CHAPTER 20 Local Anesthesia in Endodontics
Effective local anesthesia is the bedrock of pain control in endodontics. Regardless of the clinician’s skills, endodontic treatment cannot be delivered without effective pain control. This chapter reviews the pharmacology of local anesthetics and the relative advantages and limitations of various anesthetics and routes of administration. Other chapters in this book provide complementary information on the use of local anesthetics in diagnosis (see Chapter 1), the treatment of emergency patients (see Chapter 2), and the development of a comprehensive pain-control plan (see Chapter 19). The authors assume that the reader is familiar with various anesthetic injection techniques; several excellent texts are available for review regarding this point.116,158
Mechanisms of Action for Anesthetics
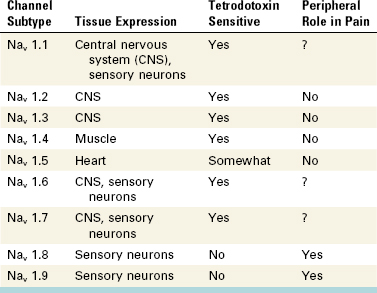
Most dental pharmacology courses teach that local anesthetics block sodium channels by partitioning into two types, the uncharged basic form of the molecule (RN), which crosses cell membranes, and the charged acid form of the molecule (RNH+), which binds to the inner pore of the sodium channel. As a first approximation, this model is reasonably accurate. However, molecular research has demonstrated the existence of at least nine subtypes of voltage-gated sodium channels (VGSCs) that differ in their expression pattern, biophysical properties, and roles in mediating peripheral pain (Table 20-1). These channels have a clear clinical relevance.18,101,143
The broad class of VGSCs can be divided into channels that are blocked by a toxin (tetrodotoxin [TTX]) and those that are resistant to the toxin (TTX-R). Most TTX-R channels are found primarily on nociceptors (e.g., Nav 1.8 and Nav 1.9).273 These channels also are relatively resistant to local anesthetics216 and are sensitized by prostaglandins.83 As is explained later in the chapter, the presence of TTX-R sodium channels may explain why local anesthetics are less effective when injected into patients with odontalgia. Moreover, the sensitization of these channels by prostaglandins suggests that rapid-acting nonsteroidal antiinflammatory drugs (NSAIDs) may be useful as a pretreatment to enhance the efficacy of local anesthetics in patients with odontogenic pain112,179 (see Chapter 19). Many of the adverse effects of local anesthetics are attributed to their ability to block other VGSCs expressed in the central nervous system (CNS) or heart (see Table 20-1).
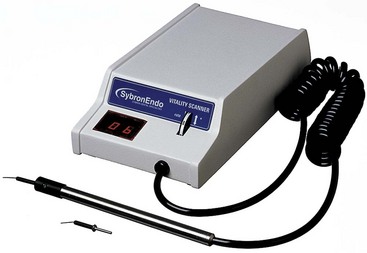
VGSCs consist of an alpha (α) and a beta (β) subunit. The α subunit serves as a voltage sensor, leading to channel activation and sodium ion passage when the channel detects an electrical field. The biologic basis for an electrical pulp tester, therefore, is the generation of a small electrical field across the dental pulp that can activate VGSCs.101 Interestingly, sensitization of TTX-R channels by prostaglandins lowers the activation threshold and increases the amount of sodium ions that flow through the channel.83 Put another way, an inflammation-induced elevation in prostaglandin levels sensitizes TTX-R channels, leading to depolarization at lower levels of stimulus strengths. This may explain the increased responsiveness to electrical pulp testing seen in patients with irreversible pulpitis.
Local anesthetics have other mechanisms that may contribute to their pharmacology for treating odontogenic pain. For example, local anesthetics modulate certain G protein–coupled receptors (GPCRs). The GPCRs are a major class of cell membrane receptors, and many classes of dental drugs (e.g., opioids, catecholamines) and endogenous mediators produce their effects by activating specific GPCRs and their related second messenger pathways. Studies suggest that local anesthetics inhibit the G-alpha-q (Gαq) class of GPCRs, which includes receptors activated by inflammatory mediators such as bradykinin.108 Local anesthetics may therefore block the actions of a major hyperalgesic agent.
Other studies have indicated that local anesthetics potentiate the actions of the G-alpha-i (Gαi) class of GPCRs.11 This could have a major effect in potentiating the actions of vasoconstrictors, including the newly recognized analgesic role that vasoconstrictors play in inhibiting pulpal nociceptors.20,100 Prolonged alteration of GPCR function might explain why analgesia obtained with long-acting local anesthetics persists well beyond the period of anesthesia.40,55,185 More research is needed on this exciting aspect of local anesthetic pharmacology.
Clinically Available Local Anesthetics
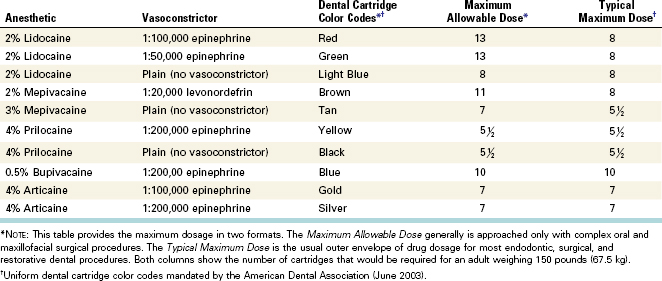
The most common forms of injectable local anesthetics are in the amide class. In 2003, the American Dental Association specified a uniform color code for dental cartridges to prevent confusion among brands (see www.ada.org/prof/resources/topics/color.asp) (Table 20-2). Local anesthetics can be divided roughly into three types: short duration (30 minutes of pulpal anesthesia), intermediate duration (60 minutes of pulpal anesthesia), and long duration (over 90 minutes of pulpal anesthesia). However, clinical anesthesia does not always follow these guidelines, depending on whether the local anesthetic is used as a block or for infiltration. For example, bupivacaine is classified as a long-acting agent, and when it is used in an inferior alveolar nerve (IAN) block, this is true.58 But when it is used for infiltration for anterior teeth, it has a shorter duration of anesthetic action than 2% lidocaine with 1:100,000 epinephrine43,90 (discussed in more detail later in the chapter).
Selection of a Local Anesthetic: Possible Adverse Effects, Medical History, Preoperative Anxiety
Possible Adverse Effects
Possible adverse reactions to local anesthetics can be divided into six major categories: cardiovascular reactions, systemic effects, methemoglobinemia, peripheral nerve paresthesia, allergic reactions to the anesthetic and/or latex, and reactions to anesthetics containing a sulfite antioxidant. These reactions range from fairly common (e.g., tachycardia after intraosseous injection of 2% lidocaine with 1:100,000 epinephrine) to extremely rare (e.g., allergic reactions to lidocaine).
Cardiovascular Reactions
Although classic research studies have reported that large dosages or intravenous (IV) injections of local anesthetics were required to produce cardiovascular effects,114,262 it now is well recognized that even comparatively small amounts of epinephrine can induce measurable tachycardia after nerve block or intraosseous injection.59,85,220 Several authors have reported increases in heart rate with infiltration injections and nerve blocks using 2% lidocaine with 1:100,000 epinephrine1,102,140,234,261; others have reported that no significant changes in heart rate occurred or that the changes were clinically insignificant.173,260,264 When specific information was given on dosing and heart rate increases, several studies found mean heart rate increases.1,102,139,261 Two studies found increases on average of about 4 beats/min with approximately 20 µg of epinephrine102,139; three studies recorded increases of 10 to 15 beats/min with 45 to 80 µg of epinephrine1,139,234; and one study found increases of approximately 21 beats/min using 144 µg of epinephrine.261 Increasing the amount of epinephrine in an infiltration or block injection therefore increases the likelihood of an elevated heart rate.
Tachycardia after injection is primarily a pharmacologic effect. The cardiovascular effects are the result of α-adrenoceptor stimulation by systemic distribution of the vasoconstrictor throughout the vascular compartment. The patient may also report heart palpitations associated with anxiety or fear and may experience transient tachycardia and changes in blood pressure. Large doses or inadvertent IV injection may lead to lidocaine toxicity and CNS depression.61,189 To reduce this risk, the clinician should always aspirate before making the injection, inject slowly, and use dosages within accepted guidelines. The maximal dosages for local anesthetics are listed in Table 20-2.
Systemic Effects
The acute toxicity of an overdose of a local anesthetic often is the result of inadvertent IV administration or of a cumulative large dose (e.g., repeated injections). As shown in Table 20-1, VGSCs are found in the CNS and the myocardium, the two major areas of anesthetic-induced toxicity. Although systemic effects from a local anesthetic are rare, they can include an initial excitatory phase (e.g., muscle twitching, tremors, grand mal convulsions) and a subsequent depressive phase (e.g., sedation, hypotension, and respiratory arrest).48,61 It should be noted that symptomatic management (possibly including cardiopulmonary resuscitation [CPR], airway support, and supplemental oxygen) is the primary response to this adverse event.135,137 An acute hypotensive crisis with respiratory failure also has been interpreted as the result of hypersensitivity to local anesthetics30; these patients should be evaluated with allergy testing. To reduce the risk of systemic effects from anesthetics, the clinician must always aspirate before giving the injection and must use dosages within accepted guidelines (see Table 20-2). Finder and Moore61 proposed a “rule of 25” as a simple means of remembering maximal local anesthetic dosages: with currently formulated local anesthetic cartridges, it generally is safe to use one cartridge of local anesthetic for every 25 pounds of patient weight (e.g., six cartridges for a patient weighing 150 pounds [67.5 kg]).
Methemoglobinemia
Metabolism of certain local anesthetics (e.g., prilocaine, benzocaine, articaine, and to a lesser extent lidocaine) can produce a metabolite that causes methemoglobinemia; this effect often occurs several hours after injection of the local anesthetic.162,276 Typical signs and symptoms include cyanosis, dyspnea, emesis, and headache. In a study on benzocaine-induced methemoglobinemia, 67% of reported adverse effects of benzocaine were associated with methemoglobinemia; of these events, 93% occurred with spray formulations of benzocaine, and only one case involved the gel formulation.186 To reduce the risk of methemoglobinemia, clinicians should take care to refrain from giving excessive dosages of local anesthetics.
Peripheral Nerve Paresthesia
Postinjection paresthesia is a rare adverse effect of local anesthetics.96,162,282 A retrospective study reported that articaine is associated with a fivefold higher incidence of paresthesia compared with lidocaine.96 A recent study evaluated patients referred with a diagnosis of damage to the inferior alveolar and/or lingual nerve which could only have resulted from an IAN block.212 Thirty-five percent were caused by a lidocaine formulation, and 30% were caused by an articaine formulation. The conclusion was that there was not a disproportionate nerve involvement from articaine. However, with any paresthesia, documentation of the patient’s reported area of altered sensation, the type of altered sensation (e.g., anesthesia, paresthesia, dysesthesia), and regular follow-up are important.
Allergic Reactions to Local Anesthetics and Latex
The amide local anesthetics appear to have little immunogenicity and therefore have an extremely low rate of allergic reactions.239 One study included more than 140 patients specifically referred for allergy testing because of adverse effects after injection of a local anesthetic; none of these patients had hypersensitivity reactions to intradermal local anesthetics,228 but case reports of hypersensitivity reactions after administration of local anesthetics have been published.19,30,187,239 Some concern has been raised that the rubber latex stopper in dental anesthetic cartridges might be a source of allergen to patients allergic to latex. In a review of this literature (1966 to 2001), Shojaei and Haas241 concluded that some evidence for exposure to the latex allergen exists, although no causal study has been published.
Reactions to Anesthetic Formulations Containing a Sulfite Antioxidant
Local anesthetic formulations that contain vasoconstrictors also contain sulfite to prevent oxidation of this agent. Sulfite-induced reactions came to prominence with the report of six deaths after exposure to salad bars or homemade wine.6 Common reported signs and symptoms include allergic-like reactions such as urticaria, bronchospasm, and anaphylaxis. Risk factors include an active history of asthma (perhaps 5% of asthmatics are at risk) and atopic allergy. The use of local anesthetics without vasoconstrictors is a possible alternative with these patients. No sulfite reaction in dental practice has ever been documented, possibly because the amount of sulfite in local anesthetic cartridges is relatively small.
Effects of Systemic Diseases or Conditions on Local Anesthetics
Several systemic diseases or disorders may require modification of the dosage of local anesthetic. Cardiac patients (e.g., those with unstable angina pectoris, history of myocardial infarction or stroke within the past 6 months, severe hypertension, uncontrolled congestive heart failure, or heart transplant) should not receive a local anesthetic containing a vasoconstrictor and should consult their physicians before undergoing endodontic treatment.189 A review suggests that patients with Hodgkin’s disease or breast cancer who have received radiation treatment to the chest are at risk for radiation-induced coronary artery disease, and this condition also may require medical consultation regarding a reduced dosage of local anesthetic containing a vasoconstrictor.65
Alcoholics have been found to be more sensitive to painful stimulation.254 Alcoholics with a history of depression/unhappiness may also have shallower pulpal anesthesia.62 In contrast, alcoholics in recovery may not be at increased risk for inadequate pain control with local anesthesia.62
Any of the commonly available local anesthetics are safe for use in pregnant or lactating women.97 The most important aspect of care with pregnant patients is to eliminate the source of pain by performing the indicated endodontic treatment; this reduces the need for systemic medications.97
Local anesthetics may interact with a patient’s medications, so a thorough review of the medical history is an absolute requirement. Potential drug-drug interactions occur primarily with the vasoconstrictors in local anesthetic formulations (Table 20-3). Judicious use of local anesthetic solutions without vasoconstrictors (e.g., 3% mepivacaine) is a reasonable alternative for adult patients.
TABLE 20-3 Possible Drug Interactions With Vasoconstrictors
| Drugs | Possible Adverse Effects | Recommendations |
|---|---|---|
| TRICYCLIC ANTIDEPRESSANTS | ||
| Amitriptyline, doxepin | Increased cardiovascular responses | Reduce or eliminate vasoconstrictors |
| NONSELECTIVE β-BLOCKERS | ||
| Nadolol, propranolol | Hypertension, bradycardia | Reduce or eliminate vasoconstrictors |
| RECREATIONAL DRUGS | ||
| Cocaine | Hypertension, myocardial infarction, dysrhythmias | Instruct patient to abstain from drug use for 48 hours before procedure; do not use vasoconstrictors |
| COMT INHIBITORS | ||
| Entacapone, tolcapone | Increased cardiovascular responses | Reduce or eliminate vasoconstrictors |
| ANTIADRENERGIC DRUGS | ||
| Guanadrel, guanethidine | Increased cardiovascular responses | Reduce or eliminate vasoconstrictors |
| NONSELECTIVE α-ADRENERGIC BLOCKERS | ||
| Chlorpromazine, clozapine, haloperidol | Increased cardiovascular responses | Reduce or eliminate vasoconstrictors |
| DIGITALIS | ||
| Digoxin | Dysrhythmias (especially with large dosage of vasoconstrictor) | Reduce or eliminate vasoconstrictor |
| THYROID HORMONES | ||
| Levothyroxine | Dysrhythmias (especially with large dosage of vasoconstrictor) | Euthyroid: No precaution Hyperthyroid: Reduce or eliminate vasoconstrictors |
| MONOAMINE OXIDASE35 INHIBITORS | ||
| Furazolidone, linezolid, selegiline, tranylcypromine | No interaction | None |
Modified from Naftalin L, Yagiela JA: Vasoconstrictors: indications and precautions. Dent Clin North Am 46:733, 2002.
Authors have found that women try to avoid pain more than men, accept it less, and fear it more.51,60,147,188 A study found women find postsurgical pain more intense than males, but men are more disturbed than women by low levels of pain that lasts several days.188 Another study found gender differences in analgesia for postoperative endodontic pain.233 Anxiety may also modulate differences in pain responses between males and females. We should be aware that women might react differently to pain than men.60
Clinical Anesthesia and Routes of Administration
Recognition is growing that evidence-based therapeutics offers an excellent source of information that should become an aspect of treatment in conjunction with the practitioner’s clinical skills and the patient’s particular needs. In many areas of dentistry, this is a limited concept because few randomized, placebo-controlled, double-blind clinical trials have been conducted. However, this is not the case with dental pharmacology. The astute clinician can make informed decisions on various local anesthetics and routes of injection based on a large collection of well-designed clinical trials. The following discussion focuses on the clinical aspects of local anesthesia, with special emphasis on endodontics.
Important Clinical Factors in Local Anesthesia
Traditional Methods of Confirming Anesthesia
Traditional methods of confirming anesthesia usually involve questioning the patient (“Is your lip numb?”), soft-tissue testing (e.g., lack of mucosal responsiveness to a sharp explorer), or simply beginning treatment. However, these approaches may not be effective for determining pulpal anesthesia.28,106,169,266 Moreover, from a research perspective, they provide only bimodal responses (e.g., yes or no) and therefore are of little use for detecting parametric differences between anesthetics or routes of injection.
Determining Pulpal Anesthesia in Painless Vital Teeth
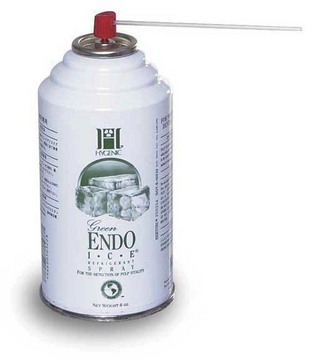
Anesthesia in painless vital teeth can be measured more objectively by applying a cold refrigerant (Fig. 20-1) or by using an electric pulp tester (EPT; Fig. 20-2). Application of cold or the electric pulp tester can be used to test the tooth under treatment for pulpal anesthesia before a clinical procedure is started.26,52,120,154
Determining Pulpal Anesthesia in Painful Vital Teeth
In painful vital teeth and after administration of local anesthesia, the cold test or electric pulp tester can be used to test for pulpal anesthesia before an endodontic procedure is started.36,52,200,217 If the patient responds to the stimulus, pulpal anesthesia has not been obtained, and supplemental anesthesia should be administered. However, in painful vital teeth (e.g., irreversible pulpitis), the lack of a response to pulp testing may not guarantee pulpal anesthesia.52,200,217 Therefore, if a patient experiences pain when the endodontic procedure is started, supplemental anesthesia is indicated regardless of the responsiveness to pulpal testing. If the chamber is necrotic and the canals are vital, no objective test can predict the level of clinical anesthesia.
Patient Who Has Had Previous Difficulty With Anesthesia
Anesthesia is more likely to be unsuccessful in patients who report a history of previous difficulty with anesthesia.129 These patients generally make comments such as “Novocaine doesn’t work on me” or “It takes a lot of shots to get my teeth numb.” A good clinical practice is to ask the patient if dentists previously have had difficulty obtaining anesthesia in the individual’s mouth. If the answer is yes, supplemental injections should be considered.
Failure to Achieve Anesthesia in Patients With Pain
Obtaining anesthesia often is difficult in patients with endodontic pain who have pulpal pathosis. A number of explanations have been proposed for this.101 One is that conventional anesthetic techniques do not always provide profound pulpal anesthesia, and patients with preexisting hyperalgesia may be unable to tolerate any noxious input. Another explanation relates to the theory that inflamed tissue has a lower pH, which reduces the amount of the base form of anesthetic that penetrates the nerve membrane. Consequently, less of the ionized form is available in the nerve to achieve anesthesia. This explanation does not account for the mandibular molar with pulpitis that is not readily blocked by an inferior alveolar injection administered at some distance from the area of inflammation. Correlating localized inflammatory changes with failure of the IAN block is difficult.
Another explanation for failure is that nerves arising from inflamed tissue have altered resting potentials and decreased excitability thresholds.24,268 Two studies demonstrated that local anesthetics were unable to prevent impulse transmission because of these lowered excitability thresholds.180,268 Another factor might be the TTX-R sodium channels, which are resistant to the action of local anesthetics232 and are increased in inflamed dental pulp.271,273 A related factor is the increased expression of sodium channels in pulps diagnosed with irreversible pulpitis.250,271,273
Finally, patients in pain often are apprehensive, which lowers the pain threshold. Therefore practitioners should consider supplemental techniques (e.g., intraosseous injections197,200,206,217 or periodontal ligament injections36) if an IAN block fails to provide pulpal anesthesia for patients with irreversible pulpitis.
Use of Topical Anesthetics
Fear of needle insertion is a major cause of apprehension in dental patients.138,177,178 Although some studies have demonstrated the effectiveness of topical anesthetics,102,108,192,215 others have shown no significant pain reduction.82,131,163 Interestingly, one study showed that patients who thought they were receiving a topical anesthetic anticipated less pain regardless of whether they actually received the anesthetic.163 The most important aspect of a topical anesthetic may not be its clinical effectiveness but rather its psychologic effect on the patient who believes the practitioner is doing everything possible to prevent pain.
Reversing the Action of Local Anesthesia
Phentolamine mesylate (0.4 mg in a 1.7 ml cartridge, OraVerse, Novalar Pharmaceuticals, San Diego, CA) is a recently developed agent that shortens the duration of soft-tissue anesthesia. The duration of soft-tissue anesthesia is longer than pulpal anesthesia and is often associated with difficulty eating, drinking, and speaking.104,144 The greatest value of using OraVerse is in the majority of dental procedures where postoperative pain is not of concern. However, some endodontic patients may benefit from the use of a reversal agent when they have speaking engagements, important meetings, or perform in musical or theatrical events. OraVerse may be used to shorten the duration of soft-tissue anesthesia if the patient presents with an asymptomatic tooth and little postoperative pain is anticipated.
Mandibular Anesthesia with 2% Lidocaine and 1:100,000 Epinephrine
Because failure occurs most often with the IAN block,129 factors that modify mandibular anesthesia must be carefully reviewed. The technique for administering an IAN block can be reviewed in available textbooks.116,158 This discussion reviews the expected outcomes after administration of a conventional IAN block to asymptomatic patients using 1.8 ml of 2% lidocaine with 1:100,000 epinephrine (Xylocaine, Lignospan, Octocaine). Although anesthesia requirements vary among dental procedures, the following discussion concentrates on pulpal anesthesia.
Anesthetic Success
One way to define anesthetic success is the percentage of subjects who achieve two consecutive 80 readings on electric pulp testing within 15 minutes and continuously sustain this lack of responsiveness for 60 minutes. In other words, the objective is to achieve anesthesia within 15 minutes and to have it last 1 hour. This endpoint is as important for restorative dentistry as it is for endodontic treatment, so it is used as a benchmark for clinically significant information from research on local anesthetics. Using this criterion, the percentage of cases in which anesthesia was obtained after IAN block injections ranged from 35% (lateral incisor) to 60% (first premolar and first molar).* It is important to note that all patients from these studies reported a positive lip sign (e.g., profound lip numbness); therefore profound lip numbness does not predict pulpal anesthesia. However, lack of soft-tissue anesthesia is a useful indicator that the block injection was not administered accurately for that patient. Missed blocks occur in about 5% of cases, and the clinician should readminister the nerve block before continuing with treatment.
Anesthetic Failure
Anesthetic failure can be defined as the percentage of subjects who never achieved two consecutive 80 EPT readings at any time during a 60-minute period. Using this criterion, anesthetic failure ranged from 11% (first premolar) to 32% (lateral incisor).†
Noncontinuous Anesthesia
Another measure of mandibular anesthesia is noncontinuous anesthesia, which may be related to the action of the anesthetic solution on the nerve membrane (blocking and unblocking the sodium channels). This occurs in about 12% to 20% of cases in mandibular teeth.*
Slow Onset
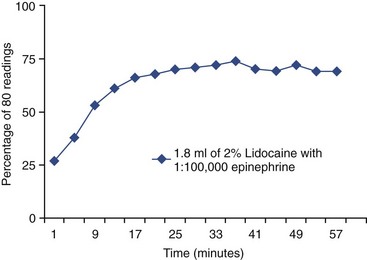
After a conventional IAN block injection, the onset of pulpal anesthesia occurs within 10 to 15 minutes in most cases (Fig. 20-3).† Slow onset can be defined as the percentage of subjects who achieved an 80 EPT reading after 15 minutes. In mandibular teeth, slow onset occurs in 19% to 27% of patients.
Duration
The duration of action for pulpal anesthesia in the mandible is very good.‡ If patients are anesthetized initially, anesthesia usually persists for approximately  hours.58 Fig. 20-3 depicts the time course for complete pulpal anesthesia for an asymptomatic first molar, as defined by the percentage of patients who did not respond to an 80 stimulus (EPT) across time for 60 minutes. Most patients achieved pulpal anesthesia within 15 minutes and had a duration of anesthesia of at least 1 hour, but the success rate was not 100% for the population.
hours.58 Fig. 20-3 depicts the time course for complete pulpal anesthesia for an asymptomatic first molar, as defined by the percentage of patients who did not respond to an 80 stimulus (EPT) across time for 60 minutes. Most patients achieved pulpal anesthesia within 15 minutes and had a duration of anesthesia of at least 1 hour, but the success rate was not 100% for the population.
Alternative Anesthetic Solutions for the Inferior Alveolar Nerve Block
Plain Solutions: 3% Mepivacaine (Carbocaine, Polocaine, Scandonest) and 4% Prilocaine (Citanest Plain)
In a study of volunteers without dental pathosis, anesthesia from IAN injection of 3% mepivacaine plain and 4% prilocaine plain were as effective as 2% lidocaine with 1:100,000 (Fig. 20-4).169 A clinical study of patients with irreversible pulpitis also found that 3% mepivacaine and 2% lidocaine with 1:100,000 epinephrine were equivalent for IAN blocks.36 These findings support the selection of 3% mepivacaine as a local anesthetic when medical conditions or drug therapies suggest caution in the administration of solutions containing epinephrine.
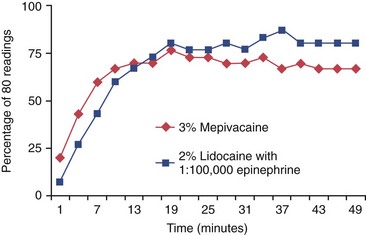
FIG. 20-4 Incidence of first mandibular molar anesthesia: comparison of 3% mepivacaine to 2% lidocaine with 1:100,000 epinephrine. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 50 minutes. No significant difference between the two solutions was noted.
4% Prilocaine With 1:200,000 Epinephrine (Citanest Forte) and 2% Mepivacaine With 1:20,000 Levonordefrin (Carbocaine With Neo-Cobefrin)
In a study of volunteers without dental pathosis, IAN injection of 4% prilocaine with 1:200,000 epinephrine or 2% mepivacaine with 1:20,000 levonordefrin worked as well as 2% lidocaine with 1:100,000 in achieving pulpal anesthesia.106
Levonordefrin has 75% α activity and only 25% β activity, making it seemly more attractive than epinephrine (50% α activity and 50% β activity).158 However, levonordefrin is marketed as a 1:20,000 concentration in dental cartridges.158 Clinically, the higher concentration of levonordefrin makes it equipotent to epinephrine in clinical and systemic effects,92,106 so 1:20,000 levonordefrin offers no clinical advantage over 1:100,000 epinephrine.
Articaine With 1:100,000 Epinephrine (Septocaine)
Articaine has been reported to provide very effective local anesthesia.236 It was approved for use in the United States in April 2000 and is marketed as Septocaine (Septodont, New Castle, DE) and as a 4% solution with either 1:100,000 or 1:50,000 epinephrine.162,184 Articaine is classified as an amide. It has a thiophene ring (instead of a benzene ring, as do the other amide local anesthetics) and an extra ester linkage, which results in hydrolysis of articaine by plasma esterases.162 A number of studies have evaluated articaine and concluded that it is safe when used in appropriate doses.* Lidocaine and articaine have the same maximal dose of 500 mg for adult patients (recommended dose: 6.6 to 7 mg/kg), but the maximum number of cartridges is different because of the differences in drug concentration (see Table 20-2).158
Clinical Effectiveness of Articaine for Inferior Alveolar Nerve Blocks
The available literature indicates that articaine is equally effective when statistically compared to other local anesthetics.† When comparing the anesthetic efficacy of 4% articaine with 1:100,000 epinephrine to 2% lidocaine with 1:100,000 epinephrine for IAN blocks, one study found that the two solutions were not significantly different (Fig. 20-5).176 Two studies found no difference in efficacy between 4% articaine with 1:100,000 and 1:200,000 epinephrine.184,259 Another study compared the anesthetic efficacy of 4% articaine with 1:100,000 epinephrine to 2% lidocaine with 1:100,000 epinephrine for IAN blocks in patients experiencing irreversible pulpitis, in mandibular posterior teeth.32 The success rate (none or mild pain upon endodontic access or initial instrumentation) for the IAN block using the articaine solution was 24% and for the lidocaine solution success was 23%. There was no significant difference between the articaine and lidocaine solutions. Neither solution resulted in an acceptable rate of anesthetic success in mandibular posterior teeth. In summary, repeated clinical trials have failed to demonstrate any statistical superiority of articaine over lidocaine for nerve blocks.
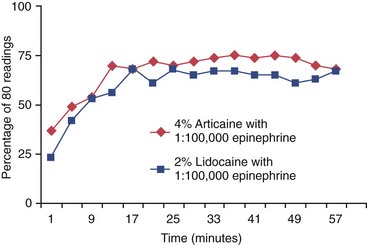
FIG. 20-5 Incidence of first mandibular molar anesthesia: comparison of 4% articaine with 1:100,000 epinephrine to 2% lidocaine with 1:100,000 epinephrine. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 60 minutes. No significant difference between the two solutions was noted.
Articaine and Uncorroborated Insurance Carrier Warning
A letter was sent to thousands of U.S. dentists in 2006 by insurer Emery and Webb/Ace USA stating, “…we have noticed an increase in reversible and, in some cases, nonreversible paresthesias (with Septocaine) … We are writing you to alert you to these events in hopes that you will not fall victim to one of these incidents.”156 Knowledgeable dentists and educators communicated their concerns, and a Notice of Retraction was issued:
Unfortunately, we at Emery & Webb discovered upon further review, and subsequent to the mailings, that both documents contained inaccuracies and an alarmist tone, which was not warranted … Emery and Webb has not noted an increase in malpractice claims or lawsuits in connection with articaine … It should be made clear that Emery and Webb has not conducted any scientific investigation, sampling, testing, or other investigation of the articaine anesthetic, and has no independent knowledge or data which would restrict the use of the product.156
Astute clinicians should be very careful of Web chat sites and colleagues’ clinical endorsements, because they may not accurately reflect the correct information regarding articaine.
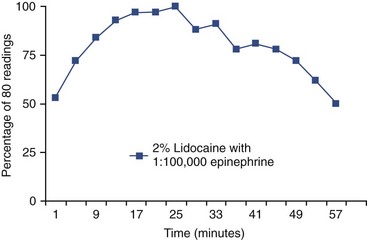
Long-Acting Anesthetics
Clinical trials with bupivacaine (Marcaine) and etidocaine (Duranest) have been done in patients undergoing oral surgery,46,230 endodontic treatment,55,185 and periodontic treatment.40,151 Etidocaine was recently withdrawn from the market by DENTSPLY Pharmaceuticals (York, PA). Bupivacaine provides prolonged analgesia and is indicated when postoperative pain is anticipated, but not all patients want lip numbness for an extended period.230 Patients should be questioned about their preference. Bupivacaine has a somewhat slower onset than lidocaine, but its duration of pulpal anesthesia in the mandible is almost twice as long (approximately 4 hours; Fig. 20-6).58
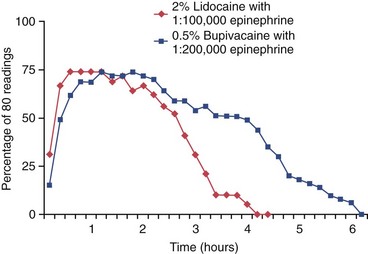
FIG. 20-6 Incidence of first mandibular molar anesthesia: comparison of 0.5% bupivacaine with 1:200,000 epinephrine to 2% lidocaine with 1:100,000 epinephrine. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 6 hours. The bupivacaine solution showed a longer duration of anesthesia than the lidocaine solution.
Ropivacaine (Naropin), a relatively new long-acting local anesthetic, is a structural homolog of bupivacaine.132 A number of studies have shown that ropivacaine has a lower potential for toxic CNS and cardiovascular effects than bupivacaine but produces equivalent pharmacologic effects.132 Ropivacaine and levobupivacaine are being developed as potentially new local anesthetics based on their stereochemistry. Both are S-isomers and are thought to cause less toxicity than the racemic mixture of bupivacaine currently marketed.245 A clinical trial has indicated that levobupivacaine showed significantly better postoperative pain control at 4 and 24 hours after infiltration injection than ropivacaine.205 Because of their decreased potential for cardiac and CNS toxicity, ropivacaine and levobupivacaine may replace bupivacaine with epinephrine in clinical dental practice.
Alternative Injection Sites
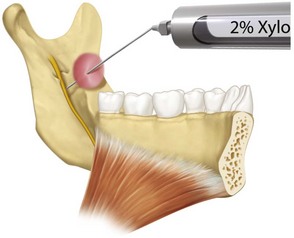
Gow-Gates and Vazirani-Akinosi Techniques
Some clinicians have reported that the Gow-Gates technique88 has a higher success rate than the conventional IAN block injection,157,158 but controlled experimental studies have failed to show superiority of the Gow-Gates technique.2,84,182,258 Neither has the Vazirani-Akinosi technique3,84,158 been found superior to the standard inferior alveolar injection.84,164,246,258,288 In a small study of 21 patients, no difference was found between lidocaine (11 patients) and articaine (10 patients) formulations for the Gow-Gates injection in patients with irreversible pulpitis.240 These techniques do not replace the conventional IAN block. The Vazirani-Akinosi technique is indicated for cases involving a limited mandibular opening.
Incisive Nerve Block at the Mental Foramen
The incisive nerve block alone is successful for anesthetizing the premolar teeth,121,193,275 but it does not anesthetize the central and lateral incisors.193 A slow injection (60 seconds) did not increase success over a fast injection (15 seconds).275 The combination of an incisive nerve block and an IAN block increases success of anesthetization of mandibular first molars, but an intraosseous or PDL injection is a better choice for supplemental anesthesia of the first molar if the IAN block fails.193
Infiltration Injections of a Lidocaine Solution
Labial or lingual infiltration injections alone are not very effective for obtaining pulpal anesthesia in mandibular teeth.94,95,286 A combination of labial and lingual infiltration significantly increases success in anterior teeth over either labial or lingual infiltration alone.172 Adding a labial infiltration (1.8 ml of 2% lidocaine with 1:100,000 epinephrine) to a conventional IAN injection increases the success of pulpal anesthesia in mandibular anterior teeth but not in the mandibular first molar.33,64
Mandibular First Molar Infiltration Injections of an Articaine Solution
Four studies showed articaine was significantly better than lidocaine for a primary buccal infiltration of the mandibular first molar.38,122,124,225 Success rates (two consecutive 80 readings with the electric pulp tester) of 64%, 54%, 64% to 70%, and 87% were recorded for an articaine formulation in these studies. However, the duration of pulpal anesthesia declined over 60 minutes.
Mandibular First Molar Infiltration Injections of an Articaine Solution Following an Inferior Alveolar Nerve Block
A recent study found 4% articaine with 1:100,000 epinephrine resulted in a higher success rate (88%) than 2% lidocaine with 1:100,000 epinephrine (71% success rate) for mandibular first molar buccal infiltrations following an IAN block.98 Success was defined as achieving two consecutive 80 readings within 10 minutes following the IAN block plus infiltration injections, and the 80 reading was continuously sustained through the 60th minute. The finding is important to dentists and patients because we now have a way to help anesthetize the mandibular first molar when the IAN block fails in asymptomatic patients.
Attempts to Increase Success of the Inferior Alveolar Nerve Block
Increasing the Volume of Anesthetic
A possible method for increasing anesthetic success is to double the injection volume of local anesthetic solution. However, increasing the volume of 2% lidocaine with epinephrine to 3.6 ml (two cartridges) does not increase the incidence of pulpal anesthesia with the IAN block (Fig. 20-7).*
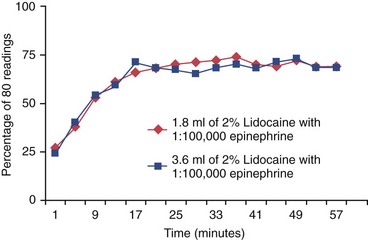
FIG. 20-7 Incidence of first mandibular molar anesthesia: comparison of 3.6 ml and 1.8 ml of 2% lidocaine with 1:100,000 epinephrine. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 60 minutes. No significant difference between the two volumes was noted.
Increasing the Epinephrine Concentration
A second approach for increasing the success of the IAN block is to increase the concentration of epinephrine. However, when this technique was evaluated in clinically normal teeth, no advantage was seen in using a higher concentration (1:50,000) of epinephrine.42,267
Addition of Hyaluronidase
Hyaluronidase reduces the viscosity of the injected tissue, permitting a wider spread of injected fluids.7 Early studies in dentistry found that an IAN block was more easily attained and was more complete when hyaluronidase was added to an anesthetic solution.136,155 However, a controlled clinical trial found that adding hyaluronidase to a lidocaine solution with epinephrine did not statistically increase the incidence of pulpal anesthesia in IAN blocks.222 In addition, hyaluronidase increased the occurrence of adverse effects (i.e., increased pain and trismus).222
Carbonated Anesthetic Solutions
Experimentally, carbonated anesthetic solutions are more effective because the anesthetic is trapped in the nerve.28 In addition, carbon dioxide (CO2) has a synergistic relationship with local anesthetics and a direct depressant action on nerves.28 However, a controlled clinical study was unable to demonstrate a superior effect of lidocaine hydrocarbonate in IAN blocks.28
Diphenhydramine as a Local Anesthetic Agent
Diphenhydramine (Benadryl) has been advocated for patients who are allergic to commonly used local anesthetics. Two studies found diphenhydramine was less effective than lidocaine for extractions.174,272 Another study found the combination of lidocaine/diphenhydramine with epinephrine and diphenhydramine with epinephrine were significantly less effective for pulpal anesthesia than lidocaine with epinephrine for IAN blocks.277 They also found that the diphenhydramine solutions were more painful upon injection and had a high incidence of moderate postoperative pain.
Factors in Failure of the Inferior Alveolar Nerve Block
Accessory Innervation
The mylohyoid nerve is the accessory nerve most often cited as a cause of failure of mandibular anesthesia.70,278 A controlled clinical trial compared the IAN block alone to a combination of the IAN block and mylohyoid nerve block using 2% lidocaine with 1:100,000 epinephrine (Fig. 20-8), which was aided by the use of a peripheral nerve stimulator.34 The investigators found that the mylohyoid injection did not significantly enhance pulpal anesthesia of the IAN block (Fig. 20-9), so the study does not support the hypothesis that the mylohyoid nerve is a major factor in failure of the IAN block.
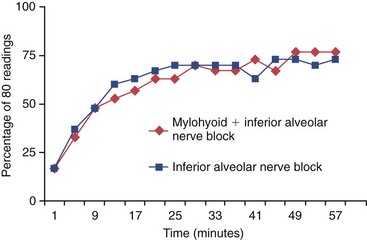
FIG. 20-9 Incidence of first mandibular molar anesthesia: comparison of the combination mylohyoid infiltration plus the inferior alveolar nerve block to the inferior alveolar nerve block alone. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 60 minutes. No significant difference between the two techniques was noted.
Accuracy of Injection
It has been theorized that an inaccurate injection contributes to inadequate mandibular anesthesia, but a number of studies determined that use of a medical ultrasound unit or radiographs to guide needle placement for IAN blocks did not result in more successful pulpal anesthesia.14,74,99 The authors of these studies speculated that the anesthetic solution migrated along the path of least resistance, which was determined by fascial planes and structures encountered in the pterygomandibular space. These studies highlight an important clinical point: Lack of pulpal anesthesia is not necessarily the result of an inaccurate injection.
Needle Deflection
Needle deflection has been proposed as a cause of failure with the IAN block.37,45,107a Several in vitro studies have shown that beveled needles tend to deflect toward the nonbeveled side (i.e., away from the bevel).* To compensate for this, a bidirectional needle rotation technique using the computer-assisted Wand (CompuDent, Milestone Scientific, Deerfield, IL) has been proposed in which the Wand handpiece assembly and needle are rotated in a fashion similar to the rotation of an endodontic hand file.107a The technique was found to reduce deflection during insertion of the needle. A controlled clinical trial compared the anesthetic success of the conventional IAN block using two needle insertion methods.133 No significant difference in anesthetic success was seen when the needle bevel was oriented away from the mandibular ramus (so that the needle would deflect toward the mandibular foramen [50% success]) and when the bidirectional Wand needle rotation technique was used (56% success).133 Neither technique resulted in an acceptable rate of anesthetic success in patients with irreversible pulpitis.
Needle Bevel and Success
In asymptomatic subjects, the orientation of the needle bevel away or toward the mandibular ramus for an IAN block did not affect anesthetic success or failure.252 Therefore, the use of commercial needles with markers to indicate needle bevel is not necessary.
Speed of Injection and Success
A slow IAN block injection (60 seconds) resulted in higher success rates (electric pulp testing) than a rapid injection (15 seconds).123
Cross-Innervation
Cross-innervation from the contralateral inferior alveolar nerve has been implicated in failure to achieve anesthesia in anterior teeth after an IAN injection. Experimentally, cross-innervation occurs in incisors227,286 but plays a very small role in failure with IAN block.
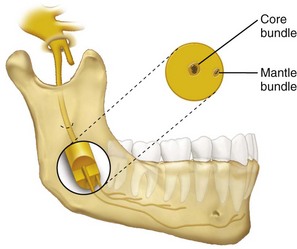
A Theory on Why Failure Occurs With the Inferior Alveolar Nerve Block in Asymptomatic Patients
The central core theory may be the best explanation of why failure occurs with the IAN block.47,255 According to this theory, nerves on the outside of the nerve bundle supply molar teeth, and nerves on the inside of the nerve bundle supply anterior teeth (Fig. 20-10). Even if deposited at the correct site, the anesthetic solution may not diffuse into the nerve trunk and reach all nerves to produce an adequate block. Although this theory may explain the higher experimental failure rates with the IAN block in anterior teeth compared with posterior teeth*, it does not explain the increased failure rate observed in painful teeth.
Enhancement of Mandibular Anesthesia in Asymptomatic Patients
Supplemental Intraligamentary Injection
Experimental studies in volunteers without dental pathosis have shown that the addition of an intraligamentary injection of 2% lidocaine with 1:100,000 epinephrine (delivered with a high-pressure syringe) to an IAN block significantly increased the success of pulpal anesthesia for 23 minutes.29 The short incidence of anesthesia was related to the small amount of anesthetic solution administered.
Supplemental Intraosseous Injection
Several studies have shown that supplemental Stabident intraosseous injection, when added to an IAN block and using local anesthetics with vasoconstrictors, significantly increased the success of pulpal anesthesia for 60 minutes in the first molar (Fig. 20-11).54,92,251 The intraosseous injection was more successful than the periodontal ligament injection because more anesthetic solution was delivered with the intraosseous injection. The addition of a supplemental intraosseous injection reduced the incidence of slow onset of pulpal anesthesia to zero compared with the IAN block alone (18% incidence).54
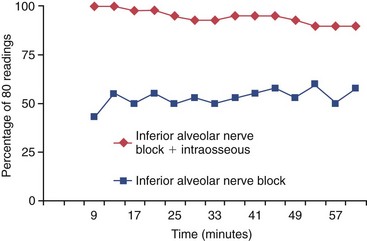
FIG. 20-11 Incidence of first mandibular molar anesthesia: comparison of the combination intraosseous injection of 2% lidocaine with 1:100,000 epinephrine plus the inferior alveolar nerve block to the inferior alveolar nerve block alone. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 60 minutes. The combination technique was significantly better at all postinjection times.
Another clinical study has shown that the use of 3% mepivacaine as a supplemental intraosseous injection after an IAN block significantly increased the success of pulpal anesthesia for 30 minutes (Fig. 20-12).77 The shorter duration of the 3% mepivacaine, compared with 2% lidocaine with 1:100,000 epinephrine, was related to the lack of a vasoconstrictor.
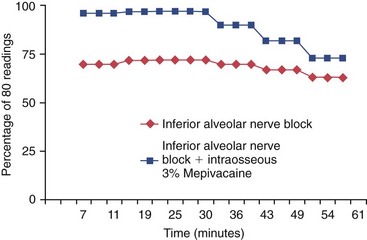
FIG. 20-12 Incidence of first mandibular molar anesthesia: comparison of the combination intraosseous injection with 3% mepivacaine plus the inferior alveolar nerve block to the inferior alveolar nerve block alone. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 60 minutes. The combination technique proved significantly better for approximately 30 minutes.
Use of Mannitol
An Ohio State University research group studied the use of mannitol to increase the efficacy of nerve blocks. Mannitol, a hyperosmotic sugar solution, is thought to temporarily disrupt the protective covering (perineurium) of sensory nerves, allowing the local anesthetic to gain entry to the innermost part of the nerve.8 These researchers found that the use of mannitol in combination with lidocaine increased anesthetic success in IAN blocks about 15% to 20%. The drug combination may be introduced sometime in the future.
Maxillary Anesthesia with 2% Lidocaine and 1:100,000 Epinephrine
Descriptions of conventional techniques for maxillary anesthesia are available for review in numerous articles and textbooks.116,158
Clinically, maxillary anesthesia is more easily obtained than mandibular anesthesia.129 As a frame of reference, the most commonly used injection for anesthetization of maxillary teeth is infiltration with 1.8 ml of 2% lidocaine (1:100,000 epinephrine).
Success Rate
In anterior and posterior teeth, infiltration anesthesia results in a high incidence (90% to 95%) of successful pulpal anesthesia (obtaining an 80 reading on an EPT that ranges from 0 to 80 in intensity).* Failure (never achieving an 80 reading) occurs about 5% to 10% of the time.† Maxillary infiltration anesthesia, therefore, is more successful than an IAN block. The technique does not achieve 100% pulpal anesthesia because of individual variations in response to the drug used and variations in anatomy and tooth position.
Onset of Anesthesia
The onset of pulpal anesthesia usually occurs within 5 to 7 minutes,90,126,166,175 but slow onset of anesthesia (defined in these cases as achieving an 80 EPT reading after 7 minutes) occurs about 20% of the time in first molars.90,126,166,175
Duration of Anesthesia
The potential problem with infiltration anesthesia in the maxilla is duration. The incidence of short duration of anesthesia (achieving an 80 reading and then losing this reading) ranges from about 60% in lateral incisors to 38% in first molars.90,126,166,175 Pulpal anesthesia in anterior teeth starts to decline after about 20 to 30 minutes; in molar teeth, anesthesia declines after about 30 to 45 minutes. These time courses have clinical implications. In an emergency endodontic procedure on a first molar, the pulp usually can be removed within 20 to 30 minutes, so the duration of anesthesia is of little consequence. However, if the practitioner is preparing to obturate the tooth and this procedure takes an hour, the patient might experience pain. Therefore additional local anesthetic should be administered.
Time Course of Pulpal Anesthesia for the Maxillary First Molar
Fig. 20-13 shows the time course for complete pulpal anesthesia for an asymptomatic first molar, as defined by the percentage of patients who do not respond to an 80 EPT stimulus across time. Some patients (20%) had a slow onset of anesthesia until around 11 minutes. The overall success rate (no response at the 80 reading) is 95% to 100%, with peak effects observed at around 30 minutes after injection.
Alternative Anesthetic Solutions for Infiltration Injections
Plain Solutions: 3% Mepivacaine (Carbocaine, Polocaine, Scandonest) and 4% Prilocaine (Citanest Plain)
Solutions of 3% mepivacaine plain and 4% prilocaine plain provide a short duration of pulpal anesthesia, averaging about 15 to 20 minutes (Fig. 20-14),126,166 and are indicated for procedures of short duration. These agents are generally not as safe as solutions with vasoconstrictors if large volumes are administered, because they are rapidly absorbed systemically, resulting in excessive plasma concentrations and possible toxic reactions.158

FIG. 20-14 Incidence of first maxillary molar anesthesia: comparison of 3% mepivacaine to 2% lidocaine with 1:100,000 epinephrine. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 60 minutes. The 3% mepivacaine showed a shorter duration of anesthesia than the lidocaine solution.
4% Prilocaine With 1:200,000 Epinephrine (Citanest Forte)
The effect of 4% prilocaine (1:200,000 epinephrine) is similar to that of an infiltration injection with 2% lidocaine (1:100,000 epinephrine).126
Articaine With 1:100,000 Epinephrine (Septocaine)
Several studies have shown that articaine with epinephrine was similar in action to prilocaine with epinephrine and lidocaine with epinephrine for maxillary infiltration injections.50,94,95,263 A recent study found maxillary infiltration of 4% articaine with 1:100,000 epinephrine statistically improved anesthetic success, when compared to 2% lidocaine with 1:100,000 epinephrine, in the lateral incisor but not in the first molar. 57
0.5% Bupivacaine With 1:200,000 Epinephrine (Marcaine)
Success rates (no response to EPT) with bupivacaine range from 80% to 95% in the maxillary lateral incisor, compared with 50% in the maxillary second premolars.43,90,132,257 Although bupivacaine provides long-term anesthesia in the mandible, it does not provide prolonged pulpal anesthesia with maxillary infiltration injection.43,90,132 In the lateral incisor, bupivacaine has a shorter duration of pulpal anesthesia than lidocaine.43,90 In the first molar, bupivacaine’s duration of pulpal anesthesia is equivalent to that of lidocaine.90
Extending the Duration of Maxillary Infiltrations
Increasing the Solution Volume
For maxillary infiltrations, increasing the volume of 2% lidocaine with 1:100,000 epinephrine from 1.8 ml to 3.6 ml provided a statistically longer duration of pulpal anesthesia.175 A repeated infiltration of 1.8 ml of 2% lidocaine with 1:100,000 epinephrine given 30 minutes following an initial infiltration of 1.8 ml of 2% lidocaine with 1:100,000 epinephrine significantly improved the duration of pulpal anesthesia (from 37 minutes through 90 minutes) in the maxillary lateral incisor238 (Fig. 20-15).
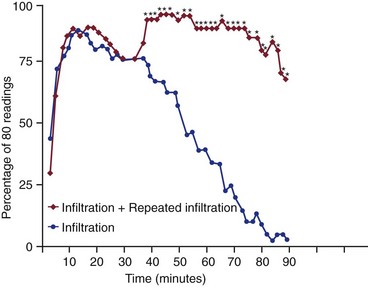
FIG. 20-15 Incidence of maxillary lateral incisor pulpal anesthesia using an initial infiltration and a repeated infiltration 30 minutes later (both infiltrations used 1.8 ml of 2% lidocaine with 1:100,000 epinephrine). Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings). The repeated infiltration injection significantly prolonged the duration of pulpal anesthesia.
Alternative Maxillary Injection Techniques
Posterior Superior Alveolar (PSA) Nerve Block
The PSA nerve block provides pulpal anesthesia for the second and third molars and in some first molars.154 Generally, with the first molar, an additional buccal infiltration injection may be needed after the PSA block to ensure patient comfort. The PSA injection often is indicated when all the molar teeth require anesthesia. If the procedure involves the first molar, an infiltration injection is a better choice because it is more predictable for pulpal anesthesia than the PSA injection.
Infraorbital Nerve Block
The infraorbital nerve block produces profound lip numbness.12,125 It successfully anesthetizes the first and second premolars, but the duration of pulpal anesthesia is less than 60 minutes.12,125 The infraorbital block does not successfully anesthetize the pulps of the central or lateral incisors.12,125 Essentially, this injection technique is the same as an infiltration injection over the premolar teeth for pulpal anesthesia.
Second Division Nerve Block
The second division nerve block successfully anesthetizes the pulps of molar teeth and about 50% of the second premolars.22,165 It does not routinely anesthetize the pulps of anterior teeth.22,165 The high tuberosity approach is preferred over the greater palatine technique because the success rate is similar and the procedure is less painful.22
Palatal–Anterior Superior Alveolar (P-ASA) Nerve Block
Traditionally, maxillary anterior teeth have been anesthetized with an infiltration injection near the apex of the target tooth. In the late 90s the P-ASA injection, a site-specific injection for maxillary anterior teeth, was introduced.68,69 The P-ASA injection involves a palatal injection into the incisive canal and derives its name from the injection’s supposed ability to anesthetize both the right and left anterior superior alveolar nerves (Fig. 20-16). A P-ASA injection of 0.9 to 1.4 ml of anesthetic solution has been reported to produce anesthesia of the maxillary incisors and usually the canines, with an expected duration of approximately 60 minutes.68 One study compared the anesthetic efficacy of 2% lidocaine with 1:100,000 epinephrine and 3% mepivacaine using the computer-assisted Wand Plus injection system and the P-ASA injection route.23 Neither anesthetic produced greater than 58% successful pulpal anesthesia and therefore would not clinically ensure predictable pulpal anesthesia for the four maxillary incisors and canines.
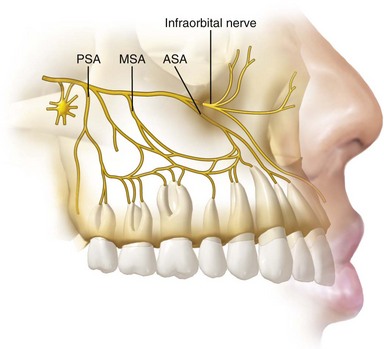
FIG. 20-16 Distribution of the maxillary division of the trigeminal nerve, showing the anterior superior alveolar (ASA) nerve, the middle superior alveolar (MSA) nerve, and the posterior superior alveolar (PSA) nerve.
Moreover, 30% to 43% of patients report moderate to severe pain from the needle insertion for the P-ASA injection.195 For needle placement into the incisive canal, 54% to 58% of subjects reported moderate to severe pain. For deposition of the anesthetic solution, 8% to 12% of subjects reported moderate pain. Postoperatively, approximately 12% to 18% of the subjects experienced temporary numbness or paresthesia of the incisive papilla, and 20% to 28% had swelling or soreness of the incisive papilla. The P-ASA injection, therefore, can be a painful injection, and it has a low to modest success rate.
Anterior Middle Superior Alveolar (AMSA) Nerve Block
The AMSA injection is another new technique for anesthetizing maxillary teeth.66,67,69 The AMSA injection site is located palatally at a point that bisects the premolars and is approximately halfway between the midpalatine raphe and the crest of the free gingival margin (Fig. 20-17). The AMSA injection supposedly can anesthetize both the anterior and middle superior alveolar nerves66,67,69 (see Fig. 20-16). Injection of 0.6 to 1.4 ml of anesthetic solution has been reported to produce pulpal anesthesia of the maxillary central and lateral incisors, canines, and first and second premolars, with an expected duration of 45 to 60 minutes.66,67,69 A bilateral AMSA injection supposedly anesthetizes 10 maxillary teeth, extending from the second premolar on one side to the second premolar on the opposite side.67
Two studies of the AMSA technique found rather modest to low success rates, slow onset, and declining duration of pulpal anesthesia over 60 minutes.73,146 The AMSA injection would not ensure predictable pulpal anesthesia from the second premolar to the central incisor.73,146 Moreover, the AMSA injection, whether made with a computer-assisted injection system or a conventional syringe, produced moderate pain on needle insertion in 32% to 38% of study subjects and moderate pain upon solution deposition in 25% to 40% of subjects.198
When the Wand Plus was used for the AMSA injection, statistically lower pain ratings were recorded for deposition of the anesthetic solution. However, regardless of whether the Wand Plus or a conventional syringe is used, the AMSA injection can be a painful injection, and it has a low to modest success rate.
Supplemental Anesthesia
Supplemental injections are essential when, as frequently occurs, anesthesia from conventional injections is inadequate and the pain is too severe for the practitioner to proceed. Three such supplemental techniques can be used: the intraligamentary injection, the intraosseous injection, or the intrapulpal injection.
If the patient has profound lip numbness and experiences pain upon endodontic access, repeating the IAN block does not help the problem. Clinicians may think another injection is helpful because the patient sometimes achieves pulpal anesthesia after the second injection, but the patient may simply be experiencing slow onset of pulpal anesthesia from the first injection.
Infiltrations of Articaine Following Maxillary or Mandibular Anesthesia in Patients With Irreversible Pulpitis
Using a visual analog scale to evaluate success, no significant differences were found between an articaine solution and a lidocaine solution when used as a supplemental infiltration after IAN blocks or maxillary infiltrations in patients with irreversible pulpitis.229 In a small study of 19 patients, no difference was found between lidocaine (9 patients) and articaine (10 patients) formulations in maxillary infiltrations for patients with irreversible pulpitis.240
Supplemental Buccal Infiltration of Articaine After a Failed Inferior Alveolar Nerve Block in Patients With Irreversible Pulpitis
A recent study found that when IAN block failed, there was only a 58% success rate for a supplemental buccal infiltration of 1.8 ml of 4% articaine with 1:100,000 epinephrine in mandibular posterior teeth in patients with irreversible pulpitis.167 This success rate was much lower than a supplemental intraosseous injection.
Intraligamentary Anesthesia
The technique for intraligamentary injection of anesthesia is reviewed in a number of published papers and textbooks.
Success of Intraligamentary Injection
The success of supplemental intraligamentary injections in achieving pulpal anesthesia for endodontic procedures has been reported to be 50% to 96%.36,159,249,269 Intraligamentary injection produced a 50% to 79% success rate in endodontic treatment when used as a primary anesthetic technique.127,159 If the first intraligamentary injection failed, reinjection was successful in 71% of patients, for an overall success rate of 92%.269 Similar results have been reported by other investigators.36,249 Intraligamentary injection is not successful in mandibular anterior teeth.172,274
Mechanism of Action
An intraligamentary injection forces anesthetic solutions through the cribriform plate into the marrow spaces around the tooth.53,72,215,248,270 The primary route is not via the periodontal ligament, and unlike the intrapulpal injection,17,265 the mechanism of action is not a pressure anesthesia.56,183 The intraligamentary injection should be considered an intraosseous injection.
Back-Pressure
Studies have shown that the most important factor for anesthetic success with an intraligamentary injection is injection under strong back-pressure.248,269 Pressure is necessary to force the solution into the marrow spaces.
Anesthetic Solutions
A vasoconstrictor significantly increases the efficacy of an intraligamentary injection.89,128,134,170,237 Injection of a vasoconstrictor alone (1:100,000 epinephrine) does not produce pulpal anesthesia.237 Anesthetic solutions with reduced vasoconstrictor concentrations (bupivacaine or etidocaine with 1:200,000 epinephrine) are not very effective with this technique.89,119,128
Amount of Solution Delivered
Usually about 0.2 ml of solution is deposited with each mesial and distal injection, using a traditional or pressure syringe. The exact amount is not always known because some of the anesthetic solution may escape from the sulcus during the injection.
Injection Discomfort
When an intraligamentary injection is given as a primary injection, needle insertion and injection of the anesthetic solution are only mildly discomforting in posterior teeth41,159,237,274; however, in maxillary lateral incisors, an intraligamentary injection can be painful.274
When the intraligamentary injection is given as a supplemental injection to anesthetize symptomatic vital teeth (i.e., in irreversible pulpitis), the patient may have moderate pain.52 Patients should be informed of this possibility.
Onset of Anesthesia
The onset of anesthesia is immediate with an intraligamentary injection,* which means no waiting period is required for the anesthesia to take effect.
Duration
Experimental studies with the EPT have shown that when the intraligamentary injection is given as a primary injection, the duration of profound pulpal anesthesia is approximately 10 to 20 minutes.183,237,274 When the injection is used as a supplemental technique in asymptomatic teeth after an IAN block, the duration of pulpal anesthesia is approximately 23 minutes.29 Therefore, when the intraligamentary injection is used as a supplemental technique in endodontic therapy, the clinician must work fairly quickly and be prepared to reinject if profound anesthesia dissipates.
Postoperative Discomfort
Most patients have postoperative discomfort (mostly mild pain) when an intraligamentary injection is used as a primary technique.41,237,274 Most of this discomfort occurs the first day after injection, and the duration of discomfort averages 14 hours to 3 days.41,237,274 Postinjection discomfort is related to damage from insertion of the needle and not from the pressure of solution deposition.41 About 40% of patients report that the tooth feels high in occlusion.237,274
When an intraligamentary injection is used as a supplemental technique for endodontic therapy, pain from the intraligamentary injection probably occurs in addition to any postoperative pain from the endodontic treatment.
Avulsion
In a letter to the editor of the Journal of the American Dental Association, Nelson191 reported on the avulsion of a tooth following intraligamentary injections. However, no clinical or experimental study has reported avulsion or loosening of teeth with this technique.183,237,274 Avulsion should not be a concern with intraligamentary injections.
Selective Anesthesia
Although some have reported that the intraligamentary injection can be used in the differential diagnosis of pulpally involved teeth,153,242 experimental studies have shown that adjacent teeth may also become anesthetized with intraligamentary injection for a single tooth.183,237,274 Therefore the intraligamentary injection should not be used for differential diagnosis.
Systemic Effects
When a high-pressure syringe was used in dogs, intraligamentary injection of solutions containing epinephrine caused cardiovascular responses similar to those seen with IV injections.247 Clinical studies using a high-pressure syringe in human beings found that intraligamentary injections of such solutions did not significantly change the heart rate, rhythm, amplitude, or the blood pressure.25,194 These studies support the conclusion that intraligamentary injections do not cause significant changes in heart rate in human beings.
Needle Gauge
Different needle gauges (25, 27, or 30) have been shown to be equally effective.159,269
Ligamental Syringes
Special ligamental syringes have not proved any more effective than a standard syringe.41,249,269
Safety to the Periodontium
Clinical and animal studies have demonstrated the relative safety of the intraligamentary injection technique.* Minor transient damage occurs only at the site of needle penetration, and the tissue subsequently undergoes repair. In very rare cases, periodontal abscesses and deep pocket formation have occurred after intraligamentary injections.29,274 A very small clinical risk of periodontal abscess formation and bone loss exists with this technique, and although these effects are rare, the clinician should be aware of them. Localized areas of root resorption after intraligamentary periodontal ligament injections have also been reported.207,223
Safety to the Pulp
Clinical and animal studies have shown that intraligamentary injections have no permanent effect on the pulp.† However, intraligamentary injection of a solution with epinephrine produces a rapid, prolonged decrease in blood flow.134 Some have suggested that using this injection technique during restorative procedures could result in accumulation of inflammatory mediators that would not be effectively removed because of the reduced blood flow.134 This hypothesis was directly tested, and intraligamentary injection of an anesthetic solution containing a vasoconstrictor in conjunction with a deep cavity preparation did not produce a more severe reaction than in controls (cavity preparation only).211 Rather, the depth of the cavity preparation was the most important factor dictating pulpal responses. Intraligamentary injections are therefore unlikely to cause pulpal necrosis.
Safety in Primary Teeth
One study has shown that intraligamentary injection of primary teeth may cause enamel hypoplasia of the developing permanent teeth.21 The effect noted was not caused by the injection technique but by the anesthetics used—that is, the cytotoxic anesthetic agents bound to the enamel matrix in the developing tooth germ. The same effect seemingly would be produced by an infiltration injection next to the developing tooth, so the recommendation that intraligamentary injections be used with great care on primary teeth close to developing permanent teeth21 may not be correct.
Safety in Periodontally Involved Sites
Intraligamentary injections have been shown to be safe in cases of mild to moderate gingival inflammation or incipient periodontitis.39
Precautions
No research as yet has shown how painful an intraligamentary injection would be or if it would result in anesthesia in teeth with cellulitis or abscess formation (symptomatic necrotic teeth with periradicular radiolucencies).
New Technology for Intraligamentary Injections: The Wand
A computer-assisted local anesthetic delivery system was introduced by Milestone Scientific (Livingstone, NJ) that can be used to administer an intraligamentary injection. The Wand (also called CompuDent or CCLAD) accommodates a standard local anesthetic cartridge that is linked by sterile microtubing to a disposable, penlike handpiece with a Luer-Lok needle (Fig. 20-18). The device is activated by a foot control, which automates the infusion of local anesthetic solution at a controlled rate. Two flow rates, slow or fast, may be initiated and maintained by a foot pedal control. The fast rate delivers 1.4 ml of solution in 1 minute. The slow rate delivers 1.4 ml of solution in approximately 4 minutes, 45 seconds. The slow rate is used for the intraligamentary injection.
Anesthetic Success of the Intraligamentary Injection, Using the Wand in Asymptomatic Vital Teeth
An experimental study recently compared the anesthetic efficacy of primary intraligamentary injection of 1.4 ml of 4% articaine with 1:100,000 epinephrine and 1.4 ml of 2% lidocaine with 1:100,000 epinephrine administered with a computer-controlled local anesthetic delivery system in the mandibular first molar.13Successful pulpal anesthesia (two consecutive 80 EPT readings) was obtained 86% of the time with the articaine solution and 74% of the time with the lidocaine solution. No significant difference was seen between the articaine and lidocaine solutions. The duration of pulpal anesthesia ranged from 31 to 34 minutes, longer than the 10 minutes recorded in a similar study using a pressure syringe and 0.4 ml of a lidocaine solution.274 Therefore the computer-controlled local anesthetic delivery system offers the advantage of increasing the duration of pulpal anesthesia; however, the anesthesia slowly decreases over 60 minutes.
Anesthetic Success of the Intraligamentary Injection Using the Wand in Symptomatic Vital Teeth
Supplemental intraligamentary injection, administered with a computer-controlled anesthetic delivery system in mandibular posterior teeth diagnosed with irreversible pulpitis after failure of an IAN injection, produced a 56% anesthesia success rate.196 These results were somewhat disappointing because the computer-controlled anesthetic delivery system should have been capable of delivering approximately 1.4 ml of anesthetic solution with the intraligamentary injection by consistent maintenance of a precise flow rate.
Intraosseous Anesthesia
Stabident and X-Tip Systems
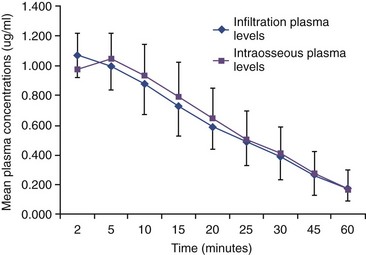
The intraosseous route delivers a local anesthetic solution directly into the cancellous bone adjacent to the tooth to be anesthetized. Infiltration injections of lidocaine formulations are not effective for anesthesia of the mandibular molar teeth because of the thickness of the cortical plate; therefore dentists do not attempt infiltration anesthesia in the posterior mandible. The intraosseous injection overcomes this problem by allowing direct access to the cancellous bone. One clinical study directly compared the infiltration and intraosseous injection techniques, using 1.8 ml of 2% lidocaine with 1:100,000 epinephrine in the maxillary lateral incisor.201 The two techniques produced similar results, except that the intraosseous technique had a quicker onset and a shorter duration of anesthesia (Fig. 20-19).
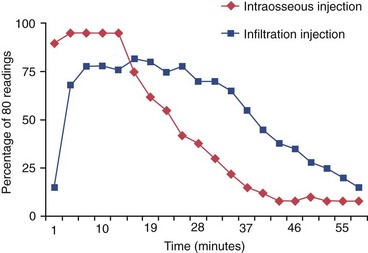
FIG. 20-19 Incidence of anesthesia for intraosseous and infiltration injections. Results were determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80 readings) across time for 60 minutes. The intraosseous injection showed a quicker onset and a shorter duration of anesthesia.
Two intraosseous systems have been studied clinically: the Stabident system (Fairfax Dental Inc, Miami, FL) and the X-tip system (DENTSPLY, Tulsa, OK). Two other anesthetic systems have been introduced: the IntraFlow (Pro-Dex Inc, Irvine, CA) and the Comfort Control Syringe (DENTSPLY International, York, PA). The IntraFlow system combines a slow-speed handpiece with an anesthetic cartridge dispenser system and a rotating needle/drill. The anesthetic solution is delivered after the cortical bone is perforated. When the IntraFlow system was used as a primary technique in a small group of 15 patients with irreversible pulpitis, an 87% success rate was reported (two consecutive 80 readings with a pulp tester).216 While encouraging, more research on the IntraFlow system is needed. The Comfort Control Syringe is an electronic delivery system and has five preprogrammed injection rates. No published controlled studies have evaluated the Comfort Control Syringe system in clinical dentistry.
The Stabident system is composed of a slow-speed, handpiece-driven perforator, a solid 27-gauge wire with a beveled end that drills a small hole through the cortical plate (Fig. 20-20). The anesthetic solution is delivered to cancellous bone through the 27-gauge, ultrashort injector needle placed into the hole made by the perforator (Fig. 20-21).
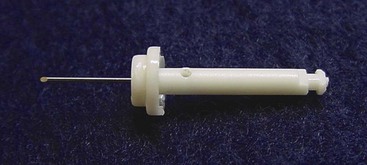
FIG. 20-20 Stabident perforator, a solid 27-gauge wire with a beveled end that is placed in a slow-speed handpiece.

FIG. 20-21 The anesthetic solution is delivered to the cancellous bone through the needle placed into the hole made by the perforator.
The X-tip anesthesia delivery system consists of an X-tip that separates into two parts, the drill and the guide sleeve (Fig. 20-22). The drill, a special hollow needle, leads the guide sleeve through the cortical plate, whereupon it is separated and withdrawn. The remaining guide sleeve is designed to accept a 27-gauge needle for injection of the anesthetic solution (Fig. 20-23). The guide sleeve is removed after the intraosseous injection is complete.
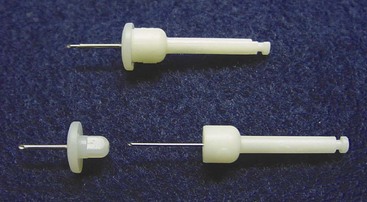
FIG. 20-22 The X-tip anesthesia delivery system consists of an X-tip (top) that separates into two parts: the drill (a special hollow needle) and the guide sleeve component (bottom).
The technique for intraosseous injection of anesthesia using the Stabident or X-tip system can be reviewed in the systems’ instruction manuals or in published papers.35,78,218-220
Perforation Pain and Solution Deposition with Irreversible Pulpitis
Generally the Stabident system produces a very low incidence of moderate pain from perforation and solution deposition in asymptomatic patients.35,78,218-220 A higher incidence was reported when the system was used to make intraosseous injections in mandibular posterior teeth with irreversible pulpitis. Up to 9% of patients reported moderate to severe pain after perforation, and 5% to 31% reported moderate to severe pain during deposition of the anesthetic solution.200,217
With the X-tip system, 48% of patients with irreversible pulpitis had moderate to severe pain with perforation, and 27% had moderate pain with solution deposition.197 Patients with irreversible pulpitis may experience a transient but moderate to severe pain on perforation and solution deposition when either the Stabident or X-tip system is used. The higher pain ratings, compared with those for asymptomatic teeth, are probably related to preexisting hyperalgesia, which leads to increased pain responsiveness and preoperative anxiety.
Perforator Breakage
In about 1% of cases, the metal perforator separates from the plastic shank during use.35,54,79,197,218-220 The metal wire is easily removed with a hemostat. This separation usually occurs during a difficult perforation (e.g., dense cortical bone); the wire probably is heated excessively, causing the plastic hub to melt. No perforator breakage (metal perforator breaking into parts) has been reported in numerous studies.35,54,79,197,218-220
Optimal Location for Injection Site
Injection at a site distal to the tooth to be anesthetized produces the best anesthesia.* Maxillary and mandibular second molars are an exception to this rule. A mesial site should be selected for these teeth because of the increased thickness of the cortical plate in the mandible and the difficulty with perforation and needle placement at a distal site.
Site Selection: Attached Gingiva or Alveolar Mucosa
Both the Stabident and X-tip intraosseous systems instruct the user to locate the perforation site in attached gingiva. The gingival site allows the perforation to be made through a minimal thickness of cortical bone and generally is equidistant between adjacent root structures. However, because the guide sleeve remains in place with the X-tip system, two studies have successfully used it in alveolar mucosa at a more apical location.79,197 The X-tip system has a definite clinical advantage over the Stabident system, because the X-tip perforation may be made at an apical location in unattached gingiva. If the Stabident system is used apically in alveolar mucosa, the hole for delivering the anesthetic solution is almost impossible to find. The clinician may want to consider using the X-tip in an apical location in specific clinical situations. For example, when periodontal pocketing does not allow perforation into cancellous bone through the more coronal attached gingiva or when interproximal space is lacking (i.e., roots are too close together), the X-tip system can be used to achieve pulpal anesthesia. If the Stabident system fails, the clinician may want to consider using the X-tip apically to achieve pulpal anesthesia.
Success of the Inferior Alveolar Nerve Block in Patients With Irreversible Pulpitis
Clinical studies of endodontics in patients with irreversible pulpitis have found that success (mild or no pain upon endodontic access or initial instrumentation) with the IAN block occurred between 19% and 56% of the time.* These studies would indicate that anesthesia is often difficult to achieve in irreversible pulpitis with only the IAN block.
Success of Intraosseous Anesthesia With Irreversible Pulpitis
Stabident System
In a clinical trial on patients with posterior teeth with irreversible pulpitis, a supplemental mandibular intraosseous Stabident injection (1.8 ml of 2% lidocaine with 1:100,000 epinephrine) was 91% successful in achieving total pulpal anesthesia.200 A second clinical trial evaluated the Stabident intraosseous injection in patients with irreversible pulpitis when conventional local anesthetic techniques failed. These researchers found that an initial supplemental intraosseous injection (0.45 to 0.9 ml of 2% lidocaine with 1:100,000 epinephrine) was successful in 79% of posterior mandibular teeth.206 A second intraosseous injection of the remaining cartridge increased the success rate to 91%. Therefore, initially giving a quarter to a half cartridge of 2% lidocaine with 1:100,000 epinephrine was less successful than initially giving a full cartridge. A third clinical trial in patients with mandibular teeth with irreversible pulpitis showed that supplemental intraosseous injection of 1.8 ml of 3% mepivacaine increased the success rate to 80% compared with the IAN block alone (25% success).217 A repeat intraosseous injection of 1.8 ml of 3% mepivacaine increased the success rate to 98%. Therefore one cartridge of 3% mepivacaine plain is not as effective as one cartridge of 2% lidocaine with 1:100,000 epinephrine. However, injection of 3% mepivacaine does not produce the tachycardia observed with solutions that contain epinephrine.
X-Tip System
One clinical trial evaluated a supplemental X-tip intraosseous injection (1.8 ml of 2% lidocaine with 1:100,000 epinephrine) in patients with irreversible pulpitis when a conventional IAN block failed.197 The X-tip injection site was 3 to 7 mm apical to the mucogingival junction of the mandibular molar or premolar tooth. The results showed an 82% success rate for anesthesia; it also showed an 18% failure rate caused by backflow of the anesthetic solution into the oral cavity. These researchers concluded that when an IAN block fails to provide profound pulpal anesthesia, the X-tip system, when used in an apical location without backflow of the anesthetic solution into the oral cavity, successfully achieves pulpal anesthesia in mandibular posterior teeth with irreversible pulpitis.
Intraosseous Success With an Articaine Solution in Patients With Irreversible Pulpitis
For posterior teeth diagnosed with irreversible pulpitis, the supplemental intraosseous injection of 1.8 ml of 4% articaine with 1:100,000 epinephrine was 86% successful when the IAN block failed.15 Therefore, the success rate of the articaine solution was similar to a solution of lidocaine.
Repeating the Intraosseous Injection
Repeating the intraosseous injection, using 1.4 ml of 2% lidocaine with 1:100,000 epinephrine 30 minutes after the initial intraosseous injection, provided an additional 15 to 20 minutes of pulpal anesthesia—similar to the duration of the initial intraosseous injection.117
Key to Successful Intraosseous Injection
The key to a successful intraosseous injection is flow of the anesthetic into the cancellous space. If anesthetic solution leaks out of the perforation site into the oral cavity, no anesthetic effect is achieved. Reperforation or use of another perforation site is a practical way to gain access to the cancellous bone in such cases. In fewer than 10% of cases, constricted cancellous spaces may limit the distribution of the anesthetic solution around the apices of the teeth.* In such cases, failure may result even if the anesthetic solution is delivered intraosseously.
Duration
In patients with irreversible pulpitis, supplemental intraosseous injection using either the Stabident or X-tip system provided anesthesia for the entire débridement appointment.197,200,217
Timing of Intraosseous Injection
Considering the high failure rate of the IAN block in patients in pain, prudent practice would be to give all patients with irreversible pulpitis a supplemental intraosseous injection after an IAN block—that is, once the signs of lip numbness have developed, an intraosseous injection should be given. This technique significantly reduces pain and allows treatment to start sooner.
Many practitioners do not use this regimen because clinicians essentially do what they were taught in their initial clinical training, and sometimes change can be difficult. For example, a 1998 study in the Journal of the American Medical Association urged the use of anesthesia during circumcision5; nevertheless, up to 96% of baby boys currently don’t receive anesthesia. Because many physicians were taught during their residencies not to administer anesthesia, changing their practice philosophy probably will be a slow process. This is a common problem in many health care disciplines, and it emphasizes the need for practitioners to stay current with recent advances.
Anesthetic Success in Painful Teeth With Totally Necrotic Pulps and Radiolucent Areas
No study has investigated the use of intraosseous anesthesia in patients with painful teeth, totally necrotic pulps, and radiolucent areas. In a preliminary study performed at Ohio State, anesthetic solution deposition was very painful in these teeth, and the study had to be terminated.
Anesthetic Success in Partially Vital Teeth
The intraosseous injection should work in teeth in which the chamber is necrotic, the canals are vital or partially vital, and widening of the periodontal ligament can be seen radiographically. A recent history of hot and cold sensitivity should differentiate this condition from that of a necrotic tooth experiencing an acute exacerbation (Phoenix abscess).
Systemic Effects of Intraosseous Injection
Cardiovascular Effects
A transient increase in heart rate has been reported in 46% to 93% of cases involving Stabident and X-tip intraosseous injection of solutions containing epinephrine or levonordefrin.* Four clinical trials using techniques such as objective electrocardiographic recordings and pulse oximetry have shown that subjects experienced a transient tachycardia (mean increase of 12 to 32 beats/min) after Stabident intraosseous injection of 1.8 ml of 2% lidocaine with 1:100,000 epinephrine, 2% mepivacaine with 1:20,000 levonordefrin, or 1.8 ml of 1.5% etidocaine with 1:200,000 epinephrine.27,92,221,251 Another clinical trial reported transient tachycardia after intraosseous injection, but not with infiltration injection, of 1.8 ml of 2% lidocaine with 1:100,000 epinephrine in the maxillary anterior region.279 Generally, all these studies showed that the heart rate returned to baseline readings within 4 minutes in most patients. Therefore injection of anesthetic solutions containing vasoconstrictors, using either the Stabident or X-tip systems, results in a transient tachycardia. No significant change in diastolic, systolic, or mean arterial blood pressure has been observed with intraosseous injection of 2% lidocaine with 1:100,000 epinephrine.27,221
An intraosseous injection of 1.4 ml of 2% lidocaine with 1:100,000 epinephrine with the Wand (CompuDent, CCLAD, Milestone Scientific, Livingston, NJ) at a fast rate resulted in a significantly higher heart rate when compared to a slow solution deposition using either the Wand or traditional syringe.256
Clinical Significance of Increased Heart Rate
Although the patient is likely to notice the transient tachycardia that occurs after Stabident or X-tip intraosseous injection of 2% lidocaine with 1:100,000 epinephrine, it generally is not clinically significant in healthy patients.221 The clinical significance, cardiovascular effects, and contraindications to the use of vasoconstrictors in intraosseous injections have been reviewed.221
Lack of Heart Rate Effect Of 3% Mepivacaine in Intraosseous Anesthesia
No significant tachycardia occurs when 3% mepivacaine is used for intraosseous anesthesia.77,221 Clinicians should keep in mind that this anesthetic is an alternative for intraosseous injection in patients whose medical condition or drug therapy suggests caution in the use of solutions containing epinephrine or levonordefrin.77,221
Cautious Use of Long-Acting Anesthetics for Intraosseous Anesthesia
In an attempt to increase the duration of pulpal anesthesia with intraosseous injections, some clinicians may consider using long-acting anesthetics. Bupivacaine (Marcaine) and etidocaine (Duranest) are long-acting anesthetics but only for IAN blocks. Long-acting anesthetics do not show an extended duration of anesthesia when injected by the intraosseous or maxillary infiltration routes.43,90,109,251 Bupivacaine and etidocaine have cardiotoxic effects10 and for intraosseous anesthesia basically are equivalent to 2% lidocaine with epinephrine in terms of efficacy, duration, and heart rate effects. Therefore bupivacaine and etidocaine offer no advantage clinically and should not be used for intraosseous anesthesia.
Plasma Levels of Lidocaine After Intraosseous Injection
Some authors have cautioned that administration of an overly large volume of local anesthetic with an intraosseous injection could lead to overdose reactions.113 One experimental study using volunteers found that injection of 1.8 ml of 2% lidocaine with 1:100,000 epinephrine produced venous plasma levels of lidocaine that were the same for maxillary anterior intraosseous and infiltration injections (Fig. 20-24).279Although systemic concentrations of vasoconstrictors have a short-lived effect on the heart rate, the plasma concentration of lidocaine delivered with intraosseous injection is no more than that delivered with infiltration, so the intraosseous technique should not be considered an intravascular injection with regard to lidocaine. Also, if it were an intravascular injection, little or no anesthetic effect would be demonstrated—that is, all the local anesthetic solution would be carried into the vascular system, with none left for pulpal anesthesia. Obviously, clinical and experimental studies have demonstrated clinical anesthesia with intraosseous techniques.* Therefore the precautions for the maximum amount of lidocaine for an infiltration injection would seem to apply to an intraosseous injection.
Postoperative Discomfort
When intraosseous injections are given with the Stabident system, either as a primary or a supplemental technique, most patients report no or only mild pain; approximately 2% to 15% report moderate pain.35,92,218-220 Less postoperative discomfort is reported for the Stabident intraosseous injection than for periodontal ligament injection.237
One study found that significantly more men experienced postoperative pain with the X-tip system than with the Stabident system.78 The authors interpreted these results as being due to the denser, more mineralized bone in the posterior mandible in men and to the fact that the diameter of the X-tip perforating system is larger than that of the Stabident perforator, meaning that the X-tip system generates more frictional heat during perforation. In patients with irreversible pulpitis, the postoperative pain of the endodontic procedure likely adds to any postoperative pain from the intraosseous injection.
Postoperative Problems
With the Stabident system, fewer than 5% of patients develop swelling or exudate at the site of perforation.35,92,218-220 The X-tip system may show a higher incidence of postoperative swelling clinically.78 With both systems, swelling or exudate (or both) may persist for weeks after the injection, but this resolves with time.35,78,92,218-220 Slow healing of perforation sites may be the result of overheating of the bone caused by pressure during perforation.
With both the Stabident and X-tip systems, approximately 4% to 15% of patients report that for a few days, the tooth “feels high” during chewing.35,78,92,218-220 This feeling most likely is an increased awareness to biting that results from soreness in the area caused by damage from perforation or inflammation of the bone. The incidence for the intraosseous injection is lower than that reported for the periodontal ligament injection (36% to 49%).41,237
Intrapulpal Injection
In about 5% to 10% of mandibular posterior teeth with irreversible pulpitis, supplemental injections, even when repeated, do not produce profound anesthesia; pain persists when the pulp is entered. This is an indication for an intrapulpal injection.
The major drawback of the intrapulpal injection technique is that the needle is placed and the injection is made directly into a vital and very sensitive pulp; this injection is often moderately to severely painful.200 Because endodontics currently offers more successful methods of supplemental anesthesia, the intrapulpal injection should be given only after all other supplemental techniques have failed. Another disadvantage of the technique is the possible duration of pulpal anesthesia (15 to 20 minutes). The bulk of the pulpal tissue must be removed quickly, at the correct working length, to prevent reoccurrence of pain during instrumentation. Yet another disadvantage is that the pulp obviously must be exposed to allow direct injection. Anesthetic problems frequently occur before exposure while the clinician is still working in dentin.196,197,200,217
The advantage of the intrapulpal injection is that it produces profound anesthesia if given under back-pressure.17,265 The onset of anesthesia is immediate, and no special syringes or needles are required. The methods for this technique can be found in many excellent endodontic textbooks. As mentioned previously, strong back-pressure is a major factor in achieving successful intrapulpal anesthesia.17,265 Depositing the anesthetic solution passively into the chamber is insufficient because the solution will not diffuse throughout the pulp.
Management of Specific Endodontic Situations
Irreversible Pulpitis
When irreversible pulpitis is a factor, the teeth that are most difficult to anesthetize are the mandibular molars, followed by the mandibular premolars, the maxillary molars and premolars, and the mandibular anterior teeth. The fewest problems arise in the maxillary anterior teeth.
In some teeth, irreversible pulpitis is the condition in the apical portion of the canals; the tissue in the chamber is necrotic and does not respond to pulp testing. The pulp chamber can be entered easily, but when attempts are made to place a file to length, severe pain results. Intraosseous injections are helpful in these cases, and an intrapulpal injection may be used. However, irreversible pulpitis must be differentiated from a symptomatic necrotic tooth with apical pathosis. In the latter condition, it is unknown whether intraosseous injections are effective, and bacteria may be forced into the periradicular tissues by an intrapulpal injection.
Mandibular Teeth
Up until the 1980s, before supplemental intraligamentary and intraosseous injections became popular, clinicians would administer conventional anesthesia. After signs of soft-tissue anesthesia became evident, the pain abated and the patient relaxed. Local anesthesia produced the classic soft-tissue signs and relieved the painful symptoms, but pain frequently resulted when the access opening was begun or the pulp was entered. Currently, this pain has been significantly reduced with supplemental techniques.
Integration of the results of many recent clinical trials has changed the paradigm for anesthesia in these cases. Now, after administering conventional anesthesia and observing signs of soft-tissue anesthesia (which is required for a successful supplemental injection), the clinician administers an intraosseous injection. The patient should be informed that the tooth is not as numb as desired and that a little extra anesthetic will ensure his or her comfort. The clinician then explains that this extra anesthetic is placed next to the tooth and that the patient may feel some discomfort during the injection. For mandibular teeth with irreversible pulpitis, the supplemental intraosseous injection has evolved into a routine second injection, which is made before the clinician places a rubber dam and begins the access opening preparation.
The authors recommend using 1.8 ml of 3% mepivacaine plain (e.g., 3% Carbocaine) for the intraosseous injection. The basis for this recommendation is not the cardiovascular risks associated with anesthetic solutions containing a vasoconstrictor but rather the results of clinical research, which indicate that 3% mepivacaine is reasonably effective and has no clinical side effect of increased heart rate.77,221 A few patients may overreact to the heart rate increase produced by solutions containing epinephrine, making treatment difficult or time consuming because the patient must be calmed before treatment can begin. However, many clinicians also use 2% lidocaine with 1:100,000 epinephrine for intraosseous anesthesia. Individual clinicians may want to experiment to determine which anesthetic solution (3% mepivacaine or 2% lidocaine with epinephrine) works best for them.
After anesthesia has been given, the rubber dam is placed, and the access preparation is slowly begun. The patient should be assured that the procedure will be stopped if he or she feels pain.
If the initial pain occurs in dentin, the rubber dam is removed and another cartridge of 3% mepivacaine administered, which should be successful.217 Again, the clinician should make sure that lip numbness has developed from the IAN block and that the anesthetic solution is deposited into medullary bone.
If the initial pain occurs when the pulp is entered, the rubber dam is removed, and another cartridge of 3% mepivacaine is administered. If the patient still has pain, an intrapulpal injection is given. Prudent practitioners often modify the access preparation under these conditions by creating a straight-line shaft that directly opens the pulp tissue with little lateral access preparation (i.e., creating an entry hole the size of a #2 round bur). This provides quick access to the pulp, and the small size of the access facilitates intrapulpal injection with high back-pressure if this technique is indicated.
Maxillary Molar and Premolar Teeth
The initial anesthetic dose of 2% lidocaine with 1:100,000 epinephrine is doubled (to 3.6 ml) for the buccal infiltration.175 A small amount of anesthetic solution usually is administered palatally for the rubber dam retainer. Although fewer anesthetic problems develop with the maxillary molars and premolars than with the mandibular posterior teeth, the clinician should be aware that they can occur.200 Administration of an intraosseous injection before proceeding with access may prove helpful in anesthetizing these teeth. As an alternative, the clinician can administer the anesthetic and then test the pulp with an EPT or cold refrigerant. If the response is negative, access preparation may proceed. If the response is positive, an intraosseous injection should be given. The clinician must keep in mind that pulp testing may not guarantee pulpal anesthesia in teeth with irreversible pulpitis.52,200,217 Therefore, if a patient experiences pain despite a negative result on pulp testing, an intraosseous injection should be given.
Infiltration anesthesia does not last as long in maxillary teeth as in mandibular teeth. If the patient experiences pain during the later stages of instrumentation, an additional infiltration injection is necessary. Occasionally, pain is experienced in the palatal canal of molars. Infiltration over the palatal apex with 0.5 ml of anesthetic solution enhances pulpal anesthesia and may prove helpful.91
Maxillary Anterior Teeth
Anesthetic can be administered initially as a labial infiltration. Articaine with 1:100,000 epinephrine may be used.57 Palatal anesthesia may be necessary for the rubber dam clamp. Although supplemental anesthesia is not often necessary, the intraosseous injection should be successful when given. The duration of anesthesia may be less than 1 hour. An additional infiltration injection may be necessary if the patient experiences pain during the later stages of instrumentation.
Symptomatic Teeth With Total Pulp Necrosis and Periradicular Radiolucencies
Symptomatic teeth with total pulp necrosis and periradicular radiolucencies are an indicator of pain in the periradicular tissue. These teeth may be painful to manipulation and movement during treatment and require extra care.
For mandibular teeth, the IAN block (and long buccal injection) are given in all situations. For maxillary teeth with no swelling, anesthesia is administered with conventional infiltration or a block. If soft-tissue swelling is present (i.e., cellulitis or abscess), infiltration should be done on either side of the swelling, or a block should be administered (second division nerve block, PSA nerve block or infraorbital nerve block). These provide some degree of bone and soft-tissue anesthesia. After signs of anesthesia are observed, the rubber dam is placed, and the access is begun slowly. The pulp chamber usually can be entered without causing the patient discomfort if the tooth is not torqued excessively. Hand and rotary file shaping can be performed without causing much pain if instruments are used with gentleness and care.
Occasionally, the conventional injections do not provide profound anesthesia, particularly in the maxillary teeth. Although results from clinical trials are lacking for treating this region, anecdotal experience suggests that careful consideration of a supplemental injection consisting of an additional palatal infiltration injection may be helpful.
Asymptomatic Teeth With Total Pulp Necrosis and Periradicular Radiolucencies
Asymptomatic teeth with pulp necrosis are the easiest to anesthetize; patient comfort usually is attained without difficulty. Although it may be tempting to proceed without anesthesia, the patient may have pain during instrumentation.
The conventional injections are administered: IAN block and long buccal injection for mandibular teeth, infiltration injections for maxillary teeth. The clinician then proceeds with access and file placement. The patient usually is comfortable in such cases. Rarely, some discomfort may be felt during canal preparation, requiring an intraosseous injection. An intrapulpal injection should not be given, because bacteria and debris may be forced from the canal into the periradicular tissue. Additional infiltration may be necessary in the maxilla if anesthesia begins to wear off.
Incision and Drainage
Clinicians should always attempt to achieve some degree of anesthesia before performing an incision and drainage procedure, because patients tolerate such procedures better. In the mandible, a conventional IAN injection and long buccal injection are given. In the maxilla, 1.8 ml of 2% lidocaine with 1:100,000 epinephrine is infiltrated on both sides of the facial swelling. As an alternative, because we are mostly concerned with soft-tissue anesthesia, a PSA or second division nerve block can be used for premolar and molar teeth and an infraorbital injection given for anterior teeth. For palatal swelling, 0.5 ml of 2% lidocaine with 1:100,000 epinephrine is infiltrated over the greater palatine foramen (molar and premolar teeth) or nasopalatine foramen (anterior teeth). These injections should not be used if swelling is present over the foramen; infiltration should be done on either side of the swelling. The Wand system reduces the pain of palatal injections. Except in a few studies,9,86,235 the computer-assisted injection system caused less pain than the conventional syringe technique for AMSA, palatal injections, and IAN block injections.*
Profound anesthesia usually is difficult to achieve in these cases, and this must be explained to the patient. The swelling is not injected, because traditionally it has been believed that injection directly into a swelling is contraindicated. Reasons for this included the possible spread of infection and the contention that the inflamed tissue’s lower pH would make the anesthetic solution less effective. These ideas may have some merit, but swellings are not injected basically because it is very painful and relatively ineffective. An area of cellulitis has an increased blood supply, and an anesthetic injected into this area is largely carried away into the systemic circulation, which diminishes the anesthetic’s local effectiveness. (See Chapters 2 and 15 for additional information on incision and drainage procedures.)
Periradicular Surgery
In the mandible, the inferior alveolar and long buccal injections are reasonably effective. Additional buccal infiltration injections in the vestibule may be useful to achieve vasoconstriction, particularly in the mandibular anterior region. In the maxilla, infiltration injections are generally effective; usually larger volumes are necessary to provide anesthesia over the surgical field.
If the area of operation is inflamed, anesthesia may not be totally successful. After the flap is reflected, if anesthesia is inadequate, attempts to enhance or regain anesthesia (through additional infiltrations or injecting the sensitive area) are not particularly effective. The effectiveness of surgical anesthesia is decreased by half when compared to anesthesia for nonsurgical procedures, because when reflecting a flap and opening into bone, the anesthetic solution is diluted by bleeding and removed by irrigation.284
As a prophylactic measure, an intraosseous injection using an anesthetic agent with 1:100,000 epinephrine may be administered at the site—after the above injections and before the surgery. This seems to enhance depth of anesthesia and may provide better hemostasis.
Use of a long-acting anesthetic has been advocated for surgery.46,230 In the mandible, this is reasonably effective. In the maxilla, long-acting agents have a shorter duration of anesthesia and decreased epinephrine concentrations, which result in more bleeding during surgery.40,284
After periradicular surgery, administration of a long-acting anesthetic has been suggested.158 However, postsurgical pain is usually not severe and can be managed by analgesics.171
Interim Treatment for Irreversible Pulpitis Using Pulpotomy
Patients often have to decide between extraction and endodontic treatment for irreversible pulpitis. Because of financial circumstances, patients may choose extraction if they are only presented with two choices. One study performed pulpotomies in patients with irreversible pulpitis and restored the teeth with IRM or IRM base/glass ionomer core.161 They found pain was present in 10% of patients at 6 months and in 22% at 12 months. While not ideal, the third option of pulpotomy and temporary restoration may allow the patient time to find the means to finance complete endodontic treatment.49,130,168
Pain Reduction in Irreversible Pulpitis When Endodontic Treatment Is Impossible
Endodontic débridement (pulpectomy or pulpotomy) most predictably relieves the pain of irreversible pulpitis.204 When débridement is not possible, clinicians may prescribe strong analgesics and penicillin in an attempt to relieve the pain. Unfortunately, the pain persists, and penicillin has no effect on the pain of untreated irreversible pulpitis.190 One clinical trial evaluated pain reduction in untreated irreversible pulpitis by giving an intraosseous injection of Depo-Medrol (a long-acting methylprednisolone).76 Clinically, the authors found that Depo-Medrol reduced the pain to manageable levels for up to 7 days before the patient received endodontic treatment, supporting this as a method for controlling a patient’s pain until definitive endodontic treatment can be performed.
Oral Conscious Sedation
Oral conscious sedation is beneficial in reducing patient’s anxiety, but it is not a way to reduce pain during dental treatment.150 Profound local anesthesia is still required to control the patient’s pain.
Summary and Future Directions
The emergence of evidence-based dentistry has rapidly drawn interest across all fields of dentistry. Fortunately, the large number of high-quality, randomized, controlled studies in anesthesia and analgesia provide a wealth of information supporting evidence-based recommendations. The practitioner must focus on high-quality research when making clinical decisions. In contrast, little evidence is available when decisions are based on clinical anecdotes or advertisements. This chapter adopted the evidence-based approach in providing a comprehensive summary of local anesthetic clinical trials for the treatment of patients with endodontic pain.
The prudent practitioner knows that there is no “magic bullet” in pain control. Rather, the clinician must be knowledgeable about the advantages and disadvantages of several anesthetic-vasoconstrictor combinations and the various routes of injection. Clearly, judicious selection of the combination local anesthetics, possibly delivered through multiple sites of injection, is likely to provide predictable anesthesia with minimal exposure to side effects.
Research continues in the development of new or improved anesthetics. Investigations on extended-duration anesthetic formulations suggest that local anesthetics may prove useful for treating postprocedural pain.80,289 In the future, clinicians may be able to provide anesthesia of a specific area for a day or maybe a number of days using liposomal-encapsulated anesthetic agents. The timing of anesthesia would be tailored by how the liposome is formulated to dissolve and the amount of drug in the liposome.
The use of adjuvants to shorten the onset or increase the duration of local anesthetics also has been evaluated. The addition of hyaluronic acid significantly increases bupivacaine anesthesia in rats.253 Tramadol has both a unique central mechanism of action and peripheral anesthetic properties. For patients in pain, 30 to 200 mg of tramadol significantly enhanced postoperative analgesia when combined with 1.5% mepivacaine.224 Other studies have shown that the addition of 1 mg of morphine to a local anesthetic solution significantly increases postoperative analgesia in human beings and animals.63,148 Clonidine directly inhibits pulpal pain neurons99 and enhances anesthesia when combined with a local anesthetic.111,141 Also, it does not increase the risk of cardiotoxicity seen with local anesthetics.93 In a clinical model of postsurgical pain, the combination of lidocaine with bupivacaine produced better long-term pain control than lidocaine alone.145
Considerable ongoing research is directed at the development of new local anesthetic formulations that allow clinicians to better treat patients in pain.
1. Aelig W, Laurence D, O’Neil R, Verrill P. Cardiac effects of adrenaline and felypressin as vasoconstrictors in local anaesthesia for oral surgery under diazepam sedation. Br J Anaesth. 1970;42:174.
2. Agren E, Danielsson K. Conduction block analgesia in the mandible. A comparative investigation of the techniques of Fischer and Gow-Gates. Swed Dent J. 1981;5:91.
3. Akinosi J. A new approach to the mandibular nerve block. Br J Oral Surg. 1977;15:83.
4. Aldous J. Needle deflection: a factor in the administration of local anesthetics. J Am Dent Assoc. 1968;77:602-604.
5. Andersson C. Local anesthesia for infants undergoing circumcision. JAMA. 1998;279:1170.
6. Anonymous: New sulfite regulations. FDA Drug Bull. 1986;16:17.
7. Anonymous: Wydase lyophilized hyaluronidase 150 units, package insert. Philadelphia, Pa: Wyeth Laboratories Inc, 2004.
8. Antonijevic I, Mousa S, Schafer M, Stein C. Perineurial defect and peripheral opioid analgesia in inflammation. J Neurosci. 1995;15:165.
9. Asarch T, Allen K, Petersen B, Beiraghi S. Efficacy of a computerized local anesthesia device in pediatric dentistry. Pediatr Dent. 1999;21:421.
10. Bacsik C, Swift J, Hargreaves K. Toxic systemic reactions of bupivacaine and etidocaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:18.
11. Benkwitz C, Garrison JC, Linden J, Durieux ME, Hollmann MW. Lidocaine enhances G alpha i protein function. Anesthesiology. 2003;99:1093.
12. Berberich G, Reader A, Beck M, Meyers W. Evaluation of the infraorbital nerve block in human maxillary anesthesia. J Endod. 1990;16:192. (abstract)
13. Berlin J, Nusstein J, Reader A, Beck M, Weaver J. Efficacy of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:361.
14. Berns J, Sadove M. Mandibular block injection: a method of study using an injected radiopaque material. J Am Dent Assoc. 1962;65:736.
15. Bigby J, Reader A, Nusstein J, Beck M, Weaver J. Articaine for supplemental intraosseous anesthesia in patients with irreversible pulpitis. J Endod. 2006;32:1044.
16. Bigby J, Reader A, Nusstein J, Beck M. Anesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2007;33:7.
17. Birchfield J, Rosenberg PA. Role of the anesthetic solution in intrapulpal anesthesia. J Endod. 1975;1:26.
18. Black JA, Liu S, Tanaka M, Cummins TR, Waxman SG. Changes in the expression of tetrodotoxin-sensitive sodium channels within dorsal root ganglia neurons in inflammatory pain. Pain. 2004;108:237.
19. Bosco DA, Haas DA, Young ER, Harrop KL. An anaphylactoid reaction following local anesthesia: a case report. Anesth Pain Control Dent. 1993;2:87.
20. Bowles WR, Flores CM, Jackson DL, Hargreaves KM. beta 2-Adrenoceptor regulation of CGRP release from capsaicin-sensitive neurons. J Dent Res. 2003;82:308.
21. Brannstrom M, Lindskog S, Nordenvall K. Enamel hypoplasia in permanent teeth induced by periodontal ligament anesthesia of primary teeth. J Am Dent Assoc. 1984;109:735.
22. Broering R, Reader A, Drum M, Nusstein J, Beck M. A prospective, randomized comparison of the anesthetic efficacy of the greater palatine and high tuberosity second division nerve blocks. J Endod. 2009;35:1337.
23. Burns Y, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of the Palatal-Anterior Superior Alveolar injection. J Am Dent Assoc. 2004;135:1269.
24. Byers MR, Taylor PE, Khayat BG, Kimberly CL. Effects of injury and inflammation on pulpal and periapical nerves. J Endod. 1990;16:78.
25. Cannell H, Kerwala C, Webster K, Whelpton R. Are intraligamentary injections intravascular? Br Dent J. 1993;175:281.
26. Certosimo A, Archer R. A clinical evaluation of the electric pulp tester as an indicator of local anesthesia. Oper Dent. 1996;21:25.
27. Chamberlain T, Davis R, Murchison D, Hansen S, Richardson B. Systemic effects of an intraosseous injection of 2% lidocaine with 1:100,000 epinephrine. Gen Dent. 2000;May-June:299.
28. Chaney MA, Kerby R, Reader A, Beck FM, Meyers WJ, Weaver J. An evaluation of lidocaine hydrocarbonate compared with lidocaine hydrochloride for inferior alveolar nerve block. Anesth Prog. 1991;38:212.
29. Childers M, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the periodontal ligament injection after an inferior alveolar nerve block. J Endod. 1996;22:317.
30. Chiu CY, Lin TY, Hsia SH, Lai SH, Wong KS. Systemic anaphylaxis following local lidocaine administration during a dental procedure. Pediatr Emerg Care. 2004;20:178.
31. Chng H, Pitt Ford T, McDonald F. Effects of prilocaine local anesthetic solutions on pulpal blood flow in maxillary canines. Endod Dent Traumatol. 1996;12:89-95.
32. Claffey E, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2004;30:568.
33. Clark K, Reader A, Beck M, Meyers W. Anesthetic efficacy of an infiltration injection in mandbular anterior teeth following an inferior alveolar nerve block. Anesth Prog. 2002;49:49.
34. Clark S, Reader A, Beck M, Meyers WJ. Anesthetic efficacy of the mylohyoid nerve block and combination inferior alveolar nerve block/mylohyoid nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:557.
35. Coggins R, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the intraosseous injection in maxillary and mandibular teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:634.
36. Cohen H, Cha B, Spangberg L. Endodontic anesthesia in mandibular molars: a clinical study. J Endod. 1993;19:370.
37. Cooley R, Robison S. Comparative evaluation of the 30-gauge dental needle. Oral Surg Oral Med Oral Pathol. 1979;48:400.
38. Corbett IP, Kanaa MD, Whitworth JM, Meechan JG. Articaine infiltration for anesthesia of mandibular first molars. J Endod. 2008;34:514.
39. Cromley N, Adams D. The effect of intraligamentary injections on diseased periodontiums in dogs. Gen Dent. 1991;39:33.
40. Crout RJ, Koraido G, Moore PA. A clinical trial of long-acting local anesthetics for periodontal surgery. Anesth Prog. 1990;37:194.
41. D’Souza J, Walton R, Peterson L. Periodontal ligament injection: An evaluation of extent of anesthesia and postinjection discomfort. J Am Dent Assoc. 1987;114:341.
42. Dagher FB, Yared GM, Machtou P. An evaluation of 2% lidocaine with different concentrations of epinephrine for inferior alveolar nerve block. J Endod. 1997;23:178.
43. Danielsson K, Evers H, Nordenram A. Long-acting local anesthetics in oral surgery: an experimental evaluation of bupivacaine and etidocaine for oral infiltration anesthesia. Anesth Prog. 1985;32:65.
44. Daublander M, Muller R, Lipp M. The incidence of complications associated with local anesthesia in dentistry. Anesth Prog. 1997;44:132-141.
45. Davidson M. Bevel-oriented mandibular injections: needle deflection can be beneficial. Gen Dent. 1989;37:410.
46. Davis W, Oakley J, Smith E. Comparison of the effectiveness of etidocaine and lidocaine as local anesthetic agents during oral surgery. Anesth Prog. 1984;31:159.
47. DeJong R. Neural blockade by local anesthetics. J Am Dent Assoc. 1997;238:1383.
48. Dernedde M, Furlan D, Verbesselt R, Gepts E, Boogaerts JG. Grand mal convulsion after an accidental intravenous injection of ropivacaine. Anesth Analg. 2004;98:521.
49. DeRosa T. A retrospective evaluation of pulpotomy as an alternative to extraction. Gen Den. 2006;54:37.
50. Donaldson D, James-Perdok L, Craig B, Derkson G, Richardson A. A comparison of Ultracaine DS (articaine HCl) and Citanest forte (prilocaine HCl) in maxillary infiltration and mandibular nerve block. J Can Dent Assoc. 1987;53:38.
51. Dougher MJ, Goldstein D Induced anxiety and pain KA L J Anxiety Discord 1 1987 259
52. Dreven LJ, Reader A, Beck M, Meyers WJ, Weaver J. An evaluation of an electric pulp tester as a measure of analgesia in human vital teeth. J Endod. 1987;13:233.
53. Dreyer WP, van Heerden JD The route of periodontal ligament injection of local anesthetic solution de VJJJ J Endod 9 1983 471
54. Dunbar D, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the intraosseous injection after an inferior alveolar nerve block. J Endod. 1996;22:481.
55. Dunsky JL, Moore PA. Long-acting local anesthetics: a comparison of bupivacaine and etidocaine in endodontics. J Endod. 1984;10:457.
56. Edwards R, Head T. A clinical trial of intraligamentary anesthesia. J Dent Res. 1989;68:1210.
57. Evans G, Nusstein J, Drum M, Reader A, Beck M. A prospective, randomized, double-blind comparison of articaine and lidocaine for maxillary infiltrations. J Endod. 2008;34:389.
58. Fernandez C, Reader A, Beck M, Nusstein J. A prospective, randomized, double-blind comparison of bupivacaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005;31:499.
59. Fernieini EM, Bennett JD, Silverman DG, Halaszynski TM. Hemodynamic assessment of local anesthetic administration by laser Doppler flowmetry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:526.
60. Fillingim R, Edwards R. The relationship of sex and clinical pain to experimental pain responses. Pain. 1999;83:419.
61. Finder R, Moore PA. Adverse drug reactions to local anesthesia. Dent Clin North Am. 2002;46:747.
62. Fiset L, Leroux B, Rothen M, Prall C, Zhu C, Ramsay DS. Pain control in recovering alcoholics: effects of local anesthesia. J Stud Alcohol. 1997;58:291.
63. Fletcher D, Gentili M, Mazoit JX, Samii K. Additivity of bupivacaine and morphine for peripheral analgesia in rats. Fundam Clin Pharmacol. 2000;14:327.
64. Foster W, McCartney M, Reader A, Beck M. Anesthetic efficacy of buccal and lingual infiltrations of lidocaine following an inferior alveolar nerve block in mandibular posterior teeth. Anesth Prog. 2007;54:163.
65. Friedlander AH, Sung EC, Child JS. Radiation-induced heart disease after Hodgkin’s disease and breast cancer treatment: dental implications. J Am Dent Assoc. 2003;134:1615.
66. Friedman M, Hochman M. A 21st century computerized injection system for local pain control. Compendium. 1997;18:995.
67. Friedman M, Hochman M. The AMSA injection: a new concept for local anesthesia of maxillary teeth using a computer-controlled injection system. Quintessence Int. 1998;29:297.
68. Friedman M, Hochman M. P-ASA block injection: a new palatal technique to anesthetize maxillary anterior teeth. J Esthetic Dent. 1999;11:63.
69. Friedman M, Hochman M. Using AMSA and P-ASA nerve blocks for esthetic restorative dentistry. Gen Dent. 2001;5:506.
70. Frommer J, Mele F, Monroe C. The possible role of the mylohyoid nerve in mandibular posterior tooth sensation. J Am Dent Assoc. 1972;85:113.
71. Froum SJ, Tarnow D, Caiazzo A, Hochman MN. Histologic response to intraligament injections using a computerized local anesthetic delivery system. A pilot study in mini-swine. J Periodontol. 2000;71:1453-1459.
72. Fuhs QM, Walker WA3rd, Gough RW, Schindler WG, Hartman KS. The periodontal ligament injection: histological effects on the periodontium in dogs. J Endod. 1983;9:411.
73. Fukayama H, Yoshikawa F, Kohase H, Umino M, Suzuki N. Efficacy of anterior and middle superior alveolar (AMSA) anesthesia using a new injection system: The Wand. Quintessence Int. 2003;34:537.
74. Galbreath J. Tracing the course of the mandibular block injection. Oral Surg Oral Med Oral Pathol. 1970;30:571.
75. Galili D, Kaufman E, Garfunkel AA, Michaeli Y. Intraligamental anesthesia: a histological study. Int J Oral Surg. 1984;13:511-516.
76. Gallatin E, Reader A, Nist R, Beck M. Pain reduction in untreated irreversible pulpitis using an intraosseous injection of Depo-Medrol. J Endod. 2000;26:633.
77. Gallatin E, Stabile P, Reader A, Nist R, Beck M. Anesthetic efficacy and heart rate effects of the intraosseous injection of 3% mepivacaine after an inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:83.
78. Gallatin J, Nusstein J, Reader A, Beck M, Weaver J. A comparison of injection pain and postoperative pain of two intraosseous anesthetic techniques. Anesth Prog. 2003;50:111.
79. Gallatin J, Reader A, Nusstein J, Beck M, Weaver J. A comparison of two intraosseous anesthetic techniques in mandibular posterior teeth. J Am Dent Assoc. 2003;134:1476.
80. Garry MG, Jackson DL, Geier HE, Southam M, Hargreaves KM. Evaluation of the efficacy of a bioerodible bupivacaine polymer system on antinociception and inflammatory mediator release. Pain. 1999;82:49.
81. Gibson RS, Allen K, Hutfless S, Beiraghi S. The Wand vs. traditional injection: a comparison of pain related behaviors. Pediatr Dent. 2000;22:458-462.
82. Gill C, Orr D. A double-blind crossover comparison of topical anesthetics. J Am Dent Assoc. 1979;98:213.
83. Gold M, Reichling D, Shuster M Hyperalgesic agents increase a tetrodotoxin-resistant Na+-current in nociceptors J L Proc Natl Acad Sci 93 1996 1108 U S A
84. Goldberg S, Reader A, Drum M, Nusstein J, Beck M. A Comparison of the anesthetic efficacy of the conventional inferior alveolar, Gow-Gates and Vazirani-Akinosi techniques. J Endod. 2008;34:1306.
85. Goldstein DS, Dionne R, Sweet J, et al. Circulatory, plasma catecholamine, cortisol, lipid, and psychological responses to a real-life stress (third molar extractions): effects of diazepam sedation and of inclusion of epinephrine with the local anesthetic. Psychosom Med. 1982;44:259.
86. Goodell G, Gallagher F, Nicoll B. Comparison of a controlled injection pressure system with a conventional technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:88.
87. Goodman A, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks. Anesth Prog. 2006;53:131.
88. Gow-Gates G. Mandibular conduction anesthesia: a new technique using extra-oral landmarks. Oral Surg Oral Med Oral Pathol. 1973;36:321.
89. Gray R, Lomax A, Rood J. Periodontal ligament injection: with or without a vasoconstrictor? Br Dent J. 1987;162:263.
90. Gross R, McCartney M, Reader A, Beck M. A prospective, randomized, double-blind comparison of bupivacaine and lidocaine for maxillary infiltrations. J Endod. 2007;33:1021.
91. Guglielmo A, Nist R, Reader A. Palatal and buccal infiltrations in maxillary first molar anesthesia. J Dent Res. 1993;72:274. (abstract)
92. Guglielmo A, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy and heart rate effects of the supplemental intraosseous injection of 2% mepivacaine with 1:20,000 levonordefrin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:284.
93. Gulec S, Aydin Y, Uzuner K, Yelken B, Senturk Y. Effects of clonidine pre-treatment on bupivacaine and ropivacaine cardiotoxicity in rats. Eur J Anaesthesiol. 2004;21:205.
94. Haas D, Harper D, Saso M, Young E. Comparison of articaine and prilocaine anesthesia by infiltration in maxillary and mandibular arches. Anesth Prog. 1990;37:230.
95. Haas D, Harper D, Saso M, Young E. Lack of differential effect by Ultracaine (articaine) and Citanest (prilocaine) in infiltration anaesthesia. J Can Dent Assoc. 1991;57:217.
96. Haas DA, Lennon D. A 21 year retrospective study of reports of paresthesia following local anesthetic administration. J Can Dent Assoc. 1995;61:319.
97. Haas DA, Pynn BR, Sands TD. Drug use for the pregnant or lactating patient. Gen Dent. 2000;48:54.
98. Haase A, Reader A, Nusstein J, Beck M, Drum M. Comparing anesthetic efficacy of articaine versus lidocaine as a supplemental buccal infiltration of the mandibular first molar after an inferior alveolar nerve block block. J Am Dent Assoc. 2008;139:1228.
99. Hannan L, Reader A, Nist R, Beck M, Meyers WJ. The use of ultrasound for guiding needle placement for inferior alveolar nerve blocks. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:658.
100. Hargreaves KM, Jackson DL, Bowles WR. Adrenergic regulation of capsaicin-sensitive neurons in dental pulp. J Endod. 2003;29:397.
101. Hargreaves KM, Keiser K. Local anesthetic failure in endodontics: mechanisms and management. Endod Topics. 2003;1:26.
102. Hasse AL, Heng MK, Garrett NR. Blood pressure and electrocardiographic response to dental treatment with use of local anesthesia. J Am Dent Assoc. 1986;113:639.
103. Hersh E, Houpt M, Cooper S, Feldman R, Wolff M, Levin L. Analgesic efficacy and safety of an intraoral lidocaine patch. J Am Dent Assoc. 1996;127:1626.
104. Hersh E, Moore P, Papas A, et al. Reversal of soft-tissue local anesthesia with phentolamine mesylate in adolescents and adults. J Am Dent Assoc. 2008;139:1080.
105. Hidding J, Khoury F. General complications in dental local anesthesia. Dtsch Zahnarztl Z. 1991;46:831-836.
106. Hinkley SA, Reader A, Beck M, Meyers WJ. An evaluation of 4% prilocaine with 1:200,000 epinephrine and 2% mepivacaine with 1:20,000 levonordefrin compared with 2% lidocaine with:100,000 epinephrine for inferior alveolar nerve block. Anesth Prog. 1991;38:84.
107. Hochman M, Chiarello D, Hochman CB, et al. Computerized local anesthetic delivery vs. traditional syringe technique. Subjective pain response. NY State Dent J. 1997;63:24-29.
107a. Hochman M, Friedman M. In vitro study of needle deflection: a linear insertion technique versus a bidirectional rotation insertion technique. Quintessence Int. 2000;31:33.
108. Hollmann MW, Herroeder S, Kurz KS, et al. Time-dependent inhibition of G protein-coupled receptor signaling by local anesthetics. Anesthesiology. 2004;100:852.
109. Hull T, Rothwell B. Intraosseous anesthesia comparing lidocaine and etidocaine. J Dent Res. 1998;77:197. (abstract)
110. Hutchins H, Young F, Lackland D, Fishburne C. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44:87.
111. Hutschala D, Mascher H, Schmetterer L, et al. Clonidine added to bupivacaine enhances and prolongs analgesia after brachial plexus block via a local mechanism in healthy volunteers. Eur J Anaesthesiol. 2004;21:198.
112. Ianiro SR, Jeansonne JB, McNeal SF, Eleazer PD. The effect of preoperative acetaminophen or a combination of acetaminophen and ibuprofen on the success of the inferior alveolar nerve block for teeth with irreversible pulpitis. J Endod. 2007;33:11.
113. Ingle J, Bakland L Endodontics vol. 5 2002 BC Decker Hamilton, Ontario p. 391
114. Jage J. Circulatory effects of vasoconstrictors combined with local anesthetics. [Review] [33 refs]. Anesth Pain Control Dent. 1993;2:81.
115. Jakobs W, Ladwig B, Cichon P, Ortel R, Kirch W. Serum levels of articaine 2% and 4% in children. Anesth Prog. 1995;42:113-115.
116. Jastak J, Yagiela J Local anesthesia of the oral cavity D D 1995 Elsevier Health Science New York
117. Jensen J, Nusstein J, Drum M, Reader A, Beck M. Anesthetic efficacy of a repeated intraosseous injection following a primary intraosseous injection. J Endod. 2008;34:126.
118. Jeske A, Boschart B. Deflection of conventional versus nondeflecting dental needles in vitro. Anesth Prog. 1985;32:62-64.
119. Johnson G, Hlava G, Kalkwarf K. A comparison of periodontal intraligamental anesthesia using etidocaine HCL and lidocaine HCL. Anesth Prog. 1985;32:202.
120. Jones VR, Rivera EM, Walton RE. Comparison of carbon dioxide versus refrigerant spray to determine pulpal responsiveness. J Endod. 2002;28:531.
121. Joyce AP, Donnelly JC. Evaluation of the effectiveness and comfort of incisive nerve anesthesia given inside or outside the mental foramen. J Endod. 1993;19:409.
122. Jung IY, Kim JH, Kim ES, Lee CY, Lee SJ. An evaluation of buccal infiltrations and inferior alveolar nerve blocks in pulpal anesthesia for mandibular first molars. J Endod. 2008;34:11.
123. Kanaa MD, Meechan JG, Corbett IP, Whitworth JM. Speed of injection influences efficacy of inferior alveolar nerve blocks: a double-blind randomized controlled trial in volunteers. J Endod. 2006;32:919.
124. Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine and lidocaine mandibular buccal infiltration anesthesia; a prospective randomized double-blind cross-over study. J Endod. 2006;32:296.
125. Karkut B, Reader A, Nist R, Beck M, Meyers W. Evaluation of the extraoral infraorbital nerve block in maxillary anesthesia. J Dent Res. 1993;72:274. (abstract)
126. Katz S, Reader A, Beck M, Meyers W. Anesthetic comparison of prilocaine and lidocaine in human maxillary infiltrations. J Endod. 1989;15:173. (abstract)
127. Kaufman E, Galili D, Garfunkel A. Intraligamentary anesthesia: a clinical study. J Pros Dent. 1983;49:337.
128. Kaufman E, Solomon V, Rozen L, Peltz R. Pulpal efficacy of four lidocaine solutions injected with an intraligamentary syringe. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1994;78:17.
129. Kaufman E, Weinstein P, Milgrom P. Difficulties in achieving local anesthesia. J Am Dent Assoc. 1984;108:205.
130. Keenan JV, Farman A, Fedorowicz Z, Newton JT. A Cochrane systematic review finds no evidence to support the use of antibiotics for pain relief in irreversible pulpitis. J Endod. 2006;32:87.
131. Keller B. Comparison of the effectiveness of two topical anesthetics and a placebo in reducing injection pain. Hawaii Dent J. 1985;16:10.
132. Kennedy M, Reader A, Beck M, Weaver J. Anesthetic efficacy of ropivacaine in maxillary anterior infiltration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:406.
133. Kennedy S, Reader A, Nusstein J, Beck M, Weaver J. The significance of needle deflection in success of the inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2003;29:630.
134. Kim S. Ligamental injection: a physiological explanation of its efficacy. J Endod. 1986;12:486.
135. Kindler CH, Paul M, Zou H, et al. Amide local anesthetics potently inhibit the human tandem pore domain background K+ channel TASK-2 (KCNK5). J Pharmacol Exp Ther. 2003;306:84.
136. Kirby C, Eckenhoff J, Looby J. The use of hyaluronidase with local anesthetic agents in nerve block and infiltration anesthesia. Surgery. 1949;25:101.
137. Klein SM, Pierce T, Rubin Y, Nielsen KC, Steele SM. Successful resuscitation after ropivacaine-induced ventricular fibrillation. [Erratum appears in Anesth Analg. 2004 Jan;98(1):200]. Anesth Analg. 2003;97:901.
138. Kleinknecht R, Klepac R, Alexander L. Origins and characteristics of fear of dentistry. J Am Dent Assoc. 1993;86:842.
139. Knoll-Kohler E, Frie A, Becker J, Ohlendorf D. Changes in plasma epinephrine concentration after dental infiltration anesthesia with different doses of epinephrine. J Dent Res. 1989;68:1098.
140. Knoll-Kohler E, Knoller M, Brandt K, Becker J. Cardiohemodynamic and serum catecholamine response to surgical removal of impacted mandibular third molars under local anesthesia: a randomized double-blind parallel group and crossover study. J Oral Maxillofac Surg. 1991;49:957.
141. Kopacz DJ, Bernards CM. Effect of clonidine on lidocaine clearance in vivo: a microdialysis study in humans. Anesthesiology. 2001;95:1371.
142. Krupinski J, Krupinska A. Dental pulp analgesia before its amputation or removal. Czasopismo Stomatologiczne. 1976;29(5):383-392.
143. Lai J, Porreca J, Hunter J Voltage-gated sodium channels and hyperalgesia M G Ann Rev Pharmacol 44 2004 371
144. Laviola M, McGavin S, Freer G, et al. Randomized study of phentolamine mesylate for reversal of local anesthesia. J Dent Res. 2008;87:635.
145. Lee-Elliott CE, Dundas D, Patel U. Randomized trial of lidocaine vs lidocaine/bupivacaine periprostatic injection on longitudinal pain scores after prostate biopsy. J Urol. 2004;171:247.
146. Lee S, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of the Anterior Middle Superior Alveolar (AMSA) injection. Anesth Prog. 2004;51:80.
147. Liddell A Gender and age differences in attitudes to dental pain and dental control D L Community Dent Oral Epidemiol 25 1997 314
148. Likar R, Koppert W, Blatnig H, et al. Efficacy of peripheral morphine analgesia in inflamed, non-inflamed and perineural tissue of dental surgery patients. J Pain Sympt Manag. 2001;21:330.
149. Lin L., et al. Periodontal ligament injection: effects on pulp tissue. J Endod. 1985;11(12):529-534.
150. Lindemann MRA, Nusstein J, Drum M, Beck M. Effect of sublingual triazolam on the efficacy of the inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2008;34:1167.
151. Linden E, Abrams H, Matheny J, Kaplan A, Kopczyk R, Jasper S. A comparison of postoperative pain experience following periodontal surgery using two local anesthetic agents. J Periodontol. 1986;57:637.
152. List G, et al. Gingival crevicular fluid response to various solutions using the intraligamentary injection. Quint Inter. 1988;19:559-563.
153. Littner MM, Tamse A, Kaffe I. A new technique of selective anesthesia for diagnosing acute pulpitis in the mandible. J Endod. 1983;9:116.
154. Loetscher C, Melton D, Walton R. Injection regimen for anesthesia of the maxillary first molar. J Am Dent Assoc. 1988;117:337.
155. Looby J, Kirby C. Use of hyaluronidase with local anesthetic agents in dentistry. J Am Dent Assoc. 1949;38:1.
156. Malamed S. Articaine versus lidocaine: the author responds. Calif Dent J. 2007;35:383.
157. Malamed S. The Gow-Gates mandibular block. Evaluation after 4,275 cases. Oral Surg Oral Med Oral Pathol. 1981;51:463.
158. Malamed S Handbook of local anesthesia 5th edition 2004 Mosby St Louis
159. Malamed S. The periodontal ligament (PDL) injection: an alternative to inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol. 1982;53:117.
160. Malamed S, Gagnon S, Leblanc D. A comparison between articaine HCl and lidocaine HCl in pediatric dental patients. Pediatr Dent. 2000;22:307.
161. Malamed S, Gagnon S, Leblanc D. Efficacy of articaine: a new amide local anesthetic. J Am Dent Assoc. 2000;131:635.
162. Malamed SF, Gagnon S, Leblanc D. Articaine hydrochloride: a study of the safety of a new amide local anesthetic. J Am Dent Assoc. 2001;132:177.
163. Martin M, Ramsay D, Whitney C, Fiset L, Weinstein P. Topical anesthesia: Differentiating the pharmacological and psychological contributions to efficacy. Anesth Prog. 1994;41:40.
164. Martinez G, Benito P, Fernandez C, San Hipolito M, Penarrocha D. A comparative study of direct mandibular nerve block and the Akinosi technique. Med Oral. 2003;8:143.
165. Martinkus A, Reader A, Nusstein J, Beck M. Anesthetic efficacy of lidocaine and mepivacaine in the maxillary second division nerve block. J Endod. 2004;30:263. (abstract)
166. Mason R, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine and 3% mepivacaine for maxillary infiltrations. J Endod. 2009;35:1173.
167. Matthews R, Drum M, Reader A, Nusstein J, Beck M. Articaine for supplemental, buccal mandibular infiltration anesthesia in patients with irreversible pulpitis when the inferior alveolar nerve block fails. J Endod. 2009;35:343.
168. McDougal RA, Delano EO, Caplan D, Sigurdsson A. Success of an alternative for interim management of irreversible pulpitis. J Am Dent Assoc. 2004;135:1707.
169. McLean C, Reader A, Beck M, Meyers WJ. An evaluation of 4% prilocaine and 3% mepivacaine compared with 2% lidocaine (1:100,000 epinephrine) for inferior alveolar nerve block. J Endod. 1993;19:146.
170. Meechan J. A comparison of ropivacaine and lidocaine with epinephrine for intraligamentary anesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:469.
171. Meechan J, Blair G. The effect of two different local anaesthetic solutions on pain experience following apicoectomy. Br Dent J. 1993;175:410.
172. Meechan J, Ledvinka J. Pulpal anesthesia for mandibular central incisor teeth: a comparison of infiltration and intraligamentary injections. Int Endod J. 2002;35:629.
173. Meechan JG, Rawlins MD. The effects of two different dental local anesthetic solutions on plasma potassium levels during third molar surgery. Oral Surg Oral Med Oral Pathol. 1988;66:650.
174. Meyer R, Jakubowski W. Use of tripelenamine and diphenhydramine as local anesthetics. J Am Dent Assoc. 1964;69:112.
175. Mikesell A, Drum M, Reader A, Beck M. Anesthetic efficacy of 1.8 mL and 3.6 mL of 2% lidocaine with 1:100,000 epinephrine for maxillary infiltrations. J Endod. 2008;34:121.
176. Mikesell P, Nusstein J, Reader A, Beck M, Weaver J. A comparison of articaine and lidocaine for inferior alveolar nerve blocks. J Endodon. 2005;31:265.
177. Milgrom P, Coldwell S, Getz T, Weinstein P, Ramsay D. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756.
178. Milgrom P, Fiset L, Melnick S, Weinstein P. The prevalence and practice management consequences of dental fear in a major US city. J Am Dent Assoc. 1988;116:61.
179. Modaresi J, Dianat O, Mozayeni MA. The efficacy comparison of ibuprofen, acetaminophen-codeine, and placebo premedication therapy on the depth of anesthesia during treatment of inflamed teeth. Oral Surg Oral Med Oral Pathol. 2006;102:399.
180. Modaresi J, Dianat O, Soluti A. Effect of pulp inflammation on nerve impulse quality with or without anesthesia. J Endod. 2008;34:438.
181. Moller R, Covine B. Cardiac electrophysiologic effects of articaine compared with bupivacaine and lidocaine. Anesth Analg. 1993;76:1266-1273.
182. Montagnese TA, Reader A, Melfi R. A comparative study of the Gow-Gates technique and a standard technique for mandibular anesthesia. J Endod. 1984;10:158.
183. Moore KD, Reader A, Meyers WJ, Beck M, Weaver J. A comparison of the periodontal ligament injection using 2% lidocaine with 1:100,000 epinephrine and saline in human mandibular premolars. Anesth Prog. 1987;34:181.
184. Moore PA, Boynes SG, Hersh EV, et al. Dental anesthesia using 4% articaine 1:200,000 epinephrine: two clinical trials. J Am Dent Assoc. 2006;137:1572.
185. Moore PA, Dunsky JL. Bupivacaine anesthesia—a clinical trial for endodontic therapy. Oral Surg Oral Med Oral Pathol. 1983;55:176.
186. Moore TJ, Walsh CS, Cohen MR. Reported adverse event cases of methemoglobinemia associated with benzocaine products. Arch Intern Med. 2004;164:1192.
187. Morais-Almeida M, Gaspar A, Marinho S, Rosado-Pinto J. Allergy to local anesthetics of the amide group with tolerance to procaine. Allergy. 2003;58:827.
188. Morin C, Lund JP, Villarroel T, Clokie CM Differences between the sexes in post-surgical pain JS F Pain 85 2000 79
189. Naftalin L, Yagiela J. Vasoconstrictors: indications and precautions. Dent Clin North Am. 2002;46:733.
190. Nagle D, Reader A, Beck M, Weaver J. Effect of systemic penicillin on pain in untreated irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:636.
191. Nelson P. Letter to the editor. J Am Dent Assoc. 1981;103:692.
192. Nicholson JW, Berry TG, Summitt JB, Yuan CH, Witten TM. Pain perception and utility: a comparison of the syringe and computerized local injection techniques. Gen Dent. 2001;49:167-173.
193. Nist RA, Reader A, Beck M, Meyers WJ. An evaluation of the incisive nerve block and combination inferior alveolar and incisive nerve blocks in mandibular anesthesia. J Endod. 1992;18:455.
194. Nusstein J, Berlin J, Reader A, Beck M, Weaver J. Comparison of injection pain, heart rate increase and post-injection pain of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system. Anesth Prog. 2004;51:126.
195. Nusstein J, Burns Y, Reader A, Beck M, Weaver J. Injection pain and postinjection pain of the palatal-anterior superior alveolar injection, administered with the Wand Plus system, comparing 2% lidocaine with 1:100,000 epinephrine to 3% mepivacaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:164.
196. Nusstein J, Claffey E, Reader A, Beck M, Weaver J. Anesthetic effectiveness of the supplemental intraligamentary injection, administered with a computer-controlled local anesthetic delivery system, in patients with irreversible pulpitis. J Endod. 2005;31:354.
197. Nusstein J, Kennedy S, Reader A, Beck M, Weaver J. Anesthetic efficacy of the supplemental X-tip intraosseous injection in patients with irreversible pulpitis. J Endod. 2003;29:724.
198. Nusstein, J, Lee S, Reader A, Weaver J: Injection pain and postinjection pain of the anterior middle superior alveolar injection administered with the Wand or conventional syringe. 98:124, 2004.
199. Nusstein J, Reader A, Beck FM. Anesthetic efficacy of different volumes of lidocaine with epinephrine for inferior alveolar nerve blocks. General Dentistry. 2002;50(4):372-375. quiz 376–377
200. Nusstein J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irreversible pulpitis. J Endod. 1998;24:487.
201. Nusstein J, Wood M, Reader A, Beck M, Weaver J. Comparison of the degree of pulpal anesthesia achieved with the intraosseous injection and infiltration injection using 2% lidocaine with 1:100,000 epinephrine. Gen Dent. 2005;53:50.
202. Nusstein JM, Beck M. Effectiveness of 20% benzocaine as a topical anesthetic for intraoral injections. Anesth Prog. 2003;50:159.
203. Oertel R, Ebert U, Rahn R, Kirch W. The effect of age on pharmacokinetics of the local anesthetic drug articaine. Reg Anesth Pain Med. 1999;24:524-528.
204. Oguntebi B, DeSchepper E, Taylor T, White C, Pink F. Postoperative pain incidence related to the type of emergency treatment of symptomatic pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1992;73:479.
205. Papagiannopoulou P, Argiriadou H, Georgiou M, Papaziogas B, Sfyra E, Kanakoudis F. Preincisional local infiltration of levobupivacaine vs ropivacaine for pain control after laparoscopic cholecystectomy. Surg Endosc. 2003;17:1961.
206. Parente SA, Anderson RW, Herman WW, Kimbrough WF, Weller RN. Anesthetic efficacy of the supplemental intraosseous injection for teeth with irreversible pulpitis. J Endod. 1998;24:826.
207. Pertot W, Dejou J. Bone and root resorption. Effects of the force developed during periodontal ligament injections in dogs. Oral Surg, Oral Med, Oral Pathol. 1992;74:357.
208. Peterson J, Matsson L, Nation W. Cementum and epithelial attachment response to the sulcular and periodontal ligament injection techniques. Pediatr Dent. 1983;5:257-260.
209. Peurach J. Pulpal response to intraligamentary injection in cynomologus monkey. Anesth Prog. 1985;32:73-75.
210. Pitt Ford T, Seare M, McDonald F. Action of adrenaline on the effect of dental local anaesthetic solutions. Endod Dent Traumatol. 1993;9:31-35.
211. Plamondon T, Walton R, Graham G, Houston G, Snell G. Pulp response to the combined effects of cavity preparation and periodontal ligament injection. Oper Dent. 1990;15:86.
212. Pogrel M. Permanent nerve damage from inferior alveolar nerve blocks—an update to include atricaine. Calif Dent J. 2007;35:217.
213. Premdas C, Pitt Ford T. Effect of palatal injections on pulpal blood flow in premolars. Endod Dent Traumatol. 1995;11:274-278.
214. Primosch R, Brooks R. Influence of anesthetic flow rate delivered by the Wand local anesthetic system on pain response to palatal injections. Am J Dent. 2002;15:15-20.
215. Rawson R, Orr D. Vascular penetration following intraligamental injection. J Oral Maxillofac Surg. 1985;43:600.
216. Reemers T, Glickman G, Spears R, He J. The efficacy of the IntraFlow intraosseous injection as a primary anesthesia technique. J Endod. 2008;34:280.
217. Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:676.
218. Reitz J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of a repeated intraosseous injection given 30 min following an inferior alveolar nerve block/intraosseous injection. Anesth Prog. 1998;45:143.
219. Reitz J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the intraosseous injection of 0.9 mL of 2% lidocaine (1:100,000 epinephrine) to augment an inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:516.
220. Replogle K, Reader A, Nist R, Beck M, Weaver J, Meyers WJ. Anesthetic efficacy of the intraosseous injection of 2% lidocaine (1:100,000 epinephrine) and 3% mepivacaine in mandibular first molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:30.
221. Replogle K, Reader A, Nist R, Beck M, Weaver J, Meyers WJ. Cardiovascular effects of intraosseous injections of 2 percent lidocaine with 1:100,000 epinephrine and 3 percent mepivacaine. J Am Dent Assoc. 1999;130:649.
222. Ridenour S, Reader A, Beck M, Weaver J. Anesthetic efficacy of a combination of hyaluronidase and lidocaine with epinephrine in inferior alveolar nerve blocks. Anesth Prog. 2001;48:9.
223. Roahen JO, Marshall FJ. The effects of periodontal ligament injection on pulpal and periodontal tissues. J Endod. 1990;16:28.
224. Robaux S, Blunt C, Viel E, et al. Tramadol added to 1.5% mepivacaine for axillary brachial plexus block improves postoperative analgesia dose-dependently. Anesth Analg. 2004;98:1172.
225. Robertson D, Nusstein J, Reader A, Beck M. Anesthetic efficacy of articaine and lidocaine in buccal infiltration injections of the mandibular first molar. J Am Dent Assoc. 2007;138:1104.
226. Robison SF, Mayhew RB, Cowan RD, Hawley RJ. Comparative study of deflection characteristics and fragility of 25-, 27-, and 30-gauge short dental needles. J Am Dent Assoc. 1984;109:920-924.
227. Rood J. The nerve supply of the mandibular incisor region. Br Dent J. 1977;143:227.
228. Rood JP. Adverse reaction to dental local anesthetic injection—‘allergy’ is not the cause. Br Dent J. 2000;189:380.
229. Rosenberg PA, Amin KG, Zibari Y, Lin LM. Comparison of 4% articaine with 1:100,000 epinephrine and 2% lidocaine with 1:100,000 epinephrine when used as a supplemental anesthetic. J Endod. 2007;33:403.
230. Rosenquist J, Rosenquist K, Lee P. Comparison between lidocaine and bupivacaine as local anesthetics with diflunisal for postoperative pain control after lower third molar surgery. Anesth Prog. 1988;35:1.
231. Rosivack R, Koenigsberg S, Maxwell K. An analysis of the effectiveness of two topical anesthetics. Anesth Prog. 1990;37:290.
232. Roy M, Nakanishi T. Differential properties of tetrodotoxin-sensitive and tetrodotoxin-resistant sodium channels in rat dorsal root ganglion neurons. J Neurosci. 1992;12:2104.
233. Ryan JF, Jureidini B, Hodges JS, Baisden M, Swift JQ, Bowles WR. Gender differences in analgesia for endodontic pain. J Endod. 2008;34:552.
234. Salomen M, Forsell H, Sceinin M. Local dental anesthesia with lidocaine and adrenalin: effects on plasma catecholamines, heart rate, and blood pressure. Int J Oral Maxillofac Surg. 1988;17:392.
235. Saloum F, Baumgartner J, Marshall G A clinical comparison of pain perception to the Wand and a traditional syringe J T Oral Surg Oral Med Oral Pathol Oral Radiol Endod 86 2000 691
236. Schertzer E, Malamed S. Articaine vs. Lidocaine. J Am Dent Assoc. 2000;131:1248.
237. Schleder JR, Reader A, Beck M, Meyers WJ. The periodontal ligament injection: a comparison of 2% lidocaine, 3% mepivacaine, and 1:100,000 epinephrine to 2% lidocaine with 1:100,000 epinephrine in human mandibular premolars. J Endod. 1988;14:397.
238. Scott J, Drum M, Reader A, Nusstein J, Beck M. Efficacy of a repeated infiltration to prolong duration of pulpal anesthesia in maxillary lateral incisors. J Am Dent Assoc. 2009;140:318.
239. Seng G, Kraus K, Cartridge G. Confirmed allergic reactions to amide local anesthetics. Gen Den. 1996;44:52.
240. Sherman MG, Flax M, Namerow K, Murray PE. Anesthetic efficacy of the Gow-Gates injection and maxillary infiltration with articaine and lidocaine for irreversible pulpitis. J Endod. 2008;34:656.
241. Shojaei A, Haas D. Local anesthetic cartridges and latex allergy: a literature review. J Can Dent Assoc. 2002;68:62206.
242. Simon D, Jacobs L, Senia E, Walker W. Intraligamentary anesthesia as an aid in endodontic diagnosis. Oral Surg, Oral Med, Oral Pathol. 1982;54:77.
243. Simon F, Reader A, Meyers W, et al. Evaluation of a peripheral nerve stimulator in human mandibular anesthesia. J Dent Res. 1990;69:278. (abstract)
244. Simon M, Gielen M, Alberink N, et al. Intravenous regional anesthesia with 0.5% articaine, 0.5% lidocaine, or 0.5% prilocaine. A double-blind randomized clinical study. Reg Anesth. 1997;22:20-34.
245. Sinnott CJ, Strichartz GR. Levobupivacaine versus ropivacaine for sciatic nerve block in the rat. Reg Anesth Pain Med. 2003;28:294.
246. Sisk A. Evaluation of the Akinosi mandibular block technique in oral surgery. Oral Maxillofac Surg. 1986;44:113.
247. Smith G, Pashley D. Periodontal ligament injection: evaluation of systemic effects. Oral Surg Oral Med Oral Pathol. 1983;56:571.
248. Smith G, Walton R. Periodontal ligament injections: Distribution of injected solutions. Oral Surg, Oral Med, Oral Pathol. 1983;55:232.
249. Smith G, Walton R, Abbott B. Clinical evaluation of periodontal ligament anesthesia using a pressure syringe. J Am Dent Assoc. 1983;107:953.
250. Sorensen H, Skidmore L, Rzasa R, Kleier S, Levinson S, Henry M. Comparison of pulpal sodium channel density in normal teeth to diseased teeth with severe spontaneous pain. J Endod. 2004;30:287. (abstract)
251. Stabile P, Reader A, Gallatin E, Beck M, Weaver J. Anesthetic efficacy and heart rate effects of the intraosseous injection of 1.5% etidocaine (1:200,000 epinephrine) after an inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:407.
252. Steinkruger G, Nusstein J, Reader A, Beck M, Weaver J. The significance of needle bevel orientation in success of the inferior alveolar nerve block. J Am Dent Assoc. 2006;137:1685.
253. Stevens MF, Hoppe M, Holthusen H, Lipfert P. Tetrodotoxin-induced conduction blockade is prolonged by hyaluronic acid with and without bupivacaine. [Republished from Acta Anaesthesiol Scand. 2004 Jan;48(1):128–134; PMID: 14674985]. Acta Anaesthesiol Scand. 2004;48:128.
254. Stewart SH, Finn PR, Pihi RO. A dose-response study of the effects of alcohol on the perceptions of pain and discomfort due to electric shock in men at high familial-genetic risk for alcoholism. Psychopharmacology. 1995;119:261.
255. Strichartz G. Molecular mechanisms of nerve block by local anesthetics. Anesthesiology. 1967;45:421.
256. Susi L, Reader A, Nusstein J, Beck M, Weaver J, Drum M. Heart rate effects of intraosseous injections using slow and fast rates of anesthetic solution deposition. Anesth Prog. 2008;55:9.
257. Teplitsky P, Hablichek C, Kushneriuk J. A comparison of bupivacaine to lidocaine with respect to duration in the maxilla and mandible. J Can Dent Assoc. 1987;53:475.
258. Todorovic L, Stajcic Z, Petrovic V. Mandibular versus inferior alveolar dental anaesthesia: clinical assessment of 3 different techniques. Int J Oral Maxillofac Surg. 1986;15:733.
259. Tofoli GR, Ramacciato JC, de Oliveira PC, Volpato MC, Groppo FC, Ranali J. Comparison of effectiveness of 4% articaine associated with 1:100,000 or 1:200,000 epinephrine in inferior alveolar nerve block. Anesth Prog. 2003;50:164.
260. olas AG, Pflug AE, Halter JB. Arterial plasma epinephrine concentrations and hemodynamic responses after dental injection of local anesthetic with epinephrine. J Am Dent Assoc. 1982;104:41.
261. Troullos ES, Goldstein DS, Hargreaves KM, Dionne RA. Plasma epinephrine levels and cardiovascular response to high administered doses of epinephrine contained in local anesthesia. Anesth Prog. 1987;34:10.
262. Troullos ES, Hargreaves KM, Goldstein DS, Stull R, Dionne RA. Epinephrine suppresses stress-induced increases in plasma immunoreactive beta-endorphin in humans. J Clin Endocrinol Metab. 1989;69:546.
263. Vahatalo K, Antila H, Lehtinen R. Articaine and lidocaine for maxillary infiltration anesthesia. Anesth Prog. 1993;40:114.
264. anderheyden PJ, Williams RA, Sims TN. Assessment of ST segment depression in patients with cardiac disease after local anesthesia. J Am Dent Assoc. 1989;119:407.
265. VanGheluwe J, Walton R. Intrapulpal injection—factors related to effectiveness. Oral Surg Oral Med Oral Pathol. 1997;19:38.
266. Vreeland DL, Reader A, Beck M, Meyers W, Weaver J. An evaluation of volumes and concentrations of lidocaine in human inferior alveolar nerve block. J Endod. 1989;15:6.
267. Wali M, Reader A, Beck M, Meyers W. Anesthetic efficacy of lidocaine and epinephrine in human inferior alveolar nerve blocks. J Endod. 1988;14:193. (abstract)
268. Wallace JA, Michanowicz AE, Mundell RD, Wilson EG. A pilot study of the clinical problem of regionally anesthetizing the pulp of an acutely inflamed mandibular molar. Oral Surg Oral Med Oral Pathol. 1985;59:517.
269. Walton R, Abbott B. Periodontal ligament injection: a clinical evaluation. J Am Dent Assoc. 1981;103:571.
270. Walton RE. Distribution of solutions with the periodontal ligament injection: clinical, anatomical, and histological evidence. J Endod. 1986;12:492.
271. Warren CA, Mok L, Gordon S, Fouad AF, Gold MS. Quantification of neural protein in extirpated tooth pulp. J Endod. 2008;34:7.
272. Welborn J, Kane J. Conduction anesthesia using diphenhydramine HCL. J Am Dent Assoc. 1964;69:706.
273. Wells JE, Bingham V, Rowland KC, Hatton J. Expression of Nav1.9 channels in human dental pulp and trigeminal ganglion. J Endod. 2007;33:1172.
274. White JJ, Reader A, Beck M, Meyers WJ. The periodontal ligament injection: a comparison of the efficacy in human maxillary and mandibular teeth. J Endod. 1988;14:508.
275. Whitworth J, Kanna MD, Corbett IP, Meechan JG. Influence of injection speed on the effectiveness of incisive/mental nerve block: a randomized, controlled, double-blind study in adult volunteers. J Endod. 2007;33:1149.
276. Wilburn-Goo D, Lloyd L. When patients become cyanotic: acquired methemoglobinemia. J Am Dent Assoc. 1999;130:826.
277. Willett J, Reader A, Drum M, Nusstein J, Beck M. The anesthetic efficacy of diphenhydramine and the combination of diphenhydramine/lidocaine for the inferior alveolar nerve block. J Endod. 2009;34:1446.
278. Wilson S, Johns P, Fuller P. The inferior alveolar and mylohyoid nerves: an anatomic study and relationship to local anesthesia of the anterior mandibular teeth. J Am Dent Assoc. 1984;108:350.
279. Wood M, Reader A, Nusstein J, Beck M, Padgett D, Weaver J. Comparison of intraosseous and infiltration injections for venous lidocaine blood concentrations and heart rate changes after injection of 2% lidocaine with 1:100,000 epinephrine. J Endod. 2005;31:435.
280. Wright G, Weinberger S, Friedman C, et al. The use of articaine local anesthesia in children under 4 years of age—a retrospective report. Anesth Prog. 1989;36:268-271.
281. Wright G, Weinberger S, Marti R, Plotzke O. The effectiveness of infiltration anesthesia in the mandibular primary molar region. Pediatr Dent. 1991;13:278.
282. Wynn RL, Bergman SA, Meiller TF. Paresthesia associated with local anesthetics: a perspective on articaine. Gen Dent. 2003;51:498.
283. Yared GM, Dagher FB. Evaluation of lidocaine in human inferior alveolar nerve block. J Endod. 1997;23(9):575-578.
284. Yamazaki S, Seino H, Ozawa S, Ito H, Kawaai H. Elevation of a periosteal flap with irrigation of the bone for minor oral surgery reduces the duration of action of infiltration anesthesia. Anesth Prog. 2006;53:8.
285. Yesilyurt CBG, Tasdemir T. Summary of: pain perception during inferior alveolar injection adminsitered with the Wand or conventional syringe. Br Dent J. 2008;205(5):258-259.
286. Yonchak T, Reader A, Beck M, Clark K, Meyers WJ. Anesthetic efficacy of infiltrations in mandibular anterior teeth. Anesth Prog. 2001;48:55.
287. Yonchak T, Reader A, Beck M, et al. Anesthetic efficacy of unilateral and bilateral inferior alveolar nerve blocks to determine cross innervation in anterior teeth. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, & Endodontics. 2001;92(2):132-135.
288. Yucel E, Hutchison I. A comparative evaluation of the conventional and closed mouth technique for inferior alveolar nerve block. Aust Dent J. 1995;40:15.
289. Zhang JM, Li H, Munir MA. Decreasing sympathetic sprouting in pathologic sensory ganglia: a new mechanism for treating neuropathic pain using lidocaine. Pain. 2004;109:143.
290. Zorian EV, Sharagin NV. [Comparative evaluation of the topical action of anesthetics on the dental tissues in experimental conditions.]. Stomatologiia. 1974;53(4):1-4.