporomandibular joint. A, Finger is placed in external auditory meatus. B, Movement of condyle is palpated on opening and closing. C, Asymmetric joint movement.
Perform accessory motions of the TMJ by placing the gloved thumbs intraorally over the lower teeth and wrapping the fingers around the mandible externally (Figure 6-17). Apply passive stress in long-axis distraction, lateral glide, and anterior-to-posterior (A-P) glide (Box 6-3). Normally, a springing end feel is perceived (Figure 6-18).
A general survey of the oral cavity should be done to rule out dental or oral lesions. Ask the patient to close the teeth together quickly and sharply. Normally, this is not painful, and a broad clicking of the dental surface should be heard. If local pain is produced or only a faint, single striking sound is heard, a dental source (acute malocclusion, tooth abscess, or periodontal disease) is indicated, and a referral to a dentist is advised. In addition, it is important to remember the intimate neurologic relation of the TMJ with the atlanto-occipital articulation and the need to evaluate both joints when either is symptomatic.
Adjustive procedures
The manipulative techniques used to treat TMJ disorders aim to restore normal joint mechanics, which will then ideally allow full pain-free functioning of the mandible. Two basic types of adjustive procedures are used for the different forms of TMJ dysfunction: distraction and translation techniques (Box 6-4). See Box 5-3 for abbreviations used in illustrating techniques.
Distraction Techniques
Distraction procedures create a slow and controlled joint gapping or separation of the joint surfaces. Typically, they require an intraoral contact, making the use of rubber gloves necessary.
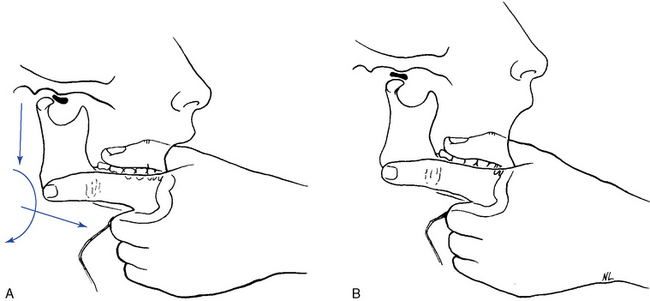
 Figure 6-20 Distraction technique for an anteriorly dislocated disc for the temporomandibular joint. A, Starting position. B, Distraction of the condyle with tilt and anterior translation under the disc.
Figure 6-20 Distraction technique for an anteriorly dislocated disc for the temporomandibular joint. A, Starting position. B, Distraction of the condyle with tilt and anterior translation under the disc.
The TMJ is prone to plica formation (synovial fold) especially with sustained, extreme opening. When a synovial fold becomes entrapped, pain is produced on occlusion and when the disc moves medially or the condyle moves laterally. To reduce the entrapped fold of synovial tissue, the distraction technique must be combined with contraction of the patient’s ipsilateral masseter muscle.
Translation Techniques
Translational adjustive techniques use a line of correction parallel to the plane of the joint surfaces. In addition, a compressive loading force may be applied. The primary effect of this procedure is to move the disc posteriorly, which is specifically indicated for releasing minor disc adhesions (intracapsular adhesions). Translational techniques use extraoral contacts, and gloves are not necessary. Caution must be the rule when using translational techniques, because they carry a higher risk of complication than distraction techniques. If a translational technique is applied to a joint in which the disc is displaced anterior to the condyle, it is possible to injure the retrodiscal tissue or produce a hemarthrosis (blood in the joint) resulting in a medical emergency.
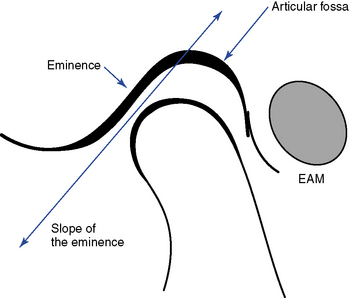
Figure 6-23 The slope of the articular eminence must first be established because this will determine or influence the direction of a translational thrust. External palpation of the eminence is used to determine the slope.
(Modified from Curl D: Acute closed lock of the temporomandibular joint: Manipulative paradigm and protocol, J Chiro Tech 3[1]:13, 1991.)
One of the greatest difficulties encountered when adjusting the TMJ is the patient’s inability to adequately relax the jaw muscles. Furthermore, it is detrimental to the joint to overstretch the upper joint compartment; therefore, care must be taken when using intraoral contacts.
Shoulder
The primary role of the shoulder is to place the hand in a functional position. To achieve this function, a great deal of joint mobility is necessary, which requires complex anatomy and biomechanics. The shoulder is not one joint, but rather is a relationship of anatomic and physiologic joints, forming a four-joint complex. The glenohumeral joint is a true anatomic joint and forms the shoulder proper. The sternoclavicular and acromioclavicular joints are also true anatomic joints formed between the manubrium of the sternum, the clavicle, and the acromial process of the scapula, respectively. The scapulocostal joint lacks a joint capsule and is therefore considered a physiologic joint, necessary to allow the smooth gliding of the scapula over the ribs (Figure 6-26).
These joints provide for an extensive range of active movement for the upper extremity. Many muscles work together synergistically to produce coordinated actions across multiple joints. Dysfunction from trauma or pathologic processes to any of the articulations can cause a significant reduction in the effectiveness of the entire upper limb.
Functional anatomy
Osseous Structures
The convex articular surface of the proximal humerus is directed slightly posteriorly, medially, and superiorly, and is met by the articular surface of the glenoid fossa of the scapula (Figure 6-27). A 45-degree angle is formed between the articular surface and the shaft of the humerus. The glenoid fossa is not a deep impression into the bone of the scapula, and by itself it is incongruous with the humeral head. The glenoid labrum is a fibrocartilaginous rim that encircles the fossa and provides a greater surface area of contact for the humerus, which helps provide some stability (Figure 6-28).
The S-shaped clavicle provides for more movement during elevation of the arm. The distal third of the clavicle is concave anteriorly, which directs the distal articular surface anteriorly and somewhat superiorly. The proximal end of the clavicle articulates with the upper and lateral edge of the manubrium and the superior surface of the first rib costocartilage (Figure 6-29). An intra-articular disc lies between the clavicle and manubrium joint surfaces and is important in preventing medial dislocations of the clavicle.
The scapula lies at a 30-degree angle away from the coronal plane and forms a 60-degree angle with the clavicle15 (Figure 6-30). It has the coracoid process for muscular attachment, projecting anteriorly and lying just medial to the glenoid fossa. The spine of the scapula arises from the medial border at about the T3 level and courses laterally and superiorly, ending as the acromion process.
Ligamentous Structures
Many ligaments are associated with the shoulder, connecting one bone to another and providing a secondary source of joint stability (Figure 6-31). With the varied movements the shoulder can perform, these ligaments will become either slack or taut. Remember that a ligament is painlessly palpated unless it is injured or stretched.
The glenohumeral joint capsule is thin, lax, and redundant, with anterior folds when the arm is at rest. The glenohumeral ligaments provide some reinforcement to the joint capsule anteriorly while helping to check external rotation and possibly abduction. The coracohumeral ligament runs from the coracoid process to the greater tubercle, reinforces the superior aspect of the capsule, and checks external rotation and possible extension. The transverse humeral ligament attaches across the greater and lesser tubercles and serves to contain the tendon of the long head of the biceps muscle.
The acromioclavicular ligament strengthens the superior aspect of the joint capsule. It is intrinsically weak, however, and gives way when a force is applied to the acromion process or glenohumeral joint from above (Figure 6-32). The major stabilizing ligaments of the acromioclavicular joint are the coracoclavicular ligaments, which include the conoid and trapezoid ligaments. The conoid ligament twists on itself as it connects between the coracoid process and clavicle. It prevents excessive superior movement of the clavicle on the acromion, as well as retraction of the scapula, by not allowing the scapuloclavicular angle to widen. Furthermore, the conoid ligament tightens on humeral abduction, causing axial rotation of the clavicle that is necessary for full elevation of the arm. The trapezoid ligament also connects between the coracoid process and the clavicle, but lies distal to the conoid ligament. Its role is to check lateral movement of the clavicle, thereby preventing overriding of the clavicle on the acromion process. The trapezoid ligament also prevents excessive scapular protraction by not allowing the scapuloclavicular angle to narrow.
The sternoclavicular joint capsule is reinforced anteriorly and posteriorly by the anterior and posterior sternoclavicular ligaments, respectively (see Figure 6-32). The interclavicular ligaments reinforce the capsule superiorly. Lying just lateral to the joint, the costoclavicular ligament attaches between the clavicle and first rib and serves to check elevation of the clavicle. Its posterior fibers prevent medial movement, and the anterior fibers prevent lateral movement of the clavicle.
Musculature
Because of the high degree of mobility and the numerous muscles necessary to provide stability to the joint, eight or nine bursae are found about the shoulder joint to reduce friction between the moving parts. Irritation to the bursae, leading to an inflammatory response, is a common clinical occurrence. Of specific clinical significance are the subscapular bursae and the subacromial or subdeltoid bursae (see Figure 6-31). The subscapular bursa lies beneath the subscapularis muscle and overlies as well as communicates with the anterior joint capsule. Distension of this bursa occurs with articular effusion. The subacromial or subdeltoid bursa extends over the supraspinatus tendon and under the acromion process and deltoid muscle (Figure 6-33). It is susceptible to impingement beneath the acromial arch, and inflammation often follows supraspinatus tendinitis.
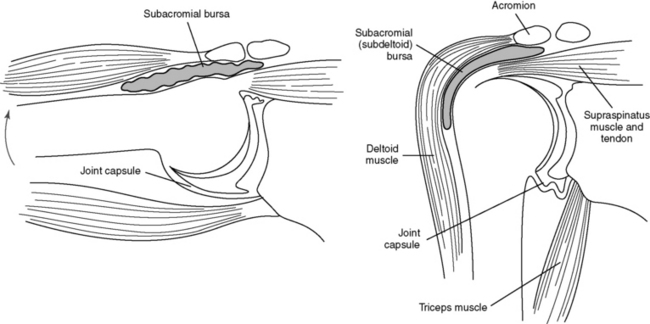
Figure 6-33 Subacromial bursa. A, With humerus pendulous. B, With humerus abducted.
(Modified from Hertling D, Kessler RM: Management of common musculoskeletal disorders: Physical therapy principles and methods, ed 2, Philadelphia, 1990, JB Lippincott.)
A review of the location and function of the numerous muscles that stabilize and supply the force for performing the varied movements of the shoulder is necessary to understand the dysfunctional conditions that affect the shoulder joint complex (Table 6-3). Although muscle tendons tend to lend stability to the joint, they do not prevent downward dislocation. The rotator cuff is composed of the supraspinatus, infraspinatus, teres minor, and subscapularis muscles. It is most notably the horizontal running fibers that prevent dislocation as they check the lateral excursion of the glenoid cavity, which in turn allows downward movement of the humerus. The factors preventing downward dislocation include the slope of the glenoid fossa, which forces the humerus laterally as it is pulled down; tightening of the upper part of the capsule and of the coracohumeral ligament; and the activity of the supraspinatus muscle working with the posterior fibers of the deltoid.
TABLE 6-3 Actions of the Muscles of the Shoulder Joint Complex
| Action | Muscles |
|---|---|
| Flexion | Anterior deltoid, coracobrachialis, and pectoralis major (clavicular) |
| Extension | Latissimus dorsi, teres major, and posterior deltoid |
| Abduction | Middle deltoid, supraspinatus, and serratus anterior (scapular stability) |
| Adduction | Pectoralis major and latissimus dorsi |
| External rotation | Infraspinatus, teres minor, and posterior deltoid |
| Internal rotation | Subscapularis, pectoralis major, latissimus dorsi, teres major, and anterior deltoid |
| Scapular stabilization | Trapezius, serratus anterior, and rhomboids |
| Scapular retraction (medial glide) | Rhomboid major and minor |
| Scapular elevation | Trapezius and levator scapulae |
The tendon of the long head of the biceps is unique in its relationship to the joint in that it originates from within the joint capsule. It arises from the upper margin of the glenoid fossa as a continuation of the glenoid labrum. It penetrates the capsule and passes through the intertubercular groove, which has been converted to a tunnel by the transverse humeral ligament. The passage through the capsule, over the humeral head and between the two tubercles, is facilitated by a tubular sheath of synovial membrane.
Shoulder abduction can be artificially divided into two phases of movement, each involving different muscles to a greater or lesser degree. Shoulder movement is fluid, however, and the various muscular actions and motions run into one another. The first phase of movement, from 0 to 90 degrees of abduction, involves a coupling of the deltoid and supraspinatus muscles that draws the humerus up. To go farther, the scapula and shoulder girdle must also move. In the second phase, the serratus anterior, along with the upper and lower trapezius, tip the scapula so that the inferior angle moves laterally and the acromion process is elevated. This allows movement between 90 and 180 degrees.
Forward flexion of the shoulder begins with the contraction of the anterior fibers of the deltoid, coracobrachialis, and clavicular division of the pectoralis major muscles. Up to 60 degrees of flexion can occur before the scapula and shoulder girdle must move. Again, the serratus anterior and the upper and middle trapezius contract, tipping the scapula, raising the acromion process, and causing axial rotation at the acromioclavicular and sternoclavicular joints.
Internal (medial) rotation is accomplished by contraction of subscapularis, teres major, pectoralis major, latissimus dorsi, and the anterior deltoid muscles. For extreme ranges of internal rotation, the scapula will abduct from the pull of the serratus anterior and the pectoralis minor muscles.
The external (lateral) rotator muscles, in comparison with the internal rotators, are quite weak but are still very important to normal function of the upper limb. Clinically, they are easily strained. The infraspinatus, teres minor, and to a lesser degree, posterior deltoid muscles are responsible for external rotation of the humerus, with the rhomboids and trapezius muscles adducting the scapula for extreme movement.
Shoulder extension is accomplished by contraction of the latissimus dorsi, teres major, and posterior deltoid muscles, with some adduction of the scapula from contraction of the middle trapezius and rhomboid muscles. Adduction of the humerus is accomplished by contraction of the latissimus dorsi, teres major, and pectoralis major muscles, with the rhomboids adducting the scapula.
Biomechanics
Scapulohumeral Rhythm
For the arm to be abducted from the side to overhead, motion of the scapula must be simultaneous and synchronous. During the first 30 degrees of abduction, the scapula seeks a stable position on the rib cage through contraction of the trapezius, serratus anterior, and rhomboid muscles (Figure 6-34). Beyond 30 degrees, 2 degrees of glenohumeral movement occur for every 1 degree of scapulocostal movement. Thus, 15 degrees of arm abduction results from 10 degrees of glenohumeral joint movement and 5 degrees of scapulocostal joint movement. Rotation of the scapula during abduction also enhances mechanical stability by bringing the glenoid fossa directly under the humeral head.
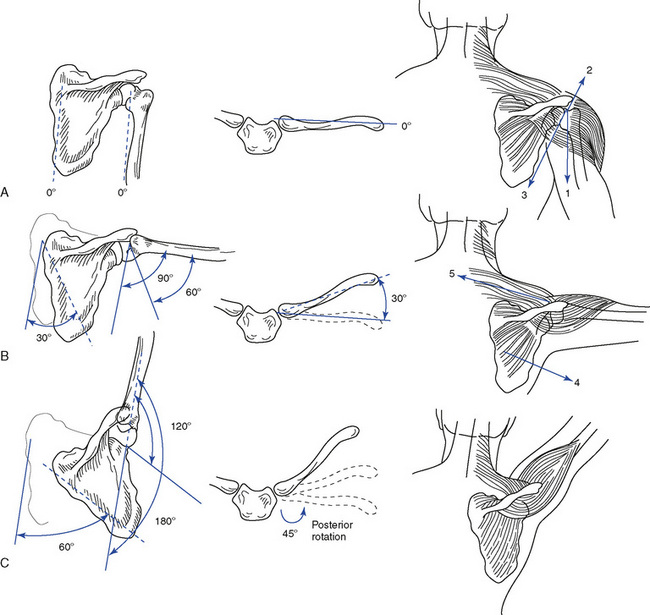
Figure 6-34 Scapulohumeral rhythm. A, Shoulder at 0-degree abduction, with the scapula, humerus, and clavicle in neutral positions. The weight of the extremity (1) is balanced by a force couple comprising an upward pull from the deltoid muscle (2) and a downward pull from rotator cuff muscles plus the pressure and friction of the humeral head (3). B, Shoulder at 90-degree abduction, with 30-degree scapular rotation and 60-degree humeral abduction; clavicle elevates 30 degrees; serratus anterior muscle (4) and upper trapezius muscle (5) force couple balance and rotate scapula. C, Shoulder at 180-degree abduction, with 60-degree scapular rotation and 120-degree humeral abduction; clavicle rotates 45 degrees to reach an additional 30-degree elevation.
(Modified from Wadsworth CT: Manual examination and treatment of the spine and extremities, Baltimore, 1988, Williams & Wilkins.)
Acromioclavicular Joint
Arm abduction also requires axial rotation of the clavicle. For every 10 degrees of arm abduction, the clavicle must elevate 4 degrees. After 90 degrees of arm abduction (60 degrees of humeral abduction and 30 degrees of scapular rotation), the clavicle rotates to accommodate the scapula through its full 60 degrees of motion. This is achieved through the S-shape of the clavicle.16 The acromioclavicular joint usually has a meniscus that functionally divides the joint. Rotational movements occur through the conoid ligament and between the acromion and the meniscus. Hinging movements occur between the meniscus and the clavicle.17
Glenohumeral Joint
The rotator cuff muscles pull the humerus inferiorly (depression), and the glenohumeral joint capsule creates external rotation during abduction to permit the greater tuberosity to pass under the acromion and coracoacromial ligament (Figure 6-35). Carefully evaluate patients complaining of loss of full abduction with or without pain to determine whether the humerus is displaced superiorly or has lost inferior glide movements because of capsular ligament fibroadhesions or improper functioning of the rotator cuff muscles.
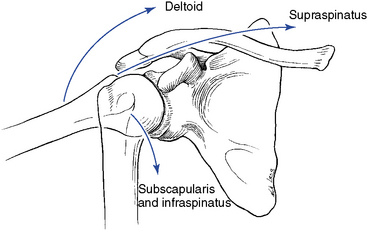
Figure 6-35 The actions of the rotator cuff muscles to depress the humeral head during shoulder abduction.
During shoulder movements away from the body (flexion, abduction, and extension), the superior aspect of the glenohumeral joint capsule becomes lax, so that it can no longer maintain joint integrity against external forces. The rotator cuff muscles carry the responsibility for keeping the humerus oriented to the glenoid fossa. Table 6-4 identifies the normal ranges of motion (ROMs) for the shoulder joint complex, and Table 6-5 describes the close-packed and loose-packed positions of the shoulder joints.
TABLE 6-4 Arthrokinematic and Osteokinematic Movements of the Shoulder Joints
| Osteokinematic Movements | Degrees | Arthrokinematic Movements |
|---|---|---|
| Glenohumeral flexion | 120 | Rotation and glide |
| Glenohumeral extension | 55 | Rotation and glide |
| Glenohumeral abduction | 120 | Roll and glide |
| Glenohumeral adduction | 45 | Roll and glide |
| Glenohumeral internal rotation | 90 | Rotation |
| Glenohumeral external rotation | 90 | Rotation |
| Clavicle internal and external rotation | 10 | Rotation |
| Clavicle elevation and depression | 5 | Roll and glide |
| Clavicle abduction and adduction | 10 | Roll and glide |
| Scapular internal and external rotation | 25 | Rotation and glide |
TABLE 6-5 Close-Packed and Loose-Packed (Rest) Positions for the Shoulder Joints
| Articulation | Close-Packed Position | Loose-Packed Position |
|---|---|---|
| Glenohumeral | Full abduction with external rotation | 55 degrees of abduction with 30 degrees of horizontal adduction |
| Acromioclavicular | 90 degrees of abduction | Physiologic rest position |
| Sternoclavicular | Full arm elevation | Physiologic rest position |
The minimally constrained ball-and-socket glenohumeral joint allows for a significant amount of movement, but is also susceptible to injury and instability. Rotational movements are the most frequent surface motion, although combinations of gliding and rolling also occur.17 For other movements, the humeral ball must displace with respect to the glenoid fossa.
Sternoclavicular Joint
Considerable gliding movements occur at the sternoclavicular joint, with the costoclavicular ligament serving as a fulcrum during shoulder motion. Similar to the acromioclavicular joint, in the sternoclavicular joint, the meniscus divides the joint into two functional units. A-P gliding occurs between the sternum and the meniscus, and superior-to-inferior (S-I) gliding occurs between the clavicle and the meniscus.12 Rotation of the clavicle about its long axis is possible. A reciprocal motion occurs between the sternoclavicular joint and acromioclavicular joint during glide motions but not during rotational motions.
Evaluation
The acromioclavicular joint is relatively weak and inflexible for the constant burden and repeated stresses it bears. A force applied to the acromion process or the glenohumeral joint from above causes the scapula to rotate around an axis located at the coracoid process. The acromioclavicular ligament, being intrinsically weak, gives way, and the joint disrupts. A second mechanism of injury comes with a downward force of greater intensity, which lowers the clavicle on the first rib, with the rib becoming a fulcrum. Both the acromioclavicular and coracoclavicular ligaments tear, causing a complete acromioclavicular separation. This usually happens with a fall on the point of the shoulder or a fall on the hand of an outstretched arm. The sternoclavicular and costoclavicular ligaments also may be sprained during shoulder trauma.
Rotator cuff muscle strains are caused by falls on an outstretched arm, impingement against the coracoacromial arch, and minor or repetitive stresses to a compromised tendon. Most injuries are to the supraspinatus tendon.
Because of the relatively poor blood supply near the insertion of the supraspinatus, nutrition to this area may not meet the demands of the tendon tissue. An inflammatory response arises in the tendon, creating a tendinitis that probably is a result of the release of enzymes and resultant dead tissue acting as a foreign body. The body may react by laying down scar tissue or even calcific deposits. This is then referred to as calcific tendinitis.
Bursitis, as a primary condition resulting from local trauma, is rare. As a secondary progression from tendinitis, however, it is very common. Acute bulging of the tendon compresses the bursa against the coracoacromial arch, resulting in inflammation and swelling of the bursa. This produces severe limitation of motion, as well as severe pain. The subacromial and subdeltoid bursae are most frequently involved.
Capsulitis (adhesive capsulitis or “frozen shoulder”) is a further progression of tendinitis-bursitis clinical phenomenon, with resultant adherence of the bursal walls, causing the supraspinatus and deltoid muscles to become “stuck together.” Continued immobility leads to capsular tightening and eventual capsular fibrosis. Degenerative joint disease, rheumatoid arthritis, immobilization, and reflex sympathetic dystrophy also cause capsular tightening that may lead to capsulitis.
The shoulder and arm are common sites for referred pain from the cervical spine, myocardium, gallbladder, liver, diaphragm, and breast. Usually the patient’s history suggests the origin of pain. Moreover, many of the muscles responsible for shoulder movement and proper function receive innervation from the C5 or C6 nerve root (NR), again signifying the importance of evaluating the cervical spine.
To begin the evaluation of the shoulder, observe the shoulder posture for the presence of asymmetry of shoulder heights, position of scapulae, and position of the humerus. Inspect the soft tissues for signs of atrophy and swelling. Identify osseous symmetry and pain production through static palpation of the sternoclavicular joint, clavicle, coracoid process, acromioclavicular joint, acromion process, greater tuberosity, bicipital groove, lesser tuberosity, spine of the scapula, and borders and angles of the scapula. Tone, texture, and tenderness changes should be identified through soft tissue palpation of the bursa, pectoralis major, biceps, deltoid, trapezius, rhomboids, levator, latissimus dorsi, serratus anterior, rotator cuff muscles, and teres major. Accessory joint motions for each of the four-component articulations should be evaluated when joint dysfunction is suspected (Table 6-6).
TABLE 6-6 Accessory Joint Movements of the Shoulder Joint Complex
| Joint | Movement |
|---|---|
| Glenohumeral | |
| Sternoclavicular | |
| Acromioclavicular | |
| Scapulocostal |
A-P, Anterior-to-posterior; I-S, inferior-to-superior; L-M, lateral-to-medial; M-L, medial-to-lateral; P-A, posterior-to-anterior; S-I, superior-to-inferior.
Assess long-axis distraction of the glenohumeral joint with the patient in the supine position and the involved arm at the side of body. Stand at the side of the table and use the inside hand to stabilize the scapula in the patient’s axilla. Use the other hand to grasp the humerus and stress it caudal, feeling for a springing motion (Figure 6-36).
Evaluate A-P glide with the patient supine and the involved arm slightly abducted. Standing between the patient’s arm and table, grasp the axillary, medial aspect of the proximal humerus with your inside hand and grasp the anterolateral aspect of the proximal humerus with your outside hand. Thumbs should be together. Stress the proximal humerus anteriorly to posteriorly by applying pressure with the thumbs. Conduct P-A glide with these same contacts, stressing the proximal humerus posteriorly to anteriorly with the fingers (Figure 6-37).

 Figure 6-37 Assessment of anterior-to-posterior and posterior-to-anterior glide of the right glenohumeral joint.
Figure 6-37 Assessment of anterior-to-posterior and posterior-to-anterior glide of the right glenohumeral joint.
Medial-to-lateral (M-L) glide can be done with the patient in the supine position. Grasp the medial aspect of the proximal humerus with one hand while stabilizing the distal humerus at the elbow with the other hand. Using the elbow as a fulcrum, stress the proximal humerus medially to laterally (Figure 6-38).

Figure 6-38 Assessment of medial-to-lateral glide Long Axis Distraction (LAD) of the right glenohumeral joint.
Assess internal and external rotation with the patient in the supine position, with the involved arm slightly abducted. Stand at the side of the table and use both hands to grasp the proximal humerus. Stress the humerus internally and externally (Figure 6-39).
Evaluate inferior glide in flexion with the patient in the supine position and the involved arm flexed to 90 degrees. Stand at the side of table, interlace the fingers of both hands around the proximal humerus, and rest the patient’s elbow against your shoulder. Using the patient’s elbow against your shoulder as a fulcrum, stress the patient’s shoulder inferiorly (Figure 6-40).
Perform inferior glide in abduction with the patient in the supine position, with the involved arm abducted to 90 degrees. Stand at the head of the table and place the cephalic hand on the superior aspect of the proximal humerus while grasping the inferior aspect of the elbow with the other hand. Then stress the proximal humerus inferiorly (Figure 6-41).
The sternoclavicular joint has accessory movements in inferior glide, superior glide, posterior glide, and anterior glide. To evaluate each of these movements, stand behind the seated patient. Reach in front of the patient’s neck and use a thumb contact on the proximal clavicle to stress it inferiorly, superiorly, posteriorly, and anteriorly (Figure 6-42).
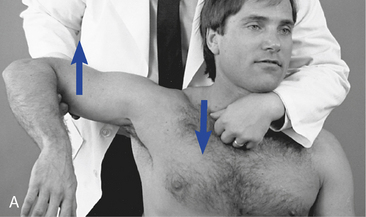
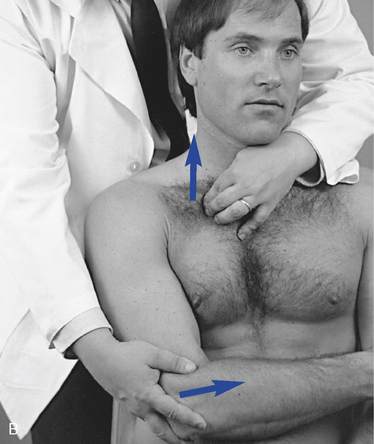
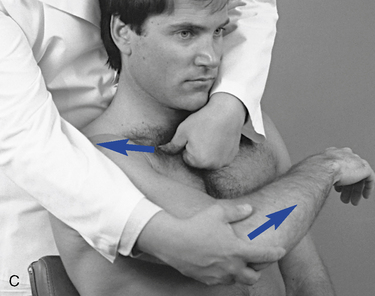
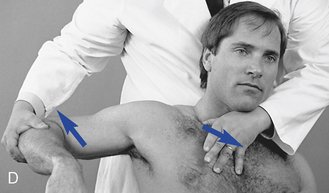
 Figure 6-42 Assessment of the right sternoclavicular joint. A, Superior-to-inferior glide. B, Inferior-to-superior glide. C, Anterior-to-posterior glide. D, Posterior-to-anterior glide.
Figure 6-42 Assessment of the right sternoclavicular joint. A, Superior-to-inferior glide. B, Inferior-to-superior glide. C, Anterior-to-posterior glide. D, Posterior-to-anterior glide.
Evaluate the acromioclavicular joint for accessory movements standing at the patient’s side, with the patient seated. Grasp the distal clavicle with one hand and stabilize the scapula and shoulder with the other hand. Then stress the distal clavicle anteriorly, posteriorly, inferiorly, and superiorly (Figure 6-43).


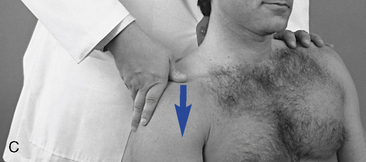
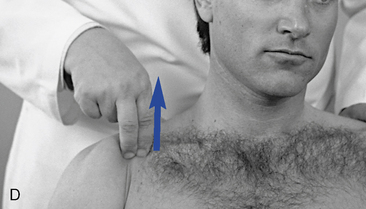
 Figure 6-43 Assessment of the right acromioclavicular joint. A, Posterior-to-anterior glide. B, Anterior-to-posterior glide. C, Superior-to-inferior glide. D, Inferior-to-superior glide.
Figure 6-43 Assessment of the right acromioclavicular joint. A, Posterior-to-anterior glide. B, Anterior-to-posterior glide. C, Superior-to-inferior glide. D, Inferior-to-superior glide.
The scapulocostal joint, although not an anatomic joint, also undergoes a stress evaluation. The findings are somewhat different in that a springing end feel or joint play movement is not expected. The stress evaluation is used to determine the integrity of the subscapular soft tissues and the supporting musculature. Decreased movement is still the positive finding. The movements assessed are medial glide, lateral glide, and rotation in both directions. Perform the evaluation standing at the side of the table, with the patient lying in the prone position. For medial glide, bring the patient’s arm to rest along the side of the body and use both hands to contact the lateral aspect (axillary border) of the scapula. Stress the scapula medially (Figure 6-44). For rotational glide moving the inferior angle medially, place the patient’s arm in the small of the back and use both hands to grasp the scapula so that the caudal thumb hooks the lateral aspect of the inferior angle. With both hands, twist the scapula so that the inferior angle is stressed medially (Figure 6-45). For rotational glide moving the inferior angle laterally, place the patient’s hand behind his or her head and use both hands to grasp the scapula so that the cephalic thumb hooks the superior aspect of the axillary border and the caudal fingers hook the medial aspect of the inferior angle. With both hands, twist the scapula so that the inferior angle is stressed laterally (Figure 6-46). For M-L glide, the patient’s arm hangs off the table; stand on the opposite side of the table and use both hands to contact the medial aspect (vertebral border) of the scapula. With both hands, stress the scapula laterally (Figure 6-47).

 Figure 6-45 Assessment of the right scapulocostal articulation for clockwise rotation, gliding the inferior angle medially.
Figure 6-45 Assessment of the right scapulocostal articulation for clockwise rotation, gliding the inferior angle medially.
Adjustive procedures
The manipulative techniques used to treat shoulder disorders aim to restore normal joint mechanics, which will then ideally allow full pain-free functioning of the shoulder joints. All four joints should be evaluated for characteristics of dysfunction when there are shoulder symptoms present. Box 6-5 identifies the adjustive procedures for the joints of the shoulder.
BOX 6-5 Shoulder Adjustive Techniques
Glenohumeral supine:
Glenohumeral prone:
Glenohumeral Joint
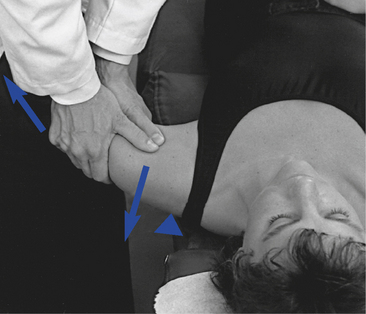
 Figure 6-49 Adjustment for anterior-to- posterior glide of the left glenohumeral joint in the supine position.
Figure 6-49 Adjustment for anterior-to- posterior glide of the left glenohumeral joint in the supine position.

 Figure 6-50 Adjustment for inferior glide in flexion of the left glenohumeral joint in the supine position.
Figure 6-50 Adjustment for inferior glide in flexion of the left glenohumeral joint in the supine position.

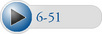 Figure 6-51 Adjustment for inferior glide in abduction of the left glenohumeral joint in the supine position.
Figure 6-51 Adjustment for inferior glide in abduction of the left glenohumeral joint in the supine position.
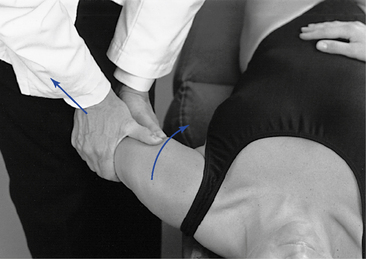
 Figure 6-52 Adjustment for internal rotation of the left glenohumeral joint with distraction. External rotation is done with the same procedure, using external rotation prestress and thrust.
Figure 6-52 Adjustment for internal rotation of the left glenohumeral joint with distraction. External rotation is done with the same procedure, using external rotation prestress and thrust.
Prone:
Standing:
Sitting:
Acromioclavicular Joint
Supine:
Sternoclavicular Joint
Supine:
Sitting:
Scapulocostal Articulation
Side posture:
Elbow
Although outwardly the elbow appears to be a simple singular joint, it is actually an intricate mechanism that depends on the integrated action of three bones that form four distinct articulations. This peripheral joint complex must work together to enable the movements of flexion and extension (humeroulnar and humeroradial joints), as well as pronation and supination (proximal and distal radioulnar joints) of the forearm and hand. Performance of the unique manual skills of the upper extremity depends largely on the proper functioning of the bones, ligaments, and muscles around the elbow joint.
Functional anatomy
Osseous Structures
The cylindrical shaft of the humerus becomes flattened and spreads out distally to form the medial and lateral epicondyles. The distal end of the humerus contains two articular surfaces: the trochlea, which resembles an hourglass on its side, and the capitulum, which is spherical (Figure 6-76). The radial fossa and coronoid fossa on the anterior surface and the olecranon fossa on the posterior surface allow an increased range of flexion and extension by delaying impact of the respective bony prominences on the humeral shaft.16 The proximal end of the ulna contains the coronoid process and olecranon process, with the trochlear notch lying between. This surface of the ulna articulates with the trochlea of the humerus. The trochlear articular surface is asymmetric, which directs the ulna, and hence the forearm, into an abducted position on full extension. The forearm forms an angle with the arm ranging from 5 to 15 degrees, which is commonly referred to as the carrying angle (Figure 6-77).
The superior surface of the radial head is concave to accept the spherical capitulum. The radial or bicipital tuberosity protrudes anteriorly and medially, just distal to the head of the radius.
Ligamentous Structures
Besides the joint capsule that encloses the three-joint complex (humeroulnar joint, radiohumeral joint, and radioulnar joint), three primary ligaments stabilize the elbow. The annular ligament encircles the head of the radius and maintains its contact with the ulna. It is lined with articular cartilage so that the radial head has an articular surface with the ulna, humerus, and annular ligament (Figure 6-78). The medial and lateral collateral ligaments reinforce the joint capsule of the elbow. They restrict medial and lateral angulation and glide of the ulna on the humerus. Each collateral ligament spreads from its respective epicondyle attachment to reinforce the annular ligament anteriorly while providing medial and lateral stability through attachments to the radius and ulna, respectively.
Musculature
Several significant muscle groups cross the elbow joint and, therefore, serve as predominant stabilizers of the elbow (Table 6-7). The wrist flexors cross the elbow to attach at the medial epicondyle, and the wrist extensors cross the elbow to attach to the lateral epicondyle. Tendons from both of these muscles blend into the fibers of their respective collateral ligaments. Although these muscles cross the elbow joint, their primary function is wrist movement. Elbow flexion is accomplished by the brachialis,brachioradialis, and biceps brachii muscles. Extension of the elbow occurs through the action on only one muscle, the triceps brachii, although the anconeus is thought to provide some extension. Supination of the forearm is produced by the contraction of the supinator and, to a lesser degree, the biceps. The pronator quadratus and pronator teres muscles provide the contractive force for the pronation of the forearm.
TABLE 6-7 Actions of the Muscles of the Elbow
| Action | Muscles |
|---|---|
| Flexion | Brachialis |
| Flexion in supination | Biceps |
| Rapid flexion or flexion with loads | Brachioradialis |
| Extension | Triceps and anconeus |
| Supination | Supinator and biceps |
| Pronation | Pronator quadratus |
| Rapid pronation or pronation with loads | Pronator teres |
| Medial stability and some extension | Wrist flexors |
| Lateral stability and some flexion | Wrist extensors |
The olecranon bursa lies between the skin and the olecranon process to reduce friction between the large bony process and the skin (Figure 6-79). A bicipitoradial bursa lies between the tendon of the biceps muscle and the radius.
Biomechanics
The elbow joint is a modified hinge, classified as a compound paracondylar joint in that one bone, the humerus, articulates with two others that lie side by side by way of two distinct facets.18 Flexion and extension movements occur between the trochlea of the humerus and the trochlear notch of the ulna. Within a single joint cavity lie the hinged (ginglymus) humeroulnar articulation, the gliding (plane) humeroradial articulation, and the pivotal (trochoid) superior radioulnar articulation.15 Table 6-8 shows the normal ROMs for the elbow joint.
TABLE 6-8 Arthrokinematic and Osteokinematic Movements of the Elbow Joints
| Osteokinematic Movements | Degrees | Arthrokinematic Movements |
|---|---|---|
| Flexion | 135 to 165 | Roll and glide |
| Extension | 0 to 5 | Roll and glide |
| Supination | 90 | Rotation and glide |
| Pronation | 90 | Rotation and glide |
Flexion and extension movements occur around an axis that passes through the centers of arcs described by the trochlear sulcus and the capitulum, permitting 145 degrees of active and 160 degrees of passive movement from full extension to flexion (Figure 6-80). Extension with supination is the closed-packed position for the humeroulnar joint, whereas the closed-packed position for the humeroradial joint is at 90 degrees of flexion with 5 degrees of supination. For the elbow to move from extension to flexion, the radius and ulna must undergo roll and glide movements in relation to the capitulum and the trochlea, respectively. Active flexion is limited by compression of the soft tissues in the anterior aspect of the forearm and arm, with passive flexion being limited by the tension of the posterior joint capsule and tension in the triceps. Extension is limited by contact of the olecranon process in the olecranon fossa.
The anatomic and mechanical arrangement of the proximal radioulnar joint accounts for the uniqueness of this joint, but also adds difficulty to its treatment. A fibro-osseous ring, which is part of the annular ligament, as opposed to true articular cartilage, composes 80% of the articular surface. The distal radioulnar joint has a convex ulnar head fitting into a shallow concavity on the radius. The distal ulnar also articulates with the triangular fibrocartilage forming part of the ulnocarpal joint.
The mechanical axis for forearm pronation and supination movements is a line passing from the center of the radial head to near the styloid process of the ulna distally. Normally, between 175 and 180 degrees of movement occur from pronation to supination. This motion is primarily the function of the proximal and distal radioulnar joint with some rotational movement occurring at the humeroradial joint (Figure 6-81). During pronation, the radius (and hand) cross over a relatively fixed ulna. The ulna is essentially stationary through the movements of supination and pronation. The radius and the ulna are bound together by the interosseous membrane. Compressive and distractive forces along the length of the forearm place stress on the attachments of the interosseous membrane that can be a source of deep aching pain in the forearm. The distal radioulnar joint will be considered with the wrist and hand.
Figure 6-81 Transverse section through the proximal radioulnar articulation. A, Pronation. B, Supination.
As mentioned, when the arm is extended in its anatomic position, the longitudinal axis of the arm and forearm forms a lateral (valgus) angle at the elbow, known as the carrying angle. The normal carrying angle measures approximately 5 degrees in men and between 10 and 15 degrees in women. An increased angulation can be caused by epiphyseal damage secondary to lateral epicondylar fracture and may cause a delayed nerve palsy, which presents as an ulnar nerve distribution in the hand. A decrease in the carrying angle, called a gunstock deformity, is often the result of trauma, such as a supracondylar fracture in childhood.
Arthrokinematics of the elbow are dictated by the spiral shape of the articular surface of the trochlea. Flexion and extension movements are impure swing movements that couple adduction with flexion and abduction with extension. The close-packed and loose-packed positions for the elbow joints are identified in Table 6-9.
TABLE 6-9 Close-Packed and Loose-Packed (Rest) Positions for the Elbow Joints
| Articulation | Close-Packed Position | Loose-Packed Position |
|---|---|---|
| Humeroulnar | Full extension in supination | 70 degrees of flexion with 10 degrees of supination |
| Humeroradial | 90 degrees of flexion with 5 degrees of supination | Full extension and supination |
| Proximal radioulnar | 5 degrees of supination | 35 degrees of supination with 70 degrees of flexion |
Evaluation
The elbow is exposed to numerous traumatic events that can lead to joint injury and dysfunction. A common cause of elbow problems is a result of muscle activity across the joint. Lateral epicondylitis results from such activity of the wrist extensors. The extensor mass, and especially the deeply located extensor carpi radialis, rubs and rolls over the lateral epicondyle and radial head during forced contraction of the muscle. The forced contractions of the muscle group produce tugs on the origin, resulting in microtears in the tendon and a pulling away of the periosteum. This, coupled with the irritation of soft tissue rubbing over bony prominences, results in a painful elbow condition. Typically, a pain pattern extending down the forearm, following the extensor muscle group, and point tenderness over the lateral epicondyle both occur. The pain is intensified by resisted extension of the wrist and fingers, as well as by shaking hands. The pain may progress to the point that the patient has difficulty picking up a coffee cup or turning a doorknob. The action of the backhand stroke in tennis has been a frequent cause, hence the name tennis elbow.
Medial epicondylitis occurs because of forced muscle activity of the wrist flexors. The clinical picture is much the same as for lateral epicondylitis, but the pain is medial and follows the wrist flexors. It has been referred to as golfer’s elbow, being associated with forced flexion during a golf swing.
Subluxation of the radial head can occur in a young person who is forcibly pulled up from the floor by grabbing the wrist. This action creates traction on the annular ligament on one side by the pull of the arm and on the other side by the pull of the body. This condition, called pulled elbow or nursemaid’s elbow, results in a limitation of supination and tenderness over the radial head. The patient will usually refuse to use the arm, and it will hang limp at the side, with the hand in pronation.
Trauma to the posterior aspect of the elbow, either by a fall on the flexed elbow or by recurrent irritation, can lead to inflammation of the olecranon bursa. Swelling will be visible and palpable and will result in pain on palpation and movement. Olecranon bursitis is frequently seen in individuals such as students who lean on their elbows on a hard surface for long periods. The ligamentous stability of the elbow can be breached, causing an elbow sprain in hyperextension, hyperabduction, and hyperadduction.
The ulnar nerve is vulnerable to trauma as it passes through the ulnar groove at the medial aspect of the elbow. It can be contused by a direct blow, stretched by a valgus force to the elbow, trapped in scar tissue after trauma to the elbow, and irritated by bone spurs. Any or all of these processes can create a peripheral entrapment of the ulnar nerve known as cubital tunnel syndrome. Elbow pain may or may not be associated with this problem. The cardinal symptoms of ulnar nerve injury are tingling and burning of the little finger and ulnar half of the ring finger. Motor function of the opponens digiti minimi and interosseous muscles also may be impaired.
The effective treatment and management of patients with elbow problems obviously depends on first establishing the nature and extent of the lesion, being aware of which anatomic structures have been potentially injured. The elbow is largely derived from C6 and C7 and may therefore be a site of referred pain, as well as a source for referral of pain to other structures from these segments (Figure 6-82).
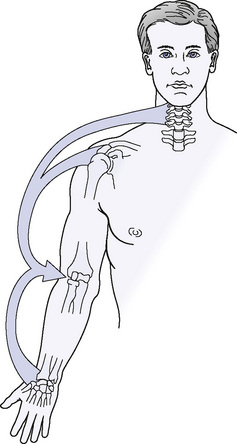
Figure 6-82 The elbow may be the site of referred pain, as well as the source of referral.
(From Magee DJ: Orthopedic Physical Assessment, ed 5, St Louis, 2008, Saunders.)
To begin the evaluation of the elbow, observe the elbow for evidence of swelling, asymmetry of contours, posture, and attitude. Also note functional use of the arm during gait, position changing, and other activities. Evaluate the carrying angle by having the patient straighten his or her supinated elbows (anatomic position) and measuring the angle from the junction of the longitudinal axis of the upper arm and forearm.
Identify osseous symmetry and pain production through static palpation of the radial head, medial epicondyle, lateral epicondyle, olecranon process, and fossa. Structural integrity of the elbow joint can be evaluated through the relationship of the olecranon process to the humeral epicondyles. With the elbow extended and viewed from the posterior, the three landmarks should lie in a horizontal line. Then flex the elbow to 90 degrees; the three landmarks should form an isosceles triangle, with the apex pointing downward (Figures 6-83 and 6-84). Any appreciable deviation from this alignment may indicate some anatomic problem and may require further investigation.19
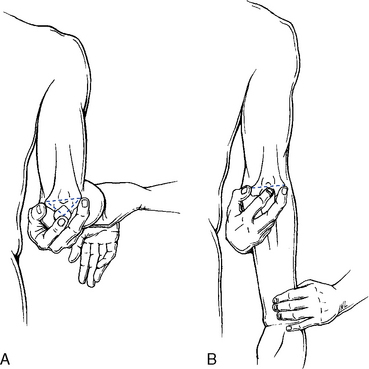
Figure 6-83 Palpational relationship between the epicondyles and olecranon process in a normal elbow.
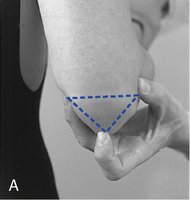
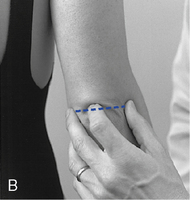
Figure 6-84 Palpational relationship between the epicondyles and olecranon process. A, Flexion landmarks form an isosceles triangle. B, Extension landmarks form a straight line. Deviations indicate a structural problem.
Identify tone, texture, and tenderness changes through soft tissue palpation of the olecranon bursa, collateral ligaments, annular ligament, ulnar nerve, wrist flexor muscle group, wrist extensor muscle group, triceps, brachial radialis, and biceps. Evaluate accessory joint motions for the elbow articulations (Box 6-6) to determine the presence of joint dysfunction. Assess long-axis distraction, primarily of the humeroulnar joint, with the patient sitting or supine and his or her elbow bent slightly. Stand to the side of involvement, facing the patient, and use your inside hand to stabilize the humerus while your outside hand grasps the distal forearm. Then stress the forearm along its long axis, feeling for a springing end feel (Figure 6-85).
Evaluate M-L glide of the humeroradial and humeroulnar joints with the patient seated and the affected arm extended at the elbow and flexed at the shoulder. Stand and face the patient on the medial side of the affected arm. Stabilize the patient’s arm against your body with your outer arm while your inside hand takes a calcaneal contact over the medial aspect of the elbow joint. With the forearm stabilized, stress the elbow from medial to lateral, assessing for the presence of a springing joint play movement (Figure 6-86).
Assess L-M glide of the humeroradial and humeroulnar joint with the patient in a seated position and the affected arm extended at the elbow and flexed at the shoulder. Stand and face the patient on the lateral aspect of the affected arm. Stabilize the patient’s forearm, using the inside arm to hold the patient’s arm against your body. Your outside arm takes a calcaneal contact over the lateral aspect of the elbow joint. With the patient’s forearm stabilized against your body, stress the elbow laterally to medially, determining the presence of a springing joint play movement (Figure 6-87).
Evaluate P-A glide of the humeroulnar joint in extension, with the patient sitting and the affected arm extended at the elbow and flexed at the shoulder. Stand and face the patient on the lateral side of the affected arm. Form a ring with your thumb and index finger of your outside hand and place it over the posterior aspect of the olecranon process. Rest your other hand on the anterior aspect of the distal forearm. With very little downward pressure on the distal forearm, apply a gentle P-A stress to the olecranon process, looking for a springing joint play movement (Figure 6-88).
Assess A-P and P-A glide of the radioulnar joint, with the patient in the seated position and the affected arm extended at the elbow and flexed at the shoulder. Stand and face the patient on the lateral aspect of the affected arm. With your inside arm, stabilize the patient’s forearm against your body and grasp the distal humerus and proximal ulna. With your outside hand, hold the radial head between the thumb and index finger. While stabilizing the ulna and humerus, stress the radial head from anterior to posterior and from posterior to anterior, determining the presence of a springing joint play movement (Figure 6-89).
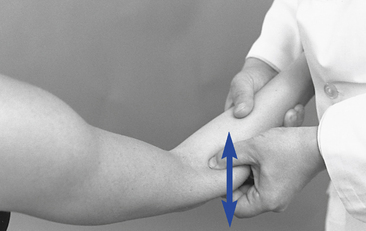
 Figure 6-89 Assessment of anterior-to-posterior and posterior-to-anterior glide of the right radioulnar joint.
Figure 6-89 Assessment of anterior-to-posterior and posterior-to-anterior glide of the right radioulnar joint.
Evaluate P-A glide of the radioulnar joint in pronation with the patient in the seated position and the affected arm extended at the elbow and flexed at the shoulder. Stand and face the lateral aspect of the affected arm. With your outside hand, grasp the distal forearm, with digital contacts of the index, middle, and ring fingers on the posterior aspect of the radius. With your inside hand, place a thumb contact on the posterior aspect of the radial head. Use your outside hand to pronate the forearm. At the contact over the radial head, you should first perceive a rotational movement of the radial head, and at the end point of movement, apply a P-A stress to the radial head to determine the presence of a springing end-feel movement (Figure 6-90).
Adjustive procedures
The manipulative techniques used to treat elbow disorders aim to restore normal joint mechanics, which will then ideally allow full pain-free functioning of the elbow joints. Box 6-7 identifies the adjustive procedures for the joints of the elbow.
BOX 6-7 Elbow Adjustive Techniques
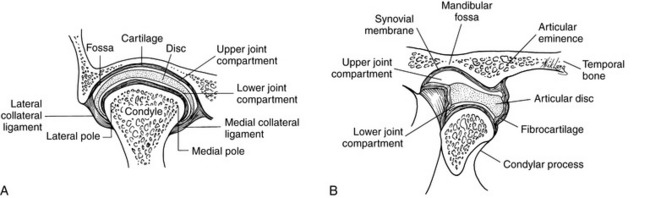
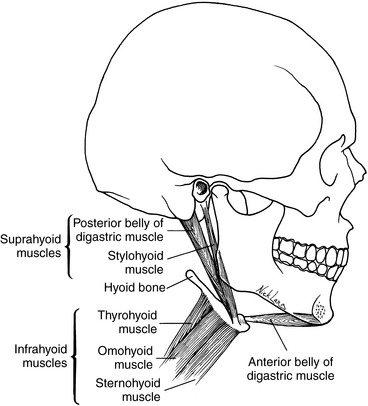
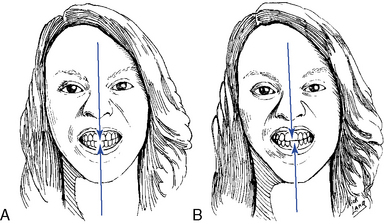
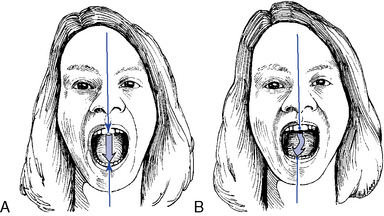
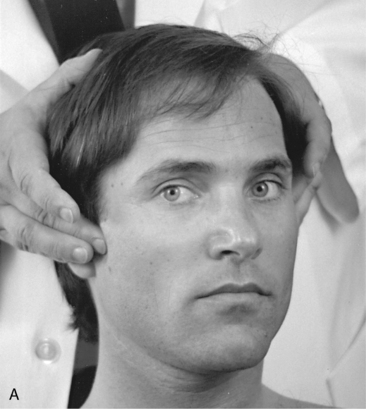
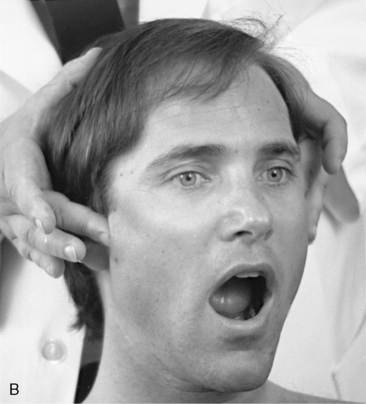
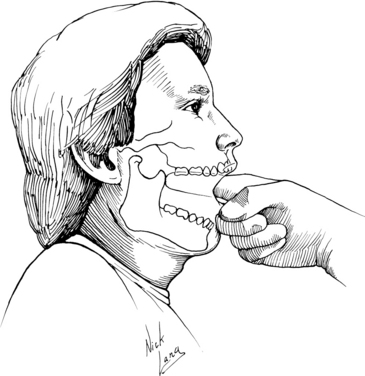

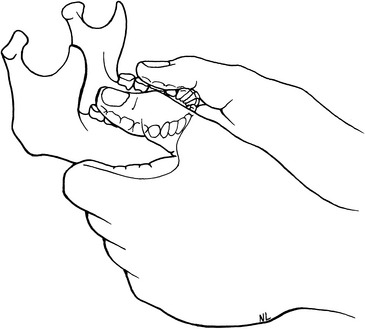

 Figure 6-18
Figure 6-18
 Figure 6-19
Figure 6-19
 Figure 6-21
Figure 6-21
 Figure 6-22
Figure 6-22
 Figure 6-24
Figure 6-24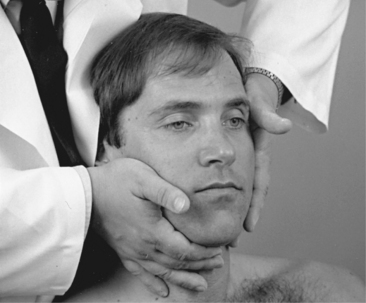
 Figure 6-25
Figure 6-25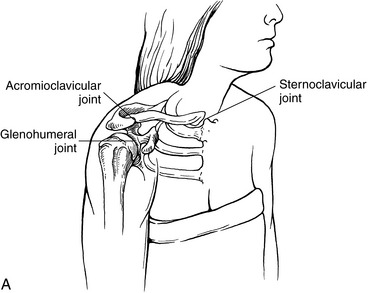
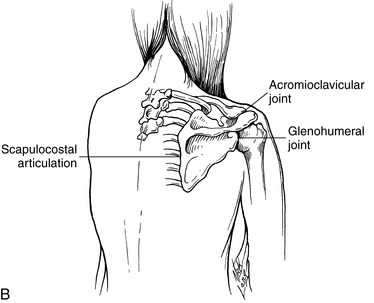
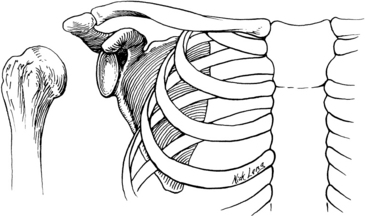
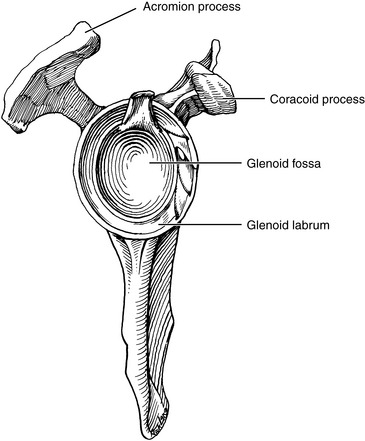
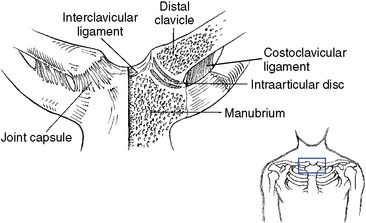
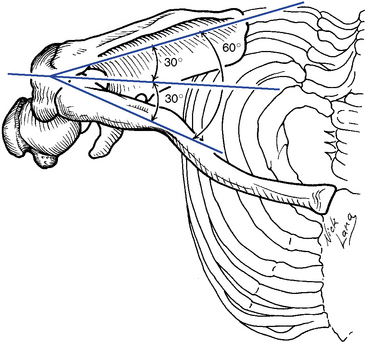
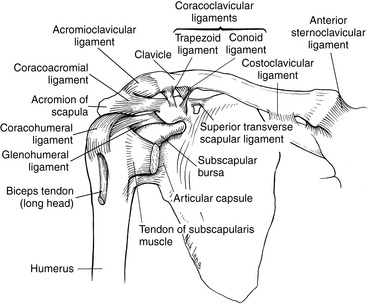
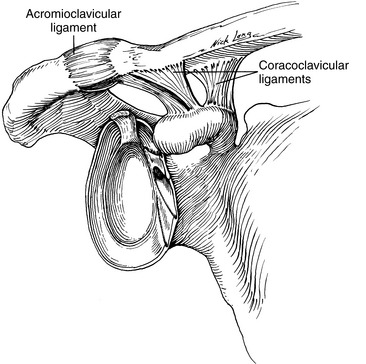
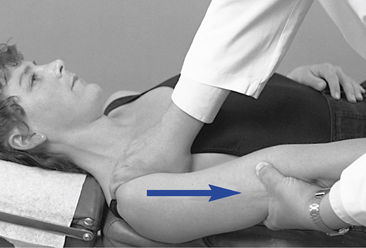
 Figure 6-36
Figure 6-36
 Figure 6-39
Figure 6-39
 Figure 6-40
Figure 6-40
 Figure 6-41
Figure 6-41
 Figure 6-44
Figure 6-44
 Figure 6-46
Figure 6-46
 Figure 6-47
Figure 6-47
 Figure 6-48
Figure 6-48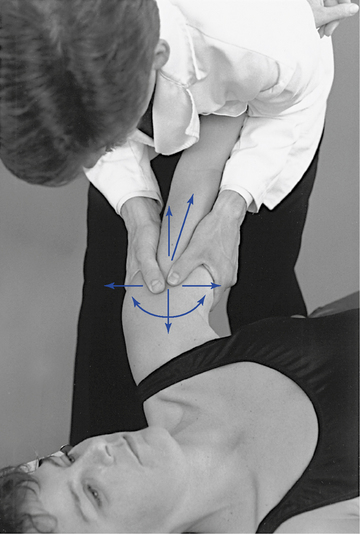
 Figure 6-53
Figure 6-53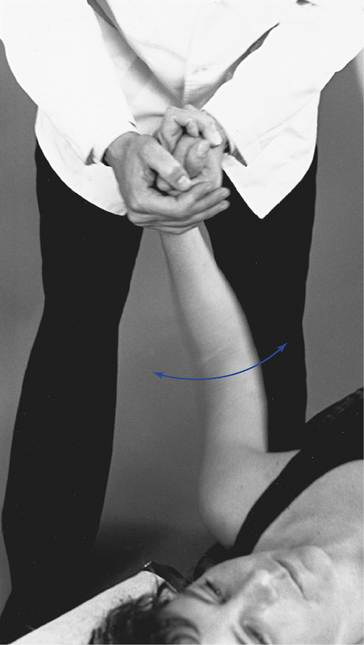
 Figure 6-54
Figure 6-54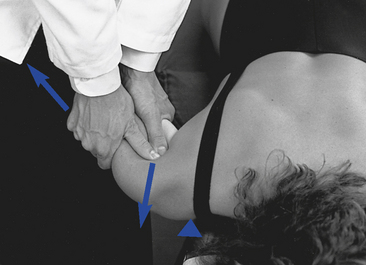
 Figure 6-55
Figure 6-55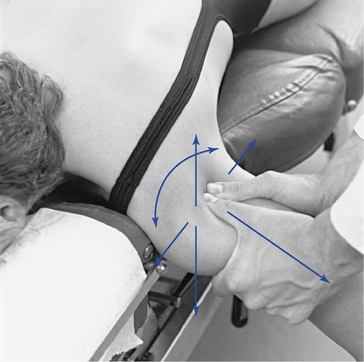
 Figure 6-56
Figure 6-56
 Figure 6-57
Figure 6-57
 Figure 6-58
Figure 6-58
 Figure 6-59
Figure 6-59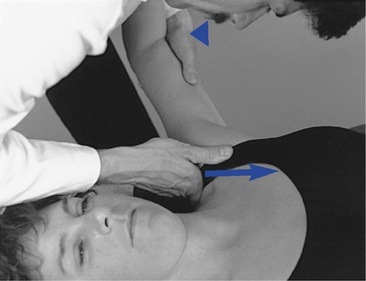
 Figure 6-60
Figure 6-60
 Figure 6-61
Figure 6-61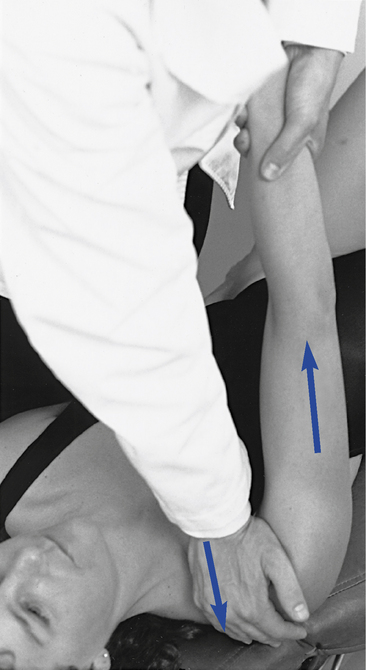
 Figure 6-62
Figure 6-62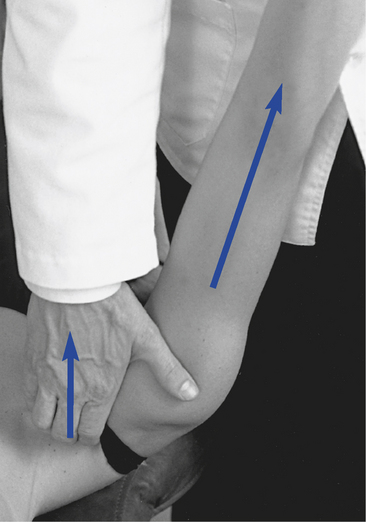
 Figure 6-63
Figure 6-63
 Figure 6-64
Figure 6-64
 Figure 6-65
Figure 6-65
 Figure 6-66
Figure 6-66
 Figure 6-67
Figure 6-67
 Figure 6-68
Figure 6-68
 Figure 6-69
Figure 6-69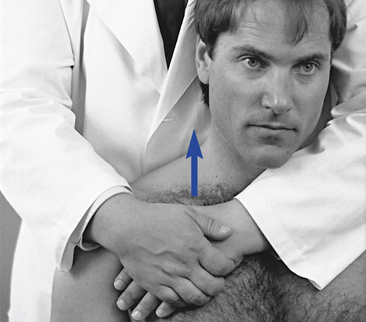
 Figure 6-70
Figure 6-70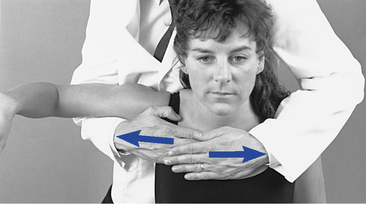
 Figure 6-71
Figure 6-71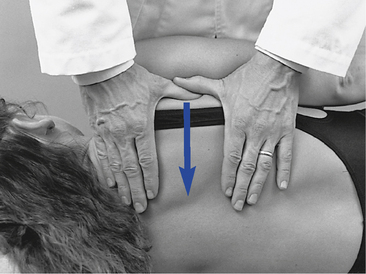
 Figure 6-72
Figure 6-72
 Figure 6-73
Figure 6-73
 Figure 6-74
Figure 6-74
 Figure 6-75
Figure 6-75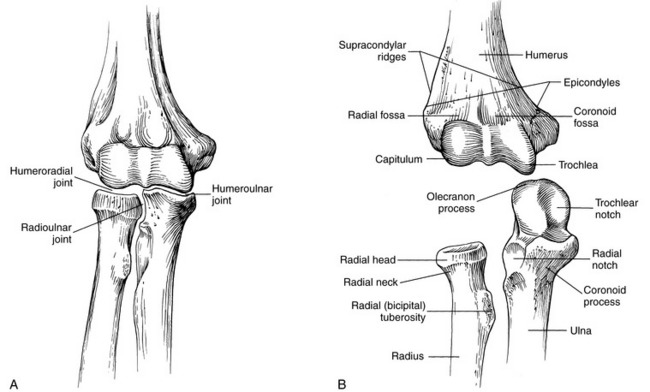
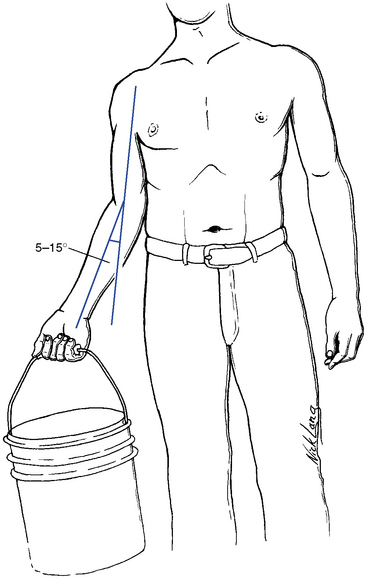
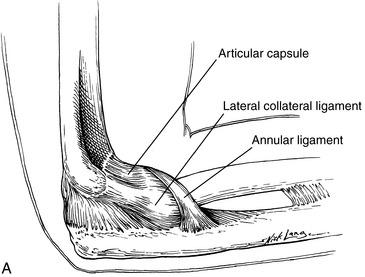
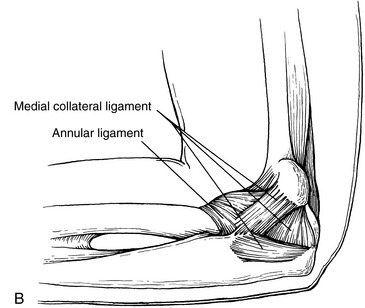
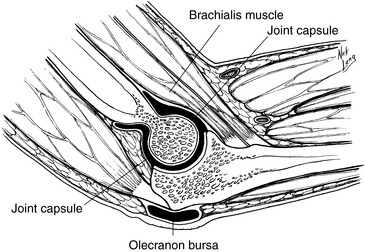
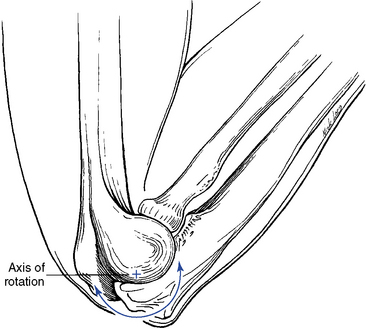

 Figure 6-85
Figure 6-85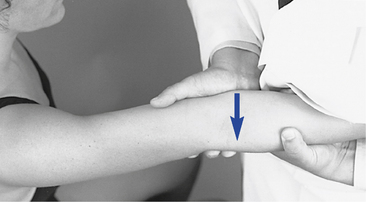
 Figure 6-86
Figure 6-86
 Figure 6-87
Figure 6-87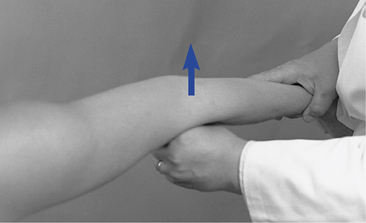
 Figure 6-88
Figure 6-88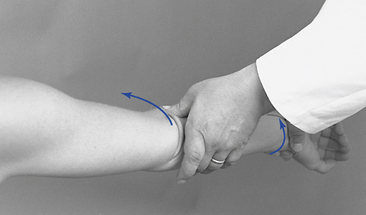
 Figure 6-90
Figure 6-90
 Figure 6-91
Figure 6-91
 Figure 6-92
Figure 6-92
 Figure 6-93
Figure 6-93
 Figure 6-94
Figure 6-94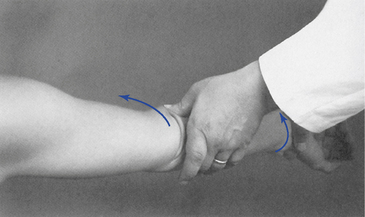
 Figure 6-95
Figure 6-95
 Figure 6-96
Figure 6-96
 Figure 6-97
Figure 6-97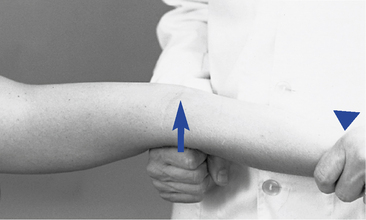
 Figure 6-98
Figure 6-98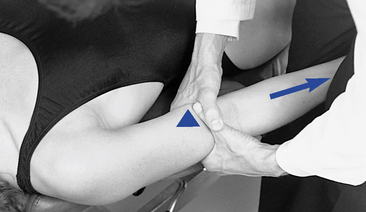
 Figure 6-99
Figure 6-99
 Figure 6-100
Figure 6-100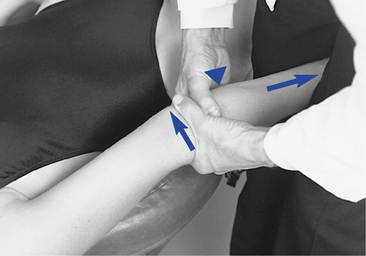
 Figure 6-101
Figure 6-101