Chapter 10 Effects of radiation
 A beam of X-ray photons is gradually attenuated as it passes through matter by being absorbed and scattered.
A beam of X-ray photons is gradually attenuated as it passes through matter by being absorbed and scattered. The most important interactions that result in attenuation are photoelectric absorption and Compton scatter.
The most important interactions that result in attenuation are photoelectric absorption and Compton scatter. Photoelectric absorption is more likely to occur in dense materials with atoms of high proton number.
Photoelectric absorption is more likely to occur in dense materials with atoms of high proton number. Photoelectric absorption is responsible for differential absorption in the body’s tissues that results in a radiographic image.
Photoelectric absorption is responsible for differential absorption in the body’s tissues that results in a radiographic image. Compton scatter occurs alongside photoelectric absorption and is the dominant process above a setting of 75 kV.
Compton scatter occurs alongside photoelectric absorption and is the dominant process above a setting of 75 kV. Attenuation in the body’s tissues with the transfer of energy and subsequent ionisation may result in deterministic or stochastic biological effects.
Attenuation in the body’s tissues with the transfer of energy and subsequent ionisation may result in deterministic or stochastic biological effects. Radiation protection regulations aim to reduce the risk of stochastic effects and avoid deterministic effects.
Radiation protection regulations aim to reduce the risk of stochastic effects and avoid deterministic effects. Effective dose measured in sieverts (Sv) takes into account different types of radiation and their damaging potential on different tissues and organs in the body.
Effective dose measured in sieverts (Sv) takes into account different types of radiation and their damaging potential on different tissues and organs in the body. X-ray photons produce fluorescence in phosphors, a property utilised in some image recording systems.
X-ray photons produce fluorescence in phosphors, a property utilised in some image recording systems.INTRODUCTION
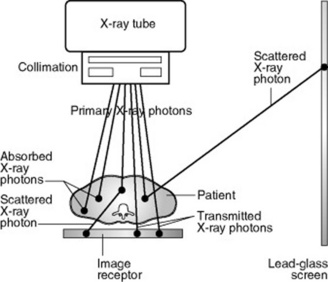
The beam of X-ray photons produced from the X-ray tube will lose its energy by interacting with atoms as it passes through various materials. These include the wall of the X-ray tube and its surrounding oil, the added filter, the collimators, the air, the exposed part of the patient, the couch, the image receptor and the floor. X-ray photons travel through air at virtually the velocity of light (3 × 108 m s−1) so they interact with these materials and transfer their energy almost instantaneously. Some of this energy will be absorbed in the various materials but some will also be scattered in different directions from the primary beam and will lose energy by interacting with other adjacent structures, such as parts of the patient not in the primary beam, the walls of the room and the lead-glass screen.
ATTENUATION
As each X-ray photon can be considered as a tiny packet of energy, the beam of X-ray photons carries energy from the X-ray target into the matter through which it passes. On penetrating matter, X-ray photons transfer energy by interacting with its atoms; this transfer of energy is called attenuation. The beam of X-ray photons is attenuated differently in various materials: in general, the denser the matter, the greater the attenuation. Denser materials include metals (particularly lead) and bone.
Attenuation is partly due to some X-ray photons being totally absorbed and partly to the energy of some X-ray photons being partially absorbed while the remainder is scattered in various directions (Fig. 10.1). Some X-ray photons are transmitted through the material unchanged, without interacting with any atoms.
When a beam of X-ray photons passes through the body, the difference between parts through which X-ray photons are transmitted and those where they are absorbed results in an image.
ATTENUATION AND THICKNESS OF MATERIAL
The number of X-ray photons transmitted compared to the number attenuated in any particular type of material depends on the thickness of that material. In general, the thicker the material, the greater the attenuation. However, it is not a linear relationship where the same numbers of X-ray photons are attenuated in an equal thickness of material, but an equal percentage is attenuated in equal thickness. For example, 20% of photons may be attenuated in the first centimetre of material, then 20% of what is left in the second centimetre, and 20% of the remainder in the third centimetre, etc. This is called an exponential relationship and the percentage attenuated in each thickness is known as the linear attenuation coefficient (LAC or μ) for the specific material. This relationship is used in practice during quality control checks on X-ray equipment to measure the half value thickness/layer (HVT or HVL) of an X-ray unit. The measurement gives the thickness of aluminium that will attenuate 50% of the X-ray photons at a specific kV setting. This gives an indication of the penetrating power of the beam: the thicker the aluminium required to attenuate half of the beam, the more penetrating it is and it can be related (using published tables) to the total filtration present in the beam (see pp. 100, 107).
PHOTOELECTRIC ABSORPTION
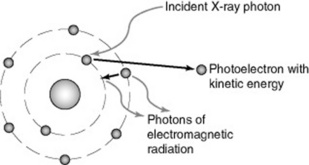
Photoelectric (PE) absorption occurs when an X-ray photon interacts with a bound electron, usually in the inner shell of an atom, when its energy exceeds the binding energy of the electron (Fig. 10.2). The atom may be in the patient (an atom of calcium in bone, for example) or it might be an atom of carbon in the carbon-fibre tabletop; or an atom of lead in the lead-glass screen.
The X-ray photon disappears, by transferring all its energy to the bound electron. This energy overcomes the binding energy of the electron, which then escapes the atom as a photoelectron, carrying any extra energy as kinetic energy.
As a result, the atom is ionised but will quickly regain stability as electrons rearrange within the atom to restore the original electron configuration, resulting in small bursts of electromagnetic radiation being released. This process is similar to that in the X-ray target following ionisation of target atoms by high-speed electrons to release characteristic radiation. In tissue, where elements have low proton numbers and correspondingly low binding energies, the characteristic radiation energies are extremely low and are usually absorbed within the atom with negligible effect.
FACTORS AFFECTING PHOTOELECTRIC ABSORPTION
An X-ray photon is more likely to undergo photoelectric absorption in dense matter containing atoms of higher proton number. It is also more likely to occur with a bound electron whose binding energy is just below the X-ray photon’s energy: this means PE absorption is much more likely to occur in tissue with lower energy X-ray photons of less than 25 keV.
THE IMPLICATIONS OF PHOTOELECTRIC ABSORPTION IN PRACTICE
The main implications to consider are:
The radiographic image
Human tissue can be divided into two basic types: bone and soft tissue. There is also air within the body; for example in the lungs, and there may be pockets of air in the stomach and bowel.
Bone has a fairly high density and contains atoms of calcium and phosphorus, giving an effective proton number (Zeff) of approximately 12. Soft tissues, such as muscle and fat, are lower in density and contain atoms of lower proton number (particularly carbon, hydrogen and oxygen), giving an effective proton number of approximately 7. Air is primarily nitrogen and oxygen, giving a similar effective proton number to soft tissue, but has very low density (Table 10.1).
Table 10.1 The principal constituents of human tissue1
| Material | Density (kg m−3) | Effective proton number |
|---|---|---|
| Bone | 1700 | 12.3 |
| Soft tissue (muscle) | 1000 | 7.6 |
| Soft tissue (fat) | 900 | 6.5 |
| Air | 1 | 7.8 |
All of these elements found in tissue have low binding energies, so typical mean X-ray photon energies of 25 keV used in radiographic imaging (corresponding to a setting of 75 kV; see p. 113) are likely to undergo PE absorption. If all these elements attenuated X-ray photons equally, we would not be able to tell the difference between bone and muscle or bone and air on an X-ray image. But the bone tissue with higher proton number and higher density will experience relatively more PE absorptions – at least eight times more than soft tissue – and air will barely experience any attenuation due to its very low density, leading to what is called differential absorption.
On an X-ray image, this is why bones appear white (many PE absorptions), soft tissues appear grey (some PE absorptions) and air appears black (very few PE absorptions).
X-ray tube filtration
In atoms such as aluminium (Z = 13), with low K shell binding energies, low X-ray photon energies are preferentially absorbed. The quality of the X-ray beam produced from an X-ray tube is increased by attenuating the low energy X-ray photons in a filter made of aluminium (see p. 100).
Use of contrast media
When it is necessary to image the walls and movements of soft tissue structures such as the gastrointestinal tract, a high density/high atomic number contrast medium is introduced. When using iodine or barium-based contrast media (Z = 53 and 56, respectively) K shell binding energies are much higher compared to the body’s tissues, so higher energy X-ray photons are absorbed. This is why higher kV settings are used for contrast examinations.
Shielding
Lead has a very high proton number (82) and is very dense so virtually all X-ray photons are likely to undergo PE absorption in lead. However, a proportion of higher energy photons from the primary X-ray beam will penetrate lead, depending on its thickness. Photons scattered from the primary beam (that have undergone a Compton scatter interaction) will always have lower energy, so lead-glass screens and lead-rubber protective items are designed to prevent the passage of scattered photons.
Absorption edges
Photoelectric absorption is more likely to occur with a bound electron whose binding energy is just below the X-ray photon’s energy, so there will be situations where some bound electrons have binding energies higher than those of the interacting X-ray photons. These electrons cannot contribute to the attenuation of the beam by PE absorption. For example, in lead the binding energy of the K shell electrons is 88 keV and of the L shell 15 keV, so a beam produced at 80 kV will not contain any X-ray photons of sufficient energy to interact with the K shell electrons, only those of the L shell and beyond. If the kV is increased to 90, the beam will contain photons of 90 keV able to interact with K shell electrons. This leads to a large increase in photoelectric absorption of the X-ray photons with energy greater than 88 keV and is known as an absorption edge. Photons with slightly lower energies than 88 keV are much less likely to be attenuated and therefore more likely to be transmitted. This means shielding materials using lead may be slightly less efficient at attenuating photons of this energy. Some manufacturers promote the use of protective aprons made of a composite of materials to give increased attenuation below the 88 keV absorption edge for lead.
Absorption edges also have significance in materials used for filtration. If lead or another material with a high K shell binding energy was used, in addition to attenuating the low photon energies as required, an undesirable proportion of high photon energies at the absorption edge would be attenuated.
Radiation dose
Photoelectric absorption is greater for lower energy X-ray photons and results in total absorption of the photon energy, increasing the radiation dose to the patient. In general, higher kV settings will result in less photoelectric absorption, reducing patient dose, but should not be so high that differential absorption is decreased to the extent of not producing a diagnostic image.
In mammography, where differential absorption in the breast tissue must be maximized, low kV settings are used to increase PE absorption and the contrast between adjacent structures.
COMPTON SCATTER
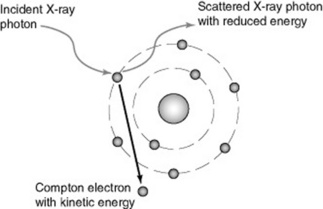
Compton scatter is the alternative interaction process that occurs alongside PE absorption: the two cannot be separated or prevented. In an X-ray beam of mean energy 25 keV (i.e. a setting in the region of 75 kV), approximately half of the interactions occurring will be PE absorptions and the other half Compton scatters. Compton scatter may occur when an X-ray photon interacts with a bound electron in an atom whose binding energy is negligible in comparison with the X-ray photon’s energy.
Compton-type interactions may occur equally with any electron in any atom within the body – in atoms found in soft tissue and in bone as well as with electrons in higher atomic number atoms such as lead.
The X-ray photon transfers some of its energy to the electron and retains the remainder: the photon may retain virtually all of its initial energy and be very slightly deviated or scattered from its track. This is called forward scatter and occurs more frequently with photons of higher energy. Alternatively, lower energy X-ray photons may be scattered out to the side retaining less energy (side scatter) or backwards retaining least energy (backscatter). Scattered X-ray photons always have less energy than the original photon (Fig. 10.3). In all cases, an electron escapes from the atom as a Compton electron, carrying the transferred energy as kinetic energy. Electrons will rearrange in the shells with the emission of electromagnetic radiation as before.
A 25 keV X-ray photon has approximately a 50% probability of undergoing a Compton scatter, irrespective of atomic number. At higher photon energies, there is increased transmission and PE absorption is less likely, so Compton scatter dominates.
FACTORS AFFECTING COMPTON SCATTER
Compton scatter is more likely to occur where the X-ray photon energy is much higher than the binding energy of the electron with which it interacts. It dominates for X-ray photon energies greater than 25 keV. As photon energy increases, the proportion of forward scatter increases whilst back and side scatter decrease. Compton scatter is also more likely to occur in materials containing a higher proportion of hydrogen, such as water, a major component of the body’s soft tissues.
THE IMPLICATIONS OF COMPTON SCATTER
The two main implications to consider are:
Image degradation
A forward scattered X-ray photon may leave the body and reach the image receptor. As it has not travelled in a straight line from the X-ray tube, it may be travelling in a direction as if it had penetrated bone. A large amount of scatter like this reaching the image receptor will cause what should be ‘white’ areas on the image to become grey, or light grey to become darker. This loss of contrast reduces the differences due to PE absorption and degrades the image.
Compton scatter can be reduced by limiting the volume of tissue exposed to the X-ray beam, by collimating to the area of interest. Where a large volume must be exposed, for example when imaging the abdomen, a radiation grid can be used, such as a Bucky oscillating grid built into the couch. These grids absorb (by PE absorption) most of the X-ray photons that have been scattered at a variety of angles towards the image receptor whilst allowing the linearly transmitted photons to pass.
Radiation dose
As the majority of scattered photons are produced from interactions within the patient, some of these photons will be scattered within the patient’s body and will contribute to a low radiation dose to parts of the body other than that intentionally exposed. This cannot be prevented but good collimation, as mentioned above, will minimise internal scatter.
Some scatter will be produced from X-ray photons interacting with structures in the X-ray tube and casing, such as the filter, and from the collimator blades. These scattered photons may also contribute to radiation dose to parts of the body outside that being imaged. The use of appropriate shielding will attenuate most of these photons; for example to protect the gonads during chest radiography.
Compton scattered photons may travel towards the operator: the lead-glass screen is designed to attenuate these scattered photons.
THE FATE OF THE SECONDARY ELECTRONS: PHOTOELECTRONS AND COMPTON ELECTRONS
The photoelectrons and Compton electrons that escape the atom carrying kinetic energy will interact with neighbouring atoms by ionisation and excitation until all their kinetic energy is lost. A typical secondary electron will produce several hundred ionisations within a fraction of a millimetre. This transfer of energy to the surrounding atoms is responsible for radiation dose and may result in biological effects in the individual.
BIOLOGICAL EFFECTS OF X-RAY PHOTONS
Each X-ray photon that interacts in the body by either PE absorption or Compton scatter causes ionisation of the atom and releases a photoelectron or Compton electron that causes further ionisations of surrounding atoms. The majority of these ionisations will occur in atoms that make up non-critical cell structures, such as the cytoplasm. The ionised atom will quickly return to its previous state with no detrimental effect on the cell.
However, the ionisation may occur in an important atom that is part of the DNA molecule in the nucleus of a cell, resulting in a breakage of the chemical bonds between atoms. DNA, or deoxyribonucleic acid, is the part of a cell that carries the genetic code and determines each cell’s type and function. Normally, the cell’s monitoring systems will detect any damage to the DNA and enable a repair.
IONISATION DAMAGE RESULTING IN CELL DEATH: DETERMINISTIC EFFECTS
Sometimes, particularly if both DNA strands are broken, the damage may not be repairable. In this case, the cell will die either immediately, or when the cell attempts division, or of old age, which may be days or even years later. The death of a single cell among millions in a particular tissue does not cause any signs or symptoms. However, higher doses of radiation that might occur following certain lengthy procedures using fluoroscopy, such as angiography/angioplasty or lithotripsy, could damage a significant number of cells and lead to an observable clinical effect.
This type of damage is known as a deterministic effect, or tissue reaction, and gives symptoms related to the tissue damaged once a certain threshold dose is reached. As the radiation dose is increased, the severity of the damage increases. For example, damage to the skin where the X-ray beam has entered the body may result in a reddening in this area (erythema) that appears within a few days of exposure; further or higher doses of ionising radiation may result in a thinning of the skin (desquamation). Damage to the lens of the eye may result in a clouding of the lens in the years following exposure; with higher doses this may progress to a cataract. These types of effect do not normally occur following diagnostic imaging procedures as radiation doses are too low.
However, embryonic tissue is very sensitive to ionising radiation damage, and doses from abdominal/pelvic computed tomography (CT) examinations or a barium enema, particularly if performed more than once during the first two weeks of gestation, could result in death of the embryo or gross malformations.
IONISATION DAMAGE RESULTING IN MISREPAIRED DAMAGE: STOCHASTIC EFFECTS
There is a possibility that following ionisation of an atom making up a DNA molecule, the damage is misrepaired, resulting in a gene mutation. In most cases, the cell will die as a result. If the cell survives, the mutation may contribute to the induction of malignancy in the cell; that is, the start of a cancer. Radiation-induced cancers are usually leukaemias or lymphomas rather than the more common types, such as cancer of the lung, breast or prostate. If the mutation occurs in a sperm or egg cell, an induced cancer could occur in a subsequent child.
There is a risk of inducing cancer with any dose of ionising radiation and the risk increases with increasing dose.
RADIATION PROTECTION
The risk of stochastic effects and the potential for deterministic effects mean the use of ionising radiation for diagnostic imaging is a compromise between maximising the diagnostic information and minimising the radiation dose to the patient. All exposures should be as low as possible to reduce the risk of stochastic effects and avoid deterministic effects.
People working with ionising radiation may also be exposed to levels higher than those received from natural background radiation.
In the UK, the Health and Safety Executive enforces regulations relating to ionising radiation (see p. 13). These are in two parts: the current Ionising Radiations Regulations 1999 apply to employers using ionising radiation, such as hospital Trusts, and requires them to protect all employees by ensuring any exposures are as low as reasonably achievable and do not exceed specified dose limits. This is achieved by ensuring equipment, shielding and working practices are safe and by monitoring effective doses received by employees during their work.
The Ionising Radiation (Medical Exposure) Regulations [IR(ME)R] 2000 apply primarily to patients undergoing investigations or treatment using ionising radiation, such as radiographic imaging. Every medical exposure must be:
HOW DO WE QUANTIFY ‘RADIATION DOSE’?
When we use the terms ‘dose of ionising radiation’ or just ‘radiation dose’, we mean how much energy has been deposited in the organs and tissues of the body following attenuation of a beam of ionising radiation. This is called the absorbed dose and is measured in units of gray (Gy), where 1 Gy equates to 1 joule of energy deposited per kilogram mass.
However, absorbed dose does not take into account the damaging potential of different ionising radiations, such as alpha particles, nor the sensitivity to the induction of stochastic effects of different organs and tissues in the body. The International Commission for Radiological Protection (ICRP) has calculated factors to take into account both of these variables. Radiation weighting factors for different types of ionising radiations convert absorbed dose into equivalent dose. Tissue weighting factors convert equivalent dose into effective dose, measured in sieverts (Sv) or, more usually in radiation protection, a thousandth of a sievert: the millisievert (mSv). Effective dose can then be used to compare absorbed doses from different ionising radiations and to an exposed part of the body, such as the chest, in relation to the effect of that dose on the whole body.
For example, an absorbed dose of 1 mGy of X-ray photons to the whole body would include all the sensitive structures, giving an effective dose of 1 mSv. If an absorbed dose of 1 mGy was confined to the lungs, using the ICRP’s tissue weighting factors, the effective dose would be 0.12 mSv, owing to no other sensitive organs in the body receiving any of the dose. If the 1 mGy were confined to the thyroid gland, the effective dose would be 0.05 mSv. This indicates the greater sensitivity of the lungs to the risk of stochastic effects compared to the thyroid. If both of these organs are irradiated but no part of any other sensitive structure, the effective dose would be 0.17 mSv.
Effective doses for the average-sized person can be approximated for radiographic imaging of all parts of the body and can be compared to the effective dose received from natural background radiation over a period of time. The average background dose in the UK is 2.2 mSv per year (Table 10.2).
Table 10.2 Typical effective doses for diagnostic medical exposures2
| X-ray examination | Typical effective doses (mSv) | Equivalent period of natural background radiation |
|---|---|---|
| Limbs and joints (except hip) | <0.01 | <1.5 days |
| Teeth (single bitewing) | <0.01 | <1.5 days |
| PA chest | 0.02 | 3 days |
| Skull | 0.07 | 11 days |
| Cervical spine | 0.08 | 2 weeks |
| Hip | 0.3 | 7 weeks |
| Thoracic spine | 0.7 | 4 months |
| Pelvis/abdomen | 0.7 | 4 months |
| Lumbar spine | 1.3 | 7 months |
| Barium swallow | 1.5 | 8 months |
| IVU | 2.5 | 14 months |
| Barium meal | 3.0 | 16 months |
| Barium enema | 7.0 | 3.2 years |
| CT head | 2.0 | 1 year |
| CT chest | 8.0 | 3.6 years |
| CT abdomen/pelvis | 10.0 | 4.5 years |
CT, computed tomography; PA, posteroanterior; IVU, intravenous urogram
In practice, effective dose is a complicated calculation for the individual patient, so if the X-ray set is fitted with a DAP (dose–area product) ionisation chamber (see pp. 126–127), a DAP reading can be recorded. This is the radiation dose to air multiplied by the area exposed, giving a reading in Gy cm2. Again, it is not easily related to effective dose, but the accumulated DAP reading can be recorded for each examination and used to compare relative exposures. If other factors such as source–image distance (SID) and kV are recorded, effective dose can be calculated retrospectively if required.
FLUORESCENCE
Some materials, called phosphors, convert X-ray photons into light photons. This means they glow when exposed to an X-ray beam. As the energy of an X-ray photon is much greater than that of a light photon, one X-ray photon may be converted into hundreds of light photons. The colour of the light emitted depends on the type of phosphor. In certain phosphors this effect is instantaneous and is known as fluorescence. Fluorescent phosphors such as gadolinium oxysulphide are utilised in the intensifying screens used in conventional film-screen imaging systems (see p. 140).
Some phosphors store the X-ray photon energy temporarily and emit the energy as light over a period of time (luminescence). Other phosphors store the X-ray photon energy for an indefinite length of time. When the atoms storing the energy are stimulated by the energy in a laser beam, the energy is converted into light and emitted. These phosphors (e.g. barium fluorohalide) are known as ‘storage phosphors’ and are used in computed radiography (CR) imaging plates.
1 Johns HE, Cunningham JR. The physics of radiology, 4th edn, Springfield, Ill: Charles C Thomas; 1983:723-724.
2 Health Protection Agency (HPA). www.hpa.org.uk/radiation/understand/radiation_topics/medical/ted_equivalent.htm
Ball J, Moore AD. Essential physics for radiographers, 3rd edn. Oxford: Blackwell Science, 1997.
This text provides useful background physics of energy, atomic structure and electricity plus deeper insights into key areas of radiographic science. Note, however, it was published in 1997, prior to the current Ionising Radiations Regulations of 1999 and 2000, as given below..
SC Bushong. Radiologic science for technologists, 8th edn. St Louis: Mosby. 2004.
Chapters 33 to 37 give a deeper insight into the biological effects of ionising radiation, including a review of human biology, radiobiology and the early and late effects of exposure to ionising radiation.
Be aware that subsequent chapters refer to radiation protection legislation in the United States and although the principles are the same anywhere in the world, the regulations are not!
The Ionising Radiations Regulations 1999 (SI No. 3232). London: HMSO.
The Ionising Radiations (Medical Exposure) Regulations 2000 (SI No. 1059) London: HMSO.