Evaluation
• Discuss the relationship between critical thinking and evaluation.
• Describe the standards of professional nursing practice for evaluation.
• Explain the relationship among goals of care, expected outcomes, and evaluative measures when evaluating nursing care.
• Give examples of evaluation measures for determining a patient’s progress toward outcomes.
• Evaluate the outcomes of care for a patient.
• Describe how evaluation leads to discontinuation, revision, or modification of a plan of care.
http://evolve.elsevier.com/Potter/fundamentals/
When a repairman comes to a home to fix a leaking faucet, he turns the faucet on to determine the problem, changes or adjusts parts, and rechecks the faucet to determine if the leak is fixed. After a patient diagnosed with pneumonia completes a course of antibiotics, the health care provider often has him or her return to the office to have a chest x-ray examination to determine if the pneumonia has cleared. When a nurse provides wound care, including application of a warm compress, several steps are involved. He or she assesses the appearance of the wound, determines its severity, applies the appropriate form of compress, and returns later to determine if the condition of the wound has improved. These three scenarios depict what ultimately occurs during the process of evaluation. The repairman rechecks the faucet, the physician orders a chest x-ray film, and the nurse reinspects the patient’s wound. Evaluation involves two components: an examination of a condition or situation and a judgment as to whether change has occurred. Ideally after an intervention takes place, evaluation reveals an improvement, a desired outcome.
The previous chapters on the nursing process describe how you apply critical thinking to gather patient data, form nursing diagnoses, develop a plan of care, and implement interventions in the care plan. Evaluation, the final step of the nursing process, is crucial to determine whether, after application of the nursing process, the patient’s condition or well-being improves. You apply all that you know about a patient and his or her condition and your experiences with previous patients to evaluate whether nursing care was effective. You conduct evaluative measures to determine if your patients met expected outcomes, not if nursing interventions were completed. The expected outcomes established during planning are the standards against which the nurse judges whether goals have been met and if care is successful.
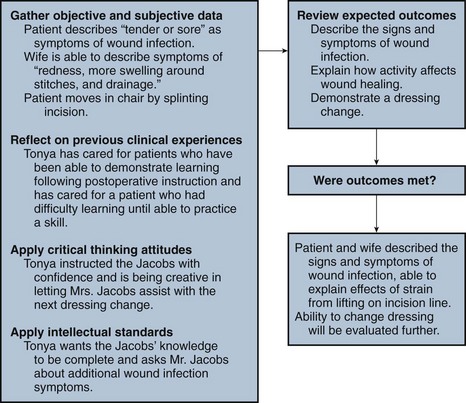
In the continuing case study, Tonya has instructed Mr. Jacobs about necessary wound care. Mrs. Jacobs also participates in the education session. Tonya discusses with the family the importance of wound care in preventing infection and has Mr. and Mrs. Jacobs observe the dressing change. During the dressing change Tonya uses safe and appropriate intervention techniques to protect the integrity of the wound and minimize transmission of infection. She also discusses how physical stress such as bending and lifting strains a suture line; thus Mr. Jacobs needs to limit activity for the first few weeks after surgery. Tonya encourages the Jacobs to ask any questions they have about wound care. Tonya returns to Mr. Jacobs’ room an hour later to evaluate the results of her instruction. For the nursing diagnosis of deficient knowledge, Tonya set the expected outcomes of: “Patient and wife will describe the signs and symptoms of a wound infection, explain how activity affects wound healing, and demonstrate a dressing change correctly.” Mr. Jacobs is resting in bed, and Mrs. Jacobs is reading one of the instruction brochures as Tonya enters the room. Tonya says, “Mrs. Jacobs, I see that you’re reviewing the booklet I gave you. Do you have any questions”? Mrs. Jacobs responds, “I guess I understand what to look for with an infection. I hope I can recognize changes.” Tonya asks, “Tell me the signs of infection.” Mrs. Jacobs replies, “Redness, more swelling around the stitches, and drainage.” Tonya asks Mr. Jacobs, “Are there any other signs of infection?” Mr. Jacobs responds, “You said that my incision would feel more tender or sore and that I might have a fever.” “That’s right,” Tonya remarks. “Tell me why your doctor has limited your lifting for a month.” Mr. Jacobs answers, “So I don’t strain my incision and pull out the stitches.” “Right again,” Tonya affirms,” I think that before you go home tomorrow we should let you watch one more dressing change and even let your wife help me.”
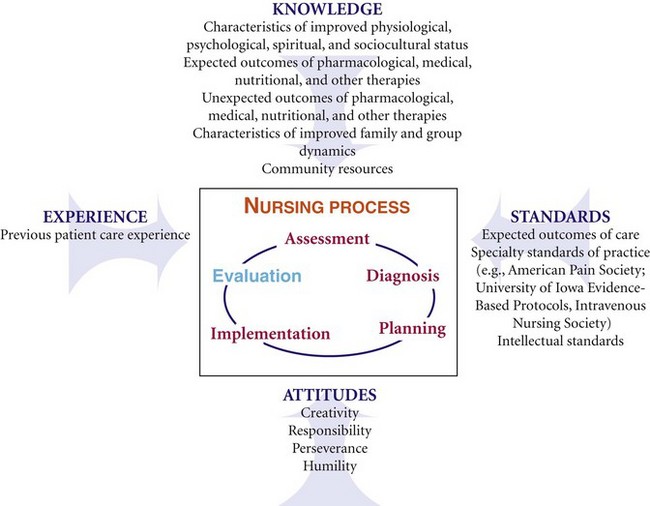
Evaluation is an ongoing process that occurs whenever you have contact with a patient. Once you deliver an intervention, you gather subjective and objective data from the patient, family, and health care team members. You also review knowledge regarding the patient’s current condition, treatment, resources available for recovery, and expected outcomes. By referring to previous experiences caring for similar patients, you are in a better position to know how to evaluate your patient. You can anticipate what to evaluate. Apply critical thinking attitudes and standards to determine whether outcomes of care are achieved (Fig. 20-1). If outcomes are met, the overall goals for the patient also are met. Compare patient behavior and responses that you assessed before delivering nursing interventions with behavior and responses that occur after administering nursing care. Critical thinking directs you to analyze the findings from evaluation (Fig. 20-2). Has the patient’s condition improved? Is the patient able to improve, or are there physical factors preventing recovery? To what degree does this patient’s motivation or willingness to pursue healthier behaviors influence responses to therapies?
During evaluation you make clinical decisions and continually redirect nursing care. For example, when Tonya evaluates the Jacobs’ learning, she applies knowledge of patient education principles and postoperative wound healing to interpret whether learning has occurred and whether further instruction is needed. Tonya knows that repetition is important in learning and thus plans another instruction session with the family during a dressing change the next day. Evaluative findings determine Tonya’s next course of action. In the Jacobs’ case Tonya knows that this is the first time Mr. Jacobs has had major surgery. Mrs. Jacobs voiced concern about recognizing the signs of infection. To meet the outcomes of care, Tonya plans to discuss the appearance of the wound during normal healing and specifically how signs of infection present. She reinforces this explanation during the dressing change so Mr. and Mrs. Jacobs can look at the wound closely again under Tonya’s instruction.
Positive evaluations occur when the patient meets desired outcomes, which leads you to conclude that the nursing intervention(s) were effective. For example, in the case study Tonya notes that Mrs. Jacobs identified three signs and symptoms of infection and Mr. Jacobs identified two. Therefore Tonya determines the expected outcome of “describing signs and symptoms of wound infection” was partially met by the patient. However, further instruction is necessary. Unmet or undesirable outcomes such as incorrect or incomplete knowledge indicate that interventions are not effective in minimizing or resolving the actual problem or avoiding an at-risk problem. An unmet outcome reveals that the patient has not responded to interventions as planned. As a result, the nurse changes the plan of care by trying different therapies or changing the frequency or approach of existing therapies.
This sequence of critically evaluating and revising therapies continues until you and the patient successfully and appropriately resolve the problems defined by nursing diagnoses. Remember that evaluation is dynamic and ever changing, depending on the patient’s nursing diagnoses and conditions. As problems change, so do expected outcomes. A patient whose health status continuously changes requires more frequent evaluation. In addition, you evaluate priority diagnoses first. For example, Tonya continues to evaluate Mr. Jacobs’ acute pain before evaluating the status of his deficient knowledge.
Standards for Evaluation
Nursing care helps patients resolve actual health problems, prevent the occurrence of potential problems, and maintain a healthy state. The evaluation process is an integral step to that end. The American Nurses Association (ANA) defines standards of professional nursing practice, which include standards for the evaluation step of the nursing process (see Chapter 1). The standards are authoritative statements of the duties that all registered nurses, regardless of role, patient population they serve, or specialty, are expected to perform competently (ANA, 2010). The competencies for evaluation include being systematic and using criterion-based evaluation, collaborating with patients and other professionals, using ongoing assessment data to revise the plan, and communicating results to patients and families. It is also important to ensure the responsible and appropriate use of interventions to minimize unwarranted or unwanted treatment (ANA, 2010).
Criterion-Based Evaluation
You evaluate nursing care by knowing what to look for as described in the criterion-based standards included in a patient’s goals and expected outcomes. The goals and outcomes are objective criteria needed to judge a patient’s response to care.
Goals
A goal is the expected behavior or response that indicates resolution of a nursing diagnosis or maintenance of a healthy state. It is a summary statement of what will be accomplished when the patient has met all expected outcomes. For Mr. Jacobs Tonya selected the goal of, “Patient expresses acceptance of health status by day of discharge” for the nursing diagnosis of anxiety (see Chapter 18). Successful achievement of this goal depends on Tonya delivering interventions selected from the Nursing Interventions Classification (NIC), including acceptance of health status and anxiety level (see Nursing Care Plan, Chapter 18).
Goals often are also based on standards of care or guidelines established for minimal safe practice. For example, the Infusion Nurses Society (INS) has standards of care for prevention of the intravenous (IV) complication phlebitis (INS, 2006). When a nurse cares for a patient with a peripheral IV line, the goal, “The IV site will remain free of phlebitis,” is established on the basis of sound practice standards. The INS phlebitis scale contains physical criteria for determining phlebitis (see Chapter 41).
Expected Outcomes
An expected outcome is an end result that is measurable, desirable, and observable and translates into observable patient behaviors (ANA, 2010). It is a measure that tells you if the interventions applied in patient care led to successful goal achievement. When nurses apply the nursing process, a nursing-sensitive outcome is a measurable patient or family state, behavior, or perception largely influenced by and sensitive to nursing interventions (Moorhead et al., 2008). The interventions must be within the scope of nursing practice and integral to the processes of nursing care. Examples of nursing-sensitive outcomes include reduction in pain frequency, incidence of pressure ulcers, and incidence of falls (Box 20-1). In comparison, medical outcomes are largely influenced by medical interventions. Examples include patient mortality, surgical wound infection, and hospital readmissions. Outcomes are statements of progressive, step-by-step physical, emotional, or behavioral responses that the patient needs to accomplish to achieve the goals of care. When you achieve outcomes, the related factors for a nursing diagnosis usually no longer exist. Two of the expected outcomes for Mr. Jacobs’ goal of, “Patient expresses acceptance of health status by day of discharge,” are “Patient describes surgical outcomes in discussion with surgeon in 24 hours,” and “Patient shares concerns with wife before day of discharge.” Tonya evaluates Mr. Jacobs by observing for behaviors that reflect anxiety and discussing what the patient has learned from the surgeon and discussed with his wife. The related factor of “uncertainty over recovery” no longer exists if Mr. Jacobs is able to relate surgical outcomes discussed with the surgeon and reports having had a discussion about those outcomes with his wife.
Evaluation is not a description of the achievement of an intervention. Evaluation of Mr. Jacobs does not involve observing his ability to perform relaxation exercises for his anxiety. Evaluation does involve observation of the patient’s behavior (facial expression) during discussions about his recovery.
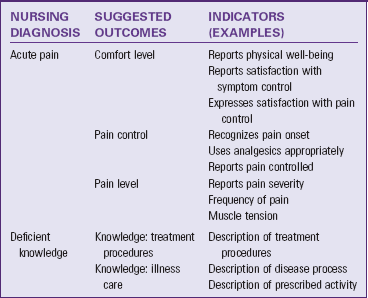
A valuable resource for selecting outcomes is the Nursing Outcomes Classification (NOC) (see Chapter 18). It offers a language for the evaluation step of the nursing process. The purposes of NOC are (1) to identify, label, validate, and classify nurse-sensitive patient outcomes; (2) to field test and validate the classification; and (3) to define and test measurement procedures for the outcomes and indicators using clinical data (Moorhead et al., 2008). Within the NOC taxonomy you can select outcomes specific for nursing interventions that relate to nursing diagnoses. The NOC project complements the work of NANDA International (NANDA-I) and the NIC project. The NOC classification offers nursing-sensitive outcomes for NANDA-I nursing diagnoses (Table 20-1). For each outcome there are specific recommended evaluation indicators (i.e., the patient behaviors or responses that are measures of outcome achievement).
Collaborate and Evaluate Effectiveness of Interventions
An important aspect of patient-centered care and evaluation is collaboration. A nurse must respect the patient and family as a core member of the health care team, meaning that the patient and family must be actively involved in the evaluation process. When you develop patient care goals and expected outcomes with a patient, he or she becomes an important resource for being able to tell you if outcomes are being met. For example, a patient knows best if pain has lessened or if breathing is easier. The same holds true for the family, who often can recognize changes in patient behavior sooner than you can because of their familiarity with the patient. Members of the health care team who contribute to the patient’s care also gather evaluative findings.
Proper evaluation determines the effectiveness of nursing interventions, allowing you to answer the following questions: What is the patient’s response to nursing care? Was the therapy effective in improving the patient’s physical or emotional health? It is important to evaluate whether each patient reaches a level of wellness or recovery that the health care team and patient established in the goals of care. In addition, have you met the patient’s expectations of care? Ask patients about their perceptions of care such as, “Did you receive the type of pain relief you expected?” “Did you receive enough information to change your dressing when you return?” This level of evaluation determines the patient’s satisfaction with care and strengthens partnering between you and the patient.
Evaluative Measures
Evaluating a patient’s response to nursing care requires the use of evaluative measures, which are assessment skills and techniques (e.g., observations, physiological measurements, patient interview) (Fig. 20-3). In fact, evaluative measures are the same as assessment measures, but you perform them at the point of care when you make decisions about the patient’s status and progress. The intent of assessment is to identify which, if any, problems exist. The intent of evaluation is to determine if the known problems have remained the same, improved, worsened, or otherwise changed.


FIG. 20-3 Evaluative measures. A, Nurse evaluates patient’s vital signs. B, Nurse evaluates patient’s lung sounds.
In many clinical situations it is important to collect evaluative measures over a period of time to determine if a pattern of improvement or change exists. A one-time observation of a pressure ulcer is insufficient to determine that the ulcer is healing. It is important to note a consistency in change. For example, over a period of 2 days is the pressure ulcer gradually decreasing in size, is the amount of drainage declining, and is the redness of inflammation resolving? Recognizing a pattern of improvement or deterioration allows you to reason and decide whether the patient’s problems (expressed in nursing diagnoses) are resolved. This is very important in the home care or nursing home setting. It may take weeks or even months to determine if interventions led to a pattern of improvement. For example, when evaluating a patient’s risk for falls over time, has the patient, family, or health care team successfully reduced fall risks in the home such as eliminating barriers in the home, removing factors impairing the person’s vision, or providing direction for proper use of assistive devices?
Interpreting and Summarizing Findings
A patient’s clinical condition often changes during an acute illness. In contrast, chronic illness results in slow, subtle changes. When you evaluate the effect of interventions, you interpret or learn to recognize relevant evidence about a patient’s condition, even evidence that sometimes does not match clinical expectations. By applying your clinical knowledge and experience, you recognize complications or adverse responses to illness and treatment in addition to expected outcomes.
Careful monitoring and early detection of problems are a patient’s first line of defense. Always make clinical judgments on your observations of what is occurring with a specific patient and not merely on what happens to patients in general. Frequently changes are not obvious. Evaluations are patient specific, based on a close familiarity with each patient’s behavior, physical status, and reaction to caregivers. Critical thinking skills promote accurate evaluation, which leads to the appropriate revision of ineffective care plans and discontinuation of therapy that has successfully resolved a problem.
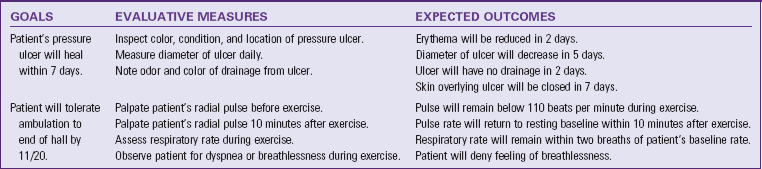
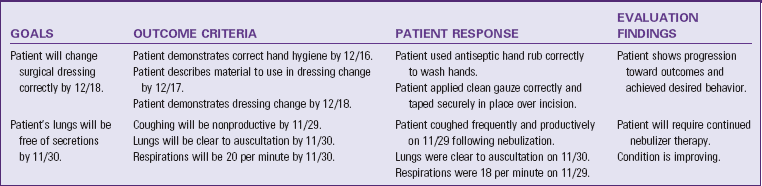
Using evidence, you make judgments about a patient’s condition. To develop clinical judgment you match the results of evaluative measures with expected outcomes to determine whether or not a patient’s status is improving. When interpreting findings, you compare the patient’s behavioral responses and the physiological signs and symptoms you expect to see with those actually seen from your evaluation. Comparing expected and actual findings allows you to interpret and judge the patient’s condition and whether predicted changes have occurred (Table 20-2). To objectively evaluate the degree of success in achieving outcomes of care, perform the following steps:
1. Examine the outcome criteria to identify the exact desired patient behavior or response.
2. Evaluate the patient’s actual behavior or response.
3. Compare the established outcome criteria with the actual behavior or response.
4. Judge the degree of agreement between outcome criteria and the actual behavior or response.
5. If there is no agreement (or only partial agreement) between the outcome criteria and the actual behavior or response, what is/are the barrier(s)? Why did they not agree?
Evaluation is easier to perform after you care for a patient over a long period. You are then able to make subtle comparisons of patient responses and behaviors. When you have not cared for a patient over an extended time, evaluation improves by referring to previous experiences or asking colleagues who are familiar with the patient to confirm evaluation findings. The accuracy of any evaluation improves when you are familiar with the patient’s behavior and physiological status or have cared for more than one patient with a similar problem.
Remember to evaluate each expected outcome and its place in the sequence of care. If not, it is difficult to determine which outcome in the sequence was not met. Thus you cannot revise and redirect the plan of care at the most appropriate time. If the patient achieves the expected outcomes, you either continue the care plan to maintain a therapeutic status or discontinue interventions because the goal of care is met. If evaluation determines that the expected outcomes were not met or only partially met, you begin reassessment and revision of the care plan. If the patient’s behavior begins to show changes but does not yet meet criteria set, the goal is partially met. If there is no progress, the goal is not met (Table 20-3).
Document Results
Documentation and reporting are important parts of evaluation. Accurate information needs to be present in a patient’s medical record and shared during handoff communication so nurses and other health care team members know if a patient is progressing and to make ongoing clinical decisions. In settings in which the same nurse will not be providing care throughout a patient’s stay, it becomes very important to have consistent, thorough documentation of the patient’s progress towards expected outcomes. The use of nursing diagnostic language and the NIC and NOC is becoming more common in electronic medical records (Hendrix, 2009). The use of standardized nursing languages can improve the quality, consistency, and accuracy of what is documented by providing a broad base of nursing knowledge at the point of care (Lunney, 2006). In addition, electronic systems provide linkages to make it easier to interpret cues regarding whether interventions led to expected patient outcomes. When documenting a patient’s response to your interventions, describe the interventions, the evaluative measures used, the outcomes achieved, and the continued plan of care. For example:
1430: Instructed patient on importance of handwashing and need to change surgical dressing if it becomes soiled, moist, or loosened. Asked patient to describe when it is necessary to change a surgical dressing. Patient was able to identify a soiled or moist dressing. Discussed further the need for a dressing to be secure. Provided pamphlet with outline of dressing change principles. Will discuss wound care with patient and wife one more time before discharge.
Your aim in documenting is to present a clear argument from the evaluative data as to whether a patient is progressing or not.
Disseminate results to patients and families. One of the ANA standards for evaluation is to share results of care with patients and their families according to federal and state regulations (ANA, 2010). Keep patients and families informed about the patients’ progress. Be aware of guidelines of your agency for the type of clinical information (e.g., diagnostic findings, results of treatment) that you can communicate.
Care Plan Revision
Each time you evaluate a patient you determine if the plan of care continues or whether revisions are necessary. If your patient meets a goal successfully, discontinue that portion of the care plan. Unmet and partially met goals require you to continue intervention. It may be appropriate to modify or add nursing diagnoses for a new plan of care with appropriate goals, expected outcomes, and interventions. You must also redefine priorities. An important step in critical thinking is knowing how the patient is progressing and how problems either resolve or worsen.
Tonya’s evaluation of Mr. Jacobs’ interventions for deficient knowledge revealed the following: The patient and wife are able to identify signs and symptoms of wound infection, and the patient knows that strain on the suture line can affect healing. Tonya sees that the outcomes of care are partially met. She still hopes to evaluate Mr. and Mrs. Jacobs’ ability to continue wound care at home through a demonstration planned for tomorrow. However, she also recognizes that, although Mr. Jacobs knows that strain on his incision can pull out the stitches, he may not realize which activities that he normally does at home would strain it. Thus she decides to modify her instructional approach by reassessing the types of activities Mr. Jacobs does at home (e.g., type of lifting, exercise, manual work) and incorporate that information into her teaching strategies.
Discontinuing a Care Plan
After you determine that expected outcomes and goals have been met, confirm this evaluation with the patient when possible. If you and the patient agree, you discontinue that portion of the care plan. Documentation of a discontinued plan ensures that other nurses will not unnecessarily continue interventions for that portion of the plan of care. Continuity of care assumes that care provided to patients is relevant and timely. You waste much time when you do not communicate achieved goals.
Modifying a Care Plan
When goals are not met, you identify the factors that interfere with their achievement. Usually a change in the patient’s condition, needs, or abilities makes alteration of the care plan necessary. For example, when teaching self-administration of insulin, a nurse discovers that the patient has developed a new problem, a tremor associated with a side effect of a medication. The patient is unable to draw medication from a syringe or inject the needle safely. As a result, the original outcomes, “Patient will correctly prepare insulin in a syringe,” and “Patient will administer insulin injection independently,” cannot be met. The nurse introduces new interventions (instructing a family member in insulin preparation and administration) and revises outcomes, “Family caregiver will correctly prepare insulin in syringe,” and “Family caregiver will administer insulin injection correctly,” to meet the goal of care.
At times a lack of goal achievement results from an error in nursing judgment or failure to follow each step of the nursing process. Patients often have multiple and complex problems. Always remember the possibility of overlooking or misjudging something. When a goal is not met, no matter what the reason, repeat the entire nursing process sequence for that nursing diagnosis to identify necessary changes to the plan. Reassess the patient, determine accuracy of the nursing diagnosis, establish new goals and expected outcomes, and select new interventions.
Reassessment: A complete reassessment of all patient factors relating to the nursing diagnosis and etiology is necessary when modifying a plan. Reassessment requires critical thinking as you compare new data about the patient’s condition with previously assessed information. Knowledge from previous experiences helps you direct the reassessment process. Caring for patients and families who have had similar health problems gives you a strong background of knowledge to use for anticipating patient needs and knowing what to assess. Reassessment ensures that the database is accurate and current. It also reveals a missing link (i.e., a critical piece of new information that was overlooked and thus interfered with goal achievement). You sort, validate, and cluster all new data to analyze and interpret differences from the original database. You also document reassessment data to alert other nursing staff to the patient’s status.
Redefining Diagnoses: After reassessment, determine which nursing diagnoses are accurate for the situation. Ask whether you selected the correct diagnosis and whether the diagnosis and the etiological factor are current. Then revise the problem list to reflect the patient’s changed status. Sometimes you make a new diagnosis. You base your nursing care on an accurate list of nursing diagnoses. Accuracy is more important than the number of diagnoses selected. As the patient’s condition changes, the diagnoses also change.
Goals and Expected Outcomes: When revising a care plan, review the goals and expected outcomes for necessary changes. In addition, examine the goals for unchanged nursing diagnoses for their appropriateness because a change in one problem sometimes affects the goals in others. Determining that each goal and expected outcome is realistic for the problem, etiology, and time frame is particularly important. Unrealistic expected outcomes and time frames make goal achievement difficult.
Clearly document goals and expected outcomes for new or revised nursing diagnoses so all team members are aware of the revised care plan. When the goal is still appropriate but has not yet been met, try changing the evaluation data to allow more time. You may also decide at this time to change interventions. For example, when a patient’s pressure ulcer does not show signs of healing, you choose to use a different support surface or a different type of wound cleanser.
Interventions: The evaluation of interventions examines two factors: the appropriateness of the intervention selected and the correct application of the intervention. Appropriateness is based on the standard of care for a patient’s health problem. A standard of care is the minimum level of care accepted to ensure high quality of care to patients. Standards of care define the types of therapies typically administered to patients with defined problems or needs. For example, if a patient who is receiving chemotherapy for leukemia has the nursing diagnosis nausea related to pharyngeal irritation, the standard of care established by the nursing department for this problem might include pain-control measures, mouth care guidelines, and diet therapy. The nurse reviews the standard of care to determine whether the right interventions have been chosen or whether additional ones are required.
Increasing or decreasing the frequency of interventions is another approach to ensure appropriate application of an intervention. You adjust interventions on the basis of the patient’s actual response to therapy and your previous experience with similar patients. For example, if a patient continues to have congested lung sounds, you increase the frequency of coughing and deep-breathing exercises to remove secretions.
During evaluation you find that some planned interventions are designed for an inappropriate level of nursing care. If you need to change the level of care, substitute a different action verb, such as assist in place of provide or demonstrate in place of instruct. For example, assisting a patient to walk requires a nurse to be at the patient’s side during ambulation, whereas providing an assistive device (e.g., a cane or walker) suggests that the patient is more independent. In addition, demonstration requires you to show a patient how a skill is performed rather than simply telling the patient how to perform it. Sometimes the level of care is appropriate, but the interventions are unsuitable because of a change in the expected outcome. In this case discontinue the interventions and plan new ones.
Make any changes in the plan of care based on the nature of the patient’s unfavorable response. Consulting with other nurses often yields suggestions for improving the care delivery approach. Experienced nurses are often excellent resources. Simply changing the care plan is not enough. Implement the new plan and reevaluate the patient’s response to the nursing actions. Evaluation is continuous.
Occasionally during evaluation you discover unmet patient needs. This is normal. The nursing process is a systematic, problem-solving approach to individualized patient care, but there are many factors affecting each patient with health care problems. Patients with the same health care problem are not treated the same way. As a result, you sometimes make errors in judgment. The systematic use of evaluation provides a way for you to catch these errors. By consistently incorporating evaluation into practice you minimize errors and ensure that the patient’s plan of care is appropriate and relevant. The evaluation of nursing care is a professional responsibility, and it is a crucial component of nursing care.
Key Points
• Evaluation is a step of the nursing process that includes two components: an examination of a condition or situation and a judgment as to whether change has occurred.
• During evaluation apply critical thinking to make clinical decisions and redirect nursing care to best meet patient needs.
• Positive evaluations occur when you meet desired outcomes and they lead you to conclude that your interventions were effective.
• Criterion-based standards for evaluation are the physiological, emotional, and behavioral responses that are a patient’s goals and expected outcomes.
• Evaluative measures are assessment skills or techniques that you use to collect data for determining if outcomes were met.
• It sometimes becomes necessary to collect evaluative measures over time to determine if a pattern of change exists.
• When interpreting findings, you compare the patient’s behavioral responses and physiological signs and symptoms that you expect to see with those actually seen from your evaluation and judge the degree of agreement.
• Documentation of evaluative findings allows all members of the health care team to know whether or not a patient is progressing.
• A patient’s nursing diagnoses, priorities, and interventions sometimes change as a result of evaluation.
• Evaluation examines two factors: the appropriateness of the interventions selected and the correct application of the intervention.
Clinical Application Questions
Preparing for Clinical Practice
Tonya examines Mr. Jacobs’ surgical incision and notices a 1.25-cm (0.5-inch) circle of yellowish drainage on the gauze dressing. On close inspection of the suture line, she also observes an area of swelling around two stitches. Mr. Jacobs notices Tonya’s expression as she looks at the dressing and asks, “Is anything wrong?” Tonya responds, “A small amount of drainage is coming from your incision. Don’t be alarmed.” As Tonya applies mild pressure over the incision, she asks Mr. Jacobs if the area is tender. He grimaces a bit and says, “Yes, a little.” Tonya says, “I’m going to let your surgeon know about this.” After she consults with the physician, an intravenous (IV) antibiotic is ordered. While in Mr. Jacobs’ room, Tonya notices that the patient is breathing faster and looks up to the ceiling and sighs.
1. When Tonya evaluated the surgical incision, two components of evaluation occurred. Describe each.
2. Based on this clinical scenario, how might Tonya need to modify the patient’s care plan? Refer to the concept map (Fig. 19-2) on p. 257 in Chapter 19.
3. Identify two evaluative measures that Tonya used to evaluate the condition of Mr. Jacobs’ wound.
![]() Answers to Clinical Application Questions can be found on the Evolve website.
Answers to Clinical Application Questions can be found on the Evolve website.
Are You Ready to Test Your Nursing Knowledge?
1. A nurse caring for a patient with pneumonia sits the patient up in bed and suctions his airway. After suctioning, the patient describes some discomfort in his abdomen. The nurse auscultates the patient’s lung sounds and gives him a glass of water. Which of the following is an evaluative measure used by the nurse?
2. A nurse caring for a patient with pneumonia sits the patient up in bed and suctions the patient’s airway. After suctioning, the patient describes some discomfort in his abdomen. The nurse auscultates the patient’s lung sounds and gives him a glass of water. Which of the following would be appropriate evaluative criteria used by the nurse? (Select all that apply.)
1. Patient drinks contents of water glass.
2. Patient’s lungs are clear to auscultation in bases.
3. Patient reports abdominal pain on scale of 0 to 10.
4. Patient’s rate and depth of breathing are normal with head of bed elevated.
3. The evaluation process includes interpretation of findings as one of its five elements. Which of the following is an example of interpretation?
1. Evaluating the patient’s response to selected nursing interventions
2. Selecting an observable or measurable state or behavior that reflects goal achievement
3. Reviewing the patient’s nursing diagnoses and establishing goals and outcome statements
4. Matching the results of evaluative measures with expected outcomes to determine patient’s status
4. A goal specifies the expected behavior or response that indicates:
1. The specific nursing action was completed.
2. The validation of the nurse’s physical assessment.
3. The nurse has made the correct nursing diagnoses.
4. Resolution of a nursing diagnosis or maintenance of a healthy state.
5. A patient is recovering from surgery for removal of an ovarian tumor. It is 1 day after her surgery. Because she has an abdominal incision and dressing and a history of diabetes, the nurse has selected a nursing diagnosis of risk for infection. Which of the following is an appropriate goal statement for the diagnosis?
1. Patient will remain afebrile to discharge.
2. Patient’s wound will remain free of infection by discharge.
3. Patient will receive ordered antibiotic on time over next 3 days.
4. Patient’s abdominal incision will be covered with a sterile dressing for 2 days.
6. Unmet and partially met goals require the nurse to do which of the following? (Select all that apply.)
4. Gather assessment data on a different nursing diagnosis
5. Compare the patient’s response with that of another patient
7. A patient comes to a medical clinic with the diagnosis of asthma. The nurse practitioner decides that the patient’s obesity adds to the difficulty of breathing; the patient is 5 feet 7 inches tall and weighs 200 pounds (90.7 kg). Based on the nursing diagnosis of imbalanced nutrition: more than body requirements, the practitioner plans to place the patient on a therapeutic diet. Which of the following are evaluative measures for determining if the patient achieves the goal of a desired weight loss? (Select all that apply.)
1. The patient eats 2000 calories a day.
2. The patient is weighed during each clinic visit.
3. The patient discusses factors that increase the risk of an asthma attack.
4. The patient’s food diary that tracks intake of daily meals is reviewed.
8. The nurse follows a series of steps to objectively evaluate the degree of success in achieving outcomes of care. Place the steps in the correct order.
1. The nurse judges the extent to which the condition of the skin matches the outcome criteria.
2. The nurse tries to determine why the outcome criteria and actual condition of skin do not agree.
3. The nurse inspects the condition of the skin.
4. The nurse reviews the outcome criteria to identify the desired skin condition.
5. The nurse compares the degree of agreement between desired and actual condition of the skin.
9. The nurse checks the intravenous (IV) solution that is infusing into the patient’s left arm. The IV solution of 9% NS is infusing at 100 mL/hr as ordered. The nurse reviews the nurses’ notes from the previous shift to determine if the dressing over the site was changed as scheduled per standard of care. While in the room, the nurse inspects the condition of the dressing and notes the date on the dressing label. In what ways did the nurse evaluate the IV intervention? (Select all that apply.)
1. Checked the IV infusion location in left arm
2. Checked the type of IV solution
3. Confirmed from nurses’ notes the time of dressing change and checked label
10. Which of the following statements correctly describe the evaluation process? (Select all that apply.)
1. Evaluation is an ongoing process.
2. Evaluation usually reveals obvious changes in patients.
11. A clinic nurse assesses a patient who reports a loss of appetite and a 15-pound weight loss since 2 months ago. The patient is 5 feet 10 inches tall and weighs 135 pounds (61.2 kg). She shows signs of depression and does not have a good understanding of foods to eat for proper nutrition. The nurse makes the nursing diagnosis of imbalanced nutrition: less than body requirements related to reduced intake of food. For the goal of, “Patient will return to baseline weight in 3 months,” which of the following outcomes would be appropriate? (Select all that apply.)
1. Patient will discuss source of depression by next clinic visit.
2. Patient will achieve a calorie intake of 2400 daily in 2 weeks.
12. A patient is being discharged after abdominal surgery. The abdominal incision is healing well with no signs of redness or irritation. Following instruction, the patient has demonstrated effective care of the incision, including cleansing the wound and applying dressings correctly to the nurse. These behaviors are an example of:
13. A patient has limited mobility as a result of a recent knee replacement. The nurse identifies that he has altered balance and assists him in ambulation. The patient uses a walker presently as part of his therapy. The nurse notes how far the patient is able to walk and then assists him back to his room. Which of the following is an evaluative measure?
1. Uses walker during ambulation
2. Presence of altered balance
14. A patient is being discharged today. In preparation the nurse removes the intravenous (IV) line from the right arm and documents that the site was “clean and dry with no signs of redness or tenderness.” On discharge the nurse reviews the care plan for goals met. Which of the following goals can be evaluated with what you know about this patient?
1. Patient expresses acceptance of health status by day of discharge.
2. Patient’s surgical wound will remain free of infection.
3. Patient’s IV site will remain free of phlebitis.
4. Patient understands when to call physician to report possible complications.
15. A nursing student is talking with one of the staff nurses who works on a surgical unit. The student’s care plan is to include nursing-sensitive outcomes for the nursing diagnosis of acute pain. A nursing-sensitive outcome suitable for this diagnosis would be:
Answers: 1. 3; 2. 2, 4; 3. 4; 4. 4; 5. 2; 6. 1, 2; 7. 2, 4; 8. 4, 3, 5, 1, 2; 9. 3, 4; 10. 1, 3, 4; 11. 2, 3; 12. 2; 13. 4; 14. 3; 15. 3.
References
American Nurses Association. Scope and standards of practice: nursing, ed 2. Silver Spring Md: American Nurses Association; 2010.
Brown, DS, et al. Nursing-sensitive benchmarks for hospitals to gauge high-reliability performance. J Healthc Qual. 2010;32(6):9.
Hendrix, SE. An experience with implementation of NIC and NOC in a clinical information system. CIN: Comput Inform Nurs. 2009;27(1):7.
Infusion Nurses Society (INS). 2006 Infusion nursing standards of practice. J Infus Nurs. 2006;29(suppl 1):S1.
Lunney, M. Helping nurses use NANDA, NOC, and NIC: novice to expert. Nurse Educator. 2006;31(1):40.
Moorhead, S, et al. Nursing outcomes classification (NOC), ed 4. St Louis: Mosby; 2008.