Chapter 5 Adaptation and sport
Sheehan (1990) has written: ‘All of us are athletes, only some of us are training and some are not’.
Hasselman (1995) notes that 30% of office visits to primary care sports medicine practices relate to muscle strain. And with ‘pain’ being the single most common symptom presented to health-care providers of all fields, it is worth reflecting that sport and leisure activity mishaps and overuse account for a great deal of that pain.
In this chapter, some important general influences of sport on the musculoskeletal system will be reviewed, as well as the relation between different types of dysfunction and specific sporting/exercise activities. It will not, however, be possible to evaluate all possible sporting influences on adaptation and dysfunction. The examples chosen are designed to provide insights into broad themes, among the most important of which is the topic of overuse in general, with specific reference to over-training in young people. ‘Young people’ in this context means those who have not yet completed their primary growing stages, with a cut-off point at approximately age 21. People differ and some continue to grow beyond that age, and certainly most continue to mature, but ossification of bones is usually complete by 21. As Hodson (1999) says: ‘Active epiphyses (growth plates) are weakest during puberty and at the end of growth, as they lose their elasticity. Bones are not fully mature until 18–21 years of age’. Examples from athletics, gymnastics and soccer, in particular, provide graphic evidence of the perils of doing too much, especially if this is too soon.
‘Too soon’ reflects the tendency for inappropriate treatment being initiated too soon after injury, before tissue inflammation has moderated and repair has consolidated. It also refers to a return to activity too soon after injury, without adequate rehabilitation. Finally, and most importantly, it refers to too much activity (training and competition) in the young, where ‘too much too soon’ can often lead to irreparable damage.
First principles
Since recovery from most minor traumas is automatic, as the self-regulating mechanisms of the body perform their roles, the practitioner’s job, in many cases, is to simply support a natural healing process, without getting in the way. In some instances, however, therapeutic interventions are essential if long-term damage is to be avoided. One of the major roles of the alert practitioner is to make a responsible decision as to when to refer instantly for clinical assessment or treatment elsewhere and/or when to introduce specific therapeutic and rehabilitation interventions within the office setting, or when matters are best left more or less alone, with simple self-help protocols explained and encouraged (ice, rest, nonstressful movement, etc.). In this chapter, the descriptions of injuries to young athletes are coupled with advice from expert sources on indicators of the existence of serious underlying damage. Such warning signs should never be ignored.
An osteopathic perspective
Allen (1997) offers an osteopathic perspective on sporting-related injuries and dysfunction, which is easily translatable into the context of other manual therapy disciplines. He starts from the principle that the human body has an inherent capacity to cope with (and successfully adapt to) most of the normal demands of the environment. However, it is necessary to recognize that:
Many factors impair this capacity and the natural tendency toward recovery. Among the most important factors are local disturbances of the musculoskeletal system. Athletes, who frequently exercise in temperature extremes and who experience profound physical stress, often sustain musculoskeletal system injuries … [which] … account for the majority of sports-related problems. However, since fewer than 5% of the musculoskeletal problems found in athletes require surgical intervention, the osteopathic physician with skills in musculoskeletal diagnosis and manipulative treatment is well-equipped to liberate the body’s [self-healing] resources.
We believe that these same skills are to be found in a broad range of practitioners and therapists within the fields of physical and occupational therapy, chiropractic, massage therapy, manual medicine and athletic training. The clinical features emphasized within this volume and its accompanying text (Volume 1) offer the tools for the successful assessment, referral, treatment and/or rehabilitation of most sports-related dysfunctions.
Feinberg (1997), a chiropractor, discusses the natural history of recovery from soft tissue injury.
The body’s response to soft tissue trauma follows a predictable sequence of events. These events have been divided into three phases: inflammatory phase, repair phase and maturation (or remodelling) phase. The timing of the three phases is generally predictable but varies with the severity, extent and type of tissue injured, as well as the age, general health, and nutrition of the athlete.
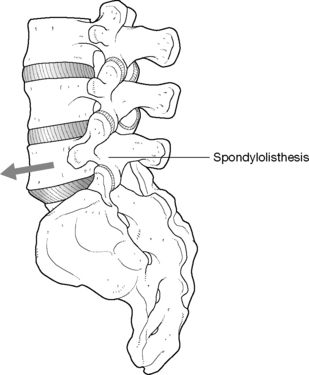
It is critical that active treatment of structures which are in a state of reorganization and repair should not be initiated too early, before there is a sufficient degree of structural integrity in the tissues. Figure 5.1 provides a schematic representation of the stages of repair, which is, of course, a generalization since some will pass through these stages more rapidly while many will be delayed in the recovery process, sometimes due to ill-advised activity or because treatment was initiated too early.
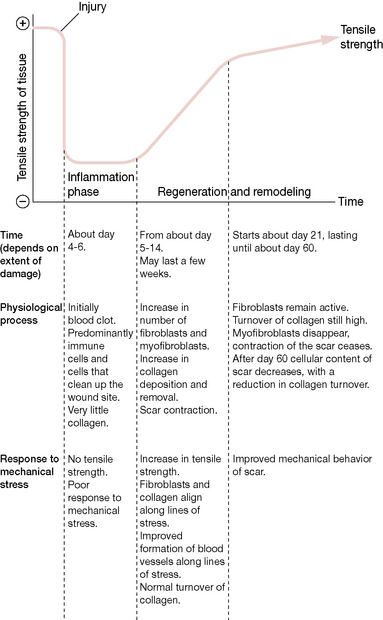
Figure 5.1 Stages of the repair process
(reproduced with permission from Chaitow & DeLany (2008) (after Lederman).
Specific adaptation to imposed demand (‘training’)
The balancing act that is necessary in sport and exercise training lies in achieving the level of appropriate (to the given sport) activity in order to maximize the training response, without overloading the adaptive potentials of the individual’s musculotendinous system.
Norris (2000) offers the mnemonic SAID (Specific Adaptation to Imposed Demand), which describes the changes that occur in the body in response to particular training and sporting activities. This mnemonic has, of course, wider implications than sports since it can be applied to any regularly performed task or activity, such as playing a musical instrument, working with a computer keyboard, mouse or trackball, using a work-or hobby-related tool (such as a paint brush, used for home improvement or artistic purposes), digging a garden or performing household activities such as vacuuming - or doing any other prolonged or repetitive activity.
This same concept of tissues ‘specifically adapting to imposed demands’ also offers the opportunity to design precise rehabilitation postures, stretches and exercises in order to encourage healthy adaptation in those structures which require stability or strength retraining. While the demanding posture cannot always be eliminated, specific strategies to counteract the effects produced by them will help to minimize the potential damage.
Evidence of healthy adaptation to exercise has emerged from research into the benefits noted in conditions as diverse as hypertension, obesity, diabetes, chronic pulmonary disease and a variety of psychological disorders (Allen 1997). However, when potentially beneficial exercise is itself misapplied, problems emerge. If training is undertaken when musculoskeletal imbalance or poor muscular coordination already exists, when the individual or the tissues being worked are in a fatigued state, if there has been inadequate rehabilitation from previous injuries, if the training approach is inappropriate or if training is being poorly applied through inadequate skill, then overtraining or ‘overreaching’ may well result.
Latent trigger points may serve as an adaptional mechanism, forming when specific demands necessitate, for instance, when additional tension is needed to stabilize a hypermobile joint. Although this offers needed assistance locally, one could question the more global consequences of such a feature. Lucas et al (2004) investigated the role of latent trigger points in altered muscle activation patterns. Looking at deficiencies in proximal segments of the upper extremity kinetic chain and whether these might be associated with changes in more distal segments in order to preserve the same movement outcome at the most distal segment, they determined that latent trigger points (LTrs) display the ability to alter the timing of muscle activation, even in muscles further down the kinetic chain. This is clinically relevant, since latent trigger points commonly present without pain. The practitioner and patient (athlete) may be unaware that they exist, although the consequences of their presence may substantially alter performance.
Training variations
There are three broad exercise areas that characterize different training variations.
• Strength training involves high-resistance, low-repetition exercise.
• Endurance training involves low-resistance, high-repetition exercise.
• Sprint training involves a combination of strength and endurance exercises.
Each variation involves different muscle fiber types. According to Ball & Harrington (1998): ‘It appears that most types of training lead to a change in fiber type towards [either] a slower isoform, e.g. Type IIb [fast twitch, fatigue sensitive] [or] Type IIa [fast twitch, fatigue sensitive] [or] Type I [slow twitch, fatigue resistant]’. (See Volume 1, Chapter 2 for discussion of muscle physiology.)
The problems that emerge from overtraining and overuse injuries have multiple predisposing causes including repetitive specific movements, often involving forces greater than those to which the tissues are normally exposed. Even though loads may be within the physiological tolerance of the tissues they are sometimes repeated so frequently as to deny the tissues adequate recovery time. Such chronic loading ‘generates a prolonged period of tissue inflammation and cellular proliferation which does not allow the maturation of injured tissues and resolution of the injury’ (Gross 1992).
Strength training
Strength training leads to an increase in muscle size due largely to increase in individual muscle fiber size (resulting from an increase in myofibril numbers within each fiber) as well as an increase in fiber numbers. There is also an increase in connective tissue (collagen) with (weight) resistance training.
The types of damage that can occur in strength training are multiple, including microtrauma (e.g. myofibrillar splitting) often resulting from concentric contractions, for example in triceps brachii (MacDougall 1986).
Excessive strength training frequently results in imbalances between opposing muscle groups as those which are being strengthened inhibit and overwhelm their antagonists. This effect is not inevitable but reflects poorly designed training programs or poor concordance by the athlete.
Eccentric exercise patterns (as in lowering weights slowly, as the arms extend) within a strength training program can cause significant tissue damage. Research has shown that z-discs (which separate sarcomeres) may be disrupted and damaged (Ball & Harrington 1998) (see Fig. 5.2).
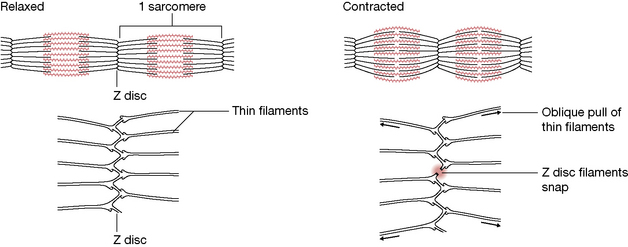
Figure 5.2 Possible mechanisms of myofibril splitting. When force development is rapid, the oblique pull of actin filaments is believed to result in splitting of Z-discs
(adapted from Goldspink (1983)).
Degenerative changes in muscle have been noted for approximately 7 days following excessive eccentric exercise (Jones & Newham 1986).
The rate at which tissue damage resolves (i.e. inflammatory phase = 4–6 days; regeneration = from approximately days 5 to 14 and lasting several weeks; remodeling phase after day 21 (see Fig. 5.1)) suggests that the recovery period following exercise-induced microtrauma, and the automatic inflammatory response that results, preclude early application of uncontrolled or aggressive stretching, frictional techniques or deep tissue work, which could delay reorganization and recovery. However, mild elongation and movement of the tissues during this phase is critical so that the connective tissue reorganizes along parallel lines rather than in random patterns that may ultimately restrict movement (DeLany 2000, Lederman 1997, Oschman 1997, Weiss 1961).
Lymph drainage techniques, which may be initiated immediately, encourage the removal of excessive fluid and waste from repair, and reduce potential damage from localized edema (Wallace et al 1997).
Endurance training
The extent to which endurance running, for example, can lead to functional regression is demonstrated by evidence that maximum peak work capacity declines by up to 50% for up to a week following running a marathon (Sherman et al 1984).
Athletes who continue to train vigorously following a marathon show a significantly slower rate of recovery compared to those who rest or who avoid demanding activity for at least a week. The sort of tissue damage that occurs involves necrosis of the muscle, thought to be caused by the significant degree of eccentric activity, especially when running downhill (Hikida & Staron 1983).
Tendon damage may result from endurance (as well as resistance) training. Ball & Harrington (1998) report that: ‘Failure to adapt to external stressors in the Achilles tendon has been characterized by degenerative changes, fibrosis and metaplastic calcification of the tendon’.
Sprint training
Sprint training frequently involves injuries to biceps femoris, semitendinosis or semimembranosus, which are all involved in the extremely rapid stretch and contraction processes involved in sprinting. Injury becomes more likely if any of a wide range of predisposing features exist and these are listed in the discussion of hamstring injury later in this chapter.
Overtraining issues
It is clear that high-intensity training can lead to physiological as well as psychological adaptations and these adaptations are not always beneficial. Detrimental training effects may result from the relative immaturity of the individual (as in the examples relating to young soccer players and gymnasts later in this chapter) or to the phenomenon of overtraining syndrome (OTS). Overtraining is a potential cause of a great many symptoms and two particular aspects of this phenomenon are explored in Boxes 5.1 and 5.2 (overtraining in female athletes and overtraining in young people). In both categories very severe repercussions can develop.
Griffin & Unnithan (1999) have evaluated the problem of the overtrained child, a phenomenon which they define as follows: ‘Overtraining has been used as a term to describe both the process of excessive training and the resulting condition of “staleness” or “burnout”.’ They note that multiple ‘positive’ and ‘negative’ factors can affect an athlete’s training state, leading to the ‘exhaustion’ phase of Selye’s adaptation syndrome (Selye 1956) (see Fig. 5.3).
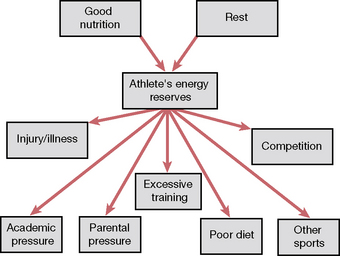
Figure 5.3 Positive and negative factors that affect an athlete’s training state
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):93).
The features of overtraining identified by Griffin & Unnithan are similar to those involved in the ‘female athlete’ discussion in Box 5.1 and include signs and symptoms to which the practitioner should be alert.
General overtraining symptoms:
• weight loss and loss of appetite
• tiredness and disturbed sleep pattern
• greater susceptibility to illness or allergic reactions
• general decline in performance during training and competition
Specific overtraining signs (Griffin 1999, Maglischo 1993):
• increased resting heart rate of 5–10 beats/min
• reduced maximal heart rate of approximately 10 beats/min
• increased exercising heart rate by as much as 24 beats/min
• increased time for heart to return to normal at rest
• increased resting blood lactate levels
• increased submaximal levels of blood lactate
• large reductions in blood lactate at maximal exercise
Symptoms such as fatigue, reduced performance, frequent infections or allergic reactions, depression, etc. should signal the aware practitioner to rapidly refer the child athlete to an exercise physiologist or other expert in the field of sports medicine for the sophisticated tests necessary to demonstrate the biochemical markers listed above.
Griffin & Unnithan (1999) note specifically that often: ‘By the time overtraining has been diagnosed it is usually too late, the damage has already been done. Training duration and intensity should be immediately reduced, but it is not advisable to stop training completely’. Stopping training for a highly motivated individual might increase anxiety and compound the problem. Weeks and sometimes months may be required to rehabilitate a chronically overtrained young athlete.
Maglischo (1993) has suggested the following principles be applied.
• 80% of training should be at basic endurance levels.
• Get sufficient rest (and adequate sleep).
• Resolve emotional conflicts that may be compounding the problem (which may involve academic pressures).
• Increase carbohydrate consumption. Research shows nutrition to be a key factor and a balanced diet containing 55–65% carbohydrate (mainly complex carbohydrates such as wholemeal bread and pasta), 12–15% protein and under 30% fat is suggested.
• Check for nutritional deficiencies, particularly iron.
• Take a 1-week break from all training if the condition is severe.
The aware practitioner should bear the possibility of overtraining in mind when faced with symptoms that alert suspicion, so that rapid and appropriate referral can be made. Such referrals might be regarding physical components, psychological elements or both. Later in this chapter, we focus on overuse injuries in relation to young soccer players. Before examining the particular stresses involved in that sport, especially when excessive competition and training is undertaken by immature individuals, it is important to distinguish between overtraining and overuse.
Overuse injuries have localized effects, as a rule, while overtraining leads to excessive generalized stress being applied to the athelete’s adaptive mechanisms as a whole. This ‘stress overload’ may reach the point of breakdown, leading to a condition that often manifests with chronic fatigue and reduced performance efficiency as key markers. Although the overtrained female and the overtrained child are the objects of attention in the surveys in Boxes 5.1 and 5.2, the background information contained in these boxes is broadly relevant to all athletes, young or adult, professional or amateur.
Overuse injuries and the young soccer player
Alan Hodson (1999), Head of Sports Medicine, Medical Education Centre, British Football Association, defines an overuse injury as ‘one which involves certain bones or muscles/tendons of the body, which develops over a period of time, due to too much repetitive activity. The injury becomes worse with continued activity at the same level’.
In effect, repetitive microtrauma continues until appropriate action is taken. ‘Appropriate’ action may involve the individual ceasing the activity that is causing the problem, because of discomfort, in which case the condition would usually be self-limiting.
This problem of overuse injury is apparently increasing markedly as playing time and training time increase, especially in relation to immature musculoskeletal systems. Gifted youngsters are asked to train and play competitively at ever younger ages, often to a greater degree than their less gifted contemporaries, leading to tragic consequences in many cases. Effective inclusion of planned recovery time within a training schedule can help to avoid such consequences.
The features that lead to overuse injuries can be summarized to include:
How widespread is the problem of overuse injury in youngsters?
There are an estimated 2.6 million emergency department visits annually in the United States for sports-related injuries in patients aged 5 to 24 years, with the highest percentage occurring in 5– to 14-year-old male athletes. (Damore et al 2003) The sports associated with the highest number of visits are basketball, cycling, football, and soccer (Burt & Overpeck 2001).
Skeletally immature athletes acquire many of the same injuries sustained by adults, but are also at risk of damaging their growth plates, apophyses, and joint surfaces. Overuse injuries represent chronic injuries related to repetitive stress on tissues of the musculoskeletal system, with insufficient recovery time, so overwhelming normal repair processes (Soprano & Fuchs 2007).
Overuse injuries in young athletes often occur when there has been a rapid increase in training, such as may occur during sports camps, or during high levels of athletic training. Extrinsic factors that may contribute to overuse injuries include the relative hardness of training surfaces, inappropriate equipment, and poor coaching (see Chapter 4, the ‘close environment’) (Soprano & Fuchs 2007).
Intrinsic factors include extremity malalignment, such as excess femoral anteversion or foot hyperpronation, scoliosis, decreased flexibility, excessive ligament laxity (see Box 1.3, Chapter 1), muscle weakness or imbalance, and female gender (Busch et al 2004).
• Clinical inquiry should focus on the location and character of the pain, the type of sport played, as well as the intensity, duration, and frequency of participation.
• Clinical examination should focus on signs of inflammation, strength, range of motion of involved joints, and movements that exacerbate symptoms, as well as overall posture and use patterns (gait, etc.).
• Treatment of overuse injuries should include relative rest, possibly confined to a decrease in the intensity and/or frequency of the suspected activity, rather than total avoidance.
• In addition, strategies to reduce inflammation, as well as to retain and regain strength, while maintaining and enhancing range of motion are required.
• In the United Kingdom, in 1992, 34 young soccer players took part in a competition to gain scholarships as part of the British Football Association’s (FA) National School of Excellence scheme. The examination of the youngsters was undertaken by the FA’s Medical Division who found that of the 34 trialists, 12 (35%) were suffering from overuse injuries.
• Five had spondylolisthesis of the lumbar spine which was potentially career threatening (Fig. 5.4).
• Two had tibial growth plate problems in the knee area.
• One had a fibular stress fracture.
• Two had Osgood–Schlatter’s disease (Fig. 5.5).
• One had Sever’s disease (osteochondrosis of the ankle area) (Fig. 5.6).
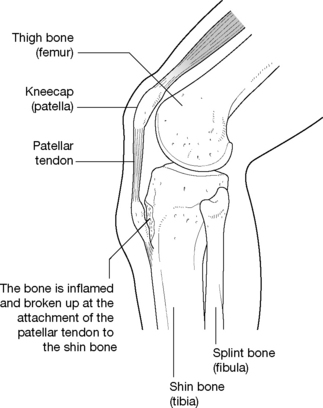
Figure 5.5 The overuse condition of Osgood–Schlatter’s disease
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):88).
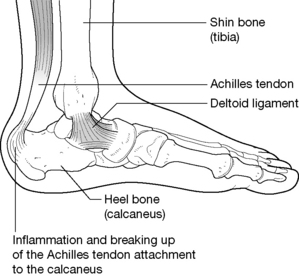
Figure 5.6 The overuse condition of Sever’s disease
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):88).
A year later, out of a different group of 36 trialist boys trying out for FA scholarships, 15 (41.6%) showed evidence of a variety of overuse injuries.
• Six had Osgood–Schlatter’s disease.
• One had a cruciate ligament problem.
• One had knee and ankle pain.
Further investigation (bone scans, MRI, oblique X-rays) involving 15 other boys from this same group of 36 showed one with spondylolisthesis and five with stress-related back injuries that had resulted in bone changes.
There is also a particular risk of avulsion injuries, as repetitive action may produce damage where powerful muscles attach to bone (Fig. 5.7).
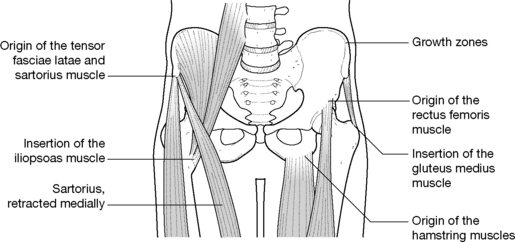
Figure 5.7 Sites of possible avulsion injuries
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):89).
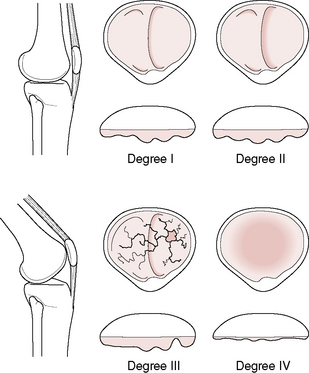
Another major risk for immature musculoskeletal systems is for damage to occur to the knee joint through overuse injury. Some conditions are relatively rare but extremely serious, such as osteochondritis dessicans, in which the articular cartilage of the joint is damaged (Fig. 5.8). Raissakia et al (2007) observe that growth cartilage, articular cartilage and apophyseal insertions are the least resistant sites to repetitive microtrauma in the immature skeleton. Tendonitis, stress fractures, osteochondritis and traction apophysitis are all examples of overuse injuries that are more prevalent in adolescents (Raissakia et al 2007).
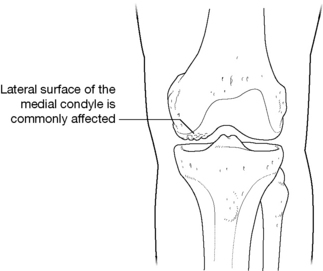
Figure 5.8 Osteochondritis dessicans
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):88).
If the articular cartilage of the patella itself is damaged the condition known as chondromalacia patellae may develop. Apart from pain in the knee, the young patient may demonstrate loss of strength and even atrophy of the quadriceps (Fig. 5.9).
Prevention of overuse injuries
Hodson (1999) provides suggestions that are summarized below as to what to be aware of and what to do if young people demonstrate signs of overuse injury. He urges therapists and practitioners to remain alert to the risks: ‘Careers can be shortened by non-recognition or poor action in the early years. It is the responsibility of the coach, manager, therapist, administrator and parent to acknowledge the particular susceptibility of young players to injury’. Benny Vaughn AT comments (personal communication 2001):
Parents, in particular, should be alert and aware and seek proper attention early on. Non-attention in the early stages is one of the biggest factors leading to permanent problems. I saw this as an athletic trainer when we would receive 18-year-old freshman (American) football players for their preseason physicals, arriving from high school where often they were not able to receive an adequate caliber of care because of financial constraints or due to just plain ignorance on the part of coaches or because they did not have a certified athletic trainer available to evaluate, prevent and treat the athletic and overuse injuries they had sustained.
Signs of overuse injury in young soccer players
• Problems usually become apparent slowly, rather than appearing suddenly, and symptoms continue when the player continues to train, rather than easing off, as would be normal for residual stiffness/discomfort related to an old trauma.
• Aching discomfort is the main symptom, usually in the area of the injury.
• Specific movements may produce pain.
• There is seldom a history of direct trauma.
• The player will frequently complain of localized aching and stiffness during or after competition or training.
• Several days may pass before these symptoms abate after a match/training session.
• Direct pressure over the injured area may be very tender.
• If the overuse injury affects a knee or ankle there may be visible swelling.
• There will often be a history of missed training sessions or matches because of the overuse injury.
• The problem persists and worsens with continued training.
• If symptoms such as these are present in a young active athlete, medical advice should be sought from someone active in sports medicine, so that a suitable course of action can be formulated. It is worth emphasizing that overuse patterns such as those described are a likely predisposing feature of the evolution of myofascial trigger points, which are commonly involved as part of the symptom picture of overtrained individuals, as in all overuse syndrome patterns (Simons et al 1999).
Handling overuse injuries
• Signs and symptoms of pain, such as swelling, tenderness and aching, should never be ignored as they represent the body’s response to a problem; if addressed early, intervention might prevent the termination of a promising career.
• The number of training sessions and competitive events should be limited to what is thought to be a safe level based on the age and the physical demands involved, in consultation with experts in the sport.
• The activities involved in training and playing soccer, or any sport, should be directed as much at enjoyment as at ‘success’.
Appropriate treatment and rehabilitation protocols should be initiated to prevent minor problems becoming chronic. A number of such protocols are described throughout the clinical applications chapters of this book and its accompanying Volume 1 (upper body).
Tibial stress fracture
A stress fracture involves a hairline or very thin, partial or complete fracture of a bone as a result of its inability to withstand the imposition on it of rhythmic, repetitive, submaximal forces over time. Most research into stress fractures has involved athletics and the military so there is little reliable data as to the frequency of stress fracture in the general population. The incidence of stress fractures is reported to make up 10% of all sports-related injuries (Matheson et al 1986).
McBryde (1976) reported that 95% of all stress fractures in athletes involve the lower extremity, with the upper third of the tibia (the site of approximately 50% of all stress fractures seen in adolescents), the metatarsals and the fibula being the most common sites. Causes can include:
• sudden increases in training or activity
• inappropriately hard playing or running surfaces
• nutritional and/or menstrual status. (Lloyd & Triantafyllou (1986) report that deficiencies of calcium and other nutrients in the diet of amenorrheic gymnasts, ballet dancers and female distance runners contribute to stress fractures occurring due to loss of bone density. See also Box 5.1 on overtraining issues in female athletes.)
Box 5.1 Overtraining and the female athlete
In relation to the female athlete, Birch & George (1999) report that:
There is so much individual variability in the physiological and psychological responses to overtraining (OT) that diagnosis has been nigh on impossible. The most obvious and consistent markers of OT are high levels of fatigue and performance decrements; however, how much fatigue and how much performance decrement represents the OT syndrome is highly arguable.
Other features and markers that suggest the possibility of overtraining syndrome include: weight loss, increased or decreased heart rate at rest (depending on whether sympathetic or parasympathetic dominance exists), disturbed sleep, decreased appetite, emotional instability, increased or decreased resting blood pressure (sympathetic/parasympathetic), hypoglycemia following exercise, lethargy and/or depression. There is commonly an increase in upper respiratory tract infections associated with overtraining (which might reflect either volume or intensity of training) (Heath et al 1991).
Endocrine imbalance
Many of the symptoms of OTS apply equally to male and female athletes and both genders have been shown to demonstrate endocrine imbalances as part of the syndrome. In males this may manifest as an altered testosterone:cortisol ratio, which may produce alterations in the reproductive system. However, it is the incidence of ‘secondary athletic amenorrhea’ that has attracted the greatest attention as a symptom of OTS. This condition is defined as absence of menstruation for 6 months or more following at least a year of normal menstruation. Amenorrhea affects approximately 5% of the general population but has been reported to reach an incidence of 40% among female athletes (Bullen et al 1985).
Athletic amenorrhea is reversible, usually by the simple expedient of reducing training schedules by 10% or so. Recovery usually takes 6–12 weeks and Budgett (1990) recommends that this period should include: ‘rest, relaxation, massage, hydrotherapy, good nutrition and light exercise, with particular care over calcium intake’. If amenorrhea persists medical advice should be sought.
Associated effects of endocrine imbalance that leads to amenorrhea include increased levels of low-density lipoproteins, which have been implicated in cardiovascular disease, and also bone mineral density reduction, leading to the possibility of increased stress fractures and possibly osteoporosis later in life (Constantini 1994).
Preventing overtraining in the female athlete
A variety of preventive strategies have been suggested (Fry et al 1991, Keen 1995, Prior & Vigna 1992) including:
• training programs should allow adequate recovery and regeneration time
• there should be monitoring for OT symptoms during the training program
• normal fatigue that results from vigorous exercise should not be confused with unnatural fatigue
• intensive training in short bursts with sudden increases in training load should be avoided
• diet should contain at least 55% carbohydrates and female athletes should consume not less than 1500 mg calcium daily.
There are two types of stress fracture.
• A fatigue stress fracture is caused by repeated abnormal muscular stress (or torque) applied to normal bone that has appropriate elastic resistance potential and density.
• Insufficiency stress fracture is caused by normal muscular forces applied to mineral-deficient or abnormally inelastic bone (Van Der Velde & Hsu 1999).
Just as in any form of applied stress to tissue, an adaptive process ensues. With training, these processes accelerate but if the remodeling (adaptive) response fails to keep up with the training demands, a stress fracture will occur.
Diagnosis
Clinical diagnosis of stress fracture requires considerable skill and patience and usually requires radiographic evidence, although this is not always conclusive. Van Der Velde & Hsu (1999) report that:
Although periosteal elevation or sclerosis may be apparent 2–3 weeks after the onset of pain, significant changes may not be evident on radiographic film for up to 3 months after the onset of symptoms. Radiographs have a very poor sensitivity, estimated to be as low as 15% in the early stages of stress fractures.
(Author’s note: however, scan images readily show evidence of stress fractures.)
Clinical clues and signs of stress fracture
• Pain that usually started gradually (sometimes suddenly) shortly after an abrupt alteration in intensity or activity.
• Pain that is increased by activity and decreases with rest.
• Pain that usually commenced as a dull ache after activity and then eased, but which over time persists for longer periods after activity until it becomes more or less constant.
• Eventually the pain may localize to the fracture site and may be present at night during rest.
• Examination offers few clues but localized tenderness, warmth, possibly discoloration and swelling may be noticed over the site. Direct palpation of the bone over the fracture site is likely to produce an exquisitely painful response.
• A slight thickening may be palpable on the periosteum.
• Application of ultrasound may produce pain and this sign is used diagnostically by some practitioners.
Treatment
• Treatment necessitates a cessation (or drastic modification) of stressful activity in order to allow repair to take place.
• Removal of stressful activity does not mean that the individual should not continue to walk around normally during rehabilitation. However, if after several days of reduced activity, pain has not reduced considerably, total immobilization may be required for a period of several days.
• Therapeutic application of ice massage, electrotherapy and the use of anti-inflammatory medication may prove helpful.
• Exercises that stretch and strengthen the limb are advocated.
• Non-impact activities such as swimming and cycling may be useful to help maintain cardiovascular fitness during the recovery period, which usually takes 4–6 weeks, after which a graduated return to training should be possible, as long as pain is no longer a feature.
• Factors contributing to the initial injury should be assessed and appropriate action taken to avoid repetition.
Enhanced human performance or treatment of dysfunction?
For the elite top-level athlete, whether professional or amateur, an injury or dysfunction that would be considered relatively unimportant to a sedentary non-athlete may assume great importance, especially if it impacts on performance potentials. Vaughn (1998) has made the distinction between the objectives of those practitioners working with athletes whose focus is on producing optimal, injury-free performance, as compared with those practitioners whose objective is the recovery of function following injury.
In top-level athletics a degree of muscular fine tuning and joint efficiency that allows for a gain of one-hundredth of a second in sprint time may make the difference between winning a gold rather than an ‘alsoran’ medal. The objectives are different and the interpretation of injury has a very different significance for the athlete as compared to the non-athlete, where discomfort or restriction may represent no more than an annoyance rather than an obstacle to the realization of long-held ambition.
Athletics
Unless long-distance runners introduce crosstraining in flexibility, there is a danger of patterns of imbalance becoming chronic. Watkins (1996) reports: ‘Low back pain as well as interscapular and shoulder and neck pain are commonly reported by runners’. Fortunately, regular stretching can usually keep symptoms at bay but this does not necessarily provide the balance and stability required to avoid long-term problems.
Abdominal weakness is not uncommon, as are flexor/extensor imbalances in the legs and trunk. Such imbalances are likely to involve some muscles being shorter and tighter than is optimal, with inhibition of their antagonists, altered muscle-firing sequences and joint instability as a result. Refer to Volume 1, Chapters 4, 5 and 6 for a detailed account of the evolution of soft tissue dysfunction involving this common sequence of changes (tight, inhibited, uncoordinated soft tissues and joint instability) (see also the Essential Information material at the beginning of this volume).
Within these structures, myofascial trigger points will inevitably evolve, to add to the physiological mayhem. Treatment and rehabilitation strategies for such patterns of dysfunction are to be found throughout the clinical applications chapters of this text and its companion volume.
Watkins suggests various preventive and rehabilitation strategies for runners with back pain, including:
• vigorous stretching of lower extremities and trunk muscles
• crosstraining and muscle-strengthening techniques which strengthen antagonists, for example, hip and knee extensors
• strengthening programs for the abdominal group using isometric stability exercises
• exercises that enhance maintenance of a ‘chest-out’ posture
• use of appropriate footwear to ensure cushioning and good foot function.
Hamstring injuries and the athlete
A common athletic injury involves damage, often a rupture within the musculotendinous unit, of biceps femoris, semitendinosus or semimembranosus, resulting from violent stretch or rapid contraction. Some possible predisposing factors to a hamstring injury may include poor flexibility, fatigue, unbalanced reciprocal actions in opposing muscle groups, imbalance between quadriceps and hamstring strength (normal ratio is 3:2), inadequate warm-up before the sporting activity, presence of active trigger points within the hamstring muscles (or the antagonists), restrictions in associated joints, presence of fibrous (scar) tissue within the muscles from previous, unresolved injury, etc. (Kulund 1988, Sutton 1984, Vaughn 1996).
Reed (1996) maintains that weakness in the hamstrings is a predictor of injury. He states:
It has been demonstrated [byTidball 1991] that hamstring muscles are subjected to high forces during both open and closed kinetic chain activities of sprinting. Thus a stronger hamstring can absorb greater forces. The mechanics of injury often involve a quick explosive contraction of hamstrings while the hip is in flexion and the knee extended. Additionally certain situations will generate the forces necessary to produce injury to the sacroiliac ligaments; sudden violent contraction of the hamstrings is one of these forces.
It is easy to see how a powerful quadriceps group could cause the hamstring to contract against an (almost) unyielding force when the knee is locked in extension in this way, resulting in tissue damage.
A range of other biomechanical features could predispose to hamstring injury, including the medial hamstring being excessively tight and so producing internal thigh rotation and a toe-in gait pattern; or the ipsilateral ilium could be posteriorly rotated, producing altered leg length and uneven stress on the hamstrings; or relative hamstring weakness could allow the ipsilateral ilium to rotate anteriorly, altering biomechanical balance; or the injury site may relate to an unresolved dysfunction elsewhere in the kinetic chain.
Feinberg (1997) provides a graphic example of such a long-distance influence when he describes the ‘Dizzy Dean syndrome’.
Dizzy Dean was a professional baseball pitcher during the 1930s. During an all-star game his foot was hit by a line drive, fracturing his toe. He was subsequently given an oversized shoe so that he could continue to play. Although he was able to pitch, an abnormal alteration in the function of his kinetic chain resulted in a shoulder injury that ended his career. Thus, a change in one part of the kinetic chain produced dramatic effects at another part of the chain.
The concept of a kinetic chain necessitates keeping in mind the relationships between whatever local dysfunctions are identified and all the other structures involved in the total function being performed. Thus in the baseball pitcher’s case the entire wind-up and release of the ball creates a series of interacting processes involving the entire body, from the feet through to the hand that is holding and eventually throwing the ball. In the case of a hamstring injury, the kinetic chain would depend upon the action being performed. The activity of sprinting clearly involves everything from the toes to the spine, as well as much of the trunk and upper extremities.
How to choose where and what to treat within the kinetic chain
The concept of a kinetic chain commonly being involved in a local dysfunction, such as an injured hamstring, allows the practitioner to explore the possibilities as to what might be influencing the tissues in question.
• Is there weakness or imbalance, for example between hamstrings and quadriceps? Functional tests (see Chapter 3) can often offer information regarding over-activity in the hamstrings and an imbalance between these and the gluteals in, for example, the hip extension test.
• Is there relative shortness of any of the muscles (for example, in the hamstrings) associated with the activity (sprinting in this case) that resulted in injury? Straight leg raise tests will provide evidence of this (see description on the next page).
• Is there an associated joint restriction, particularly involving knee, hip or pelvis? Motion palpation and assessment would offer evidence of this (see Chapter 11).
• Are there active trigger points present in the muscles associated with the injury? NMT evaluation would provide evidence of this.
• Are posture and gait normal? See Chapters 2 and 3 for full discussion of these key functional features.
By broadening the investigative process to include the entire kinetic chain, the practitioner opens herself to therapeutic possibilities that a local focus would limit. It is recommended to have in place a referral network when evaluation presents possible dysfunctions that lie outside the scope of practice, training or expertise of the practitioner.
A model of care for hamstring injuries
Reed (1996) provided a detailed and clinically useful model for assessment of the hamstrings. It is presented below, slightly modified, as an indication of the width and breadth of assessment necessary to make sense of even an apparently ‘simple’ injury.
The physical examination of the athlete with an injured hamstring starts with a postural screening. Examination of the patient should begin with the observation of the patient’s posture standing, sitting and lying down. Observing the patient’s movement from sitting to standing, or other alterations of position is [also] important.
Posterior aspect of body
• Is there evidence of (abnormal) foot inversion or eversion?
• Are there any abnormal muscle contractures of the legs?
• Is there rotation of the entire pelvis in relation to the trunk?
• Does one iliac crest flare more than the other?
• Does palpation of the greater trochanters reveal that one femur is more laterally or medially rotated than the other?
• Is there an increase or decrease in the lumbar area, i.e. is the lumbar curve flat or exaggerated?
Lateral aspect of the body
• Has there been anterior or posterior rotation of the pelvis?
• Is there an increase or decrease in lumbar lordosis?
Reed (1996) then suggests:
Examination of the hamstring includes placing the athlete in a supine position and performing straight leg raise, noting the position of pain or painful arc. This should be performed bilaterally. While the athlete is still supine, the hip should be flexed to 90° with the knee flexed. With the foot in a neutral position, the knee is then extended to the point of pain. This test is repeated with both internal and external tibial rotation. Internal tibial rotation will place more stretch on biceps femoris. External tibial rotation will place a greater stretch on the semimembranosus and semitendinosus. Once again, there should be bilateral comparison. The area of pain should be noted and followed by palpation of the area. Palpation is important to determine if there are any defects in the muscle. Palpation should be performed with the athlete’s thigh in a position of comfort… The thigh should also be observed for haematoma. This may not be present initially, but may take several days [to emerge].
Protocols for treatment of this type of injury will be found in the sections of this text that cover the muscle(s) in question. However, the broad advice would be to encourage healing during the early stages by use of lymphatic drainage methods and hydrotherapy (such as contrast bathing and ice massage, which can be usefully applied as home care) as well as mobilization of associated soft tissues and joint structures, while avoiding direct treatment of inflamed tissues. Deactivation of associated trigger points should be considered. Early non-painful use of the limb is advisable, avoiding any tissue stress (although immobilization should be avoided if at all possible); isometric contractions of antagonist muscles can be usefully employed to release (through reciprocal inhibition) hypertonicity in damaged tissues when they are too sensitive to work on directly (DeLany 1996). Positional release methods (as described in the clinical application chapters of this text and its companion Volume 1) can be applied directly to traumatized tissues without fear of retarding tissue recovery (Chaitow 2007, Deig 2001, Jones 1995).
Nutrition
Although antiinflammatory medications and strategies should be carefully moderated to avoid interfering with this essential part of the healing process, Werbach (1996) reports that citrus-based bioflavonoid supplements can reduce recovery time from muscle strains and other sports injuries. He cites a study (Broussard 1963) involving 48 American football players who received 600 mg citrus bioflavonoids before lunch and 300 mg before suit-up time. When muscle strains occurred during the game, the average recovery time was 18.9% longer for the players who had received a placebo instead of the bioflavonoids. Werbach also reports on the value (in reducing and resolving bruising damage) of pineapple enzymes (bromelain) or papain enzymes (from unripe green papaya fruit) in doses of 400–500 mg three times daily away from mealtimes.
Bodywork and rehabilitation
While waiting for local healing to progress, therapeutic attention should be given to any dysfunctional muscles or joints within the kinetic chain that showed up during the assessment summarized previously. Once the initial stages of the healing process have passed (probably not less than 2 weeks post injury) strengthening and endurance of the traumatized tissues should be encouraged by carefully designed exercises. At the same time, appropriate non-traumatizing soft tissue technique application should start, aiming first to prevent adhesion formation (including mild deep tissue work and light transverse friction). Following this, light functional activity and skill reacquisition should commence before a slow return to the demanding environment of the main athletic activity.
Note: See also the information regarding the intimate relationship between hamstring function and the SI joint, which is discussed in both Chapter 11 (The pelvis) and Chapter 3 (Gait analysis) (Fig. 5.10).
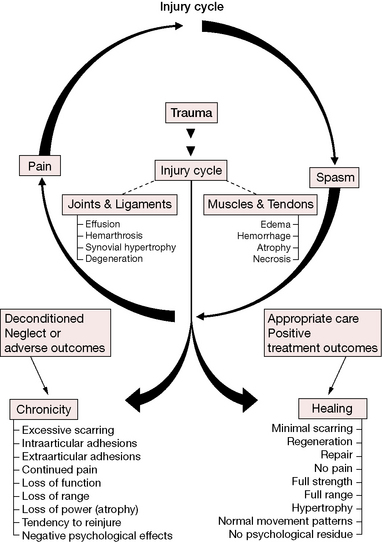
Figure 5.10 Schematic representation of the injury cycle. At least part of this widely held theory (‘pain–spasm–pain cycle’) is assumptive and is discussed as hypothetical by Mense & Simons (2001)
(reproduced with permission from Chaitow & DeLany (2008)).
Groin strains and the athlete
Groin strains involve the adductor group of muscles (adductors magnus, longus and brevis, as well as gracilis and pectineus). These muscles arise from the pubic bone and inferior ramus of the pubis to attach (for the most part) to the linea aspera (Fig. 5.11). These muscles have been shown, in Chapter 3, to be significantly involved in walking and they are also major players in the process of running and in most other sporting activities. Pelvic obliquities and other pelvic structural distortions can also be connected to shortness in adductor muscles (see Chapter 11).
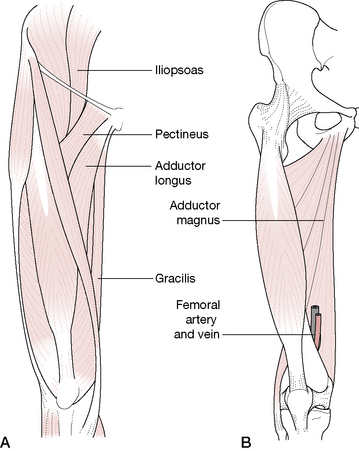
Figure 5.11 A: superficial adductors of the thigh. B: Deeper view of thigh adductors
(reproduced with permission from Journal of Bodywork and Movement Therapies 2(3):140)
The patient who reports internal thigh and inguinal pain following a strained movement may well have nothing more sinister than a groin strain. However, as Newton (1998) reminds us:
In many cases there may be chronic joint and/or soft tissue conditions which predate the presenting acute symptoms to the adductor region. They could also have predisposed the patient to injury and could lead to reinjury if not countered. Examples of two such conditions are hypomobility of the hip, and inguinal disruption [also known as a ‘sports hernia’ or ‘Gilmore’s groin’].
See Box 5.3 for details of this condition.
Box 5.3 Gilmore’s groin, sports hernia or inguinal disruption (Newton 1998)
A common cause of groin pain, particularly related to field sport injuries, involves damage ‘to the external oblique aponeurosis, dilation of the superficial inguinal ring, a tear of the conjoint tendon and a dihiscence between the inguinal ligament and the conjoint tendon’ (Newton 1998). The pattern of pain is of severe localized pain that may radiate to the medial thigh via the groin (see Fig. 5.12).
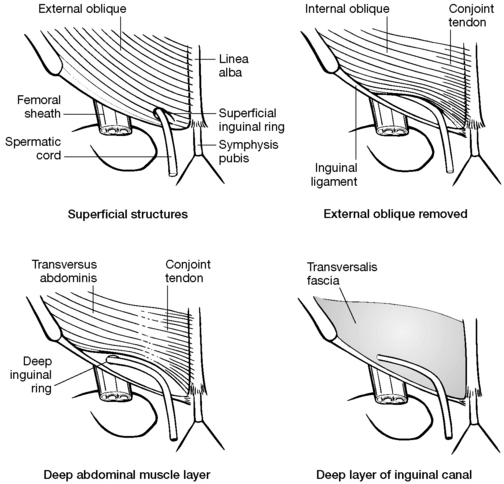
Figure 5.12 A: Superficial structures. B: External oblique removed. C: Deep abdominal muscle layer. D: Deep layer of inguinal canal
(reproduced with permission from Journal of Bodywork and Movement Therapies2(3): 137).
The diagnosis is arrived at by a process of eliminating all other possible causes of pain in the area, as there are no definitive tests for this form of dysfunction.
• Restricted (hypomobile) spine and ipsilateral hip.
• Pain aggravated by cough or Valsalva maneuver.
• Pain aggravated by resisted (by practitioner) supine double straight leg raise. If the superficial inguinal ring is simultaneously palpated, a severe local (and sometimes referred) pain to the groin area may be reported.
With muscular injuries, suspicion is raised by reported pain symptoms that involve areas other than the relatively localized sites that would be expected from a purely muscular strain. Pure groin muscle strain commonly presents with symptoms such as:
The patient should be able to make a strong (but painful) contraction of the muscle. If only a weak contraction is possible the damage may be severe or there may be a neurological factor involved.
Clues as to whether the condition is a simple strain or a more complex condition may be suggested by discovering whether or not a cough aggravates the pain. If it does, the condition is unlikely to be purely groin strain and possibly involves abdominal muscle attachments in the same region. Alternatively, if the patient reports an aching and stiff hip as part of the symptomatology, a hip restriction (hypomobility) should be suspected.
All such suspicions should then be assessed by specific tests that include evaluating whether there is pain on palpation or whether the symptoms are aggravated by stretching and/or contracting the suspect muscles. Further differential assessment is also necessary as a number of other muscles (notably sartorius and iliopsoas), as well as various pathological conditions, can produce pain in the groin area.
Renstrom (1992) lists the following non-musculoskeletal conditions that need to be eliminated as possible causes of groin pain.
It should also be noted that lymph nodes of the inguinal region may be enlarged due to infection in the lower extremity or abdominal region or due to the presence of lymphatic cancer. If these enlargements are found, the practitioner should refer immediately for evaluation and under no circumstances should the lymph nodes be squeezed, irritated or drained until conclusive evidence determines the cause of the lymph swelling (see also Chapter 12).
Beam (1998) refers to Hasselman (1995) when he reports: ‘Pain in the adductor region can originate as referred pain from pathology in the abdomen, hip joint, sacroiliac joint, symphysis pubis or rectus abdominis’. Trigger points in adductor longus, multifidi, the lower lateral abdominal wall muscles (such as external oblique) or on the superior border of the pubis can all produce pain referrals into the inguinal region and also to intrapelvic regions (Simons et al 1999, Travell & Simons 1992) (Fig. 5.13).
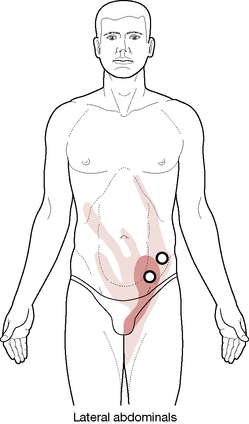
Figure 5.13 Trigger points in the lower lateral abdominal wall muscles (such as external oblique, shown here) can all produce pain referrals into the inguinal region
(adapted from original illustration by Barbara Cummings, with permission, from Simons et al (1999)).
Details of appropriate palpation, as well as assessment (and treatment) protocols are found in Chapter 12, which discusses the hip and its dysfunctions. Pain patterns are shown here in Figures 5.14 and 5.15.
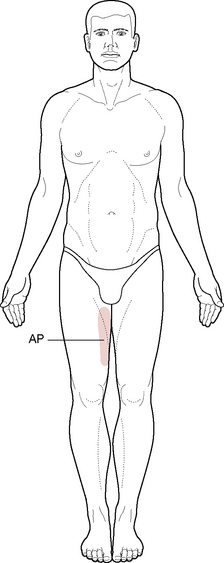
Figure 5.14 Adductor pain (AP) is a common symptom area caused by an adductor strain or by trigger points in adductor muscles
(reproduced with permission from Journal of Bodywork and Movement Therapies2(3): 135).
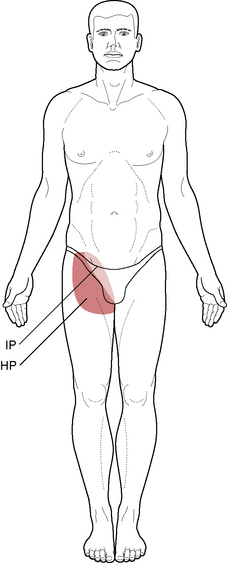
Figure 5.15 Inguinal pain (IP) is a common symptom area caused by inguinal disruption. Hip pain (HP) is a common symptom area caused by the hip joint and by hypomobility
(reproduced with permission from Journal of Bodywork and Movement Therapies2(3): 135).
The wide range of possibilities touched on in this brief discussion of groin strain indicates the need for care and diligence when confronted by an apparently simple ‘sports injury’. Nothing should be taken at purely face value. A thorough evaluation is always necessary if potentially serious associated conditions are to be discovered or ruled out.
If the diagnosis is of a simple musculotendinous groin strain, the objectives of treatment will be restoration of full flexibility, strength and control of the hip musculature in general and the adductors in particular. This will usually involve a great deal of self-applied, and very specific, stretching and toning.
Gymnastics and dance
Excessive lumbar lordosis is a common feature in dancers and gymnasts (especially juvenile) and is not uncommon in power athletes such as sprinters and jumpers. This can lead to high pressure forces being applied to the facet joints and to alteration in disc function. The facet joint stresses are compounded by the effects of jarring impact forces, following jumps. The muscular repercussions of exaggerated lumbar lordosis are seen in the lower crossed syndrome pattern (Janda & Schmid 1980), which is discussed and illustrated in Chapter 10. In the ‘crossed’ pattern the lumbar erector spinae progressively tighten and shorten, as do the hamstrings, while the abdominal and gluteal muscles are inhibited and frequently lengthened (Jull & Janda 1987, Norris 2000) (see also Volume 1, Chapter 5). Lewit (1985) is explicit:
Gymnastics as usually taught makes muscular imbalance even worse, particularly in exercises in which the trunk and the legs are held straight and at right angles to each other. In order to achieve this, the action of the abdominal muscles naturally approaching the sternum to the pubic symphysis must be overcompensated and inhibited by the erector spinae and the iliopsoas – the best way to provoke the ‘lower crossed syndrome’.
Lewit suggests that the leverage that such activities create puts stress on the lumbodorsal junction and endangers the discs of the region.
Apparatus-focused gymnastics also creates imbalances according to Lewit’s analysis, particularly involving the upper fixators of the shoulder. The speed of change of direction of movements on gymnastic apparatus adds to the chance of injury. Lewit’s remedial approach includes slow movements, such as those used in classic yoga and tai chi, and general recommendations for healthy physiological and safe exercise include walking, dancing and cross-country skiing, which: ‘has much in its favour. It makes use of all four limbs, and the snow provides a soft terrain’.
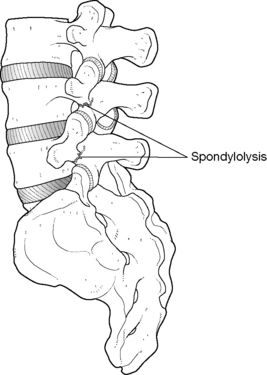
Watkins (1996) suggests that gymnastics is the sport most connected with lumbar spinal injuries. The frequency with which young soccer players display dysfunction, as evidenced by Hodson (1999), highlights just how dangerous these sports can be to the immature spine. Particular blame for spinal damage in young gymnasts has been attached to activities such as the hyperlordotic positioning involved in back walkovers, flips and vaulting dismounts. A common injury involves fatigue fracture of the neural arch (‘Scotty dog’ fracture or spondylolysis) (Hensinger 1989), for which there is an 11% reported incidence in female gymnasts, according to Jackson (1979).
Enhanced trunk strength can reduce these risks and appropriate exercises to help achieve this objective are now widely encouraged in gymnastic training (Garrick & Requa 1980). The frequency of spinal injury in gymnasts can be compared with the results of a Polish study, involving 289 young athletes aged between 14 and 25 years, which showed that over 5% had spondylolysis (see Fig. 5.16) and over 2% had spondylolisthesis (Marciniak 1998). Spondylolysis commonly presents with low back and referred pain (to varying sites depending on the level involved), as well as paraspinal muscle spasm.
Restoration of stability of the low back requires recruitment and training of the deep abdominal support/stabilizing musculature as well as restoration of the pelvic tilt toward normal. Rehabilitation guidelines will be given in Chapters 10 and 11 which, together with appropriate manual therapy, can assist in achieving these goals.
Dancers and gymnasts whose training and activities involve a variety of multijoint exercises in which the body itself provides resistance have been shown to have enhanced proprioception, rapid muscle reaction speed and kinesthetic sense (Lephart & Fu 1995) that usually allows rehabilitation procedures to be speedily learned and applied.
Ballet creates many of the same stresses as those occurring in gymnastics, particularly in performance of arabesques in which extension and rotation of the lumbar spine is required. Additional stresses are involved in turned-out leg positions, off-balance bending (where balance must be precisely maintained) and the lifting of other dancers, often in unusual positions. Both spondylolysis and spondylolisthesis are more common in ballet dancers than the general population.
Breakdance activities, where training is often unsupervised and self-initiated, are, if anything, potentially more stressful to the spine and extremity joints than ballet movements, with head-spins providing the ultimate in cervical stress.
High-impact landing occurs in both dance and gymnastic settings and Schafer (1987) reports that while the ankle and foot are commonly considered the main sites of injury in dance, the hip, knee, leg or spine may all be involved. ‘In trained dancers, faulty technique appears to be the [most] common cause of injury’.
Details regarding therapeutic effects offered by the Pilates principles of exercise, (Figs. 5.17 and 5.18) as well as proper sequencing required in non-operative care of athletic injuries in general, can be found in Boxes 5.4 and 5.5, respectively.
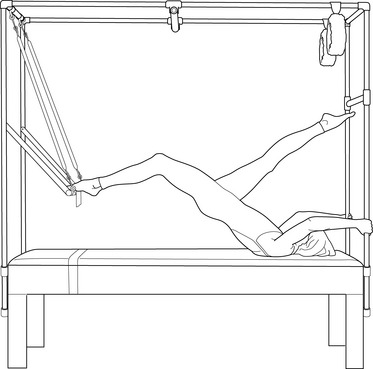
Figure 5.17 Pilates equipment (trapeze table) being utilized by a dancer to enhance awareness of correct hamstring and hip extensor activation, while maintaining core control and spinal stability
(adapted from Journal of Bodywork and Movement Therapies 4(2):103).
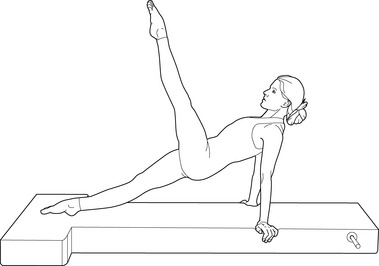
Figure 5.18 Pilates mat exercise in which deep abdominal, spinal and posterior shoulder girdle stabilizing muscles are activated during controlled hip flexion
(adapted from Journal of Bodywork and Movement Therapies 4(2):104).
It is not surprising that exercises which encourage both strength and suppleness are popular in the dance community, based to a large extent on Pilates principles. Lange et al (1999) have reviewed the current availability, claims and methodology of ‘Pilates-inspired’ exercise programs.
Pilates was influenced by hatha yoga, gymnastics, modern dance and other movement systems … His exercises have been further influenced by fields as diverse as physical therapy, somatics (e.g. Feldenkrais Method™Body/Mind™ Centering™Bartenieff Fundamentals) and Chinese medicine.
Not surprisingly, with current Pilates-inspired practice emerging out of this eclectic background, there is no such thing as a standardized set of ‘pure Pilates’ exercises. This is why Lange et al speak of ‘Pilates-inspired’ (PI) exercises. They define the learning goals of PI practitioners as follows.
• Clients should learn to ultimately perform the PI exercises without the practitioner’s corrections and support.
• Breathing, core control, body awareness and coordination learned through PI exercises should be transferred to functional (everyday) tasks.
• The way PI exercises are taught should be structured to encourage retention and transfer of the motor skills acquired through exercising under supervision.
How successful PI training is in achieving these goals seems to be an open question. Lange et al report that:
Only a small number of published experimental studies document measured improvements in posture, or functional tasks, that are unequivocally attributable to PI exercises (Parrott 1993, Fitt et al 1994, Krasnow et al 1997, McMillan et al 1998). Roughly an equal number of studies also report the failure of PI exercises to elicit improvements (Fitt et al 1994, Krasnow et al 1997, McClain et al 1997). Despite the lack of supportive, research-based data on PI exercises, anecdotal reports by practitioners and clients indicate that significant benefits do indeed exist.
The key to successful teaching of PI exercises may well lie in adequate standardization of training for instructors, which is not yet established.
Watkins (1996) summarizes the therapeutic sequence required in non-operative care of athletic injuries in general, once inflammation has ceased (remembering that inflammation represents the initial repair response and is a necesssary phase of healing) (see Volume 1, Chapter 7).
• Restore aerobic conditioning.
• Restore balance and coordination.
• Adapt the rehabilitation approach to meet the specific needs of the sport in question.
Some practitioners may be unable to fulfill the specific rehabilitation requirements of particular sports but most should be capable of assisting in the restoration of strength and flexibility and guiding the athlete/patient in protocols for achieving aerobic conditioning and coordination (see Chapter 3).
Weight training and the low back: key points (Norris 2000, Watkins 1996)
Appropriate weight training has value in recovery from back problems, particularly if the individual’s normal occupational or sporting activities involve lifting or working against resistance. Inappropriate weight training can make back problems much worse.
While weight training can enhance the stability achieved following the diligent application of carefully crafted rehabilitation (to gain stability and strength) exercises, it is an inappropriate activity if thought of as a replacement for such exercises.
Norris (2000) suggests:
Weight training has several important advantages for those with lower back problems. First, it can increase limb strength that some people need. Second, it can further enhance trunk muscle strength/stability to the level often required in sports – especially contact sports where abdominal strength can have protective function for the internal organs. Finally, weight training can help to guard against further back injury.
The three phases of weight lifting require different muscular skills and activities: concentric contraction for lifting, isometric for holding steady and eccentric for lowering. If the lift is snatched and the descent is achieved by dropping the weight, two of the phases will be neglected and stability will not be achieved. A ratio of 3 seconds to lift, 2 seconds to hold and 4 seconds to lower is suggested (Norris 1995).
Errors made during weight training can result in severe injury. Common errors include: weights not being controlled throughout, which can lead to traumatic or overuse injuries; weights should not be too heavy for the individual to easily control or compensating bodily misalignments are likely to lead to strains and/or injury; pain as a signal that all is not well should never be ignored during lifting.
Watkins (1996) reports that: ‘the incidence of lower back pain and problems in weight lifters is estimated to be 40%’. Additional statistics show that the incidence of spondylolysis in adult, competitive weightlifters is estimated at 30% and spondylolisthesis at 37% (Aggrawal 1979, Kotani 1981).
Watkins suggests that the most dangerous time during the lift is when there is a shift from spinal flexion to extension as the weight is taken over the head. This transition should be made with ‘tight’ muscle control, using the lumbodorsal fascia. Watkins maintains that by including in a weight-training program general body conditioning, flexibility, aerobic conditioning, speed and crosstraining, injuries would be drastically minimized.
Note: The lifting methods that were analyzed in relation to the descriptions above relate to competitive, professional or Olympic standard training and lifting and not to the relatively safe (if supervised) approaches available in health clubs, fitness centers and gyms.
Key guidelines for successful weight training include:
• ensure equipment is adjusted to individual needs (height, weight, etc.) before starting
• avoid loose clothing, use appropriate footwear and tie back hair (if long)
• be aware of body alignment throughout
• stabilizing the low back by means of abdominal hollowing when lifting, holding and lowering weights
The Valsalva maneuver (breath holding during lifting or bracing) carries with it particular dangers for those with high blood pressure (Linsenbardt et al 1992). This maneuver is appropriate for very short periods, during heavy weight lifting, if the individual’s cardiovascular status is sound (and is used by virtually all professional weight-lifters in competitive and training settings). The caution regarding blood pressure elevation applies to those using weight training for rehabilitation or fitness purposes, who should avoid holding the breath during such activities. Learning to ‘hollow the abdomen’, while at the same time continuing to breathe normally, is a useful tactic as this recruits the transversus abdominis (spinal support) and pelvic floor muscles. This will be described in Chapter 10, which discusses low back issues.
Water sports
Anyone who has ever swum a pool length performing the butterfly stroke will remember the phenomenal stresses imposed throughout the body. To a lesser degree, all swimming strokes inflict specialized loads and therefore evoke specific adaptation responses. Watkins (1996) comments on two of these.
…certain kicks, such as the butterfly, produce vigorous flexion/extension of the lumbar spine, especially in young swimmers. The swimmer must attain good abdominal tone and strength in order to protect his or her back during vigorous kicking motion. Thoracic pain and round back deformities in young female breast strokers can be a problem, because of the repeated round shoulder-type stroke motion.
Lewit (1985) comments on his perception of the risks attached to swimming.
The breast stroke and even the crawl make the pectoralis muscles overactive and taut, so that most swimmers become round-shouldered. On the other hand, the breast stroke and even more the ‘butterfly’ produce lumbar hyperlordosis and hypermobility. In the older age groups most people hold their head out of the water while swimming, keeping the cervical spine in hyperlordosis.
Lewit encourages swimming as a potentially healthy activity but recommends swimming on the back and mentions that crawl offers the least stress for the low back compared with other face-down strokes.
Similar (to butterfly stroke) flexion/extension actions are a part of many diving maneuvers and similar strength and stability cautions apply to those who spend hours daily perfecting their style and performance. These are the same cautions that apply in soccer and gymnastics, especially where young swimmers and divers are concerned. Competitive swimmers may spend many hours daily performing their ritual number of training lengths and it is essential for the health of their musculoskeletal systems (if nothing else) that the particular stresses are balanced by appropriate toning and stretching protocols.
Also of potential concern is significant exposure to chlorine, an agent usually added to pool water as a disinfectant. Nemery et al (2002) note that chlorination may affect the respiratory health of those who work at the pool as well as those who use the pools as customers, including children, the general public, and competitive swimmers. Although severe manifestations will depend on the intensity of the exposure and other factors, they report that the more severe conditions may include laryngeal edema, asthma attacks and chemical burns of the upper and lower airway mucosa, and even chemical pneumonitis, while less frequent (less serious) conditions include transient lachrymation, nasopharyngeal irritation, and hyperventilation.
American football
More injuries occur during training in football than in actual competition (Davies 1980). Depending on their role on the team, football players require great leg and upper body strength as well as enormous agility. In addition to excellent eye-hand coordination, jumping and throwing ability (and the stresses this imposes on the upper body), lower back stability is required to cope with rapid back extensions against forces that occur in blocking.
Watkins (1996) notes:
The effect [of blocking] is similar to the weight-lifting position of weight over the head, except that it must be generated with forward leg motion, off-balance resistance to the weight, while trying to carry out specific maneuvers such as blocking a man in a specific direction. Lumbar spine problems in these athletes requires specific training in back strengthening exercises to prevent injury. As well as these stresses, football calls for being able to cope with rotational strains, often while off balance, leading among other things to the possibility of transverse process fracture, disc injury and lumbodorsal fascial tears.Watkins (1996)reports that these multiple and varied demands more commonly produce facet joint pain, spondylolysis (especially involving ‘aerobatic’ receivers) and spondylolisthesis.
Rotational activities
A variety of sports impose torsional stresses that, in time, produce ‘sports-specific’ damage.
Golf
Golf produces the highest level of back problems in any professional sport. In the 1985–86 PGA tour 230 out of 300 professionals reported injuries (77%) (Watkins 1996). Of these, nearly 44% were spine related and 43% lumbosacral. In golf the spine absorbs a great deal of the torsional strain caused by rotation of the hips, knees and shoulders. General advice to golfers should include reducing the extent of the backswing and the follow-through and keeping these symmetrical; encouraging better abdominal control (stability) and avoiding lateral bending. Ultimately, however, there is no way of avoiding some of the torsional forces inherent in the game.
Kuchera (1990) has shown that in healthy collegiate volunteers a significant correlation exists between a history of trauma and the type of athletic activity pursued, most notably in a golf team who displayed a rotation to the right around the right oblique sacral axis. The volunteers were subjected to a variety of assessments including palpatory structural analysis, anthropomorphic measurements, radiographic series as well as photographic center-of-gravity analyses. The volunteers were using Zink’s patterning protocol (see Volume 1 for Zink’s assessment protocol and the Essential Information chapter.
Well-compensated patterns of fascial change were noted in those who had a low incidence of back pain whereas, conversely, a higher incidence of non-compensated patterning related to back pain within the previous year. Subjects reporting a significant history of psoas muscle problems were found to have a high incidence of poorly compensated fascial patterning.
Tennis
Chard & Lachmann (1987) reported that the percentages of injured players in different racquet sports were: squash 59%, tennis 21%, badminton 20%. The speed and rotation involved in tennis in general, and the serve in particular, together with extremes of extension, sideflexion and flexion, place powerful stresses on the low back that – to an extent – can be minimized by relaxed knees. Watkins (1996) believes that: ‘Leg strength, quadriceps strength, and the ability to play in a bent-knee, hip-flexed position while protecting the back is the key to prevention of back pain [in tennis players]’. Regarding the extreme stress of the serve: ‘Gluteal, latissimus dorsi, abdominal obliques and rectus abdominis strength control the lumbodorsal fascia and deliver the power necessary through the legs up into the arm’. This is the kinetic chain that needs to be evaluated if problems arise in any parts of the chain mechanism.
Baseball
Torsional stresses are involved in both batting and pitching. The same strength of the cylindrical torso musculature is required to prevent or minimize the damage that repetitive stress encourages. As abdominal musculature weakens, lumbar lordosis increases and injury becomes more likely (see details of the crossed syndrome pattern in Chapters 2 and 11).
In addition to global torsional stresses that affect the spine, abdomen and pelvis, repetitive stress will also be placed on particular tissues, such as the humeral shaft of the pitching arm, demanding adaptations unique to that sport. Crenshaw et al (2006) note: ‘The common pattern of the throwing shoulder, to develop an increased range of external rotation and decreased internal rotation, is one of many adaptations. The ability of the athlete to adapt adequately seems to be what allows him to compete at the top levels of his chosen sport.’
While these adaptations may allow exceptional performance, they may also negatively affect the athlete. ‘The practitioner must constantly assess postural adaptations and other specialized training adaptations in order to maintain optimal function of the athlete.’
It is vital that the practitioner understands the biomechanics of the sport as well as expected adaptational patterns. For instance, along with retroversion (Fig. 5.19) that accompanies the stresses imposed by pitching baseball, the athlete will present with what appears to be increased external rotation and decreased internal rotation. This is actually a modified (posterier) placement of the normal range of motion. This should not be confused with reduced internal range since attempting to the internal range in this case might ultimately destabilize the joint. It is particularly important that these adaptations be understood when working with professional athletes in order to avoid imposing changes that might end a career.
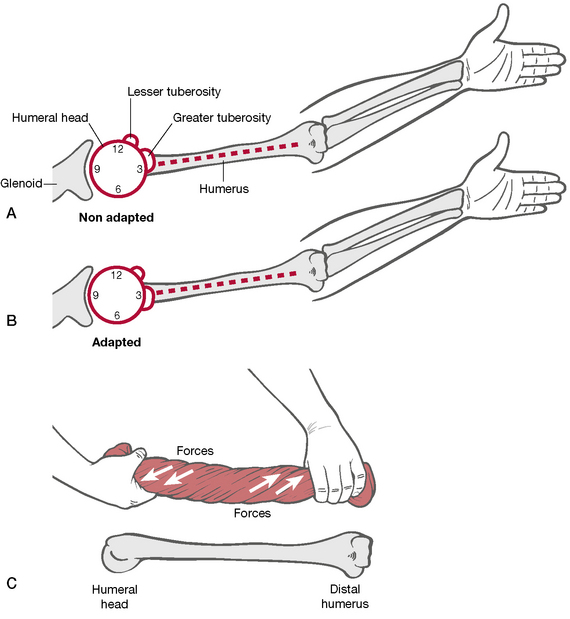
Figure 5.19 Osseous adaptations of the humerus from repetitive overhead throwing (humeral retroversion) is one of several adaptations in athletics.
(reproduced with permission from Crenshaw et al 2006 and from MET 3E p313, Figure 11.1A-C)
Risk in other sports
Other sports that carry a high risk for potential for injury, each with its own unique features, include the following.
Skiing
Severe muscular imbalances are extremely common in skiers. Schmid (1984) studied the main postural and phasic muscles in eight members of the male Olympic ski teams, from Switzerland and Liechtenstein. He found that among this group of apparently superbly fit individuals, fully six of the eight had demonstrably short right iliopsoas muscles, while five of the eight also had left iliopsoas shortness and the majority also displayed weakness of the rectus abdominis muscles. The long-term repercussions of such imbalances can be easily imagined.
A number of skiing injuries commonly occur. Although a large reduction in tibia and fibular fractures have occurred since the development of release bindings, the knee remains vulnerable to impact and torsional injuries, being accounted by Davidson and Laliotis (1996) as the most frequently injured area (35% of all injuries). Collateral and cruciate ligament strains and tears commonly affect beginner and intermediate skiers.
The most common hand injury is skier’s thumb, which involves impact on the ground (snow) while gripping the ski pole, which can result in stretch or tear of the ulnar collateral ligament. Davidson and Laliotis (1996) note ‘Changes in the design of ski pole handles, including the strapless pole, have not lessened the rate of injury and in some instances have been shown to increase the risk of injury.’ This leads them to suggest that further research is needed in the areas of skier’s thumb injuries and ski pole design.
Cycling
Rolf (1977) points out that persistent exercise such as cycling will shorten and toughen the fascial iliotibial band ‘until it becomes reminiscent of a steel cable’. This band crosses both hip and knee and spatial compression allows it to squeeze and compress cartilaginous elements such as the menisci. Ultimately, it will no longer be able to compress and rotational displacement at knee and hip will take place. Examination of anyone engaged in cycling, other than as simple means of transport, is likely to display extreme shortness of the lateral thigh structures.
Rugby football
One of the authors (LC) comes from South Africa, where rugby football is more a religion than a game. Chaitow recounts:
My first recollection of school, at around the age of 5, is not of classroom activity but of being drilled in the rudiments of lineout strategy, on bone-hard, grassless pitches, and of many, many bruises and grazes. This early experience has left me with a profound love of the game, as a spectator, not a participant.
In later years, clinical practice has seen a steady stream of injured rugby players whose dysfunctional patterns (especially for forwards, engaged in scrimmage work) almost always involve a permanent degree of hip flexion associated with psoas shortening of heroic proportions, commonly accompanied by overdeveloped upper fixators (‘gothic shoulders’). Injuries are common in rugby; many are impact traumas but a great many seem to relate to inflexibility and malcoordination caused by overdeveloped flexors and consequently inhibited extensors.
Volleyball and basketball
Liebenson (1990) has discussed the work of Sommer (1985) who found that competitive basketball and volleyball players frequently suffer patellar tendinitis and other forms of knee dysfunction due to the particular stresses they endure because of muscular imbalances resulting from postures and activities peculiar to these games. Their ability to jump is often seriously impaired by virtue of shortened psoas and quadriceps muscles with associated weakness of gluteus maximus. This imbalance leads to decreased hip extension and a tendency for hyperextension of the knee joint. Once muscular balance is restored, a more controlled jump is possible, as is a reduction in reported fatigue. Lewit (1985) has noted particular dangers relating to volleyball. ‘Those who play at the net must, as they leap up and drop back to the ground, keep the lumbar spine in hyperlordosis so as not to touch the net; this is most unphysiological and a danger to the low lumbar discs.’
Leaving aside professional sport and its pressures, the particulars of the sporting activities of non-professional athletes should clearly be an area of interest to the practitioner. Sport can be a healthy and life-enhancing pursuit and it can also be a major contributor to dysfunction and recurrent pain.
Aggrawal N. A study of changes in weight lifters and other athletes. Br J Sports Med. 1979;13:58.
Allen R. Sports medicine. In: Ward R., editor. Foundations of osteopathic medicine. Baltimore: Williams and Wilkins, 1997.
Ball D., Harrington L. Training and overload. Journal of Bodywork and Movement Therapies. 1998;2(3):161-167.
Beam J. Athletic training for groin pain. Journal of Bodywork and Movement Therapies. 1998;2(3):144-148.
Birch K., George K. Overtraining the female athlete. Journal of Bodywork and Movement Therapies. 1999;3(1):24-29.
Broussard M. Evaluation of citrus bioflavonoids in contact sports. Citrus in Medicine. 2(2), 1963.
Budgett R. Overtraining syndrome. Br J Sports Med. 1990;24:231-236.
Bullen B., Skrinar G., Beitins I. Induction of menstrual cycle disorders by strenuous exercise in untrained women. N Engl J Med. 1985;312:1349-1353.
Burt C., Overpeck M. Emergency visits for sports-related injuries. Ann Emerg Med. 2001;37:301-308.
Busch M., Marshall D., May K. Overuse injuries. In: Tornetta P., Scherl S., editors. Orthopaedic surgery essentials: pediatrics. Philadelphia: Lippincott Williams & Wilkins; 2004:281-288.
Chaitow L. Positional release techniques, ed 2. Edinburgh: Churchill Livingstone, 2007.
Chaitow L., DeLany J. Clinical application of neuromuscular techniques, vol 1, the upper body, ed 2. Edinburgh: Churchill Livingstone, 2008.
Chard M., Lachmann S. Raquet sports – patterns of injury. Br J Sports Med. 1987;21:150.
Constantini N. Clinical consequences of athletic amenorrhea. Sports Medicine. 1994;17:213-223.
Crenshaw K., Shaw N., Porterfield R. MET in treatment of athletic injuries. In: Chaitow L., editor. Muscle energy techniques. Edinburgh: Elsevier, 2006.
Damore D., Metzl J., Ramundo M., et al. Patterns of childhood sports injury. Pediatr Emerg Care. 2003;19(2003):65-67.
Davidson T., Laliotis A. Alpine skiing injuries. A nine year study. West Journal of Medicine. 1996;164(4):310-314.
Davies J. The spine in sports injuries. Br J Sports Med. 1980;14:18.
Deig D. Positional release technique. Boston: Butterworth Heinemann, 2001.
DeLany J. Neuromuscular therapy management of hamstring injury. Journal of Bodywork and Movement Therapies. 1996;1(1):16-17.
DeLany J. Connective tissue perspectives. Journal of Bodywork and Movement Therapies. 2000;4(4):273-275.
Feinberg E. Sports chiropractic. In: Redwood D., editor. Contemporary chiropractic. New York: Churchill Livingstone, 1997.
Fitt S., Sturman J., McClain-Smith S. Effects of Pilates-based conditioning on strength, alignment and range of motion of university ballet and modern dancers. Kinesiology and Medicine for Dance. 1994;16:36-51.
Fry R., Morton A., Keast D. Overtraining in athletes. J Sports Med. 1991;12:32-65.
Garrick J., Requa R. Epidemiology of women’s gymnastic injuries. American Journal of Sports Injuries. 1980;8:261.
Goldspink G. Alterations in myofibril size and structure during growth, exercise and changes in environmental temperatures. In: Peachey L., editor. Handbook of physiology (section 10). Baltimore: Williams and Wilkins, 1983.
Griffin A. The physiological effects of intense swimming competition on 16–17 year old elite female swimmers. Pediatric Exercise Science. 1999;11:22-32.
Griffin A., Unnithan V. Overtraining in child athletes. Journal of Bodywork and Movement Therapies. 1999;3(2):92-96.
Gross M. Chronic tendinitis. J Orthop Sports Phys Ther. 1992;16:248-261.
Hasselman C. When groin pain signals an adductor strain. Physician and Sports Medicine. 1995;23:53-60.
Heath G., Ford E., Craven T. Exercise and the incidence of upper respiratory tract infections. Med Sci Sports Exerc. 1991;23:152-157.
Hensinger R. Spondylolysis and spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1989;71:1098-1107.
Hikida R., Staron R. Muscle fiber necrosis associated with human marathon runners. Journal of Neurological Sciences. 1983;59:185-203.
Hodson A. Too much too soon? The risk of ‘overuse’ injuries in young football players. Journal of Bodywork and Movement Therapies. 1999;3(2):85-91.
Jackson D. Low back pain in young athletes. Am J Sports Med. 1979;7:364.
Janda V., Schmid H. Muscles as a pathogenic factor in back pain. Proceedings of the International Federation of Orthopaedic Manipulative Therapists 4th Conference. 1980:17-18. New Zealand
Jones D., Newham D. Experimental human muscle damage. J Physiol. 1986;373:435-448.
Jones L. Jones strain-counterstrain. Boise, Idaho: Jones Strain-Counterstrain, 1995.
Jull G., Janda V. Muscles and motor control in low back pain. In: Twomey L., Taylor J., editors. Physical therapy for the low back. Clinics in physical therapy. New York: Churchill Livingstone, 1987.
Keen P. The prevention of overtraining. Coaching Focus. 1995;28:12-13.
Kotani P. Studies of spondylolisthesis found in weight lifters. Br J Sports Med. 1981;9:4.
Krasnow D., Chatfield S., Barr S., et al. Imagery and conditioning practices for dancers. Dance Research Journal. 1997;29:43-64.
Kuchera M. Athletic functional demand and posture. J Am Osteopath Assoc. 1990;90(9):843-844.
Kulund D. The injured athlete, ed 2. Philadelphia: Lippincott, 1988.
Lange C., Unnithan V., Larkam E., et al. Maximizing the benefits of Pilates-inspired exercise for learning functional motor skills. Journal of Bodywork and Movement Therapies. 1999;4(2):99-108.
Lederman E. Fundamentals of manual therapy. Physiology, neurology and psychology. Edinburgh: Churchill Livingstone, 1997.
Lephart S., Fu F. The role of proprioception in the treatment of sports injuries. Sports Exercise and Injury. 1995;1:96-102.
Lewit K. Manipulative therapy in rehabilitation of the motor system. London: Butterworths, 1985.
Liebenson C. Active muscular relaxation techniques (part 2). J Manipulative Physiol Ther. 1990;13(1):2-6.
Linsenbardt S., Thomas T., Madsen R. Effect of breathing techniques on blood pressure response to resistance exercise. Br J Sports Med. 1992;26:97-100.
Lloyd T., Triantafyllou S. Women athletes with menstrual irregularities. Med Sci Sports Exerc. 1986;18:374-379.
Lucas K., Polusa B., Rich P. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. Journal of Bodywork and Movement Therapies. 2004;8:160-166.
MacDougall J. Morphological changes in human skeletal muscle following strength training and immobilization. In: Jones N., editor. Human muscle power. Champaign, Illinois: Human Kinetics, 1986.
Maglischo E. Swimming even faster. California: Mayfield Publishing, 1993.
Marciniak R. Spondylolysis and spondylolisthesis among young atheletes. Annals of Sports Medicine. 1998;4(3):125-126.
Matheson G., Clement D., McKenzie D. Stress fractures in athletes. Am J Sports Med. 1986;15:46-58.
McBryde A. Stress fractures in athletes. J Sports Med. 1976;3(2):212-217.
McClain S., Carter C., Abel J. The effect of a conditioning and alignment program on the measurement of supine jump height and pelvic alignment. Journal of Dance Medicine and Science. 1997;1:149-154.
McMillan A., Proteau L., Rebe R.-M. The effects of Pilates-based training on dancers’ dynamic posture. Journal of Dance Medicine and Science. 1998;2:101-107.
Mense S., Simons D. Muscle pain: understanding its nature, diagnosis and treatment. Baltimore: Lippincott, Williams and Wilkins, 2001.
Newton P. Physiotherapy for groin pain. Journal of Bodywork and Movement Therapies. 1998;2(3):134-139.
Nemery B., Hoet P., Nowak D. Indoor swimming pools, water chlorination and respiratory health. Eur Respir J. 2002;19:790-793.
Norris C. Weight training: principles and practice. London: A&C Black, 1995.
Norris C. Back stability. Champaign, Illinois: Human Kinetics, 2000.
Oschman J.L. What is healing energy? Pt 5: gravity, structure, and emotions. Journal of Bodywork and Movement Therapies. 1997;1(5):307-308.
Parrott A. The effects of Pilates technique and aerobic conditioning on dancers’ technique. Kinesiology and Medicine for Dance. 1993;15:45-64.
Prior J., Vigna Y. Reproduction for the athletic woman. J Sports Med. 1992;14:190-199.
Raissakia M., Apostolakia E., Karantana A. Imaging of sports injuries in children and adolescents. Eur J Radiol. 2007;62(1):86-96.
Reed M. Chiropractic management of hamstring injury. Journal of Bodywork and Movement Therapies. 1996;1(1):10-15.
Renstrom P. Tendon and muscle injuries in groin area. Clinical Sports Medicine. 1992;11(4):815-831.
Rolf I. Rolfing – integration of human structures. New York: Harper and Row, 1977.
Schafer R. Clinical biomechanics, ed 2. Baltimore: Williams and Wilkins, 1987.
Schmid H. Muscular imbalances in skiers. Manual Medicine. 1984(2):23-26.
Selye H. The stress of life. New York: McGraw-Hill, 1956.
Sheehan G. Sports medicine renaissance. Physician Sports Medicine. 1990;18(11):26.
Sherman W., Armstrong L., Murray T. Effect of a 42.2 km footrace and subsequent rest or exercise on muscular strength and work capacity. J Appl Physiol. 1984;57:1668-1673.
Simons D., Travell J., Simons L. Myofascial pain and dysfunction: the trigger point manual, vol 1, upper half of body, ed 2. Baltimore: Williams and Wilkins, 1999.
Sommer H. Patellar chondropathy and apicitis. Muscle imbalances of the lower extremity. London: Butterworths, 1985.
Soprano J., Fuchs S. Common overuse injuries the pediatric and adolescent athlete. Clinical Pediatric Emergency Medicine. 2007;8(1):7-14.
Sutton G. Hamstrung by hamstring strains. J Orthop Sports Phys Ther. 1984;5(4):184-195.
Tidball J. Myotendinous junction injury. Exercise and Sports Sciences Review. Baltimore: Williams and Wilkins, 1991.
Travell J., Simons D. Myofascial pain and dysfunction: the trigger point manual, vol 2, the lower extremities. Baltimore: Williams and Wilkins, 1992.
Van Der Velde G., Hsu W. Posterior tibial stress fracture. J Manipulative Physiol Ther. 1999;22(5):341-346.
Vaughn B. Hamstring muscle strain. Journal of Bodywork and Movement therapies. 1996;1(1):9-10.
Vaughn B. Presentation to the 1st International Journal of Bodywork and Movement Therapies Conference, Berkeley, California. 1998.
Wallace E., McPartland J., Jones J., et al. Lymphatic manipulative techniques. In: Ward R., editor. Foundations for osteopathic medicine. Baltimore: Williams and Wilkins, 1997.
Watkins R. Lumbar spine injury in the athlete. In: Liebenson C., editor. Rehabilitation of the spine. Baltimore: Williams and Wilkins, 1996.
Weiss P. The biological foundation of wound repair. Harvey Lect. 1961;55:13-42.
Werbach M. Natural medicine for muscle strain. Journal of Bodywork and Movement Therapies. 1996;1(1):18-19.