8 Contemporary removable appliances
Removable appliances are not permanently attached to the teeth and can be taken out of the mouth by the patient. During the first half of the twentieth century, orthodontic practice in Europe was based largely on the use of removable appliances. However, over the past few decades there has been a significant decline in their use, primarily as a result of more efficient fixed appliances being available and an increase in numbers of orthodontic specialists able to use them. However, simple removable appliances retain a place in modern orthodontic practice, usually as an adjunct to fixed appliance therapy or for use in the retention phase of treatment. In particular, a group of predominantly removable functional appliances, used primarily in the management of class II malocclusion, have enjoyed a considerable resurgence in popularity in recent years. In addition, new treatment systems using vacuum-formed removable appliances, not only for retention, but also for active tooth movement have been developed.
Tooth movement with removable appliances
A variety of tooth movements can be achieved with removable appliances, either individually or on groups of teeth:
Removable appliances are also useful in maintaining tooth positions during retention.
Tipping
Unlike fixed appliances, which can control the movement of a tooth in three dimensions, the force applied by a removable appliance is mediated by a spring, elastic or piece of acrylic, which can only make point contact with the tooth. As no reactionary force or couple is created, in these situations removable appliances are only capable of simple tooth tipping and apical or bodily movement is not possible. Tipping can be carried out in mesial, distal, buccal or lingual directions, with the rotation occurring about a fulcrum located close to the middle of the tooth root. For the retraction of teeth already mesially inclined, tipping can be an effective tooth movement; but it is inappropriate for teeth that are upright or distally inclined (Fig. 8.1).
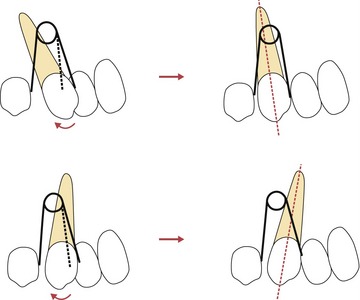
Figure 8.1 Tipping of a tooth with a removable appliance is appropriate if it needs uprighting but inappropriate if the tooth is already angulated in the direction of the intended movement. In this case a mesially angulated canine can be uprighted with an activated spring (upper panels), but this is inappropriate if the tooth is already distally angulated as this would lead to excessive tipping (lower panels).
Overbite reduction
Incorporating an anterior bite plane on a removable appliance will increase the vertical dimension and allow differential eruption of the posterior teeth, which in a growing patient is an effective way to reduce a deep overbite.
Anterior crossbite
If space is available, an anterior tooth in crossbite can be pushed over the bite using a removable appliance with an activated palatal spring or screw. Stability will depend upon achieving a positive overbite on the corrected teeth, to prevent them relapsing back into crossbite.
Posterior crossbites
By incorporating a midline expansion screw or spring in an upper removable appliance, the maxillary arch can be widened. This is effective for the correction of posterior crossbites in the mixed dentition, but will produce only tipping of the buccal teeth; the crossbite should therefore be dental not skeletal in origin.
Extrusion
A whip-spring or elastic from a removable appliance can be used to extrude teeth by engaging a fixed attachment on a tooth to generate a vertical component of force. This can be useful for extrusion of an impacted central incisor in the mixed dentition (see Fig. 10.22).
Intrusion
An elastic run underneath a fixed attachment or bracket via a removable appliance can be used to intrude teeth (Fig. 8.2). Good retention is required, as the reaction to any intrusive force will tend to unseat a poorly retained appliance.
Retention
Removable appliances are routinely used as retainers to maintain the position of teeth following active orthodontic treatment. There are numerous designs available, but the commonest are:
Retention is discussed in Chapter 11.
Components of removable appliances
Removable appliances are composed of retentive and active components connected together by a baseplate. When designing a removable appliance, consideration also needs to be given towards anchorage, ensuring that the desired teeth will move under the active force applied by the appliance (Box 8.1).
Box 8.1 Principles of removable appliance design
The starting point for the design of any removable orthodontic appliance is deciding upon the desired tooth movements and how these will be achieved by the active components. Once these points have been addressed, consideration must be given to retention, anchorage and connecting all the components together using the baseplate. Retention is the mechanism by which the appliance stays in the mouth and is provided by passive components such as clasps and labial bows. Good retention is important to ensure that the active components of the appliance are correctly placed and therefore effective. A retentive appliance is also easier for the patient to wear and therefore optimizes patient compliance.
Anchorage for a removable appliance is provided from either an intra- or extraoral source. Intraoral anchorage comes primarily from the palate and dentition of the same dental arch (intramaxillary); whilst extraoral anchorage is from headgear attached to the appliance. In certain circumstances anchorage is reciprocal when the planned tooth movements for active and reactive components are equal. However, the aim is often for specific teeth to be moved by the appliance, with others remaining stationary. To prevent undesirable tooth movement and anchorage loss, active forces should be kept light and reactionary forces reduced by limiting the number of teeth being moved at any one time. This may mean only activating one spring at a time or providing more than one appliance in order to achieve the treatment aims.
Retentive components
The retentive components of a removable appliance are concerned primarily with seating it in the correct position, but they can also contribute towards anchorage.
Adams clasp
Adams clasps are constructed in 0.7-mm stainless steel wire and most commonly used on the first molars (Fig. 8.3), although they can be used on premolars and anterior teeth. The arrowheads of the clasp engage undercuts at the mesial and distal corners of the buccal tooth surface and can easily be adjusted at the chairside to increase retention. The bridge of an Adams clasp can also be used by the patient to remove the appliance from the mouth, whilst the orthodontist can use it to attach auxiliary springs or tubes for headgear.
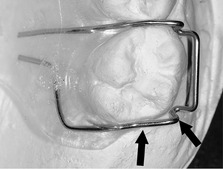
Southend clasp
The Southend clasp is also constructed in 0.7-mm stainless steel wire, but is used for retention on the incisor teeth (Fig. 8.4). This clasp is activated by bending the U-loop towards the baseplate, which carries the clasp back into the labial undercut of the tooth.
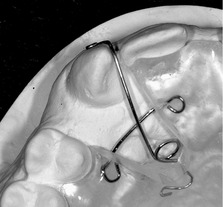
Ball-ended clasp
Ball-ended clasps engage into interproximal undercuts between the teeth (Fig. 8.5) and are activated by bending the ball towards the contact point.
Plint clasp
Plint clasps are useful when using a removable appliance in combination with a fixed appliance (Fig. 8.6). These clasps are constructed in 0.7-mm stainless steel and engage the undercuts on a maxillary molar band.
Labial bow
A labial bow is constructed from 0.7-mm stainless steel wire and can provide retention from the labial surface of the incisor teeth, which can be increased by contouring the wire around these teeth in a fitted labial bow or by placing an acrylic facing on the wire of the bow (Fig. 8.7). The labial bow is afforded flexibility by incorporating U-loops at each end, which allow activation by compression.
Active components
The active components of a removable appliance are responsible for producing the desired tooth movement. They can be categorized as springs, bows, screws and auxiliary elastics.
Springs
Mechanical principles should be considered when applying a force to any tooth with a spring:
The force (F) delivered by a spring is related to the length (L) and thickness or radius of the wire (R), as well as the deflection (D), such that
Therefore, lighter forces can be delivered by increasing the length of the wire or reducing its diameter; however, this will make the spring more susceptible to distortion and breakage. This can be prevented to a degree by shielding the arm of the spring with the acrylic baseplate or sheathing it in steel tubing. Springs are usually constructed in stainless steel, either 0.5-mm in diameter, which are activated approximately 3-mm; or 0.7-mm, which are activated by 1-mm to give a similar force.
Palatal finger springs
Palatal finger springs are constructed in 0.5- or 0.6-mm stainless steel wire and used to move teeth mesially or distally along the dental arch (Fig. 8.8). The incorporation of a helix increases the length of the wire and allows the delivery of lighter forces whilst a guard wire will protect the spring from distortion. By convention, the helix is placed such that activation of the spring is achieved as it is tightened and it unwinds as tooth movement occurs; the spring should be positioned at right angles to the planned tooth movement.
Buccal canine retractor
Buccal canine retractors are constructed in 0.7-mm stainless steel, reduced to 0.5-mm if sheathed (Fig. 8.9). These springs can be used to retract buccally placed maxillary canines; however, when activated it is mechanically difficult to apply force directly to the mesial surface of the tooth.
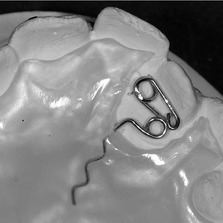
Z-spring
The Z-spring is constructed in 0.5-mm stainless steel wire and generally used to move one or two teeth labially (Fig. 8.10). Activation is achieved by pulling the spring away from the baseplate at an angle of approximately 45°, which will tend to displace the appliance away from the palate; good anterior retention is therefore important.
T-spring
T-springs are constructed in 0.5-mm stainless steel wire and used to move individual teeth either labially or buccally (Fig. 8.11). Activation is again produced by pulling the spring away from the baseplate and therefore retention also needs to be good.
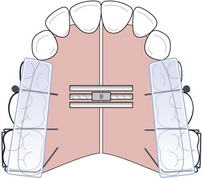
Coffin spring
A coffin spring provides a useful alternative to a screw for expansion (Fig. 8.12). This heavy spring is constructed in 1.25-mm wire and activated by pulling the two halves of the appliance apart manually or flattening the spring with pliers. Coffin springs deliver high forces that will tend to displace the appliance and good retention is important.
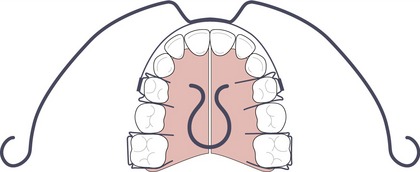
Active labial bows
An active labial bow can be used to reduce an increased overjet by tipping the teeth palatally if the upper labial segment is proclined and spaced. However, a normal labial bow will only allow a small range of activation and this can be improved either by increasing the amount of wire in the bow, as in a Mills bow, or by constructing it in a lighter wire, such as a Roberts retractor (Fig. 8.13). The Roberts retractor is constructed in 0.5-mm stainless steel with buccal arms sheathed in stainless steel tubing. Activation occurs by bending the vertical arms of the bow towards the palate and trimming the acrylic behind the upper incisors to allow palatal movement.
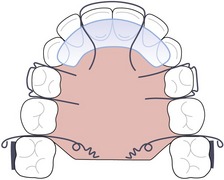
Screws
Screws can be embedded into the baseplate of an appliance and activated by the patient progressively turning a key (Fig. 8.14). Screws can be effective for expansion to correct a posterior dental crossbite, or for distal movement of the buccal segments, often supported by headgear. Each quarter turn of the screw activates it by approximately 0.2-mm and, therefore, should be done by the patient once or twice a week.
Elastics
Elastomeric forces can also be applied from a removable appliance and these can be useful in providing light force, which can be reactivated regularly by the patient. Intra-arch elastics can be used to retract the upper incisors as well as applying an intrusive force in patients with reduced periodontal support (see Fig. 8.2). Inter-arch application of elastics from removable appliances requires good retention to avoid displacement and is generally avoided.
Removable appliance design and use
Comprehensive orthodontic treatment is no longer undertaken with removable appliances alone because the results are invariably inferior to those produced by fixed appliances. However, removable appliances are relatively simple to use (Table 8.1), generally well tolerated by patients and can be used very effectively to correct minor occlusal problems (such as crossbites) in the mixed dentition or provide a valuable adjunct to fixed appliance therapy.
Table 8.1 Clinical use of removable appliances
Expansion
Removable appliances can provide an effective method for expanding the maxillary dental arch, particularly in the mixed dentition (Fig. 8.14):
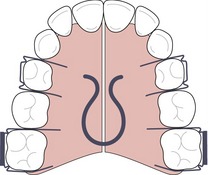
Correction of anterior crossbite
Removable appliances are also effective at correcting an anterior crossbite (Fig. 8.15). Palatal Z- or T-springs can be used to correct one or two teeth in anterior crossbite, usually in conjunction with posterior acrylic capping to open the bite and allow movement of the teeth out of crossbite. Occasionally some anterior retention in the form of a Southend clasp may also be required (Fig. 8.16).

Figure 8.16 Upper removable appliance to correct an anterior crossbite affecting the UR1 in the mixed dentition.
The design includes Adams cribs on the first permanent molars, ball-ended clasps between the deciduous molars, a modified Southend clasp on the UL1, a Z-spring for the UR1 and posterior acrylic capping.
Bite plane
In a growing patient, the incorporation of a flat anterior bite plane in a removable appliance allows eruption of the posterior teeth and reduction of a deep overbite (see Fig. 11.15). It can also facilitate earlier placement of a lower fixed appliance without impinging on the occlusion. An inclined bite plane can be useful following functional appliance therapy, either as part of a retainer or as an adjunct during the transition from fixed to functional appliances to help to maintain sagittal correction.
Distal movement of buccal segments
Removable appliances can be used in conjunction with headgear to produce distal movement of the maxillary buccal segments:
ELSAA
The expansion and labial segment alignment appliance (ELSAA) is used primarily to align and procline the upper labial segment in class II cases prior to functional appliance therapy. It is particularly useful for creating an overjet when the upper incisors are either upright or retroclined, which usually only takes a few months and then allows good posture of the mandible to be achieved with a functional appliance (Fig. 8.19).
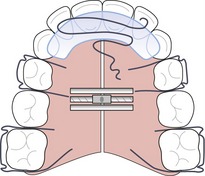
Figure 8.19 The ELSAA appliance to procline the upper incisors, expand the posterior dentition and reduce the overbite. The design includes Adams cribs on the first permanent molars and first premolars, a midline expansion screw, flat anterior bite plane and a re-curved palatal spring behind the upper incisors.
Functional appliances
Functional appliances are a group of largely removable appliances originally developed in Europe during the late nineteenth and early twentieth century. The majority are designed to correct class II malocclusion, primarily by forward posturing of the mandible in a growing child. The term functional jaw orthopoedics was coined for treatment with these types of appliances, which reflected the treatment philosophy underlying their use:
Whilst this premise is attractive in theory, the mechanism of action associated with functional appliances has remained a matter of some controversy and debate. However, regardless of exactly how they work, it is clear that in certain cases, these appliances can effect a tremendous change in the dental and skeletal relationships of a growing child in a relatively short period of time (Fig. 8.20).
Theories on how functional appliances work
Functional appliances eliminate a sagittal jaw discrepancy by posturing the mandible forward. This postural correction is fundamental to the appliances’ mode of action and influences four principle regions:
Orofacial soft tissues
The teeth sit between the tongue on one side and the lips and cheeks on the other. If the balance of these forces is altered, tooth movement can result. Simply correcting the sagittal jaw relationship with a functional appliance can often significantly improve the soft tissue environment surrounding the dentition, particularly in the presence of a lip trap. However, further alteration can also be achieved by incorporating screens or shields constructed in wire or acrylic as part of the appliance, which specifically hold the tongue or cheeks away from the teeth.
Muscles of mastication
Forward posturing of the mandible results in stretch and an alteration in activity of the muscles of mastication, particularly those involved in elevation and retraction of the mandible. These forces will be transmitted to the dentition via the appliance. Electromyographic studies have shown hyperactivity of the lateral pterygoid on protrusion of the mandible (McNamara, 1973). As this muscle is intimately related to the condyle it has been hypothesized that this activity could result in skeletal adaptation. However, some of these earlier studies used cutaneous electromyographic pads and later work using surgically implanted electrodes has shown a reduction in muscular activity on mandibular protrusion (Voudouris et al, 2003), indicating that the lateral pterygoid muscle may not be the primary factor in any skeletal remodelling of the condyle.
Dentition and occlusion
Forward posturing of the mandible also generates an intermaxillary force directed between the maxillary and mandibular dentitions. The class II component of this force can aid significantly with overjet reduction by simply tipping teeth. In addition, the altered mandibular position is also associated with a variable increase in the vertical dimension, which facilitates eruption of the buccal segments. This eruption can be controlled with the use of capping or faceting within the appliance; in particular, allowing eruption of the mandibular buccal teeth in a mesial direction and distal eruption of the maxillary buccal teeth, which aids in the correction of a class II buccal segment relationship and also in overbite reduction (Fig. 8.21).
Jaw skeleton
As a tissue, bone has the capacity to remodel when exposed to functional stimuli, which has been known since the nineteenth century. Sutural growth can be significantly influenced by the application of external force and there is some evidence that the class II force component placed upon the maxilla by a conventional functional appliance can apply some restraint upon forward maxillary growth, particularly when combined with headgear (Vargervik & Harvold, 1985; Wieslander, 1993).
How much effect a functional appliance can have upon growth of the mandible is more controversial. In a primary cartilaginous growth centre, such as the epiphysis of a long bone, growth occurs as a result of proliferation within columns of chrondrocytes and this is under genetic control. A secondary cartilage such as the mandibular condylar cartilage differs, in that stimulating the local functional environment can positively influence cell division and growth. Posturing the mandibular condyle forwards within the glenoid fossa using a functional appliance should therefore be capable of inducing skeletal change. How much change can be achieved with these appliances has been a subject of great debate within orthodontics for as long as functional appliances have been used. The boundaries of this intellectual spectrum depend upon the relative theories of how facial growth is controlled. If growth is primarily genetically determined, functional appliances will have little effect on the final size of the mandible. However, if one believes that facial growth is controlled by local factors, a functional appliance will change the local environment and exert a significant effect.
Biological effects of functional appliances
The biological effects of functional appliances and mandibular protrusion have been investigated using both animal models and clinical studies.
Animal studies
Various animal models have been used to investigate the effects of functional appliances, including both rodent and primate. Generally, these experiments involve placing fixed splints onto the dentition of these animals, which permanently advance the mandible. There is no doubt that this can produce an increase in proliferation of cells within the condylar cartilage and bony remodelling at the anterior border of the glenoid fossa, and these effects are greater in immature animals that are actively growing (Charlier et al, 1969; McNamara & Bryan, 1987; McNamara et al, 1982; Voudouris et al, 2003; Woodside et al, 1987). However, the applicability of these animal models to humans is somewhat debatable due to differences in morphology, physiology and duration of growth; in particular:
Clinical evidence
Until relatively recently the majority of clinical evidence associated with the use of functional appliances was obtained from retrospective studies, carried out on small sample groups with poorly matched controls. Cephalometric analysis of these subjects often reported skeletal change and growth as a result of appliance wear, but this was usually based upon cephalometric points difficult to identify and not necessarily representative of true skeletal or soft tissue facial change. This resulted in considerable bias and error; and as such, many of the conclusions of these studies must be viewed with caution (Tulloch et al, 1990).
In the past two decades, several large randomized controlled trials (RCTs) have investigated the effects of early treatment with functional appliances and compared them to untreated controls (Dolce et al, 2007; Ghafari et al, 1998; O’Brien et al, 2003; Tulloch et al, 2004). These trials represent the best current available evidence regarding the clinical use of functional appliances. Three of these studies were carried out in the USA and one in the UK and universally they have shown an initial small but significant increase in mandibular growth in patients undergoing treatment with a functional appliance. However, when these patients were followed through to the end of orthodontic treatment, no significant differences were found between those treated early with a functional appliance and those treated comprehensively later. Any initial growth-related benefits of using a functional appliance were lost in the longer term, a finding that had previously been suggested by retrospective investigations of early functional appliance treatment (Wieslander, 1984, 1993). These RCTs have also demonstrated no significant differences in extraction rates, experience of dentoalveolar trauma or improvements in self-esteem between groups treated with or without a functional appliance. The only significant difference is that the overall treatment time tends to be longer for patients who undergo early treatment with a functional appliance, followed by fixed appliances.
Clinical effects of functional appliances
Numerous types and designs of functional appliance have been described, each with its own treatment philosophy. In essence, all of these appliances have similar effects, with the most significant being dentoalveolar change:
Combined, these effects will result in the correction of a class II dental occlusion, an increase in lower face height and a clockwise rotation of the mandible. Regardless of how a functional appliance corrects a class II discrepancy, their efficiency at doing this can be extremely useful. Converting an occlusion with a class II buccal segment and incisor relationship into one that is class I makes subsequent occlusal detailing with a fixed appliance considerably easier to manage.
Types of functional appliance
There are many different designs of functional appliance, each usually bearing the name of the innovator. They are all designed to posture the mandible forward but they differ in the way this is achieved and how they influence the local soft tissue environment of the jaws and dentition.
Activators
Activators form a group of loosely fitting appliances that come in a single piece or monobloc. They posture the mandible forwards by lingual extension of the acrylic monobloc.
Andresen activator
The activator was originally described by Viggo Andresen and Karl Häupl and consisted of a loose-fitting monobloc appliance that advanced the mandible with lingual flanges (Fig. 8.22). Facets were cut into the acrylic to guide eruption of the mandibular posterior teeth mesially and the maxillary posterior teeth distally and buccally. The original Andresen–Häupl activator was worn at night and had minimal vertical opening. It was based upon the hypothesis of stimulating increased muscle activity in the mandibular elevator and retractor muscles to act directly on the dentition through the appliance and unload the condyle to allow remodeling and growth.
Woodside or Harvold activator
Later activators such as those described by Donald Woodside (Woodside, 1973) and Egil Harvold (Fig. 8.22) (Harvold & Vargervik, 1971) increased vertical opening beyond the freeway space because these workers believed that the masticatory musculature could not be stimulated during sleep. Therefore to be effective, the appliance had to stretch the orofacial connective tissues, including ligaments and fascial sheets, and direct forces to the teeth and supporting structures. To achieve this a vertical opening of greater than 10-mm was created on protrusion of the mandible, which makes the Woodside and Harvold-type activators more difficult to tolerate and can affect compliance.
Bionator
The Bionator was originally described by Wilhelm Balters and compared to the Andresen activator, the acrylic bulk was considerably reduced to allow increased wear and normal oral function (Fig. 8.23) (Eirew, 1981). A palatal coffin spring was incorporated into the appliance and designed to sit away from the palate, stimulating the tongue to adopt a more anterior position and helping to stabilize the Bionator in the oral cavity. Buccal wire shields were also incorporated to hold the cheeks away from the buccal segments and allow passive expansion of the dental arches.
Activators combined with headgear
Functional appliance wear can encourage a clockwise rotational effect on the dentition and dental bases, which can lead to an increase in the lower face height and greater vertical rather than sagittal change in chin position. To prevent this and optimize skeletal correction in the anteroposterior dimension, headgear can be attached to the appliance. The aim is to restrict anterior and vertical development of the maxilla, whilst encouraging forward mandibular growth.
A number of specific activator-type functional appliance systems which incorporate the use of headgear have been developed. The Teuscher appliance (Teuscher, 1978) (Fig. 8.24) has anterior spurs to torque the upper incisors and prevent their retroclination, allowing the headgear to exert a pull as far forward as possible and prevent the maxilla rotating downwards and backwards. The van Beek appliance (van Beek, 1982) is a modified activator with a headgear directly incorporated into the acrylic, which the patient wears at night and a few hours during the day. The Bass appliance is essentially a maxillary splint to which high-pull headgear is run to restrain maxillary growth, the mandible being guided anteriorly by pads that rest in the lingual sulcus behind the lower incisors (Bass, 1994). Although the logic of using headgear combined with a functional appliance makes some sense, particularly in the presence of skeletal maxillary excess or excessive incisor show in the vertical dimension (a so-called ‘gummy’ smile) (Orton et al, 1992), the potential benefits are often outweighed by the extra demand placed on compliance.
Medium opening activator (MOA)
The medium opening activator represents a cutback activator with cribs to the maxillary first molars and second premolars to improve retention and make the appliance more tolerable (Fig. 8.25). Mandibular protrusion is achieved via lingual mandibular guidance flanges, with an anterior hole cut into the acrylic to facilitate breathing and speech. The free eruption of mandibular buccal teeth is encouraged, which allows the reduction of a deep overbite at the same time as correcting the overjet.
Fränkel system
A series of removable functional appliances or functional regulators were developed by Rolf Fränkel in what was the German Democratic Republic (Fig. 8.26) (Fränkel, 1980). Fränkel was an advocate of the functional matrix theory of growth, which states that there is no direct genetic influence on the size, shape or position of the skeletal tissues. Rather, bony growth is driven by form and function of the surrounding soft tissues. Fränkel appliances are designed to change the muscular and soft tissue environment of the jaws and therefore modify growth. This is achieved with the use of wires and acrylic shields to displace the cheeks and lips away from the teeth, as well as encouraging forward posture of the mandible. Buccal shields removed pressure from the cheeks to allow for passive arch expansion, whilst theoretically stretching the periosteum to produce additional bony apposition laterally. Lower labial acrylic pads are designed to gently impede activity of the mentalis muscle thought to be an aetiological factor in the increased overjet seen in certain patients. Four types of Fränkel appliances, or functional regulators, have been described for treating class II division 1, class II division 2, class III and anterior open bite malocclusions. The treatment philosophy is based upon full-time wear, but the bulk and fragility of the appliance can make compliance difficult.
Twin block
William Clark originally described the twin block appliance, which is unusual in consisting of separate upper and lower removable appliances that work in unison (Fig. 8.27) (Clark, 1988). Each appliance incorporates a set of bite blocks that in occlusion posture the mandible forwards. The inclined planes of these blocks are set at approximately 70° with the height greater than 5-mm vertically to ensure that the patient occludes with the lower block in front of the upper and not on it. Overjet reduction can be rapid with a twin block and accompanying changes in the vertical dimension usually do not occur at the same rate, so a lateral open bite is often present at the end of overjet reduction, particularly where the overbite was originally increased (see Fig. 8.20). These open bites can be closed down once the overjet is fully reduced with selective trimming of the upper block to allow eruption of the mandibular first molars, or part-time wear of the appliance. The most significant advantage associated with the twin block is the ease with which it can be worn full-time by a patient and in many respects, this appliance has been responsible for the marked increase in popularity associated with functional appliances in recent years. The twin block also carries a number of other advantages:
Herbst appliance
The Herbst appliance is unusual in being a fixed functional appliance cemented or bonded directly to the dentition (Fig. 8.28). Protrusion of the mandible is achieved via a bilateral telescope apparatus attached to maxillary first molar and mandibular first premolar bands. The telescopic arms consist of a tube, plunger and pivot, which allows for opening and some lateral excursion, with these arms advancing the mandible so that the incisors are edge to edge. The fixed nature of this appliance means that effective compliance is not usually an issue and overjet reduction in 6 to 8 months is commonly achieved (Pancherz, 1982). However, potential disadvantages are that the Herbst appliance is expensive to fabricate, is often difficult to tolerate and can be prone to breakage.
Clinical use of functional appliances
The ideal case for treatment with a functional appliance should have the following clinical features:
Many of the earlier functional appliance systems were developed for treatment without fixed appliances and the patient generally had well-aligned dental arches or only mild crowding. Functional appliances are now often used to correct the skeletal base relationship in the presence of significant crowding, prior to a second phase of treatment with fixed appliances, often in combination with extractions. However, it should be remembered that successful treatment with functional appliances is dependent upon good appliance wear, favourable jaw growth and a well-motivated patient.
Timing of treatment
Functional appliances work most effectively in growing patients; however, the rate of facial and mandibular growth is not constant during childhood and adolescence and can be affected by growth spurts, particularly the pubertal growth spurt. The onset, duration and intensity of the mandibular pubertal growth spurt varies between individuals but generally occurs later in boys than in girls (Box 8.2). Functional appliances appear to have a slightly greater effect on skeletal growth if treatment takes place during this period (Baccetti et al, 2000). However, the precise timing of treatment does not seem to effect the long-term outcome (Tulloch et al, 1997a, b). The advantages of starting treatment in adolescence as opposed to childhood are:
Box 8.2 Prediction of adolescent growth
Functional appliances are more effective if their use is timed to coincide with the adolescent growth spurt, or more specifically peak height velocity (PHV) as the peak in adolescent maxillary and mandibular growth occurs at the same time or just after PHV (Baccetti et al, 2000). Generally puberty starts in girls approximately two years before boys and is shorter in duration. The mean PHV occurs at around 12 years of age in girls and 14 in boys (see Fig. 3.3). However, chronological age is a poor predictor as there is a huge range of individual variability. Measurement of height can be used to predict the growth spurt, by taking repeated measurements and plotting them to create a growth curve (Sullivan, 1983). The practical limitation of this method is that it requires several measurements repeated at regular intervals of every four months to construct an individual curve of growth velocity. Measurements must therefore be started at least a year before the earliest possible pubertal spurt, which will be around age 8 in girls and 10 in boys.
To overcome these limitations, various other methods for predicting the timing of PHV have been described, the most popular of which is the use of hand–wrist radiographs. These will give a measure of an individual’s skeletal maturity from stages of development of the phalanges and radius, and ossification of the adductor sesamoid of the thumb, which has been reported to precede or coincide with PHV. The predictive value of hand–wrist radiographs appears to improve closer to the PHV, but they need to be obtained at regular intervals to be of use and experience is needed to read them (Houston, 1979). As such, they have fallen out of favour and are rarely used in current orthodontic practice.
Alternate skeletal markers have been described, the most useful of which are the cervical vertebrae. These are usually visible on a lateral skull radiograph and are therefore readily available for examination by the orthodontist. During maturation, the cervical vertebrae increase in height, from wedge-shaped to rectangular and then square, becoming greater in the vertical dimension than horizontal, whilst a concavity also develops on their inferior border (Hassel & Farman, 1995). Their development has been staged and shows good correlation with skeletal maturity as measured from hand–wrist radiographs. Most important are C2, C3 and C4 because PHV and mandibular growth occurs between the times when concavities develop on the inferior borders of C3 and C4 (Franchi et al, 2000). After this point there is a gradual slowing down in adolescent growth.
Earlier treatment starting in the mixed dentition should be considered if there are psychosocial concerns relating to the aesthetic impact of maxillary incisor prominence or there is thought to be a significantly increased risk of trauma due to the increased overjet. Early treatment will necessitate an extended period of retention of any sagittal correction or even re-treatment as there will be a tendency for the original class II skeletal pattern to reassert itself. The overall treatment time will be therefore significantly increased with no ultimate difference in outcome for the patient compared to comprehensive treatment started in adolescence. This needs to be explained to the patient before starting so they can make an informed choice.
Pre-functional stage
To optimize the benefits of using a functional appliance a short period of treatment prior to fitting the appliance can often be beneficial:
Impressions and bite
Detailed impressions in alginate should be taken of both dental arches with adequate extension into the lingual and labial vestibules. This is particularly important if a Fränkel functional regulator is being prescribed, as the buccal shields and labial pads are made to actively stretch the mucosa.
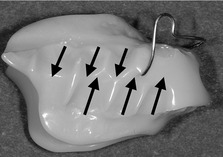
All functional appliances posture the mandible forward. To achieve this, they are constructed on simple articulators with the working models mounted to a postured bite taken in the mouth. This is usually done in wax, with the mandible as far forwards as is comfortable (Fig. 8.30).
If the overjet is 10-mm or less this will generally mean the postured bite can be taken with the incisors in an edge-to-edge relationship. If greater than 10-mm, it is unlikely that full overjet reduction can be achieved with a single appliance. Rather, the appliance may need reactivating; either by adjusting it so the mandible is postured further forwards, or by fabricating a second appliance once the overjet has been partially reduced (Box 8.3).
Box 8.3 One stage versus incremental mandibular advancement
The growth theory subscribed to will affect the clinical use of functional appliances. An example of this is how rapidly the mandible should be advanced with a functional appliance to effect most skeletal change. Advocates of progressive advancement, an increment at a time, argue that this leads to better patient compliance because it is more comfortable and results in greater maintenance of a postured bite during sleep. In addition, a single maximal advancement will generate larger class II forces, which when transmitted to the dentition will result in dentoalveolar rather than skeletal changes (Falck & Fränkel, 1989). Conversely, a single maximum advancement, which stretches the orofacial musculature, should result in a larger physiological response within the muscles and soft tissues, which in turn will generate greater skeletal growth and adaptation. In clinical practice there seems to be little difference in outcomes, either skeletal or dentoalveolar, if the mandible is maximally or incrementally postured forward (Banks et al, 2004). What is probably more important is retention of overjet reduction following active treatment, to allow consolidation of any remodelling within the glenoid fossa and condyle.
Vertically there should be approximately 2-mm of separation between the incisors. The exceptions to this are for Harvold-type activators, which are constructed to open the bite beyond the freeway space and for twin blocks, which require at least 5-mm of vertical separation in the buccal segments to allow for the inclined occlusal planes.
Appliance fitting and review
Appliances should be fitted within two weeks of the impressions being taken to ensure a good fit, as a poorly fitting appliance will negatively impact on compliance.
End of treatment with functional appliance and retention
Once the overjet is corrected, wear of the appliance should be continued on a part-time basis to retain the sagittal correction and allow occlusal settling. This is especially relevant when using an appliance such as the twin block, which does not allow free eruption of the buccal segments and often results in a transient lateral open bite at the end of treatment.
Clear orthodontic aligners—the renaissance of removable appliances
The past decade has seen the introduction of several removable appliance systems, which use a combination of thermoplastic formable materials and three-dimensional computer modelling to treat tooth malalignment. Clear plastic aligners have been available for many years as retainers and small tooth movements are possible by repositioning teeth on the dental study cast or by altering the shape of the aligner with a specially heated instrument.
More recently, computer technology has allowed high-accuracy dental impressions to be scanned and the creation of a virtual model of the malocclusion, which can then be manipulated (Invisalign®). From these manipulations, a series of removable aligners are fabricated, which the patient wears for approximate two-week intervals. These aligners can be effective for expansion, intrusion and the alignment of mild crowding (Fig. 8.31). Significantly, they are virtually invisible and can be removed by the patient, proving popular with adults. However, whilst they can be combined with fixed attachments for more complex tooth movement they cannot close space and are therefore inappropriate for cases where the degree of crowding warrants tooth extraction.
Aelbers CMF, Dermaut LR. Orthopedics in orthodontics: part 1, fiction or reality – a review of the literature. Am J Orthod Dentofacial Orthopedics. 1996;110:513-519.
Bishara SE. Functional appliances; a review. Am J Orthod Dentofacial Orthop. 1989;95:250-258.
Cozza P, Baccetti T, Franchi L, et al. Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop. 2005;129:599.e1-599.e12.
Meikle MC. Guest editorial: what do prospective randomized clinical trials tell us about the treatment of class II malocclusions? A personal viewpoint. Eur J Orthod. 2005;27:105-114.
Orton HS. Functional Appliances in Orthodontic Treatment. London: Quintessence; 1990.
Vig PS, Vig KWL. Hybrid appliances: a component approach to dentofacial orthopedics. Am J Orthod Dentofacial Orthop. 1986;90:273-285.
Baccetti T, Franchi L, Toth LR, et al. Treatment timing for Twin-block therapy. Am J Orthod Dentofacial Orthop. 2000;118:159-170.
Banks P, Wright J, O’Brien K. Incremental versus maximum bite advancement during twin-block therapy: a randomized controlled clinical trial. Am J Orthod Dentofacial Orthop. 2004;126:583-588.
Bass NM. Update on the Bass appliance system. J Clin Orthod. 1994;28:421-428.
Cetlin NM, Ten Hoeve A. Nonextraction treatment. J Clin Orthod. 1983;17:396-413.
Charlier JP, Petrovic A, Herrmann-Stutzmann J. Effects of mandibular hyperpropulsion on the prechondroblastic zone of young rat condyle. Am J Orthod. 1969;55:71-74.
Clark WJ. The twin block technique. A functional orthopedic appliance system. Am J Orthod Dentofacial Orthop. 1988;93:1-18.
Dolce C, McGorray SP, Brazeau L, et al. Timing of Class II treatment: skeletal changes comparing 1-phase and 2-phase treatment. Am J Orthod Dentofacial Orthop. 2007;132:481-489.
Eirew HL. The bionator. Br J Orthod. 1981;8:33-36.
Falck F, Frankel R. Clinical relevance of step-by-step mandibular advancement in the treatment of mandibular retrusion using the Frankel appliance. Am J Orthod Dentofacial Orthop. 1989;96:333-341.
Franchi L, Baccetti T, McNamara JAJR. Mandibular growth as related to cervical vertebral maturation and body height. Am J Orthod Dentofacial Orthop. 2000;118:335-340.
FrÄnkel R. A functional approach to orofacial orthopaedics. Br J Orthod. 1980;7:41-51.
Ghafari J, Shofer FS, Jacobsson-Hunt U, et al. Headgear versus function regulator in the early treatment of Class II, division 1 malocclusion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 1998;113:51-61.
Harvold EP, Vargervik K. Morphogenetic response to activator treatment. Am J Orthod. 1971;60:478-490.
Hassel B, Farman AG. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop. 1995;107:58-66.
Houston WJ. The current status of facial growth prediction: a review. Br J Orthod. 1979;6:11-17.
McNamara JAJR. Neuromuscular and skeletal adaptations to altered function in the orofacial region. Am J Orthod. 1973;64:578-606.
McNamara JAJR, Bryan FA. Long-term mandibular adaptations to protrusive function: an experimental study in Macaca mulatta. Am J Orthod Dentofacial Orthop. 1987;92:98-108.
McNamara JAJR, Hinton RJ, Hoffman DL. Histologic analysis of temporomandibular joint adaptation to protrusive function in young adult rhesus monkeys (Macaca mulatta). Am J Orthod. 1982;82:288-298.
O’Brien K, Wright J, Conboy F, et al. Effectiveness of early orthodontic treatment with the Twin-block appliance: a multicenter, randomized, controlled trial. Part 2: Psychosocial effects. Am J Orthod Dentofacial Orthop. 2003;124:488-494.
Orton HS, Slattery DA, Orton S. The treatment of severe ‘gummy’ Class II division 1 malocclusion using the maxillary intrusion splint. Eur J Orthod. 1992;14:216-223.
Pancherz H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod. 1982;82:104-113.
Sullivan PG. Prediction of the pubertal growth spurt by measurement of standing height. Eur J Orthod. 1983;5:189-197.
Teuscher U. A growth-related concept for skeletal class II treatment. Am J Orthod. 1978;74:258-275.
Tulloch JF, Medland W, Tuncay OC. Methods used to evaluate growth modification in Class II malocclusion. Am J Orthod Dentofacial Orthop. 1990;98:340-347.
Tulloch JF, Phillips C, Koch G, Phillips C. The effect of early intervention on skeletal pattern in Class II malocclusion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 1997;111:391-400.
Tulloch JF, Proffit WR, Phillips C. Influences on the outcome of early treatment for Class II malocclusion. Am J Orthod Dentofacial Orthop. 1997;111:533-542.
Tulloch JF, Proffit WR, Phillips C. Outcomes in a 2-phase randomized clinical trial of early Class II treatment. Am J Orthod Dentofacial Orthop. 2004;125:657-667.
van Beek H. Overjet correction by a combined headgear and activator. Eur J Orthod. 1982;4:279-290.
Vargervik K, Harvold EP. Response to activator treatment in class II malocclusions. Am J Orthod. 1985;88:242-251.
Voudouris JC, Woodside DG, Altuna G, et al. Condyle-fossa modifications and muscle interactions during Herbst treatment, Part 2. Results and conclusions. Am J Orthod Dentofacial Orthop. 2003;124:13-29.
Wieslander L. Intensive treatment of severe Class II malocclusions with a headgear-Herbst appliance in the early mixed dentition. Am J Orthod. 1984;86:1-13.
Wieslander L. Long-term effect of treatment with the headgear-Herbst appliance in the early mixed dentition. Stability or relapse? Am J Orthod Dentofacial Orthop. 1993;104:319-329.
Woodside DG Some effects of activator treatment on the mandible and the midface Trans Eur Orthod Soc 1973 443-447
Woodside DG, Metaxas A, Altuna G. The influence of functional appliance therapy on glenoid fossa remodeling. Am J Orthod Dentofacial Orthop. 1987;92:181-198.