Chapter 8 Clinical reasoning
the core of clinical practice
One of the most difficult aspects of creating a successful clinical practice revolves around developing efficient clinical reasoning skills. Proficiency in assessment directly interfaces with the ability to determine which modalities and strategies to use and which to avoid, how long and how often to apply them, which communication skills are effective for each person, when to refer to another practitioner, and a number of other critical factors of the treatment plan. The less experienced practitioner needs to acquire the skills right away, yet, by nature they develop primarily with experience and practice. This same inexperienced practitioner might usefully take a course in the concepts of clinical reasoning (or read a chapter such as this); however, true clinical reasoning skills develop over time and, while they need to contain a number of essential features, are uniquely individual to each practitioner. A component of clinical reasoning involves the individual achieving a balance between what has been termed evidence based practice and practice that is based on his/her own experience.
The first portion of this chapter looks at some of the components of clinical reasoning skills, the review of which may help the practitioner to effectively begin to develop these. The remainder of the chapter discusses evidence of effectiveness of manual techniques in the presence of known pathologies. For concepts in addressing specific conditions and discussion of ‘red flag’ warning signs, the reader is directed to Clinical application of neuromuscular techniques: Case study exercises (Chaitow & DeLany 2005, Churchill Livingstone).
A thorough discussion of clinical reasoning can be found in Clinical reasoning in the health professions, 3rd edn (Higgs et al 2008, Elsevier). The authors of this text gratefully acknowledge it as a primary source of some of the following information. An additional source of information derives from the chapter The role of clinical reasoning in the differential diagnosis and management of chronic pelvic pain by Diane Lee & Linda-Joy Lee (Chaitow and Lovegrove 2011).
Evidence vs experience
An important question arises, which impacts directly on clinical reasoning: should evidence change the way manual therapy is practiced?
Therapists and practitioners might be justifiably concerned as to whether techniques and approaches that have previously been found to be useful might need to be abandoned, due to lack of supporting research evidence or on the basis of studies that fail to provide concrete evidence of efficacy. When considering this, it is important to retain a perspective that recognizes that lack of proof does not equal disproof. It is also possible that ‘evidence-based practice’ – in the strictest sense – is not possible to achieve in manual therapy since so much of what is done clinically has not been specifically researched – and when assessment and treatment methods have been studied, results have frequently been equivocal (Seffinger et al 2004, Hsieh et al 2000).
Scientific evidence should inform practitioners about clinical work and influence assessment approaches and treatment choices. However, it is not possible to base practice only on manual palpation and treatment techniques that have been supported by high-quality evidence – this simply does not exist. It is possible that there will never be sufficient supportive evidence for all manual techniques used due to the cost and difficulty of the research that would be required.
Another consideration is that many studies examine single modalities (Ballantyne et al 2003, Lenehan et al 2003, Wilson et al 2003), while in a manual therapy practice, techniques are usually used in combination (for example, myofascial release and muscle energy techniques), rather than in isolation, as described later in the chapter (Noll et al 2000). As a result, the contribution to outcomes of individual modalities remains difficult to judge.
With these thoughts in mind, it is important to emphasize that it would be unwise to abandon techniques that have a long history of anecdotal evidence of efficacy, but which currently lack scientific support. Hence, clinical practice might benefit significantly from a combination of evidence-based research and clinical experience. See Box 8.1 for a brief evaluation of these issues.
Box 8.1 Evidence based practice (EBP)
There is unquestionably a need for research to validate the efficacy of manual treatment. To a large extent, this derives from demands from governments, health authorities, and insurers to prove that what is done in manual clinical practice actually works and is safe. There is also an academic, intellectual, desire to understand the nature of the dysfunctions being treated and why (or whether) manual treatment can effectively modify or remove these?
Research should, therefore, enable practitioners and therapists to objectively examine and determine the most effective ways to treat their patients, feeding into clinical reasoning, and evidence based practice (EBP).
And, of course, when actual evidence emerges from research that a particular approach or modality has no therapeutic benefit, or that it lacks reliability and validity as a diagnostic or therapeutic approach, or that it poses potential dangers to the patient, practitioners have an intellectual and ethical duty to reconsider their practice of that approach.
Origins
The term ‘evidence based’ was first promoted by Eddy (1991), while the expression ‘evidence based medicine’ (EBM) was coined by Guyatt et al (1991). The natural evolution of these ideas pointed towards evidence based practice (EBP). Subsequently the methodologies used to determine ‘best evidence’ were largely established by a Canadian McMaster University research group, led by David Sackett and Gordon Guyatt (Jaeschke et al 1994, Sackett et al 2000, Guyatt et al 2004).
Guyatt (1992), a Scottish epidemiologist, has been credited with increasing the acceptance of the principles behind evidence-based practice. His work led to the naming of centers of evidence based medical research, as Cochrane Centers, which form the Cochrane Collaboration. Evidence-based medicine categorizes and ranks different types of clinical evidence, using terms such as ‘levels of evidence’ and ‘strength of evidence’ to refer to the protocols for ranking evidence that emerges from research studies, based on the quality of the study being examined, and its relative freedom from bias.
The highest level of evidence for therapeutic interventions is considered to be a systematic review, or meta-analysis, that includes only randomized, double-blind, placebo-controlled trials that involve a homogenous patient population and condition.
In the EBM/EBP model, evidence that derives from expert opinion is considered to have little value, being ranked lowest due to the placebo effect, the biases inherent in both the observation, and reporting of cases, and difficulties in discerning who is actually an ‘expert’.
What are the practical implications of EBM and EBP?
Evidence-based practice (EBP) embraces all disciplines of health care (not just medicine) and has become synonymous with best practice. However, what are the practical implications of EBP?
Is it possible for a clinician to only use assessment tests, and treatment techniques/protocols, that have been validated through the scientific process, using evidence from high ranking studies as valued by the ‘levels of evidence’?
Such a clinical approach would be difficult (if not impossible) to adhere to for a variety of reasons; one being that there is unlikely to ever be enough evidence for every situation met in clinical practice?
The place for experience
Sackett et al (2000) defined evidence-based practice as ‘the integration of best research evidence, with clinical expertise and patient values’.
They note that, ‘External clinical evidence can inform, but can never replace individual clinical expertise, and it is this expertise that decides whether the external evidence applies to the patient at all, and if so, how it should be integrated into a clinical decision.’
Clinical expertise, therefore, comprises both such evidence as exists, as well as skills and experience – with the practitioner/therapist knowing what, and how, to do the right thing at the right time (i.e., a combination of clinical reasoning and skill).
• The type of knowledge gained from scientific studies contributes to building only one kind of knowledge.
• However, in evidence-based practice, according to Sackett et al’s definition (2000), clinical expertise plays an equal role alongside any research evidence.
• A third component of evidence-based practice involves the patient’s values and goals, which come from the person who all of the research and expertise is intended to benefit.
Recently, the term ‘evidence-informed’ has surfaced, the intent being to suggest that since there is not enough research evidence for every situation met in clinical practice, the clinician should be informed of what is known and make their clinical decisions accordingly. However, if we adopt Sackett et al’s definition of EBP, there is no need to modify the term, since clinical expertise (reasoning and skill) is seen to form a major part of the definition of best practice.
The implications of the discussion, and evidence found in Box 8.1 suggests that clinical reasoning – at least in part – depends on the practitioner’s grasp of the balance between evidence, information and clinical experience.
An aspect of the process of clinical reasoning, therefore, involves empiricism – the use of knowledge deriving from evidence gathered via the senses and the interpretation of what the clinician sees, hears and feels, in relation to the patient. A major feature of the gathering of evidence in manual therapy settings, therefore, derives from palpation and observation.
• Bullock-Saxton (2002) has observed that: ‘Strategies taught to enhance clinical reasoning should ensure a high level of knowledge and organization of that knowledge; the development of a capacity to accurately perform technical and manual skill … and encouragement to understand any [clinical] problem at a deeper level.’
• In relation to palpation and observation evidence, Lee & Lee (2002) suggest that clinical reasoning – for example, in a setting that involves assessment of the mobility of particular joints – requires that a number of different tests be employed to reach a conclusion of hypomobility, hypermobility or instability. They insist that such a conclusion cannot be reached from one test alone.
• The importance of not relying on only one test, or assessment method, when attempting to devise a therapeutic plan is highlighted by May et al (2010) in their systematic review of the reliability of physical examination procedures, used in 36 separate studies of the clinical examination of patients with shoulder pain. May et al found that ‘Overall, the evidence regarding reliability was contradictory’ and that ‘There is no consistent evidence that any examination procedure used in shoulder assessments has acceptable levels of reliability.’ They add that, because tests are frequently used in conjunction with each other to support clinical decision-making, it might be that when used in this way, these tests are more reliable. Clinical reasoning, in relation to any patient with a shoulder problem (and by implication, almost all musculoskeletal conditions), demands that such cautionary analysis of the validity of individual assessment tests should be kept well in mind. To repeat the caution of Lee & Lee: conclusions cannot be reached from one test alone.
• Discussing chronic pain, Dommerholt (2009) notes that the initial clinical task relates to obtaining information, regarding the causes of any problem, as well as the nature of the patient’s local and global tissue-status and stress adaptability. Clinicians are urged to strive for completeness in their observations, and, to that end, a thorough examination is required involving a detailed patient history, observation, functional evaluation, palpation and the drawing of relevant conclusions (Materson & Dommerholt 1996). It is also important, as part of the ongoing process of clinical reasoning, that new data should be collected at each encounter, with a flexible attitude being maintained regarding the initial clinical hypotheses, which may need to be modified to facilitate efficient and effective patient management (Jones 1994). An important, obvious, but often neglected observation is that a diagnosis – for example, of myofascial pain syndrome – does not exclude other possible problems being involved, such as joint dysfunction or metabolic insufficiency. The process of clinical reasoning demands – at all times – that all possible contributing factors to the pain syndrome be considered.
• Dommerholt (2009) also notes that, in the context of all possible contributing factors being considered as part of the process of clinical reasoning, particular importance should be given to evaluation of the emotional and psychological aspects of individuals with chronic pain. Attempts should be made to gain insights into cultural, familial and interpersonal dynamics, coping skills and the presence of fear avoidance (Bennett 2002, Vlaeyen & Linton 2000). With these thoughts in mind it is useful to remember that the chronicity of a pain problem may be related to specific stressful conditions or situations, and these need identifying.
The authors of this text would add other considerations to the clinical reasoning reflections required. The following are examples of strategic questions that can be used to provide comprehensive data to the assessment.
• What information has been gathered by means of observation, listening and palpation, and how does this data relate to the presenting symptoms of the patient?
• How fragile, robust, sensitive, and/or adaptively compromised is this individual?
• What factors aggravate, modulate or relieve the patient’s condition/symptoms?
• What variables can be identified (rest, activity, diet, emotions, weather, temperature, etc.) that relate to the reported symptoms?
• What lifestyle or habits-of-use changes might usefully be suggested?
• What bodywide influences – for example, posture, breathing patterns, or (lack of) lymphatic movement – might be influencing symptoms?
• What evidence exists in the literature that might inform the clinical reasoning process, based on the evidence gathered?
The issue of what has become known as clinical prediction rules, which is explored in Box 8.2, might also be considered. While it remains unclear as to the degree of value clinical prediction rules will provide, it is obvious to the authors of this text that clinical decision-making benefits from sound development of practical skills, from clinical experience, and from evidence-based research, when it is available.
Box 8.2 Clinical prediction rules (Chaitow 2010)
A trend in manual therapy has been the development of clinical prediction rules (CPR).
These are ‘rules’ that are derived statistically – literally ‘translated’ – from research evidence, with the aim of identifying the combinations of clinical examination findings that can predict a condition or outcome (Fritz et al 2003, Fritz 2009, Cook 2008).
Falk and Fahy (2009) have summarized the key element of CPR as follows:
Clinical prediction rules quantify the contribution of symptoms, clinical signs, and available diagnostic tests, and stratify patients according to the probability of having a target disorder. The outcome of interest can be diverse and be anywhere along the diagnostic, prognostic, and therapeutic spectrum.
In manual and movement therapies, this might translate into a focus on particular problems, such as nonspecific low back pain (LBP), as well as those patients enduring this condition. This allows for a degree of categorization – so predicting which forms of treatment would be most likely to be of benefit to LBP in general, and/or which specific subgroups of patients with LBP should be targeted with particular therapeutic approaches.
If such prediction were reliable, this would make clinical reasoning a lot easier. All that would be needed would be to slot a particular patient, with a particular set of symptoms, into a category, and to treat according to the prediction rules.
The obvious question arises as to the reliability of the tests involved in producing such categorization.
Reliability?
Patelma et al (2009) examined inter-tester reliability in classifying sub-acute low back pain patients, comparing specialist and non-specialist examiners. They observed:
Although a number of LBP classification systems have been proposed, such as a pathoanatomical/pathophysiological classification system, the McKenzie classification, treatment-based classification, and the movement-impairment classification, what is still unclear is which clinical tests, between two assessing clinicians, are sufficiently reliable to allow subgroup categorization. The reliability and validity of the overall classification systems has been tested and has been reported as moderate or good.
Not surprisingly, the better trained the individual practitioners, the more accurate the findings.
As to the reliability of tests used for placing types of low back pain into separate groupings, the evidence is variable.
Patelma et al (2009) summarize the current situation as follows:
• Discogenic and sacroiliac joint pain: fair to good
• Segmental dysfunction/facet pain: poor
• Clinical lumbar instability: poor to good
• Clinical central or lateral stenosis: no reliable clinical tests, however a self-reported history questionnaire has been shown to be a useful diagnostic tool for lumbar spinal stenosis.
A further obvious question is whether classification of different types of low back pain actually improves clinical outcomes. In a study involving over 2000 patients with ‘mechanical low back pain’, in which there was no direct reference to anatomic site, or pathological process, Hall et al (2009) observed that:
Caution
Lee & Lee (2011) caution that while the use of clinical prediction rules may be useful as part of decision making, they should not replace clinical judgment. Instead, they should be seen as complementary to that process – which needs to involve experience, clinical opinion, and intuition as well as research evidence (see Box 8.1).
It is important to acknowledge that while statistical evidence tells us about the average response of a group, defined by the characteristics used in design of the study, in practice, individual symptoms and circumstances may be identified to a greater or lesser degree than such averages suggest would be the case –or particular conditions might even present quite differently.
Most experienced clinicians are well aware of patients they have seen who display symptoms and characteristics that are not the same as those suggested by data from clinical trials. It is also useful to acknowledge that information deriving from research may at times be subject to bias during the process of interpretation as to the conclusions that are drawn. It is also worth reemphasizing that a lack of evidence does not invalidate a technique, or an approach that has been shown by experience to have clinical value, even if it does not fit with clinical prediction rules.
Clinical pathways
There is yet another trend in medicine, nursing and midwifery that deserves brief comment, since it seems to be a movement away from clinical reasoning, toward pre-planned therapeutic methods. This known as ‘clinical pathways’. This process is also known by other terms, including care pathways, critical pathways, integrated care pathways, or care maps.
A definition of clinical pathways has been suggested as:
A multidisciplinary management tool, based on evidence-based practice, for a specific group of patients with a predictable clinical course, in which the different interventions by the professionals involved in the patient’s care are defined, optimized and sequenced, either by hour, day (acute care) or visit (homecare). Outcomes are tied to specific interventions.
Clinical pathways have multiple aims, including standardizing practice, importing external evidence into local health care work, and improving inter-professional co-ordination.
Are clinical pathways successful?
In some settings it appears to be so, in others not.
• Barbieri et al (2009) concluded – following a meta-analysis of 22 studies – that, in relation to hip replacement surgery, ‘clinical pathways can significantly improve the quality of care even if it is not possible to conclude that the implementation of clinical pathways is a cost-effective process, because none of the included studies analyzed the cost of the development and implementation of the pathways.’
• However, in nursing and midwifery contexts, Hunter & Segrott (2006) reported that their review found limited evidence of clinical pathways’ impact on client care; although research suggests that they may be most suitable for predictable, routine surgical procedures.
Manual therapists are only likely to be confronted by this model when working as part of a multidisciplinary team. Clinical pathways’ usefulness seems to be proven where virtually mechanistic protocols apply – as in joint replacement surgery – however, its equivocal usefulness in nursing settings, does not bode well for its application in manual therapy settings – where it appears to be designed to virtually remove clinical reasoning from the process.
Further thoughts on clinical reasoning (see Figure 8.1)
Acquiring skills is imperative to performance in almost all aspects of life. Whether cooking, competing in sports, building a house, playing music, sewing, acting, or driving a car, adequate training as well as the degree and quality of practice of the skills undoubtedly play roles in the degree of excellence in performance. The same is true of performance as a practitioner in a health care practice. The knowledge and skills acquired through primary education, continuing education, and from reading books and articles, apply within the practice and directly relate to therapeutic success.
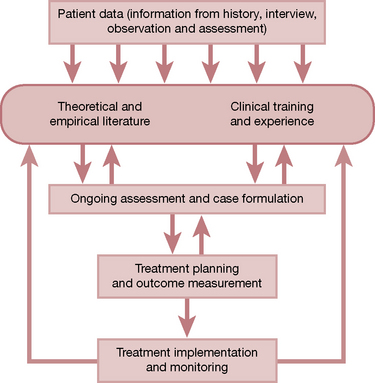
Figure 8.1 Treatment choices are based on an ongoing cycle of gathering of information, formulating ideas and implementing strategies, the results of which constantly influence future choices.
While some cases present with an enormous degree of available data and an understanding of their health condition, many patients enter the treatment room knowing very little about their own health status. It is the responsibility of the practitioner to accumulate information through interviews, assessments, examinations, tests, and details acquired from other practitioners, in order to determine the course of treatment best suited for the case. When initial information regarding a case is given, each practitioner approaches it from a unique perspective and with a skill set based on his/her own education, experience and cognition. These, combined with input from the patient’s perspective, will determine how the practitioner intellectually processes the data, constructs a treatment plan and works with the case. Clinical reasoning, therefore, forms the roots of the practice – the platform on which decisions and actions stand, and from which future inquiries and investigations will stem.
How did that master practitioner – the expert clinician – become so skilled? How can he/she seem to arrive quickly at conclusions, formulate questions that uncover key components of the case, and implement strategies for treatment? How does he/she know which simple statements made by the patient might be significant clues to the condition from which the patient suffers? How can another practitioner get to that place – as soon as possible – where the information, in its myriad of forms, can be deciphered as to which details are important, which are critical and which are simply sidebars in a complex case history? How then do clinical reasoning skills develop and how can that development be encouraged?
Higgs et al (2008) suggest the following definition of the complex phenomenon that we call clinical reasoning.
Clinical reasoning (or practice decision making) is a context-dependent way of thinking and decision making in professional practice to guide practice actions. It involves the construction of narratives to make sense of the multiple factors and interests pertaining to the current reasoning task. It occurs within a set of problem spaces informed by the practitioner’s unique frames of reference, workplace context and practice models, as well as by the patient’s or client’s contexts. It utilizes core dimensions of practice knowledge, reasoning and metacognition, and draws on these capacities in others. Decision making within clinical reasoning occurs at micro, macro and meta levels and may be individually or collaboratively conducted. It involves metaskills of critical conversations, knowledge generation, practice model authenticity and reflexivity.
Higgs et al (2008) note that the process of clinical reasoning includes core dimensions of:
• Knowledge – a base derived from specifics within the discipline (massage, physical therapy, osteopathy, etc.), including theory and research, as well as professional and personal experience.
• Cognitive or reflective inquiry – thinking skills used to analyze, evaluate and synthesize the collected data.
• Metacognition – reflective self-awareness that bridges knowledge and cognition, allowing the practitioner to evaluate inconsistencies, unexpected findings and limits in the quantity or quality of data presented.
Additionally, other dimensions are included, such as incorporating the patient in the decision-making process (mutual decision-making), contextual interaction (interface between decision makers and the situation or environment), and task impact (influences of the clinical problem or task on the reasoning process).
Higgs et al add four metaskills to these dimensions:
• ‘The ability to derive knowledge and practice wisdom from reasoning and practice …
• The location of reasoning as behaviours and strategies within chosen practice models, each with an inherent philosophy of practice
• The reflexive ability to promote positive cognitive, affective and experiential growth, not only in the well-being of the patients but also in the capabilities of oneself as practitioner
• The use of critical, creative conversations to make clinical decisions.’
Clinical reasoning, then, is not a specific process, but an integrative and synthesizing phenomenon. It includes the ability to evaluate circumstances, maintain critical conversations based on those evaluations and, where possible, promote customized, person-centered healthcare plans. There is certainly an overlap of reasoning skills between various professions; however, due to the very nature by which clinical reasoning develops, there are also significant differences – between professions and among practitioners within the same profession. These differences, while sometimes being the source of debate and conflict (even animosity), also highlight an inherent value in multi-practitioner practices and the extraordinary value of interface within multi-disciplinary practices. Since no two practitioner minds think exactly alike, each has a slightly, or sometimes significantly, different view on the meaning of the data. What one practitioner might overlook, or consider unimportant, another might find as a significant clue and take an action that otherwise would not occur.
Added to this picture is the load of information and self-awareness that the patient/client brings to the picture. Until the most recent years, the patient/client had little understanding of medical conditions and virtually no avenues to pursue understanding, other than, perhaps, a simple pamphlet given at the doctor’s office. He/she was expected to simply show up to appointments, submit to testing and diagnosis, and to compliantly follow whatever treatment plan was designed.
As the world-wide-web became available to the average living room, educational resources opened and the knowledge base broadened. The ‘patient’ became a ‘client’ and healthcare became a commodity for purchase. Smart and well-informed ‘shopping’ emerged within healthcare markets and expectations rose - for collaborative (practitioner/patient) decision-making, recognition of cultural differences, and incorporation of alternative and complementary therapies alongside (and sometimes in place of) mainstream medicine. These changes support a driving force that promotes health care reform and revisions to the very foundations by which health care is delivered. The patient/client now often seeks ‘experts’ who have deep knowledge and well-honed skills, and who also genuinely care about the patient/client’s individual needs and personal circumstances. Patient-compliance and concordance is being replaced by patient education and information sharing, collaborative decision-making, and effective communication, combined with sound knowledge and a patient-centered philosophy of practice.
NMT concepts and methods applied in situations of pathology, rather than dysfunction
The meaning of symptoms
Symptoms are frequently evidence of self-regulation in action – to be understood, respected, assisted and possibly modulated if excessive (inflammation is a clear example) – and, ideally, not to be suppressed.
Pain, arguably the most common symptom of all, epitomizes the need to understand the sources and mechanisms involved, and the processes associated with its origin and maintenance. Merely suppressing pain without such understanding and, where possible, taking appropriate action to relieve symptoms and remove causes, is a prescription for chronicity.
• a warning (hand touches a flame)
• a caution not to move the area (due to a tear, a break or a process of degeneration)
• part of a protective process
• a signal that repair is underway (inflammation, etc.)
• a remnant of past trauma or dysfunction that has little current relevance (e.g. post-herpes pain)
• evidence of neural sensitization or other forms of neurologically mediated distress or pathology
• reflexogenic activity (viscerosomatic, somaticovisceral, myofascial trigger point, etc.)
• or that an essential nutrient may be missing or out of balance, such as a vitamin or mineral.
Pain and the mind
Pain may also have many other possible meanings (e.g., psychogenic). Understanding the processes involved in the production and maintenance of pain (or other symptoms) is clearly desirable in making clinical choices; however, practitioners/therapists should always go beyond the obvious and should include not only the structural/physical aspects of any problem but also biochemical and psychosocial contextual ramifications and influences.
A comprehensive review (Linton 2000) of over 900 studies involving back and neck pain concluded that psychological factors play a significant role, not only in chronic pain but also in the etiology of acute pain – particularly in the process of transition to chronicity. Linton concluded, ‘Stress, distress or anxiety as well as mood and emotions, cognitive functioning, and pain behaviour all were found to be significant in the analysis of 913 potentially relevant articles.’
In an athletic (or any other) injury setting, the need to consider both the context and all aspects of the individual and the injury event becomes obvious.
Crown et al (1997) have observed:
Both extrinsic and intrinsic factors can increase the risk of injury. Extrinsic factors include training errors, faulty technique, poor environmental conditions, incorrect equipment and surfaces. Intrinsic factors include biomechanical deficiencies including malalignment of limbs, muscular imbalances, degenerative processes, and other anatomical factors.
A fuller list of additional factors might also include nutritional imbalances, past and present pathological processes, adaptive changes to previous injury or repetitive microtrauma, hormonal influences, and hydration. These and many other factors are considered at length, in earlier chapters, including posture (Chapter 2), gait (Chapter 3), the close environment (Chapter 4), adaptation and sport (Chapter 5), and nutrition (Chapter 6), as well as in volume 1 of this text.
Clinical reasoning requires that as many such features and factors as possible are evaluated and considered and, where evidence exists, this, too, should be a feature of the reasoning process, alongside clinical experience.
Evidence for combined use of NMT modalities
As discussed earlier in this chapter, clinical practice commonly involves the use of combinations of modalities, appropriate to the patient’s needs. In the process of clinical reasoning and decision-making, it is useful to have evidence of the value of such approaches – in a variety of therapeutic and clinical contexts, even if patients with such conditions are unlikely to be treated in a manual/physical therapy setting.
Examples are given below of just such combined use of key elements of NMT practice. Numerous additional examples of use of these methods in treatment of specific musculoskeletal conditions are found throughout this text in the appropriate chapters (lumbar spine, pelvis, hip, knee, foot, etc.) as well as in Chapter 9, in which modality variations are summarized.
Apart from the more obvious use in treatment of musculoskeletal conditions, the modalities used in NMT include a number that have been usefully employed in treatment of symptoms of pathological conditions – including myofascial release (MFR), trigger point deactivation, manual lymphatic drainage (MLD), muscle energy technique (MET), positional release (PRT), massage, and more. This discussion should not be taken to imply that these modalities aim to treat the actual pathology – rather, that the intrinsic immune and defense functions of an individual who is ill may be assisted by such treatment.
For example, whatever the underlying health condition, it seems reasonable to assume that – as examples – improved lymphatic flow, or enhanced breathing potential, or greater spinal/thoracic flexibility, may offer broad benefits in terms of the general economy of the system that is fighting to restore health.
Is there evidence that this may be a valid assumption?
In considering severely ill, hospitalized, individuals, one measure of enhanced functionality might be a comparison between people with similar conditions – such as pneumonia – some of whom receive standard medical care, and others who receive the same medical care, plus interventions that incorporate those modalities listed above.
If the manual modality group showed a reduced length of hospital stay, and/or reduced need for medication, the authors of this text believe that it would be reasonable to ascribe (at least most of) the benefits to the manual treatment.
And that’s just what has been shown in a number of important studies.
OMT
Before outlining brief details of these, it may be useful to explain a key acronym: OMT.
OMT stands for osteopathic manual treatment – and this is non-standard, in that each patient is treated according to need. Rather than each patient receiving a standard, formulaic treatment, the practitioner delivering the OMT would select from MET, PRT, MFR, HVLA, trigger point deactivation, soft tissue mobilization, etc., in an effort to (as examples) release hypertonicity, enhance circulation and drainage, ease pain, and generally to encourage self-regulating functions to operate more efficiently.
Examples of combination (including OMT) treatment approaches
Asthma
Studies have demonstrated that soft tissue manipulation (deep massage-type and stretching techniques) can improve movement of the chest, increase airflow, and generally ease the symptoms of chronic asthma (Bockenhauer et al 2002).
Chronic fatigue syndrome (CFS)
Perrin (1998, 2007) has researched a general osteopathic approach (details in bullet points below) to CFS. A clinical trial assessed 58 people with confirmed CFS. They were divided into two groups – a patient group (n = 34) and a control group (n = 24). Only those in the patient group were treated manually (see below), while the control group did not receive any manual treatment. Treatment was offered over a period of 12 months, with regular assessment – both objective (mobility of thorax, for example), and subjective, based on symptom questionnaires. The treatment group showed an overall improvement of 40% (p < 0.0005) as against a 1% worsening of symptoms for the control group.
Manual and complementary methods used:
• Effleurage techniques directed toward the subclavian region, aiding drainage of the cervical and thoracic lymphatics and resulting in increased central drainage of the lymph into the subclavian veins to reverse backflow
• Long- and short-lever mobilization methods to achieve gentle articulation of the thoracic and upper lumbar spine as well as the ribs
• Soft-tissue massage of the levator scapulae, paravertebral muscles, respiratory muscles, rhomboids, and trapezii
• High- and low-velocity manipulation of the thoracic and upper lumbar spinal segments with combined supine and side-lying leverage and thrust techniques
• Functional positional release techniques to the suboccipital region and the sacrum
• Stimulation of the cranial rhythmic impulse (CRI) by compression of the fourth ventricle
• Contrast bathing (warm and cold compresses) applied to tender areas of the back
• In addition, patient self-care was recommended in the form of prescribed exercises designed to improve mobility in the thoracic spine.
Chronic pelvic pain (CPP)
Non-malignant pain perceived in structures related to the pelvis of either men or women. In the case of documented nociceptive pain that becomes chronic, pain must have been continuous or recurrent for at least 6 months. In all cases, there often are associated negative cognitive, behavioural, sexual and emotional consequences.
In 2009, the Urological Pelvic Pain Collaborative Research Network (UPPCRN) concluded that somatic abnormalities, including myofascial trigger points and connective tissue restrictions, were common in women and men with chronic pelvic pain syndrome (CPP). (Fitzgerald et al 2009).
UPPCRN published the outcomes of a feasibility trial comparing connective tissue manipulation (CTM) and myofascial physical therapy, versus global therapeutic massage in patients with CPP. The group receiving skilled CTM and myofascial therapy had a significantly higher response rate than the group receiving massage (Fitzgerald et al 2009). Fitzgerald et al report that CTM was applied to the abdominal wall, back, buttocks and thighs that had been identified as containing connective tissue abnormalities, and/or painful myofascial trigger points. With the patient prone, treatment was applied bilaterally, from the 10th thoracic level, down to the popliteal crease, until a texture change was noted in the treated tissue layer. Additional manual techniques such as trigger point barrier release, with or without active contraction or reciprocal inhibition, manual stretching of the trigger point region, and myofascial release, were also used to deactivate the identified trigger points.
Following treatment in the prone position, patients were treated supine so that CTM could be applied to the thighs – laterally, anteriorly and medially, from the knee up to and including the thigh crease. CTM was additionally performed on the abdominal wall – from the suprapubic rim to the anterior costal cartilages, with focus on the periumbilical tissues.
Manual trigger point release techniques were used to treat any trigger points or scars identified in these regions, with an emphasis on external episiotomy scars located in the perineum or external pelvic floor. (See below for further discussion of scar implications.)
Transvaginal/transrectal treatment of the soft tissues of the pelvic floor with CTM of periurethral tissues, arcus tendineus fascia pelvis, and muscle origins and insertions was also performed. Myofascial manipulation to each muscle group was performed with the focus on restrictive bands and trigger points. Neuromuscular reeducation, focusing on lengthening the pelvic floor musculature, was performed in conjunction with myofascial manipulation, including post-isometric relaxation (muscle energy technique – MET).
Scar tissue
Scar tissue has been identified as a source of pain, in general, and in chronic pelvic pain, in particular (Fitzgerald et al 2009). For example, this has been found in women with CPP who have previously undergone laparoscopic investigation. The trochar (a surgical instrument) may have been used through the umbilicus, in the suprapubic region, or other lower abdominal sites. Subsequent formation of scar tissue has been shown to be capable of creating restriction of the ilioinguinal, iliohypogastric and genitofemoral nerves (Howard 2000). Peri-umbilical and suprapubic subcutaneous panniculosis secondary to surgical incisions have been associated with urinary urgency, frequency, and dysuria (Fitzgerald & Kotarinos 2003).
Valouchova & Lewit (2009) report that active scars in the abdomen and pelvis commonly restrict back flexion, which the patient feels as low back pain. Treatment methods are simple, involving ‘mini-myofascial release’ methods – where skin alongside scars is treated initially, with subsequent attention to deeper layers. Treatment involves ‘engaging the pathologic barrier and waiting; after a short delay, a release gradually occurs until the normal barrier is restored.’
Irritable bowel syndrome (IBS)
A French study involving over 100 patients has shown that attention to the internal pelvic muscles, specifically levator ani and coccygeus, as well as pelvic mobilization, can assist in normalizing many cases of irritable bowel syndrome (Riot et al 2004). One hundred and one patients (76 females and 25 males; mean age 54 years) with a diagnosis of levator ani syndrome (LVAS) were studied for 1 year. Internal massage was given with the patient lying on the left side. Physical treatment of associated pelvic joint disorders was given at the end of each massage session. Results: 47 patients (46.5%) suffered from both LVAS and IBS. A mean of less than two sessions of treatment was necessary. At 6 months follow-up, 69% of the patients were LVAS-free (p < 0.0001) and 10% were improved. At 12 months, 62% were still free of symptoms and 10% improved (p = 0.37). A comparable trend was found in the IBS group: 53% IBS-free initially, 78% at 6 months (p = 0.00001) and 72% at 12 months (p = 1). The results suggest a muscular and osteoligamentary etiology in LVAS.
Pancreatitis
Radjieski et al (1998) randomly assigned six patients with pancreatitis to receive standard medical care plus daily OMT (comprising myofascial release, soft tissue massage, and strain/counterstrain techniques) for the duration of their hospitalization, or to receive only standard medical care (eight patients). Osteopathic treatment involved 10–20 minutes daily of a standardized protocol, with attending physicians blinded as to group assignment. Results indicated that patients who received osteopathic attention averaged significantly fewer days in the hospital before discharge (mean reduction 3.5 days) than control subjects, although there were no significant differences in time to food intake or in use of pain medications.
Pneumonia
Noll and colleagues (2000) conducted a randomly controlled study involving elderly patients hospitalized with acute pneumonia. Patients were recruited and randomly placed into two groups: 28 in the treatment group and 30 in the control group. The treatment group received a standardized osteopathic attention protocol (including SCS and functional positional release methods), while the control group received a light touch (dummy) protocol. There was no statistical difference between groups for age, gender or simplified acute physiology scores. The treatment group had reduction in the length of hospital stay, from a mean of 8.6 days without OMT, to 6.6 days with OMT. Additional benefits for those receiving OMT included reduced length of use of intravenous antibiotics.
Post-surgical recovery and reduced trauma effects
O-Yurvati et al (2005) documented the physiological effects of postoperative OMT – mainly functional positional release of traumatized thoracic tissues – following a coronary artery bypass graft (CABG) – to determine the effects on cardiac hemodynamics. Ten subjects undergoing CABG surgery were recruited for postoperative OMT. The primary assessment compared pre-OMT versus post-OMT measurements of thoracic impedance, mixed venous oxygen saturation and cardiac index. Immediately following CABG surgery, OMT was provided to alleviate anatomic dysfunction of the rib cage caused by median sternotomy and to improve respiratory function. This adjunctive treatment occurred while subjects were completely anesthetized. Results suggested improved peripheral circulation and increased mixed venous oxygen saturation after OMT. These increases were accompanied by an improvement in cardiac index (p ≤ 0.01). The authors conclude that OMT has immediate, beneficial hemodynamic effects after CABG surgery when administered while the patient is sedated and pharmacologically paralyzed.
Prostatitis
A study at Stanford University Medical School has shown that pelvic pain associated with chronic prostatitis involving non-bacterial urinary difficulties, accompanied by chronic pelvic pain, can be effectively treated using trigger point deactivation [described as myofascial trigger point release technique –MFRT] together with relaxation therapy (Anderson et al 2005). The researchers point out that 95% of chronic cases of prostatitis are unrelated to bacterial infection, and that myofascial trigger points, associated with abnormal muscular tension in key muscles, are commonly responsible for the symptoms. The 1- month study involved 138 men, and the results produced marked improvement in 72% of the cases, with 69% showing significant pain reduction and 80% improvement in urinary symptoms. The study noted that TrPs in the anterior levator ani muscle often refer pain to the tip of the penis. The levator endopelvic fascia lateral to the prostate represents the most common location of TrPs in men with pelvic pain. Myofascial TrPs were identified and pressure was held for about 60 seconds to release. Specific techniques used in conjunction with MFRT were voluntary contraction and release/hold relax/contract–relax/reciprocal inhibition (i.e. MET), and deep tissue mobilization, including stripping, strumming, skin rolling and effleurage (i.e. NMT).
These examples suggest that broadly applied soft tissue and joint mobilizing approaches that encourage better breathing, as well as improved circulation and drainage, can assist the healing and self-regulating processes of even severely ill individuals.
Note: For obvious reasons, none of these methods should be used without the approval of the attending physician, and of the individual being treated.
This chapter serves to point out the need for a well-honed ability to perform manual treatment and a constant vigilance in the area of clinical reasoning. The remaining chapters of this book assist the practitioner in developing manual skills, as well as the ability to decipher when and where to apply the techniques.
Anderson R., Wise D., Sawyer T., et al. Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men. J Urol. 2005;174(1):155-160.
Barbieri A., Vanhaecht K., Van Herck P. Effects of clinical pathways in the joint replacement: a meta-analysis. BMC Med. 2009;7:32.
Bennett R.M. Fibromyalgia: patient perspectives on symptoms, symptom management, and provider utilization. Curr Rheumatol Rep. 2002;4(4):286-292.
Ballantyne F., et al. Effect of MET on hamstring extensibility: the mechanism of altered flexibility. Journal of Osteopathic Medicine. 2003;6(2):59-63.
Bockenhauer S., Julliard K., Lo K., et al. Quantifiable effects of osteopathic manipulative techniques on patients with chronic asthma. J Am Osteopath Assoc. 2002;102(7):371-375.
Bullock-Saxton J. The palpation reliability debate: the experts opinions. Journal of Bodywork and Movement Therapies. 2002;6(1):19-21.
Chaitow L. Clinical Prediction Rules. Editorial JBMT. 2010;14(3):207-208.
Chaitow L., DeLany J. Clinical application of neuromuscular techniques: Case study exercises. Edinburgh: Churchill Livingstone; 2005.
Chaitow L, Lovegrove R, editors: Physical Therapy approaches to Chronic Pelvic Pain and Dysfunction, Edinburgh, Churchill Livingstone, In press
Cook C. Potential pitfalls of clinical prediction rules. Journal of Manual & Manipulative Therapy. 2008;16(2):69.
Crown L., Hizon J., Rodney W. Musculoskeletal injuries in sports: the team physician’s handbook. St Louis: Mosby, 1997;361-370.
Dommerholt J. Differential diagnosis: myofascial pain syndrome. In: Chaitow L., editor. Fibromyalgia syndrome: a practitioner’s guide. Edinburgh: Elsevier, 2009.
Eddy D.M. Screening for colorectal cancer. Ann Intern Med. 1991;113(5):373-384.
Falk G., Fahey T. 2009 Clinical prediction rules. Br Med J. 2009;339:b2899.
Fall M., Baranowski A., Elneil S., et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2010;57(1):35-48.
Fitzgerald M.P., Kotarinos R. Rehabilitation of the short pelvic floor part 1 and 2. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(4):269-275.
Fitzgerald M.P., Anderson R., Potts J., et al. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J Urol. 2009;182(2):570-580.
Fritz J.M. Clinical prediction rules in physical therapy: coming of age? JOSPT. 2009;39(3):159.
Fritz J.M., Delitto A., Erhard R. Comparison of a classification-based approach to physical therapy and therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003;28:1363-1372.
Hall H., McIntosh G., Boyle C. Effectiveness of a low back pain classification system. Spine J. 2009;9:648-657.
Guyatt G.H. Evidence-based medicine. Ann Intern Med. 1991;114(Suppl 2):A-16.
Guyatt G., Cairns J., Churchill D., et al. Evidence-Based Medicine Working Group. Evidence-based medicine: A new approach to teaching the practice of medicine. JAMA. 1992;268:2420-2425.
Guyatt G., Cook D., Haynes B. Evidence based medicine has come a long way. BMJ. 2004;329:990-991.
Higgs J. The complexity of clinical reasoning: exploring the dimensions of clinical reasoning expertise as a situated, lived phenomenon. Australia: University of Sydney, 2006. Seminar presentation at the Faculty of Health Sciences, 5 May
Higgs J., Jones M., Loftus S., et al. Clinical reasoning in the health professions, ed 3. Amsterdam: Butterworth Heinemann Elsevier, 2008.
Howard F. Diagnosis and management of pelvic pain. Williams & Wilkins: Philadelphia. Lippincott, 2000.
Hsieh C.Y.J., Hong C.Z., Adams A.H., et al. Inter-examiner reliability of the palpation of trigger points in the trunk and lower limb muscles. Arch Phys Med Rehabil. 2000;81:258-264.
Hunter B., Segrott J. Re-mapping client journeys and professional identities: a review of the literature on clinical pathways. Int J Nurs Stud. 2006;45:608-625.
Jaeschke R., Guyatt G.H., Sackett D.L. User’s guides to the medical literature – what are the results and will they help me in caring for my patients. JAMA. 1994;271:703-707.
Jones M.A. Clinical reasoning process in manipulative therapy. In: Boyling J.D., Palastanga N., editors. Grieve’s modern manual therapy. Edinburgh: Churchill Livingstone; 1994:471-482.
Lee D., Lee L.J. Differential diagnosis and management of chronic pelvic pain. Chaitow L., Lee D., editors, The palpation reliability debate: the experts opinions. Journal of Bodywork and Movement Therapies. 2002;6;(1):26-27.
Lee D., Lee L.J. Chaitow L., Lovegrove R., editors. Chronic pelvic pain and dysfunction. Edinburgh: Elsevier, 2011. in press
Lenehan K.L., Fryer G., McLaughlin P. The effect of muscle energy technique on gross trunk range of motion. Journal of Osteopathic Medicine. 2003;6(1):13-18.
Linton S. Review of psychological risk factors in back and neck pain. Spine. 2000;25:1148-1156.
Materson R.S., Dommerholt J. Industrial, spine, and related rehabilitation. In: Melvin J.L., Odderson I., editors. R Physical medicine and rehabilitation clinics of North America. Philadelphia: W B Saunders; 1996:107-123.
May S., Chance-Larsen K., Littlewood C., et al. Reliability of physical examination tests used in the assessment of patients with shoulder problems: a systematic review. Physiotherapy. 2010;96:179-190.
Noll D., Shores J., Gamber R., et al. Benefits of osteopathic manipulative treatment for hospitalized elderly patients with pneumonia. J Am Osteopath Assoc. 2000;100(12):776-782.
O-Yurvati A., Carnes M., Clearfield M., et al. Hemodynamic effects of osteopathic manipulative treatment immediately after coronary artery bypass graft surgery. J Am Osteopath Assoc. 2005;105(10):475-481.
Paatelma M., Karvqnen E., Heinqnen A. inter-tester reliability in classifying acute and subacute low back pain patients into clinical subgroups: a comparison of specialists and non-specialists. Journal of Manual & Manipulative Therapy. 2009;17(4):221-229.
Perrin R. Lymphatic drainage of the neuraxis in chronic fatigue syndrome: a hypothetical model for the cranial rhythmic impulse. J Am Osteopath Assoc. 2007;107(6):218-224.
Perrin R., Edwards J., Hartley P. Evaluation of the effectiveness of osteopathic treatment on symptoms associated with myalgic encephalomyelitis [CFS]. A preliminary report. J Med Eng Technol. 1998;22(1):1-13.
Radjieski J., Lumley M., Cantieri M. Effect of osteopathic manipulative treatment on length of stay for pancreatitis: a randomized pilot study. J Am Osteopath Assoc. 1998;98(5):264-272.
Riot F., Goudet P., Mouraux J.P., et al. Levator ani syndrome, functional intestinal disorders and articular abnormalities of the pelvis: the place of osteopathic treatment. Presse Med. 2004;33(13):852-857.
Sackett D.L., Straus S., Richardson W.S., et al. Evidence-based medicine. How to practice and teach EBM. New York: Elsevier Science, 2000.
Seffinger M.A., Najm W.I., Mishra S.I., et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29:E413-E425.
Valouchová P., Lewit K. Surface electromyography of abdominal and back muscles in patients with active scars. Journal of Bodywork and Movement Therapies. 2009;13:262-267.
Vlaeyen J.W., Linton S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317-332.
Wilson E., Payton O., Donegan-Shoaf L., et al. Muscle energy technique in patients with acute low back pain: a pilot clinical trial. J Orthop Sports Phys Ther. 2003;33:502-512.
Zander K. Integrated care pathways: eleven international trends. Journal of Integrated Care Pathways. 2002;6:101-107.