10 Treating concussion, central pain and emotions
The term concussion as used in this chapter refers to two quite different concepts of “concussion”. The first is the concept of a medically diagnosed concussion also called a traumatic brain injury (TBI) or closed head injury and is defined as an alteration in mental status, with or without loss of consciousness, accompanied by a brief period of amnesia after a blow to the head. The second, more subtle, concept means any shock or trauma to the system that has a direct or indirect impact on the medulla or brain stem.
A traumatic brain injury (TBI) is associated with loss of consciousness, post-traumatic amnesia in which the patient cannot remember the events leading up to the trauma for periods up to several days and focal neurological signs (de Kruijk 2002). A mild traumatic brain injury (mTBI), the most common form of concussion, is usually defined as one in which loss of consciousness (LOC) is less than 30 minutes and the Glasgow Coma Scale (GCS) score is more than 13 at the time of injury. A GCS score of 3 signifies deep coma and a GCS score of 15 signifies a fully alert and oriented patient spontaneously conversing and following commands. In an mTBI, the patient may have incomplete memory of the traumatic event and post-traumatic amnesia (PTA) of less than 24 hours and may have been dazed and confused at the scene without loss of consciousness. An example would be the driver of the target vehicle in a rear end accident who does not remember the sound of the impact or who does not remember anything between the time she saw the impact vehicle approaching and the time several minutes later when the police officer arrived at the car window (McCrea 2002, McAllister 2002, Ropper 2007, Ryan 2003).
Both TBI and mTBI are associated with post-concussive symptoms of cognitive, emotional and behavioral disturbances that can persist for months or years after the injury. These symptoms include headache, difficulties with attention, concentration and memory and the sequencing and processing of information, problems with mood including irritability, aggression and emotional lability, sleep disturbance, fatigue, dizziness and perhaps photophobia, hyperacussis or nausea although these tend to be more problematic immediately after the injury.
Incidence of traumatic brain injuries
There are 1.5 million traumatic brain injuries affecting 128 people per 100,000 in the United States every year and even though 85% are considered mild they result in significant disability and unemployment due to the cognitive, psychological and social dysfunction they cause (Ropper 2007). Sports and bicycle accidents account for the majority of cases among 5–14-year-olds and falls and motor vehicle accidents are the most common cause of concussion in adults. Post-concussive syndrome or post-concussive symptoms (PCS) refer to a constellation of signs and symptoms that may be reported after a TBI of any severity. Post-concussive symptoms affect up to 50% of mTBI patients at one month and 15–25% at one year. Some post-concussive patients never return to their pre-morbid function (Alves 1993, Middelboe 1992). Litigation and compensation factors involved in injuries sustained in the workplace or in auto accidents are thought to affect both symptom reporting and rates of recovery (Mooney 2005).
CT scans should be done to evaluate the need for neurosurgical intervention, even in the presence of a normal neurological examination, if the patient is under 16 or older than 65 years of age, has a GCS of less than 15 within 2 hours after the injury, two or more episodes of vomiting, retrograde amnesia for greater than 30 minutes prior to the trauma or is taking anticoagulants (Ropper 2007). CT and MRI scans while easily available and adequate to diagnose gross pathology such as hematoma, frank swelling or depressed skull fracture are not sensitive enough to show the subtle reductions in cortical perfusion, frontal and temporal hypometabolism and diffuse axonal injuries that have been demonstrated on PET or SPECT in mTBI patients with persistent PCS. Several studies have demonstrated abnormal frontal and temporal lobe activity with PET and SPECT scans in TBI/PCS patients whose CT and MRI scans were normal (Gross 1996, Ruff 1994, Humayun 1989, McCrea 2008).
Pathologies associated with TBI
Multifocal axonal injuries, increased permeability of the axonal membrane due to inflammation and activation of the glial system, disruption of axonal neurofilaments leading to disruption of axoplasmic flow and secondary axonal deafferentation in the areas of the brain served by the damaged axons have been observed after mild brain trauma in both human and animal studies (Oppenheimer 1968, Blumbergs 1994). Human postmortem studies have shown loss of cortical cholinergic afferents that would account for dysfunction in hippocampal cholinergic neurons and the resulting symptoms of memory loss and difficulty with information processing (Dixon 1994, Saija 1988, Murdoch 1998, Dewar 1996). Even mild brain injury has been shown to produce evidence of diffuse axonal injuries (Povlishock 1989, 1992, 1995). Sleep disturbances common in TBI patients are thought to be produced by injury to the reticular activating system that regulates sleep–wake cycles.
Imbalance, disequilibrium, particular problems with task sequencing, vision dependent balance and panic attacks during sleep or in visually complex settings may reflect damage to the endolymphatic system, eighth nerve or the vestibular apparatus in the inner ear. Damage to the inner ear can greatly confound and complicate PCS symptoms because some of the symptoms overlap but the diagnosis and successful treatments are completely different.
There are no universally effective treatments for post-concussive symptoms (Bazarian 2005). Tincture of time produces some recovery of function. Cognitive behavioral counseling for patients and their families at the time of the injury helps patients deal with the deficits, creates realistic expectations and reduces anxiety about symptoms. Medications and various strategies are used to modify post-concussive symptoms.
Complaints of sleep disturbance seen in 30–70% of TBI patients are particularly difficult to manage because medications for sleep disturbance such as the benzodiazepines and other sedative hypnotics mimic or exacerbate the post-concussive complaints of fatigue and cognitive dysfunction. But the sleep deprivation itself may exacerbate the post-concussive symptoms of cognitive dysfunction, fatigue, irritability and anxiety. Non-pharmacologic interventions such as the teaching and reinforcement of sleep hygiene and relaxation training promote functional recovery. The use of low dose anti-convulsant medication at night may be the best choice for medical management since it can address multiple symptoms of sleep disturbance, headache and chronic neck pain.
Dysfunction in the cholinergic, catecholaminergic and dopaminergic neurotransmitters may all contribute to cognitive impairment. It is clear that disruption in cortical cholinergic function is a primary source of cognitive dysfunction but some patients respond best to cholinesterase inhibitors and others to psychostimulants that increase catecholamine levels. Both classes of medications are intended to improve attention and working memory although it is advisable to start with low doses and titrate up in small increments (McAllister 2002).
In spite of these strategies symptoms from TBI persist for years following even mild head trauma and create significant disability. In 1999 the National Institutes of Health declared mTBI and post-concussive sequelae to be a major public health problem (NIH 1999).
Van Gelder’s concussion model
The second concept of concussion is particular to one physician, a Dutch osteopath and naturopath from Australia who trained in England in the 1930s and came to practice in Vancouver, British Columbia in 1946 (Van Gelder 1985, 1989). Harry Van Gelder was mentioned in Chapter 1 of this text and it is he who bought the practice that came with the 1920s machine that came with the list of frequencies that allowed him to treat a multitude of physical conditions and complaints successfully using electromagnetic resonance along with other therapies. Although somewhat eccentric, Harry Van Gelder was beloved and acknowledged by those he treated as being superbly effective and skilled as a diagnostician and healer. He developed a more subtle concept of “concussion” to mean any shock or trauma to the system that had an impact on the medulla or brain stem. Van Gelder’s skill, reputation and clinical outcomes lead to the consideration of this more subtle condition as a treatment focus.
Functions of the medulla
The medulla is located at the base of the brain and carries the ascending and descending tracts that connect the brain with the spinal cord. The medulla also gives rise to cranial nerve X, the vagus nerve. The vagus influences every vegetative function including, but not limited to, respiration and bronchodilation, heart rate and blood pressure and digestion through its regulation of the esophagus, stomach, small intestine, gall bladder, and the secretions of the pancreas and stomach. It contributes to immune system regulation by regulating secretions in the thymus. It supplies the motor parasympathetic functions of all of the viscera except the adrenal glands.
In Van Gelder’s model of injury and illness, trauma to the medulla made it function inefficiently and created dysfunction in all of the vegetative systems including the immune system, the cardiovascular system and the digestive system. The trauma to the medulla also created dysfunction in the pituitary and the endocrine organs it regulates by changing regulatory impulses in the fibers that connect the medulla to the pituitary.
The trauma to the medulla could be physical and caused by a fall, a blow to the head or any sort of physical injury that stretched or stressed the neck and brainstem. The trauma could be from emotional shock producing a flood of impulses from the viscera pouring into the medulla via the vagus. The medulla effectively becomes overloaded by overwhelming input rather like a circuit breaker that switches off during a power surge causing the system to function less effectively. The trauma could be from “chill” or any sort of event such as infection, exhaustion or toxic exposure that shocks the viscera creating a flood of impulses from the viscera through the vagus to the medulla causing it to “switch” into something like a “safe mode”. The vagus and the medulla simply function less effectively than they did prior to the trauma. The analogy between a computer or power system and the medulla moving into a less effective but “safe mode” is an apt one. The “safe mode” preserves the most important critical functions and allows for repair and recovery at some later time.
In Van Gelder’s model, trauma leads to “paralysis” which leads to “allergy reaction” and reduction in secretions and vitality. “Paralysis” does not refer to a true medical paralysis or complete loss of function. Once again the analogy to the loss of function when a computer “locks up” and loses the ability to move to the next step is most apt. Computers move smoothly from one step to the next because of a continual flow of “do this – then do that” lines of instruction. The computer “locks up” because it has lost the line of code that tells it what to do next and becomes “paralyzed”. The frequency to remove “paralysis” is Van Gelder’s conceptual equivalent of the computer command “control–alt–delete” that reboots the computer system.
In Van Gelder’s system, as well as in our medical understanding of physiology, the body’s first response to any dysfunction is to release histamine as a way of starting the inflammatory cascade. The third problem, after “trauma” and “paralysis” that assails the medulla as it moves into “safe mode” is a histamine release or allergy reaction making the medulla less efficient by reducing both secretions and vitality and initiating inflammation as a means of repair and recovery. The loss of efficiency in the immune, digestive and endocrine systems caused by the malfunction in the medulla and vagus leads to a variety of allergy reactions and health issues while the system slowly initiates the repair process.
Treating the “constitutional factors”
Van Gelder became a physician at a time when the concept was developed that genetic factors could be turned off or turned on by life events or exposures predisposing the person to various illnesses. These genetic factors were called “constitutional factors” and probably correspond to what modern genetics calls single nucleotide polymorphisms or SNPs, places on the gene that are altered from the ideal or wild type. The constitutional factors had colorful descriptions that related them to susceptibility to the diseases of the day such as gonorrhea, syphilis and tuberculosis but they were effectively genetic predispositions to various ailments.
The practicing clinician will be familiar with the relationship between susceptibility to illness and patient family histories even if the concept of constitutional factors is not familiar. If every one of 100 people in a room is exposed to a certain bacterium only a certain percentage will contract the disease while some will fight it off successfully and a few seem not to even notice the exposure. Why is that? Van Gelder would say that the patients who fell ill had the genetic “constitution” that made them susceptible to the bacterium. Modern physicians trained in immunology and genetics would say that the immune systems of the patients who fell ill were less effective in fighting the bacterium because the minute receptors on the lymphocytes were less vigorous in defense. One interpretation of the event is more poetic and the other is more scientifically informed but different susceptibilities to illness are a known fact no matter how one chooses to interpret the causation.
The same patterns become apparent when interpreting patient family histories of illness. Physicians take a family history because it gives clues about what the individual’s risk is of contracting certain diseases. One patient will have a family history in which every adult over the age of 40 has diabetes as well as some primary relatives who have asthma and a few with multilevel disc disease and one with sarcoidosis. No one in the family suffers from alcoholism or psoriasis. The genes or SNPs would almost surely be related to inflammation and insulin regulation and the constitutional factor is related to the susceptibility to tuberculosis. Another patient will have a family history replete with stroke, heart disease, degenerative but not rheumatoid arthritis and hypertension but no one has diabetes, psoriasis or psychosis. Another will have psoriasis, eczema, irritable bowel as a personal diagnosis and in the family history but no family history of heart disease or diabetes. Another patient will have a family history replete with alcoholism and psychosis or other mental illnesses but no incidence of diabetes or heart attack. These patterns in family medical history are familiar to every practicing physician whether one chooses to interpret them in the light of modern genetics or in the light of turn of the century medical practice. Van Gelder’s device had one specific frequency that seemed to neutralize all of the constitutional factors.
Using Van Gelder’s model
Van Gelder’s model of restoring the patient to full function involved clearing “concussion” from the medulla, restoring secretions to the pituitary, turning off constitutional factors and the final step was to restore “vitality” to the system and “balance the energy centers.” This model is clearly not part of mainstream medical training or practice and it would be simpler not to teach it as part of an FSM pain treatment program taught to traditionally trained physicians.
A 6-week trial was done in which the “concussion protocol” was not performed on any of the week’s 90 patients in order to assess whether it was actually essential to the outcomes achieved. The patients but not the practitioners were blinded to the change in treatment protocol. Within a few weeks it became clear that outcomes, while not quantified, had declined and treatment results were less favorable even when every other therapy and protocol were applied as before. By the end of the 6-week trial the “concussion protocol” was again used on a regular basis and outcomes returned to their normal positive level in the week’s 90 patients. Subsequent shorter trials with both the patients and the practitioner blinded produced the same pattern of effect on outcomes.
Van Gelder’s reputation as a master physician and healer was the original reason for considering using and teaching his more subtle concussion model. The model continues to be used and taught because it produces results that cannot be achieved if it is not used. It is left to the reader to decide from personal experience whether treatment of this more subtle interpretation of concussion contributes to positive outcomes in pain management.
Concussion protocol treatment outcomes
Treatment for this mild form of “concussion” described by Van Gelder was among the first FSM protocols used in practice. Patients reported improvements in sleep, mood and general wellbeing that were both subtle and profound sometimes years after a mild head injury and even when they could recall no head trauma. Encouraged by these results, FSM was used in patients with post-concussive symptoms from brain trauma, including TBI, mTBI and stroke. One to four treatments produced consistent profound improvements in sleep, mood, cognitive function, information processing, emotional stability and fatigue in hundreds of case reports from over 1000 practitioners after 12 years of use. Only the headache has proven to be somewhat resistant to treatment. In seriously injured patients more than four treatments may be necessary and the improvements may never last for more than a few days if neural tissue has been lost. Significant objective and subjective improvements have been observed in multiple case reports from numerous clinical centers in the US and abroad.
Concussion protocol increases serotonin
The data acquired through micro-immunochromatography demonstrated that the concussion protocol produced a significant but probably temporary increase in serotonin levels. Serotonin decreased during the treatment that reduced pain in fibromyalgia patients (see Chapter 8). When the pain reached 0/10 VAS or had stopped decreasing the protocol was changed and for the next 30 minutes the patient was treated with the “concussion protocol”. The patient was blinded to the change in treatment. Serotonin levels dropped during the pain reducing portion of the treatment in every patient treated and rose with use of the concussion protocol from an average of 175.75ng/ml (± 40.20) to 244.34ng/ml (± 76.05) in each of 16 different patients whose samples were collected during the 2-month test period. The normal range for serotonin is 100–300ng/ml.
The average increase in serotonin in the 30 minutes from the zero VAS time point to the end of the concussion protocol was 68.59 ± 54.79 for a 39% increase. One patient’s serotonin level more than doubled increasing from 155.2 to 337.6ng/ml. The Wilcoxon Signed Ranks Test result was Z = −3.52 p<0.001.
These anecdotal reports give some basis to pursue an organized controlled trial including neuroimaging such as PET and SPECT scans to provide some objective evidence to validate the observed clinical improvement.
Diagnosing concussion
If the patient presents acutely after head trauma, the practitioner should perform whatever neurological examination is within their training and scope of practice. If the patient has not been evaluated in an emergency department, has focal neurological signs, is under 16 years of age or older than 65 years of age, had a GCS of less than 15 within 2 hours after the injury, had two or more episodes of vomiting after the injury, retrograde amnesia for greater than 30 minutes prior to the trauma or is taking anticoagulants, the practitioner should order a CT scan to rule out intracranial lesions or hemorrhage.
The acute signs of concussion may include headache, nausea, photophobia, sleepiness, irritability and mental confusion including problems with word finding, memory and orientation. The acute concussion protocol is described below and would be used in this patient if the CT scan were negative or if the injury was not severe enough to require a CT scan.
Unless the practitioner reading this text is a neurologist it is unlikely that the patient’s presenting complaint will be post-concussive symptoms. The PCS symptoms may be incidentally mentioned in passing or not mentioned at all in a patient that is some months or even years post head injury.
The systems engineer referred for treatment of chronic neck and shoulder pain provided a rambling, tangential and disorganized history of the auto accident that occurred 2 years previously but did not complain of having post-concussive symptoms. When asked she admitted that she was having trouble organizing projects at work, was fatigued and had trouble sleeping but attributed these problems to pain. A typical systems engineer without post-concussive symptoms provides an organized, sequential and detailed history often presented in writing. The brain MRI ordered after this patient’s visit showed a small focal lesion said to be unrelated to the trauma although no basis for this determination was provided.
Treatment with FSM and nutritional supplements helped reduce the symptoms. The diagnosis was based on observation and questioning when the quality of the history did not match the patient’s job description and presumed premorbid level of function. The basic concussion protocol included in this chapter was used on this patient in addition to more advanced protocols for chronic concussion in other areas of the brain and her symptoms were significantly improved.
There were frequencies for five general sections of the brain on the list of frequencies acquired from Van Gelder – the forebrain, midbrain, hindbrain, medulla, pineal and pituitary. The midbrain is the site of the thalamus. Concussion and post-concussive symptoms can affect any or all brain areas and questions should be asked that query the functions of each part of the brain so it can be determined which areas are most in need of treatment. Treating these areas of the brain requires a level of understanding of neurology and an appreciation of the profound effects that can be produced by FSM on nervous system tissue that are not generally available to students reading a basic level FSM text in pain management. There are protocols for treatment of acute brain injuries and chronic brain conditions taught in the FSM Core and Advanced seminars and the student who has an interest in treating these conditions would find these courses useful.
• History: Directed questioning may reveal symptoms the patient does not associate with the injury. Be aware that the patient may not be an accurate historian or may simply lack the self awareness to assess their own performance and cognitive function. When there is any doubt the patient’s family should be consulted.
• Memory and decision making problems: Are you having any problems with being forgetful? Are you having any unusual problems with memory for numbers, names, facts or words? Is decision making any more of a problem for you now than it was before the accident?
• Task sequencing: Is it difficult for you to accomplish projects that require multiple steps? Are you having problems performing errands in sequence, getting a meal on the table, or planning multistep projects?
• Sleep disturbance: Are you having any problems with getting to sleep or staying asleep?
• Fatigue: Are you more fatigued than you were before the injury? Do you fatigue more easily than you did before the injury?
• Mood: Are you more anxious, irritable, or depressed than you used to be? Do your moods shift more easily than they used to? Do you find yourself yelling or losing your temper more often than is normal for you?
• Balance and co-ordination: Do you have any new problems with balance? Can you walk around your home when you get up at night in the dark or do you need a light on? Do you fall or bump into things more often than usual?
• Hormones: Are you having any menstrual cycle irregularities (progesterone and estrogen balance)? Are you having any prostate symptoms (testosterone and estrogen balance)? When did you start having problems with acne (testosterone excess)? Have you had any weight gain since the trauma (insulin and blood sugar regulation)? Has your libido changed from what is normal for you (testosterone)? Do you awaken with hot flashes or have episodes of sweating since the accident (cortisol, estrogen)? Are you more fatigued than seems normal? Do you have difficulty performing or recovering from exercise? Are you depressed for no apparent reason (growth hormone)?
• Imaging: Unless the patient has severe symptoms or meets the criteria that require a CT scan acutely it is not necessary to order routine diagnostic imaging. MRI, PET and SPECT scanning are more revealing in chronic mTBI and the practitioner is encouraged to find a neurologist specializing in brain injuries as a referral resource.
Treating concussion – the concussion protocols
• The patient must be hydrated to benefit from microcurrent treatment.
• Hydrated means 1 to 2 quarts of water consumed in the 2 to 4 hours preceding treatment.
• Athletes and patients with more muscle mass seem to need more water than the average patient.
• The elderly tend to be chronically dehydrated and may need to hydrate for several days prior to treatment in addition to the water consumed on the day of treatment.
• DO NOT accept the statement, “I drink lots of water”.
• ASK “How much water, and in what form, did you drink today before you came in?”.
• Coffee, caffeinated tea, carbonated cola beverages do not count as water.
Frequencies
Channel A/condition frequencies
The frequencies, listed in the usual order of use, are thought to remove or neutralize the condition for which they are listed except for 81, 49 / which are thought to increase secretions and vitality respectively
| 970 / | |
| 94 / | |
| 321 / | |
| 9 / | |
| 40 / | |
| 284 / | |
| 81 / | |
| 49 / | |
| 18 / 62 | |
| 51 / | |
| 3 / | |
| 91 / | |
| 19, 43, 46 |
A / B Pairs
6.8 / 38
• Remove or reset constitutional factors.
• 6.8 / 38 is an A/B pair in which channel A is not a condition and channel B is not a tissue. The desired effect is created by the two frequencies delivered simultaneously in an interferential field. This frequency combination appears to neutralize all of the genetic factors described by Van Gelder and the physicians of the early 1900s and generally makes people feel more grounded and steadier.
35 / 102
• / 102 was the frequency on Van Gelder’s list for the pineal gland which secretes melatonin and regulates sleep wake diurnal cycles. Melatonin is a powerful antioxidant and has some anti-tumorgenic activity in preventing breast cancer and other cancers. In Van Gelder’s understanding, this frequency also resonated with the energy center at the top of the head known as the “crown center” when combined with 35 / on channel A. If the practitioner’s belief system does not include the concept of energy centers, then the frequency can be used with the intention to simply address the physical structures. This frequency combination usually makes patients feel lighter and more relaxed. The affect of the frequency combination and the outcomes achieved do not appear to be affected by the practitioner’s belief system.
Channel / B tissue frequencies
There is some debate in the FSM community as to what anatomical brain structures are included in each area. The divisions are probably imprecise and somewhat arbitrary. Response to treatment helps to disclose what functions reside in which brain part in any particular patient.
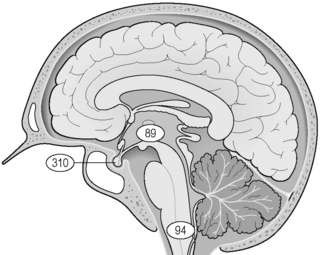
Figure 10.1 • The frequencies for portions of the brain treated with the concussion protocol or treated to remove central pain are shown in the diagram above. / 94 is the frequency for the medulla. / 310 is the frequency for the anterior pituitary. / 89 is the frequency for the midbrain and is used for pain syndromes involving the thalamus.
Midbrain: ___ / 89
• The “midbrain” is part of the mesencephalon and includes the tectum, the pretectum, the inferior and superior colliculi, the cerebral peduncle, the midbrain dorsal and ventral tegmental areas, the crus cerebri, the substantia nigra, and the cerebral aqueduct and may also include third ventricle, thalamus, hypothalamus, subthalamus, subcortical system, the amygdala (limbic system), hippocampus (limbic system). For the purposes of this chapter it has been found to successfully treat central pain and is assumed to address the thalamus and periventricular, responsible for central pain.
Solar plexus: ___ /200
• The solar plexus is an archaic term for the celiac nerve plexus of the vagus nerve just below the sternum in the epigastric area of the abdomen. This frequency is thought to address both the nerve plexus and the energy center located in this area. If your belief system does not include the concept of energy centers then the protocols can be used simply to address the physical structures. The frequencies used and outcomes achieved will not change.
General concussion protocol
Channel A condition / Channel B tissue
94 / 200 – Nervous tension
• Literally translated this frequency removes “trauma” from the solar plexus but Van Gelder used it to reduce nervous tension. It is observed to have a calming effect and to begin increasing serotonin levels.
• Treatment time: Use this frequency for at least 1–2 minutes depending on clinic time demands and the patient’s condition. If the patient is very tense and time allows this frequency may be used for up to 5 or 10 minutes.
970 / 200 – Emotional tension
• Literally translated this frequency combination balances the emotional component or removes emotional stress from the “solar plexus” and Van Gelder described it as reducing emotional tension. It is observed to have a calming effect and begins increasing serotonin levels.
• Treatment time: Use this frequency for at least 1–2 minutes depending on clinic time demands and the patient’s condition. If the patient is very tense and time allows this frequency may be used for up to 5 or 10 minutes.
94 / 94
• Remove concussion from the medulla.
• If the memory of some recent trauma is replayed in slow motion in the mind’s eye it will become apparent that there are two parts to any trauma. The first is the pain of the physical injury. The second is the “fact” of the trauma and the surprise or shock to the system that it represents. It is the “fact” of trauma and the shock to the system that is thought to be removed by using 94 /.
• Treatment time: In general all of the frequencies in the “concussion protocol” are used for 2 minutes each but if time allows and the patient’s condition requires it 94 / 94 has been used for as long as 10 minutes. If time allows, the indicators such as tissue softening or warmth discussed in Chapter 2 can be used to determine when it is time to change the frequency. If the practitioner and the patient are not sensitive to tissue softening or a feeling of warmth or induced euphoria, the practitioner can use the frequencies in a standardized protocol for 2 minutes each with good effect. The automated FSM units run each of the frequencies for 2 minutes.
94 / 310
• Remove concussion from the anterior pituitary.
• Treatment time: In general all of the frequencies in the “concussion protocol” are used for 2 minutes each but if time allows and the indicators such as tissue softening or warmth demonstrate that patient’s condition requires it, 94 / 310 has been used for as long as 10 minutes.
6.8 / 38
• Remove or reset constitutional factors arising from trauma, chill, exhaustion, toxic exposure or emotional shock. This frequency combination is an A/B pair always used together for treating “constitutional factors”. It appears to neutralize all of the genetic factors described by Van Gelder and the physicians of the early 1900s and generally makes people feel more grounded and steadier.
35 / 102
• /102 was the frequency on Van Gelder’s list for the pineal gland which secretes melatonin and regulates sleep wake diurnal cycles. Melatonin is a powerful antioxidant and has some anti-tumorgenic activity in preventing breast cancer and other cancers. In Van Gelder’s understanding, this frequency also resonated with the energy center at the top of the head known as the “crown center” when combined with 35 / on channel A. If the practitioner’s belief system does not include the concept of energy centers, then the frequency can be used with the intention to simply address the physical structures. The affect of the frequency combination and the outcomes achieved do not appear to be affected by the practitioner’s belief system.
When to use the general concussion protocol
The general concussion protocol as described by Van Gelder for “restoring health” is used on virtually every patient regardless of the presenting complaint for which they are being treated. For patients whose primary complaint is head injury the concussion protocol is used on the first visit and on every subsequent visit until maximum improvement has been achieved.
The general concussion protocol should be used on the second treatment visit for most chronic pain patients unless a head injury was involved in the mechanism that created the presenting complaint. Pain produces “concussion” in Van Gelder’s concept of medulla overload via visceral input so treating the concussion without reducing the pain is self defeating. Treat to reduce the pain first if possible then treat with the concussion protocol. Patients may return and ask for repeat treatment with the concussion protocol and this is not a problem. It has been used daily with no ill effects observed. The practitioner is advised to self treat at least once a week and any time there is unusual stress.
If the concussion protocol is to be used on infants, treat the mother and have her hold the child with skin contact. It has been used in autistic children and adolescents, a wide range of pain and general medicine patients and in the elderly and there has been no report of adverse effects occurring with use of the general concussion protocol on any patient except as noted below.
 Precaution side effect – induced euphoria
Precaution side effect – induced euphoria
The concussion protocol often produces a profound euphoric affect that is more pronounced the first few times it is used. Some patients become very relaxed and many will fall asleep. This temporary phenomenon will wear off as the other frequencies are used at the end of the treatment protocol. The patient will remain relaxed and should come to full function within an hour or so after treatment. Most patients are in full possession of their faculties by the time they are ready to leave the clinic and most report sleeping better on the night of the treatment.
Precaution: The practitioner should take care to ensure that the patient is safe to drive before allowing them to leave the clinic. In extreme cases patients have been warned against making important financial decisions until the effect has worn off.
 Precaution side effect – dizziness
Precaution side effect – dizziness
A very small percentage of patients who have vestibular injuries respond to the frequency 94 / 94 by becoming dizzy. No patient should be left unattended during the first treatment until the response to 94 / 94 has been assessed. This may be simply a very strong euphoric effect that has been interpreted as being vertiginous but it is not pleasant and may be concerning to the patient. The effect stops as soon as the frequency is changed away from 94 / 94 to some other channel A frequency. Use the remaining portion of the concussion protocol and avoid using 94 / 94. 94 / and other brain frequencies may be used with no ill effect. Only 94 / 94 has been observed to produce this temporary effect. In extreme cases if the side effect persists the patient may need one dose of an over-the-counter motion sickness pill to reverse it. This side effect has only been observed in a very small percentage of patients who have vestibular injuries. Not all patients with vestibular injuries will respond to 94 / 94 by becoming dizzy. If it occurs the patient should be evaluated at a vestibular testing center or by a vestibular specialist.
Treatment application
• Current level: Average current level 100μamps. Use lower current levels around 40–60μamps for children or very small or debilitated patients. Use higher current levels closer to 200–300μamps for larger or very muscular patients. Do not use more than 500μamps as animal studies suggest that current levels above 500μamps reduce ATP formation while current levels below 500μamps increase ATP.
• ± Polarization: Current is used in alternating mode. Alternating DC current is actually pulsed DC (direct) current that alternates its polarity from positive to negative.
• Waveslope: Use a moderate to waveslope for the general concussion protocol and chronic brain issues. Use a gentle waveslope in acute brain injuries. The waveslope refers to the rate of increase of current flow on the leading edge of the square wave. A sharp waveslope has a very steep current up ramp on the leading edge of the ramped square wave and a gentle waveslope has a gradual current up ramp on the leading edge.
• Patient position for all concussion applications: The patient can be placed in any comfortable position in which the body is well supported. Patients can become very relaxed during this protocol and may fall asleep so the head and trunk should be well supported.
• Lead placement for all concussion applications: The nervous system is an information processing system and is designed to respond to input in the form of patterns that include frequencies and even thought or emotion (Pert 1997, Lipton 2005). Consequently the frequencies for any brain structure seem to have an effect no matter where in the body they are applied. The leads can be applied any place that is convenient as long as the current and frequencies from the two channels cross in an interferential pattern.
• Graphite gloves at the neck or abdomen: The two positive electrodes may be placed in the jacks cemented to the back of one graphite glove and the two negative electrodes may be placed in the jacks cemented to the back of the second graphite glove. Graphite is a good current conductor and the glove itself may have an additional positive effect for reasons not completely understood. The gloves should be sprayed or moistened with water to improve conductivity or placed in small wet fabric contacts such as a wash cloth and placed on the skin of the abdomen and back, or on the front and back of the cervical spine.

Figure 10.2 • The graphite gloves must be moistened with water in order to conduct current comfortably. Dry graphite gloves create a strong prickling or stinging skin sensation and are quite uncomfortable. Ordinary tap water contains enough minerals to make it an effective conducting medium. Make sure the gloves are wet and place them flat on the skin with good contact. The skin will produce minute amounts of moisture from the galvanic skin response during treatment that will maintain comfortable conductivity for the average treatment.

Figure 10.3 • The concussion protocol uses only alternating current so habit is the only consideration that directs placement of positive and negative leads. One moistened glove with the two positive leads from channel A and channel B should be placed on the low back. And the other moistened glove with the two negative leads from channel A and channel B should be placed on the abdomen. The photograph shows a towel under the low back but the graphite glove could be used without being wrapped in the fabric contact.

Figure 10.4 • Place the two positive leads from channel A and channel B in a warm wet fabric contact (face cloth) using either a graphite glove or two alligator clips attached to the contact. Place the two negative leads from channel A and channel B in a warm wet fabric contact (face cloth) using either a graphite glove or two alligator clips attached to the contact. Position the contacts to ensure that they do not touch each other, which would direct current to the contacts instead of the patient and do not touch the patient’s ears which would send current through the brain.

It is not necessary to run the current or the frequencies through the brain in order to affect the brain tissues. DO NOT run current through the brain.
• Adhesive Electrode Pads: Place adhesive electrode pads anywhere on the patient’s body such that the current from channel A and the current from channel B crosses in three dimensions. For example if the positive lead from channel A is placed on the back of the right shoulder then the negative lead from A can be placed on the lower left abdomen. Then the positive lead from channel B would be placed on the back of the left shoulder and the negative lead from channel B would be placed on the lower right abdomen.
Treating central pain
When to treat central pain
The normal function of the thalamus in the midbrain is pain suppression. The rapid reduction of the sharp pain that follows abrupt contact between the shin and the edge of the coffee table is produced when the midbrain suppresses the ascending pain signals from the anterior tibia. Injuries to this part of the brain can change it from a pain suppressor into a pain generator.
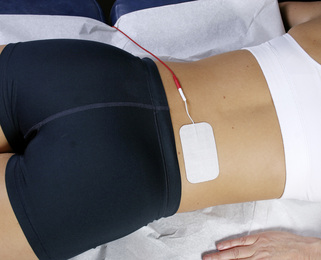
Figure 10.5 • The gel electrode pads can be used if they are more convenient. The pads need to be placed so the current and frequencies from the two channels make an “X” and cross through the patient in an interferential pattern. Place the gel electrode pads attached to the positive lead from channel A on the right side of the low back.

Figure 10.6 • Place the gel electrode pads attached to the negative lead from channel A on the left side of the abdomen.
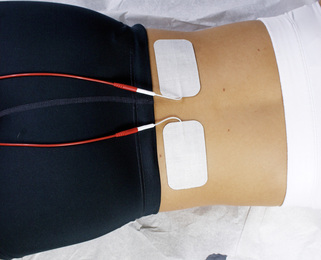
Figure 10.7 • Place the gel electrode pad attached to the positive lead from channel B on the left side of the low back. The gel electrode pads attached to the positive leads from channel A and channel B should be side by side at the low back as shown.
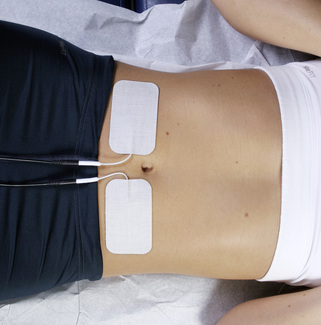
Figure 10.8 • Place the gel electrode pads attached to the negative lead from channel B on the right side of the abdomen. The gel electrode pads attached to the negative leads from channel A and channel B should be side by side on the abdomen as shown.
Central pain arises from deafferentation injuries that affect the thalamus and pain processing centers in the brain. The full body pain is described as intolerable, aching, burning, stabbing, deep, boring, sharp, dull and emotionally bothersome to a degree not seen in any other type of pain. Central pain can occur after any brain trauma such as surgery, a stroke or head injury that affects the pain processing centers in the brain. If the stroke or brain injury was on the right side of the brain the patient will have pain on the left side of the head and body. If it is in the central portion of the thalamus it will be bilaterally symmetrical and will include the head and face (see Fig. 10.9). Central pain is unresponsive to opiates and to most medications and refractory to virtually every treatment.
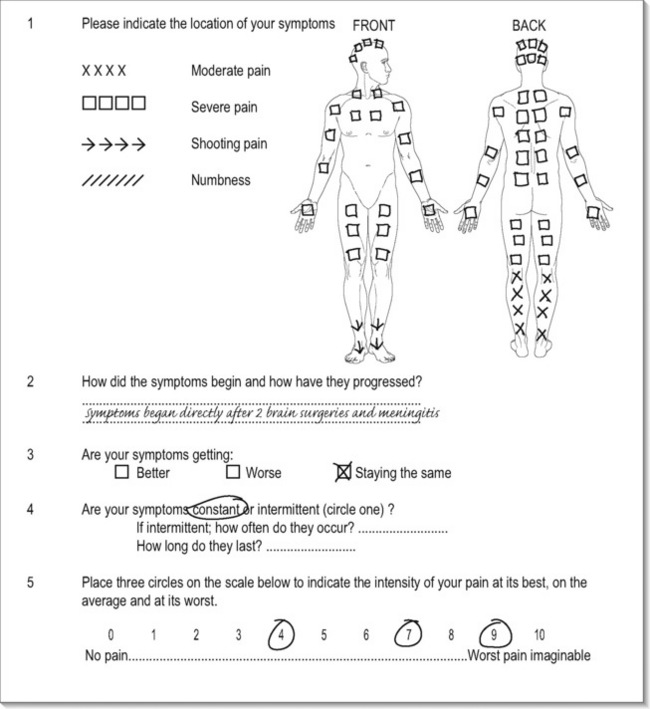
Figure 10.9 • This is the pain diagram of someone with central pain onset on the day after she had a second brain surgery to remove the second part of a pituitary tumor. It is similar to the pain diagram seen with fibromyalgia from spine trauma (CTF) except that it includes the face and head. This feature helps distinguish central pain from CTF. Central pain includes the head; fibromyalgia from spine trauma does not. Using 40 / 89 on this patient with current polarized positive from neck to feet reduced her pain from 7–8/10 to a 0/10 in 45 minutes.
Central pain can also develop after spinal cord injuries that create deafferentation in the pain pathways in the spine. If the pathways are just chemically deafferented then the protocol described in Chapter 8 appears to reduce inflammation in the cord and effectively “re-afferent” the pain pathways. But if the spinal column has been traumatized and the pain pathways are physically disrupted then treating the cord will not be effective and the brain must be treated. This kind of pain is seen in paraplegics, quadriplegics and patients with cord traction injuries.
The protocol to reduce central pain involves “reducing inflammation” in the “midbrain” – 40 / 89. This protocol has been used to resolve central pain successfully in numerous patients in different facilities around the US. The results have been consistent and there have been no negative effects and no side effects beyond the induced euphoria already described. If the damage is due to a stroke and there has been loss of brain tissue structure as well as function the pain relief has been temporary, perhaps only 12–24 hours. If the protocol reduces pain the first time it will reduce the pain every time it is used. The pain relief does not diminish with repeated use as it does with TENS devices. The pain reduction seems to be more lasting with repeated use but will always be temporary if the physical structure is severely damaged. The protocol is presented here in the hopes that expanded use will bring relief to patients with central pain and encourage study of the phenomenon.
Central pain case report
The patient was a 42-year-old male referred for FSM therapy from Kaiser Premanente pain clinic and accompanied to the appointment by a care giver. He had an aneurysm burst at the age of 28 and developed right-sided central pain at the age of 35. When he presented for treatment, his pain was rated as a 7/10 on a 0–10 visual analog scale while he was taking 100mg of oral morphine daily with the option to increase the dose to 150mg as needed. His pain diagram covered the right side of his body from the top of his head to the bottom of his right foot and there was a brace on his right lower leg. The right-sided headache was his primary complaint. His lower extremity reflexes demonstrated clonus. His MRI showed extensive tissue scarring in the left peri-ventricular area of the brain.
His was the first case of central pain ever seen at the clinic and he was told that, while treatment would be offered, it was considered very unlikely that treatment would be successful. His caregiver suggested that we follow the request of the referring physician in the name of compliance and the patient consented to treatment. The contacts were set up from neck to feet (Fig. 10.9) because the nervous system is polarized positive from neck to feet according to Becker (1985). The frequencies were chosen on the basis of what had been found to be effective in fibromyalgia (40 / 10) but the tissue was changed to the midbrain known to be the site of central pain. After 20 minutes of treatment, the patient was asked about his headache. He replied in a quizzical tone that “It appears to be gone.” In another 20 minutes he was pain free.
The pain returned within 24 hours but at a reduced level and when he returned for treatment the next day it was back to a 6–7/10. Treatment eliminated the pain again and this time it remained reduced for 48 hours. But it always returned. When the first automated unit became available it contained the protocol found to be effective for him and the patient could eliminate or manage his pain by using the protocol for central pain on the unit three times a week. He remained on a very low dose of morphine primarily to prevent having to deal with the detoxification process. These results have been reproduced on a number of patients with central pain resulting from surgeries, head trauma or strokes. So far, there has been no one with central pain who did not experience pain relief.
Treatment protocol for central pain
19, 43, 46 / 89, 45
• Remove opiates from the midbrain and nervous system. Patients with central pain may be on opiate medication. For some reason the presence of opiates slows the effectiveness of the FSM protocol. Experience shows that using these frequencies for 2–3 minutes each speeds up the pain reduction. If the patient is not on opiate medication there is no need to use this frequency combination.
• Treatment time: Use each frequency combination for 2–3 minutes each. A higher dose of opiate medication generally requires a longer use of the frequency to remove it. If the patient’s pain increases while these frequencies are being used the desired effect has been achieved and the frequencies should be changed immediately to 40 / 89.
Reduce pain
40 / 89
• Reduce inflammation / in the midbrain.
• Polarized Positive Current + applied from neck to feet is optimal.
• Treatment time: Use this frequency until the pain is reduced from its likely incoming 7–8/10 VAS level until it stops declining. This process may require up to 60 minutes. In every case treated to date the pain has been reduced to a 0–2/10 within 60 minutes. This protocol reduces central neuropathic pain and central pain amplification only. It will not reduce local orthopedic pain. For example if the patient has both a broken foot and central pain, 40 / 89 will reduce the central pain but the foot pain may still be at a 5–6/10 level, although the elevated endorphins seen with this protocol usually reduce the orthopedic pain to some extent as well.

CAUTION: If the patient has full body pain that is NOT from central sources and the midbrain is performing its normal function of pain suppression, using frequencies to reduce the activity of the mid brain reduces central suppression and causes the pain to increase temporarily.
This protocol is only effective for true central pain.
Do not use it for other types of pain. If use of 40 / 89 increases pain it is best to rethink the diagnosis. Use 81 / 89 to reverse the effect of increased pain.
 Precaution side effect – induced euphoria
Precaution side effect – induced euphoria
The central pain protocol produces a profound euphoric affect that is more pronounced the first few times it is used. Some patients become very relaxed and many will fall asleep. This temporary phenomenon should wear off as the other frequencies are used at the end of the treatment protocol. The patient will remain relaxed and should come to full function within an hour or so after treatment. Most patients are in full possession of their faculties by the time they are ready to leave the clinic and most report sleeping better on the night of the treatment.
Precaution: The practitioner should take care to ensure that the patient is safe to drive. In extreme cases patients have been warned against making important financial decisions until the effect has worn off.
Treat the midbrain
970, 94, 321, 9, 40, 284, 51, 3, 91, 81, 49 / 89
• Remove the emotional component, trauma, paralysis, allergy reaction, inflammation, chronic inflammation, fibrosis, sclerosis, and calcium influx and restore secretions and vitality / in the midbrain.
• Once the pain has been reduced, treat the midbrain to “remove the pathologies” that made it a pain generator. This appears to make the pain reduction more lasting but there is no guarantee that pain relief will be permanent. The adage that “FSM cannot put tissue back that is not there” applies to brain tissue as well as other tissues. The frequency 40 / 89 appears to be able to restore function in some way that alleviates the pain for variable periods of time. Using the frequencies above may improve tissue function so that pain relief may be longer lasting. There have been no negative effects observed from their use but common sense and prudent professional judgment should be exercised by the treating physician if side effects are observed.
• Treatment times: All of the frequencies used to treat the midbrain once the pain is eliminated are used for 1–2 minutes each on the automated FSM microcurrent units but if time allows and the patient’s condition requires it any of the condition frequencies, except for 81/ can be used for several minutes. Experience shows that 81 / may actually increase secretions in the midbrain as demonstrated by changes in patient behavior and function. This frequency should be used with respect and for no more than 1–2 minutes.
• The indicators such as warmth and softening can be used to determine when it is time to change the frequency. If the practitioner and the patient cannot feel the tissue softening or warmth, the practitioner can use the frequencies in a standardized protocol for 2 minutes each with good effect. Practitioners using manual microcurrent devices can change frequencies every 2 minutes and can customize the protocol depending on the patient’s symptoms and response.
Treatment application
If there is dense scar tissue or bony stenosis of the nerve root or spinal cord or if a disc fragment is compressing a nerve root or the spinal cord, the patient’s pain may increase when polarized positive current is applied. If the patient is positioned comfortably, it is the only time the pain will increase during treatment with polarized positive current. Pain may increase in the dermatome or at the spine or both. Assess patient position to determine whether it is contributing to the pain increase.
Stop treating immediately if pain goes up during treatment. Move the patient to a seated position if possible. Move the contacts to the abdomen, reduce current levels and change the current from polarized positive to alternating. Use 40 / 10 to reduce the increase in pain. If this is going to reduce the reaction it will do so in 5–10 minutes. If the pain continues to increase, stop treating with current. The pain should go back down in a few hours although it may take up to 24 hours to reduce to baseline. Return to 40 / 89, change the current to alternating and place the contacts on the abdomen and spine.
This reaction is diagnostic. The physical examination findings caused by brain injuries will confound the examination finding suggestive of cord stenosis. But the patient is always entitled to more than one complaint. This reaction suggests the need for imaging to confirm the presence of spinal cord compression or stenosis.
Patient position for treating central pain
The patient can be placed in any comfortable position in which the body is well supported. The patient will become very relaxed during this protocol and may fall asleep so the head and trunk should be well supported.
Lead placement for treating central pain
The nervous system is an information processing system and is designed to respond to input in the form of patterns that include frequencies and even thought or emotion. It is not necessary to run current through the brain in order to affect the brain.
Graphite gloves wrapped in a warm wet towel at neck and feet
The two positive electrodes should be placed in the jacks cemented to the back of one graphite glove or into two red alligator clips and the two negative electrodes should be placed in the jacks cemented to the back of the second graphite glove or into two black alligator clips. Graphite is a good current conductor and the glove may have an additional positive effect for reasons not completely understood. The graphite glove with the positive leads can be wrapped in a warm wet towel that is wrapped around the neck. The graphite glove with the negative leads can be placed in a warm wet towel that is wrapped around the feet. This set up appears to have the most rapid positive effect.

Figure 10.10 • Central pain seems to respond best when the contacts are placed at the neck and feet using polarized positive current. Place the two positive leads from channel A and channel B in a warm wet fabric contact (hand towel) using either a graphite glove or two alligator clips attached to the contact. Wrap the positive leads contact around the patient’s neck.
Place the two negative leads from channel A and channel B in a warm wet fabric contact (hand towel) using either a graphite glove or two alligator clips attached to the contact. Wrap the negative leads contact around the patient’s feet. The fabric should be wet but wrung out thoroughly. Cover the patient with a blanket to keep them warm as the contacts cool during the treatment.
Graphite gloves at the abdomen and spine
If the patient has spinal cord stenosis or for some other reason does not tolerate polarized positive current flow from neck to feet the gloves should be sprayed or moistened with water or placed in small wet fabric contacts such as a hand towel and placed directly on the skin of the abdomen and back. The protocol is slightly less effective when applied this way. The pain is not reduced to the same degree and is reduced more slowly with this application but it is still more effective than any other treatment available for central pain.

Figure 10.11 • If the patient has spinal stenosis or for some other reason does not tolerate current polarized positive from neck to feet the central pain protocol may be applied with the contacts at the back and abdomen.
Place the two positive leads from channel A and channel B in a warm wet fabric contact (face cloth) using either a graphite glove or two alligator clips attached to the contact. Place the positive leads contact behind the patient’s low back. Place the two negative leads from channel A and channel B in a warm wet fabric contact (face cloth) using either a graphite glove or two alligator clips attached to the contact. Place the negative leads contact on the patient’s abdomen. The fabric should be wet but wrung out thoroughly. Cover the patient with a blanket to keep them warm as the contacts cool during the treatment.
Graphite gloves may be moistened and used directly on the skin as shown above but if the gloves become dry the current will sting or prickle and be uncomfortable. The wet fabric ensures that the contacts stay moist. The current flow should be sub-sensory as long as the gloves are moist.
Electrode pads
Place adhesive electrode pads on the patient’s body such that the current from channel A and the current from channel B cross in three dimensions. For central pain if the positive lead from channel A is placed on the right side of the spine at the neck then the negative lead from A can be placed on the left foot. The positive lead from channel B would be placed on the left side of the spine at the neck and the negative lead from channel B would be placed on the right foot.

Figure 10.12 • The gel electrode pads may be used if they are more convenient. The pads need to be placed so the current and frequencies from the two channels make an “X” and cross through the patient in an interferential pattern. Place the gel electrode pads attached to the positive lead from channel A on the left side of the neck. Place the gel electrode pad attached to the negative lead from channel A on the right foot. Place the positive lead from channel B on the right side of the neck and the negative lead from channel B on the left foot.
Current level
• Average current level 100μamps. Use lower current levels around 40–60μamps for children or very small or debilitated patients. Use higher current levels closer to 200–300μamps for larger or very muscular patients. Do not use more than 500μamps as animal studies suggest that current levels above 500μamps reduce ATP formation while current levels below 500μamps increase ATP.
• + Positive Polarization: Current is used polarized positive with lead placement from neck to feet. Positive leads from both channels are placed at the neck; negative leads from both channels are placed at the feet. If the patient tolerates polarized positive current it appears to reduce pain more quickly than using alternating current at the abdomen and spine. If the patient has spinal stenosis there will be an increase in mid-scapular pain (see warning box) and the patient must be treated with alternating current applied at the abdomen and low back.
• ± Alternating DC Current: Alternating current mode is pulsed DC (direct) current that alternates its polarity from positive to negative. Alternating current is used when the contacts are placed at the abdomen and spine and when cord stenosis prevents use of polarized current.
Waveslope
Use a moderate to waveslope for treating central pain. Use a gentle waveslope in acute brain injuries that create central pain. The waveslope refers to the rate of increase of current flow on the leading edge of the square wave. A sharp waveslope has a very steep current up ramp on the leading edge of the ramped square wave and a gentle waveslope has a gradual current up ramp on the leading edge.
Adjunctive therapies
Brain injuries and central pain involve inflammation and activation of glial cells as well as reduced axonal transport. Treatment with FSM is thought to change the membrane protein configuration and reduce inflammation. Maintaining the changes achieved by FSM treatment is best achieved when the nutritional environment supports the desired state.
Nutritional support
Omega 3 essential fatty acids EPA/DHA reduce inflammation and DHA is an important component of neural membrane tissue. These lipids are found in lipid-rich animal sources such as salmon and halibut. Tuna must be consumed with care due to its tendency to be contaminated with mercury. Phosphatidyl serine and phosphatidyl choline support membrane stability. Fish oil supplements should be certified free of mercury by the manufacturer.
Lipoic acid is an important anti-oxidant that is thought to cross the blood–brain barrier. Glutathione, co-enzyme Q10, vitamin C, vitamin E and other anti-oxidants should be taken in a balanced diet or in supplement form. Professional grade supplements manufactured by nutritional companies who market to physicians are the most reliable source of these nutrients due to their quality control procedures and pharmaceutical manufacturing standards.
Behavioral support
When recovering from a brain injury or central pain the patient should be coached to think of it as they would recovery from any other physical injury. Rest, sleep and good sleep hygiene are important. Regular bedtimes in a quiet room free from electronic stimulation such as televisions and computers should be observed. If diurnal rhythms have been lost and the patient finds that they become more awake at night and take hours to become alert in the morning there are two possible strategies. The first is to sleep when sleepy as long as the patient is able to sleep for 8–9 hours a day in at least 90-minute segments. The second is to attempt to restore normal diurnal rhythm using melatonin taken one hour before desired bed time to quiet the adrenals at night and help achieve deeper sleep. Take herbs, licorice, B6, B5 and vitamin C in the morning to help increase adrenal stimulation.
Seek professional help from a neuropsychologist who specializes in brain injuries. If such advice is not available some common sense approaches can be suggested by any compassionate practitioner. Advise the patient to seek mental stimulation as tolerated such as puzzles, word games, reading or listening to certain classical composers, or books on tape. If the exercise is too frustrating or fatiguing choose a less demanding task until the brain recovers more function. Television, especially commercial television with its quick, visually and emotionally stimulating content and style, should be avoided. Avoid emotional strain and the occasions of conflict as much as possible especially if emotional lability is part of the symptom profile.
Gentle exercise such as walking or swimming provides increased circulation without jarring the brain as would happen with running or more vigorous forms of exercise. Avoid the occasions of re-injury such as bicycle riding, basketball or other contact sports, horseback riding or riding motorcycles. Once the brain and balance have recovered completely the patient may choose to resume such stimulating exposures but avoiding them during the recovery period is wise. Modifying such choices may be challenging for patients if the judgment centers in the brain that regulate such choices are impaired.
Emotional balance
When to treat for emotional states
The frequencies to balance or neutralize strong emotions came from Van Gelder along with the frequencies for concussion, emotional tension and nervous tension. The channel A frequency is 970Hz and the channel B frequency is the frequency for the organ associated with that emotion in Chinese medicine.
The frequencies do not remove the emotions but rather seem to reduce the intensity with which they are felt and the impact that they have on the nervous system and pain syndromes. Response to these frequencies has been consistent over the 11 years in which they have been used. Patients are never told what frequency is being used and are blinded to the intended effect. The practitioner treating the patient can observe the response and feel the characteristic tissue softening that occurs when the frequency is “correct”.
Emotional frequency case report
A fairly stoic, long-term clinic patient presented with a recurrence of his chronic low back pain. He rated his pain as 5–6/10; worse with any movement. Unlike his previous treatments, at this treatment the protocols for nerve, muscle, disc and facet involvement produced no softening of tissue and no reduction of pain after 15 minutes. This was such an unusual response for him that when he confirmed that he was well hydrated, the frequencies for emotions were used out of desperation without informing the patient that they were being used. The characteristic muscle softening and pain reduction happened within a few minutes especially with the frequencies for fear, grief, and resentment. He commented that his back pain was going down and asked what had finally been effective. The response to the emotional frequencies prompted a reply with a question, “Before I tell you what frequency was used can I ask how things are going at home?” His response, “You mean besides the fact that my marriage is in the toilet? Why do you ask?” “I asked because the frequencies for emotions were the only ones that reduced your back pain and softened the muscles. You responded with muscle softening to grief, resentment and fear and not at all to anger. Does that match what is going on?” He affirmed that the response matched his experience. His back pain resolved and his marriage survived the rough patch.
Treat with emotional frequencies when treatment for physical pain sources does not produce the expected effect. Every physical injury or condition creates an emotional effect so treating for emotional balance is a good strategy in almost any condition. Some patients are clearly more emotionally reactive than others and they benefit greatly from use of these protocols.
If the patient talks incessantly about their emotional reaction to a trauma, accident, event, medical or surgical procedure, the emotional balance protocol reduces the strength of their reaction. Athletes who are injured rarely talk about the emotional impact of the injury or their emotional state at the time of the injury. The frequencies seem to dissipate the emotional load and reduce the impact of the emotion on the physical tissue – without requiring that the emotion be disclosed or discussed.
The responses to these frequencies have been consistent. There is no way to blind the observer and there is no way to objectively evaluate something as subtle as the degree of fear or anger felt or expressed or its effect on the body so it is unlikely that these frequencies will ever be studied in a controlled trial. But the reader is encouraged to use them in combination with the concussion protocol and observe the effects.

Caution: These frequencies are not intended to replace appropriate counseling, psychotherapy or medication for serious mental illness or acute psychiatric distress. They have been used as adjunctive therapy in a limited number of cases by psychotherapists who anecdotally report some benefit and no ill effects. They have been used in patients taking various psychotropic medications and, while no ill effects have been reported, it is recommended that the patients be monitored for side effects.
Treatment times
Use these frequencies for 1–2 minutes each depending on clinic time demands and the patient’s emotional state. If the patient has a very strong specific emotion and time allows, any particular frequency may be used for up to 5–10 minutes.
How to use the frequencies for emotions
Start with the basics 94, 970 / 200 for 1–2 minutes each and then think about how emotions combine themselves. Pure emotion is rare. Fear is usually behind anger. Anger and fear are usually behind resentment and hurt feelings. Mental tension makes it all worse. Grief is always a combination of responses. Anger combines with grief and says “Why couldn’t you save my husband or child?” Resentment combines with grief and says, “How could you die and leave me with all this?” Worry combines with grief and says, “What if something happens to my other child?” or “Did I do something wrong?” The opposite of love and happiness is fear. Emotions are always a mix.
Emotions are mediated by brain and endocrine function. The midbrain and forebrain structures that modulate emotional response are sensitive to the neurotransmitters involved in stress. Reducing “mental tension” improves response to the other emotional frequencies. Additional protocols for emotional conditions are available in the FSM advanced training seminars.
Case report
FSM concussion protocol
The concussion protocols are among the most useful standard protocols available to practitioners of FSM. Over the years in our clinical practice, the range of situations where use of the concussion protocol has been appropriate continues to expand. In retrospect, it has helped to consider the broader meanings associated with the term, “concussion.” Though what follows is a brief discussion about the typical aspects of concussion, thinking about clinical situations where there is a sudden change in the ability to process information or simply to function on automatic pilot, because of some shock to the system, is a useful way to think about concussion. We learn about the environment from the earliest days of life on this planet, integrating complex sets of information and become able to process them to allow us to function without thinking about some very important information that we process subconsciously on a continual basis. The very core of experience in everyday life is dramatically impacted when these automatic processes no longer function according to our expectations.
Considerations in concussion
Sustaining a concussion clinically implies trauma to the head and its contents which includes the brain and the structures to which it connects (the olfactory organs, eyes, brainstem and spinal cord being the structures at significant risk for injury). It goes without saying (but sometimes it seems to be overlooked) that this includes potentially painful injury to skull, ranging from contusion all the way to fracture. In the case of the latter, the risk for pain is obvious but in the former, when the acute swelling in the scalp resolves, the reasons for persistent head pain or headache may seem less obvious. Localized trauma to the nerves to the scalp, which is also a very vascularized tissue, can lead to chronic pain in the region of the injury. As regards injury to the contents of the skull, the components of the brain most at risk depend on the type of impact, and discussion is beyond our scope. However, it is also important to keep in mind that, when a person sustains a concussion, there has likely also been other injury to the body, and all of the changes associated with such injury are going to be processed by a brain that has been traumatized.
Some of the typical sequelae will depend on the extent of trauma, with varying degrees of altered awareness extending from transient changes to extended periods of coma. The portions of the brain at obvious risk for injury in trauma are those which are adjacent to bony structures, especially the petrous portions of the temporal bones, but the brainstem is quite vulnerable because of typical types of motion that can strain the normal anatomical relationships that support the brain, but allow the brainstem to descend to become the spinal cord. Any type of motion with sudden disruption of the pattern of that motion can result in traction on the brainstem. It is important to remember that almost any structure which communicates with the rest of the body by neural connection traverses the brainstem or areas adjacent to it in the neck (such as sympathetic traffic following the arteries to the brain).
Consequences of concussion
Clinical accompaniments of concussion include changes in cognitive functions of many different types including attention, processing, memory and especially multi-tasking. Vertiginous symptoms and problems with equilibrium, balance and co-ordination are frequent, as are headaches, which have a variety of characteristics. For more extensive review of the clinical symptoms, the reader is referred to references on the topic. It is relevant, however, to review the structures localized within the brainstem which include most of the cranial nerve nuclei (other than functions of olfaction and vision, in the sense of perception, however the oculomotor nuclei reside in the brainstem and dysfunction will lead to perceptual problems because of the possibility of altered or dysconjugate movement of the two eyes simultaneously).
Our perception of the environment and our ability to function in gravity or with movement is a combination of many different sensory inputs, including the primary sensory input from the vestibular organs. But these strong stimuli are also matched to input from binocular vision, binaural hearing, and our joint perception and perception of movement in gravity sent through sensory input from our limbs and trunk, as well as the head and neck. Acute dysfunction in the vestibular organs is usually obvious and manifests itself as vertigo or severe disequilibrium. But subtle dysfunction which can occur either as an acute trauma to the peripheral vestibular input resolves or as a “mismatch” in the co-ordination of the multiple other signals is typical of the pathology associated with concussion. And though not the only remaining other structures that can be altered by concussion, the balance between sympathetic and parasympathetic functions occurs for many functions at the level of the brainstem including the higher anatomical structures which innervate the pupils, the outflow for innervations of vascular responses, heart rate and rhythm alterations, and gustatory stimuli. Discussion of this complex group of functions is beyond our task, but it makes consideration of these complex interactions imperative when one addresses issues to be addressed in any patient who has sustained even a very mild concussive injury.
FSM concussion protocol
If one reviews the standard FSM concussion protocol, it becomes obvious the emphasis on possible pathological states or alterations which are targeted within the structures traditionally localized to the brainstem and some other deeper structures in the brain. Physical, even gentle, traction injury can lead to swelling, and fluid shifts, upregulation of inflammatory signaling, which is typically acute but can become chronic, as well as a change in the activation of the supportive cells, including possibly chronic inflammation (microglial activation) or astrocytic gliosis, depending on the extent of the trauma. Treating these parameters as conditions would then lead to use of those in the protocol.
We have used the FSM concussion protocol for patients who have sustained mild traumatic brain injuries with significant success. Ours is a small office and as such the discussion which follows is mostly anecdotal, however, we have, in several patients, tested some functions pre- and post-treatment and demonstrated improvement after using the full concussion protocol. Though many practitioners have reported problems with vestibular complaints in association with certain frequency patterns, we have not had that experience in this office such that it prevented treatment.
Case report (Catherine Willner, MD, Durango, Neurological Associates, Durango, Colorado)
Our initial experience with the full concussion protocol involved treating three college students who sustained mild concussive symptoms following head trauma. The first was injured during a hockey game when she struck the wallboards with her head. Though she was wearing a regulation helmet, the impact was strong enough that her helmet was damaged and she was additionally struck by another player such that both head strikes were on the right side. She was dazed for about 60 seconds but did not think that she lost consciousness. She noticed a headache developing over the next few hours, accompanied by disequilibrium and mild nausea. Her cervical muscles were strained and gradually tightened over the next several hours. She has some mild recurrence of a previous cervical radicular pain in her left arm without any weakness or dysesthesias. This incident occurred during the week before her semester final examinations were scheduled and she had several papers and examinations that would be due or occur within 10 days. Her persistent headache and other symptoms persisted in severity to the point that she could not focus to study or complete the work on papers she had already started. She presented 3 days after the injury for clinical evaluation. On the abbreviated test of mental status, all of her answers were correct, though her processing was quite slow. She spontaneously recalled three of the four words she had been asked to remember and after missing the first, recalled it spontaneously just before she would have been given a hint to recall it. This was similar for naming objects she had been asked to remember.
There were no signs of increased intracranial pressure or nuchal rigidity. The only physical finding was stiffness in the cervical musculature and minor reflex changes on the right at C5–6, a known finding in this patient previously. Smell was completely intact and there were no frontal release signs. There was no nystagmus, and ocular movements and reflexes to assess for central vestibular dysfunction were normal. There was no weakness and cerebellar and sensory functions were intact. She had undergone a non-contrasted CT scan of the brain in the emergency room at the local hospital which was reviewed and was unremarkable including bone windows. After attention to adequate hydration, using water and a mineral supplement, we offered her frequency-specific microcurrent therapy (FSM), and using leads from back to sternal area, we ran the “full concussion protocol”. She fell asleep during the treatment after about 5 minutes. When the treatment was completed, she awakened easily, reporting that her headache and cervical tightness were significantly improved. Her headache prior to treatment was described as a tight band with mild throbbing bilaterally. Those features were gone and she reported that the level of discomfort related to the headache had decreased from a 6/10 to 1–2/10. Though we could not exclude the impact of sleep in reducing her pain, she repeated the protocol twice more on consecutive days and during the next treatment reported similar reduction in pain without falling asleep. Additionally, after the first treatment, she awoke and demonstrated to the technician that she still remembered both the words and names of objects on the test she had taken earlier that morning. Her pronouncement of the eight words was quick and accurate. She also reported that her arm symptoms were nearly gone after the second treatment, though there was no focused treatment used for radicular or cervical symptoms.
This patient was so thrilled with her response that she sent a friend from school who had sustained a concussion when she fell from her mountain bike about 3 weeks earlier. This young woman had hit a small patch of ice on a trail and fell over the handle bars, hitting her head. She thought that she might have lost awareness for about 2–3 minutes at the scene. As she was alone, she could not be completely sure about the time. She sustained contusions but no other serious injuries. She had also been evaluated at the ER after the injury and was cleared, also having labs and a CT scan of the brain (without contrast). Her persistent symptoms included headache (global, intermittently severe, sharp and throbbing with nausea when it was more severe) and dizziness which was worse with movement but not characteristic of benign positional vertigo. The vertigo gradually started to improve and by the time she was referred to try frequency-specific microcurrent, her headache was rated as intermittently a 3/10. Her major problem was that she was also having trouble concentrating to study for her final examinations. She would lose focus and fall asleep or lose interest and find that she had to exercise to stay awake and the exercise, even only mild exertion, would reproduce her headache symptoms. She came well hydrated, and underwent two consecutive full concussion protocol sessions, reporting that after these treatments she felt nearly back to normal and was able to study easily and did well on her finals. Though only an anecdotal report, she was so pleased with the outcome that she recruited a third patient to try the treatment.
This young man was also a mountain biker and participated in semi-professional races on a regular basis. He had fallen during a training session and hit his head. Though his injury was not considered severe by his interpretation, he had persistent headaches, intermittently and found that he was having some trouble juggling expectations. On further questioning he characterized the issue as problems with multi-tasking. He would work construction regularly for income and typically could finish carpentry quite easily. He had observed that his skills seemed less on target and he would frequently have to ask his co-workers how to accomplish tasks he had previously done without effort. Though he was not a seasoned carpenter, this change in his performance was concerning to him. He did admit that he had been sleeping longer and feeling less rested after a night’s sleep. Both the latter two patients passed an abbreviated test of mental status without any problems, though they were both slower than they thought that they should be in doing simple math problems and explaining proverbs. Recall was not impaired and attention was fine to simple tasks. Their examinations were neurologically normal as well. He noticed complete resolution of the headaches after the first treatment and only repeated the treatment about a week later at which time he reported that he had been to work during the week without problems in his skill sets.
None of these three patients had a history of migraine. The first woman had a history of cervical problems which would wax and wane but she did not have further symptoms of concussion after her three treatments and she also went on to pass all of her exams and complete her papers on time. She also returned to the office intermittently to focus on treatment of her cervical problems managing them easily with FSM treatments combined with physical therapy programs.
Because of the observation that this woman’s cervical issues were improved only using the concussion protocol, our technician started to use a shorter version of the concussion protocol on any patient who presented with more than one obvious problem. As we introduced this approach about a year after she had been in the office, she started to record the number of treatments on other problems required to help patients and observed that most patients required fewer focused treatments when we started with some version of the concussion protocol. This was especially true with patients who had sustained any form of physical injury prior to the onset of more focused symptoms.
Collected case reports
We did accomplish a very small pilot study on 10 patients with symptoms of mild concussion, ranging in age from 19 to 44, all of whom were classified with mild closed head injury without focal findings. None had sustained any more than a minute of altered consciousness. We performed tests of mental (math problems, verbal similarities) and physical agility (puzzle and peg placement) and accuracy pre- and post-treatments and demonstrated, on average a 35% improvement in performance following a second treatment done within 3 days. This is obviously not a well controlled experiment but we did test three other head injury patients and retest them without treatment in 3 days and they had less than 5% improvement on the scores used. Even though this data is very limited, it is our greatest hope that trials could be applied in larger settings. Given the frequency of head injury in the military especially during active duty in combat, it would be wonderful to be able to assess this treatment in that setting. Treatment done in traditional settings for head injury is usually supportive rehabilitation, when done best, it is tied to psychometric retraining. Combining such approaches with use of FSM would be a wonderful opportunity for further assessment and if our observations hold true in a larger population, this would be a significant addition to the treatments available at this time in the typical clinical setting.
Alves W., Macciocchi S., Barth J.T. Postconcussive symptoms after uncomplicated mild head injury. J. Head Trauma Rehabil.. 1993;8:48-59.
Bazarian J.J., McClung J., Shah M.N., Cheng Y.T., Flesher W., Kraus J. Mild traumatic brain injury in the United States, 1998–2000. Brain Inj.. 2005;19:85-91.
Becker R.O., Seldon G. The body electric: electromagnetism and the foundation of life. New York: Quill, William Morrow, 1985.
Blumbergs P.C., Scott G., Manavis J., et al. Staining of amyloid precursor protein to study axonal damage in mild head injury. Lancet. 1994;344(8929):1055-1056.
De Kruijk J.R., Leffers P., Menheere P.P., Meerhoff S., Rutten J., Twijnstra A. Prediction of post-traumatic complaints after mild traumatic brain injury: early symptoms and biochemical markers. J. Neurol. Neurosurg. Psychiatry. 2002;73:727-732.
Dewar D., Graham D.I. Depletion of choline acetyltransferase but preservation of M1 and M2 muscarinic receptor binding sites in the temporal cortex following head injury: a preliminary postmortem study. J. Neurotrauma.. 1996;13:181-187.
Dixon C.E., Bao J., Bergmann J.S., Johnson K.M., et al. Traumatic brain injury reduces hippocampal high affinity (3H) choline uptake but not extracellular choline levels in rats. Neurosci. Lett.. 1994;180:127-130.
Gross H., Kling A., Henry G., et al. Local cerebral glucose metabolism in patients with long-term behavioral and cognitive deficits following mild traumatic brain injury. J. Neuropsychiatry Clin. Neurosci.. 1996;8:324-334.
Humayun M.S., Presty S.K., Lafrance N.D., et al. Local cerebral glucose abnormalities in mild closed head injured patients with cognitive impairments. Nucl. Med. Commun.. 1989;10(5):335-344.
Lipton B. Biology of belief, mountain of love. Santa Rosa California: Elite Books, 2005.
McAllister T.W., Arciniegas D. Evaluation and treatment of postconcussive symptoms. NeuroRehabilitation. 2002;17:265-283.
McCrea M.A., Kelly J.P., Randolph C., Cisler R., Berger L. Immediate neurocognitive effects of concussion. Neurosurgery. 2002;50:1032-1040.
McCrea M.A. Mild traumatic brain injury and postconcussion syndrome: the new evidence base for diagnosis and treatment. New York: American Academy of Clinical Neuropsychology/Oxford University Press, 2008.
Middelboe T., Andersen H.S., Birket-Smith M., et al. Minor head injury: impact on health after 1 year. A prospective follow-up study. Acta Neurol. Scand.. 1992;85:5-9.
Mooney G., Speed J., Sheppard S. Factors related to recovery after mild traumatic brain injury. Brain Inj.. 2005;19:975-987.
Murdoch I., Perry E.K., Court J.A., et al. Cortical cholinergic dysfunction after human head injury. J. Neurotrauma. 1998;15:295-305.
National Institutes of Health. NIH consensus development panel on rehabilitation of persons with traumatic brain injury. J. Am. Med. Assoc.. 1999;282:974-983.
Oppenheimer D.R. Microscopic lesions in the brain following head injury. J. Neurol. Neurosurg. Psychiatry. 1968;31(4):299-306.
Pert C. Molecules of emotion. New York: Touchstone Publications, Simon and Schuster, Inc., 1997.
Povlishock J.T., Coburn T.H. Morphopathological change associated with mild head injury. In: Levin, Eisenberg, Benton. Mild head injury. New York: Oxford University Press; 1989:37-53.
Povlishock J.T., Erb D.E., Astrug J. Axonal response to traumatic brain injury: reactive axonal change, deafferentation and neuroplasticity. J. Neurotrauma.. 1992;9:189-200.
Povlishock J.T., Christman C.W. The pathobiology of traumatically induced axonal injury in animals and humans: a review of current thoughts. J. Neurotrauma.. 1995;12(4):555-564.
Ropper A.H., Gorson K.C. Concussion. N. Engl. J. Med.. 2007;356:166-172.
Ruff R.M., Crouch J.A., Tröster A.I., et al. Selected cases of poor outcome following a minor brain trauma: comparing neuropsychological and positron emission tomography assessment. Brain Inj.. 1994;8:297-308.
Ryan L.M., Warden D.L. Post concussion syndrome. Int. Rev. Psychiatry. 2003;15:310-316.
Saija A., Robinson S.E., Lyeth B.G., et al. The effects of scopolamine and traumatic brain injury on central cholinergic neurons. J. Neurotrauma.. 1988;5:161-170.
Van Gelder H. Inner peace through the process of knowing: essays in metapsychology. New South Wales, Australia: Robert Martin Outsound Publishing, Merry Land West, 1985.
Van Gelder H. The process of healing: a field theory approach. New South Wales, Australia: Robert Martin Outsound Publishing, Merry Land West, 1989.
