Nursing Care of the Family During Labor and Birth
• Review the factors included in the initial assessment of the woman in labor.
• Describe the ongoing assessment of maternal progress during the first, second, third, and fourth stages of labor.
• Recognize the physical and psychosocial findings indicative of maternal progress during labor.
• Describe fetal assessment during labor.
• Identify signs of developing complications during labor and birth.
• Incorporate evidence-based nursing interventions into a comprehensive plan of care relevant to each stage of labor.
• Recognize the importance of support (family, partner, doula, nurse) in fostering maternal confidence and facilitating the progress of labor and birth.
• Analyze the influence of cultural and religious beliefs and practices on the process of labor and birth.
• Describe the role and responsibilities of the nurse during emergency childbirth.
• Evaluate the effect of perineal trauma on the woman’s reproductive and sexual health.
![]() http://evolve.elsevier.com/Lowdermilk/MWHC/
http://evolve.elsevier.com/Lowdermilk/MWHC/
Animation
Audio Glossary
Case Studies
NCLEX Review Questions
Video—Assessment
Video—Childbirth
Video—Nursing Skills
The labor process is an exciting and anxious time for the woman and her significant others (support persons, family). In a relatively short period they experience one of the most profound changes in their lives.
For most women labor begins with the first uterine contraction, continues with hours of hard work during cervical dilation and birth, and ends as the woman begins to recover physically from birth and she and her significant others begin the attachment process with the newborn. Nursing care management focuses on assessment and support of the woman and her significant others throughout labor and birth, with the goal of ensuring the best possible outcome for all involved.
A woman often has lingering impressions of her childbirth experience. Satisfaction with childbirth hinges on her ability to maintain a sense of control. Caregivers who encourage a woman to be actively involved in decision making and who are respectful, supportive, protective, patient, and calm help the woman to remember her childbirth experience in positive terms. Other factors cited by women as influencing their satisfaction with their childbirth experience include degree of awareness of what is occurring, support from their partner, being together with their baby immediately after birth, type of birth (e.g., vaginal or emergency cesarean birth), and degree to which expectations were met and pain was managed (Bryanton, Gagnon, Johnston, & Hatem, 2008). A satisfactory view of childbirth contributes to a woman’s self-esteem and sense of accomplishment with her performance. Adaptation to her role as a mother may also be enhanced.
Frustrations a woman feels regarding her childbirth experience generally stem from factors such as unmet expectations, poorly managed pain, loss of control, lack of knowledge, or the negative behaviors of some caregivers. A woman who perceives her childbirth to be unsatisfactory or traumatic could be at risk for postpartum depression, posttraumatic stress disorder (PTSD), low self-esteem, impaired attachment with the newborn, and fear leading to no further pregnancies or cesarean birth for a subsequent pregnancy (Bryanton et al., 2008). It is critical that nurses recognize the factors that influence maternal satisfaction as they plan care for women and their families during childbirth.
First Stage of Labor
The first stage of labor begins with the onset of regular uterine contractions and ends with full cervical effacement and dilation. The first stage of labor consists of three phases: the latent phase (through 3 cm of dilation), the active phase (4 to 7 cm of dilation), and the transition phase (8 to 10 cm of dilation). Most nulliparous women seek admission to the hospital in the latent phase because they have not experienced labor before and are unsure of the “right” time to come in. Multiparous women usually do not come to the hospital until they are in the active phase of the first stage of labor. Even though no two labors are identical, women who have given birth before often are less anxious about the process, unless their previous experience has been negative.
Assessment
Assessment begins at the first contact with the woman, whether by telephone or in person. Many women call the hospital or birthing center first for validation that it is all right for them to come in for evaluation or admission or if it is all right for them to remain home. Many hospitals, however, discourage the nurse from giving advice regarding what to do because of legal liability. Nurses are often instructed to tell women who call with questions to call their primary health care provider or to come to the hospital if they feel the need to be checked. The nature of the telephone conversation including any advice or instructions given should be documented in the client’s record (Gilbert, 2011).
A pregnant woman may first call her primary care provider or come to the hospital while in false labor or early in the latent phase of the first stage of labor. She may feel discouraged, angry, or confused on learning that the contractions that feel so strong and regular to her are not true contractions because they are not causing cervical dilation, or that they are still not strong or frequent enough for admission. During the third trimester of pregnancy, women should be instructed regarding the stages of labor and the signs indicating its onset. They should be informed of the possibility that they will not be admitted if they are 3 cm or less dilated (see the Teaching for Self-Management box).
If the woman lives near the hospital and has adequate support and transportation, she may be encouraged to stay home or return home to allow labor to progress (i.e., until the uterine contractions are more frequent and intense). The ideal setting for the low risk woman at this time usually is the familiar environment of her home. The woman who lives at a considerable
distance from the hospital, who lacks adequate support and transportation, or who has a history of rapid labors in the past, however, may be admitted in latent labor. The same measures used by the woman at home should be offered to the hospitalized woman in early labor.
A warm shower is often relaxing during early labor. However, warm baths before labor is well established could inhibit uterine contractions and prolong the labor process (Waterbirth International, 2009). Soothing back, foot, and hand massage or a warm drink of preferred liquids such as tea or milk can help the woman to rest and even to sleep, especially if false or early labor is occurring at night. Diversional activities such as walking outdoors or in the house, reading, watching television, knitting, or talking with friends can reduce the perception of early discomfort, help the time pass, and reduce anxiety.
When the woman arrives at the perinatal unit, assessment is the top priority (Fig. 19-1). The nurse first performs a screening assessment by using the techniques of interview and physical assessment and reviews the laboratory and diagnostic test findings to determine the health status of the woman and her fetus and the progress of her labor. The nurse also notifies the primary health care provider and if the woman is admitted, a detailed systems assessment is done.

FIG. 19-1 Woman being assessed for admission to the labor and birth unit. (Courtesy Dee Lowdermilk, Chapel Hill, NC.)
When the woman is admitted, she is usually moved from an observation area to the labor room; the labor, delivery, and recovery (LDR) room; or the labor, delivery, recovery, and postpartum (LDRP) room. If the woman wishes, include her partner in the assessment and admission process. The nurse can direct
significant others not participating in this process to the appropriate waiting area. The woman undresses and puts on her own gown or a hospital gown. The nurse places an identification band on the woman’s wrist. Her personal belongings are put away safely or given to family members, according to agency policy. Women who participate in expectant parents classes often bring a birth bag or Lamaze bag with them. The nurse then shows the woman and her partner the layout and operation of the unit and room, how to use the call light and telephone system, and how to adjust lighting in the room and the different bed positions.
The nurse reassures the woman that she is in competent, caring hands and that she and persons to whom she gives permission can ask questions related to her care and status and that of her fetus at any time during labor. The nurse can minimize the woman’s anxiety by explaining terms commonly used during labor. The woman’s interest, response, and prior experience guide the depth and breadth of these explanations.
Most hospitals have specific forms, whether paper or electronic, which are used to obtain important assessment information when a woman in labor is being evaluated or admitted (Fig. 19-2). More and more hospitals now use an electronic medical record—almost all charting is done on computer. Sources of data include the prenatal record, the initial interview, physical examination to determine baseline physiologic parameters (e.g., vital signs), laboratory and diagnostic test results, expressed psychosocial and cultural factors, and the clinical evaluation of labor status.
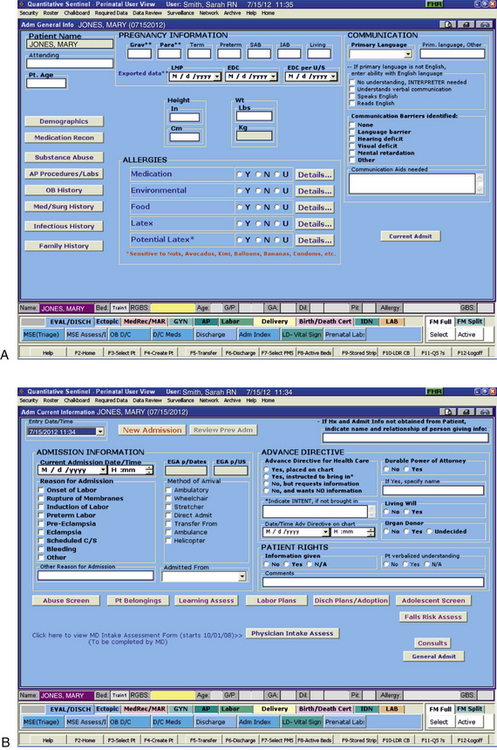
FIG. 19-2 Admission screens in an electronic medical record. A, General admission screen. B, Current admission screen. (Courtesy Kitty Cashion, Memphis, TN).
Prenatal Data
The nurse reviews the prenatal record to identify the woman’s individual needs and risks. Copies of prenatal records are generally filed in the perinatal unit at some time during the woman’s pregnancy (usually in the third trimester) or accessed by computer so that they are readily available on admission. If the woman has had no prenatal care or her prenatal records are unavailable, the nurse must obtain certain baseline information. If the woman is having discomfort, the nurse should ask questions between contractions when the woman can concentrate more fully on her answers. At times the partner or support person(s) may need to be secondary sources of essential information. According to the Health Insurance Portability and Accountability Act (HIPAA), the woman must give permission for other persons to be involved in the exchange of information regarding her care. This permission should be obtained during pregnancy and a signed form included in her health records.
Knowing the woman’s age is important so that the nurse can individualize the nursing care plan to the needs of her age-group. For example, a 14-year-old girl and a 40-year-old woman have different but specific needs, and their ages place them at risk for different problems. Accurate height and weight measurements are important. A pregnancy weight gain greater than recommended may place the woman at a higher risk for cephalopelvic disproportion and cesarean birth. This is especially true for women who are petite and have gained 16 kg or more. A prepregnancy body mass index (BMI) greater than 30 is also a cause for concern. Other factors to consider are the woman’s general health status, current medical conditions or allergies, respiratory status, and previous surgical procedures.
The nurse should carefully review the woman’s prenatal records, taking note of her obstetric and pregnancy history including gravidity, parity, and problems such as history of vaginal bleeding, gestational hypertension, anemia, pregestational or gestational diabetes, infections (e.g., bacterial, viral, sexually transmitted), and immunodeficiency status. In addition, the expected date of birth (EDB) should be confirmed. Other important data found in the prenatal record include patterns of maternal weight gain; physiologic measurements such as maternal vital signs (blood pressure, temperature, pulse, respirations); fundal height; baseline fetal heart rate (FHR); and laboratory and diagnostic test results. See Table-15-1 for a list of common prenatal laboratory tests. Common diagnostic and fetal assessment tests performed prenatally include amniocentesis, nonstress test (NST), biophysical profile (BPP), and ultrasound examination. See Chapter 26 for more information.
If this labor and birth experience is not the woman’s first, the nurse needs to note the characteristics of her previous experiences. This information includes the duration of previous labors, the type of anesthesia used, the kind of birth (e.g., spontaneous vaginal, forceps-assisted, vacuum-assisted, or cesarean birth), and the condition of the newborn. Explore the woman’s perception of her previous labor and birth experiences because this perception may influence her attitude toward her current experience.
Interview
The woman’s primary reason for coming to the hospital is determined in the interview. Her primary reason may be, for example, that her bag of waters (BOW, amniotic membranes) ruptured, with or without contractions. The woman may have come in for an obstetric check, which is a period of observation reserved for women who are unsure about the onset of their labor. This check allows time on the unit for the diagnosis of labor without official admission and minimizes or avoids cost to the woman when used by the hospital and approved by her health insurance plan.
Even the experienced woman may have difficulty determining the onset of labor. The woman is asked to recall the events of the previous days and to describe the following:
• Time and onset of contractions and progress in terms of frequency, duration, and intensity
• Location and character of discomfort from contractions (e.g., back pain, abdominal or suprapubic discomfort)
• Persistence of contractions despite changes in maternal position and activity (e.g., walking or lying down)
• Presence and character of vaginal discharge or “show”
• The status of amniotic membranes, such as a gush or seepage of fluid (spontaneous rupture of membranes [SROM]). If there has been a discharge that may be amniotic fluid, she is asked the date and time the fluid was first noted and the fluid’s characteristics (e.g., amount, color, unusual odor). In many instances, a sterile speculum examination and a Nitrazine (pH) and fern test can confirm that the membranes are ruptured (see the Procedure box: Tests for Rupture of Membranes).
These descriptions help the nurse assess the degree of progress in the process of labor. Bloody show is distinguished from bleeding by the fact that it is pink and feels sticky because of its mucoid nature. There is very little bloody show in the beginning, but the amount increases with effacement and dilation of the cervix. A woman may report a small amount of brownish to bloody discharge that may be attributed to cervical trauma resulting from vaginal examination or coitus (intercourse) within the last 48 hours.
Assessing the woman’s respiratory status is important in case general anesthesia is needed in an emergency. The nurse determines this status by asking the woman if she has a “cold” or related symptoms (e.g., “stuffy nose,” sore throat, or cough). The status of allergies, including allergies to latex and tape, and medications routinely used in obstetrics, such as opioids (e.g., hydromorphone [Dilaudid], butorphanol [Stadol], fentanyl [Sublimaze], nalbuphine [Nubain]), anesthetic agents (e.g., bupivacaine, lidocaine, ropivacaine), and antiseptics (Betadine) is reviewed. Some allergic responses cause swelling of the mucous membranes of the respiratory tract, which could interfere with breathing and the administration of inhalation
anesthesia. Because vomiting and subsequent aspiration into the respiratory tract can complicate an otherwise normal labor, the nurse records the time and type of the woman’s most recent solid and liquid intake.
The nurse obtains any information not found in the prenatal record during the admission assessment. Pertinent data include the birth plan (Box 19-1), the choice of infant feeding method, the type of pain management preferred, and the name of the pediatric health care provider. Obtain a client profile that identifies the woman’s preparation for childbirth, the support person or family members desired during childbirth and their availability, and ethnic or cultural expectations and needs. Determine the woman’s use of alcohol, drugs, and tobacco before or during pregnancy.
The nurse reviews the birth plan. If no written plan has been prepared, then the nurse helps the woman formulate a birth plan by describing options available and determining the woman’s wishes and preferences. As caregiver and advocate the nurse integrates the woman’s desires into the nursing care plan as much as possible. The nurse also prepares the woman for the possibility of change in her plan as labor progresses and assures her that the staff will provide information so that she can make informed decisions. The woman must also realize, however, that the longer her list of “wishes” is, the greater the likelihood that her expectations will not be met.
The nurse should discuss with the woman and her partner their plans for preserving childbirth memories through the use of photography and videotaping. Information should be provided about the agency’s policies regarding these practices and under what circumstances they are allowed. Protection of privacy and safety and infection control are major concerns for the expecting parents and the agency. To avoid future embarrassment and distress, the nurse should clarify with the woman exactly what parts of her childbirth she wishes to have photographed and the degree of detail. The woman’s record should reflect that the childbirth was recorded. Some hospitals and health care providers do not allow videotaping of the birth because of concerns related to legal liability.
Psychosocial Factors
The woman’s general appearance and behavior (and that of her partner) provide valuable clues to the type of supportive care she will need. However, keep in mind that general appearance and behavior may vary, depending on the stage and phase of labor (Table 19-1 and Box 19-2).
TABLE 19-1
EXPECTED MATERNAL PROGRESS IN FIRST STAGE OF LABOR
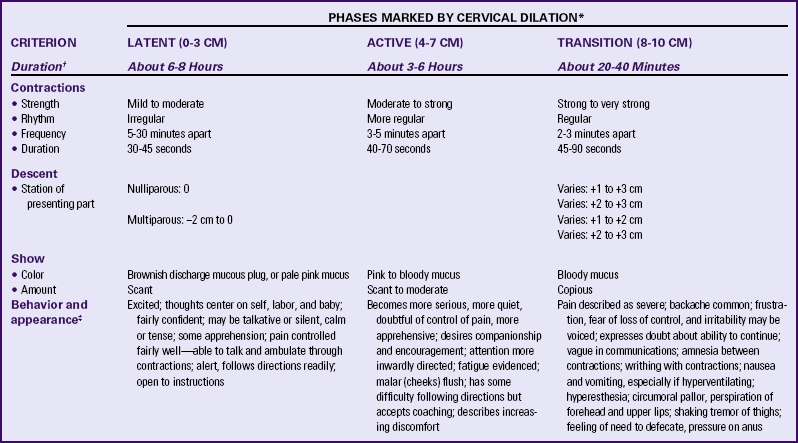
∗In the nullipara, effacement is often complete before dilation begins; in the multipara, it occurs simultaneously with dilation.
†Duration of each phase is influenced by such factors as parity, maternal emotions, position, level of activity, and fetal size, presentation, and position. For example, the labor of a nullipara tends to last longer, on average, than the labor of a multipara. Women who ambulate and assume upright positions or change positions frequently during labor tend to experience a shorter first stage. Descent is often prolonged in breech presentations and occiput posterior positions.
‡Women who have epidural analgesia for pain relief may not demonstrate some of these behaviors.
Women with a History of Sexual Abuse
Labor can trigger memories of sexual abuse, especially during intrusive procedures such as vaginal examinations. Monitors, intravenous (IV) lines, and epidurals can make the woman feel a loss of control or feel as if she is being confined to bed and “restrained.” Being observed by students and having intense sensations in the uterus and genital area, especially at the time when she must push the baby out, can also trigger memories.
The nurse can help the abuse survivor to associate the sensations she is experiencing with the process of childbirth and not with her past abuse. Help maintain her sense of control by explaining all procedures and why they are needed, validating her needs, and paying close attention to her requests. Wait for the woman to give permission before touching her, and accept her often extreme reactions to labor (Simpson, 2008). Avoid words and phrases that can cause the woman to recall the words of her abuser (e.g., “open your legs,” “relax and it won’t hurt so much”). Limit the number of procedures that invade her body (e.g., vaginal examinations, urinary catheter, internal monitor, forceps or vacuum extractor) as much as possible. Encourage her to choose a person (e.g., doula, friend, family member) to be with her during labor to provide continuous support and comfort and to act as her advocate. Nurses are advised to care for all laboring women in this manner because it is not unusual for a woman to choose not to reveal a history of sexual abuse. These care measures can help a woman perceive her childbirth experience in positive terms.
Stress in Labor
The way in which women and their support person or family members approach labor is related to the manner in which they have been socialized to the childbearing process. Their reactions reflect their life experiences regarding childbirth–physical, social, cultural, and religious. Society communicates its expectations regarding acceptable and unacceptable maternal behaviors during labor and birth. These expectations may be used by some women as the basis for evaluating their own actions during childbirth. An idealized perception of labor and birth may be a source of guilt and cause a sense of failure if the woman finds the process less than joyous, especially when the pregnancy is unplanned or is the product of a dysfunctional or terminated relationship. Often women have heard horror stories or have seen friends or relatives going through labors that appear anything but easy. Multiparous women will often base their expectations of the present labor on their previous childbirth experiences.
Discuss the feelings a woman has about her pregnancy and fears regarding childbirth. This discussion is especially important if the woman is a primigravida who has not attended childbirth classes or is a multiparous woman who has had a previous negative childbirth experience. Women in labor usually have a variety of concerns that they will voice if asked but rarely volunteer. Major fears and concerns relate to the process and effects of childbirth, maternal and fetal well-being, and the attitude and actions of the health care staff. Unresolved fears increase a woman’s stress and can slow the process of labor as a result of the inhibiting effects of catecholamines associated with the stress response on uterine contractions (Zwelling, Johnson, & Allen, 2006).
The father, coach, or significant other also experiences stress during labor. The nurse can assist and support these individuals by identifying their needs and expectations and by helping make sure these are met. The nurse can determine what role the support person intends to fulfill and whether he or she is prepared for that role by making observations and asking herself or himself such questions as, “Has the couple attended childbirth classes?” “What role does this person expect to play?” “Does he or she do all the talking?” “Is he or she nervous, anxious, aggressive, or hostile?” “Does he or she look hungry, tired, worried, or confused?” “Does he or she watch television, sleep, or stay out of the room instead of paying attention to the woman?” “Where does he or she sit?” “Does he or she touch the woman; what is the character of the touch?” Be sensitive to the needs of support persons and provide teaching and support as appropriate. In many instances the support these persons provide to the laboring woman is in direct proportion to the support they receive from the nurses and other health care providers.
Cultural Factors
Currently more than 30% of the population in the United States comes from cultural groups other than non-Hispanic whites compared with only 9% of registered nurses (Callister, 2008). As the population in the United States and Canada becomes more diverse, it is increasingly important to note the woman’s ethnic or cultural and religious values, beliefs, and practices in order to anticipate nursing interventions to add or eliminate from an individualized, mutually acceptable plan of care that provides a feeling of safety and control (Fig. 19-3). Nurses should be committed to providing culturally sensitive care and to developing an appreciation and respect for cultural diversity (Callister, 2005; 2008). Encourage the woman to request specific caregiving behaviors and practices that are important to her. If a special request contradicts usual practices in that setting, the woman or the nurse can ask the woman’s primary health care provider to write an order to accommodate the special request. For example, in many cultures, it is unacceptable to have a male caregiver examine a pregnant woman. In some cultures, it is traditional to take the placenta home; in others, the woman has only certain nourishments during labor. Some women believe that cutting her body, as with an episiotomy, allows her spirit to leave her body and that rupturing the membranes prolongs, not shortens, labor. It is important to explain the rationale for required care measures carefully (see the Cultural Considerations box).

FIG. 19-3 Birthing room specific to a Native-American population. Note the arrow pointing east, the rug on the wall, and the rope or sash belt hanging from the ceiling. (Courtesy Patricia Hess, San Francisco, CA; Chinle Comprehensive Health Care Center, Chinle, AZ.)
Within cultures, women may have an idea of the “right” way to behave in labor and may react to the pain experienced in that way. These behaviors can range from total silence to moaning or screaming, but they do not necessarily indicate the degree of pain. A woman who moans with contractions may not be in as much physical pain as a woman who is silent but winces during contractions. Some women believe that screaming or crying out in pain is shameful if a man is present. If the woman’s support
person is her mother, she may perceive the need to “behave” more strongly than if her support person is the father of the baby. She will perceive herself as failing or succeeding based on her ability to follow these “standards” of behavior. Conversely, a woman’s behavior in response to pain may influence the support received from significant others. In some cultures, women who lose control and cry out in pain may be scolded, whereas in other cultures, support persons will become more helpful (D’Avanzo, 2008).
Culture and Father Participation
A companion is an important source of support, encouragement, and comfort for women during childbirth. The woman’s cultural and religious background influences her choice of birth companion as do trends in the society in which she lives. For example, in Western societies the father is viewed as the ideal birth companion. For European-American couples, attending childbirth classes together has become a traditional, expected activity. Laotian (Hmong) husbands also traditionally participate actively in the labor process. In some other cultures the father may be available, but his presence in the labor room with the mother may not be considered appropriate, or he may be present but resist active involvement in her care. Such behavior could be perceived by the nursing staff to indicate a lack of concern, caring, or interest. Women from many cultures prefer female caregivers and want to have at least one female companion present during labor and birth. They also are usually very concerned about modesty. If couples from these cultures immigrate to the United States or Canada, their roles may change. The nurse needs to talk to the woman and her support persons to determine the roles they will assume.
The Non–English-Speaking Woman in Labor
A woman’s level of anxiety in labor increases when she does not understand what is happening to her or what is being said. Non–English-speaking women often feel a complete loss of control over their situation if no health care provider is present who speaks their language. They can panic and withdraw or become physically abusive when someone tries to do something they perceive might harm them or their babies. A support person is sometimes able to serve as an interpreter. However, caution is warranted because the interpreter may not be able to convey exactly what the nurse or others are saying or what the woman is saying, which can increase the woman’s stress level even more.
Ideally, a bilingual nurse will care for the woman. Alternatively a hospital employee or volunteer interpreter may be contacted for assistance (see Box 2-2). Ideally, the interpreter is from the woman’s culture. For some women a female is more acceptable than a male interpreter. If no one in the hospital is able to interpret, call a service so that interpretation can take place over the telephone. Even when the nurse has limited ability to communicate verbally with the woman, in most instances the woman appreciates the nurse’s efforts to do so. Speaking slowly and avoiding complex words and medical terms can help a woman and her partner understand. Often the woman understands English much better than she speaks it.
Physical Examination
The initial physical examination includes a general systems assessment and an assessment of fetal status. During the examination uterine contractions are assessed and a vaginal examination is performed. The findings of the admission physical examination serve as a baseline for assessing the woman’s progress from that point. See Chapter 4 for information regarding physical examination of women with disabilities.
The information obtained from a complete and accurate assessment during the initial examination serves as the basis for determining whether the woman should be admitted and what her ongoing care should be. Expected maternal progress and minimal assessment guidelines during the first stage of labor are presented in Table 19-1 and the Nursing Process Box: First Stage of Labor.
Birth is a time when nurses and other health care providers are exposed to a great deal of maternal and newborn blood and body fluids. Therefore, Standard Precautions should guide all assessment and care measures (Box 19-3). Hand hygiene
(e.g., washing hands with soap or application of an alcohol-based antiseptic rub) before and after assessing the woman and providing care is a critical step in the prevention of infection transmission. The nurse should explain assessment findings to the woman and her partner whenever possible. Throughout labor, accurate documentation, following agency policy, is done as soon as possible after a procedure has been performed (Fig. 19-4).
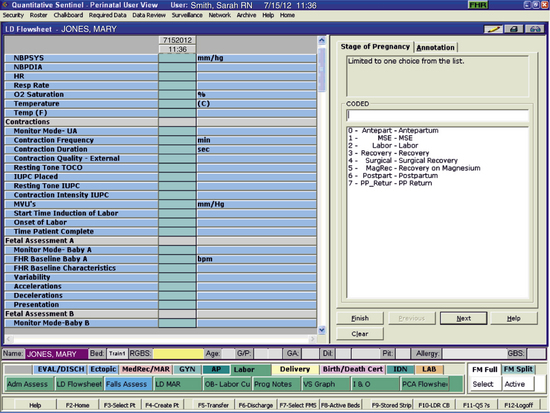
FIG. 19-4 Portion of the labor flowsheet screen in an electronic medical record. (Courtesy Kitty Cashion, Memphis, TN).
General Systems Assessment
On admission, the nurse should perform a brief systems assessment. This includes an assessment of the heart, lungs, and skin and an examination to determine the presence and extent of edema of the face, hands, sacrum, and legs. It also includes testing of deep tendon reflexes and for clonus if indicated. Also note the woman’s weight. Increasing numbers of women are overweight or obese. Excessive size can make nursing care during labor and birth more difficult and places the woman at risk for complications such as operative birth, infection, and blood clots. See Chapter 33 for further information.
Vital Signs
Assess vital signs (temperature, pulse, respirations, and blood pressure using a correct size cuff) on admission. The initial values are used as the baseline for comparison for all future measurements. If the blood pressure is elevated, reassess it 30 minutes later, between contractions, to obtain a reading after the woman has relaxed. Encourage the woman to lie on her side to prevent supine hypotension and fetal distress (Fig. 19-5). Monitor her temperature so that you can identify signs of infection or a fluid deficit (e.g., dehydration associated with inadequate intake of fluids).
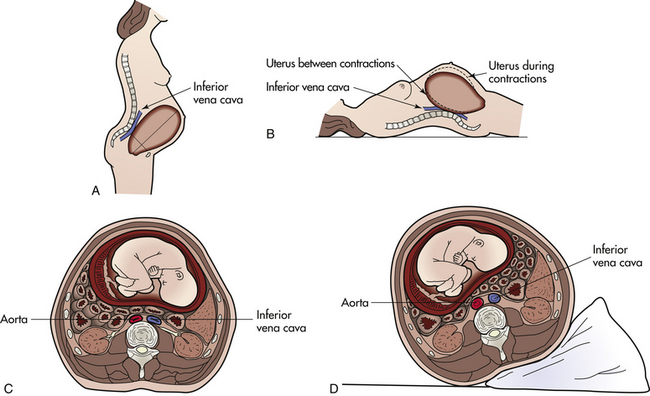
FIG. 19-5 Supine hypotension. Note relation of pregnant uterus to ascending vena cava in standing position (A), and in the supine position (B). C, Compression of aorta and inferior vena cava with woman in supine position. D, Compression of these vessels is relieved by placement of a wedge pillow under the woman’s right side.
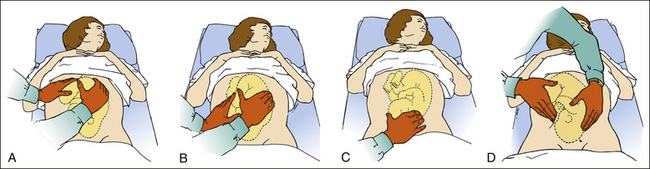
Leopold Maneuvers (Abdominal Palpation)
Leopold maneuvers are performed with the woman briefly lying on her back (see the Procedure box: Leopold Maneuvers). These maneuvers help identify the (1) number of fetuses; (2) presenting part, fetal lie, and fetal attitude; (3) degree of the presenting part’s descent into the pelvis; and (4) expected location of the point of maximal intensity (PMI) of the FHR on the woman’s abdomen.
Assessment of Fetal Heart Rate and Pattern
The PMI of the FHR is the location on the maternal abdomen at which the FHR is heard the loudest. It is usually directly over the fetal back (Fig. 19-6). In a vertex presentation, you can usually hear the FHR below the mother’s umbilicus in either the right or the left lower quadrant of the abdomen. In a breech presentation you usually hear the FHR above the mother’s umbilicus. The Nursing Process Box: First Stage of Labor summarizes assessments recommended for determining fetal status. In addition, you must assess the FHR after ROM because this is the most common time for the umbilical cord to prolapse, after any change in the contraction pattern or maternal status, and before and after the woman receives medication or a procedure is performed (Tucker et al., 2009).
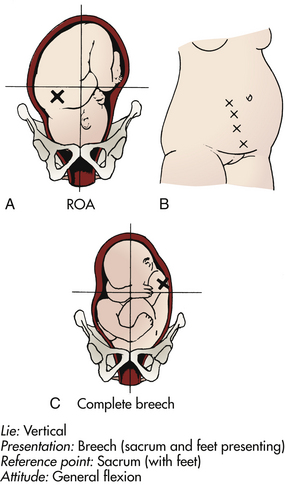
FIG. 19-6 Location of the fetal heart tones (FHTs). A, FHTs with fetus in right occipitoanterior (ROA) position. B, Changes in location of point of maximal intensity of FHTs as fetus undergoes internal rotation from ROA to OA and descent for birth. C, FHTs with fetus in left sacrum posterior position. (A and C, Courtesy Ross Laboratories, Columbus, OH.)
Assessment of Uterine Contractions
A general characteristic of effective labor is regular uterine activity (i.e., contractions becoming more frequent with increased duration), but uterine activity is not directly related to labor progress. Uterine contractions are the primary powers that act involuntarily to expel the fetus and the placenta from the uterus. Several methods are used to evaluate uterine contractions, including the woman’s subjective description, palpation and timing of contractions by a health care provider, and electronic monitoring.
Each contraction exhibits a wavelike pattern. It begins with a slow increment (the “building up” of a contraction from its onset), gradually reaches a peak, and then diminishes rapidly (decrement, the “letting down” of the contraction). An interval of rest ends when the next contraction begins. The outward appearance of the woman’s abdomen during and between contractions and the pattern of a typical uterine contraction are shown in Figure 19-7.
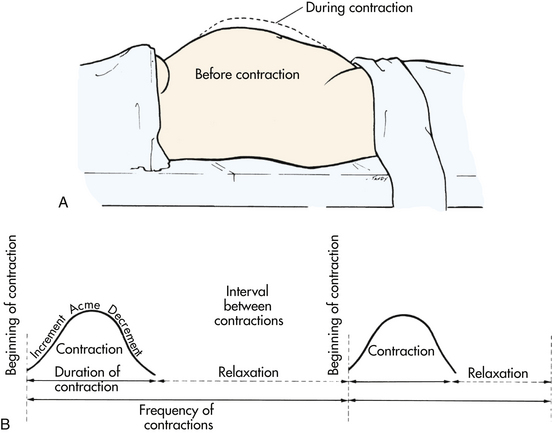
FIG. 19-7 Assessment of uterine contractions. A, Abdominal contour before and during uterine contraction. B, Wavelike pattern of contractile activity.
A uterine contraction is described in terms of the following characteristics:
• Frequency: How often uterine contractions occur; the time that elapses from the beginning of one contraction to the beginning of the next contraction
• Intensity: The strength of a contraction at its peak
• Duration: The time that elapses between the onset and the end of a contraction
• Resting tone: The tension in the uterine muscle between contractions; relaxation of the uterus
Uterine contractions are assessed by palpation or by using an external or internal electronic monitor (see Chapter 18 for further discussion). Frequency and duration can be measured by all three methods of uterine activity monitoring. The accuracy of determining intensity and resting tone varies by the method used. The woman’s description and palpation are more subjective and less precise ways of determining the intensity of uterine contractions and resting tone than is the electronic fetal monitor. The following terms describe what is felt on palpation:
• Mild: Slightly tense fundus that is easy to indent with fingertips (feels like touching finger to tip of nose)
• Moderate: Firm fundus that is difficult to indent with fingertips (feels like touching finger to chin)
• Strong: Rigid boardlike fundus that is almost impossible to indent with fingertips (feels like touching finger to forehead)
Women in labor tend to describe the pain of contractions in terms of the sensations they are experiencing in the lower abdomen or back, which are sometimes unrelated to the firmness of the uterine fundus. Therefore, their assessment of the strength of their contractions can be less accurate than that of the health care provider, although the amount of discomfort reported is valid.
External electronic monitoring provides some information about the strength of uterine contractions when the appearance of contractions on admission is compared to those that occur later in labor. Internal electronic monitoring with an intrauterine pressure catheter, however, is the most accurate way of assessing the intensity of uterine contractions and resting tone.
On admission, at least a 20- to 30-minute baseline monitoring period of uterine contractions and the fetal heart rate and pattern commonly is done using electronic monitors. The minimal times for assessing uterine activity during the various phases of labor are given in the Nursing Process boxes for the First Stage of Labor; the Second Stage of Labor and the findings expected as labor progresses are summarized in Tables 19-1 and 19-3.
You must consider uterine activity in the context of its effect on cervical effacement and dilation and on the degree of descent of the presenting part (see Chapter 16). You must also consider the effect on the fetus. You can verify the progress of labor effectively through the use of graphic charts (partograms) on which you plot cervical dilation and station (descent). This type of graphic charting assists in early identification of deviations from expected labor patterns. Figure 19-8 provides examples of partograms. Hospitals and birthing centers may develop their own assessment graphs that may include data not only on dilation and descent but also maternal vital signs, FHR, and uterine activity.
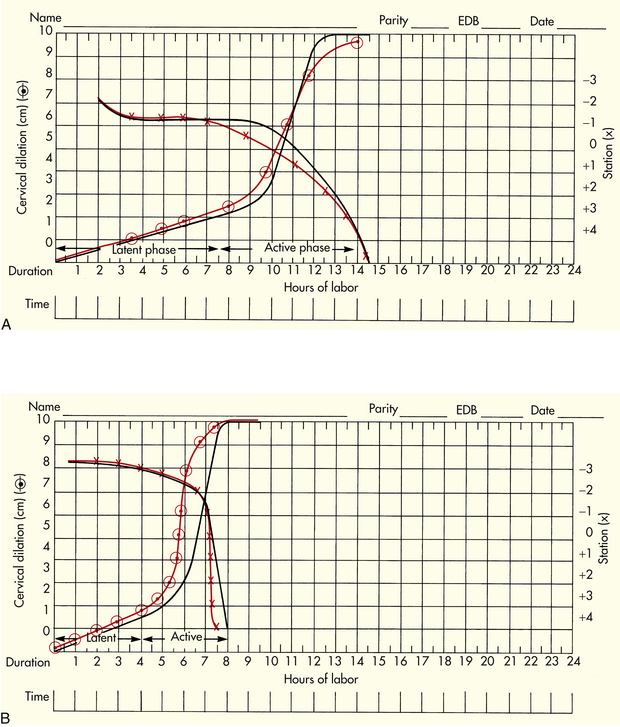
FIG. 19-8 Partograms for assessment of patterns of cervical dilation and descent. Individual woman’s labor patterns (colored) are superimposed on prepared labor graph (black) for comparison. A, Labor of a nulliparous woman. B, Labor of a multiparous woman. The rate of cervical dilation is plotted with the circled plot points. A line drawn through these symbols depicts the slope of the curve. Station is plotted with Xs. A line drawn through the Xs reveals the pattern of descent.
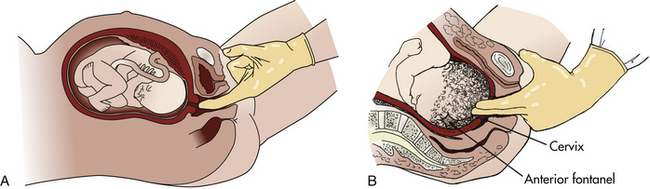
Vaginal Examination
The vaginal examination reveals whether the woman is in true labor and enables the examiner to determine whether the membranes have ruptured (Fig. 19-9). Because this examination is often stressful and uncomfortable for the woman, perform it only when indicated by the status of the woman and her fetus. For example, you should perform a vaginal examination on admission, prior to administering medications (e.g., analgesics, increasing oxytocin infusion), when significant change has occurred in uterine activity, on maternal perception of perineal pressure or the urge to bear down, when membranes rupture, or when you note variable decelerations of the FHR. A full explanation of the examination and support of the woman are important in reducing the stress and discomfort associated with the examination (Simpson, 2008) (see the Procedure box: Vaginal Examination of the Laboring Woman.)
Laboratory and Diagnostic Tests
A clean-catch urine specimen may be obtained to gather further data about the pregnant woman’s health. Analysis of the specimen is a convenient and simple procedure that can provide information about her hydration status (e.g., specific gravity, color, amount), nutritional status (e.g., ketones), infection status (e.g., leukocytes), or the status of possible complications such as preeclampsia, shown by finding protein in the urine. In most hospitals this test must be done in the laboratory rather than at the bedside, even if a urine “dipstick” is used.
Blood Tests
The blood tests performed vary with the hospital protocol and the woman’s health status. Currently, all blood tests must be performed in the hospital laboratory rather than on the perinatal unit. Often blood samples are obtained from the hub of the catheter when an IV is started. A hematocrit will likely be ordered. More comprehensive blood assessments such as white blood cell count, red blood cell count, hemoglobin level, hematocrit, and platelet values are included in a complete blood count (CBC). A CBC may be ordered for women with a history of infection, anemia, gestational hypertension, or other disorders. Any woman whose human immunodeficiency virus (HIV) status is undocumented at the time of labor should be screened with a rapid HIV test unless she declines (opts out) of testing (Centers for Disease Control and Prevention [CDC], Branson, Handsfield, Lampe, Janssen, & Taylor, et al., 2006).
Most hospitals require that a “type and screen,” to determine the woman’s blood type and Rh status, be performed on admission. Even if these tests have already been performed during pregnancy, the hospital’s laboratory or blood bank must verify the results in-house. If the woman had no prenatal care or if her prenatal records are not available, a prenatal screen will probably be drawn on admission. The prenatal screen includes laboratory tests that would normally have been drawn at the initial prenatal visit (see Table 15-2).
Other Tests
If the woman’s group B streptococci status is not known, a rapid test may be done on admission. The rapid test results are usually available within an hour or so and will determine if the woman must be given antibiotics during labor.
Assessment of Amniotic Membranes and Fluid
Labor is initiated at term by SROM in approximately 25% of pregnant women. A lag period, rarely exceeding 24 hours, may precede the onset of labor. Membranes (the BOW) also can rupture spontaneously any time during labor, but most commonly in the transition phase of the first stage of labor. The Procedure box: Tests for Rupture of Membranes explains how to determine if membranes are ruptured. If the membranes do not rupture spontaneously, the BOW will likely be ruptured artificially at some time during labor. Artificial rupture of membranes (AROM), called an amniotomy, is performed by the physician or certified nurse-midwife using a plastic AmniHook or a surgical clamp.
Whether the membranes rupture spontaneously or artificially, the time of rupture should be recorded. Other necessary documentation includes information regarding the color (clear or meconium-stained), estimated amount, and odor of the fluid. See Chapter 33 for additional information.
Infection: When membranes rupture, microorganisms from the vagina can then ascend into the amniotic sac, causing chorioamnionitis and placentitis to develop. For this reason assess maternal temperature and vaginal discharge frequently (at least every 2 hours) so that you can quickly identify an infection developing after ROM. Even when membranes are intact, however, microorganisms may ascend and cause infection.
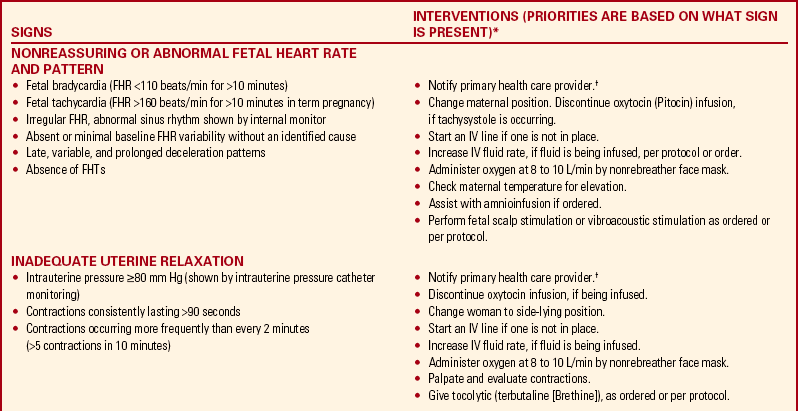
Assessment findings serve as a baseline for evaluating the woman’s subsequent progress during labor. Although some problems can be anticipated, others may appear unexpectedly during the clinical course of labor (see the Signs of Potential Complications box).
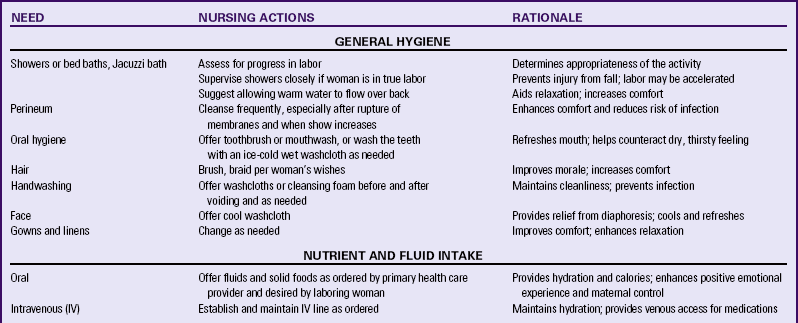
Nursing Care
The nursing process provides the framework for the nursing care management of women in labor. The physical nursing care given to a woman in labor is an essential component of her care. The current emphasis on evidence-based practice supports the management of care by using this approach to enhance the safety, effectiveness, and acceptability of the physical care measures chosen to support the woman during labor and birth (Box 19-4). The various physical needs, the necessary nursing actions, and the rationale for care are presented in Table 19-2, the Nursing Care Plan and the Nursing Process box: First Stage of Labor.
General Hygiene
Offer women in labor the use of showers or warm-water baths, if they are available, to enhance the feeling of well-being and to minimize the discomfort of contractions. ![]() Water immersion during active labor is associated with decreases in the use of analgesia and in reported maternal pain (Berghella, Baxter, & Chauhan, 2008). Also encourage women to wash their hands or use cleansing foam after voiding and to perform self-hygiene measures.
Water immersion during active labor is associated with decreases in the use of analgesia and in reported maternal pain (Berghella, Baxter, & Chauhan, 2008). Also encourage women to wash their hands or use cleansing foam after voiding and to perform self-hygiene measures.
Change the linen if it becomes wet or stained with blood, and use linen savers (Chux), changing them as needed.
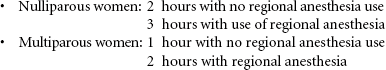
Nutrient and Fluid Intake
Prior to the 1940s women were allowed to eat and drink during labor to maintain the energy required to sustain labor and the stamina required to give birth. This practice changed, allowing the laboring woman only clear liquids or ice chips or nothing by mouth during the active phase of labor when concern arose regarding the risk of anesthesia complications and their secondary effects if general anesthesia were required in an emergency. These secondary effects include the aspiration of gastric contents and resultant compromise in oxygen perfusion, which could endanger the lives of the mother and fetus (Simpson, 2008). There have been no randomized trials evaluating the ingestion of solid foods in labor, so current management is based mostly on expert opinions. Ice chips and sips of clear liquids are still the only oral intake recommended during labor in the United States by the American Society of Anesthesiologists Task Force on Obstetrical Anesthesia (Berghella et al., 2008). This practice is being challenged by some health care providers, however, because regional anesthesia is used more often than general anesthesia, even for emergency cesarean births. Women are awake during regional anesthesia and are able to participate in their own care and protect their airway.
An adequate intake of fluids and calories is required to meet the energy demands and fluid losses associated with childbirth. The progress of labor slows, with a more rapid development of hypoglycemia and ketosis if these demands are not met and fat is metabolized. Reduced energy for bearing-down efforts (pushing) increases the risk for a forceps- or vacuum-assisted birth. This is most likely to occur in women who begin to labor early in the morning after a night without caloric intake. When women are permitted to consume fluids and food freely, they typically regulate their own oral intake, eating light foods (e.g., eggs, yogurt, ice cream, dry toast and jelly, fruit) and drinking fluids during early labor and tapering off to the intake of clear fluids and sips of water or ice chips as labor intensifies and the second stage approaches (Parsons, Bidwell, & Nagy, 2006).
Common practice is to allow clear liquids (e.g., water, tea, fruit juices without pulp, clear sodas, coffee, sports drinks, fruit ice, Popsicles, gelatin, broth) during early labor, tapering off to ice chips and sips of water as labor progresses and becomes more active. Herbal teas can provide not only hydration but also other beneficial effects. ![]() Chamomile tea can enhance relaxation, lemon balm or peppermint tea can reduce nausea, and teas of ginger or ginseng root are energizing (Walls, 2009). A woman’s culture may influence what she will eat and drink during labor. In addition, women who use nonpharmacologic pain relief measures and labor at home or in birthing centers are more likely to eat and drink during labor. The amount of solid and liquid carbohydrates to offer a woman in labor is still unclear. Though it is known that energy needs increase as labor becomes prolonged, there is limited evidence regarding the effect of oral carbohydrate intake in enhancing the progress of labor and reducing the risk for dystocia (Tranmer, Hodnett, Hannah, & Stevens, 2005).
Chamomile tea can enhance relaxation, lemon balm or peppermint tea can reduce nausea, and teas of ginger or ginseng root are energizing (Walls, 2009). A woman’s culture may influence what she will eat and drink during labor. In addition, women who use nonpharmacologic pain relief measures and labor at home or in birthing centers are more likely to eat and drink during labor. The amount of solid and liquid carbohydrates to offer a woman in labor is still unclear. Though it is known that energy needs increase as labor becomes prolonged, there is limited evidence regarding the effect of oral carbohydrate intake in enhancing the progress of labor and reducing the risk for dystocia (Tranmer, Hodnett, Hannah, & Stevens, 2005).
Withholding food and fluids in labor is unlikely to be beneficial, and offering oral fluids is demonstrably useful and should be encouraged (Hofmeyr, 2005). Nurses should follow the orders of the woman’s primary health care provider when offering the woman food or fluids during labor. As advocates, however, nurses can facilitate change by informing others of the current research findings that support the safety and effectiveness of the oral intake of food and fluid during labor and by initiating such research themselves. ![]()
Intravenous Intake
Fluids are administered intravenously to the laboring woman to maintain hydration, especially when a labor is long and the woman is unable to ingest a sufficient amount of fluid orally or if she is receiving epidural or intrathecal anesthesia. In most cases an electrolyte solution without glucose (e.g., Ringer’s lactate or normal saline) is adequate and does not introduce excess glucose into the bloodstream. The latter is important because an excessive maternal glucose level results in fetal hyperglycemia and fetal hyperinsulinism. After birth the neonate’s high level of insulin will reduce his or her glucose stores, and hypoglycemia will result. Infusions containing glucose can also reduce sodium levels in the woman and the fetus, leading to transient neonatal tachypnea. If maternal ketosis occurs, the primary health care provider may order an IV solution containing a small amount of dextrose to provide the glucose needed to assist in fatty acid metabolism.
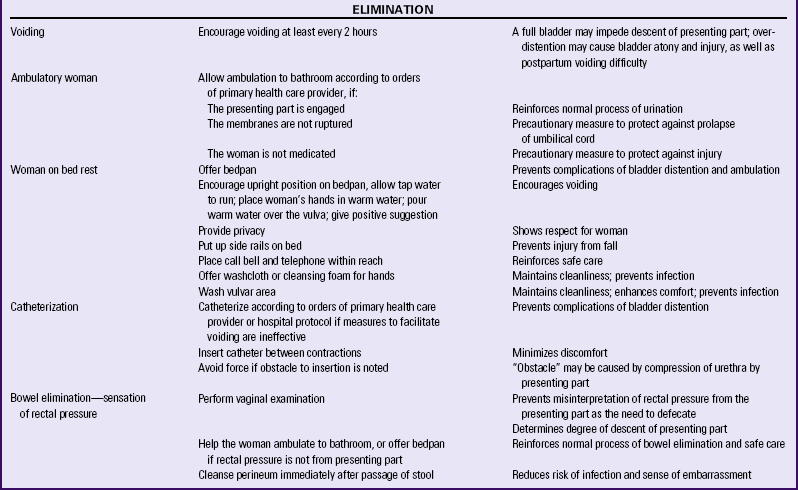
Elimination
Encourage voiding every 2 hours. A distended bladder may impede descent of the presenting part, slow or stop uterine contractions, and lead to decreased bladder tone or uterine atony after birth. Women who receive epidural analgesia or anesthesia are especially at risk for the retention of urine. Therefore, the need to void should be assessed more frequently with them.
Assist the woman to the bathroom to void or use a bedside commode, unless any of the following apply: the primary health care provider has ordered bed rest; the woman is receiving epidural analgesia or anesthesia; internal monitoring is being used; or ambulation will compromise the status of the laboring woman or her fetus. External monitoring can usually be interrupted long enough for the woman to go to the bathroom.
If using a bedpan is necessary, encourage spontaneous voiding by providing privacy and having the woman sit upright (as she would on a toilet). Other interventions to encourage urination, either in the bathroom or on the bedpan, are having the woman listen to the sound of water slowly running from a faucet, placing her hands in warm water, having her blow bubbles into a glass of water using a straw, or pouring warm water over the vulva and perineum using a peri bottle.
Catheterization
If the woman is unable to void and her bladder is distended, she may need to be catheterized. Many hospitals have protocols that rely on the nurse’s judgment concerning the need for catheterization. Before performing the catheterization, clean the vulva and perineum because vaginal show and amniotic fluid may be present. If an obstacle that prevents advancement of the catheter is present, this obstacle is most likely the presenting part. If you cannot advance the catheter, stop the procedure and notify the primary health care provider of the difficulty.
Bowel Elimination
Most women do not have bowel movements during labor because of decreased intestinal motility. Stool that has formed in the large intestine often moves downward toward the anorectal area as a result of pressure exerted by the fetal presenting part as it descends. This stool is often expelled during second-stage pushing and birth. However, the passage of stool with bearing-down efforts increases the risk of infection and may embarrass the woman, thereby reducing the effectiveness of her pushing efforts. To prevent these problems, the nurse should immediately cleanse the perineal area to remove any stool, while reassuring the woman that the passage of stool at this time is a normal and expected event, because the same muscles used to expel the baby also expel stool.
Routine use of enemas on admission for women at term has shown only modest benefits. There is a trend toward lower infection rates and the newborns have fewer lower respiratory tract infections and less need for antibiotics. However, because enemas cause discomfort for women and increase the costs of giving birth, the small benefits do not outweigh the disadvantages of this practice (Berghella et al., 2008). ![]() In addition, a recent Cochrane review of this topic found that the evidence does not support the routine use of enemas during labor (Reveiz, Gaitan, & Cuervo, 2007).
In addition, a recent Cochrane review of this topic found that the evidence does not support the routine use of enemas during labor (Reveiz, Gaitan, & Cuervo, 2007).
When the presenting part is deep in the pelvis, even in the absence of stool in the anorectal area, the woman may feel rectal pressure and think she needs to defecate. If the woman expresses the urge to defecate, the nurse should perform a vaginal examination to assess cervical dilation and station. When a multiparous woman experiences the urge to defecate, this often means birth will follow quickly.
Ambulation and Positioning
Confinement to bed is the norm for labor management in the United States. The increased use of epidurals during childbirth accompanied by multiple medical interventions (e.g., monitors, intravenous infusions) and reduced motor control contribute to this practice, thereby interfering with a woman’s freedom of movement. Upright positions and mobility during labor, however, may be more pleasant for laboring women. These practices have also been associated with improved uterine contraction intensity and shorter labors, less need for pain medications, reduced rate of operative birth (e.g., cesarean birth, forceps- and vacuum-assisted birth), increased maternal autonomy and control, distraction from labor’s discomforts, and an opportunity for close interaction with the woman’s partner and care provider as they assist her to assume upright positions and remain mobile. No harmful effects have been observed from maternal activity and position changes (Albers, 2007; Simpson, 2008; Zwelling, 2010).
Encourage ambulation if membranes are intact, if the fetal presenting part is engaged after ROM, and if the woman has not received medication for pain (Fig. 19-10). The woman also may find it comfortable to stand and lean forward on her partner, doula, or nurse for support at times during labor (Fig. 19-11, A). Ambulation may be contraindicated, however, because of maternal or fetal status.
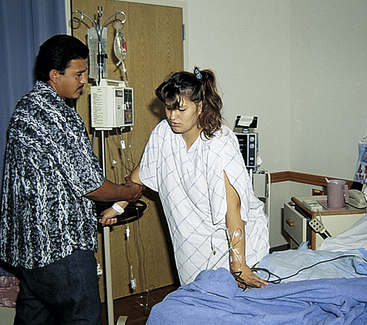
FIG. 19-10 Woman preparing to walk with partner. (Courtesy Marjorie Pyle, RNC, Lifecircle, Costa Mesa, CA.)
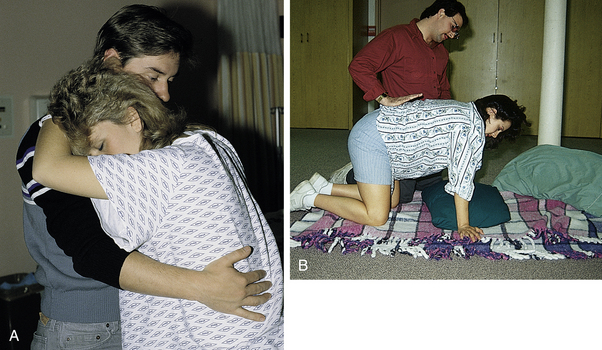
FIG. 19-11 A, Woman standing and leaning forward with support. B, Woman in hands-and-knees position. (Courtesy Marjorie Pyle, RNC, Lifecircle, Costa Mesa, CA.)
When the woman lies in bed, she will usually change her position spontaneously as labor progresses. If she does not change position every 30 to 60 minutes, assist her to do so. The side-lying (lateral) position is preferred because it promotes optimal uteroplacental and renal blood flow and increases fetal oxygen saturation (Fig. 19-12, B). If the woman wants to lie supine, the nurse should place a pillow under one hip as a wedge to prevent the uterus from compressing the aorta and vena cava (see Fig. 19-5). Sitting is not contraindicated unless it adversely affects fetal status, which you can determine by checking the FHR and pattern. If the fetus is in the occiput posterior position, it may be helpful to encourage the woman to squat during contractions because this position increases the pelvic diameter, allowing the head to rotate to a more anterior position (see Fig. 19-12, A). A hands-and-knees position during contractions or a lateral position on the same side as the fetal spine also are recommended to facilitate the rotation of the fetal occiput from a posterior to an anterior position, as gravity pulls the fetal back forward. These positions also provide access to the back for application of counterpressure by the partner, doula, or nurse (Hanson, 2009; Simpson. Cesario, Morin, Trapani, Mayberry, & Snelgrove-Clark, 2008; Zwelling, 2010) (see Fig. 19-11, B). Women with epidural anesthesia may not be able to squat or assume a hands-and-knees position depending on the degree of motor involvement resulting from the epidural.
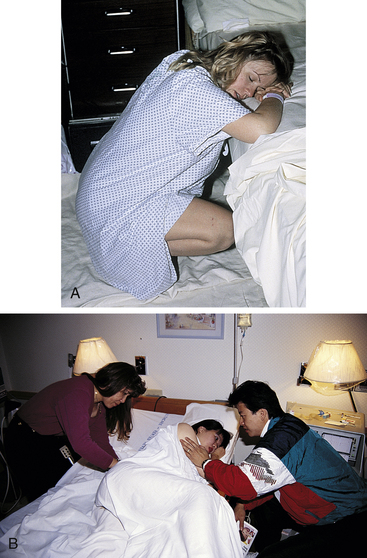
FIG. 19-12 Maternal positions for labor. A, Squatting. B, Lateral position. Support person is applying sacral pressure while partner provides encouragement. (Courtesy Marjorie Pyle, RNC, Lifecircle, Costa Mesa, CA.)
Much research continues to focus on acquiring a better understanding of the physiologic and psychologic effects of maternal position in labor. Box 19-5 describes a variety of positions that are commonly used and recommended.
The woman can use a birth ball (gymnastic ball, physical therapy ball) to support her body as she assumes a variety of labor and birth positions (Fig. 19-13). She can sit on the ball while leaning over the bed, or lean over the ball to support her upper body and reduce stress on her arms and hands when she assumes a hands-and-knees position. The birth ball can encourage pelvic mobility and pelvic and perineal relaxation when the woman sits on the firm yet pliable ball and rocks in rhythmic movements. Warm compresses applied to the

FIG. 19-13 Woman laboring using birth ball. (Courtesy Polly Perez, Cutting Edge Press, Johnson, VT.)
perineum and lower back can maximize this relaxation and comfort effect. The birth ball should be large enough so that when the woman sits, her knees are bent at a 90-degree angle and her feet are flat on the floor and approximately 2 feet apart.
Supportive Care During Labor and Birth
Support during labor and birth involves emotional support, physical care and comfort measures, and advice and information. The value of the continuous supportive presence of a person (e.g., doula, childbirth educator, family member, friend, nurse, partner) during labor has long been known. Women who have continuous support beginning in early labor are less likely to use pain medication or epidurals, more likely to have a spontaneous vaginal birth, and less likely to report dissatisfaction with their birth experience. No harmful effects from continuous labor support have been identified. To the contrary, there is good evidence that labor support improves important health outcomes (Albers, 2007; Berghella et al., 2008; Hodnett, Gates, Hofmeyer, & Sakala, 2007). ![]()
Labor rooms should be airy, clean, and homelike. The laboring woman should feel safe in this environment and free to be herself and to use the comfort and relaxation measures she prefers. To enhance relaxation, turn off bright overhead lights when not needed, and keep noise and intrusions to a minimum. Control the temperature to ensure the laboring woman’s comfort. The room should be large enough to accommodate a comfortable chair for the woman’s partner, the monitoring equipment, and hospital personnel. Encourage women to bring their own pillows to make the hospital surroundings more homelike and to facilitate position changes. Environmental modifications should reflect the preferences of the woman, including the number of visitors and availability of a telephone, television, and music.
Labor Support by the Nurse
Supportive nursing care for a woman in labor includes:
• Helping the woman maintain control and participate to the extent she wishes in the birth of her infant
• Providing continuity of care that is nonjudgmental and respectful of her cultural and religious values and beliefs
• Meeting the woman’s expected outcomes for her labor
• Listening to the woman’s concerns and encouraging her to express her feelings
• Acting as the woman’s advocate, supporting her decisions and respecting her choices as appropriate, and relating her wishes as needed to other health care providers
• Helping the woman conserve her energy and cope effectively with her pain and discomfort by using a variety of comfort measures that are acceptable to her
• Helping control the woman’s discomfort
• Acknowledging the woman’s efforts during labor including her strength and courage, as well as those of her partner, and providing positive reinforcement
Women who have attended childbirth education programs that teach the psychoprophylactic (Lamaze) approach will know something about the labor process, coaching techniques, and comfort measures. The nurse plays a supportive role and keeps the woman and her partner informed of the labor progress. If necessary, review the methods learned in class and practiced at home because it may be difficult for the woman to effectively use these methods and techniques now that the woman is in labor and in an unfamiliar setting.
Even when a laboring woman has not attended childbirth classes, the nurse can teach her simple breathing and relaxation techniques during the early phase of labor. In this case the nurse provides more of the coaching and supportive care until the support person feels ready to take on a more active coaching role (see Chapter 17). The nurse can demonstrate comfort measures while encouraging the support person to assist and the laboring woman to express her needs and feelings. Observing the comforting approaches of the nurse can help the partner to learn effective comfort measures.
Comfort measures vary with the situation (Fig. 19-14). The nurse can draw on the woman’s list of comfort measures and relaxation techniques learned during the pregnancy and through life experiences. Such measures include maintaining a comfortable, calm, supportive atmosphere in the labor and birth area; using touch therapeutically (e.g., heat or cold applied to the lower back in the event of back labor, a cool cloth applied to the forehead, massage); providing nonpharmacologic measures to relieve discomfort (e.g., hydrotherapy); and most important, just being there (MacKinnon, McIntyre, & Quance, 2005) (see Tables 19-1 and 19-2). See Chapter 17 for a full discussion of pharmacologic and nonpharmacologic comfort measures.
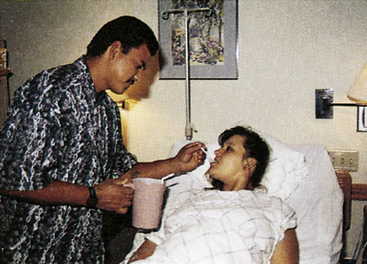
FIG. 19-14 Partner providing comfort measures. (Courtesy Marjorie Pyle, RNC, Lifecircle, Costa Mesa, CA.)
Most women in labor respond positively to touch, but you should obtain permission before using any touching measures. Women appreciate gentle handling by staff members. Back rubs and counterpressure may be offered, especially if the woman is experiencing back labor. Teach the support person to exert counterpressure against the woman’s sacrum over the occiput of the head of a fetus in a posterior position (see Fig. 19-12, B). Double hip or knee squeezes can also be helpful in reducing back pain. The back pain is caused by the occiput pressing on spinal nerves, and counterpressure lifts the occiput off these nerves, providing some relief from pain. The partner will need to be relieved after a while, however, because exerting counterpressure is hard work. Hand and foot massage also can be soothing and relaxing.
The woman’s perception of the soothing qualities of touch may change as labor progresses. Many women become more sensitive to touch (hyperesthesia) as labor progresses. This is a typical response during the transition phase (see Table 19-1). They may tell their coach to leave them alone or not to touch them. The partner who is unprepared for this normal response may feel rejected and may react by withdrawing active support. The nurse can reassure him or her that this response is a positive indication that the first stage is ending and the second stage is approaching. Women with increased sensitivity to touch may tolerate it better on surfaces of the body where hair does not grow, such as the forehead, the palms of the hands, and the soles of the feet.
Labor Support by the Father or Partner
Although another woman or a man other than the father may be the woman’s partner, the father of the baby is usually the support person during labor. He is often able to provide the comfort measures and touch that the laboring woman needs. When the woman becomes focused on her pain, sometimes the partner can persuade her to try nonpharmacologic variations of comfort measures. In addition, he usually is able to interpret the woman’s needs and desires for staff members.
The feelings of a first-time father change as labor progresses. Although he is often calm at the onset of labor, feelings of fear and helplessness begin to dominate as labor becomes more active and the father realizes that labor is more work than he anticipated. Capogna, Camorcia, and Stirparo (2007) found that fathers whose partners received epidural analgesia during labor reported less anxiety and stress and more satisfaction with their childbirth experience than fathers whose partners did not. Staff members should tell the father that his presence is helpful and encourage him to be involved in the care of the woman to the extent to which he and his partner are comfortable. He should be reassured that he is not assuming the responsibility for observation and management of his partner’s labor, but that his responsibility is to support her as the labor progresses. The nurse can suggest alternative comfort measures when those he is using are no longer helpful or are rejected by his partner.
The first-time father may feel excluded as birth preparations begin during the transition phase. Once the second stage begins and birth nears, the father’s focus changes from the woman to the baby who is about to be born. The father will be exposed to many sights and smells he may never have experienced. Therefore, the nurse needs to tell him what to expect and to make him comfortable about leaving the room to regain his composure should something occur that surprises him, but make sure that someone else is available to support the woman during his absence.
Nursing actions that support the father convey several important concepts: first, that he is a person of value; second, that he can be a partner in the woman’s care; and third, that childbearing is a team effort. Box 19-6 details ways in which the nurse can support the father-partner. A well-informed father can make an important contribution to the health and well-being of the mother and child, their family interrelationship, and his self-esteem.
Labor Support by Doulas
Continuity of care has been cited by women as a critical component of a satisfying childbirth experience. A specially trained, experienced female labor attendant called a doula can meet this need. The doula provides a continual one-on-one caring presence throughout the labor and birth of the woman she is attending (Pascali-Bonaro & Kroeger, 2004). The primary role of the doula is to focus on the laboring woman and to provide physical and emotional support by using soft, reassuring words of praise and encouragement; touching; stroking; and hugging. The doula also administers comfort measures to reduce pain and enhance relaxation and coping, walks with the woman, helps her to change positions, and coaches her bearing-down efforts. Doulas provide information about labor progress and explain procedures and events. They advocate for the woman’s right to participate actively in the management of her labor.
The doula also supports the woman’s partner, who often feels unqualified to be the sole labor support and may find it difficult to watch the woman when she is experiencing pain. The doula can encourage and praise the partner’s efforts, create a partnership as caregivers, and provide respite care. Doulas also facilitate communication between the laboring woman and her partner, as well as between the couple and the health care team (Simkin & Way, 2008).
Doula support during labor is associated with decreased use of analgesia, decreased incidence of operative birth, increased incidence of spontaneous vaginal birth, and increased maternal satisfaction with the childbirth experience (Berghella et al., 2008).
The roles of the nurse and the doula are complementary. They should work together as a team, recognizing and respecting the role each plays in supporting and caring for the woman and her partner during the childbirth process. The doula provides supportive nonmedical care measures while the nurse focuses on monitoring the status of the maternal-fetal unit, implementing clinical care protocols (including pharmacologic interventions), and documenting assessment findings, actions, and responses (Adams & Bianchi, 2004; Simkin & Way, 2008).
Labor Support by Grandparents
When grandparents act as labor coaches, it is especially important to support and treat them with respect. They may have a way to deal with pain relief based on their experience. Grandparents should be encouraged to help as long as their actions do not compromise the status of the mother or the fetus. The nurse treats grandparents with dignity and respect by acknowledging the value of their contributions to parental support, and by recognizing the difficulty parents have in witnessing the woman’s discomfort or crisis. If they have never witnessed a birth, the nurse may need to provide explanations of what is happening. Many of the activities used to support fathers also are appropriate for grandparents.
Siblings During Labor and Birth
Preparing siblings for acceptance of the new child helps promote the attachment process and may help the older children accept this change. The older child or children who know themselves to be important to the family become active participants. Rehearsal for the event before labor is essential.
The age and developmental level of children influence their responses; therefore, preparation for the children to be present during labor is adjusted to meet each child’s needs. The child younger than 2 years shows little interest in pregnancy and labor. However, for the older child, such preparation may reduce fears and misconceptions. Parents need to be prepared for labor and birth themselves and feel comfortable about the process and the presence of their children. Most parents have a “feel” for their children’s maturational level and their physical and emotional ability to observe and cope with the events of the labor and birth process. Preparation can include a description of the anticipated sights, events (e.g., ROM, monitors, IV infusions), smells, and sounds; a labor and birth demonstration; a tour of the birthing unit; and an opportunity to be around a real newborn. Storybooks about the birth process can be read to or by children to prepare them for the event. Films are available for preparing preschool and school-age children to participate in the labor and birth experience. Children must learn that their mother will be working hard during labor and birth. She will not be able to talk to them during contractions. She may groan, scream, grunt, and pant at times as well as say things she would not say otherwise (e.g., “I can’t take this anymore,” “Take this baby out of me,” or “This pain is killing me”). You can tell them that labor is uncomfortable, but that their mother’s body is made for the job.
Most agencies require that a specific person be designated to watch over the children who are participating in their mother’s childbirth experience, to provide them with support, explanations, diversions, and comfort as needed. Health care providers involved in attending women during birth must be comfortable with the presence of children and the unpredictability of their questions, comments, and behaviors.
Second Stage of Labor
The second stage of labor is the stage in which the infant is born. This stage begins with full cervical dilation (10 cm) and complete effacement (100%) and ends with the baby’s birth. The force exerted by uterine contractions, gravity, and maternal bearing-down efforts facilitates achievement of the expected outcome of a spontaneous, uncomplicated vaginal birth. The median duration of second stage labor is 50 minutes in nulliparous women and 20 minutes in multiparous women. In addition to parity, maternal size and fetal weight, position, and descent influence the length of this stage. The use of epidural anesthesia during labor often increases the length of the second stage of labor because the epidural blocks or reduces the woman’s urge to bear down and limits her ability to attain an upright position to push. The upper limits for the duration of normal second stage labor are (Battista & Wing, 2007):
A prolonged second stage is diagnosed after these time limits are reached, a thorough assessment of the status of the maternal fetal unit should be made as well as a determination regarding the likely effectiveness and safety of further bearing-down efforts (Simpson et al., 2008).
The second stage of labor is composed of two phases: the latent phase and the active pushing (descent) phase. Maternal verbal and nonverbal behaviors, uterine activity, the urge to bear down, and fetal descent characterize these phases (Hanson, 2009; Simpson et al., 2008).
The latent phase is a period of rest and relative calm (i.e., “laboring down”). During this early phase the fetus continues to descend passively through the birth canal and rotate to an anterior position as a result of ongoing uterine contractions. The woman is quiet and often relaxes with her eyes closed between contractions. The urge to bear down is not strong and some women do not experience it at all or only during the acme (peak) of a contraction. Allowing a woman to rest during this phase, and waiting until the urge to push intensifies, reduces maternal fatigue, conserves energy for bearing-down efforts, and provides optimal maternal and fetal outcomes (Simpson, 2005). Although delayed pushing is associated with a longer second stage of labor, it results in a significantly higher incidence of spontaneous vaginal birth. Other benefits of delayed pushing include less FHR decelerations, fewer forceps- and vacuum-assisted births, and less perineal damage (lacerations and episiotomies). Careful monitoring with assurance of normal fetal status should be used during delayed pushing. If descent is slow and the woman becomes anxious, she should be encouraged to change positions frequently or to stand by the bedside to use the advantage of gravity and movement to facilitate descent and progress to the active pushing phase signaled by a perception of the need to bear down (Hanson, 2009). The longer length of second stage labor is not associated with poor neonatal outcome, as long as the fetal status during this time is normal (Berghella et al., 2008; Brancato, Church, & Stone, 2008; Roberts & Hanson, 2007; Simpson & James, 2005).
During the phase of active pushing (descent) the woman has strong urges to bear down as the Ferguson reflex is activated when the presenting part presses on the stretch receptors of the pelvic floor. At this point, the fetal station is usually +1 and the position is anterior. This stimulation causes the release of oxytocin from the posterior pituitary gland, which provokes stronger expulsive uterine contractions. The woman becomes more focused on bearing-down efforts, which become rhythmic. She changes positions frequently to find a more comfortable pushing position. The woman often announces the onset of contractions and becomes more vocal as she bears down. The urge to bear down intensifies as descent progresses and the presenting part reaches the perineum. The woman may be more verbal about the pain she is experiencing; she may scream or swear and may act out of control.
The nurse encourages the woman to “listen” to her body as she progresses through the phases of the second stage of labor. When a woman listens to her body to tell her when to bear down, she is using an internal locus of control and often feels more satisfied with her efforts to give birth to her baby. This enhances her sense of self-esteem and accomplishment and her efforts become more effective. Always encourage the woman’s trust in her own body and her ability to give birth to her baby. Validate the woman’s experience of pressure, stretching, and straining as normal and a signal that the descent of the fetus is progressing and that her body is capable of withstanding birth. Honestly explain what is happening and describe the progress being made.
Care Management
The only certain objective sign that the second stage of labor has begun is the inability to feel the cervix during vaginal examination, indicating that the cervix is fully dilated and effaced. The precise moment that this occurs is not easily determined because it depends on when a vaginal examination is performed to validate full dilation and effacement. This makes timing of the actual duration of the second stage difficult. Other signs that suggest the onset of the second stage include the urge to push or feeling the need to have a bowel movement. These signs commonly appear at the time the cervix reaches full dilation. However, they can appear earlier in labor. Women with an epidural block may not exhibit such signs.
Women can begin to experience an irresistible urge to bear down before full dilation. For some, this occurs as early as 5 cm dilation. This is most often related to the station of the presenting part below the level of the ischial spines of the maternal pelvis. This occurrence creates a conflict between the woman, whose body is telling her to push, and her health care providers, who believe that pushing the fetal presenting part against an incompletely dilated cervix will result in cervical edema and lacerations, as well as slow the labor progress. Evaluate the premature urge to bear down as a sign of labor progress, possibly indicating the onset of the second stage of labor. Base the timing of when a woman pushes in relation to whether her cervix is fully dilated on research evidence rather than on tradition or routine practice. Pushing with the urge to bear down at the acme of a contraction may be safe and effective for a woman if her cervix is soft, retracting, and 8 cm or more dilated and if the fetus is at +1 station and rotating to an anterior position (Roberts, 2002).
Assessment is continuous during the second stage of labor. Professional standards and agency policy determine the specific type and timing of assessments, as well as the way in which findings are documented. Signs and symptoms of impending birth (Table 19-3) may appear unexpectedly, requiring immediate action by the nurse (Box 19-7). As with the first stage of labor, care management is guided by the nursing process (see the Nursing Process box: Second Stage of Labor).
TABLE 19-3
EXPECTED MATERNAL PROGRESS IN THE SECOND STAGE OF LABOR
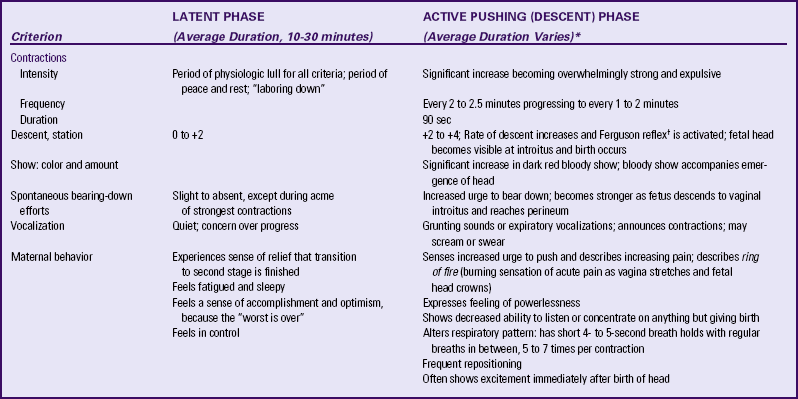
∗Duration of descent phase can vary depending on maternal parity, effectiveness of bearing-down effort, and presence of spinal anesthesia or epidural analgesia.
†Pressure of presenting part on stretch receptors of pelvic floor stimulates release of oxytocin from posterior pituitary, resulting in more intense uterine contractions.
Sources: Hanson, L. (2009). Second-stage labor care. Journal of Perinatal and Neonatal Nursing, 23(1), 31-39; Simpson, K., Cesario, S., Morin, K., Trapani, K., Mayberry, L., & Snelgrove-Clark, E. (2008). Nursing care and management of the second stage of labor: Evidence-based clinical practice guideline. (2nd ed.). Washington, DC: Association of Women’s Health, Obstetric, & Neonatal Nurses; Roberts, J. (2002). The “push” for evidence: Management of the second stage. Journal of Midwifery & Women’s Health, 47(1), 2-15; Simkin, P., & Ancheta, R. (2000). The labor progress handbook. Malden, MA: Blackwell Science.
The nurse continues to monitor maternal-fetal status and events of the second stage and provide comfort measures for the mother. This includes helping her change position; providing mouth care; maintaining clean, dry bedding; and keeping extraneous noise, conversation, and other distractions (e.g., laughing, talking of attending personnel in or outside the labor area) to a minimum. The woman is encouraged to indicate other support measures she would like (Table 19-2; Nursing Care Plan).
In the hospital, birth may occur in an LDR, LDRP, or delivery room. If the mother is to be transferred to the delivery room for birth, perform the transfer early enough to avoid rushing her. The birth area also is readied.
Preparing for Birth
No single position for childbirth exists. Labor is a dynamic, interactive process involving the woman’s uterus, pelvis, and voluntary muscles. In addition, angles between the baby and the woman’s pelvis constantly change as the infant turns and flexes down the birth canal. The woman may want to assume various positions for childbirth. She should be encouraged to change positions frequently and assisted in attaining and maintaining her position(s) of choice (Figs. 19-15 and 19-16). Supine, semirecumbent, or lithotomy positions are still widely used in Western societies despite evidence that women prefer upright positions for their bearing-down efforts and birth (Roberts & Hanson, 2007).

FIG. 19-15 A, Pushing, side-lying position. Perineal bulging can be seen. B, Pushing, semisitting position. Midwife assists mother to feel top of fetal head. (A, Courtesy Michael S. Clement, MD, Mesa, AZ. B, Courtesy Roni Wernik, Palo Alto, CA.)
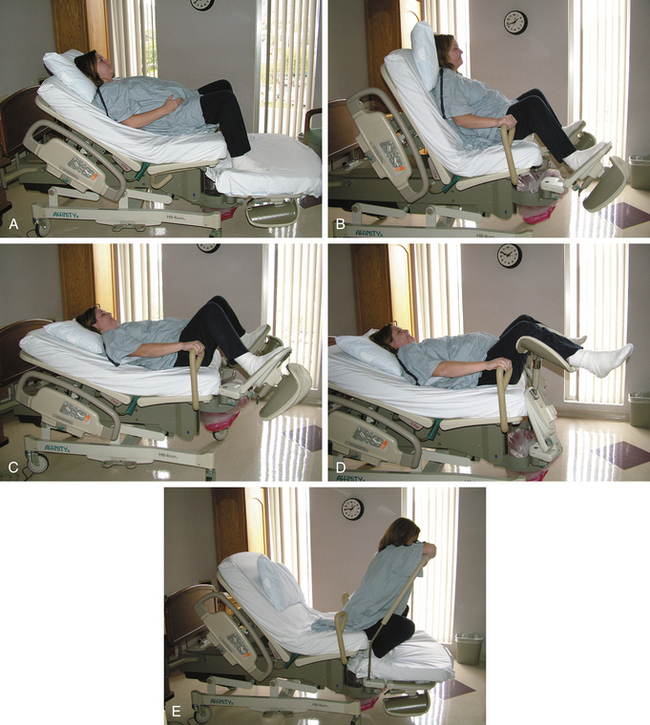
FIG. 19-16 The versatility of today’s birthing bed makes it practical in a variety of settings. Note: OB table used for lithotomy position. A, Labor bed. B, Birth chair. C, Birth bed. D, OB table. E, Squatting or birth bar. (Courtesy Julie Perry Nelson, Loveland, CO.)
Birth attendants play a major role in influencing a woman’s choice of positions for birth, with nurse-midwives tending to advocate nonlithotomy positions (e.g., upright, lateral) for the second stage of labor. The use of upright and lateral positions is associated with a shorter interval to birth, less pain and perineal damage, fewer episiotomies and abnormal FHR patterns, and
fewer operative vaginal births (Berghella et al., 2008; Roberts & Hanson, 2007; Simpson et al., 2008; Zwelling, 2010). ![]() The benefits of upright positions may be related to:
The benefits of upright positions may be related to:
• Straightening of the longitudinal axis of the birth canal and improvement in the alignment of the fetus for passage through the pelvis
• Application of gravity to direct the fetal head toward the pelvic inlet, thereby facilitating descent
• Enlargement of pelvic dimensions and restriction of the encroachment of the sacrum and coccyx into the pelvic outlet
• Increased uteroplacental circulation, resulting in more intense, efficient uterine contractions
• Enhancement of the woman’s ability to bear down effectively, thereby minimizing maternal exhaustion
Squatting is highly effective in facilitating the descent and birth of the fetus. It is one of the best and most natural positions for second stage labor and has been associated with the same benefits of other upright and lateral positions (Roberts, 2002; Simpson et al., 2008). Women should assume a modified, supported squat until the fetal head is engaged, at which time a deep squat can be used. A firm surface is required for this position, and the woman will need side support (see Fig. 19-12, A). In a birthing bed, a squat bar is available that she can use to help support herself (Fig. 19-16, E). A birth ball can also be used to help a woman maintain the squatting position. The fetus will be aligned with the birth canal, and pelvic and perineal relaxation is facilitated as she sits on the ball or holds it in front of her for support as she squats (see Box 19-5).
When a woman uses the supported standing position for bearing down, her weight is borne on both femoral heads, allowing the pressure in the acetabulum to cause the transverse diameter of the pelvic outlet to increase by up to 1 cm. This can be helpful if descent of the head is delayed because the occiput has not rotated from the lateral (transverse diameter of pelvis) to the anterior position. Birthing chairs or rocking chairs may be used to provide women with a good physiologic position to enhance bearing-down efforts during childbirth (see Box 19-5), although some women feel restricted by a chair. The upright position also provides a potential psychologic advantage in that it allows the mother to see the birth as it occurs and to maintain eye contact with the attendant.
Oversized beanbag chairs and large floor pillows may be used for both labor and birth. They can mold around and support the mother in whatever position she selects. These chairs are of particular value for mothers who wish to be actively involved in the birth process. Birthing stools can be used to support the woman in an upright position similar to squatting. Some women may feel more comfortable sitting on the toilet or commode during pushing because they are concerned about stool incontinence during this stage. Encourage them to empty their bladder to avoid the effects of a distended bladder. You must closely monitor these women, however, and remove them from the toilet before birth becomes imminent. Because sitting on chairs, stools, toilets, or commodes can increase perineal edema and blood loss, assist the woman to change her position frequently (e.g., every 10 to 15 minutes).
The side-lying, or lateral, position, with the upper part of the woman’s leg held by the nurse or coach or placed on a pillow, is an effective position for the second stage of labor (see Fig. 19-15, A and Box 19-5). Some women prefer a semisitting (semirecumbent) position instead (see Fig. 19-16, B and Box 19-5). If the semirecumbent position is used, do not force the woman’s legs against her abdomen as she bears down. This position will increase perineal stretching and the risk for perineal trauma as well as spinal and lower extremity neurologic injuries (Simpson et al., 2008). The hands-and-knees position is yet another effective position for birth (see Fig. 19-11, B and Box 19-5).
The birthing bed commonly used can be set for different positions according to the woman’s needs (Figs. 19-16 and 19-17). The woman can squat, kneel, sit, recline, or lie on her side, choosing the position most comfortable for her without having to climb into bed for the birth. At the same time, the birthing bed provides excellent exposure for examinations, electrode placement, and birth. You can position the bed for the administration of anesthesia and it is ideal to help women receiving an epidural to assume different positions to facilitate birth. You can also use the bed to transport the woman to the operating room if a cesarean birth is necessary. The woman can use squat bars, over-the-bed tables, birth balls, and pillows for support.
Bearing-Down Efforts
As the fetal head reaches the pelvic floor, most women experience the urge to bear down. Reflexively the woman will begin to exert downward pressure by contracting her abdominal muscles while relaxing her pelvic floor. This bearing down is an involuntary response to the Ferguson reflex. A strong expiratory grunt or groan (vocalization) often accompanies pushing when the woman exhales as she pushes. This natural vocalization by women during open-glottis bearing-down efforts should not be discouraged.
When coaching women to push, encourage them to push as they feel like pushing (instinctive, spontaneous pushing) rather than to give a prolonged push on command (directed, closed-glottis pushing). Prolonged breath-holding, or sustained, directed bearing down is still a common practice often beginning at 10 cm dilation and before the urge to bear down is perceived. The woman is coached to hold her breath, closing her glottis, and to push while the nurse or partner counts to 10. This method of bearing down may trigger the Valsalva maneuver, which occurs when the woman closes her glottis (closed-glottis pushing), which increases intrathoracic and cardiovascular pressure. This reduces cardiac output and decreases perfusion of the uterus and the placenta. Adverse effects associated with prolonged breath-holding and forceful pushing efforts include fetal hypoxia and subsequent acidosis, increased risk for pelvic floor damage (structural and neurogenic), and perineal trauma (Schaffer, Bloom, Casey, McIntire, Nihira, & Leveno, 2005; Simpson & James, 2005; Simpson et al., 2008). The benefits of spontaneous pushing efforts rather than sustained Valsalva pushes include less hypoxic stress for the fetus and less pelvic or perineal damage for the woman, reducing her risk for future incontinence and pelvic organ prolapse (Roberts & Hanson, 2007). In addition, these more effective bearing-down efforts conserve maternal energy and reduce the risk for operative vaginal births (Roberts, 2002; Sampselle, Miller, Luecha, Fischer, & Rosten, 2005; Simpson & James, 2005). ![]() Based on this evidence, it is essential that perinatal nurses advocate for the practice of delayed and spontaneous bearing-down efforts with the woman in an upright or lateral position (Hanson, 2009).
Based on this evidence, it is essential that perinatal nurses advocate for the practice of delayed and spontaneous bearing-down efforts with the woman in an upright or lateral position (Hanson, 2009).
A woman can become confused and anxious when she is being told to do something in conflict with what her body is telling her. Using phrases such as “You are doing so well, do it again,” “You are moving the baby down,” and “Follow what your body is telling you,” rather than “Push, push, push,” encourages a woman to feel confident in her body and what she is feeling (Hanson, 2009; Sampselle et al., 2005).
Monitor the woman’s breathing so that she does not hold her breath for more than 6 to 8 seconds at a time followed by a slight exhale (a combination of open-glottis and voluntary closed-glottis pushing). Remind her to ventilate her lungs fully by taking deep cleansing breaths before and after each contraction. Bearing down while exhaling (open-glottis pushing) and taking breaths between bearing-down efforts help to maintain adequate oxygen levels for the mother and fetus, thus enhancing fetal well-being. The active pushing phase of the second stage of labor is considered to be the most physiologically stressful part of labor. Therefore, every effort should be made to ensure that women use nondirected spontaneous pushing to conserve energy and maximize the effect of each bearing-down effort. A woman’s bearing-down efforts naturally will become more forceful and frequent as the second stage progresses to birth (Simpson et al., 2008).
A woman may reach the second stage of labor and then experience a lack of readiness to complete the process and give birth to her child. She may have doubts about her readiness to be a mother or may desire to wait for her support person or primary health care provider to arrive. Fear, anxiety, or embarrassment regarding unfamiliar or painful sensations and behaviors during pushing (e.g., sounds made, passage of stool) may be other inhibiting factors. Fear that the baby will be in danger once it emerges from the protective intrauterine environment also may be present. By recognizing that a woman may experience a need to hold back the birth of her baby, you can address the woman’s concerns and effectively coach her during this stage of labor.
To ensure the slow birth of the fetal head, encourage the woman to control the urge to bear down by coaching her to take panting breaths or exhale slowly through pursed lips as the baby’s head crowns. At this point the woman needs simple, clear directions from one person. Amnesia between contractions often occurs in the second stage; therefore, you may have to rouse the woman to get her to cooperate in the bearing-down process. Parents who have attended childbirth education classes may have devised a set of verbal cues for the laboring woman to follow.
Fetal Heart Rate and Pattern
As noted, you must check the fetal heart rate regularly (see Chapter 18 for further discussion). If the baseline rate begins to slow, if a loss of variability occurs, or if deceleration patterns develop (e.g., late, variable, or prolonged), initiate interventions promptly. Turn the woman onto her side to reduce the pressure of the uterus against the ascending vena cava and descending aorta (see Fig.19-5). Oxygen can be administered by nonrebreather mask at 8 to 10 L/min (Tucker et al., 2009). These interventions are often all that is necessary to restore a normal pattern. If the FHR and pattern do not become normal immediately, notify the primary health care provider because the woman may need medical intervention to give birth. See the Emergency box for more interventions related to abnormal FHR.
Support of the Father or Partner
During the second stage the woman needs continuous support and coaching (see Table 19-3). Because the coaching process is often physically and emotionally tiring for support persons, the nurse offers them nourishment and fluids and encourages them to take short breaks as needed (see Box 19-6). If birth occurs in an LDR or LDPR room, the support person usually wears street clothes. Instruct the support person who attends the birth in a delivery room to put on a cover gown or scrub clothes, mask, hat, and shoe covers, if required by agency policy. The nurse also specifies support measures that can be used for the laboring woman and points out areas of the room in which the partner can move freely.
Encourage partners to be present at the birth of their infants if doing so is in keeping with their cultural and personal expectations and beliefs. The presence of partners maintains the psychologic closeness of the family unit, and the partner can continue to provide the supportive care given during labor. The woman and her partner need to have an equal opportunity to initiate the attachment process with the baby.
Supplies, Instruments, and Equipment
To prepare for birth in any setting, the birthing table is usually set up during the transition phase for nulliparous women and during the active phase for multiparous women.
Prepare the birthing bed or table, and arrange instruments on the instrument table or delivery cart (Fig. 19-18). Follow standard procedures for gloving, identifying and opening sterile packages, adding sterile supplies to the instrument table, unwrapping sterile instruments, and handing them to the primary health care provider. Ready the crib or radiant warmer and equipment for the support and stabilization of the infant (Fig. 19-19).
The items used for birth may vary among different facilities; therefore, consult each facility’s procedure manual to determine the protocols specific to that facility.
The nurse estimates the time until the birth will occur and notifies the primary health care provider if he or she is not in the woman’s room. Even the most experienced nurse can miscalculate the time left before birth occurs; therefore, every nurse who attends a woman in labor must be prepared to assist with an emergency birth if the primary health care provider is not present (see Box 19-6).
Birth in a Delivery Room or Birthing Room
The woman will need assistance if she must move from the labor bed to the delivery table (Fig. 19-20). The various positions assumed for birth in a delivery room are the Sims or lateral position in which the attendant supports the upper part of the woman’s leg, the dorsal position (supine position with one hip elevated), and the lithotomy position.
The lithotomy position makes dealing with complications that arise more convenient for the primary health care provider (see Fig. 19-16, D). To place the woman in this position, bring her buttocks to the edge of the bed or table and place her legs in stirrups. Take care to pad the stirrups, to raise and place both legs simultaneously, and to adjust the shanks of the stirrups so that the calves of the legs are supported. No pressure should be placed on the popliteal space. Stirrups that are not the same height will strain ligaments in the woman’s back as she bears down, leading to considerable discomfort in the postpartum period. The lower portion of the table may be dropped down and rolled back under the table.
The maternal position for birth in a birthing room varies from a lithotomy position with the woman’s feet in stirrups or resting on footrests or with her legs held and supported by the nurse or support person, to one in which her feet rest on footrests while she holds on to a squat bar, to a side-lying position with the woman’s upper leg supported by the coach, nurse, or squat bar. Once the woman is positioned, the foot of the bed is removed so that the primary health care provider attending the birth can gain better perineal access for performing an episiotomy, delivering a large baby, using forceps or vacuum extractor, or getting access to the emerging head to facilitate suctioning. Alternately, the foot of the bed can be left in place and lowered slightly to form a ledge that allows access for birth and that also serves as a place to lay the newborn (see Fig. 19-16, A).
Once the woman is positioned for birth either in a delivery room or birthing room, the vulva and perineum are cleansed. Hospital protocols and the preferences of primary health care providers for cleansing may vary.
The nurse continues to coach and encourage the woman and monitor the fetal status (see the Nursing Process Box: Second Stage of Labor). Keep the primary health care provider informed of the fetal heart rate and pattern (Tucker et al., 2009). Prepare or obtain an oxytocic medication such as oxytocin (Pitocin) so that it is ready to be administered immediately after expulsion of the placenta. Always follow Standard Precautions as care is administered during the process of labor and birth (see Box 19-3).
In the delivery room, the primary health care provider puts on a cap, a mask that has a shield or protective eyewear, and shoe covers. After washing hands, the provider puts on a sterile gown (with waterproof front and sleeves) and sterile gloves. Nurses attending the birth also may need to wear caps, protective eyewear, masks, gowns, and gloves. The woman may then be draped with sterile drapes. In the birthing room, Standard Precautions are observed, but the amount and types of protective coverings worn by those in attendance may vary.
Maintain contact with the parents by touching, verbal comforting, describing progress, explaining the reasons for care, and sharing in the parents’ joy at the birth of their child.
Mechanism of Birth: Vertex Presentation: The three phases of the spontaneous birth of a fetus in a vertex presentation are (1) birth of the head, (2) birth of the shoulders, and (3) birth of the body and extremities (see Chapter 16).
With voluntary bearing-down efforts, the head appears at the introitus (Fig. 19-21). Crowning occurs when the widest part of the head (the biparietal diameter) distends the vulva just before birth. Immediately before birth, the perineal musculature becomes greatly distended. If an episiotomy (incision into the perineum to enlarge vaginal outlet) is necessary, it is done at this time to minimize soft-tissue damage. A local anesthetic may be administered if necessary before performing an episiotomy. Box 19-8 shows the process of normal vaginal childbirth using a series of photographs.
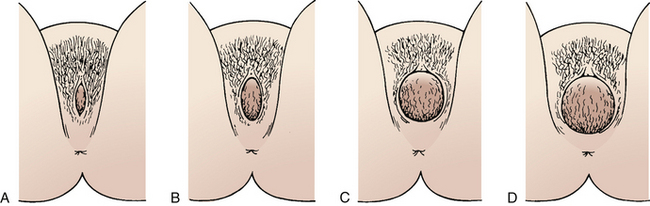
FIG. 19-21 Beginning birth with vertex presenting. A, Anteroposterior slit. B, Oval opening. C, Circular shape. D, Crowning.

FIG. 19-22 Birth of head with modified Ritgen maneuver. Note control to prevent too-rapid birth of head.
The physician or nurse-midwife may use a hands-on approach to control the birth of the head, believing that guarding the perineum results in a gradual birth that will prevent fetal intracranial injury, protect maternal tissues, and reduce postpartum perineal pain. This approach involves: (1) applying pressure against the rectum, drawing it downward to aid in flexing the head as the back of the neck catches under the symphysis pubis; (2) then applying upward pressure from the coccygeal region (modified Ritgen maneuver) (Fig. 19-22) to extend the head during the actual birth, thereby protecting the musculature of the perineum; and (3) assisting the mother with voluntary control of the bearing-down efforts by coaching her to pant while letting uterine forces expel the fetus.
Some health care providers use a hands-poised (hands-off) approach when attending a birth. In this approach, hands are prepared to place light pressure on the fetal head to prevent rapid expulsion. The provider does not place hands on the perineum or use them to assist with birth of the shoulders and body.
The hands-on and hands-poised approaches have similar results in terms of perineal and vaginal tears, but the hands-on technique is associated with a higher incidence of third-degree tears and episiotomies. In one study, the hands-poised approach resulted in fewer third-degree tears (Berghella, Baxter, & Chauhan, 2008). However, the hands-on approach may result in less perineal pain.
The umbilical cord often encircles the neck (nuchal cord) but rarely so tightly as to cause hypoxia. After the head is born, gentle palpation is used to feel for the cord. If present, the health care provider slips the cord gently over the head if possible. If the loop is tight or if there is a second loop, he or she will probably clamp the cord twice, cut between the clamps, and unwind the cord from around the neck before the birth is allowed to continue. Mucus, blood, or meconium in the nasal or oral passages may prevent the newborn from breathing. To eliminate this problem, moist gauze sponges are used to wipe the nose and mouth. A bulb syringe will be inserted first into the mouth and oropharynx and then into both nares to aspirate contents.
Fundal Pressure: Fundal pressure is the application of gentle, steady pressure against the fundus of the uterus to facilitate the vaginal birth. Historically it has been used when the administration of analgesia and anesthesia decreased the woman’s ability to push during the birth, in cases of shoulder dystocia, and when second-stage fetal bradycardia or other abnormal FHR patterns were present. Use of fundal pressure by nurses is not advised because there is no standard technique available for this maneuver. Also no current legal, professional, or regulatory standards exist for its use and no evidence related to its effectiveness in facilitating a safe vaginal birth is available (Simpson et al., 2008).![]()
Immediate Assessments and Care of the Newborn
The time of birth is the precise time when the entire body is out of the mother; you must record the time of birth. In the case of multiple births, each birth would be noted in the same way. If the newborn’s condition is not compromised, he or she may be placed on the mother’s abdomen immediately after birth and covered with a warm, dry blanket. The cord may be clamped at this time, and the primary health care provider may ask if the woman’s partner would like to cut the cord. If so, the partner is given a sterile pair of scissors and instructed to cut the cord 1 inch (2.5 cm) above the clamp.
The care given immediately after the birth focuses on assessing and stabilizing the newborn. The nurse’s main responsibility at this time is the infant, because the primary health care provider is involved with the delivery of the placenta and the care of the mother. The nurse must watch the infant for any signs of distress and initiate appropriate interventions should any appear.
Perform a brief assessment of the newborn immediately, even while the mother is holding the infant. This assessment includes assigning Apgar scores at 1 and 5 minutes after birth (see Table 24-1). Maintaining a patent airway, supporting respiratory effort, and preventing cold stress by drying and covering the newborn with a warmed blanket or placing him or her under a radiant warmer are the major priorities in terms of the newborn’s immediate care. You can postpone further examination, identification procedures, and care until later in the third stage of labor or early in the fourth stage.
Perineal Trauma Related to Childbirth
Most acute injuries and lacerations of the perineum, vagina, uterus, and their support tissues occur during childbirth. Alternative measures for perineal management, such as application of warm compresses and gentle perineal massage and stretching have been suggested to lessen the degree of perineal lacerations and trauma. Perineal massage during pregnancy has been shown to be somewhat effective for the primigravida (Beckmann & Garret (2006). There has been limited evidence, however, for the benefit of perineal measures used during the second stage of labor. In fact, research findings are mixed with some studies indicating an increased risk for perineal trauma when using these measures, whereas other studies indicate that these measures may lessen the degree of perineal lacerations (Simpson et al., 2008). ![]() Therefore, these measures should be avoided during labor until further research can provide evidence of their benefit (Albers, Sedler, Bedrick, Teaf, & Peralta, 2005; Berghella et al., 2008).
Therefore, these measures should be avoided during labor until further research can provide evidence of their benefit (Albers, Sedler, Bedrick, Teaf, & Peralta, 2005; Berghella et al., 2008).
Some degree of damage occurs during every birth to the soft tissues of the birth canal and adjacent structures. The tendency to sustain lacerations varies with each woman; that is, the soft tissue in some women may be less distensible. Damage usually is more pronounced in nulliparous women because the tissues are firmer and more resistant than are those in multiparous women. Heredity is also a factor. For example, the tissue of light-skinned women, especially those with reddish hair, is not as readily distensible as that of darker-skinned women, and healing may be less efficient. Other risk factors associated with perineal trauma include maternal position, pelvic inadequacy (e.g., narrow subpubic arch with a constricted outlet), fetal malpresentation and position (e.g., breech, occiput posterior position), large (macrosomic) infants, use of forceps or vacuum to facilitate birth, prolonged second stage of labor, and rapid labor in which there is insufficient time for the perineum to stretch.
Some injuries to the supporting tissues, whether they are acute or nonacute and whether they were repaired or not, may lead to genitourinary and sexual problems later in life (e.g., pelvic relaxation, uterine prolapse, cystocele, rectocele, dyspareunia, urinary and bowel dysfunction) (See Chapter 11). Use of Kegel exercises in the prenatal and postpartum periods improves and restores the tone and strength of the perineal muscles (See Chapter 4). Health practices, including good nutrition and appropriate hygienic measures, help maintain the integrity and suppleness of the perineal tissues, enhance healing, and prevent infection.
Perineal Lacerations: Perineal lacerations usually occur as the fetal head is being born. The extent of the laceration is defined in terms of its depth:
First degree: Laceration that extends through the skin and structures superficial to muscles
Second degree: Laceration that extends through muscles of the perineal body
Third degree: Laceration that continues through the anal sphincter muscle
Fourth degree: Laceration that also involves the anterior rectal wall
Perineal injury often is accompanied by small lacerations on the medial surfaces of the labia minora below the pubic rami and to the sides of the urethra (periurethral) and clitoris. Lacerations in this highly vascular area often result in profuse bleeding. Third- and fourth-degree lacerations must be carefully repaired so that the woman retains fecal continence. Simple perineal injuries usually heal without permanent disability, regardless of whether they were repaired. However, repairing a new perineal injury to prevent future complications is easier than correcting long-term damage.
Vaginal and Urethral Lacerations: Vaginal lacerations often occur in conjunction with perineal lacerations. Vaginal lacerations tend to extend up the lateral walls (sulci) and, if deep enough, involve the levator ani muscle. Additional injury may occur high in the vaginal vault near the level of the ischial spines. Vaginal vault lacerations are often circular and may result from use of forceps to rotate the fetal head, rapid fetal descent, or precipitous birth.
Cervical Injuries: Cervical injuries occur when the cervix retracts over the advancing fetal head. These cervical lacerations occur at the lateral angles of the external os. Most lacerations are shallow and bleeding is minimal. Larger lacerations may extend to the vaginal vault or beyond it into the lower uterine segment; serious bleeding may occur. Extensive lacerations may follow hasty attempts to enlarge the cervical opening artificially or to deliver the fetus before full cervical dilation is achieved. Injuries to the cervix can have adverse effects on future pregnancies and childbirths.
Episiotomy: An episiotomy is an incision made in the perineum to enlarge the vaginal outlet (see Fig. 19-23). It is performed more commonly in the United States and Canada than in Europe. The side-lying position for birth, used routinely in Europe, causes less tension on the perineum, making possible a gradual stretching of the perineum with fewer indications for episiotomies.
Different types of episiotomies are performed, depending on the site and direction of the incision (see Fig. 19-23); the type that provides the best outcome is unknown (Berghella et al., 2008). Midline (median) episiotomy is most commonly used in the United States. It is effective, easily repaired, and generally the least painful. However, midline episiotomies also are associated with a higher incidence of third- and fourth-degree lacerations. Sphincter tone is usually restored after primary healing and a good repair. Mediolateral episiotomy is used in operative births when the need for posterior extension is likely. Although a fourth-degree laceration may be prevented, a third-degree laceration may occur. The blood loss is also greater and the repair more difficult and painful than with midline episiotomies. It is also more painful in the postpartum period, and the pain lasts longer.
Routine use of episiotomies has declined in the United States from 55.6% in 1990 to 19.3% in 2005 (DeFrances, Cullen, & Kozak, 2007). The practice in many settings now is to support the perineum manually during birth and allow the perineum to tear rather than perform an episiotomy. Tears are often smaller than an episiotomy, are repaired easily or not at all, and heal quickly. Episiotomies are associated with more posterior perineal trauma, suturing and healing complications, and later pain with intercourse. Therefore, episiotomy should be avoided if at all possible (Berghella et al., 2008).![]()
Third Stage of Labor
The third stage of labor lasts from the birth of the baby until the placenta is expelled. The goal in the management of the third stage of labor is the prompt separation and expulsion of the placenta, achieved in the easiest, safest manner. The third stage is generally by far the shortest stage of labor (see the Nursing Process box: Third Stage of Labor). The placenta is usually expelled within 10 to 15 minutes after the birth of the baby. If the third stage has not been completed within 30 minutes, the placenta is considered to be retained and interventions to hasten its separation and expulsion are usually instituted (Battista & Wing, 2007).
Under normal circumstances the placenta is attached to the decidual layer of the basal plate’s thin endometrium by numerous fibrous anchor villi—much in the same way a postage stamp is attached to a sheet of postage stamps. After the birth of the fetus, strong uterine contractions and the sudden decrease in uterine size cause the placental site to shrink. This causes the anchor villi to break and the placenta to separate from its attachments. Normally the first few strong contractions that occur after the baby’s birth cause the placenta to shear away from the basal plate. A placenta cannot detach itself from a flaccid (relaxed) uterus because the placental site is not reduced in size.
Placental Separation and Expulsion
Depending on preference, the primary health care provider may use either a passive or an active approach to manage the third stage of labor. Passive management involves patiently watching for signs that the placenta has spontaneously separated from the uterine wall (see Nursing Process box: Third Stage of Labor). Active management of third stage labor involves administering oxytocic medication (e.g., oxytocin [Pitocin]) to hasten placental separation in order to decrease the incidence of postpartum hemorrhage and reduce total blood loss. However, the active approach has not been found to be superior in all studies of third stage labor management (Kilpatrick & Garrison, 2007).
To assist in the delivery of the placenta, the woman is instructed to push when signs of separation have occurred (Fig. 19-24). If possible, the woman should expel the placenta during a uterine contraction. Alternate compression and elevation of the fundus, plus minimal, controlled traction on the umbilical cord, may also be used to facilitate delivery of the placenta and amniotic membranes. Oxytocics are usually administered after the placenta is removed because they stimulate the uterus to contract, thereby helping to prevent hemorrhage (see the Nursing Process box: Third Stage of Labor.)
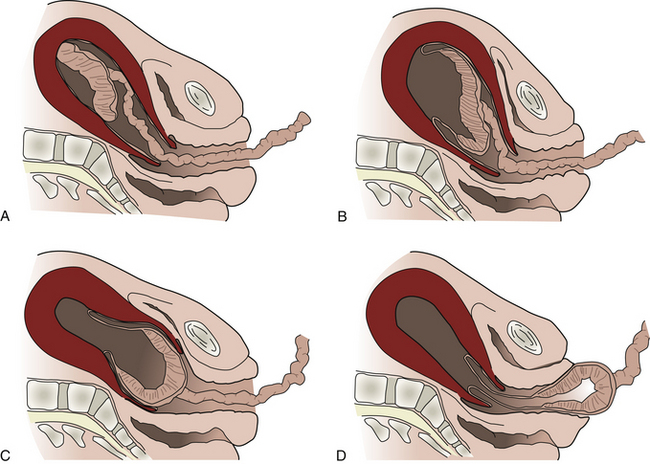
FIG. 19-24 Third stage of labor. A, Placenta begins to separate in central portion, accompanied by retroplacental bleeding. Uterus changes from discoid to globular shape. B, Placenta completes separation and enters lower uterine segment. Uterus has globular shape. C, Placenta enters vagina, cord is seen to lengthen, and there may be an increase in bleeding. D, Expulsion (delivery) of placenta and completion of third stage.
Whether the placenta first appears by its shiny fetal surface (Schultze mechanism) or turns to show its dark roughened maternal surface first (Duncan mechanism) is of no clinical importance.
After the placenta and the amniotic membranes emerge, the primary health care provider examines them for intactness to ensure that no portion remains in the uterine cavity (i.e., no fragments of the placenta or membranes are retained) (Fig. 19-25).
When the third stage of labor has been completed the primary health care provider examines the woman for any perineal, vaginal, or cervical lacerations requiring repair. If an episiotomy was performed, it will be sutured. Immediate repair promotes healing, limits residual damage, and decreases the possibility of infection. The woman usually feels some discomfort while the primary health care provider carries out the postbirth vaginal examination. Help the woman to use breathing
and relaxation or distraction techniques to assist her in dealing with the discomfort. During this time the nurse performs a quick assessment of the newborn’s physical condition, weighs the baby, and places matching identification bands on baby and mother. The baby may also receive eye prophylaxis and a vitamin K injection at this time.
After any necessary repairs have been completed, cleanse the vulvar area gently with warm water or normal saline, and apply a perineal pad or an ice pack to the perineum. Reposition the birthing bed or table, and lower the woman’s legs simultaneously from the stirrups if she gave birth in a lithotomy position. Remove any drapes, and place dry linen under the woman’s buttocks. Provide the woman with a clean gown and a blanket, which is warmed, if needed.
The nursing process continues to be used as a framework to manage nursing care during the third stage of labor (see the Nursing Process box: Third Stage of Labor).
Some women and their families may have culturally based beliefs regarding the care of the placenta and the manner of its disposal after birth, viewing the care and disposal of the placenta as a way of protecting the newborn from bad luck and illness. In Spanish the placenta is referred to as el compañero or “the companion of the child” (Callister, 2008). Requests by the woman to take the placenta home and dispose of it according to her customs sometimes conflict with health care agency policies, especially those related to infection control and the disposal of biologic wastes. Many cultures follow specific rules regarding the disposal of the placenta in terms of method (burning, drying, burying, eating), site for disposal (in or near the home), and timing of disposal (immediately after birth, time of day, astrologic signs). Disposal rituals may vary according to the gender of the child and the length of time before another child is desired. Some cultures believe that eating the placenta is a means of restoring a woman’s well-being after birth or ensuring high-quality breast milk. Health care providers can provide culturally sensitive health care by encouraging women and their families to express their wishes regarding the care and disposal of the placenta and by establishing a policy to fulfill these requests (D’Avanzo, 2008).
Fourth Stage of Labor
The first 1 to 2 hours after birth, sometimes called the fourth stage of labor, is a crucial time for mother and newborn. Both are not only recovering from the physical process of birth but are also becoming acquainted with each other and additional family members. During this time maternal organs undergo their initial readjustment to the nonpregnant state, and the functions of body systems begin to stabilize.
In most hospitals the mother remains in the labor and birth area during this recovery time. In an institution where LDR rooms are used, the woman stays in the same room where she gave birth. In traditional settings, women are taken from the delivery room to a separate recovery area for observation. Arrangements for care of the newborn vary during the fourth stage of labor. In many settings the baby remains at the mother’s bedside, and the labor or birth nurse cares for both of them. In other institutions the baby is taken to the nursery for several hours of observation after an initial bonding period with the parents, siblings, and perhaps other family members (Fig. 19-26).
Assessment
If the recovery nurse has not previously cared for the new mother, she begins with an oral report from the nurse who attended the woman during labor and birth and a review of the prenatal, labor, and birth records. Of primary importance are conditions that could predispose the mother to hemorrhage, such as precipitous labor, a large baby, grand multiparity (i.e., having given birth to six or more viable infants), induced labor, or a magnesium infusion during labor. For healthy women, hemorrhage is the most dangerous potential complication during the fourth stage of labor.
During the first hour following birth, the mother is assessed frequently. Box 19-9 describes the physical assessment of the mother during the fourth stage of labor. All factors except temperature are assessed every 15 minutes for 1 hour. Temperature is assessed at the beginning and after the first hour of the recovery period. After the fifth 15-minute assessment (which completes the first hour of recovery), if all parameters have stabilized within the normal range, the process is usually repeated once in the second hour.
Postanesthesia Recovery
The woman who has given birth by cesarean or has received regional anesthesia for a vaginal birth requires special attention during the recovery period. Obstetric recovery areas are held to the same standard of care that would be expected of any other postanesthesia recovery (PAR) unit (American Academy of Pediatrics [AAP] & American College of Obstetricians and Gynecologists [ACOG], 2007). A PAR score is determined for each woman on arrival and is updated as part of every 15-minute assessment. Components of the PAR score include activity, respirations, blood pressure, level of consciousness, and color.
If the woman received general anesthesia, she should be awake and alert and oriented to time, place, and person. Her respiratory rate should be within normal limits, and her oxygen saturation level at least 95%, as measured by a pulse oximeter. If
the woman received epidural or spinal anesthesia, she should be able to raise her legs, extended at the knees, off the bed, or flex her knees, place her feet flat on the bed, and raise her buttocks well off the bed. The numb or tingling, prickly sensation should be entirely gone from her legs. The length of time required to recover from regional anesthesia varies greatly. Often it takes several hours for these anesthetic effects to disappear completely.
Care of the New Mother
Restriction of food and fluid intake and the loss of fluids (blood, perspiration, or emesis) during labor cause many women to be very hungry and thirsty soon after birth. In the absence of complications, a woman who has given birth vaginally; has recovered from the effects of the anesthetic; and has stable vital signs, a firm uterus, and small to moderate lochial flow may have fluids and a regular diet as desired (AAP & ACOG, 2007). In the immediate postpartum period, women who give birth by cesarean are usually restricted to clear liquids and ice chips.
As soon as they have had a chance to bond with the baby and eat, most new mothers are ready for a nap, or at least a quiet period of rest. Following this rest period, the woman may want to shower and change clothes. Most new mothers are capable of self-management or are assisted in these activities by family members or support persons.
Care of the Family
Most parents enjoy being able to handle, hold, explore, and examine the baby immediately after birth. Both parents can assist with the thorough drying of the infant. Usually the infant is wrapped in a receiving blanket and given to the mother or father/partner to hold. If skin-to-skin contact is desired, place the unwrapped infant on the woman’s chest or abdomen and then cover the baby with a warm blanket. Holding the newborn next to her skin helps the mother maintain the baby’s body heat and provides skin-to-skin contact. Stockinette caps are often used to keep the newborn’s head warm and prevent heat loss.
Many women wish to begin breastfeeding their newborns at this time to take advantage of the infant’s alert state (first period of reactivity) and to stimulate the production of oxytocin that promotes contraction of the uterus and prevents hemorrhaged. In Baby Friendly Hospitals, breastfeeding is initiated within the first hour after birth. Some women prefer to wait to breastfeed until they have time to rest. In some cultures, however (e.g., Vietnamese and Hispanic), breastfeeding is not acceptable to some women until the milk comes in.
Family-Newborn Relationships
The woman’s reaction to the sight of her newborn may range from excited outbursts of laughing, talking, and even crying to apparent apathy. A polite smile and nod may be her only acknowledgment of the comments of nurses and the primary health care provider. Occasionally the reaction is one of anger or indifference; the woman turns away from the baby, concentrates on her own pain, and sometimes makes hostile comments. These varied reactions can arise from pleasure, exhaustion, or deep disappointment. When evaluating parent-newborn interactions after birth, the nurse should consider the cultural characteristics of the woman and her family and the expected behaviors of that culture. In some cultures the birth of a male child is preferred, and women may grieve when a female child is born (D’Avanzo, 2008).
Whatever the reaction and its cause, the woman needs continuing acceptance and support from all staff. Make a notation regarding the parents’ reaction to the newborn in the recovery record. Assess this reaction by asking yourself such questions as, “How do the parents look?” “What do they say?” “What do they do?” Conduct further assessment of the parent-newborn relationship as you give care during the period of recovery. This assessment is especially important if you notice warning signs (e.g., passive or hostile reactions to the newborn, disappointment with gender or appearance of the newborn, absence of eye contact, or limited interaction of parents with each other) immediately after birth. Nurses often find it helpful to discuss warning signs with the woman’s primary health care provider.
Siblings, who may have appeared only remotely interested in the final phases of the second stage, tend to experience renewed interest and excitement when the newborn appears. They can be encouraged to hold the baby (see Fig. 19-26).
Parents usually respond to praise of their newborn. Many need to be reassured that the dusky appearance of their baby’s extremities immediately after birth is normal until circulation is well established. If appropriate, explain the reason for the molding of the newborn’s head. Communicate information about hospital routine. Recognize, however, that the cultural background of the parents may influence their expectations regarding the care and handling of their newborn immediately after birth. For example, some traditional Southeast Asians believe that the head should not be touched because it is the most sacred part of a person’s body. They also believe that praise of the baby is dangerous because jealous spirits may then cause the baby harm or take it away (D’Avanzo, 2008). Hospital staff members, by their interest and concern, can provide the environment for making this a satisfying experience for parents, family, and significant others.
KEY POINTS
• The onset of labor may be difficult to determine for both nulliparous and multiparous women.
• The familiar environment of her home is most often the ideal place for a woman during the latent phase of the first stage of labor.
• The nurse assumes much of the responsibility for assessing the progress of labor and for keeping the primary health care provider informed about progress in labor and deviations from expected findings.
• The fetal heart rate and pattern reveal the fetal response to the stress of the labor process.
• Assessment of the laboring woman’s urinary output and bladder is critical to ensure her progress and to prevent injury to the bladder.
• Regardless of the actual labor and birth experience, the woman’s or couple’s perception of the birth experience is most likely to be positive when events and performances are consistent with expectations, especially in terms of maintaining control and adequacy of pain relief.
• The woman’s level of anxiety may increase when she does not understand what is being said to her about her labor because of the medical terminology used or because of a language barrier.
• Coaching, emotional support, and comfort measures assist the woman to use her energy constructively in relaxing and working with the contractions.
• The progress of labor is enhanced when a woman changes her position frequently during the first stage of labor.
• Doulas provide a continuous, supportive presence during labor that can have a positive effect on the process of childbirth and its outcome.
• The cultural beliefs and practices of a woman and her significant others, including her partner, can have a profound influence on their approach to labor and birth.
• Siblings present for labor and birth need preparation and support for the event.
• Women with a history of sexual abuse often experience profound stress and anxiety during childbirth.
• Inability to palpate the cervix during vaginal examination indicates that complete effacement and full dilation have occurred and is the only certain, objective sign that the second stage has begun.
• Women may have an urge to bear down at various times during labor; for some it may be before the cervix is fully dilated and for others it may not occur until the active phase of the second stage of labor.
• When encouraged to respond to the rhythmic nature of the second stage of labor, the woman normally changes body positions, bears down spontaneously, and vocalizes (open-glottis pushing) when she perceives the urge to push (Ferguson reflex).
• Women should bear down several times during a contraction using the open-glottis pushing method. They should avoid sustained closed-glottis pushing because this will inhibit oxygen transport to the fetus.
• Nurses can use the role of advocate to prevent routine use of episiotomy and to reduce the incidence of lacerations by empowering women to take an active role in their birth and by educating health care providers about approaches to managing childbirth that reduce the incidence of perineal trauma.
• Objective signs indicate that the placenta has separated and is ready to be expelled; excessive traction (pulling) on the umbilical cord before the placenta has separated can result in maternal injury.
• During the fourth stage of labor, the woman’s fundal tone, lochial flow, and vital signs should be assessed frequently to ensure that she is physically recovering well after giving birth.
• Most parents/families enjoy being able to handle, hold, explore, and examine the baby immediately after the birth.
![]() Audio Chapter Summaries Access an audio summary of the Key Points on
Audio Chapter Summaries Access an audio summary of the Key Points on ![]()