Psychosocial Issues Affecting Social Participation
1 Understand the dynamic interaction of emotional, cognitive, neurobehavioral, and environmental factors as they influence aspects of occupational performance through the course of typical development during infancy, childhood, and adolescence.
2 Explain means of promoting the psychosocial wellness of infants, children, and youth within natural contexts.
3 Identify the diagnostic hallmarks and contributing factors of common mental health conditions, and relate these to the occupational performance of children and adolescents.
4 Understand the continuum of services available to children and youth with psychosocial disorders.
5 Explain the variety of service delivery models and frames of reference used by occupational therapists in psychosocial settings.
6 Define the roles of occupational therapists who provide services to children and youth with psychosocial disorders, as well as those of other team members.
7 Understand evaluation and intervention processes related to the special needs of children and youth whose occupational performance has been affected by psychosocial problems.
The promotion of the child’s social participation within the contexts of family, friendships, classmates, caregivers, and teachers is an essential domain of occupational therapy in all practice settings.5,50,56,135,181 Achievement of developmental milestones and occupational goals is the result of continuously evolving interactions between aspects of the individual child and the environmental contexts that envelop him or her. Social relationships constitute a critical chunk of that environment; the mutual influences of the individual and his or her social contexts help determine the child’s quality of life and participation in those social contexts.
This chapter is organized as follows: It (1) describes dynamic aspects of healthy psychosocial development within the child and the family, (2) outlines common causes of psychosocial problems in children and adolescents and their implications for occupational performance, (3) describes the roles of occupational therapy practitioners and other team members within a variety of intervention settings, and (4) introduces selected evaluation and intervention methods, including intervention goals for common psychosocial needs.
The unifying frame of reference for this chapter is the person-environment-occupation (PEO) model.106 The PEO model emphasizes the dynamic interaction between the individual and various aspects of the environment and how these interactions influence occupational performance. “Person” factors include qualities of the individual such as gender, age, developmental levels, skills, preferences, and values. “Environment” factors encompass the social, cultural, economic, political, and physical contexts that the child functions within. Person and environment factors are viewed as reciprocally influential and as directly relevant to the child’s occupational performance. “Occupations” are the everyday tasks and activities that an individual performs, ranging from very basic actions, such as eating and using the toilet, to highly sophisticated activities, such as working a calculus problem, flirting with a classmate, or rollerblading. Appreciating and understanding the elements of the PEO model and their potential for dynamic interaction enable occupational therapists to approach intervention holistically and effectively.
TEMPERAMENT: A “PERSON” FACTOR THAT INFLUENCES AND IS INFLUENCED BY THE ENVIRONMENT
Children vary in their development of interests, habits, talents, and social competence. Standardized pediatric tests reveal variations among children in the rate and sequence of their acquisition of motor, language, and cognitive skills. Curiosity about these differences among children has inspired decades of research. Chess and Thomas were among the first scholars to study children’s styles of responding to various experiences and carrying out activities such as sleeping, eating, and exploring objects.158 Their work developed the concept of temperament. Temperament refers to a collection of inborn, relatively stable traits that influence how individuals process and respond to the environment and that contribute to the development of personality and everyday functioning.154 Chess and Thomas identified nine basic characteristics of temperament, which remain useful today. These are (1) activity level, (2) rhythmicity (i.e., the degree to which the child’s patterns of sleeping, eating, and play are predictable), (3) approach to or withdrawal from novel situations, (4) intensity of emotional responses, (5) sensory threshold, (6) mood (general emotional state), (7) adaptability, (8) distractibility, and (9) attention span and persistence.33 Temperament characteristics are not considered to be inherently good or bad, and they are not under the control of the child or the parents. However, behaviors arising from temperament traits may be more or less adaptive or pleasing, depending on the context. Children whose temperament style approaches extremes on any of the nine parameters may have more difficulty negotiating the social and emotional demands of childhood. The environmental demands and expectations must always be considered, however, when attempting to predict the effects of temperament on occupational performance. Research indicates that the assessment of each child’s temperament is influenced by the observer’s point of view and that the determination of function or dysfunction has much to do with the situational compatibility with the family and other social environments.171
Chess and Thomas were interested in learning about the influence of personality characteristics on the parent-child relationship and the child’s development.35 They applied the concept goodness of fit (from statistics) to interpersonal relationships. When the expectations of persons important to the child are compatible with the child’s temperament, there is a good fit (Case Study 13-1). When the child’s temperament is at odds with parental expectations, mutual distress may result. Although Chess and Thomas focused on parent-child fit, other research has supported the findings in teacher and peer relationships.90,91
Chess and Thomas (1983) identified three common patterns of temperament from the nine temperament traits described above. They gave these combinations the labels easy child, difficult child, and slow-to-warm-up child (Figure 13-1). The easy child is positive in mood and approach to new stimuli. This child is calm, expressive, malleable, and has a generally low to moderate activity level. Children characterized as easy tend to adapt effectively to changing situations and demands. The difficult child is at the opposite end of the temperament spectrum. Characteristics that characterize this style are a negative mood and approach, slow adaptability, a high activity level, and high emotional intensity. Extremes of sensory threshold often occur among children with a difficult temperament pattern. A slow-to-warm-up child demonstrates mild-intensity negative reactions to new stimuli in combination with slow adaptation. These children require repeated exposures to new environments before they feel comfortable. Once a slow-to-warm-up child has established a routine, he or she usually functions well, but transitions are often problematic for children of this temperament type. Research has linked various temperament characteristics to parental stress in child-rearing,34 certain psychiatric disorders in adulthood,87,129 adolescent substance abuse,179 and disruptive behavioral disorders.68 A growing body of research supports the notion that temperament, although inborn, is not unchanging across a child’s lifespan. Experiences and environmental circumstances such as the interpersonal styles of the primary caregivers have been assessed as having potentially significant influence on the developing child’s temperament style.17 These findings suggest that therapeutic intervention can be helpful in situations lacking goodness of fit between child and caregiver.
Occupational therapists often see children who are in distress and whose behavior is disruptive or upsetting to the family. Practitioners can help parents, caregivers, teachers, and children to explore and understand their temperaments and learn to predict when behavior may not match environmental demands (e.g., a very active child at the theater, a slow-to-warm-up child beginning a new school year). This perspective may decrease frustration and increase the possibility of organizing environments and activity demands to promote goodness of fit and successful occupational engagement.
ATTACHMENT: A DYNAMIC INTERACTION OF BIOLOGY AND ENVIRONMENT
A child’s neuromaturational progress greatly influences social participation. The healthy, full-term infant is biologically prepared to participate in interactions with a nurturing and consistent caregiver, resulting in a loving attachment that is essential for healthy development.11 As the infant nurses, cuddles, gazes with fascination at her mother’s face, and responds to comforting, emotions result that will become the foundation of the baby’s self-concept and a safe base from which to explore the world.159 Simultaneously, the mother experiences hormonal and neurochemical effects from interacting with her infant that promote feelings of well-being, protectiveness, and love for her baby.77 Healthy attachment occurs when the caregiver and infant consistently interrelate in such a way that the infant develops confidence that the needs will be met and that he is safe and cared for.16,116 Many experts contend that the quality of early attachment influences the capacity to form relationships later in life.55,73,178 Some researchers are studying the influence of early attachment experience on neurodevelopment itself at the biochemical and cellular levels.58,101,115 Thompson asserts that the quality of early relationships is “far more significant on early learning than are educational toys, preschool curricula, or Mozart CDs” (p. 11).159
Traits and behaviors of the parent and the child interact dynamically within environmental contexts to determine the quality of attachment that develops; each party is simultaneously influencing and influenced by the other and by other features of the environment.60 Researchers have identified four patterns of attachment behavior between parents and infants: secure, avoidant, resistant or ambivalent, and disorganized/disoriented.2,117 These are illustrated in Table 13-1.
TABLE 13-1
Patterns of Attachment in Infants and Parents
| Attachment Style | Characteristic Caregiver Behavior | Characteristic Infant Behavior |
| Secure | Emotionally available, responsive to infant’s emotional and physical needs in a timely, consistent, and effective manner | Seeks proximity to parent, but as mobility develops explores the immediate environment; demonstrates mastery motivation and self-confidence; misses parent on separation, but easily comforted on parent’s return |
| Avoidant | Emotionally unavailable, typically not adequately responsive to infant’s communications of need | Avoids parent; emotionally blunted; interacts with objects in the environment rather than with the parent |
| Resistant or ambivalent | Inconsistently available and responsive to infant’s communications of need; caregiving style is determined by parent’s moods and is an unpredictable combination of adequate and inadequate responses | Is clingy and preoccupied with the parent; does not actively explore the environment; is difficult to comfort after separation; mood may be angry or passive |
| Disorganized/disoriented | Highly anxious or threatening toward the child; does not respond effectively or appropriately to infant’s communications; may be abusive or psychotic | Is disorganized or disoriented when interacting with the parent; displays approach-avoidance behaviors including staring and “freezing,” clinging, or huddling on the floor |
Parent-child attachment relationships continuously change in relation to the child’s and the parent’s stages of development and changing environmental circumstances.144 As the infant becomes mobile and then develops language and self-care skills, the caregiving style of the parent adjusts accordingly, and the attachment relationship is altered. Attachment patterns may also be influenced by environmental factors such as the loss or addition of family members. Adjustments in attachment continue throughout the child’s developmental course, and in the best circumstances the positive reciprocity initiated early in infancy will be maintained throughout.
Understanding that patterns of attachment between children and their parents can change implies that attachment is a process that can be influenced.11 This notion is supported by research with high-risk infants and mothers who received intervention to promote healthy attachment through three home visits focused on teaching mothers how to observe and respond effectively to their infants’ behaviors.168 The group of 50 receiving the training developed significantly more secure attachments than did those in the control group. These effects from interventions to promote attachment have been found in other studies as well.40,169
Many infants, children, and adolescents served by occupational therapists have neurodevelopmental problems. Children who have intrinsic difficulty with receptive and/or expressive communication, sensory processing, or motor performance have a different social experience than do those who are developing typically.142 Difficulty with feeding, an inability to establish regular patterns of activity and sleep throughout the day and night, resistance to cuddling, and other behaviors common to infants with neurologic dysfunction are incompatible with easy attachment, and may place the process at risk. Environmental factors such as a parent’s long hours of work can limit the time available for child-focused interaction, potentially interfering with the attachment process. Likewise, a parent whose behavior is anxious, irritable, emotionally disengaged, or who has difficulty interpreting and responding to the child’s communications cannot fully participate in reciprocal interaction. When such behaviors are frequent, attachment is at risk. Occupational therapists can support healthy interaction between caregivers and children by understanding this essential process, educating parents about their child’s development and communication style, and helping them to generate solutions for problems that inhibit strong attachment formation. They can help families identify causes of stress in their daily and weekly routines and structure solutions to address them. These could involve prioritizing goals, working together to get tasks completed more efficiently, and making mindful choices about how to use time to improve quality of life and family relationships.
CHILD ABUSE AND NEGLECT: PROBLEMS WITH THE PARENT-CHILD RELATIONSHIP AND ENVIRONMENT
At its most extreme, inadequate attachment formation between a parent and a child can be a factor in the abuse or neglect of the child. This is a common problem for children and families, affecting at least 905,000 American children in 2006.166 Nearly 8% of the victims of child abuse or neglect had diagnosed disabilities. The Federal Child Abuse Prevention and Treatment Act (CAPTA), (42 U.S.C.A. §5106g), as amended by the Keeping Children and Families Safe Act of 2003, defines child abuse and neglect as follows:
• Any recent act or failure to act on the part of a parent or caretaker which results in death, serious physical or emotional harm, sexual abuse or exploitation; or
• An act or failure to act which presents an imminent risk of serious harm.
Child abuse has been categorized as neglect, physical abuse, sexual abuse, medical neglect, or “other” maltreatment; the various forms of child abuse may occur in combination.
• Neglect is defined as the withholding of nutrition, shelter, clothing, medical care, such that the child’s health is endangered. Undersupervision and abandonment are included in this category. This is the most common form of child abuse, accounting for about 64% of reported cases.
• Physical abuse affects about 16% of victims. This type of abuse includes punching, shaking, kicking, biting, throwing, burning, and other forms of injurious punishment.
• Sexual abuse is estimated to occur at a rate of about 9% and includes any seduction, coercion, or forcing of a child to observe or participate in sexual activity for the sexual gratification of a more powerful individual.
• Medical neglect is a failure by the caregiver to provide for the appropriate health care of the child although financially able to do so, or offered financial or other means to do so. This kind of maltreatment affects 2% of the reported cases.
• “Other” types of maltreatment constitute 15% of the reported cases. These include emotional abuse, such as the withholding of affection, chronic humiliation, threatening harm to the child or those he or she cares about, and criticism. Abandonment and congenital drug addiction also fall under this reporting category.166
Developmental and psychological outcomes that have been associated with childhood abuse include traumatic brain injury, depression, substance abuse, posttraumatic stress disorder, learning disorders, conduct disorders, and personality disorders.9,22,53,78,83,85,103 These problems can have long-term occupational consequences, including the increased risk of involvement in violent and nonviolent crime and of not completing high school.104 Most tragically, approximately 1530 children died from the effects of abuse or neglect in 2006.166 Clearly, such pathology is incompatible with healthy family functioning.
Attachment patterns between parents and children are the result of a dynamic interaction of factors related to the child, the parent, and the environment. Risk factors for child abuse and neglect have been identified in these three arenas (Table 13-2). No single factor is consistently associated with child abuse. The more risk factors present and the more severe each of these is, the higher the risk of abuse and neglect within a family.
A child’s level of risk decreases with age, with infants suffering the highest rate of abuse.166 Disability increases the risk of child maltreatment. The incidence of abuse and neglect may be as high as 3.4 times greater for children with disabilities than for those without.157 Disabilities that have been associated with an increased risk of maltreatment include behavioral disorders, communication disorders, cognitive disabilities, physical impairments, and craniofacial anomalies.46,84,157,173,176 Any condition that prolongs a child’s dependency or stimulates parental rejection adds to the risk of abuse or neglect. For example, having a “difficult” temperament or being born prematurely increases risk.59,153 Most of the young clients seen by occupational therapy practitioners have delayed development in one or more areas and are, as a group, at increased risk for abuse and neglect.
Environmental factors interact dynamically with features of the child to affect the levels of risk for abuse and neglect. Certain qualities of the parents (particularly the mother, who is usually the primary caretaker) have been identified as risk factors. These include having a personality that is characterized by immaturity, a history of having been abused, egocentrism, impulsivity, and alcohol or drug abuse.131,149,184 Characteristics of the larger community may further contribute to environmental risk factors. Poverty has been shown to correlate positively with increased rates of child abuse and neglect.44,150 Social isolation is a powerful risk factor, placing children in single-parent families at significantly higher risk for abuse than those in two-parent families.82 Communities with high crime rates present a combination of a cultural acceptance of aggressive behavior, high levels of economic distress, and the social isolation that results when residents are fearful to step out onto the street.
Although poverty and a parent’s troubled background may increase the likelihood of child abuse, high levels of social integration and community morale appear to be mediating factors that can reduce its incidence.61 Successful intervention and prevention programs address family and community needs for safe and enjoyable places to gather and engage in meaningful occupation.174 A meta-analysis of abuse prevention and family wellness programs indicated that the most effective programs supported parents by using a strengths-based, empowerment approach. Successful programs continued over 6 months and provided at least two sessions per month.113 Occupational therapists have opportunities to intervene with individuals and families through direct service, program development, consultation, and administrative roles.
Children who are experiencing physical abuse and/or neglect may bear outward signs of this, and therapists should always observe for bruises, cuts, or other injuries, or behaviors that may reflect pain. The appropriateness of the child’s clothing for weather conditions and fit should be noted over time. This is not to assess fashionableness but adequacy. The occupational therapist asks the child about his or her eating and sleeping habits and activities through the day when at home, asks about how the adults at home respond to children’s misbehavior (e.g., “What kinds of things do you do that get you in trouble sometimes?” “What happens then?”) Given gentle encouragement, some children will describe inadequate or unsafe situations. School-based personnel should observe what the child has brought for lunch or how the child responds to food that is offered; a child with too little to eat at home may hoard food or eat more than is typical. Socially, children from abusive homes may behave in a variety of ways that reflect individual temperaments and coping styles. Behaviors may range from being withdrawn and guarded to acting intrusive and demanding. Often children who have been abused are themselves aggressive, but this is not universal.97 Many abused children are socially immature and emotionally needy. The description of resistant/ambivalent and disorganized/disoriented attachment styles also fits many of these children.
Occupational therapy practitioners are mandated by federal law to report suspected cases of abuse and neglect to state child protective services agencies.36 Reports of suspected child abuse or neglect may be made by telephone and should be followed with a letter documenting the child’s demographic information, specific observations leading to the report, and the practitioner’s contact information. Referrals to child protective services are held in confidence, and persons who submit referrals in good faith are protected by law from prosecution. Statutes and information about reporting abuse or neglect for each state are available on the child welfare policy website (http://www.childwelfare.gov/systemwide/laws_policies/state/). Discovery of a practitioner’s failure to report suspected cases of abuse or neglect may result in prosecution and/or disciplinary action by the practitioner’s licensing board or in the civil courts.
Referrals to child protective services are reviewed and classified according to the situational risk. Families who are evaluated often receive a variety of intervention services, including respite care, parenting education, assistance with housing, day care, home visits, individual and family counseling, substance abuse treatment, and transportation. Fewer than 20% of the children whose families are investigated for abuse and neglect are taken into protective foster care.166
ENVIRONMENTAL FACTORS AND SOCIAL PARTICIPATION
Social participation can only be fully experienced when children and families live within supportive environments that provide opportunities for self-expression and connection with others. When these conditions are unmet, even for a limited time, occupational performance suffers. When conditions are less than adequate for prolonged periods, the child’s very course of development may be altered, with lifelong effects. Assessing the nature of a child’s environment is a critical stage of clinical reasoning when trying to determine the psychosocial contributors to occupational dysfunction.
Environmental factors that relate to psychosocial performance may be roughly divided into those that are relatively brief and those that are more long-term (Box 13-1). Time-limited events include personal and family stressors that are keenly experienced and then resolved over a period of weeks or months. Long-term events or situations are those in which the stressors are pervasive and continue for months or years. These categories are further described in the next sections. Although they are useful for general conceptual purposes, they should be applied with caution. Whether an event or circumstance falls into one category or another is partially dependent on the coping style and circumstances of the individual affected. For example, the death of a grandparent may be an event that a child feels acutely sad about for several weeks and then adjusts to, especially if the relationship was limited by distance or other factors. For a child who is very sensitive, or for whom the grandparent was a primary caregiver, such a loss could result in months of grief. If the child did not know the grandparent at all, the loss may be irrelevant.
Time-Limited Environmental Stress and Its Impact on Occupational Performance
Short-acting environmental conditions such as the death of an extended family member or friend, temporary marital crises, a change of school or day care, or a family relocation, can have significant effects on the child’s social participation. A survey of 56 school-based occupational therapists indicated that many of the students with whom they worked experienced such loss and grief in their lives and that their behavior reflected this.123 Children’s reactions to such events often include decreased performance in play or academic activities. The child may act preoccupied, fatigued, or uninterested in usual pastimes. Sometimes children temporarily “lose” their skills in self-care and revert to more dependent, infantile ways.182 They may become emotionally overreactive and engage in provocative behavior such as fighting or disobeying adults’ directives.125 Occupational therapists can help children and adolescents to cope with times of increased stress through establishing a therapeutic relationship, asking about how the child is feeling and the events that are occurring in their lives, providing opportunities for self-expression through activities, and communicating with the rest of the team to ensure the best possible communication and support throughout the child’s day. Educating the child, family, and others who are in contact with the child regarding typical grief reactions and ways to respond to these can also facilitate the child’s passage through difficult experiences (Case Study 13-2).
Chronic Environmental Stress and Its Impact on Occupational Performance
Long-term sources of social stress are circumstances and events that do not resolve over the course of weeks or months (see Box 13-1). Examples of these are poverty, social discrimination, and severe family dysfunction that may occur when one or both parents suffer from substance abuse or other mental disorders. These kinds of environmental conditions may have long-term effects on children’s development and social participation through the lifespan, especially if combined with other complications such as the child’s own neurodevelopmental problems.
More than 17% of children in the United States live in poverty. Of the children aged 18 and younger living in poverty, approximately 24% are black, 21% are Hispanic, 10% are white, and 10% are Asian.164 Long-term poverty has been associated with a number of serious problems for children and adolescents and for the adults who care for them.32,42 Having a low income and living in a crime-ridden environment have been shown to correlate with increased risk of having newborns born prematurely or with low birth weight, both of which increase the risk for subsequent developmental and health problems.120
The home environments of families with few resources may offer limited access to items that are considered to be “necessities” by a majority of members of the culture, such as books, toys, a telephone, television, or computer. The language opportunities in low-income homes are often different and reduced when compared with those found in middle-class homes (Case Study 13-3).108 Due to a combination of health and environmental factors, children who live in chronic economic deprivation are at increased risk for having lower cognitive abilities and more behavioral problems.18,42 Parents who experience the stress of chronically worrying about meeting basic needs for food, shelter, and safety are more prone to discipline their children harshly, have marital conflicts, experience depression, and have substance abuse problems.15,42,86,121 They may be too overwhelmed, discouraged, or disorganized to become involved in their children’s schooling. These conditions place many low-income students at a disadvantage and diminish their future opportunities. Some children who have experienced lifetimes of severe family and community dysfunction reach adolescence feeling hopeless about their futures. Their occupational performance is clearly affected by this as they struggle with society’s expectations to further their education in order to prepare for a productive adulthood, while from the discouraged adolescent’s perspective this is impossible to achieve.
Case Study 13-3 illustrates how poverty and other chronic stress factors can affect a child’s occupational performance, both in terms of the preparation for and availability of opportunities to achieve social participation. Although environmental factors are clearly influential in determining a child’s occupational performance, the PEO model reflects a balance of emphasis among its three components.106 Each individual has capacities and desires that strongly influence occupational expression. The following section provides information regarding the role that mental functioning plays in the enactment and development of children’s occupational performance.
MENTAL HEALTH FACTORS AFFECTING SOCIAL PARTICIPATION
Children’s developmental progress and occupational performance depend as much on how well their psychosocial needs are being met as they do on the adequacy of the nutrition and shelter they receive. In 1999, Dr. David Satcher, Surgeon General of the United States Public Health Service, supervised the publication of the results of a multiagency effort sharing the expertise of hundreds of service providers, researchers, and consumers. The Surgeon General’s Report on Mental Health states: “From early childhood until death, mental health is the springboard of thinking and communication skills, learning, emotional growth, resilience, and self-esteem. These are the ingredients of each individual’s successful contribution to community and society” (Chapter 1, Introduction & Themes).167
A fixed definition of mental health is difficult to formulate; behaviors and beliefs that are construed as “healthy” by one individual in a particular context may be considered to be inappropriate or unhealthy by someone else or in another context. The Surgeon General’s definition of mental health suggests cultural variables influence what behaviors are expected and, therefore, how mental health is defined: “Mental health is a state of successful performance of mental function, resulting in productive activities, fulfilling relationships with other people, and the ability to adapt to change and to cope with adversity. Mental health is indispensable to personal well-being, family and interpersonal relationships, and contribution to community or society.”167 For example, American parents of Northern European descent often value independence and achievement. Such parents might be concerned about the behavior of their five-year-old son, who wants his mother to help him with dressing and bathing, even though he can do these things for himself. This behavior might cause them to wonder if their child is immature or “spoiled.” Parents from a cultural background that promotes a climate of interdependence, such as that found in Japan, might expect such behavior and find it quite acceptable. It is clear that practitioners must be competent in assuming a multicultural approach in order to effectively evaluate social and emotional behavior.
Children and adolescents’ ability to participate socially and academically may be severely impaired by poor mental health. It is estimated that nearly 13% of children have mental or emotional problems, and 32.8% have mental and emotional problems along with other types of functional disorders.82 It is thought that increasing numbers of children are being diagnosed with mental disorders as a result of combination of increasingly sensitive diagnostics and contributing social pressures and problems.37,71,140,184 Effective interventions for these types of conditions typically require a combination of family education, special services at school, various therapies for the child and family, and, often, medication.
Occupational therapists approach their work with a client-centered, occupational performance—rather than a medical or pathology-focused—perspective.26,106 However, client-centered approaches do not preclude understanding the nature and course of a client’s illness or disability. To develop and implement client-centered, contextually appropriate intervention, the child’s symptoms, medication effects and side effects, and prognosis must be understood. Additionally, practitioners who recognize the diagnostic hallmarks of mental disorders that occur in childhood and adolescence can play an important role in referring children and adolescents in need of a diagnostic evaluation to specialists such as psychologists or psychiatrists. In many settings the occupational therapist may be the only team member who understands the symptoms and various interventions for mental disorders and their implications for occupational performance in school, child care, and at home. The following section presents an overview of selected mental disorders that can affect children and their implications for occupational performance. It is not unusual for individuals to experience multiple disorders simultaneously, such as depression and anxiety, Asperger’s syndrome and depression, or cognitive impairment and attention deficit disorder.6 A common criterion for all diagnoses of mental disorder is that the individual’s daily life and activities are significantly impaired by the symptoms.6
SELECTED MENTAL DISORDERS COMMONLY AFFECTING CHILDREN AND ADOLESCENTS
Mood disorders involve long-term changes in the child’s prevailing emotions. The presence of symptoms may be cyclic, increasing and decreasing periodically, but they may last for months or years if untreated.6,99 The diagnostic criteria for major depression stipulates that symptoms must have reached a level of severity that results in changes in occupational performance or significant distress during daily activities.6 Depression manifests as persistent or repeated episodes of a combination of irritability, loss of interest in and enjoyment of usual activities, increased or decreased activity level, sadness, periods of crying, decreased energy, inability to concentrate and learn, agitation, sleep and/or appetite disturbance, anxiety, guilt, and/or thoughts of death or suicide. Depression is estimated to occur in 3% of children and 8% of teens.124 Children and adolescents who have experienced clinical depression are at increased risk to have repeated episodes into adulthood.6,69,100 The diagnostic evaluation of depression should be made by a psychologist or psychiatrist through structured interviews with the child and parents.124,146 Ascertaining a diagnosis in children may be complicated because the outward symptoms may appear inconsistently; the child may play and seem happy some of the time. Intervention often includes a combination of medications and psychotherapy or counseling parents.124,146 Brief hospitalization may be required if there is risk of suicide.
Occupational performance and satisfaction are adversely affected by the symptoms of depression. Difficulty with thinking and the loss of enjoyment and interest reduce the child’s motivation to play and decrease ability to attend and learn in school. Children with depression may sleep during the day, even in classes, and often experience aches and pains. They often complain of being tired or bored during previously preferred activities. Activity levels may be decreased or increased, so the child may be chastised for being “lazy” or “out of control,” depending on the situation. Unexpected tearfulness or displays of temper place the child in social jeopardy with adults and peers. Changes in appetite may affect social interactions during meals, as the child is scolded for eating too little or too much. There may be resistance to attending family, church, and other social activities. Among the most occupationally debilitating aspects of depression are the child’s feelings of incompetence, hopelessness, and helplessness. These emotions, however irrational, are symptoms of depression that can prevent children and adolescents from participating in activities that involve any risk of failure or humiliation: deciding which answer to choose on a test, raising one’s hand in class, inviting a peer to play, or joining in a game. Adolescents with depression must add the anxiety and self-doubt of depression to the feelings of self-consciousness typically experienced at this phase of life. Depression increases the risk of alcohol and drug use, as sufferers seek relief from emotions that are overwhelmingly painful.6,112
Bipolar disorder, or manic-depressive illness, is increasingly being recognized as a condition that often emerges during childhood or adolescence.25,72 Individuals with bipolar disorder experience “mania,” or periods of extreme overactivity, agitation, irritability, rapid (“pressured”) speech, and reduced periods of sleep.6 Less often, children and adolescents may display elation, giddiness, or grandiosity.19,88 Episodes of mania are juxtaposed by periods of typical or depressed mood. These mood states may fluctuate quite rapidly, sometimes even presenting as mixed states, or can alternate over a period of weeks or months.6,25 Sometimes a child’s changes in mood may be difficult to distinguish from voluntary behaviors aimed at provoking or controlling others.88 Mania in children may be misdiagnosed as attention deficit disorder, oppositional defiant disorder, or temporal lobe epilepsy.72 During manic phases some people have confused and bizarre thinking that may involve feelings of omnipotence, euphoria, and/or hallucinations. Children and adolescents with bipolar disorder are prone to episodes of aggression and despair and may pose a danger to themselves or others.72 Approximately 10% to 12% of adolescents with recurrent episodes of major depression will develop bipolar disorder.6 Individuals with bipolar disorder are at increased risk for suicide, especially during transitions from a manic to depressed mood state. A diagnostic evaluation should be completed by a psychologist or psychiatrist specializing in the care of children and adolescents, using structured interviews with the child and parents and direct behavioral observation. Intervention often includes medication, psychotherapy or counseling, and client/family education.72,88,146
Children and adolescents who have bipolar disorder may have periods of time when their behavior is noticeably “out of character” or socially inappropriate, or they may seem consistently irritable and active.19 Behaviors that are commonly experienced during low levels of mania include continuously talking, attention-seeking, disregard for others’ feelings or social norms, abruptly changing emotions, and impulsiveness. The child may resist adults’ attempts at guidance or correction or correct him and may act “bossy” toward adults. There may be aggressive outbursts toward property, other children, adults, or himself or herself. These behaviors are not compatible with performance as a student and may occur sometimes even if the child is taking medication. It is important that the adults who regularly interact with a child who has recurring symptoms of bipolar disorder know that these behaviors may not always be under the child’s control and have plans in place to respond effectively, avoiding behavioral outbursts that are disruptive or dangerous. Occupational therapy should include helping the child adopt regular sleeping habits, learn about the illness, engage in effective stress management strategies, and learn ways to communicate well with others. All team members should participate in monitoring the child’s behavior as it relates to medication effects. Some of the most effective medications used to treat bipolar disorder can cause life-threatening side effects if the child becomes dehydrated or the timing of dosage is incorrect.25
Anxiety Disorders
Anxiety disorders are characterized by pervasive and persistent (longer than 6 months) feelings of uneasiness, fearfulness, or dread that are not founded on realistic concerns.6 Estimated to occur in 4% to 13% of children, anxiety is a relatively common problem that is thought to result from a combination of inborn/genetic traits and environmental factors.25 The diagnosis of an anxiety disorder is made by a psychiatrist or psychologist through observation, interviews with the child and family, and self-report questionnaires.145 Symptoms of anxiety and depression often occur together, and medications and psychotherapy may be combined to address both kinds of problems.25,88 Subclinical levels of anxiety may also have a negative impact on children’s occupational performance and social participation and should receive attention by occupational therapists and others who work with children in schools and other settings.
Social anxiety disorder is estimated to affect up to 11% of all children and adolescents.38 Characteristic symptoms include excessive worrying about others’ evaluations of oneself or about one’s past and future behavior. Those affected exhibit considerable self-consciousness and a high need for reassurance by others.6,70,107 Children and adolescents who have social anxiety may be unable to participate in many of the activities in which they would like, or are expected, to engage.13,151 Any time the child feels he is at risk of criticism or embarrassment, he may become overwhelmed by automatic reactions such as a racing heart, blushing, feeling out of breath, and perspiring. Thinking is derailed by emotions of fear or even panic. The anxious child’s behavioral reactions to these overwhelming emotions (e.g., crying, resisting an activity, having a tantrum) may draw critical attention from others, further increasing social anxiety. Acute anxiety reactions can occur in an array of daily situations, such as being called on to perform in class, taking a piano lesson, walking into church, or learning to drive a car. Such experiences are subjectively unpleasant and may cause embarrassment due to others’ real or imagined reactions. Children and adolescents who have symptoms of social anxiety avoid and miss out on participating in many required and cherished activities.45
Obsessive-compulsive disorder (OCD), another subset of the anxiety disorders, is characterized by intrusive thoughts and repetitive behaviors that have little or no functional purpose beyond decreasing tension.6 OCD has been measured as affecting relatively few children and adolescents (fewer than 1%), but is thought by some experts to be underreported, as its expression is often confined to the home.63 Symptoms of obsessive-compulsive disorder may occur consistently or episodically, but they tend to be durable over many years, and are exacerbated by stress.160 OCD typically emerges between the ages of 6 to 15 years in males and 20 to 29 years in females.6
Children and adolescents with OCD may spend many hours per day engaging in behaviors such as hand washing, counting objects, arranging objects in a particular way, checking on the status of something (such as whether an appliance is unplugged), or cleaning. These behaviors may be visible to the casual observer or performed surreptitiously. In either case, if the repetitive activity is interrupted or prevented, the affected individual experiences anxiety. Intervention typically includes medication, client and family education, and cognitive behavioral therapy.25,63 Children and adolescents with neurologic impairments such as learning disabilities, Tourette’s syndrome, and autistic spectrum disorders are at increased risk of also having OCD.63,145
The daily balance of activity is negatively affected by the amount of time spent on obsessive-compulsive rituals in children and adolescents with this disorder. Tasks that would ordinarily take minutes may require hours as the child restarts the process again and again. Task interruption may occur as he or she stops to readjust unrelated objects or to wash hands repeatedly. Studying, packing a book bag, bathing, using the toilet, and getting dressed are just some examples of activities that could be severely affected by obsessive-compulsive symptoms. The child or adolescent with OCD also suffers socially, because even though he may know that his repetitive actions are irrational and, by others’ standards, “weird,” he feels compelled to continue doing them. It becomes easier to spend time alone and at home, rather than to cope with others’ reactions and misunderstanding. Occupational therapists can support team interventions by helping affected children and adolescents to understand the nature of this neurologically based disorder, teaching stress management skills, and helping them identify and reduce exposure to environmental triggers that stimulate obsessive thoughts.
Attention Deficit Disorder
Attention deficit disorder is characterized by significant difficulty with selective and/or sustained attention to tasks; this central problem may be accompanied by difficulties with overactivity and/or impulsivity. Attention deficit disorders are estimated to affect 8% of children and adolescents, with more boys than girls represented.6 A diagnosis is made through structured observations in a variety of settings and across time. Intervention often includes a combination of medication, behavior management, client education, support, and environmental adaptation.185
Children and adolescents with attention deficit disorder may have difficulty performing tasks in environments that are moderately or highly stimulating, such as the typical classroom or household. When trying to engage in activities, the child may have to work at continuously redirecting her attention from extraneous sounds and sights and back to the targeted task. Reading comprehension and listening skills are often affected. Impulsiveness may result in acting before thinking, leading to errors on schoolwork or inappropriate social behavior. Adolescents with attention deficit disorder may have difficulty following through on commitments due to disorganization and forgetfulness. They are less able to organize their time and materials than most of their peers. They may have difficulty sustaining effort on tasks, quickly become “bored” and leave tasks unfinished.
Occupational therapy for children with attention deficits should address the personal, environmental, and occupational factors. Children and teens can be taught to understand that they have a neurologically based problem. They can then learn ways to manage this through adherence to medication routines and attending and responding to their sensory and emotional states. Framing the child’s difficulty as a set of solvable problems, rather than as deliberate misbehavior, can help all parties feel better and behave more productively. Teachers, parents, and clients can learn ways to create and maintain physical environments that minimize auditory and visual distractions during tasks that require concentration and to modify tasks to allow well-timed breaks and opportunities for feedback. All involved parties can learn to structure and support a well-regulated routine of daily activities, with established and balanced patterns of sleeping, eating, work, and play.
Disruptive Behavior Disorders
Oppositional defiant disorder (ODD) is characterized by a well-established pattern of disobedience and hostility toward authority figures that lasts for over 6 months. Children who fit this diagnosis often have excessive displays of temper, are irritable, deliberately refuse to comply with rules and directives, blame others for their actions, and act vindictively.6 They seek to provoke others by verbally threatening or insulting them. ODD is generally diagnosed by 8 years of age, and rarely after early adolescence; rates of its occurrence range from 2% to 16%.6 Conduct disorders are characterized by the many of the same behaviors as those seen in oppositional defiant disorder, but include more intrusive and severe forms of chronic misbehavior such as physical aggression toward property, animals, or people, theft, and/or lying. Environmental factors appear to play a large role in the development of disruptive behavior disorders; there is also evidence of genetic influence and a high rate of co-occurrence with neurologically based problems such as learning disabilities and attention deficit disorder.38 Many children with a conduct disorder are also diagnosed as having depression and/or attention deficit disorder and may receive medication for these problems.
Disruptive behavior disorders affect up to 10% of children and adolescents and seriously impede participation in family, school, and community activities.6,38 Conduct disorders place children at risk of harming others, breaking the law, and being placed in restrictive correctional or mental health facilities. Occupational therapists with clients who have disruptive behavior disorders are positioned to join a team effort to help children learn prosocial, adaptive ways to enjoy school, play, and rejuvenation. This begins with establishing a therapeutic alliance that includes well-understood and maintained expectations for positive behavior and reliable and fair consequences for behavioral infractions.38 Therapy that promotes achievement of recognition and feelings of competence through engaging in valued activities provides children with alternatives to antisocial behavior and motivation to behave in ways that allow participation in the larger community. Teaching the child how to use anger and stress management techniques, social interaction skills, and conflict resolution skills can be part of the occupational therapy plan. Consultation with other team members may include helping teachers and parents identify educational and functional tasks that are motivating, highly structured, and provide the “just right” level of challenge for that particular child or adolescent.
Autism Spectrum Disorders
Autism spectrum disorders, which manifest within the first 3 years of life, are characterized by (1) abnormal ways of relating to people, objects, and events; (2) delayed or missing speech, language, and/or nonverbal communication skills; and (3) restricted, repetitive, and stereotyped patterns of behavior, interests, and/or activities.6 Children with autism spectrum disorder exhibit a wide range of ability and variation in severity of symptoms. At one extreme, children have functional language and cognitive skills at levels that allow their participation in typical classrooms; children at the other end of the spectrum are functionally nonverbal and require continuous assistance and accommodation. Problems that may co-occur with autistic spectrum disorders include sensory processing dysfunction, cognitive impairment, anxiety, depression, hyperactivity, seizure disorder, fragile X syndrome, and tuberous sclerosis.127 The diagnosis of autism spectrum disorder has increased over the past 20 years, spurring debate as to whether this marks an actual increase in the incidence of the disorders or an increased sensitivity in diagnosing new cases.71 The number of special education students classified as having autism spectrum disorder increased by 189,000 between 1994 and 2006.81 Current estimates indicate that approximately 1 in 150 children have an autism spectrum disorder.31 This apparent increase has been attributed variously to a broadening of the diagnostic criteria, the advent of assessments that allow earlier diagnosis, and a possible increase in mistaking other language and cognitive disorders for autism.71,146 Children with autistic spectrum disorders may grow up to achieve full independence and community participation in adulthood or may require assistance throughout their lives. An individual’s long-term outcome is determined by a combination of factors, including the severity of the autistic disorder, cognitive ability, and social factors.39
Intervention for problems associated with autism spectrum disorders often includes behavioral methods, psychoeducational approaches, communication interventions, social skills training, and a variety of medications to address specific symptoms.6,127,136,146 (See Chapter 14 for additional information on this topic.) There is a growing body of evidence linking autistic disorders and sensory processing dysfunction.51,75 Occupational therapy may include sensory integration therapy, life skills training, and social skills training.10,74,114 Clinical trials have demonstrated positive effects for most of these interventions; however, the evidence is limited (see Case-Smith & Arbesman’s review of intervention applied by occupational therapists29). As with all interventions, families should be encouraged and supported in making a critical evaluation of the evidence to date before engaging in a particular intervention.146
The Occupational Therapist’s Role Relative to Psychotropic Medication
All of the mental disorders described above may be treated with medications as a central or adjunctive intervention. Research evidence to date indicates that, just as for adults, a combination of medication and therapy is more effective than either approach alone for anxiety and attention deficit disorders.64,92,98,136 The use of psychotropic medications among children and adolescents has increased significantly over the past 15 years.64,132 Approximately 17% to 22% of all students receiving special education services use psychotropic medications; this includes 42% to 52% of students classified as having emotional disturbance.130
Many children who receive occupational therapy services take psychotropic or seizure medications. The medical management of such drugs is made challenging by the children’s rapid growth and development, as well by as the lack of research to guide decision making.64,88 Although occupational therapists do not administer medications, they should stay apprised of their clients’ medications, and assume responsibility to be informed about the medications’ expected effects, possible side effects, and precautions. As a general guideline, therapists should consistently observe their clients for positive changes and possible unwanted drug effects and report these to the prescribing physician and in the client’s official record. Brown and colleagues have published a useful array of forms that can be used to systematically document behaviors and symptoms that reflect a child’s responses to medication.25 Any time a child displays an abrupt or marked change in his state of arousal (e.g., acts unusually drowsy or agitated), demonstrates signs of neurologic change (such as previously unobserved motor or cognitive difficulties), or complains of discomfort such as nausea or headaches, the possibility of medication side effects should be considered. If the observed symptoms are severe or of sudden onset, the situation should be treated as a medical emergency requiring the immediate notification of the child’s parents and evaluation by a qualified medical practitioner, such as a physician or registered nurse. All such observations and referrals should be documented by the occupational therapy practitioner in a timely manner.
Children and adolescents with psychological and behavioral problems live, work, and play in an array of environments. Their problems and needs may become apparent in a variety of ways, depending on the context. The following section explores the wide range of possible settings in which occupational therapists work with children whose occupational performance is affected by psychosocial dysfunction and how occupational therapy may be practiced in each.
PRACTICE ENVIRONMENTS
This section describes ways in which occupational therapists provide psychosocial intervention in a representative selection of settings and to illustrate how occupational therapists apply holistic, client-centered approaches. A variety of treatment settings are described, representing a continuum from less to more psychiatrically oriented and from less to more intensive and restrictive. The mission, clientele, services, frames of reference, and staffing patterns for each type of facility, as well as traditional or potential roles for occupational therapists in each setting, are outlined. Case studies synthesized from the author’s clinical experiences illustrate psychosocial intervention in a variety of traditional and nontraditional settings.
Therapeutic environments may include early childhood intervention programs, public schools, outpatient mental health services, day treatment programs, residential treatment centers, correctional facilities, and inpatient acute care hospitals. Some of these programs are designed specifically to assist children and adolescents who have identified mental health problems; other programs are oriented toward meeting more general developmental, educational, or social needs. Occupational therapists are established practitioners in some of these settings and are pioneers in other settings. In any case, pediatric occupational therapists have the knowledge base, the skills, and the opportunities to provide psychosocial intervention to children and adolescents with mental health and social problems in all service settings.
Early Childhood Intervention Programs
The primary mission of early childhood intervention (ECI) programs is the prevention and amelioration of developmental disabilities in children from birth to 3 years of age. According to the Individuals with Disabilities Act (IDEA), clients include infants and toddlers who are diagnosed as having developmental delay, those who are considered to be at risk for developmental problems, and their families. Although infants and toddlers are referred primarily to early intervention for evaluation and treatment of neurologic and physical conditions, children may be referred when their development is at risk because of parental mental health problems, such as chemical dependency, domestic violence, parental depression, or other psychiatric disorders. Occasionally the identified infant may have a diagnosed mental disorder, such as failure to thrive or pervasive developmental disorder.6
Professionals working in ECI programs are likely to use developmental, neurodevelopmental, rehabilitative, behavioral, interactional, and familial systems as frames of reference (Table 13-3). Occupational therapists, educated to recognize and treat persons with mental illness, contribute significantly to the ECI team’s effectiveness with high-risk families. For example, mothers who are experiencing anxiety or depression are often unable to meet their infant’s needs for responsive interaction.41,80,137 Parents who are addicted to drugs are at increased risk of neglecting or abusing their children.149,184 Occupational therapists can observe clients for signs of problems such as depression and substance abuse and can facilitate clients’ access to evaluation and treatment by a qualified care provider. Environmental stressors such as poverty, social isolation, and community violence also need to be evaluated and addressed, since they play a part in a family’s ability to meet the needs of infants and children.44,64,79,174 If the parent of a child with medical complications reports that the family is having difficulty following through with the child’s care because of unemployment and marital stress, the ECI team is positioned to refer the parents for financial assistance, work placement, and counseling services. Once these concerns are resolved, parents have more energy available for child care. If there appears to be a danger of child abuse or neglect, the occupational therapist is mandated by law to report these concerns to the state child protection agency. Case Study 13-4 presents an example of family-centered early intervention.
Public School Systems
Students whose special needs are primarily psychosocial are classified by the school system as emotionally disturbed (ED). Federal regulations for IDEA define this special education classification as:
a condition exhibiting one or more of the following characteristics over a long period of time and to a marked degree, which adversely affects educational performance: (A) An inability to learn that cannot be explained by intellectual, sensory, or health factors; (B) An inability to build or maintain satisfactory interpersonal relationships with peers or teachers; (C) Inappropriate types of behavior or feelings under normal circumstances; (D) A general pervasive mood of unhappiness or depression; or (E) A tendency to develop physical symptoms or fears associated with personal or school problems. This category does not include children who demonstrate socially maladjusted behavior (e.g., delinquency, school truancy, conduct disorder) in the absence of the problems previously listed. Other categories in which psychosocial problems and behavioral disorders are often present include pervasive developmental disorders, mental retardation, and traumatic brain injuries [Code of Federal Regulations, Title 34, § 300.7(c)(4)(i)].
Emotional disturbance was the primary disability category for about 1 in 12 special education students in the year 2000 to 2001.82 The rate of educational diagnoses of emotional disturbance increases with age and grade level. Most children in need do not receive professional mental health care, so the public schools serve more children with behavioral and emotional disorders than any other agency.76 Students with mental health problems do not qualify for special education services unless their symptoms significantly disrupt their school performance, so their needs are often underserved at school, as well as in the community and health care systems.12 Occupational therapists working in the schools have an important responsibility to observe the students with whom they work for signs of emotional distress, as many children with mental health problems also have the learning and attentional disorders that are typically referred for services at school.
The primary mission of public education is academic and social preparation for future education and work roles. Research shows that this goal has been largely unreached for students who have emotional and behavioral problems.20,27,110,177 Students with moderate to severe behavioral problems are unable to take full advantage of education and experience repeated academic and social failure. More than 50% of students with emotional or behavioral disorders drop out of high school.165 These students have a significantly increased risk for economic dependency and crime.20,175 The public schools represent an arena in which occupational therapists have an unrealized opportunity to have a tremendous effect on the lives of children with psychosocial problems.12,123 See Chapter 24 for further description of school mental health programs.
A variety of school settings serve special education students with ED. Self-contained classroom arrangements allow students whose behavior is frequently disruptive or otherwise inappropriate to receive intensive behavioral intervention while being educated in a small group setting. However, students in such classrooms are segregated from peers and role models and suffer the stigma of being identified as “different.” This segregation contradicts the goal of full inclusion of special education students in regular education settings.172 In a full inclusion model, students attend regular education classrooms with support services that may include a resource room for specific subjects, classroom aides, crisis intervention, and counseling services. Benefits of this approach include regular exposure to a typical school environment, opportunities to interact with typically developing peers, and positive experiences that reinforce learning of social skills. Problems can arise with this approach when the teachers have large numbers of students and little training in preventing or managing disruptive behaviors. Teachers and students then feel inadequate and frustrated.
Many classroom teachers incorporate social skills training programs into their regular curricula. These programs are suitable for all children, and they address areas such as communication and social skills,66 violence prevention,23 and drug abuse prevention.67 Such educational programs can provide an excellent means of developing prosocial thinking and behavior in typically developing children. However, these programs do not provide the intensive guidance required by many children and adolescents who have psychosocial dysfunction affecting performance in these areas.143
School-based therapeutic intervention is directed toward enhancing students’ academic and future vocational performance with an emphasis on both scholastic and social development. Traditionally the school psychologist, counselor, or social worker assumes responsibility for evaluating psychosocial needs and may work with students in individual or small group sessions. These professionals serve the needs of all students, not just those in special education, and may not have an extensive clinical background in psychopathology.110 They apply behavioral, cognitive, and developmental approaches (see Table 13-3).
Many leaders in education and occupational therapy believe that the services provided to students with behavioral disorders are inadequate in quantity and quality.* Teachers express despair as they sacrifice creative educational methods to address behavioral crises. Parents of students with behavioral disorders are frustrated by the paucity of services to address their children’s particular needs. All parents are concerned about their children’s safety and education while they are at school.
Occupational therapy activity groups have been described as effective for elementary students who have social and behavioral difficulties.50,147,148 Motivating activities such as planning and preparing meals, creating craft projects, producing a newspaper, performing skits and plays, and refinishing furniture help students develop competencies in daily living skills while practicing adaptive responses to interpersonal challenges and developing self-confidence. The goal of this type of approach is to support improved occupational functioning in the classroom and other school settings. Students’ behavioral improvements in occupational therapy task groups have been shown to generalize to the classroom and other contexts, thus winning the support of educators and administrators in the school.1,148 Agrin speculated that the students’ future success in less restrictive settings could be predicted by the development of their social skills in the activity groups.1
Students who are referred for occupational therapy services to address fine motor, perceptual, or orthopedic problems may also have social and emotional needs that impair academic performance. Case Study 13-5 exemplifies how one student’s multiple needs were addressed. General education teachers are working with increasing numbers of special needs children, including those who have educational diagnoses of emotional disturbance. Additionally, their classrooms include children who are not enrolled in special education, but who are troubled and preoccupied with acute and/or chronic life stresses such as poverty, community violence, and family turmoil. In some schools the majority of students are trying to learn despite a climate of constant crises in their homes and neighborhoods. Behavioral disruptions are frequent and educators feel endangered and unsupported. Occupational therapists are positioned to provide consultation to teachers who need ideas regarding environmental adaptation and group management and to help determine which students should be referred for occupational therapy or other related services evaluations. By educating and supporting teachers, therapists can have a positive influence on the school experiences of hundreds of children.
The School to Work Opportunities Act (1994) and IDEA (2004) both reflect the high priority placed on preparing students for gainful employment. Middle and high school students who have emotional and behavioral problems are considered by many to be among the most challenging to transition successfully into independent living and satisfying, economically sustaining work.27,111,175 Although no universally successful means have been identified, research to date indicates that the most promising interventions include individualized planning that involves the student and parents. The intervention should also include social skills training and support, classroom education regarding work values and life skills, and actual work experience in positions where the fit between students and jobs is optimal.110 Age- and situation-appropriate occupations should be emphasized over performance components training, and environments should be structured to facilitate students’ success.24,134 Occupational therapists are able to provide any and all of these interventions, and they can serve educational teams, as well as transitional planning specialists.
School-based occupational therapists do not consistently emphasize psychosocially oriented intervention.12,30,123 On the basis of a review of the special education literature, Schultz concluded that teachers would welcome the kind of assistance that occupational therapists can provide in improving students’ social skills.147 School administrators who are concerned about occupational therapists meeting the needs of the traditional referrals may initially be less encouraging. School-based therapists who are committed to providing holistic services need to educate and persuade colleagues regarding the potential effectiveness of occupational therapy approaches to help students meet central academic goals by developing essential skills needed for social participation. This may be approached directly through discussions with key administrators, in-services for teachers and related services professionals, program development, and case-by-case demonstration. Occupational therapists should advocate including psychosocial goals in students’ individual education programs. Trends in inclusionary and transitional education have created an atmosphere in which occupational therapy leadership in comprehensive holistic intervention approaches are needed and often welcomed. Examples of evidence-supported, activity-based interventions used by school-based occupational therapists in their work with students with emotional disturbances are listed in Box 13-2.
Mental Health Services
In the United States, mental health services for children and adolescents have been chronically underfunded, with the result that most young people who have mental disorders do not gain access to expert professional services.109,163,167,183 In 1992, Congress responded to this problem by authorizing the Comprehensive Community Mental Health Services for Children and their Families Program.165 This program provides federal funding through demonstration grants to states and communities and is designed to develop and promote effective ways to organize, coordinate, and deliver mental health services and supports for children and adolescents and their families. Private foundations have joined in the effort, resulting in the coordination of multiple agencies within communities working together to provide innovative, client-centered, culturally appropriate services. A universal goal of contemporary community-based mental health services for children is to facilitate successful participation within the family, community, and school. Best-practice standards for children with severe and complex needs involve a “wraparound” planning and management process, in which the family and all involved care providers work closely together to ensure well-coordinated, comprehensive intervention.183 Although few occupational therapists identify mental health settings as their primary site of practice, many practice in settings that participate in the coordinated care of young people with mental health problems.126 These settings include early intervention services, day care programs, preschools, schools, and hospital-based outpatient clinics. Although most mental health centers and private practices do not include occupational therapists as part of their core team, occupational therapists can participate as valuable ad hoc members of the extended, community-based mental health team and as consultants. Understanding the forms and functions of contemporary mental health systems allows occupational therapists to engage effectively with the professionals working within the system and to join in providing coordinated care from a unique perspective.
Outpatient treatment is the mental health intervention most commonly accessed by children and adolescents.167 Outpatient mental health services may be provided through freestanding clinics, hospital-based programs, publicly funded community mental health centers, health maintenance organizations, and private practices. Funding sources may include the clients’ families, private insurance, Medicaid, federal grants, and state monies.102,118 An agency’s sources of funding influence the types of clientele served and the types of services provided.
Children and adolescents who seek outpatient mental health services often have significant behavioral disturbances that have caused moderate to severe levels of disturbance for family, school, or community members.102 The primary goals of outpatient mental health services are the diagnosis and management of mental health problems to improve functioning within the community and prevent crises necessitating hospitalization.
The child’s initial contact with an outpatient mental health practitioner—typically a social worker, psychologist, psychiatrist, or licensed counselor—consists of an intake interview exploring the nature and severity of the child’s and the family’s problems. Responses to the interview form the basis for decisions regarding appropriate evaluation and intervention. Possible dispositions include outpatient evaluation at a later date or crisis evaluation with immediate short-term intervention.
Frames of reference used in outpatient programs and practices vary, but they commonly draw from cognitive behavioral, behavioral, family systems, neurobiologic, and psychodynamic theories (see Table 13-3). Treatment approaches are most commonly goal-focused and time-limited and involve the family and school. Clients generally attend one or two 1-hour sessions per week for a specified period. In publicly funded mental health centers, payment for services is based on the individual’s income. Third-party payers have varied levels of coverage for mental health care. Therapeutic modalities commonly include play therapy (for young children), talking therapy, expressive art, therapeutic board games, group discussions, family discussions, and parenting education sessions. These programs can be staffed by a combination of psychologists, social workers, psychiatrists, psychiatric nurses, and licensed counselors.118
Day treatment programs and therapeutic schools are offered in a variety of settings, including psychiatric hospitals, community mental health facilities, and schools for students with special needs.141 Such programs provide a therapeutic level of intensity between outpatient intervention and hospitalization and are popular for clinical and economic reasons.54 Clients typically attend programming from 4 to 6 hours per day, 5 days per week, and are at home during evenings and weekends.21 Interventions often include a variety of therapies, including occupational therapy and specialized academic classes.
Day treatment programs or schools can facilitate a child’s transition from the hospital back to the home and community, provide crisis stabilization, allow comprehensive evaluation, or serve as an intensive therapeutic alternative to outpatient or inpatient treatment.141 Programming often follows a psychoeducational model and may include vocational evaluation and training for adolescents.128 A psychiatrist or psychologist who specializes in child and adolescent mental health or a special educator typically leads intervention teams. Other team members are listed in Table 13-3 and can include occupational therapists.
Occupational therapy activities in day programs can address academic, sensorimotor, daily living, and psychosocial goals. Crafts, role-playing exercises, cooperative action games, board games, cooking, sensorimotor interventions, and field trips are popular modalities in such occupational therapy programs. Hygiene and grooming, telephone and e-mail etiquette, how to order food in a restaurant, and other such daily living needs can be addressed. Working with the client’s parents, child care providers, teachers, job coach, or school-based occupational therapist can facilitate the transition from intensive day treatment programs to the community and public school and enhance the carryover of interventions and goals. The family may also benefit from assistance with locating and securing social and leisure resources. Case Study 13-6 describes how a consultative model of intervention can be used to assist with the transition of a client from day treatment back to full community involvement. The focus in this example is on educating and problem solving with personnel from another agency.
Residential Treatment Centers
About 3% of children and adolescents receiving state-funded mental health services utilize residential treatment centers, facilities providing around-the-clock care.165 Residential care is highly restrictive and costly and is typically utilized only when other means of intervention have failed. Lengths of stay in residential treatment centers vary from weeks to years and are influenced by funding constraints, the facility’s philosophy, and the needs of the client and family.155 Program philosophies range from highly institutional to more naturalistic and homelike environments, and some facilities provide educational programs on-site. Residential treatment centers vary in size from tens to hundreds of residents. The most common reasons for placement are aggressive behaviors toward self or others, mental disorders with severe and persistent symptoms, lack of family supports, and abuse. More than half of the children admitted into residential care come from other congregate care settings, such as acute care hospitals, juvenile corrections, foster homes, and other residential care centers.3
The immediate mission of residential care programs is to provide a safe and therapeutic environment for children and adolescents whose behavioral, emotional, and social problems preclude their safety and competence in the community.156 The intended outcome of residential care is for children and adolescents to function as full participants within the community and family, foster family, transitional living, or independent living settings. Experts in the area of residential care assert that treatment may include individual, group, and family therapy sessions. To be meaningful, therapeutic intervention must continue in the everyday experiences of children as they interact with child care staff and their peers.14,52,156 The effectiveness of intervention is determined by the skills of the therapeutic, educational, and childcare staff in building relationships, managing children’s behavior, and structuring leisure and work activities.48,162
Staffing reflects each residential care facility’s philosophy and target populations. All residential care facilities employ childcare workers who are paraprofessionals with various levels of expertise. Other team members include psychiatrists, psychologists, social workers, nurses, teachers, and “therapeutic activities personnel,” who may include occupational therapists.3 Some residential treatment facilities may contract occupational therapy services that can include consultation to the house staff regarding the residents’ developmental needs and limitations, ways to organize and guide household responsibilities to include the residents, and ways to teach residents self-care and community living skills (Case Study 13-7). Other occupational therapists provide services within the residential centers’ school programs, addressing goals related to academic and social performance. Frames of reference often used in residential care include cognitive behavioral, behavioral, psychodynamic, and psychoeducational approaches.89,156 Children who live in even the most deluxe institutional settings do not have access to many occupational experiences that are a part of the daily activities for children in family homes and the community. At this time, occupational therapy is not a mandated service as determined by accreditation standards for residential care facilities. Published literature describing or testing the effectiveness of occupational therapy within residential care facilities for children is minimal. As a member of a small community of practitioners who have provided occupational therapy in residential care for more than 10 years, this author asserts that occupational therapy can have a tremendous impact on the quality of life and effectiveness of residential treatment in preparing children and adolescents for successful transitions to lives in the larger community. Direct intervention with the children and adolescents in residential care can include many of the goals and approaches outlined in the discussion of occupational therapy in day treatment programs. Additionally, occupational therapists can facilitate the resident’s participation in community activities such as shopping, playing sports, participating in activity clubs, and attending church. Opportunities for as much family interaction as possible during such activities increase the benefits of such experiences.93,155
Juvenile Corrections
The more than 100,000 children and adolescents who are housed by the juvenile justice system share many of the needs of those in residential treatment centers and represent another underserved group with serious psychosocial and occupational needs.82 Youth who have been incarcerated for committing crimes often have serious emotional disturbances that have not been addressed therapeutically.8 In a review of the literature on juvenile detention, Goldstrom and colleagues estimated that up to 95% of youth in the juvenile justice system have mental, emotional, or behavioral health problems, 20% of these with severe mental disorders.65 Those incarcerated are completely removed from the home and community and lack opportunities to gain or maintain skills they need to reintegrate into the community on release. Boredom and hopelessness can contribute to antisocial behavior within the facility, posing a danger to the prisoners and staff. Most correctional institutions for youth provide traditional psychotherapeutic care but not rehabilitation-focused care.82 Occupational therapists should be involved in the comprehensive psychiatric and functional evaluations of children and adolescents who are either under consideration for psychiatric commitment or who are to be tried as adults. They can provide therapeutic services to address their psychosocial and daily living skills needs and help to educate staff members about the developmental and neurobehavioral issues that this group shares. Youth offenders who are enrolled in diversional programs or who are being treated in state or other psychiatric facilities would be good candidates for occupational therapy.
Inpatient Psychiatric Hospitals
Inpatient psychiatric hospitals provide the most restrictive, intensive, and costly therapeutic intervention.167 They are used for children and adolescents who pose a serious safety risk to themselves or others, have complicating medical conditions, or require specialized teams for rapid diagnosis and stabilization.138 Very often individuals are hospitalized when in crisis, such as after a suicide attempt, an assault, or a psychotic episode. Sometimes patients are admitted for comprehensive psychological and medical evaluation of complex chronic problems. Due to the high cost of inpatient care, lengths of stay are brief, with a range of 2 to 27 days and a median of 4.5 days.28
Inpatient psychiatric units may be found in general hospitals, state psychiatric hospitals, and private psychiatric hospitals. Child and adolescent inpatient psychiatric units are usually locked facilities that are directed by a psychiatrist and staffed by nurses and paraprofessionals who are trained in the care and management of severely impaired patients.47 The treatment team is interdisciplinary and may include psychiatrists, nurses, paraprofessional direct care staff, psychologists, neuropsychologists, and social workers. The professional staff apply a variety of psychosocial theories, with neurobiologic and cognitive behavioral approaches among the most commonly used. Due to brief lengths of stay, occupational therapists are rarely part of the core intervention team in acute care psychiatric units for children and adolescents. An occupational therapist may be brought in to contribute to the developmental, neurodevelopmental, and functional evaluations for severely impaired patients.
The case examples presented throughout this chapter depict a number of ways to intervene with children and adolescents who have psychosocial problems. The following section outlines occupational therapy evaluation and intervention options more specifically and in more detail.
EVALUATION AND INTERVENTION
The evaluation process is foundational to the intervention process and largely determines its success. Evaluating children who exhibit behavioral problems can be challenging, due to the complex nature of the task and the fact that the child may be unable to cooperate with traditional assessment approaches. As much information as possible should be gleaned indirectly from past and current school or medical records. Evaluating therapists can learn a great deal from teacher and parent checklists and naturalistic observations in typical contexts, such as various settings within the school, home, institution, and community.
The evaluation process begins with an occupational profile that includes an occupational history, the client’s perceptions of current occupational functioning, the client’s concerns about occupational performance, and priorities for intervention.4 A thorough occupational profile includes information about the person, environment, and occupations. The occupational profile may be obtained through informal interviews or with the assistance of a structured interview such as the Canadian Occupational Therapy Performance Measure.105 An interview or paper-and-pencil activity may be used to gain an understanding of the child’s habits and balance of activity. Some children are better able to express their concerns and hopes for the future in pictures. For them a large piece of paper and some colorful markers or crayons, along with an invitation to “draw a picture of yourself doing something” or “make a picture of some things you want to be doing next month” may give the therapist and the child a way to begin their dialog. The purpose of beginning the evaluation process with an occupational profile is to obtain a sense of the scope and immediacy of issues concerning the client. For occupational therapists working with children, the “client” includes the referring adult, who could be a parent, a teacher, a foster parent, or some other closely involved person. When the child is very young, has limited functional communication, or is being seen in the context of school, the occupational profile should include information from the involved adults. This information will guide decisions about subsequent steps in the evaluation process and help with formulating intervention goals and methods, facilitating their efficiency and quality.
In school settings, a pre-assessment checklist for teachers to complete prior to evaluation can help to define issues of concern and inform teachers about the scope of occupational therapy (Figure 13-2). This tool is designed with items related to written schoolwork listed first, and cast with a positive slant (“Works independently on written assignments”). The last 12 items relate more to cognitive and social performance, and the items are cast from a more problem-oriented perspective (“Has difficulty learning new motor tasks”). Teachers rate the consistency of performance and then may write in specific concerns. The results can help to target areas of strength and possible limitations that require further evaluation.
One of the most valuable assessment methods with children and adolescents who have social participation problems is to observe them interacting with peers or family members during motivating activities such as crafts, board games, or preparing and enjoying food.133 During such sessions the therapist can see the child in action as she responds to opportunities to initiate interactions, make choices, share opinions, request help, try something new, cope with competition or conflict, and other typical demands of social participation. The activity-focused session can also allow observations of performance areas, such as functional reading, planning and organization, safety awareness, concentration, problem solving, postural control, or small tool use. If the session includes classmates, family members, or others with whom the child relates at home or school, information about the child’s social environment is also gathered.
An evaluation of play can provide invaluable, multifaceted information about a child’s social, emotional, cognitive, and motor development and addresses a critical area of occupational performance. Assessments for this purpose include structured observational measures, such as the Preschool Play Scale94–96 or the Test of Playfulness.152 Florey and Greene outline an activity observation guide to facilitate practitioners’ evaluation of play in children aged 6 to 12 years.57
The Social Skills Rating System was developed by psychologists to evaluate and classify social behavior in students from kindergarten through 12th grade.66 There are three versions of the protocols, each for a different grade range. Through a combination of teacher, parent, and student (self-) rating scales, this tool measures perceived performance in the domains of social skills, academic competence, and problem behaviors. The 30 social skills scale items are stated in positive terms (e.g., “Initiates conversation with peers”) and include items indicative of cooperation, assertion, responsibility, empathy, and self-control. Respondents are asked to rate the items in terms of frequency and importance. The problem behavior items, answered only by parents and teachers, classify behaviors as externalizing (behaviors that are intrusive or disruptive), internalizing (behaviors reflecting anxiety or sadness), and hyperactivity. The Social Skills Rating System results are easily translated into intervention and individualized education plan goals and objectives.
The School Function Assessment (SFA) is an observational assessment that assists with the evaluation of school performance of students with disabilities.43 It is administered as a paper-and-pencil form that can be completed by the occupational therapist, child’s teacher, and others who know his school behavior well. It is followed by a structured interview that elaborates on the written responses. More than 100 items on the SFA pertain to social participation in categories of functional communication, memory and understanding, following social conventions, compliance with adult directives and school rules, task behavior/completion, positive interaction, behavior regulation, and safety.
The Occupational Therapy Psychosocial Assessment of Learning (OTPAL) uses a combination of observation and interviewing to evaluate students’ psychosocial abilities as they relate to their specific school environment.161 This assessment is designed for children in elementary school who have been identified as having social participation difficulties.
Standardized assessments of skills, such as measures of the child’s fine and gross motor abilities, developmental levels, handwriting, sensory integration, and cognitive-perceptual abilities, should be employed as needed for intervention planning. Some standardized assessments such as the Miller Function and Participation Scales122 include behavioral checklists that provide valuable insight from the parent’s or teacher’s perspective.
General guidelines for the structured evaluation of students who may resist following directions are:
1. Remember that the main goal is first to form a therapeutic alliance and then to measure the student’s best performance on assessment items.
2. Allow extra time for relationship building and breaks during the assessment sessions. Take several brief sessions to complete the battery, if that is needed to ensure a valid measure. Do not be afraid to stop a session early if the child becomes agitated or intractable; crisis prevention is always preferable to crisis intervention.
3. Ask the teacher beforehand for tips about the child’s preferences and dislikes. Find out what behavior management techniques work well in the classroom and what interaction styles to avoid. Ask if there is any history of aggressive behavior and, if so, what forms it takes.
4. Be prepared to use rewards to help the child persevere. Favored items include stickers, small candies, and an enjoyed activity at the session’s end.
5. Involve the student as a partner in the evaluation process by explaining the nature and purposes of the assessments, interviewing personably, asking for feedback, and making responsive adjustments as often as possible.
Intervention
If it is to be meaningful and effective, intervention with children and adolescents who have social performance problems must include goals that directly address these concerns. These goals should relate directly to the contexts and activities in which the child needs and wants to participate. Examples of such goals are presented next for James, a 10-year-old who wants to participate in the general physical education classes but has struggled with frequent behavioral “meltdowns” and noncompliance. The intervention team has designed the following goals:
Long-term goal I: James will participate successfully in physical education classes, requiring 0 to 1 verbal correction per class session by (date).
Short-term goal Ia: Given verbal reminders and adult support, James will consistently take turns with peers during a 20- minute ball game by (date).
Short-term goal Ib: James will independently locate his “square” upon entering the gym, and, given occasional verbal cues, will sit or stand on his square as directed by the teacher on 4 of 5 days by (date).
Short-term goal Ic: James will refrain from leaving the gym without permission 100% of the time by (date).
Short-term goal Id: Given opportunities to take brief “breaks” as needed, James’ behavior will be age-appropriate and polite during sports and games in physical education classes, on 4 of 5 opportunities by (date).
Contemporary models of occupational therapy emphasize interventions using activities within their natural contexts.4,106 In order to be optimally therapeutic, activities must
• Be interesting and motivating to the client
• Challenge at least one (preferably more than one) of the skills or abilities targeted for improvement
• Be graded to challenge the child at a level that requires effort and facilitates learning but does not overwhelm
Schultz described such an approach with boys who have been classified with behavior disorders in school, using the model of Occupational Adaptation (Research Note 13-1).147,148
In contrast with the environmentally focused approach of Occupational Adaptation, other interventions may be occupation-focused in which the therapists provide highly structured activities. For example, behavioral methods such as point- or token-reward systems may be incorporated into activities-based therapy (Case Study 13-8). This type of operant behaviorism has been well researched and found to be effective in promoting new skills.139 However, operant behavioral approaches have been criticized by some because they take power away from the naturalistic environmental influences and the child’s learning and place it more on the artificial rewards and the therapist.148,170 Ideally, operant behavioral methods, if used at all, are temporary facilitators for children who have learned to get their needs met through unacceptable behaviors and who can quickly learn adaptive behaviors, given a temporary reward that is then faded as the naturally occurring social rewards become available.
A more socially based behavioral approach is that of rational intervention (RI), a cross-disciplinary decision making system that assists those interacting with children and adolescents with the clinical reasoning needed to make immediate responses that facilitate social participation (Table 13-4).49 The primary goal of RI is to help children attain and maintain behaviors that are adaptive and appropriate for participation in natural contexts and to create a consistent approach that supports this for all staff members and adult family members who interact with the child. General principles of RI are as follows:
• Every interaction between a child and an adult is a learning session.
• Intervention begins with the adult’s consistent enactment of respectfulness and caring toward the child.
• The main goals of intervention are all persons’ immediate safety and the continuous improvement of the child’s ability to make decisions that support successful participation in life, at home and in the community.
• Opportunities for making choices and decisions are built into daily activities as often as possible. Children should have regular, frequent opportunities to practice skills needed for community living through educational and leisure experiences in the community.
• In order to promote children’s opportunities for decision making, adults should impose the least amount of external control needed to maintain safety and promote positive, functional behavior.
When using an RI approach, the therapist initially observes and assesses the child’s behavior and then classifies it as belonging in one of three color-coded zones (Case Study 13-9). Green zone behaviors are adaptive and would be acceptable in most community and home settings. Yellow zone behaviors are mildly to moderately problematic and require monitoring, environmental modification, or cueing to facilitate adaptive social behavior. Red zone behaviors present a threat or actuality of danger to the child or others and require direct and immediate verbal or physical management. Therapeutic responses include facilitation, monitoring, gentle correction, moderate correction, and strong correction and may be incorporated into therapy sessions and all social participation contexts (Box 13-3).
SUMMARY
Children and adolescents with emotional, cognitive, and behavioral problems have limited participation in home, school, and community life. Social problems such as poverty, family sociopathic conditions, and cultural violence have been linked with an increased incidence of psychosocial dysfunction in young people.37,140,184 Such social problems are steadily increasing in our country, while mental health services for young people continue to be inadequate in quantity and quality. Occupational therapists who work with children and adolescents have the knowledge and skills to help improve their clients’ occupational functioning by addressing key psychosocial needs. This may be accomplished through individual and group therapy, program development, and consultation. Pediatric occupational therapists in all settings need to be psychosocial practitioners to meet effectively the urgent and growing needs of young people and their families.
REFERENCES
1. Agrin, A. Occupational therapy with emotionally disturbed children in a public school. American Journal of Occupational Therapy. 1987;7:105–114.
2. Ainsworth, M.D., Blehar, M.C., Waters, E., Wall, S. Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Earlbaum, 1978.
3. American Association of Children’s Residential Treatment Centers. Outcomes in children’s residential treatment centers: A national survey. Washington, DC: AACRC, 1999.
4. American Occupational Therapy Association Commission on Practice. Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy. 2002;56(6):609–639.
5. American Occupational Therapy Association. Psychosocial aspects of occupational therapy. American Journal of Occupational Therapy. 2004;58(6):669–672.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association, 2000.
7. Amundson, S. Evaluation Tool for Children’s Handwriting. Homer, AK: OT Kids, 1995.
8. Atkins, D., Pumariega, A., Rogers, K., Montgomery, L., Nybro, C., Jeffers, G., et al. Mental health and incarcerated youth: II. Prevalence and nature of psychopathology. Journal of Child and Family Studies. 1999;8(2):193–204.
9. Bagley, C., Mallick, K. Prediction of sexual, emotional and physical maltreatment and mental health outcomes in a longitudinal cohort of 290 adolescent women. Child Maltreatment. 2000;5:218–226.
10. Baker, J. Social skills training for children and adolescents with Asperger’s syndrome and social-communications problems. Shawnee Mission, KS: Autism Aspergers Publishing, 2003.
11. Barnekow, K., Kraemer, G. The psychobiological theory of attachment: A viable frame of reference for early intervention providers. Physical and Occupational Therapy in Pediatrics. 2005;25:3–15.
12. Beck, A., Barnes, K., Vogel, K., Grice, K. The dilemma of psychosocial occupational therapy in public schools: The therapists’ perceptions. Occupational Therapy in Mental Health. 2006;22:1–17.
13. Beidel, D.C., Turner, S.M., Morris, T.L. A new inventory to assess child social phobia: The Social Phobia and Anxiety Inventory for Children. Psychological Assessment. 1995;7:73–79.
14. Beker, J., Feuerstein, R. The modifying environment and other environmental perspectives in group care: A conceptual contrast and integration. Residential Treatment for Children and Youth. 1991;8(3):21–36.
15. Belle, D. Poverty and women’s mental health. American Psychologist. 1990;45:385–389.
16. Belsky, J. Quantity of nonmaternal care and boys’ problem behavior/adjustment at ages 3 and 5: Exploring the mediating role of parenting. Psychiatry. 1999;62(1):1–20.
17. Belsky, J., Fish, M., Isabella, R. Continuity and incontinuity in infant negative and positive emotionality: Family antecedent and attachment consequences. Developmental Psychology. 1991;27:421–431.
18. Bendersky, M., Lewis, M. Environmental risk, biological risk, and developmental outcome. Developmental Psychology. 1994;30:484–494.
19. Biederman, J. Is there a childhood form of bipolar disorder? Harvard Mental Health Letter. 1997;13:8.
20. Blackorby, J., Wagner, M. Longitudinal post school outcomes of youth with disabilities: Findings from the National Longitudinal Transition Study. Exceptional Children. 1996;62:399–413.
21. Block, B., Lefkovitz, P. Standards and guidelines for partial hospitalization. Alexandria, VA: American Association for Partial Hospitalization, 1992.
22. Boden, J., Horwood, L., Fergusson, D. Exposure to childhood sexual and physical abuse and subsequent educational achievement outcomes. Child Abuse and Neglect. 2007;31:1101–1114.
23. Botvin, G., Griffin, K., Nichols, T., Preventing youth violence and delinquency through a universal school-based prevention approach. Prevention Science 2006;7. Retrieved May 2009, from, http://www.springerlink.com/content/g7437517441m5l1l/fulltext.html.
24. Brollier, C., Shepherd, J., Markley, K. Transition from school to community living. American Journal of Occupational Therapy. 1994;48:346–353.
25. Brown, R., Carpenter, L., Simerly, E. Mental health medications for children: A primer. New York: Guilford Press, 2005.
26. Burke, J.P. Philosophical basis of human occupation. In: Kramer P., Hinojosa J., Royeen C.B., eds. Perspectives in human occupation: Participation in life. New York: Lippincott Williams & Wilkins; 2003:32–44.
27. Carson, R.R., Sitlington, P.L., Frank, A.R. Young adulthood for individuals with behavioral disorders: What does it hold? Behavioral Disorders. 1995;20:127–135.
28. Case, B., Olfson, M., Marcus, S., Siegel, C. Trends in inpatient mental health treatment of children and adolescents in U.S. community hospitals between 1990 and 2000. Archives of General Psychiatry. 2007;64:89–96.
29. Case-Smith, J., Arbesman, M. Evidence-based review of interventions for autism used in or of relevance to occupational therapy. American Journal of Occupational Therapy. 2008;62:416–429.
30. Case-Smith, J., Archer, L. School-based services for students with emotional disturbance: Findings and recommendations. OT Practice. 2008;13:17–21.
31. Centers for Disease Control and Prevention, 2008.
32. Chafel, J.A., Hadley, K.G. Poverty and the well-being of children and families. In: Walker C.E., Roberts M.C., eds. Handbook of clinical psychology. New York: John Wiley & Sons; 2001:48–71.
33. Chess, S. Temperament: Theory and clinical practice. The Harvard Mental Health Letter. 1997;14(5):5–7.
34. Chess, S., Thomas, A. Dynamics of individual behavioral development. In: Levine M.D., Carey W.B., Crocker A.C., Gross R.T., eds. Developmental-behavioral pediatrics. Philadelphia: W.B. Saunders; 1983:158–175.
35. Chess, S., Thomas, A. Know your child. New York: Basic Books, 1987.
36. Child Welfare Information Gateway Home page, 2008. Retrieved May 2009, from, http://www.childwelfare.gov/.
37. Constantino, J. Parents, mental illness, and primary health care of infants and young children. Zero to Three. 1993;13(5):1–10.
38. Cooley, M. Mental health and learning disorders in the regular classroom: How to recognize, understand, and help challenged (and challenging) students succeed. Minneapolis: Free Spirit Publishing, 2007.
39. Coplan, J., Counseling parents regarding prognosis in autistic spectrum disorder. Pediatrics 2000;105. Retrieved May, 2009, from, http://www.pediatrics.org/cgi/content/full/105/5/e65.
40. Cornell, T., Hamrin, V. Clinical interventions for children with attachment problems. Journal of Child and Adolescent Psychiatric Nursing. 2008;21:35–47.
41. Correia, L., Linhares, M. Maternal anxiety in the pre- and postnatal period: A literature review. Review of Latino-American Enfermagem. 2007;15:677–683.
42. Costello, E.J., Compton, S., Keeler, G., Angold, A. Relationships between poverty and psychopathology: A natural experiment. Journal of the American Medical Association. 2003;290:2023–2029.
43. Coster, W., Deeney, T., Haltiwanger, J., Haley, S. School function assessment. San Antonio, TX: Psychological Corporation, 1998.
44. Coulton, C., Korbin, J., Su, M., Chow, J. Community level factors and child maltreatment rates. Child Development. 1995;66:1262–1276.
45. Crick, N.R., Ladd, G.W. Children’s perceptions of their peer experiences: Attributions, loneliness, social anxiety and social avoidance. Developmental Psychology. 1993;29:244–254.
46. Cuevas, C., Finkelhor, D., Ormrod, R., Turner, H. Psychiatric diagnosis as a risk marker for victimization in a national sample of children. Journal of Interpersonal Violence. 2009;24(4):636–652.
47. Dalton, R., Forman, M. Psychiatric hospitalization of school-age children. Washington, DC: American Psychiatric Press, 1992.
48. Daly, D., Schmidt, M., Spellman, D., Criste, T., Dinges, K., Teare, J. The Boys’ Town residential treatment center: Treatment implications and preliminary outcomes. Child and Youth Care Forum. 1998;27(4):267–279.
49. Davidson, D. Measuring the outcome of Rational Intervention: A behavior management approach for children and adolescents in residential care. Unpublished manuscript, 2001.
50. Davidson, D., LaVessar, P. Facilitating adaptive behaviors in school-aged children with psychosocial problems. In: Case-Smith J., ed. AOTA self-study series: Occupational therapy: Making a difference in school based practice. Bethesda, MD: American Occupational Therapy Association, 1998.
51. Dunn, W. Sensory processing issues associated with Asperger syndrome: A preliminary investigation. Focus on Autism and Other Developmental Disabilities. 2002;56:97–102.
52. Durrant, M. Residential treatment: A cooperative, competency-based approach to therapy and program design. New York: W.W. Norton, 1993.
53. Egeland, B., Sroufe, A., Erickson, M. The developmental consequences of different patterns of maltreatment. Child Abuse and Neglect. 1983;7:459–469.
54. Erker, G., Searight, H.R., Amant, E., White, P. Residential versus day treatment for children: A long-term follow-up study. Child Psychiatry and Human Development. 1993;24:31–39.
55. Feeny, J.A. Attachment, caregiving, and marital satisfaction. Personal Relationships. 1996;3:401–416.
56. Florey, L. Nationally speaking: Treating the whole child: Rhetoric or reality? American Journal of Occupational Therapy. 1989;43:365–368.
57. Florey, L., Greene, S. Play in middle childhood. In: Parham L.D., Fazio L.S., eds. Play in occupational therapy for children. 2nd ed. St. Louis: Mosby; 2008:279–299.
58. Fox, N., Card, J. Walker C.E., Roberts M.C., eds. Handbook of clinical psychology, 3rd ed., New York, John Wiley & Sons, 1999:226–245.
59. Frodi, A. Contribution of child characteristics to child abuse. American Journal of Mental Deficiency. 1981;85:341–345.
60. Fuertes, M., Lopes Dos Santos, P., Beeghly, M., Tronick, E. More than maternal sensitivity shapes attachment: Infant coping and temperament. Annals of the New York Academy of Sciences. 2006;1094:292–296.
61. Gabarino, J., Kostelny, K. Child maltreatment as a community problem. Child Abuse and Neglect. 1992;16:455–464.
62. Galantino, M., Galbavy, R., Quinn, L. Therapeutic effects of yoga for children: A systematic review of the literature. Pediatric Physical Therapy. 2008;20:66–80.
63. Gilbert, B.O., Greening, L., Dollinger, S.J. Neurotic disorders in children: Obsessive-compulsive, somatoform, dissociative, and post-traumatic stress disorders. In: Walker C.E., Roberts M.C., eds. Handbook of clinical psychology. 3rd ed. New York: John Wiley & Sons; 2001:414–431.
64. Gleason, M., Egger, H., Emslie, G., Greenhill, L., Kowatch, R., Lieberman, et al. Pharmacological treatment for very young children: Contexts and guidelines. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1532–1572.
65. Goldstrom, I., Jaiquan, F., Henderson, M., Male, M.A., Manderscheid, R.W. Jail mental health services: A national survey. In: Manderscheid R.W., Henderson M.J., eds. Mental Health, United States, 1998. Washington, DC: U.S. Government Printing Office; 2000:176–187. [DHHS Publication No.SMA-99-3285].
66. Gresham, F., Elliot, S. Social skills intervention guide: Systematic approaches to social skills training. Special Services in the Schools. 1993;8:137–158.
67. Griffin, K.W., Botvin, G.J., Nichols, T.R. Effects of a school-based drug abuse prevention program for adolescents on HIV risk behaviors in young adulthood. Prevention Science. 2006;7:103–112.
68. Harden, P.W., Zoccolillo, M. Disruptive behavior disorders. Current Opinions in Pediatrics. 1997;9:339–345.
69. Harrington, R., Fudge, H., Rutter, M., Pickles, A., Hill, J. Adult outcomes of childhood and adolescent depression I. Archives of General Psychiatry. 1990;47:465–473.
70. Harvard Health Publications. Children’s fears and anxieties. Harvard Mental Health Letter. 2004;21(6):1–4.
71. Harvard Health Publications. In brief: Is the rate of autism rising? Harvard Mental Health Letter. 2005;22(3):6.
72. Harvard Health Publications. Bipolar disorder in children: Difficult to diagnose, important to treat. Harvard Mental Health Letter. 2007;23(11):1–4.
73. Hazan, C., Zeifman, D. Pair bonds as attachments. In: Cassidy J., Shaver P., eds. Handbook of attachment: Theory, research, and clinical applications. New York: Guilford Press; 1999:336–354.
74. Hickman, L., Orentilicher, M. Transition from school to adult life for students with autism. In: Miller-Kuhaneck H., ed. Autism: A comprehensive occupational therapy approach. Bethesda, MD: American Occupational Therapy Association; 2001:237–268.
75. Hilton, C., Graver, K., LaVessar, P. Relationship between social competence and sensory processing in children with high functioning autism spectrum disorders. Research in Autism Spectrum Disorders. 2006;1:164–173.
76. Hoagwood, K., Burnes, B., Kiser, L., Ringeisen, H., Schoenwald, S. Evidence-based practices in child and adolescent mental health services. Psychiatric Services. 2001;52:1179–1189.
77. Hofer, M. Hidden regulators in attachment, separation, and loss. Monographs for the Society for Research in Child Development. 1994;59:192–207. [250-283].
78. Hoffman-Plotkin, D., Twentyman, C. A multimodal assessment of behavioral and cognitive deficits in abused and neglected preschoolers. Child Development. 1984;55:794–802.
79. Humphry, R. Families who live in chronic poverty: Meeting the challenge of family-centered services. American Journal of Occupational Therapy. 1995;49:687–693.
80. Hurley, K., Black, M., Papas, M., Caufield, L. Community and international nutrition: Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. Journal of Nutrition. 2008;138:799–805.
81. IDEAdata.org Data tables for OSEP state reported data, 2008. Retrieved August, 2008, from, https://www.ideadata.org/index.html.
82. Jans, L., Stoddard, S., Kraus, L. Chartbook on mental health and disability in the United States. An InfoUse Report. Washington, DC: U.S. Department of Education, National Institute on Disability and Rehabilitation Research, 2004.
83. Jasinski, J.L., Williams, L.M., Siegel, J. Childhood physical and sexual abuse as a risk factor for heavy drinking among African-American women: A prospective study. Child Abuse and Neglect. 2000;24:1061–1071.
84. Jaudes, P.K., Diamond, L.J. The handicapped child and child abuse. Child Abuse and Neglect. 1985;9:341–347.
85. Johnson, R., Kotch, J., Catellier, D., Winsor, J., Dufort, V., Hunter, W., et al. Adverse behavioral and emotional outcomes from child abuse and witnessed violence. Child Maltreatment. 2002;7:179–186.
86. Jones-Webb, R.J., Snowden, I., Herd, D., Short, B., Hannan, P. Alcohol-related problems among black, Hispanic, and white men: The contributions of neighborhood poverty. Journal of Studies on Alcohol. 1997;58:539–545.
87. Kagan, J., Zentner, M. Early childhood predictors of adult psychopathology. Harvard Review of Psychiatry. 1996;3:341–350.
88. Katic, A., Steingard, R.J. Pharmacotherapy. In: Walker C.E., Roberts M.C., eds. Handbook of clinical psychology. 3rd ed. New York: John Wiley & Sons; 2001:928–951.
89. Kennedy, P., Kupst, M., Westman, G., Zaar, C., Pines, R., Schulman, J. Use of timeout procedures in a child psychiatry inpatient milieu: Combining dynamic and behavioral approaches. Child Psychiatry and Human Development. 1990;20:207–216.
90. Keogh, B.K. Temperament and schooling: Meaning of “goodness of fit”? New Directions in Child Development. 1986;31:89–108.
91. Keogh, B.K., Burstein, N.D. Relationship of temperament to preschoolers’ interactions with peers and teachers. Exceptional Child. 1988;54:456–461.
92. Khalid-Khan, S., Santibanez, M., McMicken, C., Rynn, M. A social anxiety disorder in children and adolescents: Epidemiology, diagnosis, and treatment. Pediatric Drugs. 2007;9:227–237.
93. Knis-Matthews, L., Richard, L., Marquez, L., Mevawala, N. Implementation of occupational therapy services for an adolescent residence program. Occupational Therapy in Mental Health. 2005;21:57–72.
94. Knox, S. A play scale. In: Reilly M., ed. Play as exploratory learning: Studies in curiosity behavior. Beverly Hills, CA: Sage, 1974.
95. Knox, S. Development and current use of the Knox Preschool Play Scale. In: Parham L.D., Fazio L.S., eds. Play in occupational therapy for children. 1st ed. St. Louis: Mosby; 1997:35–51.
96. Knox, S. Development and current use of the Revised Knox Preschool Play Scale. In: Parham L.D., Fazio L.S., eds. Play in occupational therapy for children. 2nd ed. St. Louis: Mosby; 2008:55–70.
97. Kolko, D.J. Child physical abuse. In Myers J.E.B., Berliner L., Briere J., Hendrix C.T., Jenny C., et al, eds.: The APSAC handbook on child maltreatment, 2nd ed., Thousand Oaks, CA: Sage, 2002.
98. Kolko, D., Bukstein, O., Barron, J. Methylphenidate and behavior modification in children with ADHD and co-morbid ODD or CD: Main and incremental effects across settings. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:578–586.
99. Kovacs, M., Feinberg, T.L., Crouse-Novak, M.A., Paulauskas, S.L., Finkelstein, R. Depressive disorders in childhood. I. Archives of General Psychiatry. 1984;41:229–237.
100. Kovacs, M., Feinberg, T.L., Crouse-Novak, M.A., Paulauskas, S.L., Finkelstein, R. Depressive disorders in childhood. II. Archives of General Psychiatry. 1984;41:643–649.
101. Kraemer, G. A psychobiological theory of attachment. Behavioral and Brain Sciences. 1992;15:493–541.
102. Landolf, B. Out-patient private practice model. In: Steele R., Roberts M., eds. Handbook of mental health services for children, adolescents, and families. New York: Kluwer Academic/Plenum Publishers, 2005.
103. Lang, A., Aarons, G., Gearity, J., Laffaye, C., Satz, L., Dresselhaus, T., et al. Direct links between child maltreatment, posttraumatic stress disorder, and women’s health. Behavioral Medicine. 2008;33:125–135.
104. Lansford, J., Miller-Johnson, S., Berlin, L., Dodge, K., Bates, J., Pettit, G. Early physical abuse and later violent delinquency: A prospective longitudinal study. Child Maltreatment. 2007;12:233–245.
105. Law, M., Baptiste, S., Carswell, A., McColl, M., Polatajko, H., Pollack, N. The Canadian Occupational Performance Measure (revised). Ottawa, Ontario: Canadian Association of Occupational Therapy, 2005.
106. Law, M., Cooper, B., Strong, S., Stewart, D., Rigby, P., Letts, L. The person-environment-occupation model: A transactive approach to occupational performance. Canadian Journal of Occupational Therapy. 1996;63:9–23.
107. Leary, M.R., Kowalski, R.M. Social anxiety. New York: Guilford Press, 1995.
108. Locke, A., Ginsborg, J., Peers, I. Development and disadvantage: Implications for the early years and beyond. International Journal of Language and Communication Disorders. 2003;37:3–15.
109. Lourie, I. A history of community child mental health. In: Pumariega A., Winters N., eds. Handbook of community-based systems of care: The new child and adolescent community psychiatry. New York: Jossey-Bass, 2003.
110. Maag, J.W., Katsiyannis, A. Counseling as a related service for students with emotional or behavioral disorders: Issues and recommendations. Behavioral Disorders. 1996;21:293–305.
111. Maag, J., Katsiyannis, A. Challenges facing successful transition for youths with E/BD. Behavioral Disorders. 1998;23:209–221.
112. Macro International, Inc. Annual report to congress on the evaluation of the comprehensive community mental health services for children and their families program, 1997. [Atlanta, Georgia].
113. MacLeod, J., Nelson, G. Programs for the promotion of family wellness and the prevention of child maltreatment: A meta-analytic review. Child Abuse and Neglect. 2000;24:1127–1149.
114. Mailloux, Z., Roley, S.S. Sensory integration. In: Miller-Kuhaneck H., ed. Autism: A comprehensive occupational therapy approach. Bethesda, MD: American Occupational Therapy Association, 2001.
115. Main, M. Attachment: Overview, with implications for clinical work. In: Goldberg S., Muir R., Kerr J., eds. Attachment theory: Social, developmental, and clinical perspectives. Hillsdale, NJ: Analytic Press; 1995:407–474.
116. Main, M. Overview of the field of attachment. Journal of Consulting and Clinical Psychology. 1996;64:237–243.
117. Main, M., Solomon, J. Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation. In: Greenberg M.T., Cicchetti D., Cummings E.M., eds. Attachment in the preschool years: Theory, research, and intervention. Chicago: University of Chicago Press; 1990:121–160.
118. Manderscheid, R.W., Sonnenschein, M.A. Mental health, United States, 1992. Washington, DC: US Government Printing Office, 1992. [DHSS Publication No. ADM 92-1942].
119. Martin, K., Lloyd, J., Kauffman, J., Coyne, M. Teachers’ perceptions of educational placement decisions for pupils with emotional and behavioral disorders. Behavioral Disorders. 1995;20:106–117.
120. Masi, Hawkley, L., Piotrowski, Z., Pickett, K. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Social Science in Medicine. 2007;65:2440–2457.
121. McLoyd, V.C. The impact of economic hardship on black families and children: Psychological distress, parenting, and socioemotional development. Child Development. 1990;61:311–346.
122. Miller, L. Miller Function and Participation Scales (M-FUN). New York: Harcourt, 2006.
123. Milliken, B., Goodman, G., Bazyk, S., Flinn, S. Establishing a case for occupational therapy in meeting the needs of children with grief issues in school-based settings. Occupational Therapy in Mental Health. 2007;23:75–100.
124. Milling, L.S. Depression in preadolescents. In: Walker C.E., Roberts M.C., eds. Handbook of clinical psychology. 3rd ed. New York: John Wiley & Sons; 2001:373–392.
125. Moller, B. A grieving child. The ASCA School Counselor. 2001;39:14–17.
126. National Board for Certification in Occupational Therapy Executive summary for the practice analysis study, 2008. Retrieved September 2008, from, http://www.nbcot.org.
127. National Institutes of Mental Health Autism spectrum disorders: Pervasive developmental disorders (addendum January 2007), 2007. Retrieved August, 2008, from, http://www.nimh.nih.gov/health/publications/autism/complete-publication.shtml.
128. Nelson, R., Condrin, J. A vocational readiness and independent living skills program for psychiatrically impaired adolescents. Occupational Therapy in Mental Health. 1987;7:105–113.
129. Nigg, J., Goldsmith, H. Developmental psychopathology, personality, and temperament: Reflections on recent behavioral genetics research. Human Biology. 1998;70(2):387–412.
130. Office of Special Education and Rehabilitation Services, U.S. Department of Education 25th annual report to congress on the implementation of the individuals with disabilities education act, 2005. Retrieved September 20, 2008, from, http://www.ed.gov/about/reports/annual/osep/2003/25th-vol-1.pdf.
131. Ogata, S., Silk, K., Goodrich, S., Lohr, N., Westen, D., Hill, E. Childhood sexual and physical abuse in adult patients with borderline personality disorder. American Journal of Psychiatry. 1990;147:1008–1013.
132. Olfson, M., Blanco, C., Liu, L., Moreno, C., Laje, G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Archives of General Psychiatry. 2006;63:679–685.
133. Olson, L. Activity groups in family-centered treatment: psychiatric occupational therapy approaches for parents and children. New York: Haworth Press, 2006.
134. Orentlicher, M.L., Olson, L.J. Transition from school to adult life for students with autism. In Miller-Kuhaneck H., ed.: Autism: A comprehensive occupational therapy approach, 2nd ed., Bethesda, MD: American Occupational Therapy Association, 2004.
135. Peloquin, S. The patient-therapist relationship: Beliefs that shape care. American Journal of Occupational Therapy. 1993;47:935–942.
136. Pfefferbaum, B. Posttraumatic stress disorder in children: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1503–1511.
137. Pickens, J., Field, T. Facial expressivity in infants of depressed mothers. Developmental Psychology. 1993;29:986–988.
138. Pottick, K., McAlpine, D., Andelman, R. Changing patterns of psychiatric inpatient care for children and adolescents in general hospitals, 1988-1995. American Journal of Psychiatry. 2000;157:1267–1273.
139. Powers, S.W. Behavior therapy with children. In: Walker C.E., Roberts M.C., eds. Handbook of clinical psychology. 3rd ed. New York: John Wiley & Sons, Inc; 2001:4825–4839.
140. Prothro-Stith, D. Deadly consequences: How violence is destroying our teenage population and a plan to begin solving the problem. New York: Harper Collins, 1991.
141. Pruitt, D., Kiser, L. Day treatment: Past, present, and future. In: Lewis M., ed. Child and adolescent psychiatry: A comprehensive textbook. Baltimore: Williams & Wilkins, 1991.
142. Richardson, P. The school as social context: Social interaction patterns of children with physical disabilities. American Journal of Occupational Therapy. 2002;56:296–304.
143. Robinson, K., Rapport, L. Outcomes of a school-based mental health program for youth with serious emotional disorders. Psychology in the Schools. 2002;3:661–676.
144. Rothbart, M.K. Temperament: A developmental framework. In: Strelau J., Angleitner A., eds. Explorations in temperament: International perspectives on theory and measurement. London: Plenum Press; 1991:2235–2260.
145. Rothe, E.M., Castellanos, D. Anxiety disorders in children and adolescents. In: Vance H.B., Pumariega A.J., eds. Clinical assessment of child and adolescent behavior. New York: John Wiley & Sons; 2001:383–412.
146. Sabatino, D.A., Webster, B., Vance, H.B. Childhood mood disorders: History, characteristics, diagnosis, and treatment. In: Vance H.B., Pumariega A.J., eds. Clinical assessment of child and adolescent behavior. New York: John Wiley & Sons; 2001:413–449.
147. Schultz, S. School-based occupational therapy for students with behavioral disorders. Occupational Therapy in Health Care. 1992;8:173–196.
148. Schultz, S. AOTA continuing education article: Psychosocial occupational therapy in schools. OT Practice. 2003. [September 2003, CE-1-CE-8].
149. Sidebotham, P., Golding, J. Avon longitudinal study of parents and children. Child Abuse and Neglect. 2001;25:1177–1200.
150. Sidebotham, P., Herson, J. Child maltreatment in the “children of the nineties”: A cohort study of risk factors. Child Abuse and Neglect. 2006;30:497–522.
151. Silverman, W.K., Ginsberg, G.S. Anxiety disorders. In: Ollendick T.H., Hersen M., eds. Handbook of child psychopathology. 3rd ed. New York: Plenum Press; 1998:239–268.
152. Skard, G., Bundy, A. Test of Playfulness. In: Parham L.D., Fazio L.S., eds. Play in occupational therapy for children. 2nd ed. St. Louis: Mosby; 2008:71–91.
153. Spencer, N., Wallace, A., Sundrum, R., Bachus, C., Logan, S. Child abuse registration, fetal growth, and preterm birth: A population based study. Journal of Epidemiology and Community Health. 2006;60:337–340.
154. Sperry, L. Handbook of diagnosis and treatment of DSM-IV-TR personality disorders, 2nd ed. New York: Brunner-Routledge, 2003.
155. Spreat, S., Jampol, R. Residential services for children and adolescents. In: Ammerman R.T., Hersen M., eds. Intervention in the real world context: Handbook of prevention and treatment with children and adolescents. New York: John Wiley & Sons; 1997:106–133.
156. Stein, F. Residential treatment of adolescents and children: Issues, principles, and techniques. Chicago: Nelson-Hall Publishers, 1995.
157. Sullivan, P.M., Knutson, J.F. Maltreatment and disabilities: A population-based epidemiological study. Child Abuse and Neglect. 2000;24:1257–1273.
158. Thomas, A., Chess, S., Birch, H. Temperament and behavior disorders in children. New York: New York University Press, 1968.
159. Thompson, R. The view from research: The roots of school readiness in social and emotional development. The Kauffman Early Education Exchange. 2002;1(1):8–29.
160. Thomsen, P., Mikkelsen, H. Course of OCD in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1432–1440.
161. Townsend, S., Carey, P., Hollins, N., Helfrich, C., Blondis, M., Hoffman, A., et al. Occupational therapy psychosocial assessment of learning. Chicago: Model of Occupational Therapy Products, 2001.
162. Trieschman, A., Whittaker, J., Brendtro, J. The other 23 hours: Child-care work with emotionally disturbed children in a therapeutic milieu. Chicago: Aldine Publishing Company, 1969.
163. Tuma, J. Mental health services for children: The state of the art. American Psychologist. 1989;44:188–199.
164. DeNavas-Walt, C., Proctor, B., Lee, C. Income, Poverty, and health insurance coverage in the United States. U.S. Census Bureau, 2006.
165. U.S. Department of Health and Human Services Comprehensive community mental health services program for children and their families, 2004. Retrieved September 20, 2008, from, http://mentalhealth.samhsa.gov/publications/allpubs/Ca-0013/default.asp.
166. U.S. Department of Health and Human Services, Administration on Children, Youth and Families Child maltreatment 2006, Washington, DC, U.S. Government Printing Office, 2006. Retrieved September 15, 2008, from, http://www.acf.hhs.gov/programs/cb/stats_research/index.htm#can.
167. U.S. Public Health Service Mental health: A report of the Surgeon General, 1999. Retrieved May, 2009, from, http://www.surgeongeneral.gov/library/mentalhealth/home.html.
168. van den Boom, D. Preventive intervention and the quality of mother-infant interaction and infant exploration in irritable infants. In: Koops W., Soppe H.J.G., van der Linden J.L., Molenaar P.C.M., Schroots J.J.F., eds. Developmental psychology behind the dikes: An outline of developmental psychology research in the Netherlands. Amsterdam: Eburon; 1990:249–270.
169. van IJzendoorn, M., Juffer, F., Duyvesteyn, M. Breaking the intergenerational cycle of insecure attachment: A review of the effects of attachment-based interventions on maternal sensitivity and infant security. Journal of Child Psychology and Psychiatry. 1995;36:225–248.
170. VanderVen, K. Point and level systems”: Another way to fail children and youth. Child and Youth Care Forum. 1995;24:345–367.
171. Vaughn, B.R., Bost, K.K. Attachment and temperament: redundant, independent, or interactive influences on interpersonal adaptation and personality development? In: Cassidy J., Shaver P., eds. Handbook of attachment: Theory, research, and clinical applications. New York: Guilford Press; 1999:198–225.
172. Vaughn, S., Kim, A., Sloan, C., Hughes, M., Elbaum, B., Spridhaur, D. Social skills interventions for young children with disabilities: A synthesis of group design studies. Remedial and Special Education. 2003;24:2–15.
173. Verdugo, M.A., Bermejo, B.G., Fuertes, J. The maltreatment of intellectually handicapped children and adolescents. Child Abuse and Neglect. 1995;19:205–215.
174. Vondra, J.I. Sociological and ecological factors. In: Ammerman R.T., Hersen M., eds. Children at risk: An evaluation of factors contributing to child abuse and neglect. New York: Plenum Press; 1990:149–165.
175. Wagner, M.M. Outcomes for youths with serious emotional disturbance in secondary school and early adulthood. Future Child. 1995;5(2):90–112.
176. Wald, R.L., Knutson, J.F. Childhood disciplinary experiences reported by adults with craniofacial anomalies. Child Abuse and Neglect. 2000;24:1623–1627.
177. Walker, R., Bunsen, T. After high school: The status of youth with emotional and behavioral disorders. Career Development of Exceptional Individuals. 1995;18:97–107.
178. Waters, E., Stroufe, A. Social competence as a developmental construct. Developmental Review. 1983;3:79–97.
179. Weinberg, N., Rahdert, E., Colliver, J., Glantz, M. Adolescent substance abuse: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(3):252–261.
180. Williams, M., Shellengerger, S. How does your engine run? A leader’s guide to the ALERT program for self-regulation. Therapy Works: Albequerque, NM, 1996.
181. Williamson, G. Enhancing the social competence of children with learning disabilities. Sensory Integration Special Interest Section Newsletter. 1993;16:1–2.
182. Willis, C. The grieving process in children: Strategies for understanding, educating, and reconciling children’s perceptions of death. Early Childhood Education Journal. 2002;29:221–226.
183. Winters, N., Pumariega, A. Practice parameter on child and adolescent mental health care in community systems of care. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:284–299.
184. Wolfner, G., Gelles, R. A profile of violence toward children: A national study. Child Abuse and Neglect. 1993;17:197–212.
185. Zametin, A.J., Ernst, M. Review article: Problems in the management of attention-deficit-hyperactivity disorder. New England Journal of Medicine. 1999;340(1):40–46.
 CASE STUDY 13-1
CASE STUDY 13-1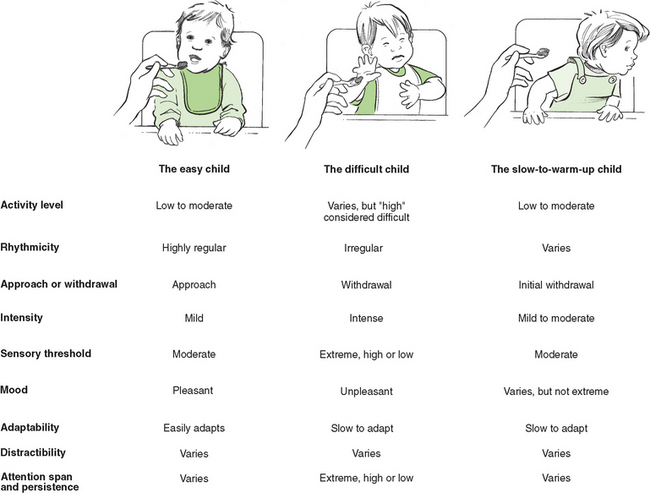
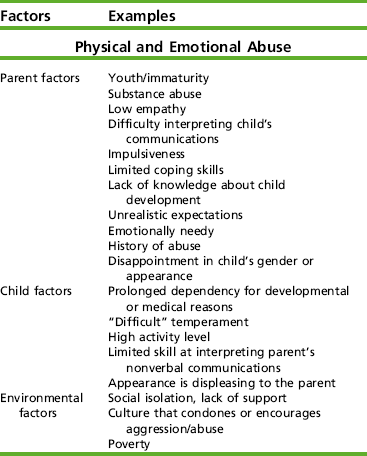
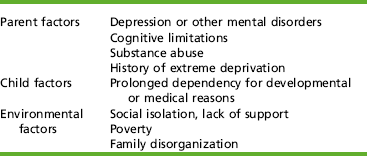
 CASE STUDY 13-2
CASE STUDY 13-2 CASE STUDY 13-3
CASE STUDY 13-3 CASE STUDY 13-4
CASE STUDY 13-4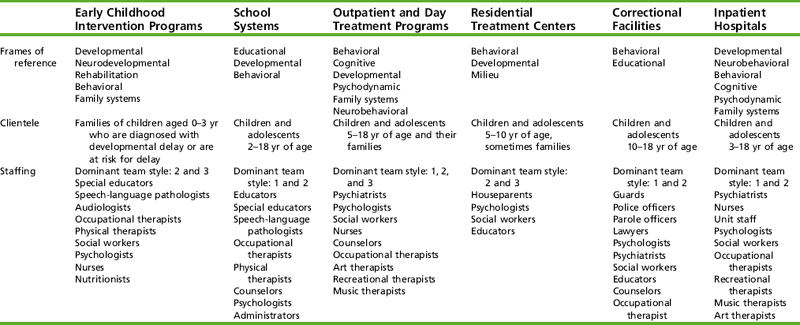
 CASE STUDY 13-5
CASE STUDY 13-5 CASE STUDY 13-6
CASE STUDY 13-6 CASE STUDY 13-7
CASE STUDY 13-7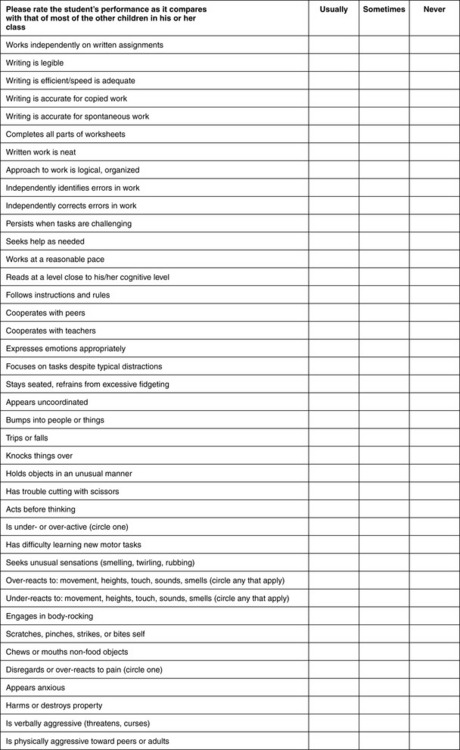
 RESEARCH NOTE 13-1
RESEARCH NOTE 13-1 CASE STUDY 13-8
CASE STUDY 13-8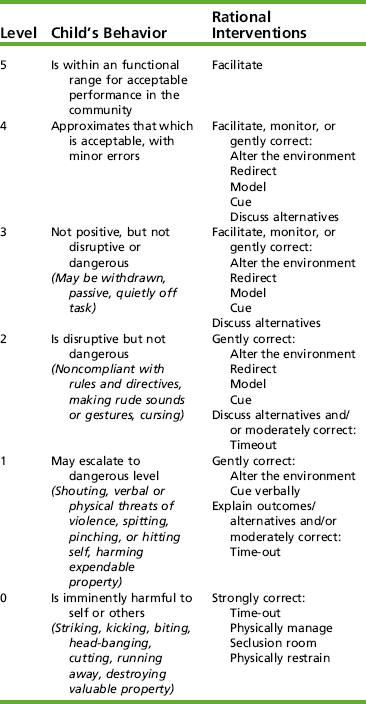
 CASE STUDY 13-9
CASE STUDY 13-9