Assessment and Health Promotion
• Identify the structures and functions of the female reproductive system.
• Describe the menstrual cycle in relation to hormonal, ovarian, and endometrial response.
• Review the four phases of the sexual response cycle.
• Analyze barriers that may affect a woman’s decision to seek health care.
• Investigate adaptation of the history and physical examination for women with special needs.
• Examine signs of abuse, screening, and referral to community agencies.
• Describe the history and physical examination.
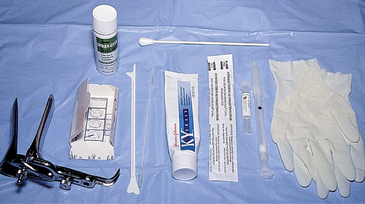
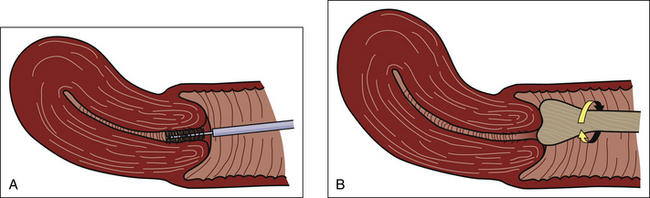
• Identify the steps for assisting with and collecting specimens for Papanicolaou (Pap) testing.
• Review client teaching of breast self-examination.
• Analyze conditions that increase health risks for women across the life span.
• Describe anticipatory guidance that prevents disease, promotes health and self-management.
• Outline health-screening and immunization recommendations for women across the life span.
Most females initially enter the health care system because of a woman’s health-related concern such as the need for a Pap test, vaginal infection, irregular menses, contraceptive needs, or pregnancy. It is important for health care providers to recognize the need for health promotion, health maintenance, and disease prevention and to offer these services across the life span of women.
This chapter reviews female anatomy and physiology including the menstrual cycle. Physical assessment and screening for disease prevention for women are presented. Barriers to seeking health care and an overview of conditions that increase health risks across the life span such as cardiovascular disease, obesity, and nutritional deficiencies are described. Anticipatory guidance suggestions including nutrition, exercise, and health screenings for women across the life span are discussed.
Female Reproductive System
The female reproductive system consists of external structures visible from the pubis to the perineum and internal structures located in the pelvic cavity. The external and internal female reproductive structures develop and mature in response to estrogen and progesterone, starting in fetal life and continuing through puberty and the childbearing years. Reproductive structures atrophy with age or in response to a decrease in ovarian hormone production. A complex nerve and blood supply supports the functions of these structures. The appearance of the external genitals varies greatly among women. Heredity, age, race, and the number of children a woman has borne influence the size, shape, and color of her external organs.
External Structures
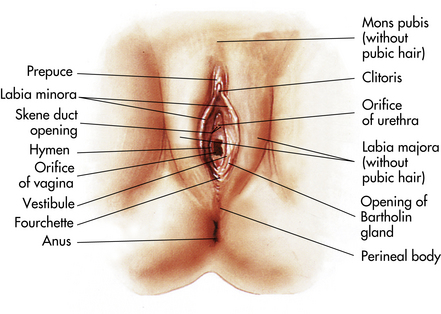
The external genital organs, or vulva, include all structures visible externally from the pubis to the perineum: the mons pubis, the labia majora, the labia minora, the clitoris, the vestibular glands, the vaginal vestibule, the vaginal orifice, and the urethral opening. The external genital organs are illustrated in Figure 4-1. The mons pubis is a fatty pad that lies over the anterior surface of the symphysis pubis. In the postpubertal female, the mons is covered with coarse, curly hair. The labia majora are two rounded folds of fatty tissue covered with skin that extend downward and backward from the mons pubis. The labia are highly vascular structures whose outer surfaces develop hair after puberty. They protect the inner vulvar structures. The labia minora are two flat reddish folds of tissue visible when the labia majora are separated. No hair follicles are in the labia minora, but many sebaceous follicles and a few sweat glands are present. The interior of the labia minora is composed of connective tissue and smooth muscle and supplied with extremely sensitive nerve endings. Anteriorly, the labia minora fuse to form the prepuce (hoodlike covering of the clitoris) and the frenulum (fold of tissue under the clitoris). The labia minora join to form a thin flat tissue called the fourchette underneath the vaginal opening at midline. The clitoris is located underneath the prepuce. It is a small structure composed of erectile tissue with numerous sensory nerve endings. During sexual arousal the clitoris increases in size.
The vaginal vestibule is an almond-shaped area enclosed by the labia minora that contains openings to the urethra, Skene glands, vagina, and Bartholin glands. The urethra is not a reproductive organ but is considered here because of its location. It usually is found about 2.5 cm below the clitoris. Skene glands are located on each side of the urethra and produce mucus, which aids in lubrication of the vagina. The vaginal opening is in the lower portion of the vestibule and varies in shape and size. The hymen, a connective tissue membrane, surrounds the vaginal opening. It can be perforated during strenuous exercise, insertion of tampons, masturbation, and vaginal intercourse. Bartholin glands (see Fig. 4-1) lie under the constrictor muscles of the vagina and are located posteriorly on the sides of the vaginal opening, although the ductal openings are usually not visible. During sexual arousal, the glands secrete a clear mucus to lubricate the vaginal introitus.
The area between the fourchette and the anus is the perineum, a skin-covered muscular area that covers the pelvic structures. The perineum forms the base of the perineal body, a wedge-shaped mass that serves as an anchor for the muscles, fascia, and ligaments of the pelvis. The pelvic organs are supported by muscles and ligaments that form a sling.
Internal Structures
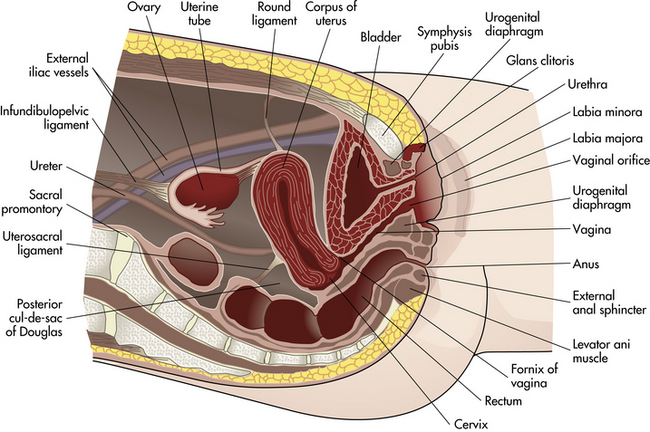
The internal structures include the vagina, the uterus, the uterine tubes, and the ovaries. The vagina is a fibromuscular, collapsible tubular structure that extends from the vulva to the uterus and lies between the bladder and rectum. During the reproductive years the mucosal lining is arranged in transverse folds called rugae. These rugae allow the vagina to expand during childbirth. Estrogen deprivation that occurs after childbirth, during lactation, and at menopause causes dryness and thinning of the vaginal walls and smoothing of the rugae. The vagina, particularly the lower segment, has few sensory nerve endings. Vaginal secretions are slightly acidic (pH 4 to 5) so that vaginal susceptibility to infections is reduced. The vagina serves as a passageway for menstrual flow, as a female organ of copulation, and as a part of the birth canal for vaginal childbirth. The uterine cervix projects into a blind vault at the upper end of the vagina. There are anterior, posterior, and lateral pockets called fornices (singular, fornix) that surround the cervix. The internal pelvic organs can be palpated through the thin walls of these fornices.
The uterus is a muscular organ shaped like an upside-down pear that sits midline in the pelvic cavity between the bladder and rectum and above the vagina. Four pairs of ligaments support the uterus: the cardinal, the uterosacral, the round, and the broad. Single anterior and posterior ligaments also support the uterus. The cul-de-sac of Douglas is a deep pouch, or recess, posterior to the cervix formed by the posterior ligament.
The uterus is divided into two major parts, an upper triangular portion called the corpus and a lower cylindric portion called the cervix (Fig. 4-2). The fundus is the dome-shaped top of the uterus and is the site at which the uterine tubes enter the uterus. The isthmus (lower uterine segment) is a short, constricted portion that separates the corpus from the cervix.
The uterus serves for reception, implantation, retention, and nutrition of the fertilized ovum and later of the fetus during pregnancy, and for expulsion of the fetus during childbirth. It also is responsible for cyclic menstruation.
The uterine wall comprises three layers: the endometrium, the myometrium, and part of the peritoneum (membrane that covers the abdominal wall). The endometrium is a highly vascular lining made up of three layers, the outer two of which are shed during menstruation. The myometrium is made up of layers of smooth muscles that extend in three different directions (longitudinal, transverse, and oblique) (Fig. 4-3). Longitudinal fibers of the outer myometrial layer are found mostly in the fundus, and this arrangement assists in expelling the fetus during the birth process. The middle layer contains fibers from all three directions, which form a figure-eight pattern encircling large blood vessels. These fibers assist in ligating blood vessels after childbirth and control blood loss. Most of the circular fibers of the inner myometrial layer are around the site where the uterine tubes enter the uterus and around the internal cervical os (opening). These fibers help keep the cervix closed during pregnancy and prevent menstrual blood from flowing back into the uterine tubes during menstruation.
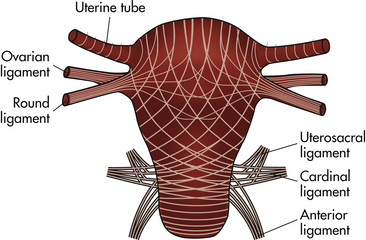
FIG. 4-3 Schematic arrangement of directions of muscle fibers. Note that uterine muscle fibers are continuous with supportive ligaments of uterus.
The cervix is made up of mostly fibrous connective tissues and elastic tissue, making it possible for the cervix to stretch during vaginal childbirth. The opening between the uterine cavity and the canal that connects the uterine cavity to the vagina (endocervical canal) is the internal os. The narrowed opening between the endocervix and the vagina is the external os, a small circular opening in women who have never been pregnant. The cervix feels firm (like the end of a nose) with a dimple in the center, which marks the external os.
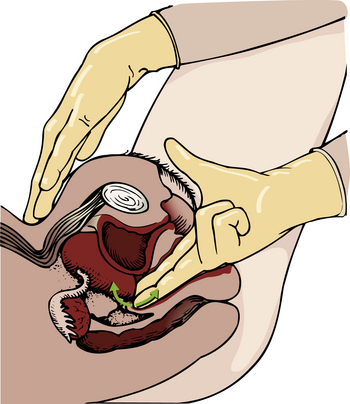
The outer cervix is covered with a layer of squamous epithelium. The mucosa of the cervical canal is covered with columnar epithelium and contains numerous glands that secrete mucus in response to ovarian hormones. The squamocolumnar junction, where the two types of cells meet, is usually located just inside the cervical os. This junction also is called the transformation zone, the most common site for neoplastic changes (see Fig. 11-12); cells from this site are scraped for the Pap test (see later discussion).
The uterine tubes (fallopian tubes) attach to the uterine fundus. The tubes are supported by the broad ligaments and range from 8 to 14 cm in length. The tubes are divided into four sections: the interstitial portion is closest to the uterus; the isthmus and the ampulla are the middle portions; and the infundibulum is closest to the ovary. The uterine tubes form passages between the ovaries and the uterus for the passage of the ovum. The infundibulum has fimbriated ends, which pull the ovum into the tube. The ovum is pushed along the tubes to the uterus by rhythmic contractions of the muscles of the tubes and by the current that is produced by the movement of the cilia that line the tubes. The ovum is usually fertilized by the sperm in the ampulla portion of one of the tubes.
The ovaries are almond-shaped organs located on each side of the uterus below and behind the uterine tubes. During the reproductive years they are approximately 3 cm long, 2 cm wide, and 1 cm thick; they diminish in size after menopause. Before menarche each ovary has a smooth surface; after menarche they become nodular because of repeated ruptures of follicles at ovulation. The two functions of the ovaries are ovulation and hormone production. Ovulation is the release of a mature ovum from the ovary at intervals (usually monthly). Estrogen, progesterone, and androgen are the hormones produced by the ovaries.
The Bony Pelvis
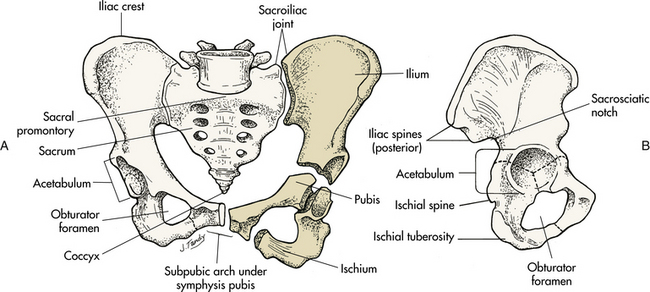
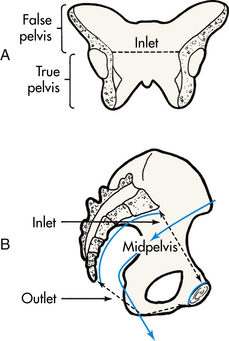
The bony pelvis serves three primary purposes: protection of the pelvic structures, accommodation of the growing fetus during pregnancy, and anchorage of the pelvic support structures. Two innominate (hip) bones (consisting of ilium, ischium, and pubis), the sacrum, and the coccyx make up the four bones of the pelvis (Fig. 4-4). Cartilage and ligaments form the symphysis pubis, the sacrococcygeal joint, and two sacroiliac joints that separate the pelvic bones. The pelvis is divided into two parts: the false pelvis and the true pelvis (Fig. 4-5). The false pelvis is the upper portion above the pelvic brim or inlet. The true pelvis is the lower, curved bony canal, which includes the inlet, the cavity, and the outlet through which the fetus passes during vaginal birth. The upper portion of the outlet is at the level of the ischial spines, and the lower portion is at the level of the ischial tuberosities and the pubic arch (see Fig. 4-4). Variations that occur in the size and shape of the pelvis are usually due to age, race, and sex. Pelvic ossification is complete at about age 20 years.
Breasts
The breasts are paired mammary glands located between the second and sixth ribs (Fig. 4-6). About two thirds of the breast overlie the pectoralis major muscle, between the sternum and midaxillary line, with an extension to the axilla referred to as the tail of Spence. The lower third of the breast overlies the serratus anterior muscle. The breasts are attached to the muscles by connective tissue or fascia.
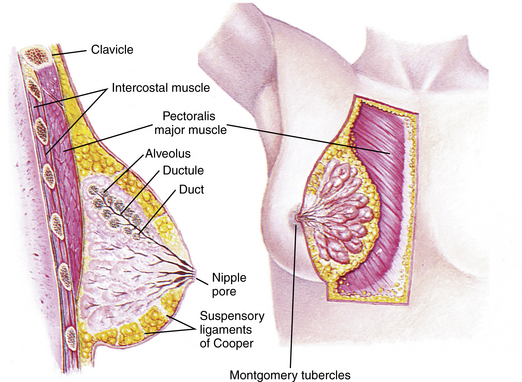
FIG. 4-6 Anatomy of the breast, showing position and major structures. (Adapted from Seidel, H., et al. [2011]. Mosby’s guide to physical examination [7th ed.]. St. Louis: Mosby.)
The breasts of healthy mature women are approximately equal in size and shape, but often are not absolutely symmetric. The size and shape vary depending on the woman’s age, heredity, and nutrition. However, the contour should be smooth, with no retractions, dimpling, or masses. Estrogen stimulates growth of the breast by inducing fat deposition in the breasts, development of stromal tissue (i.e., increase in its amount and elasticity), and growth of the extensive ductile system. Estrogen also increases the vascularity of breast tissue.
Once ovulation begins in puberty, progesterone levels increase. The increase in progesterone causes maturation of mammary gland tissue, specifically the lobules and acinar structures. During adolescence, fat deposition and growth of fibrous tissue contribute to the increase in the gland’s size. Full development of the breasts is not achieved until after the end of the first pregnancy or in the early period of lactation.
Findings from several studies using ultrasound imaging to investigate the anatomy of the breast found differences from previous descriptions (Geddes, 2007; Love & Barsky, 2004; Ramsay, Kent, Hartmann, & Hartmann, 2005). The following description incorporates these findings. Each mammary gland is made of a number of lobes that are divided into lobules. Lobules are clusters of acini. An acinus is a saclike terminal part of a compound gland emptying through a narrow lumen or duct. The acini are lined with epithelial cells that secrete colostrum and milk. Just below the epithelium is the myoepithelium (myo, or muscle), which contracts to expel milk from the acini.
The ducts from the clusters of acini that form the lobules merge to form larger ducts draining the lobes. Ducts from the lobes converge in a single nipple (mammary papilla) surrounded by an areola. The anatomy of the ducts is similar for each breast but varies among women. Protective fatty tissue surrounds the glandular structures and ducts. Cooper’s ligaments, or fibrous suspensory, separate and support the glandular structures and ducts. Cooper’s ligaments provide support to the mammary glands while permitting their mobility on the chest wall (see Fig. 4-6). The round nipple is usually slightly elevated above the breast. On each breast the nipple projects slightly upward and laterally. It contains 4 to 20 openings from the milk ducts. The nipple is surrounded by fibromuscular tissue and covered by wrinkled skin (the areola). Except during pregnancy and lactation, there is usually no discharge from the nipple.
The nipple and surrounding areola are usually more deeply pigmented than the skin of the breast. The rough appearance of the areola is caused by sebaceous glands directly beneath the skin called Montgomery tubercles. These glands secrete a fatty substance, thought to lubricate the nipple. Smooth muscle fibers in the areola contract to stiffen the nipple to make it easier for the breastfeeding infant to grasp.
Besides their function of lactation, breasts function as organs for sexual arousal in the mature adult.
The vascular supply to the mammary gland is abundant. In the nonpregnant state, the skin has no obvious vascular pattern. The normal skin is smooth without tightness or shininess. The skin covering the breasts contains an extensive superficial lymphatic network that serves the entire chest wall and is continuous with the superficial lymphatics of the neck and abdomen. In the deeper portions of the breasts, the lymphatics form a rich network as well. The primary deep lymphatic pathway drains laterally toward the axillae.
The breasts change in size and nodularity in response to cyclic ovarian changes throughout reproductive life. Increasing levels of both estrogen and progesterone in the 3 to 4 days before menstruation increase the vascularity of the breasts, induce growth of the ducts and acini, and promote water retention. The epithelial cells lining the ducts proliferate in number, the ducts dilate, and the lobules distend. The acini become enlarged and secretory, and lipid (fat) is deposited within their epithelial cell lining. As a result, breast swelling, tenderness, and discomfort are common symptoms just before the onset of menstruation. After menstruation, cellular proliferation begins to regress; the acini begin to decrease in size; and retained water is lost. After breasts have undergone changes numerous times in response to the ovarian cycle, the proliferation and involution (regression) are not uniform throughout the breast. In time, after repeated hormonal stimulation, small persistent areas of nodulations may develop. This normal physiologic change must be remembered when breast tissue is examined. Nodules may develop just before and during menstruation, when the breast is most active. The physiologic alterations in breast size and activity reach their minimal level about 5 to 7 days after menstruation stops.
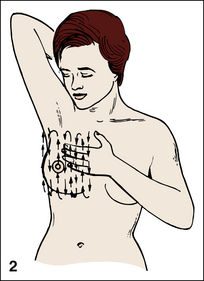
The best time for a woman who wishes to perform a breast self-examination (BSE) (palpation of breasts to detect changes in breast tissue) is during this phase of the menstrual cycle or whenever the breasts are not tender or swollen (see Teaching for Self-Management box: Breast Self-Examination).
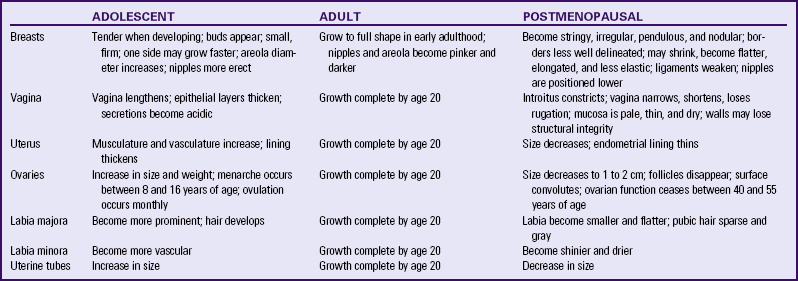
Table 4-1 compares the variations in physical assessment related to age differences in women.
Menstruation And Menopause
Nurses should be knowledgeable about menarche, the hypothalamic-pituitary cycle, the ovarian cycle, the endometrial cycle, other cyclic changes, and the climacteric because they provide care for women across the life span.
Menarche and Puberty
Although young girls secrete small, rather constant amounts of estrogen, a marked increase occurs between ages 8 and 11 years. The term menarche denotes first menstruation. Puberty is a broader term that denotes the entire transitional stage between childhood and sexual maturity. Increasing amounts and variations in gonadotropin and estrogen secretion develop into a cyclic pattern at least a year before menarche. In North America this occurs in most girls at about age 13 years.
Initially, for most women, periods are irregular, unpredictable, painless, and anovulatory (no ovum released from the ovary). After 1 or more years, a hypothalamic-pituitary rhythm develops, and the ovary produces adequate cyclic estrogen to make a mature ovum. Ovulatory (ovum released from ovary) periods tend to be regular, monitored by progesterone.
Although pregnancy can occur in exceptional cases of true precocious puberty, most pregnancies in young girls occur after the normally timed menarche. All young adolescents of both sexes would benefit from knowing that pregnancy can occur at any time after the onset of menses.
Menstrual Cycle
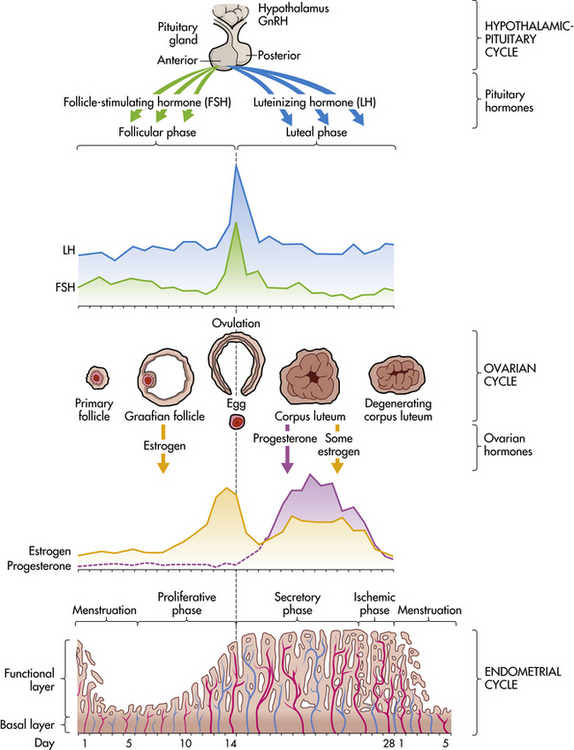
Menstruation is the periodic uterine bleeding that begins approximately 14 days after ovulation. It is controlled by a feedback system of three cycles: hypothalamic-pituitary, ovarian, and endometrial. The average length of a menstrual cycle is 28 days, but variations are normal. The first day of bleeding is designated day 1 of the menstrual cycle, or menses (Fig. 4-7). The average duration of menstrual flow is 5 days (range, 3 to 6 days), and the average blood loss is 50 ml (range, 20 to 80 ml), but these vary greatly.
For about 50% of women, menstrual blood does not appear to clot. The menstrual blood clots within the uterus, but the clot usually liquefies before being discharged from the uterus. Uterine discharge includes mucus and epithelial cells in addition to blood.
The menstrual cycle is a complex interplay of events that occur simultaneously in the endometrium, the hypothalamus, the pituitary glands, and the ovaries. The menstrual cycle prepares the uterus for pregnancy. When pregnancy does not occur, menstruation follows. The woman’s age, physical and emotional status, and environment influence the regularity of her menstrual cycles.
Hypothalamic-Pituitary Cycle
Toward the end of the normal menstrual cycle, blood levels of estrogen and progesterone decrease. Low blood levels of these ovarian hormones stimulate the hypothalamus to secrete gonadotropin-releasing hormone (GnRH). In turn, GnRH stimulates anterior pituitary secretion of follicle-stimulating hormone (FSH). FSH stimulates development of ovarian graafian follicles and their production of estrogen. Estrogen levels begin to decrease, and hypothalamic GnRH triggers the anterior pituitary to release luteinizing hormone (LH). A marked surge of LH and a smaller peak of estrogen (day 12; see Fig. 4-7) precede the expulsion of the ovum from the graafian follicle by about 24 to 36 hours. LH peaks at about day 13 or 14 of a 28-day cycle. If fertilization and implantation of the ovum have not occurred by this time, regression of the corpus luteum follows. Levels of progesterone and estrogen decline, menstruation occurs, and the hypothalamus is once again stimulated to secrete GnRH. This process is called the hypothalamic-pituitary cycle.
Ovarian Cycle
The primitive graafian follicles contain immature oocytes (primordial ova). Before ovulation from 1 to 30 follicles begin to mature in each ovary under the influence of FSH and estrogen. The preovulatory surge of LH affects a selected follicle. The oocyte matures, ovulation occurs, and the empty follicle begins its transformation to the corpus luteum. This follicular phase (preovulatory phase; see Fig. 4-7) of the ovarian cycle varies in length from woman to woman. Almost all variations in ovarian cycle length are the result of variations in the length of the follicular phase (Fehring, Schneider, & Raviele, 2006). On rare occasions (i.e., 1 in 100 menstrual cycles), more than one follicle is selected, and more than one oocyte matures and undergoes ovulation.
After ovulation, estrogen levels decrease. For 90% of women only a small amount of withdrawal bleeding occurs, so it goes unnoticed. In 10% of women there is sufficient bleeding for it to be visible, resulting in what is termed midcycle bleeding.
The luteal phase begins immediately after ovulation and ends with the start of menstruation. This postovulatory phase of the ovarian cycle usually requires 14 days (range, 13 to 15 days). The corpus luteum reaches its peak of functional activity 8 days after ovulation, secreting the steroids estrogen and progesterone. Simultaneously with peak luteal functioning, the fertilized ovum is implanted in the endometrium.
If implantation does not occur, the corpus luteum regresses, steroid levels decrease, and the functional layer of the uterine endometrium is shed through menstruation.
Endometrial Cycle
The four phases of the endometrial cycle are (1) the menstrual phase, (2) the proliferative phase, (3) the secretory phase, and (4) the ischemic phase (see Fig. 4-7). During the menstrual phase shedding of the functional two thirds of the endometrium (the compact and spongy layers) is initiated by periodic vasoconstriction in the upper layers of the endometrium. The basal layer is always retained, and regeneration begins near the end of the cycle from cells derived from the remaining glandular remnants or stromal cells in this layer.
The proliferative phase is a period of rapid growth lasting from about the fifth day to the time of ovulation. The endometrial surface is completely restored in approximately 4 days, or slightly before bleeding ceases. From this point on, an eight- to tenfold thickening occurs, with a leveling off of growth at ovulation. The proliferative phase depends on estrogen stimulation derived from ovarian follicles.
The secretory phase extends from the day of ovulation to about 3 days before the next menstrual period. After ovulation larger amounts of progesterone are produced. An edematous, vascular, functional endometrium becomes apparent. At the end of the secretory phase the fully matured secretory endometrium reaches the thickness of heavy, soft velvet. It becomes luxuriant with blood and glandular secretions, a suitable protective and nutritive bed for a fertilized ovum.
Implantation of the fertilized ovum generally occurs about 7 to 10 days after ovulation. If fertilization and implantation do not occur, the corpus luteum, which secretes estrogen and progesterone, regresses. With the rapid decrease in progesterone and estrogen levels, the spiral arteries go into spasm. During the ischemic phase the blood supply to the functional endometrium is blocked, and necrosis develops. The functional layer separates from the basal layer, and menstrual bleeding begins, marking day 1 of the next cycle (see Fig. 4-7).
Other Cyclic Changes
When the hypothalamic-pituitary-ovarian axis functions properly, other tissues undergo predictable responses. Before ovulation, the woman’s basal body temperature (BBT) is often less than 37° C; after ovulation, with increasing progesterone levels, her BBT increases. Changes in the cervix and cervical mucus follow a generally predictable pattern. Preovulatory and postovulatory mucus is viscous (thick), so that sperm penetration is discouraged. At the time of ovulation, cervical mucus is thin and clear. It looks, feels, and stretches like egg white. This stretchable quality is termed spinnbarkeit (see Chapter 8). Some women have localized lower abdominal pain called mittelschmerz that coincides with ovulation. Some spotting may occur.
Prostaglandins
Prostaglandins (PGs) are oxygenated fatty acids classified as hormones. The different kinds of PGs are distinguished by letters (PGE, PGF), numbers (PGE2), and letters of the Greek alphabet (PGF2α).
Prostaglandins are produced in most organs of the body, including the uterus. Menstrual blood is a potent prostaglandin source. PGs are metabolized quickly by most tissues. They are biologically active in minute amounts in the cardiovascular, gastrointestinal, respiratory, urogenital, and nervous systems. They also exert a marked effect on metabolism, particularly on glycolysis. Prostaglandins play an important role in many physiologic, pathologic, and pharmacologic reactions. PGF2α, PGE4, and PGE2 are most commonly used in reproductive medicine.
Prostaglandins affect smooth muscle contractility and modulation of hormonal activity. Indirect evidence suggests that PGs have an effect on ovulation, fertility, changes in the cervix, and cervical mucus that affect receptivity to sperm, tubal and uterine motility, sloughing of endometrium (menstruation), onset of abortion (spontaneous and induced), and onset of labor (term and preterm).
After exerting their biologic actions, newly synthesized PGs are rapidly metabolized by tissues in such organs as the lungs, the kidneys, and the liver.
Prostaglandins may play a key role in ovulation. If PG levels do not increase along with the surge of LH, the ovum remains trapped within the graafian follicle. After ovulation, PGs may influence production of estrogen and progesterone by the corpus luteum.
The introduction of PGs into the vagina or into the uterine cavity (from ejaculated semen) increases the motility of uterine musculature, which can assist the transport of sperm through the uterus and into the oviduct.
Prostaglandins produced by the woman cause regression of the corpus luteum, regression of the endometrium, and sloughing of the endometrium, resulting in menstruation. PGs increase myometrial response to oxytocic stimulation, enhance uterine contractions, and cause cervical dilation. They may be a factor in the initiation of labor, the maintenance of labor, or both. They also may be involved in dysmenorrhea (see Chapter 6) and preeclampsia-eclampsia (see Chapter 27).
Climacteric and Menopause
The climacteric is a transitional phase during which ovarian function and hormone production decline. This phase spans the years from the onset of premenopausal ovarian decline to the postmenopausal time when symptoms stop. Menopause (from the Latin mensis, month, and Greek pausis, to cease) refers only to the last menstrual period. Unlike menarche, however, menopause can be dated with certainty only 1 year after menstruation ceases. The average age at natural menopause is 51.4 years, with an age range of 35 to 60 years. Perimenopause is a period preceding menopause that lasts about 4 years. During this time, ovarian function declines. Ova slowly diminish, and menstrual cycles may be anovulatory, resulting in irregular bleeding. The ovary stops producing estrogen, and eventually menses no longer occur.
Sexual Response
The hypothalamus and anterior pituitary gland in females regulate the production of FSH and LH. The target tissue for these hormones is the ovary, which produces ova and secretes estrogen and progesterone. A feedback mechanism between hormone secretion from the ovaries, the hypothalamus, and the anterior pituitary aids in the control of the production of sex cells and steroid sex hormone secretion.
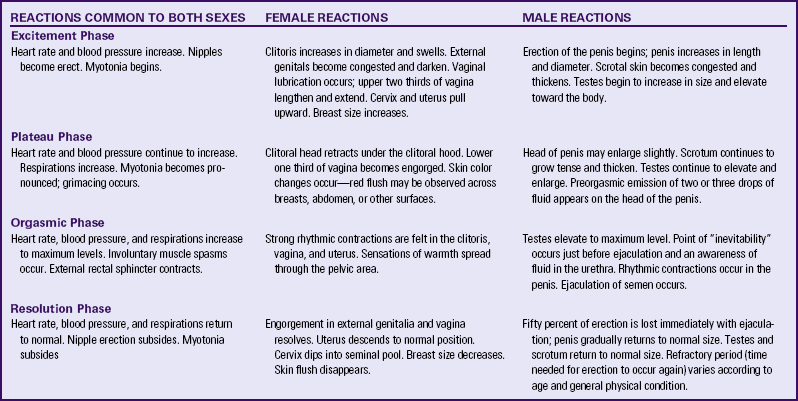
Although the first outward appearance of maturing sexual development occurs at an earlier age in females, both females and males achieve physical maturity at approximately age 17 years; however, individual development varies greatly. Anatomic and reproductive differences notwithstanding, women and men are more alike than different in their physiologic response to sexual excitement and orgasm. For example, the glans clitoris and the glans penis are embryonic homologues. Little difference exists between female and male sexual response; the physical response is essentially the same whether stimulated by coitus, fantasy, or masturbation. Physiologically, according to Masters (1992), sexual response can be analyzed in terms of two processes: vasocongestion and myotonia.
Sexual stimulation results in an increase in circulation to circumvaginal blood vessels (lubrication in the female), causing engorgement and distention of the genitals. Venous congestion is localized primarily in the genitals, but it also occurs to a lesser degree in the breasts and other parts of the body. Arousal is characterized by myotonia (increased muscular tension), resulting in voluntary and involuntary rhythmic contractions. Examples of sexually stimulated myotonia are pelvic thrusting, facial grimacing, and spasms of the hands and feet (carpopedal spasms).
The sexual response cycle is divided into four phases: excitement phase, plateau phase, orgasmic phase, and resolution phase. The four phases occur progressively, with no sharp dividing line between any two phases. Specific body changes take place in sequence. The time, intensity, and duration for cyclic completion also vary for individuals and situations. Table 4-2 compares male and female body changes during each of the four phases of the sexual response cycle.
Reasons for Entering the Health Care System
Women’s health assessment and screening focus on a systems evaluation, beginning with a careful history and physical examination. During the assessment and evaluation, the responsibilities for self-management, health promotion, and enhancement of wellness are emphasized. Nursing care includes assessment, planning, education, counseling, and referral as needed, as well as commendations for good self-care that the woman has practiced. This enables women to make informed decisions about their own health care.
Preconception Counseling and Care
Preconception health promotion provides women and their partners with information that is needed to make decisions about their reproductive future. Preconception counseling guides couples on how to prevent unintended pregnancies and to achieve pregnancy when desired, stresses risk management, and identifies healthy behaviors that promote the well-being of the woman and her potential fetus (Moos, 2006).
All providers who treat women for well-woman care or other routine care should incorporate preconception health screening as part of the routine care for women of reproductive age (Johnson, Posner, Biermann, Cordero, Atrash, Parker, et al., 2006). The initiation of activities that promote healthy mothers and babies must occur before the period of critical fetal organ development, which is between 17 and 56 days after fertilization. By the end of the eighth week after conception and certainly by the end of the first trimester, any major structural anomalies in the fetus are already present. Because many women do not realize that they are pregnant and do not seek prenatal care until well into the first trimester, the rapidly growing fetus may be exposed to many types of intrauterine environmental hazards during this most vulnerable developmental phase.
Preconception care is important for women who have had a problem with a previous pregnancy (e.g., miscarriage, preterm birth). Although causes are not always identifiable, in many cases, problems can be identified and treated and may not recur in subsequent pregnancies. Preconception care is also important to minimize fetal malformations. For example, the woman may be exposed to teratogenic agents such as drugs, viruses, and chemicals, or she may have a genetically inherited disease. Preconception counseling can educate the woman about the effects of these agents and diseases, which can help prevent harm to the fetus or allow the woman to make an informed decision about her willingness to accept potential hazards should a pregnancy occur (Atrash, Johnson, Adams, Cordero, & Howse, 2006).
A model for preconception care of women of reproductive age targets all women from menarche to menopause at every encounter, not just in maternity and women’s health. Providing optimal health care for women whether or not they desire to conceive can result in a high level of preconception wellness (Moos, 2006). Suggested components of preconception care, such as health promotion, risk assessment, and interventions, are outlined in Box 4-1.
Pregnancy
A woman’s entry into health care is often associated with pregnancy, either for diagnosis or for actual care. The possibility of pregnancy is realized most commonly when a woman is late with her menses. If she is pregnant, it is desirable for a woman to enter prenatal care within the first 12 weeks. This allows early pregnancy counseling, especially for the woman who has had no preconception care. Major goals of prenatal care are found in Box 4-2 and should be initiated at the first visit. Extensive discussion of pregnancy is found in Chapter 15.
Well-Woman Care
Current trends in the health care of women have expanded beyond a reproductive focus. A holistic approach to women’s health care includes a woman’s health needs throughout her lifetime. This view goes beyond simply her reproductive needs. This restructuring places women’s health within the primary health care delivery system. Women’s health assessment and screening focus on a multisystem evaluation emphasizing the maintenance and enhancement of wellness.
Many women first enter the health care delivery system for a Pap test or contraception. Visits to the nurse may be their only contact with the system unless they become ill. Some women postpone examination until a specific need arises, such as pregnancy, pain, abnormal bleeding, or vaginal discharge.
Health care needs vary with culture, religion, age, and personal differences. The changing responsibilities and roles of women, their socioeconomic status, and their personal lifestyles also contribute to differences in the health and behavior of women. Employment outside of the home, physical disability, inadequate or no health insurance, divorce, single parenthood, and sexual orientation also can affect women’s ability to seek and receive health care in clinical settings. As women age, many continue to address their primary health care needs within their established gynecologic care setting; therefore, well-women’s health care should include a complete history, physical examination, age-appropriate screening, and health promotion.
Fertility Control and Infertility
As women become more informed about themselves and their health care, they are more willing to seek counseling and contraception appropriate to their varied and specific needs. Some women first enter the health care system to obtain such advice. More than half of the pregnancies in the United States each year are unintended, many even with contraception use (Trussell, 2007). Education is the key to encouraging women to make family planning choices based on preference and actual benefit-to-risk ratios. Providers can influence the user’s motivation and ability to use the method correctly (see Chapter 8 for further discussion of contraception).
The concept of health promotion applies to contraception, as can be seen in Box 4-3. The nurse can influence women positively regarding the need for child spacing, methods of family planning that are consistent with religious and personal preferences, noncontraceptive benefits of certain methods, the appropriate use of methods selected, and the protection of future fertility when so desired.
Women also enter the health care system because of their desire to achieve a pregnancy. Approximately 15% of couples in the United States have some degree of infertility. Many couples have delayed starting their families until they are in their 30s or 40s, which allows more time to be exposed to situations negatively affecting fertility (including age-related infertility for the woman). In addition, sexually transmitted infections (STIs), which can predispose to decreased fertility, are becoming more common, and many women and men are in workplaces and home settings where they may be exposed to reproductive environmental hazards.
Steps toward prevention of infertility should be undertaken as part of ongoing routine health care, and such information is especially appropriate in preconception counseling. Primary care providers can undertake initial evaluation and counseling before couples are referred to specialists. For additional information about infertility, see Chapter 9.
Menstrual Problems
Irregularities or problems with the menstrual period are among the most common concerns of women and often cause them to seek help from the health care system. Common menstrual disorders include amenorrhea, dysmenorrhea, premenstrual syndrome, endometriosis, and menorrhagia or metrorrhagia. Simple explanation and counseling may handle the concern; however, history and examination must be completed, as well as laboratory or diagnostic tests, if indicated. Questions should never be considered inconsequential. Age-specific reading materials are recommended, especially for teenagers. Information should also consider cultural relevance and be available in languages appropriate for the population with whom the nurse is working. See Chapter 6 for an in-depth discussion of menstrual problems.
Perimenopause
The body responds to this natural transition in a number of ways, most of which are due to the decrease in estrogen. Most women seeking health care during the perimenopausal period do so because of irregular bleeding. Others are concerned about vasomotor symptoms (hot flashes and flushes). Although fertility is greatly reduced during this period, women are urged to maintain some method of contraception because pregnancies still can occur. All women need to have factual information, the dispelling of myths, a thorough examination, and periodic health screenings thereafter. See Chapter 6 for discussion of perimenopause and menopause.
Barriers to Seeking Health Care
Parts of the health care delivery system remain in a state of flux. Great variation occurs depending on type and size of the system, source of payment for services, private versus public programs, availability of and accessibility to providers, individual preferences, and insurance coverage or ability to pay. The existing system continues to be oriented to treatment of acute or episodic conditions rather than the promotion of health and comprehensive care (see discussion in Chapter 1).
A health care reform bill was signed by President Obama on March 23, 2010. However, the impact of this legislation on the American people will not be known for years because not all benefits will be immediate (Gaulin, 2010).
Cultural Issues
As our nation becomes more racially, ethnically and culturally diverse, the health of minority groups becomes a major issue. A variety of reasons are given to explain some of the differences in accessing care when financial barriers are adjusted. Unfair treatment was described by women who experienced racial discrimination or disrespectful, disillusioning, or discouraging encounters with community service providers such as social services and health care providers. A lack of training in cross-cultural communication may present problems. Desired health outcomes are best achieved when the health care providers have a knowledge and understanding about the culture, language, values, priorities, and health beliefs of minority groups. Conversely, members of the group should understand the health goals to be achieved and the methods proposed to do so. Language differences can produce profound barriers between women and health care providers. Even with an interpreter, information may be skewed in either direction.
Providers must consider culturally based differences that could affect the treatment of diverse groups of women, and the women themselves should share their practices and beliefs that could influence their management, responses, or willingness to comply (see Cultural Considerations box: Female Genital Mutilation). For example, women in some cultures value privacy to such an extent that they are reluctant to disrobe and, as a result, avoid physical examination unless absolutely necessary. Other women rely on their husbands to make major decisions, including those affecting the woman’s health. Religious beliefs may dictate a specified plan of care, such as limiting assisted reproductive technology, contraception measures, blood transfusions, cardiopulmonary resuscitation, or assisted ventilation. Some cultural groups prefer folk medicine, homeopathy, or prayer to traditional Western medicine, and others attempt combinations of various practices
Gender Issues
Gender influences provider-client communication and may influence access to health care in general. The most obvious gender consideration is that between men and women. Researchers have reported significant male-female differences in receipt of major diagnostic and therapeutic interventions, especially with cardiac and kidney problems. Women tend to use primary care services more often than men and, some believe, more effectively. The sex of the provider plays a role; studies have shown that female clients have Pap tests and mammograms more consistently if they are seen by female providers.
Sexual orientation may produce another barrier. Lesbian women have primary erotic attractions and relations with other women. Some lesbians may not disclose their orientation to
health care providers because they feel they may be at risk for hostility, inadequate health care, or breach of confidentiality. In many health care settings, heterosexuality is assumed, and the setting may be one in which the woman does not feel welcome (magazines, brochures, and environment reflect heterosexual couples, or the health care provider shows discomfort interacting with the woman). Another problem is that lesbians themselves may hold beliefs that are incorrect, such as that they have immunity to human immunodeficiency virus (HIV), STIs, and certain cancers (e.g., cervical). The perceived lack of risk can result in lesbians avoiding medical care as well as in health care providers giving incorrect advice or not doing appropriate cancer screening for these women. Not all gynecologic cancers are related to sexual activity; lesbians who have never had children may be more at risk for breast, ovarian, and endometrial cancer. Their risk for heart disease, cancer of the lung, and colon cancer is the same as that of the heterosexual woman. To offset stereotypes, it is necessary for providers to develop an approach that does not assume that all women are heterosexual. Revising forms to be inclusive of sexual diversity and providing an environment that promotes acceptance and inclusiveness are two strategies suggested by researchers (Goldberg, 2005-2006; Roberts, 2006).
Health Risks in the Childbearing Years
Maintaining optimal health is a goal for all women. Essential components of health maintenance are identification of unrecognized problems and potential risks and the education and the health promotion needed to reduce them. This is especially important for women in their childbearing years, because conditions that increase a woman’s health risks are not only of concern for her well-being but also are potentially associated with negative outcomes for both mother and baby in the event of a pregnancy. Prenatal care is an example of prevention that is practiced after conception; however, prevention and health maintenance are needed before pregnancy because many of the mother’s risks can be identified and then eliminated or at least modified. An overview of conditions and circumstances that increase health risks in the childbearing years follows.
Age
As a girl progresses through development, she may be at risk for conditions that are age related. All teens undergo progressive growth of sexual characteristics and undertake developmental tasks of adolescence, such as establishing identity, developing sexual preference, emancipating from family, and establishing career goals. Some of these situations can produce great stress for the adolescent, and the health care provider should treat her carefully. Female teenagers who enter the health care system usually do so for screening (Pap tests start at age 21 or 3 years after the girl becomes sexually active) or because of a problem such as episodic illness or accidents. Gynecologic problems are often associated with menses (either bleeding irregularities or dysmenorrhea), vaginitis or leukorrhea, STIs, contraception, or pregnancy. The adolescent also is at risk for depression (Huff, Abuzz, & Omar, 2007).
Teenage Pregnancy: Pregnancy in the teenager who is 16 years old or younger often introduces additional stress into an already stressful developmental period. The emotional level of such teens is commonly characterized by impulsiveness and self-centered behavior, and they often place primary importance on the beliefs and actions of their peers. In attempts to establish a personal and independent identity, many teens do not realize the consequences of their behavior, and planning for the future is not part of their thinking processes.
Teenagers usually lack the financial resources to support a pregnancy and may not have the maturity to avoid teratogens or to have prenatal care and instruction or follow-up care. Children of teen mothers can be at risk for abuse or neglect because of the teen’s inadequate knowledge of growth, development, and parenting. Implementation of specialized adolescent programs in schools, communities, and health care systems is demonstrating continued success in reducing the birth rate in teens.
Young and Middle Adulthood
Because women ages 20 to 40 years have need for contraception, pelvic and breast screening, and pregnancy care, they can prefer to use their gynecologic or obstetric provider as their primary care provider also. During these years the woman may be “juggling” family, home, and career responsibilities, with resulting increases in stress-related conditions. Health maintenance includes not only pelvic and breast screening but also promotion of a healthy lifestyle, that is, good nutrition, regular exercise, no smoking, little or no alcohol consumption, sufficient rest, stress reduction, and referral for medical conditions and other specific problems. Common conditions requiring well-woman care include vaginitis, urinary tract infections, menstrual variations, obesity, sexual and relationship issues, and pregnancy.
Parenthood After Age 35: A woman older than 35 years does not have a different physical response to a pregnancy, per se, but rather has had health status changes as a result of time and the aging process. These changes may be responsible for age-related pregnancy conditions. For example, a woman with type 2 diabetes may not have had expression of her diabetes at age 22, but may have full-blown disease at age 38. Other chronic or debilitating diseases or conditions increase in severity with time, and these in turn may predispose to increased risks during pregnancy (National Women’s Health Resource Center [NWHRC], 2008). Of significance to women in this age-group is the risk of giving birth to a child with certain genetic anomalies (e.g., Down syndrome), and the opportunity for genetic counseling should be available to all (March of Dimes, 2010).
Late Reproductive Age
Women of later reproductive age are often experiencing change and reordering of their personal priorities. Generally the goals of education, career, marriage, and family have been achieved, and now the woman has increased time and opportunity for new interests and activities. Conversely, divorce rates are high at this age, and children leaving home may produce an “empty nest syndrome,” resulting in increased levels of depression. Chronic diseases also become more apparent. Most problems for the well woman are associated with perimenopause (e.g., bleeding irregularities and vasomotor symptoms). Health maintenance screening continues to be of importance because some conditions such as breast disease or ovarian cancer occur more often during this stage.
Socioeconomic Status
Differences exist among people from different socioeconomic levels and ethnic groups with respect to risk for illness and distribution of disease and death. Some diseases are more common among people of selected ethnicity, for example, sickle cell anemia in African-Americans, Tay-Sachs disease in Ashkenazi Jews, adult lactase deficiency in Chinese, beta thalassemia in Mediterranean peoples, and cystic fibrosis in northern Europeans. Cultural and religious influences also increase health risks because the woman and her family may have life and societal values and a view of health and illness that dictate practices different from those expected in the Judeo-Christian Western model. These practices may include food taboos or frequencies, methods of hygiene, effects of climate, care-seeking behaviors, willingness to undergo screening and diagnostic procedures, and value conflicts.
Socioeconomic status affects birth outcomes. Social consequences for poor women as single parents are great because many mothers with few skills are caught in the bind of having income that is insufficient to afford child care. These families generate fewer and fewer resources and increase their risks for health problems. Multiple roles for women in general produce overload, conflict, and stress, resulting in higher risks for psychologic illness.
Substance Use and Abuse
Use of illicit drugs and inappropriate use of prescription drugs continue to increase and are found in all ages, races, ethnic groups, and socioeconomic strata. Addiction to substances is seen as a biopsychosocial disease, with several factors contributing to risk. These include biogenetic predisposition, lack of resilience to stressful life experiences, and poor social support. Women are less likely than men to abuse drugs, but the rate in women is increasing significantly. Substance-abusing pregnant women create severe problems for themselves and their offspring, including interference with optimal growth and development and addiction. In many instances, the use of substances is identified through screening programs in prenatal clinics and obstetric units (see Chapter 32).
Smoking
Cigarette smoking is a major preventable cause of death and illness. Smoking is linked to cardiovascular heart disease, various types of cancers (especially lung and cervical), chronic lung disease, and negative pregnancy outcomes. Tobacco contains nicotine, which is an addictive substance that creates a physical and a psychologic dependence. There is little difference in the rate of smoking between men and women, although rates for women are slightly less (American Cancer Society [ACS], 2010a). Cigarette smoking impairs fertility in women and men, may reduce the age for menopause, and increases the risk for osteoporosis after menopause. Smoking during pregnancy is known to cause a decrease in placental perfusion and is a cause of low birth weight (Kliegman, 2006).
Alcohol
Women ages 35 to 49 years have the highest rates of chronic alcoholism, but women ages 21 to 34 have the highest rates of specific alcohol-related problems. About one third of alcoholics are women, and many relate onset of their drinking problem to stressful events. Women who are problem drinkers are often depressed, have more motor vehicle injuries, and have a higher incidence of attempted suicide than women in the general population. They also are at risk for alcohol-related liver damage. Early case finding and treatment are important in alcoholism for both the ill individual and for family members. See Chapter 32 for further discussion about alcohol use in women.
Prescription Drugs
Psychotherapeutic medications such as stimulants, sleeping pills, tranquilizers, and pain relievers are used by an estimated 2% of American women. Such medications can bring relief from undesirable conditions such as insomnia, anxiety, and pain, but because the medications have mind-altering capacity, misuse can produce psychologic and physical dependency in the same manner as illicit drugs. Risk-to-benefit ratios should be considered when such medications are used for more than short periods.
Depression is the most common mental health problem in women. Many kinds of medications are used to treat depression. All of these psychotherapeutic drugs can have some effect on the fetus when taken during pregnancy and must be very carefully monitored (see Chapter 32).
Illicit Drugs
Illicit drugs are taken for unlawful purposes. When they are unprescribed, they are usually obtained on the street for the purpose of getting high or for their body-mind–altering characteristics. Almost any drug can be abused or even illegal if taken in excess, including alcohol and prescription medication (see Chapter 32 for further discussion of substance abuse).
Nutrition
Good nutrition is essential for optimal health. A well-balanced diet helps prevent illness and treat certain health problems. Conversely, poor eating habits, eating disorders, and obesity are linked to disease and debility.
Dietary Guidelines for Americans 2010 provides evidenced-based recommendations to promote health and reduce risks for chronic diseases through diet (U.S. Department of Health and Human Services [USDHHS] & U.S. Department of Agriculture [USDA], 2010) (www.cnpp.usda.gov/Dietaryguidelines/htm).
Nutritional Deficiencies
Overt disease caused by lack of certain nutrients is rarely seen in the United States; however, insufficient amounts or imbalances of nutrients do pose problems for individuals and families. Overweight or underweight status, malabsorption, listlessness, fatigue, frequent colds and other minor infections, constipation, dull hair and thin nails, and dental caries are examples of problems that can be related to nutrition and indicate the need for further nutritional assessment. Poor nutrition, especially related to obesity and high fat and cholesterol intake, may lead to more serious conditions and is said to contribute to four of the six leading causes of death in the United States: heart disease, malignant neoplasms, cerebrovascular disease, and diabetes (Kung, Hoyert, Xu, & Murphy, 2008).
Obesity
During the last 20 years, obesity in the United States has increased dramatically. Estimates indicate that one third of women older than 20 years are obese (body mass index [BMI] 30 or higher) (NWHRC, 2006). In the United States the prevalence of obesity is highest among non-Hispanic black women, followed by Hispanic women and non-Hispanic white women (CDC, 2009). The BMI is defined as a measure of an adult’s weight in relation to his or her height, specifically the adult’s weight in kilograms divided by the square of his or her height in meters (see Table 14-2).
Overweight and obesity are known risk factors for premature death, diabetes, heart disease, dyslipidemia, stroke, hypertension, gallbladder disease, diverticular disease, some anemias, oral disease, constipation, osteoarthritis, gout, osteoporosis, respiratory dysfunction and sleep apnea, and some types of cancer (uterine, breast, colorectal, kidney, and gallbladder) (ACS, 2010b). In addition, obesity is associated with high cholesterol, menstrual irregularities, hirsutism (excess body/facial hair), stress incontinence, depression, complications of pregnancy, increased surgical risk, and shortened life span (USDHHS & USDA, 2010). Obesity-related pregnancy complications include macrosomia, gestational diabetes, hypertensive disorders, preterm birth, and cesarean birth. Pregnant women who are morbidly obese are at increased risk for intrauterine growth restriction and intrauterine fetal demise (Smith, Hulsey, & Goodnight, 2008).
Other Considerations
Other dietary extremes also can produce risk. For example, insufficient amounts of calcium can lead to osteoporosis, too much sodium can aggravate hypertension, and megadoses of vitamins can cause adverse effects in several body systems. Fad weight-loss programs and yo-yo dieting (repeated weight gain and weight loss) result in nutritional imbalances and, in some instances, medical problems. Such diets and programs are not appropriate for weight maintenance. Adolescent pregnancy produces special nutritional requirements because the metabolic needs of pregnancy are superimposed on the teen’s own needs for growth and maturation at a time when eating habits are less than ideal.
Anorexia Nervosa: Some women have a distorted view of their bodies and, no matter what their weight, perceive themselves to be much too heavy. As a result, they undertake strict and severe diets and rigorous extreme exercise. This chronic eating disorder is known as anorexia nervosa. Women can carry this condition to the point of starvation, with resulting endocrine and metabolic abnormalities. If not corrected, significant complications of arrhythmias, amenorrhea, cardiomyopathy, and congestive heart failure occur and, in the extreme, can lead to death. The condition commonly begins during adolescence in young women who have some degree of personality disorder. They gradually lose weight over several months, have amenorrhea, and are abnormally concerned with body image. Diagnosis can be difficult, especially if the person tries to hide the problem. Denial of a problem and secrecy around eating are common features of anorexia. Depression usually accompanies anorexia. There are no specific tests to diagnose anorexia nervosa. A medical history, physical examination, and screening tests help identify women at risk for eating disorders. Several tools are available to use in primary care settings. The SCOFF questionnaire is easy to administer and can help the nurse decide whether an eating disorder is likely and if the woman needs further assessment and possibly psychiatric and medical intervention (Parker, Lyons, & Bonner, 2005; Wolfe, 2005) (Box 4-4).
Bulimia Nervosa: Bulimia refers to secret, uncontrolled binge eating alternating with methods to prevent weight gain: self-induced vomiting, use of laxatives or diuretics, strict diets, fasting, and rigorous exercise. During a binge episode, large numbers of calories are consumed, usually consisting of sweets and “junk foods.” Binges occur at least twice per week. Bulimia usually begins in early adulthood (ages 18 to 25 years) and is found primarily in women. Complications can include dehydration and electrolyte imbalance, gastrointestinal abnormalities, and cardiac arrhythmias (Wolfe, 2005). Bulimia is somewhat similar to anorexia in that it is an eating disorder and usually involves some degree of depression. Unlike those with anorexia, individuals with bulimia may feel shame or disgust about their disorder and tend to seek help earlier. The SCOFF assessment also can be used to screen for bulimia (see Box 4-4).
Binge Eating Disorder: The hallmark of binge eating disorder is eating large amounts of food in a short period (a couple of hours) and not being able to stop eating. The woman may eat when she’s not hungry or until uncomfortably full. She may choose to eat alone because she is embarrassed about how much she eats. Binge eating disorder involves bingeing that alternates with a restricted dietary intake. An associated syndrome called night eating syndrome is when limited food is eaten early in the day and most of the day’s food intake is consumed after the evening meal. Over time, obesity and related complications of being overweight can develop. Common personality traits found in those with binge eating disorder include excessive concern about body size and shape and low self-esteem. Depression and anxiety commonly occur along with binge eating, which makes treatment and recovery more difficult. Binge eating is not associated with anorexia nervosa or bulimia nervosa.
Physical Fitness and Exercise
Physical activity promotes health, psychological well-being, and ideal body weight for height. It enhances independence, and improves quality of living across the life span. Women should engage in 2½ hours per week of moderate intensity or 1¼ hours per week of vigorous intensity aerobic physical activity or a combination of both according to the current Physical Activity Guidelines for Americans (USDHHS, 2008).
Exercise can reduce risks for a variety of conditions that are influenced by obesity and a sedentary lifestyle such as cardiovascular disease, cerebrovascular disease, and diabetes. Exercise plays an important role in the management of chronic conditions such as hypertension, arthritis, respiratory disorders, and osteoporosis. Exercise contributes to stress reduction and improving the quality of sleep. Women report that engaging in regular exercise improves their body image and self-esteem and acts as a mood enhancer.
Aerobic exercise contributes to cardiovascular fitness while increasing oxygen levels to working muscles. Anaerobic exercise, such as weight training, improves individual muscle mass without stress on the cardiovascular system. Because women are concerned about both cardiovascular and bone health, weight-bearing aerobic exercises such as walking, running, racket sports, and dancing may be preferred. Sustained excessive exercise can lead to hormonal imbalances, such as amenorrhea, which can usually be reversed when the body returns to normal levels of activity.
Stress
The modern woman faces increasing levels of stress and as a result is prone to a variety of stress-induced complaints and illnesses. Stress often occurs because of multiple roles, such as when coping with job and financial responsibilities conflicts with parenting and duties at home. To add to this burden, women are socialized to be caretakers, which is an emotionally draining role in itself. They also may find themselves in positions of minimal power that do not allow them to have control over their everyday environments. Some stress is normal and contributes to positive outcomes. Many women thrive in busy surroundings. However, excessive or high levels of ongoing stress trigger physical reactions in the body, such as rapid heart rate, elevated blood pressure, slowed digestion, release of additional neurotransmitters and hormones, muscle tenseness, and a weakened immune system. Consequently, constant stress can contribute to clinical illnesses such as flare-ups of arthritis or asthma, frequent colds or infections, gastrointestinal upsets, cardiovascular problems, and infertility. Box 4-5 lists symptoms that may be related to chronic or extreme stress. Psychologic signs such as anxiety, irritability, eating disorders, depression, insomnia, and substance abuse are associated with stress.
Sexual Practices
Potential risks related to sexual activity are undesired pregnancy and STIs. The risks are particularly high for adolescents and young adults who engage in sexual intercourse at earlier and earlier ages. Adolescents report many reasons for wanting to be sexually active, among which are peer pressure, desire to love and be loved, experimentation, enhancing self-esteem, and having fun. However, many teens do not have the decision-making or values-clarification skills needed to take this important step at a young age, and they lack the knowledge base regarding contraception and STIs. They also do not believe that becoming pregnant or getting an STI will happen to them.
Although some STIs can be cured with antibiotics, many can cause significant problems. Possible sequelae include infertility, ectopic pregnancy, neonatal morbidity and mortality, genital cancers, acquired immunodeficiency syndrome (AIDS), and even death (CDC, Workowski, & Berman, 2006). The incidence of STIs is increasing rapidly and reaching epidemic proportions. Choice of contraception has an effect on the risk of contracting an STI; however, no method of contraception offers complete protection. (See Chapter 7 for discussion of STIs and Chapter 8 for contraception.)
Medical Conditions
Most women of reproductive age are relatively healthy. Heart disease; lung, breast, colon, and gynecologic cancers; stroke; chronic lung disease; and diabetes are among the leading causes of death in adult women (Heron & Tejada-Vera, 2008) (Box 4-6). Certain medical conditions present during pregnancy can have deleterious effects on both the woman and the fetus. Of particular concern are risks from all forms of diabetes, urinary tract disorders, thyroid disease, hypertensive disorders of pregnancy, cardiac disease, and seizure disorders. Effects on the fetus vary and include intrauterine growth restriction, macrosomia, anemia, prematurity, immaturity, and stillbirth. Effects on the woman also can be severe. These conditions are discussed in later chapters.
Gynecologic Conditions
Women are at risk throughout their reproductive years for pelvic inflammatory disease, endometriosis, STIs and other vaginal infections, uterine fibroids, uterine deformities such as bicornuate uterus, ovarian cysts, interstitial cystitis, and urinary incontinence related to pelvic relaxation. These gynecologic conditions may contribute negatively to pregnancy by causing infertility, miscarriage, preterm labor, and fetal and neonatal problems. Gynecologic cancers also affect women’s health, although the risk for most cancers is low in pregnancy. Risk factors depend on the type of cancer. The effect of developing a gynecologic problem or cancer in women and their families is shaped by a number of factors including the specific type of problem or cancer, the implications of the diagnosis for the woman and her family, and the timing of the occurrence in the woman’s and family’s lives. These conditions are discussed in Chapters 6, 7, and 11.
Environmental and Workplace Hazards
Environmental hazards in the home, the workplace, and the community can contribute to poor health at all ages. Categories and examples of health-damaging hazards include the following: (1) pathogenic agents (viruses, bacteria, fungi, parasites); (2) natural and synthetic chemicals (natural toxins from animals, insects, and plants; consumer and industrial products such as pesticides and hydrocarbon gases; medical and diagnostic devices; tobacco; fuels; and drug and alcohol abuse); (3) radiation (radon, heat waves, sound waves); (4) food substances (added components that are not necessary for nutrition); and (5) physical objects (moving vehicles, machinery, weapons, water, and building materials).
Environmental hazards can affect fertility, fetal development, live birth, and the child’s future mental and physical development. Environmental hazards are discussed throughout other chapters as they are identified as specific risks to women’s and infants’ health.
Violence Against Women
Violence against women is a major health care problem in the United States, affecting millions of women each year and costing millions of dollars in annual medical costs. Women of all races and of all ethnic, educational, religious, and socioeconomic backgrounds are affected. Pregnancy is often a time when violence begins or escalates. The magnitude of the problem is far greater than the statistics indicate because violent crimes against women are the most underreported data as a result of fear, lack of understanding, and stigma surrounding violent situations. Maternity and women’s health nurses, by the very nature of their practice, are in a unique position to conduct case finding, provide sensitive care to women experiencing abusive situations, engage in prevention activities, and influence health care and public policy toward decreasing the violence. For further discussion of violence against women, see Chapter 5.
Health Assessment
Women’s health trends have expanded beyond a reproductive focus to include a holistic approach to health care across the life span and places women’s health within the scope of primary care. Women’s health assessment and screening focus on a systems evaluation beginning with a careful history and physical examination. During the assessment and evaluation, the responsibility for self-care, health promotion, and wellness enhancement is emphasized.
In a market-driven system such as managed care, specific guidelines may be provided for health screening by the insurer or the managed care organization. A nurse often takes the history, orders diagnostic tests, interprets test results, makes referrals, coordinates care, and directs attention to problems requiring medical intervention. Advanced practice nurses who have specialized in women’s health, such as nurse practitioners, clinical nurse specialists, and nurse-midwives, perform complete physical examinations, including gynecologic examinations.
Interview
The contact with the woman usually begins with an interview. This interview should be conducted in a private, comfortable, and relaxed setting (Fig. 4-8). The woman is addressed by her title and name (e.g., Mrs. Gonzalez), and the nurse introduces herself or himself by using name and title. It is important to phrase questions in a sensitive and nonjudgmental manner. Body language should match verbal communication. The nurse is cognizant of a woman’s vulnerability and assures her of strict confidentiality. For many women, fear, anxiety, and modesty make the examination a dreaded and stressful experience. Many women are uninformed, misguided by myths, or afraid they will appear ignorant by asking questions about sexual or reproductive functioning. The woman is assured that no question is irrelevant. The history begins with an open-ended question such as, “What brings you in to the office/clinic/hospital today? Anything else? Tell me about it.”

FIG. 4-8 Nurse interviews woman as part of history taking prior to physical examination. (Courtesy Ed Lowdermilk, Chapel Hill, NC.)
Additional ways to get women to share information include the following:
• Facilitation: Using a word or posture that communicates interest; leaning forward; making eye contact; or saying “Mm-hmmm” or “Go on”
• Reflection: Repeating a word or phrase that a woman has used
• Clarification: Asking the woman what is meant by a word or phrase
• Empathic responses: Acknowledging the feelings of a woman by statements such as “That must have been frightening”
• Confrontation: Identifying something about the woman’s behavior or feelings not expressed verbally or apparently inconsistent with her history
• Interpretation: Putting into words what you infer about the woman’s feelings or about the meaning of her symptoms, events, or other matters
Direct questions may be necessary to elicit specific details. These should be worded in language that is understandable to the woman and expressed neutrally, so that the woman will not be led into a specific response. The nurse asks about one item at a time and proceeds from the general to the specific (Seidel, Ball, Dains, Flynn, Soloman, & Stewart, 2011).
Cultural Considerations
Recognizing signs and symptoms of disease and deciding when to seek treatment are influenced by cultural perceptions. It is essential that a nurse have respect for the rich and unique qualities that cultural diversity brings to individuals. In recognizing the value of these differences, the nurse can modify the plan of care to meet the needs of each woman.
To understand the woman’s point of view, it is important to ask the right questions. Galanti (2008) suggests the use of the 4 C’s of Cultural Competence. These include:
1. Call—What do you call your problem?
2. Cause—What do you think caused your problem?
3. Cope—How do you cope with your condition?
4. Concerns—What are your concerns regarding your condition?
Using the 4 C’s of Cultural Competence along with cultural proficiency, biomedical values and evidence-based practice allows the nurse to individualize care with a client-focused approach. Trust that the woman is the expert on her life, culture, and experiences. If the nurse asks with respect and a genuine desire to learn, the woman will tell the nurse how to care for her. Modifications may be necessary for the physical examination. In some cultures, it may be considered inappropriate for the woman to disrobe completely for the physical examination. In many cultures, a female examiner is preferred. Communication may be hindered by different beliefs even when the nurse and woman speak the same language (see Box 2-1, p. 25, and Cultural Considerations box above).
Women with Special Needs
Women with emotional or physical disorders have special needs. Women who have vision, hearing, emotional, or physical disabilities should be respected and involved in the assessment and physical examination to the full extent of their abilities. The nurse should communicate openly and directly with sensitivity. It is often helpful to learn about the disability directly from the woman while maintaining eye contact (if eye contact is culturally appropriate). Family and significant others should be relied on only when absolutely necessary. The assessment and physical examination can be adapted to each woman’s individual needs.
Communication with a woman who is hearing impaired can be accomplished without difficulty. Most of these women read lips, write, or both; thus an interviewer who speaks and enunciates each word slowly and in full view may be easily understood. If a woman is not comfortable with lip reading, she may use an interpreter. In this case, it is important to continue to address the woman directly, avoiding the temptation to speak directly with the interpreter.
The visually impaired woman needs to be oriented to the examination room and may have her guide dog with her. As with all women, the visually impaired woman needs a full explanation of what the examination entails before proceeding. Before touching her, the nurse explains, “Now I am going to take your blood pressure. I am going to place the cuff on your right arm.” The woman can be asked if she would like to touch each of the items that will be used in the examination.
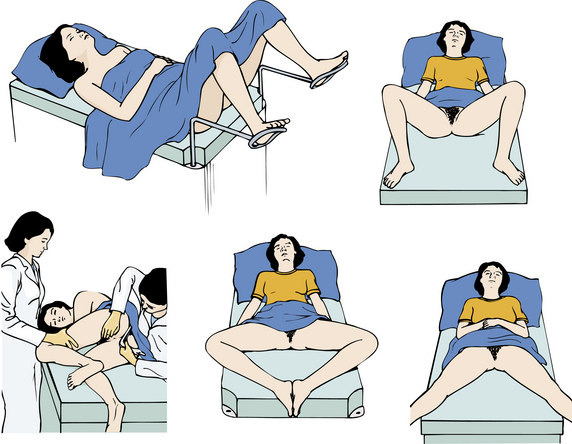
Many women with physical disabilities cannot comfortably lie in the lithotomy position for the pelvic examination. Several alternative positions may be used, including a lateral (side-lying) position, a V-shaped position, a diamond-shaped position, and an M-shaped position (Piotrowski & Snell, 2007) (Fig. 4-9). The woman can be asked what has worked best for her previously. If she has never had a pelvic examination, or has never had a comfortable pelvic examination, the nurse proceeds by showing her a picture of various positions and asking her which one she prefers. The nurse’s support and reassurance can help the woman to relax, which will make the examination go more smoothly.
Abused Women
Nurses should screen all women entering the health care system for potential abuse. Help for the woman may depend on the sensitivity with which the nurse screens for abuse, the discovery of abuse, and subsequent intervention. The nurse must be familiar with the laws governing abuse in the state in which she or he practices.
Pocket cards listing emergency numbers (abuse counseling, legal protection, and emergency shelter) may be available from the local police department, a women’s shelter, or an emergency department. It is helpful to have these on hand in the setting where screening is done. An abuse-assessment screen (Fig. 4-10) can be used as part of the interview or written history. If a male partner is present, he should be asked to leave the room because the woman may not disclose experiences of abuse in his presence, or he may try to answer questions for her to protect himself. The same procedure would apply for partners of lesbians, parents of teens, or adult children of older women.
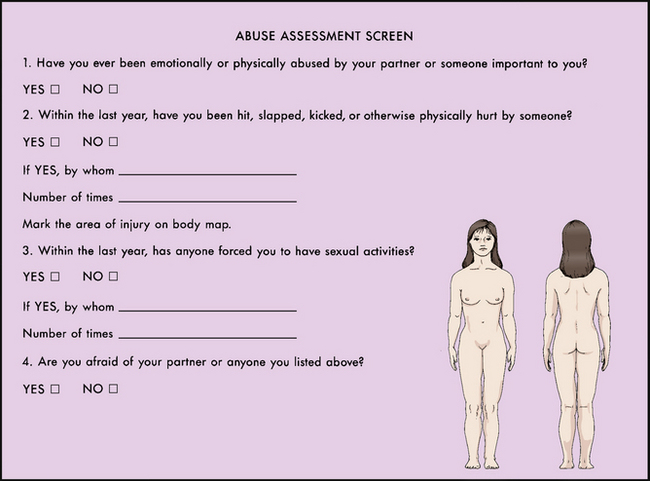
FIG. 4-10 Abuse assessment screen. (Modified from the Nursing Research Consortium on Violence and Abuse. [1991].)
Fear, guilt, and embarrassment may keep many women from giving information about family violence. Clues in the history and evidence of injuries on physical examination should give a high index of suspicion. The areas most commonly injured in women are the head, the neck, the chest, the abdomen, the breasts, and the upper extremities. Burns and bruises in patterns resembling hands, belts, cords, or other weapons may be seen as well as multiple traumatic injuries. Attention should be given to women who repeatedly seek treatment for somatic complaints such as headaches, insomnia, choking sensation, hyperventilation, gastrointestinal symptoms, and pain in the chest, back, and pelvis. During pregnancy the nurse should assess for injuries to the breasts, the abdomen, and the genitals. See Chapter 5 for further discussion of violence.
Adolescents (Ages 13 to 19 Years)
As a young woman matures, she should be asked the same questions that are included in any history. Particular attention should be paid to hints about risky behaviors, eating disorders, and depression. Do not assume that a teenager is not sexually active. After rapport has been established, it is best to talk to a teen with the parent (partner or friend) out of the room. Questions should be asked with sensitivity and in a gentle and nonjudgmental manner (Seidel et al., 2011).
A teen’s first speculum examination is the most important because she will develop perceptions that will remain with her for future examinations. What the examination entails should be discussed with the teen while she is dressed. Models or illustrations can be used to show exactly what will happen. All of the necessary equipment should be assembled so that there are no interruptions. Pediatric speculums that are 1 to 1.5 cm wide can be inserted with minimal discomfort. If the teen is sexually active, a small adult speculum may be used.
Injury prevention should be a part of the counseling at routine health examinations, with special attention to seat belts, helmets, firearms, recreational hazards, and sports involvement. The use of drugs and alcohol and the nonuse of seat belts contribute to motor vehicle injuries, accounting for the greatest proportion of accidental deaths in women. Contraceptive use and STI prevention information may be needed for teens who are sexually active.
To provide developmentally appropriate care, it is important to review the major tasks for women in this stage of life. Major tasks for teens include values assessment; education and work goal setting; formation of peer relationships that focus on love, commitment, and becoming comfortable with sexuality; and separation from parents. Individuality may be reflected in areas such as sexuality, politics, and career choices. Conflict exists between making and keeping commitments to keep options open. The teen is egocentric as she progresses rapidly through emotional and physical change. Her feelings of invulnerability may lead to serious misconceptions, such as that unprotected sexual intercourse will not lead to pregnancy.
Midlife and Older Women (Ages 50 Years and Older)
The assessment of women ages 50 and older presents unique challenges. Women may be experiencing major lifestyle changes, such as children leaving home, care for their aging parents, job change, retirement, separation, divorce or death of a partner, and aging-related changes and health problems. The nurse uses reflection and empathy to communicate in an open and caring manner. It may be necessary to schedule a longer appointment time because older women have longer histories or have a need to talk. Some women may fail to report symptoms because they fear their complaints will be attributed to old age, or they feel that they have lived with a chronic condition (e.g., incontinence, dyspareunia, interstitial cystitis, decreased libido, depression) for so long that nothing can be done. Women may choose to ignore a problem if they have symptoms that are life threatening (e.g., chest pain or a breast lump) because they traditionally put the needs of others first. As a result, the nurse should encourage the woman to express her concerns and fears and reassure her that her problems are important and will be addressed. Exercise, hormone therapy, diet, vitamins, calcium with vitamin D supplementation, daily aspirin, breast self-examination, Pap and mammogram recommendations, colonoscopy, immunization updates, and sun protection should be discussed.
Functional assessment is included as part of the history in women older than 70 years and those with disabilities. In the review of systems, the nurse should ask about self-management activities such as walking, getting to the bathroom, bathing, hair combing, dressing, and eating. Questions about driving, using public transportation, using the telephone or the Internet, hanging up clothes, buying groceries, taking medications, and meal preparation should be included.
Sexual assessment continues to be important in women 50 and older. Unless directly asked, women may omit mention of sexual concerns. Questions asked with sensitivity may invite responses regarding changes in sexual desire or response or physical issues that challenge her sexual enjoyment. Open and reflective questions also affirm a woman’s right to sexual enjoyment throughout the life span.
Women older than 50 years commonly experience menopause and have physical changes associated with decreased estrogen. A decrease in estrogen causes numerous cytologic and structural changes of the vagina, vulva, and lower urinary tract. Estrogen deficiency leads to a narrowing and shortening of the vagina and thinning of the vaginal walls. This can result in vaginal dryness, itching, burning, and dyspareunia. Estrogen loss also causes reduced smooth muscle relaxation, decreased vaginal blood flow and decreased vaginal secretions (North American Menopause Society [NAMS], 2007).
Estrogen plays a role in the formation of bone matrix, and a decrease may lead to osteoporosis. The risk for heart disease increases because of changes in lipid metabolism related to declining estrogen levels. Decreases in estrogen can cause a relaxation of ligaments and connective tissue, which affects the support of the bladder and uterus. Decreases in estrogen affect the hypothalamus, causing hot flashes, which are disturbing to most women (see Chapter 6).
Physical changes can result in increased discomfort during the pelvic examination. It is important to be both gentle and thorough during the examination. A small adult speculum may be used to view the cervix. The uterus in a menopausal woman is small and firm, and the ovaries are nonpalpable. In postmenopausal women the specimen from the vaginal pool may be useful to detect endometrial cells. A woman with palpable adnexal masses or vaginal bleeding after menopause needs immediate gynecologic referral.
A respectful and reassuring approach toward caring for women ages 50 and older will ensure their continued participation in seeking health care. Because the risk of breast, ovarian, uterine, cervical, colon, and skin cancers increases with age, the nurse has the opportunity to educate women about the importance of preventive screening. It is the nurse’s responsibility to ensure a positive health care experience that encourages future visits for prevention and chronic and acute care.
Advance directives can be introduced on any entry into a health care system. It is a good idea to have a formal statement in the medical record regarding a woman’s wishes in the event of accident or illness regarding life-maintaining measures or organ donation. Most states have laws formalizing such statements in writing. The durable power of attorney for health care can be used by a woman to delegate decision-making authority to a trusted relative or friend.
Many studies done on religion and health suggest that religious people are healthier and generally live longer than nonreligious people. Religious people have lower rates of uterine, cervical, and intestinal cancer; ulcer disease; coronary artery disease; and high blood pressure. Those who attend church once a week are less likely to become ill than those who do not. The studies did not control for rates of smoking and drinking, so no inference can be made as to whether the improved health status was from better health habits or religion. In general, it is known that religious people do tend to have healthier lifestyles overall than people who are not religious (Condon, 2004). Spiritual wellness can be estimated by answering questions such as those suggested in Box 4-7.
Healthy Aging: Women in the United States can expect on average to live to be 80 years old and may spend one third of their lives as postmenopausal women. With a healthy lifestyle, many women are living to be 100 years old or older. Proper nutrition, exercise, and mental and social stimulation are critical to keeping the body healthy and the mind active and alert into old age. Menopause is a time to evaluate, take stock, and prepare for many healthy years to come (Minikin & Wright, 2005).
History
At a woman’s first visit, she is often expected to fill out a form with biographic and historic data before meeting with the examiner. This form aids the health care provider in completing the history during the interview. Most forms include information about the following categories:
Box 4-8 describes a complete health history and review of systems based on the above categories.
Physical Examination
In preparation for the physical examination, the woman is instructed on undressing and given a gown to wear during the examination. She is usually given the opportunity to undress privately. Objective data are recorded by system or location. A general statement of overall health status is a good way to start. Findings are described in detail.
• General appearance: age, race, sex, state of health, posture, height, weight, development, dress, hygiene, affect, alertness, orientation, cooperativeness, and communication skills
• Vital signs: temperature, pulse, respiration, blood pressure
• Skin: color; integrity; texture; hydration; temperature; edema; excessive perspiration; unusual odor; presence and description of lesions; hair texture and distribution; nail configuration, color, texture, condition, or presence of nail clubbing
• Head: size, shape, trauma, masses, scars, rashes, or scaling; facial symmetry; presence of edema or puffiness
• Eyes: pupil size, shape, reactivity, conjunctival injection, scleral icterus, fundal papilledema, hemorrhage, lids, extraocular movements, visual fields and acuity
• Ears: shape and symmetry, tenderness, discharge, external canal, and tympanic membranes; hearing—Weber should be midline (loudness of sound equal in both ears) and Rinne negative (no conductive or sensorineural hearing loss); should be able to hear whisper at 3 feet
• Nose: symmetry, tenderness, discharge, mucosa, turbinate inflammation, frontal or maxillary sinus tenderness; discrimination of odors
• Mouth and throat: hygiene, condition of teeth, dentures, appearance of lips, tongue, buccal and oral mucosa, erythema, edema, exudate, tonsillar enlargement, palate, uvula, gag reflex, ulcers
• Neck: mobility, masses, range of motion, trachea deviation, thyroid size, carotid bruits
• Lymphatic: cervical, intraclavicular, axillary, trochlear, or inguinal adenopathy; size, shape, tenderness, and consistency
• Breasts: skin changes, dimpling, symmetry, scars, tenderness, discharge or masses; characteristics of nipples and areolae
• Heart: rate, rhythm, murmurs, rubs, gallops, clicks, heaves, or precordial movements
• Peripheral vascular: jugular vein distention, bruits, edema, swelling, vein distention, positive Homans sign, or tenderness of extremities
• Lungs: chest symmetry with respirations, wheezes, crackles, rhonchi, vocal fremitus, whispered pectoriloquy, percussion, and diaphragmatic excursion; breath sounds equal and clear bilaterally
• Abdomen: shape, scars, bowel sounds, consistency, tenderness, rebound, masses, guarding, organomegaly, liver span, percussion (tympany, shifting, dullness), costovertebral angle tenderness
• Extremities: edema, ulceration, tenderness, varicosities, erythema, tremor, or deformity
• Genitourinary: external genitalia, perineum, vaginal mucosa, cervix, inflammation, tenderness, discharge, bleeding, ulcers, nodules, masses, internal vaginal support; bimanual and rectovaginal palpation of cervix, uterus, and adnexae
• Rectal: sphincter tone, masses, hemorrhoids, rectal wall contour, tenderness, and stool for occult blood
• Musculoskeletal: posture, symmetry of muscle mass, muscle atrophy, weakness, appearance of joints, tenderness or crepitus, joint range of motion, instability, redness, swelling, or spine deviation
• Neurologic: mental status, orientation, memory, mood, speech clarity and comprehension, cranial nerves II to XII, sensation, strength, deep tendon and superficial reflexes, gait, balance, and coordination with rapid alternating motions
Pelvic Examination
Many women are intimidated by the gynecologic portion of the physical examination. The nurse in this instance can take an advocacy approach that supports a partnership relationship between the woman and the care provider.
The woman is assisted into the lithotomy position (see Fig. 4-9) for the pelvic examination. When she is in the lithotomy position, the woman’s hips and knees are flexed, with the buttocks at the edge of the table, and her feet are supported by heel or knee stirrups.
Some women prefer to keep their shoes or socks on, especially if the stirrups are not padded. Many women express feelings of vulnerability and strangeness when in the lithotomy position. During the procedure, the nurse assists the woman with relaxation techniques such as taking slow deep breaths. Distraction is another technique that can be used effectively (e.g., placement of interesting pictures on the ceiling over the head of the table).
Many women find it distressing to attempt to converse in the lithotomy position. Most women appreciate an explanation of the procedure as it unfolds, as well as coaching for the types of sensations they may expect. Generally, however, women prefer not to have to respond to questions until they are again upright and at eye level with the examiner. Questioning during the procedure, especially if they cannot see their questioner’s eyes, may make women tense.
External Inspection: The examiner sits at the foot of the table for the inspection of the external genitals and for the speculum examination. In good lighting, external genitals are inspected for sexual maturity: clitoris, labia, and perineum. After childbirth or other trauma, there may be healed scars.
External Palpation: The examiner proceeds with the examination by using palpation and inspection. The examiner wears gloves for this portion of the assessment. Before touching the woman, the examiner explains what is going to be done and what the woman should expect to feel (e.g., pressure). The examiner may touch the woman in a less sensitive area such as the inner thigh to alert her that the genital examination is beginning. This gesture may put the woman more at ease. The labia are spread apart to expose the structures in the vestibule: urinary meatus, Skene glands, vaginal orifice, and Bartholin glands (Fig. 4-11). To assess the Skene glands, the examiner inserts one finger into the vagina and “milks” the area of the urethra. Any exudate from the urethra or the Skene glands is cultured. Masses and erythema of either structure are assessed further. Ordinarily the openings to the Skene glands are not visible; prominent openings may be seen if the glands are infected (e.g., with gonorrhea). During the examination, the examiner keeps in mind the data from the review of systems, such as history of burning on urination.

FIG. 4-11 External examination. Separation of the labia. (From Wilson, S., & Giddens, J. [2009]. Health assessment for nursing practice [4th ed.]. St. Louis: Mosby.)
The vaginal orifice is examined. Hymenal tags are normal findings. With one finger still in the vagina, the examiner repositions the index finger near the posterior part of the orifice. With the thumb outside the posterior part of the labia majora, the examiner compresses the area of Bartholin glands located at the 8 o’clock and 4 o’clock positions and looks for swelling, discharge, and pain.
The support of the anterior and posterior vaginal wall is assessed. The examiner spreads the labia with the index and middle fingers and asks the woman to strain down. Any bulge from the anterior wall (urethrocele or cystocele) or posterior wall (rectocele) is noted and compared with the history, such as difficulty to start the stream of urine or constipation.
The perineum (area between the vagina and anus) is assessed for scars from old lacerations or episiotomies, thinning, fistulas, masses, lesions, and inflammation. The anus is assessed for hemorrhoids, hemorrhoidal tags, and integrity of the anal sphincter. The anal area also is assessed for lesions, masses, abscesses, and tumors. If there is a history of STI, the examiner may want to obtain a culture specimen from the anal canal at this time. Throughout the genital examination, the examiner notes the odor. Odor may indicate infection or poor hygiene.
Vulvar Self-Examination: The pelvic examination provides a good opportunity for the practitioner to emphasize the need for regular vulvar self-examination (VSE) or genital self-examination (GSE) and to teach this procedure. Because there has been a dramatic increase in cancerous and precancerous conditions of the vulva in recent years, a VSE should be performed as an integral part of preventive health care by all women who are sexually active or ages 18 years or older. Most lesions, including malignancy, condyloma acuminatum (wartlike growth), and Bartholin cysts, can be seen or palpated and are easily treated if diagnosed early.
The VSE can be performed by the practitioner and woman together, by using a mirror. A simple diagram of the anatomy of the vulva can be given to the woman, with instructions to perform the examination herself that evening to reinforce what she has learned. She does the examination in a sitting position with adequate lighting, holding a mirror in one hand and using the other hand to expose the tissues surrounding the vaginal introitus. She then systematically examines the mons pubis, the clitoris, the urethra, the labia majora, the perineum, and the perianal area and palpates the vulva, noting any changes in appearance or abnormalities, such as ulcers, lumps, warts, and changes in pigmentation.
Internal Examination: A vaginal speculum consists of two blades and a handle. Speculums come in a variety of types and styles. A vaginal speculum is used to view the vaginal vault and cervix (see Procedure box: Assisting with Pelvic Examination). The speculum is gently placed into the vagina and inserted to the back of the vaginal vault. The blades are opened to reveal the cervix and are locked into the open position. The cervix is inspected for position and appearance of the os: color, lesions, bleeding, and discharge (Fig. 4-12). Cervical findings that are not within normal limits include ulcerations, masses, inflammation, and excessive protrusion into the vaginal vault. Anomalies,.

FIG. 4-12 Insertion of speculum for vaginal examination. A, Opening of the introitus. B, Oblique insertion of the speculum. C, Final insertion of the speculum. D, Opening of the speculum blades. (From Wilson, S., & Giddens, J. [2009]. Health assessment for nursing practice [4th ed.]. St. Louis: Mosby.)
such as a cockscomb (a protrusion over the cervix that looks like a rooster’s comb), a hooded or collared cervix (seen in diethylstilbestrol [DES] daughters), or polyps, are noted
Collection of Specimens: The collection of specimens for cytologic examination is an important part of the gynecologic examination. Infection can be diagnosed through examination of specimens collected during the pelvic examination. These infections include candidiasis, trichomoniasis, bacterial vaginosis, group B streptococci, gonorrhea, chlamydia, and herpes simplex virus (see Chapter 7). Once the diagnoses have been made, treatment can be instituted.
Papanicolaou (Pap) Test: Carcinogenic conditions, potential or actual, can be determined by examination of cells from the cervix collected during the pelvic examination (see Procedure box: Papanicolaou Test). This is termed a Pap test
Vaginal Examination: After the specimens are obtained, the vagina is viewed when the speculum is rotated. The speculum blades are unlocked and partially closed. As the speculum is withdrawn, it is rotated, and the vaginal walls are inspected for color, lesions, rugae, fistulas, and bulging.
Bimanual Palpation: The examiner stands for this part of the examination. A small amount of lubricant is placed on the first and second fingers of the gloved hand for the internal examination. To avoid tissue trauma and contamination, the thumb is abducted and the ring and little fingers are flexed into the palm (Fig. 4-13).
The vagina is palpated for distensibility, lesions, and tenderness. The cervix is examined for position, shape, consistency, motility, and lesions. The fornix around the cervix is palpated.
The other hand is placed on the abdomen halfway between the umbilicus and the symphysis pubis and exerts pressure downward toward the pelvic hand. Upward pressure from the pelvic hand traps reproductive structures for assessment by palpation. The uterus is assessed for position, size, shape, consistency, regularity, motility, masses, and tenderness.
With the abdominal hand moving to the right lower quadrant and the fingers of the pelvic hand in the right lateral fornix, the adnexa is assessed for position, size, tenderness, and masses. The examination is repeated on the woman’s left side.
Just before the intravaginal fingers are withdrawn, the woman is asked to tighten her vagina around the fingers as much as she can. If the muscle response is weak, the woman is assessed for her knowledge about Kegel exercises.
Rectovaginal Palpation: To prevent contamination of the rectum from organisms in the vagina (such as Neisseria gonorrhoeae), it is necessary to change gloves, add fresh lubricant, and then reinsert the index finger into the vagina and the middle finger into the rectum (Fig. 4-14). Insertion is facilitated if the woman strains down. The maneuvers of the abdominovaginal examination are repeated. The rectovaginal examination permits assessment of the rectovaginal septum, the posterior surface of the uterus, and the region behind the cervix and the adnexa. The vaginal finger is removed and folded into the palm, leaving the middle finger free to rotate 360 degrees. The rectum is palpated for rectal tenderness and masses.
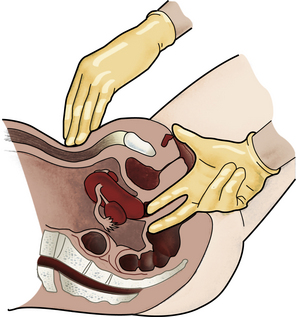
FIG. 4-14 Rectovaginal examination. (From Seidel, H., et al. [2011]. Mosby’s guide to physical examination [7th ed.]. St. Louis: Mosby.)
After the rectal examination, the woman is assisted into a sitting position, given tissues or wipes to cleanse herself, and given privacy to dress. The examiner returns after the woman is dressed to discuss findings and the plan of care.
Pelvic Examination During Pregnancy
The pelvic examination is done in the same way as it is during a routine examination on a nonpregnant woman. Pelvic measurements are completed, and uterine size is estimated. A Pap test may be done initially, as well as collection of cytologic specimens to test for gonorrhea, chlamydia, human papillomavirus, herpes simplex virus, and group B streptococci. As the pregnancy progresses, the nurse will inspect the woman’s abdomen, palpate fetal size and position, auscultate fetal heart tones, and measure fundal height at each visit.
While the pregnant woman is in lithotomy position, the nurse must watch for supine hypotension, caused by the weight of the abdomen pressing on the vena cava and aorta and triggering a decrease in blood pressure (see Fig. 19-5). Symptoms of supine hypotension include pallor, dizziness, faintness, breathlessness, tachycardia, nausea, clammy skin, and sweating. The woman should be positioned on her side until symptoms resolve and vital signs stabilize. The vaginal examination can be done with the woman in the lateral position..
Pelvic Examination After Hysterectomy
The pelvic examination is done much as it is done on a woman with a uterus. Vaginal screening using the Pap test is not recommended in women who have had a hysterectomy for benign disease. Because of the epidemic of human papillomavirus, which causes vaginal intraepithelial neoplasia, sampling of the vaginal cuff and vaginal walls after hysterectomy may still be practiced (see Table 4-3).
Laboratory and Diagnostic Procedures
The following laboratory and diagnostic procedures are ordered at the discretion of the clinician, considering the woman and her family history: hemoglobin, fasting plasma glucose, total blood cholesterol, lipid profile, urinalysis, syphilis serology (Venereal Disease Research Laboratory [VDRL] or rapid plasma reagin [RPR]) and other screening tests for sexually transmitted infections, mammogram, tuberculosis skin testing, hearing, visual acuity, electrocardiogram, chest X-ray, pulmonary function, fecal occult blood, flexible sigmoidoscopy, and bone mineral density scan. Results of these tests may be reported in person, by phone call, or by letter. Tests for HIV and drug screening may be offered with informed consent in high risk populations. These test results usually are reported in person.
Anticipatory Guidance for Health Promotion and Illness Prevention
Over the past several decades women have made tremendous strides in education, careers, policy making, and overall participation in today’s complex society. There have been costs for these advances, and although women are living longer, they may not be living better.
As a result, the health care system must pay greater attention to the health consequences for women. In addition, women must be active participants in their own health promotion and illness prevention. Health promotion is the motivation to increase well-being and actualize health potential. Illness prevention is the desire to avoid illness, detect it early, or maintain optimal functioning when illness is present.
Nurses have a major opportunity and responsibility to help women understand risk factors and to motivate them to adopt healthy lifestyles that prevent disease. Lifestyle factors that affect health over which the woman has some control include diet; tobacco, alcohol, and substance use; exercise; sunlight exposure; stress management; and sexual practices. Other influences, such as genetic and environmental factors, may be beyond the woman’s control, although some opportunities for prevention exist (e.g., through environmental legislation activism or genetic counseling services).
Knowledge alone is not enough to bring about healthy behaviors. The woman must be convinced that she has some control over her life and that healthy life habits, including periodic health examinations, are a sound investment. She must believe in the efficacy of prevention, early detection, and therapy and in her ability to perform self-management practices, such as BSE. Many people believe that they have little control over their health, or they become immobilized by fear and anxiety in the face of life-threatening illnesses, such as cancer, so they delay seeking treatment. The nurse must explore the reality of each woman’s perceptions about health behaviors and individualize teaching if it is to be effective
Nutrition
To maintain good nutrition, women should be counseled to include recommended servings from the major food categories of MyPyramid. Recommended servings from the food groups also provide adequate vitamins, minerals, iron, and fiber. Fluid intake is not included in the food pyramid, but individuals should be encouraged to drink at least six to eight glasses of water every day in addition to other fluids such as juices. Coffee, tea, soft drinks, and alcoholic beverages should be used in moderation..
Folic acid helps reduce high levels of homocysteine, an amino acid that damages the heart and blood vessels and increases the risk of heart disease, stroke, and dementia. Folic acid is present in citrus fruits, broccoli, spinach, asparagus, peas, lettuce, beans, whole grains, and orange juice. It is in many fortified grains and pasta or can be taken as a daily vitamin supplement (USDHHS & USDA, 2010).
Antioxidants are thought to be effective in helping to prevent oxidative damage in the body such as cancer, heart disease, and stroke; however, more research is needed in this area. Vitamins C and E; selenium (a mineral); and a group known as beta-carotenes (carotenoids) can be found in a diet containing fruits, vegetables, and whole grains.
Most women do not recognize the importance of calcium to health, and their diets are insufficient in calcium. Women who are unlikely to have enough calcium in the diet may need calcium supplements in the form of calcium carbonate with vitamin D, which contains more elemental calcium than do other preparations.
Vitamin D is essential for strong bones and a healthy immune system. Recent epidemiologic studies have shown a relationship between low vitamin D levels and multiple disease states such as increased cardiovascular mortality, cancer incidence, diabetes, osteoporosis, chronic pain and autoimmune diseases such as multiple sclerosis (Kulie, Groff, Redmer, Hounshell, & Schrager, 2009). Women can fulfill their vitamin D requirements by ingesting vitamin D and vitamin D–enhanced foods or being exposed to the sun for enough time to produce adequate amounts. It has been postulated that exposure of the arms and legs for 5 to 30 minutes between the hours of 10 am and 3 pm twice a week can be adequate to prevent vitamin D deficiency (Holick, 2007). With concerns about skin cancer, most women are cautious about sun exposure. Sources of natural vitamin D include egg yolks, shitake mushrooms, tuna, mackerel, sardines, salmon, and cod liver oil. Vitamin D–enhanced foods include milk, orange juice, infant formulas, yogurt, butter, margarine, cheese, and breakfast cereals. Researchers continue to investigate the optimum levels of vitamin D needed by healthy adults; most experts agree that less than 20 ng/ml represents deficiency (Kulie et al.).
The diet can be assessed by using a standard assessment form—a 24-hour recall is adequate and quick—and then food likes and dislikes, including cultural variations and typical food portions and dietary habits should be discussed and incorporated into counseling (see Chapter 14).
Exercise
Physical activity and exercise counseling for women of all ages should be undertaken at schools, worksites, and primary care settings. American Heart Association (AHA) (2010) recommendations include 30 to 60 minutes of moderate to vigorous activity on most days of the week. Activities do not need to be strenuous to bring health benefits. What is important is to include activities as part of a regular health routine. Activities that are especially beneficial when performed regularly include brisk walking, hiking, stair climbing, aerobic exercise, jogging, running, bicycling, rowing, swimming, soccer, and basketball. Few Americans exercise as often as they should, and physical activity is known to decrease with age, especially during adolescence and early adulthood.
The nurse should stress the importance of daily exercise throughout life for weight management and health promotion, suggesting exercises that are enjoyable to the individual (Fig. 4-15). Physical activity builds healthy bones, muscles, and joints and reduces the risk of colon and breast cancer. It also reduces feelings of depression and anxiety and improves mood and promotes a feeling of well-being. Many women who are sedentary during leisure time can benefit from gradually increasing their physical activity. They may be encouraged to exercise with their children or in groups with friends. Programs such as Curves for women, worksite fitness programs, or community-based programs such as the AHA’s Choose To Move are increasingly available. Young women can be involved in fitness centers, cheerleading, gymnastics, sports teams, or individual competitive sports.

FIG. 4-15 Exercise should be a part of one’s regular health routine. A cycle class is fun and provides moderate to vigorous exercise. (Courtesy Shari Rivera Sharpe, Chapel Hill, NC.)
For women who are sedentary or are not able to exercise vigorously, even moderate- and low-intensity activities, when performed daily, can have long-term health benefits such as lowering the risk of cardiovascular disease. Regular physical activity can reduce or eliminate some of these risk factors by lowering blood pressure, maintaining a reasonable weight or facilitating weight loss, and lowering cholesterol levels to less than 200 mg/dl.
Home maintenance, yard work, and gardening are other activities that promote health and a sense of well-being, especially for older adults. Attention to safety factors and wearing clothing and shoes appropriate to each activity are advised. Care should be taken not to aggravate existing conditions or create muscle and joint discomfort by an overly aggressive approach to exercise.
Kegel Exercises
Kegel exercises, or pelvic muscle exercises, were developed to strengthen the supportive pelvic floor muscles to control or reduce incontinent urine loss. These exercises also are beneficial during pregnancy and postpartum. They strengthen the muscles of the pelvic floor, providing support for the pelvic organs and control of the muscles surrounding the vagina and urethra. Educational strategies for teaching women how to perform Kegel exercises were compiled by nurse researchers who conducted a research utilization project for the Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN) are described in the Teaching for Self-Management box: Kegel Exercises.
Stress Management
Because it is neither possible nor desirable to avoid all stress, women must learn how to manage stress. The nurse should assess each woman for signs of stress by using therapeutic communication skills to determine risk factors and the woman’s ability to function. See Box 4-5 for identifying symptoms of stress.
Women are twice as likely as men to have depression, anxiety, or panic attacks (NWHRC, 2009). Nurses must be alert to the symptoms of serious mental disorders, such as depression and anxiety. Women having major life changes such as divorce and separation, bereavement, serious illness, and unemployment need special attention.
For many women, the nurse is able to provide comfort, reassurance, and advice concerning helping resources, such as support groups. Many centers offer support groups to help women prevent or manage stress. The nurse can help women become more aware of the relationship between good nutrition, rest, relaxation, and exercise, and diversion, and their ability to deal with stress. In the case of role overload, determining what needs immediate attention and what can wait is important. Practical advice includes having regular breaks, taking time for friends, developing interests outside of work or the home, setting realistic goals, and learning self-acceptance. Discussing how women can maintain meaningful relationships is important. Social support and good coping skills can improve a woman’s self-esteem and give her a sense of mastery. Anticipatory guidance for developmental or expected situational crises can help her plan strategies for dealing with potentially stressful events.
The abundant literature on stress management interventions includes role-playing, relaxation techniques, biofeedback, meditation, desensitization, imagery, assertiveness training, yoga, diet, exercise, and weight control, techniques nurses can include in their repertoire of helping skills. Insufficient time prevents one-on-one assistance in many situations, but the more nurses know about these interventions, the better able they are to intervene, counsel, and direct women to appropriate resources.
Some women must be referred for counseling or other mental health therapy. Careful follow-up of all women experiencing difficulty in dealing with stress is important.
Substance Use Cessation
All women of all ages will receive substantial and immediate benefits from smoking cessation. However, this task is not easy, and most people stop several times before they accomplish their goal (Box 4-9). Many are never able to do so. Those who wish to stop smoking can be referred to a smoking-cessation program where individualized methods can be implemented. At the very least, individuals should be guided to self-help materials available from the March of Dimes, the American Lung Association, and the ACS. During pregnancy, women seem to be highly motivated to stop or at least to limit smoking. Insult to the fetus can be reduced or even prevented if cessation is accomplished by the end of the first trimester (Bernstein, Mongeon, Badger, Solomon, Heil, & Higgins, 2005).
New approaches to increase cessation among smokers and to discourage smoking among young women—especially in adolescence and during pregnancy—are needed. Health care providers can have a positive effect on smoking behavior and should attempt to motivate smokers to stop.
Counseling women who appear to be drinking alcohol excessively or using drugs may include promoting strategies to increase self-esteem and teaching new coping skills to resist and maintain resistance to alcohol abuse and drug use. Appropriate referrals should be made, with the health care provider arranging the contact and then following up to be sure that appointments are kept. General referral to sources of support also should be provided. National groups that provide information and support for those who are chemically dependent have local branches or contacts that are listed in the local telephone book.
Anticipatory guidance includes teaching about the health and safety risks of alcohol and mind-altering substances and discouraging drug experimentation among preteen and high school students, because the use of drugs at an early age tends to be a predictor of greater involvement later.
Sexual Practices That Reduce Risk
Prevention of STIs is predicated on the reduction of high risk behaviors by educating toward a behavioral change. Behaviors of concern include multiple and casual sexual partners and unsafe sexual practices. The abuse of alcohol and drugs also is a high risk behavior and results in impaired judgment and thoughtless acts. Specific self-management measures to reduce risk are described in Chapter 7.
In addition to the prevention of STIs, women of childbearing years need information regarding contraception and family planning (see Chapter 8).
Health Screening Schedule
Periodic health screening includes history, physical examination, education, counseling, immunizations, and selected diagnostic and laboratory tests. This regimen provides the basis for overall health promotion, prevention of illness, early diagnosis of problems, and referral for appropriate management. Such screening should be customized according to a woman’s age and risk factors. In most instances it is completed in health care offices, clinics, or hospitals; however, portions of the screening are now being carried out at events such as community health fairs. An overview of health screening recommendations and immunizations for women 18 years and older is provided in Table 4-3.
TABLE 4-3
HEALTH SCREENING GUIDELINES AND IMMUNIZATION RECOMMENDATIONS FOR WOMEN AGES 18 YEARS AND OLDER
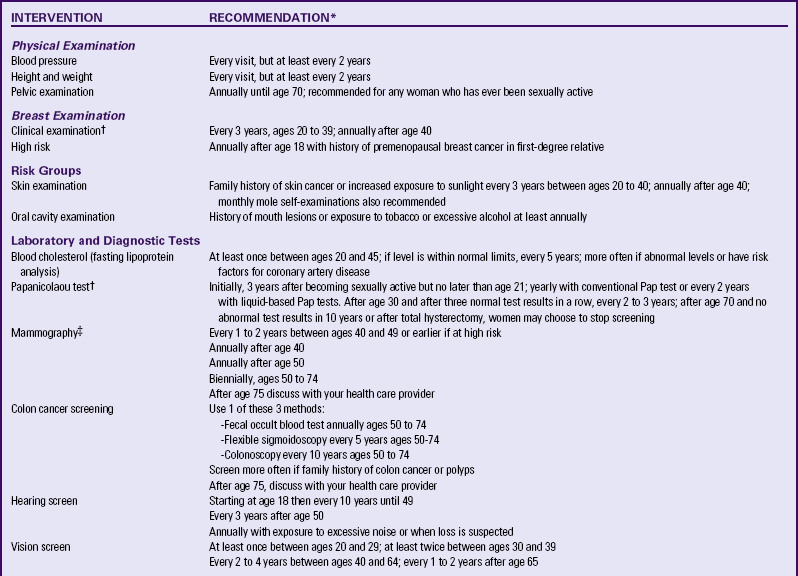
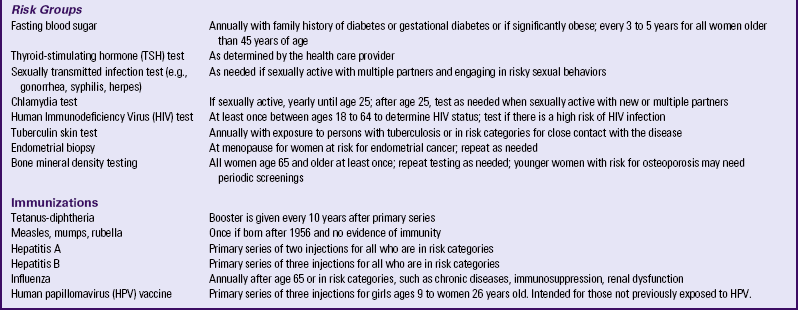
∗The information in this table is only a guide; health care providers will individualize the timing of tests and immunizations for each woman.
†American Cancer Society (ACS). (2010a). Cancer facts and figures, 2010. New York: ACS.
‡Note: No consensus has been reached regarding mammograms for women between 40 and 49 years of age; therefore, various recommendations are listed. Women are urged to discuss circumstances with their health care providers.
Sources: American Cancer Society (ACS). (2010a). Cancer facts and figures, 2010. New York: ACS; American College of Obstetricians and Gynecologists (ACOG). (2009). Response of the American College of Obstetricians and Gynecologists to new breast cancer screening recommendations from the U.S. Preventive Services Task Force. Available at www.acog.org. Accessed January 8, 2010; Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices. (2009). Recommended adult immunization schedule, United States, 2009. Available at www.cdc.gov/vaccines/pubs/ACIP-list.htm. Accessed May 4, 2010; CDC, Workowski, K., & Berman, S. (2006). Sexually transmitted diseases treatment guidelines, 2006. Morbidity and Mortality Weekly Report. Recommendations and Reports, 55(RR11), 1-94; Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. (2001). Executive summary of the third report of the national education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Journal of the American Medical Association, 285(19), 2486-2497; National Women’s Health Resource Center. (2007). Women and health screenings. National Women’s Health Report, 29(5), 1-7; National Women’s Health Information Center. (2009). General screenings and immunizations for women. Available at www.4woman.gov. Accessed January 20, 2010; U.S. Preventive Services Task Force (USPSTF). (2009). Guide to clinical preventive services. Agency for Healthcare Research and Quality (AHRQ) Pub. No. 09-1P006, Rockville MD: AHRQ.
Health Risk Prevention
Simple safety factors often are forgotten or perceived not to be important, yet injuries continue to have a major effect on the health status of all age-groups. Being aware of hazards and implementing safety guidelines will reduce risks. The nurse should frequently reinforce the following common-sense concepts that will protect the individual:
• Wear seat belts at all times in a moving vehicle.
• Wear safety helmets when riding a motorcycle, bicycle, or inline skates.
• Follow driving “rules of the road.”
• Place smoke alarms throughout the home and workplace. Avoid secondhand smoke.
• Lock doors and windows to ensure personal safety.
• Reduce noise pollution or safeguard against hearing loss.
• Protect skin and eyes from ultraviolet light with the use of sunscreen, protective clothing, sunglasses, and hats.
• Never walk or run alone, especially at night.
• Consider storing personal health information (PHI) in a digital database that can be accessed from anywhere you travel.
• Never share computer passwords with strangers to safeguard financial, personal, and health data.
Health Protection
Nurses can make a difference in stopping violence against women and preventing further injury. Educating women that abuse is a violation of their rights and facilitating their access to protective and legal services constitutes a first step. Encouraging health care institutions to implement appropriate domestic violence screening programs also is of great value (see Chapter 5). Other helpful measures for women to discourage their entry into abusive relationships include promoting assertiveness and self-defense courses; suggesting support and self-help groups that encourage positive self-regard, confidence, and empowerment; and recommending educational and skills development classes that will enhance independence and self-care.
Numerous national and local organizations provide information and assistance for women in abusive situations. All nurses who work in women’s health care should become familiar with local services and legal options.
KEY POINTS
• Culture, religion, socioeconomic status, personal circumstances, individual preference, and stage of development are among the factors that influence a woman’s desire for care and her response to the health care system.
• The changing status and roles of women affect their health, needs, and ability to cope with problems.
• Anticipatory guidance is enhanced in a private, safe environment in which the interaction is culturally competent, nonjudgmental, and confidential.
• Preconception counseling allows identification and possible remediation of potentially harmful personal and social conditions, medical and psychologic conditions, environmental conditions, and barriers to care before conception.
• Conditions that increase a woman’s health risks also increase risks for her offspring.
• Periodic health screening, including history, physical examination, immunizations, and diagnostic and lab tests, provide the basis for overall health promotion, prevention of illness, early diagnosis of problems, and referral for management.
• Physical Activity Guidelines for Americans include 2½ hours a week of moderate intensity or 1¼ hours per week of vigorous-intensity exercise, or a combination of both (USDHHS, 2008).
• Health promotion and prevention of illness assists women in actualizing health potential by increasing motivation, providing information, and incorporating recommendations for accessing specific resources.
![]() Audio Chapter Summaries Access an audio summary of the Key Points on
Audio Chapter Summaries Access an audio summary of the Key Points on ![]()