Chapter 87External Skeletal Fixation
History and Development
Using external skeletal fixation to treat fractures in the horse has only recently received some enthusiasm from equine surgeons. Although external skeletal fixation of fractures works well in small animals and has undergone periods of enthusiastic use, these same devices do not withstand the loads of weight bearing in an adult horse and therefore are not versatile enough to meet the needs of equine surgeons. Using transfixation pins in plaster, transfixation pins in fiberglass casts, or an external skeletal fixation device, has allowed salvage of some horses with difficult fractures that could not have been saved using internal fixation (Figure 87-1).

Fig. 87-1 Dorsopalmar (A), dorsolateral-palmaromedial oblique (B), and dorsomedial-palmarolateral oblique (C) preoperative radiographic images show a severely comminuted fracture of the proximal phalanx. The fracture was open and the horse was managed using a tapered sleeve pin external skeletal fixation device. D, Five years after fracture there is radiological evidence of healing of the proximal phalanx and fusion of the metacarpophalangeal joint, but healing was delayed by motion (see broken screws). The proximal interphalangeal joint fused spontaneously, as usually occurs when the original fracture enters this joint. To date this mare has successfully foaled five offspring.
The incorporation of a walking bar cast, with transfixation pins placed in the bone above the fracture, was described in 1991 to manage fractures in horses and ponies.1 An overall success rate of 57% was reported for a variety of fractures in 35 horses and 21 ponies. The authors suggested that using transfixation pins incorporated into the cast material may help prevent fracture through these pin sites. Major complications of the technique included infection in nine horses or ponies, fracture through the bone or pin sites in six horses or ponies, and loss of circulation to the distal phalanx in two horses or ponies. Complications in the remaining seven nonsurvivors were not reported.1 Using in vitro tests, McClure and colleagues2,3 suggested that a walking bar was not necessary when using fiberglass casts and that divergent transfixation pins may be helpful in preventing fracture through the pin tract sites.
Although transfixation pins have been used successfully in fiberglass casts, this technique represents a compromise compared with classical external skeletal fixation. In horses managed with transfixation pin casts, wounds, skin, and pin sites must be covered in the cast, and at the time of every cast change, fractures are remobilized, allowing fracture collapse or shortening of the limb segment. In addition, pin loosening, pin breakage, and local infection at pin sites are common sequelae of this form of transfixation pinning, often necessitating pin replacement through new pinholes. The use of tapered-sleeve pins (TSPs) in a fiberglass cast has been reported.4 This technique increases the strength and durability of the pin and appears superior to use of unprotected pins alone, and fewer pins may be needed in the pin cast.4 This technique is used as an intermediate step after removal of the newly designed TSP external skeletal fixation device (ESFD) (see later).
The development of an equine ESFD in our laboratory had its origins before the first horse was treated in 1981, and we described the design and development of that device in the first 15 horses in 1986.5 The ESFD was designed to allow immediate full weight bearing in an adult horse and was used in horses with severely comminuted fractures of the distal aspect of the limb, in which internal fixation was not indicated or was impossible to carry out. A follow-up study including five additional horses along with further development of the device was published in 1992.6
Although the previous models of the ESFD proved the feasibility of using external skeletal pin transfixation in a frame device for immediate full weight bearing in an adult horse, there were substantial problems associated with the treatment itself. The original device used three unprotected 9.6-mm–diameter centrally threaded stainless steel pins loaded in bending within the intact bone (the third metacarpal bone [McIII]) above the fracture site, with two sidebars that connected the pins to a ground support through a base plate that was nailed to the horse’s hoof, much like a shoe. This allowed the forces of weight bearing to bypass a comminuted fracture with support through the pins, sidebars, and base. Six (22%) of 27 horses in which the original device was used developed fractures of the McIII through one of the pin holes (usually the proximal pin hole while wearing the device) either when wearing the device or shortly after removal of the device. Problems associated with catastrophic failure of the McIII through a pin hole after device removal were controlled by removing the device while the horse was standing rather than subjecting horses to the rigors of recovery from general anesthesia. After this modification there were no further incidents of McIII fracture after device removal (used in 12 horses without incident).
In 2001 we described a radical change of design of the transfixation pins that was aimed at reducing the incidence of these McIII failures through the pin holes.7 Several horses treated with this new design as well as horses treated with the old design were among a larger group of 64 horses with comminuted proximal phalangeal fractures reported in 2004.8
Mechanics of External Skeletal Fixation
The normal loading regimen for a transfixation pin is in bending. This is similar to hanging a weight in the middle of a clothesline stretched between two poles. The weight of the object causes the clothesline to sag, which can be compared with bending of the transfixation pin when the horse’s weight is transmitted down the bone through the pins to the sidebars. The amount of deflection in the pin is related to the load, the pin diameter, the pin material, the distance from the bone to the sidebar, and the cortex thickness. Pin stiffness is a function of the fourth power of its diameter, whereas pin deflection is proportional to the cube of the distance between the bone and the sidebars. These power relationships show that very small changes in pin diameter or distance to the sidebars make a large difference in the performance parameters of the device. Theoretically to prevent bending of the pin one should reduce the bone-sidebar distance to zero, and the pin diameter should approach infinity. Obviously these parameters are unacceptable in a clinical situation, in which skin and soft tissues represent a barrier to the zero distance, and large holes drilled into bone will decrease bone strength leading to failure, especially if the diameter of the hole is greater than 30% of the smallest cross-sectional diameter of the bone.4
Up to 90% of the magnitude of the total stress at the bone-pin interface is attributed to stresses generated by the bending moment.7 The highest stresses are seen on the surface of the bone at the pin junction, and because bone fails (breaks) at about 2% strain regardless of load, lowering the bone-pin stress should allow an increased load before failure. The solution for this problem was to load the pin uniformly in shear instead of bending to get a uniform load all along the pin as it passed through the bone.7 To accomplish this goal we used transcortical pins that slid into a tapered sleeve. The TSP ends are threaded and compress the tapered sleeves against the bone when fasteners (nuts and lock washers) are used to provide tension in the pins. The pins are then biaxially loaded in tension via the nuts and in shear via the axial load on the bone (Figure 87-2).7

Fig. 87-2 This drawing shows the concept of sleeves that slide over the transfixation pins to give protection from bending in the external skeletal fixation device. The large diameter of the sleeves and the proximity to the bone eliminate bending as a loading mode and ensure a more uniform loading on the pin in shear. This protects the outer bone cortex from the loads of a bending pin and allows the device to be loaded to about 10 times body weight before bone failure.
Although the device could be made in many sizes, it was sized for light horses, ranging from an adult Arabian to larger Warmblood crosses. It ideally fits Thoroughbred (TB) and Standardbred (STB) horses, in which the device has been used most frequently. Two 7.94-mm pins are incorporated into the tapered sleeve and attached through a welded collar steel tube system to the aluminum-magnesium base through an aluminum foot plate. The device is always applied with the horse under general anesthesia (Figure 87-3).
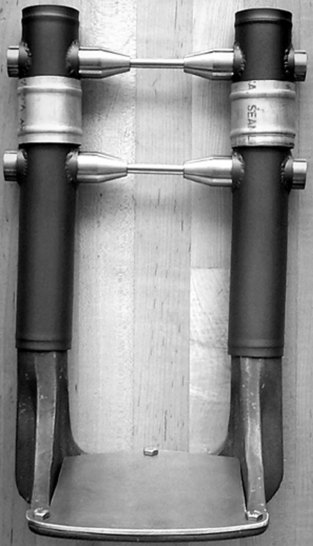
Fig. 87-3 The present tapered sleeve pin external skeletal fixation device is shown. The device is assembled easily over the tapered sleeves using the footplate attached to the base.
The TSP ESFD with all the tools to apply and remove it is commercially available (rane@magnolia-net.com, Ron Nash Engineering, 977 Stephens Highway, Magnolia, Arkansas, United States).
Preoperative Planning, Indications, Tips, and Limitations
The TSP ESFD was designed to treat horses with catastrophic injuries of the distal limb. Indications include comminuted fractures of the proximal phalanx when no strut (intact piece of bone from the proximal to the distal articular surface) is available for use with internal fixation (see Chapter 35), comminuted fractures of the middle phalanx, fracture dislocations, or traumatic disruptions of the suspensory apparatus with massive soft tissue injury (see Chapters 36 and 104). Expanded use of the ESFD could be considered in horses with severe laminitis. In its present form the TSP ESFD is designed for use when the McIII or the third metatarsal bone (MtIII) is intact. The only other requirement is that the blood supply to the distal limb must be intact. In addition to applying the ESFD, it is sometimes helpful to insert bone screws, used in lag fashion through stab incisions, to hold large fragments together. This can be done under radiographic guidance, and these fixations do not need to resist weight-bearing forces, because the ESFD supports the entire weight of the horse. It is necessary that the hoof fits on the base plate of the device, and, if large, the hoof needs to be trimmed. This must be accomplished to allow the aluminum base plate to attach to the magnesium-alloy base using the three cap screws. A compression bandage (elastic bandage) is wrapped around the fractured bone before and during surgery to bring the bone fragments closer together and reduce swelling, which helps with reduction of badly comminuted fractures.
Abbreviated instructions for application of the TSP ESFD are included to show the simplicity of the system. The procedure is completed with the horse under general anesthesia. The only surgical requirement for application of the device is to drill two holes in the McIII, although additional internal fixation may be used when appropriate. The footplate is attached using a glue-on system (www.soundhorse.com). The limb is prepared for aseptic surgery. With the drill guide supplied, two 7.94-mm holes are drilled, one at the junction of the proximal and middle thirds and the other at the junction of the middle and distal thirds of the McIII from the lateral aspect. Holes are placed in the center of the bone and marrow cavity and perpendicular to the long axis of the bone. This is facilitated using the dual drill guide, which places the holes parallel and properly spaced. Next the 7.94-mm pins are inserted using the threaded cap to protect the threads. The sleeves over the pins are assembled on the medial and lateral sides and secured with nuts. The sleeve-skin junction is wrapped with a sterile bandage, and the rest of the assembly is performed using nonsterile technique. The side tubes are then assembled using ring connectors over the tapered sleeves on both sides of the limb. The base is slid into the distal ends of the tubes, and the base is fastened to the footplate using cap screws supplied. The reinforcing rods are then inserted into tubes on the medial and lateral sides, and electrical tape is placed around all the tubular junctions to prevent leakage. The fracture is reduced and stabilized by placing traction on the limb in a position that allows the tubes to be filled. The polymer (Conathane UC41, Cytec Industries, Olean, New York, United States) is then mixed (2 : 1 by volume) and poured into the sidebars. The tubing is cooled, using cold saline solution if necessary, to prevent heating of the pins. Last, the now wet sterile wrap around the tapered sleeves is removed, and the ESFD is covered with a bandage. The horse is then recovered from general anesthesia. The current ESFD is shown being worn in Figure 87-4.
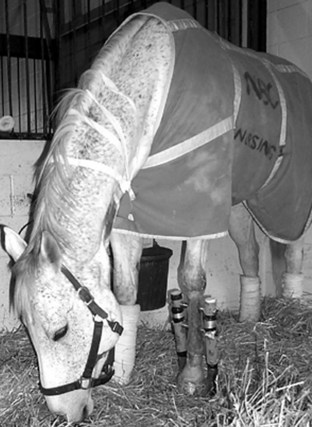
Fig. 87-4 A tapered sleeve pin external skeletal fixation device is used to manage a horse with a comminuted fracture of the middle phalanx.
The contralateral foot often has a shoe applied that elevates the limb so that the horse stands squarely. Without this elevated shoe the horse has a tendency to point the foot in the TSP ESFD while standing. It is important to keep the horse standing squarely on both limbs to help prevent laminitis from occurring in the supporting, non-injured limb.
Postoperative Care
After recovery from general anesthesia the horse is immediately fully weight bearing and usually comfortable on the limb. In fact, this is a major advantage of this type of fracture management. Skin care around the pin sites is important during the initial postoperative period and is done easily using antiseptic-soaked sponges. The TSP ESFD is checked for tightness using an appropriate deep socket wrench every few days. Pin loosening does not occur, because one has the ability to tighten the pins with the fastener nuts already in place, which is easily done and does not require sedation of the horse. Reducing pin loosening helps to diminish pin tract infections and allows the horse to remain fully weight bearing. Local antiseptic application at the pin sites may decrease severity of pin site infections. Some horses may be discharged from the hospital with the TSP ESFD in place. If the owner or trainer can provide pin care, discharging the horse as soon as possible decreases the cost of hospitalization. The horse is returned to the hospital for removal of the TSP ESFD after 8 to 10 weeks. Although the device can be left on longer, substantial osteoporosis of the McIII or the MtIII below the lowest pin may be detrimental to the end result. Radiologically the fracture site may not appear healed (based on the observation of mature callus) at this time, because osteoid will have formed, but calcification of this soft callus will not yet have occurred without the stimulus of weight bearing. The TSP ESFD is removed in the standing, sedated horse, and a fiberglass cast is applied. Serial radiographic examinations are then performed until radiological evidence of fracture healing is visible. Spontaneous fusion of the proximal interphalangeal joint will occur in horses with comminuted fractures of the proximal phalanx. If arthrodesis of the metacarpophalangeal or metatarsophalangeal joint is necessary, additional internal fixation, usually screws alone, will be needed because spontaneous fusion rarely occurs (see Figure 87-1). Most horses with fractures of the proximal phalanx managed with the TSP ESFD need arthrodesis of the metacarpophalangeal or metatarsophalangeal joint to maintain comfort.
Removing the External Skeletal Fixation Device
Removal of the ESFD is accomplished with the horse standing, with use of light sedation and a special pin removal device supplied by the manufacturer. The foot plate is removed using a sharp box knife, cutting the material at the junction of the hoof and plate.
An electric Sawzall or hacksaw can be used to cut the lateral sidebar tube just below the lower tapered sleeve on one side of the frame very quickly.
The nuts are removed from the threaded pins on the tapered sleeves. The pin extractor is placed over the distal tapered sleeve and the pin engaged and removed by turning the extractor with an end wrench. This is repeated as necessary on the proximal tapered sleeve. Once the pins have been removed, the frame can be lifted away. A standing cast is usually applied to preserve the structure and function of the extremity for an additional time until healing is sufficient for unrestricted weight bearing. It is at this juncture that the TSPs can be incorporated into the cast if desired. Radiographic examination is helpful in making these decisions.
Results of Treatment (2008)
Of 27 horses managed with the original ESFD (three 9.6-mm unprotected pins through the McIII or the MtIII) over a period of 14 years, nine survived (33%). The complication of the McIII or the MtIII fracture through pin sites in six horses led us to abandon this device and introduce the two-pin TSP ESFD in 1996. Early experience with the TSP ESFD has been favorable, and five (71%) of seven horses survived; only one horse developed a fracture through the pin site. Both nonsurvivors had chronic infections of the original fracture site and laminitis on the contralateral forelimb. Four fractures were open, six were comminuted fractures of the proximal phalanx (see Figure 87-1), and one was a comminuted fracture of the middle phalanx.