CHAPTER 29 Face and scalp
SKIN
The scalp and buccolabial tissues are described here. The structure of the eyelids is described in Chapter 39.
SCALP
The scalp extends from the top of the forehead in front to the superior nuchal line behind. Laterally it projects down to the zygomatic arch and external acoustic meatus. It consists of five layers: skin, subcutaneous tissue, occipitofrontalis (epicranius) and its aponeurosis, subaponeurotic loose areolar tissue and periosteum of the skull (pericranium).
The skin of the scalp is hairy and rich in sebaceous glands: it is the commonest site for sebaceous cysts. The dense subcutaneous connective tissue has the richest cutaneous blood supply in the body. The anterior and posterior muscular bellies of occipitofrontalis are connected by a tough, fibrous, epicranial aponeurosis, and this layer is therefore often called the aponeurotic layer (galea aponeurotica). These three upper layers of the scalp can easily slide on the underling layer of loose connective tissue. A scalp flap can be raised within the plane between the galea and the pericranium without compromising either the blood or nerve supply of the scalp, because all of these structures lie in the subcutaneous layer (superficial fascia). Anteriorly based subgaleal scalp flaps (bicoronal) provide excellent access to the craniofacial skeleton for the correction of congenital deformity such as craniosynostoses; treatment of craniofacial fractures involving the frontal bone, nasoethmoid complex, orbit or zygomatic arch; skull base surgery or craniotomies. Pericranial flaps can be used to separate the frontal sinus floor from the nasal cavity in the management of fractures of the posterior wall of the frontal sinus (frontal sinus cranialization). Traumatic scalp avulsion may occur if hair becomes trapped in moving machinery or a shearing force is applied in the subgaleal plane during a road traffic accident or fall injury.
The arterial blood supply to the scalp is particularly rich, and there are free anastomoses between branches of the occipital and superficial temporal vessels. Scalp lacerations continue to bleed profusely because the elastic fibres of the underlying galea aponeurotica prevent initial vessel retraction. Their repair requires a two-layer closure technique to approximate the galea aponeurotica and skin layers. The pericranial layer, if involved, cannot usually be closed because it retracts.
EYEBROWS
The eyebrows are two arched eminences of skin which surmount the orbits. Numerous short, thick hairs are set obliquely in them. Fibres of orbicularis oculi, corrugator and the frontal part of occipitofrontalis, are inserted into the dermis of the eyebrows.
BUCCOLABIAL TISSUE
Cheeks
The cheeks are continuous in front with the lips. The external junction is indicated by the nasolabial groove (sulcus) and further laterally by the nasolabial fold, which descends from the side of the nose to the angle of the mouth. The cheek is covered on the outer surface by skin and on the inner surface by mucosa. Each cheek contains the buccinator muscle, and a variable, but usually considerable, amount of adipose tissue which is often encapsulated to form a biconcave mass, the buccal fat pad (of Bichat), particularly evident in infants. The walls of the cheek also contain fibrous connective tissue, vessels, nerves and numerous small buccal mucous (salivary) glands. The buccal fat pad can be used to reconstruct small intraoral defects of the palate, buccal and retromolar regions following surgery.
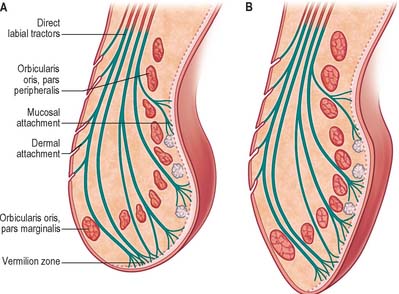
Lips
The lips are two fleshy folds surrounding the oral orifice. The centre of each lip contains a thick fibrous strand, consisting of parallel bundles of skeletal muscle fibres (orbicularis oris, together with incisivus superior and inferior, and the direct labial tractors), and their attachments to skin, mucosa or other muscle fibres. The free external surface of each lip is covered by a thin keratinized epidermis, and is continuous with the mucosa at the vermilion (red) zone of the lip. The dermis is well vascularized and contains numerous hair follicles (many of them large in the male), sebaceous glands (Fordyce spots) and sweat glands. Subcutaneous adipose tissue is scanty. The internal mucous surfaces are lined with a thick non-keratinizing stratified squamous epithelium. The submucosa is well vascularized and contains numerous minor salivary glands, which may be harvested for histological confirmation of Sjögren’s connective tissue disease.
Between the skin and mucosa, the vermilion zone is covered with a specialized keratinized stratified squamous epithelium which is thin near the skin, increases in thickness slightly as the mucosa is approached, and then thickens abruptly when true mucosa is reached. The epithelium is covered with transparent, dead squames and its deep surface is highly convoluted, interdigitating with abundant long dermal papillae. The latter carry a rich capillary plexus which imparts a dusky red colour. These surfaces are hairless, their dermis lacks sebaceous, sweat or mucous glands, and they are moistened with saliva by the tip of the tongue. The dense innervation of the lips is reflected in their acute sensitivity to light touch sensation, attributable mainly to the increased density of Meissner’s corpuscles in the dermal papillae.
The size and curvature of the exposed red lip surfaces is subject to considerable individual, gender, and ethnic variation. The line of contact between the lips, the oral fissure, lies just above the incisal edges of the anterior maxillary teeth. On each side a labial commissure forms the angle (corner) of the mouth, usually near the first premolar tooth. The labial epithelia and internal tissues radiate over the boundaries of the commissure to become continuous with those of the cheek. With age, buccolabial (labiomarginal) grooves appear at the corners of the mouth. On each side, the upper lip is separated from the cheek laterally by the nasolabial groove and is continuous above the nasal ala with the circumalar groove (sulcus). The lower lip is separated from the chin by the mentolabial groove (sulcus).
Externally, the central region of the upper lip presents a shallow vertical groove, the philtrum, which is limited above by its attachment to the columella of the nose, and ends below in a slight tubercle limited by lateral ridges. The lower lip shows a small depression in the midline that corresponds to the tubercle. The junction between the external, hair-bearing skin and the red, hairless surface of the upper lip almost invariably takes the form of a double-curved Cupid’s bow. From the centre it rises rapidly on each side to an apex that corresponds to the lower end of each ridge of the philtrum, and then slopes gently downwards towards the angle of the mouth. The line of contact between the red lip surfaces is typically almost horizontal. The Cupid’s bow is interrupted in cleft lip anomalies.
In the upper lip, a narrow band of smooth tissue related to the subnasal maxillae marks the point at which labial mucosa becomes continuous with gingival mucosa. The corresponding reflexion in the lower lip coincides approximately with the mentolabial sulcus, and here the lip is continuous with mental tissues. The upper and lower lips differ in cross-sectional profile in that neither is a simple fold of uniform thickness. The upper lip has a bulbous asymmetrical profile: the skin and red-lip have a slight external convexity, and the adjoining red-lip and mucosa a pronounced internal convexity, creating a mucosal ridge or shelf that can be wrapped around the incisal edges of the parted teeth. The lower lip is on a more posterior plane than the upper lip. In the position of neutral lip contact, the external surface of the lower lip is concave, and there is little or no elevation of the internal mucosal surface. The profile of the lips can be modified by muscular activity.
RELAXED SKIN TENSION LINES AND SKIN FLAPS ON THE FACE
The direction in which facial skin tension is greatest varies regionally. Skin tension lines which follow the furrows formed when the skin is relaxed are known as ‘relaxed skin tension lines’ (Borges & Alexander 1962). In the living face, these lines frequently (but not always) coincide with wrinkle lines (Fig. 29.1) and can therefore act as a guide in planning elective incisions.

Fig. 29.1 A, Distribution of relaxed skin tension lines (Kraissl’s lines) lateral view. B, Anterior view.
When lesions on the face such as scars, pigmented lesions and skin cancers are excised, the dimensions of these lesions often require excision as an ellipse, so that the resulting defect can be closed as a straight line. If the resulting scar is to be aesthetically acceptable it is important to make the long axis of the ellipse parallel to the natural relaxed skin tension lines, so that the scar will look like a natural skin crease. If the excision line runs contrary to the skin tension lines, the scar may be more conspicuous and will tend to stretch transversely as a result of natural expressive facial movements.
When larger lesions are excised it may be necessary to advance or rotate adjacent soft tissue to fill the defect. The ability to raise these skin flaps is entirely dependent on the regional blood supply and both random pattern and axial pattern skin flaps are used surgically. Because of the richness of the subdermal plexus in the face, random pattern flaps can be raised with a greater length : breadth ratio than in any other area of the body.
The following are examples of axial pattern flaps that can be used to reconstruct defects on the face and scalp. Supratrochlear/supraorbital arteries support forehead flaps that are useful for nasal reconstruction: there is usually enough skin laxity to allow the majority of the donor site to be closed directly. The frontal branch of the superficial temporal artery anastomoses in the midline with its opposite number, and consequently the entire forehead skin can be raised on a narrow pedicle based on just one of the superficial temporal arteries. These flaps can be used to repair many facial defects and also intraoral defects, but the donor site defect cannot be closed directly and must be covered by a skin graft. The parietal branch of the superficial temporal artery and the occipital artery can support hair-bearing flaps from the scalp which are useful for reconstructing defects involving the scalp. The nasolabial flap utilizes the lax skin just lateral to the nasolabial groove. It is not supplied by a named axial artery but rather its blood supply is provided by many small branches from the underlying facial artery. These branches run perpendicular to the skin surface. Nasolabial flaps can be either superiorly or inferiorly based.
SOFT TISSUE
FASCIAL LAYERS
Fascia of scalp
The superficial fascia of the scalp is firm, dense and fibroadipose, and adheres closely to both skin and the underlying epicranius and its aponeurosis. Posteriorly it is continuous with the superficial fascia of the back of the neck, and laterally it is prolonged into the temporal region, where it is looser in texture.
Fascial layers and tissue planes in the face
On the basis of gross dissection and complementary histological studies, four distinct tissue planes are recognized on the face superficial to the plane of the facial nerve and its branches. From superficial to deep, these layers are the skin; a subcutaneous layer of fibro-adipose tissue; the superficial musculo-aponeurotic system (SMAS); and the parotid–masseteric fascia.
Subcutaneous fibroadipose tissue
This homogeneous layer is present throughout the face, although the degree of adiposity varies in different parts of the face and with age. Anteriorly, it crosses the nasolabial fold onto the lip, and superiorly it crosses the zygomatic arch. In both locations the layer is more fascial than fatty. The fat content of the subcutaneous tissue in the cheek accounts for the cheek mass: part of the subcutaneous adipose tissue is the malar fat pad, a more or less discrete aggregation of fatty tissue inferolateral to the orbital margin.
Superficial musculo-aponeurotic system (SMAS)
This is described as a single tissue plane in the face. In some areas it is composed of muscle fibres, and elsewhere it is composed of fibrous or fibroaponeurotic tissue: it is not directly attached to bone. When traced below the level of the lower border of the mandible it becomes continuous with platysma in the neck. Microdissection has revealed that the SMAS becomes indistinct on the lateral aspect of the face approximately 1 cm below the level of the zygomatic arch. Anteromedially, the SMAS layer becomes continuous with some of the mimetic muscles including zygomaticus major, frontalis and the peri-orbital fibres of orbicularis oculi.
In most areas of the face, a distinct sub-SMAS plane can be defined deep to SMAS. It is continuous with the plane between platysma and the underlying investing layer of deep cervical fascia in the neck. However, where it overlies the parotid gland, the SMAS is firmly blended with the superficial layer of the parotid fascia, which means that a clear sub-SMAS plane is difficult, if not impossible, to define in the region of the parotid.
Parotid–masseteric fascia
This is a filmy areolar layer that overlies the filamentous branches of the facial nerve and the parotid duct as these structures lie on the surface of masseter. Further anteriorly the parotid–masseteric fascia overlies the buccal fat pad which lies superficial to buccinator. Having crossed the surface of the buccal fat pad, the fascia blends with the epimysium on the surface of buccinator. Below the lower border of the mandible, it is continuous with the investing layer of deep cervical fascia.
Parotid fascia (capsule)
The parotid gland is surrounded by a fibrous capsule called the parotid fascia or capsule. Traditionally this has been described as an upward continuation of the investing layer of deep cervical fascia in the neck which splits to enclose the gland within a superficial and a deep layer. The superficial layer is attached above to the zygomatic process of the temporal bone, the cartilaginous part of the external acoustic meatus, and the mastoid process. The deep layer is attached to the mandible, and to the tympanic plate, styloid and mastoid processes of the temporal bone. The prevailing view is that the deep layer of the parotid gland is derived from the deep cervical fascia. However, the superficial layer of the parotid capsule appears to be continuous with the fascia associated with platysma, and is now regarded as a component of the SMAS (Mitz & Peyronie 1976; Wassef 1987; Gosain et al 1993). It varies in thickness from a thick fibrous layer anteriorly to a thin translucent membrane posteriorly. It may be traced forwards as a separate layer which passes over the masseteric fascia (itself derived from the deep cervical fascia), separated from it by a cellular layer which contains branches of the facial nerve and the parotid duct. Histologically, the parotid fascia is atypical in that it contains muscle fibres which parallel those of platysma, especially in the lower part of the parotid capsule. Although thin fibrous septa may be seen in the subcutaneous layer at the histological level, macroscopically there is little evidence of a distinct layer of superficial fascia.
The deep fascia covering the muscles forming the parotid bed (digastric and styloid group of muscles) contains the stylomandibular and mandibulostylohyoid ligaments. The stylomandibular ligament passes from the styloid process to the angle of the mandible. The more extensive mandibulostylohyoid ligament (angular tract) passes between the angle of the mandible and the stylohyoid ligament for varying distances, generally reaching the hyoid bone. It is thick posteriorly but thins anteriorly in the region of the angle of the mandible. There is some dispute as to whether the mandibulostylohyoid ligament is part of the deep cervical fascia (Ziarah & Atkinson 1981), or lies deep to it (Shimada & Gasser 1988). The stylomandibular and mandibulostylohyoid ligaments separate the parotid gland region from the superficial part of the submandibular gland, and so are landmarks of surgical interest.
Temporo-parietal and temporal fasciae
Above the level of the zygomatic arch, on the lateral side of the head, the temporo-parietal fascia (superficial temporal fascia) constitutes a fascial layer which lies in the same plane as, but is not continuous with, the SMAS. It is quite separate from, and superficial to, the temporal fascia (deep temporal fascia). More superiorly, it blends with the galea aponeurotica. The plane between the temporo-parietal fascia and the underlying deep temporal fascia contains loose areolar tissue and a small amount of fat. This tissue plane, the temporo-parietal fat pad, is continuous superiorly with the subgaleal plane of loose areolar tissue in the scalp. Running superiorly in the temporo-parietal fascia or just deep to it are the superficial temporal vessels, the auriculotemporal nerve and its branches, and the temporal branches of the facial nerve. When raising a bicoronal flap, identification of the temporoparietal fat pad helps to separate these two fascial layers; subsequent dissection in a plane deep to the temporoparietal fascia protects the temporal branch of the facial nerve. The temporal fascia is a dense aponeurotic layer which lies deep to the temporo-parietal fat pad and covers temporalis: the deep surface of the fascia affords attachment to the superficial fibres of temporalis. Above, it is a single layer attached along the length of the superior temporal line, blending with the periosteum. Below, at approximately the level of the superior orbital rim, it splits into superficial and deep laminae which run downwards to attach to the lateral and medial margins of the upper surface of the zygomatic arch respectively. These fascial attachments have a clinical application in the reduction of fractures of the zygomatic complex via a Gillies approach: an instrument is inserted deep to the deep lamina of temporalis fascia through a scalp incision and used to elevate depressed zygomatic complex fractures. The fat enclosed between these two layers is termed the superficial temporal fat pad; it contains the zygomatico-orbital branch of the superficial temporal artery and a cutaneous nerve, the zygomatico-temporal branch of the maxillary nerve. The temporal fascia is overlapped by auriculares anterior and superior, the epicranial aponeurosis and part of orbicularis oculi, and the superficial temporal vessels and auriculotemporal nerve ascend over it.
Buccopharyngeal fascia
Buccinator is covered by a thin layer of fascia, the buccopharyngeal fascia, which also covers the superior constrictor of the pharynx.
Retaining ligaments of the face
These ligaments are fascial bands at specific sites which serve to anchor the skin to the underlying bone. The general cutaneous laxity that attends the ageing process renders facial skin subject to gravitational pull. However, at sites where retaining ligaments are present, the effect of gravitational pull is resisted. When performing facelift procedures, these ligaments must be surgically divided in order to facilitate redraping of facial skin. Examples of retaining ligaments in the face are the zygomatic ligament (also known as McGregor’s patch) and the mandibular ligament.
Fascial spaces
Two tissue spaces on the face may be involved in spread of odontogenic infection. They are the buccal tissue space, lying between the skin and surface of buccinator, and the infraorbital tissue space, lying between the bony attachments of levator labii superioris and levator anguli oris.
BONES OF THE FACIAL SKELETON AND CRANIAL VAULT
The skull consists of the facial skeleton and cranial vault (calvarium) attached at the skull base. The cranial vault encloses and protects the brain. The facial skeleton is the anterior part of the skull and includes the mandible. The bones of the nasoethmoidal and zygomaticomaxillary complexes are described here. The mandible is described in Chapter 30.
PARIETAL BONE
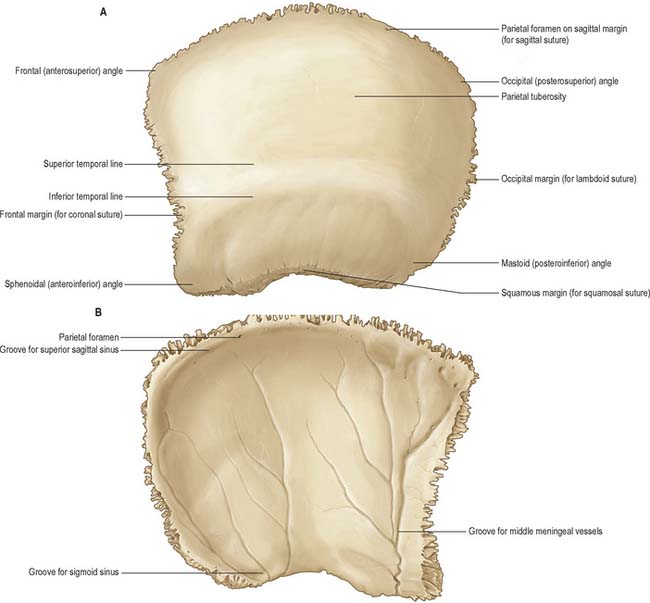
The two parietal bones form most of the cranial roof and sides of the skull. Each is irregularly quadrilateral and has two surfaces, four borders and four angles (Fig. 29.2).
The external surface is convex and smooth, with a central parietal tuber (tuberosity). Curved superior and inferior temporal lines cross it and form posterosuperior arches. The temporal fascia is attached to the superior line or arch and temporalis is attached to the inferior line or arch. The epicranial aponeurosis lies above these lines, and part of the temporal fossa lies below. Posteriorly, close to the sagittal (superior) border, an inconstant parietal foramen transmits a vein from the superior sagittal sinus and sometimes a branch of the occipital artery.
The internal surface is concave and marked by impressions of cerebral gyri and by grooves for the middle meningeal vessels. The latter ascend, inclining backwards, from the sphenoidal (anteroinferior) angle and posterior half (or more) of its inferior border. A groove for the superior sagittal sinus lies along the sagittal border, and is completed by the groove on the opposite parietal bone. The falx cerebri is attached to the edges of the groove. Granular foveolae for arachnoid granulations flank the sagittal sulcus, and are most pronounced in old age.
The dentated sagittal border, longest and thickest, articulates with the opposite parietal bone at the sagittal suture. The anterior part of the squamosal (inferior) border is short, thin and truncated, bevelled externally and overlapped by the greater wing of the sphenoid. The middle part of the inferior border is arched, bevelled externally and overlapped by the squamous part of the temporal bone. The posterior part of the inferior border is short, thick and serrated for articulation with the mastoid part.
The frontal border is deeply serrated, bevelled externally above, internally below, and articulates with the frontal bone to form one half of the coronal suture. The occipital border, deeply dentated, articulates with the occipital bone, forming one half of the lambdoid suture.
The frontal (anterosuperior) angle, which is approximately 90°, is at the bregma, where sagittal and coronal sutures meet, and marks the site of the anterior fontanelle in the neonatal skull. The sphenoidal (anteroinferior) angle lies between the frontal bone and greater wing of the sphenoid. Its internal surface is marked by a deep groove or canal that carries the frontal branches of the middle meningeal vessels. The frontal, parietal, sphenoid and temporal bones usually meet at the pterion, which marks the site of the sphenoidal fontanelle in the embryonic skull. The frontal bone sometimes meets the squamous part of the temporal bone, in which case the parietal bone fails to reach the greater wing of the sphenoid bone. The rounded occipital (posterosuperior) angle is at the lambda, the meeting of the sagittal and lambdoid sutures, which marks the site of the posterior fontanelle in the neonatal skull. The blunt mastoid (posteroinferior) angle articulates with the occipital bone and the mastoid portion of the temporal bones at the asterion. Internally it bears a broad, shallow groove for the junction of the transverse and sigmoid sinuses.
Ossification
Each parietal bone is ossified from two centres which appear in dense mesenchyme near the tuberosity, one above the other, at about the seventh week in utero. These two centres unite early and ossification subsequently radiates from them towards the margins. The angles are therefore the last parts to be ossified, and fontanelles occur at these sites. At birth the temporal lines are low down; they only reach their final position after the eruption of the molar teeth. Occasionally the parietal bone is divided by an anteroposterior suture.
FRONTAL BONE
The frontal bone is like half a shallow, irregular cap forming the forehead or frons (Fig. 29.3). It has three parts, and contains two cavities, the frontal sinuses.
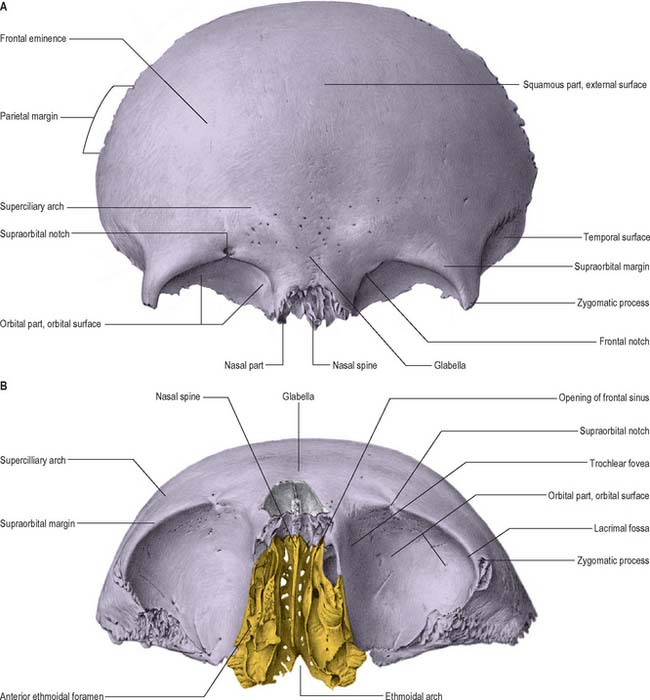
Fig. 29.3 Frontal bone. A, anterior view; B, inferior view, including the articulations between the frontal, ethmoid and nasal bones.
(From Sobotta 2006.)
Squamous part
The squamous part forms the major portion of the frontal bone. Its external surface has a rounded frontal tuber (tuberosity) approximately 3 cm above the midpoint of each supraorbital margin. These tubera vary, but are especially prominent in young skulls and more so in adult females than males. Below them and separated by a shallow groove, are two curved superciliary arches, medially prominent and joined by a smooth median elevated glabella. The arches are more prominent in males; prominence depends partly on the size of the frontal sinuses, but is occasionally associated with small sinuses. The curved supraorbital margins of the orbital openings lie inferior to the superciliary arches. The lateral two-thirds of each margin are sharp, the medial third rounded; a supraorbital notch or foramen, which transmits the supraorbital vessels and nerve, lies at the junction between them. A small frontal notch or foramen lies medial to the supraorbital notch in 50% of skulls. Both features show sexual dimorphism. The supraorbital margin ends laterally in a strong, prominent zygomatic process that articulates with the zygomatic bone. A line curves posterosuperiorly from the process and divides into superior and inferior temporal lines, which are continued on the squamous part of the temporal bone. The area of the frontal bone below and behind the temporal lines is known as the temporal surface and forms the anterior part of the temporal fossa. The parietal (posterior) margin is thick, deeply serrated, and bevelled internally above and externally below. Inferiorly it becomes a rough, triangular surface that articulates with the greater wing of the sphenoid.
The internal surface of the frontal bone is concave. Its upper, median, part displays a vertical sulcus whose edges unite below as the frontal crest. The sulcus contains the anterior part of the superior sagittal sinus. The crest ends in a small notch which is completed by the ethmoid bone to form a foramen caecum. The anterior portion of the falx cerebri is attached to the margins of the sulcus and to the frontal crest. The internal surface shows impressions of cerebral gyri, small furrows for meningeal vessels, and granular foveolae for arachnoid granulations near the sagittal sulcus.
Nasal part
The nasal part of the frontal bone lies between the supraorbital margins. A serrated nasal notch articulates with the nasal bones inferiorly and with the frontal processes of the maxillae and the lacrimal bones laterally. From the centre of the notch posteriorly the bone projects anteroinferiorly behind the nasal bones and the frontal processes of the maxillae, and supports the nasal bridge. The region ends in a sharp nasal spine, on each side of which a small grooved surface partly roofs the ipsilateral nasal cavity. The nasal spine makes a very small contribution to the nasal septum: it articulates anteriorly with the crest of the nasal bones and posteriorly with the perpendicular plate of the ethmoid bone.
Orbital parts
Most of the frontal bone is thick, and consists of trabecular tissue lying between two compact laminae. In contrast, the orbital plates consist entirely of compact bone and are thin and often translucent posteriorly, indeed they may be partly absorbed in old age.
The orbital plates form the largest part of the orbital roofs and are two thin, curved, triangular laminae separated by a wide ethmoidal notch. The orbital surface of each plate is smooth and concave, and bears a shallow anterolateral fossa for the lacrimal gland. The trochlear fovea (or spine) for attachment of a fibrocartilaginous trochlea through which the tendon of superior oblique plays, lies below and behind the medial end of the supraorbital margin, midway between the supraorbital notch and frontolacrimal suture. The convex cerebral surface is marked by frontal gyri and faint grooves for meningeal vessels.
The quadrilateral ethmoidal notch is occupied by the cribriform plate of the ethmoid bone. Inferior to its lateral margins, the bone articulates with the labyrinths of the ethmoid bone and impressions of the ethmoidal air cells can be seen on this surface. Two transverse grooves across each margin are converted into anterior and posterior ethmoidal canals by articulation with the ethmoid bone: these canals open on the medial orbital wall and transmit the anterior and posterior ethmoidal nerves and vessels. The posterior borders of the orbital plates are thin and serrated and articulate with the lesser wings of the sphenoid; their lateral parts usually appear in the middle cranial fossa between the greater and lesser wings of the sphenoid.
The frontal sinuses are two irregular cavities that ascend posterolaterally for a variable distance between the frontal laminae. They are separated by a thin septum and usually deflected from the median plane, which means that they are rarely symmetrical. The sinuses are variable in size and usually larger in males. Their openings lie anterior to the ethmoidal notch and lateral to the nasal spine, and each communicates with the middle meatus in the ipsilateral nasal cavity by a frontonasal canal.
The frontal sinuses are rudimentary at birth and can barely be distinguished. They show a primary expansion with eruption of the first deciduous molars at about 18 months, and again when the permanent molars begin to appear in the sixth year. Growth is slow in the early years but it can be detected radiographically by 6 years. They reach full size after puberty, although with advancing age osseous absorption may lead to further enlargement. Their degree of development appears to be linked to the prominence of the superciliary arches, which is thought to be a response to masticatory stresses. The frontal sinuses are described in Chapter 32.
Ossification
The frontal bone is ossified in fibrous mesenchyme from two primary centres that appear in the eighth week in utero, one near each frontal tuber. Ossification extends superiorly to form half of the main part of the bone; posteriorly to form the orbital part, and inferiorly to form nasal parts. Two secondary centres for the nasal spine appear about the tenth year. At birth the bone consists of two halves. The median suture usually disappears by about 8 years, but may persist as the metopic suture. Metopism has been assessed at 0–7.4% of individuals in various ethnic groups.
ETHMOID BONE
The ethmoid bone is cuboidal and fragile (Fig. 29.3B, Fig. 29.4, Fig. 29.5, Fig. 29.6). It lies anteriorly in the cranial base and contributes to the medial walls of the orbit, the nasal septum and the roof and lateral walls of the nasal cavity. It has a horizontal perforated cribriform plate, a median perpendicular plate, and two lateral labyrinths that contain the ethmoidal air cells.
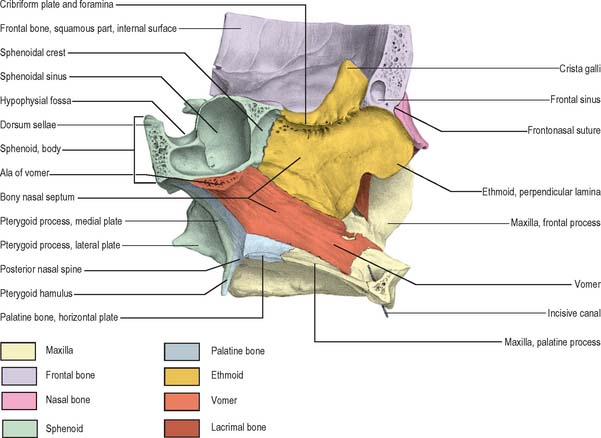
Fig. 29.4 Sagittal view of the facial skeleton, viewed from the right side of the nasal septum, looking towards the left.
(From Sobotta 2006.)
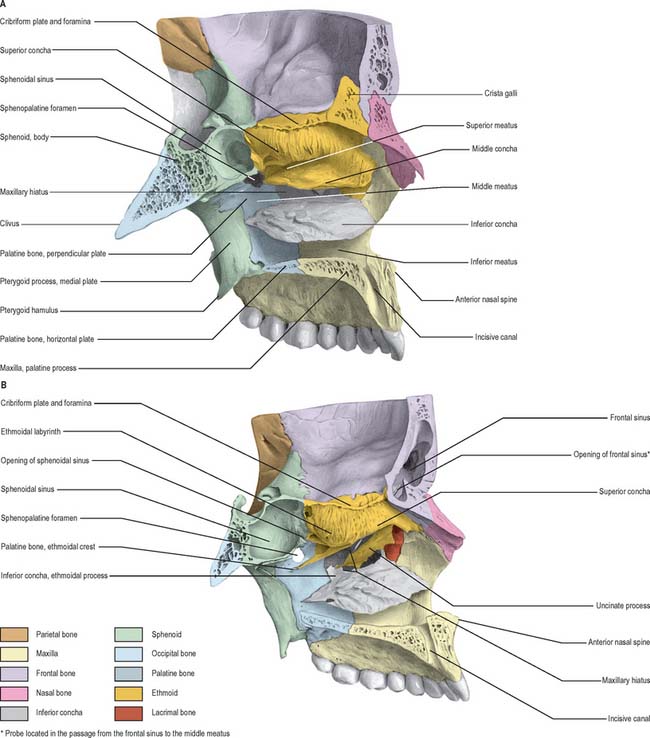
Fig. 29.5 A, B Sagittal view of the facial skeleton, showing the floor of the anterior cranial fossa, the lateral wall of the nasal cavity, the hard palate and the sphenoidal air sinus. In B, the middle concha in the lateral wall of the nasal cavity has been removed to reveal the uncinate process.
(From Sobotta 2006.)
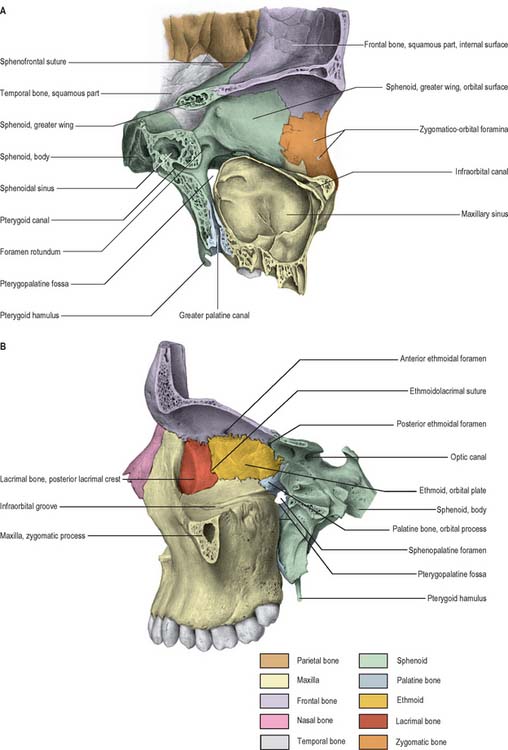
Fig. 29.6 A, Sagittal view of the facial skeleton, showing the bones forming the lateral wall of the left orbit and the maxillary air sinus. B, The bones forming the medial wall and the floor of the left orbit.
(From Sobotta 2006.)
Cribriform plate and crista galli
The cribriform plate fills the ethmoidal notch of the frontal bone and forms a large part of the nasal roof. It derives its name from the fact that it is penetrated by numerous foramina that transmit branches of the olfactory nerves and their associated meninges. A thick, smooth, triangular, median process, the crista galli, projects upwards from the centre of the cribriform plate. The falx cerebri is attached to its thin and curved posterior border, while its shorter, thick, anterior border articulates with the frontal bone by two small alae, so completing the foramen caecum. Its sides are generally smooth, but may show slight bulges that are related to underlying ethmoidal air cells. On both sides of the crista galli, the cribriform plate is narrow and depressed and is related to the gyrus rectus and the olfactory bulb which lie above it. On each side of the crista anteriorly there is a small slit occupied by dura mater. Just anterolateral to the slit, a foramen transmits the anterior ethmoidal nerve and vessels to the nasal cavity. A groove runs forwards to the foramen caecum from the anterior ethmoidal canal.
Perpendicular plate
The perpendicular plate is thin, flat, quadrilateral and median. It descends from the cribriform plate to form the upper part of the nasal septum, usually deviating slightly from the midline. Its anterior border articulates with the nasal spine of the frontal bone and the crests of the nasal bones, and its posterior border articulates with the crest of the body of the sphenoid bone above and the vomer below. The thick inferior border is attached to the nasal septal cartilage. Its surfaces are smooth except above, where numerous grooves and canals that transmit filaments of the olfactory nerves lead to medial foramina in the cribriform plate.
Ethmoidal labyrinths
The ethmoidal labyrinths consist of thin-walled ethmoidal air cells between two vertical plates. The lateral surface (orbital plate) of the labyrinth is part of the medial orbital wall. The air cells are arranged in anterior, middle and posterior groups. On average there are 11 anterior ethmoidal air cells, three middle, and six posterior. In the disarticulated bone, many air cells are open, but in life, and in the articulated skull, they are closed by proximity to adjoining bones, except where they open into the nasal cavity. The superior surface is crossed by two grooves that are converted into the anterior and posterior ethmoidal canals by the frontal bone; it shows open-air cells that are covered by the edges of the ethmoidal notch of the frontal bone. On the posterior surface open air cells are covered by the sphenoidal conchae and the orbital process of the palatine bone. The middle and posterior ethmoidal air cells are covered by a thin, smooth, oblong orbital plate that articulates superiorly with the orbital plate of the frontal bone, inferiorly with the maxilla and orbital process of the palatine bone, anteriorly with the lacrimal bone and posteriorly with the sphenoid bone. The walls of the air cells lying anterior to the orbital plate are completed by the lacrimal bone and frontal process of the maxilla.
A thin, curved uncinate process, variable in size, projects posteroinferiorly from the labyrinth. The upper edge of this process is a medial boundary of the hiatus semilunaris in the middle meatus. The uncinate process appears in the medial wall of the maxillary sinus as it crosses the ostium of the maxillary sinus to join the ethmoidal process of the inferior nasal concha.
The medial surface of the labyrinth forms part of the lateral nasal wall. It appears as a thin lamella that descends from the inferior surface of the cribriform plate and ends as the convoluted middle nasal concha. Superiorly the surface contains numerous vertical grooves that transmit bundles of olfactory nerves. Posteriorly it is divided by the narrow, oblique superior meatus, bounded above by the thin, curved superior nasal concha. Posterior ethmoidal air cells open into the superior meatus. The convex surface of the middle nasal concha extends along the entire medial surface of the labyrinth, anteroinferior to the superior meatus. Its lower edge is thick and its lateral surface is concave and forms part of the middle meatus. Middle ethmoidal air cells produce a swelling, the bulla ethmoidalis, on the lateral wall of the middle meatus, and open into the meatus, either on the bulla or above it. A curved infundibulum extends up and forwards from the middle meatus and communicates with the anterior ethmoidal sinuses. In more than 50% of crania it continues up as the frontonasal duct to include the drainage point for the frontal sinus. (The ethmoidal air cells are described further in Chapter 32.)
Ossification
The ethmoid bone ossifies in the cartilaginous nasal capsule from three centres, one in the perpendicular plate, and one in each labyrinth. The latter two appear in the orbital plates between the fourth and fifth months in utero, and extend into the ethmoid conchae. At birth, the labyrinths, although ill-developed, are partially ossified, and the remainder are cartilaginous. The perpendicular plate begins to ossify from the median centre during the first year, and fuses with the labyrinths early in the second year. The cribriform plate is ossified partly from the perpendicular plate, and partly from the labyrinths. The crista galli ossifies during the second year. The parts of the ethmoid bone unite to form a single bone at around 3 years of age. Ethmoidal air cells begin to develop at about 3 months in utero, and are therefore present at birth, however, they are difficult to visualize radiographically until the end of the first year. They grow slowly and have almost reached adult size by the age of 12 years.
INFERIOR NASAL CONCHA
The inferior nasal conchae are curved horizontal laminae in the lateral nasal walls (Fig. 29.5) (see also Ch. 32). Each has two surfaces (medial and lateral), two borders (superior and inferior) and two ends (anterior and posterior). The medial surface is convex, much perforated, and longitudinally grooved by vessels. The lateral surface is concave and part of the inferior meatus. The superior border, thin and irregular, may be divided into three regions: an anterior region articulating with the conchal crest of the maxilla; a posterior region articulating with the conchal crest of the palatine bone; and a middle region with three processes, which are variable in size and form. The lacrimal process is small and pointed and lies towards the front. It articulates apically with a descending process from the lacrimal bone, and at its margins with the edges of the nasolacrimal groove on the medial surface of the maxilla, thereby helping to complete the nasolacrimal canal. Most posteriorly, a thin ethmoidal process ascends to meet the uncinate process of the ethmoid bone. An intermediate thin maxillary process curves inferolaterally to articulate with the medial surface of the maxilla at the opening of the maxillary sinus. The inferior border is thick and spongiose, especially in its midpart. Both the anterior and posterior ends of the inferior nasal concha are more or less tapered, the posterior more than the anterior.
LACRIMAL BONE
The lacrimal bones are the smallest and most fragile of the cranial bones and lie anteriorly in the medial walls of the orbits (Fig. 29.5B). Each has two surfaces (medial and lateral) and four borders (anterior, posterior, superior and inferior). The lateral (orbital) surface is divided by a vertical posterior lacrimal crest. Anterior to the crest is a vertical groove whose anterior edge meets the posterior border of the frontal process of the maxilla to complete the fossa that houses the lacrimal sac. The medial wall of the groove is prolonged by a descending process that contributes to the formation of the nasolacrimal canal by joining the lips of the nasolacrimal groove of the maxilla and the lacrimal process of the inferior nasal concha. A smooth part of the medial orbital wall lies behind the posterior lacrimal crest: the lacrimal part of orbicularis oculi is attached to this surface and crest. The surface ends below in the lacrimal hamulus which, together with the maxilla, completes the upper opening of the nasolacrimal canal. The hamulus may appear as a separate lesser lacrimal bone. The anteroinferior region of the medial (nasal) surface is part of the middle meatus. Its posterosuperior part meets the ethmoid to complete some of the anterior ethmoidal air cells. The anterior border of the lacrimal bone articulates with the frontal process of the maxilla, the posterior border with the orbital plate of the ethmoid bone, the superior border with the frontal bone, and the inferior border with the orbital surface of the maxilla.
NASAL BONE
The nasal bones are small, oblong, variable in size and form, and placed side by side between the frontal processes of the maxillae (Fig. 29.4, Fig. 29.5, Fig. 29.6B). They jointly form the nasal bridge. Each nasal bone has two surfaces (external and internal) and four borders (superior, inferior, lateral and mesial). The external surface has a descending concavo-convex profile and is transversely convex. It is covered by procerus and nasalis and perforated centrally by a small foramen that transmits a vein. The internal surface, transversely concave, bears a longitudinal groove that houses the anterior ethmoidal nerve. The superior border, thick and serrated, articulates with the nasal part of the frontal bone. The inferior border, thin and notched, is continuous with the lateral nasal cartilage. The lateral border articulates with the frontal process of the maxilla. The medial border, thicker above, articulates with its fellow and projects behind as a vertical crest, thereby forming a small part of the nasal septum. It articulates from above with the nasal spine of the frontal bone, the perpendicular plate of the ethmoid bone, and the nasal septal cartilage.
VOMER
The vomer is thin, flat, and almost trapezoid (Fig. 29.4). It forms the posteroinferior part of the nasal septum and presents two surfaces and four borders. Both surfaces are marked by grooves for nerves and vessels. A prominent groove for the nasopalatine nerve and vessels lies obliquely in an anteroinferior plane. The superior border is thickest, and possesses a deep furrow between projecting alae which fits the rostrum of the body of the sphenoid bone. The alae articulate with the sphenoidal conchae, the vaginal processes of the medial pterygoid plates of the sphenoid bone, and the sphenoidal processes of the palatine bones. Where each ala lies between the body of the sphenoid and the vaginal process, its inferior surface helps to form the vomerovaginal canal. The inferior border articulates with the median nasal crests of the maxilla and palatine bones. The anterior border is the longest, and articulates in its upper half with the perpendicular plate of the ethmoid bone. Its lower half is cleft to receive the inferior margin of the nasal septal cartilage (see Ch. 32). The concave posterior border is thick and bifid above and thin below: it separates the posterior nasal apertures. The anterior extremity of the vomer articulates with the posterior margin of the maxillary incisor crest and descends between the incisive canals.
Ossification
The nasal septum is at first a plate of cartilage, part of which is ossified above to form the perpendicular plate of the ethmoid. Its anteroinferior region persists as septal cartilage. The vomer is ossified in a layer of connective tissue which covers the cartilage posteroinferiorly on each aspect. About the eighth week in utero, two centres appear flanking the midline, and in the twelfth week these unite below the cartilage, to form a deep groove for the nasal septal cartilage. Union of the bony lamellae progresses anterosuperiorly while the intervening cartilage is absorbed. By puberty the lamellae are almost united, but evidence of their bilaminar origin remains in the everted alae and anterior marginal groove.
ZYGOMATIC BONE
Each zygomatic bone forms the prominence of a cheek, contributes to the floor and lateral wall of the orbit and the walls of the temporal and infratemporal fossae, and completes the zygomatic arch. Each is roughly quadrangular and is described as having three surfaces, five borders and two processes (Fig. 29.7).
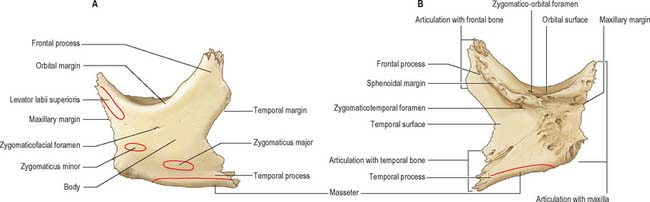
Fig. 29.7 Zygomatic bone. A, Anterolateral aspect. B, Posterolateral aspect. Muscle attachments shown in A.
The lateral (facial) surface is convex and is pierced near its orbital border by the zygomaticofacial foramen, which is often double and occasionally absent, and transmits the zygomaticofacial nerve and vessels. This surface gives attachment to zygomaticus major posteriorly and zygomaticus minor anteriorly. The posteromedial (temporal) surface has a rough anterior area for articulation with the zygomatic process of the maxilla, and a smooth, concave posterior area that extends up posteriorly on its frontal process as the anterior aspect of the temporal fossa. It also extends back on the medial aspect of the temporal process as an incomplete lateral wall for the infratemporal fossa. The zygomaticotemporal foramen pierces this surface near the base of the frontal process. The smooth and concave orbital surface forms the anterolateral part of the floor and adjoining lateral wall of the orbit, and extends up on the medial aspect of its frontal process. It usually bears zygomatico-orbital foramina which represent the openings of canals leading to the zygomaticofacial and zygomaticotemporal foramina.
The smoothly concave anterosuperior (orbital) border forms the inferolateral circumference of the orbital opening, and separates the orbital and lateral surfaces of the bone. The anteroinferior (maxillary) border articulates with the maxilla. Its medial end tapers to a point above the infraorbital foramen. A part of levator labii superioris is attached at this surface. The posterosuperior (temporal) border is sinuous, convex above and concave below, and is continuous with the posterior border of the frontal process and upper border of the zygomatic arch. The temporal fascia is attached to this border. There is often a small, easily palpable, marginal tubercle below the frontozygomatic suture. The posteroinferior border is roughened for the attachment of masseter. The serrated posteromedial border articulates with the greater wing of the sphenoid bone above, and the orbital surface of the maxilla below. Between these serrated regions a short, concave, non-articular part usually forms the lateral edge of the inferior orbital fissure. Occasionally absent, the fissure is then completed by the articulation of the maxilla and sphenoid (or with a small sutural bone between them).
The frontal process, thick and serrated, articulates above with the zygomatic process of the frontal bone and behind with the greater wing of the sphenoid bone. A tubercle of varying size and form, Whitnall’s tubercle, is usually present on its orbital aspect, within the orbital opening and about 1 cm below the frontozygomatic suture. This tubercle provides attachment for the lateral palpebral ligament, the suspensory ligament of the eye, and part of the aponeurosis of levator palpebrae superioris. The temporal process, directed backwards, has an oblique, serrated end that articulates with the zygomatic process of the temporal bone to complete the zygomatic arch.
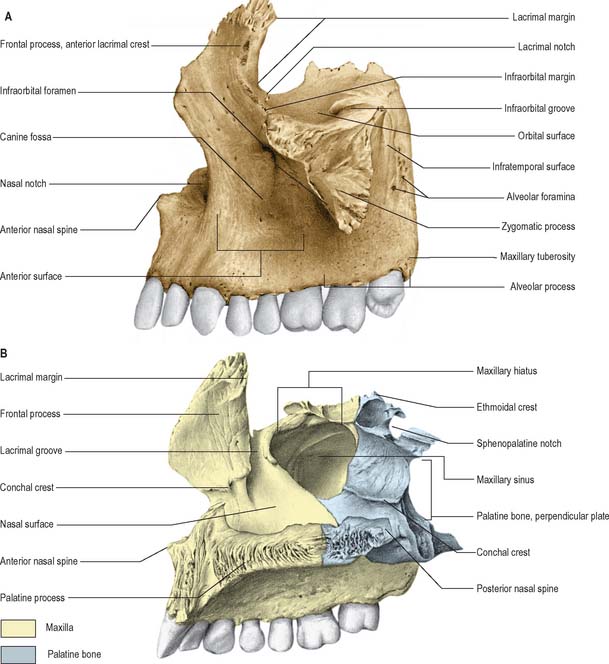
MAXILLA
The maxillae are the largest of the facial bones, other than the mandible, and jointly form the whole of the upper jaw. Each bone forms the greater part of the floor and lateral wall of the nasal cavity, and of the floor of the orbit, contributes to the infratemporal and pterygopalatine fossae, and bounds the inferior orbital and pterygomaxillary fissures. Each maxilla has a body and four processes, namely the zygomatic, frontal, alveolar and palatine processes (Fig. 29.6, Fig. 29.8).
Body
The body of the maxilla is roughly pyramidal, and has anterior, infratemporal (posterior), orbital and nasal surfaces that enclose the maxillary sinus.
Anterior surface
This surface faces anterolaterally and displays inferior elevations overlying the roots of teeth. There is a shallow incisive fossa above the incisors to which depressor septi is attached. A slip of orbicularis oris is attached to the alveolar border below this fossa, and nasalis is attached superolateral to it. Lateral to the incisive fossa is a larger, deeper canine fossa: levator anguli oris is attached to the bone of this fossa. The incisive and canine fossae are separated by the canine eminence, which overlies the socket of the canine tooth. The infraorbital foramen lies above the fossa and transmits the infraorbital vessels and nerve. Above the foramen a sharp border separates the anterior and orbital surfaces of the bone and contributes to the infraorbital margin. Levator labii superioris is attached here above the infraorbital foramen and levator anguli oris below it. Medially the anterior surface ends at a deeply concave nasal notch, terminating in a pointed process which, with its contralateral fellow, forms the anterior nasal spine. Nasalis and depressor septi are attached to the anterior surface near the notch.
Infratemporal surface
This surface is concave and faces posterolaterally, forming the anterior wall of the infratemporal fossa. It is separated from the anterior surface by the zygomatic process and a ridge (jugal crest) that ascends to it from the first molar socket. Near its centre are the openings of two or three alveolar canals which transmit posterior superior alveolar vessels and nerves. Posteroinferior is the maxillary tuberosity, roughened superomedially where it articulates with the pyramidal process of the palatine bone. A few fibres of medial pterygoid are attached here. Above the tuberosity the smooth anterior boundary of the pterygopalatine fossa is grooved by the maxillary nerve as it passes laterally and slightly upwards into the infraorbital groove on the orbital surface.
Orbital surface
This surface is smooth and triangular, and forms most of the floor of the orbit. Anteriorly its medial border bears a lacrimal notch, behind which it articulates with the lacrimal bone, the orbital plate of the ethmoid and, posteriorly, with the orbital process of the palatine bone. Its posterior border is smoothly rounded, and forms most of the anterior edge of the inferior orbital fissure. The infraorbital groove lies centrally. The anterior border is part of the orbital margin, and is continuous medially with the lacrimal crest of the frontal process of the maxilla. The infraorbital groove transmits the infraorbital vessels and nerve, and begins midway on the posterior border, where it is continuous with a groove on the posterior surface. It passes forwards into the infraorbital canal which opens on the anterior surface below the infraorbital margin. Near its midpoint, the infraorbital canal gives off a small lateral branch, the canalis sinuosus, that transmits the anterior superior alveolar nerve and vessels. The canalis sinuosus descends in the orbital floor lateral to the infraorbital canal, curves medially in the anterior wall of the maxillary sinus, and then passes below the infraorbital foramen to the margin of the anterior nasal aperture in front of the anterior end of the inferior concha. It follows the lower margin of the aperture and opens near the nasal septum in front of the incisive canal. The site of the attachment of inferior oblique may be indicated by a small depression in the bone at the anteromedial corner of the orbital surface, lateral to the lacrimal groove.
Nasal surface
This surface displays posterosuperiorly a large, irregular maxillary hiatus that leads into the maxillary sinus. Parts of air sinuses that are completed by articulation with the ethmoid and lacrimal bones lie at the upper border of the hiatus. The smooth concave surface below the hiatus is part of the inferior meatus. Posteriorly, the surface is roughened where it articulates with the perpendicular plate of the palatine bone. This surface is traversed by a groove which descends forwards from the midposterior border, and is converted into a greater palatine canal by the perpendicular plate. Anterior to the hiatus, a deep nasolacrimal groove, continuous above with the lacrimal groove, makes up about two-thirds of the circumference of the nasolacrimal canal. The rest is contributed by the descending part of the lacrimal bone and the lacrimal process of the inferior nasal concha. This canal conveys the nasolacrimal duct to the inferior meatus. More anteriorly, an oblique conchal crest articulates with the inferior nasal concha. The concavity below it is part of the inferior meatus, while the surface above it is part of the atrium of the middle meatus.
Zygomatic process
Anterior, infratemporal and orbital surfaces of the maxilla converge at a pyramidal projection, the zygomatic process. Anteriorly, the process merges into the facial surface of the body of the maxilla. Posteriorly, it is concave and continuous with the infratemporal surface. Superiorly, it is roughly serrated for articulation with the zygomatic bone. Inferiorly, a bony arched ridge, the zygomaticoalveolar ridge or jugal crest, separates the facial (anterior) and infratemporal surfaces.
Frontal process
The frontal process projects posterosuperiorly between the nasal and lacrimal bones. Its lateral surface is divided by a vertical anterior lacrimal crest which gives attachment to the medial palpebral ligament and is continuous below with the infraorbital margin. A small palpable tubercle at the junction of the crest and orbital surface is a guide to the lacrimal sac. The smooth area anterior to the lacrimal crest merges below with the anterior surface of the body of the maxilla. Parts of orbicularis oculi and levator labii superioris alaeque nasi are attached here. Behind the crest, a vertical groove combines with a groove on the lacrimal bone to complete the lacrimal fossa. The medial surface is part of the lateral nasal wall. A rough subapical area articulates with the ethmoid, and closes anterior ethmoidal air cells. Below this an oblique ethmoidal crest articulates posteriorly with the middle nasal concha, and anteriorly underlies the agger nasi, a ridge anterior to the concha on the lateral nasal wall. The ethmoidal crest forms the upper limit of the atrium of the middle meatus. The frontal process articulates above with the nasal part of the frontal bone. Its anterior border articulates with the nasal bone and its posterior border articulates with the lacrimal bone.
Alveolar process
The alveolar process is thick and arched, wide behind, and socketed for the roots of the upper teeth. The eight sockets on each side vary according to the tooth type. The socket for the canine is deepest, the sockets for the molars are widest and subdivided into three by septa, those for the incisors and second premolar are single, and that for the first premolar usually double. Buccinator is attached to the external alveolar aspect as far forwards as the first molar. In articulated maxillae the processes form the alveolar arch. Occasionally a variably prominent maxillary torus is present in the midline of the palate.
Palatine process
The palatine process, thick and horizontal, projects medially from the lowest part of the medial aspect of the maxilla. It forms a large part of the nasal floor and hard palate and is much thicker in front. Its inferior surface is concave and uneven, and with its contralateral fellow it forms the anterior three-fourths of the osseous (hard) palate. The palatine process displays numerous vascular foramina and depressions for palatine glands and, posterolaterally, two grooves that transmit the greater palatine vessels and nerves. The infundibular incisive fossa is placed between the two maxillae, behind the incisor teeth. The median intermaxillary palatal suture runs posterior to the fossa, and although a little uneven, is usually relatively flat on its oral aspect. Its bony margins are sometimes raised into a prominent longitudinal palatine torus. Two lateral incisive canals, each ascending into its half of the nasal cavity, open in the incisive fossa: they transmit the terminations of the greater palatine artery and nasopalatine nerve. Two additional median openings, anterior and posterior incisive foramina, are occasionally present: they transmit the nasopalatine nerves, the left usually passing through the anterior, and the right through the posterior foramen. On the inferior palatine surface a fine groove, sometimes termed the incisive suture, and prominent in young skulls, may be observed in adults. It extends anterolaterally from the incisive fossa to the interval between the lateral incisor and canine teeth. The superior surface of the palatine process is smooth, concave transversely, and forms most of the nasal floor. The incisive canal lies anteriorly, near its median margin. The lateral border is continuous with the body of the maxilla. The medial border, thicker in front, is raised into a nasal crest that, with its contralateral fellow, forms a groove for the vomer. The front of this ridge rises higher as an incisor crest, prolonged forwards into a sharp process which, with its fellow, forms an anterior nasal spine. The posterior border is serrated for articulation with the horizontal plate of the palatine bone.
Maxillary sinus
The maxillary sinus is the largest of the paranasal sinuses and is situated in the body of the maxilla. It is described in detail in Chapter 32.
Ossification
The maxilla ossifies from a single centre in a sheet of mesenchyme that appears above the canine fossa at about the sixth week in utero and spreads into the rest of the maxilla and its processes. The pattern of spread of ossification may initially leave an unmineralized zone roughly corresponding to a site where a premaxillary suture may occur. However, this deficiency is soon ossified; there is no evidence of a separate centre of ossification for the incisor-bearing portion of the maxilla (i.e. premaxilla).
The maxillary sinus appears as a shallow groove on the nasal aspect at about the fourth month in utero. Though small at birth, the sinus is identifiable radiologically. After birth it enlarges with the growing maxilla, though it is only fully developed following the eruption of the permanent dentition. The infraorbital vessels and nerve are for a time in an open groove in the orbital floor; the anterior part of the groove is subsequently converted into a canal by a lamina that grows in from the lateral side.
At birth the transverse and sagittal maxillary dimensions are greater than the vertical. The frontal process is prominent, but the body is little more than an alveolar process, because the alveoli reach almost to the orbital floor. In adults the vertical dimension is the greatest, reflecting the development of the alveolar process and enlargement of the sinus. When teeth are lost, the bone reverts towards its infantile shape: its height diminishes, the alveolar process is absorbed, and the lower parts of the bone contract and become reduced in thickness at the expense of the labial wall.
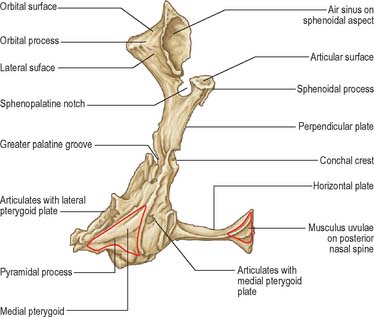
PALATINE BONE
The palatine bones are posteriorly placed in the nasal cavity, between the maxillae and the pterygoid processes of the sphenoid bones. They contribute to the floor and lateral walls of the nose, to the floor of the orbit and the hard palate, to the pterygopalatine and pterygoid fossae, and to the inferior orbital fissures. Each has two plates (horizontal and perpendicular) arranged as an L-shape, and three processes (pyramidal, orbital and sphenoidal) (Fig. 29.9).
Horizontal plate
The horizontal plate is quadrilateral, with two surfaces (nasal and palatine) and four borders (anterior, posterior, lateral and medial). The nasal surface, transversely concave, forms the posterior nasal floor. The palatine surface forms the posterior quarter of the bony palate with its contralateral fellow. There is often a curved palatine crest near its posterior margin. The posterior border is thin and concave: the expanded tendon of tensor veli palatini is attached to it and to its adjacent surface behind the palatine crest. Medially, with its contralateral fellow, the posterior border forms a median posterior nasal spine to which the uvular muscle is attached. The anterior border is serrated and articulates with the palatine process of the maxilla. The lateral border is continuous with the perpendicular plate of the palatine bone and is marked by a greater palatine groove. The medial border is thick and serrated and articulates with its contralateral fellow in the midline, forming the posterior part of the nasal crest which articulates with the posterior part of the lower edge of the vomer.
Perpendicular plate
The perpendicular plate is thin and oblong, and has two surfaces (nasal and maxillary) and four borders (anterior, posterior, superior and inferior). The nasal surface bears two crests (conchal and ethmoidal) and shows areas which contribute to the inferior, middle and superior meatuses. Inferiorly, the nasal surface is concave where it contributes to part of the inferior meatus. Above this is a horizontal conchal crest that articulates with the inferior concha. Above the conchal crest the surface presents a shallow depression that forms part of the middle meatus; it is limited above by an ethmoidal crest for the middle nasal concha, above which a narrow, horizontal groove forms part of the superior meatus.
The maxillary surface is largely rough and irregular and articulates with the nasal surface of the maxilla. Posterosuperiorly it forms a smooth medial wall to the pterygopalatine fossa. Its anterior area, also smooth, overlaps the maxillary hiatus from behind to form a posterior part of the medial wall of the maxillary sinus. A deep, obliquely descending greater palatine groove (converted into a canal by the maxilla) lies posteriorly on this maxillary surface: it transmits the greater palatine vessels and nerve.
The anterior border is thin and irregular. Level with the conchal crest, a pointed lamina projects below and behind the maxillary process of the inferior concha: it articulates with it and so appears in the medial wall of the maxillary sinus. The posterior border articulates via a serrated suture with the medial pterygoid plate. It is continuous above with the sphenoidal process of the palatine bone and expands below into its pyramidal process. Orbital and sphenoidal processes project from the superior border, and are separated by the sphenopalatine notch, which is converted into a foramen by articulation with the body of the sphenoid. This foramen connects the pterygopalatine fossa to the posterior part of the superior meatus, and transmits sphenopalatine vessels and the posterior superior nasal nerves. The inferior border is continuous with the lateral border of the horizontal plate and bears the lower end of the greater palatine groove in front of the pyramidal process.
Pyramidal process
The pyramidal process slopes down posterolaterally from the junction of the horizontal and perpendicular palatine plates into the angle between the pterygoid plates of the sphenoid bone. On its posterior surface a smooth, grooved triangular area, limited on each side by rough articular furrows which articulate with the pterygoid plates, completes the lower part of the pterygoid fossa. Anteriorly the lateral surface articulates with the maxillary tuberosity. This area gives attachment to fibres of the superficial head of medial pterygoid. Posteriorly a smooth triangular area appears low in the infratemporal fossa between the tuberosity and the lateral pterygoid plate. The inferior surface, near its union with the horizontal plate, bears the lesser palatine foramina which transmit the lesser palatine nerves and vessels.
Orbital process
The orbital process is directed superolaterally from in front of the perpendicular plate, and has a constricted “neck”. It encloses an air sinus and presents three articular and two non-articular surfaces. Of the articular surfaces, the oblong anterior (maxillary) surface faces down and anterolaterally and articulates with the maxilla. The posterior (sphenoidal) surface is directed up and posteromedially, and bears the opening of an air sinus. It usually communicates with the sphenoidal sinus, and is completed by a sphenoidal concha. The medial (ethmoidal) surface faces anteromedially and articulates with the labyrinth of the ethmoid bone. The sinus of the orbital process sometimes opens on the surface, and communicates with the posterior ethmoidal air cells. More rarely it opens on both the ethmoidal and sphenoidal surfaces, and communicates with both posterior ethmoidal air cells and the sphenoidal sinus.
Of the non-articular surfaces, the triangular superior (orbital) surface is directed superolaterally to the posterior part of the orbital floor. The lateral surface is oblong, faces the pterygopalatine fossa and is separated from the orbital surface by a rounded border that forms a medial part of the lower margin of the inferior orbital fissure. This surface may present a groove, directed superolaterally, for the maxillary nerve, and is continuous with the groove on the upper posterior surface of the maxilla. The border between the lateral and posterior surfaces descends anterior to the sphenopalatine notch.
Sphenoidal process
The sphenoidal process is a thin plate that is smaller and lower than the orbital process, and is directed superomedially. Its superior surface articulates with the sphenoidal concha and, above it, with the root of the medial pterygoid plate. It carries a groove that contributes to the formation of the palatovaginal canal. The concave inferomedial surface forms part of the roof and lateral wall of the nose. Posteriorly the lateral surface articulates with the medial pterygoid plate, while its smooth anterior region forms part of the medial wall of the pterygopalatine fossa. The posterior border articulates with the vaginal process of the medial pterygoid plate. The anterior border is the posterior edge of the sphenopalatine notch. The medial border articulates with the ala of the vomer. The sphenopalatine notch, between the two processes, is converted into a foramen by articulation with the body of the sphenoid bone.
Ossification
Ossification is in mesenchyme from one centre in the perpendicular plate that appears during the eighth week in utero. From this centre, ossification spreads into all parts. At birth, the height of the perpendicular plate equals the width of the horizontal plate, but in adults it is almost twice as great, a change in proportions that accords with those that occur in the maxilla.
FRACTURES OF THE FACIAL SKELETON
Fractures affecting the facial bones are common. They occur in road traffic accidents, sports injuries, accidents at work and, increasingly, as a consequence of interpersonal violence, often alcohol-related. Given that most people are right-handed, fractures resulting from assault occur more commonly on the left side of the facial skeleton. Skull fractures tend to adopt well-recognized patterns reflecting the shape and structure of the facial bones, local anatomical factors, and stress points which constitute sites of weakness.
Frequently these fractures do not occur as bilateral symmetrical fractures but occur in various combinations, e.g. both together, on the same side, and involving both sides. Typically these fractures arise from force applied anteriorly over a wide area. Such injuries are seen in road traffic accidents where, e.g. a driver or passenger is thrown forwards on to the steering wheel or dashboard. The direction of the applied force determines the displacement of these fractures. With the possible exception of the relatively weak lateral pterygoids, muscle pull plays a relatively small role. As the fractures are generally displaced backwards, because of the angulation of the strong skull base, there is also a downward component, which results clinically in a lengthening of the face and a dished-in appearance. There may be airway obstruction if this downwards and backwards displacement is severe.
Although the fractures that occur in severe injuries are often complex, it is convenient to describe them as arising in the upper, middle and lower thirds of the face, even though fractures may involve one or more of these areas. Upper third fractures involve the frontal bones. Middle third fractures involve the nasoethmoidal complex, orbit, zygomatic complex and maxilla. Lower third fractures correspond to fractures of the mandible.
Upper third of face
Fractures in the upper third of the face are almost invariably comminuted and are often associated with fractures of the middle third of the face. Fractures of the frontal bone may involve the frontal sinuses and/or orbital roof. If the frontonasal duct is traumatized its drainage may be impaired, which predisposes to ascending intracranial infection and mucocele development within the frontal sinuses. This risk may be minimized with frontonasal stents or frontonasal duct and frontal sinus obliteration with autogenous bone graft (see Ch. 32). Fractures that involve both the anterior and posterior walls of the frontal sinus also carry a risk of early and delayed intracranial infection, and often it is necessary to obliterate the frontal sinuses or cranialize the frontal sinuses in order to prevent this complication. Cranialization of the frontal sinuses involves the removal of the posterior wall and all frontal sinus mucosa, typically through a frontal craniotomy approach. Fractures of the posterior wall of the frontal sinus may be associated with dural tears (and cerebrospinal rhinorrhoea) which must be repaired at the same time. Fractures involving the orbital roof may be associated with displacement of the globe of the eye, diplopia and supraorbital nerve injury.
Middle third of the face
The middle third of the face is defined as that area bounded above by a transverse line connecting the two zygomaticofrontal sutures, passing through the frontomaxillary and frontonasal sutures, and limited below by the occlusal plane of the maxillary teeth. Posteriorly the region is limited by the sphenoethmoidal junction, but it includes the free margins of the pterygoid plates inferiorly. Fractures of the middle third of the facial skeleton may involve the maxillae, palatine bones, zygomatic bones, zygomatic processes of the temporal bones, nasal bones, vomer, ethmoid bone together with its nasal conchae, and the body and greater and lesser wings of the sphenoid bone. They are subdivided into fractures involving the central block and fractures involving the lateral middle thirds.
Central middle third of the face
The majority of the skeleton of the central middle third is composed of wafer thin sheets of cortical bone with stronger reinforcements, i.e. the palate and alveolar process; the lateral rim of the piriform aperture extending upwards (via the canine fossa) to the medial orbital rim, and finally to the glabella; the zygomatic buttress and its connections to the inferior and lateral orbital margins and the zygomatic arch; the orbital rims and the pterygoid plates. The strength lies in the facial surface of the skeleton which, although thin in most areas, is cross-braced. The design is ideally suited to transmit occlusal forces vertically to the skull base.
Central middle third fractures may involve the nasoethmoidal complex in isolation or as part of a more complex Le Fort pattern of injury. Le Fort I, II or III fractures inevitably involve the infratemporal fossa. The bones of the midface transmit the forces of impact directly to the cranium. The most important strut related to the infratemporal and pterygopalatine fossae is the pterygomaxillary strut. Fractures involving this strut may extend elsewhere to involve the cranial base and orbit. The associated soft tissue damage which accompanies these fractures may damage nerves, blood vessels and muscles. Injuries to the second or third divisions of the trigeminal nerve or the chorda tympani nerve result in altered sensation to the oral cavity, face and jaws, including impaired taste; fractures extending into the orbit may result in decreased visual acuity and ophthalmoplegia and neural damage to motor nerves or direct damage to muscles may result in problems with chewing, swallowing, speech, middle ear function and eye movements; injuries involving the pterygopalatine or otic ganglia interfere with lacrimation, nasal secretions and salivation.
Fractures may involve the osteocartilaginous framework of the nose in isolation or as part of complex injuries that also involve the paranasal sinuses and/or the orbits.
Simple fractures involve the nasal bones and/or frontal process of the maxilla. Only if there is displacement of the bones is a closed reduction of the fracture required. The terminal branch of the anterior ethmoidal nerve and its accompanying vessels are at risk when injuries involve the dorsum of the nose.
Complex nasal injuries may include nasofrontal suture disjunction, nasolacrimal and frontonasal duct injury and fracture of the ethmoid complex. The skeletal foundation of the nasoethmoidal complex consists of a strong triangular-shaped frame. However, all these structures are fragile and any force sufficient to fracture the frame results in severe comminution and displacement. The ethmoid air cells act as a crumple zone protecting the skull base from mechanical forces. A severe impact delivered to the midface, particularly over the bridge of the nose, may result in these structures being driven backwards between the orbits. This may result in traumatic hypertelorism, producing an increase in distance between the pupils. Associated displacement of the medial canthal ligaments results in traumatic telecanthus. Increased intercanthal distance (normal range 24–39 mm in Caucasians) may be corrected using microplates, stainless steel wire and acrylic canthal splints. Damage to the lacrimal system requires approximation of the severed canalicular ends or dacrocystorhinostomy. Comminution of the cribriform plates of the ethmoid may result in dural tears and cerebrospinal rhinorrhoea. Often nasoethmoidal fractures are combined with more extensive fractures of the frontal bone. The complexity of the injury has implications for subsequent facial reconstruction.
Le Fort I fractures (Guerin’s fracture)
Le Fort I fractures consist of a horizontal fracture line above the level of the floor of the nose involving the lower third of the nasal septum. The mobile segment consists of the palate, the alveolar process and the lower thirds of the pterygoid plates.
Le Fort II fractures (pyramidal fracture)
Le Fort II fractures are pyramidal fractures involving the maxillary bones. From the nasal bridge, the fracture enters the medial wall of the orbit to involve the lacrimal bone and then crosses the inferior orbital rim, usually at the junction of the medial one-third and lateral two-thirds, and often involves the infraorbital foramen. The fracture line then runs beneath the zygomaticomaxillary suture, traversing the lateral wall of the maxillary sinus to extend posteriorly and horizontally across the pterygoid plates. The zygomatic bones and arches remain attached to the skull base.
Le Fort III fractures run parallel with the base of the skull, separating the entire mid-facial skeleton from the cranial base. The fracture extends through the nasal base and continues posteriorly across the ethmoid bone. The fracture then crosses the lesser wing of the sphenoid and, on occasion, involves the optic foramen. Usually, however, it slopes down medially passing below the optic foramen to reach the pterygomaxillary fissure and pterygopalatine fossa. From the base of the inferior orbital fissure the fracture runs laterally and upwards, separating the greater wing of the sphenoid from the zygomatic bone, to reach the frontozygomatic suture. It also extends downwards and backwards across the pterygopalatine fossa to involve the root of the pterygoid plates. The zygomatic arch is usually fractured at the zygomaticotemporal suture.
Lateral middle third of the face
Fractures of the lateral middle third involve the zygomaticomaxillary complex. The zygomatic bone forms the prominence of the cheek. Since the most common cause of a zygomatic fracture is a blow from a fist, depressed fractures of the zygomaticomaxillary complex are a common injury. These injuries may occur in isolation or in association with orbital blow-out fractures. Isolated fractures of the zygomatic arch are relatively unusual.
Classic zygomatic complex fractures involve the zygomaticomaxillary, zygomaticotemporal and zygomaticofrontal sutures. The fracture line extends from the lateral wall of the orbit laterally into the infratemporal fossa at the zygomaticofrontal suture. From this point the fracture line extends inferiorly to join the most lateral aspect of the inferior orbital fissure, continues inferiorly along the posterior surface of the zygomatic buttress – where it communicates with the lateral bulge of the maxillary antrum – and runs around the zygomatic buttress, high in the buccal sulcus in the upper molar region, and then extends upwards towards the infraorbital foramen. It finally runs laterally along the floor of the orbit to reach the lateral extension of the inferior orbital fissure. Clinical signs may include facial asymmetry, infraorbital nerve paraesthesia/anaesthesia, limitation of mouth opening (if there is impingement of the coronoid process by a depressed arch fracture) and signs of orbital blow-out fracture (see below).
As zygomatic fractures involve the maxillary sinus (the lateral wall of which is frequently comminuted) and the infratemporal fossa, there is potential for spread of infection between these structures and then via foraminae in the skull base to the middle cranial fossa. Patients with zygomatic complex fractures must be advised to refrain from sneezing or nose-blowing which may force air from the antrum into the surrounding tissues (surgical emphysema) or into the orbit, resulting in proptosis of the eye.
The orbit is invariably involved in fractures of the zygomatic bone and in Le Fort II and III fractures. The orbit may also be involved in fractures of the frontal bone and extensive nasal complex injuries. Direct blunt trauma to the globe may result in displacement of the globe and fracture of the thin orbital floor (or medial wall) without associated rim involvement and is known as a ‘blow-out’ fracture. This protective mechanism of injury helps to maintain the integrity of the globe itself in preference to the orbital walls. There may be associated herniation of periorbital fat and/or inferior rectus muscle resulting in restriction of eye movement, diplopia, ipsilateral lowering of pupillary height, and enophthalmos (due to increased orbital volume). Fortunately the optic foramen which is situated within the lesser wing of the sphenoid bone is surrounded by dense bone and is only rarely involved in fractures. Direct injury to the optic nerve is therefore unusual.
Lower third of face (mandible)
The mandible is essentially a tubular bone bent into a blunt V-shape (see Ch. 30). This basic configuration is modified by sites of muscle attachment, principally masseter and medial pterygoid at the angle, and temporalis at the coronoid process. The presence of teeth, particularly those with long roots such as the canines, or of unerupted teeth, produces lines of weakness in the mandible. When the teeth are lost, or fail to develop, the subsequent progressive resorption of the alveolar bone means that the mandible reverts to its underlying tubular structure. Like all tubular bones, the strength of the mandible resides in a dense cortical plate, thickened anteriorly and at its lower border: it follows that the mandible is strongest anteriorly in the midline and is progressively weaker posteriorly towards the condylar processes. Again, like all tubular bones, the mandible has great resistance to compressive forces, but fractures at sites of tensile strain. It is liable to particular patterns of distribution of tensile strain when forces are applied to it. Anterior forces applied to the mental symphysis, or over the body of the mandible, lead to strain at the condylar necks and also along the lingual cortical plates on the contralateral side in the molar region. The mandible therefore often fractures at two sites and isolated fractures are relatively unusual. In order of frequency, fractures occur most commonly at the neck of the condyle, the angle, the parasymphysial region and the body of the mandible.
Condylar process
The condyle is protected from direct injury by the zygomatic arches. Fractures occur usually by the transmission of force following a blow to the front of the mandible or to the contralateral body. Except in children, most condylar fractures are not intracapsular, and occur in the neck. They usually run obliquely downwards and backwards from the mandibular notch. The condyle is usually displaced anteromedially (because of the attachment of lateral pterygoid to the temporomandibular joint disc, capsule and anterior border of the neck of the condyle).
Angle of the mandible
The majority of fractures of the mandible run posteriorly and inferiorly from the alveolar bone to the angle. The presence of a third molar tooth produces a line of weakness and a fracture line will pass through its socket. The unopposed pull of the powerful elevator muscles (masseter, medial pterygoid and temporalis) will typically displace the posterior fragment superiorly, anteriorly and medially.
Ramus and coronoid process
Fractures at the ramus exhibit very little displacement as a consequence of the splinting activity of medial pterygoid medially and masseter laterally, the pterygo-masseteric sling: their wide attachments to the ramus extend across the fracture lines. Similarly the coronoid process is rarely significantly displaced because it is splinted by the tendinous insertion of temporalis.
Body of the mandible
Most fractures of the body of the mandible occur as the result of direct trauma and tend to be concentrated in the first molar or canine region. The more anterior the site of the fracture, the more the upward displacement of the elevators is counteracted by the downward pull of geniohyoid and the anterior belly of digastric. When teeth are present displacement is limited by the dental occlusion (i.e. further displacement is resisted by the lower and upper teeth), whereas displacement may be considerable in an edentulous patient.
Campbell’s lines
Campbell’s lines are five lines that are systematically traced when assessing maxillofacial radiographs. Line 1 joins the two zygomaticofrontal sutures: it runs along the superior orbital margins and crosses the midline in the region of the glabella. Line 2 runs along the zygomatic bone and the inferior orbital margin, crosses the frontal process of the maxilla and lateral wall of the nose, then passes through the nasal septum to follow a similar course to the contralateral zygomatic bone. Line 3 begins at the condyle of the mandible, passes across the mandibular notch and coronoid process of the mandible, then crosses the maxillary sinus from its lateral to medial walls and continues through the lateral wall of the nose at the level of the nasal floor; it follows a similar course on the contralateral side. Line 4 follows the occlusal plane of the upper and lower teeth, and line 5 follows the lower border of the mandible.
Cranial base
The cranial base, namely the frontal, ethmoid, sphenoid and occipital bones, is a relatively solid platform inclined at an angle of 45° to the maxillary occlusal plane. Fractures of the cranial base are not readily visible on normal radiographs and are best detected on CT scans. They result in bleeding in the floor of the middle cranial fossa which often presents as bruising over the mastoid process (Battle’s sign). These fractures may be associated with dural tears and escape of cerebrospinal fluid from the nose (rhinorrhoea) or ruptured tympanic membrane (otorrhoea). Alternatively, if this membrane remains intact it may be seen as blue and bulging, haemotympanum.
SKELETAL ACCESS SURGERY
The craniofacial skeleton has an excellent blood supply, and so can be dismantled as a series of osteoplastic flaps. The surgical disarticulation of the craniofacial skeleton has been used to gain access to otherwise inaccessible sites in order to allow the surgeon to attend to pathology in the skull base, cervical spine and anterior and posterior cranial fossae. The aim is to provide increased and more direct exposure of both the pathology and the adjacent vital structures without the need to resect uninvolved structures. The craniofacial skeleton can be divided into a series of modular osteotomies, which permit both independent and conjoined mobilization.
The zygomatic and nasal bones and the maxilla may be exposed and mobilized, pedicled on the overlying soft tissues either unilaterally or bilaterally. These approaches improve access to the nasal cavity, maxillary, ethmoid and sphenoid sinuses, the soft palate and nasopharynx, and the infratemporal fossa and pharyngeal space. The exposures may be extended to gain access to the anterior and middle cranial fossae, cavernous sinus, clivus, craniocervical junction and upper cervical vertebrae.
A variety of different access osteotomies have been described and found to be useful in specific clinical situations. Most of the osteotomies described follow the conventional patterns of facial fractures described above. The entire hemimaxilla and zygoma can be mobilized, and pedicled on the soft tissues of the face by making bone cuts that follow the lines of a Le Fort II fracture on one side. The osteotomy is completed by dividing the upper alveolus and palate just to the side of the nasal septum and perpendicular plate of the vomer. The maxilla may be mobilized at the Le Fort I level and downfractured, pedicled on the palatoglossal muscles and soft tissue attachments. This gives good access to the nasopharynx, clivus and upper cervical spine, particularly if the palate is divided in the midline.
Lateral zygomatic osteotomies may be performed to gain access to the orbital apex and infratemporal fossa. The surgical approach is from behind using a hemi- or bicoronal flap. The zygomatic complex is mobilized inferiorly pedicled on masseter. When combined with a mandibular ramus osteotomy, access is gained to the retromaxillary area and pterygoid space as well as to the infratemporal fossa. In combination with a frontotemporal craniotomy, the zygomatic osteotomy has been used for access to the middle cranial fossa, cavernous sinus, apex of the petrous temporal bone and the interpeduncular cistern.
Dividing the lower lip in the midline, and dividing the mandible either in the midline or just in front of the mental foramen, allows the hemimandible to be swung laterally. The technique is used to give improved access to the floor of the mouth, the base of the tongue, tonsillar fossa, soft palate, oropharynx, posterior pharyngeal wall, supraglottic larynx and pterygomandibular region. By extending the dissection laterally access is gained to the pterygoid space, infratemporal fossa and parapharyngeal space. By dissecting more medially access is gained to the nasopharynx, lower part of the clivus and all seven of the cervical vertebrae. A modification of the mandibular swing procedure increases access up to the skull base, by combining the classic mandibular swing with a horizontal osteotomy of the mandibular ramus above the level of the lingula.
MUSCLES OF THE FACE
Craniofacial muscles are associated with the orbital margins and eyelids, external nose and nostrils, lips, cheeks and mouth, pinna, scalp and cervical skin, and collectively are often called, not very accurately, ‘muscles of facial expression’ (Fig. 29.10). Their organization differs from that of muscles in most other regions of the body because there is no deep membranous fascia beneath the skin of the face, and many small slips of muscle that are attached to the facial skeleton insert directly into the skin.
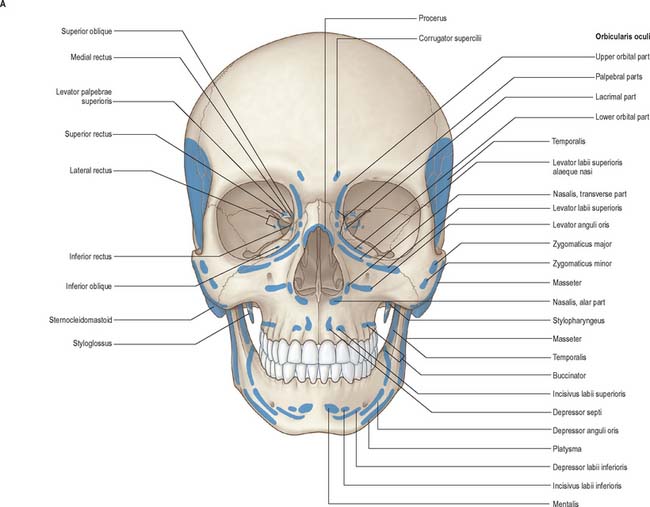
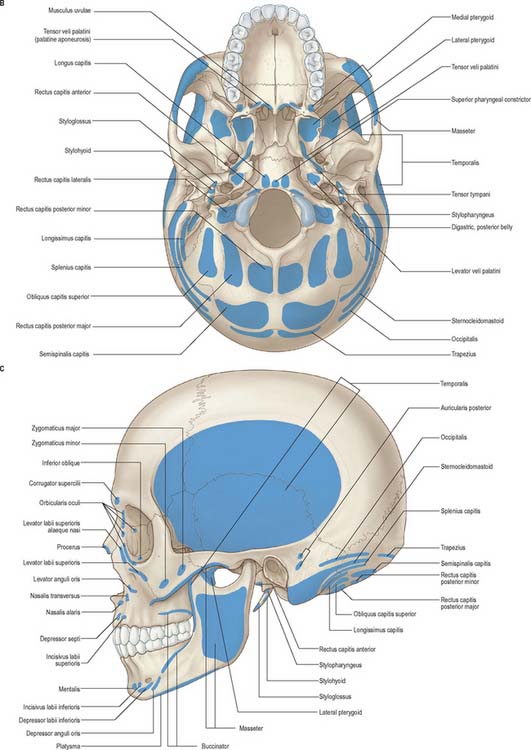
Fig. 29.10 A, Anterior view of the skull, showing muscle attachments. B, Basal view of the skull, showing muscle attachments. C, Lateral view of the skull, showing muscle attachments.
Although these muscles produce movements of the facial skin that reflect emotions, it is usually argued that their primary function is to act as sphincters and dilators of the facial orifices and that the function of facial expression has developed secondarily. Embryologically, they are derived from the mesenchyme of the second branchial arch and so are innervated by the facial nerve. Topographically and functionally the muscles of facial expression may be subdivided into epicranial, circumorbital and palpebral, nasal, and buccolabial groups (Fig. 29.11).
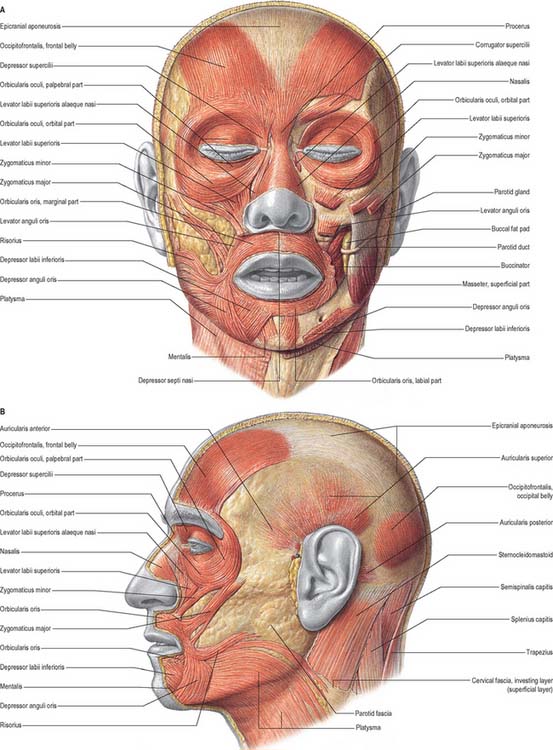
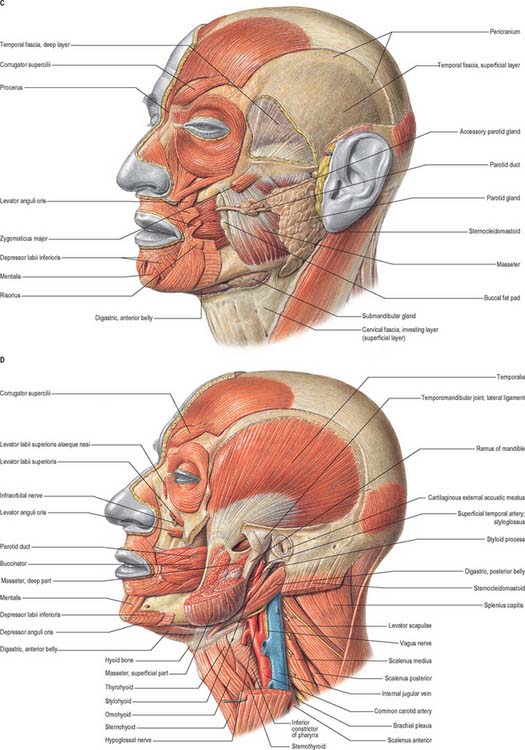
Fig. 29.11 The superficial muscles of the head and neck. A, frontal view; B–D show the muscles of the left lateral side of the head and upper part of the neck at progressively deeper levels.
(From Sobotta 2006.)
EPICRANIAL MUSCLE GROUP
Epicranius
Epicranius consists of occipitofrontalis and temporoparietalis.
Occipitofrontalis
Occipitofrontalis covers the dome of the skull from the highest nuchal lines to the eyebrows. It is a broad, musculofibrous layer and consists of four thin, muscular quadrilateral parts, two occipital and two frontal, connected by the epicranial aponeurosis. Each occipital part (occipitalis) arises by tendinous fibres from the lateral two-thirds of the highest nuchal line of the occipital bone and the adjacent region of the mastoid part of the temporal bone, and extends forwards to join the aponeurosis. The gap between the two occipital parts is occupied by an extension of the epicranial aponeurosis. Each frontal part (frontalis) is adherent to the superficial fascia, particularly of the eyebrows. Although frontalis has no bony attachments of its own, its fibres blend with those of adjacent muscles – procerus, corrugator supercilii and orbicularis oculi – and ascend to join the epicranial aponeurosis in front of the coronal suture.
Occipitofrontalis is supplied by branches of the superficial temporal, ophthalmic, posterior auricular and occipital arteries.
The occipital part of occipitofrontalis is supplied by the posterior auricular branch of the facial nerve and the frontal part is supplied by the temporal branches of the facial nerve.
Acting from above, the frontal parts raise the eyebrows and the skin over the root of the nose (e.g. as in expressions of surprise or horror). Acting from below, the frontal parts draw the scalp forwards, throwing the forehead into transverse wrinkles. The occipital parts draw the scalp backwards. Acting alternately, the occipital and frontal parts can move the entire scalp backwards and forwards.
A thin muscular slip, transversus nuchae, is present in 25% of people. It arises from the external occipital protuberance or from the superior nuchal line, either superficial or deep to trapezius. It is frequently inserted with auricularis posterior, but may blend with the posterior edge of sternocleidomastoid.
Epicranial aponeurosis
The epicranial aponeurosis covers the upper part of the cranium and, with the epicranial muscle, forms a continuous fibromuscular sheet that extends from the occiput to the eyebrows. Posteriorly, between the occipital parts of occipitofrontalis, it is attached to the external protuberance and highest nuchal line of the occipital bone. Anteriorly it splits to enclose the frontal parts and sends a short narrow prolongation between them. Laterally, the anterior and superior auricular muscles are attached to it; the aponeurosis is thinner, and continues over the temporal fascia to the zygomatic arch. It is united to the skin lying over the cranial vault by fibrous superficial fascia, but it is connected more loosely to the underlying pericranium by areolar tissue, an arrangement that allows it to move freely, carrying with it the skin of the scalp.
CIRCUMORBITAL AND PALPEBRAL MUSCLE GROUP
The circumorbital and palpebral group of muscles are orbicularis oculi, corrugator supercilii and levator palpebrae superioris. The first two are described here; levator palpebrae superioris is described in Chapter 39.
Orbicularis oculi
Orbicularis oculi is a broad, flat, elliptical muscle which surrounds the circumference of the orbit and spreads into the adjacent regions of the eyelids, anterior temporal region, infraorbital cheek and superciliary region. It has orbital, palpebral and lacrimal parts and a small ciliary bundle.
The orbital part arises from the nasal component of the frontal bone, the frontal process of the maxilla and from the medial palpebral ligament. The fibres form complete ellipses, without interruption on the lateral side, where there is no bony attachment. The upper orbital fibres blend with the frontal part of occipitofrontalis and corrugator supercilii. Many of them are inserted into the skin and subcutaneous tissue of the eyebrow and constitute depressor supercilii. Inferiorly and medially, the ellipses overlap or blend to some extent with adjacent muscles (levator labii superioris alaeque nasi, levator labii superioris and zygomaticus minor). At the extreme periphery, sectors of complete, and sometimes incomplete, ellipses have a loose areolar connection with the temporal extension of the epicranial aponeurosis.
The palpebral part arises from the medial palpebral ligament, mainly from its superficial surface, and from the bone immediately above and below the ligament. The fibres sweep across the eyelids anterior to the orbital septum, interlacing at the lateral commissure to form the lateral palpebral raphe. A small group of fine fibres, close to the margin of each eyelid behind the eyelashes, constitutes the ciliary bundle.
The lacrimal part arises from the upper part of the lacrimal crest, and the adjacent lateral surface, of the lacrimal bone. It passes laterally behind the nasolacrimal sac (where some fibres are inserted into the associated fascia), and divides into upper and lower slips. Some fibres are inserted into the tarsi of the eyelids close to the lacrimal canaliculi, but most continue across in front of the tarsi and interlace in the lateral palpebral raphe.
Orbicularis oculi is supplied by branches of the facial, superficial temporal, maxillary and ophthalmic arteries.
Orbicularis oculi is the sphincter muscle of the eyelids and plays an important role in facial expression and various ocular reflexes. The orbital portion is usually activated under voluntary control. Contraction of the upper orbital fibres produces vertical furrowing above the bridge of the nose, narrowing of the palpebral fissure, and bunching and protrusion of the eyebrows, which reduces the amount of light entering the eyes. Eye closure is largely affected by lowering of the upper eyelid, but there is also considerable elevation of the lower eyelid. The palpebral portion can be contracted voluntarily, to close the lids gently as in sleep, or reflexly, to close the lids protectively in blinking. The palpebral part has upper depressor and lower elevator fascicles. The lacrimal part of the muscle draws the eyelids and the lacrimal papillae medially, thereby exerting traction on the lacrimal fascia, and may aid drainage of tears by dilating the lacrimal sac. It may also influence pressure gradients within the lacrimal gland and ducts. This activity may assist in the sinuous flow of tears across the cornea, direct the lacrimal punctum into the lacus lacrimalis, and express secretions of the ciliary and tarsal glands. When the entire orbicularis oculi muscle contracts, the skin is thrown into folds which radiate from the lateral angle of the eyelids. Such folds, when permanent, cause wrinkles in middle age (the so-called ‘crow’s feet’).
Corrugator supercilii
Corrugator supercilii is a small pyramidal muscle located at the medial end of each eyebrow, lying deep to the frontal part of occipitofrontalis and orbicularis oculi, with which it is partially blended. It arises from bone at the medial end of the superciliary arch and its fibres pass laterally and slightly upwards to exert traction on the skin above the middle of the supraorbital margin.
NASAL MUSCLE GROUP
The nasal muscle group, which consists of procerus, nasalis and depressor septi, is described in Chapter 32.
BUCCOLABIAL MUSCLE GROUP
The shape of the mouth and the posture of the lips are controlled by a complex three-dimensional assembly of muscular slips. These include elevators, retractors and evertors of the upper lip (levator labii superioris alaeque nasi, levator labii superioris, zygomaticus major and minor, levator anguli oris and risorius); depressors, retractors and evertors of the lower lip (depressor labii inferioris, depressor anguli oris, and mentalis); a compound sphincter (orbicularis oris, incisivus superior and inferior); and buccinator.
Levator labii superioris alaequae nasi
Levator labii superioris alaequae nasi is described in Chapter 32.
Levator labii superioris
Levator labii superioris arises from the maxilla and zygomatic bone above the infraorbital foramen. Its fibres converge into the muscular substance of the upper lip between the lateral slip of levator labii superioris alaequae nasi and zygomaticus minor.
Zygomaticus major
Zygomaticus major arises from the zygomatic bone, just in front of the zygomaticotemporal suture, and passes to the angle of the mouth where it blends with the fibres of levator anguli oris, orbicularis oris and more deeply placed muscular bands.
Zygomaticus minor
Zygomaticus minor arises from the lateral surface of the zygomatic bone immediately behind the zygomaticomaxillary suture, and passes downwards and medially into the muscular substance of the upper lip. Superiorly it is separated from levator labii superioris by a narrow triangular interval, and inferiorly it blends with this muscle.
Zygomaticus minor elevates the upper lip, exposing the maxillary teeth. It also assists in deepening and elevating the nasolabial furrow. Acting together, the main elevators of the lip – levator labii superioris alaequae nasi, levator labii superioris and zygomaticus minor – curl the upper lip in smiling, and in expressing smugness, contempt or disdain.
Levator anguli oris
Levator anguli oris arises from the canine fossa of the maxilla, just below the infraorbital foramen and inserts into and below the angle of the mouth. Its fibres mingle there with other muscle fibres (zygomaticus major, depressor anguli oris, orbicularis oris). Some superficial fibres curve anteriorly and attach to the dermal floor of the lower part of the nasolabial furrow. The infraorbital nerve and accompanying vessels enter the face via the infraorbital foramen between the origins of levator anguli oris and levator labii superioris.
Malaris
Malaris is a thin sheet of muscle that is sometimes found covering and blending with zygomaticus major and minor and levator labii superioris. It is subject to considerable variation. When present, it is continuous with the inferior limit of orbicularis oculi, from which it is possibly derived. Its fibres incline medially and downwards. Some of its superficial fascicles have a dermal attachment to the nasolabial ridge and sulcus, and others pass directly to the angle of the mouth and to the outer third of the upper lip to intersect with bundles of orbicularis oris.
Mentalis
Mentalis is a conical fasciculus lying at the side of the frenulum of the lower lip. The fibres arise from the incisive fossa of the mandible and descend to attach to the skin of the chin.
Depressor labii inferioris
Depressor labii inferioris is a quadrilateral muscle that arises from the oblique line of the mandible, between the symphysis menti and the mental foramen. It passes upwards and medially into the skin and mucosa of the lower lip, blending with its contralateral fellow and with orbicularis oris. Below and laterally it is continuous with platysma.
Depressor anguli oris
Depressor anguli oris has a long, linear origin from the mental tubercle of the mandible and its continuation, the oblique line, below and lateral to depressor labii inferioris. It converges into a narrow fasciculus that blends at the angle of the mouth with orbicularis oris and risorius, and some fibres continue into levator anguli oris. Depressor anguli oris is continuous below with platysma and cervical fasciae. Some of its fibres may pass below the mental tubercle and cross the midline to interlace with their contralateral fellows, thereby forming transversus menti (the ‘mental sling’).
Buccinator
The muscle of the cheek, buccinator, is a thin quadrilateral muscle which occupies the interval between the maxilla and the mandible. Its upper and lower boundaries are attached to the outer surfaces of the alveolar processes of the maxilla and mandible respectively opposite the molar teeth, and its posterior border is attached to the anterior margin of the pterygomandibular raphe. In addition, a few fibres spring from a fine tendinous band that bridges the interval between the maxilla and the pterygoid hamulus, between the tuberosity of the maxilla and the upper end of the pterygomandibular raphe. On its way to the soft palate the tendon of tensor veli palatini pierces the pharyngeal wall in the small gap that lies behind this tendinous band. The posterior part of buccinator is deeply placed, internal to the mandibular ramus and in the plane of the medial pterygoid plate. Its anterior component curves out behind the third molar tooth to lie in the submucosa of the cheek and lips. The fibres of buccinator converge towards the modiolus near the angle of the mouth. Here the central (pterygomandibular) fibres intersect, those from below cross to the upper part of orbicularis oris, and those from above cross to the lower part. The highest (maxillary) and lowest (mandibular) fibres of buccinator continue forward to enter their corresponding lips without decussation. As buccinator courses through the cheek and modiolus substantial numbers of its fibres are diverted internally to attach to submucosa.
Posteriorly, buccinator lies in the same plane as the superior pharyngeal constrictor, which arises from the posterior margin of the pterygomandibular raphe, and is covered there by the buccopharyngeal fascia. Superficially, the buccal pad of fat separates the posterior part of buccinator from the ramus of the mandible, masseter and part of temporalis. Anteriorly, the superficial surface of buccinator is related to zygomaticus major, risorius, levator and depressor anguli oris, and the parotid duct. It is crossed by the facial artery, facial vein and branches of the facial and buccal nerves. The deep surface of buccinator is related to the buccal glands and mucous membrane of the mouth. The parotid duct pierces buccinator opposite the third upper molar tooth, and lies on the deep surface of the muscle before opening into the mouth opposite the maxillary second molar tooth.
Buccinator is supplied by branches from the facial artery and the buccal branch of the maxillary artery.
Buccinator compresses the cheek against the teeth and gums during mastication, and assists the tongue in directing food between the teeth. As the mouth closes, the teeth glide over the buccolabial mucosa, which must be retracted progressively from their occlusal surfaces by buccinator and other submucosally attached muscles. When the cheeks have been distended with air, the buccinators expel it between the lips, an activity important when playing wind instruments, and which accounts for the name of the muscle (Latin buccinators = trumpeter).
Pterygomandibular raphe
The pterygomandibular raphe is a thin band of tendinous fibres that stretches from the hamulus of the medial pterygoid plate down to the posterior end of the mylohyoid line of the mandible. It is easily palpated medially, where it is covered by the mucous membrane of the mouth, and laterally it is separated from the ramus of the mandible by a quantity of adipose tissue. It gives attachment posteriorly to the superior constrictor of the pharynx, and anteriorly to the central part of buccinator. The pterygomandibular raphe is a useful anatomical landmark for the administration of inferior alveolar nerve blocks because the nerve lies lateral to it.
Orbicularis oris
Orbicularis oris is so named because it was once assumed that the oral fissure was surrounded by a series of complete ellipses of striated muscle which acted together in the manner of a sphincter. However, it is now recognized that the muscle actually consists of four substantially independent quadrants (upper, lower, left and right), each of which contains a larger pars peripheralis and a smaller pars marginalis. Marginal and peripheral parts are apposed along lines that correspond externally to the lines of junction between the vermilion zone of the lip and the skin. Thus, orbicularis oris is composed of eight segments, each of which is named systematically according to its location. Each segment resembles a fan that has its stem at the modiolus and is open in peripheral segments and almost closed in marginal segments.
Pars peripheralis
Pars peripheralis has, in each quadrant, a lateral stem attached to the labial side of the modiolus over its full thickness, from apex to base, including the corresponding upper or lower cornu. Most of these stem fibres are thought to originate within the modiolus (although it is possible that some are direct continuations from the other modiolar muscles). The consensus view is that stem fibres are reinforced directly by fibres from buccinator (upper fibres and decussating lower central fibres), levator anguli oris and the superficial part of zygomaticus major in the upper lip, and from buccinator (lower fibres and decussating upper central fibres), and depressor anguli oris in the lower lip.
The fibres of orbicularis oris enter their respective superior and inferior labial areas and diverge to form triangular muscular sheets. These are thickest at the junctions between skin and the vermilion zone and become progressively thinner as they reach the limits of the labial region (as defined above). The greater part of each sheet enters the free lip, where its fibres aggregate into cylindrical bundles orientated parallel to the vermilion zone. Fibres of the direct labial tractors pass to their submucosal attachments between these cylindrical bundles and between pars peripheralis and pars marginalis. In the upper lip, the highest fibres run near the nasolabial sulcus, a few fibres attach to the sulcus, and a few to the nasal ala and septum. In the lower lip, the lowest fibres reach and attach to the mentolabial sulcus. A small proportion of the main body of fibres is thought to end in the labial connective tissue, dermis or submucosa as it traverses its quadrant of free lip. Most fibres continue towards the median plane and cross some 5 mm into the opposite half-lip. At this point the fibres from the two sides interlace on their way to their dermal insertions, creating the ridges of the philtrum of the upper lip and the less marked corresponding depression in the lower lip.
Pars marginalis
Pars marginalis of orbicularis oris is developed to a unique extent in human lips and is closely associated with speech and the production of some kinds of musical tone. In each quadrant the pars marginalis consists of a single (occasionally double) band of narrow diameter muscle fibres lodged within the tissues of each vermilion zone. At their medial end, the marginal fibres meet and interlace with their contralateral fellows and then attach to the dermis of the vermilion zone a few millimetres beyond the median plane in a manner similar to pars peripheralis. At their lateral ends, the fibres converge and attach to the deepest part of the modiolar base along a horizontal strip level with the buccal angle.
The relations between pars marginalis and pars peripheralis are complex. In a full thickness section of an upper lip at right angles to the vermilion zone, the cylindrical bundles of peripheralis fibres form an S-shape, with an external convexity above, and an internal convexity below: the classic analogy is to the shank and initial curved part of a hook. Beyond peripheralis, the hook-shape is completed by the blunted triangular profile of marginalis, which occupies the core of the vermilion zone with its base adjacent to peripheralis and its apex reaching upwards and anteriorly towards the junction between vermilion zone and skin. In a similar section through the lower lip, peripheralis bundles form a continuous curve that is concave towards the external surface. This is surmounted by the flattened triangular profile of marginalis, which curves anteriorly, its apex again nearing the vermilion/cutaneous junction. Thus, throughout the vermilion zones of both lips, marginalis lies substantially anterior to the adjacent bundles of peripheralis. However, as the muscles are traced laterally beyond the vermilion zone and across the buccal angle, this relationship alters and marginalis becomes inverted as it wraps progressively around the adjacent edge of peripheralis to reach its deep (submucosal) surface, and maintains this position up to its attachment at the modiolar base.
Orbicularis oris is supplied mainly by the superior and inferior labial branches of the facial artery, the mental and infraorbital branches of the maxillary artery and the transverse facial branch of the superficial temporal artery.
Incisivus labii superioris
Incisivus labii superioris has a bony origin from the floor of the incisive fossa of the maxilla above the eminence of the lateral incisor tooth. Initially it lies deep to orbicularis oris pars peripheralis superior. Arching laterally, its fibre bundles become intercalated between, and parallel to, the orbicular bundles. Approaching the modiolus, it segregates into superficial and deep parts: the former blends partially with levator anguli oris and attaches to the body and apex of the modiolus and the latter is attached to the superior cornu and base of the modiolus.
Incisivus labii inferioris
Incisivus labii inferioris, an accessory muscle of the orbicularis oris muscle complex, has many features in common with incisivus labii superioris. Its osseous attachment is to the floor of the incisive fossa of the mandible, lateral to mentalis and below the eminence of the lateral incisor tooth. Curving laterally and upwards, it blends to some extent with orbicularis oris pars peripheralis inferior before reaching the modiolus, where superficial bundles attach to the apex and body, and deep bundles attach to the base and inferior cornu.
Platysma
Platysma is described as a muscle of the neck (see Ch. 28) but it is considered here as a contributor to the orbicularis oris muscle complex. It has mandibular, labial and modiolar parts. Pars mandibularis attaches to the lower border of the body of the mandible. Posterior to this attachment, a substantial flattened bundle separates and passes superomedially to the lateral border of depressor anguli oris, where a few fibres join this muscle. The remainder continue deep to depressor anguli oris and reappear at its medial border. Here they continue within the tissue of the lateral half of the lower lip, as a direct labial tractor, platysma pars labialis. Pars labialis occupies the interval between depressor anguli oris and depressor labii inferioris and is in the same plane as these muscles. The adjacent margins of all three muscles blend and they have similar labial attachments. Platysma pars modiolaris constitutes all the remaining bundles posterior to pars labialis, other than a few fine fascicles that end directly in buccal dermis or submucosa. Pars modiolaris is posterolateral to depressor anguli oris and passes superomedially, deep to risorius, to apical and subapical modiolar attachments.
Risorius
Risorius is a highly variable muscle that ranges from one or more slender fascicles to a wide, thin superficial fan. Its peripheral attachments may include some or all of the following: the zygomatic arch, parotid fascia, fascia over the masseter anterior to the parotid, fascia enclosing platysma pars modiolaris, and fascia over the mastoid process. Its fibres converge to apical and subapical attachments at the modiolus.
MOVEMENTS OF THE FACE AND LIPS
Direct labial tractors
Direct labial tractors, as their name suggests, pass directly into the tissues of the lips and not via the modioli. In broad terms, the force exerted by tractors is directed vertically at an approximate right angle to the oral fissure. Their action will therefore elevate and/or evert the whole, or part, of the upper lip and depress and/or evert the whole, or part, of the lower lip. The tractors are, from medial to lateral, the labial part of levator labii superioris alaequae nasi; levator labii superioris and zygomaticus minor in the upper lip; depressor labii inferioris and platysma pars labialis in the lower lip.
In both upper and lower lips the tractors blend into a continuous sheet that divides into a series of superimposed coronal sheets which are anterior to the muscle bundles of pars peripheralis orbicularis oris as they enter the free lip. The sheets may be divided into three groups at increasing depths from the skin surface, each with a distinct zone of attachment (Fig. 29.12). The superficial group comprises a succession of fine fibre bundles which curve anteriorly a short distance before attaching in a series of horizontal rows to the dermis between the hair follicles, sebaceous glands and sweat glands. The intermediate group attaches to the dermis of the vermilion zone, which they reach by two routes: the more superficial bundles continue past the skin/vermilion junction, then curve posteriorly over pars marginalis orbicularis oris to punctate attachments on the ventral half of the dermis of the vermilion zone, while the deeper bundles first pass posteriorly between pars peripheralis and pars marginalis, then curve anteriorly to punctate attachments on the dorsal half of the dermis of the vermilion zone. The deep group is closely applied to the anterior surface of pars peripheralis orbicularis oris, and sends fine tractor fibres between its parallel bundles to attach posteriorly into the submucosa and periglandular connective tissue.
Movements of the lips
The various groups of direct labial tractors may act together or individually, and their effects may involve a complete labial quadrant, or be restricted to a short segment. For example, partial contraction of the superior labial tractors can result in localized elevation of a segment of the upper lip, in a postural expression reminiscent of the ‘canine snarl’. Normally, however, the activity of the tractors is modified by the superimposed activity of orbicularis oris and the modiolar muscles. The resultant actions range from delicate adjustments of the tension and profile of the lip margins to large increases of the oral fissure with eversion of the lips.
Lip protrusion is passive in its initial stages. It may be suppressed by powerful contraction of the whole of orbicularis oris or enhanced by selective activation of parts of the direct labial tractors. However, lip movements must accommodate separation of the teeth brought about by mandibular depression at the temporomandibular joints. Beyond a certain range of mouth opening, labial movements are almost completely dominated by mandibular movements. Thus over the last 2.5–3 cm interincisal distance of wide jaw separation, strong contraction of orbicularis oris cannot effect lip contact, and instead it causes full-thickness inflection of upper and lower lips, including the vermilion zone, towards the oral cavity, wrapping them around the incisal edges, canine cusps and premolar occlusal surfaces. The involvement of the lips in speech is described in Chapter 34, but some aspects relevant to the actions of orbicularis oris pars marginalis will be described here. Contraction of marginalis is considered to alter the cross-sectional profile of the free margin of the vermilion zone such that both the gentle bulbous profile of the upper lip and the smooth posterosuperior convexity of the lower lip change to a narrow, symmetrical triangular profile. The transformed rims, whose length and tension can be delicately controlled, have been named labial cords. They are known to be involved in the production of some consonantal (labial) sounds. A labial cord may also function as a ‘vibrating reed’ in whistling or playing a wind instrument such as the trumpet.
The modiolus and its role in facial movements
On each side of the face a number of muscles converge towards a focus just lateral to the buccal angle, where they interlace to form a dense, compact, mobile, fibromuscular mass called the modiolus. This can be palpated most effectively by using the opposed thumb and index finger to compress the mucosa and skin simultaneously. At least nine muscles, depending on the classification employed, are attached to each modiolus. Moreover, the muscles lie in different planes, their modiolar stems are often spiralized, and most divide into two bundles, some into three or four, each of them interlacing and attaching in a distinctive way. Not surprisingly, therefore, the three-dimensional organization of the modiolus has proved difficult to analyse.
The shape and dimensions of the modiolus are given approximately because they are subject to individual, age, sexual and ethnic variation. Furthermore the modiolus has no precise histological boundaries, and is an irregular zone where dense, compact interlacing tissue grades into the stems of individually recognizable muscles. The modiolus has the rough form of a blunt cone. The base of the cone (basis moduli) is adjacent and adherent to the mucosa. It is roughly elliptical in outline and extends vertically 20 mm above and 20 mm below a horizontal line through the buccal angle. It also extends laterally a similar distance from the angle. The blunt apex of the cone (apex moduli) is 4 mm across, and is centred approximately 12 mm lateral to the buccal angle. From mucosa to dermis the thickness of the mass is usually 10 mm, divided approximately equally into basal, central and apical parts. The central body has an oblique fibrous cleft or channel that transmits the facial artery, an arrangement that may limit the extent to which it is compressed by contraction of the buccolabial musculature. The cone shape is modified by two round-edged flanges (or cornua) that extend into the lateral free lip tissues above and below the corner of the mouth. The tip of the superior cornu extends 5.5 mm medial to the buccal angle, the tip of the inferior cornu only 3.5 mm. With these additions, the modiolar base becomes kidney-shaped, with the buccal angle projecting towards the hilum.
The apex of the modiolus is deep and adherent to the panniculus carnosus, which extends posteromedially as a thin sloping sheet down to the buccal angle. There, its free border forms a crescentic, narrow, flexible, subcutaneous fibroelastic cord that accommodates the varying postures of the modioli, lips, mouth and jaws.
Controlled three-dimensional mobility of the modioli enables them to integrate the activities of the cheeks, lips and oral fissure, the oral vestibule and the jaws. Such activities include biting, chewing, drinking, sucking, swallowing, changes in vestibular contents and pressure, the innumerable subtle variations involved in speech, the modulation (and occasional generation) of musical tones, production of harsher sounds in shouting and screaming, crying, and all the permutations of facial expression, ranging from mere hints to gross distortion, symmetrical or asymmetrical. Major modiolar movements appear to involve many, if not all, of its associated muscles, and there is little value in considering the actions of the individual muscles in isolation. While the most obvious determinant of modiolar position and mobility is the balance between the forces exerted by muscles that are directly attached to it, another influential factor is the degree of separation or ‘gape’ between the upper and lower teeth. Starting from the occlusal position, and with the lips maintained in contact, the teeth can be separated by approximately 1.25 cm near the midline, and the mentolabial sulcus descends by a similar distance. With further separation the lips part, and as gape increases to its maximum, interlabial and interdental distances approach 4 cm, at which point the mentolabial sulcus has descended a further 2 cm. In this posture the modiolus has descended about 1 cm to lie over the interdental space, into which its basal and surrounding buccal mucosa projects a few millimetres, and its cornua diverge into their respective lips at an obtuse angle to each other, the dispositions of the modiolar muscles being correspondingly modified. The general hexagonal shape of the labial area changes as the mouth and jaws open progressively. In maximal opening, the distance between the superior and inferior boundaries has increased by 3–3.5 cm at the centre; the transverse distance between its lateral angles has decreased by 1 cm and the angles are obtuse; the nasolabial sulci are longer, straighter and more vertical; and the inferior buccolabial sulci are less deep and curved. These soft tissue changes radiate from the bilateral modioli.
With the lips in contact and the teeth in tight occlusion, the modiolus can move a few millimetres in all directions. However, mobility is maximal when there is 2–3 mm clearance between the teeth: the apex of the modiolus may then move vertically upwards 10 mm, downwards 5 mm, posterolaterally 10 mm, and anteromedially 10 mm, these movements occurring in the curved planes of the cheek and lips. Specific movements of the modiolus may occur to any point, and along any path, within the boundaries of the envelope of movement thus defined. When the mouth is opened wide, the modiolus becomes immobile. From the neutral position the modiolus may be displaced superficially along its apicobasal axis for up to 5–10 mm by liquids or solids in the vestibule, or by an increase in air pressure that ‘balloons’ the cheeks and lips.
Many activities take place in three phases. Initially, a particular modiolar muscle group becomes dominant over its antagonists and the modiolus is rapidly relocated. Next, the modiolus is transiently fixed in this new site by simultaneous contraction of modiolar muscles, principally zygomaticus major, levator anguli oris, depressor anguli oris, platysma pars modiolaris, and this provides a fixed base from which the main physiological effectors, buccinator and orbicularis oris, carry out their specific actions. These actions are usually integrated with partial separation or closure of the jaws, and with varying degrees of activity in the direct labial tractors. All these factors combine to determine the positions of the lips and oral fissure from moment to moment. Modiolar movements may be bilaterally symmetrical, unilateral or asymmetrical.
MUSCLES OF MASTICATION
Masseter and temporalis, two of the muscles of mastication, are seen on the face. Masseter covers the ramus of the mandible, and temporalis lies over the temporal fossa. These muscles are described in detail with the other main muscles of mastication in Chapter 31.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
ARTERIAL SUPPLY TO THE FACE
The main arterial supply to the face is derived from the facial and superficial temporal arteries, with additional supply from branches of the maxillary and ophthalmic arteries. The back of the scalp is supplied by the posterior auricular and occipital arteries. There are numerous anastomoses between the branches.
Facial artery
The facial artery arises in the neck from the external carotid artery (see Ch. 28). It initially lies beneath platysma, passing onto the face at the anteroinferior border of masseter, where its pulse can be felt as it crosses the mandible. The artery is deep to skin, the fat of the cheek and, near the angle of the mouth, zygomaticus major and risorius, and superficial to buccinator and levator anguli oris. It may pass over or through levator labii superioris, and pursues a tortuous course along the side of the nose towards the medial corner of the eye. At its termination it is embedded in levator labii superioris alaequae nasi.
Occasionally, the facial artery barely extends beyond the angle of the mouth, in which case its normal territory beyond this region is taken over by an enlarged transverse facial branch from the superficial temporal artery and by branches from the contralateral facial artery. The facial vein is posterior to the artery, and runs a more direct course across the face. At the anterior border of masseter, the two vessels are in contact, whereas in the neck the vein is superficial to the artery.
The facial artery supplies branches to the muscles and skin of the face (Fig. 29.13). Its named branches on the face are the premasseteric artery, the superior and inferior labial arteries and the lateral nasal artery. The part of the artery distal to its terminal branch is called the angular artery.
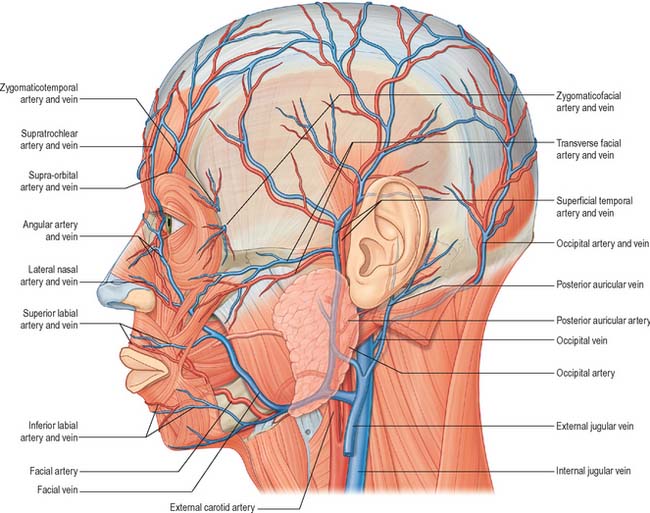
Fig. 29.13 The arteries and veins of the left side of the face, head and neck and their main branches. The infraorbital artery is shown in Fig. 25.1.
The premasseteric artery is small and inconstant. When present, it passes upwards along the anterior border of masseter and supplies the surrounding tissues.
The inferior labial artery arises near the angle of the mouth, passes upwards and forwards under depressor anguli oris, then penetrates orbicularis oris to run sinuously near the margin of the lower lip, between the muscle and the mucous membrane. It supplies the inferior labial glands, mucous membrane and muscles, and anastomoses with its contralateral fellow and with the mental branch of the inferior alveolar artery.
The superior labial artery is larger and more tortuous than the inferior labial artery. It pursues a similar course along the superior labial margin, between the mucous membrane and orbicularis oris, anastomoses with its contralateral fellow, and supplies the upper lip. It gives off an alar branch and a septal branch, which ramifies anteroinferiorly in the nasal septum.
Superficial temporal artery
The superficial temporal artery is the smaller terminal branch of the external carotid artery. It arises in the parotid gland behind the neck of the mandible, where it is crossed by temporal and zygomatic branches of the facial nerve. Initially deep, it becomes superficial as it passes over the posterior root of the zygomatic process of the temporal bone, where its pulse can be felt. It then runs up the scalp for approximately 4 cm and divides into frontal (anterior) and parietal (posterior) branches. The artery is accompanied by corresponding veins, and by the auriculotemporal nerve which lies just posterior to it.
The superficial temporal artery supplies the skin and muscles at the side of the face and in the scalp, the parotid gland and the temporomandibular joint. It is occasionally biopsied when a histological diagnosis of giant cell arteritis is required. The named branches of the superficial temporal artery are the transverse facial, auricular, zygomatico-orbital, middle temporal, frontal and parietal arteries. The relative sizes of the frontal, parietal and transverse facial branches vary; the frontal and parietal branches may be absent, and the transverse facial may replace a shortened transverse facial artery.
The transverse facial artery arises before the superficial temporal artery emerges from the parotid gland. It traverses the gland, crosses masseter between the parotid duct and the zygomatic arch (accompanied by one or two facial nerve branches) and divides into numerous branches that supply the parotid gland and duct, masseter and adjacent skin. The branches anastomose with the facial, masseteric, buccal, lacrimal and infraorbital arteries, and may have a direct origin from the external carotid artery.
The branches of the auricular artery are distributed to the lobule and lateral surface of the auricle and to the external acoustic meatus.
The zygomatico-orbital artery may arise independently from the superficial temporal artery or from its middle temporal or parietal branches. It runs close to the upper border of the zygomatic arch, between the two layers of temporal fascia, to the lateral orbital angle. It supplies orbicularis oculi and anastomoses with the lacrimal and palpebral branches of the ophthalmic artery. A well-developed zygomatico-orbital artery is associated with a delayed division into frontal and parietal branches.
The middle temporal artery arises just above the zygomatic arch and perforates the temporal fascia to supply temporalis. It anastomoses with the deep temporal branches of the maxillary artery.
Facial branches of the maxillary artery
The maxillary artery is the larger of the two terminal branches of the external carotid artery, and has three branches that supply the face, namely the mental, buccal and infraorbital arteries.
The mental artery arises from the first part of the maxillary artery as a terminal branch of the inferior alveolar artery. It emerges onto the face from the mandibular canal at the mental foramen, supplies muscles and skin in the chin region, and anastomoses with the inferior labial and submental arteries.
The buccal artery is a branch of the second part of the maxillary artery. It emerges onto the face from the infratemporal fossa, crosses buccinator to supply the cheek, and anastomoses with the infraorbital artery and with branches of the facial artery.
The infraorbital artery arises from the third part of the maxillary artery. It runs through the infraorbital foramen and onto the face, supplying the lower eyelid, the lateral aspect of the nose and the upper lip. The infraorbital artery has extensive anastomoses with the transverse facial and buccal arteries and with branches of the ophthalmic and facial arteries.
Facial branches of the ophthalmic artery
The ophthalmic artery is a branch of the internal carotid artery. Its supratrochlear, supraorbital, lacrimal, medial palpebral, dorsal nasal and external nasal branches supply the face.
The supratrochlear artery emerges from the orbit onto the face at the frontal notch. It supplies the medial parts of the upper eyelid, forehead and scalp, and anastomoses with the supraorbital artery and with its contralateral fellow.
The supraorbital artery leaves the orbit through the supraorbital notch or foramen. It divides into superficial and deep branches that supply the skin and muscle of the upper eyelid, forehead and scalp. It anastomoses with the supratrochlear artery, frontal branch of the superficial temporal and its contralateral fellow. At the supraorbital margin it often sends a branch to the diploë of the frontal bone and may also supply the mucoperiosteum in the frontal sinus.
The lacrimal artery appears on the face at the upper lateral corner of the orbit and supplies the lateral part of the eyelids. Within the orbit, it gives off a zygomatic artery which subdivides into zygomaticofacial and zygomaticotemporal arteries. The zygomaticofacial artery passes through the lateral wall of the orbit to emerge onto the face at the zygomaticofacial foramen, and supplies the region overlying the prominence of the cheek. The zygomaticotemporal artery also passes through the lateral wall of the orbit, via the zygomaticotemporal foramen, and supplies the skin over the non-beard part of the temple. The lacrimal artery anastomoses with the deep temporal branch of the maxillary artery and the transverse facial branch of the superficial temporal artery.
Superior and inferior medial palpebral arteries arise from the ophthalmic artery below the trochlea. They descend behind the nasolacrimal sac to enter the eyelids where each divides into two branches that course laterally along the edges of the tarsal plates, forming the superior and inferior arches and supplying the eyelids. They anastomose with branches of the supraorbital, zygomatico-orbital and lacrimal arteries. The inferior arch also anastomoses with the facial artery.
Occipital artery
The occipital artery arises in the neck from the external carotid artery (see Ch. 28). It runs in a groove on the temporal bone, medial to the mastoid process. Accompanied by the greater occipital nerve, the occipital artery enters the back of the scalp by piercing the investing layer of deep cervical fascia that connects the cranial attachments of trapezius and sternocleidomastoid. Tortuous branches run between the skin and the occipital belly of occipitofrontalis, anastomosing with the opposite occipital, posterior auricular and superficial temporal arteries as well as with the transverse cervical branch of the subclavian artery. These branches supply the occipital belly of occipitofrontalis and the skin and pericranium associated with the scalp as far forward as the vertex. The artery may give off a meningeal branch which traverses the parietal foramen.
Posterior auricular artery
The posterior auricular artery arises in the neck from the external carotid artery, and ascends between the auricle and mastoid process. It supplies the cranial surface of the auricle via its auricular branch, and the occipital belly of occipitofrontalis and the scalp behind and above the auricle via its occipital branch. The posterior auricular artery anastomoses with the occipital artery.
VEINS OF THE FACE
The veins of the face are subject to considerable variations: the following description concerns those that are relatively constant (Fig. 29.13).
Supratrochlear vein
The supratrochlear vein starts on the forehead from a venous network connected to the frontal tributaries of the superficial temporal vein. Veins from this network form a single trunk that descends to the bridge of the nose, near the midline and parallel with its contralateral fellow. The veins are joined by a nasal arch across the nose. They then diverge, each joining a supraorbital vein to form the facial vein near the medial canthus of the eye.
Supraorbital vein
The supraorbital vein begins near the zygomatic process of the frontal bone, connecting with branches of the superficial and middle temporal veins. It passes medially above the orbital opening, pierces orbicularis oculi and unites with the supratrochlear vein near the medial canthus of the eye to form the facial vein. A branch passes through the supraorbital notch, where it receives veins from the frontal sinus and frontal diploë, and subsequently connects with the superior ophthalmic vein.
Facial vein
The facial vein is the main vein of the face. After receiving the supratrochlear and supraorbital veins, it travels obliquely downwards by the side of the nose, passes under zygomaticus major, risorius and platysma, descends to the anterior border and then passes over the surface of masseter. It crosses the body of the mandible, and runs down in the neck to drain into the internal jugular vein. The facial vein initially lies behind the more tortuous facial artery, but crosses the artery at the lower border of the mandible. The uppermost segment of the facial vein, above its junction with the superior labial vein, is also called the angular vein: any infection of the mouth or face can spread via the angular veins to the cavernous sinuses resulting in thrombosis (see Ch. 27).
Near its origin, the facial vein connects with the superior ophthalmic vein, both directly and via the supraorbital vein, and so is linked to the cavernous sinus. The facial vein receives tributaries from the side of the nose and, below this, an important deep facial vein from the pterygoid venous plexus. It also receives the inferior palpebral, superior and inferior labial, buccinator, parotid and masseteric veins, and other tributaries which join it below the mandible.
Superficial temporal vein
A widespread venous network across the scalp receives branches from the supratrochlear, supraorbital, posterior auricular and occipital veins. Anterior and posterior tributaries from this network unite above the zygomatic arch to form the superficial temporal vein on each side. The vein accompanies its artery, usually lying behind it, crosses the posterior root of the zygoma, and enters the parotid gland where it joins the maxillary vein to form the retromandibular vein.
The tributaries are the parotid veins, rami draining the temporomandibular joint, anterior auricular, transverse facial and middle temporal veins. The middle temporal vein receives the orbital vein (formed by the lateral palpebral veins), pierces the temporal fascia and then passes back between the layers of the fascia to join the superficial temporal vein just above the level of the zygomatic arch.
Buccal, mental and infraorbital veins
The buccal, mental and infraorbital veins drain the cheek and chin regions and pass into the pterygoid venous plexus.
Posterior auricular and occipital veins
The posterior auricular vein arises in a parieto-occipital network that also drains into tributaries of the occipital and superficial temporal veins. It descends behind the auricle to join the posterior division of the retromandibular vein in, or just below, the parotid gland, to form the external jugular vein. It receives a stylomastoid vein and tributaries from the cranial surface of the auricle, drains the region of the scalp behind the ear and drains into the external jugular vein. The occipital vein begins in a posterior network in the scalp, pierces the cranial attachment of trapezius, turns into the suboccipital triangle and joins the deep cervical and vertebral veins. It may be joined by a vein draining the diploë in the occipital bone and then passes to either the internal jugular, posterior auricular, deep cervical or vertebral veins. Emissary veins connect the occipital vein to the intracranial venous sinuses via the mastoid and parietal foramina and through the posterior condylar canal and occipital protuberances.
LYMPHATIC DRAINAGE OF THE FACE AND SCALP
Lymph vessels from the frontal region above the root of the nose drain to the submandibular nodes (Fig. 29.14; see Fig. 28.15). Vessels from the rest of the forehead, temporal region, upper half of the lateral auricular aspect and anterior wall of the external acoustic meatus drain to the superficial parotid nodes, which lie just anterior to the tragus, either on or deep to the parotid fascia. These nodes also drain lateral vessels from the eyelids and skin of the zygomatic region, and their efferent vessels pass to the upper deep cervical nodes. A strip of scalp above the auricle, the upper half of the cranial aspect and margin of the auricle, and the posterior wall of the external acoustic meatus all drain to the upper deep cervical and posterior auricular nodes. The posterior auricular nodes are superficial to the mastoid attachment of sternocleidomastoid and deep to auricularis posterior, and drain to the upper deep cervical nodes. The auricular lobule, floor of the external acoustic meatus and skin over the mandibular angle and lower parotid region all drain to the superficial cervical or upper deep cervical nodes. Superficial cervical nodes lie along the external jugular vein superficial to sternocleidomastoid. Some efferents pass round the anterior border of sternocleidomastoid to the upper deep cervical nodes, others follow the external jugular vein to the lower deep cervical nodes in the subclavian triangle.
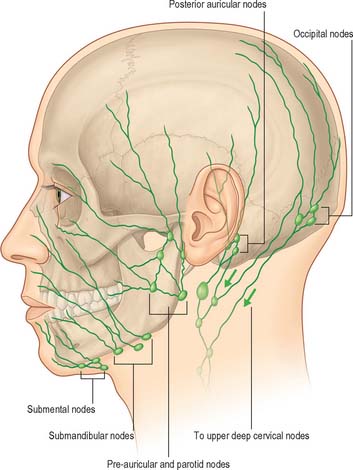
Fig. 29.14 The lymphatic drainage of the face and scalp. Arrows indicate direction of flow.
(From Drake, Vogl and Mitchell 2005.)
The occipital region of the scalp drains partly to the occipital nodes, and partly by a vessel that runs along the posterior border of sternocleidomastoid to the lower deep cervical nodes. Occipital nodes are commonly superficial to the upper attachment of trapezius, but occasionally lie in the superior angle of the posterior triangle.
There are usually three submandibular nodes, internal to the deep cervical fascia in the submandibular triangle. One lies at the anterior pole of the submandibular gland, and two flank the facial artery as it reaches the mandible. Other nodes are often embedded in the gland or deep to it. Submandibular nodes drain a wide area, including vessels from the submental, buccal and lingual groups of nodes, and their efferents pass to the upper and lower deep cervical nodes. The external nose, cheek, upper lip and lateral parts of the lower lip drain directly to the submandibular nodes; the afferent vessels may have a few buccal nodes along their course and near the facial vein. The mucous membrane of the lips and cheek drains to the submandibular nodes and the lateral part of the cheek drains to the parotid nodes. The central part of the lower lip, buccal floor and tip of the tongue all drain to the submental nodes which lie on mylohyoid between the anterior bellies of the digastric muscles. These nodes receive afferents bilaterally, some decussating across the chin; their efferents pass to the submandibular and jugulo-omohyoid nodes.
INNERVATION
The numerous muscles of facial expression are supplied by the facial nerve, while the two muscles of mastication that relate to the face are innervated by the mandibular division of the trigeminal nerve. The sensory innervation is primarily from the three divisions of the trigeminal nerve, with smaller contributions from the cervical spinal nerves. The detailed innervation of the auricle is considered on p. 620.
TRIGEMINAL NERVE
Three large areas of the face can be mapped out to indicate the peripheral nerve fields associated with the three divisions of the trigeminal nerve. The fields are not horizontal but curve upwards (Fig. 29.15), apparently because the facial skin moves upwards with growth of the brain and skull. Embryologically, each division of the trigeminal nerve is associated with a developing facial process which gives rise to a specific area of the adult face: the ophthalmic nerve is associated with the frontonasal process, the maxillary nerve with the maxillary process, and the mandibular nerve with the mandibular process.
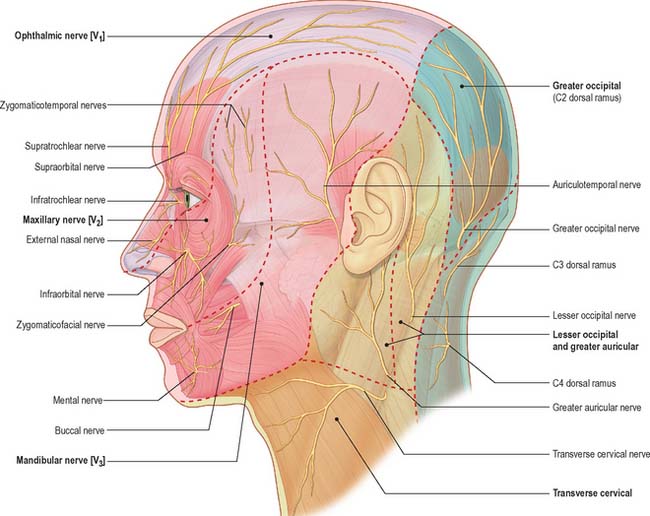
Fig. 29.15 Cutaneous innervation of the face and neck, showing dermatomes (in bold).
(Adapted from Drake, Vogl and Mitchell 2005.)
Ophthalmic nerve
The cutaneous branches of the ophthalmic nerve supply the conjunctiva, skin over the forehead, upper eyelid and much of the external surface of the nose.
Supratrochlear nerve
The supratrochlear nerve is the smaller terminal branch of the frontal nerve. It runs anteromedially in the roof of the orbit, passes above the trochlea, and supplies a descending filament to the infratrochlear branch of the nasociliary nerve. The nerve emerges between the trochlea and the supraorbital foramen at the frontal notch, curves up on the forehead close to the bone with the supratrochlear artery and supplies the conjunctiva and the skin of the upper eyelid. It then ascends beneath the corrugator and the frontal belly of occipitofrontalis before dividing into branches which pierce these muscles to supply the skin of the lower forehead near the midline.
Supraorbital nerve
The supraorbital nerve is the larger terminal branch of the frontal nerve. It traverses the supraorbital notch or foramen and supplies palpebral filaments to the upper eyelid and conjunctiva. It ascends on the forehead with the supraorbital artery, and divides into medial and lateral branches which supply the skin of the scalp nearly as far back as the lambdoid suture. These branches are at first deep to the frontal belly of occipitofrontalis. The medial branch perforates the muscle to reach the skin, while the lateral branch pierces the epicranial aponeurosis.
Lacrimal nerve
The lacrimal nerve is the smallest of the main ophthalmic branches and pierces the orbital septum to end in the lateral region of the upper eyelid, which it supplies. It anastomoses with filaments of the facial nerve. Occasionally it is absent, in which case it is replaced by the zygomaticotemporal nerve: the relationship is reciprocal, and when the zygomaticotemporal nerve is absent it is replaced by a branch of the lacrimal nerve.
Maxillary nerve
The maxillary nerve passes through the orbit to supply the skin of the lower eyelid, the prominence of the cheek, the alar part of the nose, part of the temple, and the upper lip. It has three cutaneous branches, the zygomaticotemporal, zygomaticofacial and infraorbital nerves.
Zygomaticotemporal nerve
The zygomaticotemporal nerve traverses a canal in the zygomatic bone and emerges into the anterior part of the temporal fossa, where it ascends between the bone and temporalis before piercing the temporal fascia about 2 cm above the zygomatic arch to supply the skin of the temple. It communicates with the facial and auriculotemporal nerves. As it pierces the deep layer of the temporal fascia it sends a slender twig between the two layers of the fascia towards the lateral angle of the eye: the branch carries parasympathetic postganglionic fibres from the pterygopalatine ganglion to the lacrimal gland.
Zygomaticofacial nerve
The zygomaticofacial nerve traverses the inferolateral angle of the orbit, and emerges on the face through a foramen in the zygomatic bone. It perforates orbicularis oculi to supply the skin on the prominence of the cheek and forms a plexus with zygomatic branches of the facial nerve and palpebral branches of the maxillary nerve. Occasionally the nerve is absent.
Infraorbital nerve
The infraorbital nerve emerges onto the face at the infraorbital foramen, where it lies between levator labii superioris and levator anguli oris. It gives off palpebral, nasal and superior labial branches. The palpebral branches ascend deep to orbicularis oculi, pierce the muscle to supply the skin in the lower eyelid and join with the facial and zygomaticofacial nerves near the lateral canthus. Nasal branches supply the skin of the side of the nose and of the movable part of the nasal septum, and join the external nasal branch of the anterior ethmoidal nerve. Superior labial branches, which are large and numerous, descend behind levator labii superioris to supply the skin of the anterior part of the cheek and upper lip. They are joined by branches from the facial nerve to form the infraorbital plexus. The infraorbital nerve is commonly implicated in trigeminal neuralgia, and is amenable to cryotherapy where medical therapy fails.
Mandibular nerve
The mandibular nerve supplies skin over the mandible, the lower lip, the fleshy part of the cheek, part of the auricle of the ear and part of the temple via the buccal, mental and auriculotemporal nerves.
Buccal nerve
The buccal nerve emerges onto the face from behind the ramus of the mandible and passes laterally in front of masseter to unite with the buccal branches of the facial nerve. It supplies the skin over the anterior part of buccinator.
Mental nerve
The mental nerve is the terminal branch of the inferior alveolar nerve (see Ch. 30). It enters the face through the mental foramen, where it is directed backwards, and supplies the skin of the lower lip and labial gingivae. Occasionally the mental nerve is important aetiologically in the pain of trigeminal neuralgia, and it is amenable to cryotherapy surgery.
Auriculotemporal nerve
The auriculotemporal nerve emerges onto the face behind the temporomandibular joint within the superior surface of the parotid gland. It ascends posterior to the superficial temporal vessels, passes over the posterior root of the zygoma, and divides into superficial temporal branches. The cutaneous branches of the auriculotemporal nerve supply the tragus and part of the adjoining auricle of the ear and the posterior part of the temple. The nerve may be damaged during parotid gland surgery resulting in impaired sensation of the tragus and temple. It communicates with the temporofacial division of the facial nerve, usually by two rami that pass anterolaterally behind the neck of the mandible. These communications anchor the facial nerve close to the lateral surface of the condylar process of the mandible, and limit its mobility during surgery. Communications with the temporal and zygomatic branches of the facial nerve loop around the transverse facial and superficial temporal vessels.
FACIAL NERVE
The facial nerve emerges from the base of the skull at the stylomastoid foramen and almost immediately gives off the nerves to the posterior belly of digastric and stylohyoid, and the posterior auricular nerve, which supplies the occipital belly of occipitofrontalis and some of the auricular muscles (Fig. 29.16A).
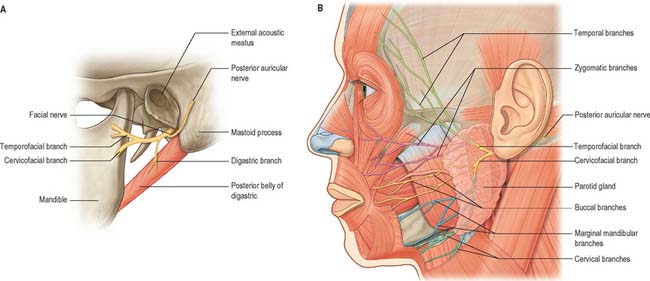
Fig. 29.16 Distribution of the facial nerve. A, The branches given off immediately after the nerve exits the stylomastoid foramen. B, The branches of the nerve on the face.
(From Drake, Vogl and Mitchell 2005.)
The nerve next enters the parotid gland high up on its posteromedial surface and passes forwards and downwards behind the mandibular ramus. Within the substance of the gland it branches into superior (temporofacial) and inferior (cervicofacial) trunks, usually just behind and superficial to the retromandibular vein. The trunks branch further to form a parotid plexus (pes anserinus). Five main terminal branches arise from the plexus, they diverge within the gland and leave by its anteromedial surface, medial to its anterior margin, to supply the muscles of facial expression (Fig. 29.16B). Six distinctive anastomotic patterns were originally classified by Davis et al (1956) and these are illustrated in Fig. 29.17. Numerous microdissection studies have demonstrated that branching patterns and anastomoses between branches, both within the parotid and on the face, exhibit considerable individual variation (e.g. Lineaweaver et al 1997; Kwak et al 2004): the account that follows is therefore an overview. In surgical terms these anastomoses are important, and presumably explain why accidental or deliberate division of a small branch often fails to result in the expected facial nerve weakness. The surface anatomy of the facial nerve is described in Chapter 25.
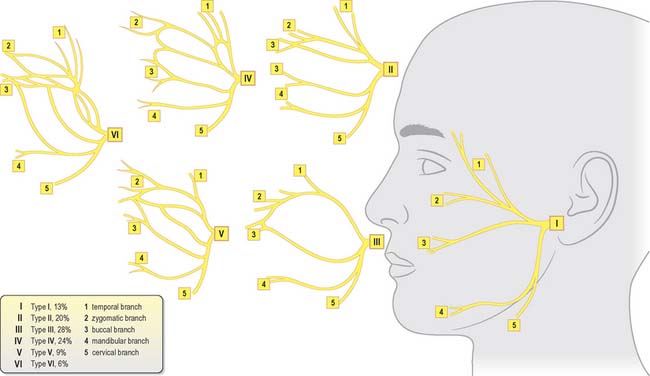
Fig. 29.17 Pattern of branching of the facial nerve.
(Modified with permission from Berkovitz BKB, Moxham BJ 2002 Head and Neck Anatomy. London: Martin Dunitz, and from Davis RA, Anson BJ, Budinger JM, Kurth IE 1956 Surgical anatomy of the facial nerve and parotid gland based upon a study of 350 cervicofacial halves. Surg Gynecol Obstet 102: 385–412, with permission from the American College of Surgeons.)
The temporal branch usually divides into anterior and posterior rami soon after piercing the parotidomasseteric fascia below the zygomatic arch; there is often a middle (frontal) ramus. These rami cross the arch in subcutaneous tissue and above the arch lie in the subgaleal space, where their course is extremely variable. Twigs supply intrinsic muscles on the lateral surface of the auricle, and the anterior and superior auricular muscles, and communicate with the zygomaticotemporal branch of the maxillary nerve and the auriculotemporal branch of the mandibular nerve. The more anterior branches supply the frontal belly of occipitofrontalis, orbicularis oculi and corrugator, and join the supraorbital and lacrimal branches of the ophthalmic nerve.
Zygomatic branches are generally multiple. They cross the zygomatic bone to the lateral canthus of the eye and supply orbicularis oculi: they may also supply muscles innervated by the buccal branch. Twigs communicate with filaments of the lacrimal nerve and the zygomaticofacial branch of the maxillary nerve.
The buccal branch is usually single. It has a close relationship to the parotid duct for about 2.5 cm after emerging from the parotid gland, and typically lies below the duct. Superficial branches run beneath the subcutaneous fat and superficial musculo-aponeurotic system (SMAS). Some branches pass deep to procerus and join the infratrochlear and external nasal nerves. Upper deep branches supply zygomaticus major and levator labii superioris, and form an infraorbital plexus with the superior labial branches of the infraorbital nerve. They also supply levator anguli oris, zygomaticus minor, levator labii superioris alaequae nasi and the small nasal muscles: these branches are sometimes described as lower zygomatic branches. Lower deep branches supply buccinator and orbicularis oris; they communicate with filaments of the buccal branch of the mandibular nerve.
There are usually two marginal mandibular branches. They run forwards towards the angle of the mandible under platysma, then turn upwards across the body of the mandible to pass under depressor anguli oris. The branches supply risorius and the muscles of the lower lip and chin, and filaments communicate with the mental nerve. The marginal mandibular branch has an important surgical relationship with the lower border of the mandible (see Ch. 25).
The cervical branch emerges from the lower part of the parotid gland and runs anteroinferiorly under platysma to the front of the neck. Typically single, it supplies platysma and communicates with the transverse cutaneous cervical nerve.
Cutaneous branches of the facial nerve accompany the auricular branch of the vagus; they are believed to innervate the skin on both auricular aspects, in the conchal depression and over its eminence.
Facial nerve lesions
Facial paralysis may be due to an upper motor neurone lesion (when frontalis is partially spared due to the bilateral innervation of the muscle of the upper part of the face), or a lower motor neurone lesion (when all branches may be involved). Ipsilateral lower motor neurone facial paralysis occurs in Bell’s palsy and Ramsay Hunt syndrome, and may be the consequence of an acoustic neuroma, a malignant parotid tumour or, more commonly, cheek laceration. Only those muscles innervated by degenerating or demyelinating branches of the facial nerve become weak.
The facial nerve is routinely isolated as part of a superficial parotidectomy operation – typically in the treatment of parotid tumours – when that part of the gland lying superficial to the plane of the facial nerve is removed. Although all branches of the facial nerve are preserved, there is often some postoperative facial weakness caused by bruising and ischaemia of the nerve which may result in temporary demyelination of the nerve fibres. Although this can affect all the branches of the facial nerve, the weakness is often confined to the territory innervated by the marginal mandibular branch and is manifested by a weakness of the lower lip on the affected side. This is because anastomotic arcades between the marginal mandibular branch and other branches of the facial nerve are relatively rare, whereas they are plentiful between the various branches of the temporofacial division and the buccal branch of the cervicofacial division of the facial nerve.
Cervical spinal nerves
Cervical spinal nerves have cutaneous branches which supply areas of skin in the face and scalp (Fig. 29.15). The named branches are the great auricular and lesser occipital nerves, which are part of the cervical plexus, and are described on page 435 (see Fig. 28.1) and the greater occipital nerve which is described on page 755 (see Fig. 42.52, Fig. 43.6).
PAROTID SALIVARY GLAND
The paired parotid glands are the largest of the salivary glands. Each has an average weight of 25 g and is an irregular, lobulated, yellowish mass, lying largely below the external acoustic meatus between the mandible and sternocleidomastoid. The gland also projects forwards onto the surface of masseter (Fig. 29.16B). In 20% of cases, a small, usually detached, part called the accessory parotid gland (pars accessoria or socia parotidis) lies between the zygomatic arch above and the parotid duct below. The overall shape of the parotid gland is variable. Viewed laterally, in 50% of cases it is roughly triangular in outline. However in 30% of cases the gland is more or less of even width throughout, and the upper and lower poles are rounded.
In its usual inverted pyramidal form, the parotid gland presents a small superior surface, and superficial, anteromedial and posteromedial surfaces. It tapers inferiorly to a blunt apex. The concave superior surface is related to the cartilaginous part of the external acoustic meatus and posterior aspect of the temporomandibular joint. Here the auriculotemporal nerve curves round the neck of the mandible, embedded in the capsule of the gland. The apex overlaps the posterior belly of digastric and the carotid triangle to a variable extent.
The superficial surface is covered by skin and superficial fascia, which contains the facial branches of the great auricular nerve, superficial parotid lymph nodes and the posterior border of platysma. It extends upwards to the zygomatic arch, backwards to overlap sternocleidomastoid, downwards to its apex posteroinferior to the mandibular angle, and forwards to lie on masseter below the parotid duct.
The anteromedial surface is grooved by the posterior border of the mandibular ramus. It covers the posteroinferior part of masseter, the lateral aspect of the temporomandibular joint and the adjoining part of the mandibular ramus. It passes forwards, medial to the ramus of the mandible, to reach medial pterygoid. The gland may therefore be subdivided into a larger superficial part and a smaller part, the deep ‘lobe’, deep to the ramus, the two being joined by an isthmus. Branches of the facial nerve emerge on the face from the anterior margin of this surface.
The posteromedial surface is moulded to the mastoid process, sternocleidomastoid, posterior belly of the digastric, and the styloid process and its associated muscles. The external carotid artery grooves this surface before entering the gland, and the internal carotid artery and internal jugular vein are separated from the gland by the styloid process and its associated muscles (Fig. 29.18). The anteromedial and posteromedial surfaces meet at a medial margin that may project so deeply that it contacts the lateral wall of the pharynx.
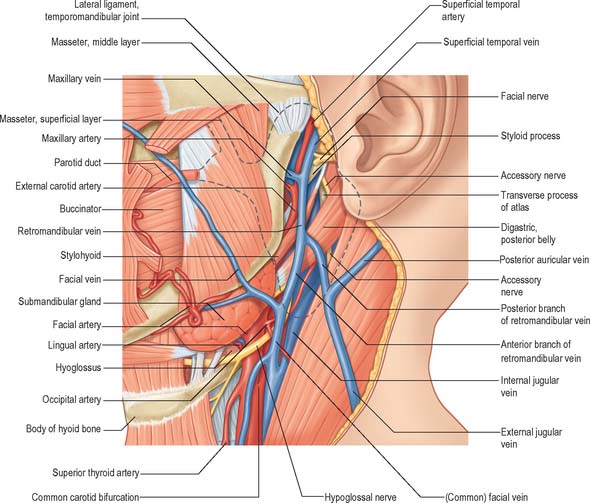
Fig. 29.18 The principal immediate deep relations of the parotid gland. The outline of the parotid gland is indicated by the interrupted black line.
The deep ‘lobe’ of the gland extends behind the mandibular ramus, where its deep surface lies immediately lateral to the superior constrictor of the pharynx. When a parotid tumour, either benign or malignant, occurs in the deep ‘lobe’, the mass presents as a swelling in the lateral wall of the pharynx and not as a facial swelling, which means that it is important to examine the oropharynx when following-up a patient who has undergone parotid surgery for the removal of a tumour.
STRUCTURES WITHIN THE PAROTID GLAND
The external carotid artery, retromandibular vein and facial nerve, either in part or in whole, traverse the gland and branch within it. The external carotid artery enters the posteromedial surface, and divides into the maxillary artery, which emerges from the anteromedial surface, and the superficial temporal artery, which gives off its transverse facial branch in the gland and ascends to leave its upper limit (Fig. 29.16). The posterior auricular artery may also branch from the external carotid artery within the gland, leaving by its posteromedial surface.
The retromandibular vein, formed by the union of the maxillary and superficial temporal veins (which enter near the points of exit of the corresponding arteries), is superficial to the external carotid artery. It descends in the parotid gland and emerges behind the apex of the gland, where it usually divides into an anterior branch, which passes forwards to join the facial vein, and a posterior branch, which joins the posterior auricular vein to form the external jugular vein. Occasionally it is not connected to the external jugular vein, which is then small, and the anterior jugular vein is enlarged.
PAROTID CAPSULE
The parotid gland is enclosed within an unyielding parotid capsule derived from the investing layer of deep cervical fascia. Acute inflammation of the parotid gland (acute sialadenitis) may cause exquisite pain in the preauricular region as a result of stretching of the capsule and stimulation of the great auricular nerve. The pain is usually exacerbated at mealtimes when the gustatory stimulus to the gland results in further turgor within the capsule. Causes of acute sialadenitis include parotid duct obstruction (calculus, mucus plug and duct stricture) and mumps.
PAROTID DUCT
The average dimensions of the parotid duct are 5 cm long and 3 mm wide (although it is narrower at its oral orifice). It begins by the confluence of two main tributaries within the anterior part of the parotid gland: the duct appears at the anterior border of the upper part of the gland and passes horizontally across masseter, approximately midway between the angle of the mouth and the zygomatic arch (Fig. 29.16). If the duct arises lower down, it may run obliquely upwards. It crosses masseter, turns medially at its anterior border at almost a right angle, and traverses the buccal fat pad and buccinator opposite the crown of the upper third molar tooth. The duct then runs obliquely forwards for a short distance between buccinator and the oral mucosa before it opens upon a small papilla opposite the second upper molar crown. The submucosal passage of the duct serves as a valvular mechanism preventing inflation of the gland with raised intraoral pressures. While crossing masseter, the duct lies between the upper and lower buccal branches of the facial nerve, and may receive the accessory parotid duct.
The accessory part of the gland and the transverse facial artery lie above the parotid duct; the buccal branch of the mandibular nerve, emerging from beneath temporalis and masseter, lies just below, at the anterior border of masseter. The parotid duct may be crossed by anastomosing branches between the zygomatic and buccal branches of the facial nerve.
The ramifications of the ductal systems, and their patterns and calibres, can be demonstrated radiographically by injecting a radio-opaque substance into the parotid duct via a cannula. In a lateral parotid sialogram the main duct can be seen to be formed near the centre of the posterior border of the mandibular ramus by the union of two or three ducts which ascend or descend respectively at right angles to the main duct. As it crosses the face, the main duct also receives from above five or six ductules from the accessory parotid gland (Fig. 29.19). As it curves round the anterior border of masseter it is often compressed and its shadow is attenuated. Deep lacerations of the cheek where the integrity of the parotid duct is in doubt should be explored and repaired using microsurgical techniques, to prevent saliva leaking into the soft tissues of the cheek and subsequent sialocele formation.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
The parotid gland receives its arterial supply from the external carotid artery and its branches within and near the gland. The veins drain to the external jugular vein via local tributaries.
Lymph nodes occur in the skin overlying the parotid gland (preauricular nodes) and in the substance of the gland. There are usually 10 lymph nodes present in the gland, the majority lie in the superficial part of the gland above the plane related to the facial nerve. Lymph from the parotid gland drains to the upper deep cervical lymph nodes.
INNERVATION
Preganglionic nerves travel in the lesser petrosal branch of the glossopharyngeal nerve and synapse in the otic ganglion. Postganglionic secretomotor fibres reach the gland via the auriculotemporal nerve.
Gustatory sweating (Frey’s syndrome or auriculotemporal syndrome)
Gustatory sweating (auriculotemporal syndrome) commonly occurs following parotid surgery or other surgery or trauma that results in opening of the parotid capsule. It is thought to reflect aberrant innervation of sweat glands on the face by regrowing parasympathetic secretomotor axons that would previously have innervated the parotid gland. Frey’s syndrome is characterized by sweating, warmth and redness of the face as a result of salivary stimulation by the smell or taste of food. The management of Frey’s syndrome is difficult. Denervation by tympanic neurectomy or auriculotemporal nerve avulsion have been advocated, but are often not curative. The symptoms can be managed by the subcutaneous infiltration of purified botulinum toxin into the affected area, and use of antiperspirant.
Borges AF, Alexander JE. Relaxed skin tension lines, Z-plasties on scars, and fusiform excision of lesions. Br J Plast Surg. 1962;15:242-254.
Davis RA, Anson BJ, Budinger JM, Kurth LE. Surgical anatomy of the facial nerve and parotid gland based upon a study of 350 cervicofacial halves. Surg Gynecol Obstet. 1956;102:385-412.
Fromer J. The human accessory parotid gland: its incidence, nature and significance. Oral Surg Oral Med Oral Pathol. 1977;43:671-676.
Gosain AK, Yousif NJ, Madiedo G, Larson DL, Matloub HS, Sanger JR. Surgical anatomy of the SMAS: a reinvestigation. Plast Reconstruct Surg. 1993;92:1254-1263.
Kwak HH, Park HD, Youn KH, Hu KS, Koh KS, Han SH, Kim HJ. Branching patterns of the facial nerve and its communication with the auriculotemporal nerve. Surg Radiol Anat. 2004;26:494-500.
Lineaweaver W, Rhoton A, Habal MB. Microsurgical anatomy of the facial nerve. Craniofac Surg. 1997;8:6-10.
Langdon JD. Parotid surgery. In: Langdon JD, Patel MF. Operative Maxillofacial Surgery. London: Chapman and Hall; 1998:381-390.
A detailed account of the procedures for the safe dissection of the intraparotid part of the facial nerve..
Markus AF, Delaire J, Smith WP. Facial balance in cleft lip and palate II. Cleft lip and palate and secondary deformities. Br J Oral Maxillofac Surg. 1992;30:296-304.
Discusses the anatomical basis for the repair of cleft lip and palate deformities..
Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstruct Surg. 1976;58:80-88.
Myint K, Azian AL, Khairul FA. The clinical significance of the branching pattern of the facial nerve in Malaysian subjects. Med J Malaysia. 1992;47:114-121.
de Norman JE, McGurk M. Color Atlas and Text of the Salivary Glands. London: Mosby-Wolfe, 1995.
Park IY, Lee ME. A morphological study of the parotid gland and the peripheral part of the facial nerve in Koreans. Yonsei Med J. 1977;18:45-51.
Shimada K, Gasser RF. Morphology of the mandibulo-stylohyoid ligament in human adults. Anat Rec. 1988;222:207-210.
Wassef M. Superficial fascial and muscular layers in the face and neck: a histological study. Aesth Plast Surg. 1987;11:171-176.
Yousif NJ, Mendelson BC. Anatomy of the midface. Clin Plast Surg. 1995;22:227-240.
Ziarah HA, Atkinson ME. The surgical anatomy of the mandibular distribution of the facial nerve. Br J Oral Surg. 1981;19:159-170.