Chapter 36 The Metacarpophalangeal Joint
Anatomical Considerations
The metacarpophalangeal (fetlock) joint is an intensely loaded, high-motion joint that is frequently injured in athletic horses. Fetlock region lameness can occur in horses of any occupation, but the joint is at particularly high risk in horses performing at maximal speed. Countering the high load experienced by the joint is the elastic suspensory apparatus that constrains the range of extension. Both the superficial and deep digital flexor muscle tendon units additionally serve to actively support the fetlock joint because of their position on the palmar aspect of the joint. Loss of this active support by the digital flexor tendons may lead to overload of the suspensory apparatus support and some degree of hyperextension. Extreme extension of the metacarpophalangeal joint results in impingement of the proximal rim of the proximal phalanx against the dorsal aspect of the third metacarpal bone (McIII), high compressive forces on the distal, palmar aspect of the McIII opposing the proximal sesamoid bones (PSBs), and both tensile and bending forces on the PSBs intercalated within the suspensory apparatus.1 Complex forces of torsion on the loaded fetlock joint result in a myriad of injuries.
The metacarpophalangeal joint is anatomically composed of the distal aspect of the McIII, the proximal phalanx, and both PSBs. A single synovial space extends on its palmar aspect at least 3 cm proximal to the apex of the PSBs. Dorsally, a bilobed synovial “pad” is located on the proximal dorsal articular rim of the distal aspect of the McIII; this pad presumably functions to help cushion the impingement of the McIII and proximal phalanx. The ligamentous elements of the fetlock joint are complex and important. Well-developed medial and lateral collateral metacarpophalangeal and metacarposesamoidean ligaments constrain the almost purely sagittal motion of this joint, but both abduction and rotation occur.2 The suspensory branches insert on the proximal, palmar abaxial margins of the PSBs and functionally continue through the distal sesamoidean ligaments to attach the distal portion of the PSBs to the proximal phalanx (cruciate or deep and oblique or middle) and the middle phalanx (straight or superficial). The intersesamoidean ligament attaches the axial aspects of the PSBs.
The digital flexor tendon sheath and its contents are described elsewhere (see Chapter 74). The common digital extensor tendon is unsheathed as it passes over the dorsal aspect of the joint. Branches of the medial and lateral palmar and metacarpal nerves primarily supply innervation to the fetlock joint,3 but small subcutaneous branches of the ulnar nerve supply a minor amount of dorsal sensory innervation.
Diagnosis
Careful physical examination to detect heat, swelling (effusion with or without periarticular fibrosis), and pain with palpation or manipulation is critical for diagnosis of lameness of the metacarpophalangeal joint. However, physical findings may be subtle or seemingly nonexistent, whereas diagnostic analgesia often pinpoints the joint or region as the source of pain. Interpretation of fetlock flexion test results should be made with caution because many horses have false-positive responses to forced flexion of this joint, especially if the toe is used to increase leverage. Pain originating in the limb distal to the fetlock joint often is exacerbated by fetlock or lower limb flexion tests. False-negative responses to fetlock joint flexion also are common, especially in horses with subchondral bone injury and chip fractures. Flexion tests are discussed further in Chapter 8. Increased fluid in the fetlock joint can also be a false localizing sign. The presence of an effusion in the absence of heat and pain may indicate some derangement in synovial function but not necessarily point to the source of a clinically relevant lameness. Lameness characteristically occurs with weight bearing and usually, but not always, is worse with the limb on the inside of a circle. If clinical signs do not adequately localize lameness, perineural or intrasynovial analgesia can specify the region relatively easily. In the absence of localizing clinical signs, the foot and pastern regions should first be eliminated as sources of pain by a midpastern digital nerve block with a dorsal subcutaneous ring. Ideally this is followed by intraarticular analgesia of the metacarpophalangeal joint. If the lameness does not improve within 15 to 20 minutes of intraarticular analgesia, the clinician should perform a low palmar block or palmar and palmar metacarpal nerve blocks. In most horses with intraarticular chip fractures, synovitis, capsulitis, and osteoarthritis (OA), lameness improves after intraarticular analgesia. Horses with major fractures, nonarticular fractures, subchondral bone injuries, and tendon and tendon sheath lesions usually are only markedly improved with perineural analgesia. Perineural techniques are superior to definitively abolish pain associated with the fetlock joint. Pain in horses that do not respond to intraarticular analgesia should not necessarily be presumed to originate elsewhere. False-positive results to intraarticular analgesia can also be obtained; lameness associated with a suspensory branch injury or injury of the proximal aspect of the oblique, cruciate, or straight sesamoidean ligaments may be substantially improved or abolished. Subchondral bone pain will not always, or completely, be eliminated with intraarticular analgesia.
Several techniques are used for intrasynovial analgesia of the fetlock joint. One author (DWR) prefers to inject the local anesthetic solution with the horse’s limb on the ground. The dorsal aspect of the fetlock is readily accessible when the horse is bearing weight. As the clinician faces forward and presses the back of his or her arm against the horse’s carpus, a 22-gauge, 2.5-cm needle attached to a 75-cm extension set is inserted horizontally into the dorsal aspect of the joint just proximal to the margin of the proximal phalanx and deep to the common digital extensor tendon. One of us (DWR) uses 10 to 15 mL of 2% mepivacaine, but many practitioners use no more than 6 to 10 mL. One author (SJD) prefers to inject into the palmar pouch through the metacarposesamoidean ligament, with the limb flexed, using a 21-gauge, 3.8-cm needle, injecting 6 to 10 mL of 2% mepivacaine depending on the size of the horse. Other techniques are described in Chapter 10.
Imaging Considerations
The fetlock joint is easy to image accurately because of the size and accessibility. Numerous flexed and oblique radiographic images to specifically silhouette or separate structures help to identify subtle lesions. The same advantages apply to scintigraphic and ultrasonographic imaging. For example, flexed lateral scintigraphic images can help determine whether a lesion in the palmar aspect of the fetlock involves the base of a PSB or the palmar surface of the McIII. A minimum set of radiographs should include dorsopalmar, lateromedial, flexed lateromedial, and both oblique images. The size of the region and absence of overlying soft tissues results in excellently detailed radiographs, even with portable x-ray machines, if suitable screen–film combinations are used or computed or digital radiography is available. A number of specific radiographic images should be obtained if certain lesions are suspected. For example, if a subchondral injury involving the distal palmar aspect of the McIII is suspected, the oblique images should be taken in a more proximal to distal direction than usual. If a lateral condylar fracture is identified, a partially flexed dorsopalmar image should be used to help identify comminution along the distal palmar aspect of the fracture line.4,5 Osteochondrosis of the sagittal ridge of the McIII and incomplete sagittal fractures of the proximal phalanx are lesions that can be difficult to identify in overexposed lateromedial images or underexposed dorsopalmar images, but digital radiography has largely eliminated the need to obtain numerous exposures with different techniques. Reference to the location of soft tissue attachments in the fetlock region is necessary for accurate interpretation.6
Nuclear scintigraphy has proven to be an exceptionally valuable tool to evaluate the fetlocks of active racehorses because so many injuries involve those joints, especially the distal metacarpal/metatarsal condyles. Flexed lateral images and dorsopalmar/plantarodorsal images allow excellent anatomic discrimination of which specific structures in the fetlock region have increased radiopharmaceutical uptake (IRU).7 In particular, flexed lateral and dorsal scintigraphic images can be very helpful to separate palmar metacarpal and PSB uptake. Scintigraphy is also useful for detection of subchondral and trabecular bone injuries in sports horses.8,9
Ultrasonographic evaluation of the fetlock can be valuable for evaluation of tendon and ligament injuries around the fetlock, especially the digital flexor tendons, the palmar annular ligament (see Chapter 74), and the dorsal synovial pad/plica, as well as the bone margins.10,11 Ultrasonography (96%) was more accurate than radiology (44%) in predicting the number and location of osseous fragments on the dorsal aspect of the metacarpophalangeal and metatarsophalangeal joints identified using arthroscopy.12 Three-dimensional imaging modalities such as computed tomography (CT)13-15 (see Chapter 20) or magnetic resonance imaging (MRI) (see Chapter 21) can also be very valuable in the fetlock, especially in areas like the distal palmar McIII condyle, the axial aspect of the PSBs, and the periarticular soft tissues.16-19
Types of Fetlock Joint Lameness
Most fetlock joint lamenesses can be categorized into one of three types:
Conditions specific to the metatarsophalangeal joint and a detailed description of sagittal fractures of the proximal phalanx are discussed elsewhere (see Chapters 35 and 42). Injuries of the digital flexor tendon sheath, superficial and deep digital flexor tendons, the palmar annular ligament, and the proximal digital annular ligament are discussed in Chapter 74. Suspensory ligament (SL) branch injuries are discussed in Chapter 72. Injuries of the distal sesamoidean ligaments are discussed in Chapter 82. Traumatic disruption of the suspensory apparatus is discussed in Chapter 104.
Acute or Repetitive Overload Injuries
Capsulitis/Synovitis
Clinical Signs
Virtually every young racehorse has one or more episodes of metacarpophalangeal capsulitis or synovitis that is characterized by heat, effusion, and pain with flexion. Overt lameness usually is mild and often not evident after the horse warms up. Signs typically manifest as the horse increases the speed and distance of its exercise regimen. If the typical localizing signs are missed, the major indication may be a decrease in performance. In horses with chronic disease, visible thickening of the periarticular tissues usually is noticeable, with decreased range of motion of the joint. In mature sports horses, capsulitis and/or synovitis is less common as a primary condition but is more likely to be associated with sudden-onset moderate to severe lameness.
Diagnosis
A diagnosis of primary capsulitis or synovitis usually is made by clinical observations and the absence of radiological or scintigraphic bony abnormalities. Synovitis and capsulitis may also accompany other causes of fetlock joint lameness, such as chip fractures. Synovial fluid analysis has not been particularly useful in diagnosis or prognosis for most fetlock joint injuries except to help identify infection.
Treatment
In most young horses the condition resolves with nonsteroidal antiinflammatory drugs (NSAIDs), adjustments in training, and increased fitness. Intraarticular hyaluronan (20 mg) is helpful in horses with acute, mild to moderate synovitis, but a combination of hyaluronan with a low dose of a corticosteroid (e.g., 3 to 5 mg of triamcinolone acetonide or 20 to 30 mg of methylprednisolone acetate) is more consistently effective in resolving the clinical signs of inflammation. Injection should be followed by a decrease in exercise intensity for at least 1 to 2 weeks. Postexercise icing of the involved fetlock joints can be helpful. Generic OA treatments, including oral glucosamine with or without chondroitin sulfate, intramuscular polysulfated glycosaminoglycans (PSGAGs), and intravenous hyaluronan merit consideration, but they do not usually yield the consistent response seen with intraarticular therapy. Topical application of 1% diclofenac sodium (Surpass, IDEXX Pharmaceuticals, Inc., Greensboro, North Carolina, United States) appears to reduce inflammation.
Chronic Proliferative (Villonodular) Synovitis
Clinical Signs
Chronic capsulitis/synovitis is caused by repetitive injury of the dorsal aspect of the fetlock joint. The lesion is defined by a thickening of the normally dorsally located bilobed synovial pad that hangs down on either side of the sagittal ridge of the McIII. With extreme extension of the fetlock joint, the dorsal rim of the proximal phalanx impinges on the synovial pad, and repetitive trauma results in its inflammation and subsequent fibrosis. The tissue can become so thick that the dorsal profile of the joint is visibly disfigured. The characteristic swelling is asymmetrical on the midproximodorsal aspect of the fetlock (Figure 36-1) rather than simply spherical in outline as in a typical osteoarthritic fetlock joint (this is called an osselet). Exercise inflames the tissue further, and clinical signs of lameness or diminished performance can result.
Diagnosis
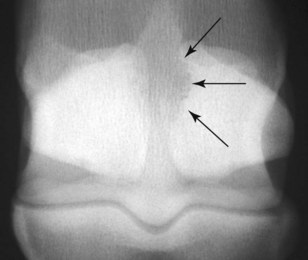
The diagnosis of proliferative synovitis is based on physical examination, radiography, ultrasonography, or a combination of these modalities. The most common radiological sign of the lesion is a crescent-shaped, radiolucent “cut-out” on the dorsal aspect of the McIII at the level of the joint capsule attachment (Figure 36-2). The proliferative lesion may undergo dystrophic mineralization and be radiologically visible. Radiographic contrast studies can be used, but ultrasonography is simpler and more reliable (Figure 36-3). Normal thickness on ultrasonographic examination has been described as less than 2 mm,10,11 but mere identification of a slightly thicker than average structure is certainly not an indication for surgical excision. Many older racehorses have a substantially thicker synovial pad without any associated discomfort. Horses with severe OA have proliferative synovitis in the palmar pouch, and a large concave outline of the distal palmar aspect of the McIII is seen proximal to the PSBs (Figure 36-4 and Figure 34-17), which is associated with a poor prognosis.

Fig. 36-2 Chronic proliferative (villonodular) synovitis of the metacarpophalangeal joint with a typical erosive lesion (arrows) along the proximal dorsal margin of the sagittal ridge of the third metacarpal bone seen in a lateromedial radiographic image. The fibrotic tissue may have small fragments of bone and cartilage or dystrophic mineralization.
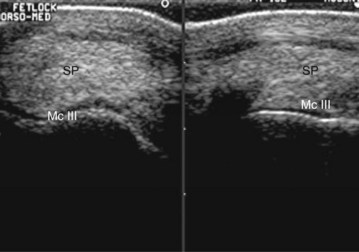
Fig. 36-3 Transverse (left) and longitudinal (right) ultrasonographic images of the distal dorsal metacarpal region. Ultrasonographic examination can confirm a thickened synovial pad, but the diagnosis usually is made based on physical examination and radiological findings. McIII, Third metacarpal bone; SP, synovial pad.

Fig. 36-4 Flexed lateromedial radiographic image of a Thoroughbred racehorse with severe chronic synovitis and osteoarthritis that led to the development of a large erosive lesion of the distal palmar aspect of the third metacarpal (McIII) bone. There is a large concave outline of the palmar cortex of the McIII just proximal to the proximal sesamoid bones.
Treatment
Treatment for proliferative synovitis usually consists of aggressive intraarticular therapy (e.g., hyaluronan and corticosteroids), rest, and alterations in training. Many horses require frequent medication until the joint becomes stiff enough to prevent dorsal impingement. Horses appear to be able to work through this problem as they develop increasing strength and fitness. If the horse does not respond to medical treatment, surgical excision using an arthroscopic technique is recommended.20,21 Surgical debridement must be followed with continued medical treatment and careful attention to the training regimen. It is important to recognize that the thickening of the proximal dorsal synovial pad may be just one part of a chronic, osteoarthritic joint. In such horses, any therapy such as surgery directed solely at this lesion probably will fail.
Osteochondral Fragments in the Synovial Pad
Well-rounded osteochondral fragments in the synovial pad on the dorsoproximal aspect of the fetlock have been described in Warmblood horses in both forelimbs and hindlimbs, either as an incidental finding in presale radiographs obtained at 2 and 3 years of age (n = 102) or in association with fetlock joint pain in mature horses (n = 2).22 Radiological differentiation between these fragments and those that are a manifestation of osteochondrosis may not be possible. However, ultrasonographic examination has confirmed their presence within the synovial pad, and this has been verified at arthroscopic examination and by histology. Histological examination revealed that these fragments consistently comprised an osseous center covered with cartilage on one side and surrounded by fibrous tissue. In a study of 127 joints, multivariable analysis of variance showed a significant association between the presence of a fragment more than 10 mm in length and severe synovial proliferation, wear lines on the dorsal aspect of the McIII, and cartilage erosions. The long-term clinical significance of such lesions has not been determined. The etiology of these fragments has not been established.
Osteoarthritis
Clinical Signs
OA of the metacarpophalangeal joint is common, especially in racehorses, endurance horses, polo ponies, event horses, and show jumpers. There is usually a progression of disease from medial to lateral, reflecting the biomechanical loading of the joint.23 The degree of lameness varies from mild to severe depending on the stage of the disease and recent work history. There is often associated synovitis and/or capsulitis, with palpable distention and/or thickening of the joint capsule. However, the absence of joint effusion does not preclude the presence of OA. There is often resentment of passive flexion of the joint and exacerbation of lameness by flexion; however, the absence of these clinical signs also does not preclude the presence of OA. The range of passive joint motion may be reduced because of increased stiffness of the soft tissues on the dorsal aspect of the joint.
Diagnosis
Lameness is usually abolished by perineural analgesia using a “low four-point block,” but the response to intraarticular analgesia is variable, depending on the degree of subchondral bone pain. Increased intraarticular pressure may be a significant contributor to pain and lameness.24 Radiography usually reveals periarticular modeling on the dorsoproximal aspects of the proximal phalanx, medially more than laterally, with or without modeling of the distal dorsal aspects of the McIII. There may be thickening of the proximal subchondral bone plate of the proximal phalanx. Subchondral radiolucent areas are rare. With advanced OA there may be supracondylar lysis of the distal palmar aspect of the McIII and modeling of the proximal and distal articular margins of the PSBs. In some horses the only radiological change is narrowing of the joint space, reflecting advanced articular cartilage loss and a poor prognosis. It is important not to overlook this and to appreciate its clinical significance.
Treatment
Intraarticular medication with corticosteroids (triamcinolone acetonide) and hyaluronan or PSGAGs is usually effective in early OA, combined with correction of any foot imbalance. Modification of the training program and selection of work surfaces may be important. Local therapy (e.g., whirlpool boots, spa therapy) can be of benefit. The value of oral nutraceuticals is difficult to quantify but may have a management role. Autologous conditioned serum (interleukin–1 receptor antagonist) is being used with increasing frequency with anecdotally favorable results. If the clinical signs are inconsistent with the radiological abnormalities or there is a poor response to treatment, further investigation by exploratory arthroscopy (in the presence of joint effusion) or MRI (in the absence of joint effusion) may be warranted.
Traumatically Induced Cartilage and/or Subchondral Bone Injury
Trauma to the fetlock, the result of hitting a jump, getting a show jump pole tangled between the forelimbs, falling, or stumbling, may result in sudden onset of lameness associated with effusion of the metacarpophalangeal joint.8,25 Lameness is abolished by intraarticular analgesia. At the time of acute onset of lameness there may be no detectable radiological abnormality, and follow-up radiographs may also have no detectable lesion. Although there may be a transient response to intraarticular medication, effusion and lameness usually persist. Exploratory arthroscopy may reveal a focal area of cartilage loss usually on the dorsal distal aspect of the condyle of the McIII, with exposure of subchondral bone, and some softening of the immediately surrounding articular cartilage or peeling off of a large piece of cartilage—a “delamination” injury. Debridement of such lesions invariably results in clinical improvement. If the lesion is located dorsal to the region of maximum weight bearing, the horse may become sound, but lesions on the major weight-bearing aspect result in a guarded prognosis for return to full athletic function.
Alternatively, follow-up radiographs may reveal a radiolucent area in the subchondral bone of the distal aspect of the McIII, seen best in a dorsal 25° proximal-palmarodistal oblique image. Such osseous cystlike lesions are usually associated with an overlying area of full-thickness cartilage loss. Like the cartilage lesions described above, lesions on the weight-bearing part of the McIII usually result in persistent lameness, but some horses have returned to full athletic function following debridement of more dorsally located lesions. However, the presence of extensive wear lines in the articular cartilage reflecting concurrent OA warrants a guarded prognosis. Trauma through an accident while jumping has also resulted in osseous fragmentation of the dorsoproximal medial or lateral aspects of the proximal phalanx. High-detail radiographs may be necessary to differentiate this fragmentation from periarticular osteophyte formation. However, the immediate recognition of such radiological abnormalities soon after an accident is diagnostic of traumatic joint injury rather than OA. Such fragmentation may be associated with a traumatically induced deep groove in the opposing articular cartilage of the distal aspect of the McIII; therefore, although arthroscopic removal of the fragments is likely to result in clinical improvement, long-term repeated intraarticular medication of the joint is likely to be required to maintain soundness. Secondary OA may ensue.
Subchondral Bone Injury
Clinical Signs
Subchondral bone injury is an extremely important cause of lameness involving the metacarpophalangeal joint, especially in racehorses.26,27 Similar lesions are being recognized with increasing frequency in elite endurance horses and also in other sports horses. There are no specific localizing clinical signs in many horses other than variable lameness and an observable diminution in performance. Signs such as heat, swelling, or response to flexion can be absent or extremely subtle, even in horses with overt lameness. Although subchondral bone injury is far more common in racehorses, it appears that single-step overload injuries that focally damage a portion of the McIII or the proximal phalanx can occur in nonracehorses. Such injuries may result in radiologically visible increased radiopacity or radiolucency. The severity of the lameness in such horses can be surprising, and infection may be a differential diagnosis.
Diagnosis
The inconsistent response to local analgesia can make diagnosis difficult unless a reasonably high index of suspicion for these lesions is maintained. Many horses do not achieve soundness with intraarticular analgesia. Horses with full-thickness cartilage injury overlying the subchondral injury may be most likely to experience improvement in lameness because of the access of the local anesthetic agent to the site. Lameness in most horses improves dramatically with low palmar analgesia (four-point block); however, subcarpal analgesia of the palmar metacarpal nerves is sometimes required for complete resolution of lameness.
The two most common locations for subchondral injury of the fetlock in racehorses are the distal palmar aspect of the McIII and the proximal phalanx under the center of the weight-bearing portion of the medial or lateral articular surfaces. The palmar McIII lesion appears to develop as a focal overload injury where the base of the PSB impacts during maximal weight bearing.15,16 In this location, linear or crescent-shaped lucencies are the most common indications of a major advanced subchondral bone injury (Figure 36-5). These often can be seen on a lateromedial image, but special radiographic images may improve the likelihood of seeing a lesion. A slightly flexed, horizontal beam dorsopalmar image silhouetting the distal palmar aspect of the McIII can help define an irregular subchondral outline (Figure 36-6).4,5 Oblique images obtained in a slightly (25 to 30 degrees) proximal-distal direction also allow a better evaluation of the palmar aspect of the condyle and the identification of radiolucent defects (see Figure 42-1).7 With lesions of the proximal phalanx, an increase in subchondral radiopacity may be evident before radiolucent lesions develop, but increased radiopacity in the McIII is much more difficult to recognize, and differentiation between normal adaptive modeling and injury is not easy.

Fig. 36-5 Lateromedial radiographic image of a metacarpophalangeal joint. Subchondral crescent-shaped (arrow) and linear radiolucencies in the distal palmar articular surface of the third metacarpal bone are important radiological findings. Most horses with such lesions have clinical signs of fetlock pain, especially with hard training. The cartilage overlying such lesions is damaged and often unstable.
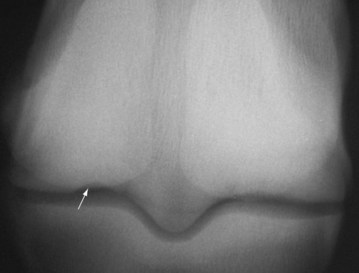
Fig. 36-6 Slightly flexed dorsopalmar radiographic image of the metacarpophalangeal joint is helpful to define lesions (arrow) of the distal palmar aspect of the third metacarpal bone.
Scintigraphy is the most sensitive routine diagnostic tool and can identify lesions in racehorses well before radiological lesions are evident (Figure 36-7). Scintigraphy can also be useful in sports horses (positive in 12 of 15 horses with subchondral and trabecular bone lesions detected using MRI), but if trabecular sclerosis is the principal lesion, then scintigraphy may be negative.8 Even arthroscopic diagnosis can be difficult in the fetlock joint because the anatomical location of these lesions makes evaluation difficult. If the lesions are accessible, the overlying cartilage may be thin or discolored. The amount of cartilage fibrillation or crazing of the joint surface is variable. MRI is expensive but provides more detailed information about the precise location of injury and some information about the type of bone injury, distinguishing early phases of repetitive stress injury (see Figure 107-7).16-19 MRI may reveal areas of reduced signal intensity in T1- and T2-weighted images consistent with mineralization (so-called sclerosis or densification) of the bone. There may also be areas of high signal intensity on fat-suppressed images and low signal intensity on T1-weighted images that may reflect bone edema, hemorrhage, fibrosis, or necrosis. High-field images may also reveal areas of cartilage pathology.
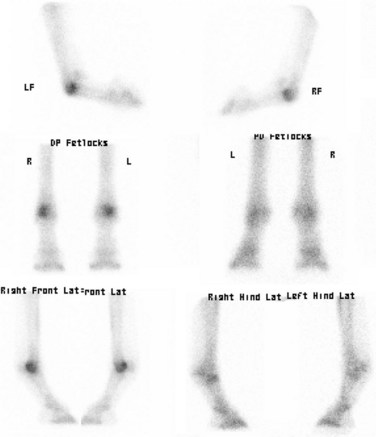
Fig. 36-7 Typical scintigraphic appearance of repetitive stress injury to the distal palmar aspect of the third metacarpal bone. The pattern of increased radiopharmaceutical uptake is made more definitive by comparing standing and flexed lateral images.
In 13 sports and pleasure horses, MRI revealed areas of thickening of the subchondral bone plate and altered signal intensity in the trabecular bone, with mild lesions of one of the collateral ligaments in 5.16 Mediolateral distribution of injuries was similar. Six of 13 horses returned to full function with conservative management.
Treatment
Rest, or at least decreased training intensity, is the most common recommendation for subchondral bone injury in racehorses. It is currently very difficult to define which horses with injury of this location are going to develop more serious problems such as condylar fractures if they continue in hard work. However, in a recent post mortem MRI study of horses (n = 47) subjected to euthanasia on a UK racecourse as a result of a lateral condylar fracture, compared with the contralateral limb (n = 46) and a limb from control horses subjected to euthanasia for unrelated reasons (n = 98), a combined thickness of the subchondral bone and trabecular mineralization of the palmar aspect of the condyle of the McIII of more than 2 cm resulted in an odds ratio for fracture of 4.23 compared with controls.28 Medications such as bisphosphonates (tiludronate), isoxsuprine, and aspirin are frequently recommended; however, there is little information to support their efficacy. Damaged bone can heal if the horse is rested, but the prognosis depends on the amount of structural damage to the overlying cartilage and any loss in the normal architecture of this critical area.
Injuries to the Proximal Phalanx
Osteochondral Fragments: Dorsoproximal Aspect of the Proximal Phalanx
Clinical Signs
The most common chip fracture in Thoroughbred (TB) racehorses involves the proximal dorsal aspect of the proximal phalanx and is an important differential diagnosis in any young TB with acute swelling or heat in a metacarpophalangeal joint. Affected horses rarely are lame for more than 2 days after a fracture and may never show overt lameness. An observant groom or trainer may notice an effusion with some heat, and forced flexion usually causes a painful response. Common historical findings include diminished performance, refusal to change leads, and bearing in or out, especially in the stretch.
Dorsal chip fractures can also be seen in yearlings and nonracehorses as an incidental finding. Most presumably occur as a traumatic event during early development and simply go unrecognized until presale radiographs are obtained. Juvenile fragments occur equally in the forelimbs and hindlimbs, whereas traumatic injuries in active racehorses and sports horses are more common in the forelimbs.
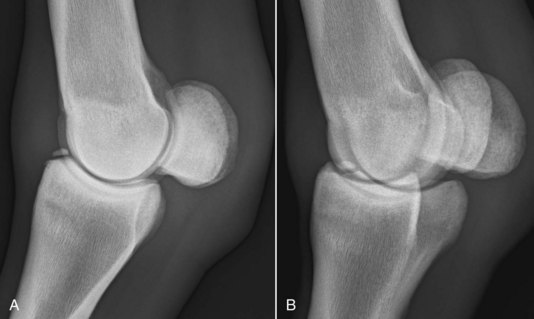
Diagnosis
Chip fractures of the proximodorsal aspect of the proximal phalanx of any size are not difficult to diagnose if they are displaced, but nondisplaced fragments may require nearly perfect radiographs. Most chips occur on the prominence just medial to the median sagittal groove of the proximal phalanx. The left forelimb is slightly more commonly affected than the right forelimb in North American TBs. Bilateral chips are fairly common, and thus radiographs of both fetlocks should be obtained before surgery is performed. The fragments generally are seen best on a dorsolateral-palmaromedial oblique or lateromedial image, depending on the obliquity of the fracture line and image (Figure 36-8, A and B). Correct radiographic technique is especially important for small chips because overexposure burns out the lesion on a lateromedial image and underexposed oblique images do not have enough penetration. Although most radiologically diagnosed fractures are dorsomedial, it is important to evaluate arthroscopically the entire dorsal rim of the proximal phalanx because small chondral fractures are common. Horses in which a dorsolateral fragment is seen radiologically usually also have a lesion on the dorsomedial side. Finally, it is fairly common for fractures to be more evident on early radiographs than on follow-up images because they can become crushed into much smaller fragments pushed back down into the original fracture bed following exercise.
Treatment
Treatment for horses with these chip fractures is less controversial since the advent of arthroscopy. The previous morbidity associated with large incisions on the dorsal aspect of the fetlock to remove rather small fragments made surgical treatment much less attractive. With arthroscopic technique, however, the fragments can be easily and atraumatically removed. An excellent prognosis after a short (approximately 4 to 6 weeks) postoperative convalescence can be given if there are no other degenerative changes in the joint.29-31 In economically unworthy animals, a period of 3 to 4 months’ rest, followed by intraarticular medications as needed, also affords a favorable prognosis, especially if the fragment is not markedly displaced. In our opinion, superior conditioning when these horses return to work helps prolong careers. Injecting a horse with a corticosteroid after it develops an acute chip fracture also can achieve a favorable short-term result and is always a consideration if the horse’s immediate racing demands will not allow a substantial period of rest. However, training and racing a horse with an unstable chip fracture may lead to more rapid degenerative changes in the fetlock. Such horses often have extensive score lines, thin cartilage, and more advanced osteoarthritic changes if the fragment is removed arthroscopically at a later date.
Short Sesamoidean Avulsions (Osteochondral Fragments) from the Palmar Aspect of the Proximal Phalanx
Clinical Signs
Characterization of osteochondral fragments arising from the proximal palmar aspect of the proximal phalanx is somewhat controversial. Many consider these fragments to be manifestations of osteochondrosis because they are recognized in very young, untrained animals. It seems most probable that the fragments result from avulsion of a portion of the incompletely ossified proximal phalanx followed by development of a traumatic secondary ossification center.32,33 The fragments are consistently attached to the short sesamoidean ligament and there is often a small defect in the proximal aspect of the proximal phalanx (Figure 36-9). These fragments are much more common in the hindlimbs (see Chapter 42) and most common in the Standardbred (STB) racehorse. They are also commonly recognized in European Warmbloods. Medial fragments are more common than lateral, but fragments can be numerous and in several limbs. These fragments often are found on presale radiographs, and the relevance to lameness should always be questioned. Many successful athletic horses perform with these lesions. Racehorses in which the fragments affect performance rarely show overt lameness. TBs may be unable to maintain a straight path or fail to change leads properly, and STBs tend to ride a shaft or take a line. Horses in which the lesions cause clinically significant lameness usually have an effusion. Most are not painful to fetlock manipulation. It is possible for fragments in this location to be acute avulsions in older horses, and it is also possible for a fragment that was previously clinically silent to become displaced and painful.

Fig. 36-9 A typical osteochondral fragment avulsed from the proximal palmar/plantar margin of the proximal phalanx. In the dissection, the attachment of the fragment to the base of the sesamoid by the short sesamoidean ligament is evident, as is the smoothly remodeled defect in the rim of the proximal phalanx.
Diagnosis
Oblique radiographic images are best for delineating fragments arising from the palmar proximal aspect of the proximal phalanx. A flexed image helps to further separate the fragment from the base of the PSBs. This separation is useful with proliferative change at the distal dorsal margin of the PSBs or small, basilar sesamoid fractures. Proximal phalangeal fragments usually are well rounded but can also have odd polygonal shapes.
Training a horse after intraarticular analgesia and recognition of improvement in gait should be diagnostic, but the subtle nature of the lameness can make this difficult. Clinical improvement after empirical intraarticular medication also supports the relevance of a radiological lesion. Scintigraphic localization of a lesion may also help confirm the diagnosis, but IRU may be only mild or increased in other parts of the joint, making diagnosis difficult in many racehorses.
Treatment
Treatment consists of arthroscopic removal of the lesion if the clinician is confident that the fragment or fragments are the source of pain causing lameness or if the horse is going to public sale. The most common situation is that the fragments are identified before a horse enters training and the fragments are removed prophylactically. Arthroscopic removal is much less traumatic than arthrotomy for this type of lesion. The prognosis is excellent if the lameness diagnosis is correct.34 If good arthroscopic technique with minimal soft tissue trauma is used, horses require a short convalescence (4 to 6 weeks). Intraarticular injection of corticosteroids with or without hyaluronan can also improve the clinical signs, but surgery is preferable.
Larger Palmar Fragments of the Proximal Phalanx
Large fracture fragments often cause a more obvious lameness than the more common rounded fragments from the proximal palmar rim of the proximal phalanx. They must be distinguished from more palmar fragments that involve the insertions of the true distal sesamoidean ligaments because the latter are not equally good candidates for surgical removal. Very large, acute fractures of the palmar process of the proximal phalanx can be repaired with screws if recognized early (see Chapter 35). Large fragments occur in foals and weanlings, but clinical signs may abate quickly or be nonexistent. Lameness may be evident only when training or racing ensues. In foals, these fragments may be recognized radiologically if there is effusion, mild to moderate lameness, and obvious periarticular swelling. Lameness is seldom commensurate with fragment size. The lesions in foals are largely cartilaginous and can be followed over time as they develop as a separate center of ossification. These fractures should be differentiated from an avulsion fracture at the site of the medial (or, less commonly, the lateral) collateral ligament (see page 410).
Major Fractures of the Proximal Phalanx: Sagittal Fractures
The most common major fracture of the proximal phalanx is a sagittal crack propagating from the proximal sagittal groove. Horses with long sagittal, displaced sagittal, and comminuted fractures developing from an original fracture in the sagittal or frontal plane have obvious localizing signs of swelling and pain. Horses with shorter sagittal fractures may show more subtle signs. Degree of lameness with short, incomplete sagittal fractures is remarkably variable; some horses are almost unable to bear weight, whereas in others the lameness is barely perceptible (see Chapter 35). There is usually effusion of the fetlock joint, pain on manipulation (flexion and twisting), and pain with firm pressure over the middorsal aspect of the proximal phalanx. Sagittal fractures of the proximal aspect of the proximal phalanx are obvious radiologically if they extend more than a few centimeters from the joint surface, but a short, incomplete fracture is very frequently missed without good-quality radiographs. Although historically short incomplete fractures of the proximal aspect of the proximal phalanx were all thought to be dorsally located, recent information from MRI indicates that some short incomplete fractures are located midway between the dorsal and palmar cortices.25 If a dorsal fracture is more than 10 days old, there is usually a definite periosteal change on the dorsal cortex seen on a lateromedial image just distal to the capsular attachments. Initially the change is very indistinct, but within a few more weeks, distinct periosteal new bone is obvious. Whenever proliferative change is seen in this area, the dorsopalmar images should be carefully evaluated for a sagittal fracture. Underexposure results in lesions being missed. However, a fracture midway between the dorsal and palmar cortices will not be associated with periosteal new bone formation, although in a dorsopalmar view it may be possible to detect thickening of the subchondral bone plate in the region of the sagittal groove compared with the contralateral limb. These fractures are more common in STBs than TBs but are also being recognized with increasing frequency in elite endurance horses and frequently involve more than one limb. These fractures also occur in other sports horses,8,35,36 and as in racehorses there is some evidence that preexisting pathological modeling of the bone may predate fracture. Even though these fractures are short and indistinct, they may cause surprisingly severe lameness. The clinician should always suspect such fractures because blocking followed by lunging, high-speed training, or pasture exercise may catastrophically propagate the fracture (Figure 36-10). For management and prognosis, see Chapter 35.
Dorsal Frontal Fractures of the Proximal Phalanx
See Chapters 35 and 42 for a discussion of dorsal frontal fractures of the proximal phalanx.
Conditions of the Proximal Sesamoid Bones
Sesamoiditis
Clinical Signs
The PSBs are an integral part of the suspensory apparatus and metacarpophalangeal articulation. They are susceptible to injury in all athletic horses, but particularly in those that perform at speed. Lameness resulting from sesamoiditis in sports horses is comparatively rare. Sesamoiditis is a clinically distinctive condition, although it is poorly characterized pathologically. There is usually pain with direct, firm palpation over the abaxial aspect of the affected PSB(s) and sometimes pain with fetlock flexion. Often, however, the lameness is manifest only after hard exercise. It is important to recognize that the radiological detection of an increased number and size of vascular channels may be an incidental finding. In a study to determine prevalence of radiological changes in the repository radiographs of 1162 TB yearlings selling in Kentucky, most yearlings (98%) had radiologically apparent vascular channels in the PSBs.37 Irregular channels (>2 mm wide or with nonparallel sides) were more common (79%) than were regular vascular channels (56%). In a second study, race performance of these yearlings was studied. Yearlings with enthesophyte formation of the PSBs in the hindlimbs placed in a significantly smaller percentage of starts and earned significantly less money per start; however, the presence of abnormal vascular channels did not appear to influence performance.38 However, the evidence is conflicting. In a study of 487 TB yearlings, those with vascular channels with nonparallel sides and more than 2 mm in width had a reduced number of race starts at 2 years of age and reduced earnings at 2 and 3 years of age compared with normal horses. Contour of the PSBs did not influence performance.39 In a longitudinal radiological study of 71 2-year-old STBs examined at 3-monthly intervals over 1 year, 22% had no vascular channels and 55% had one or two vascular channels less than 1 mm in width, which did not change and did not influence performance. Three or more vascular channels less than 1 mm wide were seen in 13% of horses at the start of the study; the percentage decreased with time as some horses were removed from training. If lameness was observed, it was attributed to suspensory desmitis or superficial digital flexor tendonitis. Seven horses (10%) had wide abnormally shaped vascular channels, all of which were considered to be associated with lameness during training.40 In a radiological study of 753 STB trotters in Norway examined between 6 and 21 months of age, the presence of radiological abnormalities did not influence race earnings at 3 and 4 years of age.41
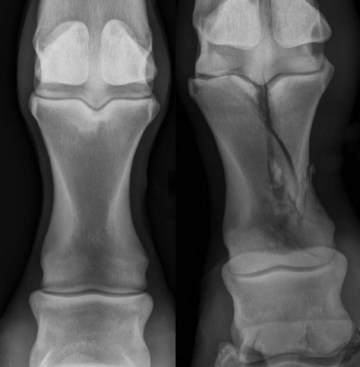
Diagnosis
The pain causing lameness is eliminated with perineural, but not intraarticular, analgesia. Radiological evidence of sesamoiditis involves four basic changes: marginal osteophytes, enthesophytes, enlarged vascular channels, and focal radiolucent defects (Figure 36-11). Marginal osteophytes occur at the proximal dorsal and distal dorsal extremities of the PSBs. Best seen on lateromedial images, these lesions represent later changes of generalized OA of the fetlock joint and usually can be considered a poor prognostic sign. Enthesophytes occur along the palmar aspect of the proximal half of the abaxial ridge of the PSB or the distal third of the bone at the sites of origin of the distal sesamoidean ligaments. These changes are frequently abaxial in location and therefore seen best on oblique images. Interpretation of vascular channels in the PSBs is always subjective. The direction of any linear radiolucency is important to note; vascular channels have a radial orientation, whereas hairline fractures usually extend farther and are closer to transverse (parallel to the ground) (Figure 36-12).

Fig. 36-11 Sesamoiditis lesions have a range of radiological pathology, including enlarged vascular channels, radiolucency, and enthesophytes.

Fig. 36-12 Very subtle transverse lucencies in a proximal sesamoid bone can be an indication of an incomplete fracture (left). A midbody fracture (right) developed in a race a few weeks after the radiograph on the left was obtained.
True radiolucent changes that are not associated with the normal trabecular pattern or vascular channels may indicate infection (see Chapters 72 and 74). Such lesions may arise after known trauma to the region, especially a penetrating injury. Such lesions are usually extremely painful on palpation. A second important differential diagnosis is an avulsion fracture at the attachment of the palmar annular ligament (see Chapter 74). Radiolucent defects of hindlimb PSBs have also been described as a sequel to routine catheterization of the dorsal metatarsal artery for the measurement of intraoperative arterial blood pressure, with the development of severe lameness within 21 days of surgery.42 It was speculated that the lesions may be caused by ischemic necrosis or hematogenous spread of bacteria.
Nuclear scintigraphy is exceptionally useful for diagnosis of sesamoiditis and can identify early changes and help confirm whether a chronic radiological change is currently active. A complete series of scintigraphic images, including standing lateral, flexed lateral, and dorsal, can aid in exact localization of a lesion within a particular PSB.
Treatment
Treatment of horses with sesamoiditis is difficult and usually involves enforced rest and symptomatic treatment to counter inflammation and pain. Many racehorses with sesamoiditis are clinically helped considerably by postexercise icing and altered training regimens, such as swimming. It seems to be easier to manage older, proven racehorses with sesamoiditis by such methods than younger, unraced horses. Aspirin and isoxsuprine have been used, but there is no reliable evidence for efficacy. Shock wave therapy is probably the best current therapeutic option for horses with active sesamoiditis, although its efficacy and mechanisms of action are still debatable. Tiludronate has also been used for sesamoiditis and may have some rationale, but there is no good information about its efficacy.
Proximal Sesamoid Bone Fractures
There is anatomical variation in configuration of PSB fractures, substantially influencing clinical signs and outcome. Biaxial PSB fractures are a potentially catastrophic injury. A recent post mortem study indicated that TB racehorses with severe PSB fractures (75 of 121 fractures were transverse midbody fractures) had a higher exercise intensity in the previous 12 months compared with horses with other musculoskeletal injuries or other causes of death.43
Clinical Signs
Because the PSBs are such important elements in the suspensory apparatus and support of the fetlock joint, fractures are usually associated with obvious clinical signs of heat, swelling, and pain with flexion or direct pressure, as well as an obvious weight-bearing lameness.
Diagnosis
Lameness caused by most PSB fractures is eliminated or greatly reduced by intraarticular or perineural analgesia. Apical, midbody, and basilar fractures of the PSBs usually are easy to diagnose radiologically with routine views. Abaxial fractures more frequently are missed and are best demonstrated by a lateral proximal-medial distal or medial proximal-lateral distal oblique image that is tangential to the abaxial surface of the suspect PSB. This projection also is useful in determining whether the fracture is articular. Axial fractures usually are associated with displaced condylar fractures of the McIII or third metatarsal bone (MtIII). Diagnosis requires a well-penetrated dorsopalmar image that is well positioned. Even slight obliquity obscures the fracture line. Midbody fractures frequently have wedge-shaped, comminuted fragments present at the abaxial margins. They should not be confused with the overlapping lines of the palmar and dorsal cortices that occur because of fracture displacement and failure to obtain the radiograph directly through the fracture line.
Ultrasonography can be a valuable adjunct in evaluating PSB fractures because soft tissue attachments of the SL, intersesamoidean ligament, and distal sesamoidean ligaments can be simultaneously injured.
Apical Fractures
Apical fractures comprising less than 30% of the bone occur primarily in racehorses, but they can occur in all types of horses. Forelimb apical PSB fractures are much less common than hindlimb injuries in racing TBs44,45 and STBs.46 In sports horses this injury is most common in event horses and show jumpers. These injuries are caused by a combination of bending and suspensory tensile forces. In young STBs the fracture is particularly common in the right hind lateral PSB. Horses with apical PSB fractures are usually mildly to moderately lame unless a concomitant SL injury is present. Although lameness in some horses has been managed successfully with rest alone, arthroscopic removal of the fractured fragment generally is recommended. Both prognosis and convalescent time depend on fragment size and presence of suspensory desmitis. Horses with small, apical fragments without major SL ligament injury can resume training within 4 to 6 weeks after surgery, especially if they were fit at the time of injury. Horses with large fragments usually associated with suspensory branch injury may need 6 to 12 months of convalescence and have a poor prognosis. The prognosis for return to racing was poorer for forelimb injuries than hindlimb injuries in racing TBs. In horses less than 2 years of age, 55% of 11 horses with a forelimb fracture raced after arthroscopic removal of the fragment, whereas 86% of 139 horses with a hindlimb injury raced.44 In horses 2 years of age or more, 67% of 30 horses with a forelimb fracture returned to racing after surgery compared with 83% of 54 horses with hindlimb injury. In both age categories, fracture of a medial PSB significantly reduced the likelihood of return to racing.45
Abaxial Fractures
Abaxial fractures are true avulsion injuries involving the insertion of the SL on the abaxial surface. Most involve a narrow rim of the articular surface and can be removed by an arthroscopic approach. Displaced fragments should be removed, whereas extremely large fragments can be repaired with 3.5-mm screws. Horses with nondisplaced fragments sometimes can be treated with rest. The prognosis depends on the size of the fragment and the concomitant suspensory compromise. In a study of 47 horses, predominantly TB and Quarter Horse racehorses and Western performance horses with an abaxial sesamoid fracture, 38 had a forelimb fracture, usually of the medial PSB. Nonracehorses had a better prognosis for return to full athletic function (6/6, 100%) after arthroscopic removal of the fracture compared with racehorses (25/35, 71%), with only 16 of 35 (46%) racing at the same class as preinjury.47
Basilar Fractures
Basilar fractures of the PSBs are seen in all athletic horses and are treated according to configuration.48,49 Horses with smaller, wedge-shaped fragments that do not extend more than 50% to 75% of the dorsopalmar width of the PSB are clear candidates for surgical excision of the fragment (Figure 36-13). Such fragments do not heal with rest and cause persistent lameness, presumably because of instability and incongruity at the articular surface. The prognosis with arthroscopic technique is at least 50% for return to athletic function because the distal sesamoidean ligaments are not disrupted. Horses are usually given 4 to 6 months of rest after removal of such fragments (3 months with very small pieces). Nonarticular fractures can be removed via an incision in the straight sesamoidean ligament, and 9 of 10 horses from a variety of disciplines returned to their intended use.50

Fig. 36-13 Lateromedial radiographic image of a metacarpophalangeal joint. There is a basilar sesamoid fracture (arrow). Small, triangular, basilar sesamoid fragments that do not involve the major distal sesamoidean ligaments are appropriate candidates for arthroscopic removal.
Horses with larger, basilar PSB fractures that extend to the palmar aspect of the bone have the poorest prognosis because fractures often are substantially displaced and involve a greater proportion of distal sesamoidean ligament origin (Figure 36-14). They also are more difficult to repair than midbody fractures because of the size and shape of the fracture. The prognosis for horses with large, displaced, or comminuted basilar PSB fractures is poor for return to any reasonable level of athletic activity.

Fig. 36-14 Flexed lateromedial radiographic image of a metacarpophalangeal joint. There is a large displaced basilar sesamoid fracture (arrow). Large basilar fractures are very difficult to successfully repair. There are extensive attachments of the distal sesamoidean ligaments; therefore the prognosis associated with surgical removal is poor.
Some horses with severe OA develop small basilar fractures. These fractures typically are more rounded, irregular, or multiply fragmented than acute chip fractures (Figure 36-15). Acute chip fractures have a sharply demarcated triangular shape. Horses with these degenerate basilar fractures are very poor candidates for any surgical treatment, and horses have a grave prognosis for return to athletic activity. Radiologically evident narrowing of the joint space between the PSB and the McIII (Figure 36-16) and the development of a radiological “waist” in the distal aspect of the McIII are associated signs of severe OA (Figure 36-17).

Fig. 36-15 Dorsomedial-palmarolateral oblique radiographic image of a metacarpophalangeal joint. There are fragments distal to the proximal sesamoid bone (arrow). Irregular, “crumbled” fragments from the base of the proximal sesamoid bone usually are seen in joints with moderate to severe osteoarthritis. Note also the modeling of the articular margins of the proximal phalanx.

Fig. 36-16 Lateromedial radiographic image of a metacarpophalangeal joint. Note the loss of space between the proximal sesamoid bones (PSBs) and the third metacarpal bone (McIII) (arrows). Near-complete loss of joint space between the McIII and the PSBs can precede that between the distal aspect of the McIII and the proximal phalanx. Horses with this degree of cartilage damage are often candidates for euthanasia or arthrodesis.

Fig. 36-17 Slightly oblique flexed lateromedial radiographic image of a metacarpophalangeal joint. Development of a “waist” around the proximal joint margin on the third metacarpal bone, both dorsally and palmarly (white arrows), is indicative of severe, chronic osteoarthritis. There is a pronounced defect of the distal palmar aspect of the third metacarpal bone (black arrows).
Midbody PSB Fractures
Midbody fractures of the PSB can occur in any horse, but they usually are seen in racehorses. In North American TBs, the medial PSBs of the forelimb are most commonly affected. In the STB, hind lateral midbody PSB fractures are most common. Numerous surgical techniques have been used to repair such fractures, including cast coaptation alone, bone grafting and casting, lag screws (distal to proximal or proximal to distal) with or without cancellous grafting, and hemicerclage wiring and graft.51,52 Regardless of the technique used, midbody PSB fractures are serious injuries, and horses require an extended period of rest after surgery. With surgery, 60% to 70% of horses with midbody fractures can return to athletic function, but most horses drop substantially in class. The owner or trainer should be advised that almost a year of convalescence is required for horses with such injuries.
Axial PSB Fractures
Axial PSB fractures are nearly always seen in combination with displaced lateral condylar fractures of the McIII or MtIII (Figure 36-18). They are recognized radiologically only on a dorsopalmar image, and it is difficult to determine fracture depth. Some fractures involve deep gouges in the articular surface, and most are avulsions by the intersesamoidean ligament. They usually are not treated specifically because of inaccessibility and the likelihood that the condylar fracture and overall joint damage will limit return to function. Recognition of an axial PSB fracture is important primarily as an indicator of more severe trauma to the joint and a poorer prognosis. The prognosis for a horse returning to race after this injury is extremely poor.53 Early metacarpophalangeal arthrodesis should be seriously considered in horses with a displaced axial sesamoid fracture.

Fig. 36-18 Displaced lateral condylar fracture of the third metacarpal bone with a nondisplaced axial fracture (arrows) of the lateral PSB (left). In horses with very badly displaced lateral condylar fractures, the axial fragment of the PSB can become completely avulsed (right). Clinicians should look for axial PSB fractures in every horse with a displaced lateral condylar fracture. This type of fracture is associated with a very poor prognosis for return to racing.
Intraarticular Fragmentation Associated with Suspensory Branch Injury
The distal dorsal aspect of the branches of the SL are subsynovial and therefore intimately associated with the fetlock joint. Occasionally in association with injury of the medial or lateral branch of a SL, there is associated distention of the fetlock joint capsule; in a flexed lateromedial radiographic image, several small osseous fractures can be identified on the proximal dorsal aspect of the ipsilateral PSB. Such fracture fragments must be surgically removed for a successful outcome. Prognosis depends on the severity of the suspensory branch injury.
Intersesamoidean Ligament Injury
Intersesamoidean ligamentous injury without fracture is difficult to diagnose unless it is accompanied by radiolucency along the axial aspect of one or both PSBs (Figure 36-19). Affected horses often are extremely lame even at a walk. Scintigraphy frequently identifies an area of intense, focal IRU. The intersesamoidean ligament also can be evaluated ultrasonographically to a limited extent. The ligamentous lesion may be visible and debrided arthroscopically, but it is not known if this alters the outcome. Horses generally are treated with support bandages and stall rest for several months. The prognosis for return to high-level athletic activity appears to be guarded, especially with conservative management, but a large series of horses has not been reviewed. Lameness resolved in eight horses treated by surgical debridement.55 Differential diagnosis for radiolucent lesions in the intersesamoidean region also includes osteomyelitis.37 If an infection is the cause of the bone loss, horses typically have more obvious localizing signs, such as joint capsule and digital flexor tendon sheath distention, and the prognosis is poor.
PSB Fractures in Young Foals
PSB fractures in young foals (apical, abaxial, midbody, and basilar) can occur at pasture and appear to be underdiagnosed because clinical signs are surprisingly subtle and foals often are not thoroughly examined for mild lameness. Because most fractures involve only one PSB and the suspensory apparatus is still functional, severe lameness does not develop. Clinicians should look for subtle clinical signs of fetlock region swelling, pain with flexion, and pain with pressure over the PSBs in any foal with mild to moderate lameness. Several bones can be affected. Signs often abate quickly, especially in young foals (<2 months of age), in which these fractures are most common. Good-quality radiographs are essential because the fractured apical, basilar, or abaxial fragments are often poorly mineralized. Unlike in older horses, PSB fractures in foals frequently progress to form a bony union (see Figures 128-6 and 128-7). If the fragments have any displacement, however, an enlarged PSB can result. These oversized PSBs often are diagnosed in yearlings or 2-year-olds on prepurchase or presale radiographs. Surprisingly, enlargement of the fetlock joint is usually difficult to detect. Although some horses have raced successfully with enlarged PSBs, this abnormality can be a source of lameness as the horse proceeds in training.
PSB fractures in foals are essentially a management problem. Avoidance of situations in which a young, weak foal has to chase its dam around a large pasture to the point of exhaustion can prevent many fractures. It is essential to slowly return foals back to pasture if they have been stall confined for any reason. Early recognition of lameness in foals can allow diagnosis before the fragments become markedly displaced. Early diagnosis improves prognosis considerably because minimally displaced fractures nearly always heal completely with rest alone. Uncontrolled exercise by the foal must be avoided because the degree of displacement dictates the eventual PSB deformity. Surgical treatment of foal PSB fractures is primarily indicated in markedly displaced fractures close to the midbody of the bone. A suturing technique with high-tensile–strength flexible fiber is probably the best current option.
Fractures of the Third Metacarpal Bone
Condylar Fractures
Clinical Signs
The most important fracture of the fetlock joint is that involving the condyles of the McIII. They occur almost exclusively in racehorses and elite endurance horses, usually only when horses are running at racing speeds. This is also an occasional injury in event horses. Because the fractures involve a major weight-bearing surface, most horses are overtly lame, with clear localizing signs of pain and swelling. Most are very positive to any manipulation of the fetlock. Degree of lameness often does not directly correlate with the degree of displacement. Many horses with incomplete, acute fractures are lamer than one with a clearly displaced, complete fracture. This is particularly true with incomplete medial fractures. Although it appears that many horses that develop condylar fractures have preexisting subchondral damage of the distal palmar aspect of the condyle,27,56 the majority do not have a strong history of previous fetlock lameness (see Chapter 42 for fractures of the MtIII).
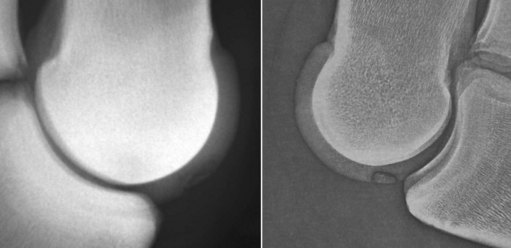
Diagnosis
Radiological diagnosis is not difficult in most horses. A dorsopalmar image should be centered over the condyle and the x-ray beam directed 15 to 20 degrees downward. If the beam is too horizontal, the PSBs may obscure the distal articular surface of the McIII. Lesions may be missed if images are underexposed. The most common fractures involve the lateral condyle and clearly propagate toward the lateral cortex. Some extend only 1 to 2 cm proximally from the joint surface, and these can be particularly difficult to see without good-quality radiographs. Lateral condylar fractures rarely spiral or extend into the middiaphysis. Medial condylar fractures, however, usually extend up the diaphysis in a spiraling fashion or have an occult Y-shaped configuration at the middiaphysis. It is essential to remember the difference between lateral and medial fractures. Horses with medial condylar fractures must have a complete, high-quality set of radiographs that encompass the entire length of the McIII in an attempt to identify fracture configuration. Most importantly, the owner or trainer must be informed immediately of the substantial risk associated with medial fractures, especially those involving a hindlimb.
The prognosis for horses with displaced, lateral condylar fractures, regardless of treatment, is much poorer for return to function compared with those with nondisplaced fractures. This is almost certainly the result of a combination of preexisting disease of the fetlock joint and the magnitude of damage done to the joint when the fracture occurs. Accurate prognosis requires radiographic examination of the palmar distal aspect of the McIII. The radiographer should slightly flex the fetlock and use a horizontal beam to obtain a dorsopalmar image (Figure 36-20). This helps to define comminution of the condyle along the fracture margin, as well as subchondral radiolucent defects that may have preceded the fracture.

Fig. 36-20 A standard dorsopalmar image of a lateral condylar fracture obtained at a 10- to 15-degree proximal to distal obliquity will separate the distal aspect of the third metacarpal bone from the base of the proximal sesamoid bones (left), but a dorsopalmar image obtained with the fetlock slightly flexed is needed to silhouette the distal palmar margin of the bone where comminution typically occurs (right).
Most horses with condylar fractures are best treated with lag screws. Nondisplaced or minimally displaced fractures can be repaired through stab incisions alone, but arthroscopic evaluation of the joint should allow a more accurate assessment of the prognosis. Displaced fractures require accurate reduction of the distal articular surface, so they must be reduced under arthroscopic guidance or through an open incision. Horses with medial condylar fractures should undergo surgery with extreme caution because catastrophic failure in the middiaphysis can occur during recovery from general anesthesia or even several days to weeks after repair (see Chapter 42). Horses with spiral fractures extending the length of the diaphysis may be successfully repaired with carefully positioned lag screws alone, but those with medial fractures that disappear in the middiaphysis should be repaired with a bone plate combined with lag screws across the condyle. Most complications of condylar fractures occur because of a failure to recognize potential problems before surgery. Even if certain complications cannot be entirely avoided, forewarning the owner of the risks is advisable.
Other fractures of the distal third of the McIII bone are discussed in Chapter 37.
Osteochondrosis
Sagittal Ridge of the Third Metacarpal Bone
The most common site of osteochondrosis in the metacarpophalangeal joint (excluding proximal palmar lesions) is the dorsal sagittal ridge of the McIII/MtIII (Figure 36-21).57 These lesions often are clinically silent, but mild to moderate effusion and lameness may be noted. They are often diagnosed in weanlings or on yearling presale radiographs. They are best seen on a dorsopalmar image or a slightly underexposed flexed lateromedial image. If no fragment is obvious and clinical signs are minimal, it is advisable to rest the horse for a couple of months because some healing may occur, especially in younger horses. Arthroscopic debridement is an option, but the resulting bony defect will remain evident, and thus the likelihood of a rewarding sale price is lessened. If the lesion does not fill in radiologically by the spring of its yearling year, arthroscopic evaluation may be suggested. A completely conservative (i.e., nonsurgical) approach is justified if the clinical signs are minimal. The prognosis likely depends on the size of the lesion. Horses with lesions more proximal on the sagittal ridge may have a better prognosis than those closer to its distal aspect.
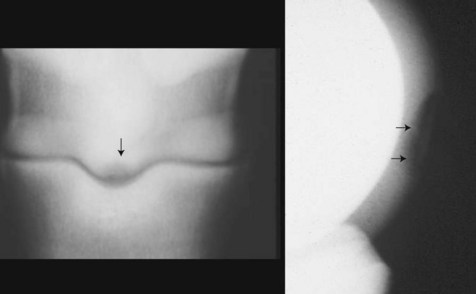
Fig. 36-21 Dorsopalmar (left) and flexed lateromedial (right) images of a metacarpophalangeal joint. Note the radiolucent defect (arrow) in the sagittal image in the dorsopalmar image and the smoothly outlined defect in the dorsal aspect of the sagittal ridge (arrows) of the third metacarpal bone in the lateromedial image.
In older horses, traumatic chip fractures may occur on the distal aspect of the sagittal ridge in a similar location to that of typical osteochondrosis (Figure 36-22). This injury may occur in jumpers striking an obstacle with the fetlock joint in a palmarly flexed position. These fragments usually are unstable and should be arthroscopically removed. The prognosis is favorable if the fragment is fairly small.
Osseous Cystlike Lesions of the Third Metacarpal Bone
Osseous cystlike lesions of the distal aspect of the McIII/MtIII occur on the weight-bearing surface of the condyle and may be a manifestation of osteochondrosis. Most occur in the medial condyle and are diagnosed in yearlings or early in training as a 2-year-old. The lesions are easy to recognize radiologically, and horses have obvious lameness exacerbated by lower limb flexion. Perineural analgesia and scintigraphy also localize the problem. Surgical debridement has been the typical treatment, and the reported results are unexpectedly favorable.58
Collateral Ligament Injury
The fetlock joint has strong anatomical constraints, and the equine limb and gait have a strongly sagittal orientation; therefore mediolateral instability is relatively uncommon except after severe trauma (e.g., foot in a hole or lower limb in a gate or fence). Mild forms of collateral desmitis are suspected in horses with pain on fetlock manipulation, focal pain, and swelling over the affected ligament or lameness exacerbated with valgus or varus stress. The diagnosis is confirmed by ultrasonographic examination. However, localizing clinical signs may be absent, and if a horse has pain causing lameness localized to the fetlock region by perineural analgesia and little response to intraarticular analgesia, then the collateral ligaments should be included in a routine ultrasonographic assessment of the periarticular structures. It must be borne in mind that the deep and superficial components of each collateral ligament cannot be evaluated simultaneously because of their different fiber orientations. Radiographs usually are not helpful unless there is an avulsion fracture or lack of congruency of the joint surfaces. However, radiographic examination is important if there is joint laxity because there may be concurrent intraarticular fragments. Joint instability is most likely to be demonstrated on non–weight-bearing, valgus or varus stressed dorsopalmar (plantar) radiographs.
Treatment of horses with collateral ligament injury usually consists of rest and adequate external coaptation. The fetlock is an inherently stable joint in the sagittal plane; thus minimal support is necessary unless the injury is severe. If the joint is very unstable, a cast extending to the proximal metacarpal region is maintained for 4 to 6 weeks. If the injury is not overtly unstable, a single polyvinyl chloride pipe splint applied on the side ipsilateral to the collateral injury should be adequate. The duration of rest should be based on clinical soundness, palpable stability, and the ultrasonographic appearance of the ligamentous tissues (see Chapter 17). Shock wave therapy for insertional desmopathies may be beneficial, but firm data are still unavailable. Stem cells, acellular matrices, and platelet-rich plasma are also empirically used. Eight of 16 horses with rupture of a collateral ligament of the metacarpophalangeal or metatarsophalangeal joint returned to pleasure riding after casting for a mean of 71 days.59
Collateral ligament avulsion injuries involving the insertion on the proximal phalanx are perhaps the most commonly recognized fetlock collateral ligament injury. These may easily be mistaken for the more common dorsal chip fractures on oblique views, but careful scrutiny reveals that the fragment is too far abaxial for a typical chip fracture (Figure 36-23). If a fracture is seen abaxial to the apex of the dorsal eminences of the proximal phalanx, the fragment is almost certainly not going to be from the typical articular margin location. In addition, the fracture can also usually be seen in an abaxial position on a dorsopalmar (dorsoplantar) image. These fragments often involve a portion of the articular margin and cause lameness. Arthroscopic removal should be performed, but it can be difficult because of the limited space on the medial or lateral aspects. The arthroscope portal should be dorsoproximal on the same side as the lesion. The instrument portal should be just dorsal to the edge of the collateral ligament. The fragments may be tightly attached along the abaxial margin, and an arthroscopic scalpel or other sharp dissection tool may be needed to separate them. The most important issue with these fragments is that the clinician accurately discriminates between them and a more typical articular margin fracture; otherwise, the surgical procedure may be very frustrating.

Fig. 36-23 Collateral ligament avulsions from the proximal phalanx are usually visible on the dorsopalmar (left) and the oblique (right) radiographic images. On the oblique image, these fragments appear a long way from the third metacarpal bone and that distinguishes them from a typical dorsal proximal phalanx chip fracture.
Traumatic Disruption of the Suspensory Apparatus
See Chapter 104 for a discussion of traumatic disruption of the suspensory apparatus and associated catastrophic injuries.