Labor and Birth Processes
• Explain the five major factors that affect the labor process.
• Describe the anatomic structure of the bony pelvis.
• Recognize the normal measurements of the diameters of the pelvic inlet, cavity, and outlet.
• Explain the significance of the size and position of the fetal head during labor and birth.
• Summarize the cardinal movements of the mechanism of labor for a vertex presentation.
• Examine the maternal anatomic and physiologic adaptations to labor.
• Describe factors thought to contribute to the onset of labor.
During late pregnancy a woman and fetus prepare for the labor process. The fetus has grown and developed in preparation for extrauterine life. The woman has undergone various physiologic adaptations during pregnancy that prepare her for birth and motherhood. Labor and birth represent the end of pregnancy, the beginning of extrauterine life for the newborn, and a change in the lives of the family. This chapter discusses the factors affecting labor, the process involved, the normal progression of events, and the adaptations made by both the woman and fetus.
Factors Affecting Labor
At least five factors affect the process of labor and birth. These are easily remembered as the five P’s: passenger (fetus and placenta), passageway (birth canal), powers (contractions), position of the mother, and psychologic response. The first four factors are presented here as the basis of understanding the physiologic process of labor. The fifth factor is discussed in Chapter 17. Other factors that may be a part of the woman’s labor experience may be important as well. VandeVusse (1999) identified external forces including place of birth, preparation, type of provider (especially nurses), and procedures. Physiology (sensations) was identified as an internal force. These factors are discussed generally in Chapter 19 as they relate to nursing care during labor. Further research investigating essential forces of labor is recommended.
Passenger
The way the passenger, or fetus, moves through the birth canal is determined by several interacting factors: the size of the fetal head, fetal presentation, fetal lie, fetal attitude, and fetal position. Because the placenta also must pass through the birth canal, it can be considered a passenger along with the fetus; however, the placenta rarely impedes the process of labor in normal vaginal birth, except in cases of placenta previa.
Size of the Fetal Head
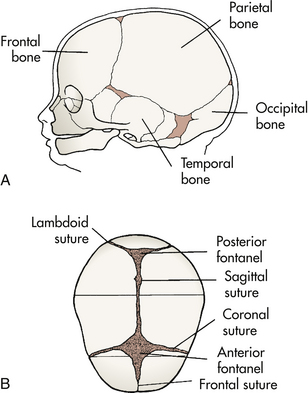
Because of its size and relative rigidity, the fetal head has a major effect on the birth process. The fetal skull is composed of two parietal bones, two temporal bones, the frontal bone, and the occipital bone (Fig. 16-1, A). These bones are united by membranous sutures: sagittal, lambdoidal, coronal, and frontal (see Fig. 16-1, B). Membrane-filled spaces called fontanels are located where the sutures intersect. During labor, after rupture of membranes, palpation of fontanels and sutures during vaginal examination reveals fetal presentation, position, and attitude.
The anterior and posterior fontanels are the two most important (see Fig. 16-1, B). The larger of these, the anterior fontanel, is diamond shaped, is about 3 cm by 2 cm, and lies at the junction of the sagittal, coronal, and frontal sutures. It closes by 18 months after birth. The posterior fontanel lies at the junction of the sutures of the two parietal bones and the occipital bone, is triangular, and is about 1 cm by 2 cm. It closes 6 to 8 weeks after birth.
Sutures and fontanels make the skull flexible to accommodate the infant brain, which continues to grow for some time after birth. However, because the bones are not firmly united, slight overlapping of the bones, or molding of the shape of the head, occurs during labor. This capacity of the bones to slide over one another also permits adaptation to the various diameters of the maternal pelvis. Molding can be extensive, but the heads of most newborns assume their normal shape within 3 days after birth.
Although the size of the fetal shoulders may affect passage, their position can be altered relatively easily during labor, so one shoulder may occupy a lower level than the other. This creates a shoulder diameter that is smaller than the skull, facilitating passage through the birth canal. The circumference of the fetal hips is usually small enough not to create problems.
Fetal Presentation
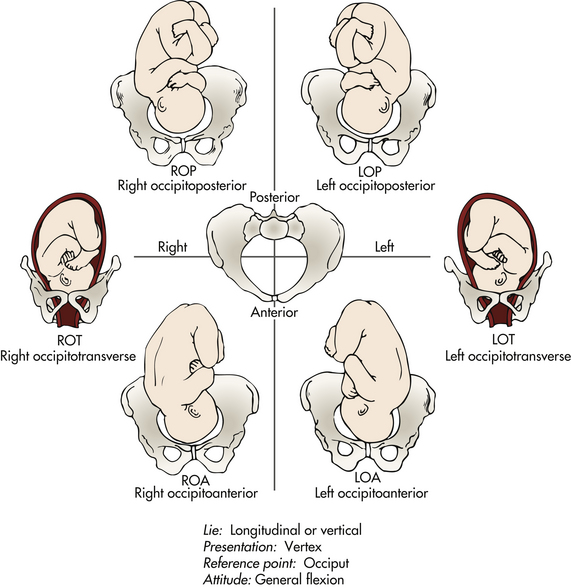
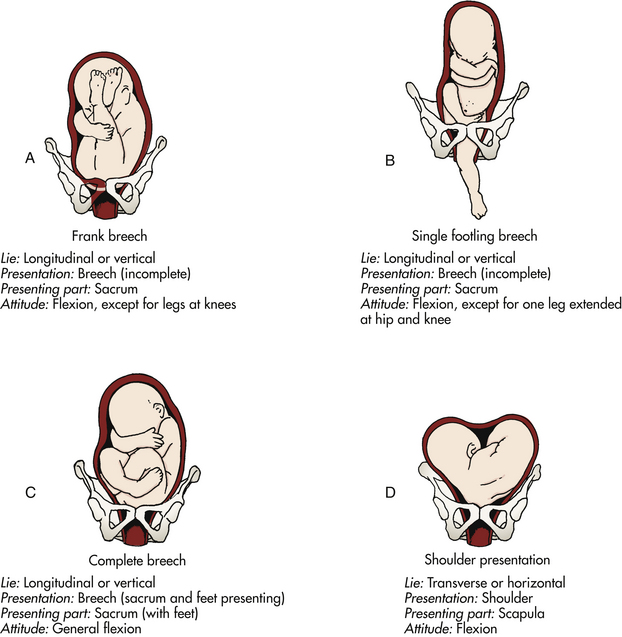
Presentation refers to the part of the fetus that enters the pelvic inlet first and leads through the birth canal during labor. The three main presentations are cephalic presentation (head first), occurring in 96% of births (Fig. 16-2); breech presentation (buttocks, feet, or both first), occurring in 3% of births (Fig. 16-3, A-C); and shoulder presentation, seen in 1% of births (see Fig. 16-3, D). The presenting part is that part of the fetus that lies closest to the internal os of the cervix. It is the part of the fetal body first felt by the examining finger during a vaginal examination. In a cephalic presentation the presenting part is usually the occiput; in a breech presentation it is the sacrum; in the shoulder presentation it is the scapula. When the presenting part is the occiput, the presentation is noted as vertex (see Fig. 16-2). Factors that determine the presenting part include fetal lie, fetal attitude, and extension or flexion of the fetal head.
Fetal Lie
Lie is the relation of the long axis (spine) of the fetus to the long axis (spine) of the mother. The two primary lies are longitudinal, or vertical, in which the long axis of the fetus is parallel with the long axis of the mother (see Fig. 16-2); and transverse, horizontal, or oblique, in which the long axis of the fetus is at a right angle diagonal to the long axis of the mother (see Fig. 16-3, D). Longitudinal lies are either cephalic or breech presentations, depending on the fetal structure that first enters the mother’s pelvis. Vaginal birth cannot occur when the fetus stays in a transverse lie. An oblique lie, one in which the long axis of the fetus is lying at an angle to the long axis of the mother, is less common and usually converts to a longitudinal or transverse lie during labor (Cunningham, Leveno, Bloom, Hauth, Rouse, & Spong, 2010).
Fetal Attitude
Attitude is the relation of the fetal body parts to each other. The fetus assumes a characteristic posture (attitude) in utero partly because of the mode of fetal growth and partly because of the way the fetus conforms to the shape of the uterine cavity. Normally the back of the fetus is rounded so that the chin is flexed on the chest, the thighs are flexed on the abdomen, and the legs are flexed at the knees. The arms are crossed over the thorax, and the umbilical cord lies between the arms and the legs. This attitude is termed general flexion (see Fig. 16-2).
Deviations from the normal attitude may cause difficulties in childbirth. For example, in a cephalic presentation, the fetal head may be extended or flexed in a manner that presents a head diameter that exceeds the limits of the maternal pelvis, leading to prolonged labor, forceps or vacuum-assisted birth, or cesarean birth.
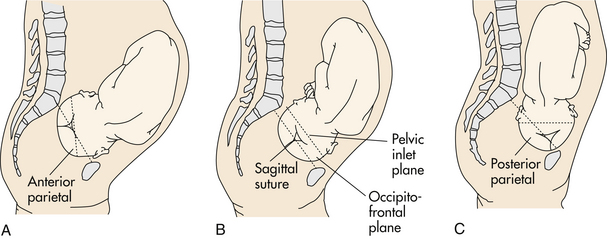
Certain critical diameters of the fetal head are usually measured. The biparietal diameter, which is about 9.25 cm at term, is the largest transverse diameter and an important indicator of fetal head size (Fig. 16-4, B). In a well-flexed cephalic presentation, the biparietal diameter is the widest part of the head entering the pelvic inlet. Of the several anteroposterior diameters, the smallest and the most critical one is the suboccipitobregmatic diameter (about 9.5 cm at term). When the head is in complete flexion, this diameter allows the fetal head to pass through the true pelvis easily (see Fig. 16-4, A; Fig. 16-5, A). As the head is more extended, the anteroposterior diameter widens, and the head may not be able to enter the true pelvis (see Fig. 16-5, B and C).
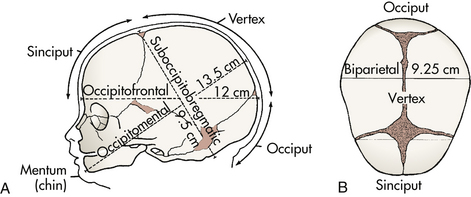
FIG. 16-4 Diameters of the fetal head at term. A, Cephalic presentations: occiput, vertex, and sinciput; and cephalic diameters: suboccipitobregmatic, occipitofrontal, and occipitomental. B, Biparietal diameter.
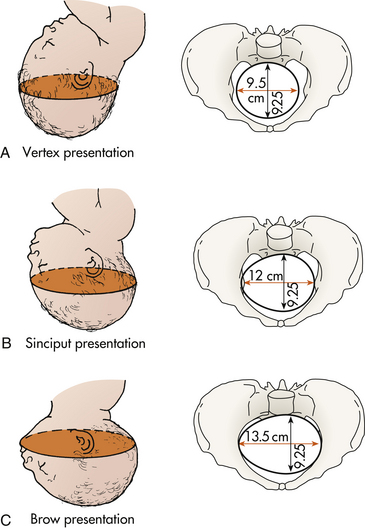
FIG. 16-5 Head entering pelvis. Biparietal diameter is indicated with shading (9.25 cm). A, Suboccipitobregmatic diameter: complete flexion of head on chest so that smallest diameter enters. B, Occipitofrontal diameter: moderate extension (military attitude) so that large diameter enters. C, Occipitomental diameter: marked extension (deflection), so that the largest diameter, which is too large to permit head to enter pelvis, is presenting.
Fetal Position
The presentation or presenting part indicates that portion of the fetus that overlies the pelvic inlet. Position is the relationship of a reference point on the presenting part (occiput, sacrum, mentum [chin], or sinciput [deflexed vertex]) to the four quadrants of the mother’s pelvis (see Fig. 16-2). Position is denoted by a three-part abbreviation. The first letter of the abbreviation denotes the location of the presenting part in the right (R) or left (L) side of the mother’s pelvis. The middle letter(s) stands for the specific presenting part of the fetus (O for occiput, S for sacrum, M for mentum [chin], and Sc for scapula [shoulder]). The final letter stands for the location of the presenting part in relation to the anterior (A), posterior (P), or transverse (T) portion of the maternal pelvis. For example, ROA means that the occiput is the presenting part and is located in the right anterior quadrant of the maternal pelvis (see Fig. 16-2). LSP means that the sacrum is the presenting part and is located in the left posterior quadrant of the maternal pelvis (see Fig. 16-3).
Station is the relationship of the presenting fetal part to an imaginary line drawn between the maternal ischial spines and is a measure of the degree of descent of the presenting part of the fetus through the birth canal. The placement of the presenting part is measured in centimeters above or below the ischial spines (Fig. 16-6). For example, when the lowermost portion of the presenting part is 1 cm above the spines, it is noted as being minus (−) 1. At the level of the spines, the station is said to be 0 (zero). When the presenting part is 1 cm below the spines, the station is said to be plus (+) 1. Birth is imminent when the presenting part is at +4 to +5 cm. The station of the presenting part should be determined when labor begins so that the rate of descent of the fetus during labor can be accurately determined.
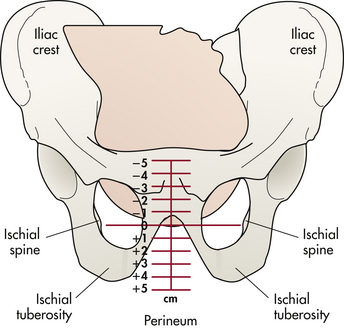
FIG. 16-6 Stations of presenting part, or degree of descent. The lowermost portion of the presenting part is at the level of the ischial spines, station 0.
Engagement is the term used to indicate that the largest transverse diameter of the presenting part (usually the biparietal diameter) has passed through the maternal pelvic brim or inlet into the true pelvis and usually corresponds to station 0. Engagement often occurs in the weeks just before labor begins in nulliparas and may occur before labor or during labor in multiparas. Engagement can be determined by abdominal or vaginal examination.
Passageway
The passageway, or birth canal, is composed of the mother’s rigid bony pelvis and the soft tissues of the cervix, the pelvic floor, the vagina, and the introitus (the external opening to the vagina). Although the soft tissues, particularly the muscular layers of the pelvic floor, contribute to vaginal birth of the fetus, the maternal pelvis plays a far greater role in the labor process because the fetus must successfully accommodate itself to this relatively rigid passageway. The determination of the size and shape of the pelvis can be done at the initial prenatal visit or on admission in labor. This information can then be used in the assessment of labor progress (Thorp 2009).
Bony Pelvis
The anatomy of the bony pelvis is described in Chapter 4. The following discussion focuses on the importance of pelvic configurations as they relate to the labor process. (It may be helpful to refer to Fig. 4-4.)
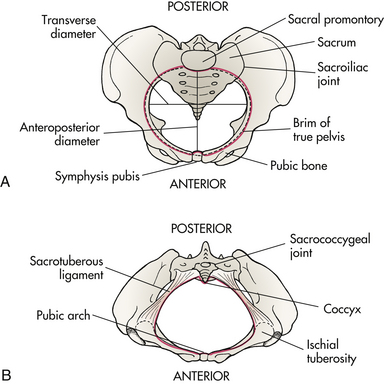
The bony pelvis is formed by the fusion of the ilium, the ischium, the pubis, and the sacral bones. The four pelvic joints are the symphysis pubis, the right and left sacroiliac joints, and the sacrococcygeal joint (Fig. 16-7, A). The bony pelvis is separated by the brim, or inlet, into two parts: the false pelvis and the true pelvis. The false pelvis is the part above the brim and plays no part in childbearing. The true pelvis, the part involved in birth, is divided into three planes: the inlet, or brim; the midpelvis, or cavity; and the outlet.
The pelvic inlet, which is the upper border of the true pelvis, is formed anteriorly by the upper margins of the pubic bone, laterally by the iliopectineal lines along the innominate bones, and posteriorly by the anterior, upper margin of the sacrum and the sacral promontory.
The pelvic cavity, or midpelvis, is a curved passage with a short anterior wall and a much longer concave posterior wall. It is bounded by the posterior aspect of the symphysis pubis, the ischium, a portion of the ilium, the sacrum, and the coccyx.
The pelvic outlet is the lower border of the true pelvis. Viewed from below it is ovoid, somewhat diamond shaped, and bounded by the pubic arch anteriorly, the ischial tuberosities laterally, and the tip of the coccyx posteriorly (see Fig. 16-7, B). In the latter part of pregnancy the coccyx is movable (unless it has been broken in a fall during skiing or skating, for example, and has fused to the sacrum during healing).
The pelvic canal varies in size and shape at various levels. The diameters at the plane of the pelvic inlet, midpelvis, and outlet, plus the axis of the birth canal (Fig. 16-8), determine whether vaginal birth is possible and the manner by which the fetus may pass down the birth canal.
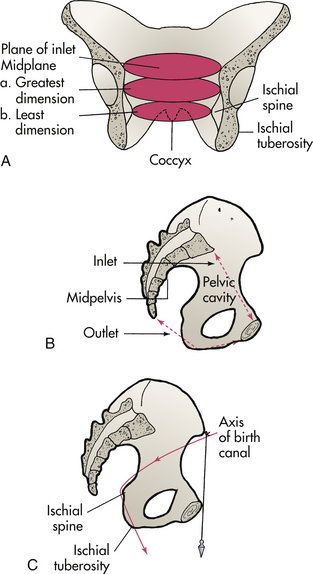
FIG. 16-8 Pelvic cavity. A, Inlet and midplane. Outlet not shown. B, Cavity of true pelvis. C, Note curve of sacrum and axis of birth canal.
The subpubic angle, which determines the type of pubic arch, together with the length of the pubic rami and the intertuberous diameter, is of great importance. Because the fetus must first pass beneath the pubic arch, a narrow subpubic angle will be less accommodating than a rounded, wide arch. The method of measurement of the subpubic arch is shown in Fig. 16-9. A summary of obstetric measurements is given in Table 16-1.
TABLE 16-1
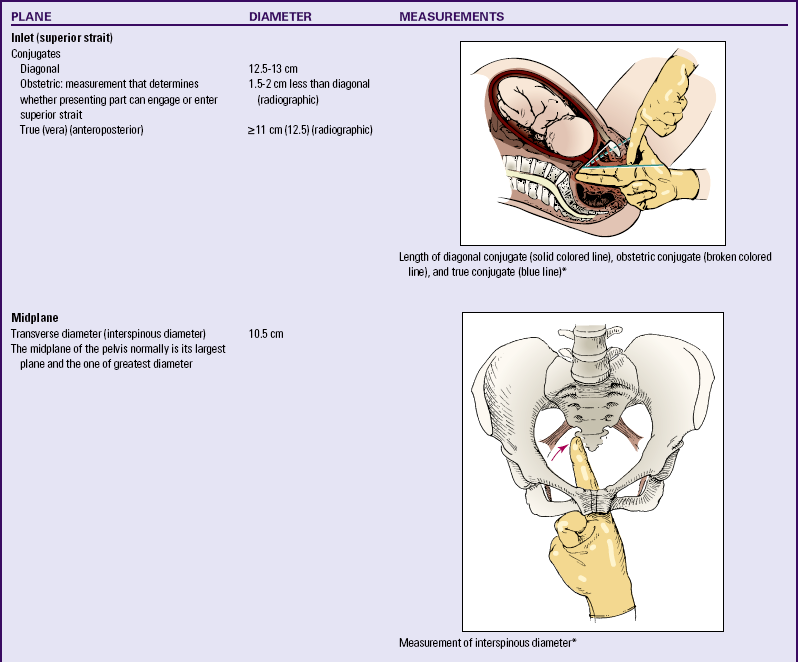
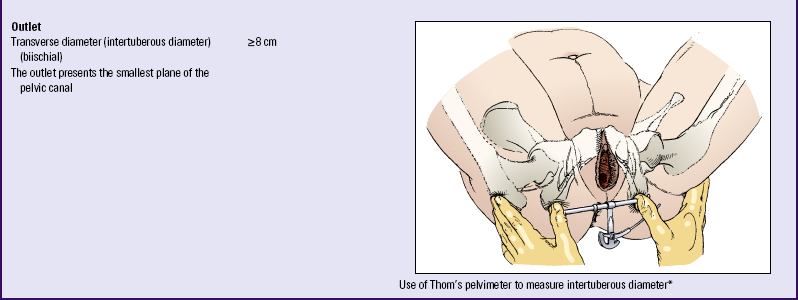
∗From Seidel, H., Ball, J., Dains, J., Flynn, J., Solomon, B., and Stewart, R. (2011). Mosby’s guide to physical examination (7th ed.). St. Louis: Mosby.

FIG. 16-9 Estimation of angle of subpubic arch. With both thumbs, examiner externally traces descending rami down to tuberosities. (From Barkauskas, V., Baumann, L., & Darling-Fisher, C. [2002]. Health and physical assessment [3rd ed.]. St. Louis: Mosby.)
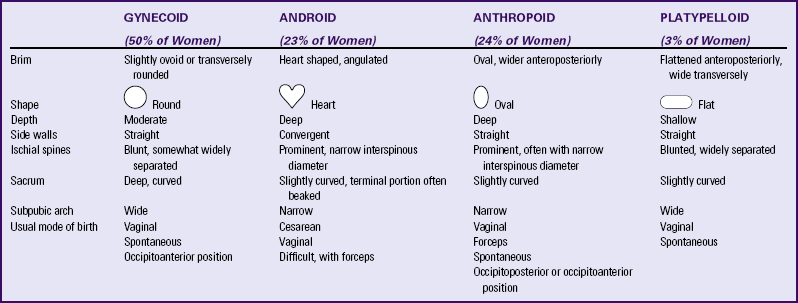
The four basic types of pelvis are classified as follows:
1. Gynecoid (the classic female type)
2. Android (resembling the male pelvis)
The gynecoid pelvis is the most common, with major gynecoid pelvic features present in 50% of all women. Anthropoid and android features are less common, and platypelloid pelvic features are the least common. Mixed types of pelves are more common than are pure types (Cunningham et al., 2010). Examples of pelvic variations and their effects on mode of birth are given in Table 16-2.
Assessment of the bony pelvis can be performed during the first prenatal evaluation and need not be repeated if the pelvis is of adequate size and suitable shape. In the third trimester of pregnancy, the examination of the bony pelvis may be more thorough and the results more accurate because there is relaxation and increased mobility of the pelvic joints and ligaments owing to hormonal influences. Widening of the joint of the symphysis pubis and the resulting instability may cause pain in any or all of the pelvic joints.
Because the examiner does not have direct access to the bony structures and because the bones are covered with varying amounts of soft tissue, size and shape are estimated. Precise bony pelvis measurements can be determined by use of computed tomography, ultrasound, or x-ray films. However, radiographic examination is rarely done during pregnancy because the x-rays may damage the developing fetus.
Soft Tissues
The soft tissues of the passageway include the distensible lower uterine segment, the cervix, the pelvic floor muscles, the vagina, and the introitus. Before labor begins, the uterus is composed of the uterine body (corpus) and the cervix (neck). After labor has begun, uterine contractions cause the uterine body to have a thick and muscular upper segment and a thin-walled, passive, muscular lower segment. A physiologic retraction ring separates the two segments (Fig. 16-10). The lower uterine segment gradually distends to accommodate the intrauterine contents as the wall of the upper segment thickens and its accommodating capacity is reduced. The contractions of the uterine body thus exert downward pressure on the fetus, pushing it against the cervix.
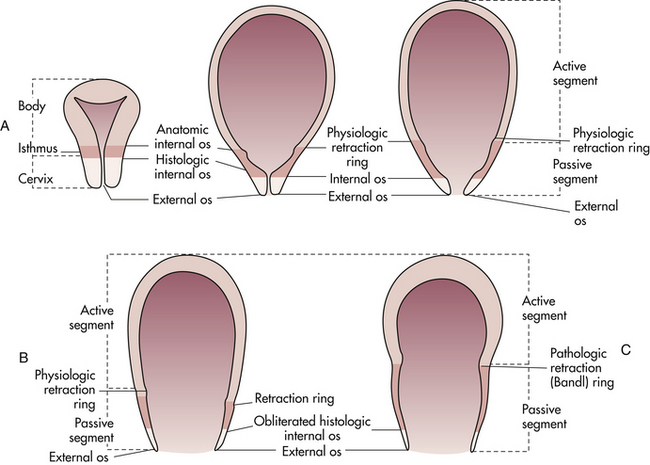
FIG. 16-10 A, Uterus in normal labor in early first stage, and B, in second stage. Passive segment is derived from lower uterine segment (isthmus) and cervix, and physiologic retraction ring is derived from anatomic internal os. C, Uterus in abnormal labor in second-stage dystocia. Pathologic retraction (Bandl) ring that forms under abnormal conditions develops from the physiologic ring.
The cervix effaces (thins) and dilates (opens) sufficiently to allow the first fetal portion to descend into the vagina. As the fetus descends, the cervix is actually drawn upward and over this first portion.
The pelvic floor is a muscular layer that separates the pelvic cavity above from the perineal space below. This structure helps the fetus rotate anteriorly as it passes through the birth canal. As noted, the soft tissues of the vagina develop throughout pregnancy until at term the vagina can dilate to accommodate the fetus and permit passage of the fetus to the external world.
Powers
Involuntary and voluntary powers combine to expel the fetus and the placenta from the uterus. Involuntary uterine contractions, called the primary powers, signal the beginning of labor. Once the cervix has dilated, voluntary bearing-down efforts by the woman, called the secondary powers, augment the force of the involuntary contractions.
Primary Powers
The involuntary contractions originate at certain pacemaker points in the thickened muscle layers of the upper uterine segment. From the pacemaker points, contractions move downward over the uterus in waves, separated by short rest periods. Terms used to describe these involuntary contractions include frequency (the time from the beginning of one contraction to the beginning of the next), duration (length of contraction), and intensity (strength of contraction at its peak).
The primary powers are responsible for the effacement and dilation of the cervix and descent of the fetus. Effacement of the cervix means the shortening and thinning of the cervix during the first stage of labor. The cervix, normally 2 to 3 cm long and about 1 cm thick, is obliterated or “taken up” by a shortening of the uterine muscle bundles during the thinning of the lower uterine segment that occurs in advancing labor. Only a thin edge of the cervix can be palpated when effacement is complete. Effacement generally is advanced in first-time term pregnancy before more than slight dilation occurs. In subsequent pregnancies, effacement and dilation of the cervix tend to progress together. Degree of effacement is expressed in percentages from 0% to 100% (e.g., a cervix is 50% effaced) (Fig. 16-11, A-C).
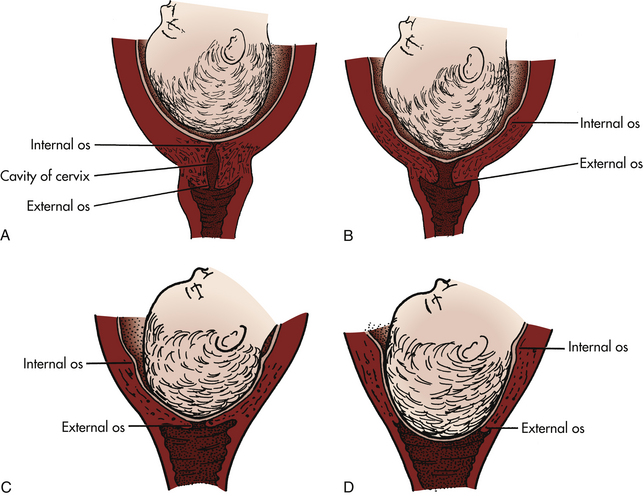
FIG. 16-11 Cervical effacement and dilation. Note how cervix is drawn up around presenting part (internal os). Membranes are intact, and head is not well applied to cervix. A, Before labor. B, Early effacement. C, Complete effacement (100%). Head is well applied to cervix. D, Complete dilation (10 cm). Cranial bones overlap somewhat, and membranes are still intact.
Dilation of the cervix is the enlargement or widening of the cervical opening and the cervical canal that occurs once labor has begun. The diameter of the cervix increases from less than 1 cm to full dilation (approximately 10 cm) to allow birth of a term fetus. When the cervix is fully dilated (and completely retracted), it can no longer be palpated (see Fig. 16-11, D). Full cervical dilation marks the end of the first stage of labor.
Dilation of the cervix occurs by the drawing upward of the musculofibrous components of the cervix, caused by strong uterine contractions. Pressure exerted by the amniotic fluid while the membranes are intact or by the force applied by the presenting part also can promote cervical dilation. Scarring of the cervix as a result of prior infection or surgery may slow cervical dilation.
In the first and second stages of labor, increased intrauterine pressure caused by contractions exerts pressure on the descending fetus and the cervix. When the presenting part of the fetus reaches the perineal floor, mechanical stretching of the cervix occurs. Stretch receptors in the posterior vagina cause release of endogenous oxytocin that triggers the maternal urge to bear down, or the Ferguson reflex.
Uterine contractions are usually independent of external forces. For example, laboring women who are paralyzed because of spinal cord lesions above the twelfth thoracic vertebra will have normal but painless uterine contractions (Cunningham et al., 2010). However, uterine contractions may decrease temporarily in frequency and intensity if narcotic analgesic medication is given early in labor. Studies of effects of epidural analgesia have demonstrated prolonged length of labor for nulliparas both in the active phase of first-stage labor and in the second stage (Salim, Nachum, Moscovici, Lavee, & Shalev, 2005; Schiessl, Janni, Jundt, Rammel, Peschers, & Kainer, 2005).
Secondary Powers
As soon as the presenting part reaches the pelvic floor, the contractions change in character and become expulsive. The laboring woman experiences an involuntary urge to push. She uses secondary powers (bearing-down efforts) to aid in expulsion of the fetus as she contracts her diaphragm and abdominal muscles and pushes. These bearing-down efforts result in increased intraabdominal pressure that compresses the uterus on all sides and adds to the power of the expulsive forces.
The secondary powers have no effect on cervical dilation, but they are of considerable importance in the expulsion of the infant from the uterus and vagina after the cervix is fully dilated. Studies have shown that pushing in the second stage is more effective and the woman is less fatigued when she begins to push only after she has the urge to do so rather than beginning to push when she is fully dilated without an urge to do so (Jacobson & Turner, 2008; Simpson & James, 2005; Yildirim & Beji, 2008).
When and how a woman pushes in the second stage is a much-debated topic. Studies have investigated the effects of spontaneous bearing-down efforts, directed pushing, delayed pushing, Valsalva maneuver (closed glottis and prolonged bearing down), and open-glottis pushing both with and without epidural analgesia (Brancato, Church, & Stone, 2008; Gupta, Hofmeyr, & Smyth, 2004; Simpson & James, 2005). The benefits of delayed pushing include an increased chance of spontaneous vaginal birth and decreased pushing time. Adverse effects associated with prolonged breath holding and forceful pushing efforts include increased fetal hypoxia and subsequent acidosis (Simpson & James). Pelvic floor problems also have been associated with directed pushing (Schaffer, Bloom, Casey, McIntire, Nihira, & Leveno, 2005). Continued study is needed to determine the effectiveness and appropriateness of strategies used by nurses to teach pushing techniques, the suitability and effectiveness of various pushing techniques related to abnormal (nonreassuring) fetal heart patterns, and the standards for length of duration of pushing in terms of maternal and fetal outcomes (Gennaro, Mayberry, & Kafulafula, 2007). (See Chapter 19 for further discussion.)
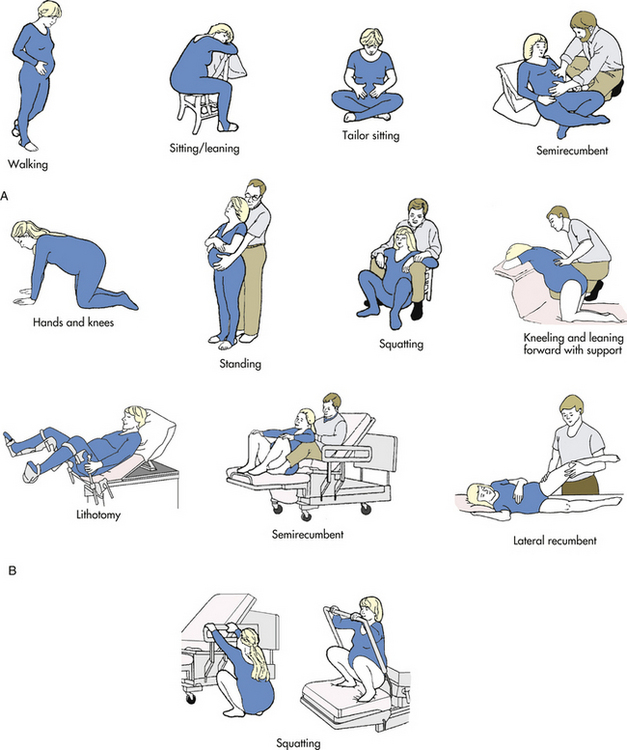
Position of the Laboring Woman
Position affects the woman’s anatomic and physiologic adaptations to labor. Frequent changes in position relieve fatigue, increase comfort, and improve circulation. Therefore, a laboring woman should be encouraged to find positions that are most comfortable for her (Fig. 16-12, A).
An upright position (walking, sitting, kneeling, or squatting) offers a number of advantages. Gravity can promote the descent of the fetus. Uterine contractions are generally stronger and more efficient in effacing and dilating the cervix, resulting in a shorter labor (Gupta et al., 2004; Lawrence, Lewis, Hofmeyr, Dowswell, & Styles, 2009; Zwelling, 2010).
An upright position also is beneficial to the mother’s cardiac output, which normally increases during labor as uterine contractions return blood to the vascular bed. The increased cardiac output improves blood flow to the uteroplacental unit and the maternal kidneys. Cardiac output is compromised if the descending aorta and ascending vena cava are compressed during labor (see Fig. 19-5). Compression of these major vessels may result in supine hypotension that decreases placental perfusion. With the woman in an upright position, pressure on the maternal vessels is reduced, and compression is prevented. If the woman wishes to lie down, a lateral position is suggested (Blackburn, 2007; Zwelling, 2010).
The “all fours” position (hands and knees) may be used to relieve backache if the fetus is in an occipitoposterior position and may assist in anterior rotation of the fetus and in cases of shoulder dystocia (Hunter, Hofmeyr & Kulier, 2007; Zwelling, 2010).
Positioning for second-stage labor (see Fig. 16-12, B) may be determined by the woman’s preference, but it is constrained by the condition of the woman and fetus, the environment, and the health care provider’s confidence in assisting with a birth in a specific position. The predominant position in the United States in physician-attended births is the lithotomy position. Alternative positions and position changes that result in more births over an intact perineum are more commonly practiced by nurse-midwives.
A woman who pushes in a semirecumbent position needs adequate body support to push effectively because her weight will be on her sacrum, moving the coccyx forward and causing a reduction in the pelvic outlet. In a sitting or squatting position, abdominal muscles work in greater synchrony with uterine contractions during bearing-down efforts. Kneeling or squatting moves the uterus forward and aligns the fetus with the pelvic inlet and can facilitate the second stage of labor by increasing the pelvic outlet (Simpson, Cesario, Morin, Trapani, Mayberry, & Snelgrove-Clark, 2008; Zwelling, 2010).
The lateral position can be used by the woman to help rotate a fetus that is in a posterior position. It also can be used when there is a need for less force to be used during bearing down, such as when there is a need to control the speed of a precipitate birth (Simpson et al., 2008; Zwelling, 2010).
No evidence exists that any of these positions suggested for second-stage labor increases the need for use of operative techniques (e.g., forceps or vacuum-assisted birth, cesarean birth, episiotomy) or causes perineal trauma. No evidence has been found that use of any of these positions adversely affects the newborn (Lawrence et al., 2009; Roberts, Algert, Cameron, & Torvaldsen, 2005).
Process of Labor
The term labor refers to the process of moving the fetus, placenta, and membranes out of the uterus and through the birth canal. Various changes take place in the woman’s reproductive system in the days and weeks before labor begins. Labor itself can be discussed in terms of the mechanisms involved in the process and the stages the woman moves through.
Signs Preceding Labor
In first-time pregnancies the uterus sinks downward and forward about 2 weeks before term, when the fetus’s presenting part (usually the fetal head) descends into the true pelvis. This settling is called lightening, or “dropping,” and usually happens gradually. After lightening, women feel less congested and breathe more easily, but usually more bladder pressure results from this shift, and consequently a return of urinary frequency occurs. In a pregnancy in a multiparous woman, lightening may not take place until after uterine contractions are established and true labor is in progress.
The woman may complain of persistent low backache and sacroiliac distress as a result of relaxation of the pelvic joints. She may identify strong and frequent but irregular uterine (Braxton Hicks) contractions.
The vaginal mucus becomes more profuse in response to the extreme congestion of the vaginal mucous membranes. The thick mucus that has obstructed the cervical canal since conception is passed (commonly referred to as the mucous plug). Brownish or blood-tinged cervical mucus may be passed (bloody show). The cervix becomes soft (ripens) and partially effaced and may begin to dilate. The membranes may rupture spontaneously.
Other phenomena are common in the days preceding labor: (1) loss of 0.5 to 1.5 kg in weight, caused by water loss resulting from electrolyte shifts that in turn are produced by changes in estrogen and progesterone levels; and (2) a surge of energy. Women speak of having a burst of energy that they often use to clean the house and put everything in order. Less commonly, some women have diarrhea, nausea, vomiting, and indigestion. Box 16-1 lists signs that may precede labor.
Onset of Labor
The onset of true labor cannot be ascribed to a single cause. Many factors, including changes in the maternal uterus, cervix, and pituitary gland, are involved. Hormones produced by the normal fetal hypothalamus, pituitary, and adrenal cortex probably contribute to the onset of labor. Progressive uterine distention, increasing intrauterine pressure, and aging of the placenta seem to be associated with increasing myometrial irritability. This is a result of increased concentrations of estrogen and prostaglandins, as well as decreasing progesterone levels. The mutually coordinated effects of these factors result in the occurrence of strong, regular, rhythmic uterine contractions (Kilpatrick & Garrison, 2007). The outcome of these factors working together is normally the birth of the fetus and the expulsion of the placenta; however, how certain alterations trigger others and how proper checks and balances are maintained is not known.
Stages of Labor
The course of labor at or near term gestation in a woman without complications and a fetus in vertex presentation consists of: (1) regular progression of uterine contractions, (2) effacement and progressive dilation of the cervix, and (3) progress in descent of the presenting part. Four stages of labor are recognized. An overview of these stages is discussed here. These stages are discussed in greater detail, along with nursing care for the laboring woman and family, in Chapter 19.
The first stage of labor is considered to last from the onset of regular uterine contractions to full effacement and dilation of the cervix. Commonly the onset of labor is difficult to establish because the woman may be admitted to the labor unit just before birth, and the beginning of labor may be only an estimate. The first stage is much longer than the second and third stages combined. Great variability is the rule, however, depending on the factors discussed previously in this chapter. Parity has a strong effect on the duration of first-stage labor (Gross, Drobnic, & Keirse, 2005). Full dilation may occur in less than 1 hour in some multiparous pregnancies. In first-time pregnancy, complete dilation of the cervix can take 20 hours or more. Variations may reflect differences in the client population (e.g., risk status, age) or in clinical management of the labor and birth.
The first stage of labor is divided into three phases: a latent phase, an active phase, and a transition phase. During the latent phase there is more progress in effacement of the cervix and little increase in descent. During the active phase and the transition phase, there is more rapid dilation of the cervix and increased rate of descent of the presenting part. Maternal prepregnancy overweight and obesity can cause the active phase of labor to be longer than for women of normal weight; specifically arrest of dilation can occur (Liao, Buhimschi, & Norwitz, 2005; Verdiales, Pacheco, & Cohen, 2009).
The second stage of labor lasts from the time the cervix is fully effaced and dilated to the birth of the fetus. The second stage takes an average of 20 minutes for a multiparous woman and 50
minutes for a nulliparous woman. Labor of up to 2 hours (up to 3 hours with use of regional anesthesia) has been considered within the normal range for the second stage, but Cesario (2004) found a wider range of normal was associated with no adverse effects on the mother or infant. Ethnicity may play a role in length of second-stage labor. Greenberg and associates (2006) found that nulliparous Asian women had a longer second stage than nulliparous Caucasian women, whereas African-American and Hispanic women had shorter second stages of labor than Caucasian women.
The second stage of labor is composed of two phases: the latent phase and the active pushing (descent) phase. During the latent phase the fetus continues to descend passively through the birth canal and rotate to an anterior position as a result of ongoing uterine contractions. The urge to bear down during this phase is not strong and some women do not experience it at all. During the active pushing phase the woman has strong urges to bear down as the presenting part of the fetus descends and presses on the stretch receptors of the pelvic floor.
The third stage of labor lasts from the birth of the fetus until the placenta is delivered. The placenta normally separates with the third or fourth strong uterine contraction after the infant has been born. After it has separated the placenta can be delivered with the next uterine contraction. The placenta is usually expelled within 10 to 15 minutes after birth of the baby. The third stage of labor is normally completed within 30 minutes. The risk of hemorrhage increases as the length of the third stage increases (Battista & Wing, 2007).
The fourth stage of labor arbitrarily lasts 1 to 2 hours after delivery of the placenta. It is the period of immediate recovery, when homeostasis is reestablished. It is an important period of observation for complications, such as abnormal bleeding (see Chapter 19).
Mechanism of Labor
As discussed, the female pelvis has varied contours and diameters at different levels, and the presenting part of the passenger is large in proportion to the passage. Therefore, for vaginal birth to occur, the fetus must adapt to the birth canal during the descent. The turns and other adjustments necessary in the human birth process are termed the mechanism of labor (Fig. 16-13). The seven cardinal movements of the mechanism of labor that occur in a vertex presentation are engagement, descent, flexion, internal rotation, extension, external rotation (restitution), and finally birth by expulsion. Although these movements are discussed separately, in actuality a combination of movements occurs simultaneously. For example, engagement involves both descent and flexion.
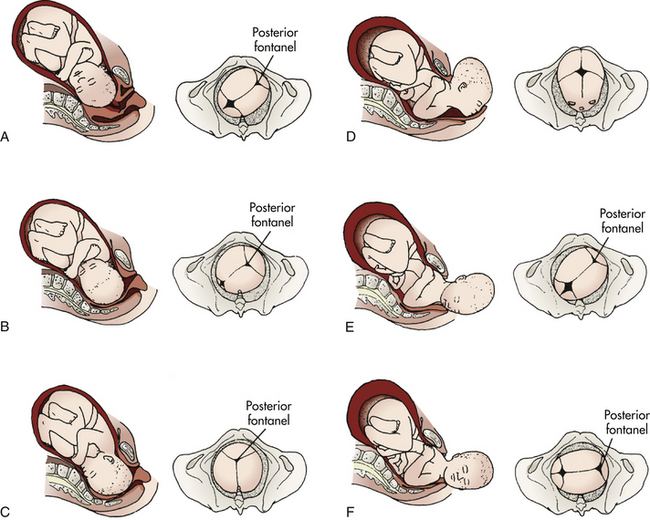
FIG. 16-13 Cardinal movements of the mechanism of labor. Left occipitoanterior (LOA) position. Pelvic figures show the position of the fetal head as seen by the birth attendant. A, Engagement and descent. B, Flexion. C, Internal rotation to occipitoanterior position (OA). D, Extension. E, External rotation beginning (restitution). F, External rotation.
Engagement
When the biparietal diameter of the head passes the pelvic inlet, the head is said to be engaged in the pelvic inlet (see Fig. 16-13, A). In most nulliparous pregnancies, this occurs before the onset of active labor because the firmer abdominal muscles direct the presenting part into the pelvis. In multiparous pregnancies, in which the abdominal musculature is more relaxed, the head often remains freely movable above the pelvic brim until labor is established.
Asynclitism: The head usually engages in the pelvis in a synclitic position—one that is parallel to the anteroposterior plane of the pelvis. Frequently asynclitism occurs (the head is deflected anteriorly or posteriorly in the pelvis), which can facilitate descent because the head is being positioned to accommodate to the pelvic cavity (Fig. 16-14). Extreme asynclitism can cause cephalopelvic disproportion, even in a normal-size pelvis, because the head is positioned so that it cannot descend.
Descent
Descent refers to the progress of the presenting part through the pelvis. Descent depends on at least four forces: (1) pressure exerted by the amniotic fluid, (2) direct pressure exerted by the contracting fundus on the fetus, (3) force of the contraction of the maternal diaphragm and abdominal muscles in the second stage of labor, and (4) extension and straightening of the fetal body. The effects of these forces are modified by the size and shape of the maternal pelvic planes and the size of the fetal head and its capacity to mold.
The degree of descent is measured by the station of the presenting part (see Fig. 16-6). As mentioned, little descent occurs during the latent phase of the first stage of labor. Descent accelerates in the active phase when the cervix has dilated to 4 to 7 cm. It is especially apparent when the membranes have ruptured.
In a first-time pregnancy descent is usually slow but steady; in subsequent pregnancies descent may be rapid. Progress in descent of the presenting part is determined by abdominal palpation (Leopold maneuvers) and vaginal examination until the presenting part can be seen at the introitus (see Chapter 19).
Flexion
As soon as the descending head meets resistance from the cervix, pelvic wall, or pelvic floor, it normally flexes, so that the chin is brought into closer contact with the fetal chest (see Fig. 16-13, B). Flexion permits the smaller suboccipitobregmatic diameter (9.5 cm) rather than the larger diameters to present to the outlet.
Internal Rotation
The maternal pelvic inlet is widest in the transverse diameter; therefore the fetal head passes the inlet into the true pelvis in the occipitotransverse position. The outlet is widest in the anteroposterior diameter; for the fetus to exit, the head must rotate. Internal rotation begins at the level of the ischial spines but is not completed until the presenting part reaches the lower pelvis. As the occiput rotates anteriorly, the face rotates posteriorly. With each contraction the fetal head is guided by the bony pelvis and the muscles of the pelvic floor. Eventually the occiput will be in the midline beneath the pubic arch. The head is almost always rotated by the time it reaches the pelvic floor (see Fig. 16-13, C). Both the levator ani muscles and the bony pelvis are important for achieving anterior rotation. A previous childbirth injury or regional anesthesia may compromise the function of the levator sling.
Extension
When the fetal head reaches the perineum for birth, it is deflected anteriorly by the perineum. The occiput passes under the lower border of the symphysis pubis first, and then the head emerges by extension: first the occiput, then the face, and finally the chin (see Fig. 16-13, D).
Restitution and External Rotation
After the head is born it rotates briefly to the position it occupied when it was engaged in the inlet. This movement is referred to as restitution (see Fig. 16-13, E). The 45-degree turn realigns the infant’s head with her or his back and shoulders. The head can then be seen to rotate further. This external rotation occurs as the shoulders engage and descend in maneuvers similar to those of the head (see Fig. 16-13, F). As noted, the anterior shoulder descends first. When it reaches the outlet, it rotates to the midline and is delivered from under the pubic arch. The posterior shoulder is guided over the perineum until it is free of the vaginal introitus.
Physiologic Adaptation to Labor
In addition to the maternal and fetal anatomic adaptations that occur during birth, physiologic adaptations must occur. Accurate assessment of the laboring woman and fetus requires knowledge of these expected adaptations.
Fetal Adaptation
Several important physiologic adaptations occur in the fetus. These changes occur in fetal heart rate, fetal circulation, respiratory movements, and other behaviors.
Fetal Heart Rate
Fetal heart rate (FHR) monitoring provides reliable and predictive information about the condition of the fetus related to oxygenation. The average FHR at term is 140 beats/min. The normal range is 110 to 160 beats/min. Earlier in gestation the FHR is higher, with an average of approximately 160 beats/min at 20 weeks of gestation. The rate decreases progressively as the maturing fetus reaches term. However, temporary accelerations and slight early decelerations of the FHR can be expected in response to spontaneous fetal movement, vaginal examination, fundal pressure, uterine contractions, abdominal palpation, and fetal head compression. Stresses to the uterofetoplacental unit result in characteristic FHR patterns (see Chapter 18 for further discussion).
Fetal Circulation
Fetal circulation can be affected by many factors, including maternal position, uterine contractions, blood pressure, and umbilical cord blood flow. Uterine contractions during labor tend to decrease circulation through the spiral arterioles and subsequent perfusion through the intervillous space. Most healthy fetuses are well able to compensate for this stress and exposure to increased pressure while moving passively through the birth canal during labor. Usually umbilical cord blood flow is undisturbed by uterine contractions or fetal position (Tucker, Miller, & Miller, 2009).
Fetal Respiration
Certain changes stimulate chemoreceptors in the aorta and carotid bodies to prepare the fetus for initiating respirations immediately after birth (Blackburn, 2007; Rosenberg, 2007). These changes occur during labor and include the following:
Maternal Adaptation
As the woman progresses through the stages of labor, various body system adaptations cause her to exhibit both objective signs and subjective symptoms (Box 16-2).
Cardiovascular Changes
During each contraction an average of 400 mL of blood is emptied from the uterus into the maternal vascular system. This increases cardiac output by about 12% to 31% in the first stage and by about 50% in the second stage of labor. The heart rate increases slightly (Gordon, 2007).
Changes in blood pressure also occur. Blood flow, which is reduced in the uterine artery by contractions, is redirected to peripheral vessels. As a result, peripheral resistance increases, and blood pressure increases (Gordon, 2007). During the first stage of labor, uterine contractions cause systolic readings to increase by about 10 mm Hg; assessing blood pressure between contractions therefore provides more accurate readings. During the second stage contractions may cause systolic pressures to increase by 30 mm Hg and diastolic readings to increase by 25 mm Hg, with both systolic and diastolic pressures remaining somewhat elevated even between contractions (Gordon). Therefore, the woman already at risk for hypertension is at increased risk for complications such as cerebral hemorrhage.
Supine hypotension (see fig. 19-5, p. 444) occurs when the ascending vena cava and descending aorta are compressed. The laboring woman is at greater risk for supine hypotension if the uterus is particularly large because of multifetal pregnancy, hydramnios, or obesity or if the woman is dehydrated or hypovolemic. In addition, anxiety and pain, as well as some medications, can cause hypotension.
The woman should be discouraged from using the Valsalva maneuver (holding one’s breath and tightening abdominal muscles) for pushing during the second stage. This activity increases intrathoracic pressure, reduces venous return, and increases venous pressure. The cardiac output and blood pressure increase and the pulse slows temporarily. During the Valsalva maneuver fetal hypoxia may occur. The process is reversed when the woman takes a breath.
The white blood cell (WBC) count can increase (Blackburn, 2007). Although the mechanism leading to this increase in WBCs is unknown, it may be secondary to physical or emotional stress or to tissue trauma. Labor is strenuous, and physical exercise alone can increase the WBC count.
Some peripheral vascular changes occur, perhaps in response to cervical dilation or to compression of maternal vessels by the fetus passing through the birth canal. Flushed cheeks, hot or cold feet, and eversion of hemorrhoids may result.
Respiratory Changes
Increased physical activity with greater oxygen consumption is reflected in an increase in the respiratory rate. Hyperventilation may cause respiratory alkalosis (an increase in pH), hypoxia, and hypocapnia (decrease in carbon dioxide). In the unmedicated woman in the second stage of labor, oxygen consumption almost doubles. Anxiety also increases oxygen consumption.
Renal Changes
During labor, spontaneous voiding may be difficult for various reasons: tissue edema caused by pressure from the presenting part, discomfort, analgesia, and embarrassment. Proteinuria of 1+ is a normal finding because it can occur in response to the breakdown of muscle tissue from the physical work of labor.
Integumentary Changes
The integumentary system changes are evident, especially in the great distensibility (stretching) in the area of the vaginal introitus. The degree of distensibility varies with the individual. Despite this ability to stretch, even in the absence of episiotomy or lacerations, minute tears in the skin around the vaginal introitus do occur.
Musculoskeletal Changes
The musculoskeletal system is stressed during labor. Diaphoresis, fatigue, proteinuria (1+), and possibly an increased temperature accompany the marked increase in muscle activity. Backache and joint aches (unrelated to fetal position) occur as a result of increased joint laxity at term. The labor process itself and the woman’s pointing her toes can cause leg cramps.
Neurologic Changes
Sensorial changes occur as the woman moves through the phases of the first stage of labor and as she moves from one stage to the next. Initially she may be euphoric. Euphoria gives way to increased seriousness, then to amnesia between contractions during the second stage, and finally to elation or fatigue after giving birth. Endogenous endorphins (morphine-like chemicals produced naturally by the body) raise the pain threshold and produce sedation. In addition, physiologic anesthesia of perineal tissues, caused by pressure of the presenting part, decreases perception of pain.
Gastrointestinal Changes
During labor, gastrointestinal motility and absorption of solid foods are decreased, and stomach-emptying time is slowed. Nausea and vomiting of undigested food eaten after onset of labor are common. Nausea and belching also occur as a reflex response to full cervical dilation. The woman may state that diarrhea accompanied the onset of labor, or the nurse may palpate the presence of hard or impacted stool in the rectum.
Endocrine Changes
The onset of labor may be triggered by decreasing levels of progesterone and increasing levels of estrogen, prostaglandins, and oxytocin (Norwitz & Lye, 2009). Metabolism increases, and blood glucose levels may decrease with the work of labor.
Accurate assessment of the mother and fetus during labor and birth depends on knowledge of these expected adaptations so that appropriate interventions can be implemented.
KEY POINTS
• Labor and birth are affected by the five P’s: passenger, passageway, powers, position of the woman, and psychologic responses.
• Because of its size and relative rigidity, the fetal head is a major factor in determining the course of birth.
• The diameters at the plane of the pelvic inlet, the midpelvis, and the outlet, plus the axis of the birth canal, determine whether vaginal birth is possible and the manner in which the fetus passes down the birth canal.
• Involuntary uterine contractions act to expel the fetus and placenta during the first stage of labor; these are augmented by voluntary bearing-down efforts of the woman during the second stage.
• The first stage of labor lasts from the time dilation begins to the time when the cervix is fully effaced and dilated.
• The second stage of labor lasts from the time of full cervical effacement and dilation to the birth of the infant.
• The third stage of labor lasts from the infant’s birth to the expulsion of the placenta.
• The fourth stage is the first 1 to 2 hours after birth.
• The cardinal movements of the mechanism of labor are engagement, descent, flexion, internal rotation, extension, restitution and external rotation, and expulsion of the infant.
• Although the events precipitating the onset of labor are unknown, many factors, including changes in the maternal uterus, cervix, and pituitary gland, are thought to be involved.
• A healthy fetus with an adequate uterofetoplacental circulation will be able to compensate for the stress of uterine contractions.
• As the woman progresses through labor, various body systems adapt to the birth process.
![]() Audio Chapter Summaries Access an audio summary of these Key Points on
Audio Chapter Summaries Access an audio summary of these Key Points on ![]()