Psoriasis – Epidemiology, pathophysiology and presentation
Definition
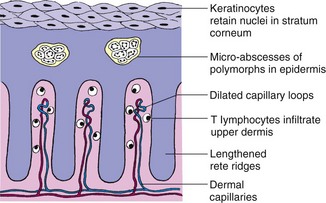
Psoriasis is a chronic, non-infectious, inflammatory dermatosis characterized by well-demarcated erythematous plaques topped by silvery scales (Fig. 1).
Epidemiology
Psoriasis affects 1.5–3% of the population in Europe and North America, but is less common in Africa, China and Japan. The sex incidence is equal. The condition may start at any age, even in the elderly. The two peaks of onset are the second to third and the sixth decades. It is unusual in children under 8 years old.
Aetiopathogenesis
Genetics
Inherited factors predispose to the development of psoriasis: genetic factors appear to be polygenic (p. 12). About 35% of patients show a family history, and identical twin studies show a concordance of 64%. There is a 14% probability that a child with one parent who has psoriasis will be affected, but this increases to 41% if both parents have psoriasis. There are strong correlations with the human leucocyte antigens (HLAs), e.g. HLA-Cw6. Environmental factors are thought to trigger the disease in susceptible individuals.
Epidermal kinetics and metabolism
Psoriatic lesions result from abnormal reactivity of skin T cells with alteration of the epidermal barrier and of inflammatory signalling. The number of cycling epidermal cells is increased seven-fold because of an increase in the basal and suprabasal proliferating cell compartment. The cell cycle time is not reduced. Growth factors, especially transforming growth factor-α, mediate these events. The upper dermal capillary plexus is expanded. At least nine possible chromosomal loci for genes linked to psoriasis have been found, e.g. PSOR1 on chromosome 6p.
Precipitating factors
A number of precipitating factors are associated with the disorder:
 Koebner phenomenon. Trauma to the epidermis and dermis, such as a scratch or surgical scar (p. 19), can precipitate psoriasis in the damaged skin (Fig. 2).
Koebner phenomenon. Trauma to the epidermis and dermis, such as a scratch or surgical scar (p. 19), can precipitate psoriasis in the damaged skin (Fig. 2).
 Infection. Typically, a streptococcal sore throat may precipitate guttate psoriasis.
Infection. Typically, a streptococcal sore throat may precipitate guttate psoriasis.
 Drugs. Beta-blockers, lithium and antimalarials can make psoriasis worse or precipitate it.
Drugs. Beta-blockers, lithium and antimalarials can make psoriasis worse or precipitate it.
 Sunlight. Exposure to sunlight can aggravate psoriasis (in about 6%), although it has a beneficial effect in the majority.
Sunlight. Exposure to sunlight can aggravate psoriasis (in about 6%), although it has a beneficial effect in the majority.
 Psychological stress. Stress can cause and exacerbate psoriasis.
Psychological stress. Stress can cause and exacerbate psoriasis.
Pathology
The epidermis is thickened, with keratinocytes retaining their nuclei (see Fig. 1). There is no granular layer, and keratin builds up loosely at the horny layer. The rete ridges are elongated, and polymorphs infiltrate up into the stratum corneum where they form micro-abscesses. Capillaries are dilated in the papillary dermis. T lymphocytes infiltrate the earliest psoriatic lesions.
Clinical presentation
Psoriasis varies in severity from the trivial to the life-threatening. Its appearance and behaviour also range widely from the readily recognizable chronic plaques on the elbows to the acute generalized pustular form. Psoriasis can be confused with other conditions (Table 1).
Table 1 Differential diagnosis of psoriasis
| Variant of psoriasis | Differential diagnosis |
|---|---|
| Plaque psoriasis | Psoriasiform drug eruption (due to beta-blockers) Hypertrophic lichen planus |
| Palmoplantar psoriasis | Hyperkeratotic eczema Reiter’s disease |
| Scalp psoriasis | Seborrhoeic dermatitis |
| Guttate psoriasis | Pityriasis rosea |
| Flexural psoriasis | Candidiasis of the flexures |
| Nail psoriasis | Fungal infection of the nails |
Presentation patterns of psoriasis include:
Plaque
Well-defined, raised disc-shaped plaques (Fig. 3) involving the elbows, knees, scalp, hair margin or sacrum are the classic presentation (see also p. 16; Fig. 1). The plaques are usually red and covered by waxy white scales which, if detached, may leave bleeding points. Plaques vary in diameter from 2 cm or less to several centimetres, and are sometimes pruritic.
Guttate
Guttate psoriasis is an acute symmetrical eruption (a ‘flurry’) of ‘drop-like’ lesions with little scale in the early stage, usually on the trunk and limbs. This form mostly occurs in adolescents or young adults and may follow a streptococcal throat infection (Fig. 4).
Flexural
This variant of psoriasis affects the axillae, submammary areas, groin and natal cleft (Fig. 5). Plaques are smooth and often glazed. It is mostly found in the elderly.
Localized forms
Psoriasis can also present in a number of localized forms:
 Palmoplantar pustulosis is characterized by yellow- to brown-coloured sterile pustules on the palms or soles (Fig. 6). A minority of subjects have classic plaque psoriasis elsewhere. It is most common in middle-aged women who are cigarette smokers, and it follows a protracted course.
Palmoplantar pustulosis is characterized by yellow- to brown-coloured sterile pustules on the palms or soles (Fig. 6). A minority of subjects have classic plaque psoriasis elsewhere. It is most common in middle-aged women who are cigarette smokers, and it follows a protracted course.
 Acrodermatitis of Hallopeau is an uncommon indolent form of pustular psoriasis affecting the digits and nails (see p. 31, Fig. 3).
Acrodermatitis of Hallopeau is an uncommon indolent form of pustular psoriasis affecting the digits and nails (see p. 31, Fig. 3).
 Scalp psoriasis may be the sole manifestation of the disease (see p. 31, Fig. 2). It can be confused with dandruff but is generally better demarcated and more thickly scaled.
Scalp psoriasis may be the sole manifestation of the disease (see p. 31, Fig. 2). It can be confused with dandruff but is generally better demarcated and more thickly scaled.
 Napkin psoriasis is a well-defined psoriasiform eruption in the nappy area of infants, few of whom later develop true psoriasis.
Napkin psoriasis is a well-defined psoriasiform eruption in the nappy area of infants, few of whom later develop true psoriasis.
Generalized pustular
Generalized pustular is a rare but serious and even life-threatening form of psoriasis. Sheets of small, sterile yellowish pustules develop on an erythematous background and may spread rapidly (Fig. 7). The onset is often acute. The patient is unwell, with fever and malaise, and requires hospital admission.
Nail involvement
Psoriasis affects the matrix or nail bed in 25–50% of cases (Fig. 8). Thimble pitting is the commonest change, followed by onycholysis (separation of the distal edge of the nail from the nail bed). An oily or salmon pink discoloration of the nail bed is seen, often adjacent to onycholysis. Subungual hyperkeratosis, with a build-up of keratin beneath the distal nail edge, mostly affects the toenails. Nail changes are frequently associated with psoriatic arthropathy. Treatment is often difficult.

Fig. 8 Nail involvement in psoriasis: pitting (left) and subungual hyperkeratosis with onycholysis (right).
Psoriasis
 Psoriasis affects 1.5–3% of western populations.
Psoriasis affects 1.5–3% of western populations.
 Inheritance is polygenic: 35% have a family history.
Inheritance is polygenic: 35% have a family history.
 Geneticists have identified loci for possible psoriasis genes, e.g. PSOR1 on chromosome locus 6p.
Geneticists have identified loci for possible psoriasis genes, e.g. PSOR1 on chromosome locus 6p.
 Peaks of onset are in the second to third and the sixth decades.
Peaks of onset are in the second to third and the sixth decades.
 The number of proliferating keratinocytes is increased seven-fold, but the epidermal cell cycle time is not shortened.
The number of proliferating keratinocytes is increased seven-fold, but the epidermal cell cycle time is not shortened.
 Presentation is variable: the chronic plague form affecting the elbows, knees and scalp is the commonest.
Presentation is variable: the chronic plague form affecting the elbows, knees and scalp is the commonest.
 Precipitating factors include streptococcal infection, drugs, sunlight, alcohol, smoking and psychological stress.
Precipitating factors include streptococcal infection, drugs, sunlight, alcohol, smoking and psychological stress.
 Nail involvement is found in 25–50% of cases and is difficult to treat.
Nail involvement is found in 25–50% of cases and is difficult to treat.