CHAPTER 21 Toothbrushing
Self-care or homecare refers to client behaviors undertaken to achieve, maintain, or promote health or oral health. Oral biofilm or plaque control is the daily removal of as much bacterial burden from the teeth, tongue, and adjacent oral tissues as possible to prevent or control oral diseases. Although 100% removal is not possible, the host can tolerate some plaque and inflammation.
Mechanical removal of oral biofilm via toothbrushing is the most widely accepted means for plaque control. Mechanical cleansing devices such as toothbrushes are indispensable because, to date, no chemotherapeutic agents totally prevent the formation of oral biofilm in the mouth.1
MANUAL TOOTHBRUSHES
The most commonly used device for removing oral biofilm, the manual toothbrush, is well designed to remove plaque from the facial, lingual, and occlusal tooth surfaces (Box 21-1). Although many features of toothbrushes and toothbrushing methods have been studied, numerous knowledge gaps make it difficult to make definitive toothbrush recommendations to clients.2-4 Compelling evidence is yet to emerge showing any individual manual toothbrush design to be consistently superior in removing plaque or preventing and controlling periodontal diseases; however, short-term studies have demonstrated promising results.5
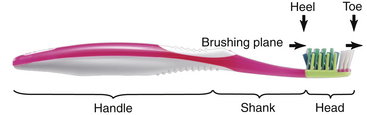
Parts of the Toothbrush (Figure 21-1)
Manual toothbrushes have several parts, as follows:
 Head—Contains the filaments (bristles) and is approximately 1 to 1¼ inches (25.4 to 31.8 mm) long and
Head—Contains the filaments (bristles) and is approximately 1 to 1¼ inches (25.4 to 31.8 mm) long and  to ⅜ inch (7.9 to 9.5 mm) wide. Head size is selected based on the size of the client's mouth rather than on the age of the client. The head should be large enough to remove plaque efficiently and small enough to facilitate access to all areas of the mouth. Contemporary toothbrush head designs are less rectangular and more tapered and oval in shape (Figure 21-2).
to ⅜ inch (7.9 to 9.5 mm) wide. Head size is selected based on the size of the client's mouth rather than on the age of the client. The head should be large enough to remove plaque efficiently and small enough to facilitate access to all areas of the mouth. Contemporary toothbrush head designs are less rectangular and more tapered and oval in shape (Figure 21-2). Handle—Used for grasping the toothbrush by the hand during use; may be aligned in a straight plane with the toothbrush head or angled like a dental mirror, curved, or offset. Consumers should select their preferred handle shape, that is, one that is comfortable to grasp, durable, and lightweight.
Handle—Used for grasping the toothbrush by the hand during use; may be aligned in a straight plane with the toothbrush head or angled like a dental mirror, curved, or offset. Consumers should select their preferred handle shape, that is, one that is comfortable to grasp, durable, and lightweight.Toothbrush Filament Design
The toothbrush head contains tufts typically composed of nylon filaments rather than natural bristles such as boar's hair. Tufts are individual bundles of filaments secured in a hole in the toothbrush head. Number and length of filaments in a tuft, number of tufts, and arrangement of tufts vary with toothbrush designs (see Figure 21-2). Less common and more expensive to manufacture, in-mold tufting has filaments inserted individually into the head. The brushing plane (surface of the toothbrush head used for cleaning the teeth and tissues) may be flat with all of filaments the same length; bilevel, multilevel; rippled (see Figure 21-2); or crisscrossed with tufts angled in at least two different directions (Figure 21-3).

Figure 21-3 Crisscross bristle design of the Oral-B CrossAction Pro-Health toothbrush.
(Courtesy Procter & Gamble, Professional and Scientific Relations, Cincinnati, Ohio.)
Filament design is assumed to affect toothbrushing efficacy, particularly in difficult-to-access areas of the dentition such as the lingual, posterior, and interproximal regions. Evidence remains inconclusive regarding the superiority of any single bristle design. Dental professionals generally assert that toothbrush bristles should have rounded ends to prevent soft-tissue lesions, but this remains uncertain. Despite claims of end-rounding, many new toothbrush filaments have nonuniform characteristics.6 It is interesting to note that within a short period of use the sharp edges of nonuniform filament ends become rounded.6 Emerging research on tapered, conical, and feathered filaments shows positive findings in plaque removal in vitro.
It is often recommended that clients use toothbrushes with soft nylon filaments, in the belief that they are less traumatic to the oral tissues and remove as much or more plaque than hard toothbrushes. However, the influence of bristle stiffness on plaque removal and trauma remains unclear.2 Nylon toothbrush filaments have a range of diameters from 0.15 mm to 0.4 mm. Filament stiffness is primarily related to the filament's diameter and length, with shorter- and wider-diameter filaments resulting in a harder toothbrush. Traditionally most filaments have been 10 to 12 mm long. Many manufacturers vary the type, length, and diameter of the filaments within a single toothbrush head, further complicating the assessment of bristle characteristics.
Toothbrush Bristle Wear
Indications of a worn toothbrush are bristles that are splaying, bending, curling, spreading, or matting (Figure 21-4). Because a worn toothbrush is believed to reduce toothbrush efficacy, toothbrushes or power toothbrush heads should be replaced. Filament wear varies considerably with different individuals over time.7 Therefore rather than using the usual 2 to 3 months as an indicator for toothbrush replacement, clients should be educated about identifying the visible signs of worn filaments. Although it makes intuitive sense that worn toothbrush filaments would be less effective for dental cleansing than filaments in good condition, evidence supporting this assumption is limited and conflicting.7
POWER TOOTHBRUSHES
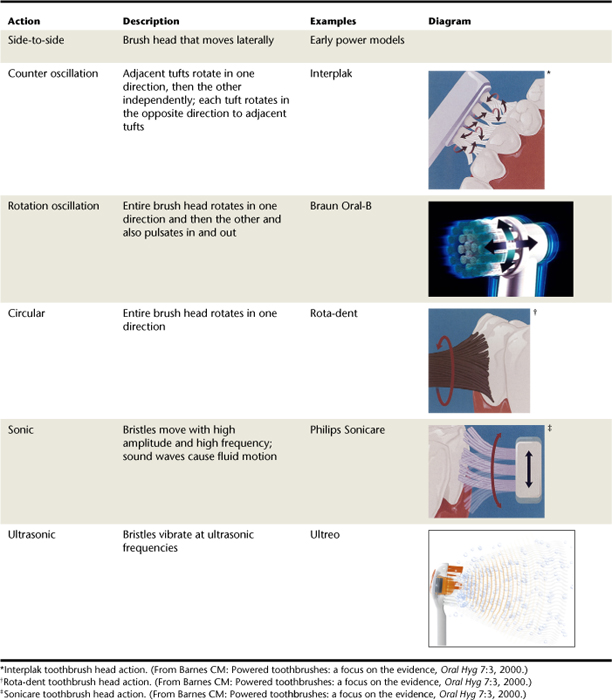
Rechargeable power toothbrushes, defined by their modes of action, are typically activated by electricity or battery (Tables 21-1 and 21-2). When used properly, both power and manual toothbrushes are effective in removing plaque and preventing and controlling gingival disease. In a Cochrane systematic review and meta-analysis (Box 21-2), power toothbrushes using several different modes of action were compared with a traditional manual toothbrush (rectangular head with a flat brushing plane); only the rotational oscillating design power brush significantly outperformed the manual toothbrush in plaque reduction (7%) and gingivitis reduction (17%) in both short- and longer-term studies.4 Because the power toothbrushes were clustered into groups by mode of action, subtle differences among toothbrushes could not be detected, and therefore the effectiveness of some individual power toothbrushes may have been masked by the ineffectiveness of others.4 The Cochrane analyses did not compare power toothbrushes with other power toothbrushes with regard to design.
Since the Cochrane reviews, additional studies comparing power toothbrushes with various manual toothbrushes or with other power toothbrushes have been inconclusive. There has also been research conducted with hybrid toothbrush designs (Figure 21-5), that is, combining design features from manual and power brushes, further complicating the evaluation of effectiveness. Battery-powered toothbrushes and less-expensive rechargeable models increase accessibility of power toothbrushing. However, these new devices require further empirical research to determine effectiveness.

Figure 21-5 Oral-B Dual Action brush head hybrid.
(Courtesy Procter & Gamble, Professional and Scientific Relations, Cincinnati, Ohio.)
To date, power toothbrushes have been shown to be safe and effective. Therefore a power toothbrush is suitable for almost any client (Box 21-3). Power toothbrushes have a high level of acceptance, and technologic advancements and decreasing costs are likely.
TOOTHBRUSHING INSTRUCTION
Toothbrushes require client-specific instructions on thoroughness, duration, frequency, method, and force to achieve an effective technique and adherence. Also, when giving instruction the dental hygienist considers client characteristics such as risk and susceptibility to disease, dexterity, personal values, and preferences. In addition, communication should be appropriate to the client's (caregiver's) age, language, educational level, culture, learning style, and readiness to adopt new behaviors.
Regardless of the toothbrushing method, the client is taught to clean the mouth and tongue thoroughly using a systematic approach and to understand the link among oral biofilm, oral and systemic diseases, and the importance of controlling plaque and inflammation. Gingival, periodontal, and dental assessment findings provide data to review with the client and correlate with the presence of oral biofilm. Quantitative plaque, gingivitis, and bleeding indices are used to improve client understanding, monitor self-care, motivate positive behaviors, and measure outcomes of care.
Toothbrushing Duration
To remove plaque, clients are taught to use a standardized sequence of toothbrushing for an adequate period of time. There are many possibilities for sequencing one's toothbrushing pattern, but the individual should be encouraged to select a logical sequence and to use it consistently to avoid omission of any area. This concept is particularly important to instill early in children.
Recent reports emphasized the importance of brushing time; 2 minutes is often the recommended duration. The average brushing time is ≤1 minute, but clients typically approximate their brushing times to be more thanf double that. Although research has yet to establish an ideal brushing time, the benefits of brushing longer than 2 minutes do not outweigh the potential risk of gingival damage. Risk of tissue damage with increased brushing time is difficult to evaluate because of variation in factors such as toothbrush design, force, and technique.
If the client will benefit from increasing brushing time, different teaching strategies can be used such as counting strokes before proceeding to the next area of the mouth or using an egg timer or a small hourglass. Newly designed power toothbrushes reflect current consensus on toothbrushing duration with built-in 2-minute timers to encourage clients to brush longer.
Toothbrushing Frequency
In addition to brushing duration and thoroughness, frequency must be considered. There is no standard recommendation for how many times per day persons should brush. Because gingival disease can occur after plaque removal is suspended for approximately 48 hours, toothbrushing should occur at least that often; however, more frequent toothbrushing is more socially acceptable.
Because most people cannot achieve 100% plaque removal in a single oral hygiene session, twice-daily brushing is recommended to control plaque biofilm and oral malodor (halitosis), the condition of having unpleasant breath. Brushing before bedtime and after a period of sleep should be encouraged (i.e., in the morning and at night). However, the decisions about when and how often to brush need to be made through a shared decision-making process based on clinical findings and client preferences.
Toothbrushing Force (Pressure)
Most literature on force applied during toothbrushing has focused on its association with damaging soft tissue (gingival abrasion and recession) and hard tissue (dental abrasion), and fewer researchers have examined the effect of force on plaque reduction. Some studies reveal that up to a point, increased force during toothbrushing will increase the amount of plaque removed; others have shown that decreasing force will increase plaque removal, and still others have found no correlation between force and efficacy.
Earlier concerns regarding excessive force leading to tissue damage with power toothbrushes have not been substantiated. Power toothbrush designs equipped with indicators or automatic shut-offs when excessive force is applied to the tooth surface contribute to improved safety. This technologic improvement is important because one's ability to perceive pressure with power toothbrushes is less acute than with manual toothbrushes. Evaluating if a client is exerting excessive toothbrushing force is challenging because of the multifactorial etiology of soft- and hard-tissue lesions.8 Therefore the dental hygienist takes many factors into consideration when determining if a client is brushing too aggressively. The dental hygienist makes client recommendations based on specific client assessment findings.
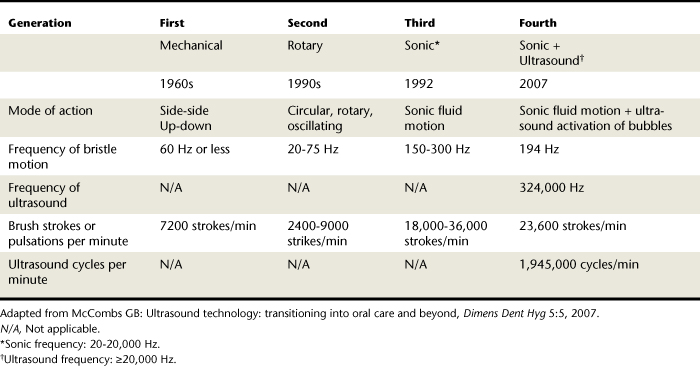
Toothbrushing Methods
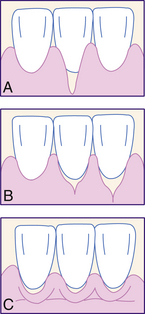
Table 21-3 summarizes key toothbrushing techniques and indications for use. In general, the Bass and Stillman methods of toothbrushing concentrate on the cervical portion of the teeth and the adjacent sulcular tissues. Both methods can be modified to add a roll stroke (i.e., modified Bass and modified Stillman). When this is the case, the toothbrush bristles are rolled occlusally to clean the entire facial and lingual surfaces after the cervical area is cleaned. The Bass method, because it emphasizes sulcular cleaning, is the most commonly recommended toothbrushing method (Figure 21-6). Over 90% of people use their “personal toothbrushing method,” typically a scrub technique. Although this method will remove oral biofilm from smooth tooth surfaces, it is considered to be less effective in other areas of the dentition and may be more injurious to the soft and hard tissues.
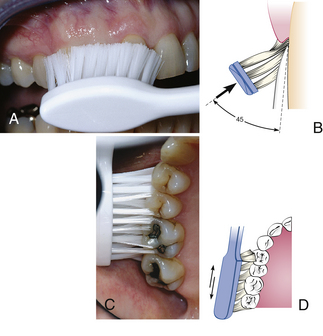
Figure 21-6 The Bass toothbrushing method. A, Proper intrasulcular position of brush in the mouth aims the filaments toward and into the gingival sulcus. B, Diagram shows the ideal placement with slight subgingival penetration of the filament tips. C, Place toothbrush so that filaments are angled approximately 45 degrees from the long axis of the tooth. D, Start at the most distal tooth in the arch and use a vibrating, back-and-forth motion to brush.
(B and D, From Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds: Carranza's clinical periodontology, ed 10, St Louis, 2006, Saunders.)
Research has not convincingly shown one method to be consistently superior.9 Specific claims about particular methods producing better outcomes surrounding gingival stimulation, preventing recession, or sulcular cleansing have not been substantiated in the literature.
Selection of the toothbrushing method should be dependent on client needs, dexterity, and preferences. Dental hygienists need to assess the client's oral hygiene, level of health or disease, and current toothbrushing practices to make meaningful recommendations. No toothbrushing method can adequately clean interproximal surfaces, and the client should be made aware that some means of interdental cleansing and use of an antimicrobial mouth rinse significantly improves oral biofilm and disease control.
For most manual toothbrushing techniques, the toothbrush can be grasped with a palm grasp and placed as follows:
 The brush head is moved from one group of teeth (two to three teeth) to the next by overlapping with the previously completed group.
The brush head is moved from one group of teeth (two to three teeth) to the next by overlapping with the previously completed group. On facial and lingual surfaces of posterior teeth the toothbrush head is positioned parallel to the arch.
On facial and lingual surfaces of posterior teeth the toothbrush head is positioned parallel to the arch. On anterior teeth the toothbrush head is placed parallel to the arch when the labial surfaces are brushed; on lingual surfaces the brush will likely need to be placed parallel with the long axis of the teeth (or vertically).
On anterior teeth the toothbrush head is placed parallel to the arch when the labial surfaces are brushed; on lingual surfaces the brush will likely need to be placed parallel with the long axis of the teeth (or vertically). On occlusal surfaces the toothbrush head is pressed firmly into the surfaces so that the filament ends can penetrate into the pits and fissures as much as possible, and a back-and-forth brushing stroke is activated. The brush is advanced section by section until all occlusal surfaces have been cleaned.
On occlusal surfaces the toothbrush head is pressed firmly into the surfaces so that the filament ends can penetrate into the pits and fissures as much as possible, and a back-and-forth brushing stroke is activated. The brush is advanced section by section until all occlusal surfaces have been cleaned.Toothbrushing techniques that require brush filament placement on an angle in relation to the teeth are more difficult for clients to achieve consistently. This challenge can limit toothbrushing effectiveness and client motivation. Therefore the dental hygienist observes and evaluates each client's toothbrushing skills so that problems can be identified, errors corrected, or more acceptable methods introduced. When modifying a client's toothbrushing technique, it is critical to demonstrate the new technique on a mouth model and then in the client's mouth. However, this does not replace the need to monitor the client actually performing the new technique and to provide feedback to ensure that the skill is acquired.
Clients also require instruction with power toothbrushes. Although these instructions vary with manufacturer and design, in general, power toothbrushing is relatively straightforward because the mechanism of action has removed the task of manipulating the toothbrush from the user. Most designs recommend that the client hold the brush head in place for a few seconds on each tooth or small group of teeth before guiding the brush head slowly to the next tooth or group of teeth and allowing the brush to do the work. The filaments will flare slightly while the brush is activated for cleansing the sulcus (Figure 21-7). The client must apply sufficient pressure, focus on the gingival margin, and keep the toothbrush engaged for a sufficiently long period of time before moving to the next area.

Figure 21-7 Counterrotational power toothbrush head placement.
(From Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds: Carranza's clinical periodontology, ed 10, St Louis, 2006, Saunders.)
A client's dexterity and vision may deteriorate with time, necessitating ongoing assessment and modifications to suggested methods and toothbrush selection. Over time at maintenance appointments, the reinforcement of instruction, observation of client's technique, and ongoing encouragement are effective means of achieving oral biofilm removal and adherence to professional recommendations.
SOFT- AND HARD-TISSUE LESIONS
As part of making toothbrushing recommendations, the dental hygienist assesses soft and hard tissues for damage from toothbrushing. Although the client may be removing oral biofilm adequately, he may also be causing trauma from the toothbrushing technique or toothbrush selection. Negative changes in tissues can be detected anywhere in the mouth, although they are often seen on the facial tooth surfaces at the gingival margin.
Soft-Tissue Lesions
Very vigorous toothbrushing in combination with a hard or stiff toothbrush has traditionally been associated with gingival abrasions and recession. However, the cause of gingival trauma is multifactorial, with toothbrushing technique having a less-certain influence.10 If observed, toothbrush trauma in the form of gingival abrasions can appear as redness, scuffing, or punctate lesions. These early abrasions can lead to more permanent soft-tissue lesions including gingival recession, clefts, or festooning (Figures 21-8 and 21-9). There is no doubt that toothbrushing is typically traumatic to soft tissues, with post-toothbrushing scanning electron microscopy showing moderate to severe gingival injuries. However, these microlesions are transient, and it is currently unknown how these short-term changes influence gingival recession in the long term.10
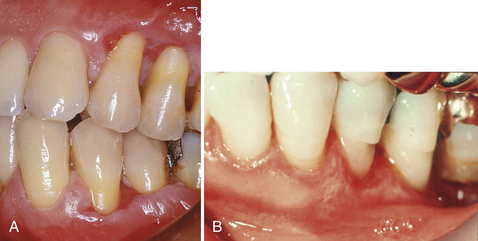
Figure 21-9 A, Trauma from vigorous toothbrushing with an abrasive dentifrice. Note trauma to gingival and root surface abrasion and gingival recession. B, Tooth abrasion attributed to long-term aggressive toothbrushing.
(From Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds: Carranza's clinical periodontology, ed 10, St Louis, 2006, Saunders.)
Although visible gingival abrasions are not a common clinical finding, gingival recession affects 80% to 100% of middle-aged Americans to some degree. Prevalence and severity of recession are dependent on increasing age, but younger individuals also can have aggressive levels of recession. Recession is a concern for several reasons, including its association with increased risk of dentinal hypersensitivity, loss of tooth support, root caries, and aesthetic dissatisfaction.
The cause of recession is multifactorial. Factors include the following:
 Toothbrushing factors (e.g., toothbrush bristle stiffness and toothbrushing technique, duration, and frequency)10
Toothbrushing factors (e.g., toothbrush bristle stiffness and toothbrushing technique, duration, and frequency)10The combined benefit of softer toothbrushes, less-abrasive toothpastes, and good toothbrushing technique may be having an overall positive impact on preventing the development of gingival lesions (see Chapter 23 on dentifrices).
Hard-Tissue Lesions
Hard-tissue lesions have been attributed to toothbrushing. Tooth abrasion, the wearing away of the tooth surface typically located around the cementoenamel junction (CEJ) (see Figure 21-9), has been believed to be caused by toothbrush trauma. Clinically, tooth abrasions appear as cervical notches surrounding the CEJ, increasing dentinal hypersensitivity and unpleasant aesthetics and possibly requiring restorations. Cervical defect shapes associated with toothbrushing include V-wedged, U-rounded, and combinations, with the former being most common; these defects change shape over time.
Tooth abrasions have been considered distinct from dental abfractions, similarly shaped cervical defects caused by excessive occlusal loading resulting in tooth flexure and subsequent loss of hard tooth structure at the CEJ. Data surrounding loss of cervical hard tissue are limited, but the literature available has not supported the distinction in causes between abrasions and abfractions. The term noncarious cervical lesion has been adopted, reflecting the multifactorial etiology of the condition.
Despite studies showing an association between hard-tissue wear and greater brushing frequency and duration, and the use of a scrubbing techniques, it is now recognized that toothbrushing itself has only minor influence on cervical wear.8 In vitro studies have demonstrated the contribution that toothpaste makes in the development of hard-tissue noncarious cervical lesions, with some laboratory studies showing no increase in abrasion when toothbrushing occurs without toothpaste. It is now believed that the act of the toothpaste being moved across the hard dental surface causes the cervical lesion over time (see Chapter 33).
Increased cervical wear also is associated with soft toothbrushes. This is believed to occur for the following two reasons:
 Increased flexing of softer filaments is associated with an increased contact area with the tooth surface.
Increased flexing of softer filaments is associated with an increased contact area with the tooth surface.Both factors result in a greater opportunity for tooth structure wear. Tooth abrasion is almost entirely linked to toothpaste use rather than to toothbrushing when considered on its own.11 Even with the use of toothpaste, toothbrushing for many years will produce minimal damage.
One exception to these assertions is in situations where the client has experienced demineralization as a result of chemical erosion. There may be a synergistic effect between toothbrushing and previously eroded hard tissue, resulting in more clinically significant noncarious cervical lesions than seen in the absence of dental erosion.
Tongue Cleansing
The dorsum of the tongue is a bacterial habitat. Tongue cleaning reduces the number of organisms, thereby controlling oral malodor, decreasing the opportunity for microorganisms to translocate, improving the client's taste perception, and contributing to overall oral cleanliness.
Although tongue scrapers and cleansers are marketed, tongue cleansing can be achieved with a manual toothbrush or a power toothbrush with a special head. A tongue cleaning device may be preferred to reduce the risk of stimulating the gag reflex.
If a toothbrush is to be used for tongue cleansing, the client does the following:
 Extends the tongue and, with the toothbrush head placed horizontally across the tongue and the bristles angled slightly posteriorly, draws the bristles forward with light pressure (Figure 21-10)
Extends the tongue and, with the toothbrush head placed horizontally across the tongue and the bristles angled slightly posteriorly, draws the bristles forward with light pressure (Figure 21-10)
Figure 21-10 Oral-B CrossAction Pro-Health with tongue cleaner on head of brush.
(Courtesy Procter & Gamble, Professional and Scientific Relations, Cincinnati, Ohio.)
Clients should be advised not to scrub the tongue with the toothbrush or a tongue cleaner because tissue trauma could result. Use of an antibacterial mouth rinse after mechanical tongue cleaning further improves tongue hygiene.
Toothbrush Contamination
Toothbrushes can be a mode of indirect transmission for pathogenic organisms. The toothbrush can act as a fomite (an inanimate object that houses and transmits potentially infectious agents). Microorganisms, either originating from the toothbrush user during toothbrushing or from the storage environment, can proliferate in toothbrush filaments and then be (re)introduced to the toothbrush user.12 Therefore it is biologically plausible that a pathogenic organism could infect the toothbrush user via the toothbrush.
Toothbrushes support a wide variety of microorganisms. Solid toothbrush designs have been shown to be less conducive to sustaining colonization of microorganisms than hollow designs. Similarly, microorganisms are less able to survive within individual in-mold filament placement in toothbrushes, but these are less commonly marketed than tufted designs. Toothbrush caps and holders may further encourage microbial growth and subsequent oral infection.12
If concern is warranted—for example, for immunocompromised persons—several alternatives are proposed for use:
 After-brushing antimicrobial sprays or rinses such as 0.12% chlorhexidine gluconate to disinfect the toothbrush12
After-brushing antimicrobial sprays or rinses such as 0.12% chlorhexidine gluconate to disinfect the toothbrush12 Before-brushing antimicrobial rinse to reduce the overall bacterial load within the oral cavity before the toothbrush is introduced
Before-brushing antimicrobial rinse to reduce the overall bacterial load within the oral cavity before the toothbrush is introduced Toothpastes such as those with strong surfactants to reduce the ability of microorganisms to survive on filaments
Toothpastes such as those with strong surfactants to reduce the ability of microorganisms to survive on filaments Toothbrushes (and interdental brushes) with chlorhexidine-coated filaments to reduce the ability of microorganisms to survive on filaments
Toothbrushes (and interdental brushes) with chlorhexidine-coated filaments to reduce the ability of microorganisms to survive on filamentsOverall, the literature is yet to compellingly demonstrate that intraindividual or interindividual contamination is a health risk for most people.
THE DENTAL HYGIENE PROCESS OF CARE AND TOOTHBRUSHING
Because oral hygiene instruction is part of the implementation phase of care, the dental hygienist will have completed the client's assessment including current self-care behaviors, type of toothbrush used, frequency and duration of toothbrushing, toothbrush replacement practices, level of satisfaction with tools and technique, and personal values and preferences. As part of oral hygiene instruction the client should be asked to demonstrate the toothbrushing method used, so the dental hygienist can observe the client's technique, skill, and dexterity.
Information about the client's self-care is linked with clinical and radiographic observations and allows the dental hygienist to identify the client's unmet human need deficits related to oral health (dental hygiene diagnoses), along with the corresponding causes, signs, and symptoms. Through this process the dental hygienist and client, in shared decision making, formulate a plan of care that includes self-care recommendations (Table 21-4; see Chapter 20).
TABLE 21-4 Shared Decision-Making Model
| Knowledge transfer | |
| Deliberation and decision making |
Oral biofilm may be present at the assessment appointment because the client has not been able to brush for several hours; conversely, absence of biofilm may be the result of thorough brushing immediately before the appointment rather than an indication of adequate daily plaque removal. Assessment of the soft and hard tissues for measurable signs of oral disease yields more valid findings surrounding the adequacy of self-care.
At times, clients avoid toothbrushing because of discomfort, but avoidance results in oral biofilm maturation. Examples of these clients include those with necrotizing ulcerative gingivitis, acute soft-tissue injuries, healing surgical site, or new dental appliances. In these situations, special toothbrushing instructions or mouth rinsing with 0.12% chlorhexidine gluconate is indicated.
Positive reinforcement of client attempts to incorporate positive oral health behaviors is provided throughout the process of care. Regardless of the client's situation, instruction, practice, and reinforcement are indicated at all appointments subsequent to the planning phase. Dental hygienists spend the least amount of educational time with clients for whom they hold the lowest expectations—that is, clients with the highest plaque levels. It is important that dental hygienists be aware of their personal biases and be accepting of all clients' personal abilities and values.2
CLIENT EDUCATION Tips
LEGAL, ETHICAL, AND SAFETY ISSUES
 It is the dental hygienist's ethical responsibility to use the highest level of professional knowledge, judgment, and ability and increase public awareness and understanding of high-quality oral health practices.
It is the dental hygienist's ethical responsibility to use the highest level of professional knowledge, judgment, and ability and increase public awareness and understanding of high-quality oral health practices. The dental hygienist has an ethical obligation to review scientific literature related to preventive interventions and to apply the knowledge to client care.
The dental hygienist has an ethical obligation to review scientific literature related to preventive interventions and to apply the knowledge to client care. Dental hygiene care requires allocation of time for instruction, repetition, reinforcement, and continual assessment of each client's oral health practices.
Dental hygiene care requires allocation of time for instruction, repetition, reinforcement, and continual assessment of each client's oral health practices. The legal standard of care requires that dental hygienists educate clients about oral self-care considering the client's age, language, culture, and learning style.
The legal standard of care requires that dental hygienists educate clients about oral self-care considering the client's age, language, culture, and learning style. Care plans should include evaluation of the presence and distribution of oral biofilm and its retentive factors and client self-care.
Care plans should include evaluation of the presence and distribution of oral biofilm and its retentive factors and client self-care.KEY CONCEPTS
 The manual toothbrush is the most commonly used device for removing oral biofilm from the facial, lingual, and occlusal surfaces.
The manual toothbrush is the most commonly used device for removing oral biofilm from the facial, lingual, and occlusal surfaces. A toothbrush that has a small enough head to adapt to all areas of the mouth with a comfortable handle designed to secure a good grasp is desirable.
A toothbrush that has a small enough head to adapt to all areas of the mouth with a comfortable handle designed to secure a good grasp is desirable. Damage to soft and hard oral tissues has a multifactorial etiology; although toothbrush selection and toothbrushing variables contribute to negative effects, dentifrice use and other factors are likely to be more influential.
Damage to soft and hard oral tissues has a multifactorial etiology; although toothbrush selection and toothbrushing variables contribute to negative effects, dentifrice use and other factors are likely to be more influential. Both manual toothbrushes and power toothbrushes have greater benefit when dental professionals provide advice and instruction in methods for using these devices.
Both manual toothbrushes and power toothbrushes have greater benefit when dental professionals provide advice and instruction in methods for using these devices. Power toothbrushes are as effective as manual toothbrushes; oscillating, rotating power toothbrush designs have been shown to be more effective than traditional manual toothbrushes in reducing plaque and gingivitis.
Power toothbrushes are as effective as manual toothbrushes; oscillating, rotating power toothbrush designs have been shown to be more effective than traditional manual toothbrushes in reducing plaque and gingivitis. Comprehensive toothbrush instruction includes toothbrush selection and replacement, toothbrushing method, evaluation of toothbrushing effectiveness, and tongue brushing.
Comprehensive toothbrush instruction includes toothbrush selection and replacement, toothbrushing method, evaluation of toothbrushing effectiveness, and tongue brushing. Evaluation of toothbrushing effectiveness includes observation of the client's toothbrushing, using disclosing agents to visualize and quantify plaque, and gingival evaluation for signs of inflammation; corrective measures are undertaken as needed.
Evaluation of toothbrushing effectiveness includes observation of the client's toothbrushing, using disclosing agents to visualize and quantify plaque, and gingival evaluation for signs of inflammation; corrective measures are undertaken as needed. Interdental cleaning, tongue brushing, and use of an antimicrobial agent should be planned along with toothbrushing instructions.
Interdental cleaning, tongue brushing, and use of an antimicrobial agent should be planned along with toothbrushing instructions.CRITICAL THINKING EXERCISES
Case Study: Mrs. Truman, a 65-year-old retired school- teacher, is being treated by the dental hygienist. Assessment findings reveal that the client has generalized heavy oral biofilm, gingival inflammation, and bleeding on probing. Early in the appointment Mrs. Truman said, “Lately my arthritis has been particularly bothersome in my hands, and I find it difficult to brush my teeth.” Proceed with your counseling of Mrs. Truman regarding her home care. Consider her age, language, educational level, culture, learning style, and readiness to adopt new behaviors. What type of toothbrush and toothbrushing method should be recommend for Mrs. Truman and why?
Role-Playing Exercise: Working in pairs, one student assumes the role of the dental hygienist and the other student acts as the client. The dental hygienist interviews the client about current homecare devices, behaviors, and techniques and provides client-specific education and feedback based on the evidence. Student pairs can use their dental models for demonstration purposes; or if in the clinical setting, demonstrate techniques intraorally. Students can then reverse roles so that both experience the roles.
1. Gurenlian J.R. The role of dental plaque biofilm in oral health. J Dent Hyg. 2007. 81:116
2. Asadoorian J. CDHA position paper on toothbrushing. Can J Dent Hygiene. 2006;40:232.
3. Brothwell D.J., Jutai D.K.G., Hawkins R.J. An update of mechanical oral hygiene practices: evidence-based recommendations for disease prevention. J Can Dent Assoc. 1998;64:295.
4. Robinson P.G., Deacon S.A., Deery C., et al. Manual versus powered toothbrushing for oral health. Cochrane Database Syst Rev. (2):2005. CD002281
5. Cugini M., Warren P.R. The Oral-B CrossAction manual toothbrush: a 5-year literature review. J Can Dent Assoc. 2006;72:323.
6. Jung M., Koçkapan C., Wetzel W.E. Bristle end rounding of manual toothbrushes and reproducibility of end rounding classification. Am J Dent. 2003;16:299.
7. Galgut P.N. The influence of toothbrush wear on the variables of plaque and gingivitis in clinical trials. J Dent Hyg. 2001;75:150.
8. Litonjua L.A., Andreana S., Cohen R.E. Toothbrush abrasions and noncarious cervical lesions: evolving concepts. Compend Contin Educ. 2005;26:767.
9. Poyato-Ferrera M., Segura-Egea J.J. Bullón-Fernández P: Comparison of modified Bass technique with normal toothbrushing practices for efficacy in supragingival plaque removal. Int J Dent Hyg. 2003;1:110.
10. Litonjua L.A., Andreana S., Bush P.J., Cohen R.E. Toothbrushing and gingival recession. Int Dent J. 2003;53:67.
11. Addy M., Hunter M.L. Can toothbrushing damage your health? Effects on oral and dental tissues. Int Dent J. 2003;53:177.
12. Mehta A., Sequeira P.S., Bhat G. Bacterial contamination and decontamination of toothbrushes after use. N Y State Dent J. 2007;73:20.
Visit the  website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..
website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..