Malocclusion and Dentofacial Deformity in Contemporary Society
The Changing Goals of Orthodontic Treatment
Crowded, irregular, and protruding teeth have been a problem for some individuals since antiquity, and attempts to correct this disorder go back at least to 1000 BC. Primitive (and surprisingly well-designed) orthodontic appliances have been found in both Greek and Etruscan materials.1 As dentistry developed in the eighteenth and nineteenth centuries, a number of devices for the “regulation” of the teeth were described by various authors and apparently used sporadically by the dentists of that era.
After 1850, the first texts that systematically described orthodontics appeared, the most notable being Norman Kingsley’s Oral Deformities.2 Kingsley, who had a tremendous influence on American dentistry in the latter half of the nineteenth century, was among the first to use extraoral force to correct protruding teeth. He was also a pioneer in the treatment of cleft palate and related problems.
Despite the contributions of Kingsley and his contemporaries, their emphasis in orthodontics remained the alignment of the teeth and the correction of facial proportions. Little attention was paid to bite relationships, and since it was common practice to remove teeth for many dental problems, extractions for crowding or malalignment were frequent. In an era when an intact dentition was a rarity, the details of occlusal relationships were considered unimportant.
To make good prosthetic replacement teeth, it was necessary to develop a concept of occlusion, and this occurred in the late 1800s. As the concepts of prosthetic occlusion developed and were refined, it was natural to extend this to the natural dentition. Edward H. Angle (Figure 1-1), whose influence began to be felt about 1890, can be credited with much of the development of a concept of occlusion in the natural dentition. Angle’s original interest was in prosthodontics, and he taught in that department in the dental schools at Pennsylvania and Minnesota in the 1880s. His increasing interest in dental occlusion and in the treatment necessary to obtain normal occlusion led directly to his development of orthodontics as a specialty, with himself as the “father of modern orthodontics.”
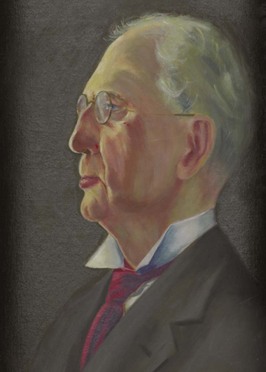
FIGURE 1-1 Edward H. Angle in his fifties, as the proprietor of the Angle School of Orthodontia. After establishing himself as the first dental specialist, Angle operated proprietary orthodontic schools from 1905 to 1928 in St. Louis; New London, Connecticut; and Pasadena, California, in which many of the pioneer American orthodontists were trained.
Angle’s classification of malocclusion in the 1890s was an important step in the development of orthodontics because it not only subdivided major types of malocclusion but also included the first clear and simple definition of normal occlusion in the natural dentition. Angle’s postulate was that the upper first molars were the key to occlusion and that the upper and lower molars should be related so that the mesiobuccal cusp of the upper molar occludes in the buccal groove of the lower molar. If the teeth were arranged on a smoothly curving line of occlusion (Figure 1-2) and this molar relationship existed (Figure 1-3), then normal occlusion would result.3 This statement, which 100 years of experience has proved to be correct—except when there are aberrations in the size of teeth, brilliantly simplified normal occlusion.
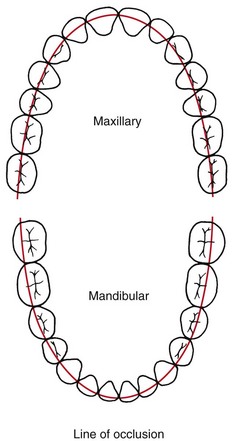
FIGURE 1-2 The line of occlusion is a smooth (catenary) curve passing through the central fossa of each upper molar and across the cingulum of the upper canine and incisor teeth. The same line runs along the buccal cusps and incisal edges of the lower teeth, thus specifying the occlusal as well as interarch relationships once the molar position is established.
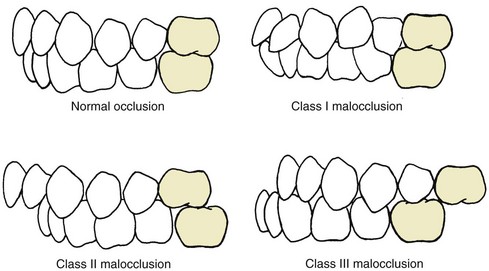
FIGURE 1-3 Normal occlusion and malocclusion classes as specified by Angle. This classification was quickly and widely adopted early in the twentieth century. It is incorporated within all contemporary descriptive and classification schemes.
Angle then described three classes of malocclusion, based on the occlusal relationships of the first molars:
Class I: Normal relationship of the molars, but line of occlusion incorrect because of malposed teeth, rotations, or other causes
Class II: Lower molar distally positioned relative to upper molar, line of occlusion not specified
Class III: Lower molar mesially positioned relative to upper molar, line of occlusion not specified
Note that the Angle classification has four classes: normal occlusion, Class I malocclusion, Class II malocclusion, and Class III malocclusion (see Figure 1-3). Normal occlusion and Class I malocclusion share the same molar relationship but differ in the arrangement of the teeth relative to the line of occlusion. The line of occlusion may or may not be correct in Class II and Class III.
With the establishment of a concept of normal occlusion and a classification scheme that incorporated the line of occlusion, by the early 1900s orthodontics was no longer just the alignment of irregular teeth. Instead, it had evolved into the treatment of malocclusion, defined as any deviation from the ideal occlusal scheme described by Angle. Since precisely defined relationships required a full complement of teeth in both arches, maintaining an intact dentition became an important goal of orthodontic treatment. Angle and his followers strongly opposed extraction for orthodontic purposes. With the emphasis on dental occlusion that followed, however, less attention came to be paid to facial proportions and esthetics. Angle abandoned extraoral force because he decided this was not necessary to achieve proper occlusal relationships. He solved the problem of dental and facial appearance by simply postulating that the best esthetics always were achieved when the patient had ideal occlusion.
As time passed, it became clear that even an excellent occlusion was unsatisfactory if it was achieved at the expense of proper facial proportions. Not only were there esthetic problems, it often proved impossible to maintain an occlusal relationship achieved by prolonged use of heavy elastics to pull the teeth together as Angle and his followers had suggested. Under the leadership of Charles Tweed in the United States and Raymond Begg in Australia (both of whom had studied with Angle), extraction of teeth was reintroduced into orthodontics in the 1940s and 1950s to enhance facial esthetics and achieve better stability of the occlusal relationships.
Cephalometric radiography, which enabled orthodontists to measure the changes in tooth and jaw positions produced by growth and treatment, came into widespread use after World War II. These radiographs made it clear that many Class II and Class III malocclusions resulted from faulty jaw relationships, not just malposed teeth. By use of cephalometrics, it also was possible to see that jaw growth could be altered by orthodontic treatment. In Europe, the method of “functional jaw orthopedics” was developed to enhance growth changes, while in the United States, extraoral force came to be used for this purpose. At present, both functional and extraoral appliances are used internationally to control and modify growth and form. Obtaining correct or at least improved jaw relationships became a goal of treatment by the mid-twentieth century.
The changes in the goals of orthodontic treatment, which are to focus on facial proportions and the impact of the dentition on facial appearance, have been codified now in the form of the soft tissue paradigm.4
Modern Treatment Goals: The Soft Tissue Paradigm
A paradigm can be defined as “a set of shared beliefs and assumptions that represent the conceptual foundation of an area of science or clinical practice.” The soft tissue paradigm states that both the goals and limitations of modern orthodontic and orthognathic treatment are determined by the soft tissues of the face, not by the teeth and bones. This reorientation of orthodontics away from the Angle paradigm that dominated the twentieth century is most easily understood by comparing treatment goals, diagnostic emphasis, and treatment approach in the two paradigms (Table 1-1). With the soft tissue paradigm, the increased focus on clinical examination rather than examination of dental casts and radiographs leads to a different approach to obtaining important diagnostic information and that information is used to develop treatment plans that would not have been considered without it.
TABLE 1-1
Angle Versus Soft Tissue Paradigms: A New Way of Looking at Treatment Goals
| Parameter | Angle paradigm | Soft tissue paradigm |
| Primary treatment goal | Ideal dental occlusion | Normal soft tissue proportions and adaptations |
| Secondary goal | Ideal jaw relationships | Functional occlusion |
| Hard/soft tissue relationships | Ideal hard tissue proportions produce ideal soft tissues | Ideal soft tissue proportions define ideal hard tissues |
| Diagnostic emphasis | Dental casts, cephalometric radiographs | Clinical examination of intraoral and facial soft tissues |
| Treatment approach | Obtain ideal dental and skeletal relationships, assume the soft tissues will be OK | Plan ideal soft tissue relationships and then place teeth and jaws as needed to achieve this |
| Function emphasis | TM joint in relation to dental occlusion | Soft tissue movement in relation to display of teeth |
| Stability of result | Related primarily to dental occlusion | Related primarily to soft tissue pressure/equilibrium effects |
More specifically, what difference does the soft tissue paradigm make in planning treatment? There are several major effects:
1. The primary goal of treatment becomes soft tissue relationships and adaptations, not Angle’s ideal occlusion. This broader goal is not incompatible with Angle’s ideal occlusion, but it acknowledges that to provide maximum benefit for the patient, ideal occlusion cannot always be the major focus of a treatment plan. Soft tissue relationships, both the proportions of the soft tissue integument of the face and the relationship of the dentition to the lips and face, are the major determinants of facial appearance. Soft tissue adaptations to the position of the teeth (or lack thereof) determine whether the orthodontic result will be stable. Keeping this in mind while planning treatment is critically important.
2. The secondary goal of treatment becomes functional occlusion. What does that have to do with soft tissues? Temporomandibular (TM) dysfunction, to the extent that it relates to the dental occlusion, is best thought of as the result of injury to the soft tissues around the TM joint caused by clenching and grinding the teeth. Given that, an important goal of treatment is to arrange the occlusion to minimize the chance of injury. In this also, Angle’s ideal occlusion is not incompatible with the broader goal, but deviations from the Angle ideal may provide greater benefit for some patients, and should be considered when treatment is planned.
3. The thought process that goes into “solving the patient’s problems” is reversed. In the past, the clinician’s focus was on dental and skeletal relationships, with the tacit assumption that if these were correct, soft tissue relationships would take care of themselves. With the broader focus on facial and oral soft tissues, the thought process is to establish what these soft tissue relationships should be and then determine how the teeth and jaws would have to be arranged to meet the soft tissue goals. Why is this important in establishing the goals of treatment? It relates very much to why patients/parents seek orthodontic treatment and what they expect to gain from it.
The following sections of this chapter provide some background on the prevalence of malocclusion, what we know about the need for treatment of malocclusion and dentofacial deformity, and how soft tissue considerations, as well as teeth and bone, affect both need and demand for orthodontic treatment. It must be kept in mind that orthodontics is shaped by biological, psychosocial, and cultural determinants. For that reason, when defining the goals of orthodontic treatment, one has to consider not only morphologic and functional factors, but a wide range of psychosocial and bioethical issues as well.
The Usual Orthodontic Problems: Epidemiology of Malocclusion
Angle’s “normal occlusion” more properly should be considered the ideal. In fact, perfectly interdigitating teeth arranged along a perfectly regular line of occlusion are quite rare. For many years, epidemiologic studies of malocclusion suffered from considerable disagreement among investigators about how much deviation from the ideal should be accepted within the bounds of normal. By the 1970s, a series of studies by public health or university groups in most developed countries provided a reasonably clear worldwide picture of the prevalence of various occlusal relationships or malrelationships.
In the United States, two large-scale surveys carried out by the U.S. Public Health Service (USPHS) covered children ages 6 to 11 years between 1963 and 1965 and youths ages 12 to 17 years between 1969 and 1970.5,6 As part of a large-scale national survey of health care problems and needs in the United States in 1989-1994 (National Health and Nutrition Estimates Survey III [NHANES III]), estimates of malocclusion again were obtained. This study of some 14,000 individuals was statistically designed to provide weighted estimates for approximately 150 million persons in the sampled racial/ethnic and age groups. The data provide current information for U.S. children and youths and include the first good data set for malocclusion in adults, with separate estimates for the major racial/ethnic groups.7
The characteristics of malocclusion evaluated in NHANES III included the irregularity index, which is a measure of incisor alignment (Figure 1-4); the prevalence of midline diastema larger than 2 mm (Figure 1-5); and the prevalence of posterior crossbite (Figure 1-6). In addition, overjet (Figure 1-7) and overbite/open bite (Figure 1-8) were measured. Overjet reflects Angle’s Class II and Class III molar relationships. Because overjet can be evaluated much more precisely than molar relationship in a clinical examination, molar relationship was not evaluated directly.
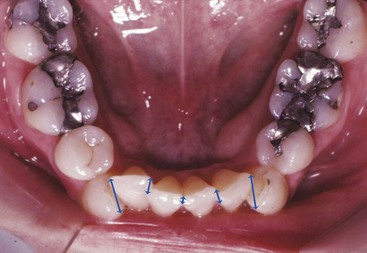
FIGURE 1-4 Incisor irregularity usually is expressed as the irregularity index; the total of the millimeter distances from the contact point on each incisor tooth to the contact point that it should touch, as shown by the blue lines. For this patient, the irregularity index is 10 (mm).

FIGURE 1-5 A space between adjacent teeth is called a diastema. A maxillary midline diastema is relatively common, especially during the mixed dentition in childhood, and disappears or decreases in width as the permanent canines erupt. Spontaneous correction of a childhood diastema is most likely when its width is not more than 2 mm.

FIGURE 1-6 Posterior crossbite exists when the maxillary posterior teeth are lingually positioned relative to the mandibular teeth, as in this patient. Posterior crossbite most often reflects a narrow maxillary dental arch but can arise from other causes. This patient also has a one-tooth anterior crossbite, with the lateral incisor trapped lingually.
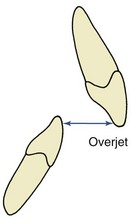
FIGURE 1-7 Overjet is defined as horizontal overlap of the incisors. Normally, the incisors are in contact, with the upper incisors ahead of the lower by only the thickness of their incisal edges (i.e., 2 to 3 mm overjet is the normal relationship). If the lower incisors are in front of the upper incisors, the condition is called reverse overjet or anterior crossbite.
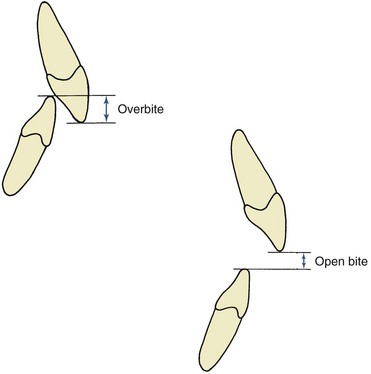
FIGURE 1-8 Overbite is defined as the vertical overlap of the incisors. Normally, the lower incisal edges contact the lingual surface of the upper incisors at or above the cingulum (i.e., normally there is a 1 to 2 mm overbite). In open bite, there is no vertical overlap, and the vertical separation of the incisors is measured to quantify its severity.
Current data for these characteristics of malocclusion for children (age 8 to 11), youths (age 12 to 17), and adults (age 18 to 50) in the U.S. population, taken from NHANES III, are displayed graphically in Figures 1-9 to 1-11.
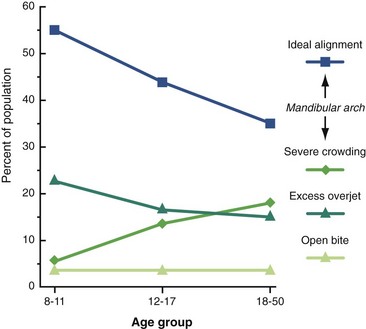
FIGURE 1-9 Changes in the prevalence of types of malocclusion from childhood to adult life, United States, 1989-1994. Note the increase in incisor irregularity and decrease in severe overjet as children mature, both of which are related to mandibular growth.
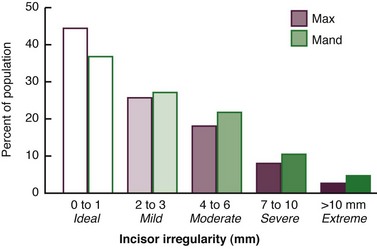
FIGURE 1-10 Incisor irregularity in the U.S. population, 1989-1994. One-third of the population have at least moderately irregular (usually crowded) incisors, and nearly 15% have severe or extreme irregularity. Note that irregularity in the lower arch is more prevalent at any degree of severity.
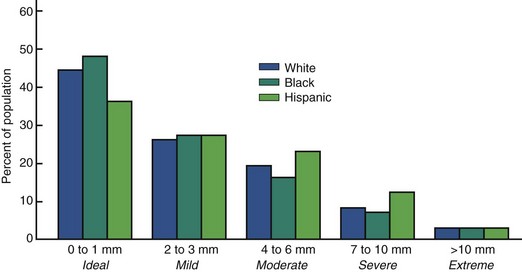
FIGURE 1-11 Incisor irregularity by racial-ethnic groups. The percentage of the Hispanic population with ideal alignment is lower than the other two groups, and the percentage with moderate and severe crowding is higher. This may reflect the low number of Hispanics with orthodontic treatment at the time of the NHANES-III survey.
Note in Figure 1-9 that in the age 8 to 11 group, just over half of U.S. children have well-aligned incisors. The rest have varying degrees of malalignment and crowding. The percentage with excellent alignment decreases in the age 12 to 17 group as the remaining permanent teeth erupt, then remains essentially stable in the upper arch but worsens in the lower arch for adults. Only 34% of adults have well-aligned lower incisors. Nearly 15% of adolescents and adults have severely or extremely irregular incisors, so that major arch expansion or extraction of some teeth would be necessary to align them (see Figure 1-9).
A midline diastema (see Figure 1-5) often is present in childhood (26% have >2 mm space). Although this space tends to close, over 6% of youths and adults still have a noticeable diastema that compromises the appearance of the smile. Blacks are more than twice as likely to have a midline diastema than whites or Hispanics (p < .001).
Occlusal relationships must be considered in all three planes of space. Posterior crossbite reflects deviations from ideal occlusion in the transverse plane of space. It is relatively rare at all ages. Overjet or reverse overjet indicates anteroposterior deviations in the Class II/Class III direction, and overbite/open bite indicates vertical deviations from ideal. Overjet of 5 mm or more, suggesting Angle’s Class II malocclusion, occurs in 23% of children, 15% of youths, and 13% of adults (Figure 1-12). Reverse overjet, indicative of Class III malocclusion, is much less frequent. This affects about 3% of American children and increases to about 5% in youths and adults. Severe or extreme Class II and Class III problems, at the limit of orthodontic correction or too severe for nonsurgical correction, occur in about 4% of the population, with severe Class II much more prevalent. Severe Class II problems are less prevalent and severe Class III problems are more prevalent in the Hispanic than the white or black groups.
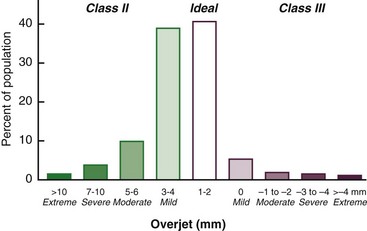
FIGURE 1-12 Overjet (Class II) and reverse overjet (Class III) in the U.S. population, 1989-1994. Only one-third of the population have ideal anteroposterior incisor relationships, but overjet is only moderately increased in another one-third. Increased overjet accompanying Class II malocclusion is much more prevalent than reverse overjet accompanying Class III.
Vertical deviations from the ideal overbite of 0 to 2 mm are less frequent in adults than children but occur in half the adult population, the great majority of whom have excessive overbite (Figure 1-13). Severe deep bite (overbite ≥5 mm) is found in nearly 20% of children and 13% of adults, while severe open bite (negative overbite ≥2 mm) occurs in less than 1%. There are striking differences between the racial/ethnic groups in vertical dental relationships. Severe deep bite is nearly twice as prevalent in whites as blacks or Hispanics (p < .001), while open bite >2 mm is five times more prevalent in blacks than in whites or Hispanics (p < .001). This almost surely reflects the slightly different craniofacial proportions of the black population groups (see Chapter 5 for a more complete discussion). Despite their higher prevalence of anteroposterior problems, vertical problems are less prevalent in Hispanics than either blacks or whites.
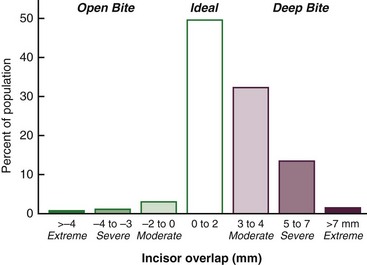
FIGURE 1-13 Open bite/deep bite relationships in the U.S. population, 1989-1994. Half the population have an ideal vertical relationship of the incisors. Deep bite is much more prevalent than open bite, but vertical relationships vary greatly between racial groups.
From the survey data, it is interesting to calculate the percentage of American children and youths who would fall into Angle’s four groups. From this perspective, 30% at most have Angle’s normal occlusion. Class I malocclusion (50% to 55%) is by far the largest single group; there are about half as many Class II malocclusions (approximately 15%) as normal occlusions; and Class III (less than 1%) represents a very small proportion of the total.
Differences in malocclusion characteristics between the United States and other countries would be expected because of differences in racial and ethnic composition. Although the available data are not as extensive as for American populations, it seems clear that Class II problems are most prevalent in whites of northern European descent (for instance, 25% of children in Denmark are reported to be Class II), while Class III problems are most prevalent in Asian populations (3% to 5% in Japan, nearly 2% in China, with another 2% to 3% pseudo-Class III [i.e., shifting into anterior crossbite because of incisor interferences]). African populations are by no means homogenous, but from the differences found in the United States between blacks and whites, it seems likely that Class III and open bite are more frequent in African than European populations and deep bite less frequent.
Why is Malocclusion So Prevalent?
Although malocclusion now occurs in a majority of the population, that does not mean it is normal. Skeletal remains indicate that the present prevalence is several times greater than it was only a few hundred years ago. Crowding and malalignment of teeth were unusual until relatively recently but not unknown (Figure 1-14). Because the mandible tends to become separated from the rest of the skull when long-buried skeletal remains are unearthed, it is easier to be sure what has happened to alignment of teeth than to occlusal relationships. The skeletal remains suggest that all members of a group might tend toward a Class III or, less commonly, a Class II jaw relationship. Similar findings are noted in present population groups that have remained largely unaffected by modern development: crowding and malalignment of teeth are uncommon, but the majority of the group may have mild anteroposterior or transverse discrepancies, as in the Class III tendency of South Pacific islanders8 and buccal crossbite (X-occlusion) in Australian aborigines.9
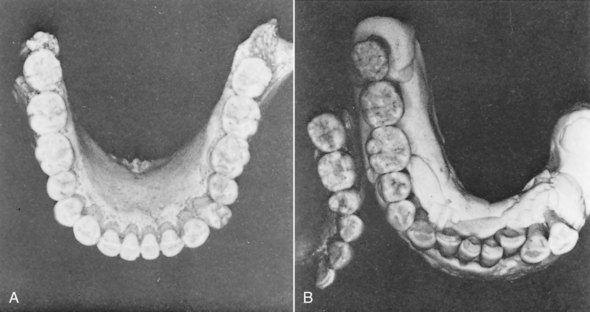
FIGURE 1-14 Mandibular dental arches from specimens from the Krapina cave in Yugoslavia, estimated to be approximately 100,000 years old. A, Note the excellent alignment in this specimen. Near-perfect alignment or minimal crowding was the usual finding in this group. B, Crowding and malalignment are seen in this specimen, which had the largest teeth in this find of skeletal remains from approximately 80 individuals. (From Wolpoff WH. Paleoanthropology. New York: Alfred A Knopf; 1998.)
Although 1000 years is a long time relative to a single human life, it is a very short time from an evolutionary perspective. The fossil record documents evolutionary trends over many thousands of years that affect the present dentition, including a decrease in the size of individual teeth, in the number of the teeth, and in the size of the jaws. For example, there has been a steady reduction in the size of both anterior and posterior teeth over at least the last 100,000 years (Figure 1-15). The number of teeth in the dentition of higher primates has been reduced from the usual mammalian pattern (Figure 1-16). The third incisor and third premolar have disappeared, as has the fourth molar. At present, the human third molar, second premolar, and second incisor often fail to develop, which indicates that these teeth may be on their way out. Compared with other primates, modern humans have quite underdeveloped jaws.
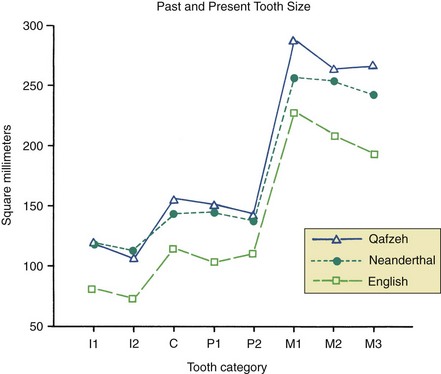
FIGURE 1-15 The generalized decline in the size of human teeth can be seen by comparing tooth sizes from the anthropological site at Qafzeh, dated 100,000 years ago; Neanderthal teeth, 10,000 years ago; and modern human populations. (Redrawn from Kelly MA, Larsen CS, eds. Advances in Dental Anthropology. New York: Wiley-Liss; 1991.)
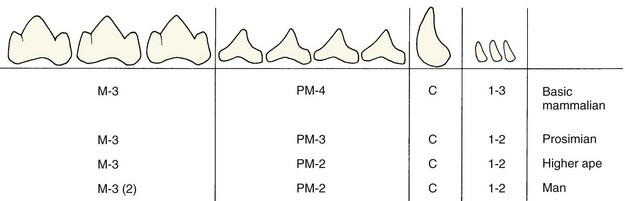
FIGURE 1-16 Reduction in the number of teeth has been a feature of primate evolution. In the present human population, third molars are so frequently missing that it appears a further reduction is in progress, and the variability of lateral incisors and second premolars suggests evolutionary pressure of these teeth.
It is easy to see that the progressive reduction in jaw size, if not well matched to a decrease in tooth size and number, could lead to crowding and malalignment. It is less easy to see why dental crowding should have increased quite recently, but this seems to have paralleled the transition from primitive agricultural to modern urbanized societies. Cardiovascular disease and related health problems appear rapidly when a previously unaffected population group leaves agrarian life for the city and civilization. High blood pressure, heart disease, diabetes, and several other medical problems are so much more prevalent in developed than underdeveloped countries that they have been labeled “diseases of civilization.”
There is some evidence that malocclusion increases within well-defined populations after a transition from rural villages to the city. Corruccini, for instance, reported a higher prevalence of crowding, posterior crossbite, and buccal segment discrepancy in urbanized youths compared with rural Punjabi youths of northern India.10 One can argue that malocclusion is another condition made worse by the changing conditions of modern life, perhaps resulting in part from less use of the masticatory apparatus with softer foods now. Under primitive conditions, of course, excellent function of the jaws and teeth was an important predictor of the ability to survive and reproduce. A capable masticatory apparatus was essential to deal with uncooked or partially cooked meat and plant foods. Watching an Australian aboriginal man using every muscle of his upper body to tear off a piece of kangaroo flesh from the barely cooked animal, for instance, makes one appreciate the decrease in demand on the masticatory apparatus that has accompanied civilization (Figure 1-17). An interesting proposal by anthropologists is that the introduction of cooking, so that it did not take as much effort and energy to masticate food, was the key to the development of the larger human brain. Without cooked food, it would not have been possible to meet the energy demand of the enlarging brain. With it, excess energy is available for brain development and robust jaws are unnecessary.11

FIGURE 1-17 Sections from a 1960s movie of an Australian aboriginal man eating a kangaroo prepared in the traditional (barely cooked) fashion. Note the activity of muscles, not only in the facial region, but throughout the neck and shoulder girdle. (Courtesy M.J. Barrett.)
Determining whether changes in jaw function have increased the prevalence of malocclusion is complicated by the fact that both dental caries and periodontal disease, which are rare on the primitive diet, appear rapidly when the diet changes. The resulting dental pathology can make it difficult to establish what the occlusion might have been in the absence of early loss of teeth, gingivitis, and periodontal breakdown. The increase in malocclusion in modern times certainly parallels the development of modern civilization, but a reduction in jaw size related to disuse atrophy is hard to document, and the parallel with stress-related diseases can be carried only so far. Although it is difficult to know the precise cause of any specific malocclusion, we do know in general what the etiologic possibilities are and these are discussed in some detail in Chapter 5.
What difference does it make if you have a malocclusion? Let us consider now the reasons for orthodontic treatment.
Who Needs Treatment?
Protruding, irregular, or maloccluded teeth can cause three types of problems for the patient: (1) discrimination because of facial appearance; (2) problems with oral function, including difficulties in jaw movement (muscle incoordination or pain), TM joint dysfunction (TMD), and problems with mastication, swallowing, or speech; and (3) greater susceptibility to trauma, periodontal disease, or tooth decay.
Psychosocial Problems
A number of studies in recent years have confirmed what is intuitively obvious: that severe malocclusion is likely to be a social handicap. The usual caricature of an individual who is none too bright includes protruding upper incisors. A witch not only rides a broom, she has a prominent lower jaw that would produce a Class III malocclusion. Well-aligned teeth and a pleasing smile carry positive status at all social levels and ages, whereas irregular or protruding teeth carry negative status.12 Children anticipating orthodontic treatment typically expect an improvement in their social and psychologic well-being and see an improvement in function as a secondary advantage of treatment.13 Appearance can and does make a difference in teachers’ expectations and therefore in student progress in school, in employability, and in competition for a mate. There is no doubt that social responses conditioned by the appearance of the face and teeth can severely affect an individual’s whole adaptation to life.14
This places the concept of “handicapping malocclusion” in a larger and more important context. If the way you interact with other individuals is affected constantly by your teeth, your dental handicap is far from trivial. Current data suggest that in a low-income (Medicaid) population, early partial treatment to improve rather than totally correct obvious malocclusions does produce psychosocial benefits.15
It is interesting that psychic distress caused by disfiguring dental or facial conditions is not directly proportional to the anatomic severity of the problem. An individual who is grossly disfigured can anticipate a consistently negative response. An individual with an apparently less severe problem (e.g., a protruding chin or irregular incisors) is sometimes treated differently because of this but sometimes not. It seems to be easier to cope with a defect if other people’s responses to it are consistent rather than if they are not. Unpredictable responses produce anxiety and can have strong deleterious effects.16
The impact of a physical defect on an individual also will be strongly influenced by that person’s self-esteem. The result is that the same degree of anatomic abnormality can be merely a condition of no great consequence to one individual but a genuinely severe problem to another. It seems clear that the major reason people seek orthodontic treatment is to minimize psychosocial problems related to their dental and facial appearance. These problems are not “just cosmetic.” They can have a major effect on the quality of life.
Oral Function
Although severe malocclusion surely affects oral function, oral function adapts to form surprisingly well. It appears that malocclusion usually affects function not by making it impossible but by making it difficult, so that extra effort is required to compensate for the anatomic deformity. For instance, everyone uses as many chewing strokes as it takes to reduce a food bolus to a consistency that is satisfactory for swallowing, so if chewing is less efficient in the presence of malocclusion, either the affected individual uses more effort to chew or settles for less well-masticated food before swallowing it. Tongue and lip posture adapt to the position of the teeth so that swallowing rarely is affected (see Chapter 5). Similarly, almost everyone can move the jaw so that proper lip relationships exist for speech, so distorted speech is rarely noted even though an individual may have to make an extraordinary effort to produce normal speech. As methods to quantify functional adaptations of this type are developed, it is likely that the effect of malocclusion on function will be appreciated more than it has been in the past.
The relationship of malocclusion and adaptive function to TMD, manifested as pain in and around the TM joint, is understood much better now than only a few years ago. The pain may result from pathologic changes within the joint but more often is caused by muscle fatigue and spasm. Muscle pain almost always correlates with a history of clenching or grinding the teeth as a response to stressful situations or of constantly posturing the mandible to an anterior or lateral position.
Some dentists have suggested that even minor imperfections in the occlusion serve to trigger clenching and grinding activities. If this were true, it would indicate a real need for perfecting the occlusion in everyone, to avoid the possibility of developing facial muscle pain. Because the number of people with at least moderate degrees of malocclusion (50% to 75% of the population) far exceeds the number with TMD (5% to 30%, depending on which symptoms are examined), it seems unlikely that dental occlusion alone is enough to cause hyperactivity of the oral musculature. A reaction to stress usually is involved. Some individuals react with clenching and grinding their teeth, while others develop symptoms in other organ systems. An individual almost never has both ulcerative colitis (also a common stress-induced disease) and TMD.
Some types of malocclusion (especially posterior crossbite with a shift on closure) correlate positively with TM joint problems and other types do not, but even the strongest correlation coefficients are only 0.3 to 0.4. This means that for the great majority of patients, there is no association between malocclusion and TMD.17 Therefore orthodontics as the primary treatment for TMD almost never is indicated, but in special circumstances (see Chapter 18) it can be a useful adjunct to other treatment for the muscle pain.
Relationship to Injury and Dental Disease
Malocclusion, particularly protruding maxillary incisors, can increase the likelihood of an injury to the teeth (Figure 1-18). There is about one chance in three that a child with an untreated Class II malocclusion will experience trauma to the upper incisors, but most of the time, the result is only minor chips in the enamel. For that reason, reducing the chance of injury when incisors protrude is not a strong argument for early treatment of Class II problems (see Chapter 13). Extreme overbite, so that the lower incisors contact the palate, can cause significant tissue damage leading to early loss of the upper incisors and also can result in extreme wear of incisors. Both of these effects can be avoided by orthodontic treatment (see Chapter 18).

FIGURE 1-18 Fractured maxillary central incisors in a 10-year-old girl. There is almost one chance in three of an injury to a protruding incisor, though fortunately the damage rarely is this severe. Most of the accidents occur during normal activity, not in sports.
It certainly is possible that malocclusion could contribute to both dental decay and periodontal disease by making it harder to care for the teeth properly or by causing occlusal trauma. Current data indicate, however, that malocclusion has little if any impact on diseases of the teeth or supporting structures. An individual’s willingness and motivation determine oral hygiene much more than how well the teeth are aligned, and presence or absence of dental plaque is the major determinant of the health of both the hard and soft tissues of the mouth. If individuals with malocclusion are more prone to tooth decay, the effect is small compared with hygiene status. Occlusal trauma, once thought to be important in the development of periodontal disease, now is recognized to be a secondary, not a primary, etiologic factor. There is only a tenuous link between untreated malocclusion and major periodontal disease later in life.
Could orthodontic treatment itself be an etiologic agent for oral disease? Long-term studies show no indication that orthodontic treatment increased the chance of later periodontal problems.18 The association between early orthodontic and later periodontal treatment appears to be only another manifestation of the phenomenon that one segment of the population seeks dental treatment while another avoids it. Those who have had one type of successful dental treatment, like orthodontics in childhood, are more likely to seek another like periodontal therapy in adult life.
In summary, it appears that both psychosocial and functional handicaps can produce significant need for orthodontic treatment. The evidence is less clear that orthodontic treatment reduces the development of later dental disease.
Type of Treatment: Evidence-Based Selection
If treatment is needed, how do you decide what sort of treatment to use? The present trend in health care is strongly toward evidence-based treatment; that is, treatment procedures should be chosen on the basis of clear evidence that the selected method is the most successful approach to that particular patient’s problem(s). The better the evidence, the easier the decision.
Randomized Clinical Trials: The Best Evidence
Orthodontics traditionally has been a specialty in which the opinions of leaders were important, to the point that professional groups coalesced around a strong leader. Angle, Begg, and Tweed societies still exist, and new ones whose primary purpose is to promulgate its leader’s opinions are still being formed in the early twenty-first century. As any professional group comes of age, however, there must be a focus on evidence-based rather than opinion-based decisions. This now is a major focus of organized dentistry in general and orthodontics in particular.
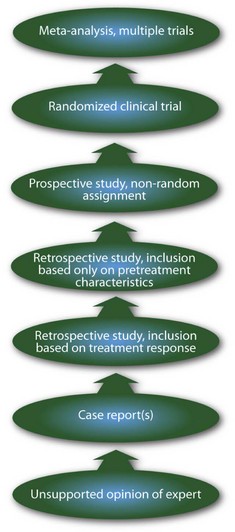
As Box 1-1 illustrates, a hierarchy of quality exists in the evidence available to guide clinical decisions. It reflects, more than anything else, the probability that an accurate conclusion can be drawn from the group of patients who have been studied. The unsupported opinion of an expert is the weakest form of clinical evidence. Often, the expert opinion is supported by a series of cases that were selected retrospectively from practice records.
The problem with that, of course, is that the cases are likely to have been selected because they show the expected outcome. A clinician who becomes an advocate of a treatment method is naturally tempted to select illustrative cases that show the desired outcome, and if even he or she tries to be objective, it is difficult to avoid introducing bias. When outcomes are variable, picking the cases that came out the way they were supposed to and discarding the ones that didn’t is a great way to make your point. Information based on selected cases, therefore, must be viewed with considerable reserve. One important way to control bias in reporting the outcomes of treatment is to be sure that all of the treated cases are included in the report.
If retrospective cases are used in a clinical study, it is much better to select them on the basis of their characteristics when treatment began, not on the outcome, and better yet to select the cases prospectively before treatment begins. Even then, it is quite possible to bias the sample so that the “right” patients are chosen. After experience with a treatment method, doctors tend to learn subtle indications that a particular patient is or is not likely to respond well, although they may have difficulty verbalizing exactly what criteria they used. Identifying the criteria associated with success or failure is extremely important, and a biased sample makes that impossible.
For this reason, the gold standard for evaluating clinical procedures is the randomized clinical trial, in which patients are randomly assigned in advance to alternative treatment procedures. The great advantage of this method is that random assignment, if the sample is large enough, should result in a similar distribution of all variables between (or among) the groups. Even variables that were not recognized in advance should be controlled by this type of patient assignment—and in clinical work, often important variables are identified only after the treatment has been started or even completed. The clinical trials in orthodontics that have been reported are referred to in some detail later in this book.
Unfortunately, randomized trials cannot be used in many situations for ethical or practical reasons. For instance, a randomized trial of extraction versus nonextraction orthodontic treatment would encounter ethical concerns, would be very difficult and expensive to organize and manage if ethical difficulties could be overcome, and would require following patients for many years to evaluate long-term outcomes.
Retrospective Studies: Control Group Required
A second acceptable way to replace opinion with evidence is by careful retrospective study of treatment outcomes under well-defined conditions. The best way to know—often the only way to know—whether a treatment method really works is to compare treated patients with an untreated control group. For such a comparison to be valid, the two groups must be equivalent before treatment starts. If the groups were different to start with, you cannot with any confidence say that differences afterward were due to the treatment.
There are a number of difficulties in setting up control groups for orthodontic treatment. The principal ones are that the controls must be followed over a long period of time, equivalent to the treatment time, and that sequential radiographs usually are required. Radiation exposure for untreated children is problematic. At present, it is very difficult to get permission to expose children to x-rays that will be of no benefit to them personally. This means that longitudinal growth studies of untreated children in the mid-twentieth century, now 50 or more years ago, still are being used to provide control data, especially in studies involving growth modification. When historic controls are the best that are available, it is better to have them than nothing, but the limitations must be kept in mind. A lot has changed in the last 50 years.
An additional way to gain better data for treatment responses is the application of metaanalysis. This draws on recently-developed statistical techniques to group the data from several studies of the same phenomenon. Orthodontic research is an excellent example of an area in which numerous small studies have been carried out toward similar ends, often with protocols that were at least somewhat similar but different enough to make comparisons difficult. Metaanalysis is no substitute for new data collected with precise protocols, and including poorly done studies in a metaanalysis carries the risk of confusing rather than clarifying the issue. Nevertheless, applying it to clinical questions has considerable potential to reduce uncertainty about the best treatment methods. Several recent reviews have taken advantage of this method to improve the quality of evidence about the outcomes of orthodontic treatment procedures.19-21
The era of orthodontics as an opinion-driven specialty clearly is at an end. In the future, it will be evidence-driven, which is all for the best. In the meantime, clinical decisions still must be made using the best information currently available. When the latest new method appears with someone’s strong recommendation and a series of case reports in which it worked very well, it is wise to remember the aphorism “Enthusiastic reports tend to lack controls; well-controlled reports tend to lack enthusiasm.”
In this and the subsequent chapters, recommendations for treatment are based insofar as possible on solid clinical evidence. Where this is not available, the authors’ current opinions are provided and labeled as such.
Demand for Treatment
Epidemiologic Estimates of Orthodontic Treatment Need
Psychosocial and facial considerations, not just the way the teeth fit, play a role in defining orthodontic treatment need. For this reason, it is difficult to determine who needs treatment and who does not just from an examination of dental casts or radiographs. Nevertheless, it seems reasonable that the severity of a malocclusion correlates with need for treatment. This assumption is necessary when treatment need is estimated for population groups.
Several indices for scoring how much the teeth deviate from the normal, as indicators of orthodontic treatment need, were proposed in the 1970s but not widely accepted for screening potential patients. The Index of Treatment Need (IOTN), developed by Shaw and coworkers in the United Kingdom,22 places patients in five grades from “no need for treatment” to “treatment need” that correlate reasonably well with clinician’s judgments of need for treatment. The index has a dental health component derived from occlusion and alignment (Box 1-2) and an esthetic component derived from comparison of the dental appearance to standard photographs (Figure 1-19). There is a surprisingly good correlation between treatment need assessed by the dental health and esthetic components of IOTN (i.e., children selected as needing treatment on one of the scales are also quite likely to be selected using the other).23

FIGURE 1-19 The stimulus photographs of the IOTN esthetic index. The score is derived from the patient’s answer to “Here is a set of photographs showing a range of dental attractiveness. Number 1 is the most attractive and number 10 the least attractive arrangement. Where would you put your teeth on this scale?” Grades 8 to 10 indicate definite need for orthodontic treatment, 5 to 7 moderate/borderline need, 1 to 4 no/slight need.
With some allowances for the effect of missing teeth, it is possible to calculate the percentages of U.S. children and youths who would fall into the various IOTN grades from the NHANES III data set.24 Figure 1-20 shows the percentage of youths age 12 to 17 in the three major racial/ethnic groups in the U.S. population estimated by IOTN to have mild/moderate/severe treatment need and the percentage who had treatment at that time. As the graph shows, the number of white children who received treatment was considerably higher than blacks or Hispanics (p < .001). Treatment almost always produces an improvement but may not totally eliminate all the characteristics of malocclusion, so the effect is to move some individuals from the severe to the mild treatment need categories. The higher proportion of severe malocclusion among blacks probably reflects more treatment in the white group, which moved them down the severity scale, rather than the presence of more severe malocclusion in the black population.
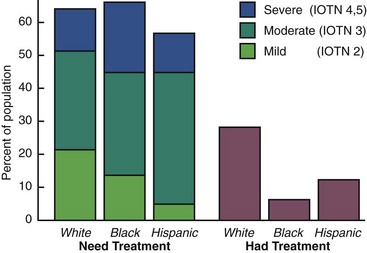
FIGURE 1-20 Orthodontic need by severity of the problem for white, black, and Mexican-American youths age 12 to 17 in the United States 1989-1994 and the percentage of each group who report receiving orthodontic treatment. The greater number of whites who receive treatment probably accounts for the smaller number of severe problems in the white population.
How do the IOTN scores compare with what parents and dentists think relative to orthodontic treatment need? The existing (rather weak) data suggest that in typical American neighborhoods, about 35% of adolescents are perceived by parents and peers as needing orthodontic treatment. Note that this is larger than the number of children who would be placed in IOTN grades 4 and 5 as severe problems definitely needing treatment, but smaller than the total of grades 3, 4, and 5 for moderate and severe problems.
Dentists usually judge that only about one-third of their patients have normal occlusion, and they suggest treatment for about 55% (thereby putting about 10% in a category of malocclusion with little need for treatment). It appears that they would include all the children in IOTN grade 3 and some of those in grade 2 in the group who would benefit from orthodontics. Presumably, facial appearance and psychosocial considerations are used in addition to dental characteristics when parents judge treatment need or dentists decide to recommend treatment.
Who Seeks Treatment?
Demand for treatment is indicated by the number of patients who actually make appointments and seek care. Not all patients with malocclusion, even those with extreme deviations from the normal, seek orthodontic treatment. Some do not recognize that they have a problem; others feel that they need treatment but cannot afford it or cannot obtain it.
Both the perceived need and demand vary with social and cultural conditions. More children in urban areas are thought (by parents and peers) to need treatment than children in rural areas. Family income is a major determinant of how many children receive treatment (Figure 1-21). This appears to reflect two things: not only that higher income families can more easily afford orthodontic treatment, but also that good facial appearance and avoidance of disfiguring dental conditions are associated with more prestigious social positions and occupations. The higher the aspirations for a child, the more likely the parents are to seek orthodontic treatment for him or her. It is widely recognized that severe malocclusion can affect an individual’s entire life adjustment, and every state now provides at least some orthodontic treatment for low-income families through its Medicaid program, but Medicaid and related programs support only a tiny fraction of the population’s orthodontic care. From that perspective, it is interesting that even in the lowest income group almost 5% of the youths and over 5% of adults report receiving treatment, with 10% to 15% treated at intermediate income levels. This indicates the importance placed on orthodontic treatment by families who judge that it is a factor in social and career progress for their children.
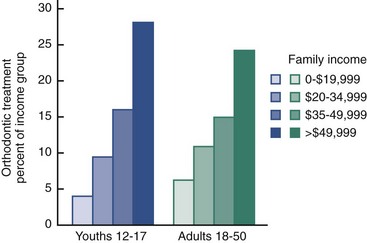
FIGURE 1-21 The percentage of the U.S. population 1989-1994 who received orthodontic treatment, as a function of family income. Although severe malocclusion is recognized as an important problem and all states offer at least some coverage to low-income children through their Medicaid programs, this funds treatment for a very small percentage of the population. Nevertheless, nearly 5% of the lowest income group and 10% to 15% of intermediate income groups have had some orthodontic treatment. This reflects the importance given to orthodontic treatment—it is sought even when it stretches financial resources in less-affluent families.
The effect of financial constraints on demand can be seen most clearly by the response to third-party payment plans. When third-party copayment is available, the number of individuals seeking orthodontic treatment rises considerably, but even when all costs are covered, some individuals for whom treatment is recommended do not accept it. It seems likely that under optimal economic conditions, demand for orthodontic treatment will at least reach the 35% level thought by the public to need treatment. In higher socioeconomic areas in the United States, 35% to 50% of children and youths now are receiving orthodontic care.
Orthodontic treatment for adults was rare until the latter half of the twentieth century. As late as the 1960s, only 5% of all orthodontic patients were adults (age 19 or older) (Figure 1-22). By 1990, about 25% of all orthodontic patients were adults (18 or older). Interestingly, the absolute number of adults seeking orthodontic treatment remained constant for the next decade while the number of younger patients grew, so by 2000 the proportion of adults in the orthodontic patient population had dropped to about 20%. The most recent estimates (2010) suggest that it has increased again to over 25% of the total.
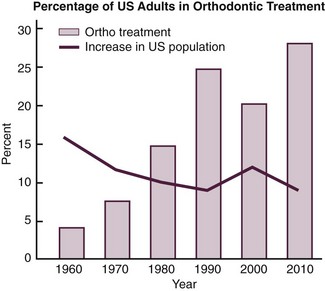
FIGURE 1-22 From the mid-twentieth century when almost no adults received orthodontic treatment, to the present time when adults comprise 25% to 30% of the total treatment population, there has been an almost steady rise in the number of adult patients. This does not at all parallel the percentage increase in the total population. In the 1980s, a “baby bust” period, the increasing number of adult patients was the major source of the overall increase in orthodontics, while in the 1990s, a “baby boom” period, the number of adult patients increased a little but most of the growth was treatment of children. There has been a further increase in treatment of adults in the first decade of the twenty-first century.
Many of these adult patients indicate that they wanted treatment earlier but did not receive it, often because their families could not afford it; now they can. Wearing braces as an adult is more socially acceptable than it was previously, though no one really knows why, and this too has made it easier for adults to seek treatment. Recently, an increased number of older adults (40 and over) have sought orthodontics, usually in conjunction with other treatment, to save their teeth. In 2006, 4.2% of all orthodontic patients were over 40; 20% of that group were over 60, and the majority of that oldest subgroup were male (every other age group from childhood on has more females). As the population ages, these older adults are likely to be the fastest-growing group who seek orthodontic treatment.
Many of the children and adults who seek orthodontic treatment today have dentofacial conditions that are within the normal range of variation, at least by definitions that focus tightly on obvious degrees of handicap. Does that mean treatment is not indicated for those with lesser problems? Today, medical and dental interventions that are intended to make the individual either “better than well” or “beyond normal” are called enhancements. Typical medical and surgical enhancements are drugs to treat erectile dysfunction, face lifts, and hair transplants. In dentistry, a good example of enhancement is tooth bleaching.
In this context, orthodontics often can be considered an enhancement technology. It is increasingly accepted that appropriate care for individuals often should include enhancement to maximize their quality of life. If you really want it because you are convinced you need it, perhaps you really do need it—whether it is orthodontics or many other types of treatment. Both Medicaid/Medicare and many insurance companies now have accepted the reality that at least some enhancement procedures have to be accepted as reimbursable medical expenses. Similarly, when orthodontic benefits are included in insurance coverage, the need for treatment is no longer judged just by the severity of the malocclusion. The bottom line: enhancement is appropriate dental and orthodontic treatment, just as it is in other contexts.
Orthodontics has become a more prominent part of dentistry in recent years, and this trend is likely to continue. The vast majority of individuals who had orthodontic treatment feel that they benefited from the treatment and are pleased with the result. Not all patients have dramatic changes in dental and facial appearance, but nearly all recognize an improvement in both dental condition and psychologic well-being.
References
1. Corruccini, RS, Paciani, E. “Orthodontistry” and dental occlusion in Etruscans. Angle Orthod. 1989;59:61–64.
2. Kingsley, NW. Treatise on Oral Deformities as a Branch of Mechanical Surgery. New York: Appleton; 1880.
3. Angle, EH, Treatment of malocclusion of the teeth and fractures of the maxillae. Angle’s System, ed 6. . SS White Dental Mfg Co: Philadelphia, 1900.
4. Ackerman, JL, Proffit, WR, Sarver, DM. The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin Orthod Res. 1999;2:49–52.
5. Kelly, JE, Sanchez, M, Van Kirk, LE. An Assessment of the Occlusion of Teeth of Children. Washington, DC: National Center for Health Statistics; 1973. [DHEW Publication No. (HRA) 74-1612].
6. Kelly, J, Harvey, C. An Assessment of the Teeth of Youths 12-17 Years. Washington, DC: National Center for Health Statistics; 1977. [DHEW Pub No. (HRA) 77-1644].
7. Brunelle, JA, Bhat, M, Lipton, JA. Prevalence and distribution of selected occlusal characteristics in the US population, 1988-91. J Dent Res. 1996;75:706–713.
8. Baume, LJ. Uniform methods for the epidemiologic assessment of malocclusion. Am J Orthod. 1974;66:251–272.
9. Brown, T, Abbott, AA, Burgess, VB. Longitudinal study of dental arch relationships in Australian aboriginals with reference to alternate intercuspation. Am J Phys Anthropol. 1987;72:49–57.
10. Corruccini, RS. Anthropological aspects of orofacial and occlusal variations and anomalies. In: Kelly MA, Larsen CS, eds. Advances in Dental Anthropology. New York: Wiley-Liss; 1991.
11. Wrangham, R. Catching Fire: How Cooking Made Us Human. New York: Basic Books; 2009.
12. Shaw, WC, Rees, G, Dawe, M, et al. The influence of dentofacial appearance on the social attractiveness of young adults. Am J Orthod. 1985;87:21–26.
13. Bresnahan, B, Kiyak, A, Masters, SH, et al. Quality of life and economic burdens of malocclusion in US patients enrolled in. Medicaid. J Am Dent Assn. 2010;141:1202–1212.
14. Meyer-Marcotty, P, Gerdes, AB, Reuther, T, et al. Persons with cleft lip and palate are looked at differently. J Dent Res. 2010;89:400–404.
15. Jolley, C, Huang, GJ, Greenlee, G, et al. Dental effects of interceptive orthodontic treatment in a Medicaid population: interim results from a randomized clinical trial. Am J Orthod Dentofac Orthop. 2010;137:324–333.
16. Macgregor, FC. Social and psychological implications of dentofacial disfigurement. Angle Orthod. 1979;40:231–233.
17. Macfarlane, TV, Kenealy, P, Kingdon, HA, et al. Twenty-year cohort study of health gain from orthodontic treatment: temporomandibular disorders. Am J Orthod Dentofac Orthop. 2009;192:e1–e8.
18. Jonsson, T, Karlsson, KO, Ragnarsson, B, et al. Long-term development of malocclusion traits in orthodontically treated and untreated subjects. Am J Orthod Dentofac Orthop. 2010;137:277–284.
19. Bollen, AM, Cunha-Cruz, J, Bakko, DW, et al. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. Am J Orthod Dentofac Orthop. 2008;135:413–422.
20. Liu, Z, McGrath, C, Haag, U. The impact of malocclusion/orthodontic treatment need on the quality of life: a systematic review. Angle Orthod. 2009;79:585–591.
21. Weltman, B, Vig, KWL, Fields, HW, et al. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofac Orthop. 2010;137:462–476.
22. Brook, PH, Shaw, WC. The development of an index for orthodontic treatment priority. Eur J Orthod. 1989;11:309–332.
23. Richmond, S, Shaw, WC, O’Brien, KD, et al. The relationship between the index of treatment need and consensus opinion of a panel of 74 dentists. Br Dent J. 1995;178:370–374.
24. Proffit, WR, Fields, HW, Moray, LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthod Orthogn Surg. 1998;13:97–106.