CHAPTER 31 Infratemporal and pterygopalatine fossae and temporomandibular joint
INFRATEMPORAL FOSSA
The infratemporal fossa lies deep to the ramus of the mandible. It communicates with the temporal fossa deep to the zygomatic arch and the pterygopalatine fossa through the pterygomaxillary fissure. The major structures that occupy the infratemporal fossa are the lateral and medial pterygoid muscles, the mandibular division of the trigeminal nerve, the chorda tympani branch of the facial nerve, the otic parasympathetic ganglion, the maxillary artery and the pterygoid venous plexus.
The infratemporal fossa has a roof, and lateral and medial walls, and is open to the neck posteroinferiorly, i.e. the fossa has no anatomical floor. The roof is formed by the infratemporal surfaces of the temporal bone and of the greater wing of the sphenoid, and contains the foramena ovale and spinosum and the petrotympanic fissure: it is open superiorly to the temporal fossa. The medial wall is formed anteriorly by the lateral pterygoid plate of the pterygoid process of the sphenoid, and more postero-medially by the pharynx and tensor and levator veli palatini. It contains the pterygomaxillary fissure across which structures pass between the infratemporal and pterygopalatine fossae (Fig. 31.1). The lateral wall is formed by the medial surface of the ramus of the mandible.
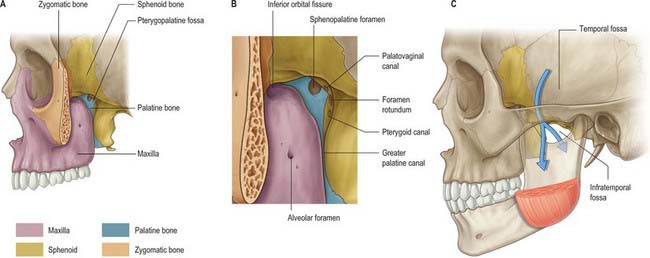
Fig. 31.1 A, Pterygopalatine fossa after detachment of the mandible and removal of the zygomatic arch; B, anteromedial view; C, lateral view; arrows show that the floor of the temporal fossa is open medially to the infratemporal fossa and laterally to the region containing the masseter.
(From Drake, Vogl and Mitchell 2005.)
Lateral pterygoid provides a key to understanding the relationships of structures within the infratemporal fossa. This muscle lies in the roof of the fossa and runs anteroposteriorly in a more or less horizontal plane from the region of the pterygoid plates to the mandibular condyle (Fig. 31.1). Branches of the mandibular nerve and the main origin of medial pterygoid are deep relations and the maxillary artery is superficial. The buccal branch of the mandibular nerve passes between the two heads of lateral pterygoid. Medial pterygoid and the lingual and inferior alveolar nerves emerge below its inferior border and the deep temporal nerves and vessels emerge from its upper border. A venous network, the pterygoid venous plexus, lies around and within lateral pterygoid and is important in the spread of infection.
BONES
The sphenoid bone, the paired maxillae and temporal bones, and the mandible, collectively provide the skeletal framework to the infratemporal and pterygopalatine regions. The mandible and the two temporal bones articulate at the right and left temporomandibular joints. The disarticulated maxilla is described in Chapter 29, the temporal bone is described in Chapter 36, and the sphenoid and mandible are described here.
Sphenoid bone
The sphenoid bone lies in the base of the skull between the frontal, temporal and occipital bones. It has a central body, paired greater and lesser wings that spread laterally from the body, and two pterygoid processes that descend from the junction of the body and greater wings (Fig. 31.2).
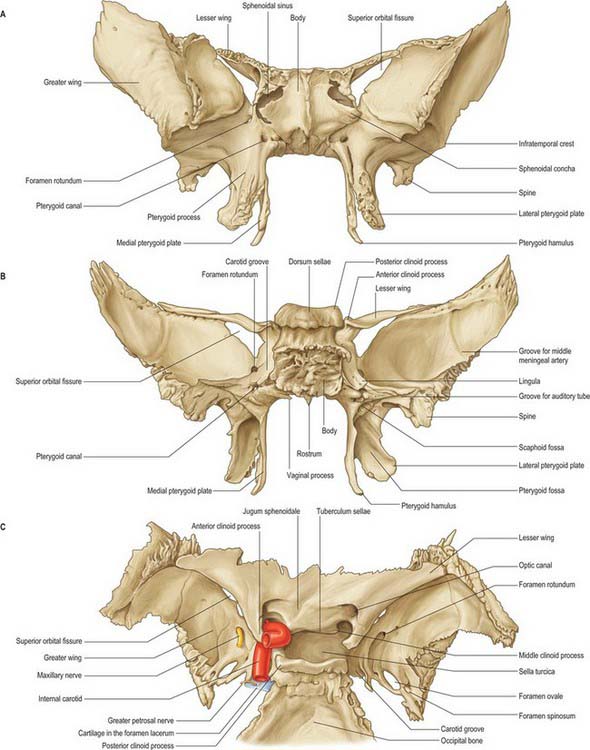
Fig. 31.2 Sphenoid bone. A, anterior view; B, posterior view; C, superior view.
(From Sobotta 2006.)
Body
The body of the sphenoid is cuboidal. It contains two air sinuses, separated by a septum (see Ch. 32). Its cerebral (superior) surface articulates in front with the cribriform plate of the ethmoid bone. Anteriorly is the smooth jugum sphenoidale, which is related to the gyri recti and olfactory tracts. The jugum is bounded behind by the anterior border of the sulcus chiasmatis, which leads laterally to the optic canals. Posteriorly is the tuberculum sellae, behind which is the deeply concave sella turcica. In life the sella contains the hypophysis cerebri in the hypophysial fossa. Its anterior edge is completed laterally by two middle clinoid processes, while posteriorly the sella turcica is bounded by a square dorsum sellae, the superior angles of which bear variable posterior clinoid processes. The diaphragma sella and the tentorium cerebelli are attached to the clinoid processes (see Ch. 27). On each side, below the dorsum sellae, a small petrosal process articulates with the apex of the petrous part of the temporal bone. The body of the sphenoid slopes directly into the basilar part of the occipital bone posterior to the dorsum sellae, together these bones form the clivus. In the growing child this is the site of the spheno-occipital synchondrosis: premature closure of this joint gives rise to the skull appearances seen in achondroplasia.
The lateral surfaces of the body are united with the greater wings and the medial pterygoid plates. A broad carotid sulcus accommodates both the internal carotid artery and the cranial nerves associated with the cavernous sinus above the root of each wing (see Ch. 27). The sulcus is deepest posteriorly. It is overhung medially by the petrosal part of the temporal bone and has a sharp lateral margin, the lingula, which continues back over the posterior opening of the pterygoid canal.
A median triangular, bilaminar sphenoidal crest on the anterior surface of the body of the sphenoid makes a small contribution to the nasal septum. The anterior border of the crest joins the perpendicular plate of the ethmoid bone, and a sphenoidal sinus opens on each side of it (see Ch. 32). In the articulated state the sphenoidal sinuses are closed anteroinferiorly by the sphenoidal conchae, which are largely destroyed when disarticulating a skull. Each half of the anterior surface of the body of the sphenoid possesses a superolateral depressed area joined to the ethmoid labyrinth which completes the posterior ethmoidal sinuses; a lateral margin which articulates with the orbital plate of the ethmoid above and the orbital process of the palatine bone below; and an inferomedial, smooth, triangular area, which forms the posterior nasal roof, and near whose superior angle lies the orifice of a sphenoidal sinus.
The inferior surface of the body of the sphenoid bears a median triangular sphenoidal rostrum, embraced above by the diverging lower margins of the sphenoidal crest. The narrow anterior end of the rostrum fits into a fissure between the anterior parts of the alae of the vomer, and the posterior ends of the sphenoidal conchae flank the rostrum, articulating with its alae. A thin vaginal process projects medially from the base of the medial pterygoid plate on each side of the posterior part of the rostrum, behind the apex of the sphenoidal concha.
Greater wings
The greater wings of the sphenoid curve broadly superolaterally from the body. Posteriorly each is triangular, fitting the angle between the petrous and squamous parts of the temporal bone at a sphenosquamosal suture. The cerebral surface contributes to the anterior part of the middle cranial fossa. Deeply concave, its undulating surface is adapted to the anterior gyri of the temporal lobe of the cerebral hemisphere. The foramen rotundum lies anteromedially and transmits the maxillary nerve. Posterolateral to the foramen rotundum is the foramen ovale, which transmits the mandibular nerve, accessory meningeal artery and sometimes the lesser petrosal nerve, although the latter nerve may have its own canaliculus innominatus medial to the foramen spinosum. A small emissary sphenoidal foramen, which transmits a small vein from the cavernous sinus, lies medial to the foramen ovale (on one or both sides) in approximately 40% of skulls. The foramen spinosum, which transmits the middle meningeal artery and meningeal branch of the mandibular nerve, lies behind the foramen ovale.
The lateral surface is vertically convex and divided by a transverse infratemporal crest into temporal (upper) and infratemporal (lower) surfaces. Temporalis is attached to the temporal surface. The infratemporal surface is directed downwards and, with the infratemporal crest, is the site of attachment of the upper fibres of lateral pterygoid. It contains the foramen ovale and foramen spinosum. The small downward projecting spine of the sphenoid lies posterior to the foramen spinosum; the sphenomandibular ligament is attached to its tip. The medial side of the spine bears a faint anteroinferior groove for the chorda tympani nerve and appears in the lateral wall of the sulcus for the pharyngotympanic (auditory) tube. Medial to the anterior end of the infratemporal crest, a ridge passes downwards to the front of the lateral pterygoid plate, thereby forming a posterior boundary of the pterygomaxillary fissure.
The quadrilateral orbital surface of the greater wing faces anteromedially, and forms the posterior part of the lateral wall of the orbit. It has a serrated upper edge which articulates with the orbital plate of the frontal bone, and a serrated lateral margin which articulates with the zygomatic bone. Its smooth inferior border is the posterolateral edge of the inferior orbital fissure, and its sharp medial margin forms the inferolateral edge of the superior orbital fissure, on which a small tubercle gives partial attachment to the common anular ocular tendon. Below the medial end of the superior orbital fissure a grooved area forms the posterior wall of the pterygopalatine fossa; the latter is pierced by the foramen rotundum.
The irregular margin of the greater wing, from the body of the sphenoid to the spine, is an anterior limit of the medial half of the foramen lacerum. It also displays the posterior aperture of the pterygoid canal. Its lateral half articulates with the petrous part of the temporal bone at a sphenopetrosal synchondrosis. Inferior to this, the sulcus tubae contains the cartilaginous pharyngotympanic (auditory) tube. Anterior to the spine of the sphenoid the concave squamosal margin is serrated – bevelled internally below, externally above – for articulation with the squamous part of the temporal bone. The tip of the greater wing, bevelled internally, articulates with the sphenoidal angle of the parietal bone at the pterion. Medial to this, a triangular rough area articulates with the frontal bone: its medial angle is continuous with the inferior boundary of the superior orbital fissure, and its anterior angle joins the zygomatic bone by a serrated articulation.
Lesser wings
The lesser wings of the sphenoid are triangular pointed plates that protrude laterally from the anterosuperior regions of the body. The superior surface of each wing is smooth and related to the frontal lobe of the cerebral hemisphere. The inferior surface is a posterior part of the orbital roof and upper boundary of the superior orbital fissure, and overhangs the middle cranial fossa. The posterior border projects into the lateral fissure of the cerebral hemisphere. The medial end of the lesser wing forms the anterior clinoid process. The anterior and middle clinoid processes are sometimes united to form a caroticoclinoid foramen. The lesser wing is connected to the body by a thin flat anterior root and a thick triangular posterior root, between which lies the optic canal. Growth of the posterior root is closely associated with variations in the geometry of the canal. The cranial opening of the canal may be duplicated, or more commonly, the division is incomplete.
Superior orbital fissure
The superior orbital fissure connects the cranial cavity with the orbit. It is bounded medially by the body of the sphenoid, above by the lesser wing of the sphenoid, below by the medial margin of the orbital surface of the greater wing, and laterally, between the greater and lesser wings, by the frontal bone. The contents of the superior orbital fissure are described in Chapter 39.
Pterygoid processes
The pterygoid processes descend perpendicularly from the junctions of the greater wings and body. Each consists of a medial and lateral plate, whose upper parts are fused anteriorly. The plates are separated below by the angular pterygoid fissure, whose margins articulate with the pyramidal process of the palatine bone, and diverge behind. Medial pterygoid and tensor veli palatini lie in the cuneiform pterygoid fossa between the plates. Above is the small, oval, shallow scaphoid fossa, which is formed by division of the upper posterior border of the medial plate. Part of tensor veli palatini is attached to the fossa. The anterior surface of the root of the pterygoid process is broad and triangular and forms the posterior wall of the pterygopalatine fossa: it is pierced by the anterior opening of the pterygoid canal.
Lateral pterygoid plate
The lateral pterygoid plate is broad, thin and everted. The lateral surface forms part of the medial wall of the infratemporal fossa; the lower part of lateral pterygoid is attached to it. The medial surface is the lateral wall of the pterygoid fossa; most of the deep head of medial pterygoid is attached to it. The upper part of its anterior border is a posterior boundary of the pterygomaxillary fissure, and the lower part articulates with the palatine bone. The posterior border is free.
Medial pterygoid plate
The medial pterygoid plate is narrower and longer than the lateral. Its lower end is continued into an unciform projection, the pterygoid hamulus, which curves laterally. The pterygomandibular raphe is attached to the hamulus and the tendon of tensor veli palatini winds around the hamulus. The lateral surface forms the medial wall of the pterygoid fossa and the medial surface provides a lateral boundary of the posterior nasal aperture. The medial plate is prolonged above on the inferior aspect of the body of the sphenoid as a thin vaginal process that articulates anteriorly with the sphenoidal process of the palatine bone and medially with the ala of the vomer. The plate articulates with the posterior border of the perpendicular plate of the palatine bone in the lower part of its anterior margin. Inferiorly it bears a furrow, which is converted anteriorly into the palatovaginal canal by the sphenoidal process of the palatine bone. The palatovaginal canal transmits pharyngeal branches of the maxillary artery and pterygopalatine ganglion. The pharyngobasilar fascia is attached to the whole of the posterior margin of the medial plate, and the superior pharyngeal constrictor is attached to its lower end. The small pterygoid tubercle is found at the upper end of the plate, just below the posterior opening of the pterygoid canal. The processus tubarius, which supports the cartilaginous pharyngeal end of the pharyngotympanic tube, projects back near the midpoint of the margin of the medial pterygoid plate.
Sphenoidal conchae
The sphenoidal conchae are two thin, curved small plates, attached anteroinferiorly to the body of the sphenoid bone. The superior concave surface of each forms the anterior wall and part of the floor of a sphenoidal sinus. In situ, each has vertical quadrilateral anterior and horizontal triangular posterior parts. The anterior part consists of a superolateral depressed area, which completes the posterior ethmoidal sinuses and joins below with the orbital process of a palatine bone, and a smooth and triangular inferomedial area, which forms part of the nasal roof and is perforated above by the round opening connecting the sphenoidal sinus and sphenoethmoidal recess.
Anterior parts of the two bones meet in the midline, and protrude as the sphenoidal crest. The horizontal part appears in the nasal roof and completes the sphenopalatine foramen. Its medial edge articulates with the rostrum of the sphenoid and the ala of the vomer. Its apex, directed posteriorly, is superomedial to the vaginal process of the medial pterygoid plate and joins the posterior part of the ala. A small conchal part sometimes appears in the medial wall of the orbit, lying between the orbital plate of the ethmoid in front, the orbital process of the palatine bone below and the frontal bone above.
Ossification
Until the seventh or eighth month in utero the sphenoid body has a presphenoidal part, anterior to the tuberculum sellae, with which the lesser wings are continuous, and a postsphenoidal part, consisting of the sella turcica and dorsum sellae, and integral with the greater wings and pterygoid processes. Much of the bone is preformed in cartilage. There are six ossification centres for the presphenoidal parts, and eight for the postsphenoidal parts.
Presphenoidal part
About the ninth week of fetal life, a centre appears in each wing, lateral to the optic canal, and a little later two bilateral centres appear in the presphenoidal body. Each sphenoidal concha has a centre, appearing superoposteriorly in the nasal capsule in the fifth month in utero. As this enlarges it partly surrounds a posterosuperior expansion of the nasal cavity, which becomes the sphenoidal sinus. The posterior conchal wall is absorbed and the sinus invades the presphenoid component. In the fourth year the concha fuses with the ethmoidal labyrinth and before puberty it fuses with the sphenoid and palatine bones. Its anterior deficiency persists as an opening for the sphenoidal sinus.
Postsphenoidal part
The first centres appear in the greater wings about the eighth week of fetal life, one in the basal cartilage of each wing below the foramen rotundum. These centres only contribute to the root of the greater wing (near the foramen rotundum and pterygoid canal). The remainder of the greater wing and the lateral pterygoid plate are ossified in mesenchyme. About the fourth month of fetal life two centres appear, flanking the sella turcica, and soon fuse. The medial pterygoid plates are also ossified in ‘membrane’, a centre in each probably appearing about the ninth or tenth week. The hamulus is chondrified during the third fetal month and at once begins to ossify. Medial and lateral pterygoid plates join about the sixth fetal month. During the fourth month, a centre appears for each lingula, soon joining the body. The optic canal in the neonate is relatively large and has a keyhole or ‘figure of eight’ shape rather than the circular profile seen in the adult.
Postnatal details
Presphenoidal and postsphenoidal parts fuse about the eighth month in utero, but an unciform cartilage persists after birth in lower parts of the junction. At birth the bone is tripartite and consists of a central part (body and lesser wings) and two lateral parts (each consisting of a greater wing and pterygoid process). During the first year the greater wings and body unite around the pterygoid canals and the lesser wings extend medially above the anterior part of the body, meeting to form the smooth, elevated jugum sphenoidale. By the 25th year, sphenoid and occipital bones are completely fused. An occasional vascular foramen, often erroneously termed the craniopharyngeal canal, is occasionally seen in the anterior part of the hypophysial fossa. Although the sphenoidal sinus can be identified in the fourth month of fetal life as an evagination of the posterior part of the nasal capsule, by birth it represents an outgrowth of the sphenoethmoidal recess. Pneumatization of the body of the sphenoid commences in the second or third year and spreads first into the presphenoid, and later invades the postsphenoid, part. It reaches full size in adolescence, but often enlarges further by absorption of its walls as age advances.
Certain parts of the sphenoid are connected by ligaments that may occasionally ossify, e.g. the pterygospinous ligament between the sphenoid spine and upper part of lateral pterygoid plate; the interclinoid ligament joining the anterior to the posterior clinoid process; and the caroticoclinoid ligament that connects the anterior to the middle clinoid process.
Premature synostosis of the junction between pre- and post-sphenoidal parts, or of the spheno-occipital suture, produces a characteristic appearance, obvious in profile, of an abnormal depression of the nasal bridge (hypertelorism).
Mandible
The mandible is the largest, strongest and lowest bone in the face. It has a horizontally curved body that is convex forwards, and two broad rami that ascend posteriorly (Fig. 31.3). The body of the mandible supports the mandibular teeth within the alveolar process. The rami bear the coronoid and condylar processes. Each condyle articulates with the adjacent temporal bone at the temporomandibular joint.
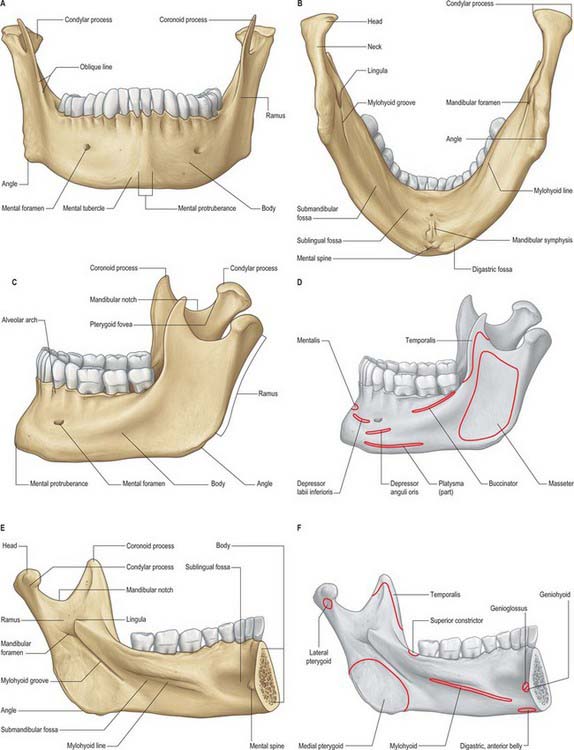
Fig. 31.3 Adult mandible. A, anterior view; B, inferior view; C, lateral view (with muscle attachments in D); E, internal view (with muscle attachments in F).
(Redrawn with permission from Sobotta 2006.)
Body
The body is somewhat U-shaped. It has external and internal surfaces separated by upper and lower borders. Anteriorly, the upper external surface shows an inconstant faint median ridge indicating the site of the fused symphysis menti. Inferiorly this ridge divides to enclose a triangular mental protuberance; its base is centrally depressed but raised on each side as a mental tubercle. The mental protuberance and mental tubercles constitute the chin. The mental foramen, from which the mental neurovascular bundle emerges, lies below either the interval between the premolar teeth, or the second premolar tooth, midway between the upper and lower borders of the body. The posterior border of the foramen is smooth, and accommodates the nerve as it emerges posterolaterally. A faint external oblique line ascends backwards from each mental tubercle, and sweeps below the mental foramen; it becomes more marked as it continues into the anterior border of the ramus.
The lower border of the body, the base, extends posterolaterally from the mandibular symphysis into the lower border of the ramus behind the third molar tooth. Near the midline on each side there is a rough digastric fossa which gives attachment to the anterior belly of digastric. Behind the fossa the base is thick and rounded: it has a slight anteroposterior convexity which changes to a gentle concavity as the ramus is approached, and so the base has an overall sinuous profile.
The upper border, the alveolar part, contains 16 alveoli for the roots of the lower teeth. It consists of buccal and lingual plates of bone joined by interdental and inter-radicular septa. Near the second and third molar teeth the external oblique line is superimposed upon the buccal plate. Like the maxilla, the form and depth of the tooth sockets is related to the morphology of the roots of the mandibular teeth. The sockets of the incisor, canine and premolar teeth usually contain a single root, while those for the three molar teeth each contain two or three roots. The third molar is variable in its position and root presentation. It may be impacted vertically, horizontally, mesially or distally, and its roots may be bulbous, hooked, divergent or convergent, and occasionally embrace the mandibular (inferior dental) canal (see Ch. 30). The internal surface of the mandible is divided by an oblique mylohyoid line that gives attachment to mylohyoid (and, above its posterior end, to the superior pharyngeal constrictor, some retromolar fascicles of buccinator, and the pterygomandibular raphe behind the third molar). The mylohyoid line extends from a point approximately 1 cm from the upper border behind the third molar as far forwards as the mental symphysis; it is sharp and distinct near the molars, but faint further forwards. The mylohyoid groove extends downwards and forwards from the ramus below the posterior part of the mylohyoid line and contains the mylohyoid neurovascular bundle. The area below the line is a slightly concave submandibular fossa and is related to the submandibular gland. The area above the line widens anteriorly into a triangular sublingual fossa and is related to the sublingual gland: the bone is covered by oral mucosa above the sublingual fossa as far back as the third molar. In an edentulous subject it may be necessary to reduce any ridge-like prominence of the mylohyoid line in order that dentures may fit without traumatizing the overlying oral mucosa.
Above the anterior ends of the mylohyoid lines, the posterior symphysial aspect bears a small elevation, often divided into upper and lower parts, the mental spines (genial tubercles). The spines are sometimes fused to form a single eminence, or they may be absent, in which case their position is indicated merely by an irregularity of the surface. The upper part gives attachment to genioglossus, the lower part to geniohyoid. Above the mental spines, most mandibles display a lingual (genial) foramen which opens into a canal that traverses the bone to 50% of the buccomandibular dimension of the mandible, and which contains a branch of the lingual artery. A rounded torus mandibularis sometimes occurs above the mylohyoid line, medial to the molar roots: it is only of clinical significance if repeatedly traumatized.
Ramus
The mandibular ramus is quadrilateral, and has two surfaces (lateral and medial), four borders (superior, inferior, anterior and posterior) and two processes (coronoid and condylar). The lateral surface is relatively featureless and bears the (external) oblique ridge in its lower part. The medial surface presents, a little above centre, the mandibular foramen, through which the inferior alveolar neurovascular bundle passes to gain access to the mandibular canal (see below). Anteromedially, the mandibular foramen is overlapped by a thin, sharp triangular spine, the lingula, to which the sphenomandibular ligament is attached, and which is also the landmark for an inferior alveolar local anaesthetic block injection. Below and behind the foramen, the mylohyoid groove runs obliquely downward and forward.
The inferior border is continuous with the mandibular base and meets the posterior border at the angle, which is typically everted in males, but frequently inverted in females. The thin superior border bounds the mandibular incisure, which is surmounted in front by the somewhat triangular, flat, coronoid process and behind by the condylar process. The thick, rounded posterior border extends from the condyle to the angle, and is gently convex backwards above, and concave below. The anterior border is thin above, where it is continuous with the edge of the coronoid process, and thicker below where it is continuous with the external oblique line. The temporal crest is a ridge that descends on the medial side of the coronoid process from its tip to the bone just behind the third molar tooth. The triangular depression between the temporal crest and the anterior border of the ramus is the retromolar fossa.
The ramus and its processes provide attachment for the four primary muscles of mastication. Masseter is attached to the lateral surface, medial pterygoid is attached to the medial surface, temporalis is inserted into the coronoid process and lateral pterygoid is attached to the condyle.
Mandibular canal
The mandibular foramen leads into the mandibular canal, which runs obliquely downward and forward within the ramus, and then horizontally forward within the body under the roots of the molar teeth, with which it communicates by small openings. The canal is not always easy to define, especially anterior to the mental foramen. Its walls may be formed either by a thin layer of cortical bone or, more frequently, by trabecular bone. Although the buccal-lingual and superior-inferior positions of the canal vary considerably between mandibles, in general, the mandibular canal is situated nearer the lingual cortical plate in the posterior two-thirds of the bone, and closer to the labial cortical plate in the anterior third. Bilateral symmetry (location of the canal in each half of the mandible) is reported to be common. Near the mental foramen the inferior alveolar nerve branches into the mental nerve, which ultimately leaves the mandible via the mental foramen, and the incisive nerve, which remains within the bone and supplies the anterior teeth. The mental nerve may extend anteriorly for 2–3 mm within the mandible before curving back to the mental foramen (the ‘anterior loop’ of the mental nerve). The intra osseous anatomy of the mental nerve is of particular importance in dental implant surgery: the nerve may be damaged if the interforaminal area of the mandible is invaded during surgery or while harvesting block grafts from the symphysial region.
Coronoid process
The coronoid process projects upwards and slightly forwards as a triangular plate of bone. Its posterior border bounds the mandibular incisure, and its anterior border continues into that of the ramus.
Condylar process
The mandibular condyle varies considerably both in size and shape. When viewed from above, the condyle is roughly ovoid in outline, its anteroposterior dimension (approximately 1 cm) being roughly half its mediolateral dimension. The medial aspect of the condyle is wider than the lateral. The long axis of the condyle is not at right angles to the ramus, but diverges posteriorly from a strictly coronal plane. Thus, the lateral pole of the condyle lies slightly anterior to the medial, and if the long axes of the two condyles are extended, they meet at an obtuse angle (approximately 145°) at the anterior border of the foramen magnum. The articular head of the condyle joins the ramus through a thin bony projection, the neck of the condyle. The pterygoid fovea, a small depression situated on the anterior surface of the neck below the articular surface, receives part of the attachment of lateral pterygoid.
The condyle consists of a core of cancellous bone covered by a thin outer layer of compact bone whose intra-articular aspect is covered by layers of fibrocartilage. The condyle is the commonest site of mandibular fractures.
Accessory foramina of the mandible
These are usually unnamed and infrequently described, yet they are numerous. They may transmit auxiliary nerves to the teeth (from facial, mylohyoid, buccal, transverse cervical cutaneous and other nerves), and their occurrence is significant in dental anaesthetic blocking techniques.
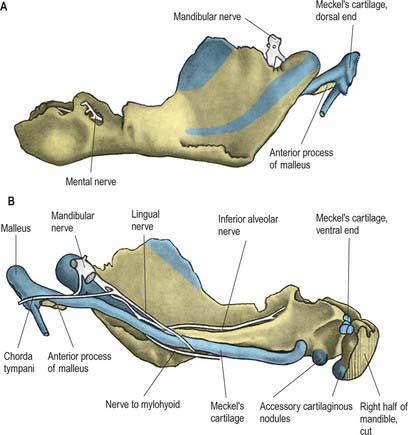
Ossification
The mandible forms in dense fibromembranous tissue lateral to the inferior alveolar nerve and its incisive branch, and also in the lower parts of Meckel’s cartilage (first branchial arch). Each half is ossified from a centre that appears near the mental foramen about the sixth week in utero. From this site, ossification spreads medially and posterocranially to form the body and ramus, first below, and then around, the inferior alveolar nerve and its incisive branch. Ossification then spreads upwards, initially forming a trough, and later crypts, for the developing teeth. By the tenth week, Meckel’s cartilage below the incisor rudiments is surrounded and invaded by bone. Secondary cartilages appear later (Fig. 31.4): a conical mass, the condylar cartilage, extends from the mandibular head downwards and forwards in the ramus, and contributes to its growth in height. Although it is largely replaced by bone by midfetal life, its proximal end persists as proliferating cartilage under the fibrous articular lining until about the third decade. Another secondary cartilage, which soon ossifies, appears along the anterior coronoid border, and disappears before birth. One or two cartilaginous nodules also occur at the symphysis menti. At about the seventh month in utero these may ossify as variable mental ossicles in symphysial fibrous tissue: they unite with adjacent bone before the end of the first postnatal year.
Age changes in the mandible
At birth the two halves of the mandible are united by a fibrous symphysis menti (Fig. 31.5). The anterior ends of both rudiments are covered by cartilage, separated only by a symphysis. Until fusion occurs, new cells are added to each cartilage from symphysial fibrous tissue, and ossification on its mandibular side proceeds towards the midline. When the latter process overtakes the former, and ossification extends into median fibrous tissue, the symphysis fuses. At this stage the body is a mere shell which encloses the imperfectly separated sockets of deciduous teeth. The mandibular canal is near the lower border, and the mental foramen opens below the first deciduous molar and is directed forwards. The coronoid process projects above the condyle.
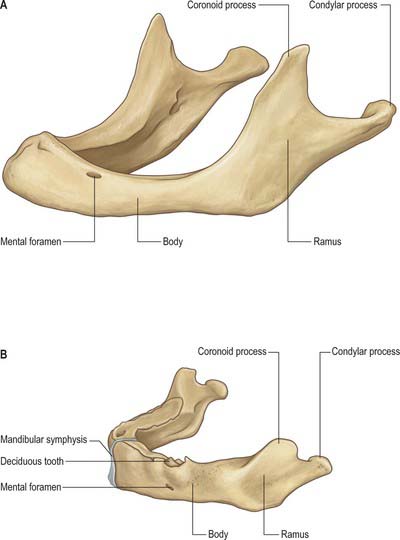
Fig. 31.5 A, Edentulous mandible; note position of mental foramen; B, Neonatal mandible.
(Redrawn with permission from Sobotta 2006.)
During the first three postnatal years, the two halves join at their symphysis from below upwards, although separation near the alveolar margin may persist into the second year. The body elongates, especially behind the mental foramen, providing space for three additional teeth. During the first and second years, as a chin develops, the mental foramen alters direction: it no longer faces forwards but now faces backwards, as in the adult mandible, and accommodates the changing direction of the emerging mental nerve.
In general terms, increase in height of the body of the mandible is achieved primarily by formation of alveolar bone associated with the developing and erupting teeth, although some bone is also deposited on the lower border. Increase in length of the mandible is accomplished by deposition of bone on the posterior surface of the ramus and concomitant compensatory resorption on the anterior surface (accompanied by deposition of bone on the posterior surface of the coronoid process and resorption on the anterior surface of the condylar process). Increase in width of the mandible is produced by deposition of bone on the outer surface of the mandible and resorption on the inner surface. An increase in the comparative size of the ramus compared with the body of the mandible occurs during postnatal growth and tooth eruption.
The role of the condylar cartilages in mandibular growth remains controversial. One view states that continued proliferation of this cartilage is primarily responsible for the increase in both the mandibular length and the height of the ramus. Alternatively, there is persuasive experimental evidence that proliferation of the condylar cartilage is an adaptive response to function, rather than being genetically determined. Condylar growth and remodeling has been shown to be influenced significantly by local factors, notably movement and loading of the temporomandibular joint, and to be relatively immune to systemic influences such as vitamin C and D deficiency. Considering the changes that occur in the dentition throughout life, continuous adaptation of the temporomandibular articulation is required in order to maintain functional occlusal alignment between the upper and lower arches of teeth: this adaptation is thought to be largely the result of ongoing condylar remodelling.
In adults, alveolar and subalveolar regions are about equal in depth, and the mental foramen appears midway between the upper and lower borders. If teeth are lost, alveolar bone is resorbed, which means that the mandibular canal (which runs parallel to the mylohyoid line) and the mental foramen come to lie much nearer to the superior border (Fig. 31.5), indeed, sometimes they may both disappear, so that the nerves lie just beneath the oral mucosa.
TEMPOROMANDIBULAR JOINT
The temporomandibular joint is a synovial joint between the articular fossa (also known as the mandibular fossa or glenoid fossa) of the temporal bone above and the mandibular condyle. It is unusual in that its articular surfaces are lined by fibro-cartilage (rather than hyaline cartilage) and its joint cavity is divided into two by an articular disc.
The articular eminence, a transversely elliptical region sinuously curved in the sagittal plane and tilted downwards anteriorly at approximately 25° to the occlusal plane, forms most of the articular surface of the mandibular fossa. Its steepness is variable, and it becomes flatter in the edentulous subject. Its anterior limit is the summit of the articular eminence, a transverse ridge that extends laterally out to the zygomatic arch as far as the articular tubercle. Articular tissue extends anteriorly beyond the articular summit and on to the preglenoid plane. Posteriorly it extends behind the depth of the fossa as far as the squamotympanic fissure. A postglenoid tubercle (at the root of the zygomatic arch, just anterior to the fissure) is usually poorly developed in human skulls.
The articular surface of the mandibular condyle is slightly curved and tilted forward at approximately 25° to the occlusal plane. Like the articular eminence, its slope is variable. In the coronal plane its shape varies from that of a gable (particularly marked in those whose diet is hard), to roughly horizontal in the edentulous.
It is probably impossible to measure the pressure developed on the articular surfaces of the human jaw joint when biting, however direct measurement of loads across the joint in animals has demonstrated significant intermittent loading during mastication. There is also irrefutable theoretical evidence based on Newtonian mechanics that the jaw joint is a weight-bearing joint. With a vertical bite force of 500 N on the left first molar, the right condyle must support a load of well over 300 N (Osborn 1995a). The non-working condyle is more loaded than the condyle on the working side, which may help explain why patients with a fractured condyle choose to bite on the side of the fracture.
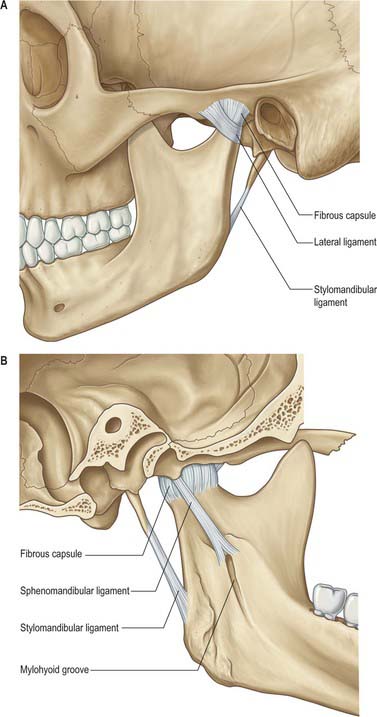
Fibrous capsule
The lower part of the joint is surrounded by tight fibres which attach the condyle of the mandible to the disc. The upper part of the joint is surrounded by loose fibres which attach the disc to the temporal bone (Fig. 31.6). Thus the articular disc is attached separately to the temporal bone and to the mandibular condyle forming what could be considered two joint capsules. Longer fibres joining the condyle directly to the temporal bone may be regarded as reinforcing. The capsule is attached above to the anterior edge of the preglenoid plane, posteriorly to the lips of the squamotympanic fissure, between these to the edges of the articular fossa, and below to the periphery of the neck of the mandible.
Ligaments
Sphenomandibular ligament
The sphenomandibular ligament is medial to, and normally separate from, the capsule (Fig. 31.6). It is a flat, thin band that descends from the spine of the sphenoid and widens as it reaches the lingula of the mandibular foramen. Some fibres traverse the medial end of the petrotympanic fissure and attach to the anterior malleolar process. This part is a vestige of the dorsal end of Meckel’s cartilage.
With the jaw closed, there is approximately 5 mm slack within the ligament, but it becomes taut when the jaw is about half open. Lateral pterygoid and the auriculotemporal nerve are lateral relations, the chorda tympani nerve lies medial near its upper end and medial pterygoid is an inferomedial relation. The sphenomandibular ligament is separated from the neck of the mandible below lateral pterygoid by the maxillary artery and from the ramus of the mandible by the inferior alveolar vessels and nerve and a parotid lobule. At this point the vessels and nerve to mylohyoid pierce the ligament. It is separated from the pharynx by fat and a pharyngeal vein.
Stylomandibular ligament
The stylomandibular ligament is a thickened band of deep cervical fascia that stretches from the apex and adjacent anterior aspect of the styloid process to the angle and posterior border of the mandible (Fig. 31.6). Its position and orientation indicate that it cannot mechanically constrain any normal movements of the mandible and does not seem to warrant the status of a ligament of the joint.
Temporomandibular (lateral) ligament
The broad temporomandibular ligament is attached above to the articular tubercle on the root of the zygomatic process of the temporal bone (Fig. 31.6). It extends downwards and backwards at an angle of approximately 45° to the horizontal, to attach to the lateral surface and posterior border of the neck of the condyle, deep to the parotid gland. A short, almost horizontal, band of collagen connects the articular tubercle in front to the lateral pole of the condyle behind. It may function to prevent posterior displacement of the resting condyle.
Synovial membrane
The synovial membrane lines the inside of the capsule of the joint but does not extend to cover the disc or the articular surfaces.
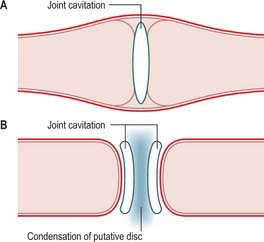
Development of the temporomandibular joint
The bony components of the secondary jaw joint develop in membrane as two separate ectomesenchymal condensations between the 8th and 12th week in utero. This arrangement is different from that seen with most synovial joints, where a single blastema cavitates to form a joint space and the articulating bones are derived from the same condensation of tissue (see Ch. 51). The separate development of the temporal and condylar parts of the temporomandibular joint means that the articular surface of each bone is covered by a persisting layer of proliferative cells that is continuous with the periosteum surrounding each separate bony component (Fig. 31.7).
Articular surfaces
The fibrocartilaginous covering of the condyle is composed of four distinct layers (De Bont et al 1984). The most superficial layer consists of densely packed fibres of type I collagen that are arranged mostly parallel to the articular surface. This covers a thin cellular layer, the proliferative zone, that is continuous with the cambial layer of the periosteum beyond the margins of the joint. The third layer, of hypertrophic cartilage, is rich in intercellular matrix: it contains chondrocytes scattered throughout its depth, and randomly oriented fibres of collagen type II. The fourth layer, immediately above the subchondral bone, is the zone of calcification. Although the number of chondrocytes within the hypertrophic zone decreases with age, undifferentiated mesenchymal cells have been identified in post mortem specimens of all ages (Hansson 1977). This indicates that a capacity for proliferation persists in condylar cartilage, and may be the reason why condylar remodeling occurs throughout life (Robinson 1993, Toller 1974).
Articular disc
The transversely oval articular disc is composed predominantly of dense fibrous connective tissue with some chondrification in areas of maximum loading (Fig. 31.8). It has a thick margin which forms a peripheral anulus and a central depression in its lower surface that accommodates the articular surface of the mandibular condyle. The depression probably develops as a mechanical response to pressure from the condyle as it rotates inside the anulus. The disc is stabilized on the condyle in three ways. Its edges are fused with the part of the capsular ligament that tightly surrounds the lower joint compartment and is attached around the neck of the condyle; well-defined bands in the capsular ligament attach the disc to the medial and lateral poles of the condyle, and additionally, the thick anulus prevents the disc sliding off the condyle, provided that the condyle and disc are firmly lodged against the articular fossa (as is normally the case).
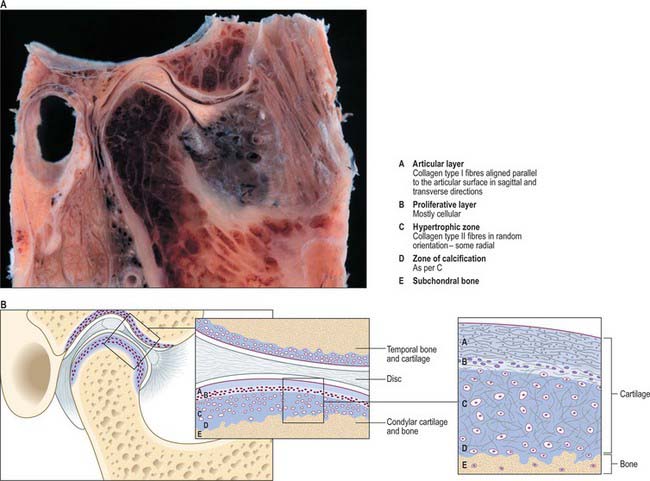
Fig. 31.8 A,B, Sagittal sections through the right temporomandibular joint. A, Note the relationship of the external auditory meatus and articular disc to the mandibular condyle. B, The microstructure of condylar cartilage.
(By courtesy of Professor Cristina Manzanares Céspedes, Anatomy and Human Embryology Unit, Bellvitge Campus, University of Barcelona.)
In sagittal section, the disc appears to possess a thin intermediate zone and thickened anterior and posterior bands, and its upper surface appears concavo-convex where it fits against the convex articular eminence and the concavity of the articular fossa. Posteriorly the disc is attached to a region of loose vascular and nervous tissue which splits into two laminae, the bilaminar region: unlike the rest of the disc, its normal function is to provide attachment rather than intra-articular support. The upper lamina, composed of fibroelastic tissue, is attached to the squamotympanic fissure, and the lower lamina, composed of fibrous non-elastic tissue, is attached to the back of the condyle. The bilaminar region contains a venous plexus, but the central part of the disc is avascular. Cells in the disc also secrete chondroitin sulphate (a glycosaminoglycan found in cartilage) which is most heavily concentrated in the centre of the disc and which probably gives the disc some of the resilience and compressive strength of cartilage. The amount increases in response to load and to age, and by the fifth decade the disc shows signs of ageing including fraying, thinning and perforation.
Functions of the articular disc
The functions of the articular disc remain controversial. It is generally believed that the disc helps to stabilize the condyle within the temporomandibular joint (although see below). The articulating surfaces of the mandibular condyle and the articular fossa fit together poorly and so are separated by an irregular space. Muscle forces control the position of the mandible, and therefore of the condyle, in relation to the articular eminence, and these in turn determine the shape and thickness of the irregular space. The position of the disc is controlled by neuromuscular forces: the upper head of lateral pterygoid anteriorly, and the elastic tissue in the bilaminar region posteriorly, together pull the disc forward or backward to keep the joint space filled and thereby stabilize the condyle.
The presence of an articular disc may also reduce wear, because the frictional force on the condyle and the articular eminence is halved by separating slide and rotation into different joint compartments, and may aid lubrication of the joint by storing fluid squeezed out from loaded areas to create a weeping lubricant.
There is an alternative view that a slippery articular disc doubles the number of virtually friction-free sliding surfaces, and so destabilizes the condyle in the same way that stepping on a banana skin destabilizes the foot. All other joints are most heavily loaded when their articular surfaces are closely fitted together, creating a large area of contact, and braced to prevent further movement. However the condyle of the mandible is most heavily loaded when it is required to move, sliding backward during the buccal phase of the power stroke of a masticatory cycle on the opposite side of the jaw.
Relations
Superiorly a thin plate of temporal bone (2–3 mm) separates the upper joint space from the middle cranial fossa. This bony partition is occasionally breached inadvertently during surgery to the joint, particularly for release of ankylosis, or rarely by the condyle being driven superiorly by violent trauma to the mandible. The maxillary artery and its proximal branches, most notably the middle meningeal artery, lie medially, just beyond the joint capsule. The uppermost part of the parotid capsule enclosing the branches of the facial nerve that supply the muscles of the upper face, including obicularis oculi, are lateral to the joint capsule: the thread-like nerves are at risk during surgical approach to the joint. The upper part of the infratemporal space, which contains the two heads of lateral pterygoid, is anterior to the condyle (Fig. 31.9). It is into this space anterior to the articular eminence that the condyle is displaced in cases of dislocation of the TMJ or fracture dislocation of the condylar head. Posteriorly is the tegmen tympani and behind it the middle ear cavity. Perforation through this thin bony wall into the middle ear is a recognized complication of TMJ arthroscopy. Just below the joint, the maxillary artery winds around the posterior aspect of the condylar neck.
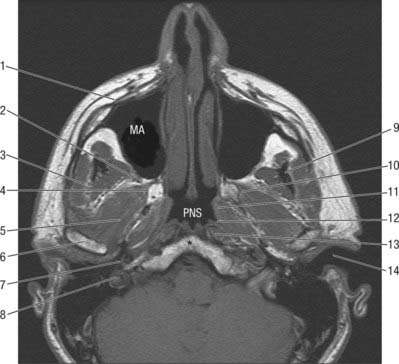
Fig. 31.9 Axial MRI at level of external acoustic meatus: 1. Body of zygoma; 2. Pterygopalatine fossa; 3. Temporalis; 4. Medial pterygoid plate; 5. Lateral pterygoid; 6. Condylar head; 7. Internal carotid artery; 8. Jugular bulb/foramen; 9. Coronoid process; 10. Lateral pterygoid plate; 11. Torus tubarius; 12. Fossa of Rosenmüller; 13. Longus colli; 14. External auditory meatus. MA, Maxillary antrum; PNS, Postnasal space. *, Anterior arch of atlas.
Vascular supply and innervation
The articular tissues and the dense part of the articular disc have no nerve supply. Branches of the auriculotemporal and masseteric nerves and postganglionic sympathetic nerves supply the tissues associated with the capsular ligament and the looser posterior bilaminar extension of the disc. The temporomandibular joint capsule, lateral ligament and retroarticular tissue contain mechanoreceptors and nociceptors. The input from mechanoreceptors provides a source of proprioceptive sensation that helps control mandibular posture and movement.
The joint derives its arterial supply from the superficial temporal artery laterally and the maxillary artery medially. Penetrating vessels that supply lateral pterygoid may also supply the condyle. Veins drain the anterior aspect of the joint and associated tissues into the plexus surrounding lateral pterygoid, and posteriorly they drain into the vascular region that separates the two laminae of the bilaminar region of the disc. Pressure produced by forward and backward movement of the condyle shunts blood between these regions. Lymphatics drain deeply to the upper cervical lymph nodes surrounding the internal jugular vein.
Jaw movements
Movements of the condyle in the temporomandibular joint
The major function of the mandible is to exert, via the teeth, the force necessary to break down food into smaller particles and so facilitate digestion. Pure vertical movements of the lower teeth create a crushing force that is ineffective in breaking up tough fibrous food. Man uses a lateral movement of the lower jaw to create a shear component of force that enhances the effectiveness of the power stroke of mastication. Bodily lateral movement of the whole jaw, the Bennett shift, is insignificant. Extensive lateral movement is only possible when the jaw is rotated horizontally about one condyle while the other condyle slides backward and forward.
The temporomandibular joint is structurally adapted to accommodate both sliding and rotation in a parasagittal plane. Sliding occurs because the capsular ligament which surrounds the upper joint compartment is loose, whereas the capsular ligament which encloses the lower joint compartment is tight, and only allows the condyle to rotate over the depression inside the anulus of the articular disc. The normal range of maximum mouth opening measured between the upper and lower incisor tips is 35–50 mm. The adult range of movements is reached at around 10 years in females and 15 years in males. Lateral excursions of the chin can normally achieve 8–12 mm of movement at the lower incisors.
Symmetrical opening
Symmetrical jaw opening is associated with preparation for incising. At the start, each mandibular condyle rotates in the lower joint compartment inside the anulus of its disc. After a few degrees of opening, the condyle continues rotating inside its disc, and, in addition, both slide forward down the articular eminence of the upper joint compartment. Without this forward slide, it becomes impossible to continue opening the jaw beyond a gape of approximately 25 mm.
There are conflicting views about the reason why forward slide occurs, probably because direct experimental testing is not possible. No other animal has an articular eminence constraint and ligaments comparable to man, which means that most supporting evidence for any theory is based on analyses of human joint dysfunction. It has been argued that a sensory input from the rotary movement, possibly from either the joint capsule or the jaw muscles, initiates a response that reflexly activates muscles that cause the slide. The fact that the condyle in a cadaver still slides forward when the jaw is rotated open suggests that it is not a neuromuscular response, but that it is the mechanical result of physical constraints. When the jaw is rotated open the temporomandibular ligament rapidly becomes taut (Osborn 1995b). The taut ligament acts as a constraint that allows the mandible only two rotary movements: it can swing about the upper attachment of the ligament and rotate about the lower attachment. The lower end of the taut ligament acts as a moving fulcrum that converts the downward and backward pull of the opening rotary force (created at the front by digastric and geniohyoid) into one that drives the condyle upward and forward into the concavity of the overlying articular disc. This now pushes the disc forward. Swing about the upper attachment creates space above for the disc to slide further forward which is possible because the upper part of the capsular ligament is loose. The two movements, rotation and swing, are inextricably linked by the taut ligament and, via the condyle, combine to keep the disc in firm contact with the articular eminence while the jaw is opened. The disc is stabilized by its tight attachment to the condyle and by the thickened margins of its anulus that prevent it sliding through the thinner compressed region between the centre of the condyle and the articular eminence.
As forward slide of the condyle continues, the controlling influence exerted by the temporomandibular ligament diminishes. The lingula of the mandible moves away from the spine of the sphenoid, tautening the originally slack sphenomandibular ligament, which now acts in the same way as the temporomandibular ligament, to maintain the condyle against the articular eminence. Symmetrical opening thus appears to consist of at least three separate phases: an early phase controlled by the temporomandibular ligament and articular eminence; a short middle phase in which either both, or neither, temporomandibular and sphenomandibular ligaments act to constrain movements; and a late phase controlled by the sphenomandibular ligament and articular eminence.
Changes in disc position during movement
With the teeth in occlusion, the condyle is in the glenoid fossa and the intra-articular disc sits on the condylar head; its posterior band above the summit of the condyle (Fig. 31.10A). As mouth opening begins (Fig. 31.10B), the condyle rotates within the lower joint space and the disc remains stationary. At about mid-opening, the condyle and disc begin to move forward together so that their relative position is maintained (Fig. 31.10C). At maximum gape (Fig. 31.10D) the condylar head slides further anteriorly than the disc so that the anterior band of the articular disc is above the summit of the condyle. Mouth closure involves the disc moving back in tandem with the condyle (Fig. 31.10E) which also reverses its angular rotation (Fig. 31.10F) to reassume the starting position of the cycle.
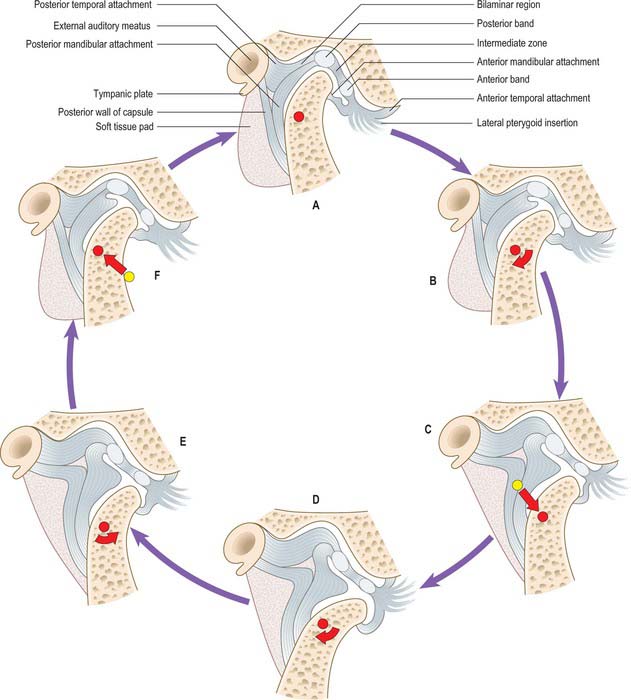
Fig. 31.10 Changing relationships of the condyle of the mandible, the articular disc and the articular surface of the temporal bone during one complete opening (A → D) and closing (D → A) cycle of the mouth.
Commonly, the shifts in disc position become out of phase with those of the condyle, which causes obstruction to smooth jaw movement. The disc is typically pulled anteromedially by lateral pterygoid, so preventing forward translation of the condyle. As the force from the condyle on the disc increases, the elastic posterior attachments of the disc are stretched until the resistance to movement is overcome and the energy that had been stored is then released with an audible click (audible to the patient, and occasionally to others). The normal disc–condyle relation is then reestablished and the mouth is free to achieve maximum gape (Fig. 31.10C,D). The disc may then snap back in front of the condyle on mouth closure. This phenomenon is called reciprocal clicking or disc displacement with reduction.
If the disc is pulled completely anterior to the condylar head, so that it is not reduced during opening, the condyle is prevented from any forward translation and mouth opening is limited to the rotational component and therefore a maximum gape of 25 mm. This is also a common clinical condition and is known appropriately as closed lock or disc displacement without reduction.
Eccentric jaw opening
Eccentric jaw opening is associated with preparing for the power stroke of mastication. The mandibular condyle on the non-working side slides back and forth during lateral movements associated with the power stroke on the working side. Although the jaw muscles now have the major control over mandibular movements, the temporomandibular and sphenomandibular ligaments keep the condyle firmly against its articular eminence during opening.
Eccentric and symmetrical jaw closing
The resultant of the jaw closing muscles of the mandible has a component that forces the joint surfaces together. This compresses the joint tissues and potentially shortens the ligaments so that they no longer constrain jaw movements. Under these conditions, jaw movements and the positions of the condyles are controlled by neuromuscular processes (within the limits of constraints imposed by the articular eminence, the occluding surfaces of the teeth and the presence of food between them). Note that the non-working condyle moves the furthest, and is the most heavily loaded, during the power stroke of mastication. The loads on each joint, balancing and working, drive each condyle more forcefully into its articular eminence.
The envelope of motion
The envelope of motion is the volume of space within which all movements of a point on the mandible have to occur because the limits are set by anatomical features, i.e. by the shape or size of the upper and lower jaws, by tooth contacts, and by the attachment of muscle and ligaments.
In consciously controlled movement of the jaw from the rest position to the fully opened position, the trajectory of the mandibular incisal edge is two-phased. The first phase is a hinge-like movement during which the condyles are retruded within the mandibular fossae. When the teeth are opened by approximately 25 mm, the second phase of opening occurs by anterior movement or protrusion of the condyles down the articular eminences with further rotation.
If conscious effort is used, a closure path can then be followed in which the jaw is closed to an extreme protruded tooth contact position after which it has to be retruded to the starting position. The free, habitual, unconscious movement during both jaw opening and closing has a significantly more limited trajectory. Similar considerations apply to lateral movements: mandibular rotation around a retruding condyle and the protraction of the opposite condyle are anatomically limiting factors that are again rarely encountered in normal function.
Imaging of the temporomandibular joint
Magnetic resonance imaging (MRI) and arthrography have enriched the information available about pathological changes that can occur in all components of the joint, particularly the disc. It is of interest that the advent of these techniques has coincided with a significant reduction in numbers of open surgical operations for abnormality of disc position (collectively known as internal derangements). MRI has shown that although disc position and clinical symptoms are often linked, a significant proportion of subjects with no TMJ abnormality in terms of function have grossly abnormal disc movements, and that patients who have undergone disc repositioning procedures often show functional improvement despite persistent displacement of their intra-articular disc. It would appear that the adaptive remodeling capacity of the joint, especially of the mandibular condyle, is an important mechanism for maintaining function of the TMJ.
MUSCLES
The four principal muscles of mastication are medial and lateral pterygoid, temporalis and masseter: their actions produce movements of the mandible at the temporomandibular joints. The infratemporal fossa contains medial and lateral pterygoid and the tendon of temporalis. Masseter lies on the face, on the lateral surface of the ramus of the mandible, but will be considered here.
Masseter
Masseter (Fig. 31.11) consists of three layers which blend anteriorly. The superficial layer is the largest. It arises by a thick aponeurosis from the maxillary process of the zygomatic bone and from the anterior two-thirds of the inferior border of the zygomatic arch. Its fibres pass downwards and backwards, to insert into the angle and lower posterior half of the lateral surface of the mandibular ramus. Intramuscular tendinous septa in this layer are responsible for the ridges on the surface of the ramus. The middle layer of masseter arises from the medial aspect of the anterior two-thirds of the zygomatic arch and from the lower border of the posterior third of this arch. It inserts into the central part of the ramus of the mandible. The deep layer arises from the deep surface of the zygomatic arch and inserts into the upper part of the mandibular ramus and into its coronoid process. There is still debate as to whether fibres of masseter are attached to the anterolateral part of the articular disc of the temporomandibular joint. Masseteric hypertrophy, e.g. in response to excessive use of masseter, may be treated by surgical reduction from the deep aspect of masseter or injections of botulinus toxin to paralyse the motor nerves.
Skin, platysma, risorius, zygomaticus major, the parotid gland and duct, branches of the facial nerve and the transverse facial branches of the superficial temporal vessels are all superficial relations. Temporalis and the ramus of the mandible lie deep to masseter. The anterior margin of masseter is separated from buccinator and the buccal branch of the mandibular nerve by a buccal pad of fat and crossed by the facial vein. The posterior margin of the muscle is overlapped by the parotid gland. The masseteric nerve and artery reach the deep surface of masseter by passing over the mandibular incisure (mandibular notch).
Masseter is supplied by the masseteric branch of the maxillary artery, the facial artery and the transverse facial branch of the superficial temporal artery.
Masseter elevates the mandible to occlude the teeth in mastication and has a small effect in side-to-side movements, protraction and retraction. Its electrical activity in the resting position of the mandible is minimal.
Submasseteric space infections
Sometimes infection around a mandibular third molar tooth tracks backwards, lateral to the mandibular ramus and pus localizes deep to the attachment of masseter in the submasseteric tissue space. Such an abscess, lying deep to this thick muscle produces little visible swelling, but is accompanied by profound muscle spasm and severe limitation of jaw opening (trismus).
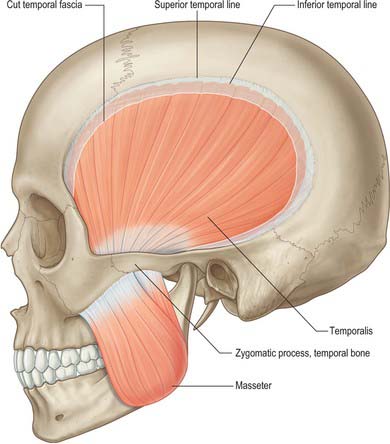
Temporalis
Temporalis (Fig. 31.11) arises from the whole of the temporal fossa up to the inferior temporal line – except the part formed by the zygomatic bone – and from the deep surface of the temporal fascia. Its fibres converge and descend into a tendon which passes through the gap between the zygomatic arch and the side of the skull. A plane exists beneath the temporal fascia, which is attached to the superior surface of the zygomatic arch, and the muscle, which passes beneath the arch. An elevator introduced into this plane through an incision above the hairline may therefore be placed beneath a fractured zygomatic arch or bone in order to reduce the fracture (Gillies approach). Temporalis is attached to the medial surface, apex, anterior and posterior borders of the coronoid process and to the anterior border of the mandibular ramus almost up to the third molar tooth. Its anterior fibres are orientated vertically, the most posterior fibres almost horizontally, and the intervening fibres with intermediate degrees of obliquity, in the manner of a fan. Fibres of temporalis may occasionally gain attachment to the articular disc.
Skin, auriculares anterior and superior, temporal fascia, superficial temporal vessels, the auriculotemporal nerve, temporal branches of the facial nerve, the zygomaticotemporal nerve, the epicranial aponeurosis, the zygomatic arch and the masseter muscle are all superficial relations. Posterior relations of temporalis are the temporal fossa above and the major components of the infratemporal fossa below. Behind the tendon of the muscle, the masseteric nerve and vessels traverse the mandibular notch. The anterior border is separated from the zygomatic bone by a mass of fat.
Temporalis is supplied by the deep temporal branches from the second part of the maxillary artery. The anterior deep temporal artery supplies 20% of the muscle anteriorly, the posterior deep temporal supplies 40% of the muscle in the posterior region and the middle temporal artery supplies 40% of the muscle in its mid-region.
Temporalis elevates the mandible and so closes the mouth and approximates the teeth. This movement requires both the upward pull of the anterior fibres and the backward pull of the posterior fibres, because the head of the mandibular condyle rests on the articular eminence when the mouth is open. The muscle also contributes to side-to-side grinding movements. The posterior fibres retract the mandible after it has been protruded.
Lateral pterygoid
Lateral pterygoid (Fig. 31.12) is a short, thick muscle consisting of two parts. The upper head arises from the infratemporal surface and infratemporal crest of the greater wing of the sphenoid bone. The lower head arises from the lateral surface of the lateral pterygoid plate. From the two origins, the fibres converge, and pass backwards and laterally, to be inserted into a depression on the front of the neck of the mandible (the pterygoid fovea). A part of the upper head may be attached to the capsule of the temporomandibular joint and to the anterior and medial borders of its articular disc. Unlike the other muscles of mastication, lateral pterygoid is not pennate, nor does it have a significant number of Golgi tendon organs associated with its attachments.
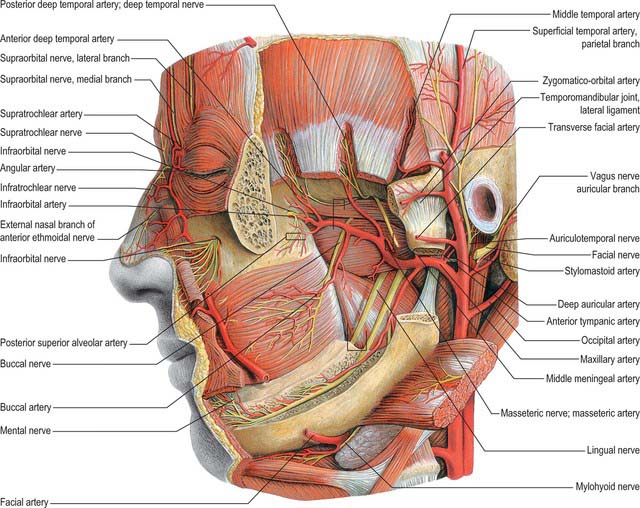
Fig. 31.12 Arteries and nerves of the head; deeper lateral regions. Most of the zygomatic arch and the ramus and body of the mandible have been removed; masseter has been cut and reflected laterally.
(From Sobotta 2006.)
The mandibular ramus and masseter, the maxillary artery – which crosses either deep or superficial to the muscle – and the superficial head of medial pterygoid and the tendon of temporalis, are all superficial relations. Deep to the muscle are the deep head of medial pterygoid, the sphenomandibular ligament, the middle meningeal artery, and the mandibular nerve. The upper border is related to the temporal and masseteric branches of the mandibular nerve and the lower border is related to the lingual and inferior alveolar nerves. A deeply placed posterior superior alveolar nerve block has been known to also anaesthetize the lingual nerve. The buccal nerve and the maxillary artery pass between the two heads of the muscles. In temporomandibular joint dysfunction syndrome, spasm of lateral pterygoid can give rise to tenderness when palpating behind the maxillary tuberosity high in the buccal sulcus (the pterygoid sign).
Lateral pterygoid is supplied by pterygoid branches from the maxillary artery which are given off as the artery crosses the muscle and from the ascending palatine branch of the facial artery.
The nerves to lateral pterygoid (one for each head) arise from the anterior trunk of the mandibular nerve, deep to the muscle. The upper head and the lateral part of the lower head receive their innervation from a branch given off from the buccal nerve. However, the medial part of the lower head has a branch arising directly from the anterior trunk of the mandibular nerve.
When left and right muscles contract together the condyle is pulled forward and slightly downward. This protrusive movement alone has little or no function except to assist opening the jaw. Digastric and geniohyoid are the main jaw opening muscles: unlike lateral pterygoid, when acting alone they rotate the jaw open, provided other muscles attached to the hyoid prevent if from being pulled forward. If only one lateral pterygoid contracts, the jaw rotates about a vertical axis passing roughly through the opposite condyle and is pulled medially toward the opposite side. This contraction together with that of the adjacent medial pterygoid (both attached to the lateral pterygoid plate) provides most of the strong medially directed component of the force used when grinding food between teeth of the same side. It is arguably the most important function of the inferior head of lateral pterygoid. It is often stated that the upper head is used to pull the articular disc forward when the jaw is opened. But electromyography studies have proved that the upper head is inactive during jaw opening and most active when the jaws are clenched. An explanation for this surprising activity is as follows (Osborn 1995a). Most of the power of a clenching force is due to contractions of masseter and temporalis. The associated backward pull of temporalis is greater than the associated forward pull of (superficial) masseter, and so their combined jaw closing action potentially pulls the condyle backward. This is prevented by the simultaneous contraction of the upper head of lateral pterygoid.
Medial pterygoid
Medial pterygoid (Fig. 31.12) is a thick, quadrilateral muscle with two heads of origin. The major component is the deep head which arises from the medial surface of the lateral pterygoid plate of the sphenoid bone and is therefore deep to the lower head of lateral pterygoid. The small, superficial head arises from the maxillary tuberosity and the pyramidal process of the palatine bone, and therefore lies on the lower head of lateral pterygoid. The fibres of medial pterygoid descend posterolaterally and are attached by a strong tendinous lamina to the posteroinferior part of the medial surface of the ramus and angle of the mandible, as high as the mandibular foramen and almost as far forwards as the mylohyoid groove. This area of attachment is often ridged. Inferior alveolar nerve block injection can occasionally cause haemorrhage into the muscle, which may give rise to painful trismus.
The lateral surface of medial pterygoid is related to the mandibular ramus, from which it is separated above its insertion by lateral pterygoid, the sphenomandibular ligament, the maxillary artery, the inferior alveolar vessels and nerve, the lingual nerve and a process of the parotid gland. The medial surface is related to tensor veli palatini and is separated from the superior pharyngeal constrictor by styloglossus and stylopharyngeus and by some areolar tissue.
Medial pterygoid derives its main arterial supply from the pterygoid branches of the maxillary artery.
The medial pterygoid muscles assist in elevating the mandible. Acting with the lateral pterygoids they protrude it. When the medial and lateral pterygoids of one side act together, the corresponding side of the mandible is rotated forwards and to the opposite side, with the opposite mandibular head as a vertical axis. Alternating activity in the left and right sets of muscles produces side-to-side movements, which are used to triturate food.
Pterygospinous ligament
The pterygospinous ligament, which is occasionally replaced by muscle fibres, stretches between the spine of the sphenoid bone and the posterior border of the lateral pterygoid plate near its upper end. It is sometimes ossified, and then completes a foramen which transmits the branches of the mandibular nerve to temporalis, masseter and lateral pterygoid.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Maxillary artery
The maxillary artery, the larger terminal branch of the external carotid artery, arises behind the neck of the mandible, and is at first embedded in the parotid gland (see Ch. 29). It then crosses the infratemporal fossa to enter the pterygopalatine fossa through the pterygomaxillary fissure. The artery is widely distributed to the mandible, maxilla, teeth, muscles of mastication, palate, nose and cranial dura mater (Figs 31.12, 31.13). It will be described in three parts, mandibular, pterygoid and pterygopalatine.
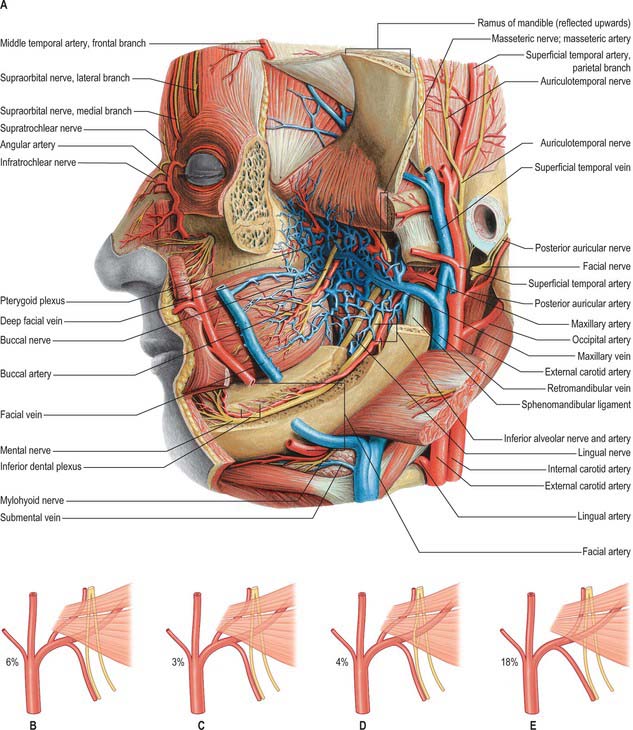
Fig. 31.13 A, Vessels and nerves of the head, exposed at a level deeper than that shown in Fig. 31.12 Note the pterygoid venous plexus. B–E, Variations in the course of the maxillary artery. In B, the maxillary artery passes medial to lateral pterygoid, and to the lingual and inferior alveolar nerves; in C, the artery passes between the lingual and inferior alveolar nerves; in D, the artery passes through a loop formed by the inferior alveolar nerve; in E, the middle meningeal artery branches off distal to the inferior alveolar artery.
(From Sobotta 2006.)
The mandibular part runs horizontally by the medial surface of the ramus. It passes between the neck of the mandible and the sphenomandibular ligament, parallel with and slightly below the auriculotemporal nerve. It next crosses the inferior alveolar nerve and skirts the lower border of lateral pterygoid. The pterygoid part ascends obliquely forwards medial to temporalis and in 60% of cases is superficial to the lower head of lateral pterygoid. When it runs deep to lateral pterygoid it lies between the muscle and branches of the mandibular nerve, and may project as a lateral loop between the two parts of lateral pterygoid. Asymmetry in this pattern of distribution may occur between the right and left infratemporal fossae and ethnic differences have been reported. Where the maxillary artery runs superficial to the lower head of lateral pterygoid, the commonest pattern is that the artery passes lateral to the inferior alveolar, lingual and buccal nerves. Less frequently, only the buccal nerve crosses the artery laterally, and rarely the artery passes deep to all the branches of the mandibular nerve. The pterygopalatine part passes between the two heads of lateral pterygoid to reach the pterygomaxillary fissure before it passes into the pterygopalatine fossa, where it terminates as the third part of the maxillary artery.
The mandibular part of the maxillary artery has five branches which all enter bone, namely, deep auricular, anterior tympanic, middle meningeal, accessory meningeal and inferior alveolar arteries. The pterygoid part of the maxillary artery has five branches that do not enter bone, but supply muscle, and include deep temporal, pterygoid, masseteric and buccal arteries. The branches of the pterygopalatine part of the artery accompany similarly named branches of the maxillary nerve (including those associated with the pterygopalatine ganglion) and are described in Chapter 32.
Deep auricular artery
The deep auricular artery pierces the osseous or cartilaginous wall of the external acoustic meatus and supplies the skin of the external acoustic meatus and part of the tympanic membrane. A small branch contributes to the arterial supply of the temporomandibular joint.
Anterior tympanic artery
The anterior tympanic artery passes through the petrotympanic fissure to supply part of the lining of the middle ear and accompanies the chorda tympani nerve.
Middle meningeal artery
The middle meningeal artery is the main source of blood to the bones of the vault of the skull (Fig. 31.14). It may arise either directly from the first part of the maxillary artery or from a common trunk with the inferior alveolar artery. When the maxillary artery lies superficial to lateral pterygoid, the middle meningeal artery is usually the first branch of the maxillary artery. However, when the maxillary artery takes a deep course in relation to the muscle this is not usually the case. The middle meningeal artery ascends between the sphenomandibular ligament and lateral pterygoid, passes between the two roots of the auriculotemporal nerve and leaves the infratemporal fossa through the foramen spinosum to enter the cranial cavity medial to the midpoint of the zygomatic bone. Its further course is described in Chapter 27.
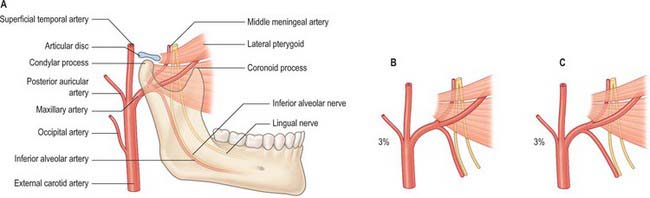
Fig. 31.14 Variations in the origin of the middle meningeal artery. In A, the middle meningeal artery branches off proximal to the inferior alveolar artery; in B, the artery branches off opposite the inferior alveolar artery; in C, the artery branches off distal to the inferior alveolar artery.
(From Sobotta 2006.)
Accessory meningeal artery
The accessory meningeal artery runs through the foramen ovale into the middle cranial fossa and may arise directly from the maxillary artery or as a branch of the middle meningeal artery itself. In its course in the infratemporal fossa, the accessory meningeal artery is closely related to tensor and levator veli palatini and usually runs deep to the mandibular nerve. Although it runs intracranially, its main distribution is extracranial, principally to medial pterygoid, lateral pterygoid (upper head), tensor veli palatini, the greater wing and pterygoid processes of the sphenoid, branches of the mandibular nerve and the otic ganglion. The accessory meningeal artery is sometimes replaced by separate small arteries.
Deep temporal arteries
The anterior, middle and posterior branches of the deep temporal arteries pass between temporalis and the pericranium, producing shallow grooves in the bone. They anastomose with the middle temporal branch of the superficial temporal artery. The anterior deep temporal artery connects with the lacrimal artery by small branches which perforate the zygomatic bone and greater wing of the sphenoid.
Masseteric artery
The masseteric artery, which is small, accompanies the masseteric nerve as it passes behind the tendon of temporalis through the mandibular incisure (notch) to enter the deep surface of masseter. Its branches can also supply the temporomandibular joint. The masseteric artery anastomoses with the masseteric branches of the facial artery and with the transverse facial branch of the superficial temporal artery.
Pterygoid arteries
The pterygoid arteries are irregular in number and origin, and are distributed to lateral and medial pterygoid.
Buccal artery
The buccal artery runs obliquely forwards between medial pterygoid and the attachment of temporalis and supplies the skin and mucosa over buccinator, accompanying the lower part of the buccal branch of the mandibular nerve. It anastomoses with branches of the facial and infraorbital arteries. A small lingual branch may be given off to accompany the lingual nerve and supply structures in the floor of the mouth.
Maxillary veins and the pterygoid venous plexus
Maxillary vein
The maxillary vein is a short trunk which accompanies the first part of the maxillary artery (Fig. 31.13A). It is formed from the confluence of veins from the pterygoid plexus and passes back between the sphenomandibular ligament and the neck of the mandible, to enter the parotid gland. It unites within the substance of the gland with the superficial temporal vein to form the retromandibular vein.
Pterygoid venous plexus
The pterygoid plexus of veins is found partly between temporalis and lateral pterygoid and partly between the two pterygoid muscles. Sphenopalatine, deep temporal, pterygoid, masseteric, buccal, alveolar (dental), greater palatine and middle meningeal veins and a branch or branches from the inferior ophthalmic vein are all tributaries. The plexus connects with the facial vein via the deep facial vein and with the cavernous sinus through veins that pass through the sphenoidal emissary foramen, foramen ovale and foramen lacerum. Its deep temporal tributaries often connect with tributaries of the anterior diploic veins and thus with the middle meningeal veins.
INNERVATION
The infratemporal fossa contains the major subdivisions of the mandibular branch of the trigeminal nerve, together with the chorda tympani, which enters the fossa and joins the lingual nerve, and the otic ganglion, which is functionally related to the parotid gland. The main sensory branches of the mandibular nerve extend beyond the infratemporal fossa and their distribution to the face is described in Chapter 29.
Mandibular nerve
The mandibular nerve is the largest trigeminal division and is a mixed nerve. Its sensory branches supply the teeth and gums of the mandible, the skin in the temporal region, part of the auricle – including the external meatus and tympanic membrane – and the lower lip, the lower part of the face and the mucosa of the anterior two-thirds (presulcal part) of the tongue and the floor of the oral cavity (Figs 31.12, 31.13A, 31.15). The motor branches innervate the muscles of mastication. The large sensory root emerges from the lateral part of the trigeminal ganglion and exits the cranial cavity through the foramen ovale. The small motor root passes under the ganglion and through the foramen ovale to unite with the sensory root just outside the skull. As it descends from the foramen ovale, the nerve is usually around 4 cm from the surface and a little anterior to the neck of the mandible. The mandibular nerve immediately passes between tensor veli palatini, which is medial, and lateral pterygoid, which is lateral, and gives off a meningeal branch and the nerve to medial pterygoid from its medial side. The nerve then divides into a small anterior and large posterior trunk. The anterior division gives off branches to the four main muscles of mastication and a buccal branch which is sensory to the cheek. The posterior division gives off three main sensory branches, the auriculotemporal, lingual and inferior alveolar nerves, and motor fibres to supply mylohyoid and the anterior belly of digastric.
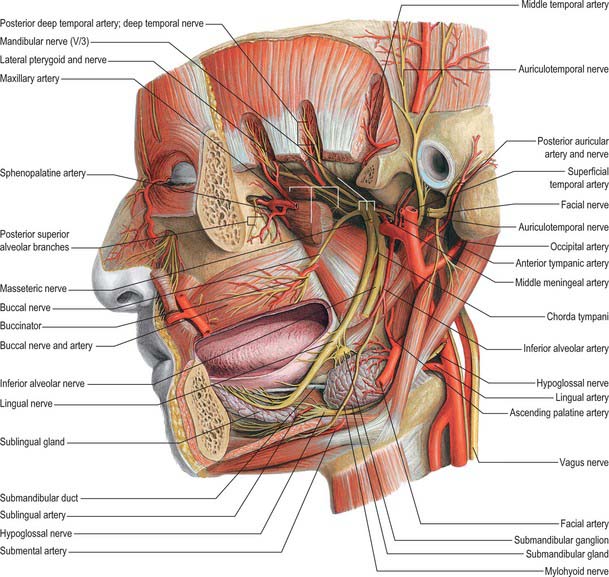
Fig. 31.15 Arteries and nerves of the head, deepest lateral regions. Compare with Figs 31.12 and 31.13A.
(From Sobotta 2006.)
Meningeal branch (nervus spinosus)
The meningeal branch re-enters the cranium through the foramen spinosum with the middle meningeal artery. It divides into anterior and posterior branches which accompany the main divisions of the middle meningeal artery and supply the dura mater in the middle cranial fossa and, to a lesser extent, in the anterior fossa and calvarium.
Nerve to medial pterygoid
The nerve to medial pterygoid is a slender ramus which enters the deep aspect of the muscle. It supplies one or two filaments that pass through the otic ganglion without interruption to supply tensor tympani and tensor veli palatini.
Anterior trunk of mandibular nerve
The anterior trunk of the mandibular nerve gives rise to the buccal nerve, which is sensory, and the masseteric, deep temporal and lateral pterygoid nerves, which are all motor.
Buccal nerve
The buccal nerve passes between the two heads of lateral pterygoid. It descends deep to the tendon of temporalis, passes laterally in front of masseter, and anastomoses with the buccal branches of the facial nerve. It carries the motor fibres to lateral pterygoid, and these are given off as the buccal nerve passes through the muscle. It may also give off the anterior deep temporal nerve. The buccal nerve supplies sensation to the skin over the anterior part of buccinator and the buccal mucous membrane, together with the posterior part of the buccal gingivae adjacent to the second and third molar teeth.
Nerve to masseter
The nerve to masseter passes laterally above lateral pterygoid, on to the skull base, anterior to the temporomandibular joint and posterior to the tendon of temporalis. It crosses the posterior part of the mandibular notch with the masseteric artery and ramifies on and enters the deep surface of masseter. It also provides articular branches which supply the temporomandibular joint.
Deep temporal nerves
The deep temporal nerves usually consist of two branches, anterior and posterior, although there may be a middle branch. They pass above lateral pterygoid to enter the deep surface of temporalis. The anterior nerve frequently arises as a branch of the buccal nerve. The small posterior nerve sometimes arises in common with the nerve to masseter.
Nerve to lateral pterygoid
The nerve to lateral pterygoid enters the deep surface of the muscle. It may arise separately from the anterior division of the mandibular nerve or from the buccal nerve.
Posterior trunk of mandibular nerve
The posterior trunk of the mandibular nerve is larger than the anterior and is mainly sensory, although it receives fibres from the motor root for the nerve to mylohyoid. It divides into auriculotemporal, lingual and inferior alveolar (dental) nerves.
Auriculotemporal nerve
The auriculotemporal nerve usually has two roots which encircle the middle meningeal artery. It runs back under lateral pterygoid on the surface of tensor veli palatini, passes between the sphenomandibular ligament and the neck of the mandible, and then runs laterally behind the temporomandibular joint related to the upper part of the parotid gland. Emerging from behind the joint, it ascends over the posterior root of the zygoma, posterior to the superficial temporal vessels, and divides into superficial temporal branches. It communicates with the facial nerve and otic ganglion. The rami to the facial nerve, usually two, pass anterolaterally behind the neck of the mandible to join the facial nerve at the posterior border of masseter. Filaments from the otic ganglion join the roots of the auriculotemporal nerve close to their origin. The sensory distribution of the auriculotemporal nerve on the face is described in Chapter 29.
Lingual nerve
The lingual nerve is sensory to the mucosa of the anterior two-thirds of the tongue, the floor of the mouth and the mandibular lingual gingivae. It arises from the posterior trunk of the mandibular nerve and at first runs beneath lateral pterygoid and superficial to tensor veli palatini, where it is joined by the chorda tympani branch of the facial nerve, and often by a branch of the inferior alveolar nerve. Emerging from under cover of lateral pterygoid, the lingual nerve then runs downwards and forwards on the surface of medial pterygoid, and is thus carried progressively closer to the medial surface of the mandibular ramus. It becomes intimately related to the bone a few millimetres below and behind the junction of the vertical ramus and horizontal body of the mandible. Here it lies anterior to, and slightly deeper than, the inferior alveolar (dental) nerve. It next passes below the mandibular attachment of the superior pharyngeal constrictor and pterygomandibular raphe, closely applied to the periosteum of the medial surface of the mandible, until it lies opposite the posterior root of the third molar tooth, where it is covered only by the gingival mucoperiosteum. At this point it usually lies 2–3 mm below the alveolar crest and 0.6 mm from the bone, however in 5% of cases it lies above the alveolar crest. It next passes medial to the mandibular origin of mylohyoid, and this carries it progressively away from the mandible, and separates it from the alveolar bone covering the mesial root of the third molar tooth. The rest of the nerve is described with the mouth and oral cavity in Chapter 30.
Inferior alveolar (dental) nerve
The inferior alveolar nerve descends behind lateral pterygoid. At the lower border of the muscle the nerve passes between the sphenomandibular ligament and the mandibular ramus and enters the mandibular canal via the mandibular foramen. Below lateral pterygoid it is accompanied by the inferior alveolar artery, a branch of the first part of the maxillary artery, which also enters the canal with associated veins. The subsequent course of the inferior alveolar nerve is described in Chapter 30.
Otic ganglion
This is a small, oval, flat reddish-grey ganglion situated just below the foramen ovale. It is a peripheral parasympathetic ganglion related topographically to the mandibular nerve, but connected functionally with the glossopharyngeal nerve. Near its junction with the trigeminal motor root, the mandibular nerve lies lateral to the ganglion; tensor veli palatini lies medially, separating the ganglion from the cartilaginous part of the pharyngotympanic tube, and the middle meningeal artery is posterior to the ganglion. The otic ganglion usually surrounds the origin of the nerve to medial pterygoid.
Like all parasympathetic ganglia, there are three roots, motor, sympathetic and sensory. Only the parasympathetic fibres relay in the ganglion. The motor, parasympathetic, root of the otic ganglion is the lesser petrosal nerve, conveying preganglionic fibres from the glossopharyngeal nerve which originate from neurones in the inferior salivatory nucleus. The lesser petrosal nerve runs intracranially in the middle cranial fossa on the anterior surface of the petrous bone before passing through the foramen ovale to join the otic ganglion. The nerve synapses in the otic ganglion, and postganglionic fibres pass by a communicating branch to the auriculotemporal nerve and so to the parotid gland. The sympathetic root is from a plexus on the middle meningeal artery. It contains postganglionic fibres from the superior cervical sympathetic ganglion which traverse the otic ganglion without relay and emerge with parasympathetic fibres in the connection with the auriculotemporal nerve to supply blood vessels in the parotid gland. The sensory fibres from the gland are derived from the auriculotemporal nerve. Clinical observations suggest that in humans the gland also receives secretomotor fibres through the chorda tympani.
Branches
A branch connects the otic ganglion to the chorda tympani nerve, while another ramus ascends to join the nerve of the pterygoid canal. These branches may form an additional pathway by which gustatory fibres from the anterior two-thirds of the tongue may reach the facial ganglion without traversing the middle ear, and they do not synapse in the otic ganglion. Motor branches to tensor veli palatini and tensor tympani, derived from the nerve to medial pterygoid, also pass through the ganglion without synapsing.
Chorda tympani
The chorda tympani nerve enters the infratemporal fossa region by passing through the medial end of the petrotympanic fissure behind the capsule of the temporomandibular joint. The nerve descends medial to the spine of the sphenoid bone – which it sometimes grooves – lying posterolateral to tensor veli palatini. It is crossed medially by the middle meningeal artery, the roots of the auriculotemporal nerve and by the inferior alveolar nerve (Fig. 31.15). The chorda tympani joins the posterior aspect of the lingual nerve at an acute angle. It carries taste fibres for the anterior two-thirds of the tongue and efferent preganglionic parasympathetic (secretomotor) fibres destined for the submandibular ganglion in the floor of the mouth.
SPREAD OF INFECTION FROM THE INFRATEMPORAL FOSSA
Infections from most teeth in the upper jaw or the front of the lower jaw usually drain harmlessly into the oral cavity, either via the vestibule buccally, or via the palate or mouth lingually. In contrast, a pericoronitis that affects a mandibular third molar tooth which communicates with the oral cavity, or, less commonly, either a dental abscess associated with this tooth, or a postoperative infection, may spread along tissue planes. Spread may be buccal, submasseteric, parapharyngeal, submandibular, or, more rarely, infratemporal. The main symptom caused by infection of the pterygomandibular region is trismus (painful reflex muscle spasm) which usually affects medial pterygoid. When the submandibular, sublingual and submental areas are primarily affected (Ludwig’s angina), there is a risk that the airway may become obstructed. Infection may (potentially) spread further, either along the tissue spaces of the neck below or the tissue planes of the face above, when it may even reach the orbit via the inferior orbital fissure. Once in the orbit, further spread directly through the superior orbital fissure into the cranial cavity, resulting in a life threatening cavernous sinus thrombosis, remains a remote possibility. Infection may also spread to the cavernous sinus from the pterygoid plexus and ophthalmic veins.
PTERYGOPALATINE FOSSA
The pterygopalatine fossa is a small pyramidal space below the apex of the orbit on the lateral side of the skull. The posterior boundary is the root of the pterygoid process and adjoining anterior surface of the greater wing of the sphenoid, and the anterior boundary is the superomedial part of the infratemporal surface of the maxilla. The perpendicular plate of the palatine bone, with its orbital and sphenoidal processes forms the medial boundary, and the pterygomaxillary fissure is the lateral boundary. The fossa communicates with the nasal cavity via the sphenopalatine foramen, with the orbit via the medial end of the inferior orbital fissure, and with the infratemporal fossa via the pterygomaxillary fissure, which lies between the back of the maxilla and the pterygoid process of the sphenoid and transmits the maxillary artery. It also communicates with the oral cavity via the greater palatine canal, which opens in the posterolateral aspect of the hard palate. There are two openings in the posterior wall of the pterygopalatine fossa, the foramen rotundum, which transmits the maxillary nerve, and the pterygoid canal, which transmits the nerve of the pterygoid canal (Vidian nerve). When the anterior aspect of the pterygoid plate is examined in a disarticulated sphenoid, the foramen rotundum is seen to lie above and lateral to the pterygoid canal (see Fig. 31.2).
The main contents of the pterygopalatine fossa are the third part of the maxillary artery, the maxillary nerve and many of its branches, and the pterygopalatine ganglion.
Maxillary artery
The maxillary artery passes through the pterygomaxillary fissure from the infratemporal fossa into the pterygopalatine fossa, where it terminates as the third part of the maxillary artery. It gives off numerous branches including the posterior superior alveolar, infraorbital, sphenopalatine and greater palatine arteries.
Posterior superior alveolar artery
The posterior superior alveolar artery arises from the maxillary artery within the pterygopalatine fossa and runs through the pterygomaxillary fissure onto the maxillary tuberosity. It gives off branches which penetrate the bone here to supply the maxillary molar and premolar teeth and the maxillary air sinus, and other branches that supply the buccal mucosa. Occasionally the posterior superior alveolar artery arises from the infraorbital artery.
Infraorbital artery
The infraorbital artery enters the orbit through the inferior orbital fissure. It runs on the floor of the orbit in the infraorbital groove and infraorbital canal and emerges onto the face at the infraorbital foramen to supply the lower eyelid, part of the cheek, the side of the external nose, and the upper lip. While within the infraorbital canal it gives off the anterior superior alveolar artery which runs downwards to supply the anterior teeth and the anterior part of the maxillary sinus. A middle superior alveolar artery is also often described. When present, it branches from the infraorbital artery within the infraorbital canal and runs inferiorly along the lateral wall of the maxillary sinus toward the region of the canine and lateral incisor teeth and anastomoses with the anterior and posterior superior alveolar arteries.
Artery of the pterygoid canal
The artery of the pterygoid canal (Vidian artery) arises as a branch of either the distal part of the maxillary artery (70%) or the petrous segment of the internal carotid artery (30%). It passes through the pterygoid canal and anastomoses with the pharyngeal, ethmoidal and sphenopalatine arteries in the pterygopalatine fossa and with the ascending pharyngeal, accessory meningeal, ascending palatine and descending palatine (occasionally) arteries in the oropharynx and around the pharyngotympanic tube. Through these complex anastomoses, the artery of the pterygoid canal contributes to the supply of part of the pharyngotympanic tube, the tympanic cavity, and the upper part of the pharynx. It may also anastomose with the artery of the foramen rotundum, and so communicate with branches of the cavernous portion of the internal carotid artery.
Pharyngeal artery
The pharyngeal branch of the maxillary artery passes through the palatovaginal canal, accompanying the nerve of the same name, and is distributed to the mucosa of the nasal roof, nasopharynx, sphenoidal air sinus and pharyngotympanic tube.
Greater (descending) palatine artery
The greater palatine artery leaves the pterygopalatine fossa through the greater (anterior) palatine canal, within which it gives off two or three lesser palatine arteries. The greater palatine artery supplies the inferior meatus of the nose, then passes onto the roof of the hard palate at the greater (anterior) palatine foramen and runs forwards to supply the hard palate and the palatal gingivae of the maxillary teeth. It gives off a branch that runs up into the incisive canal to anastomose with the sphenopalatine artery, and so contribute to the arterial supply of the nasal septum. The lesser palatine arteries emerge onto the palate through the lesser (posterior) palatine foramen, or foramina, and supply the soft palate.
Sphenopalatine artery
The sphenopalatine branch of the maxillary artery passes through the sphenopalatine foramen and enters the nasal cavity posterior to the superior meatus. From here its posterior lateral nasal branches ramify over the conchae and meatuses, anastomosing with the ethmoidal arteries and nasal branches of the greater palatine artery to supply the frontal, maxillary, ethmoidal and sphenoidal air sinuses. The sphenopalatine artery next crosses anteriorly on the inferior surface of the sphenoid and ends on the nasal septum in a series of posterior septal branches which anastomose with the ethmoidal arteries. A branch descends on the vomer to the incisive canal to anastomose with the greater palatine artery and the septal branch of the superior labial artery.
Maxillary nerve
The maxillary division of the trigeminal nerve is wholly sensory (Fig. 31.16). It leaves the skull via the foramen rotundum, which leads directly into the posterior wall of the pterygopalatine fossa. Crossing the upper part of the pterygopalatine fossa, the nerve gives off two large ganglionic branches which contain fibres destined for the nose, palate and pharynx, and these pass through the pterygopalatine ganglion without synapsing. It then inclines sharply laterally on the posterior surface of the orbital process of the palatine bone and on the upper part of the posterior surface of the maxilla in the inferior orbital fissure (which is continuous posteriorly with the pterygopalatine fossa): it lies outside the orbital periosteum, and gives off its zygomatic, and then posterior superior alveolar branches. About halfway between the orbital apex and the orbital rim the maxillary nerve turns medially to enter the infraorbital canal as the infraorbital nerve. The subsequent course of the maxillary nerve is described in Chapter 29.
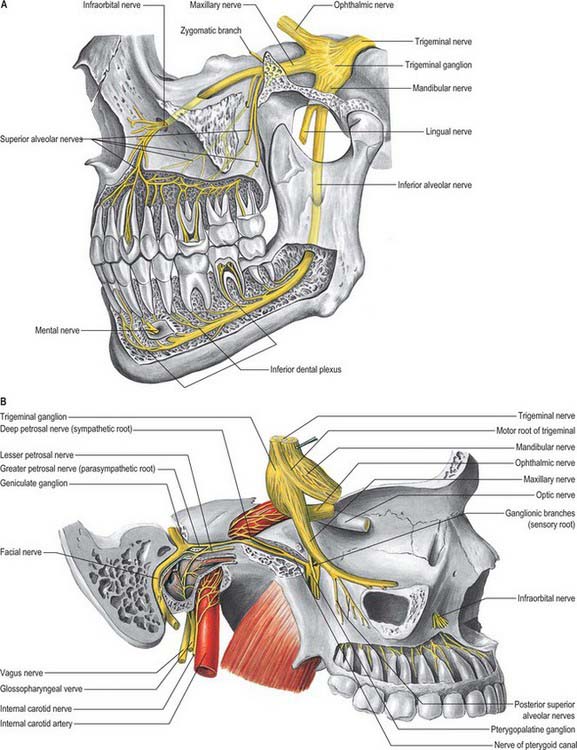
Fig. 31.16 A, Maxillary and mandibular nerves; B, Pterygopalatine ganglion, showing its connections with the nerve of the pterygoid canal and the maxillary division of the trigeminal. The trigeminal ganglion has been lifted forwards out of the trigeminal impression. Note the sympathetic plexus on the internal carotid artery.
(From Sobotta 2006.)
The maxillary nerve gives off many of its branches in the pterygopalatine fossa. They can be subdivided into those that come directly from the nerve, and those that are associated with the pterygopalatine parasympathetic ganglion. Named branches from the main trunk are meningeal, ganglionic, zygomatic, posterior, middle and anterior superior alveolar and infraorbital nerves. Named branches from the pterygopalatine ganglion are orbital, nasopalatine, posterior superior nasal, greater (anterior) palatine, lesser (posterior) palatine and pharyngeal.
Meningeal nerve
The meningeal branch of the maxillary nerve arises within the middle cranial fossa and runs with the middle meningeal vessels. It contributes to the innervation of the dura mater.
Ganglionic branches
There are usually two ganglionic branches that connect the maxillary nerve to the pterygopalatine ganglion.
Zygomatic nerve
The zygomatic branch of the maxillary nerve leaves the pterygopalatine fossa through the inferior orbital fissure together with the maxillary nerve. Its subsequent course is described in Chapter 29.
Posterior superior alveolar nerve
The posterior superior alveolar nerve leaves the maxillary nerve in the pterygopalatine fossa. Its subsequent course and distribution is described in detail in Chapter 30.
Infraorbital nerve
The infraorbital nerve can be regarded as the terminal branch of the maxillary nerve. It leaves the pterygopalatine fossa to enter the orbit at the inferior orbital fissure, and its subsequent course and distribution are described in Chapter 29.
Pterygopalatine ganglion
The pterygopalatine ganglion is the largest of the peripheral parasympathetic ganglia. It is placed deeply in the pterygopalatine fossa, near the sphenopalatine foramen, and anterior to the pterygoid canal and foramen rotundum (Fig. 31.16B). It is flattened, reddish-grey in colour, and lies just below the maxillary nerve as it crosses the pterygopalatine fossa. The majority of the ‘branches’ of the ganglion are connected with it morphologically, but not functionally, because they are primarily sensory branches of the maxillary nerve. Thus they pass through the ganglion without synapsing, and enter the maxillary nerve through its ganglionic branches, but they convey some parasympathetic fibres to the palatine, pharyngeal and nasal mucous glands.
Preganglionic parasympathetic fibres destined for the pterygopalatine ganglion run initially in the greater petrosal branch of the facial nerve, and then in the nerve of the pterygoid canal (Vidian nerve), after the greater petrosal unites with the deep petrosal nerve. The nerve of the pterygoid canal enters the ganglion posteriorly. Postganglionic parasympathetic fibres leave the ganglion and join the maxillary nerve via a ganglionic branch, then travel via the zygomatic and zygomaticotemporal branches of the maxillary nerve to the lacrimal gland. Preganglionic secretomotor fibres of uncertain origin also travel in the nerve of the pterygoid canal. They synapse in the pterygopalatine ganglion, and postganglionic fibres are distributed to palatine, pharyngeal and nasal mucous glands via palatine and nasal branches of the maxillary nerve.
Postganglionic sympathetic fibres pass through the ganglion without synapsing and supply blood vessels and orbitalis. They arise in the superior cervical ganglion and travel via the internal carotid plexus and deep petrosal nerve to enter the pterygopalatine ganglion within the nerve of the pterygoid canal.
General sensory fibres destined for distribution via orbital, nasopalatine, superior alveolar, palatine and pharyngeal branches of the maxillary division of the trigeminal nerve run through the ganglion without synapsing.
Orbital branches
Fine orbital branches enter the orbit through the inferior orbital fissure and supply orbital periosteum. Some fibres also pass through the posterior ethmoidal foramen to supply the sphenoidal and ethmoidal sinuses. The orbital branches probably join branches of the internal carotid nerve to form a ‘retro-orbital’ plexus from which orbital structures such as the lacrimal gland and orbitalis receive an autonomic innervation.
Nasopalatine nerve
The nasopalatine nerve leaves the pterygopalatine fossa through the sphenopalatine foramen and enters the nasal cavity. It passes across the cavity to the back of the nasal septum, runs downwards and forwards on the septum in a groove in the vomer, and then turns down through the incisive fossa in the anterior part of the hard palate to enter the roof of the mouth. When an anterior and a posterior incisive foramen exist in this fossa, the left nasopalatine nerve passes through the anterior foramen, and the right nerve passes through the posterior foramen. The nasopalatine nerve supplies the lower part of the nasal septum and the anterior part of the hard palate, where it communicates with the greater palatine nerve.
Posterior superior nasal nerves (lateral and medial)
The posterior superior alveolar nerves enter the back of the nasal cavity through the sphenopalatine foramen. Lateral posterior superior nasal nerves (about 6) innervate the mucosa lining the posterior part of the superior and middle nasal conchae and the posterior ethmoidal sinuses. Two or three medial posterior superior nasal nerves cross the nasal roof below the opening of the sphenoidal sinus to supply the mucosa of the posterior part of the roof and of the nasal septum.
Palatine nerves (greater and lesser)
The greater and lesser palatine nerves pass downwards from the pterygopalatine ganglion through the greater palatine canal. The greater palatine nerve descends through the greater palatine canal, emerges on the hard palate from the greater palatine foramen and runs forwards in a groove on the inferior surface of the bony palate almost to the incisor teeth. It supplies the gingivae, mucosa and glands of the hard palate and also communicates with the terminal filaments of the nasopalatine nerve. In the greater palatine canal it gives off posterior inferior nasal branches that emerge through the perpendicular plate of the palatine bone and ramify over the inferior nasal concha and walls of the middle and inferior meatuses. As it leaves the greater palatine canal, it gives off branches which are distributed to both surfaces of the adjacent part of the soft palate.
The lesser (middle and posterior) palatine nerves are much smaller than the greater palatine nerve. They descend through the greater palatine canal, from which they diverge low down to emerge through the lesser palatine foramina in the tubercle or pyramidal process of the palatine bone. They innervate the uvula, tonsil and soft palate.
Fibres conveying taste impulses from the palate probably pass via the palatine nerves to the pterygopalatine ganglion. They pass through the ganglion without synapsing, and leave via the greater petrosal nerve. Their cell bodies are located in the facial ganglion and their central processes pass via the sensory root of the facial nerve (nervus intermedius) to the gustatory nucleus in the nucleus of the tractus solitarius.
Barker BCW, Davies PL. The applied anatomy of the pterygomandibular space. Br J Surg. 1972;10:43-55.
Describes the relationships of the structures within the pterygomandibular space, with particular reference to anaesthesia associated with an inferior alveolar nerve block..
Bertilsson O, Strom D. A literature survey of a hundred years of anatomic and functional lateral pterygoid muscle research. J Orofac Pain. 1995;9:17-23.
De Bont LGM, Boering G, Havinga P, Liem RSB. Spacial arrangement of collagen fibrils in the articular cartilage of the mandibular condyle. J Oral Maxillofac Surg. 1984;42:306-313.
Hansson T, Oberg T, Carlsson GE, Kopp S. Thickness of the soft tissue layers and the articular disc in the temporomandibular joint. Acta Odont Scand. 1977;35:77-83.
Hollingshead WH. The Head and Neck. 2nd edn. Anatomy for Surgeons. vol. 1. New York: Harper & Row; 1968.
Lang J. Clinical Anatomy of the Masticatory Apparatus and Peripharyngeal Spaces. New York: Thième Medical Publishers, 1995.
Provides detailed anatomical information (including quantitation) of the infratemporal fossa, relating such information to the clinic..
Langdon JD, Patel MF. Operative Maxillofacial Surgery. London: Chapman and Hall, 1998.
Langdon JD, Berkovitz BKB, Moxham BJ. The Surgical Anatomy of the Infratemporal Fossa. London: Dunitz, 2002.
Orchardson R, Cadden W. Mastication. Linden RWA, editor. The Scientific Basis of Eating. Taste and Smell, Salivation. Mastication and Swallowing and their Dysfunctions. Frontiers of Oral Biology Series Vol 9. Basel: Karger; 1998:76-121
Osborn JW. Internal derangement and the accessory ligaments around the temporomandibular joint. J Oral Rehab. 1995;22:731-740.
Analyses of the anatomy of the ligaments associated with the jaw joint and how they control the movements of the condyle during border movements of the jaw associated with jaw opening and the aetiology of jaw dislocation and disc displacement..
Pogrel MA, Renaut A, Schmidt B, Ammar A. The relationship of the lingual nerve to the mandibular third molar region. J Oral Maxillofac Surg. 1995;53:1178-1181.
Robinson PD. Articular cartilage of the temporomandibular joint – can it regenerate? Ann R Coll Surg Engl. 1993;75:231-236.
Toller PA. Temporomandibular arthropathy. Proc Roy Soc Med. 1974;67:153-159.
Turker KS. Reflex control of human jaw muscles. Crit Rev Oral Biol Med. 2002;13:85-104.