Special Considerations in Treatment for Adults
Adults who seek orthodontic treatment fall into two quite different groups: (1) younger adults (typically under 35, often in their 20s) who desired but did not receive comprehensive orthodontic treatment as youths and now seek it as they become financially independent and (2) an older group, typically in their 40s or 50s, who have other dental problems and need orthodontics as part of a larger treatment plan. For the first group, the goal is to improve their quality of life. They usually seek the maximum improvement that is possible. They may or may not need extensive treatment by other dental specialists but frequently need interdisciplinary consultation.
The second group seek to maintain what they have, not necessarily to achieve as ideal an orthodontic result as possible. For them, orthodontic treatment is needed to meet specific goals that would make control of dental disease and restoration of missing teeth easier and more effective, so the orthodontics is an adjunctive procedure to the larger periodontal and restorative goals. Until recently, the younger group has comprised most adult orthodontic patients. Because of the large number of aging “baby boomers” born during the immediate post-World War II era, it was easy to predict increasing demand for orthodontics from the second group in the early part of the twenty-first century, and this is occurring. Treatment for older adults has been the fastest growing area in orthodontics during the last decade.
Adjunctive orthodontic treatment, particularly the simpler procedures, often can and should be carried out within the context of general dental practice, and the first part of Chapter 18 is written with that in mind. This discussion does not require familiarity with the principles of comprehensive orthodontic treatment, but it does presume an understanding of orthodontic diagnosis and treatment planning.
In contrast, the discussion of comprehensive treatment for adults in the latter part of Chapter 18 builds on the principles discussed in Chapters 14 to 16 and focuses on the aspects of comprehensive treatment for adults that are different from treatment for younger patients. Comprehensive orthodontics for adults tends to be difficult and technically demanding. The absence of growth means that growth modification to treat jaw discrepancies is not possible. The only possibilities are tooth movement for camouflage or orthognathic surgery, but applications of skeletal anchorage now are broadening the scope of orthodontics to include some patients who would have required surgery even a few years ago. Applications of skeletal anchorage are discussed and illustrated in detail in this chapter; a discussion of skeletal anchorage versus surgery follows in Chapter 19.
Adjunctive Versus Comprehensive Treatment
Adjunctive orthodontic treatment for adults is, by definition, tooth movement carried out to facilitate other dental procedures necessary to control disease, restore function, and/or enhance appearance. Usually, it involves only a part of the dentition, and the primary goal usually is to make it easier or more effective to replace missing or damaged teeth. Making it easier for the patient to control periodontal problems is a frequent secondary goal and sometimes is the primary goal. The treatment duration tends to be a few months, rarely more than a year, and long-term retention usually is supplied by the restorations.
With the distinction made in this way, much of the adjunctive treatment discussed in this chapter can be carried out within the context of general dental practice, and the first part of this chapter is written from that perspective. Adjunctive procedures that probably should be done by an orthodontist are labeled as such. Whether one or several practitioners are involved, adjunctive orthodontics must be coordinated carefully with the periodontal and restorative treatment.
In contrast, the goal of comprehensive orthodontics for adults is the same as for adolescents: to produce the best combination of dental and facial appearance, dental occlusion, and stability of the result to maximize benefit to the patient. Typically, comprehensive orthodontics requires a complete fixed orthodontic appliance, intrusion of some teeth is likely to be needed, orthognathic surgery may be considered to improve jaw relationships, and the duration of treatment from braces on to braces off exceeds 1 year. Adults receiving comprehensive treatment are the main candidates for esthetically enhanced appliances; the prime examples are ceramic facial brackets, clear aligners, and lingual appliances. The complexity of the treatment procedures means that an orthodontic specialist is likely to be significantly more efficient in delivering the care.
Goals of Adjunctive Treatment
Typically, adjunctive orthodontic treatment will involve any or all of several procedures: (1) repositioning teeth that have drifted after extractions or bone loss so that more ideal fixed or removable partial dentures can be fabricated or so that implants can be placed, (2) alignment of anterior teeth to allow more esthetic restorations or successful splinting, while maintaining good interproximal bone contour and embrasure form, (3) correction of crossbite if this compromises jaw function (not all crossbites do), and (4) forced eruption of badly broken down teeth to expose sound root structure on which to place crowns or to level/regenerate alveolar bone.
Whatever the occlusal status originally, the goals of adjunctive treatment should be to:
1. Improve periodontal health by eliminating plaque-harboring areas and improving the alveolar ridge contour adjacent to the teeth.
2. Establish favorable crown-to-root ratios and position the teeth so that occlusal forces are transmitted along the long axes of the teeth.
3. Facilitate restorative treatment by positioning the teeth so that:
An old rule says that to make it clear what something is, it helps to point out what it isn’t but might be mistaken for. So, some important corollaries:
• Orthodontic treatment for temporomandibular dysfunction (TMD) should not be considered adjunctive treatment.
• Although intrusion of teeth can be an important part of comprehensive treatment for adults, it probably should be managed by an orthodontist even as an adjunctive procedure because of the technical difficulties involved and the possibility of periodontal complications. As a general guideline in treatment of adults with periodontal involvement and bone loss, lower incisor teeth that are excessively extruded are best treated by reduction of crown height, which has the added advantage of improving the ultimate crown-to-root ratio of the teeth. For other teeth, tooth–lip relationships must be kept in mind when crown height reduction is considered.
• Crowding of more than 3 to 4 mm should not be attempted by stripping enamel from the contact surfaces of the anterior teeth. It may be advantageous to strip posterior teeth to provide space for alignment of the incisors, but this requires a complete orthodontic appliance and cannot be considered adjunctive treatment.
Principles of Adjunctive Treatment
Diagnostic and Treatment Planning Considerations
Planning for adjunctive treatment requires two steps: (1) collecting an adequate diagnostic data base and (2) developing a comprehensive but clearly stated list of the patient’s problems, taking care not to focus unduly on any one aspect of a complex situation. The importance of this planning stage in adjunctive orthodontic treatment cannot be overemphasized, since the solution to the patient’s specific problems may involve the synthesis of many branches of dentistry. In adjunctive treatment, the restorative dentist usually is the principal architect of the treatment plan, and the orthodontics (whether an orthodontist is or is not part of the treatment team) is to facilitate better restorative treatment.
Nevertheless, the steps outlined in Chapter 6 should be followed when developing the problem list. The interview and clinical examination are the same whatever the type of orthodontic treatment. Diagnostic records for adjunctive orthodontic patients, however, differ in several important ways from those for adolescents and children.
For this adult and dentally compromised population, the records usually should include individual intraoral radiographs to supplement the panoramic radiograph that often suffices for younger and healthier patients (Figure 18-1). When active dental disease is present, the panoramic radiograph does not give sufficient detail. The revised guidelines from the U.S. Food and Drug Administration in late 2004 (see Table 6-5) should be followed in determining exactly what radiographs are required in evaluating the patient’s oral health status. The American Board of Orthodontics now requires evidence of pretreatment periodontal condition for all adult patients.1

FIGURE 18-1 A and B, For the periodontically compromised adults who are the usual candidates for adjunctive orthodontics, periapical radiographs of the areas that will be treated, as well as a panoramic radiograph, usually are needed. Periodontal disease now is the major indication for periapical radiographs. For this patient who is a candidate for adjunctive orthodontic treatment, adequate detail of root morphology, dental disease, and periodontal breakdown is obtained only from carefully taken periapical radiographs.
For adjunctive orthodontics with a partial fixed appliance, pretreatment cephalometric radiographs usually are not required, but it is important to anticipate the impact of various tooth movements on facial esthetics. In some instances, the computer prediction methods used in comprehensive treatment (see Chapter 7) can be quite useful in planning adjunctive treatment. Articulator-mounted casts are likely to be needed because they facilitate the planning of associated restorative procedures.
Once all of the problems have been identified and categorized, the key treatment planning question is: can the occlusion be restored within the existing tooth positions or must some teeth be moved to achieve a satisfactory, stable, healthy, and esthetic result? The goal of providing a physiologic occlusion and facilitating other dental treatment has little to do with Angle’s concept of an ideal occlusion. At this point, it is important to consider the difference between realistic and idealistic treatment planning. In older patients, searching for an “ideal” result could involve more treatment than would really benefit the patient.
Obviously, the time needed for any orthodontic treatment depends on the severity of the problem and the amount of tooth movement desired, but with efficient use of orthodontic appliances, it should be possible to reach the objectives of adjunctive treatment within 6 months. As a practical matter, this means that like comprehensive orthodontics, most adjunctive orthodontics cannot be managed well with traditional removable appliances. It requires either fixed appliances or a sequence of clear aligners to get the job done in a reasonable period of time. In addition, it is becoming increasingly apparent that skeletal anchorage makes adjunctive tooth movement more effective and efficient. For adjunctive treatment, this is almost always in the form of alveolar bone screws.
Biomechanical Considerations
Characteristics of the Orthodontic Appliance
When a partial fixed appliance is to be used for adjunctive treatment, with the possible exception of alignment of anterior teeth, we recommend the 22-slot edgewise appliance with twin brackets. The rectangular (edgewise) bracket slot permits control of buccolingual axial inclinations, the relatively wide bracket helps control undesirable rotations and tipping, and the larger slot size allows the use of stabilizing wires that are somewhat stiffer than ordinarily might be used in comprehensive treatment.
Recently, further developments in clear aligner therapy (CAT [see Chapter 10]) have provided an effective type of removable appliance that can be well suited to alignment of anterior teeth. Removable appliances of the traditional plastic-and-wire type are rarely satisfactory for adjunctive (or comprehensive) treatment. They often are uncomfortable and are likely to be worn for too few hours per day to be effective. With CAT, both discomfort and interference with speech and mastication are minimized, and patient cooperation improves. A fixed appliance on posterior teeth only is all but invisible, but it is quite apparent on anterior teeth, and the better appearance of a clear aligner also is a factor in choosing it to align anterior teeth.
Despite this esthetic advantage, there are biomechanical limitations. Control of root position is extremely difficult with clear aligners, and it also is difficult to correct rotations and to extrude teeth.2 If these limitations are not important in a particular adjunctive case, CAT can be considered. If they are, in nearly all cases adults who are candidates for adjunctive treatment will accept a lingual appliance or a visible fixed appliance.3
Modern edgewise brackets of the straight-wire type are designed for a specific location on an individual tooth. Placing the bracket in its ideal position on each tooth implies that every tooth will be repositioned if necessary to achieve ideal occlusion (Figure 18-2, A). Since adjunctive treatment is concerned with only limited tooth movements, usually it is neither necessary nor desirable to alter the position of every tooth in the arch. For this reason, in a partial fixed appliance for adjunctive treatment, the brackets are placed in an ideal position only on teeth to be moved, and the remaining teeth to be incorporated in the anchor system are bracketed so that the archwire slots are closely aligned (Figure 18-2, B). This allows the anchorage segments of the wire to be engaged passively in the brackets with little bending. Passive engagement of wires to anchor teeth produces minimal disturbance of teeth that are in a physiologically satisfactory position. This important point is illustrated in more detail in the sections on specific treatment procedures that follow.
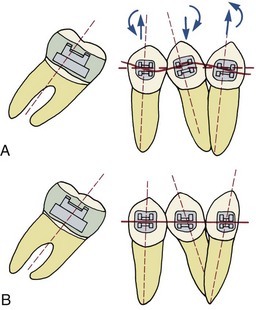
FIGURE 18-2 A, Brackets placed in the “ideal” position on moderately irregular anchor teeth for molar uprighting. For adjunctive orthodontic treatment, movement of the anchor teeth usually is undesirable, but a straight length of wire will move them if the brackets are positioned in this way. B, Brackets placed in the position of maximum convenience, lined up so that a straight length of wire can be placed without moving the anchor teeth. This makes things easier if no movement of the anchor teeth is desired. For adjunctive orthodontic procedures like molar uprighting, we recommend the use of fully adjusted “straight-wire” 22-slot brackets and working archwires that are somewhat smaller than the bracket slot to reduce unwanted faciolingual movement of anchor teeth even though the brackets are lined up in the other planes of space.
Effects of Reduced Periodontal Support
Since patients who need adjunctive orthodontic treatment often have lost alveolar bone to periodontal disease before it was brought under control, the amount of bone support of each tooth is an important special consideration. When bone is lost, the periodontal ligament (PDL) area decreases, and the same force against the crown produces greater pressure in the PDL of a periodontally compromised tooth than a normally supported one. The absolute magnitude of force used to move teeth must be reduced when periodontal support has been lost. In addition, the greater the loss of attachment, the smaller the area of supported root and the further apical the center of resistance will become (Figure 18-3). This affects the moments created by forces applied to the crown and the moments needed to control root movement. In general terms, tooth movement is quite possible despite bone loss, but lighter forces and relatively larger moments are needed.
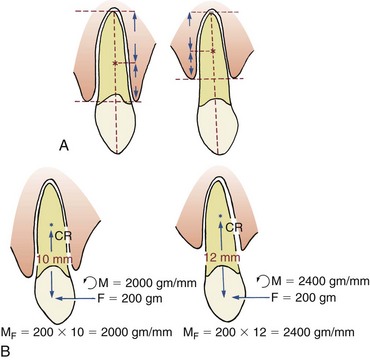
FIGURE 18-3 A, The center of resistance of a single-rooted tooth lies approximately six-tenths of the distance between the apex of the tooth and the crest of the alveolar bone. Loss of alveolar bone height, as for the tooth on the right, moves the center of resistance closer to the root apex. B, The magnitude of the tipping moment produced by a force is equal to the force times the distance from the point of force application to the center of resistance. If the center of resistance moves apically, the tipping moment produced by the force (MF) increases, and a larger countervailing moment produced by a couple applied to the tooth (MC) would be necessary to produce bodily movement. This is almost impossible to obtain with traditional removable appliances and very difficult with clear aligners, even when bonded attachments are added. For all practical purposes, a fixed appliance is required if root movement is the goal in patients who have experienced loss of alveolar bone height.
Timing and Sequence of Treatment
In the development of any orthodontic treatment plan, the first step is control of any active dental disease (Figure 18-4). Before any tooth movement, active caries and pulpal pathology must be eliminated, using extractions, restorative procedures, and pulpal or apical treatment as necessary. Endodontically treated teeth respond normally to orthodontic force, if all residual chronic inflammation has been eliminated.4 Prior to orthodontics, teeth should be restored with well-placed amalgams or composite resins. Restorations requiring detailed occlusal anatomy should not be placed until any adjunctive orthodontic treatment has been completed because the occlusion inevitably will be changed. This could necessitate remaking crowns, bridges, or removable partial dentures.
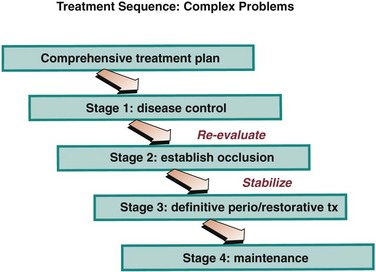
FIGURE 18-4 The sequence of steps in the treatment of patients requiring adjunctive orthodontics. Orthodontics is used to establish occlusion but only after disease control has been accomplished, and the occlusion should be stabilized before definitive restorative treatment is carried out.
Periodontal disease also must be controlled before any orthodontics begins because orthodontic tooth movement superimposed on poorly controlled periodontal health can lead to rapid and irreversible breakdown of the periodontal support apparatus.5 Scaling, curettage (by open flap procedures, if necessary), and gingival grafts should be undertaken as appropriate. Surgical pocket elimination and osseous surgery should be delayed until completion of the orthodontic phase of treatment because significant soft tissue and bony recontouring occurs during orthodontic tooth movement. Clinical studies have shown that orthodontic treatment of adults with both normal and compromised periodontal tissues can be completed without loss of attachment, if there is good periodontal therapy both initially and during tooth movement.6
During this preparatory phase, the patient’s enthusiasm for treatment and ability to maintain good overall oral hygiene should be carefully monitored. Adjunctive orthodontics has the potential to do more harm than good in patients who cannot or will not maintain good oral hygiene. If disease can be controlled, however, adjunctive orthodontics can significantly improve the final restorative and periodontal procedures.
Adjunctive Treatment Procedures
Treatment Planning Considerations
When a first permanent molar is lost during childhood or adolescence and not replaced, the second molar drifts mesially and the premolars often tip distally and rotate as space opens between them. As the teeth move, the adjacent gingival tissue becomes folded and distorted, forming a plaque-harboring pseudopocket that may be virtually impossible for the patient to clean (Figure 18-5). Repositioning the teeth eliminates this potentially pathologic condition and has the added advantage of simplifying the ultimate restorative procedures.
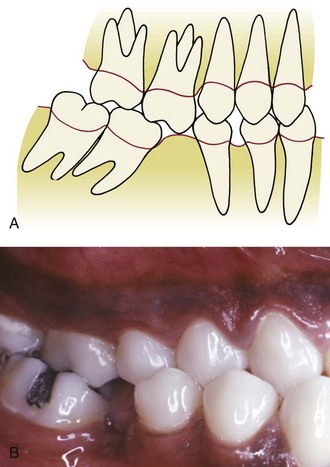
FIGURE 18-5 A, Loss of a lower molar can lead to tipping and drifting of adjacent teeth, poor interproximal contacts, poor gingival contour, reduced interradicular bone, and supra-eruption of unopposed teeth. Since the bone contour follows the cementoenamel junction, pseudopockets form adjacent to the tipped teeth. B, Note the loss of alveolar bone in the area where a mandibular first molar was extracted many years previously. Mesial drift and tipping of the second molar has closed half the space. The patient’s posterior crossbite, however, is unrelated to early loss of the molar.
When molar uprighting is planned, a number of interrelated questions must be answered:
• If the third molar is present, should both the second and third molars be uprighted? For many patients, distal positioning of the third molar would move it into a position in which good hygiene could not be maintained or it would not be in functional occlusion. In these circumstances, it is more appropriate to extract the third molar and simply upright the remaining second molar tooth. If both molars are to be uprighted, a significant change in technique is required, as described below.
• How should the tipped teeth be uprighted? By distal crown movement (tipping), which would increase the space available for a bridge pontic or implant (Figure 18-6), or by mesial root movement, which would reduce or even close the edentulous space? As a general rule, treatment by distal tipping of the second molar and a bridge or implant to replace the first molar is preferred. If extensive ridge resorption has already occurred, particularly in the buccolingual dimension, closing the space by mesial movement of a wide molar root into the narrow alveolar ridge will proceed very slowly. If uprighting with space closure is to be done successfully, skeletal anchorage in the form of a temporary skeletal anchorage often is needed, and the treatment time is likely to be around 3 years (see Figure 18-37).
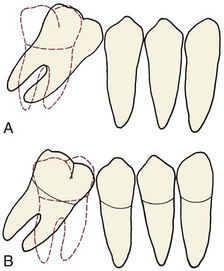
FIGURE 18-6 A, Uprighting a tipped molar by distal crown movement leads to increased space for a bridge pontic or implant, whereas uprighting the molar by mesial root movement (B) reduces space and might eliminate the need for a prosthesis, but this tooth movement can be very difficult and time-consuming to accomplish, especially if the alveolar bone has resorbed in the area where a first molar was extracted many years previously (see Figure 18-36).
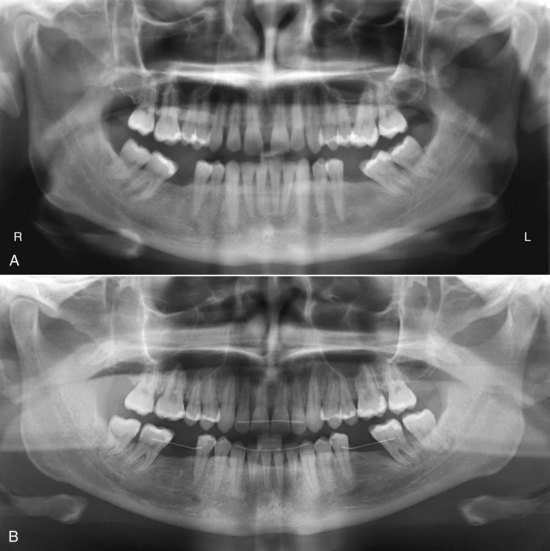
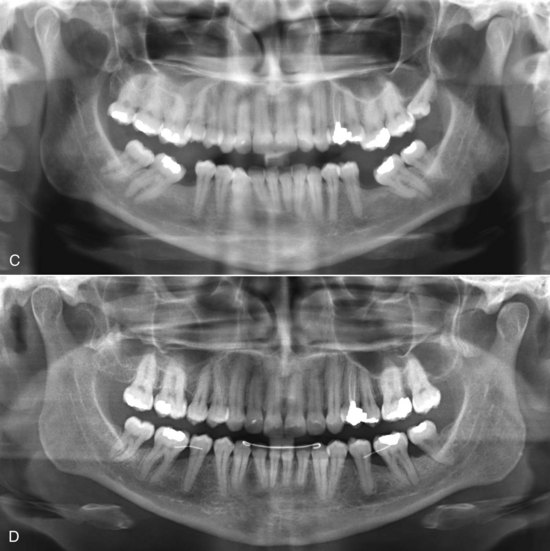
FIGURE 18-37 A, Panoramic radiograph of a 32-year-old patient who lost mandibular first molars years ago and now desired treatment to correct her malocclusion. She chose comprehensive fixed appliance treatment, including uprighting of both the second and third molars, opening space for replacement of the missing first molars with either implants or fixed bridges. Treatment time was 30 months. It would not have taken that long to only upright the molars, but uprighting two molars on each side takes much longer than uprighting only one molar, and it is difficult to maintain the occlusal relationships without a maxillary appliance. B, Posttreatment radiograph. Uprighting the second molar does not create new bone but does tend to improve the periodontal condition; in this patient the persisting one-wall pocket on the mesial of the left second molar is much more treatable than it would have been without the uprighting. Note that fixed retainers are being used to maintain both incisor alignment and the position of the molars until restorations can be placed. C, Panoramic radiograph of a 39-year-old patient who also lost mandibular first molars years ago. Comprehensive orthodontics was planned to align the anterior teeth in both arches, correct the supereruption of the maxillary first molars, and close the old extraction spaces. D, After completion of treatment, which required 36 months primarily because tooth movement into old extraction spaces like this requires remodeling of cortical bone. Note that the periodontal situation on the mesial of the second molars remains less than ideal and that fixed retainers are being used to maintain closure of the extraction spaces, as well as incisor alignment. (Courtesy Dr. D. Grauer.)
• Is extrusion of a tipped molar permissible? Uprighting a mesially tipped tooth by tipping it distally, which leaves the root apex in its pretreatment position, also extrudes it. This has the merit of reducing the depth of the pseudopocket found on the mesial surface, and since the attached gingiva follows the cementoenamel junction while the mucogingival junction remains stable, it also increases the width of the keratinized tissue in that area. In addition, if the height of the clinical crown is systematically reduced as uprighting proceeds, the ultimate crown–root length ratio will be improved (Figure 18-7). Unless slight extrusion or crown–height reduction is acceptable, which usually is the case, the patient should be considered to have problems that require comprehensive treatment and treated accordingly.
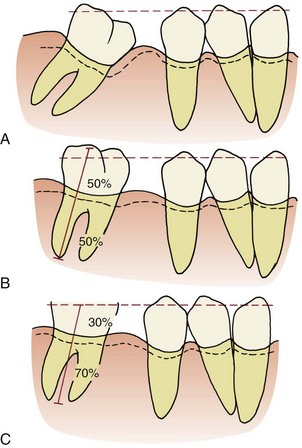
FIGURE 18-7 A to C, Uprighting a tipped molar increases the crown height while it reduces the depth of the mesial pocket. Subsequent crown reduction decreases occlusal interference and also improves the ratio of crown height to supported root length of the molar, so reducing the height of the molar crown is a routine part of molar uprighting.
• Should the premolars be repositioned as part of the treatment? This will depend on the position of these teeth and the restorative plan, but in many cases the answer is yes. It is particularly desirable to close spaces between premolars when uprighting molars because this will improve both the periodontal prognosis and long-term stability. In some instances, uprighting the molar and then moving the premolar back against it will provide a better site mesial to the premolar for an implant.
In molar uprighting, the treatment time will vary with the type and extent of the tooth movement required. Uprighting one second molar by distal crown tipping proceeds much more rapidly than mesial root movement. Failure to eliminate occlusal interferences will prolong treatment. The simplest cases should be completed in 8 to 10 weeks, but uprighting two molars in the same quadrant by tipping them distally could easily take 6 months, and the complexity of doing this puts it at the outer limit of adjunctive treatment with a partial fixed appliance.
Appliances for Molar Uprighting
A partial fixed appliance to upright tipped molars consists of bonded brackets on the premolars and canine in that quadrant and either a bonded rectangular tube on the molar or a molar band. A general guideline is that molar bands are best when the periodontal condition allows, which means for all practical purposes they would be used in younger and healthier patients. The greater the degree of periodontal breakdown around the molar to be uprighted, the more a bonded attachment should be considered.
Where premolar and canine brackets should be placed depends on the intended tooth movement and occlusion. If these teeth are to be repositioned, the brackets should be placed in the ideal position at the center of the facial surface of each tooth. However, if the teeth are merely serving as anchor units and no repositioning is planned, then the brackets should be placed in the position of maximum convenience where minimum wire bending will be required to engage a passive archwire (see Figure 18-2).
Distal crown tipping: If the molar is only moderately tipped, treatment often can be accomplished with a flexible rectangular wire. The best choice is 17 × 25 austenitic nickel–titanium (A-NiTi) that delivers approximately 100 gm of force (see Chapter 10). With this material, a single wire may complete the necessary uprighting (Figure 18-8). A braided rectangular steel wire also can be used but is more likely to require removal and reshaping. It is important to relieve the occlusion as the tooth tips upright. Failure to do this may cause excessive tooth mobility and increases treatment time.
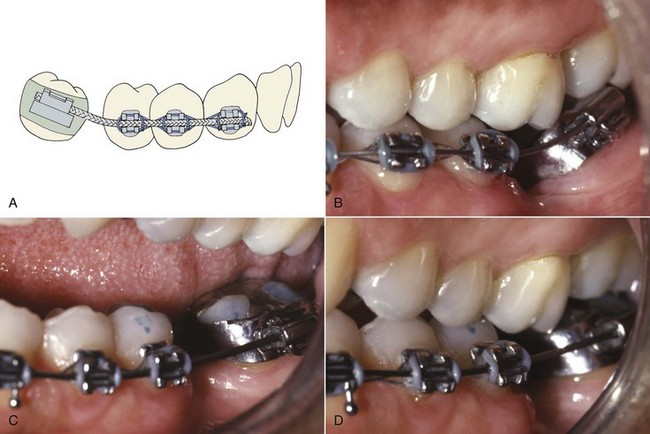
FIGURE 18-8 Fixed appliance technique for uprighting one molar with a continuous flexible wire. A, Initial bracket alignment is achieved by placing a light flexible wire such as 17 × 25 A-NiTi, from molar to canine. B, Molar uprighting with a continuous M-NiTi wire. C, Progress 1 month later. D, Uprighting essentially completed 2 months later.
If the molar is severely tipped, a continuous wire that uprights the molar will have side effects (which almost always are undesirable) on the position and inclination of the second premolar. For that reason it is better to carry out the bulk of the uprighting using a sectional uprighting spring (Figure 18-9). After preliminary alignment of the anchor teeth if necessary, stiff rectangular wire (19 × 25 steel) maintains the relationship of the teeth in the anchor segment, and an auxiliary spring is placed in the molar auxiliary tube. The uprighting spring is formed from either 17 × 25 beta-Ti wire without a helical loop or 17 × 25 steel wire with a loop added to provide more springiness. The mesial arm of the helical spring should be adjusted to lie passively in the vestibule and upon activation should hook over the archwire in the stabilizing segment. It is important to position the hook so that it is free to slide distally as the molar uprights. In addition, a slight lingual bend placed in the uprighting spring is needed to counteract the forces that tend to tip the anchor teeth buccally and the molar lingually (Figure 18-9, C).
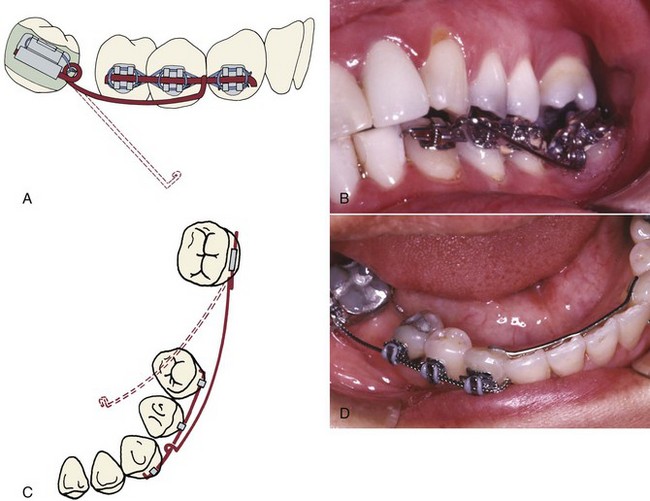
FIGURE 18-9 Uprighting with an auxiliary spring. A, If the relative alignment of the molar precludes extending the stabilizing segment into the molar bracket, then a rigid stabilizing wire, 19 × 25 stainless steel, is placed in the premolars and canine only (often with the brackets positioned so this wire is passive—see Figure 18-2). The mesial arm of the uprighting spring lies in the vestibule before engagement, and the spring is activated by lifting the mesial arm and hooking it over a stabilizing wire in the canine and premolar brackets. B, Auxiliary uprighting spring to molar just after initial placement. Note the helix bent into the steel wire that forms the spring to provide better spring qualities. C, Because the force is applied to the facial surface of the teeth, an auxiliary uprighting spring tends not only to extrude the molar but also to roll it lingually, while intruding the premolars and flaring them buccally. To counteract this side effect, the uprighting spring should be curved buccolingually so that when it is placed into the molar tube, the hook would lie lingually to the archwire prior to activation (dotted line). D, Better control of anchorage, with either a continuous wire or an auxiliary spring, is obtained when a canine-to-canine stabilizing wire is bonded on the lingual surface of these teeth.
Mesial root movement: If a mesial root movement is desired, an alternative treatment approach is indicated. Skeletal anchorage is required if the goal is to close the old extraction space (see Figure 18-36). If a small amount of mesial movement to prevent opening too much space is the goal, a single “T-loop” sectional archwire of 17 × 25 stainless steel or 19 × 25 beta-titanium (beta-Ti) wire can be effective (Figure 18-10). After initial alignment of the anchor teeth with a light flexible wire, the T-loop wire is adapted to fit passively into the brackets on the anchor teeth and gabled at the T to exert an uprighting force on the molar. Insertion into the molar can be from the mesial or distal. If the treatment plan calls for maintaining or closing rather than increasing the pontic space, the distal end of the archwire should be pulled distally through the molar tube, opening the T-loop by 1 to 2 mm, and then bent sharply gingivally to maintain this opening. This activation provides a mesial force on the molar that counteracts distal crown tipping while the tooth uprights (Figure 18-10, D). If opening the space is desired, the end of the wire is not bent over so the tooth can slide distally along it.
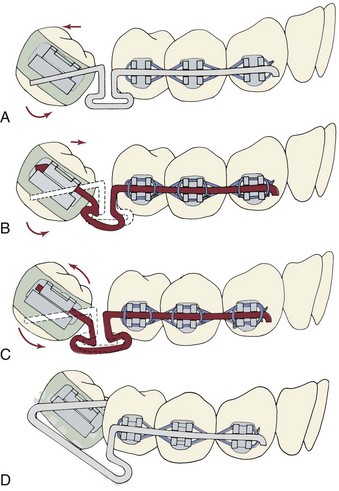
FIGURE 18-10 A, T-loop spring in 17 × 25 steel wire, showing the degree of angulation of the wire before inserting it into the molar tube that is necessary to upright a single-tipped molar. B, If a T-loop is activated by pulling the distal of the wire through the molar tube and bending it, the tooth cannot move distally. This generates a moment that results in molar uprighting by mesial root movement with space closure. C, A T-loop for uprighting by distal tipping. Note that the tooth can move back by sliding along the wire. D, Modification of a T-loop that can be used to upright a severely tipped or rotated molar by distal tipping. The wire is inserted into the distal end of the tube on the molar. The additional wire in the loop provides a longer range of action, but the uprighting still is by distal crown tipping.
The T-loop appliance also is indicated if the molar to be uprighted is severely tipped but has no occlusal antagonist. In that circumstance, a T-loop minimizes the extrusion that accompanies uprighting, which can be excessive with the other methods when there is no antagonist.
Final positioning of molar and premolars: Once molar uprighting is almost complete, often it is desirable to increase the available pontic space and close open contacts in the anterior segment. This is done best using a relatively stiff base wire, with a compressed coil spring threaded over the wire to produce the required force system. With 22-slot brackets, the base wire should be 18 mil round or 17 × 25 rectangular steel wire, which should engage the anchor teeth and the uprighted molar more or less passively. The wire should extend through the molar tube, projecting about 1 mm beyond the distal. An open coil steel spring (.009 wire, .030 lumen) is cut so that it is 1 to 2 mm longer than the space, slipped over the base wire (Figure 18-11), and compressed between the molar and distal premolar. It should exert a force of approximately 150 gm to move the premolars mesially while continuing to tip the molar distally. The coil spring can be reactivated without removing it by compressing the spring and adding a split stop to maintain the compression (Figure 18-11, B).
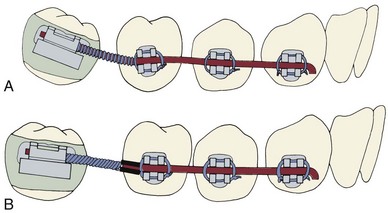
FIGURE 18-11 A, A compressed coil spring on a round wire (usually 18 mil steel) may be used to complete molar uprighting while closing remaining spaces in the premolar region. B, The coil spring can be reactivated by compressing it against a split spacer crimped over the archwire just behind the premolar bracket.
Uprighting Two Molars in the Same Quadrant
Because the resistance offered when uprighting two molars is considerable, only small amounts of space closure should be attempted. Unless comprehensive orthodontics with a complete fixed appliance is planned, the goal should be a modest amount of distal crown tipping of both teeth, which typically would leave space for a premolar-sized implant or pontic. In the lower arch, a bonded canine-to-canine lingual stabilizing wire (which is similar to a bonded retainer) is needed to control the position of the anterior teeth (see Figure 18-9, D). Trying to upright both the second and third molars bilaterally at the same time is not a good idea—significant movement of the anchor teeth is inevitable unless skeletal anchorage is used.
When both the second and third molars are to be uprighted, the third molar should carry a single rectangular tube and the second molar a bracket. Since the second molar is usually more severely tipped than the third molar, increased flexibility of the wire mesial and distal to the second molar is required. The best approach is to use a highly flexible wire initially—17 × 25 A-NiTi usually is a good choice. Excessive mobility of the teeth can result from failure to reduce occlusal interferences.
Retention
After molar uprighting, the teeth are in an unstable position until the prosthesis that provides the long-term retention is placed. Long delays in making the final prosthesis should be avoided if possible. As a general guideline, a fixed bridge can and should be placed within 6 weeks after uprighting is completed. Especially if an implant is planned, there may be a considerable delay while a bone graft heals and the implant becomes integrated. If retention is needed for more than a few weeks, the preferred approach is an intracoronal wire splint (19 × 25 or heavier steel wire) bonded into shallow preparations in the abutment teeth (Figure 18-12). This type of splint causes little gingival irritation and can be left in place for a considerable period, but it would have to be removed and rebonded to allow bone grafting and implant surgery.
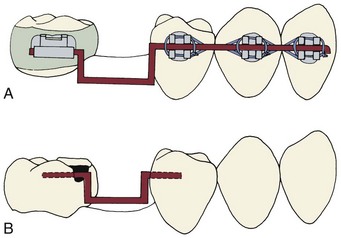
FIGURE 18-12 A molar that has been uprighted is unstable and must be maintained in its new position until a fixed bridge or implant is placed to stabilize it. There are two ways to provide temporary stabilization: A, A heavy rectangular (19 × 25) steel wire engaging the brackets passively and (B) an intracoronal splint (often called an A-splint) made with 19 × 25 or 21 × 25 steel wire that is bonded in shallow preparations in the proximal enamel with composite resin (see also Figure 17-14). This causes minimal tissue disturbance. The intracoronal splint is preferred, particularly if retention is to be continued for more than a few weeks.
Crossbite Correction
Posterior crossbites frequently are corrected using “through the bite” elastics from a conveniently placed tooth in the opposing arch, which moves both the upper and lower tooth (Figure 18-13, A). This tips the teeth into the correct occlusion but also tends to extrude them. For this reason, elastics must be used with caution to correct posterior crossbites in adults because the extrusion can change occlusal relationships throughout the mouth. One way to obtain more movement of a maxillary tooth than its antagonist in the lower arch is to have several teeth in the lower arch stabilized by a heavy archwire segment (Figure 18-13, B to D). Of course, the same approach could be used in reverse to produce more movement of a mandibular tooth. If a mesially tipped lower molar also is in buccal crossbite, an auxiliary uprighting spring can move it lingually as it uprights by two modifications in design: omitting the inward bending of the spring before it is activated (see Figure 18-9, C) and making the spring from round wire.
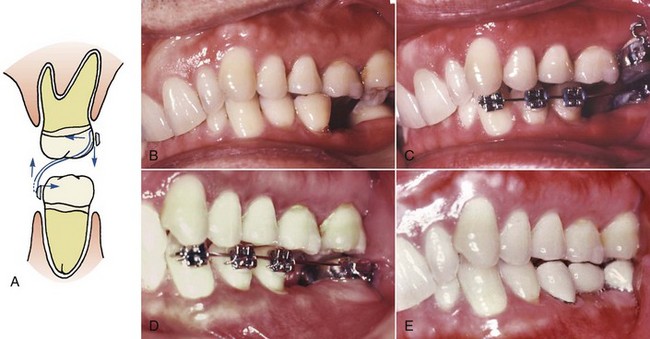
FIGURE 18-13 A, “Through the bite” or cross-elastics produce both horizontal and vertical forces and will extrude the teeth while moving them buccolingually. If these elastics are used to correct posterior crossbite in adults, care must be taken not to open the bite anteriorly too much. Cross-elastics are rarely indicated for an anterior crossbite. B, Buccal crossbite of the second molars in a patient at age 50 who had lost the mandibular first molar years previously. The lower second molar had tipped mesially and lingually. C, The standard orthodontic appliance for uprighting a lower molar was used, consisting of a band on the mandibular second molar, a bonded canine-to-canine mandibular lingual wire to augment anchorage, and bonded brackets on the facial of the premolars and canine. In addition, a lingual cleat was placed on the lower band, and a band with a facial hook was placed on the maxillary second molar, so that cross-elastics could be worn. D, The molar uprighting was completed after the crossbite was corrected. E, The completed bridge in place. This is classic adjunctive orthodontics. The anterior deep bite and incisor alignment were not problems for this patient and were not corrected.
If an anterior crossbite is due only to a displaced tooth and if correcting it requires only tipping (as perhaps in the case of a maxillary incisor that was tipped lingually into crossbite), then a removable appliance or clear aligner may be used to tip the tooth into a normal position. However, when using either type of removable appliance, tipping a tooth facially or lingually also produces a vertical change in occlusal level (Figure 18-14). Tipping maxillary incisors labially to correct anterior crossbite nearly always produces an apparent intrusion and a reduction in overbite. This can present a problem during retention, since a positive overbite serves to retain the crossbite correction. A fixed appliance generally is necessary for vertical control in correction of anterior crossbites.
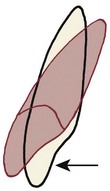
FIGURE 18-14 A labially directed force against a maxillary incisor (from a removable or fixed appliance) will tip the tooth and cause an apparent intrusion of the crown, which reduces the overbite (or makes anterior open bite worse).
If a deep overbite exists on the teeth in crossbite, correction will be much easier if a temporary bite plane that frees the occlusion is added. This bite plane should be carefully constructed to contact the occlusal surfaces of all teeth to prevent any supereruption during treatment.
Establishing a good overbite relationship is the key to maintaining crossbite correction. Crown reconstruction can be used to provide positive occlusal indexing, while eliminating any balancing interferences from the lingual cusps of posterior teeth.
Extrusion
For teeth with defects in or adjacent to the cervical third of the root, controlled extrusion (sometimes called forced eruption) can be an excellent alternative to extensive crown-lengthening surgery.7 Extruding the tooth can allow isolation under a rubber dam for endodontic therapy when it would not be possible otherwise. Extrusion also allows crown margins to be placed on sound tooth structure while maintaining a uniform gingival contour that provides improved esthetics (Figure 18-15). In addition, the alveolar bone height is not compromised, the apparent crown length is maintained, and the bony support of adjacent teeth is not compromised. As the tooth is extruded, the attached gingiva should follow the cementoenamel junction. This returns the width of the attached gingiva to its original level. However, it usually is necessary to perform some limited recontouring of the gingiva, and often of the bone, to produce a contour even with the adjacent teeth and a proper biologic width.

FIGURE 18-15 Forced eruption can move a tooth that is unrestorable because of subgingival pathology into a position that allows treatment. A, This central incisor had a crown placed after being chipped previously, but now showed gingival inflammation and elongation. B, A periapical radiograph revealed internal root resorption below the crown margin. C, The treatment plan was endodontic treatment to arrest the internal resorption, then elongation of the root so that a new crown margin could be placed on sound root structure. D, Initially, an elastomeric tie was used from an archwire segment to an attachment on the post that was cemented in the root canal. E, Then loops in a flexible rectangular wire (17 × 25 beta-Ti) were employed for quicker and more efficient tooth movement. F, 4 mm elongation occurred in as many weeks, and a temporary restoration was placed. G and H, An apically repositioned flap was used to create the correct gingival contour. I and J, Then a coping and final ceramic crown were prepared. Extraction of the tooth was avoided, and a highly esthetic restoration was possible.
As a general rule, control of apical infection should be completed before extrusion of the root begins. For some patients, however, the orthodontic movement must be completed before definitive endodontic procedures because one purpose of extrusion may be to provide better access for endodontic and restorative procedures. If so, preliminary endodontic treatment to relieve symptoms is done initially, and the tooth is maintained with a temporary root filling or other palliative treatment until it has been moved to a better position.
The distance the tooth should be extruded is determined by three things: (1) the location of the defect (e.g., fracture line, root perforation, or resorption site), (2) space to place the margin of the restoration so that it is not at the base of the gingival sulcus (typically, 1 mm is needed), and (3) an allowance for the biologic width of the gingival attachment (about 2 mm). Thus, if a fracture is at the height of the alveolar crest, the tooth should be extruded about 3 mm; if it is 2 mm below the crest, 5 mm of extrusion ideally would be needed. The size of the pulp chamber or canal at the level of the margin of the future restoration also is a consideration—the wall of the tooth at that location must not be too thin. The crown-to-root ratio at the end of treatment should be 1 : 1 or better. A tooth with a poorer ratio can be maintained only by splinting it to adjacent teeth.
Isolated one- or two-wall vertical pockets pose a particular esthetic problem if they occur in the anterior region of the mouth. Surgical correction may be contraindicated simply on esthetic grounds. Forced eruption of such teeth, with concomitant crown reduction, can improve the periodontal condition while maintaining excellent esthetics.
In general, extrusion can be as rapid as 1 mm per week without damage to the PDL, so 3 to 6 weeks is sufficient for almost any patient. Too much force, and too rapid a rate of movement, runs the risk of tissue damage and ankylosis.
Orthodontic Technique
Since extrusion is the tooth movement that occurs most readily and intrusion is the movement that occurs least readily, ample anchorage is usually available from adjacent teeth. The appliance needs to be quite rigid over the anchor teeth, and flexible where it attaches to the tooth that is being extruded. A continuous flexible archwire (see Figure 18-15) produces the desired extrusion but must be managed carefully because it also tends to tip the adjacent teeth toward the tooth being extruded, reducing the space for subsequent restorations and disturbing the interproximal contacts within the arch (Figure 18-16, A). A flexible cantilever spring to extrude a tooth (Figure 18-16, B), or a rigid stabilizing wire and an auxiliary elastomeric module or spring for extrusion (Figure 18-16, C) provide better control.
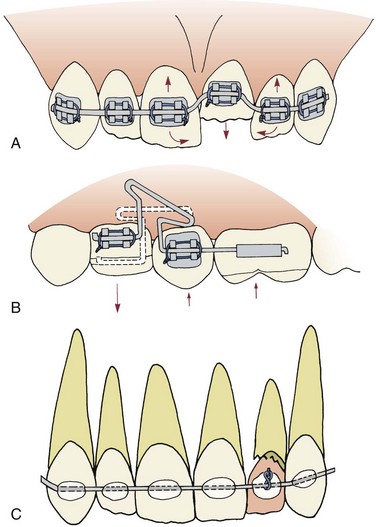
FIGURE 18-16 A, Although a continuous orthodontic wire activated as shown will produce the desired extrusive force, it will also cause the teeth on either side to tip toward each other, reducing the space available for the extruding tooth. B, A segmental T-loop in a rectangular wire (17 × 25 steel in 18-slot brackets, 19 × 25 beta-Ti in 22-slot) will extrude a tooth while controlling mesiodistal tipping of the anchor teeth. C, Extrusion also can be done without conventional orthodontic attachments by bonding a 19 × 25 steel stabilizing wire directly to the facial surface of adjacent teeth. An elastomeric module is stretched between the stabilizing wire and a pin placed directly into the crown of the tooth to be extruded. If a temporary crown is used for better esthetics while the extrusion is being done, it must be progressively cut away to make the tooth movement possible. (C courtesy Dr. L. Osterle.)
Two methods are suggested for extrusion in uncomplicated cases. The first employs a stabilizing wire, 19 × 25 or 21 × 25 stainless steel, bonded directly to the facial surface of the adjacent teeth (Figure 18-17). A post and core with temporary crown and pin is placed on the tooth to be extruded, and an elastomeric module is used to extrude the tooth. This appliance is simple and provides excellent control of anchor teeth, but better control can be obtained when orthodontic brackets are used.
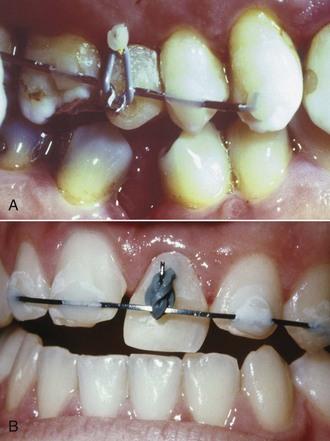
FIGURE 18-17 A, For extrusion of this fractured premolar so that a satisfactory permanent restoration could be made, an elastomeric module was stretched between the stabilizing wire and a pin placed directly into the crown of the premolar. B, The same technique can be used to extrude an incisor. The temporary restoration placed on the tooth while it is being extruded needs to be reduced at frequent intervals. (Courtesy Dr. L. Osterle.)
The alternative is to bond brackets to the anchor teeth, bond an attachment (often a button rather than a bracket) to the tooth to be extruded, and use interarch elastics (Figure 18-18) or a flexible archwire (Figure 18-19). If the buccal surface of the tooth to be extruded is intact, a bracket should be bonded as far gingivally as possible.
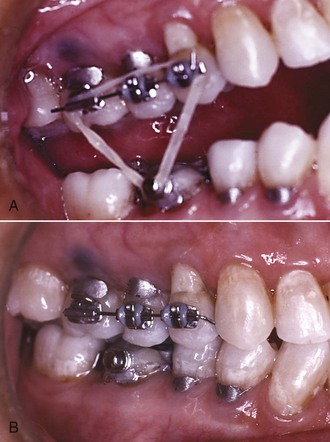
FIGURE 18-18 For this lady in her sixties, the facial surface of a lower first molar fractured to below the gingival margin. A, The maxillary premolars and first molar were bonded and stabilized, and an elastic to a button bonded on the lower molar was used to elongate it to the point that (B) the fracture line was exposed and a satisfactory crown preparation was possible.
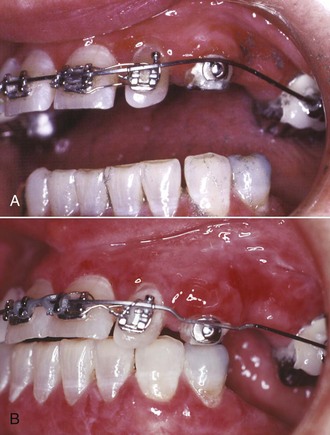
FIGURE 18-19 A bridge attached to the maxillary left canine failed because of caries beneath the crown on the canine. After endodontic treatment, a button was bonded to an amalgam temporary buildup on the root, and (A) a continuous archwire (17 × 25 beta-Ti) was used to extrude the tooth, removing amalgam from temporary buildup weekly. B, At the point at which a permanent restoration could be placed, all the amalgam buildup had been removed and the tooth had been elongated 5 mm.
If the crown of a posterior tooth is hopelessly destroyed, an orthodontic band with a bracket usually can be placed over the remaining root surface. An orthodontic band has the benefit of helping isolation procedures during emergency endodontic treatment. Once endodontic treatment is completed, a pin in the tooth can be used for the attachment, and a temporary crown can be placed if needed for esthetics. Adjacent teeth are bonded to serve as the anchor unit.
With any technique for controlled extrusion, the patient must be seen every 1 to 2 weeks to remove any occlusal contacts that would impede eruption (for instance, shorten the height of a temporary crown) if this is needed (see Figure 18-17), control inflammation, and monitor progress. After active tooth movement has been completed, at least 3 weeks but not more than 6 weeks of stabilization is needed to allow reorganization of the PDL. If periodontal surgery is needed to recontour the alveolar bone and/or reposition the gingiva, it can be done a month after completion of extrusion. As with molar uprighting, it is better to complete the definitive prosthetic treatment without extensive delay.
Alignment of Anterior Teeth
Diastema Closure and Space Redistribution
The major indication for adjunctive orthodontic treatment to correct malaligned anterior teeth is preparation for buildups, veneers, or implants to improve the appearance of the maxillary incisor teeth. The most frequent problem is a maxillary central diastema, which is often further complicated by irregular spacing related to small or missing lateral incisors (Figure 18-20).
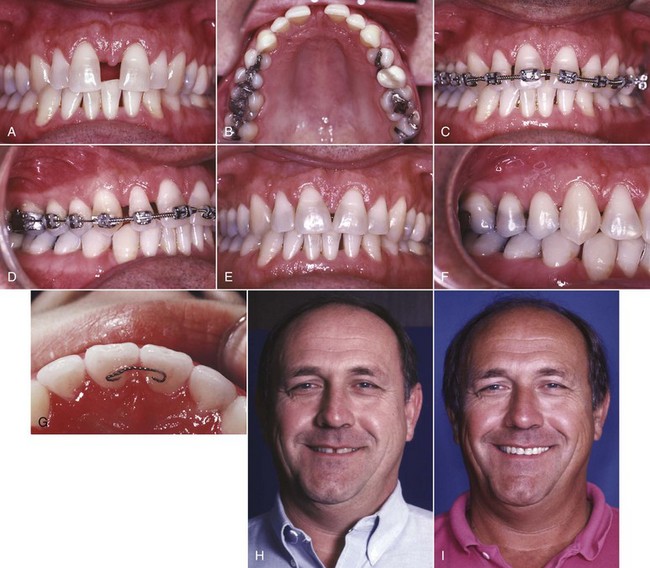
FIGURE 18-20 If spacing of maxillary incisors is related to small teeth and a tooth-size discrepancy, composite buildups are an excellent solution, but satisfactory esthetics may require redistribution of the space before the restorations are placed, as in this patient who was concerned about his large central diastema. A and B, Before treatment, age 48. C and D, Redistribution of the space using a fixed appliance with coil springs on a 16 mil steel archwire immediately before removal of the orthodontic appliance and placement of the restorations (to be done the same day). A 17.5 mil multistrand steel wire was used for initial alignment before the coil springs were placed. E and F, Completed restorations (composite buildups). G, Note the fixed retainer of bonded 21.5 mil multistrand wire on the lingual of the central incisors to prevent partial reopening of the midline space. Surgical revision of the frenum was not performed, partially in deference to the patient’s age. H, Appearance on smile before and (I) after treatment.
A “diagnostic setup” is very helpful in planning the correction of such problems. For this procedure, the study casts are duplicated and the malaligned teeth are carefully cut from the model, repositioned, and then waxed back onto the cast in a new position. If digital casts are available, a modern alternative is to do this on a computer screen (see Figure 14-1), and this is part of routine treatment planning when a sequence of clear aligners will be used in comprehensive treatment (see below). This allows evaluation of the feasibility of the orthodontic treatment in light of the crown and root movements required, the anchorage available, the periodontal support for each tooth, and the possible occlusal interferences.
There are two possible orthodontic techniques: a partial fixed appliance as shown in Figure 18-20, typically with bonded brackets on most if not all the maxillary teeth and a bonded tube on the first molars for additional anchorage control, or a sequence of clear aligners. With a fixed appliance, initial alignment is carried out using a light wire such as 16 mil A-NiTi or 17.5 mil braided steel. This wire is replaced after the teeth are aligned with a 16 or 18 mil round steel wire, along which the teeth are repositioned using elastomeric modules or coil springs. There is always a tendency for the space to reopen after any degree of diastema closure. Bonding a flexible wire on the lingual of the incisors as a semipermanent retainer is recommended.
An alternative is the use of a sequence of clear aligners. These are available commercially in two ways: (1) for modest amounts of tooth movement, aligners made by resetting the teeth on dental casts that can be reshaped by the doctor (see Figure 10-11) and (2) for more extensive tooth movement, a set of 15 to 50 aligners fabricated on stereolithographic models created from computer models of the projected tooth movement (Invisalign, ClearCorrect, others). In adjunctive treatment, the first method is potentially quite useful. The second method, discussed in more detail in the latter part of this chapter (see Figure 18-41), is almost prohibitively expensive unless comprehensive treatment is planned and requires excellent patient compliance when space closure with root movement is required.
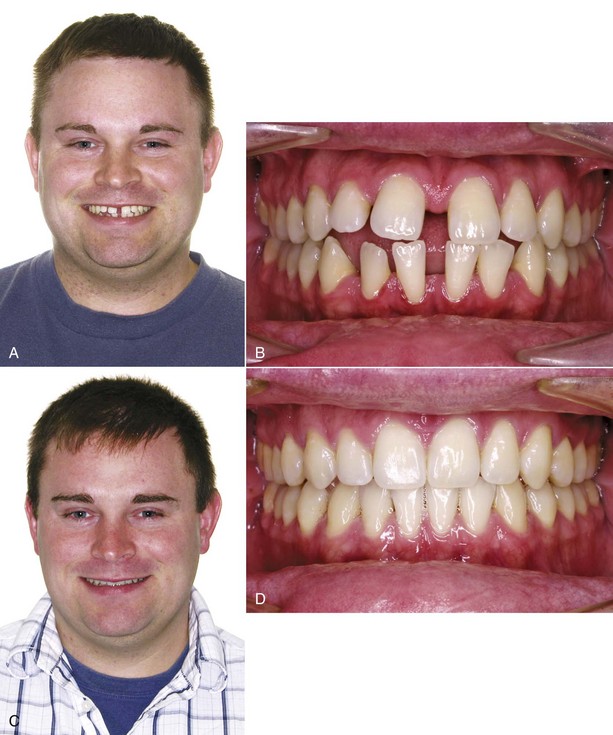
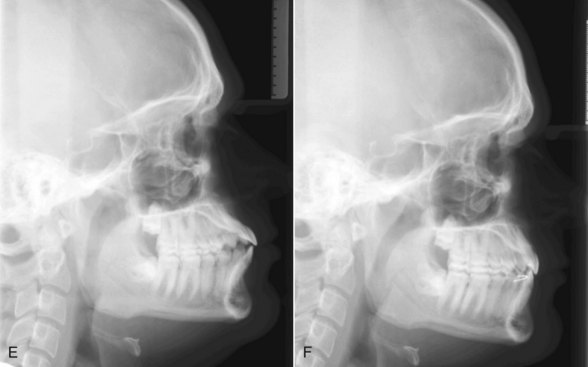
FIGURE 18-41 A and B, This 23-year-old man’s concern was severe spacing in both arches, which was treated with a series of 28 aligners, plus 3 overcorrection aligners that are fabricated by virtually shrinking the teeth, creating virtual space that then is closed with the aligners. C and D, Age 24, posttreatment views. Treatment required 16 months. Keeping spaces closed after treatment when multiple spaces were present is a problem with any alignment system. For this patient, bonded retainers were placed on the lingual of the maxillary central incisors and canine-to-canine in the mandibular arch, and vacuum-formed retainers were made to fit over the bonded retainers to prevent reopening of the spaces. E and F, Cephalometric radiographs before and after treatment, showing the degree of incisor retraction. (Courtesy Dr. W. Gierie.)
Crowded, Rotated, and Displaced Incisors
As a rule, spacing is the problem when maxillary incisors need realignment to facilitate other treatment. Crowding usually is the problem when alignment of lower incisors is considered to provide access for restorations, achieve better occlusion, or enable the patient to maintain the teeth. In some cases, alignment of incisors in both arches must be considered. The key question is whether the crowding should be resolved by expanding the arch, removing some interproximal enamel from each tooth to provide space,8 or removing one lower incisor.
Expansion of a crowded incisor segment can be done with clear aligners, but if only the lower arch is to be treated, the esthetics of the appliance is not a consideration, and a partial fixed appliance is more efficient and cost-effective (Figure 18-21). A segment of A-NiTi wire, with stops to make it slightly advanced, usually is the best way to bring the teeth into alignment (see Figure 14-8).

FIGURE 18-21 In an adult with a damaged lower incisor (in this case, the left central incisor with a crown fracture) and incisor crowding, there are two treatment possibilities: extract the damaged tooth and use the space to align the remaining teeth, or align the teeth with arch expansion and restore the damaged one. The decision has an esthetic component because the lower incisors are visible on smile in older individuals. In this patient, aligning the lower incisors without extraction would also require aligning the upper incisors, but this expansion would increase lip support and improve the overall facial appearance as well as the dental appearance. A, Smile before treatment, after loss of one corner of the lower right central incisor. B, Mandibular occlusal view. C, Frontal view. Note the moderately deep bite and lack of overjet. The restorative dentist sought orthodontic consultation, thinking that extraction of the damaged tooth might be the best plan. The patient wanted the best esthetic result and accepted a period of treatment with a fixed appliance on both arches, after which the incisor would be restored. The orthodontic alignment required 5 months. D, Mandibular occlusal view after alignment. E, Frontal view. F, Smile after restoration was completed.
Stripping the contact points of the teeth to remove enamel can provide space for alignment of mildly irregular lower incisors, and either a fixed appliance or a clear aligner sequence can provide the tooth movement. This should be undertaken with caution, however, because it may have an undesirable effect on overjet, overbite, posterior intercuspation, and esthetics.9 In severe crowding, removing one lower incisor and using the space to align the other three incisors can produce a satisfactory result and can be managed with clear aligner therapy if bonded attachments are part of the treatment plan (Figure 18-22). The treatment time and difficulty, whatever the type of appliance, put this at or across the border of comprehensive treatment. Neither stripping nor incisor extraction should be undertaken without a diagnostic setup to verify feasibility.

FIGURE 18-22 This 24-year-old patient had a congenitally missing mandibular right lateral incisor and a retained but failing primary incisor. A, Frontal view. B, Maxillary occlusal. Note the rotation of the maxillary right canine. C, Mandibular occlusal. The plan was extraction of the primary incisor and closure of the extraction site, using a series of Invisalign aligners and bonded attachments to produce the necessary rotation and root movement. Before treatment began, air-rotor stripping of the maxillary posterior quadrants was done to reduce the tooth-size discrepancy. D, Note the hard-to-see bonded attachments on the maxillary right canine and incisors and on the mandibular right canine and central incisor. The original plan called for 13 upper and 15 lower aligners, plus three overcorrection aligners. E and F, After eight aligners it was noted that the maxillary right canine was not tracking, and an elastic to additional bonded attachments was used along with the aligner to further rotate it. New records were taken, and four upper and five lower revision aligners, with three revision overcorrection aligners, were fabricated. G to I, Completion of treatment. A bonded canine-to-canine mandibular retainer was used, and the final maxillary aligner was continued at night as the maxillary retainer. J, Panoramic radiograph at the completion of treatment. Total treatment time was 19 months (which included 2 months waiting for revision aligners). (Courtesy Dr. W. Gierie.)
Remember that stretched gingival fibers are a potent force for relapse after rotations have been corrected, and that good long-term stability may require a fiberotomy (see Chapter 16). Whether clear aligners or a fixed appliance was used, retention is necessary until restorative or other treatment is completed. This can be the final aligner in a sequence (though this may be too flexible to be a good retainer), a molded thermoplastic retainer after a fixed appliance is removed, a canine-to-canine clip retainer, or a bonded fixed retainer.10
Comprehensive Treatment in Adults
A major motivation for orthodontic treatment of younger patients is the parents’ desire to do the best they can for their children. The typical child or adolescent accepts orthodontics in about the same rather passive way that he or she accepts going to school, summer camp, and the inevitable junior high school dance: as just another in the series of events that one must endure while growing up. Occasionally, of course, an adolescent actively resists orthodontic treatment, and the result can be unfortunate for all concerned if the treatment becomes the focus of an adolescent rebellion. In most instances, however, children tend not to become emotionally involved in their treatment.
Adults in both the younger and older groups, in contrast, seek comprehensive orthodontic treatment because they themselves really want it. For the younger group who are trying to improve their lot in life, exactly what they want is not always clearly expressed, and some young adults have a remarkably elaborate hidden set of motivations. It is important to explore why an individual wants treatment and why now as opposed to some other time to avoid setting up a situation in which the patient’s expectations from treatment cannot possibly be met. Sometimes, orthodontic treatment is sought as a last-ditch effort to improve personal appearance to deal with a series of complicated social problems. Orthodontic treatment obviously cannot be relied on to repair personal relationships, save jobs, or overcome a series of financial disasters. If the prospective patient has unrealistic expectations of that sort, it is much better to deal with them sooner rather than later.
Most adults in both the younger and older groups, fortunately, understand why they want orthodontics and are realistic about what they can obtain from it. One might expect those who seek treatment to be less secure and less well-adjusted than the average adult, but for the most part, they have a more positive self-image than average.11 It apparently takes a good deal of ego strength to seek orthodontic treatment as an adult, and ego strength rather than weakness characterizes most potential adult patients. A patient who seeks treatment primarily because he or she wants it (internal motivation) is more likely to respond well psychologically than a patient whose motivation is the urging of others or the expected impact of treatment on others (external motivation). External motivation is often accompanied by an increasing impact of the orthodontic problem on personality (Figure 18-23). Such a patient is likely to have a complex set of unrecognized expectations for treatment, the proverbial hidden agenda.
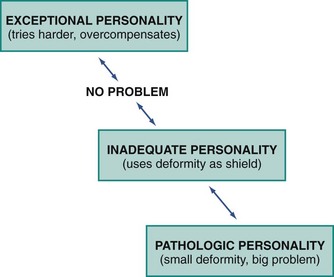
FIGURE 18-23 Dentofacial deformity can affect an individual’s life adjustment. Fortunately, most potential adult orthodontic patients fall into the “no problem” category psychologically. A few highly successful individuals (who nevertheless may seek treatment) can be thought of as almost overcompensating for their deformity with their exceptional personability, but they tend to be personable and very pleasant to work with. For some individuals, however, the orthodontic condition can become the focus for a wide-ranging set of social adjustment problems that orthodontics alone will not solve. These patients fall into the “inadequate personality” and “pathologic personality” categories, who are difficult and almost impossible, respectively, to help. An important aspect of orthodontic diagnosis for adults is understanding where a patient fits along this spectrum.
One way to identify the minority of individuals who may present problems because of their unrealistic expectations is to compare the patient’s perception of his or her orthodontic condition with the doctor’s evaluation. If the patient thinks that the appearance or function of the teeth is creating a severe problem, while an objective assessment simply does not corroborate that, orthodontic treatment should be approached with caution.
Even highly motivated adults are likely to have some concern about the appearance of orthodontic appliances. The demand for an invisible orthodontic appliance comes almost entirely from adults who are concerned about the reaction of others to obvious orthodontic treatment. In an earlier era, this was a major reason for using removable appliances in adults, particularly the Crozat appliance in the United States.
All of the possibilities for a better appearing appliance, however, lead to potential compromises in the orthodontic treatment. Plastic brackets create problems in controlling root position and closing spaces. Ceramic brackets, though much better, inevitably make treatment more difficult because of the problems outlined in Chapter 11. Lingual appliances have been greatly improved since the turn of the twenty-first century and now make all types of tooth movement quite possible but still are technically difficult for the doctor to use efficiently and can be difficult for patients to tolerate. Clear aligners manage some types of tooth movement quite well (especially tipping) but have difficulty with others (especially extrusion, rotation, and root positioning). Small bonded attachments on teeth that require complex movements give the aligner a better purchase, partially overcoming this difficulty (see Figure 18-22).
Although there is nothing wrong with using the most esthetic appliance possible for an adult patient, the compromises associated with this approach should be thoroughly discussed in advance. It is unrealistic for a patient to expect that orthodontic treatment can be carried out without other people knowing about it. The whole issue of the visibility of the orthodontic appliances is much less important, at least in the United States, than many patients fear. Orthodontic treatment for adults is certainly socially acceptable, and one does not become a victim of discrimination because of visible orthodontic appliances. In a sense, the patient’s expectations become a self-fulfilling prophecy. If the patient faces others confidently, a visible orthodontic appliance causes no problems. Only if the patient acts ashamed or defensive is there likely to be any negative reaction from others.
The question of whether an orthodontic office should have a separate treatment area for adults, separated from the adolescents who still constitute the bulk of most orthodontic practices, is related to the same set of negative attitudes. Most comprehensive orthodontic treatment for adolescents is carried out in open treatment areas, not only because the open area is efficient but also because the learning effect from having patients observe what is happening to others is a positive influence in patient adaptation to treatment. Should adults be segregated into private rooms, rather than joining the group in the open treatment area? This is logical only if the adult is greatly concerned about privacy (more true of Europeans than Americans), or vaguely ashamed of being an orthodontic patient. Sometimes, for some adults, treatment in a private area may be preferable, but for most adults, learning from interacting with other patients helps them understand and tolerate the treatment procedures. There are positive advantages in having patients at various stages of treatment compare their experiences, and this is at least as beneficial to adults as to children, perhaps more so.
Despite the fact that adults can be treated in the same area as adolescents, they cannot be handled in exactly the same way. The typical adolescent’s passive acceptance of what is being done is rarely found in adult patients, who want and expect a considerable degree of explanation of what is happening and why. An adult can be counted on to be interested in the treatment but that does not automatically translate into compliance with instructions. Unless adults understand why they have been asked to do various things, they may choose not to do them, not in the passive way an adolescent might just shrug it off but from an active decision not to do it. In addition, adults, as a rule, are less tolerant of discomfort and more likely to complain about pain after adjustments and about difficulties in speech, eating, and tissue adaptation. Additional chair time to meet these demands should be anticipated.
These characteristics might make adults sound like less desirable orthodontic patients than adolescents, but this is not necessarily so. Working with individuals who are intensely interested in their own treatment and motivated to take care of their teeth can be a pleasant and stimulating alternative to the less-involved adolescents. If the expectations of both the doctor and the patient are realistic, comprehensive treatment for adults can be a rewarding experience for both.
Temporomandibular Dysfunction as a Reason for Orthodontic Treatment
Temporomandibular pain and dysfunction (TMD symptoms) rarely are encountered in children seeking orthodontic treatment, but TMD is a significant motivating factor for some adults who consider orthodontic treatment.12 The relationship between dental occlusion and TMD is highly controversial, and it is important to view this objectively.13 Orthodontic treatment can sometimes help patients with TMD, but it cannot be relied on to correct these problems.14 Patients need to understand what may happen to their symptoms during and after orthodontics.
Types of Problems
In diagnosis of TMD problems, patients are classified as being in one of four large groups: masticatory muscle disorders, TM joint disorders, chronic mandibular hypomobility, and growth disorders.15 From the perspective of potential orthodontic treatment in adults, differentiating between the first two groups is particularly important (Figure 18-24). Because muscle spasm and joint pathology can coexist, the distinction in many patients is difficult. Nevertheless, it is unlikely that orthodontics will relieve TMD symptoms in a patient who has internal joint problems or other nonmuscular sources of pain. Those who have myofascial pain/dysfunction, on the other hand, may benefit from improved dental occlusion.
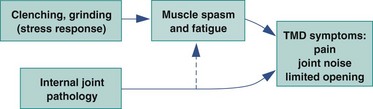
FIGURE 18-24 TMD symptoms arise from two major causes: muscle spasm and fatigue, which almost always are related to excessive clenching and grinding in response to stress, and internal joint pathology. As a general guideline, patients with symptoms of muscle spasm and fatigue may be helped by orthodontic treatment, but simpler methods should be attempted first. Orthodontics alone is rarely useful for patients with internal joint pathology.
Almost all of us develop some symptoms of degenerative joint disease as we grow older, and it is not surprising that the jaw joints sometimes are involved (Figure 18-25). Arthritic involvement of the TM joints is most likely to be the cause of TMD symptoms in patients who have arthritic changes in other joints of the body. A component of muscle spasm and muscle pain should be suspected in individuals whose only symptoms are in the TM joint area, even if radiographs show moderate arthritic degeneration of the joint.
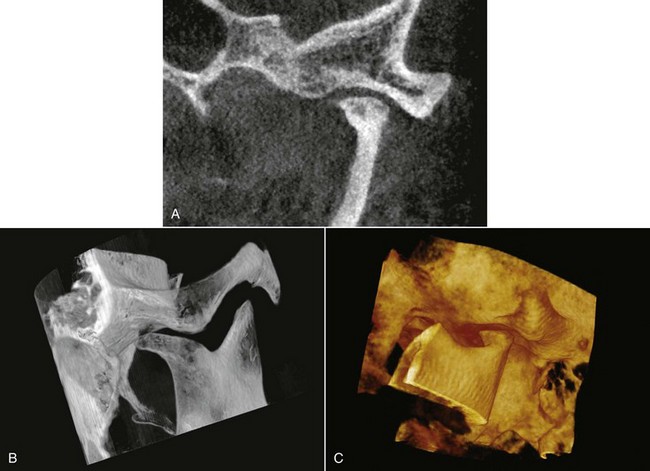
FIGURE 18-25 Three radiographic views of arthritic degeneration of a left mandibular condyle, from CBCT images. Note the flattening of the condylar head and the lipping posteriorly, which can be visualized in a view similar to what is seen in a panoramic radiograph (A) but are seen more clearly in the images that show the condylar area (B and C). With CBCT images, it is possible to rotate the field of view as desired.
Displacement of the disk (Figure 18-26) can arise from a number of causes. One possibility is trauma to the joint, so that the ligaments that oppose the action of the lateral pterygoid muscle are stretched or torn. In this circumstance, muscle contraction moves the disk forward as the mandibular condyles translate forward on wide opening, but the ligaments do not restore the disk to its proper position when the jaw is closed. The result is a click upon opening and closing, as the disk pops into place over the condylar head as the patient opens, but is displaced anteriorly on closure.
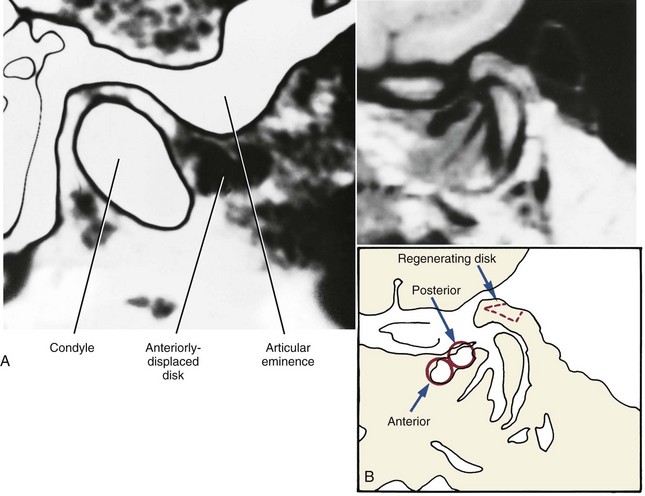
FIGURE 18-26 A, Computed tomography (CT) view of a displaced mandibular disk, which can be visualized (as a darker area) in front of the condyle. B, Magnetic resonance imaging (MRI) view of a displaced disk, with the anterior and posterior bands indicated on the adjacent sketch. There is evidence on this scan of a regenerating disk, as shown in the dashed area. MRI scans have largely replaced radiographic views for the diagnosis of disk displacement because the soft tissues can be seen more clearly and no ionizing radiation is required, while cone-beam CT (CBCT) is preferred for visualization of bony changes.
The click and symptoms associated with it can be corrected if an occlusal splint is used to prevent the patient from closing beyond the point at which displacement occurs. The resulting relief of pain influences patients and dentists to seek either restorative or orthodontic treatment to increase facial vertical dimension. However, orthodontic elongation of all posterior teeth to control disk displacement is not a treatment procedure that should be undertaken lightly. Often, the patient whose symptoms have been controlled by a splint can tolerate its reduction or removal, without requiring major occlusal changes. As a general rule, there are better ways of handling disk displacement than orthodontic treatment.
Myofascial pain develops when muscles are overly fatigued and tend to go into spasm. It is all but impossible to overwork the jaw muscles to this extent during normal eating and chewing. To produce myofascial pain, the patient must be clenching or grinding the teeth for many hours per day, presumably as a response to stress. Great variations are seen in the way different individuals respond to stress, both in the organ system that feels the strain (many problems besides TMD are related to stress) and in the amount of stress that can be tolerated before symptoms appear (tense individuals develop stress-related symptoms before their relaxed colleagues do). For this reason, it is impossible to say that occlusal discrepancies of any given degree will lead to TMD symptoms.
It is possible to demonstrate that some types of occlusal discrepancies predispose patients who clench or grind their teeth to the development of TMD symptoms. It must be kept in mind, however, that it takes two factors to produce myofascial pain: an occlusal discrepancy and a patient who clenches or grinds the teeth. Perhaps the most compelling argument against malocclusion as a primary cause of TMD is the observation that TMD is no more prevalent in patients with severe malocclusion than in the general population.16 The dictum “let your teeth alone” would solve myofascial pain problems if it could be followed by the patient.
Treatment Indications
From this perspective, three broad approaches to myofascial pain symptoms can be considered: reducing the amount of stress; reducing the patients’ reactions to stress; or improving the occlusion, thereby making it harder for patients to hurt themselves. Drastic alteration of the occlusion, by either restorative dental procedures or orthodontics, is logical only if the less invasive stress-control and stress-adaptation approaches have failed. In that circumstance, orthodontic treatment to alter the occlusion so that the patient can better tolerate parafunctional activity may be worth attempting. In some instances, this may involve orthognathic surgery to reposition the jaws.
The extent to which TMD symptoms in many adults disappear when comprehensive orthodontic treatment begins can be surprising and overly gratifying to those who do not understand the etiology of myofascial pain. Orthodontic intervention can appear almost magical in the way that TMD symptoms disappear long before the occlusal relationships have been corrected. The explanation is simple—orthodontic treatment makes the teeth sore, so grinding or clenching sensitive teeth as a means of handling stress does not produce the same subconscious gratification as previously; the parafunctional activity stops; and the symptoms vanish. The changing occlusal relationships also contribute to breaking up the habit patterns that contributed to the muscle fatigue and pain. The same benefit occurs with orthognathic surgery. No matter what the type of orthodontic treatment, symptoms are unlikely to be present while movement of a significant number of teeth is occurring, as long as treatment that produces strongly deflective contacts is avoided. Prolonged use of Class II or Class III elastics may not be well tolerated in adults who have had TMD problems and should be avoided (for that matter, prolonged use of elastics should be avoided in most other adult patients as well).
The moment of truth for TMD patients who have had orthodontic treatment comes some time after the orthodontics is completed, when the clenching and grinding that originally caused the problem tend to recur. At that point, even if the occlusal relationships have been significantly improved, it may be impossible to keep the patient from moving into extreme jaw positions and engaging in parafunctional activity that produces pain. The use of interocclusal splints in this situation may be the only way to keep symptoms from recurring. In short, the miraculous cure that orthodontic treatment often provides for myofascial pain tends to disappear with the appliance. Those who have had symptoms in the past are always at risk of having them recur.
Occasionally, orthodontic treatment is made more complicated by previous splint therapy for TMD problems. If an occlusal splint for TMD symptoms covers the posterior but not the anterior teeth, the anterior teeth that have been taken out of occlusion begin to erupt again and may come back into occlusion even though the posterior teeth are still separated (Figure 18-27). Clinically, it may appear that the posterior teeth are being intruded, but incisor eruption usually is a greater contributor to the development of posterior open bite. In only a few months, the patient may end up in a situation in which discarding the splint has become impossible. Then the only treatment possibilities are elongation of the posterior teeth, either with crowns or orthodontic extrusion, or intrusion of the anterior teeth.

FIGURE 18-27 Occlusal relationships in a 24-year-old woman who had worn a splint covering only her posterior teeth for the previous 18 months. Note the posterior open bite when the splint was taken out. This was created by a combination of intrusion of the posterior teeth and further eruption of the anterior teeth. Discarding the splint had become impossible.
Orthodontic intervention at this stage is difficult because TMD symptoms are likely to develop immediately if the splint is removed, and it is not possible to elongate the posterior teeth orthodontically without discarding or cutting down the splint. Placing orthodontic attachments on the posterior teeth and using light vertical elastics to the posterior segments can be used to bring the posterior teeth back into occlusion (Figure 18-28), if the patient can tolerate this treatment. Some re-intrusion of the elongated anterior teeth is likely to occur, but a significant increase in face height is often maintained. Although permanently increasing the vertical dimension to control disk displacement can be accomplished in this way, this treatment plan should be used with extreme caution.
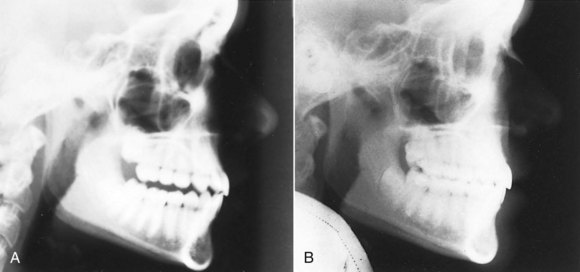
FIGURE 18-28 Cephalometric radiographs for the patient shown in Figure 18-27. Before (A) and after (B) orthodontic treatment to extrude the posterior teeth back into occlusion.
Periodontal Considerations
Periodontal problems are rarely a major concern during orthodontic treatment of children and adolescents because periodontal disease usually does not arise at an early age and tissue resistance is higher in younger patients. For the same reasons, periodontal considerations are increasingly important as patients become older, regardless of whether periodontal problems were a motivating factor for orthodontic treatment.
The prevalence of periodontal disease as a function of age in a large group of potential orthodontic patients with severe malocclusion is shown in Figure 18-29. Note that up to the late thirties, there is nearly a straight-line relationship between age and periodontal pocketing (defined here as the presence of pockets of 5 mm or more). In contrast, the prevalence of mucogingival problems peaks in the twenties. The odds are that any patient over the age of 35 has some periodontal problems that could affect orthodontic treatment, and mucogingival considerations are important in treatment of the younger adult group.
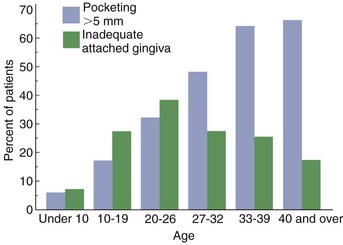
FIGURE 18-29 The prevalence of periodontal pockets of 5 mm or more and prevalence of inadequate attached gingiva as a function of age in 1000 consecutive patients with severe orthodontic problems who were referred for possible surgical-orthodontic treatment. (Redrawn from Morarity JD, Simpson DM. J Dent Res 63:[Special Issue A, #1249], 1984.)
Periodontal disease is not a continuous and steadily progressive degenerative process. Instead, it is characterized by episodes of acute attack on some but usually not all areas of the mouth, followed by quiescent periods. It is obviously important to identify high-risk patients and high-risk sites. The best indicator that disease may be present is a history of disease. At present, persistent bleeding on gentle probing is the best indicator of active and presumably progressive disease, which is why it is important for the orthodontist to probe carefully during an orthodontic clinical examination. New diagnostic procedures used by periodontists to evaluate subgingival plaque and crevicular fluids for the presence of indicator bacteria, enzymes, or other chemical mediators now are clinically useful and likely to be used on potential orthodontic patients referred for further evaluation. There appear to be at least three risk groups in the population for progression of periodontal bone loss: those with rapid progression (about 10%), those with moderate progression (the great majority, about 80%), and those with no progression (about 10%).17
There is no contraindication to treating adults who have had periodontal disease and bone loss, as long as the disease has been brought under control (Figure 18-30). Progression of untreated periodontal breakdown must be anticipated, however, and the patient’s periodontal situation must receive major attention in planning and executing orthodontic treatment for adults.

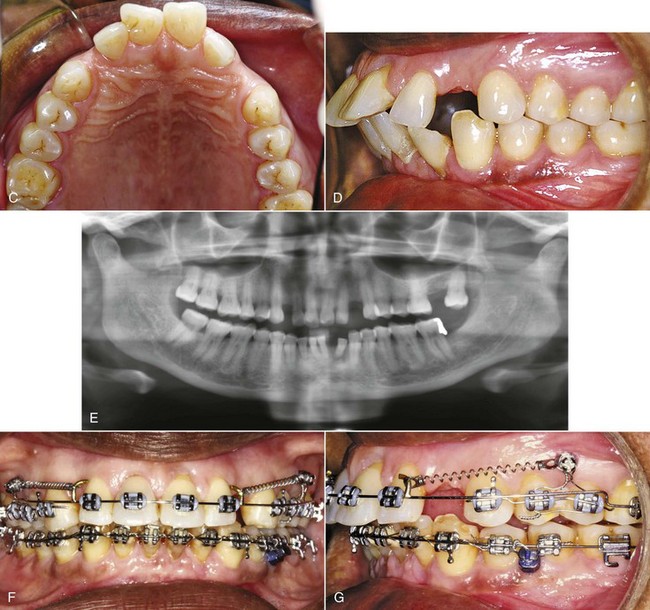

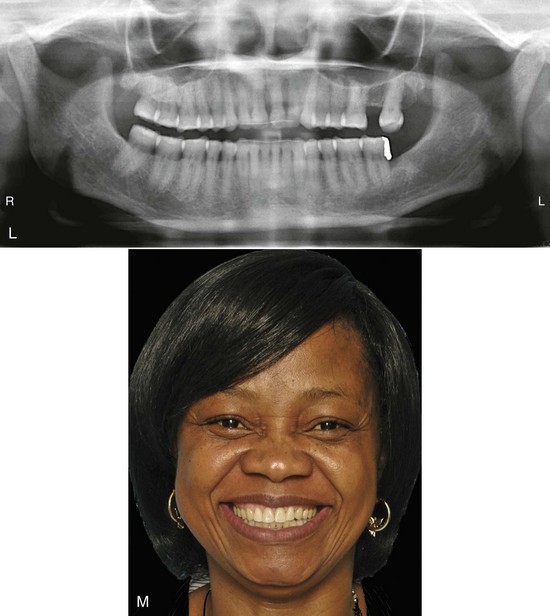
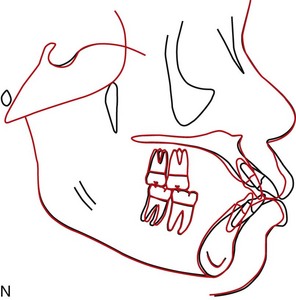
FIGURE 18-30 Comprehensive orthodontic treatment for a patient with severe periodontal disease requires that active disease has been brought under control and that control is maintained, but given that, major tooth movement without worsening the periodontal condition is quite possible. A, Initial smile and (B) initial close-up frontal view, showing the spacing in both arches created by the drifting of teeth that accompanied her severe periodontal problems. C and D, Occlusal and lateral intraoral views before treatment. E, Initial panoramic radiograph. She had moderately severe generalized periodontal disease with localized severe bone loss. After the periodontal disease was brought under control, she sought treatment to retract her protruding incisors and close the anterior spaces in both arches. The plan was to use skeletal anchorage (alveolar bone screws) in both arches to retract the incisors while maintaining normal overbite. Closure of the old maxillary left second molar extraction space was judged to be more than could be managed even with skeletal anchorage without compromising the symmetry of the anterior segment. F and G, A-NiTi coil springs and sliding mechanics were used for space closure in both arches, with screws placed between the first and second premolars in both arches. Note the combination of direct and indirect anchorage in the maxillary arch. H, Occlusal view of TAD-supported space closure in the maxillary arch. I to K, Age 58, after completion of orthodontic treatment that required 35 months. Note the improvement in dental alignment and occlusion, and the maintenance of her periodontal health. L, Posttreatment panoramic radiograph. M, Posttreatment smile. N, Cephalometric superimposition showing the major retraction of the incisors with no forward movement of the posterior teeth. (Courtesy Dr. D. Grauer.)
Treatment of Patients with Minimal Periodontal Involvement
Any patient undergoing orthodontic treatment must take extra care to clean the teeth, but this is even more important in adult orthodontics. Bacterial plaque is the main etiologic factor in periodontal breakdown, and its effect is largely determined by the host response. Orthodontic appliances simultaneously make maintenance of oral hygiene more difficult and more important. In children and adolescents, even if gingivitis develops in response to the presence of orthodontic appliances, it almost never extends into periodontitis. This cannot be taken for granted in adults, no matter how good their initial periodontal condition.
The periodontal evaluation of a potential adult orthodontic patient must include not only the response to periodontal probing but also the level and condition of the attached gingiva. Labial movement of incisors in some patients can be followed by gingival recession and loss of attachment. The risk is greatest when irregular teeth are aligned by expanding the dental arch.
The present concept is that gingival recession occurs secondarily to an alveolar bone dehiscence, if overlying tissues are stressed. The stress can be due to any of several causes. Major possibilities are toothbrush trauma, plaque-induced inflammation, or the stretching and thinning of the gingiva that might be created by labial tooth movement. Once recession begins, it can progress rapidly, especially if there is little or no keratinized attached gingiva and the attachment is only alveolar mucosa.
It was once thought that the width of the gingival attachment determined whether recession occurred. The concept now is that two characteristics are important: the width of the attached gingiva (not all keratinized gingiva is attached) and the thickness of the gingival tissue. The width of the attached gingiva can be observed most readily by inserting a periodontal probe and observing the distance between the point at which the gingival attachment is encountered and the point at which the alveolar mucosa begins. Lower incisors in patients with a prominent chin and compensation in the form of lingual tipping of these teeth are at particular risk of recession, and thin gingival tissue probably is the reason.
For adult orthodontic patients, it is much better to prevent gingival recession than to try to correct it later. For this reason, a gingival graft (Figure 18-31) must be considered in adults with minimal attached gingiva or thin tissue, particularly those for whom arch expansion will be used to align incisors and those who will have surgical mandibular advancement or genioplasty (see Chapter 19).

FIGURE 18-31 In adults who will have comprehensive orthodontic treatment, gingival grafting to create adequate quantity and thickness of attached gingiva is important before beginning orthodontic tooth movement. A, Lack of attached gingiva and thin gingival tissue in the mandibular anterior region in a patient whose lower incisors must be advanced to align them. Note the alveolar mucosa extending almost to the gingival margin on all anterior teeth. B, Surgical preparation of a bed for grafting. C, The palatal donor site for tissue for the gingival graft. D, The graft sutured in place. E, Healing 1 week later, showing incorporation of the grafts. F, Initial alignment archwire in place 3 months later, with the gingival grafts creating both a thicker contour of the gingival tissue and a generous band of attachment. (Courtesy Dr. J. Morarity.)
Moderate Periodontal Involvement
Before orthodontic treatment is attempted for patients who have preexisting periodontal problems, dental and periodontal disease must be brought under control. Preliminary periodontal therapy can include all aspects of periodontal treatment. It is important to remove all calculus and other irritants from periodontal pockets before any tooth movement is attempted, and it is often wise to use surgical flaps to expose these areas to ensure the best possible scaling. Is a bone graft slurry as part of corticotomy (accelerated osteogenic orthodontics [AOO]) (see Figure 8-16) indicated to prevent bone dehiscence and gingival recession when significant arch expansion is planned for an adult? At this time, data to indicate the point at which that might make a significant difference are lacking.
Treatment procedures to facilitate the patient’s long-term maintenance, such as osseous recontouring or repositioned flaps to compensate for areas of gingival recession, are best deferred until the final occlusal relationships have been established. A period of observation following preliminary periodontal treatment to make sure that the patient’s disease is adequately controlled and to allow healing after the periodontal therapy should precede comprehensive orthodontics.
Disease control also requires endodontic treatment of any pulpally involved teeth. There is no contraindication to the orthodontic movement of an endodontically treated tooth, so root canal therapy before orthodontics will cause no problems. Attempting to move a pulpally involved tooth, however, is likely to cause a flare-up of pulpitis and pain.
The general guideline for preliminary restorative treatment is that temporary restorations should be placed to control caries, with the definitive restorative dentistry delayed until after the orthodontic phase of treatment. Temporary restoration, however, should not be taken to mean the use of a short-lived material that will last only a few months. Composite resin is now the preferred temporary restorative material while orthodontics is being carried out. Cast restorations should be delayed until after the final occlusal relationships have been established by orthodontic treatment.
Because the margins of bands can make periodontal maintenance more difficult, it usually is better to use a fully bonded orthodontic appliance for periodontally involved adults. Self-ligating brackets or steel ligatures also are preferred for periodontally involved patients rather than elastomeric rings to retain orthodontic archwires because patients with elastomeric rings have higher levels of microorganisms in gingival plaque.18
During comprehensive orthodontics, a patient with moderate periodontal problems must be on a maintenance schedule, with the frequency of cleaning and scaling depending on the severity of the periodontal disease. Periodontal maintenance therapy at 2- to 4-month intervals is the usual plan. Adjunctive chemical agents between appointments (including chlorhexidine if needed) also should be considered.
Severe Periodontal Involvement
The general approach to treatment for patients with severe periodontal involvement is the same as that outlined earlier, but the treatment itself must be modified in two ways: (1) periodontal maintenance should be scheduled at more frequent intervals, perhaps with the patient being seen as frequently for periodontal maintenance as for orthodontic appliance adjustments (i.e., every 4 to 6 weeks), and (2) orthodontic treatment goals and mechanics must be modified to keep orthodontic forces to an absolute minimum because the reduced area of the PDL after significant bone loss means higher pressure in the PDL from any force (Figure 18-32). Sometimes it is helpful to temporarily retain a tooth that is hopelessly involved periodontally, using it to help support an orthodontic appliance that will contribute to saving other teeth.
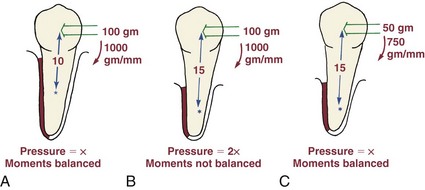
FIGURE 18-32 Bone loss around a tooth that is to be moved affects both the force and the moment needed. A, For optimum bodily movement of a premolar whose center of resistance is 10 mm apical to the bracket (i.e., normal height of alveolar bone support), a 100 gm force and a 1000 gm-mm moment is needed. B, The same force system would be inappropriate for an identical premolar whose bone support had been reduced by periodontal disease so that the PDL area is half as large as it was originally, and so that the center of resistance is now 15 mm apical to the bracket. For such a tooth, the 100 gm force would produce twice the optimum pressure in the PDL, and the moment would not be large enough to prevent tipping. C, The correct force system for the periodontally involved tooth would be a 50 gm force and a 15 × 50 = 750 gm-mm moment. Orthodontic movement of periodontally involved teeth can be done only with careful attention to forces (smaller than normal) and moments (relatively larger than normal).
It is interesting that even after severe periodontal problems have developed, orthodontic treatment can be carried out without further loss of alveolar bone if good control of the periodontal condition is maintained. Space closure in areas of major bone loss sometimes leads to an improvement in bone height if at least one wall of the periodontal pocket remains (Figure 18-33). As part of informed consent, patients like this can be told that they can have comprehensive orthodontic treatment without undue risk of making their periodontal situation worse but should not be promised an improvement.

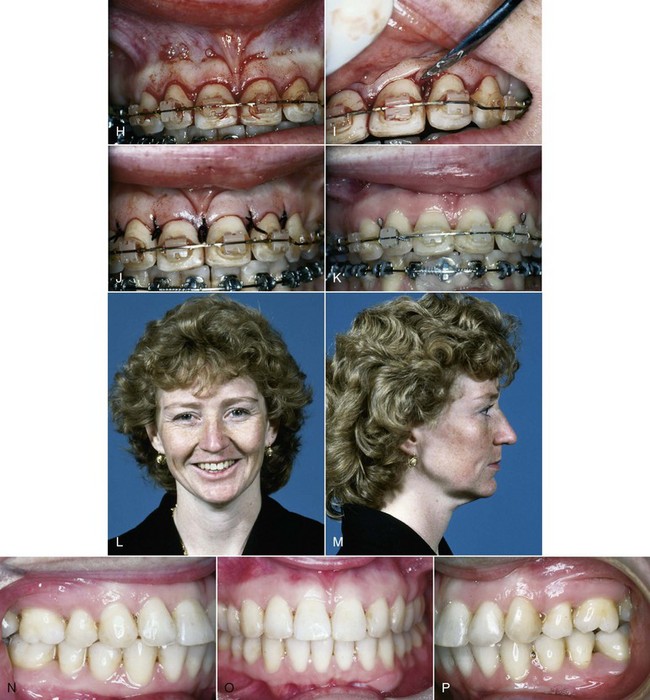
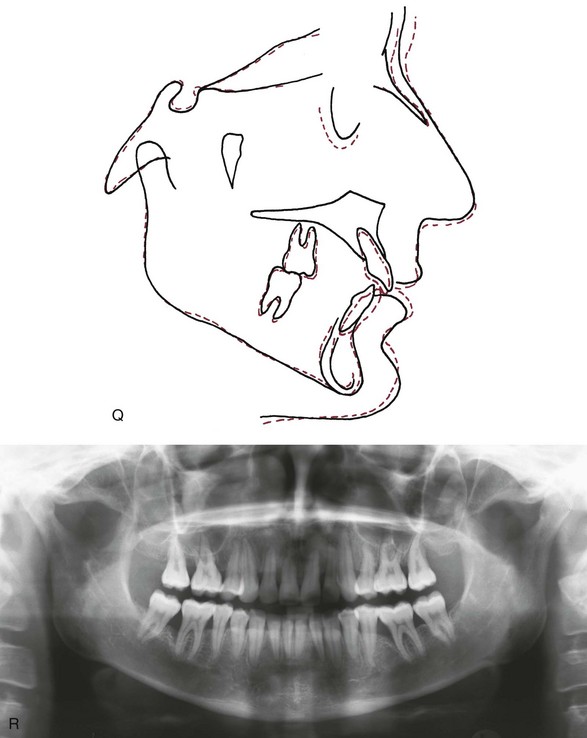
FIGURE 18-33 A to E, At age 27, this woman sought orthodontic treatment because her periodontist thought that her periodontal disease could be controlled better if the alignment of her teeth were improved, and because she had never liked the appearance of her extremely crowded and irregular maxillary incisors. There was a full-cusp Class II molar relationship and minimal overbite. F, The panoramic radiograph shows severe bone loss in multiple areas, but active disease was now under control. G, The cephalometric radiograph showed a mild skeletal Class II jaw relationship, with moderate maxillary incisor protrusion. The treatment plan called for extraction of the maxillary left first premolar and the right second premolar (chosen because of the large periodontal defect distal to it, although this would make the orthodontic treatment more difficult). The extraction space, plus reduction of interproximal enamel to compensate for the tooth-size discrepancy created by the very large maxillary lateral incisors, would allow for alignment of the upper teeth without creating incisor protrusion. H to J, Because of the severe rotations of the irregular maxillary incisors, after alignment was completed but with the orthodontic appliance still in place, repositioning of the maxillary frenum and sectioning of the elastic gingival fibers were carried out. K, Three weeks later. L to P, After 18 months of treatment, both the occlusion and appearance of the teeth were greatly improved. Q, Cephalometric superimposition shows slight retraction of the maxillary incisors and mild proclination of the mandibular incisors, as was desired in this case. R, Panoramic radiograph 1 year after the orthodontic treatment was completed. The periodontal condition remained under good control during and following the orthodontic treatment. Note the fill-in of alveolar bone in the area where the severely affected maxillary right second premolar was extracted. (Periodontal surgery by Dr. R. Williams.)
Modifications in treatment mechanics are discussed at the end of this chapter.
Prosthodontic–Implant Interactions
Adults presenting for comprehensive orthodontic treatment often also have dental problems that require restorations. Such problems include loss of tooth structure from wear and abrasion or trauma, gingival esthetic problems, and missing teeth that require replacement with either conventional prosthodontics or implants.
Problems Related to Loss of Tooth Structure
The positioning of damaged, worn, or abraded teeth during comprehensive orthodontics must be done with the eventual restorative plan in mind. Early consultation with the restorative dentist obviously becomes important. There are four important considerations in deciding where the orthodontist should position teeth that are to be restored: the total amount of space that should be created, the mesiodistal positioning of the tooth within the space, the buccolingual positioning, and the vertical positioning. It is important to determine in advance whether the orthodontic goal is to level the incisal edges and marginal ridges, the gingival margins and contours, or the bone levels.
When tooth structure has been lost all the way to beyond the normal contact point, the tooth becomes abnormally narrow, and restoration of the lost crown width, as well as height, is important. The orthodontic positioning must provide adequate space for the appropriate addition of the restorative material. The ideal position may or may not be in the center of the space mesiodistally—this would depend on whether the most esthetic restoration would be produced by symmetric addition on each side of the tooth or whether a larger buildup on one side would be better (see Figure 7-32).
Similarly, the ideal buccolingual position of a worn or damaged maxillary tooth would be influenced by how the restoration was planned. If crowns are planned, the tooth should be in the center of the dental arch without tight contact with the opposing arch. But if a facial veneer is to be used for an incisor or canine (Figure 18-34), the orthodontist should place the tooth more lingually than otherwise would be the case, in contact with its antagonist in the lower arch, to accommodate the thickness of the veneer on the facial surface. Finally, better restorations can be done if the orthodontist provides slightly more space than is required, so there is room for the restorative dentist to finish and polish proximal surfaces. The slight excess space can then be closed with a retainer.
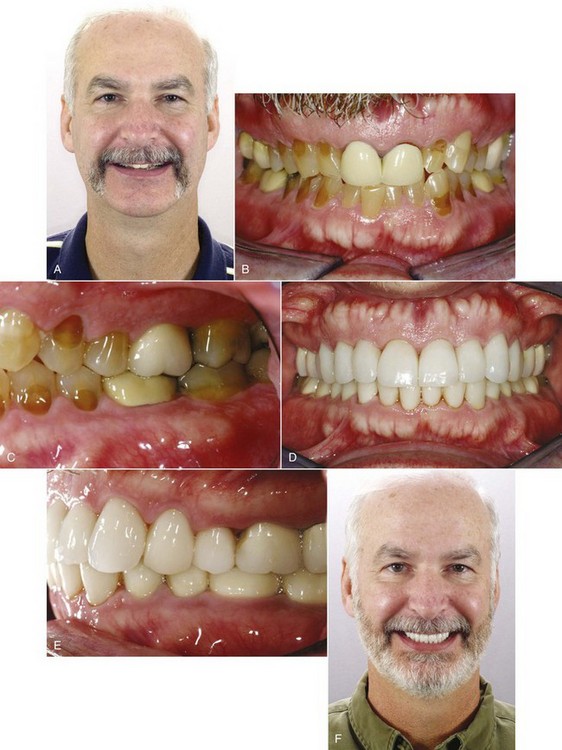
FIGURE 18-34 A, This 49-year-old man sought treatment to improve the appearance of his teeth, which were badly worn and stained. He was careful to minimize the display of his incisors on smile. B, Crowns had been placed on the maxillary central incisors, but they were too short for their width. C, The other teeth in both arches were badly worn and stained. The treatment plan was to align the teeth, opening some space to facilitate buildups and laminates. D to F, Age 51, after treatment, with crowns and laminates for correction of the wear and staining that were placed after the end of active orthodontic treatment. The posttreatment smile, with as much display of lower as upper teeth, is appropriate for his age, although slightly longer veneers for the upper incisors would have been better. The patient chose to have the crowns and laminates made whiter than was really consistent with his age and obviously valued the contrast with his previous condition.
If only a small amount of tooth structure has been lost, as for instance if the incisal edge of one incisor has been fractured, it may be possible to smooth the fractured area and elongate the damaged tooth so that the incisal edges line up. The result, however, will be uneven gingival margins, which means that elongation of a fractured tooth must be done with caution and with consideration of the extent to which the gingival margins are exposed when the patient smiles. Before acceptably esthetic composite resin buildups of anterior teeth were available, orthodontic elongation of fractured teeth was a more acceptable treatment approach than it is at present. Now, more than 1 to 2 mm of elongation rarely is a good plan unless the patient never exposes the gingiva.
Gingival Esthetic Problems
Gingival esthetic problems fall into two categories: those created by excessive and/or uneven display of gingiva and those created by gingival recession after periodontal bone loss.
The importance of maintaining a reasonably even gingival margin in the maxillary incisor area, especially when patients show the gingiva when they smile (as most do), is a factor in deciding on the best treatment when one lateral incisor is missing. Substituting a canine on one side will result in uneven gingival margins unless great care is taken to extrude the canine and reduce its crown height, even if the crown of the substituted canine is recontoured (see Figure 7-30). If several teeth have been worn or fractured, extruding them can create an unesthetic “gummy smile” even if the gingival margins are kept at the same level across all the teeth. In that circumstance, it would be better to intrude the incisors to obtain a proper gingival exposure and then restore the lost crown height. Dental esthetics is not just the teeth. A particularly distressing problem is created by gingival recession after periodontal bone loss in the maxillary incisor region, which creates “black triangles” between these teeth (see Figure 6-29). The best approach to this problem is to remove some interproximal enamel so that the incisors can be brought closer together. This moves the contact points more gingivally, minimizing the open space between the teeth. The more bulbous the crowns were initially, the more successful this approach can be.
Missing Teeth: Space Closure versus Prosthetic Replacement
Old Extraction Sites: In adults, closing an old extraction site is likely to be difficult. The problem arises because of resorption and remodeling of alveolar bone. After several years, resorption results in a decrease in the vertical height of the bone, but more importantly, remodeling produces a buccolingual narrowing of the alveolar process as well. When this has happened, closing the extraction space requires a reshaping of the cortical bone that comprises the buccal and lingual plates of the alveolar process. Cortical bone will respond to orthodontic force in most instances, but the response is significantly slower.
An old mandibular first molar extraction site often poses a particular problem because mesial drift of the second and third molars and distal drift of premolars have partially closed it, and the molars have tipped mesially. In adjunctive treatment, as shown above, a mesially tipped second molar usually is uprighted by tipping it distally, and then a bridge is placed. If comprehensive treatment is planned, should the space be closed by bringing the first molar mesially? This depends very much on the specific problems of an individual patient (Figure 18-35). Often, it is better judgment to open a partially closed old extraction site and replace the missing tooth with a bridge or implant. This decision should be considered carefully in consultation between the orthodontist and prosthodontist.
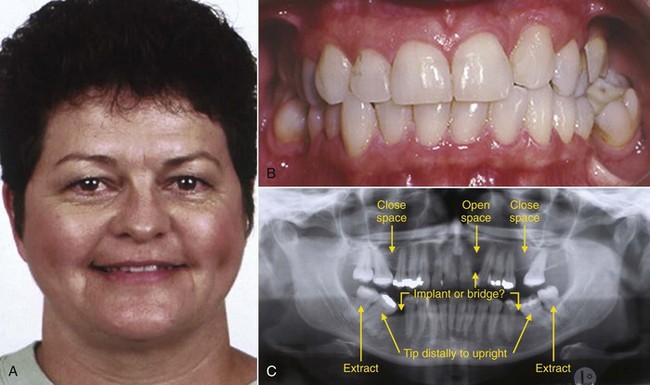
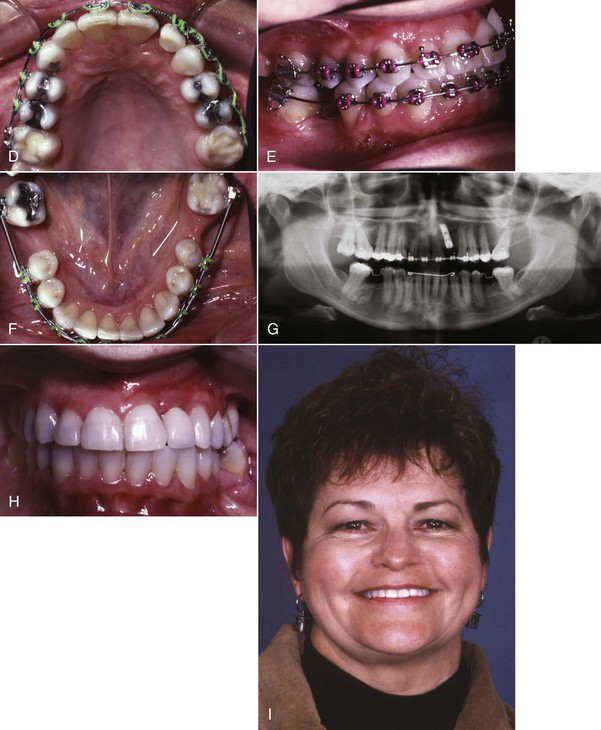
FIGURE 18-35 A, At age 48, this woman sought treatment to replace missing teeth and improve her appearance, especially her “crooked smile.” She commented that she had provided orthodontic treatment for her two children, sent both through college, and “Now it’s my turn.” B, The maxillary left lateral incisor and all four first molars were missing. The left canine had had a composite buildup to close the remaining lateral incisor space. The maxillary posterior teeth were in a crossbite relationship, especially on the left side. C, Areas of periodontal bone loss were present, but at this point, active periodontal disease had been brought under control. The key questions in planning treatment revolved around whether to close old extraction spaces or open them for prosthetic replacements. To improve symmetry in the maxillary arch and obtain better smile esthetics, opening space for replacement of the missing lateral incisor was needed, and space closure in the maxillary left molar area would facilitate opening the anterior space. The mandibular third molars would be extracted so the second molars could be uprighted and rolled lingually to improve the crossbite. D to F, Treatment progress. Note the acrylic pontic tied to the maxillary archwire in the lateral incisor space. In the mandibular arch, the teeth adjacent to the space that was opened for a replacement for the first molars required restorations, and ridge augmentation would be required on the left side for an implant, so the decision was bridges rather than implants in the lower arch. G, An implant was placed in the lateral incisor area, and the maxillary appliance was retained during initial healing as the best way to supply a temporary pontic. Note that fixed retainers are in place in the mandibular arch, where bridges are to be placed. H, Crown on implant. I, Posttreatment smile.
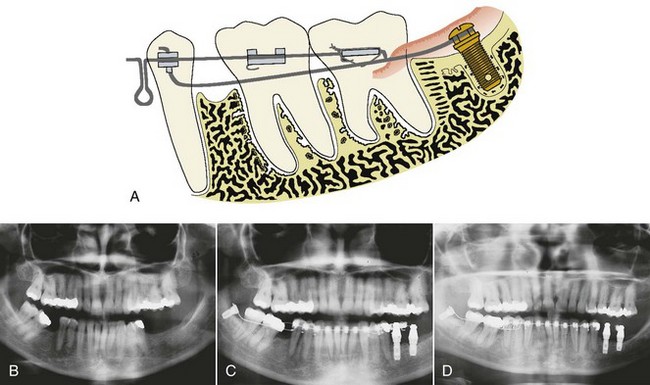
FIGURE 18-36 A to D, Use of an implant in the ramus for anchorage to move the mandibular second and third molars mesially when it is desired to close an old first molar extraction site. Note that a wire extending forward from the implant stabilizes the premolar and through it the anterior teeth, so that they are not pulled posteriorly in reaction to anterior movement of the second and third molars. (Redrawn from Roberts WE. Chapter 10. In: Graber LW, Vanarsdall RL, Vig KWL, eds. Current Orthodontic Principles and Techniques. 5th ed. St Louis: Mosby; 2012.)
If it is desired to move lower molars forward into an old first molar or second premolar extraction site, a temporary implant in the ramus can be used to provide the necessary anchorage and avoid retracting the lower anterior teeth. This technique, pioneered by Roberts, offers a level of control that cannot be obtained in any other way (Figure 18-36). Mesial root movement is technically much more difficult than distal tipping, but the larger problem is that cortical bone remodeling usually is required to close the space because of atrophy after the old extraction. Even with skeletal anchorage, the space closure is likely to be quite slow. Panoramic radiographs of two patients with similar spacing in the lower arch after early loss of mandibular first molars, one who had distal tipping for bilateral uprighting of second and third molars, the other who had bilateral space closure with mesial root movement, are shown in Figure 18-37. Both had comprehensive treatment with use of alveolar bone screws as anchorage. For the patient with space opening, the factor that determined treatment time was other aspects of the malocclusion; for the one with space closure, the long treatment time was primarily determined by the space closure.
Tooth Loss Due to Periodontal Disease: A space closure problem is also posed by the loss of a tooth to periodontal disease. Sometimes, closure of the space where a hopelessly involved tooth was extracted results in an improvement of the periodontal situation (see Figure 18-33). Unless at least one bony wall remains, however, it is better to move teeth away from such an area, in preparation for a prosthetic replacement, because normal bone formation cannot be expected as the tooth moves into the defect.
However, there is an exception. First molars and incisors are lost in some adolescents and young adults to aggressive juvenile periodontitis, which differentially attacks these teeth and is characterized by the presence of a specific microbe, Actinobacillus actinomycetemcomitans. Once the disease process has been brought under control, which now typically involves antibiotic therapy, the causative agent seems to disappear.19 Although bone around the first molars is often totally destroyed, neither the second molar nor the second premolar is significantly affected in most patients. Orthodontic closure of the incisor spaces is rarely feasible, but in adolescent or young adult patients, it often is possible to orthodontically close the first molar extraction sites, bringing the second permanent molar forward into the area where the first molar was lost, without having to resort to implants for additional anchorage. The second molar brings its own investing bone with it, and the large bony defect disappears.
This favorable response is attributed to some combination of three factors: the relatively young age of these patients, the fact that the original attack was almost entirely on the first molars, and the disappearance of the specific bacterial flora. In an older patient who has lost a tooth to periodontal disease, it is unlikely that the other teeth have been totally spared or that the bacterial flora have changed, and it would not be good judgment to attempt to close the space.
Comprehensive Orthodontics in Patients Planned for Implants: In older patients with long-standing tooth loss, bone grafts to widen the alveolar process in the area of future implants often will be required. Usually it is advantageous to go ahead with placement of grafts in areas that will receive implants while orthodontic treatment is being carried out in other areas of the mouth. The goal should be to have the patient ready for definitive prosthodontic treatment as soon as possible after the orthodontic appliances are removed, rather than having a considerable delay while both grafts and implants are done.
After the grafts have matured to the point that implants can be inserted, it also may be possible to do the implant surgery before all orthodontics is finished. The implant surgery itself rarely causes significant delay, and an osseointegration period during the orthodontic treatment is advantageous. A long delay caused by graft healing and maturation before implants can become a problem in orthodontic retention. Almost always, a fixed orthodontic retainer is the best choice to maintain a space for an implant. In the anterior area, patients often prefer a temporary resin-bonded bridge, which must be removed for implant surgery and reinserted afterward unless immediate loading of the implant is feasible.
A damaged and ankylosed maxillary incisor or canine in a teenager poses a special problem when eventual replacement with an implant is planned. The ankylosed tooth interferes with orthodontic treatment to align the other teeth and can become quite unsightly, but alveolar atrophy will occur if the tooth is extracted before vertical growth is completed and the implant can be placed. In this situation, the alveolar bone can be “banked” by removing the crown of the offending tooth but retaining the endodontically treated root (Figure 18-38), and there is a better chance of successful implant placement later without a bone graft. Meanwhile, the orthodontic treatment can be completed with a pontic tied to an archwire, and then a temporary resin-bonded bridge until vertical growth is completed and it is safe to place the implant.

FIGURE 18-38 This 14-year-old boy had a lingually displaced and ankylosed maxillary central incisor after a basketball injury. A and B, Prior to treatment. It was not possible to correct the alignment of other teeth without removing the ankylosed tooth, which eventually would be replaced with an implant, but loss of alveolar bone in the area would result from early extraction. C, The decision was to remove only the crown of the ankylosed tooth, retaining the root as a way of maintaining the alveolar bone. With an orthodontic appliance in place, a pontic was tied to the archwire when the crown was removed. The root was filled with calcium hydroxide, and gingival and palatal tissue (D) was sutured over it. E, It then was possible to expand both arches and correct the malocclusion. At the end of active treatment, a pontic was placed on the orthodontic retainer as a temporary replacement. An implant was placed successfully at age 18.
However successful the treatment is up to that point, placing an implant too soon creates a major problem. The implant becomes the equivalent of an ankylosed tooth and will appear to intrude as vertical development continues and the other teeth erupt (Figure 18-39). This creates a discrepancy of the gingival margins as well as the incisal edges, which is very difficult to manage even if the implant is removed and replaced with a new crown. To some extent this problem can occur later in life because slow vertical growth often continues into middle age (see Chapter 4).

FIGURE 18-39 For this patient, an implant to replace a missing maxillary lateral incisor was placed at age 15. At age 17, further vertical growth had led to unesthetic relative intrusion of the implant, with displacement of both the incisal edge and gingival margin. At this point, a longer crown on the implant is not a satisfactory solution. There is no good alternative to removing the implant, grafting the area, and placing a new implant.
Special Aspects of Orthodontic Therapy for Adults
Both the goals and the stages of comprehensive orthodontic treatment for adults are the same as those in the treatment of adolescents. The orthodontic treatment, however, often must be modified in several ways:
• The patient’s desire for a minimally apparent or invisible orthodontic appliance should be accommodated if possible. This requires consideration of CAT, ceramic or other nonmetallic brackets, or lingual orthodontics.
• In patients who have lost some periodontal support, orthodontic force must be kept light.
• Intrusion often is required in the leveling of both arches because of the lack of growth, particularly the small amounts of vertical growth that allow some extrusion of the posterior teeth in adolescents without leading to mandibular rotation.
• Skeletal fixation in the form of miniplates, screws, or implants is likely to be required for some types of tooth movement, especially intrusion of posterior teeth, protraction of posterior teeth, or to support maximum retraction and/or intrusion of anterior teeth.
In the following discussion, it is assumed that an appropriate and feasible treatment plan has been prepared, and these special aspects of adult treatment are reviewed.
Esthetic Appliances in Treatment of Adults
In the treatment of adults, ceramic or tooth-colored brackets are more likely to be desired than in typical treatment of adolescents, but these do not change treatment procedures from those discussed in Chapters 14 to 16. Both CAT, which is almost totally limited to adult treatment, and lingual orthodontics require a quite different approach.
Clear Aligner Therapy
The basic approach to comprehensive CAT, involving the production of a series of aligners on stereolithographic casts produced from virtual models, is described in Chapter 10. Experience has shown that some types of tooth movement are much more easily accomplished with clear aligners than others (see Box 10-1). Despite this, increasingly it is possible to treat almost all types of orthodontic problems in adults with clear aligners—if bonded attachments are used appropriately to provide a firmer grip on the teeth that require root movement, if the amount of change from one aligner to the next is reduced appropriately, and if some phases of complex treatment are provided by fixed appliances while aligners are used for the rest.
Prior to the use of bonded attachments on teeth so that an aligner could grip them more tightly, extrusion and rotation were very difficult and the amount of root movement needed for root paralleling at extraction sites was almost impossible. With judicious use of attachments and small amounts of movement from one aligner to the next, extrusion (as in the closure of anterior open bite by extruding incisors) now can be accomplished (Figure 18-40). Rotation and extrusion can be facilitated by modifying an aligner to allow use of an elastic to a button on the rotated tooth (see Figure 18-22). Space closure remains difficult but can be managed if attachments on the teeth are used correctly (Figure 18-41). It seems likely that in the future, a brief period of fixed appliance treatment (and perhaps skeletal anchorage in the form of bone screws, as shown in Figure 18-42) will be combined with aligners to make difficult tooth movement more practical in adults who want the esthetic advantage of CAT.

FIGURE 18-40 Extrusion of teeth, as in this patient to close an anterior open bite, is difficult with Invisalign but can be accomplished with the use of bonded attachments on the teeth so the aligners have a better grip. A and B, Age 24, prior to treatment. She reported previous orthodontic treatment at age 12; the open bite developed during subsequent adolescent growth. C, The ClinCheck form showing the attachments to be placed on the teeth (see Figure 18-22 for the clinical appearance of clear plastic bonded attachments). Air-rotor stripping was performed in the upper arch to provide space to retract the incisors and reduce overbite (see Figure 11-16 for the reproximation form that accompanies the ClinCheck form when this is part of the treatment plan). She had 19 upper and 10 lower aligners. Treatment required  months. D and E, Age 25, after treatment. A lower bonded retainer and a maxillary suck-down retainer were placed. The occlusion was stable on 2-year recall. (Courtesy Dr. W. Gierie.)
months. D and E, Age 25, after treatment. A lower bonded retainer and a maxillary suck-down retainer were placed. The occlusion was stable on 2-year recall. (Courtesy Dr. W. Gierie.)

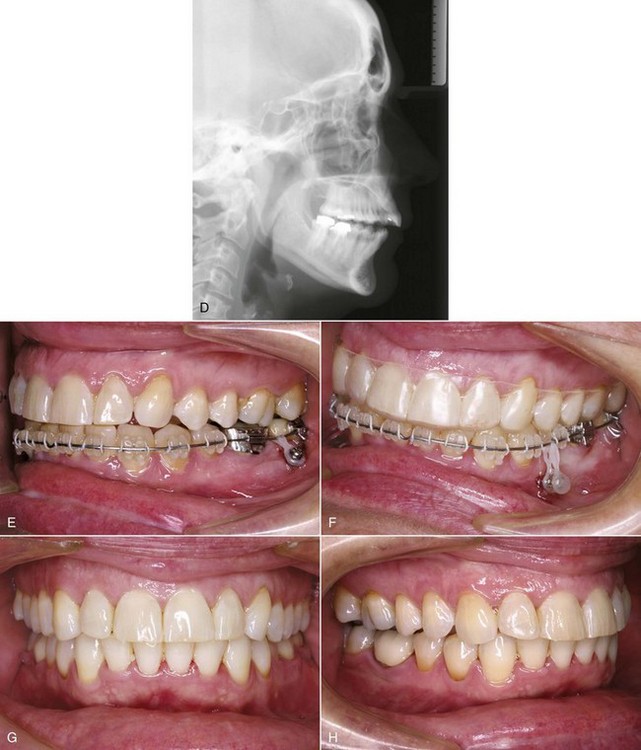
FIGURE 18-42 A and B, For this 47-year-old woman, an unusual unilateral open bite had developed slowly over the previous 5 years, with little or no change during the last year. C, The panoramic radiograph showed condylar asymmetry, with resorption of the left condyle that was tentatively attributed to osteoarthritis. D, The cephalometric radiograph showed a different vertical level of the mandibular posterior teeth on the two sides, and virtual intrusion of the mandibular posterior teeth on the left side indicated that this would allow the mandible to rotate upward and forward, closing the unilateral open bite and bringing her to nearly normal occlusion. The treatment plan was to use a fixed appliance in the lower arch with skeletal anchorage to close the posterior teeth on the left side and close the open bite, while aligning the upper arch with Invisalign and completing treatment with Invisalign in both arches. E, Bone screw as anchorage for intrusion of the mandibular molars. F, A second bone screw later for anchorage to intrude the premolars. While the intrusion was occurring, a series of aligners was used in the maxillary arch; note the final aligner being used as a retainer at this point in treatment. Once the bite was closed (which took 8 months), the expected relapse tendency was not observed during the next 6 months, and at that point, a revision series of aligners was used over a period of another 4 months to complete the treatment. G and H, Frontal and lateral posttreatment views. The open bite closure has been stable for over 3 years at this point.
Lingual Orthodontics
Progress in lingual orthodontics in the last few years has culminated in the development of techniques that use a custom-formed pad for each tooth to provide more secure bonding of the appliance, a low-profile attachment made so that wires can be inserted from above, and computer-controlled wire-bending robots to generate the archwires. These steps are described in Chapter 10 (see Figures 10-37 and 10-40).
A major difficulty in lingual orthodontics is the short span of archwires between attachments. For any wire, the shorter the span, the stiffer the material. The distances between the teeth along the archwire are so short that it can be hard to align severely crowded teeth, particularly for lower incisors. Because the lingual surfaces of the incisors, canines, and posterior teeth do not line up nearly as well as the facial surfaces, there is no way to avoid considerable shaping of all lingual archwires, including the A-NiTi wire for initial alignment. Scans to obtain the information and remotely forming the wires on a wire-bending robot make this a much more precise and less time-consuming procedure now. One way to look at it is that although modern lingual orthodontics is quite different from CAT, it is based on computer technology to a similar extent.
With lingually bonded brackets and archwires, any type of tooth movement now can be produced quite efficiently, and root positioning at extraction sites is not a particular problem (Figures 18-43 and 18-44).


FIGURE 18-43 A and B, This 45-year-old woman sought orthodontic treatment to correct her incisor crowding and improve the appearance of her smile. She chose comprehensive treatment with a lingual fixed appliance (Incognito, 3M-Unitek) to maintain dental esthetics during treatment. The treatment plan was to align the teeth, correct the buccal occlusion, and level the gingival margins rather than the incisal edges of the maxillary incisors in preparation for veneers on these teeth after the orthodontics was completed. C to E, Progress in treatment, showing the alignment achieved with computer-formed archwires. Toward the end of treatment, facial attachments were bonded to the maxillary canines and mandibular canines and premolars to make it easier for her to wear vertical elastics to settle the posterior teeth into occlusion. F, Smile appearance at the completion of orthodontics, age 47, after 24 months of active treatment. At this point, the gingival margins are correctly aligned, making the different crown heights of the incisors more obvious. G, Computer simulation of the effect of veneers on the maxillary incisors to improve their length, which led to the patient’s acceptance of this final step in treatment. (Courtesy Dr. D. Grauer.)
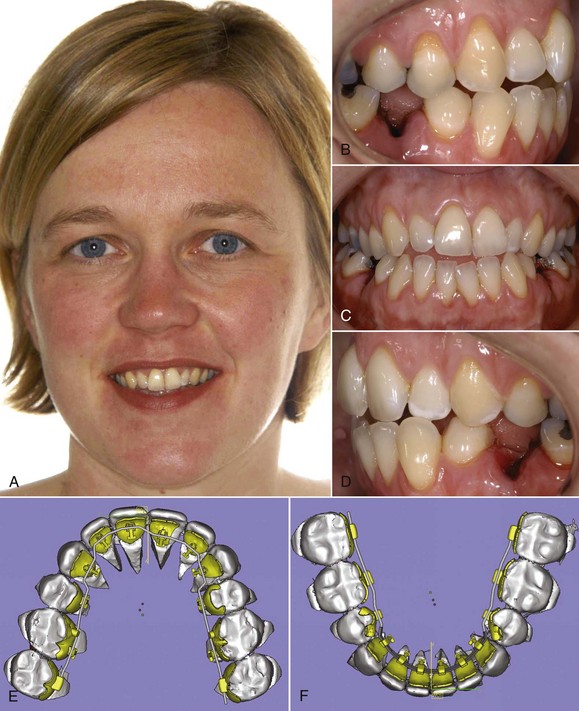
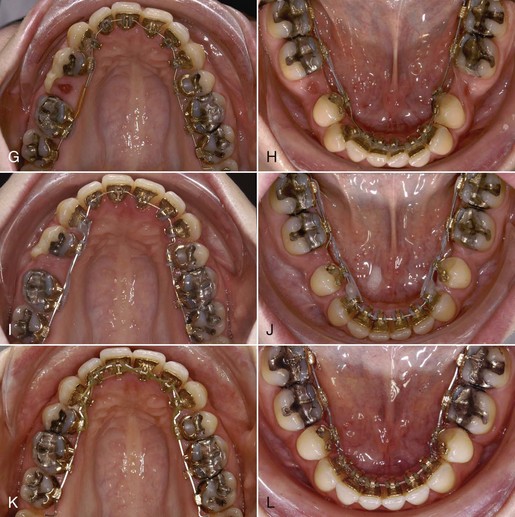

FIGURE 18-44 This 31-year-old woman sought orthodontic treatment to improve her dental appearance and function and chose lingual orthodontics to avoid the outward appearance of braces on her teeth. A, Smile before treatment. B to D, Pretreatment intraoral views. She had moderately severe crowding of lower incisors, posterior crossbite, and an anterior open bite that would have placed her in anterior crossbite if corrected without retraction of the lower incisors. Her maxillary right first premolar had been extracted when she was a child, and the dental midline was deviated to the right. The treatment plan called for extraction of the mandibular second premolars and maxillary left second premolar to provide space for alignment and repositioning of the anterior teeth. E and F, Laser scans of her dental casts were used in the Incognito software to plan both the contour of the custom lingual bonding pads for each tooth and the shape of the archwires that would be produced by a wire-bending robot. G and H, Computer-formed superelastic A-NiTi archwires were used in the initial stage of treatment. Note the use of a temporary bonded plastic facing to conceal the maxillary extraction site. I and J, Space closure was done with elastomeric chains on an undersized (16 × 22) steel rectangular archwire formed by the wire-bending robot. K and L, Full-dimension rectangular TMA archwires were used in finishing. M to O, Smile and intraoral views at the completion of treatment. Closure of the extraction spaces with good root paralleling was achieved. Cosmetic restoration of the maxillary left lateral incisor was planned as a final treatment procedure. (Courtesy Dr. D. Wiechmann.)
An important question is the extent to which the treatment plan, represented by the setup of teeth from which the shape of archwires is derived, is achieved in the posttreatment alignment and occlusion of the teeth. For the Incognito lingual technique (shown in the previous figures), this information now has been achieved by digital superimposition of the treatment outcome on the setup.20 The data show (see Figure 10-38) that there is a precise reproduction of the treatment goal in the tooth positions that are achieved (most of the time, within less than 1 mm or 5 degrees of inclination), except that second molars are not positioned quite as accurately. Feedback of this type of information to improve the computer planning has the potential to improve accuracy for all the computer-aided design/computer-aided manufacturing (CAD/CAM) methods now being introduced into orthodontics.
Applications of Skeletal Anchorage
In this potentially very important and rapidly developing area, progress is continuing in the development of the necessary hardware and clinical techniques, which means that improvements in both areas undoubtedly will appear in the near future. The devices may change, but the principles in their use will not.
There are now four major applications for skeletal anchorage in treatment of adults:
1. Positioning individual teeth when no other satisfactory anchorage is available (usually because other teeth have been lost to dental or periodontal disease).
2. Retraction of protruding incisors.
3. Distal or mesial movement of molars (and the entire dental arch if needed).
4. Intrusion of posterior teeth to close an anterior open bite or anterior teeth to open a deep bite.
Anchorage for Positioning Individual Teeth
An excellent use of bone screws for anchorage is in patients, usually adults, who do not have anchor teeth (Figure 18-45) or enough conventional anchorage for the desired tooth movement. This is adjunctive treatment with a partial fixed appliance that involves space distribution. It usually is done by an orthodontist in preparation for implants and prosthodontic replacement of missing teeth.

FIGURE 18-45 A and B, Crowded incisors and canine interference in a patient who needs replacement of missing mandibular posterior teeth. C and D, Retraction of the right canine and first premolar, using a bone screw for anchorage. E, Teeth aligned without any anterior movement prior to replacement of the missing posterior teeth.
Bone screws that penetrate directly through the oral tissues typically have a shoulder at the point of soft tissue contact and a modified head to which wires, springs, or elastics can be attached. Screws can be lightly loaded immediately or within a few days of being placed, and tend to tighten up and become firmer as tension accelerates bone remodeling. Application of heavy force increases the chance that the screw will become loose and fall out—but force heavy enough to cause that almost always is too much for optimal tooth movement anyway.
Retraction and Intrusion of Protruding Incisors
Protruding maxillary incisors usually are tipped facially, and tipping them lingually is an obvious way to correct their axial inclination. This movement also brings the incisal edges downward, which is good if increasing incisor display and closing an anterior open bite are part of the treatment plan, but bad if maintaining or decreasing incisor display and correcting an anterior deep bite are needed. With segmented arch mechanics, maxillary incisors can be both retracted and intruded (see Figure 9-48) if excellent anchorage is maintained with stabilizing lingual arches and headgear if necessary. This is technically difficult, requires excellent patient cooperation, and now has been superseded by use of skeletal anchorage.
Both bone screws in the maxillary alveolus and miniplates at the base of the zygomatic arch offer anchorage that makes retraction much easier and more predictable (Figure 18-46). The direction of force, both upward and backward, is ideal for this purpose, and A-NiTi springs provide constant known force levels.
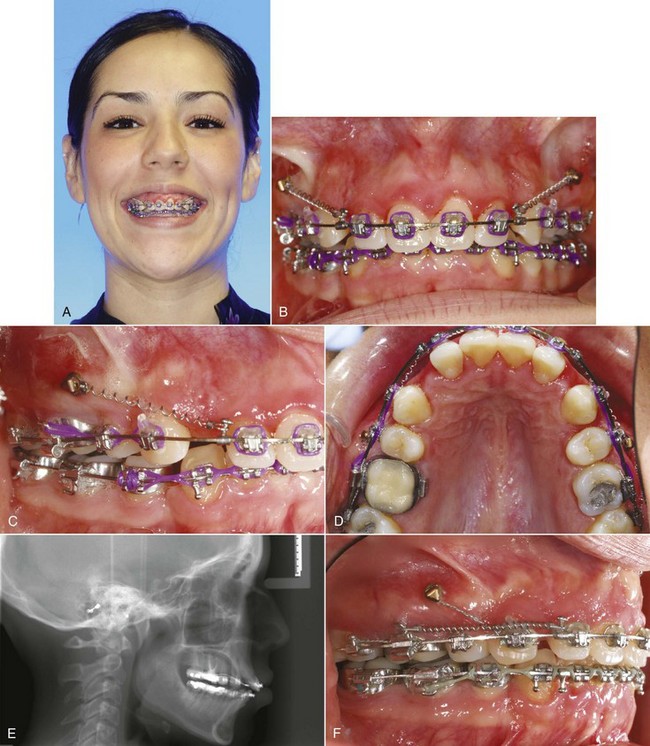
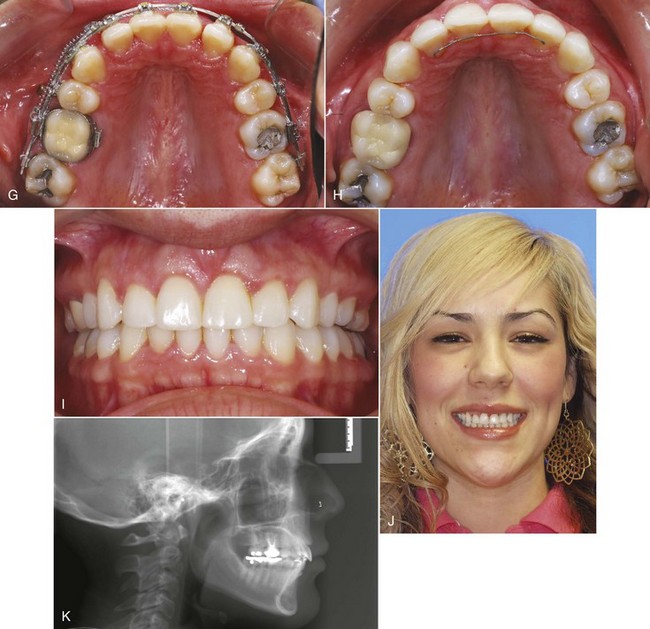
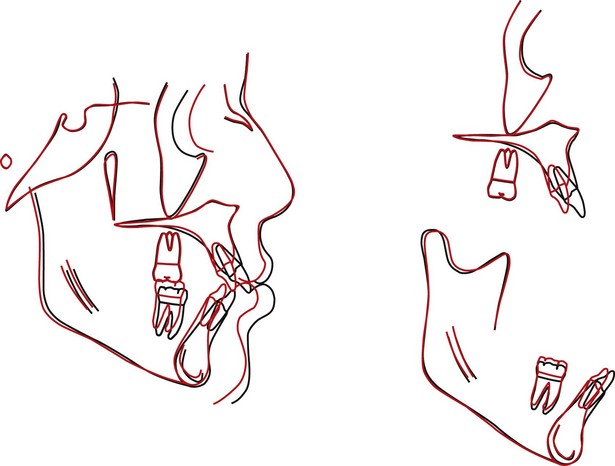
FIGURE 18-46 A to D, The treatment plan for this 26-year-old woman was retraction of the maxillary incisor segment into first premolar extraction sites and intrusion of her maxillary incisors. Alveolar bone screws placed mesial to the first molars were used initially as direct skeletal anchorage, with NiTi coil springs attached to the screws delivering 200 gm as the source of force. The mandibular first premolar extraction sites were closed without support from skeletal anchorage. E, A progress cephalometric radiograph shows the orientation of the incisors after partial space closure. Note the auxiliary intrusion arch to the anterior segment. F, Progress in maxillary space closure, with a switch to indirect anchorage after retraction of the canine (note that the canine is tied tightly to the bone screw to stabilize the posterior segment as space closure continues), while a NiTi coil from the posterior to the anterior segment provides the force. G, Space closure progress, occlusal view. H and I, Space closure completed. J, The posttreatment smile showing the decreased exposure of maxillary gingiva and improved vertical lip–tooth relationship. K, Posttreatment cephalometric radiograph. L, Cephalometric superimposition showing the retraction and intrusion of the maxillary incisors. (Courtesy Dr. N. Scheffler.)
Retraction of maxillary anterior teeth with implants in the palate was one of the first applications of skeletal anchorage. An implant in the center of the palate can be used to stabilize a lingual arch that prevents movement of the molars to which it is attached (see Figure 9-35). This would make it easier to control the molars as incisors are retracted, but the orthodontic mechanotherapy is more difficult when an upward-backward force is not derived directly from the skeletal anchor, and it can be difficult to remove a palatal implant that becomes osseointegrated. Current techniques to stabilize a lingual arch are designed around a device intended to be held in place with short screws that are more easily removed. Nevertheless, it seems likely that alveolar bone screws will largely replace palatal anchors for retracting protruding maxillary anterior teeth. Palatal anchorage still is likely to be used for molar distalization (see below).
Protruding mandibular incisors also can be retracted using alveolar bone screws for anchorage, but this is less likely to be needed because they should be tipped lingually, not torqued as usually is the case with maxillary incisors. The narrow basal bone in the mandibular anterior area usually contraindicates torque in retracting the incisors because of the risk of root resorption (see Chapter 9).
Distal Movement of Molars or the Entire Dental Arch
Maxillary Distalization: Distal movement of the maxillary molars is one way to provide space in a crowded maxillary arch; distal movement of the entire maxillary dental arch would provide a way to correct a Class II malocclusion due to a forward position of the upper teeth on their skeletal base. For both types of movement, miniplates rather than bone screws provide a more predictable outcome and allow roots to move without interference from screws in the alveolar process, but bone screws can be used if they are placed in the palate or in the infrazygomatic process away from the roots (Figure 18-47). The entire arch usually can be moved back 2 to 4 mm. Extraction of second molars to provide space for posterior movement of the dental arch or extraction of premolars so that only the anterior segment has to be moved is needed if a greater amount of incisor retraction is necessary.
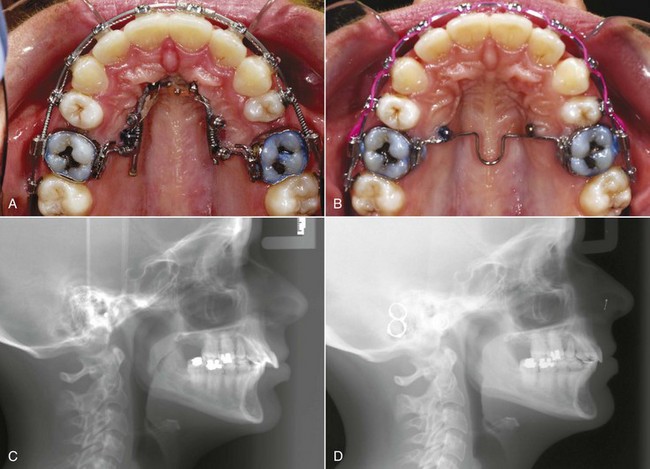
FIGURE 18-47 A, For this 28-year-old patient with protrusion of the maxillary arch and a partially corrected Class II malocclusion despite previous maxillary first premolar extraction, the treatment plan was palatal anchorage with bilateral bone screws for distalization of the entire maxillary arch. Initially, the molars were distalized to move them back to a Class II relationship rather than a super-Class II. B, Then the palatal screws were used to stabilize the molars while the other teeth were retracted. C, The pretreatment and (D) posttreatment cephalometric radiographs show the overjet reduction and attainment of the desired molar relationship. (Courtesy Dr. N. Scheffler.)
Mandibular Distalization: Moving the entire mandibular arch distally was simply impossible until skeletal anchorage became available. Now that it can be done, usually via a long bone screw in the mandibular buccal shelf or the ramus (usually less desirable), most American orthodontists still do not think of doing it in the two circumstances in which it can be helpful: (1) Class III malocclusion with a component of mandibular dental protrusion, which is almost never seen in Class III patients of European origin but does occur reasonably frequently in Asians, for whom this form of Class III camouflage can be quite acceptable (Figure 18-48), and (2) incisor protrusion created during treatment of severe crowding. This was avoided by extraction to prevent it until popularization of the idea that light forces and just the right self-ligating bracket somehow allowed nonextraction treatment without protrusion.21 In fact, lower incisor protrusion is a common accompaniment to arch expansion to correct severe crowding with all bracket types, and using skeletal anchorage to bring the whole dental arch back to a better position relative to basal bone can be quite helpful.22
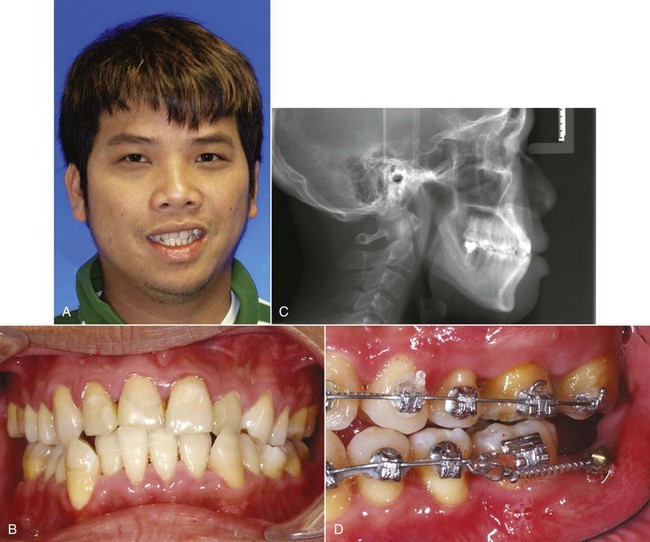

FIGURE 18-48 For patients of European descent, it is rarely appropriate to correct a Class III tendency and anterior crossbite by retracting the lower incisors. Asians, however, often have a component of mandibular dental protrusion; if so, retracting the incisors or moving the entire mandibular arch distally can correct the crossbite without harm to the facial appearance. A and B, Pretreatment smile and dental appearance, with crowding and moderate protrusion of the lower anterior teeth. C, The pretreatment cephalometric radiograph showing the protrusion of the lower incisors. One mandibular second molar had been lost previously to caries, the other had been treated endodontically, and the third molars had been removed. The plan was extraction of the remaining mandibular second molar, with distalization of the entire arch to gain a better functional molar relationship, as well as correct the crossbite. D, Bone screws were placed bilaterally in the buccal shelf of the alveolar process (which is preferred over a screw in the ramus when this area is available), and NiTi springs were used to move the dental arch posteriorly. E and F, The posttreatment dental appearance and (G) smile, with correction of the mandibular anterior crowding and crossbite. The smile was greatly improved, with little effect on apparent chin prominence. (Courtesy Dr. N. Scheffler.)
Molar Protraction: Space closure by bringing molars forward can be accomplished easily with a miniscrew to provide direct or indirect anchorage. Indirect anchorage, using the screw wired to an anchor tooth, generally is preferable, especially in the mandible where the vestibule is shorter. Direct anchorage, using a power arm from the molar so that the force direction is near the center of resistance, can be satisfactory for protraction of a maxillary molar (Figure 18-49).
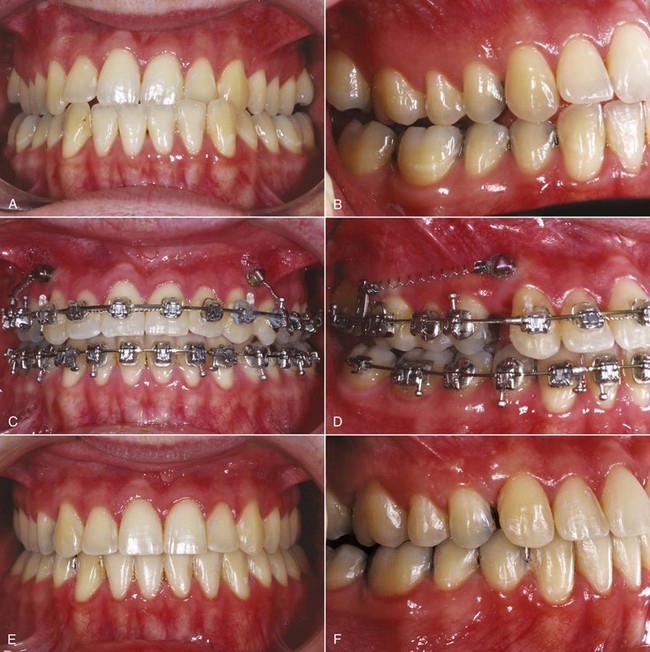
FIGURE 18-49 A and B, This 28-year-old man had a unilateral anterior crossbite and a one-half cusp Class III molar relationship, with mild skeletal maxillary deficiency. The treatment plan was movement of the entire maxillary arch forward, using skeletal anchorage to maintain the anteroposterior position of the mandibular dental arch. C, Bone screws distal to the canines were used to stabilize the maxillary posterior segments while the maxillary incisors were advanced to correct the crossbite. D, Then the space distal to the canines was closed by bringing the posterior segments forward. Note the power arm to place the point of force application closer to the center of resistance of the posterior teeth to decrease their tendency to tip as they are advanced. E and F, Dental appearance and posterior occlusion after completion of treatment. (Courtesy Dr. N. Scheffler.)
Intrusion
Intrusion of teeth in adults is a consideration in two situations: (1) overerupted incisors leading to excessive display and/or anterior deep bite and (2) overerupted molars in anterior open bite with excessive face height. Occasionally, intrusion of other teeth is indicated.
Intrusion of Incisors: In adolescents and young adults (up to about age 18 in females and 20 in males) with excessive overbite, the choice between intrusion of incisors or extrusion of posterior teeth often can be resolved in favor of extrusion because vertical growth will compensate for it. In adults, the choice often must be intrusion, which is much more effective when skeletal anchorage in the form of miniplates or screws is available and when segmented rather than continuous archwires are used. The practical effect is to make both skeletal anchorage and segmented arch treatment more important in adults than in younger patients.
One potential problem with intrusion in periodontally involved adults is the prospect that a deepening of periodontal pockets might be produced by this treatment. Ideally, of course, intruding a tooth would lead to a reattachment of the periodontal fibers, but there is no basis for expecting this. What seems to happen instead is the formation of a tight epithelial cuff, so that the position of the gingiva relative to the crown improves clinically, while periodontal probing depths do not increase. Histologic slides from experimental animals show a relative invagination of the epithelium, but with a tight area of contact that cannot be probed. It can be argued that this leaves the patient at risk for rapid periodontal breakdown if inflammation is allowed to recur. Certainly, given that bone levels tend to follow the amount of intrusion, it should never be attempted without excellent control of inflammation. On the other hand, if good hygiene is maintained, clinical experience has shown that it is possible to maintain teeth that have been treated in this way and that root length and alveolar bone height are not greatly affected.23
The crown–root ratio is a significant factor in the long-term prognosis for a tooth that has suffered periodontal bone loss. Shortening the crown has the virtue of improving the crown–root ratio. In adults with bone loss and an anterior deep bite, the orthodontist should not hesitate to remove part of the crown of elongated lower incisors as an alternative to intrusion, when this would both simplify orthodontic leveling of the arch and improve the periodontal prognosis. Reducing crown height of upper incisors must be approached cautiously because of the possible adverse effect on anterior tooth display, and often intrusion of abraded incisors so that the crown can be restored to normal height is a better approach.24
The mechanotherapy needed to produce incisor intrusion in an adult is not different from the methods for younger patients described in some detail in Chapters 9 and 14. In adults, however, careful stabilization of dental arch segments during incisor intrusion is even more important, especially if the patient also has had periodontal bone loss. For those patients, skeletal anchorage via alveolar bone screws is particularly advantageous. Differential intrusion of maxillary incisors, with more intrusion on one side or intrusion on one side and extrusion on the other, also can be used to help correct a canted maxillary occlusal plane, if the cant is not too severe (see the discussion of roll deformity in Chapter 7). This is another example of tooth movement that is not possible without skeletal anchorage.
Intrusion of Posterior Teeth to Close Anterior Open Bite: Most patients with anterior open bite have elongation of the maxillary posterior teeth, so that the mandible is rotated downward and backward. The incisor segment often is reasonably well-positioned relative to the upper lip. Extrusion of the incisors to close the bite in a patient like this is neither esthetically acceptable nor stable; intrusion of the posterior segments is the ideal approach to treatment. This was essentially impossible until segmental maxillary surgery was developed in the early 1970s so that the maxillary posterior segments could be intruded. Skeletal anchorage now makes orthodontic intrusion a possible alternative to surgery (Figure 18-50).

FIGURE 18-50 Intrusion of maxillary posterior teeth can be effective treatment for an adult or late adolescent patient with a moderate long-face, open bite problem. A, Age 26, prior to treatment for correction of anterior open bite and reduction of anterior face height. The chin was 2 to 3 mm off to the right, but this was not a problem. A chin deviation of less than 4 mm rarely is noticed—the patient was unaware of it. B, Age 27, posttreatment. Note the improved facial proportions as well as correction of the open bite. C, Frontal intraoral view, showing the 6 mm anterior open bite and contact only on the distal of the first molars and second molars. D, Right lateral view with intrusion beginning. A long bone screw into the base of the zygoma is used for anchorage, with a modified Erverdi plate (AOB plate) used to control the teeth. E, Palatal view of the AOB plate, showing the twin transpalatal arches connecting the splints, which must be off the palate initially so that they do not contact the soft tissues until intrusion is complete. F, Open bite closed. The mild dental midline discrepancy, with mandibular dentition 2 mm off to the right, was not corrected because doing so would have pulled the maxillary midline off the midline of the face. (Courtesy Dr. N. Scheffler.)
For intrusion of maxillary posterior teeth, miniplates at the base of the zygomatic arch (see Figure 15-7) provide excellent anchorage. These plates are held with multiple screws and are covered by the oral soft tissues. The fixture for attachment to the orthodontic appliance extends through the soft tissue, preferably at the junction between gingiva and mucosa.
The major problem with miniplates is that they require more surgery than most orthodontists want to do, but at present many oral-maxillofacial surgeons have not been trained to do this procedure and surgical help may not be available. A long bone screw extending into the base of the zygomatic arch, which orthodontists with experience with alveolar bone screws can place, is a possible alternative. A screw of this type should be placed through attached gingiva if possible because bone screws placed in unattached tissue are at greater risk of infection and tissue overgrowth. Some preliminary separation of roots in the region in which the screw will be placed makes it easier to avoid root contact and is recommended (Figure 18-51). The screw can be placed above and between the first and second molars (if some retraction of the maxillary arch might also be needed to assist with Class II correction) or above and between the first molar and second premolar (if the patient also has a mild Class III tendency and some mesial movement of the dental arch would help).
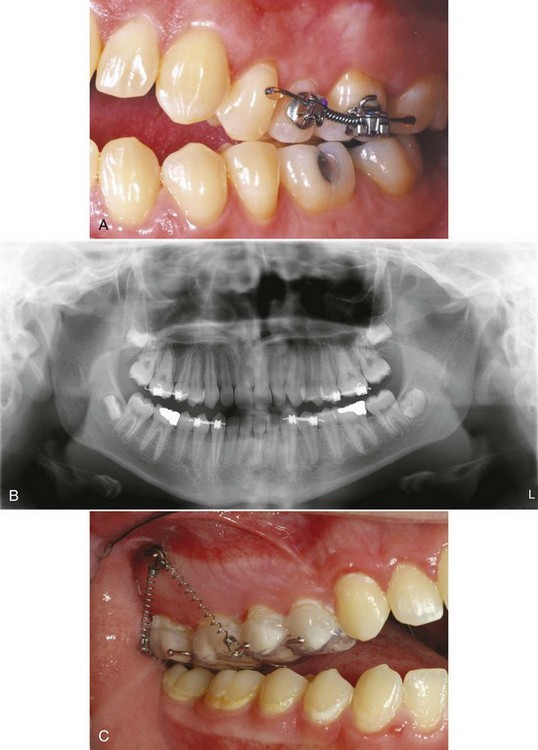
FIGURE 18-51 A, Prior to intrusion of the maxillary posterior segments to correct an anterior open bite, the roots of the second premolar and first molar are diverged to facilitate placing an alveolar bone screw between their roots. B, A panoramic radiograph of a different patient being prepared for placement of bone screws for maxillary intrusion showing the root divergence needed for placement of a long screw into the base of the zygomatic arch. C, The bone screw being used as anchorage for intrusion, using a modified Erverdi appliance to prevent buccal tipping of the teeth in the intrusion segment. (Courtesy Dr. N. Scheffler.)
An ideal force system for intrusion is created by A-NiTi springs, which provide a relatively constant known force over a considerable range of activation. An upward force on the facial of the posterior teeth is also a force to tip them facially, and control to prevent this is essential. Transpalatal lingual arches are one possibility, but controlling all the teeth in the segment being intruded is necessary. A bonded plate covering the occlusal surface of the teeth, fabricated so that it is off the palate enough to allow the intrusion, is the preferred method at present. As the mandible rotates upward and forward as the posterior teeth intrude, it may be advantageous to have a Class II or Class III component to the force, so that the maxillary arch is moved a little forward or back as the intrusion occurs, to help in obtaining correct overjet at the end of treatment. This can be facilitated by adjusting the point of attachment of the spring to the plate (Figure 18-52), as well as by locating the screw as described above.
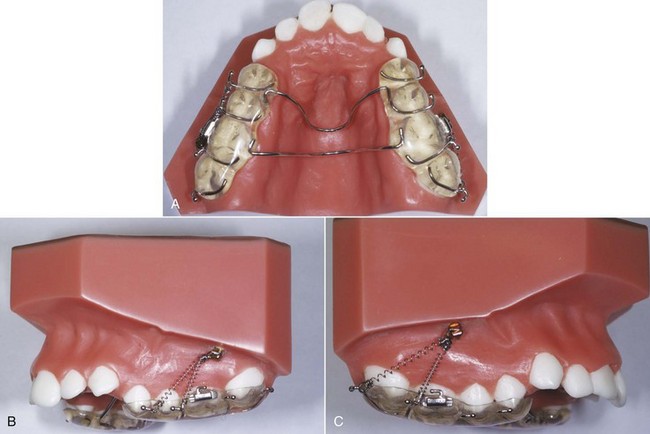
FIGURE 18-52 A, Occlusal splint for intrusion of maxillary posterior teeth. The lingual arches are off the palate, giving room for intrusion to occur without forcing them into the soft tissues. B, Intrusion springs to the bone anchor with a Class II, as well as vertical direction of force. C, Intrusion springs with a Class III direction of pull. (Courtesy Dr. N. Scheffler.)
Even with appropriate light force (not more than 50 gm to a three-tooth posterior segment), intrusion does not occur as quickly as other types of tooth movement. Space closure and most other types of movement occur at the rate of about 1 mm per month. At best, posterior intrusion occurs at half that rate. Because 1 mm intrusion of maxillary posterior teeth translates into about 2 mm closure of anterior open bite, however, a 4 mm open bite typically closes in as many months (see Figure 18-50). At that point, the rest of a complete fixed appliance can be placed, and the other necessary treatment can be completed while the intruded segment remains tied to the anchor screw or miniplate. After intrusion of the posterior segments, the same anchors used for that purpose easily can serve as anchorage for retraction or protraction of the maxillary arch.
The extent to which the posterior teeth can be intruded to close anterior open bite is not yet clear, but experience to this point suggests that on average 0.5 mm of posterior intrusion produces 1 mm closure of anterior open bite and that intrusion up to 4 mm can be obtained. Whatever the amount of intrusion, it also appears that some of it (15% to 20%?) will be lost in the short term.25 This suggests that closing a 4 to 6 mm anterior open bite is quite feasible with molar intrusion, with reasonably good short- and medium-term stability (no good data exist yet for long-term stability). Larger closure probably would require surgery to reposition the maxilla superiorly.
Patient and Doctor Perceptions of Skeletal Anchorage
How difficult is it for patients to tolerate skeletal anchorage, and how difficult is it for doctors to place and use it? The best data are for miniplates, which indicate patient acceptance is quite high and that problems with using these multiscrew anchors are surprisingly small (Figure 18-53).26 After one year, 83% of the patients said that their experience with skeletal anchorage was better than they expected, and 73% said they did not mind having the miniplate anchor. The majority commented that they did not experience pain as they thought they might. No similar study of patient reactions to bone screws has been reported, but with stability as the criterion, about 85% of bone screws are successful over a 1-year period (see Chapter 10 for more details).
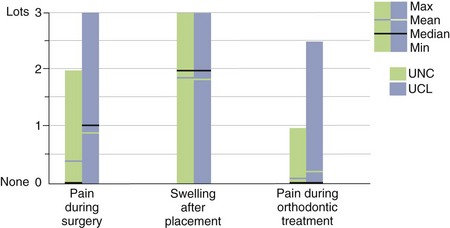
FIGURE 18-53 Pain and swelling as reported by patients treated with miniplates as temporary skeletal anchors at North Carolina (UNC) and Louvain (UCL). (Redrawn from Cornelis MA, et al. Am J Orthod Dentofac Orthop 133:18-24, 2008.)
The reaction of the doctors to miniplates was also favorable. On a 1 to 4 scale from very easy to very difficult, the surgeons who placed the skeletal anchorage rated the procedure as 1.7. The average time to place a single miniplate with two or three screws was 15 minutes. The orthodontists involved in these cases initially anticipated them to be somewhat or very difficult. However, with use of miniplates, the same cases were then considered to be very to moderately easy, and the orthodontists judged the complexity of using skeletal anchorage to be very to moderately easy over all time points (Figure 18-54). At the 1-year time point, all of the orthodontists said they would use skeletal anchorage again, and their average degree of satisfaction was 3.8 on a 1 to 4 point scale (3: moderately satisfied, 4: very satisfied).
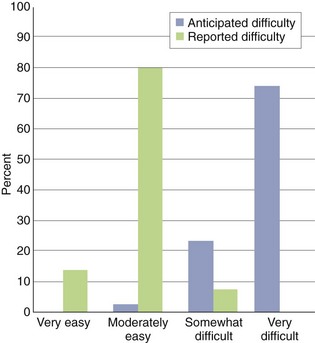
FIGURE 18-54 Orthodontists’ expectations at UNC of difficulty of treating patients for whom miniplates as anchors were planned, and the actual difficulty they reported. Although the orthodontists had expected that almost all (98%) of the cases would be somewhat difficult or very difficult, they rated almost all the actual treatment as very easy (15%) or moderately easy (80%), and none as very difficult. (Redrawn from Cornelis MA, et al. Am J Orthod Dentofac Orthop 133:18-24, 2008.)
In short, from the patients’ perspective, temporary skeletal anchorage was quite well tolerated. The surgeons found that placing it was quick and relatively easy, and the orthodontists found that its use greatly reduced the difficulty in treating the patients. Despite this, problems do occur. These problems primarily are loosening and premature removal of the screw or miniplate and erythema or irritation around the screw head or tube from the miniplate that extends into the mouth. Both of these problems also occur with alveolar bone screws. With greater clinical experience, better control of these problems should be achieved.
Finishing and Retention
Orthodontic finishing does not differ significantly in adults from the finishing procedures for younger patients, except that positioners are rarely if ever indicated as finishing devices for older patients and definitely should not be used in those with moderate to severe periodontal bone loss. These patients should be brought to their final orthodontic relationship with archwires and then stabilized with immediately placed retainers before eventual detailing of occlusal relationships by equilibration.
Part of the purpose of a traditional orthodontic retainer is to allow each tooth to move during function, independently of its neighbors, to produce a restoration of the normal periodontal architecture. This clearly does not apply to patients who have had a significant degree of periodontal bone loss and who have mobile teeth. In these patients, splinting of the teeth is necessary both short- and long-term. A clear “suck-down” retainer often is the best choice immediately upon removing the orthodontic appliance, but in adults with bone loss, undercuts must be waxed out on the casts before the retainer is formed, otherwise it will be difficult to impossible to insert and remove the retainer. Other short-term possibilities are an occlusal splint that provides positive indexing of the teeth and extends buccally and lingually to maintain tooth position or a wraparound retainer as illustrated in Chapter 17. Long-term splinting usually involves cast restorations.
One major difference in retention is in adults who have had intrusion of maxillary posterior teeth to close an anterior open bite. The long-term stability of this treatment has not yet been well studied, but it is clear that some rebound after intrusion is likely. It is important to tie the posterior segments to the skeletal anchor during the orthodontic treatment that follows intrusion, to consider leaving attachments on the posterior teeth when the rest of the brackets and bands are removed so that these teeth can remain tied to the skeletal anchor during the first year of retention, and to use a retainer with posterior bite blocks (see Figure 17-7) after the skeletal anchors are removed.
References
1. Grubb, JE, Greco, PM, English, JD, et al. Radiographic and periodontal requirements of the American Board of Orthodontics: a modification in the case display requirements for adult and periodontally involved adolescent and preadolescent patients. Am J Orthod Dentofac Orthop. 2008;134:3–4.
2. Kravitz, ND, Kusnoto, B, BeGole, E, et al. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofac Orthop. 2009;135:27–35.
3. Fritz, U, Diedrich, P, Wiechmann, D. Lingual technique—patients’ characteristics, motivation and acceptance. Interpretation of a retrospective survey. J Orofac Orthop. 2002;63:227–233.
4. Esteves, T, Ramos, AL, Pereira, CM, et al. Orthodontic root resorption of endodontically treated teeth. J Endodont. 2007;33:119–122.
5. Thilander, B. Infrabony pockets and reduced alveolar bone height in relation to orthodontic therapy. Semin Orthod. 1996;2:55–61.
6. Ogihara, S, Wang, HL. Periodontal regeneration with or without limited orthodontics for the treatment of 2- or 3-wall infrabony defects. J Periodontol. 2010;81:1734–1742.
7. Ziskind, D, Schmidt, A, Hirschfeld, Z. Forced eruption technique: Rationale and technique. J Pros Dent. 1998;79:246–248.
8. Sheridan, JJ. Air Rotor Stripping (ARS) Manual. New Orleans: Raintree Essix; 2005.
9. Grauer D, Heymann GC. Clinical management of tooth-size discrepancies. J Esthetic Restorative Dent, in press.
10. Heymann GC, Grauer D. Contemporary approach to orthodontic retention. J Esthetic Restorative Dent, in press.
11. Phillips, C, Broder, HL, Bennett, ME. Dentofacial disharmony: motivations for seeking treatment. Int J Adult Orthod Orthognath Surg. 1997;12:7–15.
12. Dahlström, L, Carlsson, GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand. 2010;68:80–85.
13. Mohlin, B, Axelsson, S, Paulin, G, et al. TMD in relation to malocclusion and orthodontic treatment. Angle Orthod. 2007;77:542–548.
14. Macfarlane, TV, Kenealy, P, Kingdon, HA, et al. Twenty-year cohort study of health gain from orthodontic treatment: temporomandibular disorders. Am J Orthod Dentofac Orthop. 2009;135:692. [e1-8; discussion 692-693].
15. Okeson, JP. Management of Temporomandibular Disorders and Occlusion, 6th ed. St. Louis: Mosby-Elsevier; 2008.
16. Rugh, JD, Solberg, WK. Oral health status in the United States: temporomandibular disorders. J Dent Educ. 1985;49:399–405.
17. Brown, LJ, Brunelle, JA, Kingman, A. Periodontal status in the United States, 1988-91: Prevalence, extent, and demographic variation. J Dent Res. 1996;75:672–683.
18. Türkkahraman, H, Sayin, MO, Bozkurt, FY, et al. Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthod. 2005;75:231–236.
19. Oh, TJ, Eber, R, Wang, HL. Periodontal diseases in the child and adolescent. J Clin Periodontol. 2002;29:400–410.
20. Grauer, D, Proffit, WR. Accuracy in tooth positioning with fully customized lingual orthodontic appliances. Am J Orthod Dentofac Orthop. 2011;140:433–443.
21. Damon, D. Treatment of the face with biocompatible orthodontics. In Graber TM, Vanarsdall RL, Vig KWL, eds.: Orthodontic Principles and Techniques, 4th ed, St Louis: Elsevier/Mosby, 2005.
22. Lin, J. Creative orthodontics blending the Damon system and TADs to manage difficult malocclusions. Taipei: Yong Chieh Co.; 2007.
23. Melsen, B. Intrusion of incisors in adult patients with marginal bone loss. Am J Orthod Dentofac Orthop. 1989;96:232–241.
24. Bellamy, LJ, Kokich, VG, Weissman, JA. Using orthodontic intrusion of abraded incisors to facilitate restoration: the technique’s effects on alveolar bone level and root length. J Am Dent Assoc. 2008;139:725–733.
25. McCall, G. The efficacy of temporary skeletal anchorage versus maxillary osteotomy in the treatment of anterior open bite. MS thesis, Chapel Hill: Univ of North Carolina; 2012.
26. Cornelis, MA, Scheffler, NR, Nyssen-Behets, C, et al. Patients’ and orthodontists’ perceptions of miniplates used for temporary skeletal anchorage: a prospective study. Am J Orthod Dentofac Orthop. 2008;133:18–24.