Chapter 9 Summary of selected NMT associated modalities
NMT evolved over many decades out of the work of a number of clinicians working in Europe and the USA. The ‘evolutionary’ development of NMT produced some confusion regarding the name itself. In its earlier stages, American ‘NMT’ represented neuromuscular ‘therapy’ whereas, in Europe, the preferred term had been neuromuscular ‘technique’. In the past decade, as a number of methods emerged, practitioners began to use these two terms interchangeably. Distinctions between the various NMT methods still exist, although there is less separation in regards to the use of the terms ‘therapy’ and ‘technique’, apart from osteopathic training in the UK, where the ‘T’ element of NMT clearly refers to ‘technique’.
A key difference between neuromuscular therapies (see page 192) – which this book describes – and neuromuscular technique (i.e. Lief’s or European NMT – see Box 9.3) is that the former incorporates under its’ definition, a host of complementary physical modalities – including Lief’s NMT. This chapter describes the range of physical modalities. It is worth noting that not all of these are ‘manual’, as they include hydrotherapy and, potentially, acupuncture and dry needling.
Box 9.3 European (Lief’s) neuromuscular technique (Chaitow 2010)
European-style NMT first emerged between the mid-1930s and early 1940. The basic techniques as developed by Stanley Lief and Boris Chaitow are described within this text but there exist many variations, the use of which will depend upon particular presenting factors or personal preference. European NMT’s history is discussed more fully in Volume 1, Chapter 9.
European NMT thumb technique
Thumb technique as employed in both assessment and treatment modes of European NMT enables a wide variety of therapeutic effects to be produced. A light, non-oily lubricant is usually used to facilitate easy, non-dragging passage of the palpating digit, unless dry skin contact is needed (such as in texture or thermal assessment).
• The tip of the thumb can deliver varying degrees of pressure by using:
• In thumb technique application, the hand is spread for balance and control with the palm arched and with the tips of the fingers providing a fulcrum, the whole hand thereby resembling a ‘bridge’ (Fig. 9.2). The thumb freely passes under the bridge toward one of the finger tips.
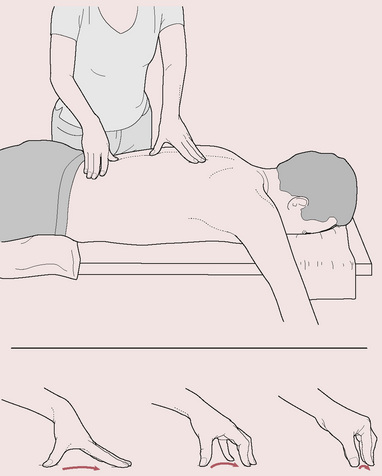
Figure 9.2 NMT thumb technique: note static fingers provide fulcrum for moving thumb
(reproduced with permission from Chaitow & DeLany 2008).
• During a single stroke, which covers between 2 and 3 inches (5–8 cm), the finger tips act as a point of balance while the chief force is imparted to the thumb tip. Controlled application of body weight through the long axis of the extended arm focuses force through the thumb, with thumb and hand seldom imparting their own muscular force except when addressing small localized contractures or fibrotic ‘nodules’.
• The thumb, therefore, never leads the hand but always trails behind the stable fingers, the tips of which rest just beyond the end of the stroke.
• The hand and arm remain still as the thumb moves through the tissues being assessed or treated.
• The extreme versatility of the thumb enables it to modify the direction and degree of imparted force in accordance with the indications of the tissue being tested/treated. The practitioner’s sensory input through the thumb can be augmented with closed eyes so that every change in the tissue texture or tone can be noticed.
• The weight being imparted should travel in as straight a line as possible directly to its target, with no flexion of the elbow or the wrist by more than a few degrees.
• The practitioner’s body is positioned to achieve economy of effort and comfort. The optimum height of the table and the most effective angle of approach to the body areas being addressed should be considered (see Volume 1, Fig. 9.10)
• The nature of the tissue being treated will determine the degree of pressure imparted, with changes in pressure being possible, and indeed desirable, during strokes across and through the tissues. When being treated, a general degree of discomfort for the patient is usually acceptable but he should not feel pain.
• A stroke or glide of 2–3 inches (5–8 cm) will usually take 4–5 seconds, seldom more unless a particularly obstructive indurated area is being addressed. In normal diagnostic and therapeutic use the thumb continues to move as it probes, decongests and generally treats the tissues. If a myofascial trigger point is being treated, more time may be required at a single site for application of static or intermittent pressure.
• Since assessment mode attempts to precisely meet and match the tissue resistance, the pressure used varies constantly in response to what is being palpated.
• A greater degree of pressure is used in treatment mode and this will vary depending upon the objective, whether to inhibit neural activity or circulation, to produce localized stretching, to decongest and so on (see Volume 1, Box 9.4).
European NMT finger technique
In certain areas the thumb’s width prevents the degree of tissue penetration suitable for successful assessment and/or treatment. Where this happens a finger can usually be suitably employed. Examples include intercostal regions and curved areas, such as the area above and below the pelvic crest or the lateral thigh.
• The middle or index finger should be slightly flexed and, depending upon the direction of the stroke and density of the tissues, should be supported by one of its adjacent members.
• The angle of pressure to the skin surface should be between 40° and 50°. A firm contact and a minimum of lubricant are used as the treating finger strokes to create a tensile strain between its tip and the tissue underlying it. The tissues are stretched and lifted by the passage of the finger which, like the thumb, should continue moving unless, or until, dense indurated tissue prevents its easy passage.
• The finger tip should never lead the stroke but should always follow the wrist, as the hand is drawn toward the practitioner, so that the entire hand moves with the stroke and elbow flexion occurs as necessary to complete the stroke. The strokes can be repeated once or twice as tissue changes dictate (see Volume 1, Box 14.8).
• The patient’s reactions must be taken into account when deciding the degree of force to be used.
• Transient pain or mild discomfort is to be expected. Most sensitive areas are indicative of some degree of associated dysfunction, local or reflexive, and their presence should be recorded.
• If tissue resistance is significant, the treating finger should be supported by another finger.
Variations
Depending upon the presenting symptoms and the area involved, other applications may be performed as the hand moves from one site to another. There may be:
• superficial stroking in the direction of lymphatic flow
• direct pressure along or across the line of axis of stress fibers
• deeper alternating ‘make and break’ stretching and pressure or traction on fascial tissue
• sustained or intermittent ischemic (‘inhibitory’) pressure, applied for specific effects.
A constantly fluctuating stream of information regarding the status of the tissues will be discernible from which variations in pressure and the direction of force are determined. The amount of pressure required to ‘meet and match’ tense, edematous, fibrotic or flaccid tissue will be varied. During assessment, if a ‘hard’ or tense area is sensed, pressure should actually lighten rather than increase, since to increase pressure would override the tension in the tissues, which is not the objective in assessment.
In evaluating for myofascial trigger points, when a sense of something ‘tight’ is noted just ahead of the contact digit as it strokes through the tissues, pressure lightens and the thumb/finger slides over the ‘tight’ area. Deeper penetration senses for the characteristic taut band and the trigger point, at which time the patient is asked whether it hurts and whether there is any radiating or referred pain. Should a trigger point be located, as indicated by the reproduction in a target area of a familiar pain pattern, then a number of choices are possible. Each of the following is discussed in this chapter or in Volume 1.
• The point should be marked and noted (on a chart and if necessary on the body with a skin pencil).
• Sustained ischemic/inhibitory pressure can be used.
• A positional release (PR) approach can be used to reduce activity in the hyperreactive tissue.
• Initiation of an isometric contraction followed by stretch (MET) could be applied.
• A combination of pressure, PRT and MET (integrated neuromuscular inhibition technique – INIT) can be introduced.
• Spray-and-stretch methods can be used.
• An acupuncture needle or a procaine injection can be used if the practitioner is duly licensed and trained.
Whichever approach is used a trigger point will only be effectively deactivated if the muscle in which it lies is restored to its normal resting length. Stretching methods such as MET can assist in achieving this.
Areas of dysfunction should be recorded on a case card, together with all relevant material and additional diagnostic findings, such as active or latent trigger points (and their reference zones), areas of sensitivity, hypertonicity, restricted motion and so on. Out of such a picture, superimposed on an assessment of whole-body features such as posture, as well as the patient’s symptom picture and general health status, a therapeutic plan should emerge.
It is a characteristic of neuromuscular therapy/technique (NMT) – of either tradition – to move from the gathering of information into treatment, almost seamlessly. As the practitioner searches for information, the appropriate modification of degree of pressure from the contact digit or hand can turn ‘finding’ into ‘fixing’, or at least having an intent to ‘fix’ what is not working optimally. One modality accompanies another as a rather ‘custom-made’ application is created that not only varies from patient to patient, but should also vary from one session to the next for a particular individual, as the condition changes.
These concepts will become clearer as the methods and objectives of NMT and its associated modalities become more familiar. This chapter reviews the modalities and choices discussed in Volume 1 and assists in determining which modalities are best suited for particular conditions. After consideration of the current status of the dysfunction (acute, subacute, chronic, inflamed, etc.) the determining factor of which method to employ is frequently reduced to which method(s) the practitioner has mastered and feels confident to use. One technique may ‘work’ as well as another, so long as it is appropriate for the conditions being addressed.
The global view
In this text, we have considered a number of features that are all commonly involved in causing or intensifying pain (Chaitow 2010). While it is simplistic to isolate factors that affect the body – globally or locally – it is also necessary at times to do this. We have presented models of interacting adaptations to stress, resulting from postural, emotional, respiratory and other factors, which have fundamental influences on health and ill health.
One such model suggests consideration of three categories under which most causes of disease, pain and the perpetuation of dysfunction can be broadly clustered:
• biomechanical (postural dysfunction, upper chest breathing patterns, hypertonicity, neural compression, trigger point activity, etc.)
• biochemical (nutrition, ischemia, inflammation, hormonal, hydration, hyperventilation effects)
• psychosocial (stress, anxiety, depression, hyperventilation tendencies).
NMT attempts to identify these altered states, insofar as they impact on the person’s condition. The practitioner can then either offer appropriate therapeutic interventions which reduce the adaptive ‘load’ and/or assist the self-regulatory functions of the body (homeostasis). When this is inappropriate or outside the practitioner’s scope of practice, she should offer referral to appropriate health-care professionals who can support that area of the patient’s recovery process.
While these health factors have tremendous potential to interface with one another, each may at times also be considered individually. It is important to address whichever of these influences on musculoskeletal pain can be identified in order to remove or modify as many etiological and perpetuating influences as possible (Simons et al 1999); however, it is crucial to do so without creating further distress or requirement for excessive adaptation. When appropriate therapeutic interventions are used, the body’s adaptation response produces beneficial outcomes. When excessive or inappropriate interventions are applied, the additional adaptive load inevitably leads to a worsening of the patient’s condition. Treatment is a form of stress and can have a beneficial or a harmful outcome depending on its degree of appropriateness. When patients report post-treatment symptoms of headache, nausea, achiness or fatigue, they are often told it is a ‘healing crisis’. Whether ‘healing’ or not, it is a ‘crisis’ all the same and often avoidable if basic measures are taken to reduce excessive adaptation responses to treatment by managing the amount and type of treatment offered.
Selecting an adequate degree of therapeutic intervention in order to catalyze a change, without overloading the adaptive mechanisms, is something of an art form. When analytical clinical skills are weak or details of techniques unclear, results may be unpredictable and unsatisfactory (DeLany 1999). Whereas, when such skills are effectively utilized and intervention methodically applied involving a manageable load, the outcome is more likely to be a sequential recovery and improvement.
In Volume 1, we noted: ‘The influences of a biomechanical, biochemical and psychosocial nature do not produce single changes. Their interaction with each other is profound’. This axiom is also true in reverse. When therapeutic modification of the influences of these factors is applied, with the objective of restoring health by removing negative influences, balancing the biochemistry and/or supporting the emotional components of wellness, the effects seldom produce single changes. Remarkable improvements can occur, sometimes rapidly. In some instances, intervention can be applied to more than one sphere of influence if homeostatic functions can efficiently handle the adaptive burden. This ‘lightening of the load’ has significant effects on the perception of pain, its intensity and the maintenance of dysfunctional states.
• Hyperventilation modifies blood acidity, alters neural reporting (initially hyper and then hypo), creates feelings of anxiety and apprehension and directly impacts on the structural components of the thoracic and cervical region, both muscles and joints (Gilbert 1998). If better breathing mechanics can be restored by addressing the musculature that controls inhalation and exhalation, emotional stability (regarding grief, fear, anxiety, etc.) may be enhanced and better breathing techniques employed, so that all that depends upon the breath (and what does not?) has potential for (often significant) improvement.
• Altered chemistry (hypoglycemia, alkalosis, etc.) affects mood directly while altered mood (depression, anxiety) changes blood chemistry, as well as altering muscle tone and, by implication, trigger point evolution (Pryor & Prasad 2002, Brostoff 1992). Therefore, addressing dietary intake, digestion and/or assimilation could result in significant changes in soft tissue conditions as well as psychological well-being, which may influence postural function.
• Altered structure (posture, for example) modifies function (breathing, for example) and therefore impacts on blood biochemistry (e.g. O2: CO2 balance, circulatory efficiency and delivery of nutrients, etc.), which impacts on mood (Foster et al, 2001). Stretching protocols, soft tissue or skeletal manipulations and ergonomically sound changes in patterns of use, all serve to restore structural alignment, which positively influences all other bodily functions.
It is most important not to offer too much too soon. Take, for example, a first treatment session, which is largely taken up with a variety of tests and assessments. This might theoretically lead not only to an introduction to bodywork and/or movement therapy, but also to suggestions for the patient to change what he is eating, how he is sitting, how much or little he is exercising, to drink more water, cut out caffeine, increase dietary fiber, avoid junk foods, take more supplements, stretch his muscles, arrange his schedule around frequent therapy sessions and, in general, to adopt a new lifestyle altogether. It is probable that the patient will not be seen again. This much change – too much, too fast, too soon – is likely to prove overwhelming to the body and to the person who lives in that body. A priority-based plan, with modifications for special needs or challenges, with step-by-step additions that would eventually impact as many influences as possible, may result in a long-term commitment to lifestyle changes. Above all, the patient needs to have a clear understanding of why each change is suggested and how it is likely to either reduce the adaptive burden he is carrying (the analogy of a tightly stretched piece of elastic may help) or how it might improve his ability to handle the adaptive load through improved function.
A home care program can be designed appropriate to the needs and current status of the patient, for both physical relief of the tissues (stretching, self-help methods, hydrotherapies see Chapter 7) and awareness of perpetuating factors (postural habits, work and recreational practices, nutritional choices, stress management). Lifestyle changes are essential if influences resulting from habits and potentially harmful choices made in the past are to be reduced (see notes on concordance in Volume 1, Chapter 8)
The purpose of this chapter
The remainder of this chapter discusses some of the neuromuscular techniques that have proven successful for altering the elements of chronic pain and musculo-skeletal dysfunction. A thorough understanding of the underlying principles will support the practitioner in making appropriate therapeutic choices for the patient. The reader is encouraged to explore the more expansive discussions of these modalities found in Volume 1.
The remaining chapters of this text are dedicated to understanding regional anatomy and the application of assessment protocols and treatment modalities as applied to individual muscles and their associated structures. When foundational understanding of the protocols is clear and the regional anatomy is understood, the practitioner can ‘custom design’ what is needed for that patient’s body at each session by selecting from the variety of techniques discussed.
The treatment methods offered in the techniques portion of this text are NMT (both American version ™and European style), muscle energy techniques (MET), positional release techniques (PRT), myofascial release (MFR) and a variety of modifications and variations of these and other supporting modalities that can be usefully interchanged, and/or combined. This is not meant to suggest that methods not discussed in this text (for example, high-velocity thrust methods and joint mobilization), which to an extent address soft tissue dysfunction, are less effective or inappropriate. It does, however, mean that the methods described throughout the clinical applications section are known to be helpful as a result of our clinical experience. Traditional massage methods are also frequently mentioned (see Box 9.1), as are applications of lymphatic drainage techniques (see Box 9.2). All these methods require appropriate training and any descriptions offered in this chapter are not meant to replace that requirement.
Box 9.1 Traditional massage techniques
A variety of massage applications can be employed in neuromuscular techniques, many of which have been included in the protocols of this text. Among many variations, the primary massage techniques are as follows.
• Effleurage: a gliding stroke used to induce relaxation and reduce fluid congestion by encouraging venous or lymphatic fluid movement toward the center. Lubricants are usually used.
• Petrissage: a wringing and stretching movement that attempts to ‘milk’ the tissues of waste products and assist in circulatory interchange. The manipulations press and roll the muscles under the hands.
• Kneading: a compressive stroke that alternately squeezes and lifts the tissues to improve fluid exchange and achieve relaxation of tissues.
• Inhibition: application of pressure directly to the belly or attachments of contracted muscles or to local soft tissue dysfunction for a variable amount of time or in a ‘make-and-break’ (pressure applied and then released) manner, to reduce hypertonic contraction or for reflexive effects. Also known as ischemic compression or trigger point pressure release.
• Vibration and friction: small circular or vibratory movements, with the tips of fingers or thumb, particularly used near origins and insertions and near bony attachments to induce a relaxing effect or to produce heat in the tissue, thereby altering the gel state of the ground substance. Vibration can also be achieved with mechanical devices with varying oscillation rates that may affect the tissue differently.
• Transverse friction: a short pressure stroke applied slowly and rhythmically along or across the belly of muscles using the heel of the hand, thumb or fingers.
Massage effects explained
A combination of physical effects occur, apart from the undoubted anxiety-reducing influences (Sandler 1983), which involve a number of biochemical changes.
• Plasma cortisol and catecholamine concentrations alter markedly as anxiety levels drop and depression is also reduced (Field 1992).
• Serotonin levels rise as sleep is enhanced, even in severely ill patients – preterm infants, cancer patients and people with irritable bowel problems as well as HIV-positive individuals (Acolet 1993, Ferel-Torey 1993, Ironson 1993, Weinrich & Weinrich 1990).
• Pressure strokes tend to displace fluid content, encouraging venous, lymphatic and tissue drainage.
• Increase of fresh oxygenated blood flow aids normalization via increased capillary filtration and venous capillary pressure.
• Edema is reduced, as are the effects of pain-inducing substances that may be present (Hovind 1974, Xujian 1990).
• Decreases the sensitivity of the gamma-efferent control of the muscle spindles and thereby reduces any shortening tendency of the muscles (Puustjarvi 1990).
• Provokes a transition in the ground substance of fascia (the colloidal matrix) from gel to sol, which increases internal hydration and assists in the removal of toxins from the tissue (Oschman 1997).
• Pressure techniques can have a direct effect on the Golgi tendon organs, which detect the load applied to the tendon or muscle.
A more in-depth discussion of massage techniques is found in Volume 1.
Box 9.2 Lymphatic drainage techniques
Lymphatic drainage, which can be assisted by coordination with the patient’s breathing cycle, enhances fluid movement into the treated tissue, improving oxygenation and the supply of nutrients to the area. Practitioners trained in advanced lymph drainage can learn to accurately follow (and augment) the specific rhythm of lymphatic flow (Chikly 1999). With sound anatomical knowledge, specific directions of drainage can be plotted, usually toward the node group responsible for evacuation of a particular area (lymphotome). Hand pressure used in lymph drainage should be very light indeed, less than an ounce (28 g) per cm2 (under 8 oz per square inch), in order to encourage lymph flow without increasing blood filtration (Chikly 1999).
Stimulation of lymphangions leads to reflexively induced peristaltic waves of contraction along the lymphatic vessel, enhancing lymphatic movement. A similar peristalsis may be activated manually by stimulation of external stretch receptors of the lymph vessels. Lymph movement is also augmented by respiration as movements of the diaphragm ‘pump’ the lymphatic fluids through the thoracic duct. Deep-pressure gliding techniques, however, which create a shearing force, can lead to temporary inhibition of lymph flow.
The lymphatic pathways have been illustrated in each regional overview of this text. Practitioners trained in lymphatic drainage are reminded by these illustrations to apply lymphatic drainage techniques before NMT procedures to prepare the tissues for treatment and after NMT to remove excessive waste released by the procedures. Practitioners who are not trained in lymphatic techniques may (with consideration of the precautions and contraindications noted in Volume 1) apply very light effleurage strokes along the lymphatic pathways before and after NMT techniques so long as basic lymph drainage guidelines are followed (see Volume 1).
There are also excellent alternative stretching methods available and both authors utilize a range of stretching variations in practice. However, in the clinical applications sections of the book, where particular areas and muscles are being addressed, with NMT protocols being described, sometimes with both a European and an American version being offered, as well as MET, MFR and PRT additions and alternatives, it was considered impractical to include the many variations available.
The methods of stretching described in this text are largely based on osteopathic MET methodology, and carry the endorsement of David Simons (Simons et al 1999) as well as some of the leading experts in rehabilitation medicine (Lewit 1999, Liebenson 2007). Some stretching approaches are described in Chapter 7 with self-help strategies.
The remainder of this chapter briefly reviews these primary and supporting modalities. It is strongly suggested that the reader also review Volume 1, Chapters 9 and 10, for more in-depth discussions of these methods and modalities.
General application of neuromuscular techniques
The following suggestions concern the application of most of the manual techniques taught in this text. While there are techniques whose application may be the exception to these ‘rules’, understanding the foundational elements of the technique, as well as the stage of healing the tissue is in, will be critical to knowing if it can be safely used at that time.
Following trauma, the involved myofibers undergo four interrelated, time dependent phases: degeneration, inflammation, regeneration, and fibrosis (Gates & Huard 2005). See Figure 9.1.
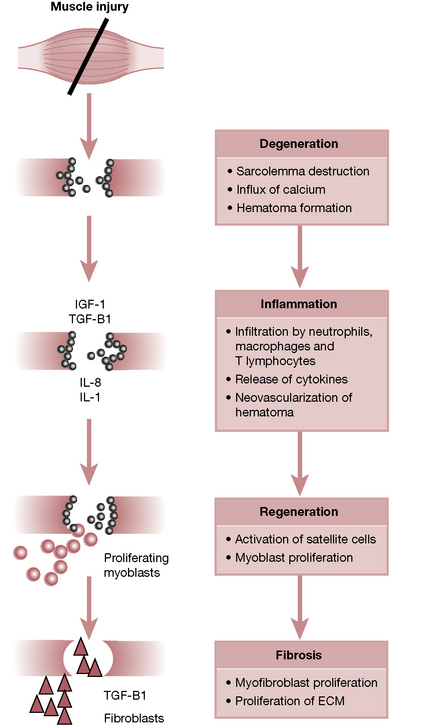
Figure 9.1 Phases of muscle healing after injury.
From Gates C Huard J 2005 Management of Skeletal Muscle Injuries in Military Personnel. Oper Tech Sports Med 13: Fig 1, p. 248.
Since NMT techniques tend to increase blood flow and reduce spasms, most are contraindicated in the initial stages of acute injury (72–96 hours post trauma) when a natural inflammatory process commences and blood flow and swelling should be reduced, rather than stimulated. Connective tissues damaged by the trauma therefore need time to repair, and the recovery process often results in splinting and swelling (Cailliet 1996).
Rest, ice, compression and elevation (RICE) are suggested with referral for qualified medical, osteopathic or chiropractic care, when indicated, although excessive icing should be avoided in order to not interfere with normal inflammatory processes. Techniques such as positional release, lymphatic drainage and certain movement therapies may be used to encourage the natural healing process, while NMT techniques are avoided or used only on other body regions to reduce overall structural distress that often accompanies injuries. After 72–96 hours, NMT may be carefully applied to the injured tissues unless otherwise contraindicated by signs of continued inflammatory response, fractures or other structural damage, which may require more healing time or surgical repair.
NMT for chronic pain
It is important to remember that it is the degree of current pain and inflammation that defines the stage of repair (acute, subacute, chronic) the tissue is in, not just the length of time since the injury. Once acute inflammation subsides, which can take weeks, a number of rehabilitation stages of soft tissue therapy are suggested in the order listed below. Chaitow & DeLany (2008) note that these modalities should be incorporated when the tissue is prepared for them, which may be immediately for some patients or a matter of weeks or even months for others. They define these as application of:
1. manual tissue mobilization techniques – appropriate soft tissue techniques aimed at decreasing spasm and ischemia, enhancing drainage of the soft tissues and deactivating trigger points
2. stretching – appropriate active, passive and self-applied stretching methods to restore normal flexibility
3. mild tissue toning – appropriately selected forms of exercise to restore normal tone and strength
4. conditioning exercises and weight-training approaches – to restore overall endurance and cardiovascular efficiency
5. restoring normal proprioceptive function and coordination – by use of standard rehabilitation approaches
6. improving posture and body use – with a particular aim of restoring normal breathing patterns.
Chaitow & DeLany (2008) emphasize:
The sequence in which these recovery steps are introduced is important. The last two (5 and 6) may be started at any time, if appropriate; however, the first four should be sequenced in the order listed in most cases. Clinical experience suggests that recovery can be compromised and symptoms prolonged if all elements of this suggested rehabilitation sequence are not taken into account. For instance, if exercise or weight training is initiated before trigger points are deactivated and contractures eliminated, the condition could worsen and recovery be delayed. In cases of recently traumatized tissue, deep tissue work and stretching applied too early in the process could further damage and reinflame the recovering tissues…Pain should always be respected as a signal that whatever is being done is inappropriate in relation to the current physiological status of the area.
Palpation and treatment
Though the order of the protocols listed in this text can be varied to some degree, there are some suggestions which have proven to be clinically imperative. These are based on our clinical experience (and of those experts cited in the text) and are suggested as a general guideline when addressing most myofascial tissue problems. Chaitow & DeLany (2008) suggest the following:
• If a frictional effect is required (for example, in order to achieve a rapid vascular response) then no lubricant should be used. In most cases, dry skin work is employed before lubrication is applied to avoid slippage of the hands on the skin.
• The use of a lubricant is often needed during NMT application to facilitate smooth passage of the thumb or finger. It is important to avoid excessive oiliness or the essential aspect of slight digital traction will be lost.
• Before the deeper layers are addressed, the most superficial tissue is softened and, if necessary, treated.
• The proximal portions of an extremity are addressed (‘softened’) before the distal portions are treated, thereby reducing restrictions to lymphatic flow before distal lymph movement is increased.
• In a two-jointed muscle, both joints are assessed. For instance, if gastrocnemius is examined, both the knee and ankle joints are considered. In multijointed muscles, all involved joints are assessed.
• Knowledge of the anatomy of each muscle (innervation, fiber arrangement, nearby neurovascular structures and all overlying and underlying muscles) will greatly assist the practitioner in quickly locating the appropriate muscles and their trigger points.
• Where multiple areas of pain are present, our experience suggests the following.
• Treat the most proximal, most medial and most painful trigger points (or areas of pain) first.
• Avoid overtreating the individual tissues as well as the structure as a whole.
• Fewer than five active trigger points should be treated at any one session if the person is frail or demonstrating symptoms of fatigue and general susceptibility as this might place an adaptive load on the individual that could prove extremely stressful.
In order to avoid the use of too much pressure and to allow the patient a degree of control over the temporary discomfort produced during an NMT examination and treatment, a ‘discomfort scale’ can usefully be established. The patient is taught to consider a scale in which 0 = no pain and 10 = unbearable pain. It is best to avoid using applied pressure or other techniques that induce a pain level of between 8 and 10, which can provoke a defensive response from the tissues. Pressures that induce a score of 5 or less usually are insufficient to produce the desired result so a score of 5, 6 or 7 is considered ideal.
Note: In application of strain–counterstrain methodology (see later this chapter) the patient is instructed to ascribe a value of 10 to whatever pain is noted in the palpated ‘tender’ point, rather than being asked what value the discomfort represents. This is distinctly different from the pressure scale noted above.
When digital pressure is applied to tissues, a variety of effects are simultaneously occurring.
1. Temporary interference with circulatory efficiency results in a degree of ischemia, which will reverse when pressure is released (Simons et al 1999).
2. Constantly applied pressure produces a sustained barrage of afferent, followed by efferent, information, resulting in neurological inhibition (Ward 1997).
3. As the elastic barrier is reached and the process of ‘creep’ commences, the tissue is mechanically stretched (Cantu & Grodin 1992).
4. Colloids change state when shearing forces are applied, thereby modifying relatively gel tissues toward a more sol-like state (Athenstaedt 1974, Barnes 1996).
5. Interference with pain messages reaching the brain is apparently caused when mechanoreceptors are stimulated (gate theory) (Melzack & Wall 1988).
6. Local endorphin release is triggered along with enkephalin release in the brain and CNS, as well as the adrenal medulla (Baldry 2005).
7. Endocannabinoids are released. These, like the better known endorphin and enkephalin systems, dampen nociception and pain, and decrease inflammation in myofascial tissues (McPartland 2008).
8. A rapid release of the taut band associated with trigger points often results from applied pressure (Simons et al 1999).
9. Acupuncture and acupressure concepts associate digital pressure with alteration of energy flow along hypothesized meridians (Chaitow 1990).
Neuromuscular therapy: american version
In this text, the American version of NMT is offered as a foundation for developing palpatory skills and treatment techniques while the European version accompanies it to offer an alternative approach (see Box 9.3). Emerging from diverse backgrounds, these two methods of NMT have similarities as well as differences in application. Volume 1, Chapter 9 discusses the history of both methods and their similarities as well as the characteristics unique to each.
NMT American version™, as presented in these textbooks, attempts to address (or at least consider) a number of features commonly involved in causing or intensifying pain (Chaitow 2010). These include, among others, the following factors which affect the whole body:
• nutritional imbalances and deficiencies
• toxicity (exogenous and endogenous)
• stress (physical or psychological)
as well as locally dysfunctional states such as:
Gliding techniques
NMT American version employs a variety of lightly lubricated gliding strokes (effleurage) which explore the tissues for ischemic bands and/or trigger points while assessing the individual tissue’s quality, internal (muscle) tension and degree of tenderness, increase blood flow, thereby ‘flushing’ tissues, create a mechanical counterpressure to the tension within the tissues and can precede deeper palpation or can follow compression or manipulation techniques to soothe and smooth the tissue. In applying the assessment and treatment strokes the following points should be kept in mind.
• The practitioner’s fingers (which stabilize) are spread slightly and ‘lead’ the thumbs (which are the actual treatment tool in most cases). The fingers support the weight of the hands and arms, which relieves the thumbs of that responsibility so that they are more easily controlled and can vary induced tension to match the tissues. (See Fig. 10.32, p. 257.)
• When two-handed glides are employed, the lateral aspects of the thumbs are placed side by side or one slightly ahead of the other with both pointing in the direction of the glide (see Volume 1, Fig. 9.2A)
• The hands move as a unit, with little or no motion taking place in the wrist or the thumb joints, which otherwise may result in joint inflammation, irritation and dysfunction.
• Pressure is applied through the wrist and longitudinally through the thumb joints, not against the medial aspects of the thumbs, as would occur if the gliding stroke were performed with the thumb tips touching end to end (see Volume 1, Fig. 9.2B)
• As the thumb or fingers move from normal tissue to tense, edematous, fibrotic or flaccid tissue, the amount of pressure required to ‘meet and match’ it will vary, with pressure being increased only if appropriate. As the thumb glides transversely across taut bands, indurations may be more defined.
• Nodules are sometimes embedded (usually at mid-fiber range) in dense, congested tissue and as the state of the colloidal matrix softens from the gliding stroke, distinct palpation of the nodules becomes clearer (see Box 9.4).
• The practitioner moves from trigger point pressure release, to various stretching techniques, heat or ice, vibration or movements, while seamlessly integrating these with the assessment strokes.
• The gliding strokes are applied repetitively (6–8 times), then the tissues are allowed to rest while working elsewhere before returning to reexamine them.
• Positional release methods, gentle myofascial release, cryotherapy, lymph drainage or other antiinflammatory measures would be more appropriate for tender or inflamed tissues than friction, heat, deep gliding strokes or other modalities that might increase an inflammatory response.
• The gliding stroke should cover 3–4 inches per second unless the tissue is sensitive, in which case a slower pace and reduced pressure are suggested. It is important to develop a moderate gliding speed in order to feel what is present in the tissue. Rapid movement may skim over congestion and other changes in the tissues or cause unnecessary discomfort while movement that is too slow may displace tissue and make identification of individual muscles difficult.
• Unless contraindicated due to inflammation, a moist hot pack can be placed on the tissues between gliding repetitions to further enhance the effects. Ice may also be used and is especially effective on attachment trigger points (see Box 9.5) where a constant concentration of muscle stress tends to provoke an inflammatory response (Simons et al 1999). See Box 9.6 for information regarding use of hydrotherapy methods and a more in-depth discussion in Volume 1, Chapter 10.
Box 9.4 Central trigger point palpation and treatment
• When locating the center of the fibers, which is also the endplate zone of most muscles and the usual location of central trigger points (CTrP), only the actual fiber length is considered and not the tendons.
• The approximate center of the fibers is located and flat or pincer compression is applied to the taut muscle fibers in search of central nodules.
• The tissue may be treated in a slightly passively shortened position or, if attachments are not inflamed, a slight stretch may be added, which may increase the palpation level of the taut band and nodule.
• As the tension becomes palpable, pressure is increased into the tissues to meet and match the tension.
• The fingers should then slide longitudinally along the taut band near mid-fiber to assess for a thickening of the associated myofascial tissue or a palpable (myofascial) nodule.
• An exquisite degree of spot tenderness is usually reported near or at the trigger point sites and the presence of a local twitch response sometimes confirms that a trigger point has been encountered.
• When pressure is increased (gradually) into the core of the nodule (CTrP), the tissue may refer sensations such as pain, tingling, numbness, itching or burning, which the patient either recognizes (active trigger point) or does not (latent trigger point).
• The degree of pressure will vary and should be adjusted so that the person reports a mid-range number between 5 and 7 on his discomfort scale, as the pressure is maintained.
• The practitioner may feel the tissues ‘melting and softening’ under the sustained pressure, at which time the pressure can usually be mildly increased as tissues relax and tension releases, provided the discomfort scale is respected.
• The length of time that pressure is maintained will vary. However, the discomfort level should drop and tension should ease within 8–12 seconds, even if pressure is sustained for a longer time.
• If it does not begin to respond within 8–12 seconds, the amount of pressure should be adjusted accordingly (usually lessened), the angle of pressure altered or a more precise location sought that displays heightened tenderness or a more distinct nodule.
• Twenty seconds is the maximum length of time to hold the pressure since the tissues are being deprived of normal blood flow while pressure is ischemically compressing (blanching) them.
• European NMT offers alternative protocols such as variable ischemic compression and INIT.
• Slightly stretching the muscle tissue often makes the taut fibers much easier to palpate as long as caution is exercised to avoid placing tension on inflamed attachment sites. The use of aggressive applications (such as strumming or friction) should be avoided while the tissue is being stretched as injury is more likely to occur in a stretched position.
• Three or four repetitions of the protocol as described above may need to be applied to the same area.
• Unless attachments are inflamed, treatment of a trigger point is usually followed with several passive elongations (stretches) of the tissue to that tissue’s range of motion barrier. Three or four active repetitions of the stretch are then performed and the patient is encouraged to continue to do them as ‘homework’.
• Trigger point treatment can be followed by one or more forms of hydrotherapy: heat (unless inflamed), ice, contrast hydrotherapy or a combination of heat to the muscle belly and ice to the tendons (see hydrotherapy in Volume 1, Chapter 7).
• Fascia elongates best when warm and more liquid (sol) and is less pliable when cold and less easily stretched (Lowe 1995). Cold tissues can be rewarmed with a hot pack or mild movement therapy used before stretches are applied. These precautions do not apply for brief exposures to cold, such as spray-and-stretch or ice-stripping techniques.
Box 9.5 Attachment trigger point location and palpation
Attachment sites may be inflamed and/or extremely sensitive so palpation should be performed cautiously. Attachment trigger points (ATrP) form at musculotendinous or periosteal sites as the result of excessive, unrelieved tension on the attachment tissues. If found to be very tender, stretching techniques or other steps that apply additional tension should not be used as undue stress to these tissues may provoke or increase an inflammatory response.
For attachment trigger points, the central trigger point should be released and cryotherapy (ice therapy) applied to the attachment sites. Manual traction can be applied locally to the centrally located shortened sarcomeres. Gliding strokes may be started at the center of the fibers with both thumbs gliding simultaneously from the center to opposite ends (see Volume 1, Chapter 9, Fig. 9.6).
Passive and active range of motion is added to the protocol at future sessions only if attachment sites have improved sufficiently.
Box 9.6 Hydrotherapies (Chaitow 1999)
The therapeutic benefits of water applications to the body, and particularly of thermal stimulations associated with them, can be employed in both clinical and home application. A more extensive discussion of hydrotherapies occurs in Volume 1, Chapter 9 and 10, while only brief descriptions of the most important points of hot and cold applications are given here.
Regarding hot and cold applications
• Hot is defined as 98–104°F or 36.7–40°C. Anything hotter than that is undesirable and dangerous.
• Cold is defined as 55–65°F or 12.7–18.3°C.
• Anything colder is very cold and anything warmer is:
• Short cold applications (less than a minute) stimulate circulation while applications of cold longer than a minute depress circulation and metabolism.
• Short hot applications (less than 5 minutes) stimulate circulation while hot applications for longer than 5 minutes depress both circulation and metabolism.
• Because long hot applications vasodilate and can leave the area congested and static, they require a cold application or massage to help restore normality.
• Short hot followed by short cold applications cause alternation of circulation followed by a return to normal. This contrasting application produces circulatory interchange and improved drainage and oxygen supply to the tissues, whether these be muscles, skin or organs. Neutral applications or baths at body heat are very soothing and relaxing.
Ice pack
Ice causes vasoconstriction in tissues because of the large amount of heat it absorbs as it turns from solid into liquid. Ice treatment is helpful for:
Applications of ice are contraindicated on the abdomen during acute bladder problems, over the chest during acute asthma or if any health condition is aggravated by cold.
Spray-and-stretch techniques
Chilling and stretching a muscle housing a trigger point rapidly deactivates the abnormal neurological behavior of the site. Travell (1952) and Mennell (1974) have described these effects in detail. Simons et al (1999) state that ‘Spray and stretch is the single most effective non-invasive method to inactivate acute trigger points’ and that the stretch component is the action and the spray is a distraction. They also point out that the spray is applied before or during the stretch and not after the muscle has already been elongated.
Travell & Simons (1992; Simons et al 1999) have discouraged the use of certain vapocoolants to chill the area due to environmental considerations relating to ozone depletion and have instead urged the use of stroking with ice in a similar manner to the spray stream to achieve the same ends. However, newer products that are ozone-safe allow for a re-emergence of this highly effective techniques. A brief description of spray and stretch is offered in Volume 1, Chapter 10 while lengthier discussions have been offered by Travell & Simons (1992) and Simons et al (1999).
Warming compress (‘cold compress’), alternating sitz baths, neutral bathing and other choices of hydrotherapy methods are recommended for both clinical and home application. A fuller discussion is found in Volume 1, Chapter 10.
Palpation and compression techniques
• Flat palpation (see Volume 1, Fig. 9.3) is applied through the skin by the whole hand, finger pads or finger tips and begins by sliding the skin over the underlying fascia to assess for restriction.
• The skin may appear to be ‘stuck’ to the underlying tissue, which may either house a trigger point or be the target referral pattern for one (Simons et al 1999). A higher level of sweat activity (increased hydrosis), revealed by a sense of friction as the finger is dragged lightly across the dry skin, may be evidence of a hyperalgesic skin zone (Lewit 1999), the precise superficial evidence of a trigger point.
• As the pressure is increased to compress the tissue against bony surfaces or muscles that lie deep to those being palpated, indurations may be felt in underlying muscles. As deeper tissues and underlying structures are evaluated, congestion, fibrotic bands, indurations and other altered tissues textures may be found. Two or three fingers can then direct pressure into or against the tissue until the slack is taken out and the tissue’s tension is ‘matched’ as the tissue is ‘captured’ between the fingers and underlying structures (bone or deeper muscles).
• Flat palpation is used primarily when the muscles are difficult to lift or compress or to add information to that obtained by compression.
• Pincer compression techniques involve grasping and compressing the tissue between the thumb and fingers with either one hand or two. The finger pads (flattened like a clothes pin) (see Volume 1, Fig. 9.4A) will provide a broad general assessment and release while the finger tips (curved like a C-clamp) (see Volume 1, Fig. 9.4B) will compress smaller, more specific sections of the tissue. The muscle or skin can be manipulated by sliding the thumb across the fingers with the tissue held between them or by rolling the tissues between the thumb and fingers.
• Snapping palpation (see Volume 1, Fig. 9.5A,B) is a technique used to elicit a twitch response, which confirms the presence of a trigger point (in tissue meeting minimal criteria) although the lack of a twitch does not rule out a trigger point. The fingers are placed approximately mid-fiber and quickly snap transversely across the taut fibers (similar to plucking a guitar string). It may also be used repetitively as a treatment technique, which is often effective in reducing fibrotic adhesions.
• Treatment tools, such as a pressure bar, may be used to help protect the hands from excessive use of applied pressure so long as precautions are taken to avoid injury to both the patient and practitioner (see Box 9.7 and Volume 1, Chapter 9).
While many treatment tools offer unique qualities, the ‘tools of the trade’ of NMT are a set of pressure bars (Volume 1, Fig. 9.8). These tools are intended to prevent overuse of the thumbs as well as reach tissues the thumbs cannot contact well, such as those located between the ribs. Descriptions are included in this text for those who have been adequately trained in their use but training is required to use the bars safely.
The pressure bars are never used at vulnerable nerve areas such as the inguinal region, intraabdominally, on extremely tender tissues or to ‘dig’ into tissues. Ischemic tissues, fibrosis and bony surfaces along with their protuberances may be ‘felt’ through the bars just as a grain of sand or a crack in the table under writing paper may be felt through a pencil when writing. Any tools that touch the skin should be scrubbed with an antibactericidal soap after each use or cleaned with cold sterilization or other procedures recommended by their manufacturers.
Muscle energy techniques (MET)
(DiGiovanna 1991, Greenman 1989, Janda 1989, Lewit 1986a, b, Liebenson 1989, 1990, Mitchell 1967, Travell & Simons 1992)
Liebenson (1996) summarizes the way in which dysfunctional patterns in the musculoskeletal system can be corrected.
• Identify, relax and stretch overactive, tight muscles.
• Mobilize and/or adjust restricted joints.
• Facilitate and strengthen weak muscles.
• Reeducate movement patterns on a reflex, subcortical basis.
METs are soft tissue manipulative methods which utilize a variety of basic protocols (described in this chapter as well as Volume 1) that can be applied to acute, chronic and rehabilitation situations. In MET, upon request, the patient actively uses his muscles from a controlled position to induce a mild effort in a specific direction against a precise counterforce. Depending upon the desired therapeutic effect, the counterforce can match the patient’s effort (isometrically), fail to match it (isotonically) or overcome it (isolytically, isotonic-eccentrically). The contraction is usually commenced from, or short of, a previously detected barrier of resistance, depending upon the relative acuteness of the situation.
The following guidelines are fundamental to the application of MET. Special notes regarding application to acute and chronic conditions need to be well understood and regarded.
1. ‘Barrier’ refers to the very first sign of palpated or sensed resistance to free movement which will be well short of the physiological or pathophysiological barrier. The very first sign of perceived restriction needs to be identified and respected (Stiles 2009).
2. Active assistance from the patient is valuable when movement is made to or through a barrier with gentle cooperation and without excessive effort.
3. When MET is applied to a joint restriction, subsequent movement is to a new barrier following the isometric contraction; no stretching is involved.
4. Although mild discomfort might be experienced, no pain should be felt during application of MET.
5. Breathing cooperation can and should be used as part of the methodology of MET if the patient is capable of cooperation.
6. Various eye movements are sometimes advocated during (or instead of) contractions and stretches (Lewit 1986b). The use of eye movement relates to the increase in muscle tone in preparation for movement when the eyes move in a given direction.
7. Light contractions (15–20% of available strength) are preferred in MET as they are as effective as a strong contraction in achieving relaxation effects while being easier to control and far less likely to provoke pain or cramping. Occasionally up to 50% available strength is used but increase of the duration of the contraction – up to 20 seconds – may be more effective than any increase in force.
Neurological explanation for MET effects
Postisometric relaxation (PIR). Historically it was thought that when a muscle contracted isometrically, a load would be placed on the Golgi tendon organs which, on cessation of effort, resulted in a period of relative hypotonicity, during which time the involved tissues could be more easily stretched than before the contraction (Lewit 1986b, Mitchell et al 1979). This explanatory model is no longer considered viable, not because PIR does not occur, but because the effect is so short-lived that it could not possibly explain the subsequent easier ability to mobilize or stretch tissues.
Reciprocal inhibition (RI). RI suggests that an isometric contraction of a muscle is accompanied by a loss of tone, or by relaxation, affecting the antagonistic muscle thereby allowing the antagonist to be more easily stretched (Levine 1954, Liebenson 2007). This model is also now thought to lack credibility in explaining the effects of MET.
Increased tolerance to stretch. The phrase ‘increased tolerance to stretch’ has emerged to describe what happens, although it does not explain how it happens.
• Magnusson et al (1996, 1998) measured the degree of applied effort used during passive knee extension, before and after muscles were stretched to the point of pain. They found that both ROM and passive torque were increased following the contraction - because subjects were able to tolerate a stronger stretch.
• Ballantyne et al (2003) confirmed these findings by showing that when the degree of post-test force applied to the muscle remained constant (i.e. the same as used in pre-testing), no change in length took place, suggesting that a single application of MET created a change in tolerance to stretch.
• Fryer (2006) explains: ‘The application of MET would appear to decrease an individual’s perception of muscle pain, and is greater than that which occurs with passive stretching. Stretching and isometric contraction stimulate muscle and joint mechanoreceptors and proprioceptors, and it is possible that this may attenuate the sensation of pain. … MET and stretching appear to produce lasting changes in stretch tolerance, and so the mechanism is likely to be more complex than just gating at the spinal cord, and may also involve changes in the higher centres of the CNS.’
• Hamilton et al (2007) suggest that techniques – such as MET – that stimulate joint proprioceptors, via the production of joint movement, or the stretching of a joint capsule, may be capable of reducing pain by inhibiting the smaller diameter nociceptive neuronal input at the spinal cord level.
• McPartland (2008) has shown that MET-like contractions stimulate release of endocannabinoids, which have analgesic effects.
MET in acute conditions
• Acute conditions are defined as those being acutely painful or those traumas which occurred within the last 3 weeks or so.
• When MET is applied in acute conditions, the first sign of palpated or sensed resistance to free movement is considered to be the initial ‘barrier’.
• Following an isometric contraction of the agonist or antagonist, the acute tissue is passively moved to the new barrier (first sign of resistance) without any attempt to stretch. Additional contraction followed by movement to a new barrier is repeated until no further gain is achieved.
• When MET is applied to a joint restriction the acute model is always used, i.e. no stretching, simply movement to the new barrier and repetition of isometric contraction of agonist or antagonist.
• The steps are repeated 3–5 times or until no further gain in range of motion is possible.
Acute setting method 1: isometric contraction using reciprocal inhibition
Indications
Method:
Isometric contraction of antagonist to affected muscle(s) is used, so employing reciprocal inhibition to relax affected muscles. Patient is attempting to push toward the barrier of restriction against practitioner’s precisely matched counterforce.
Forces:
Practitioner’s and patient’s forces are matched. Initially, 20% of patient’s strength (or less) is used, which increases to no more than 50% on subsequent contractions, if appropriate.
Duration of contraction:
7–10 seconds initially; if greater effect needed, an increase up to 20 seconds in subsequent contractions if no pain is induced by the effort.
Indications
Method:
The affected muscles (agonists) are isometrically contracted and subsequently relax via postisometric relaxation. Practitioner is attempting to push toward the barrier of restriction against the patient’s precisely matched counter effort. If there is pain on contraction this method is contraindicated and acute setting method 1 is used.
Forces:
Practitioner’s and patient’s forces are matched. Initially, 20% of patient’s strength is used, which can increase to no more than 50% on subsequent contractions.
Duration of contraction:
7–10 seconds initially, increasing to up to 20 seconds in subsequent contractions, if greater effect required.
MET in chronic conditions (non-acute)
• Chronic pain is considered to be that which remains at least 3 months after the injury or tissue insult. Subacute stages lie between acute and chronic, at which time a degree of reorganization has started and the acute inflammatory stage is past.
• The first sign of palpated or sensed resistance to free movement is identified in chronic conditions and the isometric contraction is commenced just short of it.
• Following the contraction the tissues are moved slightly beyond the new barrier and are held in that stretched state for 20–30 seconds (or longer), before being returned to a position short of the new barrier for a further isometric contraction.
• The patient assists in the stretching movement in order to activate the antagonists and facilitate the stretch, providing he can use gentle cooperation and not use excessive effort.
• There are times when ‘co-contraction’ (contraction of both agonist and antagonist) is useful. Studies have shown that this approach is particularly useful in treatment of the hamstrings, when both these and the quadriceps are isometrically contracted prior to stretch (Moore 1980).
• The steps are repeated 3–5 times or until no further gain in range of motion is possible.
Chronic setting method 1: isometric contraction using postisometric relaxation (also known as postfacilitation stretching)
Indications
• Stretching chronic or subacute restricted, fibrotic, contracted, soft tissues (fascia, muscle) or tissues housing active myofascial trigger points
Method:
The affected muscles (agonists) are isometrically contracted, and subsequently relax via postisometric relaxation. Practitioner is attempting to push toward the barrier of restriction against the patient’s precisely matched counter effort.
Forces:
Practitioner’s and patient’s forces are matched. Initially, 20% of patient’s strength (or less) is used, which increases to no more than 50% on subsequent contractions, if appropriate.
Duration of contraction:
7–10 seconds initially, increasing to up to 20 seconds in subsequent contractions, if greater effect required.
Action following contraction:
Rest period of 5 seconds or so, to ensure complete relaxation before commencing the stretch. On an exhalation the area (muscle) is taken to its new restriction barrier and a small degree beyond, painlessly, and held in this position for 20–30 seconds. The patient should, if possible, help to move the area to and through the barrier, effectively further inhibiting the structure being stretched and retarding the likelihood of a myotatic stretch reflex.
Indications
• Stretching chronic or subacute restricted, fibrotic, contracted, soft tissues (fascia, muscle) or tissues housing active myofascial trigger points
• If contraction of the agonist is contraindicated because of pain
Method:
Isometric contraction of antagonist to affected muscle(s) is used, so employing reciprocal inhibition to relax affected muscles, allowing an easier stretch to be performed. Patient is attempting to push through barrier of restriction against the practitioner’s precisely matched counter effort.
Forces:
Practitioner’s and patient’s forces are matched. Initially, 30% of patient’s strength (or less) is used, which increases to no more than 50% on subsequent contractions, if appropriate.
Duration of contraction:
7–10 seconds initially, increasing to up to 20 seconds in subsequent contractions, if greater effect required.
Action following contraction:
Rest period of 3–5 seconds, to ensure complete relaxation before commencing the stretch. On an exhalation the area (muscle) is taken to its new restriction barrier and a small degree beyond, painlessly, and held in this position for at least 20–30 seconds. The patient assists in moving to and through the barrier, thereby also employing reciprocal inhibition. Repetitions: The steps are repeated 2–3 times or until no further gain in range of motion is possible.
Indications
Method:
The contracting muscle is allowed to overcome the practitioner’s effort, with some (constant) resistance from the practitioner.
Indications
Method:
The muscle to be stretched is contracted and is prevented from doing so via greater practitioner effort. The contraction is overcome and reversed, so that the contracting muscle is stretched to, or as close as possible to, full physiological resting length.
Forces:
Practitioner’s force is greater than patient’s. Less than maximal patient’s force is employed at first. Subsequent contractions build toward this, if discomfort is not excessive.
Indications
Method:
Patient resists with moderate and variable effort at first, progressing to maximal effort subsequently, as practitioner puts joint rapidly through as full a range of movements as possible. This approach differs from a simple isotonic exercise by virtue of whole ranges of motion, rather than single motions being involved, and because resistance varies and progressively increases.
Forces:
Practitioner’s force overcomes patient’s effort to prevent movement. First movements (for instance, taking an ankle into all its directions of motion) involve moderate force, progressing to full force subsequently. An alternative is to have the practitioner (or machine) resist the patient’s effort to make all the movements.
MET method for toning and strengthening as well as releasing antagonist tone:
Isotonic eccentric contraction of antagonist can be performed slowly in order to strengthen antagonists to short postural muscles, while releasing tone in the postural tissues.
CAUTION: Avoid using isotonic eccentric contractions on head/neck muscles or at all if patient is frail, very pain-sensitive or osteoporotic.
Indications
Method:
The patient is asked to maintain the position at the barrier as the antagonists to the shortened muscle are eccentrically slowly stretched. The antagonists to a short postural muscle will be contracting while it is being lengthened by the practitioner, via superior effort. The contraction is slowly overcome and reversed, so that the contracting muscle is eccentrically stretched. Origin and insertion do not approximate. The muscle is stretched to, or as close as possible to, full physiological resting length. Subsequently the shortened postural muscle (i.e. the antagonist to the muscle that has just been eccentrically stretched) should be stretched passively.
Forces:
Practitioner’s force is greater than patient’s. Less than maximal patient’s force is employed at first. Subsequent contractions build toward this, if discomfort is not excessive.
Pulsed muscle energy techniques
The simplest use of pulsed MET involves the dysfunctional tissue or joint being held at its restriction barrier while the patient (or the practitioner, if the patient cannot adequately cooperate with the instructions) applies a series of rapid (two per second) tiny efforts. These miniature contractions toward the barrier are ideally practitioner resisted, while the barest initiation of effort is actively applied, avoiding any tendency to ‘wobble or bounce’ (Ruddy 1962).
Ruddy (1962) suggested that the effects are likely to include improved oxygenation, venous and lymphatic circulation through the area being treated. Furthermore, he believed that the method influences both static and kinetic posture because of the effects on proprioceptive and interoceptive afferent pathways.
Since shortened, hypertonic musculature or myofascial tissues harboring trigger points are often accompanied by inhibited, weakened antagonists, it is important to begin facilitating and strengthening the weakened tissues when the hypertonic ones are released. The introduction of pulsed METs involving these weak antagonists offers the opportunity for:
• strengthening facilitation of the weak antagonists
• reciprocal inhibition of tense agonists
• enhanced local circulation and drainage
• and, in Liebenson’s (1996) words, ‘reeducation of movement patterns on a reflex, subcortical basis’.
Further discussion of Ruddy’s methods as well as examples of application are found in Volume 1, Chapter 9.
Positional release techniques
Laurence Jones DO (1964) first observed the phenomenon of spontaneous release when he ‘accidentally’ placed a patient who was in considerable pain and some degree of compensatory distortion into a position of comfort (ease) on a treatment table. Despite no other treatment being given, after resting in a position of relative ease for a short period of time, the patient was able to stand upright and was free of pain. This ‘position of ease’ is the key element in what later came to be known as strain–counterstrain (SCS) (Chaitow 2007, Jones 1981, Walther 1988).
Positional release technique (PRT) involves the placement, for brief periods, of soft tissues or joints into positions of comfort, to encourage (it is suggested) self-regulating influences to operate more efficiently, resulting in greater range of motion, reduced pain, etc. Just what the underlying mechanisms of PRT are remains a matter for further research.
• In the strain–counterstrain (SCS) model of PRT, a palpated sensitive point is used as a monitor to guide the tissues towards ease, via feedback from the patient. As the reported pain level reduces (from a starting point of ‘10’ to ‘3’ or less), the tissues being palpated are felt to become slacker and less tense (Jones 1981). The ease position is then held for 90 seconds or so, before being gently released.
• In Functional PRT a similar end-point of ‘comfort’ or ‘ease’ is achieved, however without use of patient feedback, purely by the palpated sense of the tissues relaxing from their previously hypertonic state as they are carefully positioned (Johnston 1964).
• A ‘facilitated’ version of this approach also exists (Faciltated PRT), in which crowding or distraction forces are added to the ‘ease’ position, to speed up the process of release (Schiowitz 1990).
Mechanisms
Various hypotheses currently exist as to the mechanisms involved in PRT, ranging from circulatory enhancement to muscle spindle resetting (D’ambrogio & Roth 1997, Chaitow 2007, Dowling 2005)
Standley & Meltzer (2007) have tested the effects of repetitively straining laboratory tissue specimens, and then ‘placing them at ease.’ They observed that modification of fibroblast proliferation and changes in the expression and secretion of pro-inflammatory and anti-inflammatory interleukins that occur may help to explain the clinical efficacy of PRT techniques.
Solomonow (2009) has shown that crowding or light traction of ligamentous structures – as well as tendons and capsules (such as occurs in facilitated PRT) leads to temporary relaxation of associated muscles, possibly explaining the relaxed state and increased ROM following application of PRT.
Goodheart (1984) has described an almost universally applicable guide for use of SCS, which relies on the individual features displayed by the patient.
• A suitable tender point should be palpated for in the tissues opposite those ‘working’ when pain or restriction is noted.
• Muscles antagonistic to those operating at the time pain is noted in any given movement will be those housing the tender point(s).
• For example, if pain occurs (anywhere) when the neck is being turned to the left, a tender point will be located in the muscles that turn the head to the right.
• Therefore, tender points that are going to be used as ‘monitors’ during the positioning phase of this approach are not sought in the muscles opposite those where pain is noted, but in the muscles opposite those which are actively moving the patient, or area, when pain or restriction is noted.
Positional release technique (PRT) involves maintaining pressure on the monitored tender point or periodically probing it, while placing the patient into a position in which there is no additional pain in the symptomatic area and the monitored pain point has reduced in intensity by at least 70%. This is then held for approximately 90 seconds, according to Jones, but variations in length of holding time are suggested below.
Any painful point as a starting place
• All areas that palpate as painful are associated with or responding to some degree of imbalance, dysfunction or reflexive activity, which may well involve acute or chronic strain.
• We have discussed how one can work from the position of strain (when it is known) to achieve a position of ease. Conversely, any painful point found during soft tissue evaluation could be treated by positional release, whether it is known what strain produced it or not, and whether the problem is acute or chronic.
The response to positional release of a chronically fibrosed area will be less dramatic than from tissues held in simple spasm or hypertonicity. Nevertheless, even in chronic settings, a degree of release can be produced, allowing for easier access to the deeper fibrosis.
The concept of being able to treat any painful tissue using positional release is valid whether the pain is being monitored via feedback from the patient (using reducing levels of pain in the palpated point as a guide) or whether the concept of assessing a reduction in tone in the tissues is being used (as in functional technique – see below).
Resolving joint restrictions using PR (DiGiovanna 1991, Jones 1964, 1966)
Jones (1981) found that by taking a distressed joint close to the position in which the original strain took place, muscle spindles were given an opportunity to reset themselves, to become coherent again, during which time pain in the area lessened. He found that if the position of ease is held for a period (Jones suggests 90 seconds), the spasm in hypertonic, shortened tissues commonly resolves, following which it is usually possible to return the joint to a more normal resting position, if this action is performed extremely slowly.
Jones’ approach to positioning requires verbal feedback from the patient as to discomfort in a ‘tender’ point that the practitioner is palpating (i.e. using it as a monitor) while attempting to find a position of ease, subsequently held for 90 seconds.
Clinical considerations The following guidelines are fundamental to the application of PRT. These points are based on clinical experience and should be borne in mind when using PRT methods in treating pain and dysfunction, especially where the patient is fatigued, sensitive and/or distressed.
• No more than five tender points should be treated at any one session, fewer in sensitive individuals.
• Forewarn patients that there may be a ‘reaction’ (such as soreness and stiffness) on the day(s) following treatment.
• If there are multiple tender points (as in fibromyalgia) treat the most proximal and most medial first.
• Of these tender points, select those that are most painful for initial attention/treatment.
• If self-treatment of painful and restricted areas is advised apprise the patient of these rules (i.e. only a few pain points to be given attention on any one day, to expect a ‘reaction’, to select the most painful points and those closest to the head and the center of the body) (Jones 1981).
Application of PRT: guidelines
The general guidelines which Jones gives for obtaining the position of ease commonly involve the following elements.
• Locate and palpate the appropriate tender point or area of hypertonicity
• Use minimal force and minimal monitoring pressure.
• Achieve maximum ease/comfort/relaxation of tissues.
• Produce no additional pain anywhere else.
• For tender points on the anterior surface of the body, flexion, sidebending and rotation are usually toward the palpated point, followed by fine tuning to reduce sensitivity by at least 70%.
• For tender points on the posterior surface of the body, extension, sidebending and rotation are usually away from the palpated point, followed by fine tuning to reduce sensitivity by 70%.
• When the tender point is closer to the mid-line, less sidebending and rotation are required, and when further from mid-line, more sidebending and rotation are required, in order to achieve a position of ease without additional pain or discomfort being produced elsewhere.
• When trying to find a position of ease, sidebending often needs to be away from the side of the palpated pain point, especially in relation to tender points found on the posterior aspect of the body.
Explanations of the effect of positional release
Several hypotheses have been developed to explain why PRT achieves its effects on the tissues. These are discussed more fully in Volume 1, Chapter 10 but the following are of primary consideration.
• The proprioceptive hypothesis (Korr 1947, 1975, Mathews 1981) focuses on the events that occur at the moment of strain to provide the key to understanding the mechanisms of neurologically induced positional release.
• The nociceptive hypothesis (Bailey & Dick 1992, Van Buskirk 1990) focuses on nociceptive responses (which are more powerful than proprioceptive influences).
• The circulatory hypothesis focuses on localized areas of relative ischemia and lack of oxygen, which leads to the evolution of myofascial trigger points (Travell & Simons 1992). Rathbun & Macnab (1970) demonstrated that improvement of local circulation takes place when a ‘position of ease’ is attained.
As Bailey & Dick (1992) explain:
Functional PR technique (Bowles 1981, Hoover 1969)
Osteopathic functional technique relies on a reduction in palpated tone in stressed (hypertonic/spasm) tissues as the body (or part) is being positioned or fine tuned in relation to all available directions of movement in a given region.
The practitioner’s ‘listening’ (palpating) hand assesses changes in tone as her other hand guides the patient or part through a sequence of positions aimed at enhancing ‘ease’ and reducing ‘bind’. A sequence is carried out involving different directions of movement (e.g. flexion/extension, rotation right and left, sidebending right and left, etc.) with each movement starting at the point of maximum ease revealed by the previous step or combined point of ease of a number of steps. In this way one position of ease is ‘stacked’ on another until all movements have been assessed for ease. For instance:
• The tense tissues in a strained low back would be palpated. One by one, all possible planes of movement would then be introduced, while seeking the ‘position of ease’ during that movement (say, during flexion and extension) that causes the palpated tissues to feel most relaxed to the palpating hand (see Volume 1, Fig. 10.7). Once a position of ease is identified, this is maintained (i.e. no further flexion or extension), with the subsequent assessment for the next ease position being sought (say, involving sideflexion to each side), with that ease position then being stacked onto the first one and so on through all variables (rotation, translation, etc.).
• A full sequence would involve flexion/extension, sidebending and rotating in each direction, translation right and left, translation anterior and posterior, as well as compression/distraction, so involving all available directions of movement of the area.
• Finally a position of maximum ease would be arrived at and held for not less than 90 seconds. A release of hypertonicity and reduction in pain should result.
• As long as all possibilities are included, the precise sequence in which the various directions of motion are evaluated is insignificant.
Integrated neuromuscular inhibition technique (Chaitow 1994, Nagrale et al 2010)
In an attempt to develop a treatment protocol for the deactivation of myofascial trigger points, the following integrated neuromuscular inhibition technique (INIT) sequence has been suggested.
• The trigger point is identified and ischemic compression is applied, sufficient to activate the referral pattern.
• The same degree of pressure is maintained for 5–6 seconds, followed by 2–3 seconds of release of pressure.
• This pattern is repeated for up to 2 minutes until the patient reports that the local or referred symptoms (pain) have reduced or that the pain has increased, a rare but significant event sufficient to warrant ceasing application of pressure. Therefore, the ischemic compression aspect of the INIT treatment ceases if the patient reports pain decrease or increase or if 2 minutes of this off-and-on pressure application elapses.
• At this time pressure is reintroduced and whatever degree of pain is noted is ascribed a value of ‘10’ and the patient is asked to offer feedback in the form of ‘scores’ as to the pain value, as the area is repositioned according to the guidelines of positional release methodology. A position is sought which reduces reported pain to a score of 3 or less.
• This ‘position of ease’ is held for at least 20 seconds, to allow neurological resetting, reduction in nociceptor activity and enhanced local circulatory interchange.
• At this stage, the application of MET employs an isometric contraction, focused into the musculature around the trigger point, after which the tissues are stretched both locally and, where possible, in a manner that involves the whole muscle.
• In some instances, a reeducational activation of antagonists can be added to the muscle housing the trigger point using pulsed MET.
The rationale for using INIT
INIT uses several modalities to treat a particular tender/trigger point.
• First, direct pressure identifies the trigger point and when the tissues in which the trigger point lies are positioned in such a way as to take away (most of) the pain (positional release), the most stressed fibers in which the trigger point is housed will be in a position of relative ease.
• After 20 seconds in this position of ease, an isometric contraction is introduced into the tissues and held for 7–10 seconds, involving the precise fibers that had been repositioned to obtain the positional release (and which house the trigger point).
• The effect of this would be a post-isometric reduction in tone in these tissues that could then be stretched locally, or in a manner to involve the whole muscle, depending on the location, so that the specifically targeted fibers would be stretched.
Myofascial release techniques (MFR)
Having evaluated where a restricted area exists, myofascial release (MFR) techniques can be applied to the tissues before any lubrication is used as MFR methods are most effectively applied to dry skin. MFR calls for the application of a sustained gentle pressure, usually in line with the fiber direction of the tissues being treated, which engages the elastic component of the elastico-collagenous complex, stretching this until it commences, and then (eventually) ceases, to release (this can take several minutes).
Example To most easily apply a broad myofascial release to the superficial paraspinal muscles, the practitioner stands level with the middle of the fibers to be addressed, treating one side of the body at a time. The practitioner should stand at the lower chest level on the patient’s right side, in order to allow an MFR application to the right lumbar and thoracic tissues in a head-to-toe (lengthening) manner. The practitioner’s arms are crossed so that the palm of the practitioner’s caudal hand is placed on the mid-thoracic region (fingers facing cephalad) and the palm of the cephalad hand (fingers facing caudad) is placed on the tissues of the lower back of the same side of the torso, with the heels of the hands a few centimeters apart. When applying pressure to engage the elastic components, only a small amount of pressure is oriented into the torso; that is, just enough to keep the hands from sliding on the skin. The remaining pressure is applied in a horizontal direction so as to create tension on the tissues located between the two hands. As the hands move away from each other, taking up the slack, an elastic barrier will be felt and held under mild tension.
This is held until release commences as a result of what is known as the viscous flow phenomenon, in which a slowly applied load (pressure) causes the viscous medium to become more liquid (‘sol’) than would be allowed by rapidly applied pressure. As fascial tissues distort in response to pressure, the process is known by the short-hand term ‘creep’ (Twomey & Taylor 1982). Hysteresis is the process of heat and energy exchange by the tissues as they deform. (See Volume 1, Chapter 1 for discussions of hysteresis and creep.)
After 90–120 seconds (less time if skin rolling or MET has been applied first), the first release of the tissues will be felt as the gel changes to a more solute state. The practitioner can follow the release into a new tissue barrier and again apply the sustained tension. The tissues usually become softer and more pliable with each ‘release’ (Barnes 1997).
Pressure can also be applied to restricted myofascia using a ‘curved’ contact and varying directions of pressure in an attempt to manually stretch the restriction barrier (see Chapter 12, Fig. 12.33).
Tensional elements of MFR can be applied to muscle that is in a relaxed state, placed on tension (at stretch) or, as Mock (1997) notes, one which:
…involves the introduction to the process of passively induced motion, as an area of restriction is compressed while the tissues being compressed are taken passively through their fullest possible range of motion (or where the) patient actively moves the tissues through the fullest possible range of motion, from shortest to longest, while the operator offers resistance.
This version of MFR is sometimes known as ‘soft tissue release’ (Sanderson 1998).
It can be seen from the descriptions offered that there are different models of myofascial release, some taking tissue to the elastic barrier and waiting for a release mechanism to operate and others in which force (here, by active or passive movement) is applied to induce change. Whichever approach is adopted, MFR technique is used to improve movement potentials, reduce restrictions, release spasm, ease pain and prepare the tissues for palpation and application of NMT techniques.
A more in-depth discussion of myofascial release is found in Volume 1, Chapter 10.
Acupuncture and trigger points
Acupuncture points can be corroborated by electrical detection at fairly precise anatomical locations, each point being evidenced by a small area of lowered electrical resistance (Mann 1963). These points become even more easily detectable when ‘active’, as the electrical resistance lowers further. The skin overlying them also alters and becomes hyperalgesic and easy to palpate as differing from surrounding skin, with characteristics similar to trigger points (see Volume 1, Chapter 6). They are sensitive during palpation or treatment and are also amenable to treatment by direct pressure techniques.
Pain researchers Wall & Melzack (1989), as well as Simons et al (1999), note the high correspondence (about 70%) between acupuncture points and trigger point locations and that, though discovered independently and labeled differently, in relation to pain control they represent the same phenomenon.
Baldry (2005) differentiates between the structural make-up of trigger points and acupuncture points, noting that traditionally, acupuncture points are treated in skin and subcutaneous tissues while trigger points are usually located in the intramuscular tissues. He notes that A-delta afferent innervation (sensitive to sharply pointed stimuli or heat-produced stimulation) are found mainly in and just under the skin and are stimulated when carrying out the acupuncture procedure known as superficial dry needling. It is thought that trigger points predominantly use C-afferent innervation (sensitive to chemical, mechanical or thermal stimulus). Baldry aptly discusses principles of trigger point acupuncture and, when comparing dry needling to wet needling (injection of local anesthetic), he states,
there is now sound neurophysiology grounds for believing that it is more rational as well as being simpler, safer and just as effective to alleviate this type of pain by stimulating with dry needles, nerve endings in the superficial tissues directly overlying these intramuscularly situated tender points … now called trigger points.
Which route of reflex stimulation is producing a therapeutic effect or whether other mechanisms altogether are at work is open to debate. This debate can be widened if one considers the vast array of other reflex influences, including endorphin release, endocannabinoid release, neurolymphatic responses, limbic involvement and neuro-vascular reflexes (Chaitow 2010). See also Volume 1, Chapter 10.
Mobilization and articulation
The simplest description of articulation (or mobilization) is that it involves taking a joint through its full range of motion, using low velocity (slow moving) and high amplitude (largest magnitude of normal movement). This is the exact opposite to a high-velocity thrust (HVT) manipulation approach, in which amplitude is very small and speed is very fast.
The therapeutic goal of articulation is to restore freedom of range of movement where it has been reduced. The rhythmic application of articulatory mobilization effectively releases much of the soft tissue hypertonicity surrounding a restricted joint. However, it will not reduce fibrotic changes that may require more direct manual methods.
Mobilization with movement
Brian Mulligan (1992), a New Zealand physiotherapist, has developed a number of extremely useful mobilization procedures for painful and/or restricted joints. The basic concept of Mulligan’s mobilization with movement (MWM) is that a painless, gliding, translation pressure is applied by the practitioner, almost always at right angles to the plane of movement in which restriction is noted, while the patient actively (or sometimes the practitioner passively) moves the joint in the direction of restriction or pain. MWM measures will be described in relation to the sacroiliac joint as well as for the knee and some of the smaller joints of the ankle and foot (see Chapters 11 and 14).
Mulligan (1992) has also described effective MWM techniques for spinal joints. These mobilization methods carry the acronym SNAGs, which stands for ‘sustained natural apophyseal glides’. They are used to improve function if any restriction or pain is experienced on flexion, extension, sideflexion or rotation of the spine. In order to apply these methods to the spine, the practitioner must be aware of the facet angles of those segments being treated (Kappler 1997, Lewit 1986a, Mulligan 1992).
• Most applications of SNAGs commence with the patient weight bearing, usually seated.
• The movements are actively performed by the patient, in the direction of restriction, while the practitioner passively holds a spinal vertebra in an anteriorly translated direction by applying light pressure via the articular pillars or spinous process.
• In none of the SNAGs applications should any pain be experienced, although some residual stiffness/soreness is to be anticipated on the following day, as with most mobilization approaches.
• If a painless movement through a previously restricted barrier is achieved while the translation is held, the same procedure is performed several times more.
• There should be an instant, and lasting, functional improvement if the source of restriction is in the facet joint.
• The use of these mobilization methods is enhanced by normalization of soft tissue restrictions and shortened musculature, using NMT, MFR, MET, etc.
See Volume 1, Chapter 11, Box 11.10 for descriptions of application of SNAGs in the cervical region.
Rehabilitation
Rehabilitation implies returning the individual toward a state of normality that has been lost through trauma or ill health. Issues of patient compliance and home care are key features in recovery and these have been discussed in Chapter 7 as well as Volume 1 of this text.
There are many interlocking rehabilitation features involved in any particular case. Each case must be individually assessed and a program designed for recovery, employing multiple methods, which may include:
• normalization of soft tissue dysfunction
• deactivation of myofascial trigger points
• strengthening weakened structures
• proprioceptive reeducation utilizing physical therapy methods
• postural and breathing reeducation
• ergonomic, nutritional and stress management strategies
• psychotherapy, counseling or pain management approaches
• occupational therapy that specializes in activating healthy coping mechanisms
• appropriate exercise strategies to overcome deconditioning.
A team approach to rehabilitation is called for where referral and cooperation between health-care professionals allow the best outcome to be achieved. This text and its companion volume discuss numerous methods to achieve many of the above-listed elements. Additionally, the reader is encouraged to develop an understanding of the multiple disciplines with which she can interface so that the best outcome for the patient may be achieved.
Emerging modalities (and re-emergence of an older one) that are compatible with NMT
This summary includes three modalities that have become widely used as adjuncts to physical therapy, chiropractic, osteopathy and massage therapy over the past few years since the 1st edition of this book was written. As such the authors consider that they should be mentioned, albeit briefly, in this chapter on NMT-associated modalities.
Active Release Technique (ART)®
The concept used in application of ART®appears similar to the ‘pin and stretch’ methodology, except that ART® involves active rather than passive movement, which are used in ‘pin & stretch’. In ART®, tension and tissue-specific degrees of compression are applied digitally and, while practitioner maintains this contact, the associated tissues are taken from a shortened state to a lengthened state, in an active manner (by the patient). (Howitt 2006, Schiottz-Christensen 1999)
Connective Tissue Manipulation
First developed in the 1930s in Germany, Connective Tissue Massage (Bindegewebsmassage) has recently been relabeled as Connective Tissue Manipulation. In application of CTM the fingers move the skin layer on the underlying fascial layer (as in vigorous skin-rolling). When restrictions exist, this movement commonly creates a short, sharp ‘cutting’ sensation. Experience suggests that the more adherent the connective tissue to the skin, the sharper the sensation feels to the patient. Apart from skin-rolling, strong strokes applied, by thumb or fingers, to unlubricated soft tissues commonly produce a similar response (Ctak-Karakaya et al 2006, Yagci 2004).
Various theories exist regarding possible resulting reflex effects. For example, Bischof & Elmiger (1960) explain:
The specific mechanical stimulation of the pull on connective tissue seems to be the adequate stimulus to elicit the nervous reflex. Connective tissue massage acts first on the sympathetic terminal reticulum in the skin. The smallest branches of the autonomic nervous system contact the impulses activated by the pulling strokes to the sympathetic trunk and the spinal cord. The impulses travel from the skin either through a somatosensory spinal nerve via a posterior root ganglion to the grey matter or over the vascular plexus to the same segmental sympathetic ganglion or to the ganglion of the neighbouring segment, through the ramus communicans albus to the posterior root and grey matter of the spinal cord. They terminate either directly or by means of the internuncial neurons at the efferent autonomic root cells.
In the efferent pathway the impulses travel from the autonomic lateral horn, or the intermediolateral column, over the anterior root, ramus communicans albus, to the segmental sympathetic ganglion or to the ganglion of the neighbouring segment and finally to the diseased organ. The origin of the connective tissue reflex zones and the influence of the CTM depend on the relationship between the function of the internal organs, vessels, and nerves as well as the tissues of the locomotor apparatus, which descend from the same metamere.
However benefits may also result directly from a freeing of connective tissue to allow it to move (‘slide’) more freely in response to normal function.
Fascial Manipulation®
Fascial Manipulation,® developed by Luigi Stecco and his daughter, Carla Stecco MD, and son, Antonio Stecco MD, uses a series of assessment protocols to identify areas of unnatural fascial ‘densification’. In their book Fascial manipulation for musculoskeletal pain (Stecco 2004, 2009a) they describe the therapeutic options that have emerged from their years of anatomical research, that continues unabated (Stecco et al, 2007, 2009b, 2009c, 2009d, Stecco 1994).
They describe their findings in which they epitomize the fascial body as comprising a single networking organ, involving many bags, and hundreds of rope-like local ‘densifications’, with thousands of pockets within pockets, all interconnected by sturdy septa, as well as by looser connective tissue layers. The inability of these tissues to smoothly slide on each other, as a result of trauma or repetitive microtrauma, appears to be the precursor to the palpable, and treatable, changes that they identify and treat.
The target tissues are located by means of assessment protocols, based partly on the findings of their cadaver studies, as well as their understanding of the network quality of fascial function in the living body. The dysfunctional (‘densified’) tissues are highly sensitive, as well as often being characterized by a granular quality, when palpated, and appear to be capable of influencing fascial and other structures some distance from their location.
These tissues are treated using direct compressive force (finger, thumb, knuckle, elbow), in a specific manner that repetitively, and deeply, moves over the dysfunctional tissues until local symptoms modify, and/or distinctive softening changes are noted in the palpated quality of the area.
Acolet D. Changes in plasma cortisol and catecholamine concentrations on response to massage in preterm infants. Arch Dis Child. 1993;68:29-31.
Athenstaedt H. Pyroelectric and piezoelectric properties of vertebrates. Ann N Y Acad Sci. 1974;238:68-110.
Bailey M., Dick L. Nociceptive considerations in treating with counterstrain. J Am Osteopath Assoc. 1992;92:334-341.
Baldry P. Acupuncture, trigger points and musculoskeletal pain, ed 3. Edinburgh: Churchill Livingstone, 2005.
Ballantyne F., Fryer G., McLaughlin P. The effect of muscle energy technique on hamstring extensibility: the mechanism of altered flexibility. Journal of Osteopathic Medicine. 2003;6(2):59-63.
Barnes J. Myofascial release in treatment of thoracic outletsyndrome. Journal of Bodywork and Movement Therapies. 1996;1(1):53-57.
Barnes M. The basic science of myofascial release. Journal of Bodywork and Movement Therapies. 1997;1(4):231-238.
Bischof I., Elmiger G. Connective tissue massage. Licht E., editor, Massage, manipulation and traction. 1960. New Haven, Connecticut
Bowles C. Functional technique – a modern perspective. J Am Osteopath Assoc. 1981;80(3):326-331.
Brostoff J. Complete guide to food allergy. London: Bloomsbury, 1992.
Cailliet R. Soft tissue pain and disability, ed 3. Philadelphia: F A Davis, 1996.
Cantu R., Grodin A. Myofascial manipulation. Gaithersburg, Maryland: Aspen Publications, 1992.
Chaitow L. Acupuncture treatment of pain. Rochester, Vermont: Healing Arts Press, 1990.
Chaitow L. Integrated neuromuscular inhibition technique. British Journal of Osteopathy. 1994;13:17-20.
Chaitow L. Modern neuromuscular techniques, ed 3. New York: Churchill Livingstone, 2010.
Chaitow L. Positional release techniques, ed 3. Edinburgh: Churchill Livingstone, 2007.
Chaitow L. Hydrotherapy. Shaftesbury, Dorset: Element, 1999.
Chaitow L., DeLany J. Clinical application of neuromuscular techniques, volume 1 2nd edition: the upper body. Edinburgh: Churchill Livingstone, 2008.
Chikly B. Clinical perspectives: breast cancer reconstructive rehabilitation: LDT. Journal of Bodywork and Movement Therapies. 1999;3(1):11-16.
Ctak-Karakaya I., Akbayrak T., Demirtürk F., et al. Short and long-term results of connective tissue manipulation and combined ultrasound therapy in patients with fibromyalgia. J Manipulative Physiol Ther. 2006;29(7):524-528.
D’Ambrogio K., Roth G. Positional release technique. Boston: Butterworth Heinemann, 1997.
DeLany J. Clinical perspectives: breast cancer reconstructive rehabilitation: NMT. Journal of Bodywork and Movement Therapies. 1999;3(1):5-10.
DiGiovanna E. Osteopathic diagnosis and treatment. Philadelphia: JB Lippincott, 1991.
Dowling D.J. Myofascial release concepts. In: DiGiovanna E.L., Schiowitz S., Dowling D.J., editors. An osteopathic approach to diagnosis and treatment. ed 3. Philadelphia: Lippincott Williams & Wilkins; 2005:95-102.
Ferel-Torey A. Use of therapeutic massage as a nursing intervention to modify anxiety and perceptions of cancer pain. Cancer Nurs. 1993;16(2):93-101.
Field T. Massage reduces depression and anxiety in child and adolescent psychiatry patients. Journal of the American Academy of Adolescent Psychiatry. 1992;31:125-131.
Foster G., Vaziri N., Sassoon C. Respiratory alkalosis. Respir Care. 2001;46(4):384-391.
Fryer G. MET: efficacy & research. In Chaitow L., editor: Muscle energy techniques, ed 3, Edinburgh: Elsevier, 2006.
Gates C., Huard J. Management of skeletal muscle injuries in military personnel. Operative Techniques in Sports Medicine. 2005;13(4):247-256.
Gilbert C. Hyperventilation and the body. Journal of Bodywork and Movement Therapies. 1998;2(3):184-191.
Goodheart G. Detroit. Applied kinesiology. Workshop procedure manual. ed 21. 1984. Privately published
Greenman P. Principles of manual medicine. Baltimore: Williams and Wilkins, 1989.
Hamilton L., Boswell C., Fryer G. Effects of high-velocity, low-amplitude manipulation and muscle energy technique on suboccipital tenderness. International Journal of Osteopathic Medicine. 2007;10(2–3):42-49.
Hoover H. Collected papers. Academy of Applied Osteopathy Yearbook. California: Carmel, 1969.
Hovind H. Effects of massage on blood flow in skeletal muscle. Scand J Rehabil Med. 1974;6:74-77.
Howitt S. Lateral epicondylosis: a case study of conservative care utilizing ART® and rehabilitation. Journal of the Canadian Chiropractic Association. 2006;50(3):182-189.
Ironson G. Relaxation through massage associated with decreased distress and increased serotonin levels. Touch Research Institute, University of Miami School of Medicine, 1993. unpublished
Janda V. Muscle function testing. London: Butterworths, 1989.
Johnston W. Strategy of a functional approach in acute knee problems. Colorado Springs: Academy of Applied Osteopathy Yearbook, 1964.
Jones L. Spontaneous release by positioning. The DO. 1964;4:109-116.
Jones L. Missed anterior spinal lesions: a preliminary report. The DO. 1966;6:75-79.
Jones L. Strain and counterstrain. Colorado Springs: Academy of Applied Osteopathy, 1981.
Kappler R. Cervical spine. In: Ward R., editor. Foundations of osteopathic medicine. Baltimore: Williams and Wilkins, 1997.
Korr I. The neural basis of the osteopathic lesion. J Am Osteopath Assoc. 1947;48:191-198.
Korr I. Proprioceptors and somatic dysfunction. J Am Osteopath Assoc. 1975;74:638-650.
Levine M. Relaxation of spasticity by physiological techniques. Arch Phys Med Rehabil. 1954;35:214.
Lewit K. Muscular patterns in thoraco-lumbar lesions. Manual Medicine. 1986;2:105.
Lewit K. Postisometric relaxation in combination with other methods. Manuelle Medezin. 1986;2:101.
Lewit K. Manipulative therapy in rehabilitation of the locomotor system, ed 3. London: Butterworths, 1999.
Liebenson C. Active muscular relaxation techniques (parts 1 and 2). J Manipulative Physiol Ther. 1989/1990;12(6):446-451. 13(1):2–6,
Liebenson C. Rehabilitation of the spine. Baltimore: Williams and Wilkins, 1996.
Liebenson C., editor. Rehabilitation of the spine: a practitioner’s manual, ed 2, Philadelphia: Lippincott Williams & Wilkins, 2007.
Lowe W. Looking in depth: heat and cold therapy. In: Orthopedic and sports massage reviews. Bend, Oregon: Orthopedic Massage Education and Research Institute; 1995.
McPartland J. Expression of the endocannabinoid system in fibroblasts and myofascial tissues. Journal of Bodywork and Movement Therapies. 2008;12:169-182.
Magnusson M., Simonsen E., Aagaard P., et al. A mechanism for altered flexibility in human skeletal muscle. J Physiol. 1996;497(Part 1):293-298.
Magnusson M., Aagaard P., Simonsen E.B., et al. A biomechanical evaluation of cyclic and static stretch in human skeletal muscle. Int J Sports Med. 1998;19:310-316.
Mann F. The treatment of disease by acupuncture. London: Heinemann Medical, 1963.
Mathews P. Muscle spindles. Brooks V., editor. Handbook of physiology. Section 1 the nervous system, 2. Bethesda, Maryland: American Physiological Society, 1981.
Melzack R., Wall P. The challenge of pain, ed 2. Harmondsworth: Penguin, 1988.
Mennell J. Therapeutic use of cold. J Am Osteopath Assoc. 74(12), 1974.
Mitchell F.Sr. Motion discordance. Academy of Applied Osteopathy Yearbook. California: Carmel, 1967.
Mitchell F.Jr, Moran P., Pruzzo N. An evaluation of osteopathic muscle energy procedures. Valley Park: Pruzzo, 1979.
Mock L. Myofascial release treatment of specific muscles of the upper extremity (levels 3 and 4). Clinical Bulletin of Myofascial Therapy. 1997;2(1):5-23.
Moore M. Electromyographic investigation manual of muscle stretching techniques. Medical Science in Sports and Exercise. 1980;12:322-329.
Mulligan B. Manual therapy. Wellington, New Zealand: Plane View Services, 1992.
Nagrale A., Glynn P., Joshi A., et al. The efficacy of an integrated neuromuscular inhibition technique on upper trapezius trigger points in subjects with non-specific neck pain: a randomized controlled trial. Journal of Manual and Manipulative Therapy. 2010;18(1):38-44.
Oschman J.L. What is healing energy? Pt 5: gravity, structure, and emotions. Journal of Bodywork and Movement Therapies. 1997;1(5):307-308.
Pryor J., Prasad S. Physiotherapy for respiratory and cardiac problems, ed 3, Edinburgh: Churchill Livingstone; 2002:81.
Puustjarvi K. Effects of massage in patients with chronic tension headaches. Acupuncture and Electrotherapeutics Research. 1990;15:159-162.
Ramirez M. Low back pain – diagnosis by six newly discovered sacral tender points and treatment with counterstrain technique. J Am Osteopath Assoc. 1989;89(7):905-913.
Rathbun J., Macnab I. Microvascular pattern at the rotator cuff. J Bone Joint Surg. 1970;52:540-553.
Ruddy T. Osteopathic rapid rhythmic resistive technic. Carmel, California: Academy of Applied Osteopathy Yearbook, 1962.
Sanderson M. Soft tissue release. Chichester: Otter Publications, 1998.
Sandler S. The physiology of soft tissue massage. British Osteopathic Journal. 1983;15:1-6.
Schiottz-Christensen B., Mooney V., Azxad S., et al. The role of Active Release Manual Therapy for upper extremity overuse syndromes – a preliminary report. J Occup Rehabil. 1999;9(3):201-211.
Schiowitz S. Facilitated positional release. J Am Osteopath Assoc. 1990;90(2):145.
Simons D., Travell J., Simons L. Myofascial pain and dysfunction: the trigger point manual, vol 1: the upper half of body, ed 2. Baltimore: Lippincott Williams and Wilkins, 1999.
Solomonow M. Ligaments: A source of musculoskeletal disorders. Journal of Bodywork & Movement Therapies. 2009;13(2):136-154.
Standley P., Meltzer K. Modelled Repetitive Motion Strain and Indirect Osteopathic Manipulative Techniques in Regulation of Human Fibroblast Proliferation and Interleukin Secretion. J Am Osteopath Assoc.. 2007;107:527-536.
Stecco L. Neuroconnective management of back pain. Riabilitazione. 1994;27(1):15-25.
Stecco L. Fascial manipulation. Padova: Piccin ed, 2004.
Stecco C., Gagey O., Belloni A., et al. Anatomy of the deep fascia of the upper limb. Second part: study of innervation. Morphologie. 2007;91:38-43.
Stecco L., Stecco C. Fascial manipulation: practical. Padova: Piccin ed, 2009.
Stecco C., Lancerotto L., Porzionato A., et al. The palmaris longus muscle and its relations with the antebrachial fascia and the palmar aponeurosis. Clin Anat. 2009;22(2):221-229.
Stecco C., Pavan P., Porzionato A., et al. Mechanics of crural fascia: from anatomy to constitutive modeling. Surg Radiol Anat. 2009;31(7):1-7.
Stecco L., Macchi V., Stecco C. Anatomical study of myofascial continuity in the anterior region of the upper limb. Journal of Bodywork and Movement Therapies. 2009;13(1):53-62.
Stiles E. Muscle energy techniques. In: Franke H., editor. Muscle energy technique: history-model-research. Wiesbaden: Verband der Osteopathen Deutschland (VOD), 2009.
Travell J. Ethyl chloride spray for painful muscle spasm. Arch Phys Med. 1952;33:291-298.
Travell J., Simons D. Myofascial pain and dysfunction: the trigger point manual, vol 2: the lower extremities. Baltimore: Williams and Wilkins, 1992.
Twomey L., Taylor J. Flexion, creep, dysfunction and hysteresis in the lumbar vertebral column. Spine. 1982;7(2):116-122.
Van Buskirk R. Nociceptive reflexes and the somatic dysfunction. J Am Osteopath Assoc. 1990;90:792-809.
Wall P., Melzack R. Textbook of pain. London: Churchill Livingstone, 1989.
Walther D. Applied kinesiology synopsis. Pueblo, Colorado: Systems DC, 1988.
Ward R. Foundations of osteopathic medicine. Baltimore: Williams and Wilkins, 1997.
Weinrich S., Weinrich M. Effect of massage on pain in cancer patients. Appl Nurs Res. 1990;3:140-145.
Xujian S. Effects of massage and temperature on permeability of initial lymphatics. Lymphology. 1990;23:48-50.
Yagci N., Uygur F., Bek N. Comparison of connective tissue massage and spray-and-stretch technique in the treatment of chronic cervical myofascial pain syndrome. Pain Clinic. 2004;16(4):469-474.