Treatment of Skeletal Problems in Children and Preadolescents
PRINCIPLES IN TIMING OF GROWTH MODIFICATION
1 Timing in Relation to the Amount of Growth Remaining
TREATMENT OF TRANSVERSE MAXILLARY CONSTRICTION
TREATMENT OF CLASS III PROBLEMS
TREATMENT OF CLASS II PROBLEMS
Whenever a jaw discrepancy exists, the ideal solution is to correct it by modifying the child’s facial growth, so that the skeletal problem is corrected by more or less growth of one jaw than the other (Figure 13-1). Unfortunately, such an ideal solution is not always possible, but growth modification for skeletal problems can be successful. Treatment planning for skeletal problems and what has been learned about the optimum timing of treatment have been discussed extensively in Chapter 7. This chapter briefly reviews the issues in treatment timing that were presented previously but focuses on clinical treatment aimed at growth modification. Usually this is accomplished by applying forces directly to the teeth and secondarily and indirectly to the skeletal structures, instead of applying direct pressure to the bones. Tooth movement, in addition to any changes in skeletal relationships, is unavoidable. It is possible now to apply force directly against the bone by using temporary implants, miniplates, or bone screws (see Chapter 10). This approach is likely to be used more and more in the future because the dental changes that accompany growth modification often (but not always) are undesirable. Excessive tooth movement, whether it results from a weakness in the treatment plan, poor biomechanical control, or poor compliance, can cause growth modification to be incomplete and unsuccessful.
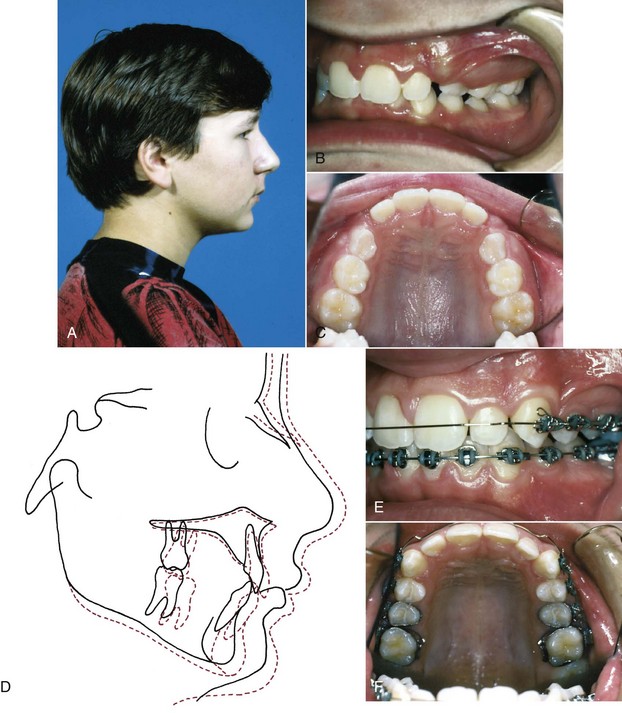
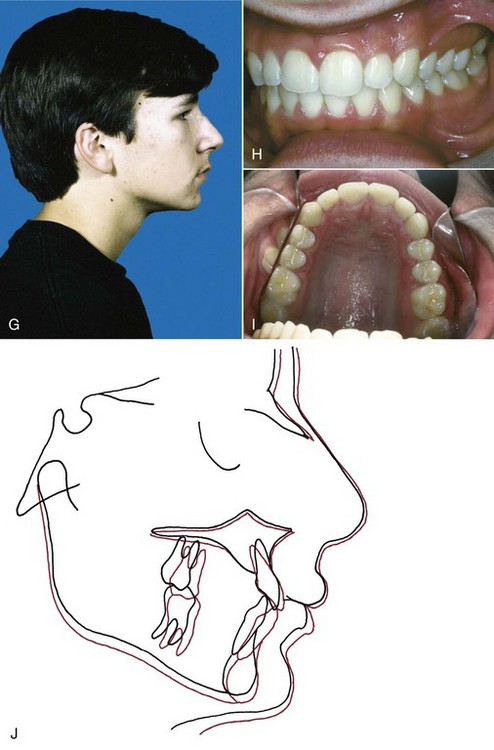
FIGURE 13-1 A to C, At age 11-10, this boy sought treatment because of trauma to his protruding front teeth and the crowding that was developing in the upper arch, where there was no room for the permanent canines. Skeletal Class II malocclusion, due primarily to mandibular deficiency, was apparent. Because of the damaged maxillary central incisors (one of which had a root fracture), the treatment plan called for cervical headgear to promote differential mandibular growth and create space in the maxillary arch. D, Fifteen months of headgear during the adolescent growth spurt produced significant improvement in the jaw relationship with differential forward growth of the mandible and created nearly enough space to bring the maxillary canines into the arch. E and F, A partial fixed appliance was placed, staying off the traumatized maxillary incisors until the very end of treatment, and light Class II elastics off a stabilized lower arch were used. G to I, The 15-month second stage of treatment produced excellent dental relationships, but note in the cephalometric superimposition (J) that minimal further anteroposterior growth occurred. This illustrates the importance of starting growth modification treatment in the mixed dentition for children whose skeletal maturity is ahead of their dental age.
The material in this chapter is organized in the context of the child’s major skeletal problem. In some cases that provides a precise description: the upper or lower jaw is clearly at fault because of its position and size and the malocclusion is almost totally due to the jaw discrepancy. More frequently, there also are dental components to the problem, with displacement of the teeth relative to their supporting bone in any or all of the planes of space and/or crowding/spacing within the dental arches. In such cases, the therapy must be based on the solutions to that specific patient’s set of problems. In particular, dental changes that would be unwanted side effects in some patients can be quite helpful in others. For this reason, the secondary (dental), as well as the primary (skeletal), effects of the various appliances are reviewed in detail in this chapter.
Principles in Timing of Growth Modification
Three important principles must be kept in mind when growth modification is considered for a preadolescent or adolescent child: (1) if you start growth modification too late, it doesn’t work—but if you start too soon, it takes too long, (2) growth occurs on a different timetable for the three planes of space, and (3) children’s compliance with treatment is affected by both their stage of maturation and the difficulty of doing what the doctor wants.
Timing in Relation to the Amount of Growth Remaining
Whatever the type of appliance that is used or the kind of growth effect that is desired, if growth is to be modified, the patient has to be growing. Growth modification must be done before the adolescent growth spurt ends or the effects are minimal. In theory, it could be done at any point up to that time.
Because of the rapid growth exhibited by children during the primary dentition years, it would seem that treatment of jaw discrepancies by growth modification should be successful at a very early age. The rationale for very early treatment at ages 4 to 6 is that because of the rapid rate of growth and the smaller and more plastic skeletal components, significant amounts of skeletal discrepancy could be overcome in a short time. This has been tested and does occur. The further rationale is that once discrepancies in jaw relationships are corrected, proper function will cause harmonious growth thereafter without further treatment.
If this were the case, very early treatment in the primary dentition would be indicated for many skeletal discrepancies. Unfortunately, although most anteroposterior and vertical jaw discrepancies can be corrected during the primary dentition years, relapse occurs because of continued growth in the original disproportionate pattern. If children are treated very early, they usually need further treatment during the mixed dentition and again in the early permanent dentition to maintain the correction. For all practical purposes, early orthodontic treatment for skeletal problems now is restricted to the mixed dentition years, with a second phase of treatment required during adolescence.
The opposite point of view would be that since treatment in the permanent dentition will be required anyway, there is no point in starting treatment until then. Delaying treatment that long has two potential problems: (1) by the time the canines, premolars, and second molars erupt, there may not be enough growth remaining for effective modification, especially in girls, and (2) some children who need it would be denied the psychosocial benefits of treatment during an important period of development.
It now is clear that a child with a jaw discrepancy can benefit from treatment during the preadolescent years if impaired esthetics and the resultant social problems are substantial. Another indication for treatment is a dental and skeletal profile highly susceptible to trauma like the increased overjet and protrusive incisors that often accompany Class II relationships (Figure 13-2). The data are clear that these individuals encounter more dental trauma.1 The type and extent of trauma is highly variable, and it has been difficult to document prevention of injuries with early treatment to reduce overjet because it is often accomplished following or concurrent with the period of most injury prevalence. Nonetheless, it is probably prudent to consider reducing overjet for the most accident-prone children. For each patient, the benefits of early treatment must be considered against the risk and cost of prolonging the total treatment period.
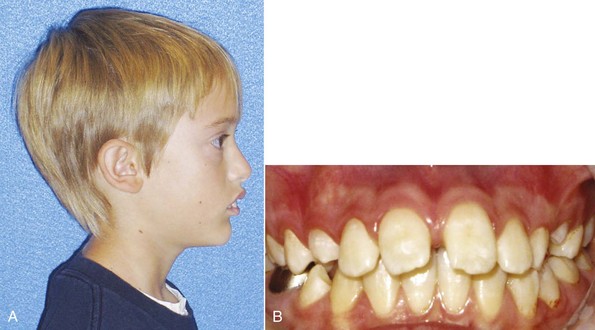
FIGURE 13-2 A, This patient has a convex, Class II profile with teeth susceptible to trauma due to the protrusion and overjet (B). Note that there are already enamel fractures present from minor trauma. Early treatment to decrease the chance of further trauma may be a consideration for this patient.
Different Timing for Different Planes of Space
The timing of maturation and the potential to effect a change in the different facial planes of space is not uniform. Maxillary growth in the transverse plane of space, the first to cease growing, stops when the first bridging of the midpalatal suture begins, not at final complete fusion. This usually means that by early adolescence palatal width increases would normally end and to mechanically alter this later with appliance therapy would require heavier forces. Transverse maxillary expansion therefore is more physiologic if done prior to adolescence.
Anteroposterior facial growth is most obvious in Class II and III malocclusions as the maxilla and mandible both move forward. Most accounts show these changes continuing until late adolescence, usually the mid-teen years and in some males until the late teens. This means that both treatment changes and failures to control growth can extend into the mid- to late-teen years and beyond. The urgency for early (preadolescent) treatment therefore is not clear. Small changes near the end of the growth period are not useful in a therapeutic way, but they can ruin retention of completed treatment.
Vertical facial growth is the last to stop. Interestingly, this growth has been detected in both males and females into the third decade. Vertical growth control is exceptionally difficult due to the extraordinary length of the growth period (see Chapters 3 and 4). So different timing for different problems is important. Palatal expansion is seemingly more urgent in earlier years, anteroposterior growth modification is more a midgrowth activity, and vertical control requires a later approach if it can be accomplished.
How one evaluates the growth stages and timing appears to make a difference, and different methods have advocates and detractors, based on the assessment approach. The cervical vertebral maturation staging (CVMS) method related to mandibular growth changes that is described in Chapter 3 may yield different results than timing based on hand–wrist radiographic estimation of skeletal maturation. In fact, differences of opinion exist on the appropriateness of each technique and even on how to apply the CVMS method. It may be that the most reliable, valid, and critical use of the CVMS method is differentiating the premandibular from postmandibular growth peak phases. Given the reduced radiation (because the images are available as part of the cephalometric radiograph), simplicity in learning, and excellent accuracy of the CVMS method among nonradiologist growth assessors like dentists and orthodontists, this method has a strong appeal and is certain to evolve.
Timing in Relation to Patient Compliance
Patient compliance is affected by both the patient’s relative maturity and the burden of treatment from the patient’s perspective. Timing of treatment interventions must be viewed relative to their effectiveness and the practical weighing of likely patient tolerance and compliance. This evaluation is not one of whether a change can be made, but whether the change is worth it in terms of time, financial and behavioral impact, and alternative treatment approaches such as surgery.
In the discussion of treatment techniques that follows, we will review the evidence that supports the timing that is advocated for different methods, along with the discussion of management of the treatment procedures.
Treatment of Transverse Maxillary Constriction
Skeletal maxillary constriction is distinguished by a narrow palatal vault (see Figure 6-71). It can be corrected by opening the midpalatal suture, which widens the roof of the mouth and the floor of the nose. This transverse expansion corrects the posterior crossbite that almost always is present (in fact, a narrow maxilla accompanied by a narrow mandible and normal occlusion should not be considered a problem just because the jaw widths are below the population mean). The expansion sometimes moves the maxilla forward a little (but is about as likely to lead to backward movement),2 increases space in the arch,3 and repositions underlying permanent tooth buds as they move along with the bone in which they are embedded. Palatal expansion can be done at any time prior to the end of the adolescent growth spurt. The major reasons for doing it sooner are to eliminate mandibular shifts on closure, provide more space for the erupting maxillary teeth, lessen dental arch distortion and potential tooth abrasion from interferences of anterior teeth, and reduce the possibility of mandibular skeletal asymmetry.4 The procedure is easiest when the midpalatal suture is not fused or has only minor initial bridging, so that extensive microfracturing is not needed to separate the palatal halves (i.e., when the expansion is done before adolescence).
In preadolescent children, three methods can be used for palatal expansion: (1) a split removable plate with a jackscrew or heavy midline spring, (2) a lingual arch, often of the W-arch or quad-helix design, or (3) a fixed palatal expander with a jackscrew, which can be either attached to bands or incorporated into a bonded appliance. Removable plates and lingual arches produce slow expansion. The fixed expander can be activated for either rapid (0.5 mm or more per day), semirapid (0.25 mm/day), or slow (1 mm/week) expansion. For each of the possible methods, appropriate questions are: Does it achieve the expansion? Does it have iatrogenic side effects? Is the expansion stable?
Palatal Expansion in the Primary and Early Mixed Dentition
Because less force is needed to open the suture in younger children, it is relatively easy to obtain palatal expansion. In the early mixed dentition, all three types of expansion appliances produce both skeletal and dental changes.5 Despite that, the three approaches are not equally sensible to use.
With a removable appliance, the rate of expansion must be quite slow, and the force employed during the process must be low because faster expansion produces higher forces that create problems with retention of the appliance. Multiple clasps that are well adjusted are mandatory. Because of the instability of the teeth during the expansion process, failure to wear the appliance even for 1 day requires adjustment of the jackscrew, usually by the practitioner, to constrict the appliance until it again fits and expansion can be resumed. Compliance in activation and wear time are always issues with these appliances. Successful expansion with a removable appliance can take so much time that it is not cost-effective.
Lingual arches of the W-arch and quad-helix designs (see Chapter 12) have been demonstrated to open the midpalatal suture in young patients (Figure 13-3). These appliances generally deliver a few hundred grams of force and provide slow expansion. They are relatively clean and reasonably effective, producing a mix of skeletal and dental change that approximates one-third skeletal and two-thirds dental change.2

FIGURE 13-3 Prior to adolescence, the midpalatal suture can be opened during maxillary expansion using a number of methods. This occlusal radiograph taken during the primary dentition years illustrates sutural opening in response to the W-arch appliance.
Fixed jackscrew appliances attached to bands or bonded splints also can be used in the early treatment of maxillary constriction but must be managed carefully. Banding permanent molars and primary second molars is relatively simple, but banding primary first molars can be challenging. Using a bonded appliance in the mixed dentition is relatively straightforward but can be difficult to remove if conventional bonding techniques are used. This appliance can deliver a variety of forces.
In young children, in comparison with an expansion lingual arch, a fixed jackscrew appliance has two major disadvantages. First, it is more bulky and more difficult to place and remove. The patient inevitably has problems cleaning it, which lead to soft tissue irritation, and either the patient or parent must activate the appliance. Second, an appliance of this type can be activated rapidly, which in young children is a disadvantage, not an advantage. Rapid expansion should not be done in a young child. There is a risk of distortion of facial structures with rapid expansion (see Figure 7-8), and there is no evidence that rapid movement and high forces produce better or more stable expansion.
Many functional appliances for Class II treatment (discussed below) incorporate some components to expand the maxillary arch, either intrinsic force-generating mechanisms like springs and jackscrews or buccal shields that reduce cheek pressure against the dentition. When arch expansion occurs during functional appliance treatment, it is possible that some opening of the midpalatal suture contributes to it, but the precise mix of skeletal and dental change is not well-documented.
On balance, slow expansion with an active lingual arch is the preferred approach to maxillary constriction in young children in the primary and early mixed dentitions. A fixed jackscrew appliance is an acceptable alternative if activated carefully and slowly. It appears that anteroposterior dental changes in terms of overjet are not consistently correlated with maxillary expansion.6
Palatal Expansion in the Late Mixed Dentition
With increasing age, the midpalatal suture becomes more and more tightly interdigitated; however, in most individuals, it remains possible to obtain significant increments in maxillary width up to the end of the adolescent growth spurt (age 15 to 18). Expansion in adolescents is discussed in some detail in Chapter 14.
Even in the late mixed dentition, sutural expansion often requires placing a relatively heavy force directed across the suture to move the halves of the maxilla apart. A fixed jackscrew appliance (either banded or bonded) is necessary (Figure 13-4). As many teeth as possible should be included in the anchorage unit. In the late mixed dentition, root resorption of primary molars may have reached the point that these teeth offer little resistance, and it may be wise to wait for eruption of the first premolars before beginning expansion.


FIGURE 13-4 A, This banded palatal expander, attached only to the first molars in a patient in the mid mixed dentition, has been stabilized after expansion using cold-cure acrylic so it will not relapse. This will remain in place for 3 months. B, For a bonded palatal expander, during fabrication the plastic base is extended over the occlusal, facial, and lingual surfaces of the posterior teeth. Generally, a composite bonding agent is used to retain the appliance, with only the facial and lingual surfaces of the posterior teeth etched. Etching the occlusal surface is not recommended—bonding there is unnecessary for retention and can greatly complicate appliance removal.
Although some studies have reported increases in vertical facial height with maxillary expansion, long-term evidence indicates this change is transitory.7 A bonded appliance that covers the occlusal surface of the posterior teeth may be a better choice for a preadolescent child with a long-face tendency because it produces less mandibular rotation than a banded appliance, but for younger patients this is not totally clear.8 Perhaps the best summary is that the older the patient when maxillary expansion is done, the less likely it is that vertical changes will be recovered by subsequent growth.
Rapid or Slow Expansion?
In the late mixed dentition, either rapid or slow expansion is clinically acceptable. As we have reviewed in some detail in Chapter 7, it now appears that slower activation of the expansion appliance (at the rate of about 1 mm/week) provides approximately the same ultimate result over a 10- to 12-week period as rapid expansion, with less trauma to the teeth and bones (see Figure 7-9).
Rapid expansion typically is done with two turns daily of the jackscrew (0.5 mm activation per day). This creates 10 to 20 pounds of pressure across the suture—enough to create microfractures of interdigitating bone spicules. When a screw is the activating device, the force is transmitted immediately to the teeth and then to the suture. Sometimes, a large coil spring is incorporated along with the screw, which modulates the amount of force, depending on the length and stiffness of the spring (Figure 13-5). The suture opens wider and faster anteriorly because closure begins in the posterior area of the midpalatal suture and the forces are transmitted to adjacent posterior structures.9 With rapid or semirapid expansion (one turn per day), a diastema usually appears between the central incisors as the bones separate in this area (Figure 13-6). When expansion has been completed, a 3-month period of retention with the appliance in place is recommended. After the 3-month retention period, the fixed appliance can be removed, but a removable retainer that covers the palate is often needed as further insurance against early relapse (Figure 13-7). A relatively heavy, expanded maxillary archwire provides retention and support if further treatment is being accomplished immediately. If not, a transpalatal lingual arch or a large expanded auxiliary wire (36 or 40 mil) in the headgear tubes will help maintain expansion while using a more flexible wire in the brackets.

FIGURE 13-5 This expander uses a coil spring to provide the force as the stop on the threaded connector is turned to compress the spring. It can be calibrated to determine and monitor the force that is active. This prevents delivery of either low or excessive forces during the expansion.

FIGURE 13-6 Usually spaces develop between the central incisors during rapid maxillary expansion. A, When the appliance is placed and treatment begins, there is only a tiny diastema. B, After 1 week of expansion, the teeth have moved laterally with the skeletal structures. C, After retention, a combination of skeletal relapse and pull of the gingival fibers has brought the incisors together and closed the diastema. Note that the expansion was continued until the maxillary lingual cusps occlude with the lingual inclines of the buccal cusps of the mandibular molars.

FIGURE 13-7 Following palatal expansion, even after 3 months of retention with the passive expander, an acrylic retainer that covers the palate is needed to control relapse and stabilize the skeletal components.
The theory behind rapid activation was that force on the teeth would be transmitted to the bone, and the two halves of the maxilla would separate before significant tooth movement could occur. In other words, rapid activation was conceived as a way to maximize skeletal change and minimize dental change. It was not realized initially that during the time it takes for bone to fill in the space that was created between the left and right halves of the maxilla, skeletal relapse begins to occur almost immediately as the maxillary halves moved toward the midline, even though the teeth were held in position. The central diastema closes from a combination of skeletal relapse and tooth movement created by stretched gingival fibers, not from tooth movement alone. The net effect is approximately equal skeletal and dental expansion.
Slow activation of the expansion appliance at the rate of 1 mm/week, which produces about 2 pounds of pressure in a mixed dentition child, opens the suture at a rate that is close to the maximum speed of bone formation. The suture is not obviously pulled apart on radiographs, and no midline diastema appears, but both skeletal and dental changes occur. After 10 to 12 weeks, approximately the same amounts of skeletal and dental expansion are present that were seen at the same time with rapid expansion. When bonded slow and rapid palatal expanders in early adolescents were compared, the major difference was greater expansion across the canines in the rapid expansion group. This translated into a predicted greater arch perimeter change but similar opening of the suture posteriorly.10 So by using slow palatal expansion (one turn every other day) in a typical fixed expansion appliance or by using a spring to produce about 2 pounds of force, effective expansion with minimal disruption of the suture can be achieved for a late mixed dentition child.
This really brings us to the question of early slower expansion or later rapid expansion as choices. Two studies that demonstrate age-appropriate approaches are instructive. One, with patients who averaged 8 years 10 months at the start, used a bonded acrylic splint and a semirapid approach of 0.25 mm expansion per day.11 The other, with patients averaging 12 years 2 months at the start, used a Haas-type rapid palatal expansion (RPE) turned twice for 0.5 mm expansion per day of treatment.12 Both followed the expansion with retention and ultimately the patients had full treatment without further purposeful expansion. At the long-term evaluation points (19 years 9 months and 20 years 5 months, respectively), the expansion across the molars and canines and the increase in arch perimeter were quite similar and seem to indicate equivalent long-term results.
Clinical Management of Palatal Expansion Devices
Most traditional palate expansion devices use bands for retention on permanent first molars and first premolars if possible. During the late mixed dentition years, the first premolars often are not fully erupted and are difficult to band. If the primary second molars are firm, they can be banded along with the permanent first molars. Alternatively, only the permanent first molars can be banded. With this approach, the appliance is generally extended anteriorly, contacting the other posterior primary and erupting permanent teeth near their gingival margins. This will provide similar posterior expansion, but less anterior changes.13 Expanders with hinged designs can differentially expand the anterior or posterior portions of the arch. For some patients, this may be an advantage (Figure 13-8). After crossbite correction is completed, band removal can be difficult because the teeth are mobile and sensitive. In those cases, sectioning the bands is appropriate.

FIGURE 13-8 Many configurations of maxillary expanders are available. This one has a hinge in the posterior and the expansion screw in the anterior. This design holds the posterior teeth and their transverse dimension stable and expands only the anterior part of the arch.
An alternative approach is to use a bonded palatal expander (see Figure 13-4, B). Because there is no band fitting, the appliance is easier to place for both the patient and doctor, and during treatment it is manipulated like any other RPE appliance. Removal of this appliance is accomplished with a band remover engaged under a facial or lingual margin to flex the appliance and break the bond. In addition, the appliance usually needs to be sectioned or portions of the occlusal plastic removed for a direct purchase on the teeth so the band remover can effectively lift and separate the plastic from the teeth. Complete removal of the bonding agent (typically a filled resin that will adhere to etched tooth surfaces and to the appliance) can be laborious, so using only an adequate amount is crucial, but inadequate resin will lead to excessive leakage onto the nonbonded surfaces, which can result in decalcification or appliance loss. For these reasons, some clinicians use glass ionomer cement for retention. The strength of the material usually is adequate, and the short-term fluoride release may be beneficial.
Treatment of Class III Problems
Anteroposterior and Vertical Maxillary Deficiency
Both anteroposterior and vertical maxillary deficiency can contribute to Class III malocclusion. If the maxilla is small or positioned posteriorly, the effect is direct; if it does not grow vertically, there is an indirect effect on the mandible, which then rotates upward and forward as it grows, producing an appearance of mandibular prognathism that may be due more to the position of the mandible than its size.
In order of their effectiveness, there are three possible approaches to maxillary deficiency: Frankel’s FR-III functional appliance, reverse-pull headgear (facemask) to a maxillary splint or skeletal anchors, and Class III elastics to skeletal anchors.
FR-III Functional Appliance
The FR-III appliance (Figure 13-9) is made with the mandible positioned posteriorly and rotated open and with pads to stretch the upper lip forward. In theory, the lip pads stretch the periosteum in a way that stimulates forward growth of the maxilla. In a review of cases selected from Frankel’s archives, Levin et al14 reported that in patients with Class III skeletal and dental relationships and good compliance who wore the FR-III appliance full time for an average of 2.5 years and then part time in retention for 3 years, there was significantly enhanced change over controls in maxillary size and position and improved mandibular position combined with more lingual lower incisor bodily position so that the patients had more overjet. This held up at the long-term follow-up over 6 years after active treatment.

FIGURE 13-9 The FR-III appliance stretches the soft tissue at the base of the upper lip, attempting to stimulate forward growth of the maxilla by stretching the maxillary periosteum while maintaining the mandible in its most retruded position. The vertical opening is used to enhance downward and forward eruption of maxillary posterior teeth.
The available data from most other studies, however, indicate little true forward movement of the upper jaw.15 Instead, most of the improvement is from dental changes. The appliance allows the maxillary molars to erupt and move mesially while holding the lower molars in place vertically and anteroposteriorly and tips the maxillary anterior teeth facially and retracts the mandibular anterior teeth (Figure 13-10). Rotation of the occlusal plane as the upper molars erupt more than the lowers also contributes to a change from a Class III to a Class I molar relationship (Figure 13-11). In addition, if a functional appliance of any type rotates the chin down and back, the Class III relationship will improve because of the mandibular rotation, not an effect on the maxilla. In short, functional appliance treatment, even with the use of upper lip pads, has little or no effect on maxillary deficiency and, if considered, should be used only on extremely mild cases. If this appliance is used, there are long treatment and retention periods that require excellent compliance to maintain limited changes.
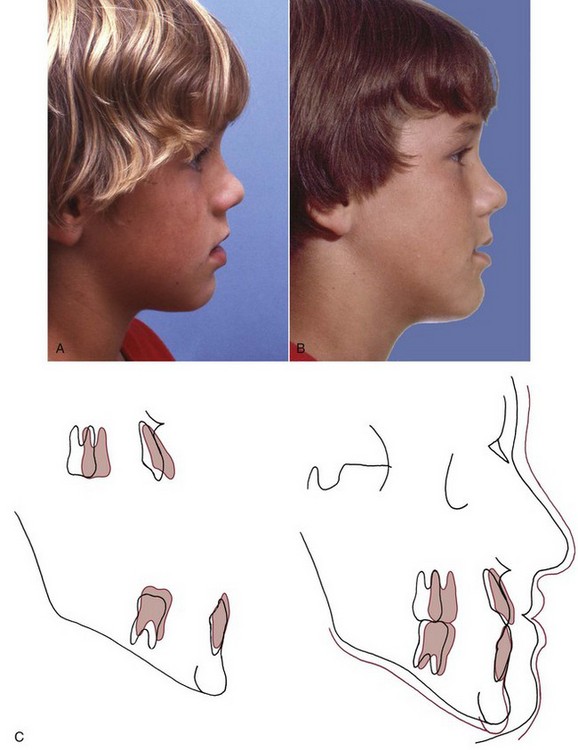
FIGURE 13-10 Response to a FR-III functional appliance. A, Pretreatment profile. B, Posttreatment profile. C, Cephalometric superimpositions. Note in the cranial base superimposition that the mandible rotated inferiorly and posteriorly to a less prominent position. The maxillary incisors moved facially while there was lower incisor eruption, but there was little if any differential forward growth of the maxilla. In essence, the treatment traded increased face height for decreased chin prominence.
Reverse-Pull Headgear (Facemask)
After Delaire’s demonstration that a facemask attached to a maxillary splint could move the maxilla forward by inducing growth at the maxillary sutures, but only if it was done at an early age, this approach to maxillary deficiency became popular in the late twentieth century (Figure 13-12). The age of the patient is a critical variable. It is easier and more effective to move the maxilla forward at younger ages. Although some recent reports indicate that anteroposterior changes can be produced up to the beginning of adolescence, the chance of true skeletal change appears to decline beyond age 8, and the chance of clinical success begins to decline at age 10 to 11.16
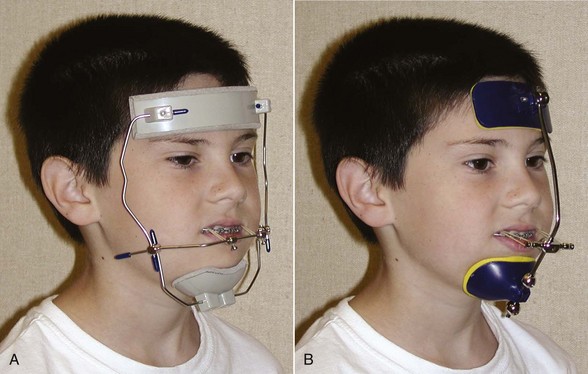
FIGURE 13-12 A, This Delaire-type facemask offers good stability when used for maxillary protraction. It is rather bulky and can cause problems with sleeping and wearing eyeglasses. With even modest facial asymmetry, it can appear to be ill-fitted on the face. Note the downward and forward direction of the pull of the elastics. B, This rail-style facemask provides more comfort during sleeping and is less difficult to adjust. It also can be adjusted to accommodate some vertical mandibular movement. Both types can lead to skin irritation caused by the plastic forehead and chin pads. These occasionally require relining with an adhesive-backed fabric lining for an ideal fit or to reduce soft tissue irritation. Clinical experience indicates that some children will prefer one type over the other, and changing to the other type of facemask can improve cooperation if the child complains.
When force is applied to the teeth for transmission to the sutures, tooth movement in addition to skeletal change is inevitable. Facemask treatment is most suited for children with minor-to-moderate skeletal problems, so that the teeth are within several millimeters of each other when they have the correct axial inclination. This type of treatment also is best used in children who have true maxillary problems, but some evidence indicates that the effects on mandibular growth during treatment go beyond simply changes caused by clockwise rotation of the mandible.17
Generally, it is better to defer maxillary protraction until the permanent first molars and incisors have erupted. The molars can be included in the anchorage unit and the inclination of the incisors can be controlled to affect the overjet. Many clinicians use protraction with a facemask following or simultaneously with palatal expansion, but a randomized clinical trial has shown that simultaneous palatal expansion makes no difference in the amount of anteroposterior skeletal change.18 If the maxilla is narrow, palatal expansion is quite compatible with maxillary protraction and the expansion device is an effective splint; there is no reason, however, to expand the maxilla just to improve the protraction. Whatever the method of attachment (Figure 13-13), the appliance must have hooks for attachment to the facemask that are located in the canine–primary molar area above the occlusal plane. This places the force vector nearer the purported center of resistance of the maxilla and limits maxillary rotation (Figure 13-14).

FIGURE 13-13 A maxillary removable splint is sometimes used to make the upper arch a single unit for maxillary protraction. A, The splint incorporates hooks in the canine-premolar region for attachment of elastics and should cover the anterior and posterior teeth and occlusal surfaces for best retention (B). Note that the hooks extend gingivally, so that the line of force comes closer to the center of resistance of the maxilla. Multiple clasps also aid in retention. If necessary, the splint can be bonded in place, but this causes hygiene problems and should be avoided if possible for long-term use. C and D, A banded expander or wire splint also can be used for delivery of protraction force. It consists of bands on primary and permanent molars or just permanent molars connected by a palatal wire for expansion and hooks on the facial for facemask attachments.
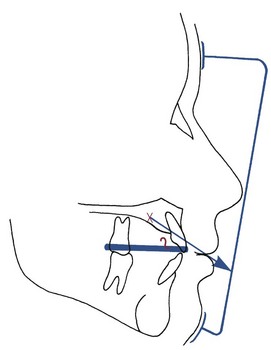
FIGURE 13-14 With the splint over the maxillary teeth and forward pull from the facemask, the hooks on the splint should be elevated. Even so, the line of force is likely to be below the center of resistance of the maxilla, so some downward rotation of the posterior maxilla and opening of the bite anteriorly can be anticipated.
For most young children, a facemask is as acceptable as conventional headgear. Contouring an adjustable facemask for a comfortable fit on the forehead is not difficult for most children. There are a variety of designs (see Figure 13-12).
Approximately 350 to 450 gm of force per side is applied for 12 to 14 hours per day. Most children with maxillary deficiency are deficient vertically, as well as anteroposteriorly, which means that a slight downward direction of elastic traction between the intraoral attachment and the facemask frame often is desirable, and some downward-backward mandibular rotation improves the jaw relationship. A downward pull would be contraindicated if lower face height was already large.
Backward displacement of the mandibular teeth and forward displacement of the maxillary teeth also typically occur in response to this type of treatment (Figure 13-15).19 As children come closer to adolescence, mandibular rotation and displacement of maxillary teeth—not forward movement of the maxilla—are the major components of the treatment result.
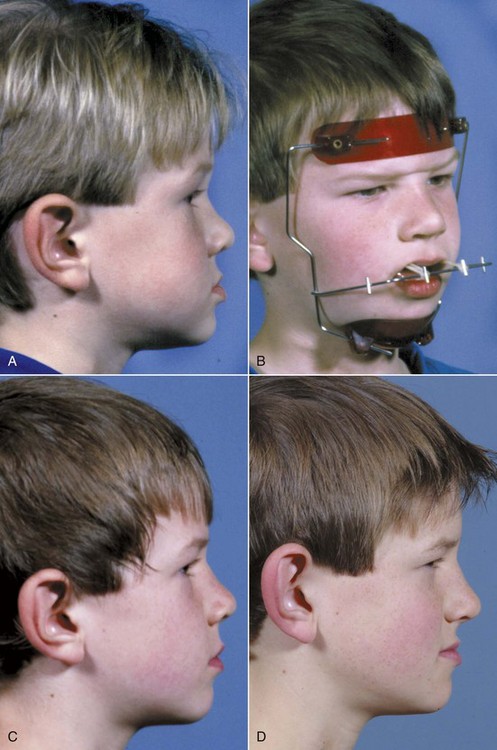
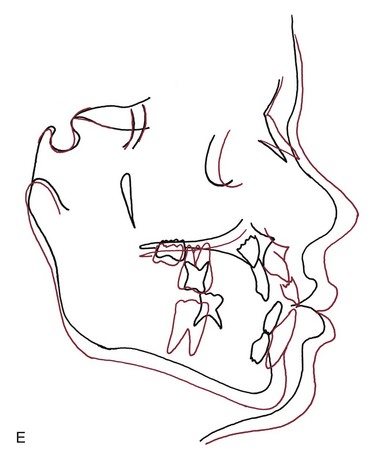
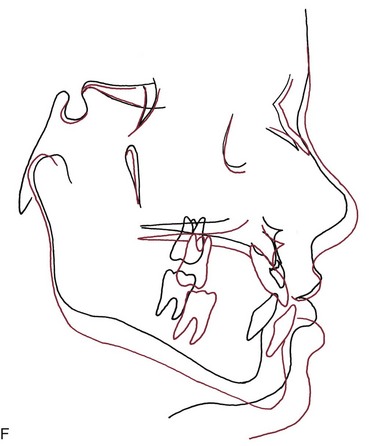
FIGURE 13-15 If forward traction is applied at an early age, it is possible to produce forward displacement of the jaw rather than just displacement of teeth. A, Age 5 years, 2 months prior to treatment. B, Age 5-2, wearing a Delaire-type facemask. C, Age 7-10, at the time facemask treatment was discontinued. Note the increased fullness of the midface. D, Age 11-3, at the beginning of phase 2 treatment. E, Cephalometric superimposition showing the changes during facemask treatment. F, Superimposition showing the changes from ages 8 to 11 following treatment. When facemask treatment is discontinued, there is usually a rebound of mandibular growth similar to what occurred for this patient. Whether surgery eventually will be required will be determined by mandibular growth during and after adolescence. (From Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby; 2003.)
Application of Skeletal Anchorage
Clearly, a major negative side effect of maxillary protraction is maxillary dental movement that detracts from the skeletal change. Before bone screws and miniplates became available, Shapiro and Kokich deliberately ankylosed primary canines so they could be used as “natural implants.”20 With traction against a maxillary arch stabilized by these teeth, they were able to demonstrate approximately 3 mm of maxillary protraction in 1 year, with minimal dental change. If a child with maxillary retrusion has spontaneous ankylosis of primary molars, a splint can be fabricated to take advantage of these teeth as implants and gain the same biomechanical advantage.
For more routine use in clinical practice, it appears that the effects of treatment to change the deficient maxillary position can be magnified in one of two ways. First, the facemask can be applied to miniplates at the base of the zygomatic arch21 or in the anterior maxilla.22 With anchors above the incisors, 400 gm of force per side, and use of the facemask for a minimum of 16 hours per day, Sar et al22 reported 0.45 mm per month of anterior maxillary movement (compared to 0.24 mm with conventional facemask) without rotation of the maxilla. For patients approaching adolescence (i.e., about age 11 and old enough for good retention of bone screws), this appears to be promising.
Alternatively, bone-supported miniplates can be placed bilaterally in the maxilla and the mandible, so that interarch force from Class III elastics is delivered to the jaws rather than the teeth (Figure 13-16).23 Three-dimensional (3-D) imaging of patients treated in this way has shown a variety of interesting responses (Figure 13-17) that include forward movement of the maxilla at a higher level than has been observed previously and displacement or remodeling in the temporomandibular (TM) fossae. In a sequence of 25 consecutive children treated in this way with full-time elastics delivering approximately 150 gm per side (about 5 ounces), the variety of changes seen in the 3-D images are summarized in Figure 13-18. More than 2 mm maxillary protraction was noted in 14 (56%) of the 25 patients.

FIGURE 13-16 A maxillary-deficient child wearing Class III elastics to miniplates at the base of the zygomatic arch and mesial to the mandibular canines. Note that the patient is wearing a biteplate to open the bite until the anterior crossbite is corrected, and that point of attachment for the lower left miniplate has been repositioned with a piece of 21 × 25 steel wire in the miniplate tube. Being able to move the point to which force is applied, of course, is one of the advantages of miniplates.
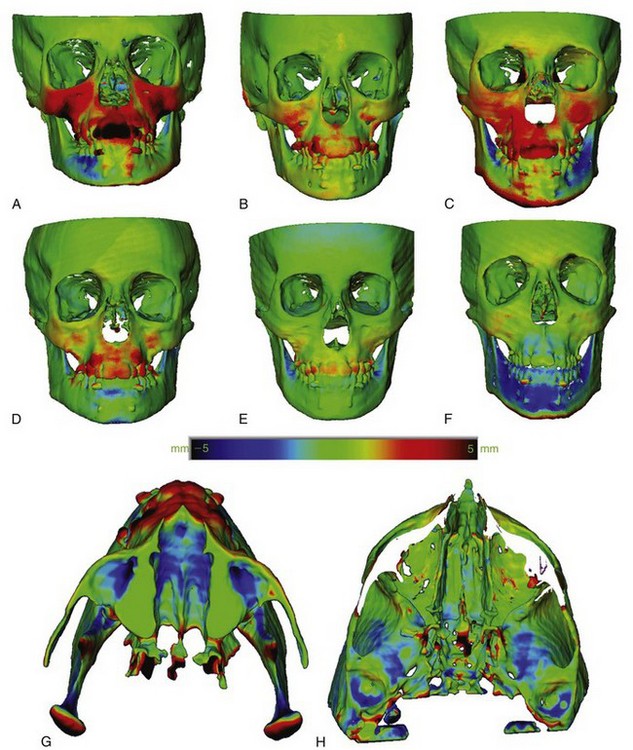
FIGURE 13-17 A to F, Frontal view of 3-D superimpositions for 6 patients, all approximately 11 years old, who were treated with Class III elastics to miniplates registered on the surface of the anterior cranial fossa. The amount of change is shown by the intensity of color in this color map display. The red color shows changes in the anteroposterior plane of space, so that red areas are moving toward you, and the darkest red corresponds to a 5 mm change; green shows areas of little or no change; blue areas are moving away from you, and the most intense blue is a 5 mm change. Note the variety of changes, from 4 to 5 mm forward movement of the maxilla extending up into the zygomatic arches to backward positioning of the mandible. G, View at the level of the condyles for patient seen in F in the frontal views, showing that the condyles have been displaced posteriorly relative to the cranial base about 3 mm (indicated by the intensity of the red color on the posterior aspect of the condyles). H, View from above at the level of the condylar fossae, showing 4 to 5 mm posterior displacement of their back walls (indicated by the intensity of the blue color). The posterior movement of the condyles and the changes in the fossae both would allow the backward movement of the mandible seen in F, but the extent to which this reflects displacement by growth versus remodeling of the fossae cannot be distinguished with an additional regional superimposition. (From Heymann G, et al. Am J Orthod Dentofac Orthop 137:274-284, 2010.)
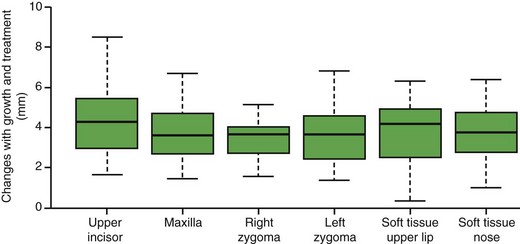
FIGURE 13-18 For a group of 25 consecutive patients treated with Class III elastics to miniplates for about 1 year starting at about 11 years of age (range 9 to 13 years), changes in position of maxillary hard and soft tissue areas shown as box plots, with the mean change (dark line in box), 75% of the sample (box dimension), and range (whiskers above/below the box). Note that all the points showed forward movement in all 25 patients but with a considerable range and mean changes of about 4 mm forward growth/displacement. (Redrawn from Nguyen T, Cevidanes L, Cornelis MA, et al. Am J Orthod Dentofac Orthop 140:790-798, 2011.)
This approach has two advantages: (1) it is clearly more effective than a facemask to a maxillary splint24 and also appears to produce more skeletal change than has been reported with facemasks to anterior miniplates and (2) wearing an extraoral appliance is not necessary and nearly full-time application of the force can be obtained. Compared to facemasks attached to a maxillary splint, it has the disadvantage of requiring surgical application and removal of the miniplates by a surgeon trained to do this, although this is not major surgery. Alveolar bone screws with Class III elastics would be simpler to place and remove than miniplates, but both the lower density of the bone in preadolescents and avoiding damage to unerupted permanent teeth pose substantial problems with their use (see Chapter 10). Miniplates attached to basal bone can be used at age 10-6 or 11. The minimum age for alveolar bone screws for this application appears to be approximately age 12, probably too late for an optimal skeletal effect.
Summary
There is no doubt that maxillary protraction at an early age usually produces clinical improvement in a Class III patient. Important concerns are the extent to which this will be maintained long-term and the chance that orthognathic surgery eventually will be necessary despite the early treatment. The answer to these issues, of course, requires recall 8 to 10 years after the initial treatment was completed. Three recent studies now show essentially the same thing: that 25% to 30% of their facemask patients ended up in anterior crossbite after adolescent growth and that the majority of these would require surgery for correction.25
There is no way to know at present whether the long-term outcomes would be better if facemasks or Class III elastics were attached to skeletal anchors, but when a Class III problem recurs, it is because of excessive mandibular growth during and following adolescence, not because of backward relapse of the maxilla. It seems unlikely that mandibular growth at adolescence would be affected by treatment some years previously with a facemask or bone-supported elastics. Nevertheless, it is reasonable to conclude that the more a child’s Class III problem is due to maxillary deficiency, the more likely it is that long-term success will be achieved with maxillary protraction, and the more the problem is mandibular prognathism, the more likely that the problem will recur with adolescent growth.
Mandibular Excess
Children who have Class III malocclusion because of excessive growth of the mandible are extremely difficult to treat. There are two possible treatment approaches at present, with a third on the horizon: Class III functional appliances, extraoral force to a chin cup, and (perhaps in the future) Class III elastics to skeletal anchors.
Functional Appliances in Treatment of Excessive Mandibular Growth
Functional appliances for patients with excessive mandibular growth make no pretense of restraining mandibular growth. They are designed to rotate the mandible down and back and to guide the eruption of the teeth so that the upper posterior teeth erupt down and forward while eruption of lower teeth is restrained. This rotates the occlusal plane in the direction that favors correction of a Class III molar relationship (see Figure 13-10). These appliances also tip the mandibular incisors lingually and the maxillary incisors facially, introducing an element of dental camouflage for the skeletal discrepancy. The only difference from a functional appliance for a maxillary deficiency patient is the absence of lip pads.
To produce the working bite for a Class III functional appliance, the steps in preparation of the wax, practice for the patient, and use of a guide to determine the correct vertical position are identical to the procedure for Class II patients (see later section in this chapter). However, the working bite itself is significantly different: the mandible is rotated open on its hinge axis but is not advanced. This type of bite is easier for the dentist to direct because light force can be placed on each side of the mandible to guide the mandible and retrude it.
How far the mandible is rotated open depends on the type of appliance and the need to interpose bite blocks and occlusal stops between the teeth to limit eruption. Less vertical opening would be needed for an appliance with lip pads to try to encourage forward movement of the maxilla than for one that encourages eruption and deliberately rotates the mandible significantly back or one that uses bite blocks to hold the mandible down beyond the patient’s postural position.
Chin-Cup Appliances: Restraint of Mandibular Growth?
In theory, extraoral force directed against the mandibular condyle would restrain growth at that location, but there is little or no evidence that this occurs in humans (see Chapter 7). What chin-cup therapy does accomplish is a change in the direction of mandibular growth, rotating the chin down and back, which makes it less prominent but increases anterior face height. The data seem to indicate a transitory restraint of growth that is likely to be overwhelmed by subsequent growth.26 In essence, the treatment becomes a trade-off between decreasing the anteroposterior prominence of the chin and increasing face height. In addition, lingual tipping of the lower incisors occurs as a result of the pressure of the appliance on the lower lip and dentition (Figure 13-19), which often is undesirable.

FIGURE 13-19 A typical response to chin-cup treatment. A, Pretreatment profile. B, Posttreatment profile. This treatment reduces mandibular protrusion primarily by increasing anterior face height, very similar to the effect of Class III functional appliances.
For chin-cup treatment, a hard plastic cup fitted to a cast of the patient’s chin or a soft cup made from an athletic helmet chinstrap can be used. The more the chin cup or strap migrates up toward the lower lip during appliance wear, the more lingual movement of the lower incisors will be produced, so soft cups produce more incisor uprighting than hard ones. The headcap that includes the spring mechanism can be the same one used for high-pull headgear. It is adjusted in the same manner as the headgear to direct a force of approximately 16 ounces per side through the head of the condyle or a somewhat lighter force below the condyle. Once it is accepted that mandibular rotation is the major treatment effect, lighter force oriented to produce greater rotation makes more sense.
From this perspective, it is apparent that more Asian than Caucasian children can benefit from chin-cup treatment because of their generally shorter face height and greater prevalence of lower incisor protrusion, not because of a difference in the treatment response. Unfortunately, the majority of Caucasian children with excessive mandibular growth have normal or excessive face height, so that only small amounts of mandibular rotation are possible without producing a long-face deformity. Many of these children ultimately need surgery, and the chin-cup treatment is essentially transient camouflage. For that reason, it has limited application.
Class III Elastics to Skeletal Anchors
The use of Class III elastics to skeletal anchors as an effective way of producing maxillary protraction has been discussed above—but as one might expect, this force system also affects the mandible23 and may eventually provide a way to restrain mandibular growth. In the recent study using 3-D superimposition on the cranial base to evaluate the outcome of this treatment, which provided the data for effects on the maxilla discussed above, posterior displacement of the mandible at the condyles and posterior ramus was observed frequently (Table 13-1). Note that despite the relative large mean changes at the condyles and posterior ramus, the mean change at the chin was essentially zero, and nearly half of the patients had some net forward movement of the chin.
TABLE 13-1
Mandibular Changes Relative to Anterior Cranial Fossa, Treatment with Class III Elastics to Skeletal Anchors*
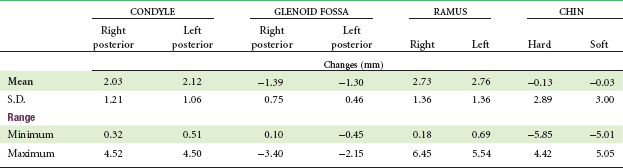
*25 consecutive patients, ages 9 to 13 years, cone-beam computed tomography (CBCT) three-dimensional (3-D) imaging.
From Nguyen T, Cevidanes L, Cornelis MA, et al. Am J Orthod Dentofac Orthop 140:790-798, 2011.
In 3-D superimpositions on the surface of the anterior cranial fossa, backward movement of the condyles and changes in the condylar fossa are seen in some patients, and this corresponds to backward movement of the mandible (see Figure 13-17, G and H).These changes, however, must be interpreted cautiously. Posterior displacement of the condyles could be related to remodeling of the condyles and/or the fossae, but it must be kept in mind that posterior displacement also could occur from downward-backward growth of the TM joint area, which would allow the condyles and chin to be displaced distally without remodeling. Downward growth of the TM joint area is occurring in this age group and is known to displace the fossa anteriorly or posteriorly (see Figure 4-9 and the discussion of condylar displacement during growth).
The result is that there are three major unanswered questions about Class III elastics to skeletal anchors as a treatment modality for excessive mandibular growth: (1) What determines whether the major effect is on the maxilla or mandible? (2) How would one arrange the treatment to maximize the effect on the mandible? and (3) What would the long-term effect be, particularly with regard to adolescent and postadolescent growth of the mandible? It seems prudent at present to limit this treatment method to children whose primary problem is maxillary deficiency.
Summary
Modifying true mandibular prognathism is a difficult task, regardless of the chosen method. This often leads to irrational choices by practitioners and parents in attempts to control crossbite and chin prominence as the child grows and to avoid surgical treatment when the child has matured. Although the theory of the Class III functional appliance is quite different from that of the chin cup, the treatment effects are quite similar, and the two approaches are approximately equally effective (or more accurately, equally ineffective). In the long-term, can mandibular growth be restrained with the use of skeletal anchors and Class III elastics? This is an intriguing possibility but not yet supported by data. The limited success of early intervention is a reality that must be recognized. For a child with severe prognathism, no treatment until orthognathic surgery can be done at the end of the growth period may be the best treatment
Treatment of Class II Problems
Possible Approaches to Treatment
In theory, functional appliances (activator, bionator, Frankel, and Twin-Block) (Figures 13-20, 13-21, and 13-22) stimulate and enhance mandibular growth, while extraoral force (headgear) retards maxillary growth—so functional appliances would seem to be an obvious choice for treatment of mandibular deficiency and headgear an equally obvious choice for maxillary excess. In reality, the distinctions between the two appliance systems and the indications for their use are not as clear-cut as the theory would imply.
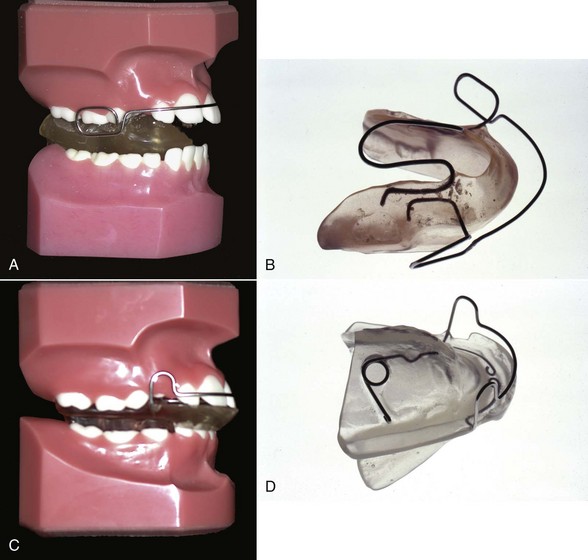
FIGURE 13-20 A, The bionator is tooth borne and induces mandibular advancement with contact of lingual flanges with the lingual mucosa. It usually has a buccal wire to maintain the lips off the teeth and can incorporate bite blocks between the posterior teeth and a tongue shield as this one does. B, The bionator also incorporates a major palatal connector to stabilize the posterior segments, but the appliance is limited in bulk and relatively easy for the patient to accommodate. C, The activator is also used to actively advance the mandible and can incorporate anterior and posterior bite blocks and a labial bow. D, The activator’s lingual shields usually extend deeper along the mandibular alveolus than other functional appliances, and sometimes the appliance incorporates a displacing spring so that the patient has to close down and advance the mandible in order to retain the appliance in place. The theory is that activating the mandibular musculature is important in obtaining a growth effect (thus the activator name), but this theory has not been supported by data and has largely been discarded.
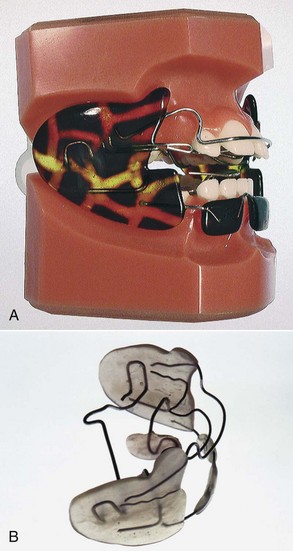
FIGURE 13-21 A, The Frankel-II appliance actively advances the mandible via contact of the lingual pad behind the lower incisors with the mucosa in that area and fosters expansion of the arches with the buccal shields. The lower lip pad also moves the lower lip facially. The appliance is largely tissue borne and potentially causes more soft tissue irritation than other functional appliances, but a patient can talk normally with it in place, which makes full-time wear feasible. B, Because of the wire framework, it is more susceptible to distortion than functional appliances made largely with plastic. (A courtesy Allesee Orthodontic Appliances (AOA), Sturtevant, WI.)

FIGURE 13-22 The Twin-Block functional appliance is retained on the teeth with conventional clasps (but can be cemented in place). The complementary inclines on the upper and lower portions are relatively steep, forcing the patient to advance the mandible in order to close. The plastic blocks also can be used to control posterior eruption. (Image courtesy Allesee Orthodontic Appliances (AOA), Sturtevant, WI.)
Development of removable and functional appliances continued in Europe in the early and mid-twentieth century despite their neglect in the United States. There were three major reasons for this trend: (1) Angle’s dogmatic approach to occlusion, with its emphasis on precise positioning of each tooth, had less impact in Europe than in the United States, (2) social welfare systems developed much more rapidly in Europe, which tended to place the emphasis on limited orthodontic treatment for large numbers of people, often delivered by general practitioners rather than orthodontic specialists, and (3) precious metal for fixed appliances was less available in Europe due to regulations in Germany that forbade the use of precious metals by dentists and then the disruptions of World War II. The interesting result was that in the 1925 to 1965 era, American orthodontics was based almost exclusively on the use of fixed appliances, while fixed appliances were essentially unknown in Europe and all treatment was done with removables, not only for growth guidance but also for tooth movement of all types.
A major part of European removable appliance orthodontics of this period was functional appliances for guidance of growth. A functional appliance by definition is one that changes the posture of the mandible and causes the patient to hold it open and/or forward. Pressures created by stretch of the muscles and soft tissues are transmitted to the dental and skeletal structures through function or through the appliances, moving teeth and modifying growth.
The monobloc developed by Robin in the early 1900s is generally considered the forerunner of all functional appliances, but the activator developed in Norway by Andresen in the 1920s was the first functional appliance to be widely accepted. Both the appliance system and its theoretical underpinnings were improved and extended elsewhere in Europe, particularly by the German school led by Haupl.
Functional appliances were introduced into American orthodontics in the 1960s through the influence of orthodontic faculty members with a background in Europe (of whom Egil Harvold was prominent) and later from personal contact by a number of American orthodontists with their European counterparts. (Fixed appliances spread to Europe at the same time through similar personal contacts.) A major boost to functional appliance treatment in the United States came from the publication of animal experiment results in the 1970s, which showed that skeletal changes really could be produced by posturing the mandible to a new position and held out the possibility that true stimulation of mandibular growth could be achieved. Although some of the enthusiasm for functional appliance treatment caused by the favorable animal experiments has faded in the light of less impressive results from clinical trials and retrospective clinical studies (see Chapter 7), functional appliances have achieved a major place in contemporary growth modification treatment.
With functional appliances, additional growth is supposed to occur in response to the movement of the mandibular condyle out of the fossa, mediated by reduced pressure on the condylar tissues or by altered muscle tension on the condyle (Figure 13-23). Although an acceleration of mandibular growth can occur and has been demonstrated now in several clinical trials,27 a long-term increase in size is difficult to demonstrate. What does happen is (1) a modest change in the size of the mandible’s overall length, which, taken over a number of types of appliances, averaged 0.16 mm per month (range = 0.09 to 0.24 mm per month),28 and (2) often a reorientation of the maxilla and the mandible, usually facilitated by a clockwise tipping of the occlusal plane and a rotation of either the maxilla, the mandible, or both. A reduction in forward growth of the maxilla (typically <1 mm per year), although small, is almost always observed along with any mandibular effects. This occurs because the elasticity of the facial soft tissues produces a reactive force against the maxilla when the mandible is held forward (Figure 13-24). Twin-Block appliances appear to be as successful at the peak of the growth spurt as when used early.29 The changes are a combination of skeletal (40%) and dental (60%) (i.e., there tends to be a strong Class II elastics effect).
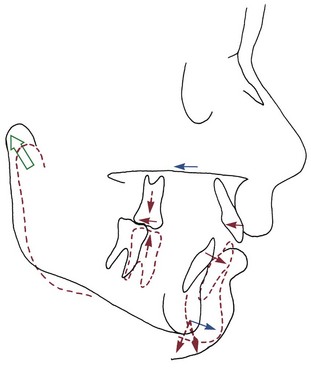
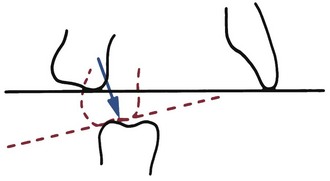
FIGURE 13-23 The potential effects of functional appliance therapy for correction of a Class II skeletal malocclusion are illustrated here. The most desirable and variable effect is for the mandible to increase in length by growth at the condyles, which may be accompanied by repositioning the articular fossa by apposition of bone on its posterior wall. The “headgear effect” restrains the maxilla and the maxillary teeth, and holding the mandible forward often creates forces against the lower teeth that cause anterior movement of the mandibular dentition. The direction in which mandibular growth is expressed, forward and/or inferiorly, is most related to the eruption of the molars. If the molars erupt more than the ramus grows in height (dashed arrows), the forward mandibular change will be negated and the Class II malocclusion will not improve.
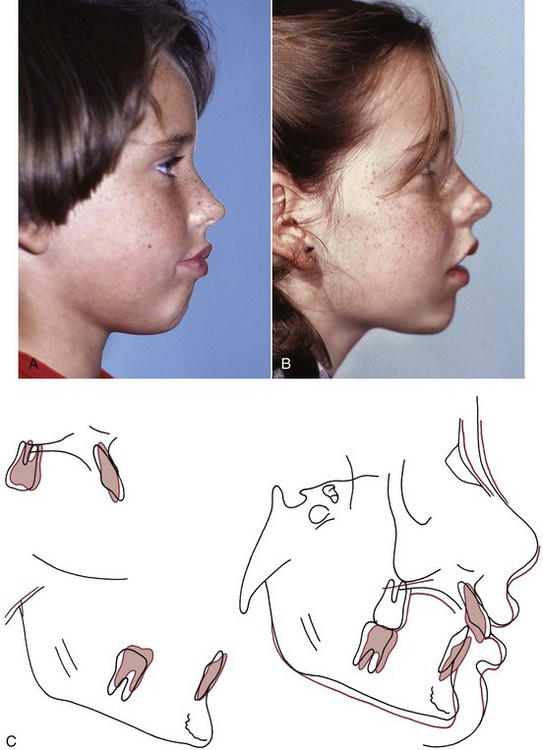
FIGURE 13-24 This child was treated with a functional appliance in an effort to correct her Class II malocclusion by changing the skeletal relationships. A, Pretreatment profile. B, Posttreatment profile. C, Cephalometric superimposition. Note that the major skeletal change seen in the cranial base superimposition is restriction of forward growth of the maxilla. This “headgear effect” is observed in most functional appliance treatment that anteriorly positions the mandible, presumably because the soft tissues are stretched when the mandible is advanced and this force is transferred to the maxilla. Note also the differential eruption of the lower molars and forward movement of the lower teeth.
Fixed Class II correctors (Herbst, mandibular anterior repositioning appliance [MARA], cemented Twin-Block; Figure 13-25) are historically newer developments that have recently become quite popular for use in the mixed and early permanent dentitions. Herbst created his appliance in the early 1900s and reported on it in the 1930s, but then it was largely forgotten until Pancherz rediscovered and popularized it in the 1970s. It forces the patient into an anterior occlusion and can generate skeletal and dental changes. In long-term studies of the outcome of treatment with the Herbst appliance, Pancherz noted substantial rebound in the immediate posttreatment period. He now recommends the Herbst appliance for the early permanent dentition when the changes are more localized to the protrusion of the mandible but not for use in the mixed dentition.30 Because the Herbst appliance can produce maxillary posterior dental intrusion, it provides better results when used in patients with normal or slightly long anterior face height.31 Less patient compliance compared to headgear or a removable functional appliance is an advantage; breakage has long been recognized as a significant disadvantage.
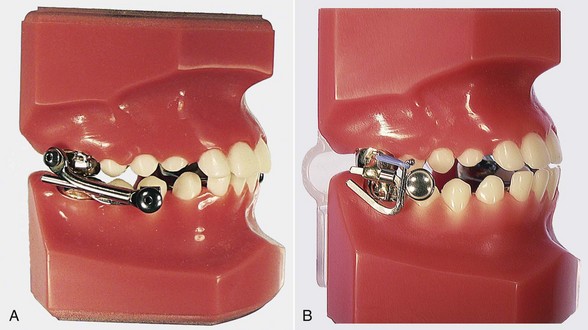
FIGURE 13-25 A, The Herbst appliance is probably most successful at the end of the mixed dentition. The most popular design currently uses crowns on the upper first molars and lower molars supported by lingual arch–type connectors for stability. The mandible is forced anteriorly in a passive manner by the plunger and tube that is anchored on the maxillary molars and cantilevered off the lower molar. Spacers can be added to the plunger to advance the mandible farther. This appliance does not require compliance for wear, since it is cemented, but it does require compliance to prevent breakage. B, The MARA appliance requires the patient to advance the mandible in order to close. Otherwise, the upper elbow interferes with the lower fixed arm. The appliance, which uses crowns on the molars connected by lingual arches, is durable and stable. Patients find it less bulky than the Herbst appliance and tend to prefer it over the Herbst. In order to increase the advancement, shims are added to the horizontal portion of the elbow and the elbow is tied back with an elastomeric tie. (Images courtesy Allesee Orthodontic Appliances (AOA), Sturtevant, WI.)
In the early 1990s, Toll and Eckhart jointly developed the MARA as a more durable and less bulky alternative to the Herbst appliance, but with the same fixed properties and anterior bite guidance. The MARA appliance appears to have at least a temporary headgear effect and affects the mandible, as measured by the SNB angle, less than the Twin-Block and Herbst.32 These appliances certainly can tip teeth. The tipping depends on which anterior and posterior teeth are included in the anchorage units through supplementary bonding or banding. In addition, they exert a protrusive effect on the mandibular dentition because the appliance contacts the lower teeth, and some of the reaction force from forward posturing of the mandible is transmitted to them with the continuous force from full-time wear.33
The combination of maxillary dental retraction and mandibular dental protrusion that all functional appliances create is similar to the effect of interarch elastics. This “Class II elastics effect” can be quite helpful in children who have maxillary dental protrusion and mandibular dental retrusion in conjunction with a Class II skeletal problem but is deleterious in patients who exhibit maxillary dental retrusion or mandibular dental protrusion. Mandibular dental protrusion usually contraindicates functional appliance treatment.
Functional appliances also can influence eruption of posterior and anterior teeth. It is possible to level an excessive curve of Spee in the lower arch by blocking eruption of the lower incisors while leaving the lower posterior teeth free to erupt. If upper posterior teeth are prohibited from erupting and moving forward while lower posterior teeth are erupting up and forward, the resulting rotation of the occlusal plane and forward movement of the dentition will contribute to correction of the Class II dental relationship. This is another effect of most functional appliance treatment for Class II problems (Figure 13-26). These changes combined with the previously mentioned skeletal effects provide the ability to correct Class II malocclusions. Early treatment is not required.
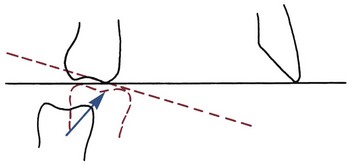
FIGURE 13-26 To facilitate Class II correction, the mesial and vertical eruption of the mandibular molar can be used advantageously. Rotating the occlusal plane upward posteriorly will in itself improve the molar relationship.
It is important to keep in mind that eruption of posterior teeth in a mandibular deficient patient is beneficial only when good vertical growth is occurring. More eruption of posterior teeth than growth of the ramus causes mandibular growth to be projected more downward than forward. In patients who have a tendency toward vertical rather than anteroposterior growth even without treatment, further posterior eruption must be prevented to avoid growth being expressed entirely vertically (Figure 13-27). The special problems created by excessive vertical growth are discussed later in this chapter.
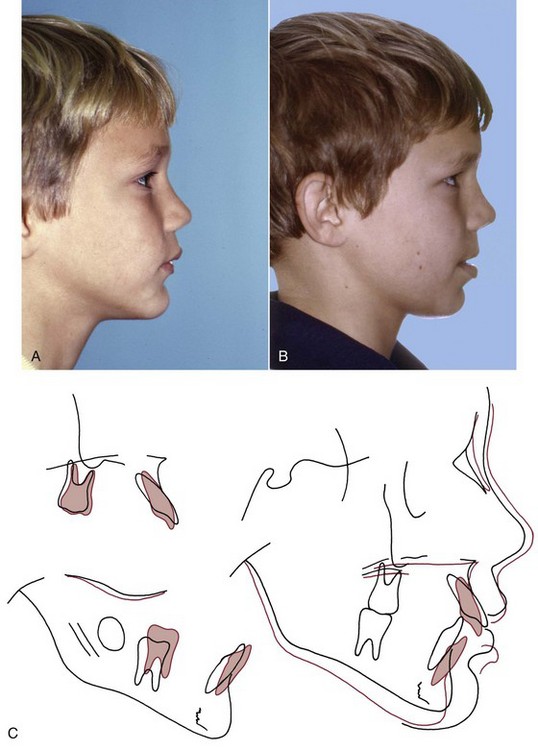
FIGURE 13-27 A poor response to Class II functional appliance treatment. A, Pretreatment profile. B, Posttreatment profile. C, Cephalometric superimpositions. Note that before treatment the child had a tendency toward increased lower face height and a convex profile. The cranial base superimposition indicates that the mandible rotated inferiorly and backward because of excessive eruption of the lower molar, which further increased the lower face height and facial convexity. Note in the mandibular and maxillary superimpositions the anterior movement of the lower incisors and retraction of the upper incisors, neither of which was desirable.
The other possible treatment for mandibular deficiency is to restrain growth of the maxilla with extraoral force (Figure 13-28) and let the mandible continue to grow more or less normally so that it catches up with the maxilla (Figure 13-29). Extraoral force, in the form of headgear appliances very similar to those used today, was used by the pioneer orthodontists of the late 1800s. As orthodontics progressed in the early twentieth century, however, extraoral appliances and mixed dentition treatment were abandoned, not because they were ineffective, but because they were considered an unnecessary complication. By 1920, Angle and his followers were convinced that Class II and Class III elastics not only moved teeth but also caused significant skeletal changes, stimulating the growth of one jaw while restraining the other. If intraoral elastics could produce a true stimulation of mandibular growth while simultaneously restraining the maxilla, there would be no need to ask a patient to wear an extraoral appliance, nor would there be any reason to begin treatment until the permanent teeth were available.

FIGURE 13-28 A Kloehn-type or cervical headgear appliance. This appliance uses a cervical neckstrap and a facebow to produce distal force on the maxillary teeth and maxilla. Its goal is to control forward growth of the maxilla while allowing the mandible to grow forward.
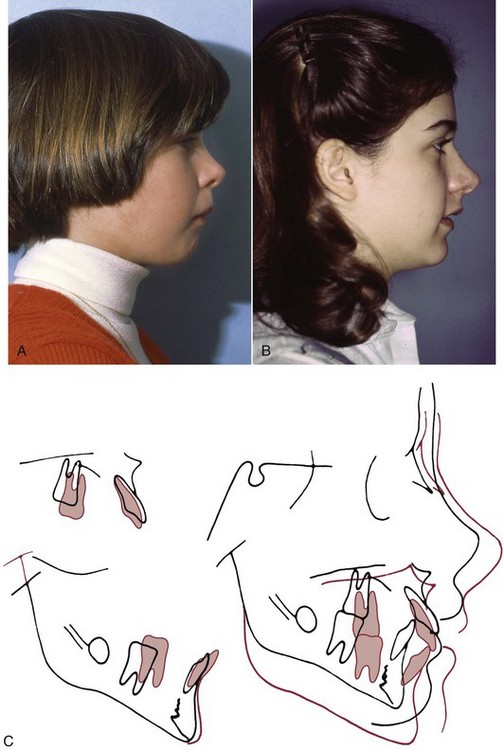
FIGURE 13-29 Headgear can be effective treatment for patients with mandibular deficiencies if the mandible grows while they are wearing it. Facial appearance before (A) and after (B) treatment using headgear and Class II elastics. C, Pretreatment and posttreatment cephalometric superimpositions. This patient showed restriction of maxillary growth and some impressive mandibular growth, combined with distal movement of the upper teeth and mesial movement of the lower teeth, which were accompanied by posterior eruption.
The first cephalometric evaluations of the effects of orthodontic treatment, which became available in the 1940s, did not support the concept that significant skeletal changes occurred in response to interarch elastics. A 1936 paper by Oppenheim revived the idea that headgear would serve as a valuable adjunct to treatment.34 However, it was not until the 1940s when Silas Kloehn’s impressive results with headgear treatment of Class II malocclusion became widely known35 that extraoral force to the maxilla again became an important part of American orthodontics. Cephalometric studies of patients treated with Kloehn-type headgear, which utilized a neckstrap and relatively light (300 to 400 gm) force, showed that skeletal change in the form of a reorientation of jaw relationships did occur.36 Experience soon revealed that although greater skeletal effects might be produced by higher levels of force than Kloehn had advocated, this required an upward direction of pull from a headcap to prevent excessive downward movement of the maxilla and a consequent downward and backward rotation of the mandible.37
No effect on the mandible would be expected, but restraint of mandibular growth along with restraint of maxillary growth is never observed, and some studies have found a small improvement in mandibular growth and chin prominence during headgear treatment.38
Beyond the skeletal effects, functional appliances and headgear also differ in their effects on the dentition. Removable functional appliances, especially those that rest against the teeth (i.e., tooth-borne ones with a labial bow), often place a distal force against the upper incisors that tends to tip them lingually and tip the lower incisors forward. Headgear force against the maxillary molar teeth often tips them distally. This often is accompanied by some distal movement of the maxillary premolars as force is transmitted to them by the supercrestal gingival fibers. There also is a vertical effect on the posterior teeth, extrusive with cervical headgear, possibly intrusive with high-pull headgear (true intrusion rarely occurs, but downward movement of the maxilla and posterior teeth is impeded). Remember that the mere fact that the teeth are moving distally will tend to open the bite anteriorly.39
There is specific information regarding early versus later treatment of Class II problems from randomized clinical trials. In the 1990s, two major projects using randomized clinical trial methodology were carried out at the University of North Carolina (UNC) and University of Florida.27,38 Another major trial at the University of Manchester in the United Kingdom was completed more recently.40 The results provide by far the best data that ever have been available for the response to early Class II treatment. The data from all the trials show that on average, children treated with either headgear or a functional appliance had a small but statistically significant improvement in their jaw relationship, while the untreated children did not. There is no question now that growth modification in Class II children is effective—it works in the majority of the patients.
A more important question relative to the timing of treatment is “Did early treatment with headgear or a functional appliance produce a long-term difference when early treatment outcomes are compared to the outcome of later (adolescent) treatment?” The UNC trial was extended into a second phase of treatment for all of the children to compare early two-stage with later one-stage treatment more completely; long-term data from the Florida trial also are available. Both the former controls and the two groups who had preadolescent growth modification treatment received comprehensive fixed appliance orthodontics (phase 2) when their permanent teeth erupted, during adolescence.
These data show that changes in skeletal relationships created during early treatment were at least partially reversed by later compensatory growth, in both the headgear and functional appliance groups. By the end of phase 2, the skeletal relationships between the former controls and the early treatment groups were similar. Peer Assessment Rating (PAR) scores, which reflect the alignment and occlusion of the teeth, also were not different at the end of phase 2 between the children who had early treatment and those who did not. The groups were also similar for extractions and eventual surgical treatment, although functional appliance treatment tended to increase the need for extractions.
From these studies, what can be concluded about the success of attempts to modify growth in Class II children and the benefits of early treatment for Class II problems? It appears that:
• Skeletal changes are likely to be produced by early treatment with headgear or a functional appliance but tend to be diminished or eliminated by subsequent growth and later treatment.
• Skeletal changes account for only a portion of the treatment effect, even when an effort is made to minimize tooth movement.
• After later comprehensive treatment, alignment and occlusion are very similar in children who did and did not have early treatment.
• Early treatment does not reduce the number of children who require extractions during a second phase of treatment or the number who eventually require orthognathic surgery.
• The duration of phase 2 treatment is quite similar in those who had a first phase of early treatment aimed at growth modification and those who did not.
Based on these results, it seems clear that for most Class II children, early treatment is no more effective than later treatment. Since early treatment takes longer and costs more, it is less efficient.
Another finding of the early treatment studies was that among the treated and control groups, both with reasonably high self-concepts to begin with, the early treatment group reported higher self-concepts, less anxiety and better physical appearance, popularity, and happiness and satisfaction than the controls at the end of phase 1. The treated patients also believed the benefits of treatment were general well-being, confidence, health of teeth, and mouth function.40 This difference, however, disappeared by the end of phase 2 when both groups finished comprehensive treatment.
What this means is that early Class II treatment is indicated for some but not all children. The data suggest that the primary indication is a child with psychosocial problems related to dental and facial appearance.
If early treatment is pursued, when the maxillary skeletal and dental effects that go along with any enhancement of mandibular growth are considered, functional appliances usually are preferred for mixed dentition treatment of mandibular deficiency. For many patients who do not have a definitive maxillary excess or mandibular deficiency as part of the Class II problem, either type of appliance that the patient will comply with can be used with some degree of success. Headgear probably is a better choice for a patient with frank maxillary excess.
Components of Removable and Fixed Class II Functional Appliances
The changes observed with functional appliances, especially the effects on the teeth, are the result of the appliance design. This section will briefly illustrate how the components of the appliances can be used to produce wanted effects and possibly mitigate unwanted effects. An appropriate appliance prescription specifies the appliance components that would be most effective in solving the patient’s specific problems. It is important to have the appliance design in mind prior to the impressions and bite registration because the impression technique is affected by what appliance components are selected, where they will be placed, and the intra-arch space required for them.
Components to Advance the Mandible
Components to advance the mandible are often classified as active or passive. If the patient has to voluntarily move the mandible to avoid an interference, the appliance is active. If it allows only a restricted path of movement or closure, it is passive. By that definition, appliances commonly used during the mixed dentition years, such as the activator, bionator, Twin-Block, and MARA, are active appliances, while the Herbst is a passive appliance.
For most mandibular deficient patients, a bionator or activator-type appliance (see Figure 13-20) is the simplest, most durable, and most readily accepted appliance. Flanges, either against the mandibular alveolar mucosa below the mandibular molars or lingual pads contacting the tissue behind the lower incisors, provide the stimulus to posture the mandible to a new more anterior position (Figure 13-30). The Frankel appliance uses lingual pads against the gingiva below the lower incisors to stimulate forward posturing of the mandible. Ramps supported by the teeth, as in the Twin-Block appliance (see Figure 13-22), are another mechanism for posturing the mandible forward. So is the elbow in the MARA appliance (see Figure 13-25). With all these appliances, the concept is that growth modification is the result of the patient using his or her own musculature to posture the mandible forward (active), as opposed to the mandible being held forward passively by the appliance, which produces external pressure on the teeth while the patient relaxes.
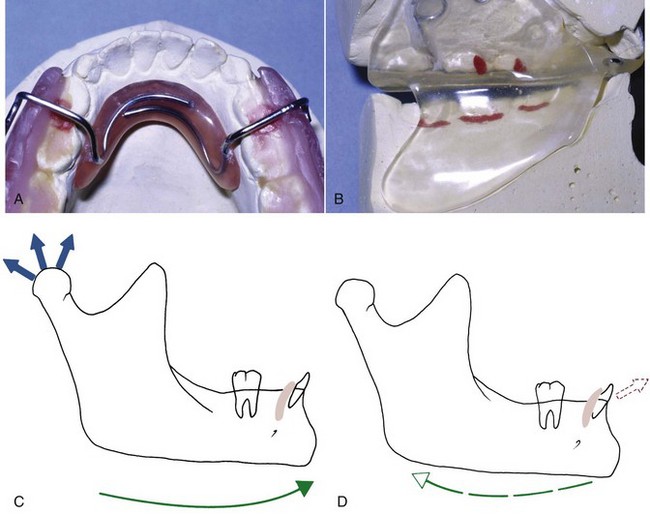
FIGURE 13-30 The lingual pad or flange determines the anteroposterior and vertical mandibular posture for most functional appliances. A, The small lingual pad from a Frankel appliance. B, The extensive lingual flange from a modified activator. C, The lingual components not only position the mandible forward but also exert a protrusive effect (D) on the mandibular incisors when the mandible attempts to return to its original position, especially if some component of the appliance contacts these teeth.
All the fixed appliances have the advantage of full-time wear and permanent postural change (at least until the dentist removes the appliance). The disadvantage is that pressure against the teeth, which produces compensatory incisor and molar movements, cannot be avoided—the patient simply cannot actively hold the mandible forward all the time. The point may be not whether the appliance is active or passive, but where and how the forces are applied to the teeth and how much dental compensation is built into the treatment. The more dental change, the less room there is for skeletal change by whatever means.
Other Possible Components
Vertical Control Components: When acrylic or wire is placed in contact with a tooth and the vertical dimension is opened past the normal postural position, the stretch of the soft tissues will exert an intrusive force on the teeth (Figure 13-31). Intrusion usually does not occur, probably because the force is not constant, but eruption is likely to be impeded. Thus the presence or absence of occlusal or incisal stops, including bite blocks, provides a way to control the vertical position of anterior or posterior teeth, allowing teeth to erupt where this is desired and preventing it where it is not. Vertical control of this type is usually included in the design of any functional appliance.
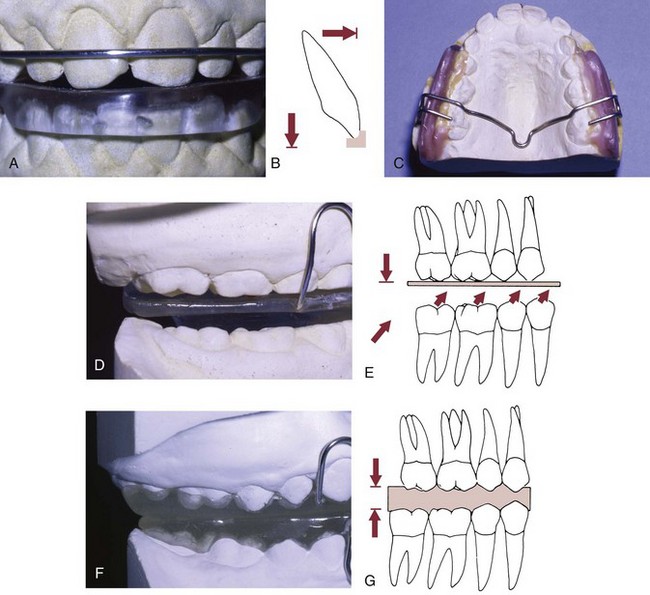
FIGURE 13-31 Incisal and occlusal stops control eruption of anterior and posterior teeth, respectively. A, The acrylic caps the lower incisors and serves as a stop for the upper incisors, which prohibits eruption of these incisors. B, Incisal stops can extend to the facial surface and control the anteroposterior incisor position, as shown for the upper arch in this diagram. C, Posterior stops can be constructed of wire or acrylic (D). E, This positioning of the occlusal stops inhibits maxillary eruption but allows mandibular teeth to erupt. F, A complete acrylic posterior bite block impedes both maxillary and mandibular eruption (G) and is useful in controlling the amount of increase in anterior face height.
The same principle applies to tongue position. Lingual shields prevent the resting tongue from being placed between the teeth (Figure 13-32). This has the effect of enhancing tooth eruption. A lingual shield is particularly important if eruption of posterior teeth is desired on one side but not the other. One caution here is that this component often limits the patient’s acceptance of the appliance because speaking can be difficult.
Stabilizing Components: An assortment of clasps can be used to help retain a functional appliance in position in the mouth (Figure 13-33, A) (see also the discussion of clasps for removable appliances in Chapter 10). Clasps often help the first-time wearer adapt to the appliance. They can be used initially and then removed, deactivated, or allowed to gradually loosen with wear if desired, when the patient has learned to use the appliance. The labial bow across the maxillary incisor teeth that is included in many functional appliances (Figure 13-33, B) should be considered and managed as a stabilizing component in almost all instances.

FIGURE 13-33 A, Clasps add retention, which is needed to help maintain some types of appliances with active components like springs and expansion screws in position. The clasps also can serve as a training device when patients are learning to accommodate to a functional appliance that repositions their jaws. Note the headgear tube, for high-pull headgear that can stabilize the appliance and provide an extraoral distal force to the maxilla. B, The purpose of a labial bow on a functional appliance is to help guide the appliance into proper position, not to tip the upper incisors lingually. For this reason, the bow is adjusted so it does not touch the teeth when the appliance is seated in position. Even then it often contacts them during movement or displacement of the appliance. Undesirable lingual tipping of incisors during functional appliance wear therefore usually reflects a failure of the child to keep the mandible positioned forward while wearing the appliance.
Passive Components: Plastic buccal shields and lip pads, both of which are incorporated into the Frankel appliance (Figure 13-34), hold the soft tissues away from the teeth. The effect is to disrupt the tongue-lip/cheek equilibrium, and this in turn leads to facial movement of the teeth and arch expansion that results in an increase in arch circumference as well. This method of obtaining tooth movement reflects the idea that the most stable tooth movement is produced by changing the soft tissue environment, but, of course, when the appliance is removed, the environment is likely to revert to what it was previously.
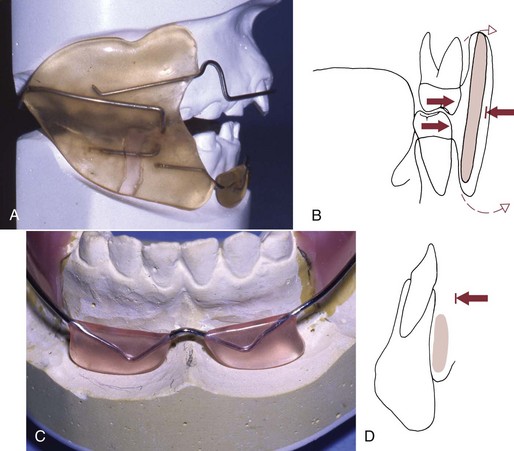
FIGURE 13-34 A, A buccal shield holds the cheek away from the dentition and facilitates posterior dental expansion (B) by disrupting the tongue–cheek equilibrium. The shield is placed away from the teeth in areas where arch expansion is desired. If the shield is extended to the depth of the vestibule, there is the potential for periosteal stretching that facilitates deposition of bone (dashed arrows). C, The lip pad holds the lower lip (or upper lip with a Frankel III appliance) away from the teeth and forces the lip to stretch to form a lip seal. D, The pad must be carefully positioned at the base of the vestibule to avoid soft tissue irritation.
Buccal shields and lip pads can be added to any appliance to facilitate arch expansion. Their disadvantage is that they add to the potential for soft tissue irritation that can inhibit patient compliance. The addition of a vertical stop over the lower incisors (Figure 13-35) decreases irritation from the lip pads and makes the appliance more comfortable to wear and more acceptable to patients.

FIGURE 13-35 Frankel deliberately configured his appliances to minimize contact with the teeth, but this means they can move in a way that creates soft tissue irritation. Adding occlusal coverage of the lower incisors stabilizes the appliance and reduces compliance problems, without detracting from the appliance’s ability to guide growth. (Courtesy Dr. A. Willis.)
Active Expansion/Alignment Components: In theory, there is no reason that growth guidance with a functional removable appliance cannot be combined with active tooth movement produced by springs or screws. The original activators did not use any springs or screws, but later, modified activators added the elements of active plates to an activator framework so that teeth could be moved while jaw growth was being manipulated (Figure 13-36).

FIGURE 13-36 Tooth-borne functional appliances can incorporate expansion screws to increase sagittal and transverse dimensions. This modification requires posterior clasps to aid in retention. The expansion activator and orthopedic corrector are examples of active tooth-borne appliances. Screws produce heavy intermittent force, not the more physiologic light continuous forces that are preferred now, and usually promote tipping of the anterior teeth in a facial direction. There are few if any indications now for use of this type of appliance.
Incorporating active elements into a functional removable appliance is a decidedly mixed blessing. There are three problems. The first is that correcting the occlusal relationships by actively moving teeth is not the goal of functional appliance therapy, and in fact the more tooth movement, the less skeletal change can be utilized or achieved (Figure 13-37). Next, precise tooth positions cannot be achieved with springs or screws in removable appliances. Finally, the tooth movement will be only from tipping, which is less stable and more susceptible to relapse. This means that in contemporary orthodontics, there are few indications for removable appliances designed to provide all aspects of treatment.
FIGURE 13-37 Cephalometric superimposition showing an unsatisfactory response to a removable functional appliance for a skeletal Class II malocclusion. Note the lack of skeletal response but dental changes, including forward movement of the lower incisors, slight retraction and elongation of the upper incisors, and downward and backward rotation of the mandible. Adding springs to a functional appliance, if it accentuates this pattern of tooth movement, makes the treatment response worse rather than better.
Treatment Procedures with Functional Appliances
Pretreatment Alignment: After treatment goals have been established and the decision has been made to use a functional appliance, the incisor position and relationships should be carefully examined. Because functional appliances for the treatment of mandibular deficiency require the mandible to be held in a protruded position to have a treatment effect, the patient’s ability to posture forward at least 4 to 6 mm is critical. Most mandibular deficient children have a large overjet and can do this readily, but in some cases incisor interferences prevent the mandible from being advanced to the correct position for the bite registration. The problem can be either lingual displacement of the upper incisors (a Class II, division 2 incisor pattern) or irregular and crowded incisors in either arch. (It must be kept in mind that facial displacement of the lower incisors, which would be produced by aligning them without creating space to do so, contraindicates functional appliance treatment that would move them even further facially.)
For both the Class II division 2 patient with limited overjet and the Class II division 1 patient with crowded and irregular upper incisors, the first step in treatment is to tip the upper incisors forward and/or align them (Figure 13-38). Either fixed or removable functional appliances can be used for this purpose, depending on the type and magnitude of tooth movement required, but a fixed functional appliance is quite compatible with bonded attachments on incisors and a removable one is not. Generally a short period of treatment with limited banding and bonding of the maxillary teeth accomplishes the necessary alignment and overjet so that an appropriate working bite can be obtained with the mandible positioned anteriorly and inferiorly to correct the horizontal and vertical deficiency. To control their tendency to relapse lingually, the repositioned incisors should be held in place for several months after being repositioned.
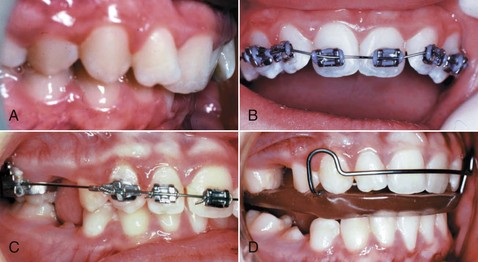
FIGURE 13-38 A, For this girl with a Class II division 2 malocclusion, it was impossible to take the bite registration for a functional appliance until the maxillary incisors were tipped facially. B, Although a change of this type was made with a removable maxillary appliance with fingersprings until recently, the prefunctional alignment now often can be accomplished more efficiently with a partial fixed appliance. In this case, the molars were banded, the canines and incisors bonded, and a superelastic NiTi wire was placed. C, The same patient 2 months later, with alignment accomplished and overjet established. D, Same patient 4 months later, with a deep bite bionator in place. (From Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St Louis: Mosby; 2003.)
Impressions and Working Bite
The next step is to make impressions of the upper and lower arches and register the desired mandibular position, the “working bite.”
The impression technique for a removable functional appliance depends on the appliance components that will be used. Good reproduction of the teeth and an accurate representation of the area where the lingual pads or flanges will be placed are mandatory. If buccal shields or lip pads are to be used, it is important not to overextend the impressions so that tissue is displaced because this makes it difficult or impossible to accurately locate the appliance components in the vestibule. Improper location of the components leads to long-term soft tissue irritation, discomfort, difficulty in appliance adjustment, and poor patient compliance.
For a cemented, bonded, or partially fixed functional appliance, accurate impressions of the teeth are essential, but extension of the impressions into the vestibules is not important. If bands or steel crowns are used to retain a Herbst appliance, they can be fabricated indirectly by a laboratory on the cast by disking the teeth to create space, and many clinicians prefer this time-saving method. If the clinician supplies the bands or crowns on casts or in impressions, separation is required before fitting the bands and at appliance delivery. If laboratory bands or crowns are used, then separation is required only before appliance delivery. Most clinicians have deserted bands for retention of fixed functional appliances because they have proved to be easily distorted and broken. Metal crowns, which are fit without reducing the teeth; cast splints that can be bonded; or bonded acrylic splints are more satisfactory. The crowns should have holes, not for the release of cement but for access to the occlusal surface during appliance removal. This provides a point of leverage on tooth structure.
The working bite is the same for fixed and removable functional appliances. It is obtained by advancing the mandible to move the condyles out of the fossa and establishing the desired vertical opening (Figure 13-39).

FIGURE 13-39 Steps for obtaining a “working bite” for functional appliance construction. A, Multiple layers of hard wax are luted together and cut to the size of the mandibular arch. The patient’s preliminary record casts can be used to trim the wax to a size that will register all posterior teeth, while not covering the anterior teeth or contacting the retromolar areas. It is important to avoid interferences from retromolar soft tissues. If such an interference is not detected, the finished appliance will not seat correctly. At best, this will require reduction of the posterior plastic stops if they were integrated into the design. At worst, a new bite registration and appliance will be necessary. B, In preparation for obtaining the working bite, the wax is softened in hot water, while the child is directed to practice the working bite position. Some children can easily reproduce working bites after only a few practice tries, but others need more opportunities and perhaps some help. The softened wax is seated on the maxillary posterior teeth and pressed into place to ensure good indexing of the teeth. C, With the anterior teeth exposed, the position of the mandible easily can be judged while the bite is being taken. The mandible is guided to the correct anteroposterior and vertical position by watching the midline relationships and the incisal separation. There must be enough space for the laboratory technician to place wire and plastic between the teeth to connect major components of the appliance and construct occlusal and incisor stops. The minimal posterior opening to achieve the vertical space is 3 to 4 mm. Interocclusal stops or facets to guide eruption, as in most activators and bionators, usually require 4 to 5 mm of posterior separation to be effective. D, Either stacked tongue blades or (E) a Boley gauge can be used to control the amount of closure and help the patient reproduce the correct bite. If a vertical stop made of tongue blades is used, it must remain in the proper orientation (parallel to the true horizontal). Otherwise, as the tongue blades incline either inferiorly or superiorly, the mandible will either be closed and retruded or opened, respectively, to an incorrect position. When the correct bite has been obtained, the wax should be cooled and removed from the mouth. The bite should be examined for adequate dental registration and soft tissue interferences and rechecked for accuracy. Definite registration of both maxillary and mandibular teeth is required for proper appliance construction.
Unless an asymmetry is to be corrected, the mandible should be advanced symmetrically so that the pretreatment midline relationships do not change appreciably. We recommend a 4 to 6 mm advancement and a 3 to 4 mm vertical opening, but always one that is comfortable for the patient and does not move the incisors past an edge-to-edge incisor relationship. The practical reason for recommending this modest advancement is better patient comfort, facial esthetics, and patient compliance than with large advancements. Small advancements lead to more appliance adjustments. The claim that small advancements are more effective because muscle adaptation is better has not been supported by evidence. From a scientific perspective, it appears that quite large, modest, or relatively small advancements all can produce growth modification and that there is little difference between the results.41
If eruption of upper and lower posterior teeth is to be limited, as in a child with excessive vertical face height (see further discussion later in this chapter), the working bite should be taken with the patient open 2 to 3 mm past the resting vertical dimension (i.e., 5 to 6 mm total opening in the molar region), so that the soft tissue stretch against the bite blocks will produce a continuous force opposing eruption.
Clinical Management of Functional Appliances
Removable Functional: When a removable functional appliance is returned from the laboratory, it should be checked for correct construction and fit on the working cast. The best technique for delivery is to adjust the appliance and work with the child to master insertion and removal before any discussion with the parent. This enables the child to be the full focus of attention initially and forestalls the effect of comments by the parents such as “That will be a mouthful!”
With any functional appliance, a break-in period is helpful. Having the child wear the appliance only a short time per day to begin with and increasing this time gradually over the first few weeks is a useful method of introduction. The child should be informed that speaking may be difficult for a while but that comfort and speaking facility will increase. Problems with speech are greatest when there is a bulk of acrylic behind or between the anterior teeth.
To be effective, functional appliances should be worn when growth is occurring and when teeth are erupting. If the appliance is in place during these hours, one can take advantage of skeletal growth and either use or inhibit tooth eruption. It is known now (see Chapter 8) that skeletal growth has a circadian rhythm. Most growth occurs during the evening hours when growth hormone is being secreted; active eruption of teeth occurs during the same time period, typically between 8 pm and midnight or 1 am. To take practical advantage of this time period, it is suggested that children wear functional appliances from after the evening meal until they awake in the morning, which should be approximately 12 hours per day. Waiting until bed time to insert the appliance misses part of the period of active growth. Wearing the appliance during the day may add a small advantage, but this is difficult to achieve because it begins to impinge on school hours and can increase the negative social impact of the appliance, as well as appliance loss and breakage.
A good appointment schedule is to recall the child at 1 and 2 weeks after insertion for inspection of the tissues and the appliance. If the patient does not call about a problem during the first week, the one-week appointment can be cancelled. Charts for children to record their “wearing time” are helpful, both for the data they provide and because the chart serves as a reinforcement for the desired behavior. Unfortunately, the time reported by patients and actual compliance often do not coincide.
If a sore spot develops, the child should be encouraged to wear the appliance a few hours each day for 2 days before the appointment, so the source of the problem can be determined accurately. Usually, smoothing the plastic components can be accomplished quickly. Gross adjustments should be avoided because appliance fit and purpose can be greatly altered. For example, heavy reduction of the lingual flanges will allow the patient to position the mandible in a more posterior position.
Because the initial mandibular advancement is limited to a modest 4 to 6 mm and many children require more anteroposterior correction, a new appliance may be needed after 6 to 12 months of wear and a favorable response. It is a good idea to reevaluate progress at 8 to 10 months after delivery with new records or at least a progress cephalometric radiograph. If little or no change has occurred in that time, then compliance is poor, the design is improper, or the patient is not responding to the appliance. In any case, a new treatment plan is needed.
Fixed Functional Appliances: At the insertion of a Herbst appliance, MARA, or cemented Twin-Block, discussion should focus on care of the appliance and acceptable mandibular movements. Because these appliances are fixed, a wear schedule is not required, but some patients initially have problems adapting to the appliance and the forward mandibular position. It is good to warn the patient and parents of this and assure them that accommodation increases rapidly after several days. Soft tissue irritation is not a major problem with the Herbst or Twin-Block, but the teeth may be more sensitive than with removable functional appliances. Patients should be instructed that the appliance is meant to remind them to posture the mandible forward and not to force the mandible forward with heavy pressure on the teeth. In this sense, sore teeth for an extended amount of time may indicate poor cooperation. Avoiding hard and sticky foods, large mouthfuls, and exaggerated mandibular movements can greatly reduce the need for repair of a fixed functional appliance.
The Herbst appliance and the newer variations of it must be carefully inspected for breakage at each visit. With the Herbst, after a positive treatment response is noted, changes in the pin and tube length can be made during treatment to increase the amount of advancement simply by adding washer-type sleeves to the pin to restrict insertion of the pin into the tube (Figure 13-40). With the MARA appliance, advancement is achieved via shims on the elbow wire to advance it. A fixed (or removable) Twin-Block appliance can have plastic resin added to the inclines to increase the advancement without totally remaking the appliance. Plastic also can be removed adjacent to the teeth to allow drift, especially on the occlusal surfaces to encourage eruption when that is desirable.
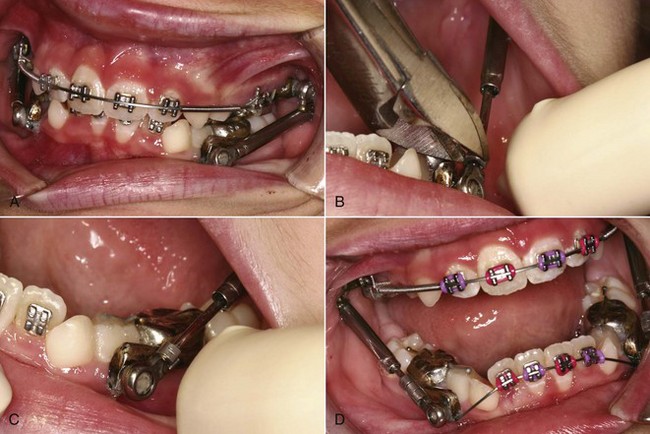
FIGURE 13-40 It is undesirable to advance the mandible more than 5 to 6 mm in a single step because this is uncomfortable to the patient. With the Herbst appliance, steps in advancement can be accomplished by placing a series of shims over the plunger. A, Herbst appliance after several weeks with the mandible in the position of initial advancement of 3 to 4 mm. B, To increase the amount of advancement, a section of a split tube is being placed over the plunger and crimped so that the opening in the wall of the tube is closed. C, The shim in place. D, Additional spacers in place after a series of adjustments.
It is possible to make a Twin-Block appliance partially fixed and partially removable (Figure 13-41). This also is possible with a Herbst appliance. In both cases, this typically involves a fixed upper and removable lower splint. In this case, the fixed and removable parts should be carefully explained, so that the child does not remove or loosen the appliance due to a misunderstanding.
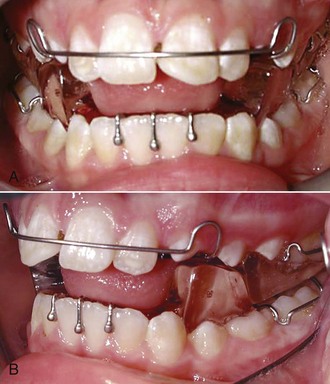
FIGURE 13-41 The Twin-Block appliance can be used as a cemented (fixed) or removable appliance. A, This patient had a Class II malocclusion treated with a removable Twin-Block appliance that advanced the mandible (B). The ramps on the separate upper and lower units force the mandible to a more protruded and vertically increased position. Adjustments can be made to the occlusal coverage and the inclines to modify eruption and the amount of advancement. Cementing the upper section greatly increases the chance that both parts of the appliance will be worn because the patient then is more comfortable with the lower section in place. (Courtesy Dr. M. Mayhew.)
When the desired advancement has been achieved with any of the fixed Class II correctors and the patient is stable (anticipating 1 to 2 mm of relapse), then the appliance can be removed. A Herbst appliance usually is worn for 8 to 12 months, at which point the desired correction should have been obtained, and similar timing is expected with the other fixed functionals. In the case of the Herbst or the MARA, a bur to cut the crowns, a crown or band slitter, or a band-removing plier inserted in the crown removal holes are possible removal methods.
Records should be obtained at the end of phase 1 growth modification treatment to document the progress and plan the details and timing of the second phase of treatment. Generally, full appliances supported by Class II elastics are the next step in treatment. If the patient is still in the mixed dentition when the desired correction is achieved, the Herbst or MARA appliance can be removed at that point, but it is important to consider use of a removable functional appliance of the activator or bionator type as a retainer when this is done (see Chapter 17). This retainer should be worn approximately 12 hours per day until the patient is ready for the second phase of fixed appliance treatment. Avoiding a prolonged retention period is a major reason for delaying fixed functional treatment until the adolescent growth spurt is beginning.
Extraoral Force: Headgear
There are two major components of a headgear appliance: the facebow and the neckstrap or headcap. Facebows are fairly standard and simply apply the force to the teeth, although they come in varying sizes to accommodate the size of the arches. A facebow is usually applied to the permanent first molars but can be applied through splints and functional appliances. The anchorage component (headcap or neckstrap) is responsible for the direction of the force, either above the occlusal plane or below the occlusal plane, respectively (Figure 13-42).
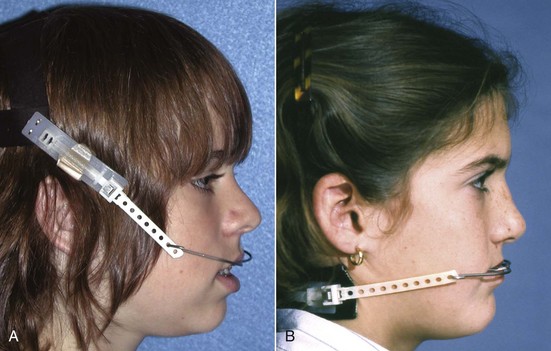
FIGURE 13-42 Various types of headgear provide different directions of force for different clinical situations. A, High-pull headgear consists of a headcap connected to a facebow. The appliance places a distal and upward force on the maxillary teeth and maxilla. B, Cervical headgear is made up of a neckstrap connected to a facebow. This appliance produces a distal and downward force against the maxillary teeth and the maxilla.
Effects of Extraoral Force on the Maxilla
Numerous studies, including the recent clinical trials, have shown that headgear force can decrease the amount of forward and/or downward growth of the maxilla by changing the pattern of apposition of bone at the sutures. Class II correction is obtained as the mandible grows downward and forward normally while similar forward growth of the maxilla is restrained, so mandibular growth is a necessary part of the treatment response to headgear (Figure 13-43). As noted earlier, there is some evidence of increased mandibular growth during treatment with headgear. Keeling et al have suggested that this might be due to the use of a biteplate in conjunction with headgear,38 but a similar acceleration of mandibular growth has been noted in other studies of headgear outcomes when a biteplate was not used. Whatever the mechanism, headgear does appear to have both maxillary and mandibular effects.

FIGURE 13-43 A good response to headgear treatment. A, Pretreatment. B, Posttreatment following approximately 2 years of headgear treatment. C, Cephalometric superimpositions. Note the favorable downward-forward mandibular growth with limited change in the maxillary position. There also were limited incisor changes other than some eruption and maxillary incisor retraction.
In a preadolescent child, headgear must be worn regularly for at least 10 to 12 hours per day to be effective in controlling growth. The growth hormone release that occurs in the early evening strongly suggests that, as with functional appliances, putting the headgear on right after dinner and wearing it until the next morning—not waiting until bed time to put it on—is an ideal schedule. The current recommendation is a force of 12 to 16 ounces (350 to 450 gm) per side. When teeth are used as the point of force application, some dental, as well as skeletal, effects must be expected. Extremely heavy forces (greater than 1000 gm total) are unnecessarily traumatic to the teeth and their supporting structures, while lighter forces may produce dental but not skeletal changes.
To correct a Class II malocclusion, the mandible needs to grow forward relative to the maxilla. For this reason it is important to control the vertical position of the maxilla and the maxillary posterior teeth. Downward movement of either the jaw or the teeth tends to project mandibular growth more vertically, which nullifies most of the forward mandibular growth that reduces the Class II relationship (Figure 13-44). The molars should not be elongated, and distal tipping of these teeth should be minimized when the objective is a change in skeletal relationships (Figure 13-45). In addition, it is necessary to try to control vertical growth of the maxilla.

FIGURE 13-44 This child had a poor response to headgear treatment for a Class II malocclusion. The cranial base superimposition indicates that the lips were retracted and the maxilla did not grow anteriorly. The maxillary superimposition shows that the incisors were retracted and the molar movement and eruption were limited. All these effects were beneficial for Class II correction, but the mandible rotated down and backward because of the inferior movement of the maxilla and eruption of the lower molar. As a result, the profile is more convex than when treatment began and the Class II malocclusion is uncorrected.
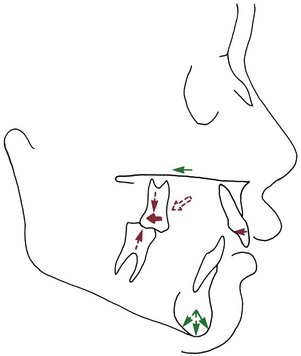
FIGURE 13-45 Headgear treatment can have several side effects that complicate correction of Class II malocclusion. If the child wears the appliance, maxillary skeletal and dental forward movement will be restricted. Although this helps in correction of the Class II malocclusion, vertical control of the maxilla and maxillary teeth is important, because this determines the extent to which the mandible is directed forward and/or inferiorly. Downward maxillary skeletal movement or maxillary and mandibular molar eruption (all shown in dashed arrows) can reduce or totally negate forward growth of the mandible.
In theory, the movement of the maxilla can be controlled in the same way as a single tooth is controlled: by managing forces and moments relative to the center of resistance of the jaw. In practice, it is difficult to analyze exactly where the center of resistance and center of rotation of the maxilla might be, but it is above the teeth and most likely above the premolar teeth. Directing the line of force closer to the center of resistance is a major reason for including an upward direction of pull for most children who have headgear force to the maxilla.
Selection of Headgear Type
There are three major decisions to be made in the selection of headgear. First, the headgear anchorage location must be chosen to provide a preferred vertical component of force to the skeletal and dental structures. A high-pull headcap will place a superior and distal force on the teeth and maxilla, while a cervical neckstrap will place an inferior and distal force on the teeth and skeletal structures (see Figure 13-42). A straight distal pull can be produced by a combination of the two. The initial choice of headgear configuration is usually based on the original facial pattern: the more signs of a vertically excessive growth pattern are present (see Chapter 6), the higher the direction of pull and vice versa. Reports of responses to headgear treatment show, however, that there is considerable variation and unpredictability in growth response. Cervical headgear does not always aggravate vertical problems, especially when there is good vertical mandibular growth42 and minimal distal movement of maxillary molars, which is the best predictor of vertical opening.
The second decision is how the headgear is to be attached to the dentition. The usual arrangement is a facebow to tubes on the permanent first molars. Alternatively, a removable maxillary splint or a functional appliance can be fitted to the maxillary teeth and the facebow attached to it. This may be indicated for children with vertically excessive growth (which is discussed further later in this chapter). Attaching headgear to an archwire anteriorly is possible but rarely practical in mixed dentition children and produces relatively heavy forces on anterior teeth.
Finally, a decision must be made as to whether bodily movement or tipping of the teeth is desired. Since the center of resistance for a molar is estimated to be in the midroot region, force vectors above this point should result in distal root movement. Forces through the center of resistance of the molar should cause bodily movement, and vectors below this point should cause distal crown tipping. The length and position of the outer headgear bow and the form of anchorage (i.e., headcap or neckstrap) determine the vector of force and its relationship to the center of resistance of the tooth. These factors determine the molar movement.
The various combinations of force direction (anchorage), length of outer bow, and position of outer bow are diagrammatically illustrated in Figure 13-46. As in any growth modification treatment, tooth movement generally is an undesirable side effect, and with headgear, tooth movement is minimized by causing the teeth to move bodily if they move at all.
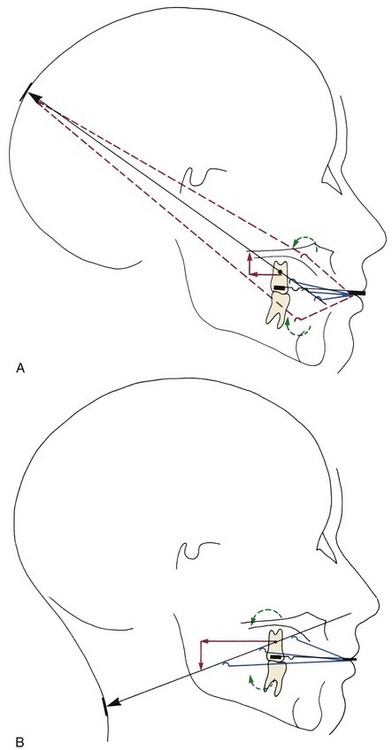
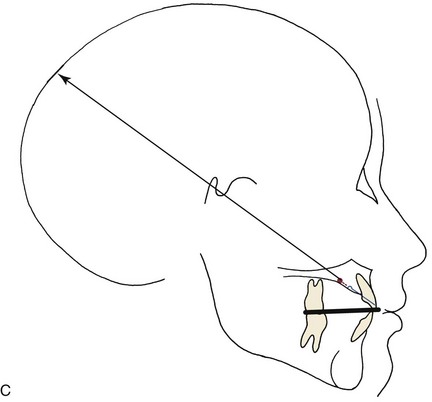
FIGURE 13-46 These diagrams illustrate effects of four commonly used types of facebow and extraoral anchorage attachments. In each diagram, the inner bow is shown in black, and the various outer bow possibilities in red or dotted red. A, High-pull headgear (headcap) to the first molar. To produce bodily movement of the molar (no tipping), the line of force (black arrow) must pass through the center of resistance of the molar tooth. This will produce both backward and upward movement of the molar. Note that the line of force is affected by the length and position of the outer bow, so that a longer outer bow bent up or a shorter one bent down could produce the same line of force. If bow length or position produces a line of force above or below the center of resistance (dotted red), the tooth will tip with the root or the crown, respectively, going distally because of the moment that is produced. B, Cervical headgear (neckstrap) to the first molar. Again, bodily movement is produced by an outer bow length and position that places the line of force through the center of resistance of the molar; but with a lower direction of pull, the tooth is extruded as well as moved backward. Note that the outer bow of a facebow used with cervical traction nearly always is longer than the outer bow used with a high-pull headcap. If the line of force is above or below its center of resistance, the tooth will tip with the root or crown, respectively, going distally as indicated by the dotted arrows. C, High-pull headgear to a short facebow inserted into a maxillary splint. With all the teeth splinted, it is possible to consider the maxilla as a unit and to relate the line of force to the center of resistance of the maxilla. As with headgear force against the first molar, the relationship of the line of force to the center of resistance of the maxilla determines the rotational effect on the maxilla.
Similar considerations apply to the maxilla: unless the line of force is through its center of resistance, rotation of the jaw (the skeletal equivalent of dental tipping) will occur. Control of the line of force relative to the maxilla is easier when a splint covering all the teeth is used to apply the headgear force. The facebow is usually attached to the splint in the premolar region, so that the force can be directed through the center of resistance of the maxilla that is estimated to be located above the premolar roots (see Figure 13-46, C). Distal tipping of the maxillary incisors is likely to occur, however, because the distal component of the force is delivered to these teeth.
Clinical Management of Headgear
For headgear treatment in a preadolescent child, molar bands with headgear tubes (and any other attachments that might be needed later in treatment) are fitted and cemented. Fitting and adjusting the preformed facebow, which must reflect the biomechanical goals of the treatment plan, are shown in Figures 13-47 and 13-48.

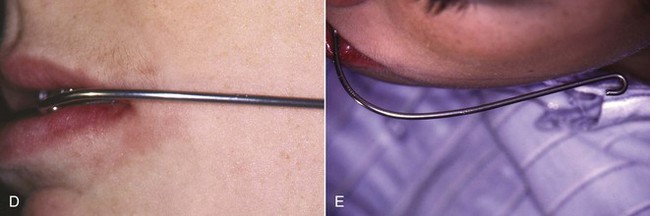
FIGURE 13-47 The steps for fitting a facebow for a headgear. A, Preformed facebows are supplied in a variety of inner bow sizes and usually also have an adjustment loop as part of the inner bow. The inner bow should fit closely around the upper arch without contacting the teeth except at the molar tubes (within 3 to 4 mm of the teeth at all points). A simple method for selecting the appropriate size is to fit the bow to the pretreatment maxillary cast. B, After the bow is placed in one molar headgear tube, the rest of the facebow is examined to see how it fits relative to the other molar tube and the teeth. C, By adjusting the loops to expand or contract the inner bow and by bending the short portion of the bow that fits into the molar tubes and facial offsets, it is possible to make the bow passive and allow clearance from the teeth. It should be easy to insert and remove at this point. Then the inner bow must be expanded by 1 to 2 mm to keep the posterior teeth out of crossbite as anteroposterior changes are made. The extension of the inner bow out the end of the headgear tubes should be evaluated. Ideally the end of the inner bow would be flush with the end of the tube, but certainly there is no need for it to extend more than 1mm past the end of the tube. This limited extension will reduce tissue irritation in the distal portion of the buccal vestibule and friction during application and removal. D, The facebow should be adjusted so that the junction of the inner and outer bows rests passively and comfortably between the lips. E, The outer bow should rest several millimeters from the soft tissue of the cheek. This adjustment must be checked both before and after the straps for the headcap or neckstrap are attached.
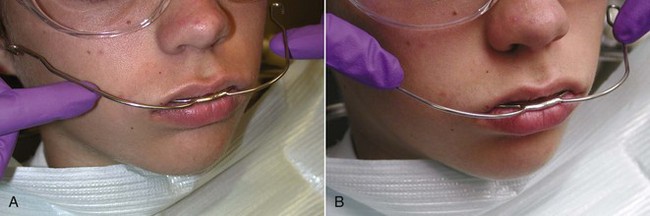
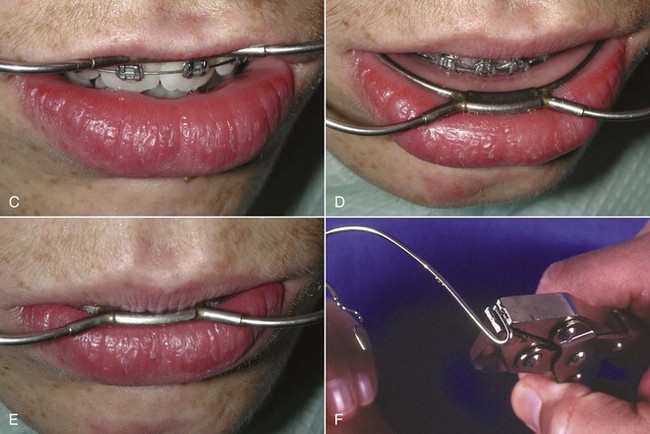
FIGURE 13-48 In order to determine the proper length needed for the outer bow, use the index fingers to apply pressure in the direction of the headgear selected. A, Pushing up and back in the direction of a high-pull headgear. B, Pushing down and back in the direction of a cervical headgear. As the fingers are moved from the anterior portion of the outer bow to the posterior portion, the position of the bow between the lips will change. C, If the bow moves up, the roots on the maxillary first molar will move distally. D, If the bow moves down on the lower lip the roots of the maxillary first molar will move mesially and the crown distally. E, If the bow does not move, the force is through the center of resistance of the maxillary first molar and the molar will move bodily and not rotate. These rules hold true for both high-pull and cervical-pull headgears. F, After the correct length is chosen and the outer bow cut with a pliers, a hook is bent at the end with a heavy pliers.
As a Class II molar relationship is corrected, the relative forward movement of the lower arch will produce a crossbite tendency unless the upper arch width is expanded. This must be taken into account from the beginning of treatment. The inner bow should be expanded by 2 mm symmetrically so that when it is placed in one tube, it rests just outside the other tube. The patient will need to squeeze the inner bow as it is inserted to make it fit the tubes, thus providing the appropriate molar expansion.
The appropriate headcap or neckstrap is fitted by selecting the appropriate size. A spring mechanism—not elastic bands or straps—is strongly recommended to provide the force. The springs deliver consistent forces that can be documented and easily adjusted. The spring attachment is adjusted to provide the correct force with the patient sitting up or standing—not reclining in the dental chair (Figure 13-49, A and B). It is usually a good idea to start with a low force level to acclimate the patient to the headgear and then gradually increase the force at subsequent appointments. Even if the correct force level is set at the first appointment, the forces will drop when the strap stretches slightly and contours to the patient’s neck. Once the forces are correct, the bow position must be rechecked since the pull of the straps and any adjustments to the inner or outer bow to improve fit and patient comfort can alter the previous bow position so that it needs adjustment.
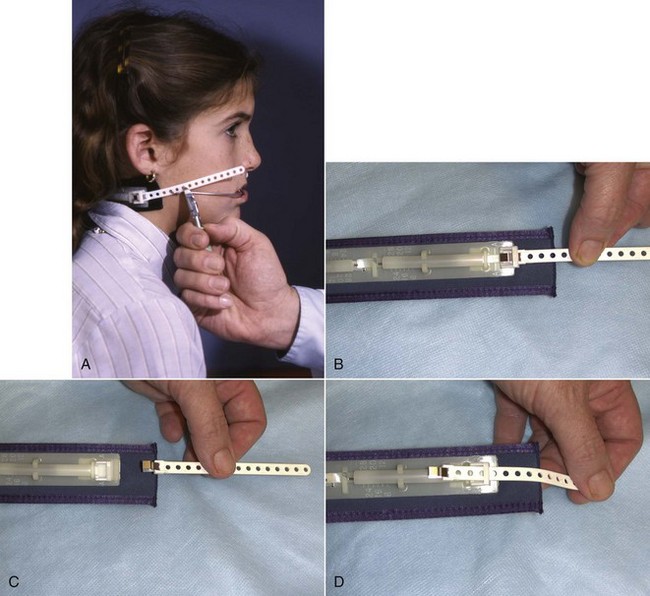
FIGURE 13-49 Adjustment of the neckstrap. A, The neckstrap is attached to the facebow and the proper force obtained from the spring mechanism by moving the hook to adjacent holes on the neckstrap. When the force is correct, the plastic connector is cut so that one extra hole is present in front of the correct hole. This provides a tab for the patient to grasp when placing the headgear. B, The spring mechanism delivers a predetermined force when the plastic connector is moved forward and aligned with a calibration mark. Here the rear of the tab is slightly anterior to the calibration mark. C, If the connector is stretched farther, such as it might be if someone grabbed the facebow and pulled on it, the plastic connector strap will release, preventing the bow from springing back into the patient’s face and causing injury. D, The connector can be reassembled by threading it through the back of the safety release.
The child should place and remove the headgear under supervision several times to be certain that he or she understands how to manipulate it and to ensure proper adjustment. Most headgear is worn after school, during relaxed evening hours, and during sleep. It is definitely not indicated during vigorous activity, bicycle riding, or general roughhousing. Children should be instructed that if anyone grabs the outer bow, they should also grab the bow with their hands. This will prevent breakage and injury. The headgear straps must be equipped with a safety-release mechanism (Figure 13-49, C and D) to prevent the bow from springing back at the child and injuring him or her if it is grabbed and pulled by a playmate. Severe injuries, including loss of sight, have occurred from headgear accidents of this type.43 In a review of commercially available headgear-release mechanisms that included 18 different designs, Stafford et al noted that almost all released at 10 to 20 pounds of force and concluded that the amount of extension before release occurred and the consistency of release were the most important variables from a safety perspective.44
Combined Vertical and Anteroposterior Problems
Some children exhibit a skeletal vertical deficiency (short face), almost always in conjunction with an anterior deep bite and some degree of mandibular deficiency and often with a Class II division 2 malocclusion. The reduced face height is often accompanied by everted and prominent lips that would be appropriate if the face height were normal.
Children with vertical deficiency can be identified at an early age. They tend to have a low mandibular plane angle (skeletal deep bite) and a long mandibular ramus. Growth is expressed in an anterior direction, with a tendency toward upward and forward rotation of the mandible. The challenge in correcting these problems is to increase eruption of posterior teeth and influence the mandible to rotate downward without decreasing chin prominence too much.
In a patient with Class II malocclusion, one way to correct such problems is with cervical headgear, taking advantage of the extrusive tendency of extraoral force directed below the center of resistance of the teeth and the maxilla (Figure 13-50). This effect and eruption of the lower molar can be accomplished using a headgear and a biteplate to open the bite. With no posterior occlusion, both upper and lower teeth can erupt.
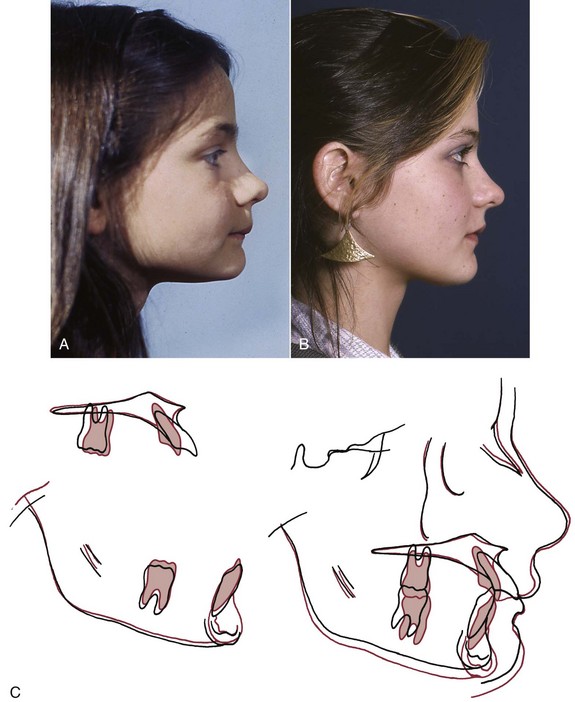
FIGURE 13-50 Increased vertical development in a child who initially had decreased lower anterior face height. A, Pretreatment profile. B, Posttreatment profile. C, Cephalometric superimpositions. This result was accomplished by increasing the maxillary molar eruption with a cervical-pull headgear, which resulted in downward movement of the mandible and improved facial esthetics. More eruption of the upper than the lower molar, however, can make it more difficult to obtain a good Class I molar relationship.
The other way is to use a functional appliance (usually with mandibular advancement, depending on the anteroposterior jaw relationship) that inhibits eruption of maxillary posterior teeth and allows free eruption of the mandibular posterior teeth (Figure 13-51). Because most short-face children also have a Class II malocclusion, it is important whether the eruption that occurs during treatment is primarily of the upper or the lower molars. Cervical headgear produces more eruption of the upper molars, while eruption can be manipulated with a functional appliance so that either the upper or lower molars erupt more. Class II correction, however, is easier if the lower molar erupts more than the upper, which means that—all other factors being equal—the functional appliance would be preferred.


FIGURE 13-51 Facial changes produced by functional appliance treatment in a boy with a short face, skeletal deep bite malocclusion. A and B, Age 10 prior to treatment. C and D, Age 12 after 26 months of treatment. Note the increase in anterior face height and decrease in the labiomental fold. E, Prior to treatment, note the gingival inflammation around the maxillary right central incisor resulting from palatal trauma from the deep bite. F, Deep bite bionator, constructed to allow eruption of lower posterior teeth and block eruption of incisors and upper posterior teeth. G, Dental relationships at the conclusion of phase 1 treatment, age 12. A second stage of treatment will be needed when the remaining succedaneous teeth erupt.
The treatment of these patients is a balance between the anteroposterior and the vertical reactions to treatment. One conservative option for a patient with a significant anteroposterior mandibular deficiency and reduced face height is to have growth expressed in an anterior direction first. To accomplish this, all vertical eruption is blocked while an appliance with the mandible advanced is used, which will create a posterior open bite when the appliance is not in place. When the Class II is corrected, the posterior bite block gradually is cut away while correct overbite is maintained anteriorly, so that slow eruption of posterior teeth back into occlusion can occur. This type of treatment places into sharp focus the interaction between the anteroposterior and vertical planes of space that must be addressed during growth modification treatment. The priority is placed on the most severe problem. It is remedied, and then the accompanying problems are addressed (Figure 13-52).
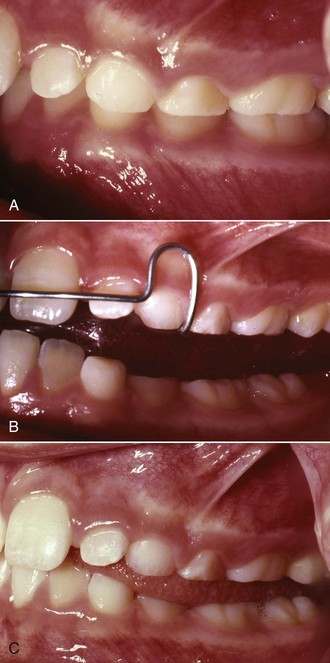
FIGURE 13-52 Posterior bite blocks can be used with any appliance that advances the mandible in an effort to limit posterior eruption and take maximum advantage of growth in an anteroposterior direction. A, The pretreatment occlusal relationships. B, When the mandible is advanced, bite blocks are incorporated to prevent posterior eruption. C, After a phase of appliance therapy that resulted in anteroposterior changes, there is a posterior open bite, which can be closed at that point by reducing the plastic bite blocks and allowing mandibular posterior eruption.
The fixed functional appliances tend not to be good choices in the mixed dentition treatment of short-face problems. Certainly, the Herbst, with its propensity to intrude the upper molars, is not an attractive option for younger patients needing increased vertical dimensions, even though the mandibular plane angle usually does not change very much in Herbst treatment.45
It is appropriate to remember that eruption occurs more rapidly in some patients than others and probably is affected by resting mandibular posture and freeway space, as well as the amount of appliance wear. Some short-face children show extremely rapid mandibular growth when the bite is opened and incisor overlap is removed, even with so simple an appliance as a biteplate. Unfortunately, this happens only occasionally, and except for the rare patients in whom there is no mandibular deficiency, posturing the mandible forward to allow the construction of a functional appliance is the better approach. Delivery and adjustment of a functional appliance for a vertically deficient patient is similar to that already discussed under mandibular deficiency.
Long Face/Open Bite
Excessive growth of the maxilla in children with Class II malocclusion has more of a vertical than an anteroposterior component (i.e., there is more excessive growth downward than forward), and if the maxilla moves downward, the mandible rotates downward and backward. The effect is to prevent mandibular growth from being expressed anteriorly. The ideal treatment for these patients would be to control all subsequent posterior vertical growth so that the mandible would rotate in an upward and forward direction (Figure 13-53). This could be accomplished by controlling all tooth eruption if there were adequate mandibular vertical ramus growth.
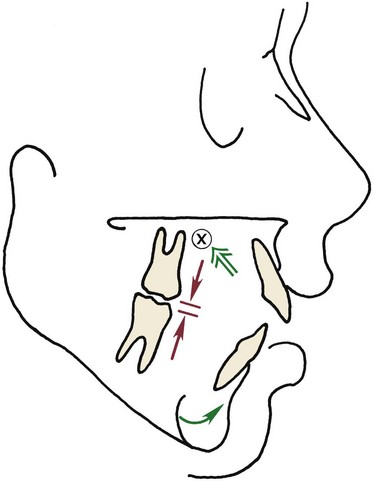
FIGURE 13-53 Mandibular-deficient children with excessive lower face height need treatment with an appliance that restricts posterior eruption and limits downward growth of the maxilla. This allows mandibular growth to be expressed anteriorly rather than vertically.
Unfortunately, vertical facial growth continues through adolescence and into the postadolescent years, which means that even if growth can be modified successfully in the mixed dentition, active retention is likely to be necessary for a number of years. Although dramatic improvement can be demonstrated in selected patients, probably the most sensible use of any of the appliances to control vertical skeletal and dental development is to use them for minor-to-moderate problems and intervene in adolescence toward the end of the growth period. This way, the problem is more manageable and treatment and retention are more circumscribed. Whatever the appliance and whenever the treatment started, retention would be critically important until vertical growth is essentially completed in the late teens or early 20s.
There are several possible approaches to the long-face pattern of growth in preadolescent children. In the order of their clinical effectiveness, they are:
1 High-Pull Headgear to the Molars
One approach to vertical excess problems is to maintain the vertical position of the maxilla and inhibit eruption of the maxillary posterior teeth. This can be attempted with high-pull headgear to the posterior teeth to be worn 14 hours a day with a force greater than 12 ounces per side (Figure 13-54). This does not control eruption of the lower molars, which can outstrip changes made by controlling the upper molar with the headgear.
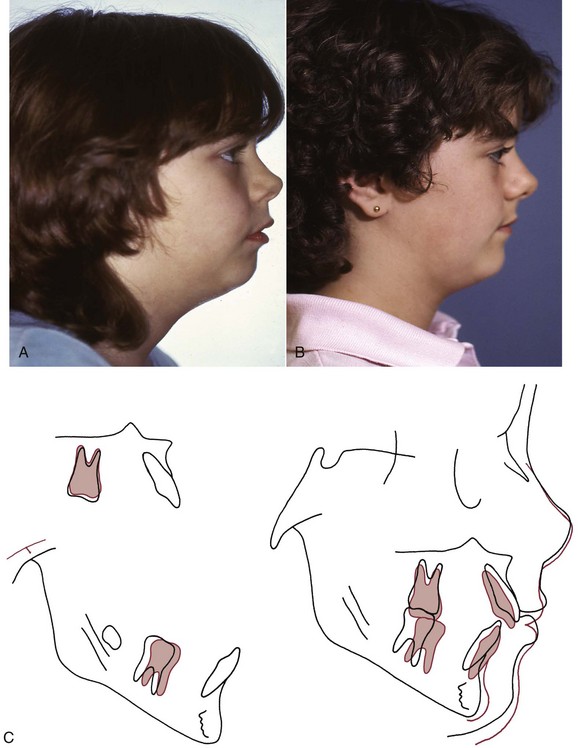
FIGURE 13-54 These photos show an excellent response to high-pull headgear for a patient with excessive lower face height. A, Pretreatment profile. B, Posttreatment profile. C, Cephalometric superimposition tracing. The cranial base superimposition shows that the maxilla and the maxillary teeth did not move inferiorly; as a result the mandible grew forward and not downward. The mandibular superimposition shows that the lower molar drifted forward into the leeway space. The incisor positions relative to the maxilla and mandible did not change.
2 High-Pull Headgear to a Maxillary Splint
Another headgear approach for children with excessive vertical development is the use of a plastic occlusal splint (Figure 13-55) to which the facebow is attached.46 This allows vertical force to be directed against all the maxillary teeth—not just the molars—and appears to have a substantial maxillary dental and skeletal effect with good vertical control. An appliance of this type would be most useful in a child with excessive vertical development of the entire maxillary arch and too much exposure of the maxillary incisors from beneath the lip (i.e., a long-face child who does not have anterior open bite). To achieve both skeletal and dental correction, the patient must be compliant throughout what can be a very long treatment period.
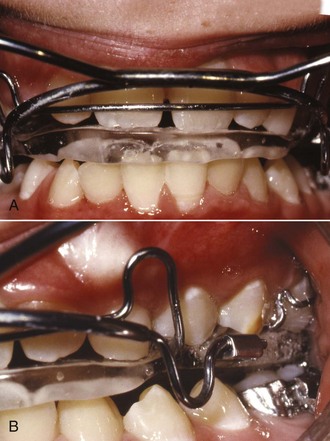
FIGURE 13-55 A and B, A plastic maxillary splint can be connected to a small conventional inner headgear bow and a high-pull headgear cap to deliver an upward and backward force to the entire maxilla. The splint limits dental eruption better than headgear just to the first molars.
Unfortunately, the maxillary splint allows mandibular posterior teeth to erupt freely, and if this occurs, there may be neither redirection of growth nor favorable upward and forward rotation of the mandible.
3 Functional Appliance with Bite Blocks
A more effective alternative is the use of a functional appliance that includes posterior bite blocks. The retraction force of the headgear is replaced by the somewhat lesser “headgear effect” of the functional appliance. The primary purpose of the appliance is to inhibit eruption of posterior teeth and vertical descent of the maxilla. The appliance can be designed with or without positioning the mandible anteriorly, depending on how much mandibular deficiency is present.
Regardless of whether the mandible is brought forward in the working bite, the bite must be opened past the normal resting vertical dimension if molar eruption is to be affected. When the mandible is held in this position by the appliance, the stretch of the soft tissues (including but not limited to the muscles) exerts a vertical intrusive force on the posterior teeth. In children with anterior open bites, the anterior teeth are allowed to erupt, which reduces the open bite, while in the less common long-face problems without open bite, all teeth are held by the bite blocks. Because there is no compensatory posterior eruption, all mandibular growth should be directed more anteriorly, at least to the extent that the overbite allows.
In the short term, this type of functional appliance treatment is effective in controlling maxillary vertical skeletal and dental growth.47 This tends to project mandibular growth anteriorly and helps to close anterior open bites (Figure 13-56). Because of the long period of continued vertical growth, if a functional appliance is used for the first phase of treatment, posterior bite blocks or other components (such as bone screws for skeletal anchorage) will be needed to control vertical growth and eruption during fixed appliance therapy and probably into retention (Figure 13-57). This is necessary because fixed appliances do not control eruption well and many biomechanical actions are extrusive.
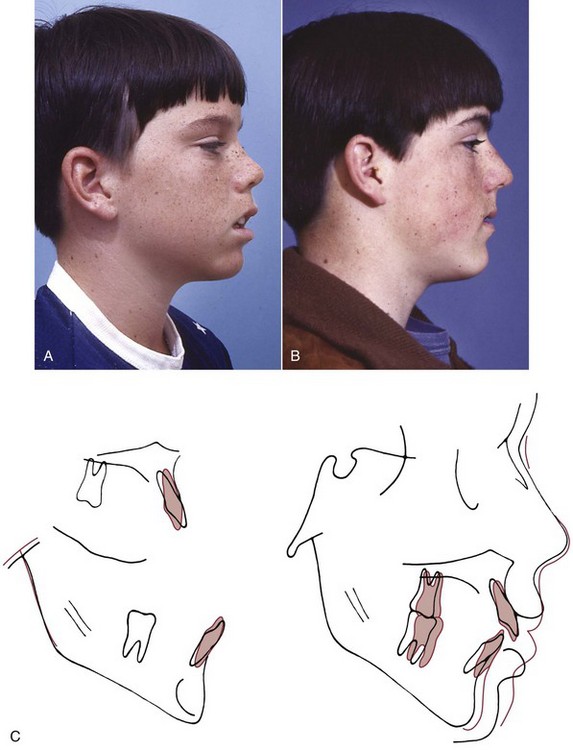
FIGURE 13-56 This patient demonstrates a good response to functional appliance treatment designed to control vertical development with posterior bite blocks in a child with excessive lower face height. A, Pretreatment profile. B, Posttreatment profile. C, Cephalometric superimposition tracing. Note that no posterior eruption occurred, and all mandibular growth was directed anteriorly. Face height was maintained, and anterior eruption closed the open bite. Maxillary and mandibular molar positions relative to their supporting bone were maintained.

FIGURE 13-57 During fixed appliance treatment, posterior eruption can be controlled by using removable posterior bite blocks to separate the posterior teeth beyond the resting vertical dimension. This creates an intrusive force on teeth in contact with the blocks, which is generated by the stretch of the facial soft tissues. The appliance is retained by clasps over the headgear tubes.
4 High-Pull Headgear to a Functional Appliance with Bite Blocks
The most aggressive approach to maxillary vertical excess and a Class II jaw relationship is a combination of high-pull headgear and a functional appliance with posterior bite blocks to anteriorly reposition the mandible and control eruption (Figure 13-58). The theory is that the extraoral force increases the control of maxillary growth and allows the force to be delivered to the whole maxilla rather than to simply the permanent first molars. The high-pull headgear improves retention of the functional appliance and produces a force direction near the estimated center of resistance of the maxilla (see Figure 13-46, C). The functional appliance provides the possibility of enhancing mandibular growth while controlling the eruption of the posterior and anterior teeth.
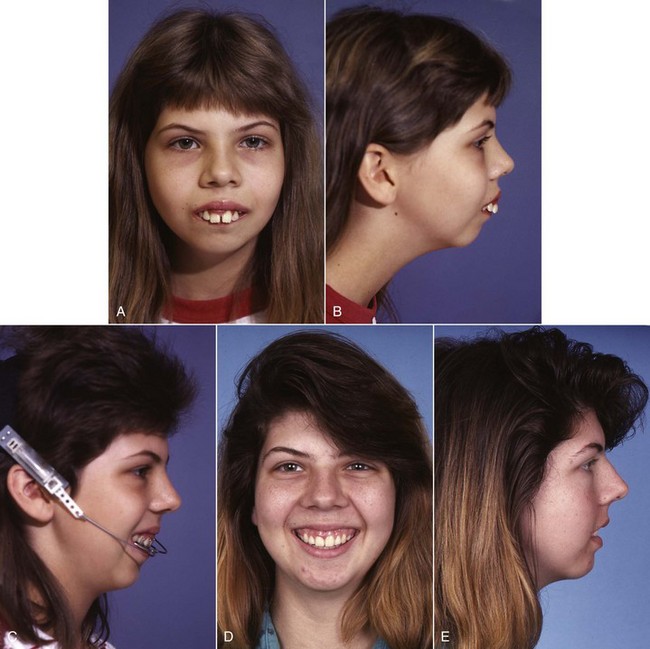
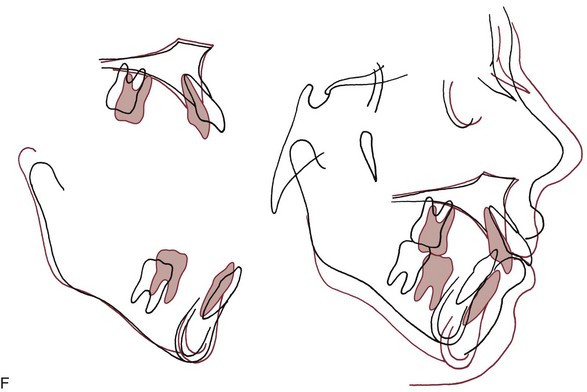
FIGURE 13-58 The maximum growth-modification approach to a severe long face, mandibular deficiency problem is high-pull headgear attached to a functional appliance with posterior bite blocks. A and B, Facial appearance before treatment. C, High-pull headgear with the facebow inserted into tubes in a functional appliance with bite blocks. D and E, Posttreatment facial appearance is improved but not ideal. F, Cephalometric superimposition showing continued downward movement of the chin but no increase in the mandibular plane angle. The major effect of treatment was retraction of the protruding maxillary incisors into a premolar extraction space; little if any modification of the growth pattern occurred.
In reality, the addition of headgear appears to provide little if any more vertical skeletal and dental control and only a modest anteroposterior maxillary skeletal impact. This benefit should be weighed against the effects of the simpler open bite functional appliance without headgear. A recent study with follow-up through a later stage of fixed appliance therapy concluded that there was so little skeletal impact of the headgear-functional appliance stage of treatment that it could no longer be recommended.48
Facial Asymmetry in Children
Although almost everyone has some facial asymmetry, asymmetric development of the jaws severe enough to cause a problem is relatively rare. Asymmetric deficiency in a child can be due to congenital anomalies (e.g., hemifacial microsomia) but usually arises as a result of a fracture of the condylar process of the mandible (Figure 13-59).49 The asymmetry in such cases is due to a restriction of growth after the injury—not the displacement of fragments that occurred at the time of injury (see Chapter 5). Asymmetric excess is due to hemimandibular hypertrophy, which rarely develops before adolescence and cannot be managed with growth modification techniques. Treatment usually requires surgery (see Chapter 19). Growth modification is a possibility for asymmetric deficient growth.
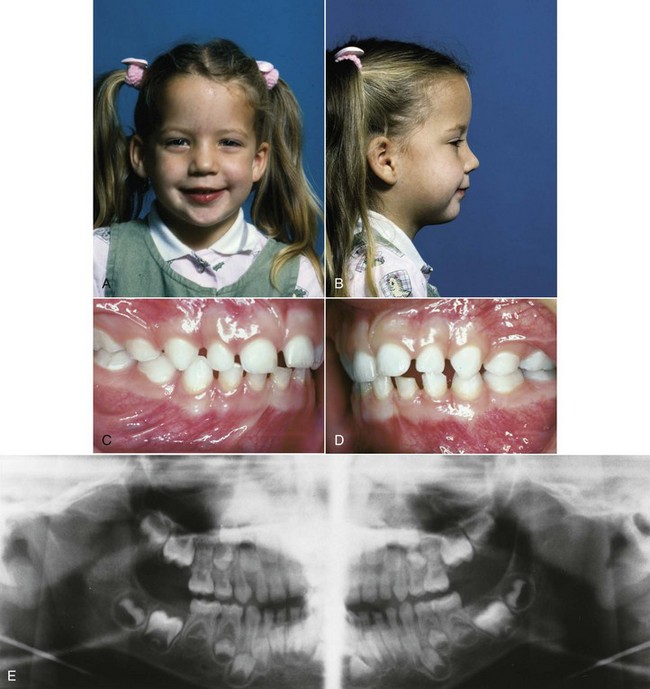
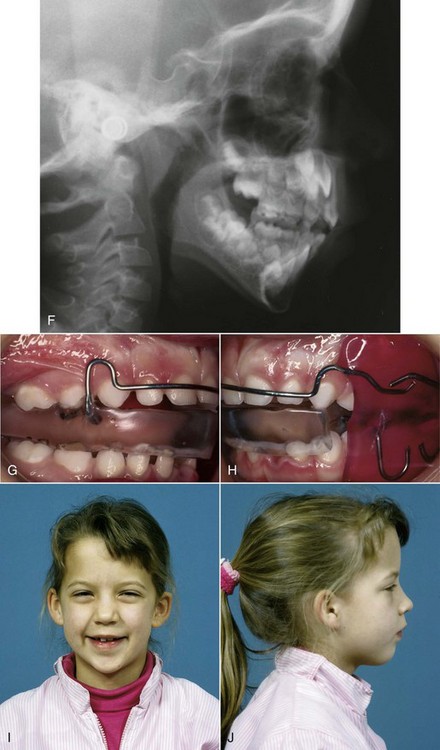
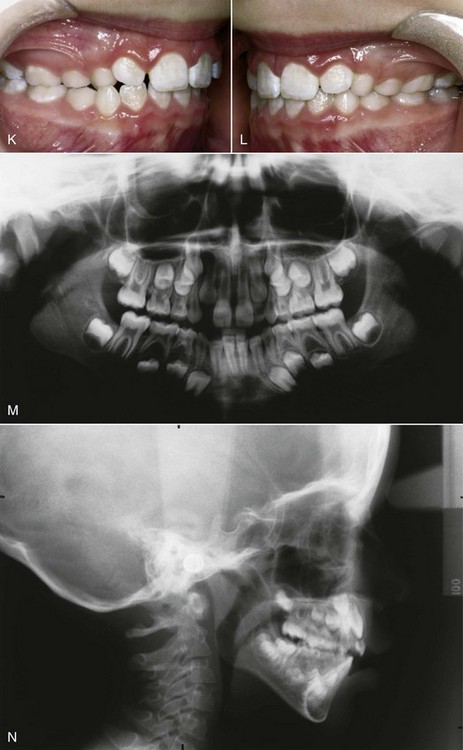
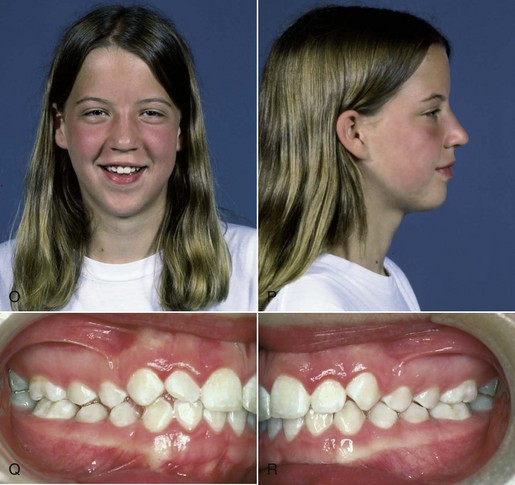
FIGURE 13-59 A and B, This 5-year-old girl’s family dentist noted her facial asymmetry, with the chin off to the left (she deviated even more on opening) and referred her for further evaluation. C and D, Her buccal occlusion was normal (Class I) on the right and Class II on the left. E, The panoramic radiograph showed the classic appearance of a unilateral condylar fracture. Note the normal condyle on the right and only a condylar stub on the left. The injury almost surely occurred at age 2 when she fell but was not diagnosed at the time. F, Note the two mandibular borders on the cephalometric radiograph due to the shorter ramus on the left. G and H, She was treated with a series of hybrid functional appliances, with buccal and lingual shields on the left, and a bite block anteriorly and on the right. The objective was to encourage mandibular growth and tooth eruption on the deficient left side and restrain eruption on the right. It is important to keep the tongue from between the teeth on the side where eruption is desired, thus the lingual shield on the left side (cannot be seen in the photos) was a critically important part of the appliance. I and J, Facial views 2 years later. K and L, Intraoral views 2 years later. Note the improvement in both facial symmetry and occlusion. Treatment with hybrid functional appliances was continued. M, Panoramic and (N) cephalometric progress views. Note the regeneration of the left condyle (seen clearly in the panoramic view) and reduction in the difference in height of the two mandibular rami, shown in the ceph. O and P, Facial and (Q and R) intraoral views at age 13, with nearly complete resolution of the facial asymmetry, although the mandible still deviates to the left on wide opening. Functional appliance treatment was discontinued at age 10, and there was no further orthodontic therapy.
When a condylar fracture is diagnosed in a child, maintaining function is the key to normal growth. Function does not mean simple opening and closing hinge movements but must also include translation of the mandibular condyles. Translation is necessary for normal growth in the long term and for regeneration and stretch of the associated soft tissues in the short term. Fortunately, most jaw fractures in preadolescent children can be treated with little or no surgical manipulation of the segments and little immobilization of the jaws because the bony segments are self-retentive and the healing process is rapid. Treatment should involve short fixation times (usually maintained with intraoral intermaxillary elastics) and rapid return to function. Open reduction of the fracture should be avoided. A functional appliance during the postinjury period can be used to minimize any growth restriction. The appliance is a conventional activator or bionator-type appliance that symmetrically advances the mandible to nearly an edge-to-edge incisor position. Using this appliance, the patient is forced to translate the mandible, and any remodeling can occur with the mandible in the unloaded and forward position.
Many condylar fractures are not diagnosed at the time of injury, so when a child with asymmetric mandibular deficiency is seen, trauma is the most likely cause even if an injury is not reported. The key to establishing the prognosis for growth modification is the extent to which the affected side can translate. Even if the mandible deviates to the affected side on opening, reasonably normal growth is possible if some degree of translation occurs. Hybrid functional appliances (see Figure 13-59, G and H) offer a way to obtain more growth on one side than the other. Although these appliances may appear confusing, they are simply various components logically combined to achieve specific purposes for individual patients.
Surgical intervention in an asymmetry situation (or other facial growth problem) prior to adolescence has only one goal: to create an environment in which growth is possible. Therefore surgery is indicated only when abnormal growth is progressively making a problem worse, as in ankylosis that keeps one side from growing or too much growth at one condyle. For these patients, treatment with a hybrid functional appliance will be needed, possibly before surgery to decompensate the dental arches and certainly after surgery to correct the primary growth problem, decompensate the dental arches vertically, and guide function. Because of the complexity of treatment planning and the probability that surgery will also be needed, children with progressive deformities usually are better managed through a major medical center.
References
1. Borzabadi-Farahani, A, Borzabadi-Farahani, A, Eslamipour, F. An investigation into the association between facial profile and maxillary incisor trauma, a clinical non-radiographic study. Dent Traumatol. 2010;26:403–408.
2. Sandikcioglu, M, Hazar, S. Skeletal and dental changes after maxillary expansion in the mixed dentition. Am J Orthod Dentofac Orthop. 1997;111:321–327.
3. Adkins, MD, Nanda, RS, Currier, GF. Arch perimeter changes on rapid palatal expansion. Am J Orthod. 1990;97:10–19.
4. Kilic, N, Kiki, A, Oktay, H. Condylar asymmetry in unilateral posterior crossbite patients. Am J Orthod Dentofac Orthop. 2008;133:382–387.
5. daSilva Filho, OG, Villas Boas, M, Capelozza Filho, L. Rapid palatal expansion in the deciduous and mixed dentitions: a cephalometric evaluation. Am J Orthod Dentofac Orthop. 1991;100:171–181.
6. Petrén, S, Bjerklin, K, Bondemark, L. Stability of unilateral posterior crossbite correction in the mixed dentition: a randomized clinical trial with a 3-year follow-up. Am J Orthod Dentofac Orthop. 2011;139:e73–e81.
7. Chang, JY, McNamara, JA, Jr., Herberger, TA. A longitudinal study of skeletal side effects induced by rapid maxillary expansion. Am J Orthod Dentofac Orthop. 1997;112:330–337.
8. Reed, N, Ghosh, J, Nanda, RS. Comparison of treatment outcomes with banded and bonded RPE appliances. Am J Orthod Dentofac Orthop. 1999;116:31–40.
9. Leonardi, R, Sicurezza, E, Cutrera, A, et al. Changes of circumaxillary sutures in young patients treated with rapid maxillary expansion. Angle Orthod. 2011;81:36–41.
10. Akkaya, S, Lorenzon, S, Ucem, TT. Comparison of dental arch and arch perimeter changes between bonded rapid and slow maxillary expansion procedures. Eur J Orthod. 1998;20:255–261.
11. Geran, RG, McNamara, JA, Baccetti, T, et al. A prospective long-term study on the effects of rapid maxillary expansion in the early mixed dentition. Am J Orthod Dentofac Orthop. 2006;129:631–640.
12. McNamara, JA, Baccetti, T, Franchi, L, et al. Rapid maxillary expansion followed by fixed appliances: a long-term evaluation of changes in arch dimensions. Angle Orthod. 2003;73:344–353.
13. Schneidman, E, Wilson, S, Erkis, R. Two-point rapid palatal expansion: an alternate approach to traditional treatment. Pediatr Dent. 1990;12:92–97.
14. Levin, AS, McNamara, JA, Jr., Franchi, L, et al. Short-term and long-term treatment outcomes with the FR-3 appliance of Fränkel. Am J Orthod Dentofac Orthop. 2008;134:513–524.
15. Ulgen, M, Firatli, S. The effects of the Fränkel’s function regulator on the Class III malocclusion. Am J Orthod Dentofac Orthop. 1994;105:561–567.
16. Kim, JH, Viana, MC, Graber, TM, et al. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofac Orthop. 1999;115:675–685.
17. Westwood, PV, McNamara, JA, Jr., Baccetti, T, et al. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofac Orthop. 2003;123:306–320.
18. Vaughn, GA, Mason, B, Moon, HB, et al. The effects of maxillary protraction therapy with or without rapid palatal expansion: a prospective, randomized clinical trial. Am J Orthod Dentofac Orthop. 2005;128:299–309.
19. da Silva Filho, OG, Magro, AC, Capelozza Filho, L. Early treatment of the Class III malocclusion with rapid maxillary expansion and maxillary protraction. Am J Orthod Dentofac Orthop. 1998;113:196–203.
20. Shapiro, PA, Kokich, VG. Treatment alternatives for children with severe maxillary hypoplasia. Eur J Orthod. 1984;6:141–147.
21. Cha, BK, Choi, DS, Ngan, P, et al. Maxillary protraction with miniplates providing skeletal anchorage in a growing Class III patient. Am J Orthod Dentofac Orthop. 2011;139:99–112.
22. Sar, C, Arman-Özçırpıcı, A, Uçkan, S, et al. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofac Orthop. 2011;139:636–649.
23. Nguyen, T, Cevidanes, L, Cornelis, MA, et al. 3D assessment of maxillary changes associated with bone anchored maxillary protraction. Am J Orthod Dentofac Orthop. 2011;140:790–798.
24. Cevidanes, L, Baccetti, T, Franchi, L, et al. Comparison of two protocols for maxillary protraction: bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010;80:799–806.
25. Wells, AP, Sarver, DM, Proffit, WR. Long-term efficacy of reverse pull headgear therapy. Angle Orthod. 2006;76:915–922.
26. Sugawara, J, Mitani, H. Facial growth of skeletal Class III malocclusion and the effects, limitations, and long-term dentofacial adaptations to chin cap therapy. Semin Orthod. 1997;3:244–254.
27. Tulloch, JF, Proffit, WR, Phillips, C. Outcomes in a 2-phase randomized clinical trial of early Class II treatment. Am J Orthod Dentofac Orthop. 2004;125:657–667.
28. Cozza, P, Baccetti, T, Franchi, L, et al. Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofac Orthop. 2006;129:599.e1–599.e12.
29. O’Brien, K, Wright, J, Conboy, F, et al. Early treatment for Class II division 1 malocclusion with the twin-block appliance: a multi-center, randomized, controlled trial. Am J Orthod Dentofac Orthop. 2009;135:573–579.
30. Pancherz, H. The effects, limitations, and long-term dentofacial adaptations to treatment with the Herbst appliance. Semin Orthod. 1997;3:232–243.
31. Franchi, L, Baccetti, T. Prediction of individual mandibular changes induced by functional jaw orthopedics followed by fixed appliances in Class II patients. Angle Orthod. 2006;76:950–954.
32. Siara-Olds, NJ, Pangrazio-Kulbersh, V, Berger, J, et al. Long-term dentoskeletal changes with the bionator, Herbst, twin block and MARA functional appliances. Angle Orthod. 2010;80:18–29.
33. Pancherz, H, Malmgren, O, Hagg, U, et al. Class II correction in Herbst and Bass therapy. Eur J Orthod. 1989;11:17–30.
34. Oppenheim, A. Biologic orthodontic therapy and reality. Angle Orthod. 1936;6:69–79.
35. Kloehn, S. Guiding alveolar growth and eruption of the teeth to reduce treatment time and produce a more balanced denture and face. Am J Orthod. 1947;17:10–33.
36. Wieslander, L. The effects of orthodontic treatment on the concurrent development of the craniofacial complex. Am J Orthod. 1963;49:15–27.
37. Armstrong, MM. Controlling the magnitude, direction and duration of extraoral force. Am J Orthod. 1971;59:217–243.
38. Keeling, SD, Wheeler, TT, King, GJ, et al. Anteroposterior skeletal and dental changes after early Class II treatment with bionators and headgear. Am J Orthod Dentofac Orthop. 1998;113:40–50.
39. Baumrind, S, Molthen, R, West, EE, et al. Mandibular plane changes during maxillary retraction, part 2. Am J Orthod. 1978;74:603–621.
40. O’Brien, K, Wright, J, Conboy, F, et al. Effectiveness of early orthodontic treatment with the Twin-block appliance: a multicenter, randomized, controlled trial. Part 2: Psychosocial effects. Am J Orthod Dentofac Orthop. 2003;124:488–494.
41. Banks, P, Wright, J, O’Brien, K. Incremental versus maximum bite advancement during twin-block therapy: a randomized controlled clinical trial. Am J Orthod Dentofac Orthop. 2004;126:583–588.
42. Haralabakis, NB, Sifakakis, IB. The effect of cervical headgear on patients with high or low mandibular plane angles and the “myth” of posterior mandibular rotation. Am J Orthod Dentofac Orthop. 2004;126:310–317.
43. Chaushu, G, Chausu, S, Weinberger, T. Infraorbital abscess from orthodontic headgear. Am J Orthod Dentofac Orthop. 1997;112:364–366.
44. Stafford, GD, Caputo, AA, Turley, PK. Characteristics of headgear release mechanisms: Safety implications. Angle Orthod. 1998;68:319–326.
45. Ruf, S, Pancherz, H. The effect of Herbst appliance treatment on the mandibular plane angle: A cephalometric roentgenographic study. Am J Orthod Dentofac Orthop. 1996;110:225–229.
46. Orton, HS, Slattery, DA, Orton, S. The treatment of severe ‘gummy’ Class II division 1 malocclusion using the maxillary intrusion splint. Eur J Orthod. 1992;14:216–223.
47. Weinbach, JR, Smith, RJ. Cephalometric changes during treatment with the open bite bionator. Am J Orthod Dentofac Orthop. 1992;101:367–374.
48. Freeman, CS, McNamara, JA, Jr., Baccetti, T, et al. Treatment effects of the bionator and high-pull facebow combination followed by fixed appliances in patients with increased vertical dimensions. Am J Orthod Dentofac Orthop. 2007;131:184–195.
49. Turvey, TA, Ruiz, R, Blakey, GH, et al. Management of facial fractures in the growing patient. In: Fonseca RJ, Walker RV, Betts NJ, et al, eds. Oral and Maxillofacial Trauma. Philadelphia: WB Saunders, 2005.