Chapter 47The Thigh
 The Gluteal Syndrome
The Gluteal Syndrome
Pain that can be demonstrated with digital pressure along a line between the wing of the ilium and the greater trochanter of the femur was first recognized as a cause of lameness more than 50 years ago.1-3 Various aspects of the origin, diagnosis, and management of the syndrome have been appreciated since its initial recognition by Dr. Churchill and myself.1-5 The condition has also been referred to as sacrosciatic lameness or pelvic myositis. We prefer to use the term gluteal syndrome because we believe that there may be more than one abnormality that will result in this type of pain.
Gluteal syndrome has been diagnosed in most breeds and uses of horses. Standardbred (STB) racehorses seem to have the highest incidence, but it is not uncommonly seen in Thoroughbred (TB) and endurance racehorses. One risk factor for STBs is related to the more recent harness and race bike designs that tend to decrease the weight borne by the forelimbs while transferring weight to the hindlimbs. Gluteal syndrome has been diagnosed in horses that are used for hunting, jumping, and eventing.
Based on dissections of cadavers, the accessory head of the middle gluteal muscle was identified as the deep structure that best corresponds anatomically to the characteristic pattern of pain. This muscle originates on the concave surface of the wing of the ilium near a tuber coxae. At its caudal extent, the accessory head of the middle gluteal muscle forms a flat tendon that passes over the cranial aspect of the greater trochanter of the femur and inserts on the crest below it. The accessory head is directly related to other aspects of the middle gluteal and superficial gluteal muscles superficially and is important in propulsion of the hindlimbs6 (Figure 47-1).
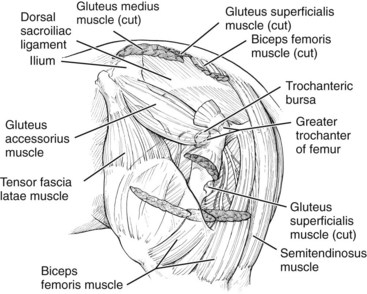
Fig. 47-1 Drawing of the anatomy of the lateral pelvic and proximal thigh regions showing the accessory head of the middle gluteal muscle, the most likely source of pain associated with gluteal syndrome. The tendon of the accessory head of the middle gluteal passes over the cranial portion of the greater trochanter, where there is a bursa. Inflammation in this region causes trochanteric bursitis.
The pathological process associated with the accessory head of the middle gluteal muscle is uncertain. It is known that in horses with some acute injuries a hematoma may form in the area between the ilium and the greater trochanter of the femur. Small, hypoechogenic areas may be demonstrated ultrasonographically in muscle tissue in the same area. In other horses, the muscle may become partially detached from the ilium. Horses with the latter condition develop a depression in the musculature caudal to a tuber coxae after the acute stage. In horses with chronic pain, the affected muscle mass may become very firm, presumably as a result of fibrosis. Post mortem evaluation of two horses with chronic refractory gluteal syndrome did not provide any conclusive information. Other potential changes such as fasciitis, gluteal tendonitis, or injury to one or more adjacent muscles have been considered. Whatever the cause, the source of pain is consistently confined to the area described.
To date, the most reliable, practical method of diagnosis is by careful, systematic physical examination of the area between the wing of the ilium and the greater trochanter of the femur with the horse standing on the limb. More specifically, the musculature should be palpated and examined for changes in resilience, swelling, or fibrosis. The position and outline of the tuber coxae should be evaluated. Next, gentle, deep pressure should be applied along the entire area described with the tips of eight digits (Figure 47-2). Initially, light digital pressure should be applied, but then the pressure is gradually increased to firm, deep pressure. The pressure is maintained briefly to evaluate the horse’s response. Finally the area caudal to the ilium, the central portion, and the caudal part of the accessory head of the middle gluteal muscle should be examined similarly. Each third of the area should be considered separately to determine whether the area is affected generally or whether the injury is confined to one or more sections. An unaffected horse will not respond to the examination of any of the areas. An affected horse leans away from the pressure while showing a reluctance to voluntarily bear full weight on the limb as long as the pressure is maintained. A positive response for this syndrome as described is specific and should not be confused with that for trochanteric bursitis (see Trochanteric Bursitis section).

Fig. 47-2 Careful palpation for pain is the only way to establish the clinical diagnosis of gluteal syndrome.
Most horses with acute gluteal syndrome tend to drag the toe of the affected limb on the ground at a walk. Horses with chronic gluteal syndrome do not drag the toe at a walk, but at a slow trot they break over on the inside of the toe and swing the leg medially and then laterally, finally landing on the outside branch or toe of the shoe. At this gait the lameness produced appears identical to that caused by trochanteric bursitis or tarsitis. When the horse trots, paces, or runs at high speed, the abnormality starts off as described, then the limb appears to tire and is carried more in abduction the further in the race or competition the horse proceeds. It appears that early in the race the horse is able to tolerate the gluteal pain and continue to use the limb for propulsion. However, with sustained speed or intensity of effort over distance, compensatory mechanisms within the limb fatigue as pain from the gluteal injury becomes overwhelming. At this point, a STB may make a break or freeze on a line; a TB may bolt or stop trying in the race; and a show horse may refuse to jump or crash when it tries. Many of these horses are believed to have a stifle problem because the quadriceps muscles fasciculate when they pull up. Others are believed to have exercise-induced pulmonary hemorrhage because they stopped like a bleeder, but no blood is seen endoscopically. Regardless, speed, intensity of work, and distance are key factors in how this problem affects an athletic horse. Some horses that accommodate to the injury or are treated and do not recover to total soundness can perform reasonably well at slower speeds or less intense work.
There is not a specific cause for gluteal syndrome. The onset is frequently directly associated with being cast in a stall, slipping or falling while playing in a paddock, or going down in a trailer or van and struggling to get up while the head is tied. Gluteal syndrome also develops when there is a chronic, preexisting problem in the distal aspect of the same limb, such as hock lameness, suspensory desmitis, or other problem that causes the horse to carry its weight on the toe at high speed. Slipping or losing footing on a soft racetrack or other muddy surface is also associated with development of the clinical signs.
Horses with this injury are best treated while in moderate, controlled exercise, regardless of the treatment approach. Rest alone, even for extended periods, has not been successful as a treatment. Several weeks of careful exercise management with repeated evaluations provide the best chance for a favorable response to treatment. Horses with acute injury, hemorrhage, and severe lameness should be rested until they are walking well and the seroma has resorbed before resuming exercise and treatment. Intramuscular injections of a counterirritant, acupuncture, and extracorporeal shock wave therapy are the best treatment options. At present, I still believe that injections of a counterirritant into the area of sensitivity yield the best results in the shortest time. The injection site is prepared with a surgical scrub followed by rinsing with 70% isopropyl alcohol. An injection grid is marked on the horse by drawing three lines in the wet hair over the accessory head of the middle gluteal muscle (Figure 47-3). One hundred milliliters of 2% iodine diluted in sesame oil solution is injected intramuscularly into 20 sites (5 mL/site) on and between the grid lines with a 4-cm, 19-gauge needle. If the pain is concentrated in the cranial or caudal third of the area between a tuber coxae and the ipsilateral greater trochanter of the femur, the injection sites can be limited to the cranial or caudal half of the area, respectively. After injection, daily moderate, controlled exercise is recommended beginning the day after injection for all horses. After injection, horses with acute or recent gluteal syndrome are walked and jogged for 3 weeks and then reexamined. If the lameness is improved but the area is still sensitive or if there has been no improvement, the injection is repeated in the same manner. Horses with chronic gluteal syndrome are walked and jogged for only 1 week before light training is resumed. Some horses respond dramatically to the treatment and appear to be pain-free within less than a week. The injury cannot heal within that time frame; therefore the temptation to resume full training too quickly must be resisted. When the treatment is successful and horses return to full work and racing, 10% to 20% may experience a recurrence of the problem. These horses generally respond well to an additional treatment as they did previously.
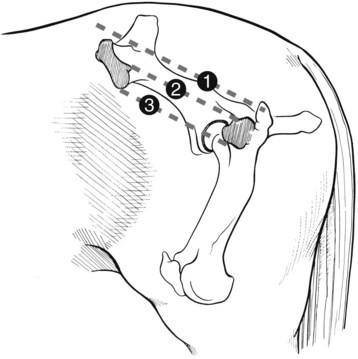
Fig. 47-3 Diagrammatic representation of the injection pattern for intramuscular injections of counterirritant solution to manage gluteal syndrome. The dashed lines (1, 2, and 3) provide a grid to guide injection into 20 sites.
Lameness that fails to improve after two or three injections at 3-week intervals is considered refractory to this mode of treatment. For these horses, I suggest that the trainer or owner try another form of treatment, such as therapeutic ultrasound, acupuncture, or shock wave therapy. Approximately 10% to 15% of horses do not respond to any mode of treatment and never recover from the injury. The prognosis is guarded initially for unilateral injury and poor if the problem is bilateral or if there is a chronic condition more distally in the same leg. In these horses with more complicated injuries, failure is related to the aggravating effect of each injury on the other.
Shoeing can be a factor in the management of the gluteal syndrome. Slipping on the racetrack, cross-country course, or show jumping arena is a major factor in development and recurrence of the injury. I recommend that TB racehorses that have or have had this condition be shod with block heels on both branches of each hind shoe. Calks applied near the end of both branches of the hind shoes during training and competition can be used in other types of horses.
 Trochanteric Bursitis
Trochanteric Bursitis
Pain elicited by firm digital pressure over the greater trochanter of the femur and the musculature immediately caudal to it is attributed to inflammation of the trochanteric bursa and is a cause of lameness in horses.1,2 Historically this condition has been referred to as trochanteric bursitis, trochanteric lameness, and whorl bone lameness.7 Anatomically the bursa is interposed between the flat tendon of the accessory head of the middle gluteal muscle and the cranial portion of the greater trochanter, which is covered with cartilage at this point. The tendon inserts on the crest below the greater trochanter (see Figure 47-1).7
Although confident, positive diagnosis is achieved by physical examination in almost all horses, a technique of injection of local anesthetic solution into the bursa has been described (see Chapter 10).8 The condition is relatively common for all breeds and uses of athletic horses and is generally considered to be a secondary problem. Trochanteric bursitis often is associated with tarsitis or other problems in the affected limb in which the horse lands on the toe. An additional cause that has been overlooked is that associated with overreaching with the hindlimbs to compensate for a chronic problem in the forelimbs. A horse that is chronically sore in front (e.g., navicular disease) will try to carry more of its weight on the hindlimbs by overextending the ipsilateral limb, which results in excessive strain on the tendon of the middle gluteal muscle. Wet, cold weather conditions appear to have a positive association with the incidence and response to treatment.
Trochanteric bursitis causes a gait abnormality that is similar to that produced by tarsitis or other sources of pain causing lameness in the distal aspect of a hindlimb. A horse with purely trochanteric lameness breaks over on the medial aspect of the toe; carries the leg medially, even crossing the midline; and then moves the leg laterally to land on the lateral aspect of the toe and branch of the shoe. The length of stride is shortened, and the hindquarters are carried toward the opposite side, which is sometimes described as “dog trotting” at a slow gait. Trochanteric lameness especially affects horses when they are racing around turns, jumping, circling, or performing precision dressage movements.
Trochanteric bursitis is generally a chronic condition that is diagnosed at the same time as a primary condition in the lower limb or ipsilateral forelimb. The more distal condition should be addressed before the bursitis is treated. Occasionally trochanteric bursitis is identified without an associated primary condition, or it may spontaneously resolve after correction of the associated primary lameness.
Rest is of no value in treating horses with trochanteric bursitis and may intensify the lameness when the horse returns to training. The most effective, practical treatment of trochanteric bursitis is injection of the soft tissues over and around the bursa with a counterirritant solution. The area for injection is prepared with a surgical scrub followed by rinsing with 70% isopropyl alcohol. Approximately 6 mL of 2% iodine diluted in sesame oil solution should be injected into eight sites with a 4-cm, 19-gauge needle (Figure 47-4). The horse should be maintained with mild, controlled exercise for 1 week before resuming normal work. Normally within 5 to 7 days after treatment the horse should become sound behind and no longer resent palpation over the bursa. Horses that require reinjection are more commonly encountered during cold, wet climatic conditions. The prognosis is good for obtaining a cure for trochanteric bursitis provided the associated primary lameness is corrected. Alternatively, solutions of a corticosteroid can be injected in the same manner. In my experience, injection of corticosteroids directly into the bursa is not necessary to alleviate the lameness.
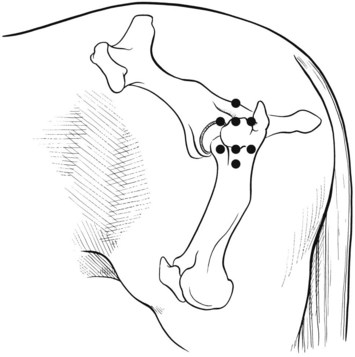
Fig. 47-4 Diagrammatic representation of the injection pattern (black circles) to manage horses with trochanteric bursitis.
Trochanteric bursitis has been addressed here as a performance-limiting condition in the athletic horse. Trochanteric bursitis that results from external trauma, infection associated with a wound, or a fracture of the greater trochanter of the femur is not discussed.
Fractures of the Femur
Fractures of the femur occur most commonly in foals and weanlings, although they may be seen in older horses. Most femoral fractures result from external trauma, such as a kick or fall with the limb in adduction or abduction. In young foals, fractures may be associated with breaking to lead. In most horses the traumatic incident is not witnessed, but the horse is found with an unstable, non–weight-bearing lameness in the affected hindlimb. Because of the energy required to fracture the femur of an adult horse, the fracture generally has a severely comminuted configuration. Although foals and weanlings most commonly acquire diaphyseal femur fractures, fractures involving the proximal or distal femoral physis are not uncommon. Salter-Harris type II distal femur fractures are most commonly seen in older weanlings and yearlings.
Diagnosis
In most horses, the diagnosis can be made after a brief physical examination. Femoral fractures result in an acute onset of severe lameness, with swelling in the area of the femur. Swelling occurs rapidly and is generally profound, particularly in adult horses with comminuted fractures. Degree of swelling can be used to differentiate fracture location (see Figure 5-12). Horses with pelvic fractures rarely develop swelling in both the medial and lateral aspects of the thigh, although horses with fractures of a tuber coxae may develop swelling of the proximal, lateral aspect of the thigh. Rotational instability is elicited when internal or external rotation is applied by grasping the proximal tibia and calcaneal tuber. Crepitation may be appreciated with manipulation of the limb. However, swelling and hemorrhage in the large muscle mass of the thigh may keep the fracture ends separated and make it difficult to elicit crepitus. The large muscle mass also makes open fractures uncommon. Swelling is most consistent with diaphyseal fractures, but it is often less obvious with proximal physeal fractures and minimally displaced distal physeal fractures. In most horses, the distance between reference points, such as the patella and the greater trochanter of the femur, is shortened because of the overriding of the fracture fragments that is caused by contraction of the quadriceps muscles. Foals with proximal physeal fractures may be able to bear some weight on the affected limb.
Radiological evaluation is required to obtain a definitive diagnosis and determine the severity of a femoral fracture (Figure 47-5). Radiography of horses larger than young foals requires use of general anesthesia unless the fracture is located in the distal aspect of the femur. Many small foals can undergo radiography safely when recumbent under heavy tranquilization or general anesthesia. Because induction and recovery of large yearlings and adults cannot be assisted sufficiently to prevent complications and discomfort, general anesthesia is contraindicated for assessment of unstable femur fractures. Ultrasonography can be used to confirm a displaced femoral fracture in a standing horse.
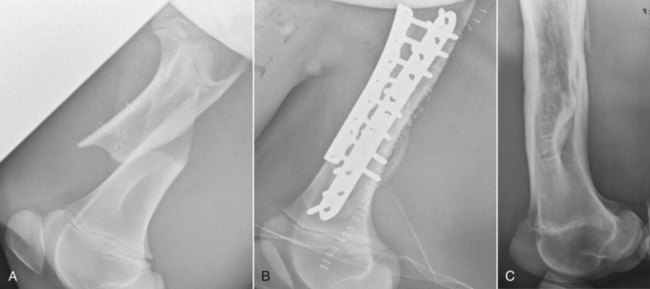
Fig. 47-5 Lateromedial digital radiographic images of a left femur. A, Initial view of a 2-month-old Thoroughbred filly with a simple, short-oblique, midshaft femoral fracture showing the typical cranioproximal displacement of the proximal fragment and caudodistal displacement of the distal fragment. The fracture was considered closed because there was no obvious communication between a superficial wound from the causative kick and the fracture site; the wound was stapled (stainless steel staples are visible) before admission. B, Postoperative image showing internal fixation using a lateral locking compression plate and a cranial limited-contact dynamic compression plate. A closed suction drain is visible. C, Radiographic image of the femur 2 years after injury and repair. The now 2-year-old filly was sound. The plates were removed 5 months after surgery; the fracture healed completely; and the stifle and hip (not shown) joints were radiologically normal.
Once the horse is in lateral recumbency with the affected limb down against the cassette and the opposite limb abducted, the x-ray beam should be directed from medial to lateral. Radiography of the diaphysis and proximal aspect of the femur requires a grid and high-capacity x-ray generator except for examination of small foals and the distal aspect of the femur of larger horses. Two exposures are generally required for the mediolateral images because of the variation in soft tissue mass around the distal and proximal aspects of the femur. Craniocaudal images are also required to assess the severity of the fracture and the degree of overriding. Evaluation of the proximal physis requires that the horse be positioned in dorsal recumbency with the cassette and grid under the coxofemoral area.
Case Selection for Treatment and Prognosis
The decision to treat horses with femoral fractures by surgical intervention depends on several variables. The size of the horse is the single most important consideration, regardless of fracture type. Successful surgical treatment of diaphyseal or proximal physeal fractures has been accomplished only in foals and small ponies.9 Distal physeal fractures have been successfully repaired in yearlings.10,11 However, adult horses or young horses weighing more than 200 kg (440 lb) with displaced diaphyseal fractures warrant humane destruction.12 Fracture location and configuration, soft tissue injury, temperament of the horse, client expectations, and economic considerations are other important determinants for case selection. Compromise of the vascular supply caused by the fracture, damaged major vessels, and swelling can result in failure because of necrosis of the distal aspect of the limb.13
Surgical techniques, complications, and the prognosis for horses with diaphyseal and proximal and distal physeal femoral fractures were reviewed.9,12,14 Of foals with diaphyseal fractures that were repaired with double plating, 50% of the fractures healed, and 75% of the horses were able to perform the intended use.15 The most common complications were seroma formation and infection. Foals with a successful outcome were younger than 3 months of age (see Figure 47-5). Additionally, an intact caudal cortex was considered necessary for a successful outcome. Newly designed implants such as the locking compression plate (LCP) may improve prognosis and make possible successful surgical repair in older horses or in those with comminuted fractures because stable anatomical alignment, exact contouring of the plate to bone, and compression of the plate to bone are not needed (see Figure 47-5).16 Successful outcome was achieved in two foals with open, comminuted femoral fractures repaired using two LCPs and a combination of locking and conventional cortex bone screws.16 Conservative management of horses with diaphyseal fractures can result in fracture healing. However, limb shortening, rotational deformity, and serious varus deformity in the contralateral limb are common complications of this approach. The prognosis of horses with distal fractures was more guarded than that for diaphyseal fractures because of the limited amount of bone for implant purchase. Success of the condylar screw plate for repair of a distal femur Salter-Harris type III fracture in a 2-year-old horse suggests this implant has application in repair of selected distal femoral fractures in horses.17 Conservative management of horses with distal fractures can result in a satisfactory outcome if the fracture is minimally displaced and stable.15
Although proximal femoral physeal fractures account for 16% of physeal fractures in the horse,18 sufficient reported results of surgical treatment to establish good prognostic information are lacking. Currently the prognosis for successful repair is guarded at best. Conservative management is unlikely to result in a comfortable horse. Unstable fixation, necrosis of the femoral head, and osteoarthritis of the coxofemoral joint are the more common complications associated with failure of surgical or conservative approaches.
Other less common types of proximal femoral fractures that cause less severe lameness in older horses include the third trochanter (see Chapter 50) and greater trochanter. Ultrasonography is helpful in confirming these fractures. Unless horses with these fractures have an associated wound or bone becomes sequestrated, they should be managed with stall rest.9 Stress fractures of the femur are rare but occasionally occur in the proximal cranial femoral cortex.
Gastrocnemius Muscle Injury
See Chapter 80 for a complete discussion of gastrocnemius muscle injury. Injury of the origin of the gastrocnemius can cause acute, severe hindlimb lameness in foals and adult horses. The diagnosis is straightforward when the reciprocal apparatus is disrupted, the most common clinical presentation in foals. Of six foals with gastrocnemius rupture, five had a history of dystocia and assisted delivery (three in a hip-locked position); four foals had complete disruption of the reciprocal apparatus and were unable to rise; life-threatening hemorrhage into the gastrocnemius muscle occurred in one foal, and concurrent perinatal diseases complicated management; and neither of the two foals discharged from the hospital were sound for athletic use.19 Successful restoration of the reciprocal apparatus after rupture of the gastrocnemius and superficial digital flexor muscles was achieved in a 6-month-old Warmblood filly using a modified Thomas splint–cast combination.20 The prognosis is grave when there is complete disruption of the reciprocal apparatus in adult horses. However, partial tearing at the origin of the gastrocnemius, musculotendonous junction, or more distally near or at the attachment on the calcaneus can occur and cause moderate hindlimb lameness that is difficult to diagnose. A peculiar gait is seen in some horses with gastrocnemius origin and tendon injury. ![]() Horses appear to have difficulty maintaining stability of the limb during late stance phase and when pushing off and exhibit marked internal rotation of the distal limb with lateral rotation of the point of the calcaneus.21 Some horses exhibit this type of hindlimb movement normally, but it is symmetrical and not accompanied by lameness. I have seen this peculiar gait in other horses with caudal thigh pain such as fracture of the tuber ischium with avulsion injury of the caudal thigh muscles. Gastrocnemius origin injury can be challenging to diagnose, but increased radiopharmaceutical uptake and bony proliferation were found in three of four horses,21 and ultrasonographic examination using comparative images of the contralateral limb is necessary, particularly in horses with injury of the more distal aspects of the gastrocnemius musculotendonous junction and tendon.
Horses appear to have difficulty maintaining stability of the limb during late stance phase and when pushing off and exhibit marked internal rotation of the distal limb with lateral rotation of the point of the calcaneus.21 Some horses exhibit this type of hindlimb movement normally, but it is symmetrical and not accompanied by lameness. I have seen this peculiar gait in other horses with caudal thigh pain such as fracture of the tuber ischium with avulsion injury of the caudal thigh muscles. Gastrocnemius origin injury can be challenging to diagnose, but increased radiopharmaceutical uptake and bony proliferation were found in three of four horses,21 and ultrasonographic examination using comparative images of the contralateral limb is necessary, particularly in horses with injury of the more distal aspects of the gastrocnemius musculotendonous junction and tendon.
Gracilis Muscle Injury
Although unusual, acute severe lameness and swelling of the medial thigh occur as a result of gracilis muscle injury. Gracilis muscle injury caused substantial hindlimb lameness in two barrel racing horses; the site of injury was confirmed using local infiltration into the affected muscles, and ultrasonographic examination confirmed injury.22 One horse developed an unusual gait consistent with fibrotic myopathy that resolved after resection of scar tissue.22 In this report, both horses returned to athletic use.22 Gracilis muscle injury is seen in polo horses (see Chapter 119, page 1164).
Other Thigh Injuries
Generalized muscle injury can cause acute swelling of the medial aspect of the thigh and pronounced lameness. Rarely, swelling, lameness, and fever are found in horses that develop abscesses in the medial thigh or inguinal region. Ultrasonographic examination for diagnosis, surgical drainage, and appropriate antimicrobial and antiinflammatory therapy are necessary. A horse with swelling of the thigh, fever, and sudden death was diagnosed with a dissecting aortic aneurysm.23 Large, dissecting hematomas from direct trauma may originate near the stifle and extend into the medial and sometimes the caudal aspects of the thigh and may require surgical drainage. Fractures of the tubera ischii, tubera coxae, and rarely luxation of the coxofemoral joint can cause swelling of the thigh. These conditions are discussed in detail in Chapters 49, 50, and 126.