6 HILA AND HILAR ABNORMALITIES
Assessing the hilar shadows can be difficult. Accurate assessment requires a basic understanding of the normal anatomy.
BASIC ANATOMY1,2
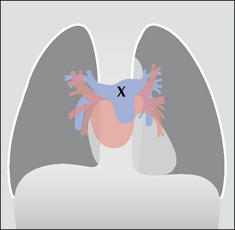
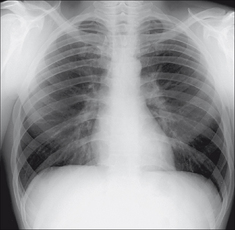
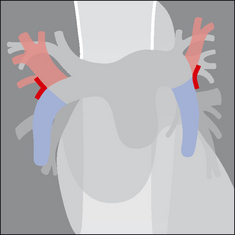
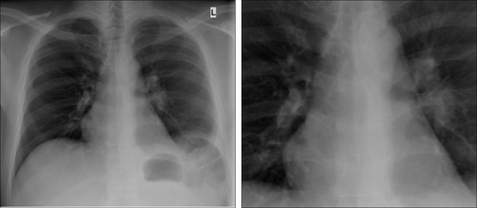
Figure 6.1 The hilar shadows are due to pulmonary arteries and pulmonary veins. X marks the main pulmonary trunk. Blue = pulmonary trunk and pulmonary arteries; brown = pulmonary veins;pink = part of left atrium…atrial appendage not shown.
 Position:
Position:
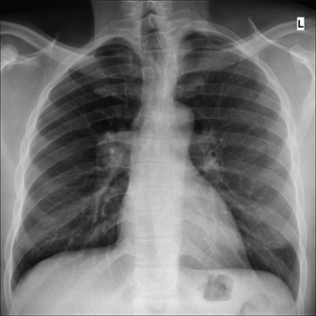
 The superior margin of the left hilum is normally higher than the right. This is because the left main pulmonary artery passes over the left main bronchus whereas the right main pulmonary artery passes in front of the right main bronchus1,2. The hila are at the same level in 5% of normal CXRs (see p. 240).
The superior margin of the left hilum is normally higher than the right. This is because the left main pulmonary artery passes over the left main bronchus whereas the right main pulmonary artery passes in front of the right main bronchus1,2. The hila are at the same level in 5% of normal CXRs (see p. 240).RELATED ADJACENT ANATOMY
 The lower lobe pulmonary arteries extend inferiorly from the hilum. Each is the size of a little finger3.
The lower lobe pulmonary arteries extend inferiorly from the hilum. Each is the size of a little finger3. On the right side: either the whole of a little finger (Fig. 6.2) or at least a (metaphorical) proximal phalanx will be visible in 94% of normal CXRs.
On the right side: either the whole of a little finger (Fig. 6.2) or at least a (metaphorical) proximal phalanx will be visible in 94% of normal CXRs. On the left side: the lower lobe pulmonary artery takes a sharp posterior course and is not always clearly identified. All the same, it appears as a little finger (or a proximal phalanx) in 62% of normal people. See Chapter 16, p. 239.
On the left side: the lower lobe pulmonary artery takes a sharp posterior course and is not always clearly identified. All the same, it appears as a little finger (or a proximal phalanx) in 62% of normal people. See Chapter 16, p. 239.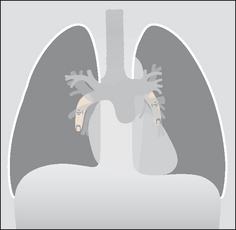
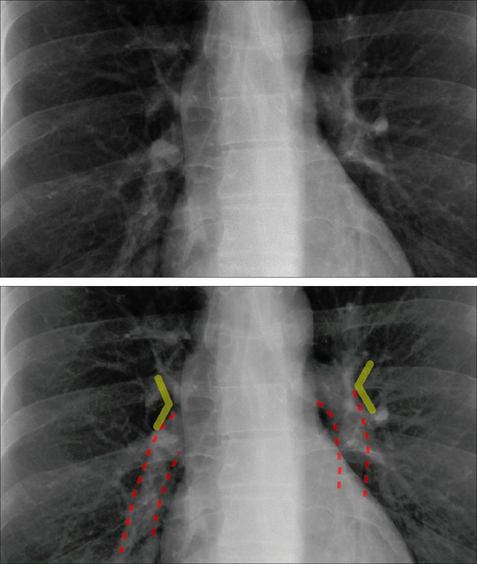
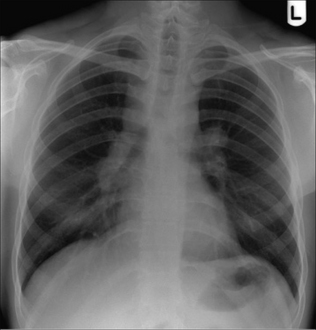
Figure 6.2 The main lower lobe pulmonary arteries can be likened to a little finger pointing downwards. Sometimes—particularly on the left side—this arterial shadow comprises only the proximal phalanx of the finger. We should see these little fingers (or at least their proximal phalanges) on virtually all normal CXRs.
Useful rule: A little finger shadow should always be looked for on both sides. If it is not identified then you should check whether there is any evidence to suggest collapse of a lower lobe (pp. 58–61).
THE HILUM—IS IT TOO HIGH OR TOO LOW?
When making this assessment, two approaches are available. In effect, both identify a similar position or site to look for, but the descriptions differ slightly. We have termed these the purist’s approach and—the one we use—the pragmatist’s approach.
PURISTS IDENTIFY THE HILAR POINT ON EACH SIDE4
On a CXR the pulmonary veins and arteries are indistinguishable from each other in the outer two-thirds of the lung. In the inner third they can be separated because of their different directions of travel. Specifically:
 Arteries radiate out from the hilum and this particular direction of travel allows them to be distinguished from the pulmonary veins. The veins run towards the left atrium.
Arteries radiate out from the hilum and this particular direction of travel allows them to be distinguished from the pulmonary veins. The veins run towards the left atrium. The main upper lobe vein converges on the left atrium and can be identified as it crosses the descending pulmonary artery. The latter is directed inferiorly and medially. This crossing position is referred to as the hilar point. The left hilar point is approximately 1 cm higher than the right.
The main upper lobe vein converges on the left atrium and can be identified as it crosses the descending pulmonary artery. The latter is directed inferiorly and medially. This crossing position is referred to as the hilar point. The left hilar point is approximately 1 cm higher than the right. Our problem: in everyday practice we find that distinguishing this vein from an artery can be difficult. Because of this difficulty we have developed a pragmatic approach when defining the level of each hilum.
Our problem: in everyday practice we find that distinguishing this vein from an artery can be difficult. Because of this difficulty we have developed a pragmatic approach when defining the level of each hilum.PRAGMATISTS CHECK THE HILAR HORIZONTAL VEES
We have always found the purist’s description of the hilar point just a little bit confusing. So we adopt a more practical approach. We look for the vee on each side as follows. First, identify the lower lobe pulmonary artery. Each lower lobe artery curls gently downwards and medially and has the approximate diameter of your little finger. Now look for the site where the most superior upper lobe vessel—either vein or artery—crosses the lateral margin of the little finger. The point of crossing forms a horizontal vee. The apex of the vee at the left hilum should be higher than the apex of the vee at the right hilum (Fig. 6.6). Occasionally, the two vees will be at the same level.
APPLIED ANATOMY—MAINLY LOBAR COLLAPSE1,2,5,6
 Whenever a left hilum appears lower than the right hilum—check whether there is other evidence suggestive of:
Whenever a left hilum appears lower than the right hilum—check whether there is other evidence suggestive of:
 If the little finger shadow of the right lower lobe artery is not seen then you must check for evidence suggesting collapse of the right lower lobe.
If the little finger shadow of the right lower lobe artery is not seen then you must check for evidence suggesting collapse of the right lower lobe. The silhouette sign. On the frontal CXR the principle of the silhouette sign(p. 45) can be applied to any mass lesion projected over a hilum. If the mass is at the hilum then it will obscure the adjacent soft tissues (i.e. the margins of the arteries at the hilum). On the other hand, if the mass is situated anterior or posterior to the hilum then the margins of the arteries at the hilum will not be obscured.
The silhouette sign. On the frontal CXR the principle of the silhouette sign(p. 45) can be applied to any mass lesion projected over a hilum. If the mass is at the hilum then it will obscure the adjacent soft tissues (i.e. the margins of the arteries at the hilum). On the other hand, if the mass is situated anterior or posterior to the hilum then the margins of the arteries at the hilum will not be obscured.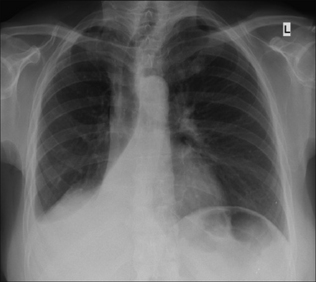
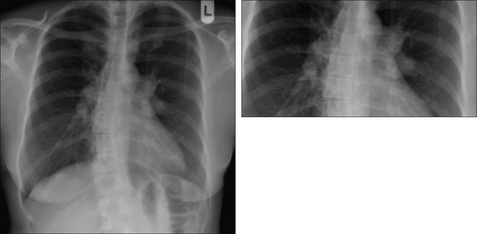
Figure 6.7 The right lower lobe is collapsed. The hilar vee site on the right side is not identified because the lower lobe pulmonary artery is now lost within the collapsed and unaerated lobe.
THE EQUIVOCAL HILUM—IS IT ENLARGED?
First—make sure that rotation is not causing one hilum to appear more conspicuous than the other. This is a very common explanation for a seemingly enlarged hilum. All the same, deciding whether a hilum is abnormal is a common problem. Even the experts have the occasional difficulty.
Second—always enquire if a previous CXR is available for comparison. If a previous CXR is not available, then ask yourself three questions. If the hilum is normal then the answer to all three questions will be “yes”.
| Question 1 | Is the left hilum in a normal position? The left hilum must never be lower than the right hilum. |
| Question 2 | Do the branches of the pulmonary artery clearly originate from the site of concern? Normal arteries can be prominent and give an initial impression that enlarged lymph nodes are present. |
| Question 3 | Are the densities of the two hila approximately equal? Anything more than a slight difference in density always raises the suspicion that there is abnormal tissue at the hilum — e.g. a hilar mass. |
If the answer to any of these three questions is in the negative, then an experienced observer should be asked to give an opinion.
WHY IS THE HILUM ENLARGED?
An enlarged hilum may be due to large nodes, tumour infiltration, or enlarged arteries (Table 6.1). These are the features to assess:
 Arterial enlargement:
Arterial enlargement:
 Compare with previous CXRs. Lack of change, or obvious interval change, will often favour a particular diagnosis.
Compare with previous CXRs. Lack of change, or obvious interval change, will often favour a particular diagnosis.Table 6.1 Synopsis: causes of hilar enlargement2,5,7,8.
| Unilateral | Bilateral |
|---|---|
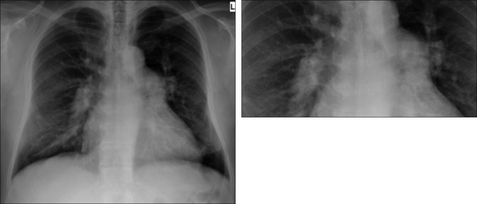
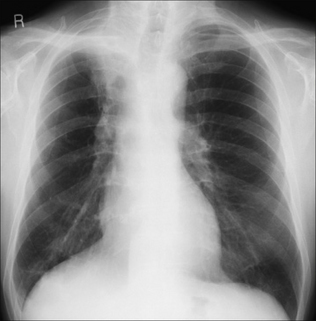
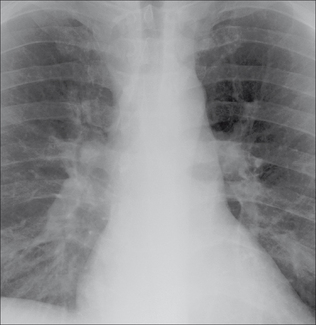
Figure 6.12 Both hila are prominent. The margins of the hilar vessels are smooth. Smaller arteries emerge and are continuous with the right and left pulmonary arteries. Pulmonary arterial hypertension.
1. Felson B. Chest Roentgenology. Philadelphia, PA: WB Saunders, 1973.
2. Fraser RG, Muller NL, Colman NC, Pare PD. Fraser and Pare’s Diagnosis of Diseases of the Chest, 4th ed. Philadelphia, PA: WB Saunders, 1999.
3. Armstrong P. Personal communication and discussion, 2007.
4. Ryan S, McNicholas M, Eustace S. Anatomy for Diagnostic Imaging, 2nd ed. Philadelphia, PA: WB Saunders, 2004.
5. Hansell DM, Armstrong P, Lynch DA, McAdams HP. Imaging of Diseases of the Chest, 4th ed. St Louis, MO: Mosby, 2005.
6. Collins J, Stern EJ. Chest Radiology: The Essentials. Philadelphia, PA: Lipincott, Williams & Wilkins, 1999.
7. Nunes H, Brillet PY, Valevre D, et al. Imaging in sarcoidosis. Semin Respir Crit Care Med. 2007;28:102-120.
8. Haramati LB, Choi Y, Widrow CA, et al. Isolated lymphadenopathy on chest radiographs of HIV infected patients. Clin Radiol. 1996;51:345-349.