Chapter 35 The Proximal and Middle Phalanges and Proximal Interphalangeal Joint
Anatomical Considerations
The term pastern originated from the shackle that was secured below the metacarpophalangeal or metatarsophalangeal joints to tether a horse to the pasture.1 The proximal interphalangeal (PIP) joint or pastern joint is a diarthrodial joint, which is formed from the distal aspect of the proximal phalanx and the proximal aspect of the middle phalanx. The pastern region is bounded dorsally by the common digital extensor tendon and on the palmar/plantar border by the distal sesamoidean ligaments, digital flexor tendons, digital flexor tendon sheath (DFTS), and the proximal and distal digital annular ligaments. The superficial digital flexor tendon (SDFT) inserts on the distal palmar/plantar aspect of the proximal phalanx and the proximal palmar/plantar aspect of the middle phalanx. The straight sesamoidean ligament arises from the base of the proximal sesamoid bones (PSBs) and extends distally to insert on the proximal palmar/plantar aspect of the middle phalanx. The oblique (middle) sesamoidean ligaments arise from the base of the PSBs and attach to the triangular region on the palmar/plantar region of the middle portion of the proximal phalanx. The medial and lateral collateral ligaments of the PIP joint provide support in the sagittal plane and attach to the collateral tubercles of the distal aspect of the proximal phalanx and proximal palmar/plantar aspect of the middle phalanx. The paired smaller abaxial and axial ligaments are located just palmar/plantar to the collateral ligaments. The neurovascular bundle of the digit runs just abaxial to the deep digital flexor tendon on the medial and lateral sides.
The palmar/plantar eminence of the middle phalanx extends proximal to the horizontal axis of the joint surface and blends proximally with a fibrocartilaginous cap at the most proximal extent of the middle phalanx. In the adult horse this is dense, and it is important to engage this portion of the bone during internal fixation of fractures or arthrodesis procedures.
The proximity of the pastern region to the ground, the paucity of soft tissue coverage over the dorsum and sides, and the important soft tissue structures on the palmar/plantar surfaces make it especially vulnerable to external trauma. Wounds in this region may involve the DFTS and warrant careful investigation. Angular deformities from growth disturbances at the pastern are uncommon but do occur. More commonly, deformities arise from physeal abnormalities of the distal aspect of the third metacarpal/metatarsal bones affecting the metacarpophalangeal/metatarsophalangeal joints. Radiological closure of the proximal physis of the proximal and middle phalanges occurs by 6 to 9 months of age, but functional closure is earlier, usually by 8 weeks of age. Radiological closure of the distal physis of the proximal phalanx occurs by 1 month of age. Radiological closure of the distal physis of the middle phalanx occurs by the time of birth.2
Lameness Examination
Physical derangements usually are obvious because of minimal soft tissue coverage of the pastern. Phalangeal fractures usually are associated with soft tissue swelling and focal pain. Effusion of the DFTS is typical of penetrating wounds of the sheath, damage to the enclosed digital flexor tendons, or injury of the sesamoidean ligaments located dorsal to the sheath. In horses with osteoarthritis (OA), new bone formation on the dorsomedial and dorsolateral aspects of the PIP joint often occurs, causing obvious swelling around the joint. Angular deformity of the digit with limb shortening often is present in horses with complex fractures of the proximal or middle phalanx. Effusion in the metacarpophalangeal or metatarsophalangeal joint is common in horses with fractures of the proximal articular surface of the proximal phalanx.
Lameness from the pastern region ranges from severe to subtle depending on the injury. Generally, disorders involving the PIP joint or DFTS cause obvious lameness, but lameness from early OA of the PIP joint may be mild, and the clinical signs and blocking pattern may be confused with foot or occasionally fetlock lameness. Pain in the pastern region may be exacerbated by distal limb flexion. There is often a weight-bearing lameness that is worse if a horse is lunged or trotted with the affected limb on the inside of a circle.
Response to intraarticular analgesia varies depending on the injury, but improvement of lameness by 50% or more implicates the PIP joint as an important source of pain. Entry into the PIP joint can be difficult, especially if new bone is present as a result of OA. Techniques for intraarticular and perineural analgesia are described in Chapter 10. Complete analgesia of the PIP joint is not always accomplished by perineural analgesia of the palmar nerves at the level of the PSBs, and a low four-point (palmar and palmar metacarpal nerves) block may be necessary. However, in some horses lameness improves with palmar/plantar digital analgesia. Intraarticular analgesia of the PIP joint should be considered in a horse with suspected metacarpophalangeal or metatarsophalangeal joint pain that has not responded to treatment. Complete analgesia of the DFTS requires intrasynovial or a low four-point block. Localization by perineural analgesia to the pastern joint does not limit the source of the lameness to the joint itself. Injury to the soft tissue structures should be carefully evaluated if radiological examination reveals no clinically significant abnormalities.
Imaging Considerations
Standard radiographic examination for evaluation of the proximal phalanx includes lateromedial, dorsopalmar (plantar), dorsal 45° lateral-palmaromedial oblique, and dorsal 45° medial-palmarolateral oblique images. Oblique radiographs that are angled distally are helpful to identify osteochondral fragments on the proximal palmar/plantar aspect of the proximal phalanx.3 If a sagittal plane fracture of the proximal phalanx is suspected, dorsopalmar/plantar radiographs that are 5 degrees medial or lateral to the midsagittal plane are useful. Slight underexposure of a lateromedial image helps to identify callus on the proximodorsal aspect of the proximal phalanx associated with chronic, short, incomplete fractures. Radiographic examination of the PIP joint includes lateromedial, dorsopalmar/plantar, and oblique images. Flexed oblique images are particularly helpful for evaluation of the articular margins.3 A well-positioned and exposed dorsopalmar/plantar image may reveal subtle joint space narrowing and increased radiopacity of the subchondral bone consistent with early OA. Comparative views of the contralateral limb may be helpful.
Contrast radiography may be used to determine the course of fistulous tracts or to identify communication between wounds and the DFTS or areas of proliferative synovium within the DFTS. Contrast radiography is performed by placement of a 50% solution of diatrizoate preglumine and diatrizoate sodium (Hypaque-76, Nyromed, Princeton, New Jersey, United States) within a draining tract or directly into the synovial structure after aseptic preparation. Standard radiographs are obtained to identify communication with draining tracts or filling defects.
Computed or digital radiography is helpful in detecting subtle changes in trabecular bone architecture and opacity and is the present state of the art for radiographic examination. Computed tomography (CT) of the distal aspect of the limb offers detailed information regarding structural injury to the bony column of the digit that may not be apparent on radiographic examination.
Ultrasonographic evaluation of the pastern region is helpful in identifying abnormalities associated with the soft tissue structures4 and is discussed in detail in Chapters 16 and 82.
Magnetic resonance imaging (MRI) of the pastern region is indicated in horses that have pain localized to the pastern region without radiological or ultrasonographic evidence of disease and may reveal soft tissue, bone, and/or cartilage pathology.5 A more detailed discussion of MRI is found in Chapter 21. Benign osseous cystlike lesions are identified more commonly with MRI than with radiology in the proximal and middle phalanges but are frequently not associated with pain and lameness, and their significance should not be overinterpreted.
Nuclear scintigraphy is useful in identifying incomplete fractures of the proximal phalanx. Incomplete fractures of the proximal articular margin of the proximal phalanx can occur in all breeds, but they are most commonly seen in Standardbred (STB) and Thoroughbred (TB) racehorses. Clinical signs and response to perineural analgesia vary. Nuclear scintigraphy should be considered to eliminate fracture in horses with lameness referable to the fetlock and clinical signs consistent with an incomplete fracture of the proximal phalanx. Nuclear scintigraphy can be helpful to identify bone modeling in the early phases of OA of the PIP joint. Other bone-related abnormalities in the pastern region often are evident radiologically, and scintigraphy is unnecessary.
Breed Predilection
Differential diagnoses of disorders of the pastern region of all breeds include OA, osteochondrosis, fractures, and infection. The types of fractures tend to be specific to breed or use. Fractures of the proximal phalanx occur most often in racing breeds, with the STB most often affected. Fractures of the middle phalanx occur most commonly in horses used for Western-type activities, such as reining, but are seen in all breeds during lunging or after kicks. Osteochondrosis of the proximal aspect of the proximal phalanx is common in yearling and 2-year-old TB and STB horses. Osteochondrosis of the distal aspect of the proximal phalanx and proximal aspect of the middle phalanx is less common with no breed predilection. OA of the PIP joint occurs most often in older horses used for riding or Western-type activities. It may be seen in young horses secondary to osteochondrosis.
Fractures of the Proximal Phalanx
Fractures of the proximal phalanx are important causes of lameness in all breeds. Racing breeds are particularly prone. Clinical signs vary from subtle to obvious. In horses with complete fractures, lameness is severe, and limb swelling and deformity may be present. In horses with incomplete fractures, lameness may be subtle, and careful clinical and radiographic examination may be necessary to define the fracture. Serial radiographs may be needed to detect radiolucency and callus formation associated with short incomplete fractures of the proximal phalanx. Nuclear scintigraphy may be helpful.
Fractures of the proximal phalanx include the following types:
Incomplete fractures of the proximal phalanx occur most commonly in racing breeds, but are also seen in sports and endurance horses. Clinical signs include mild to severe lameness. Fetlock joint effusion and mild swelling and pain over the dorsal aspect of the proximal phalanx are common but may not be present. Most fractures are readily identified radiologically, but in some horses dorsopalmar/plantar images that are slightly oblique to the sagittal plane are useful. In addition, obtaining follow-up radiographs 7 to 10 days after the fracture allows time for osteoclastic resorption along the fracture line to occur so that the fracture line becomes more obvious. However, there are some incomplete sagittal fractures that occur midway between the dorsal and palmar cortices of the proximal phalanx that may never be detectable radiologically and can only be identified using MRI or CT. Treatment of horses with incomplete sagittal fractures includes stall rest or internal fixation, depending on the degree of lameness, concern about catastrophic fracture of the bone, and economic factors. The advantages of surgical repair are well documented, but horses with incomplete short fractures of the proximal aspect of the proximal phalanx can often be managed with rest alone. In some circumstances a bone screw is placed to provide compression for short fractures to reduce the risk of fracture recurrence. Indications for internal fixation of incomplete fractures include fractures that extend more than 15 mm from the proximal articular surface, those with potential for catastrophic failure, and those that occur in horses with severe lameness. Internal fixation is accomplished by placement of 4.5- or 5.5-mm cortex bone screws in lag fashion. Although 4.5-mm screws generally are used and provide ample compression, 5.5-mm cortex screws have greater pull-out strength compared with 4.5-mm cortex screws in dense bone.6 However, the 5.5-mm cortex screws can be used to replace a stripped 4.5-mm thread. In a nondisplaced fracture, open reduction is not required, and the screws can be placed through minimal incisions. Arthroscopic examination of the dorsal and palmar/plantar aspects of the joint is recommended to evaluate articular cartilage and identify and treat additional abnormalities if present. Although most incomplete sagittal fractures of the proximal phalanx are simple, occasionally there is a transverse component, and radiographs should be examined carefully, especially when lameness is severe. Horses with incomplete fractures are reported to have a 67% to 89% chance to return to racing soundness after treatment. However, STBs returned to racing with slower racing times and reduced performance indices.7-9
Horses with complete fractures of the proximal phalanx are candidates for internal fixation to provide anatomical reduction and compression of the articular surfaces, improved comfort, reduced risk of OA, and early return to use. In horses with acute, minimally displaced fractures, reduction may be achieved by percutaneous placement of bone reduction forceps under radiographic or arthroscopic guidance. Open reduction, arthrotomy, or both may be required in horses with moderately to severely displaced fractures, chronic fractures, or fractures in which fragments of bone prevent reduction of the fracture fragments. After debridement of the fracture bed and reduction of the fracture, compression of the fracture fragments is accomplished using 4.5- or 5.5-mm cortex bone screws. External coaptation with a half-limb cast may be required for recovery from general anesthesia or the immediate postoperative period. Prognosis for horses with noncomminuted complete fractures depends on whether the PIP joint is involved. Horses with fractures that enter the PIP joint had an approximately 50% chance to return to racing. Of those with complete fractures that exited the lateral cortex, 71% returned to racing.7-9
Salter-Harris type II fractures of the proximal aspect of the proximal phalanx occur in foals and weanlings (Figure 35-1). Reduction of the fracture is accomplished with the horse under general anesthesia. Methods of coaptation include bandaging alone, bandaging with splinting, or half-limb cast application. I prefer to use a cast for 4 weeks, but it is important that the cast be changed at 2 weeks. Other clinicians prefer less aggressive coaptation because of concerns of flexor laxity and osteoporosis of the PSBs. One of the Editors (MWR) prefers internal fixation of Salter-Harris type II fractures in foals because of this concern. Techniques include the placement of 3.5- or 4.5-mm bone screws in lag fashion from the metaphyseal component (usually palmarolateral/plantarolateral) in a dorsomedial direction or use of a small bone plate applied to the dorsomedial aspect of the proximal phalanx, using the tension band principle for repair. Rigid internal fixation mitigates the need to use prolonged external coaptation (see Figure 41-7).

Fig. 35-1 Lateromedial radiographic image of a Thoroughbred weanling with a Salter-Harris type II fracture of the proximal physis of the proximal phalanx. The horse was treated by application of a cast for 6 weeks; follow-up radiology after cast removal revealed healing of the fracture and normal alignment of the digit.
Dorsal frontal fractures of the proximal aspect of the proximal phalanx occur in three general types: incomplete proximal dorsal articular fractures, complete proximal dorsal articular fractures, and fractures that originate in the midportion of the proximal articulation and extend distally into the proximal phalanx. Incomplete proximal dorsal frontal fractures occur most commonly in STB racehorses. The right hindlimb is most commonly affected. Proximal dorsal articular fractures can be treated with rest alone or internal fixation with a 3.5-mm cortex bone screw. The prognosis for horses with proximal fractures is good.10 Horses with large fractures that originate in the central portion of the metacarpophalangeal or metatarsophalangeal joint need internal fixation to preserve joint integrity, even if intended for only pasture or breeding soundness. In my experience, OA tends to be preexisting or develops despite anatomical reduction and internal fixation of the fracture, and the prognosis for athletic soundness is poorer (Figure 35-2).11 The 5.5-mm cortex screws, which have a greater resistance to bending, are recommended because there may be larger bending forces in these fractures compared with sagittal plane fractures.
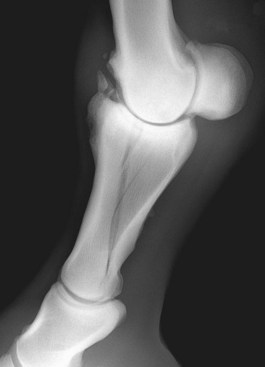
Fig. 35-2 Lateromedial radiographic image of a 12-year-old Thoroughbred mare with a large frontal plane fracture of the proximal phalanx of a forelimb. There is advanced preexisting osteoarthritis of the metacarpophalangeal joint. The fracture was repaired with 5.5-mm cortex screws in lag fashion and a cast applied for 6 weeks.
Horses with comminuted fractures of the proximal phalanx have acute, non–weight-bearing lameness and often limb deformity. Appropriate first aid is required to prevent further injury to the soft tissues and the digital arterial blood supply. A half-limb cast with a dorsally incorporated splint is appropriate to realign the bony column for transport to a surgical facility. Comminuted fractures can be divided into two categories for treatment: those with and those without an intact column (strut) of bone extending from the proximal to distal articular surfaces. An intact strut of bone allows reconstruction of many comminuted fractures of the proximal phalanx by lag screw fixation of the fracture fragments to the strut.12 Treatment strategies include the following:
In my opinion, the use of half-limb casts alone is not the best method of sole treatment for most horses with comminuted fractures of the proximal phalanx, although successful outcomes have been reported. Half-limb casts significantly reduce axial loading in the intact skeleton, but the risks of fracture compression, skin injuries leading to open fractures, and contralateral limb laminitis are substantial.13,14 The use of transfixation casts for management of these fractures has been reported. Based on the relatively poor outcome for comfort, some attempt at reconstruction of the fracture is recommended when possible.15
Horses with comminuted fractures with an existing strut of bone are candidates for open reduction and reconstruction with bone screws. An initial study reported an unacceptably high risk of infection after open reduction and internal fixation,16 but a more recent report described a good prognosis for pasture soundness.12 If the strut has a transverse fracture but enough bone stock proximal and distal to the transverse fracture, then reconstruction of proximal phalanx fractures with two 4.5-mm narrow dynamic compression or locking compression plates and bone screws is advised. With both screw fixation alone and plate and screw fixation, external coaptation with a half-limb cast is required. Partial reconstruction of the articular surfaces and placement of a transfixation cast or external fixator is elected in horses with severely comminuted fractures to reduce degenerative changes, improve short- and long-term comfort, and reduce the requirement for subsequent arthrodesis. A transfixation cast is used when comminution is severe enough to prevent anatomical reconstruction and protection of the fracture from collapse is required. Transfixation casts have been shown to significantly improve axial stability compared with standard casts in an osteotomy model.17 External fixators are used in place of transfixation casts if the fracture is open to allow direct access to the injury site (see Chapter 87).18 The use of transfixation casts and external fixators carries the risk of catastrophic failure of the third metacarpal (metatarsal) bone and prolonged healing; the overall prognosis for salvage is only fair.15
Palmar/plantar avulsion fractures of the proximal phalanx usually occur after kicks, falls, or stall injury (Figure 35-3). Lameness is variable, and fetlock effusion is usually present. Differential diagnosis includes fracture and osteochondritis dissecans fragmentation. Because this region is the distal attachment for the collateral ligaments, surgical treatment is recommended to improve bony union and prevent OA. Treatment options include lag screw fixation, with one or preferably two 3.5-mm cortex bone screws. Surgical removal is also possible for chronic or small fractures or those that cannot be properly reduced. After removal or repair, external coaptation for recovery from general anesthesia and then for an additional 4 weeks is recommended. The prognosis is considered good with either treatment in the absence of OA.

Fig. 35-3 Dorsolateral-plantaromedial oblique radiographic image of a metatarsophalangeal joint of a 2-year-old Standardbred colt. There is an avulsion fracture of the proximal plantarolateral aspect of the proximal phalanx. The fracture was stabilized with two 3.5-mm cortex screws placed in lag fashion.
Dorsal Osteochondral Fragments in the Metacarpophalangeal/Metatarsophalangeal Joint
See Chapters 36 and 42 for a discussion of dorsal osteochondral fragments in the metacarpophalangeal/metatarsophalangeal joint.
Osteochondrosis of the Proximal Interphalangeal Joint
Osteochondrosis of the PIP joint is less common than that of the metacarpophalangeal or metatarsophalangeal joints. As with other sites, osteochondrosis involves fragmentation (osteochondritis dissecans) or osseous cystlike lesions. Sites include the distal aspect of the proximal phalanx and proximal aspect of the middle phalanx. The radiolucent area at the distal central aspect of the proximal phalanx is a normal finding and represents the space between the lateral and medial condyles of the distal aspect of the proximal phalanx. Radiolucent areas or fragmentation in the condylar regions of the distal aspect of the proximal phalanx tend to cause clinical signs. In the most severe circumstances, these subchondral radiolucencies in weight-bearing portions of the joint may cause substantial OA and lameness requiring arthrodesis of the PIP joint. Osseous cystlike lesions are more common in the hindlimb than in the forelimb and can occur bilaterally. Osseous cystlike lesions can communicate with the PIP joint, and if lameness is present, radiological evidence of OA can be substantial. Subtle clinical signs often are seen in horses with osseous cystlike lesions that do not communicate with the PIP joint. Although unusual, sudden-onset severe lameness can occur as a result of osseous cystlike lesions even though the radiological abnormality was present for several months or years. Clinical relevance of osseous cystlike lesions must be established using diagnostic analgesia, and in some horses scintigraphy is required. Management of horses with osseous cystlike lesions may include intraarticular injections or arthrodesis of the PIP joint in some horses. Arthrodesis of the PIP joint can yield a good prognosis for soundness in Western performance horses or other types of sports horses that are not expected to perform at advanced levels. A periarticular drilling procedure can be used in horses with osseous cystlike lesions that do not communicate with the PIP joint. A small drill bit is used under radiographic or fluoroscopic guidance to approach the cystic cavity. Methylprednisolone acetate, expanded stem cells, or liquid bone marrow can be injected. Alternatively, cancellous bone can be packed into the cyst cavity. Radiological evidence of healing of the cyst cavity is variable, and in some horses residual lameness remains.
Osteochondral fragments associated with osteochondrosis tend to occur at the palmar/plantar eminence of the proximal aspect of the middle phalanx and cause variable lameness. They often are an incidental finding found on radiographs acquired before sale, but they certainly can complicate the sales process. Prognosis is difficult to assess in yearlings that have not been trained. Osteochondrosis fragments are more common in hindlimbs than in forelimbs. In adult horses there may be radiological evidence of advanced OA, even if lameness is mild. Because these fragments can be difficult to remove, it is important to document the true source of lameness before surgery is considered. Arthroscopic techniques for the pastern have been described and are most commonly used for dorsal fragments. Palmar/plantar fragments can be accessed arthroscopically or removed via arthrotomy, which may be preferable for large fragments (see Chapter 23 and Figure 23-1).19,20
Osteoarthritis of the Proximal Interphalangeal Joint
OA of the PIP joint is also known as high ringbone. Horses used for jumping, dressage, and Western-type activities seem to be prone to high ringbone. It can also be a consequence of articular fracture, infection, or osteochondrosis. The clinical signs of OA of the PIP joint include mild to severe lameness. Lameness is exacerbated by distal limb flexion. Obvious bony formation or angular deformity may be present in horses with advanced lameness. Diagnosis is based on clinical signs, response to perineural or intraarticular analgesia, and radiological findings. Radiological abnormalities commonly include periarticular new bone formation, subchondral bone increased radiopacity, and loss of joint space typically on the medial aspect of the PIP joint. However, small dorsal periarticular osteophytes are a frequent incidental radiological abnormality and are not necessarily of clinical significance. Angular deformity is typically only present in horses with advanced OA resulting from collapse of the joint surface typically on the medial side. Comparative radiographs of the contralateral limb should also be obtained because the condition may be bilateral. Pain associated with the PIP joint may be present without any radiological signs of OA, and scintigraphic examination is useful in documenting active bone modeling. On the other hand, horses may develop acute severe lameness with radiological evidence of existing OA that predated any clinical evidence of pain. Lameness improves after perineural or intraarticular analgesia.
In horses with mild OA of the PIP joint that is unrelated to fracture, conservative treatment includes therapeutic shoeing aimed at reducing the toe length and elevating the heel and easing breakover in some horses. Nonsteroidal antiinflammatory drugs are useful. The therapeutic value of administering intramuscular glycosaminoglycans and intravenous hyaluronan is questionable. Intraarticular injections are of considerable value. A combination of hyaluronan and corticosteroids or corticosteroids alone are most effective in horses with mild or moderate OA. However, in horses with advanced OA, particularly those with extensive periarticular new bone proliferation and extensive loss of joint space, arthrodesis should be considered. The surgical procedure is invasive and expensive but is generally considered a better solution over the long term. Natural ankylosis of the PIP joint can occur, but it is a long, painful process and one that is not necessarily complete. Surgical arthrodesis is best. Tibial neurectomy can be helpful in horses with advanced hindlimb proximal interphalangeal OA that are not meant to resume athletic careers.21
Arthrodesis of the proximal Interphalangeal Joint
Arthrodesis of the PIP joint is indicated in horses with advanced OA or an articular fracture. Lag screw fixation of simple fractures can be performed, but because of difficulty in obtaining anatomical reduction of the PIP joint surface and resisting tension forces at the palmar/plantar eminences, lag screw fixation alone is usually unsuccessful in preventing OA and returning horses to athletic soundness. Therefore I recommend PIP joint arthrodesis in horses with articular fractures.
Many methods of arthrodesis of the PIP joint are described, and opinions vary as to which is preferred. Current preferred methods involve the insertion of three parallel 4.5- or 5.5-mm screws or dorsally applied plate or plates with additional transarticular screws. I have used both methods and prefer the plating technique because when compared with screws alone it improves comfort in the immediate postoperative period as a result of increased biomechanical stability and reduces the necessity for prolonged cast application. This method requires cast coaptation for 2 to 3 weeks to protect the incision site. The plating technique provided improved stability compared with the three 5.5-mm parallel screw technique in fatigue testing.22 After arthrodesis of the PIP joint with screws alone, approximately 80% to 89% of horses with hindlimb and 46% to 80% of horses with forelimb lameness returned to athletic soundness.23-25 Long-term follow-up data for the plate/screw technique revealed 81% of horses with forelimb and 95% of horses with hindlimb arthrodesis were able to resume performance careers.26 The locking compression plate (LCP) has been recently advocated for arthrodesis of the PIP joint, and its new design with the Combi hole at one end avoids the long pointed end interfering with the extensor process of the distal phalanx. Long-term follow-up data regarding the use of LCP/screw technique for pastern arthrodesis are not yet available.
Horses with comminuted middle phalanx fractures (Figure 35-4) or those that involve the distal interphalangeal (DIP) joint should undergo arthrodesis of the PIP joint with single or double plating and potentially transfixation casts or external skeletal fixation (see Chapter 87). Comminuted fractures of the middle phalanx should be repaired if possible to preserve the DIP joint surface and, if possible, the PIP joint surface. Displacement of the distal articular surface considerably worsens prognosis. Single or double plating can be used depending on the configuration of the fracture. The use of additional screws placed in lag fashion is usually required to reduce large fragments and reconstruct the articular surface. Another plate technique using a Y-plate has been tested experimentally and shows similar biomechanical properties to the double-plate technique.27 Cast coaptation is required for 6 to 8 weeks after surgery. Transfixation pins are used to prevent collapse of the fracture in horses with severely comminuted fractures. This technique may be combined with plate and screw fixation. Prognosis after double-plate fixation of 10 horses with comminuted fracture of the middle phalanx was good for pasture soundness, and 5 horses were able to be ridden or shown, but mild lameness persisted.28

Fig. 35-4 Lateromedial radiographic image of the left hindlimb of a 7-year-old Thoroughbred-cross gelding with a comminuted articular fracture of the middle phalanx. The radiograph was obtained through a distal limb cast. The fracture was repaired using two 4.5-mm narrow dynamic compression plates and 5.5-mm cortex screws, with arthrodesis of the proximal interphalangeal joint. The gelding returned to competitive jumping.
Bone Trauma
Since the advent of MRI, one of the Editors (SJD) has recognized horses with acute-onset severe lameness associated with pain in the pastern region in the absence of detectable radiological abnormality in the acute stage. These horses have had evidence of primary osseous pathology characterized by focal or diffuse areas of increased signal intensity in fat-suppressed images and reduced signal intensity in T1-weighted images, consistent with bone edema, fibrosis, or necrosis. Some horses have made a slow but spontaneous recovery, whereas others have subsequently developed radiological evidence of OA of the proximal or DIP joints associated with persistent lameness.29-31
Subluxation of the Proximal Interphalangeal Joint
Subluxation of the PIP joint is uncommon and can occur in the palmar/plantar direction or dorsally. Palmar/plantar subluxation usually is seen after severe, traumatic soft tissue injury, such as complete tearing of the distal sesamoidean ligaments, SDFT branch injury, or a combination of soft tissue injuries or fracture. Treatment options for palmar/plantar subluxation include both conservative and surgical management. External coaptation can be successful in adult horses managed acutely. The application of a Kimzey splint (Kimzey Leg Saver Splint, Kimzey, Inc., Woodland, California, United States) is an excellent method of first aid for this injury. Cast immobilization can be successful, but instability of the PIP joint may preclude successful realignment with this method. Arthrodesis of the PIP joint is always an option. Dorsal subluxation can occur after traumatic disruption of the suspensory apparatus and arthrodesis of the fetlock joint to manage this problem, but it most commonly occurs in horses with progressive, severe suspensory desmitis. This is particularly true in the STB or TB racehorse, in which suspensory desmitis is common. Swelling along the dorsal aspect of the pastern region is the first clinical sign recognized, but progressive hyperextension (dropping) of the fetlock joint is usually present. The appearance of dorsal subluxation in any horse with chronic suspensory desmitis is a negative prognostic sign. Dorsal subluxation may also occur in association with transection of a branch of SDFT, severe injuries of the oblique sesamoidean ligaments, or rupture of the straight sesamoidean ligament. In these horses there is usually no associated hyperextension of the fetlock.
Chronic injuries of the oblique or straight sesamoidean ligaments may be associated with dorsal extension of the dorsal articular margins of the PIP joint, presumably a response to low-grade instability of the joint.3,29 This is not synonymous with OA. Although radiological abnormalities may be obvious, such changes are not necessarily associated with pain and lameness.
Dorsal subluxation of the PIP joint can occur without any identifiable structural abnormality of the pastern or metatarsal soft tissue structures. This occurs primarily in the hindlimbs in young horses, and lameness is usually absent or mild. Dorsal subluxation is most often dynamic in nature and resolves during full weight bearing. The presence of changes consistent with OA worsens prognosis. Dorsal subluxation of the PIP joint as a result of mild flexor deformity was reported in three horses. In these horses, ranging in age from 5 months to 4 years, subluxation was believed to be caused by mild contraction of the deep digital flexor tendon (DDFT) without compensatory contraction of the SDFT. Subluxation was seen primarily during early weight bearing, but the condition resolved during full weight bearing. Tenotomy of the medial head of the DDFT in the proximal metatarsal region resolved dynamic dorsal subluxation.32
Wounds and Infection in the Pastern Region
Lacerations and puncture wounds in the pastern region have a high propensity to involve the PIP joint or DFTS. Careful inspection of the wound, radiography, ultrasonography, and analysis of synovial aspirates are often required to determine the extent of the wounds. Wounds that involve the PIP joint or DFTS require aggressive management to prevent synovial infection. Treatments include synovial lavage, wound debridement, drain placement, and systemic and regional antimicrobial therapy with or without tenoscopic examination. Intrasynovial, systemic, and regional perfusion of antimicrobial agents can be used. Sequelae of PIP joint infection include OA. Sequelae of infection of the DFTS include intrasynovial adhesion formation and infectious osteitis of the PSBs (see Chapters 72 and 74).
Infectious disorders of the pastern region can be caused by injuries or hematogenous spread of bacteria, particularly in young horses. Although this chapter is not meant to be a discussion of the treatment of infection, it is important to point out some things of note. Serial radiography, ultrasonography, and MRI are useful for determining the location and extent of the infectious process. Determination of the actual structure involved can be challenging in the pastern region. Regional perfusion of antimicrobial agents is particularly useful in the pastern region to combat infection. Tissue levels can reach as high as 30 times and synovial levels up to 100 times the minimum inhibitory concentration for up to 24 hours after regional perfusion.33 Even horses with obvious bone involvement from infectious phystis/arthritis can be treated successfully with systemic and regional antimicrobial agents and lavage (Figure 35-5).
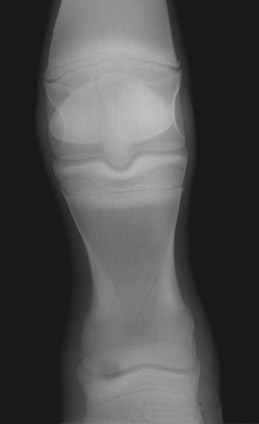
Fig. 35-5 Dorsoplantar radiographic image of a 3-month-old Thoroughbred colt with infectious arthritis/epiphysitis of the proximal aspect of the middle phalanx. Medial is to the left. Note the well-circumscribed radiolucent area in the proximomedial aspect of the epiphysis. The foal was treated with joint lavage and regional perfusion of the digit with antimicrobial agents and made a complete recovery. Presale radiographs obtained 1 year later revealed no detectable radiological abnormality.