Chapter 7 Movement
“The best time for examining a lame horse is while he is in action. An attendant should lead him on a trot, preferably on hard ground, in a straight line, allowing him freedom of his head, so that his movements may all be natural and unconstrained.”
It would be difficult to improve on Liautard’s insistence that the lame horse be examined during movement or his description for how it is best accomplished. Although all parts of the lameness examination are important, the key is the determination of the limb or limbs involved. Not all horses with musculoskeletal problems exhibit lameness that is perceptible under normal conditions, or even by use of high-speed or slow-motion cinematography, gait analysis, or other sophisticated imaging devices. Under most circumstances, however, lameness from pain or a mechanical defect in gait is discernible, and the essence of the lameness examination is to determine the source of the pain. This discussion includes relevant experimental findings to support clinical observations, but sometimes experimental findings are confusing rather than informative.
Gait
Gait, defined as the “manner or style of walking”2 or “the manner of walking or stepping,”3 is used to describe the speed and characteristics of a horse in motion. The natural gaits, those exhibited when a horse is free in a field, are the walk, trot, and gallop.4 The canter is a collected gallop. Other gaits including the pace, running walk, rack (a singlefoot or broken amble), fox trot, and amble are artificial gaits, although some pacers pace “free-legged” (without the use of hobbles) while on the track, either at a slow speed or racing speed, and occasionally a Standardbred (STB) paces free-legged in a field. In some instances a trotter switches from a trot to the pace, but this change usually is exhibited while the horse is performing at speed and may be associated with lameness or interference. Lame trotters usually “make breaks,” going off stride, by switching (breaking) from the trot to the gallop.
The term beat describes the number of foot strikes in a single stride cycle regardless of whether one or more feet strike the ground simultaneously. The following abbreviations are used for limbs: left forelimb (LF), right forelimb (RF), left hindlimb (LH), and right hindlimb (RH). The walk is a four-beat gait in which all four feet strike the ground independently without a period of suspension (in which no feet are on the ground). ![]() Depending on the part of the stride during which observations begin, the walk can appear to be lateral or diagonal. In general, in a lateral gait, both feet on one side strike the ground before the feet on the contralateral side. In a diagonal gait, one foot strike is followed by a strike of the foot located diagonal and contralateral to the initial foot (e.g., LF followed by the RH).
Depending on the part of the stride during which observations begin, the walk can appear to be lateral or diagonal. In general, in a lateral gait, both feet on one side strike the ground before the feet on the contralateral side. In a diagonal gait, one foot strike is followed by a strike of the foot located diagonal and contralateral to the initial foot (e.g., LF followed by the RH).
Lame horses should always be evaluated at the walk.![]() Stride length should be evaluated and compared with observations at the trot. Stride length and sequence of footfalls are easier to see while horses are walking than while they are trotting. Horses with hindlimb lameness may be examined for failure to track up.5 Horses normally track up, or overtrack. The hind foot is placed in or in front of the imprint of the ipsilateral front foot. Failure to track up usually is caused by hindlimb lameness or poor impulsion, and the hind foot imprint is seen behind that of the ipsilateral front foot.5 Although unusual, occasionally a horse will be observed to pace while walking, a finding that may indicate the presence of neurological disease. In breeds unassociated with the pace or similar gaits, young horses that pace should undergo careful neurological evaluation. Pacing while walking may be completely normal, and in older, “made” horses (horses that have already achieved an upper level of performance) the finding should not be overinterpreted.
Stride length should be evaluated and compared with observations at the trot. Stride length and sequence of footfalls are easier to see while horses are walking than while they are trotting. Horses with hindlimb lameness may be examined for failure to track up.5 Horses normally track up, or overtrack. The hind foot is placed in or in front of the imprint of the ipsilateral front foot. Failure to track up usually is caused by hindlimb lameness or poor impulsion, and the hind foot imprint is seen behind that of the ipsilateral front foot.5 Although unusual, occasionally a horse will be observed to pace while walking, a finding that may indicate the presence of neurological disease. In breeds unassociated with the pace or similar gaits, young horses that pace should undergo careful neurological evaluation. Pacing while walking may be completely normal, and in older, “made” horses (horses that have already achieved an upper level of performance) the finding should not be overinterpreted.
Backing is a diagonal, two-beat gait. ![]() Horses seldom back naturally, but backing commonly is required of horses during performance events, while exiting from a trailer, or while driving. Backing is useful during lameness examination to evaluate certain gait deficits, such as those associated with shivers, stringhalt, and neurological disease.
Horses seldom back naturally, but backing commonly is required of horses during performance events, while exiting from a trailer, or while driving. Backing is useful during lameness examination to evaluate certain gait deficits, such as those associated with shivers, stringhalt, and neurological disease. ![]()
The trot is a diagonal, theoretically two-beat gait, and diagonal pairs of limbs move simultaneously. ![]() The trot is theoretically a symmetrical gait, meaning both “halves” (beats) of the stride are identical, and at low speed in a sound horse, symmetry is likely achieved. However, at speed, perfect balance and fine management of weight (of the shoes) are necessary for a trotter to be perfectly symmetrical. There is a moment of suspension between impact of each diagonal pair of limbs. Some elite dressage horses do not have a two-beat gait but show advanced diagonal placement. This means that the hindlimb of a diagonal pair of limbs lands first and therefore is the only limb bearing weight. Hindlimb lameness is present in a higher percentage of horses that perform at speed at the trot compared with galloping horses because of differences in weight distribution in the trot and gallop. Compensatory lameness develops in the diagonal paired limb. LF lameness predisposes to RH lameness. Interference between limbs is more common in horses that trot at speed when compared with those that gallop. Likewise, hindlimb lameness is relatively common in dressage horses.
The trot is theoretically a symmetrical gait, meaning both “halves” (beats) of the stride are identical, and at low speed in a sound horse, symmetry is likely achieved. However, at speed, perfect balance and fine management of weight (of the shoes) are necessary for a trotter to be perfectly symmetrical. There is a moment of suspension between impact of each diagonal pair of limbs. Some elite dressage horses do not have a two-beat gait but show advanced diagonal placement. This means that the hindlimb of a diagonal pair of limbs lands first and therefore is the only limb bearing weight. Hindlimb lameness is present in a higher percentage of horses that perform at speed at the trot compared with galloping horses because of differences in weight distribution in the trot and gallop. Compensatory lameness develops in the diagonal paired limb. LF lameness predisposes to RH lameness. Interference between limbs is more common in horses that trot at speed when compared with those that gallop. Likewise, hindlimb lameness is relatively common in dressage horses.
The pace is a symmetrical, lateral, two-beat gait predominantly in STB racehorses and is characterized by movement of lateral pairs of limbs simultaneously (LH and LF; RH and RF), with a moment of suspension between lateral pairs. ![]() Pacers also have a high percentage of hindlimb lameness, but compensatory lameness usually develops in the lateral paired limb. RH lameness predisposes to RF lameness.
Pacers also have a high percentage of hindlimb lameness, but compensatory lameness usually develops in the lateral paired limb. RH lameness predisposes to RF lameness.
The gallop or run is a four-beat gait. In the gallop and the canter the horse leads with the LF or RF, the forelimb that strikes the ground last in the stride sequence. An unrestrained horse usually leads with the LF while turning to the left, or the RF while turning to the right. Fatigue also plays a role. A Thoroughbred (TB) racehorse racing counterclockwise leads with the LF on the turns but immediately after entering the stretch switches to the right lead. Failure to switch leads or constantly switching leads in the gallop or canter may reflect fatigue or lameness.
In a left lead gallop, the RH strikes the ground first, followed in sequence by the LH, RF, and LF, followed by a period of suspension. When a horse is on the right lead, the RF strikes the ground last, propelling the horse into the suspension phase of the stride. It is often assumed that a horse with RF lameness is reluctant to take the right lead. However, bone stress measured in the radius and the third metacarpal bone (McIII) is greater on the nonlead (trailing) forelimb, and thus a lame horse may change leads to protect the nonlead forelimb.6 Ground reaction forces (GRFs) are greater in the trailing (nonlead) forelimb, a fact that supports the clinical observation that horses with forelimb lameness may select leads to protect the lame forelimb. A horse with RF lameness may prefer the right lead, allowing the LF to assume the greater forces and bone stress.5
The canter (lope) is a three-beat gait. In left lead canter the RH strikes the ground first, then the LH and RF land simultaneously, followed by the LF and then a period of suspension. A horse reluctant to take a lead may be trying to compensate for hindlimb lameness. In the right lead the LH must absorb a considerable amount of concussion and then generate propulsive forces. Proneness of this limb to fatigue seems logical, but a consistent change in stride characteristics of fatigued horses to protect the LH was not seen.7 Although the LH strikes the ground first, stance time, flexion of the upper limb joints, and GRF are greater in the RH.5 It could be assumed that a horse lame in the RH would be reluctant to take the right lead and may prefer the left lead.5 Lead and stride characteristics of fatigued and lame horses are complex because of asymmetry of the gait, and forelimb and hindlimb problems could account for failure or reluctance to take a particular lead and inappropriate lead switching.
Young horses early in training or trained horses that are lame may exhibit a disunited canter. The horse may spontaneously change legs behind, but not in front. In changing from left to right lead canter, or vice versa, the forelimbs and hindlimbs should change simultaneously. Horses with back pain or hindlimb lameness may be reluctant to change leads, or may change in front but not behind.
The Lameness Examination: Which Gait Is Best?
The trot is the most useful gait to determine the location of the lame limb or limbs. Forelimb lameness in particular is difficult to observe at the pace, especially in horses that are led in hand. Lame trotters may pace, supporting the supposition that the pace is an easier gait in a lame STB. I have seen horses with severe forelimb lameness at the trot that looked barely lame when pacing.
Comparing Lameness Seen at the Walk and Trot
Although lameness score should be determined when trotting a horse (see later), it is useful to compare gait deficits at the walk and trot. In horses with forelimb lameness, an exaggerated head and neck nod may be observed while walking horses with upper limb lameness (genuine shoulder region pain, for instance), and, in fact, head and neck excursion may be more pronounced than that seen while the horse is trotting. Some horses may exhibit odd gait deficits while walking, but deficits may abate at the trot. Horses with rare upper forelimb pain from rib fractures or anomalies may manifest abduction of the forelimb during protraction at the walk but not the trot. ![]() The stance phase of the stride is relatively longer at the walk than at the trot. The deep digital flexor tendon and the collateral ligaments of the distal interphalangeal joint are stressed maximally with extension of the distal interphalangeal joint. Thus with severe injuries of either structure lameness may be more severe at the walk than at the trot because of greater extension of the distal interphalangeal joint associated with the relatively long stance duration.5 Horses with hindlimb lameness characterized by a shortened caudal phase of the stride at the walk but shortened cranial phase at the trot often have upper limb lameness, such as that caused by pelvic fractures or osteoarthritis of the coxofemoral joint or from severe pain originating from the foot. In general, horses that have limb flight characteristics that differ between walk and trot should be evaluated carefully because in my experience they often have bona fide pain originating from the upper limb or are affected with an unusual mechanical or neuromuscular deficit.
The stance phase of the stride is relatively longer at the walk than at the trot. The deep digital flexor tendon and the collateral ligaments of the distal interphalangeal joint are stressed maximally with extension of the distal interphalangeal joint. Thus with severe injuries of either structure lameness may be more severe at the walk than at the trot because of greater extension of the distal interphalangeal joint associated with the relatively long stance duration.5 Horses with hindlimb lameness characterized by a shortened caudal phase of the stride at the walk but shortened cranial phase at the trot often have upper limb lameness, such as that caused by pelvic fractures or osteoarthritis of the coxofemoral joint or from severe pain originating from the foot. In general, horses that have limb flight characteristics that differ between walk and trot should be evaluated carefully because in my experience they often have bona fide pain originating from the upper limb or are affected with an unusual mechanical or neuromuscular deficit.
Relevance of Lameness at a Trot in Hand
Is lameness seen at a trot in hand the same lameness that compromises performance at speed? Is the lameness seen at a trot in hand in a jumping horse the same problem that causes the horse to refuse fences? The answer is usually, but not invariably, yes. For instance, I have seen many STBs show subtle unilateral hindlimb lameness at a trot in hand, but when the horse was later examined at the track and hooked to a cart, pronounced contralateral hindlimb lameness was noted. Differences include the track surface, the act of pulling a cart, the additional weight of the driver, and a faster gait. Lameness often is evaluated on a smooth hard surface useful in exacerbating even subtle problems, but most horses perform on softer surfaces, when other problems may be apparent. More than one lameness problem may exist—one evident at a trot in hand and another while the horse is ridden or driven. Horses can show lameness from one problem when trotted in a straight line but lameness from an entirely different problem while being trotted in a circle. The answer to the first question is complex because performance itself entails the inextricably intertwined relationship between horse and rider or driver and the possible presence of compensatory and coexistent pain. Ideally, to evaluate the role of lameness on poor performance, horses would be evaluated at the speed, at the gait, and in the manner in which they perform, conditions that usually are not always possible to reproduce.
Horse Temperament and Lameness Examination
Safety of the handler, observers, and the horse must always be considered throughout a lameness examination, and with a difficult horse the examination may need to be modified, especially on cold, windy days. In some female horses and geldings, judicious use of the tranquilizer acetylpromazine (0.02 to 0.04 mg/kg intravenously [IV]) permits continuation of the examination. I avoid use of this tranquilizer in stallions, although the possibility of paraphimosis is remote. Low doses of sedatives such as xylazine can be used (0.15 to 0.30 mg/kg IV) in stallions or other horses but can produce mild ataxia. Detomidine may be a better choice than xylazine because the drug lasts longer, thus allowing diagnostic analgesic procedures to be performed.5
I try to avoid using tranquilization and sedation, although some clinicians use them frequently and report that lameness in most horses may be more pronounced and easier to observe. Mild muscle relaxation may reduce the tendency of the horse to guard the lame leg. Mild analgesic effects of sedatives may mask mild pain, and in racehorses care must be taken to avoid use of drugs that may cause a positive result in a drug screen. In big moving, exuberant Warmblood horses, especially dressage horses (particularly stallions), sedation may be essential to accurately assess lameness.5
Leading the Horse during Lameness Examination
The horse must be led with a loose lead shank so that it can move the head and neck freely. It is impossible to see a head nod in a fractious or excited horse that is held tightly. Use of a chain lead shank over the nose facilitates control but is resented by some horses, and use of a bridle with a lunge line attached may be preferable.5
Horses should move at a consistent speed, not too fast and not too slow. A lazy horse may need encouragement with a whip. Constantly changing speed can make assessment of lameness difficult, but occasionally, assessing a horse during deceleration may reveal useful information about the existence of subtle lameness![]() .5 A horse may have to be trotted up and down many times. It is sometimes useful for the examiner to lead the horse to assess subtle forelimb lameness, because gait abnormalities may become more obvious.
.5 A horse may have to be trotted up and down many times. It is sometimes useful for the examiner to lead the horse to assess subtle forelimb lameness, because gait abnormalities may become more obvious.
Surface Characteristics and Lameness Examination
The horse should be examined on a smooth, flat surface. I prefer a hard surface, such as pavement or concrete that creates maximal concussion and may exacerbate subtle lameness. However, the clinical relevance of mild lameness seen on hard surfaces, especially on turns, should not be overinterpreted. Many horses that are actively competing successfully show mild lameness on hard surfaces; it is important to understand that the horse does not perform on a surface of pavement, and foot strike patterns and gait could be much improved if the horse performs on firm but forgiving surfaces. Crushed rock, cobblestone, deep sand, or undulating grassy areas and potentially dangerous slippery surfaces should be avoided.
It is important that the surface be nonslip because some horses appear to lack confidence while moving on hard surfaces and alter the gait. In these situations, horses may shorten the stride for protection rather than from lameness.5 Horses with studs or caulks on the shoes may develop induced lameness unrelated to the baseline lameness when trotting on hard surfaces.5
Ideally the gait on hard and soft surfaces should be compared, to help differentiate soft tissue from bony problems. Horses with foot pain usually perform worse on a hard surface. Lameness from soft tissue injuries, such as suspensory desmitis or tendonitis, tends to be worse on soft or deep ground. To evaluate lameness during transition from a hard to a soft surface and vice versa, a horse can be examined while circling on a lunge line in an area where both surfaces coexist side by side.5 Care must be taken to prevent the horse from slipping during this examination.
Determination, Grading, and Characterization of Lameness
Six basic steps are necessary to determine, grade, and characterize lameness. The clinician should determine the following:
The primary or baseline lameness is the gait abnormality before flexion or manipulative tests are used. The practitioner attempts to abolish baseline lameness using analgesic techniques. Lameness in more than one limb may complicate determination of the worst affected limb. It is important to trot a horse even if it is quite lame at a walk, unless an incomplete or stress fracture is suspected. A horse may take a short step with a limb at walk, or can appear very lame, but trot reasonably soundly. Horses with scratches (palmar or plantar pastern dermatitis) or superficial wounds in the palmar or plantar pastern may appear quite lame at walk but trot relatively well. A STB pacer may walk extremely shortly both in front and behind but pace or trot without lameness. However, only the degree of lameness usually differs between a walk and trot. A horse may appear sound at walk and trot in hand, but lameness may be apparent trotting in a circle, in hand or on the lunge, or while being ridden. This lameness now becomes the baseline lameness, and it is under these conditions that the results of diagnostic analgesia should be evaluated. The clinician should try to recognize if the horse has bilateral forelimb or hindlimb lameness that manifests as shortness of stride or poor hindlimb impulsion, or if concurrent forelimb and hindlimb lameness are present. Moderate-to-severe hindlimb lameness can mimic ipsilateral forelimb lameness, although ipsilateral forelimb and hindlimb lameness also occurs. In these horses the veterinarian should perform diagnostic analgesia in the hindlimb first.
Compensatory Lameness
Compensatory (secondary or complementary) lameness results from overloading of the other limbs as a result of a primary lameness. It must be differentiated from the stride-to-stride compensation by a horse to avoid interference injury because of a gait deficit, or lameness, or to shift weight (load) during examination. A compensatory problem develops as the result of predictable compensation a horse may make over time for a primary lameness in a single limb. However, a horse may compensate for lameness in one limb by shortening the stride in another, a stride-to-stride change in gait that is not the result of lameness. For instance, in some trotters with severe LF lameness, reluctance to extend the LF may induce a compensatory shortening of the cranial phase of the stride in the LH limb, creating what appears to be a hike in the LH. If the veterinarian looks only at the hindlimbs, LH lameness may be diagnosed. A trotter performing at speed with LF lameness is likely to develop compensatory lameness in the RF or RH but not in the LH. However, the horse may appear to be hiking (lame) in the LH to avoid interfering with the LF. Elimination of obvious unilateral forelimb lameness usually resolves an ipsilateral pelvic hike. Most horses with pronounced forelimb lameness examined at a trot in hand will have a concomitant shortening of the cranial phase of the stride in the contralateral hindlimb, giving the false impression of coexistent lameness in this limb and vice versa. Experimental results appear to support this clinical impression. In 6 of 10 horses with stance phase forelimb lameness, compensatory movements of horses created a false lameness in the contralateral hindlimb (see following text).8 Once forelimb lameness is abolished using diagnostic analgesia, the shortened cranial phase of the stride in the contralateral hindlimb will abate.
It is often difficult to know which lameness came first, but it is important to understand how horses compensate for lameness and which limbs are at risk to develop compensatory problems. Compensatory problems range from obvious lameness to only mild palpable abnormalities that may still compromise performance. Several predictable patterns of compensatory lameness are possible; the most common is bilateral forelimb or hindlimb lameness. Horses with a specific lameness in one forelimb are at risk to develop the same condition in the opposite forelimb. This tendency may not always be compensation for the primary lameness but may reflect simultaneous injury or degeneration of bone or soft tissue of both limbs. Abnormal loading of forelimbs or hindlimbs, faulty bilateral conformation, and the same shoeing or foot conditions all likely contribute to bilateral, simultaneous lameness. In horses with bilateral lameness, eliminating lameness in one limb usually results in pronounced contralateral limb lameness. Bilateral lameness may affect both limbs equally, resulting in a short, choppy gait. ![]() The horse may be lame in one limb while being circled in one direction and lame in the contralateral limb in the opposite direction.
The horse may be lame in one limb while being circled in one direction and lame in the contralateral limb in the opposite direction. ![]()
Racehorses that gallop are most likely to develop compensatory lameness on the contralateral limb or the ipsilateral forelimb or hindlimb. A TB racehorse with a left metatarsophalangeal joint lameness is most likely to develop a similar problem in the RH but may also develop LF lameness. In a trotter the contralateral limb is most at risk, followed by the diagonal forelimb or hindlimb. If a trotter has a right carpal lameness, the left carpus should be examined carefully; compensatory lameness also may occur in the diagonal LH limb. In a pacer the ipsilateral forelimb or hindlimb should be considered after the contralateral limb. In a pacer with LH lameness the RH and LF are at risk.
The most common compensatory lameness is the same problem in the contralateral limb. However, suspensory desmitis is a common compensatory problem in both the contralateral and other limbs. In a TB racehorse or a jumper with LF lameness, RF suspensory desmitis is common. Primary RH lameness may result in suspensory desmitis in the RF. It is logical that soft tissue structures are particularly vulnerable to the effects of overload. Superficial digital flexor tendonitis may develop secondary to a primary problem in the contralateral limb. In trotters a common pattern is primary carpal lameness and compensatory osteoarthritis of the medial femorotibial joint in the diagonal hindlimb, or vice versa.
Compensatory lameness also can develop in the same limb. In horses with front foot lameness the suspensory ligament (SL) often is sore, and some horses have suspensory desmitis. In horses with lameness abolished by palmar digital analgesia, most with navicular syndrome, scintigraphic examination revealed increased radiopharmaceutical uptake (IRU) in the proximal palmar aspect of the McIII in 30% of horses, indicating possible abnormal loading of the proximal aspect of the SL (Figure 7-1).9 Complete resolution of lameness may not be achieved until high palmar analgesia is performed.
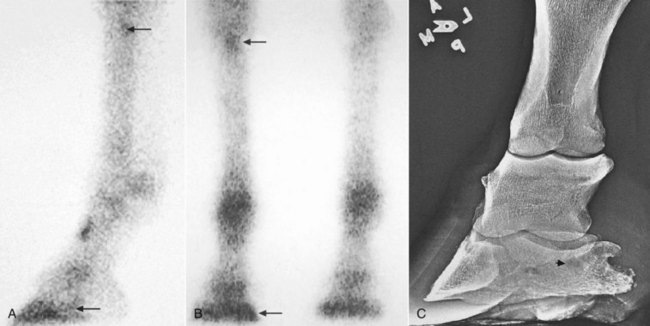
Fig. 7-1 A, Lateral delayed-phase scintigraphic view showing focal, mild increased radiopharmaceutical uptake (IRU) of the navicular bone (bottom arrow) and proximal aspect of the third metacarpal bone (McIII; top arrow). Normal modeling is seen in the dorsal aspect of the proximal phalanx. B, Dorsal delayed-phase scintigraphic image, and C, dorsomedial-palmarolateral oblique xeroradiographic image of a dressage horse with lameness abolished by palmar digital analgesia. IRU of the medial aspect of the distal phalanx (bottom arrow) corresponds to the area of subchondral radiolucency seen in the xeroradiographic image (C, arrowhead). Note the focal area of mild IRU involving the proximal aspect of the McIII (top arrow, A and B). Abnormal loading of the suspensory ligament may occur as a compensatory problem in some horses with navicular syndrome or other sources of palmar foot pain.
Horses with primary metatarsophalangeal joint lameness often have associated ipsilateral stifle pain, or vice versa.10 Determination of the primary site of lameness may be difficult without use of diagnostic analgesia and observing that blocking one site abolishes the majority of lameness. This phenomenon may be most common in STBs, but I have recognized it in all types of sport horses and in TB racehorses.
Supporting, Swinging, and Mixed Lameness
Lameness has classically been divided into three categories in an attempt to characterize the motion associated with the lame leg and to assign a cause to the lameness condition. These categories are described and discussed, but I firmly believe that adequate characterization of most lameness conditions is impossible and may be unnecessary.
Supporting limb lameness describes a lameness that results in pain during the weight-bearing phase of the stride. Most lameness conditions are of this type. Supporting limb lameness also has been referred to as stance phase lameness, but this term is inappropriate because the swing phase of the stride is also altered.
Swinging limb lameness describes lameness that primarily affects the way the horse carries the lame limb. However, most horses with painful lameness conditions alter the swing phase of the stride in a typical and repeatable fashion, and it is difficult to make a clear separation between supporting and swinging limb lameness. Swinging limb lameness should be a term reserved for mechanical defects of gait, such as fibrotic myopathy, upward fixation of the patella, stringhalt, or other lameness conditions causing a mechanical restriction of gait. ![]() In these horses, lameness is manifested in the swing phase of the stride with no apparent pain. Unfortunately, the term swinging limb lameness often is used inappropriately to describe the gait deficit in horses with painful, supporting limb lameness. Lameness associated with osteochondrosis of the scapulohumeral joint is often described as a swinging limb lameness because of a markedly shortened cranial phase of the stride. Dramatic improvement in the shortened cranial phase of the stride can be achieved by diagnostic analgesia, eliminating pain associated with lameness. Thus the gait deficit is the direct result of pain, and no clear differentiation between supporting and swinging limb lameness can be made. Horses with painful forelimb lameness almost always shorten the cranial phase of the stride, although perhaps not to the extreme as in a horse with authentic scapulohumeral joint lameness.
In these horses, lameness is manifested in the swing phase of the stride with no apparent pain. Unfortunately, the term swinging limb lameness often is used inappropriately to describe the gait deficit in horses with painful, supporting limb lameness. Lameness associated with osteochondrosis of the scapulohumeral joint is often described as a swinging limb lameness because of a markedly shortened cranial phase of the stride. Dramatic improvement in the shortened cranial phase of the stride can be achieved by diagnostic analgesia, eliminating pain associated with lameness. Thus the gait deficit is the direct result of pain, and no clear differentiation between supporting and swinging limb lameness can be made. Horses with painful forelimb lameness almost always shorten the cranial phase of the stride, although perhaps not to the extreme as in a horse with authentic scapulohumeral joint lameness. ![]() Horses with any painful hindlimb lameness consistently shorten the cranial phase of the stride, a reliable clinical indicator of which limb is affected, and when pain is abolished, the cranial phase (swing phase) of the stride improves (lengthens). Because the terminology is confusing and often erroneous, I prefer to avoid use of these terms and simply describe lameness as accurately as possible. For instance, describing a horse as grade 2 of 5 LF lame, with a marked shortening of the cranial phase of the stride reminiscent of other horses I have seen with shoulder region lameness, gives the most accurate and useful information.
Horses with any painful hindlimb lameness consistently shorten the cranial phase of the stride, a reliable clinical indicator of which limb is affected, and when pain is abolished, the cranial phase (swing phase) of the stride improves (lengthens). Because the terminology is confusing and often erroneous, I prefer to avoid use of these terms and simply describe lameness as accurately as possible. For instance, describing a horse as grade 2 of 5 LF lame, with a marked shortening of the cranial phase of the stride reminiscent of other horses I have seen with shoulder region lameness, gives the most accurate and useful information.
There is an erroneous tendency to equate a swinging limb lameness with one that is more evident when the lame limb is on the outside of a circle. Upper limb lameness is often presumed yet not confirmed by diagnostic analgesia. It is logical that if a horse is reluctant to swing a limb forward, the lameness may be most prominent when the lame limb is on the outside of a circle. However, many horses with painful weight-bearing lameness show more pronounced lameness with the limb on the outside of a circle, a finding that neither suggests that lameness originates from the upper limb nor indicates the presence of swinging limb lameness (see following text). The outer limbs must stretch further and cover a larger circumference circle than the inside limbs. Slight temporal differences in the stance and swing phases of the inside and outside limbs are necessary to maintain gait symmetry.5 Therefore the stance phase of the stride may be relatively longer for the inside hindlimb, resulting in extension of the fetlock for a longer time and stress on the suspensory apparatus, whereas for the outside hindlimb covering a longer distance in the same time, there may be greater extension of the fetlock for a relatively short time, but still with stress on the suspensory apparatus. Thus pain associated with hindlimb proximal suspensory desmitis is worse in some horses with the lame or lamer limb on the inside of the circle, whereas with others lameness is accentuated with the lame limb on the outside of a circle.
The results of cinematographic analysis of gait in lame horses seem to support reservation of the term swinging limb lameness for horses with authentic mechanical gait deficits, rather than those induced by painful lameness. In a horse with a supraglenoid tubercle fracture examined at a trot in hand, a marked decrease in the cranial phase of the stride (protraction) was observed, along with a marked head and neck nod. A markedly shortened stride could be equated with swinging leg lameness, but high-speed cinematography showed that the cranial and stance phases of the stride were shorter than in the sound limb.11 A horse with unilateral semitendinosus fibrotic myopathy had a shortened stride length and a shortened cranial phase of the stride, but the stance phase did not differ from that of the unaffected contralateral limb.12
In my experience, most lameness conditions can be considered mixed lameness, with changes in gait during weight bearing or the stance phase and during the swing phase of the stride. With the exception of mechanical defects in gait, I have not been able to categorize the clinical characteristics of most lameness conditions into swinging or supporting limb types. However, it has been suggested that swinging limb lameness is caused by muscle injury; supporting limb lameness is caused by bone, tendon, and ligament injury; and mixed lameness is caused by joint, tendon sheath, and periosteal injury.13 A shortened cranial phase of the stride is a common characteristic in forelimb and hindlimb lameness and should not be considered pathognomonic for the location or type of lameness.
Determining the Location of Lameness
The horse should be observed at both the walk and the trot from the front, behind, and side. I spend most of my time watching the horse move away and then back toward me. Medial-to-lateral limb flight and foot strike can be evaluated only from this perspective, although cranial and caudal aspects of the stride and fetlock drop (see following discussion) can be evaluated only from the side. Most important, evaluation of lameness from this perspective allows the veterinarian to use the horse as a frame of reference. I find it quite useful to evaluate forelimb lameness when the horse is traveling away from me and hindlimb lameness when the horse is traveling toward me. This perspective allows use of the horse’s top line to see a subtle head and neck nod or pelvic hike. Only by observing the horse from the side can the cranial and caudal phases of the stride be determined. When first learning to assess lameness from the side, a linear frame of reference, such as a fence or wall in the background, may be helpful to notice head nod and pelvic hike against an immovable background. Application of pieces of tape or other markers to the horse’s head or a fixed point on the pelvis can assist recognition of upward and downward movement of that body part.
Independent observation of the forelimbs and hindlimbs is needed to understand whether a horse has forelimb or hindlimb lameness or a combination. These observations then are amalgamated to form a final clinical impression.
Recognition of Forelimb Lameness
Forelimb lameness often is easier to recognize than hindlimb lameness. Understanding the concept of the head nod is vital to the correct interpretation of equine lameness. The head and neck elevate or rise when the lame forelimb is bearing weight or hits the ground and nod down or fall when the sound forelimb hits the ground. “When the [forelimb] is the lame one, the movements of the foot and head occur somewhat in unison. When the lame foot is raised, the head is elevated, but only to fall when the sound leg is brought to a rest.”1 Some clinicians find it easier to appreciate the head nod down, whereas others find it easier to recognize elevation of the head.
When slow-motion videotape of lame horses is evaluated, it is immediately obvious that the elevation of the head and neck is much easier to see than the head nod down. In slow motion the horse appears to be elevating the head and neck just before the lame limb hits the ground, and then, during the later portion of the support or stance phase, the head and neck nod down. In fact, in slow motion it is head and neck elevation from a baseline level and later settling of the head and neck (nod downward) that are seen. The head returns or settles to baseline, giving the distinct impression that the horse is unloading the lame limb rather than loading the sound limb. The head and neck nod occurs as the contralateral limb begins the support or stance phase. Both head elevation and falling are present, but head elevation is much easier to detect when it occurs in unison with the lame limb hitting the ground. It is likely that a combination of visual clues allows the clinician to decide the primary forelimb lameness. Quantification of lameness and description of the actions of the lame and compensatory limbs have been attempted using gait analysis systems. In horses with amphotericin-induced carpal lameness, head movements were the most consistent indicator of lameness, followed by sinusoidal motion, or a rising and falling action, of the head and withers.14 The motion of the lame limb was assessed, and a falling of the head and withers during the support phase of the lame limb was noted, contrary to clinical perception and evaluation of slow-motion videotape of lame horses. It was suggested that an uncoupling of the weight from the lame forelimb and a “free fall–like” phenomenon occurred during weight bearing.14 The problem with this description is that it considers only the lame limb and is confusing. When evaluating a lame horse, the observer sees both forelimbs. During the later portion of the support phase of the lame limb, the sound limb is in the later portion of the swing phase and beginning the support or stance phase. Thus the head and withers drop described experimentally appears to occur concomitantly with the sound limb hitting the ground. The observer perceives the early portion of the stance or support phase.
In general, a good correlation between clinical evaluation of forelimb lameness and that described using motion analysis has been observed. There was complete agreement between clinical determination of location of forelimb lameness and that detected by motion analysis using a computerized three-dimensional motion measurement system. However, the degree of lameness differed in 6 of 29 horses.15 In a more recent study subjective forelimb lameness grades were significantly associated with kinetic parameters, and vertical force peak and impulse had the lowest coefficients of variations and highest correlations with subjective lameness score.16 In fact, kinetic parameters using GRFs measured by force plate analysis detected subclinical lameness not seen by a trained observer, a finding that may indicate that quantitative lameness analysis may be useful in horses with subtle lameness.16 The maximal vertical acceleration of the head was the best indicator of forelimb lameness.17 Although horses with forelimb lameness shifted weight in a caudal direction to the diagonal hindlimb, the amount of withers motion was minimal. The authors reasoned that the tremendous mobility of the head and neck, allowing the horse to asymmetrically elevate the neck and thus load the nonlame forelimb, accounted for the lack of withers movement and the horse’s adaptation to forelimb lameness.17 A similar compensatory ability is not present in the hindlimb. Vertical displacement of the tuber coxae and forward motion or translation of the pelvis occur in horses with hindlimb lameness, because a mechanism such as head and neck movement does not exist.17 In a computer-generated model of a trotting horse the dynamic effects of head and neck movement accounted for the majority of load shift to the contralateral forelimb and diagonal hindlimb in horses with unilateral forelimb lameness.18 Load shift and compensation by the diagonal hindlimb in horses with unilateral forelimb lameness lend support to the clinical findings of compensatory lameness in the diagonal limbs in trotters.
Instrumented shoes have been used experimentally to study motion in horses by quantifying GRF but have had limited clinical use.19,20 Lack of correlation between an in-shoe system and force plate analysis was disappointing, and neither research nor clinical application of the system was recommended.21 Although these systems are not currently widely available, in the future these or similar systems may be useful to objectively assess lameness and the response to diagnostic analgesic techniques in clinical patients. A remote monitored sensor-based accelerometer-gyroscopic (A-G) system showed good correlation in horses with either forelimb or hindlimb lameness when compared with a video-based motion analysis system used in horses moving on a treadmill.22 Hindlimb lameness was consistently higher (in grade) using the A-G system, but the system yielded false-positive results in horses with concurrent forelimb lameness.22 However, for a skilled observer, direct observation of the horse may be more accurate than kinetic or kinematic analysis of gait when a horse is lame in more than one limb.5
Recognition of Hindlimb Lameness
Historically descriptions of hindlimb lameness have been confusing. An important principle in the recognition of hindlimb lameness is the concept of the pelvic hike or asymmetrical movement of the pelvis. This has also been termed hip hike, but I prefer the term pelvic hike because it accurately describes how the pelvis moves in a horse with unilateral hindlimb lameness. The entire pelvis, not just the lame side of the pelvis, appears to undergo elevation. Because the horse has two “hips” and only one pelvis, the term pelvic hike seems preferable. Pelvic hike is the vertical elevation of the pelvis when the lame limb is weight bearing. In other words, the pelvis “hikes” upward when the lame limb hits the ground and moves downward when the sound limb hits the ground. The “haunch settles downward when the sound leg touches the ground.…”1 Some clinicians find it easier to see the downward movement of the pelvis, on the side of the lame limb, rather than the pelvic hike.5 ![]() It may be simpler to determine which side has the most movement, rather than looking for either a hike or a drop.5 The clinician must keep in mind that the pelvic hike is the clinical impression of the change in height of the pelvis, not the absolute or measured height. It is the shifting of weight or load that occurs as the horse tries to reduce weight bearing (unload) in the lame limb and transfer weight (load) to the sound limb. The ease with which this can be seen depends on the horse’s tail carriage; in a horse with a tail set on high and that is also carried high, this may completely obscure movements of the pelvis.
It may be simpler to determine which side has the most movement, rather than looking for either a hike or a drop.5 The clinician must keep in mind that the pelvic hike is the clinical impression of the change in height of the pelvis, not the absolute or measured height. It is the shifting of weight or load that occurs as the horse tries to reduce weight bearing (unload) in the lame limb and transfer weight (load) to the sound limb. The ease with which this can be seen depends on the horse’s tail carriage; in a horse with a tail set on high and that is also carried high, this may completely obscure movements of the pelvis.
Another explanation for asymmetrical movement of the pelvis involves one of the protective or compensatory mechanisms used by the horse to assist in breakover and minimize load on the lame limb. Many horses with hindlimb lameness drift away from the lame limb toward the sound limb. Drifting may decrease the magnitude of the observed pelvic hike, but more important, it makes the lame side look lower than the sound side. ![]() This is why it is important to watch the entire pelvis as a unit rather than the individual sides of the “hips.”
This is why it is important to watch the entire pelvis as a unit rather than the individual sides of the “hips.”
In most horses with hindlimb lameness, particularly those without a substantial tendency to drift away from the lame limb, the elevation of the pelvis (pelvic hike up) when the lame limb hits the ground surpasses that when the sound limb is weight bearing. This elevation can be seen readily in slow-motion videotape analysis, but it may not be as obvious during clinical examination. Observing horses with hindlimb lameness from the front as the horse trots toward you may be useful. ![]() This approach allows the pelvic hike to be seen clearly using the horse’s top line as a frame of reference. Subtle pelvic elevation is best seen from this perspective. The use of markers on a fixed part of the pelvis can help to identify asymmetry. Stride length characteristics, height of foot flight, sound, and fetlock drop are also helpful (see following text).
This approach allows the pelvic hike to be seen clearly using the horse’s top line as a frame of reference. Subtle pelvic elevation is best seen from this perspective. The use of markers on a fixed part of the pelvis can help to identify asymmetry. Stride length characteristics, height of foot flight, sound, and fetlock drop are also helpful (see following text). ![]()
Horses with bilateral hindlimb lameness may have a short, choppy gait that lacks impulsion, but they may have no pelvic hike. Other methods to exacerbate the baseline lameness should be performed, such as circling the horse at a trot in hand or while on a lunge line. Lameness may be accentuated when the lame or lamer limb is on the inside or outside of the circle (see following discussion).
Hindlimb Lameness Confused with Forelimb Lameness
It is important to understand how a horse with unilateral hindlimb lameness modifies its gait so that hindlimb lameness can mimic forelimb lameness at the trot. When the lame hindlimb hits the ground, the horse shifts its weight cranially to transfer load away from the lame limb. This causes the head and neck to shift forward and nod down at the same time. The contralateral forelimb bears weight simultaneously with the lame hindlimb and the head nod coincides, thus mimicking lameness in the forelimb ipsilateral to the lame hindlimb.![]() I find it difficult to distinguish clinical characteristics of a head and neck nod caused by forelimb lameness from that caused by ipsilateral hindlimb lameness. Some clinicians have suggested that the head and neck nod caused by ipsilateral hindlimb lameness is less vertical in nature and more forward and downward. Head and neck movement in horses with hindlimb lameness is not always observed. Horses generally must have prominent (>3 out of 5, see later grading discussion) hindlimb lameness before compensatory head and neck movement develops. However, two horses with very similar severity of hindlimb lameness may have different characteristics of movement, which will result in an associated head nod in one, but not in the other. At the pace, a lateral gait, LH lameness mimics RF lameness and RH lameness mimics LF lameness. Evaluation of the horse moving in circles may help to determine if a head nod is related to primary forelimb or hindlimb lameness. If a head nod is exacerbated but a hindlimb lameness is less obvious, then there is probably coexistent forelimb and hindlimb lameness. However if the head nod and hindlimb lameness remain similar or both appear worse, it is more likely that the head nod reflects a primary hindlimb lameness.
I find it difficult to distinguish clinical characteristics of a head and neck nod caused by forelimb lameness from that caused by ipsilateral hindlimb lameness. Some clinicians have suggested that the head and neck nod caused by ipsilateral hindlimb lameness is less vertical in nature and more forward and downward. Head and neck movement in horses with hindlimb lameness is not always observed. Horses generally must have prominent (>3 out of 5, see later grading discussion) hindlimb lameness before compensatory head and neck movement develops. However, two horses with very similar severity of hindlimb lameness may have different characteristics of movement, which will result in an associated head nod in one, but not in the other. At the pace, a lateral gait, LH lameness mimics RF lameness and RH lameness mimics LF lameness. Evaluation of the horse moving in circles may help to determine if a head nod is related to primary forelimb or hindlimb lameness. If a head nod is exacerbated but a hindlimb lameness is less obvious, then there is probably coexistent forelimb and hindlimb lameness. However if the head nod and hindlimb lameness remain similar or both appear worse, it is more likely that the head nod reflects a primary hindlimb lameness.
Horses can have a head and neck nod at the trot caused by singular forelimb lameness, singular ipsilateral hindlimb lameness, or concurrent forelimb and ipsilateral hindlimb lameness. A prominent head nod is seen in horses with simultaneous LF and LH lameness. The examiner first must determine whether both limbs are affected. ![]() Problems arise because occasionally a horse with only LF lameness may shorten the LH stride at the trot, leading the veterinarian to question whether LH lameness also exists. More commonly, however, horses with only lameness in a single forelimb shorten the cranial phase of the stride of the contralateral hindlimb. Horses with only LH lameness can have a rather pronounced head nod, and thus the veterinarian may question the existence of LF lameness. Although a horse with LF lameness may have a compensatory shortened stride of the LH, in the absence of lameness a marked pelvic hike should not be present. A head nod consistent with LF lameness may be inappropriately severe to be caused by mild LH lameness. If a horse has simultaneous LF and LH lameness, it is essential to perform diagnostic analgesia in the hindlimb first, because moderate-to-severe hindlimb lameness produces head and neck nod that is not abolished unless the hindlimb lameness is resolved.
Problems arise because occasionally a horse with only LF lameness may shorten the LH stride at the trot, leading the veterinarian to question whether LH lameness also exists. More commonly, however, horses with only lameness in a single forelimb shorten the cranial phase of the stride of the contralateral hindlimb. Horses with only LH lameness can have a rather pronounced head nod, and thus the veterinarian may question the existence of LF lameness. Although a horse with LF lameness may have a compensatory shortened stride of the LH, in the absence of lameness a marked pelvic hike should not be present. A head nod consistent with LF lameness may be inappropriately severe to be caused by mild LH lameness. If a horse has simultaneous LF and LH lameness, it is essential to perform diagnostic analgesia in the hindlimb first, because moderate-to-severe hindlimb lameness produces head and neck nod that is not abolished unless the hindlimb lameness is resolved. ![]() Resolution of the pelvic hike and reduction in the head nod should be expected with resolution of the hindlimb lameness.
Resolution of the pelvic hike and reduction in the head nod should be expected with resolution of the hindlimb lameness.
Simultaneous lameness of a diagonal pair of limbs is less common than simultaneous ipsilateral lameness, except in trotters, because many horses perform at gaits that appear to induce compensatory lameness in the ipsilateral limbs. With simultaneous LH and RF lameness the head nod reflects the forelimb component, a mandatory clinical sign for perception of RF lameness. ![]() The horse may drift away from the LH with shortening of the cranial phase of the stride. The horse may have a short, choppy stride in the forelimbs and hindlimbs. The horse may have a rocking gait. It cannot shift weight or compensate from stride to stride in the usual manner and thus tends to rock back and forth from the hindlimbs to the forelimbs.
The horse may drift away from the LH with shortening of the cranial phase of the stride. The horse may have a short, choppy stride in the forelimbs and hindlimbs. The horse may have a rocking gait. It cannot shift weight or compensate from stride to stride in the usual manner and thus tends to rock back and forth from the hindlimbs to the forelimbs. ![]()
Reasonable agreement generally exists between clinical recognition of hindlimb lameness and that found experimentally. The use of markers placed on each tuber coxae of 13 horses with unilateral hindlimb lameness showed a consistent increase in vertical displacement of the pelvis during early weight bearing of the lame limb.23 Although the rise and fall of the pelvis was readily apparent and occurred consistently with weight bearing of the lame and sound limbs, respectively, the absolute height of the pelvis on the lame side did not rise above that of the sound limb.23 These findings are consistent with my clinical impressions. A head nod down when the diagonal forelimb was bearing weight further confirmed clinical observations that hindlimb lameness can mimic lameness of the ipsilateral forelimb.23 In a kinematic study using a three-dimensional optoelectronic locomotion system, hip acceleration quotient increased in horses with hindlimb lameness.24 Vertical displacement corresponded to the pelvic hike up on the lame limb, with a simultaneous forward movement of the head and neck during the stance phase of the lame limb.24 Pelvic height differed significantly between sound and lame limbs in an experimental study using a custom-made heart-bar shoe to induce transient hindlimb lameness.25 Pelvic height was reaffirmed as an important indicator of hindlimb lameness, but exaggerated pelvic hike seen on the lame side was proposed to be caused by push-off from the sound limb and occurred immediately before weight bearing of the lame limb.25 The importance of weight support and asymmetrical dorsoventral hindlimb movement (pelvic hike) was reaffirmed in a study using continuous three-dimensional kinematic monitoring of movement of the tubera coxae.26 The hip (pelvic) hike seen on the lame side was found to be a rapid upward movement that led to an increased dorsoventral displacement.26
GRF has been measured in normal horses and those with forelimb and hindlimb lameness.27-30 GRF is reduced in the lame forelimb or hindlimb with compensation by the other limbs. In horses with unilateral forelimb lameness, decreased horizontal GRF in the lame limb is compensated for by increased GRF in the contralateral forelimb and ipsilateral hindlimb.31 Decreased vertical GRF in the lame limb is compensated for by increased vertical GRF in the contralateral forelimb during the swing phase of the lame limb, and increased vertical GRF in both the ipsilateral and contralateral hindlimbs during the stance phase of the lame limb.31 During unilateral hindlimb lameness the decreased GRF in the lame limb is compensated for by increased GRF in the contralateral hindlimb and the contralateral and ipsilateral forelimbs.31 These experimental data support the clinical impression that a lame horse adapts by shifting load to the contralateral limb or by shifting load in a caudal direction for forelimb lameness and in a cranial direction for hindlimb lameness. Kinetic gait analysis in horses with hindlimb lameness or spinal ataxia was recently studied using a force plate mounted in an examination aisle, a setup that may prove useful for clinical use during lameness examination.32 Horses with hindlimb lameness had significant differences from normal and ataxic horses and their own contralateral hindlimbs in vertical peak force, vertical force impulse, and coefficient of variance of vertical force peaks.32 Uniquely, investigators examined ataxic horses at the trot and found significant differences in lateral force peaks (lateral hindlimb movements) between normal horses and those affected with spinal ataxia.32
Bilaterally Symmetrical Forelimb or Hindlimb Lameness
Bilateral lameness is a common cause of poor performance and may go unrecognized without additional movement, such as circling, lunging, or riding. Horses with bilaterally symmetrical forelimb lameness may have a short, choppy gait when trotted in straight lines. Horses with hindlimb lameness may lack lift to the stride, have a subtle change of balance, or have reduced hindlimb impulsion.5 If bilaterally symmetrical lameness is suspected, the veterinarian should select one limb and begin diagnostic analgesia. Horses often show pronounced lameness in the contralateral limb when the source of pain is eliminated.
The Lameness Score: Quantification of Lameness Severity
I believe it is important to have a standardized lameness scoring system that allows the clinician to quantify lameness within and between horses. Ideally it should be consistent worldwide, but currently a scale from 0 to 5 generally is used in North America, and a scale from 0 to 10 is often used in Europe. Definitions vary within the grading systems. The system adopted by the American Association of Equine Practitioners (AAEP) provides a framework.33
The AAEP system is potentially confusing because it grades lameness at both the walk and trot. It does not account for a horse that has a shortened stride at walk but trots soundly. In my experience, many lame horses show consistently observable lameness at a trot and therefore would have to be given a score of at least 3, leaving only grades 3 and 4 for use in the majority of lame horses. Horses with bilateral lameness and a shortened stride but no obvious head nod or pelvic hike are difficult to score based on this system.5 It does not permit grading under different circumstances, such as straight lines, circles on the soft in each direction, and circles on the hard.5
An alternative lameness scoring system is listed in Box 7-1. Lameness is scored only with the horse at a trot, and the grading system is used most often to describe lameness at a trot in hand. The system is useful for both forelimb and hindlimb lameness and is based on a range of 0 (sound) to 5 (non–weight bearing). In this system, a horse with unilateral hindlimb lameness of grade 3 or worse would have a head nod that mimics ipsilateral forelimb lameness. This system has limitations because as discussed previously a horse with a moderately severe hindlimb lameness may or may not have an associated head nod, depending on the gait characteristics caused by the source and degree of pain.5 There is a practical difference between this scoring system and that put forth by the AAEP. A horse with lameness grade 1 in this modified scoring system would have a lameness grade of 2 to 3 in the AAEP system. The modified scoring system is more flexible and allows clear differentiation among most lameness conditions. However, it does not account for a bilaterally symmetrical gait abnormality and may be difficult to apply in a horse with lameness in more than one limb. Many horses evaluated for subtle lameness or poor performance have a score of 0 to 1 because consistent lameness is not observed. Use of half grades provides greater flexibility and supports adoption of a scoring system from 1 to 10, assuming 0 denotes soundness. A third system is to grade lameness independently at both the walk and trot and under different circumstances—straight lines, circles on the soft, circles on the hard, and ridden—using a relatively simple 9-point scale in which 0 is sound, 2 represents mild lameness, 4 represents moderate lameness, 6 represents severe lameness, and 8 represents non–weight-bearing lameness.5 This system takes account of the fact that a horse may appear lamer at the walk than at the trot.
Lameness grades from 0 to 5 are based on observation of the horse at a trot in hand, in a straight line, on a firm or hard surface.
| 0 | Sound. |
| 1 | Mild lameness observed while the horse is trotted in a straight line. When the lame forelimb strikes, a subtle head nod is observed; when the lame hindlimb strikes, a subtle pelvic hike occurs. The head nod and pelvic hike may be inconsistent at times. |
| 2 | Obvious lameness is observed. The head nod and pelvic hike are seen consistently, and excursion is several centimeters. |
| 3 | Pronounced head nod and pelvic hike of several centimeters are noted. If the horse has unilateral singular hindlimb lameness, a head and neck nod is seen when the diagonal forelimb strikes the ground (mimicking ipsilateral forelimb lameness). |
| 4 | Severe lameness with extreme head nod and pelvic hike is present. The horse can still be trotted, however. |
| 5 | The horse does not bear weight on the limb. If trotted, the horse carries the limb. Horses that are non–weight bearing at the walk or while standing should not be trotted. |
Lameness Detection
Fetlock Drop
Assessment of fetlock drop, or extension of the metacarpophalangeal and metatarsophalangeal joints, may be helpful in recognition of the lame limb. ![]() In general, the fetlock joint of the sound limb drops farther when this limb is weight bearing than does the fetlock joint of the lame limb, because the horse is attempting to spare the lame limb by increasing load in the sound limb. This may be easier to detect by video analysis than in a clinical situation and may be more recognizable at the walk than at a trot.
In general, the fetlock joint of the sound limb drops farther when this limb is weight bearing than does the fetlock joint of the lame limb, because the horse is attempting to spare the lame limb by increasing load in the sound limb. This may be easier to detect by video analysis than in a clinical situation and may be more recognizable at the walk than at a trot. ![]() However, in some horses with moderate or severe unilateral suspensory desmitis or tendonitis, the fetlock drops markedly on the lame limb when the horse is walking, but at a trot fetlock drop usually is more pronounced in the sound limb. With bilateral suspensory desmitis or severe tendonitis the fetlock may drop further in the lamer limb. In horses with chronic hindlimb suspensory desmitis excessive fetlock excursion on the affected side may falsely reduce pelvic excursion (hike) and make hindlimb lameness less obvious and more difficult to detect.
However, in some horses with moderate or severe unilateral suspensory desmitis or tendonitis, the fetlock drops markedly on the lame limb when the horse is walking, but at a trot fetlock drop usually is more pronounced in the sound limb. With bilateral suspensory desmitis or severe tendonitis the fetlock may drop further in the lamer limb. In horses with chronic hindlimb suspensory desmitis excessive fetlock excursion on the affected side may falsely reduce pelvic excursion (hike) and make hindlimb lameness less obvious and more difficult to detect.
Use of Sound
Sound can be useful in lameness evaluation. A lame horse usually lands harder on the sound limb, resulting in a louder noise. ![]() For this sound to be appreciated, the horse must be trotted on a firm or hard surface such as pavement or concrete. However, the sound a horse makes while landing depends greatly on symmetry of the front or hind feet, and the loss of one shoe, different shoe types, or disparity in foot size confounds interpretation. Listening for regularity of rhythm and sound of footfall are important, especially when evaluating the response of lame horses to diagnostic analgesia, particularly in horses with subtle lameness.5
For this sound to be appreciated, the horse must be trotted on a firm or hard surface such as pavement or concrete. However, the sound a horse makes while landing depends greatly on symmetry of the front or hind feet, and the loss of one shoe, different shoe types, or disparity in foot size confounds interpretation. Listening for regularity of rhythm and sound of footfall are important, especially when evaluating the response of lame horses to diagnostic analgesia, particularly in horses with subtle lameness.5
Drifting
Horses with hindlimb lameness generally drift away from the lame limb. ![]() Drifting is one of the earliest adaptive responses of a horse with unilateral hindlimb lameness, allowing the horse to break over more easily or to reduce load bearing. Drifting may alleviate the need for extensive pelvic excursion (hike). It may make pelvic drop on the lame side more obvious. The horse may mask the lameness by reducing pelvic excursion. In some horses a pelvic hike is undetectable or subtle, but consistent drifting away from the lame side indicates the presence of hindlimb lameness. Many driven STBs with hindlimb lameness drift away from the lame limb or are “on the shaft.” Horses with LH lameness have a tendency to be on the right shaft and vice versa. Drifting away from the lame limb may be most evident when horses have pain from the tarsus distally, although some clinicians have different experiences.5 Drifting may result in the horse moving on three tracks.
Drifting is one of the earliest adaptive responses of a horse with unilateral hindlimb lameness, allowing the horse to break over more easily or to reduce load bearing. Drifting may alleviate the need for extensive pelvic excursion (hike). It may make pelvic drop on the lame side more obvious. The horse may mask the lameness by reducing pelvic excursion. In some horses a pelvic hike is undetectable or subtle, but consistent drifting away from the lame side indicates the presence of hindlimb lameness. Many driven STBs with hindlimb lameness drift away from the lame limb or are “on the shaft.” Horses with LH lameness have a tendency to be on the right shaft and vice versa. Drifting away from the lame limb may be most evident when horses have pain from the tarsus distally, although some clinicians have different experiences.5 Drifting may result in the horse moving on three tracks.
Horses with severe forelimb lameness also tend to drift away from the lame limb, but this tendency usually is less obvious than in horses with hindlimb lameness. Drifting is most common with carpal lameness when the horse tends to abduct the limb during the swing phase of the stride and appears to push off with the limb, forcing the horse away from the lame side. Abduction seen in horses with carpal lameness should not be confused with swinging the limb or a swinging limb lameness. During protraction abduction seen in horses with carpal region pain appears to involve the horse carrying and placing the limb lateral to the expected site of limb placement. Racehorses with either forelimb or hindlimb lameness tend to drift away from the lame limb while training or racing at speed.![]() This finding is an important piece of the lameness anamnesis.
This finding is an important piece of the lameness anamnesis.
Drifting toward the lame hindlimb is an unusual but important clinical sign. In horses that drift toward the lame limb, I suspect weakness and lameness exist simultaneously, suggesting a neurological component to the gait abnormality. ![]() However, a jumping horse at takeoff may push off more strongly with the nonlame hindlimb and drift across the fence toward the lame limb.5
However, a jumping horse at takeoff may push off more strongly with the nonlame hindlimb and drift across the fence toward the lame limb.5
Evaluation of Limb Flight
Observation and characterization of limb flight can be useful in determining the lame limb or limbs and possibly the location of pain within the limb. Abnormal limb flight also may predispose to lameness, especially in horses with faulty conformation. In my opinion, it is impossible to predict the site of pain causing lameness accurately based solely on limb flight and other characteristics, although some abnormalities lead to a high index of suspicion. I believe strongly that the location of pain should always be confirmed by using diagnostic analgesic techniques whenever possible. Some abnormalities are consistently associated with specific lameness conditions, whereas others are general patterns of limb flight seen with many different conditions.
Cranial and Caudal Phases of the Stride
Changes in limb flight in the cranial and caudal phases of the stride can be seen only when the horse is evaluated from the side. ![]() In a normal horse the length of the stride of the paired forelimbs and hindlimbs, measured from hoof imprint to hoof imprint, is nearly identical from side to side. Extension and flexion of the limbs is also similar. From a clinical perspective the length of the stride of the affected limb cranial to the stance position of the contralateral limb is called the cranial phase of the stride, and the length of the stride caudal to the stance position of the contralateral limb is called the caudal phase of the stride. Obviously in a normal horse these individual parts of the stride are symmetrical. In a lame horse the overall stride length does not appear to change. If stride length changed, the horse could not trot in a straight line. Drifting is associated with lameness and could be explained by a change in stride length, but shorter stride length would be expected in the lame limb, causing the horse to drift toward the lame side, in contrast to the usual observation, drifting away from the lame limb. In racehorses, some of the tendency to drift away or toward the inside of the track could be easily explained by mild differences in stride length or strength (power). However, with the horse at a trot in hand we can assume that total stride length does not change.
In a normal horse the length of the stride of the paired forelimbs and hindlimbs, measured from hoof imprint to hoof imprint, is nearly identical from side to side. Extension and flexion of the limbs is also similar. From a clinical perspective the length of the stride of the affected limb cranial to the stance position of the contralateral limb is called the cranial phase of the stride, and the length of the stride caudal to the stance position of the contralateral limb is called the caudal phase of the stride. Obviously in a normal horse these individual parts of the stride are symmetrical. In a lame horse the overall stride length does not appear to change. If stride length changed, the horse could not trot in a straight line. Drifting is associated with lameness and could be explained by a change in stride length, but shorter stride length would be expected in the lame limb, causing the horse to drift toward the lame side, in contrast to the usual observation, drifting away from the lame limb. In racehorses, some of the tendency to drift away or toward the inside of the track could be easily explained by mild differences in stride length or strength (power). However, with the horse at a trot in hand we can assume that total stride length does not change.
In most lame horses the cranial phase of the stride of the affected limb is shortened. ![]() The caudal phase is lengthened to maintain a near equal overall stride length side to side. Shortening of the cranial phase of the stride appears to be a learned response of the horse to reduce the time spent during the stance phase and to help during breakover. Loss of propulsion, or an unwillingness to push off with the lame limb, could also explain reduction in the cranial phase of the stride. Because most lame horses have a shortened cranial phase of the stride, this finding, although quite useful in determining in which limb the horse is lame, is not particularly useful in localizing or classifying lameness and is not synonymous with swinging limb lameness. It is also important to recognize that pain causing lameness results in altered proprioceptive responses, to protect the painful area, and these responses may persist for some time after pain has resolved.5 A classic example of attenuation of the cranial phase of the stride in the hindlimbs occurs mechanically in horses with fibrotic myopathy. This authentic swinging limb lameness causes a marked abrupt change in the later portion of the protraction phase of the affected hindlimb, shortening the cranial phase and causing a sudden downward and backward action of the limb.
The caudal phase is lengthened to maintain a near equal overall stride length side to side. Shortening of the cranial phase of the stride appears to be a learned response of the horse to reduce the time spent during the stance phase and to help during breakover. Loss of propulsion, or an unwillingness to push off with the lame limb, could also explain reduction in the cranial phase of the stride. Because most lame horses have a shortened cranial phase of the stride, this finding, although quite useful in determining in which limb the horse is lame, is not particularly useful in localizing or classifying lameness and is not synonymous with swinging limb lameness. It is also important to recognize that pain causing lameness results in altered proprioceptive responses, to protect the painful area, and these responses may persist for some time after pain has resolved.5 A classic example of attenuation of the cranial phase of the stride in the hindlimbs occurs mechanically in horses with fibrotic myopathy. This authentic swinging limb lameness causes a marked abrupt change in the later portion of the protraction phase of the affected hindlimb, shortening the cranial phase and causing a sudden downward and backward action of the limb. ![]()
The caudal phase of the stride is lengthened in most lame horses because for overall equal stride length to be maintained, this portion of the stride must compensate. I generally have not found evaluation of the caudal phase of the stride at the trot in hand clinically useful, but it is sometimes a useful observation in horses at a walk (see following text). Some horses with severe palmar foot pain have a shortened caudal phase of the stride at both walk and trot.5
Contrast of the cranial and caudal phases of the stride in the lame limb at a walk and a trot is useful. ![]() In most horses with forelimb lameness the cranial phase of the stride is slightly shortened at a walk but markedly shortened at a trot. Obviously, in horses with subtle lameness, this clinical sign is absent at the walk and only mildly apparent at the trot. Horses with pain in the dorsal aspect of the foot, such as hoof abscessation or laminitis, may have a shortened caudal phase of the stride at a walk. This response is an attempt to protect the painful area and to shorten during breakover. These horses walk with a marked camped-out appearance in the forelimbs. At the trot, however, the cranial phase of the stride is likely to be shortened, a clinical contrast useful in localizing lameness to the dorsal aspect of the hoof.
In most horses with forelimb lameness the cranial phase of the stride is slightly shortened at a walk but markedly shortened at a trot. Obviously, in horses with subtle lameness, this clinical sign is absent at the walk and only mildly apparent at the trot. Horses with pain in the dorsal aspect of the foot, such as hoof abscessation or laminitis, may have a shortened caudal phase of the stride at a walk. This response is an attempt to protect the painful area and to shorten during breakover. These horses walk with a marked camped-out appearance in the forelimbs. At the trot, however, the cranial phase of the stride is likely to be shortened, a clinical contrast useful in localizing lameness to the dorsal aspect of the hoof.
Most horses with hindlimb lameness have a reduction in the cranial phase of the stride at the walk and the trot. Horses with pelvic fractures involving the acetabulum prefer to keep the lame limb ahead of the contralateral limb at the walk and have marked shortening of the caudal phase of the stride, but at the trot the horse has a shortened cranial phase of the stride. Horses with hoof abscessation, most commonly of the dorsal aspect of the hoof, walk similarly, only to trot with a pronounced shortening of the cranial phase of the stride. An explanation for disparity at walk and trot in the phases of the stride in horses with pain at either end of the hindlimb is not readily apparent, but recognition of this phenomena has been quite useful, and consistent. Unilateral or bilateral laminitis and other severe causes of pain in the digit are rare in the hindlimbs and can cause similar clinical signs.
Shortening of the cranial phase of the stride does not always indicate that lameness is present in that limb. At speed a trotter with forelimb lameness shortens the cranial phase of the stride in the ipsilateral hindlimb to avoid interference with the lame limb. This observation sometimes is also made in horses being trotted in hand. This compensatory movement gives the impression that the horse may be lame in the ipsilateral hindlimb, with a subtle pelvic hike. Lameness of the foot and carpus in trotters most often causes this compensatory ipsilateral hindlimb pelvic hike. Once lameness has been abolished in the ipsilateral forelimb, the subtle pelvic hike and shortened cranial phase of the stride in the hindlimb abate. In trotters a shortened cranial phase of the stride and a pelvic hike may be related to faulty weight distribution and interference problems and not to lameness at all.
Abnormalities of Limb Flight
Abnormalities of limb flight can cause interference of one limb with another, particularly in trotters and pacers (Figure 7-2). However, horses performing at speed at any gait and those with faulty conformation also are at risk to develop interference injuries. In some horses, interference is of no consequence, but in others, especially trotters, it causes gait deficits. Skin lacerations, bruising, and underlying bone and soft tissue damage (interference injury) may occur. Various boots and other protective devices have been developed to protect the limbs from potential trauma. It is important to assess the presence and location of interference injuries. In some horses, only mild evidence of hitting is found, but other horses may have many painful areas. Chronic interference can be the sole reason for lameness or poor performance.
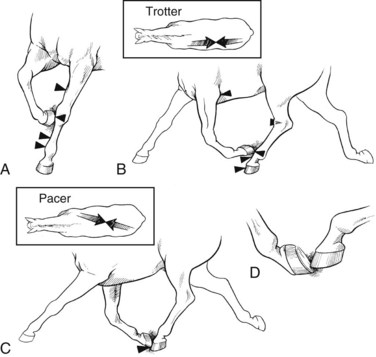
Fig. 7-2 Types of interference. A, Horses at any gait can be injured by interference of a forelimb with the opposite side. B, Interference is common in the trotter and usually involves the ipsilateral forelimb and hindlimb. Interference within a forelimb can be seen in horses that hit the elbow of the same limb. This usually occurs because of high action, excessive weight of the shoes, or a combination of these factors. C, Interference in the pacer can involve the forelimb and diagonal hindlimb, commonly called cross-firing. D, Forging occurs during trotting when the toe of the hind foot strikes the bottom of the ipsilateral front foot.
Front Foot Interference
Front Foot Hitting the Contralateral Forelimb
Horses with toed-out conformation tend to wing in during movement, predisposing to interference injuries. Horses with base-narrow conformation or those with a combination of base-narrow and toed-out conformation also are at risk. However, many horses with these conformational abnormalities do not interfere. Some horses walk very closely but widen out at faster gaits. Interference injury from one hind foot hitting the medial side of the contralateral hindlimb occurs infrequently.
All types of horses, especially STB racehorses, are at risk for interference. Interference can involve any level of the limb from the foot to the proximal antebrachium. Mild interference of this type is called brushing. STBs often “hit their knees,” which causes swelling, bruising, and lacerations of the skin on the distal medial aspect of the radius. In some horses, large, chronic swellings develop; these consist of mostly fibrous tissue. In others, osteitis of the distal radius or abscessation occurs. Even with protective gear, horses may be reluctant to perform at maximal speed to avoid injury or disruption of gait, or pain caused by interference induces the horse to go off stride.
Interference within the Same Limb
Horses can develop interference injuries within a limb when the hoof or shoe hits the ipsilateral elbow. This type of interference sometimes is seen in trotters with high action (excessive carpal flexion) and is common in gaited horses that perform with heavy shoes intended to cause high action of the forelimbs (see Figure 7-2, B).
Front Foot Hitting the Ipsilateral Hindlimb
Interference in trotters usually involves the toe of a forelimb interfering with (hitting) the dorsal aspect of the ipsilateral hindlimb (see Figure 7-2). Various names are given to the type of interference based on the location in which the injury occurs. Interference injury at the dorsal aspect of the hind foot or coronary band is called scalping; in the pastern region it is called speedy cutting; in the metatarsal region (shin) it is called shin-hitting; and in the dorsal or medial aspect of the tarsus, it is called hock-hitting. Because interference is common in trotters, it is important not to overinterpret signs of pain on palpation. Speedy cutting results in pain over the dorsal aspect of the proximal phalanx that should not be misinterpreted as pain associated with a midsagittal fracture.
Front Foot Hitting the Contralateral (the Diagonal) Hindlimb
Cross-firing, or the striking of the contralateral (diagonal) hindlimb by the front foot, usually occurs only in pacers (see Figure 7-2, C).
Hind Foot Interference
Interference as a result of a hind foot hitting the foot of the ipsilateral forelimb (forging) is common and usually does not result in injury. Many horses forge at a trot in hand or while being ridden. In horses with shoes the sound is unavoidable but may not be a sign of a pathological condition. Forging is most common in horses that are trotted in deep footing. Forging may reflect imbalance, lack of strength, incoordination, or poor foot trimming.5
Forelimb: Common Abnormalities of Limb Flight
Winging In and Winging Out
Common limb flights observed during lameness examination include winging in and winging out movement of the front feet and are often related to conformation (see Figure 4-13). Horses that are toed out tend to wing in, whereas those that are toed in tend to wing out. Such abnormalities do not necessarily compromise performance. However, such movement may result in uneven loading of the soft tissue structures and uneven hoof wear, leading to chronic imbalance. Horses that wing in tend to develop interference injuries and wear the medial aspect of the shoe excessively. Horses that wing out tend to develop lateral branch suspensory desmitis and wear the lateral aspect of the shoe excessively.
Lateral Placement of the Foot during Advancement (Abduction)
Horses normally advance the forelimbs straight ahead. When advancing the limb, horses with articular carpal pain, and some horses with pain in the proximal metacarpal region, place the foot lateral to the expected foot position. This action has been described as abduction of the limb, but this term may infer swinging the limb, and horses with carpal lameness seem to place the limb laterally rather than swinging the limb. However, ankylosis associated with severe osteoarthritis or arthrodesis of the carpus does necessitate swinging the limb during advancement, a much different movement from that seen in horses with more mild carpal region pain.
Horses with this abnormality of flight almost always have a shortened cranial phase of the stride. They tend to push off with the affected limb from the lateral location, resulting in a wide or peg leg type of motion at walk, and sometimes at trot. With bilateral carpal lameness the horse appears to move widely bilaterally. Not all horses with carpal pain move widely, and this gait change is seen more often in horses with middle carpal or carpometacarpal joint pain than in those with pain in the antebrachiocarpal joint. Some horses with upper limb lameness may carry the limb widely while walking, although this characteristic is not typical of horses with shoulder pain. A horse with a humeral stress fracture sometimes may travel widely, similar to a horse with carpal lameness, but the latter is more likely. A horse with pain in the lateral aspect of a foot may move widely in the affected limb to reduce load laterally. This characteristic is seen in STB and TB racehorses with subchondral bone trauma or early stress fractures of the distal phalanx.
Plaiting
The verb to plait means to braid or pleat, or to make something by braiding.3 The term is used to describe horses that walk or trot by placing one foot directly ahead of the other foot. ![]() Plaiting in the forelimbs is not nearly as common as in the hindlimbs and usually is the result of base-narrow, toed-out conformation. Old horses (usually broodmares) with severe carpus osteoarthritis and carpus varus limb deformities occasionally may swing the limb laterally and place the foot far enough medially to end up in front of, or lateral to, the opposite foot. Some horses with shoulder region lameness guard the limb and travel very closely in front. Plaiting in the forelimbs can be seen in horses with recent fractures of the thoracic dorsal spinous processes at the withers.5 Horses with neurological disease occasionally plait.
Plaiting in the forelimbs is not nearly as common as in the hindlimbs and usually is the result of base-narrow, toed-out conformation. Old horses (usually broodmares) with severe carpus osteoarthritis and carpus varus limb deformities occasionally may swing the limb laterally and place the foot far enough medially to end up in front of, or lateral to, the opposite foot. Some horses with shoulder region lameness guard the limb and travel very closely in front. Plaiting in the forelimbs can be seen in horses with recent fractures of the thoracic dorsal spinous processes at the withers.5 Horses with neurological disease occasionally plait.
Limb Flight in Horses with Shoulder Region Lameness
I include this section principally because the shoulder often is erroneously incriminated as the source of pain. Horses with moderate-to-severe lameness of the scapulohumeral joint or bicipital bursa have a marked shortening of the cranial phase of the stride. They also have an unusual motion of the shoulder joint that is difficult to describe.![]() Because the cranial phase of the stride is shortened, during breakover the affected shoulder joint seems to drop or buckle forward, more so than the opposite side (assuming lameness is unilateral). There may be prominent lifting of the head and neck. Limb flight is either straight ahead or somewhat close to the opposite forelimb. Horses with shoulder region pain do not consistently travel widely, or abduct the affected limb. However, racehorses with humeral stress fractures may occasionally travel widely in front. With mild lameness there are no typical gait characteristics.
Because the cranial phase of the stride is shortened, during breakover the affected shoulder joint seems to drop or buckle forward, more so than the opposite side (assuming lameness is unilateral). There may be prominent lifting of the head and neck. Limb flight is either straight ahead or somewhat close to the opposite forelimb. Horses with shoulder region pain do not consistently travel widely, or abduct the affected limb. However, racehorses with humeral stress fractures may occasionally travel widely in front. With mild lameness there are no typical gait characteristics.
Hindlimb: Common Abnormalities of Limb Flight
Stabbing or “Stabby” Hindlimb Gait
A common abnormality of limb flight seen in horses with hindlimb lameness is described as a stabbing or “stabby” gait. During protraction of the lame hindlimb or hindlimbs, the limb travels medially, close to the opposite hindlimb, and then moves laterally during the later portion of the swing phase and is placed lateral to the expected foot placement. ![]() This motion results in excessive wear of the lateral or dorsolateral aspects of the shoe. Although this gait often is seen in horses with distal hock joint pain, it can be seen with many other sites of pain from the distal tibia to the foot. Therefore diagnostic analgesia is required to localize the pain. However, horses with the most marked shoe wear consistent with this abnormality of limb flight are most likely to have tarsal lameness. Exaggerated stabbing hindlimb motion often is seen in horses with neurological disease.
This motion results in excessive wear of the lateral or dorsolateral aspects of the shoe. Although this gait often is seen in horses with distal hock joint pain, it can be seen with many other sites of pain from the distal tibia to the foot. Therefore diagnostic analgesia is required to localize the pain. However, horses with the most marked shoe wear consistent with this abnormality of limb flight are most likely to have tarsal lameness. Exaggerated stabbing hindlimb motion often is seen in horses with neurological disease.
Abduction of the Hindlimbs during Advancement
In some horses with hindlimb lameness the limb is carried forward in a position lateral to the expected position (i.e., abducted). In some horses with this limb flight the limb swings outside the expected line of limb flight, only to strike the ground near the expected position. Lateral swinging of the limb begins immediately after the lame limb leaves the ground. I have observed this abnormality most consistently in horses with stifle lameness, but it also occurs with some other upper limb lameness conditions. Care must be taken when evaluating horses that normally travel widely behind, such as trotters.
I have recognized lateral swinging of the hindlimb most commonly in pacers with articular lesions of the stifle, because the normal gait in these horses is to swing the hindlimb more than would be expected from other horses. Many horses with stifle lameness carry the limb forward lateral to the expected position, but just before impact may actually stab laterally. ![]() Therefore the veterinarian must pay close attention to limb flight directly after the lame limb leaves the ground and while it is passing the contralateral limb. Another common characteristic of horses with stifle lameness is a shortened cranial phase of the stride. The stifle joint also may appear unusually prominent and be carried somewhat away from the flank and slightly externally rotated.
Therefore the veterinarian must pay close attention to limb flight directly after the lame limb leaves the ground and while it is passing the contralateral limb. Another common characteristic of horses with stifle lameness is a shortened cranial phase of the stride. The stifle joint also may appear unusually prominent and be carried somewhat away from the flank and slightly externally rotated. ![]()
Plaiting
Plaiting is more common in the hindlimb than in the forelimb and usually results from lameness rather than faulty conformation, although plaiting can occur in a horse with severe base-narrow conformation. Plaiting can be seen in horses with unilateral or bilateral lameness. In horses with unilateral lameness, it appears that limb flight actually may be altered in both hindlimbs, resulting in both hind feet being placed ahead, or in some horses, lateral to the opposite foot. ![]() In horses with severe hindlimb lameness, it appears that the affected foot is being swung around and placed directly in front or lateral to the unaffected foot. Alternatively, the horse may be trying to support most of its weight on the unaffected limb and moves this limb inside to support the lame side. In horses with bilateral lameness, it is equally difficult to determine what exactly is causing the plaiting. The horse may be reluctant to bring either hindlimb along the expected line of flight, leaving the limb medially and forcing the opposite limb to the outside to avoid interference. A horse may swing each hindlimb around the other, ultimately ending placing one foot ahead or lateral to the other.
In horses with severe hindlimb lameness, it appears that the affected foot is being swung around and placed directly in front or lateral to the unaffected foot. Alternatively, the horse may be trying to support most of its weight on the unaffected limb and moves this limb inside to support the lame side. In horses with bilateral lameness, it is equally difficult to determine what exactly is causing the plaiting. The horse may be reluctant to bring either hindlimb along the expected line of flight, leaving the limb medially and forcing the opposite limb to the outside to avoid interference. A horse may swing each hindlimb around the other, ultimately ending placing one foot ahead or lateral to the other. ![]() An unusual rocking type of gait is observed in horses with bilateral hindlimb lameness and plaiting. I have observed plaiting most commonly in horses with osteoarthritis of the coxofemoral joint or pelvic fractures, but I also have seen it in horses with bilateral distal hock joint pain or suspensory desmitis.
An unusual rocking type of gait is observed in horses with bilateral hindlimb lameness and plaiting. I have observed plaiting most commonly in horses with osteoarthritis of the coxofemoral joint or pelvic fractures, but I also have seen it in horses with bilateral distal hock joint pain or suspensory desmitis. ![]() Plaiting also is observed in some horses with sacroiliac joint pain.5
Plaiting also is observed in some horses with sacroiliac joint pain.5
Mechanical Lameness of the Hindlimb and Limb Flight
Mechanical conditions of the hindlimb can cause profound abnormalities of limb flight (see Chapter 48). These are termed lameness conditions because of the gait abnormality exhibited, although in many horses pain is not characteristic.
Stringhalt
Stringhalt, an ill-defined neuromuscular disorder of the hindlimb, causes mild-to-severe hyperflexion of the tarsus.![]() The condition can be unilateral or bilateral and usually is most obvious at a walk but can also be seen at the trot. In horses with severe stringhalt the dorsal aspect of the hoof comes close to or hits the ventral aspect of the abdomen. Horses may exhibit the clinical signs more prominently during backing or when initially moved after previous standing.
The condition can be unilateral or bilateral and usually is most obvious at a walk but can also be seen at the trot. In horses with severe stringhalt the dorsal aspect of the hoof comes close to or hits the ventral aspect of the abdomen. Horses may exhibit the clinical signs more prominently during backing or when initially moved after previous standing.
Fibrotic Myopathy
Fibrotic myopathy is characterized by a sudden downward and backward motion of the limb (slapping motion) that occurs during, and restricts the length of, the cranial phase of the stride. Hyperflexion of the hock is not a clinical feature of this gait deficit, but the restriction of the cranial phase of the stride and the slapping motion and sound can be confused with the clinical signs of stringhalt. It is most obvious at a walk.
Upward Fixation of the Patella
Upward fixation of the patella is a classic hindlimb gait deficit and one that displays the function of the stay or reciprocal apparatus. It can be intermittent or permanent and unilateral or bilateral. When the patella is locked in position over the medial trochlear ridge of the femur, the stifle and hock joints are held in extension, whereas the digit is held in partial flexion.
Shivers
Shivers is an ill-defined neuromuscular disease and is most common in Warmbloods and draft breeds; it can occur unilaterally or bilaterally. Clinical signs usually are most obvious when a horse is backed or first moves from the stall. Horses elevate and abduct the limb, and the limb may actually shiver or shake. The tail often is elevated. Signs may be accentuated if the horse is tense.
Other Hindlimb Gait Deficits
Other unusual unexplained gait deficits affecting one or both hindlimbs are observed occasionally, and they often have characteristics similar to those seen with stringhalt, fibrotic myopathy, upward fixation of the patella, and shivers. However, some distinction usually prevents easy recognition and diagnosis. A gait deficit characterized by marked hindlimb abduction seen most prominently at the walk has been recognized. This is most similar to fibrotic myopathy, because a consistent abduction of the limb is observed, and signs tend to abate when the horse is trotted. It may be related to scarring, abnormal function of the biceps femoris and gluteal muscles, or neurological disease.
Neurological disease can cause many different gait deficits, most commonly recognized in the hindlimbs but also in forelimbs. A complete neurological evaluation usually is not performed during lameness examination unless certain abnormalities are observed. Abnormal or excessive circumduction of the hindlimbs, a bouncy, stabby hindlimb gait noticed when the horse is trotted, knuckling over behind or crouching, stumbling, and lethargy are signs that should prompt further investigation.
Evaluation of Foot Placement
It is important to critically evaluate foot placement. Ideally, both the front and hind feet should land flat and level on a firm surface. Foot strike patterns change on soft footing. Evaluation of foot strike is most important in horses with lameness localized to the foot, but it can also give clues regarding other causes of lameness. Abnormal foot placement can be the result of a current lameness problem but may also cause lameness.
In the forelimbs, horses commonly land on the lateral side of the foot first before rocking medially. This can be the result of abnormal conformation or hoof imbalance and can predispose to lameness in the digit and suspensory branch desmitis. Landing abnormalities in the dorsal-to-palmar direction are common but are difficult to recognize unless severe. Horses with profound pain in the toe caused by laminitis or hoof abscessation land heel first, giving a camped-out appearance, and have a shortened caudal phase of the stride. Horses with palmar foot pain may compensate by landing toe first, causing abnormal stress on the dorsal structures of the foot, but this characteristic is difficult to see except in slow motion.
In the hindlimbs, several patterns of abnormal landing or motion are recognized, not all of which are a cause or result of lameness. Landing on the toe is commonly considered the result of heel pain, but many horses with severe hindlimb lameness land on the toe. This tendency is particularly prominent when the horse is first moved, and most horses warm out of the lameness. Horses may land on the toe when walking up an incline or at the walk on the flat but generally place the heel on the ground when trotted. The most consistent lameness I see in horses that land on the toe is distal hock joint pain, but any cause of lameness from the tarsus to the foot can cause a horse to exhibit this abnormal landing pattern. Horses with lameness of the metatarsophalangeal joint region, including osteoarthritis, tenosynovitis of the digital flexor tendon sheath, or desmitis of the accessory ligament of the deep digital flexor tendon have a tendency to land on the toe. Horses with adhesions within the digital flexor tendon sheath may have severe mechanical restriction that causes toe-first landing. Old Western performance horses with deep digital flexor tendonitis have severe toe-first landing and may stand on the toe and even rise up in the heels during the examination. The condition can be bilateral or unilateral and is difficult to manage. Mild or moderate tendency to land on the toe also has been attributed to stifle lameness.5
Abnormal movement of the lower or entire hindlimb occasionally is noted when horses are watched from behind. Horses may place one or both hind feet in an axial position and collapse or break over the lateral aspect of the fetlock region.5 Another uncommon hindlimb motion is characterized by excessive rotation of the hindlimb. The horse plants the hind foot and rotates the heel laterally, causing abnormal loading or twisting of the distal limb.5 Although this movement can lead to lameness, it sometimes is seen in horses that are successful in various sporting endeavors. I have seen this type of hindlimb motion most often in TB racehorses.
Additional Movement During Lameness Examination
Further information about the character of lameness often can be obtained by observing the horse as it moves in circles and is ridden or driven. Some lameness conditions are apparent only under these circumstances.
Hard and Soft Surfaces
Comparison of movement on hard and soft surfaces is valuable. Foot lameness usually is worse when the horse is trotted on hard surfaces and better on a soft surface, such as grass or sand. Horses with suspensory desmitis or digital flexor tendonitis are more likely to show lameness on a soft surface. Deep sand may accentuate some lameness conditions, but an extended lameness examination under these conditions could cause proximal suspensory desmitis.5 A slight downward incline or an uneven, rough surface may make subtle lameness more apparent.5
Circling
Lameness often is much more pronounced when a horse is circled. ![]() Horses should be circled in both directions: to the left (counterclockwise, LF and LH on the inside) and to the right (clockwise, RF and RH on the inside). Lameness may be more pronounced when circling at either the walk or the trot. In some horses with incomplete fractures, baseline lameness at a trot in straight lines in hand may be subtle or absent. Lameness may be readily apparent during circling, even at the walk. The additional forces of torsion and bending during circling are added to those of compression and tension. In horses with incomplete fractures, such as those involving the proximal or distal phalanges, torsion or bending forces during circling likely cause mild separation of the fracture fragments and exacerbate lameness. In horses with other lameness conditions, exacerbation of lameness may be caused by a change of load on the affected soft tissue structure or bone, redistribution of the forces of compression and tension in a medial-to-lateral direction, or additional forces of bending and torsion.
Horses should be circled in both directions: to the left (counterclockwise, LF and LH on the inside) and to the right (clockwise, RF and RH on the inside). Lameness may be more pronounced when circling at either the walk or the trot. In some horses with incomplete fractures, baseline lameness at a trot in straight lines in hand may be subtle or absent. Lameness may be readily apparent during circling, even at the walk. The additional forces of torsion and bending during circling are added to those of compression and tension. In horses with incomplete fractures, such as those involving the proximal or distal phalanges, torsion or bending forces during circling likely cause mild separation of the fracture fragments and exacerbate lameness. In horses with other lameness conditions, exacerbation of lameness may be caused by a change of load on the affected soft tissue structure or bone, redistribution of the forces of compression and tension in a medial-to-lateral direction, or additional forces of bending and torsion.
From a clinical perspective the force of compression may be dominant to other forces in determining a horse’s response to circling, but it is not the only factor. Extension of the limb is also influential.5 When the lesion is in the outside limb while the horse is circling and undergoing compression, exacerbation of the lameness occurs. For instance, lameness in horses with medially located lesions of the distal phalanx or of the third carpal bone is worse when the limb is on the outside of the circle and the lesion is being compressed. ![]() For some soft tissue injuries, tension forces may be more important. Lameness in horses with proximal suspensory desmitis often is worse with the limb on the outside of the circle, suggesting that tension is important in the expression of lameness. The same observation is not seen in horses with more distally located suspensory desmitis.
For some soft tissue injuries, tension forces may be more important. Lameness in horses with proximal suspensory desmitis often is worse with the limb on the outside of the circle, suggesting that tension is important in the expression of lameness. The same observation is not seen in horses with more distally located suspensory desmitis.
Is the lameness seen in a horse that is moving in a circle the same lameness that is seen while the horse is walking or trotting in straight lines? In most instances, circling exacerbates the primary lameness seen in straight lines. If lameness is subtle or nonexistent when the horse is evaluated in a straight line, the lameness seen during circling becomes the baseline lameness. The clinician must recreate the same conditions of circling when evaluating the results of diagnostic analgesic techniques. There is always the possibility that lameness seen during circling may be different from the baseline lameness seen in straight lines. For example, a horse has grade 1 RF baseline lameness when it moves in a straight line that increases to grade 3 when trotted in a circle to the left, but still has grade 1 lameness when trotted to the right. Lameness in a straight line and when trotting to the right is absent after palmar digital analgesia but still is rated grade 3 when the limb is on the outside of the circle. This horse has two problems in the RF: palmar foot pain and an additional carpal lameness that becomes evident when the horse is trotted to the left (RF on the outside of the circle). With bilateral forelimb or hindlimb lameness, primary lameness often is seen in a single limb in straight lines, but during circling the lameness is seen in whichever limb is on the inside (or outside) of the circle. Circling is useful in exacerbating the primary lameness problem and identifying an additional cause of lameness not previously noted. This additional lameness must be recognized and treated separately from the baseline lameness.
Good correlation usually exists between the cause of lameness seen on the straight and that seen while circling the horse; thus it is helpful to circle the horse to try to exacerbate lameness. Circling can be done at the walk and trot in hand and while lunging or riding the horse. Horses often move more freely and naturally when lunged than when being led.5 However, lunging is not possible in some horses, particularly racehorses, and circling while being led is better than no circling. The surface should be nonslip because horses may be hesitant to move freely on slippery surfaces and shorten or alter the stride even when lameness is not present.5 Soft footing is best when the horse is first being lunged, because the horse can buck and play without risk of injury. Hard or firm surfaces are best to exacerbate many lameness conditions, but the surface must be nonslip to avoid possible injury.
That lameness of the upper forelimb or hindlimb is worse when the limb is on the outside of the circle is a common misconception. This is true in some horses, but a generalization cannot be made (see following text). Shortening of the cranial phase of the stride may appear more obvious with the limb on the outside of the circle, but exacerbation of lameness judged by the degree of head nod may not be observed. Another misconception is that horses with lameness of the foot are lamest when the limb is on the inside of the circle. Although a majority (65%) of those with lameness localized to the foot are lamest when the limb is on the inside of a circle, lameness can be worst with the lame limb on the outside of a circle. This depends in part on the location of pain within the foot.
Forelimb
Lameness Worsened with Limb on the Inside of the Circle
In many horses, lameness originating from the fetlock region to the foot is worse with the affected limb on the inside of the circle. ![]() Comparison of circling on hard and soft surfaces is useful. Baseline lameness associated with foot pain usually is dramatically increased when the horse is circling on a hard surface, but a less obvious response is seen when circling on softer surfaces. However, lameness in horses with medially located lesions can be worse with the limb on the outside of the circle.
Comparison of circling on hard and soft surfaces is useful. Baseline lameness associated with foot pain usually is dramatically increased when the horse is circling on a hard surface, but a less obvious response is seen when circling on softer surfaces. However, lameness in horses with medially located lesions can be worse with the limb on the outside of the circle.
Horses with lameness of the metacarpal region vary in response to circling. Lameness related to metacarpal bony injury and distally located lesions in the suspensory ligament or digital flexor tendons tends to be worse with the limb on the inside of the circle, whereas lameness in those with proximal suspensory desmitis is worse with the limb on the outside. Horses with suspensory branch desmitis may show a different response depending on lesion severity and whether the injured branch is undergoing tension or compression.
In my experience, the degree of lameness in horses with pain originating from the forearm, elbow joint, arm, and shoulder joint region tends to be worse with the limb on the inside of the circle, but opinions and experiences do vary.5 Observations may differ if horses are examined while led in hand as opposed to being lunged or ridden. Lameness in some horses with mechanical restriction of movement that dramatically decreases the cranial phase of the stride may be worse with the limb on the outside of the circle.
Lameness Worsened with Limb on the Outside of the Circle
Horses with medially located lesions of the lower limb, especially foot lameness, proximal metacarpal lesions (proximal suspensory desmitis or avulsion injury to the McIII at the suspensory origin), or carpal pain often are more lame with the limb on the outside of the circle. Horses with lesions in the antebrachiocarpal joint are less consistent in response to circling compared with those with middle carpal joint lesions, because most of the common injuries involve the medial aspect of the latter. Upper limb lameness is accentuated in some horses.5
Lameness Improved When Circling
Lameness that appears better on a circle than in straight lines is uncommon. Lameness in horses with medially located lesions in the foot or carpus may improve when the limb is on the inside of a circle. ![]() Baseline lameness in horses with middle carpal disease involving the third and radial carpal bones improves with the limb on the inside of the circle. A STB racehorse with grade 2 or 3 RF baseline lameness in a straight line that increases to grade 3 or 4 when circled to the left, but is only grade 1 or 2 when circled to the right, may have lameness associated with the middle carpal joint, but pain in the medial aspect of the foot also is possible.
Baseline lameness in horses with middle carpal disease involving the third and radial carpal bones improves with the limb on the inside of the circle. A STB racehorse with grade 2 or 3 RF baseline lameness in a straight line that increases to grade 3 or 4 when circled to the left, but is only grade 1 or 2 when circled to the right, may have lameness associated with the middle carpal joint, but pain in the medial aspect of the foot also is possible. ![]()
A horse with bilateral forelimb lameness (e.g., a horse with grade 3 RF baseline lameness in straight lines) may show grade 3 to 4 RF lameness when trotting to the right but grade 1 LF lameness when trotting to the left. The primary lameness is in the RF, and lameness is worse when the limb is on the inside of the circle. Circling to the left induced lameness in the LF, masking the RF lameness, because bilateral lameness existed that was not recognized when the horse was trotting in a straight line.
Hindlimb Lameness and Circling
In my experience, baseline lameness in most horses with any hindlimb lameness is worse when the limb is on the inside of the circle. Exceptions do exist, and some have different experiences and thus opinions.5 Lameness associated with proximal suspensory desmitis often is worse with the affected limb on the outside of the circle, and the horse may stumble or take bad steps. Lameness in some horses with stifle lameness appears worse with the affected limb on the outside of a circle, but in others it appears similar to the left and the right. Many conditions of the stifle involve the medial femorotibial joint, a location that would be compressed with the limb on the outside. Lameness in any horse with a medially located lesion involving the distal hindlimb could be worse with the limb on the outside of the circle. Circling may be useful in exacerbating a primary lameness but generally is not helpful in localizing pain causing lameness.
Observation during Riding
Lameness may not be apparent when the horse is evaluated in hand in straight lines and circles but is obvious when the horse is ridden. This lameness becomes the baseline lameness for further investigation. The additional weight of a rider can exacerbate both forelimb and hindlimb lameness. Gait abnormalities and performance in horses with primary back pain or those with substantial muscle pain secondary to hindlimb lameness usually are worse when they are ridden. Hindlimb gait restriction can occur in horses with back pain but may be apparent only when a horse is ridden.5 Problems related to an ill-fitting saddle or girth, behavioral problems, head shaking, abnormal posture or carriage of the head and neck, and refusal to take a lead or bend in certain directions may be evident only when a horse is ridden.
A horse may be easier to control when ridden than when in hand or on the lunge. Performance of specific maneuvers by the horse may accentuate lameness. A collected trot that forces more weight onto the hindlimbs may exacerbate hindlimb lameness. An extended trot may reveal the horse’s inability to extend one limb compared with another and reveal lameness that was completely imperceptible under all other circumstances. The primary complaint, such as poor-quality flying changes of lead at canter, may require a riding assessment regardless of whether baseline lameness is evident under other circumstances.
However, it is important for the veterinarian to separate his or her observations from those perceived by the rider. Identification of the lame limb may be difficult for a rider, although he or she may have a very strong opinion. If the veterinarian’s observations differ, the rider may be difficult to convince. It is also essential to recognize that bad riding can actually induce a false lameness that is completely unapparent if the horse is ridden well. Nonetheless, an experienced rider, trainer, or driver can be quite helpful in assessing the horse’s response to diagnostic analgesia or therapy, particularly in horses with thoracolumbar pain, subtle hindlimb lameness manifested only when ridden, and poor performance related to a musculoskeletal problem. Working regularly with a skilled, experienced, and reliable rider can be very helpful.
Subtle differences in weight distribution of the rider may exacerbate or mask the presence of forelimb and especially hindlimb lameness. When the horse is performing the posting (rising) trot, lameness may be more or less prominent depending on which diagonal the rider is using. In the rising trot the rider sits on either the left or right diagonal. On the left diagonal the rider is sitting when the LF and RH are bearing weight and rising during the swing phase of these limbs. On the right diagonal the rider is sitting when the RF and LH are bearing weight. The correct diagonal is the outside diagonal (i.e., left diagonal on the right [clockwise] rein). Hindlimb lameness often is worse when the rider sits on the diagonal of the lame limb.5 Therefore if the horse is lame in the RH, the lameness appears and feels worse when the rider sits on the left diagonal. Horses with hindlimb lameness may try to force or throw the rider to sit on the more comfortable (for both horse and rider) diagonal.5 A horse with bilateral hindlimb lameness may appear lame in the RH when the rider sits on the left diagonal and lame in the LH when the rider sits on the right diagonal.5 Forelimb lameness is influenced less by the diagonal on which the rider sits, but a similar pattern exists. RF lameness is worse with the rider sitting on the right diagonal.5 This difference in lameness expression may be perceptible only by an experienced rider. Mild hindlimb lameness may become most obvious when a horse is ridden in small figure eights (two 10-m–diameter circles linked), especially when the horse changes direction from left to right or from right to left.
Observation of Inclines
Walking or trotting a horse uphill or downhill may exacerbate lameness or identify previously unapparent lameness. Lameness in horses with suspensory desmitis may be worse when they walk uphill or downhill. Lameness associated with palmar foot pain may be worse when the horse walks downhill, and the horse may show a tendency to stumble. Horses that tend to stumble or knuckle behind while walking downhill may have loose stifles (inability to maintain the position of the patella, usually caused by lack of muscle tone). Horses with neurological disease usually show more pronounced clinical signs when walking uphill or downhill.
A superficially flat, hard surface may actually slope; this can influence lameness because the horse’s feet will be tilted with one side lower than the other. Thus the horse may appear different when trotting away from the observer than when returning.
Evaluation of Lameness with a Treadmill or Gait Analysis
The use of a treadmill for poor performance evaluation is well recognized, and its use in lameness assessment is discussed in detail in Chapter 98. The clinical relevance of lameness apparent only on a treadmill is open to debate. I do not find lameness examinations on a treadmill at high speed particularly useful unless slow-motion videotape is available. I prefer to assess the horse while training or performing. A horse may modify its normal gait on a treadmill. Good correlation was demonstrated between gait regularity in horses exercised on a track and a treadmill, but treadmill strides and steps were shorter, and the swing phase of the stride was reduced.34 Horses require at least two training sessions on a treadmill before the gait becomes consistent.35 Stride characteristics of horses galloping on a treadmill change as the slope of the treadmill increases from 0% to 8%; horses reduced the suspension phase to maintain overall stride length.36
Gait analysis is discussed in Chapter 22. To date in the clinical setting, assessment by an experienced, skilled observer has been more reliable in the identification of the lame limb or limbs than other, more sophisticated methods of gait analysis.