10 Management of the developing dentition
A number of developmental anomalies can affect both the deciduous and permanent dentitions. These include variations in the number of teeth or their individual morphology, the position they attain within the dental arches and the composition of their constituent hard tissues. The aetiological basis of these abnormalities can be genetic, environmental or multifactorial, but they can all impact upon the developing occlusion, either directly or indirectly. In this chapter the aetiology and management of malocclusion in the developing dentition is discussed.
Early loss of deciduous teeth
The early loss of deciduous teeth is usually the result of extraction due to caries or trauma and can have implications for the developing occlusion: in particular, future space distribution and symmetry within the affected dental arch. The degree of space loss and potential occlusal disruption will be influenced primarily by:

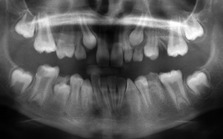
Figure 10.2 Crowding of maxillary second premolars as a result of early loss of the second deciduous molars.
The UL5 remains impacted in the palate whilst the UR5 has erupted palatally.
The timing of deciduous tooth extraction can also influence the eruption rate of permanent successors. Very early loss of deciduous teeth can delay successional tooth eruption, whilst later extraction can have the opposite effect.
Balancing and compensating extractions
Balancing and compensating extractions aim to preserve arch symmetry and occlusal relationships by extracting teeth opposing those requiring enforced extraction.
The decision to carry out a balancing or compensating extraction will depend upon a number of factors (Box 10.1). However, before the elective extraction of any deciduous tooth is instituted, a radiographic screen should be carried out to check for the presence, position and normal formation of the developing permanent dentition. Any other deciduous teeth of questionable prognosis should also be considered as candidates for balancing or compensating extraction, particularly if general anaesthesia is required. It can be more difficult to justify these extractions if local anaesthesia is used for the elective extraction of a single symptomatic tooth and cooperation for further extractions may be poor.
Box 10.1 Which deciduous teeth require balancing and compensating extractions?
Space maintenance
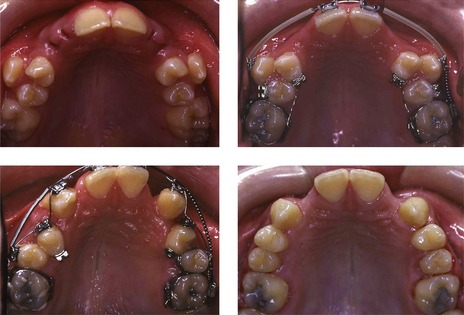
A space maintainer is a removable or fixed orthodontic appliance that preserves space within the dental arches (Fig. 10.3). These appliances are most commonly used in the mixed dentition to prevent forward drift of the first permanent molars following early loss of deciduous second molar teeth, or to maintain space and serve as a prosthesis in the labial segment after traumatic loss of permanent incisors.

Figure 10.3 Lower fixed space maintainers to preserve the arch length (left panels), preservation of labial segment position with a removable retainer (upper right and middle panels) and restoration of a LLE with a stainless steel crown to prevent space loss (lower right panel) (lower right panel courtesy of Evelyn Sheehy).
A space maintainer in the posterior dentition can be useful in the following situations:
It should always be remembered that a tooth is the ideal space maintainer and every effort should be made to preserve deciduous teeth until the time of their natural exfoliation (Fig. 10.3). If a space maintainer is to be used it should be in a mouth with good oral hygiene and ideally, a low risk of further caries. Unfortunately, cases requiring elective tooth extraction due to dental caries are often the least suitable for long-term space maintenance.
Prolonged retention of deciduous teeth
Considerable variation can exist in the timing of deciduous tooth exfoliation and the subsequent eruption of permanent successors. The presence of marked asymmetry in the retention of deciduous teeth should be investigated radiographically.
Occasionally a permanent successor will erupt having failed to resorb the roots of the overlying deciduous tooth (Fig. 10.4). The patient should be encouraged to exfoliate these retained deciduous teeth themselves and if this is not possible, they should be extracted under local anaesthetic.

Figure 10.4 Retained deciduous incisors.
The permanent incisors have failed to resorb their deciduous predecessors and erupted palatally (upper panel) and lingually (lower panel).
Crowding, or an ectopic position affecting the permanent successor, can also lead to prolonged retention of the overlying deciduous tooth.
Another cause of deciduous tooth retention is congenital absence of the permanent successor. For most of these deciduous teeth, the long-term prognosis is poor and they will either be lost naturally or ultimately require extraction. However, they can often act as useful maintainers of arch space or alveolar bone in the shorter term.
Retained second deciduous molars
The second deciduous molar can often be retained due to congenital absence of the second premolar. If this is the case, several treatment options should be considered:
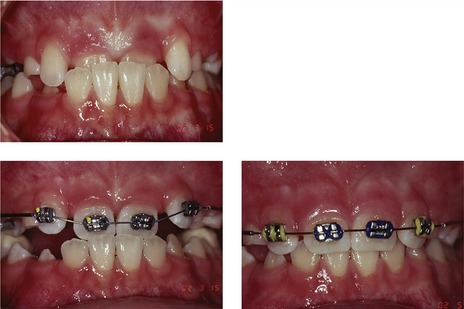
Treatment planning will depend primarily upon future space requirements for the correction of any underlying malocclusion and the long-term prognosis of the second deciduous molar. Clinical and radiographic examination of the crown, root and associated alveolar bone will give a useful indication of this (Fig. 10.5). Any of the following features, either alone or in combination, will demonstrate a potentially poor prognosis:
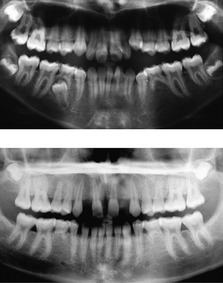
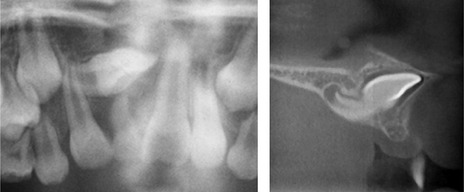
Figure 10.5 Retained deciduous molars in association with congenital absence of the second premolar.
In the upper radiograph, the LLE has a good long-term prognosis. In the lower radiograph, extensive root resorption means a poor prognosis for both the retained lower Es.
Second deciduous molars can have an excellent long-term prognosis if they are in good condition and will match the lifespan of many prostheses. Indeed, if they survive to twenty years of age, continued long-term function can be anticipated (Bjerklin & Bennett, 2000; Sletten et al, 2003).
Ankylosis and infraocclusion
A tooth becomes ankylosed when the periodontal ligament is lost and direct fusion occurs between root dentine and the surrounding alveolar bone. Ankylosis most commonly affects deciduous molars, occurring in up to 9% of children (Kurol, 1981). A number of factors are thought to contribute:
A consequence of ankylosis can be the apparent ‘submergence’ or infraocclusion of the affected tooth relative to the occlusal plane (Fig. 10.6). This occurs in the growing child because alveolar bone and occlusal height increase with development, whilst the position of the ankylosed tooth remains fixed.
Hypodontia
The congenital absence of one or more teeth is a relatively common anomaly in human populations.
The term hypodontia is generally used to describe congenital tooth absence, but the definitions are actually quite specific (Fig. 10.7):

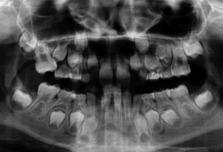
Figure 10.7 Hypodontia and oligodontia.
In the upper case there is hypodontia with UR2, UL2, LL8, LL5, LR5 and LR8 absent. In the middle case there is more severe hypodontia, with UR8, UR5, UR4, UL4, UL5, UL8, LR8, LR5, LL5 and LL8 absent. In the lower case there is oligodontia, with UR8, UR5, UR4, UR2, UL2, UL5, UL8, LL8, LL4, LL1, LR4, LR5, and LR8 absent.
Nonsyndromic hypodontia
Nonsyndromic hypodontia can either appear sporadically within a member of a family or be inherited. This form can follow autosomal dominant, autosomal recessive or autosomal sex-linked patterns of inheritance, with considerable variation in both penetrance and expressivity. This is by far the most common type of congenital tooth absence and can be further categorized based upon clinical presentation:
Within these clinical entities, certain teeth fail to develop more often than others:
Nonsyndromic hypodontia can be associated with other developmental anomalies affecting the dentition, which provides evidence of a genetic influence (Table 10.1). However, a multifactorial model has also been suggested (Brook, 1984), with the phenotypic effect being related to certain thresholds, themselves influenced by both genetic and environmental factors. Clearly, within this model, the mutation of a major gene may be a significant enough event to result in inherited tooth loss (Box 10.2).
Table 10.1 Dental anomalies associated with hypodontia
Box 10.2 Candidate genes for nonsyndromic human hypodontia
Targeted deletion of many genes in mutant mice can disrupt tooth formation and these have provided a reference point in the search for candidate genes in human populations. However, given the large number of potential genes available, it is somewhat surprising that only three have been positively identified in human familial hypodontia (Cobourne, 2007):
Syndromic hypodontia
Congenital tooth absence is also seen in association with other recognizable structural defects or abnormalities (Table 10.2).
Table 10.2 Syndromic conditions associated with hypodontia
| Syndrome | Gene |
|---|---|
| Anhidrotic ectodermal dysplasia (OMIM 305100) | EDA |
| Adult (OMIM 103285) | TP73L |
| Ehlers Danlos (OMIM 225410) | ADAMTS2 |
| Incontinentia pigmenti (OMIM 308300) | NEMO |
| Limb mammary (OMIM 603543) | TP63 |
| Reiger (OMIM 180500) | PITX2 |
| Witkop (OMIM 189500) | MSX1 |
| Ellis–van Creveld (OMIM 225500) | EVC or EVC2 |
Management
The management of congenital tooth absence will involve either:
Milder forms of hypodontia can usually be managed within an orthodontic treatment plan in consultation with either the general dental practitioner or restorative specialist and is usually carried out in the permanent dentition (see Chapter 11). More severe hypodontia or oligodontia requires complex multidisciplinary treatment and is usually carried out within a specialist centre.
Supernumerary teeth
Supernumerary teeth are teeth present in addition to the normal complement and can occur within either dentition.
In common with hypodontia, supernumerary teeth also occur either as an isolated trait or as a manifestation of a clinical syndrome (Table 10.3), but they are usually classified according to morphology and location:
Table 10.3 Syndromic conditions associated with supernumerary teeth
| Syndrome | Gene |
|---|---|
| Cleft lip and palate | |
| Cleidocranial dysostosis (OMIM 119600) | RUNX2 |
| Gardner (OMIM 175100) | APC |
| Ellis–van Creveld (OMIM 225500) | EVC; EVC2 |
| Incontinentia pigmenti (OMIM 308300) | NEMO |
Box 10.3 Managing the mesiodens
The mesiodens is one of the commonest forms of supernumerary tooth and is often detected in the anterior maxilla as a chance radiographic finding. Whilst removal is indicated if they interfere with the eruption, position or proposed orthodontic movement of adjacent teeth, quite often they are asymptomatic and in these circumstances, they should be left alone (Kurol, 2006). The potential risks associated with leaving these teeth in situ, such as follicular enlargement, cystic formation and resorption of maxillary incisor roots, would appear to be small (Tyrologou et al, 2005). In addition, if the mesiodens subsequently erupts, it can be removed with a relatively simple extraction under local anaesthesia.
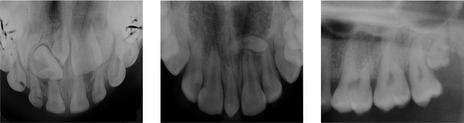
Figure 10.8 Conical supernumeraries.
Mesiodens positioned in the anterior maxilla, either vertically (left and middle) or horizontally (middle). Distomolar erupting behind the UL8 (right).

Figure 10.9 Extracted tuberculate supernumeraries and the effect of these teeth on the developing dentition.

Figure 10.10 Erupted tuberculate supernumerary.
The URA has been exfoliated and the UR1 is unlikely to erupt whilst the supernumerary is in situ.
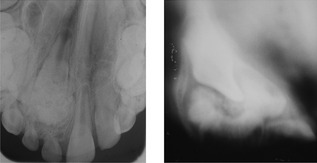
Figure 10.13 Complex odontome in the anterior maxilla.
The Scanora view on the right reveals the full extent of the odontome overlying the UR1.
Supernumerary teeth occur individually or in groups and can be unilateral or bilateral. These teeth are found most frequently in the anterior maxilla, but are also seen in the premolar and molar regions. In the permanent dentition, the majority fail to erupt and are asymptomatic, only being discovered during routine radiographic screening. However, they can also cause dental problems, which include:

Figure 10.22 The impacted UL1 has been exposed, bonded with a gold chain and traction applied using a removable appliance.
Fixed appliances were subsequently used to detail the permanent dentition.
Asymptomatic supernumerary teeth not affecting the occlusal relationships of the erupted dentition can be left in situ. These teeth should be kept under periodic radiographic review to ensure they are not damaging any adjacent structures or undergoing cystic change.
Abnormalities of tooth size
Teeth either larger or smaller than the normal population range for dimensions are usually referred to as megadont or microdont, respectively. These variations in tooth size can affect either the crown or root in isolation, or the whole tooth. Little is known about the aetiology of tooth size variation but it is almost certainly genetic.
Abnormalities of tooth form
A number of anomalies associated with tooth form have been described. These conditions are generally rare, occurring with prevalence well below 5% of Caucasians, and with the exception of double teeth, they generally affect the permanent dentition more commonly than the deciduous.

Figure 10.18 Double incisor teeth in the deciduous dentition with minor (left) and marked (right) coronal notching.
Right panel courtesy of Rudi Keane.
Abnormalities of eruption
A number of systemic conditions are associated with delayed eruption and these can affect both dentitions (Table 10.4). In the permanent dentition, great individual variation can exist in the timing of tooth eruption, with symmetrical deviation of anything up to two years from the mean not necessarily being a cause for concern. In the majority of children, local factors will be the main cause of any eruption disturbances that do occur (Table 10.5).
Table 10.4 Systemic conditions associated with delayed tooth eruption
Table 10.5 Local factors causing disturbances of tooth eruption
Primary management relies upon ensuring adequate space exists in the dental arch to accommodate the unerupted tooth and removing any potential obstruction. In these circumstances, the majority of teeth will erupt. If this fails to happen, or the unerupted tooth is ectopic from its normal path of eruption, surgical exposure, with or without orthodontic traction, may be required to accommodate the affected tooth into the dental arch (Box 10.4).
Box 10.4 Surgical exposure of impacted teeth
In the labial regions of the maxilla, and both labially and lingually in the mandible, the alveolar crest is covered by a keratinized, firmly attached gingiva, which is replaced by a more mobile, non-keratinized alveolar mucosa at the mucogingival junction. In contrast, on the palatal side of the maxilla there is no alveolar mucosa, the attached gingiva and palatal mucosa are both keratinized and firmly attached to the underlying bone, with no recognizable boundary between them. It is important for an impacted tooth to erupt through attached gingiva because this tissue provides a firm attachment at the dentogingival junction, is robust enough to maintain integrity of the periodontium during masticatory function and provides the best potential for long-term periodontal health. This will influence the method of exposure for teeth impacted in different areas of the jaws.
Impacted teeth are surgically exposed using one of two basic techniques:
The open window or closed techniques are suitable for teeth impacted beneath attached gingiva. Those situated below non-keratinized alveolar mucosa require either an apically repositioned flap or closed eruption.
Unerupted permanent maxillary incisor
A discrepancy in eruption between contralateral maxillary incisors of greater than six months, or eruption of lateral incisors before the centrals warrants radiographic investigation. Delayed eruption of maxillary incisors is most commonly associated with the presence of supernumerary teeth (particularly tuberculate), retained deciduous incisors or dilaceration. Obstruction secondary to a supernumerary tooth is by far the commonest cause.
Unerupted permanent maxillary canine
The permanent maxillary canine fails to erupt in approximately 2% of Caucasian children and these teeth will often require orthodontic management (Bishara, 1992; Ferguson, 1990). Deviation from the normal path of eruption is usually associated with subsequent impaction and in the vast majority of cases this occurs in a palatal direction, although the canine can also impact on the buccal side or within the line of the dental arch. A number of reasons have been suggested to explain the particular vulnerability of the maxillary canine to deviation from its normal eruptive path:
Clinical examination
At the age of 10 years, the maxillary canine should be palpable in the buccal sulcus adjacent to the lateral incisor root (Fig. 10.24). If it is not, or if there is any asymmetry in palpation, then an abnormal path of eruption should be suspected and radiographic investigation instigated (Ericson & Kurol, 1986). Other clinical features, which may alert the clinician to possible impaction include:
Radiographic examination
Radiographic examination is required to demonstrate the presence of the canine, its position within the maxillary arch, the condition of adjacent teeth (particularly the degree of resorption associated with the deciduous canine or presence of any resorption associated with the permanent incisors) and any other pathology. The position of the canine should be evaluated in all three planes of space:
Two films are required to definitively establish canine position and the parallax (or tube-shift) technique is commonly used to achieve this (Jacobs, 1999). Parallax is the apparent displacement of an object when observed from two different positions and, in radiological terms, relies upon taking two views with the X-ray tube in a different position for each view. Horizontal parallax uses a horizontal shift in the X-ray tube (usually with successive periapical views taken with the tube moved horizontally), whilst vertical parallax uses a vertical shift in the tube (usually achieved with a panoramic and anterior occlusal view). The advantage of the parallax technique is that it always involves an intraoral view, which gives good detail of the canine and incisors (Fig. 10.25). More recently, the use of cone beam CT has been described to precisely locate the position of ectopic canines (Walker et al, 2006) (see Box 6.5).
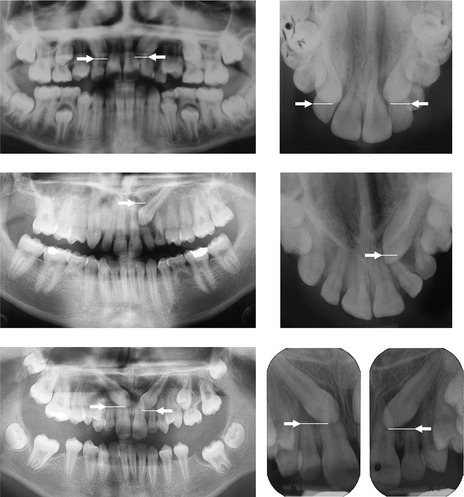
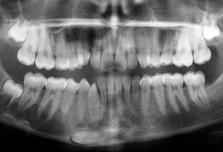
Figure 10.25 Vertical parallax to localize maxillary canine position.
In the upper radiographs, the coronal tip of both maxillary canines lie midway along the roots of the lateral incisors on the panoramic radiograph; whilst on the anterior occlusal radiograph they are clearly midway along the crowns of the lateral incisors. These canines have moved down as the X-ray tube has moved up and are therefore buccally positioned. In the middle radiographs, the UL3 is situated below the root apex of the UL2 on the panoramic radiograph; whilst on the anterior occlusal radiograph it is now situated above the tip. The canine has moved up as the X-ray tube has moved up and is therefore positioned palatally. In the lower radiographs the coronal tips of both maxillary canines are situated just below the apices of the lateral incisors on the panoramic radiograph; whilst on the periapical radiographs they are in a similar position. These canines have not moved significantly as the X-ray tube has moved and are therefore situated in the line of the dental arch.
Interceptive treatment
An impacted canine can be associated with a significant risk of damage to adjacent teeth, particularly the lateral and occasionally the central incisors (Fig. 10.26) and often requires surgical intervention combined with prolonged orthodontic treatment in order to accommodate it in the maxillary arch. Some evidence exists from prospective studies to suggest that early extraction of the deciduous canine can help prevent a palatally ectopic permanent canine becoming impacted (Fig. 10.27) (Ericson & Kurol, 1988; Power & Short, 1993), particularly if there is a lack of crowding or headgear is used to create space (Leonardi et al, 2004). Whilst this evidence is weak (Parkin et al, 2009), with radiographic evidence of an ectopic position and a lack of normal resorption associated with the deciduous canine, consideration should be given to elective extraction of this tooth. The best results seem to be obtained under the following conditions:
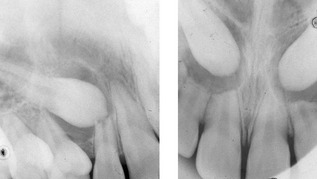
Figure 10.26 Resorption of the UR2 (left) and the UR2, UR1 and UL2 (right) root apices in association with impacted maxillary canines.
Left panel courtesy of Jackie Silvester.
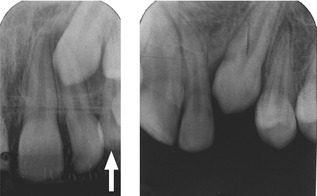
Figure 10.27 Improvement in the position of an impacted maxillary canine after extraction of its deciduous predecessor (arrowed).
If radiographic evidence of an improvement in canine position is not evident within 12 months of extraction, further treatment should be considered.
Management
The maxillary canine is a large tooth, possessing the longest root in the dentition and forming an important aesthetic and functional component of the occlusion. Every effort should be made to try and accommodate this tooth in the dental arch. However, a number of general factors should be taken into consideration when treatment planning for an impacted canine:
The treatment of choice is generally surgical exposure followed by orthodontic alignment. However, the patient may not wish to undergo the extended orthodontic treatment that might be required to accommodate a canine following surgical exposure, or the canine may be in such a poor position that orthodontic alignment is not practical. In this case, autotransplantation of the tooth directly into the correct position is a further option. Alternatively, a decision can be made to extract the impacted canine or more rarely, leave it in situ.
Surgical exposure and orthodontic alignment
Surgical exposure aims to remove any hard or soft tissue obstruction that may be impeding eruption and can be enough to induce the canine to erupt, particularly those in more favourable positions. For those that fail to respond or are more displaced, orthodontic alignment will also be required (Fig. 10.28). When embarking upon the prescription of surgical exposure and orthodontic alignment, the following should be remembered:

Figure 10.28 Surgical open (left panels) and closed (right panels) exposure and of a palatally impacted UL3 followed by orthodontic alignment.
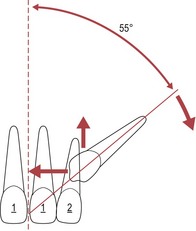
Figure 10.29 The prognosis for successful orthodontic alignment of a palatally impacted maxillary canine is influenced by the position of this tooth.
As the height increases, distance towards the dental midline reduces or angle to the mid-sagittal plane increases beyond 55°, the prognosis worsens.
The site of impaction will be an important determinant of the surgical technique used for exposing a maxillary canine (see Box 10.4):
A variety of techniques that allow orthodontic traction to be placed on an impacted canine have been described, but all will usually involve direct bonding of an orthodontic bracket (see Box. 10.4). Either removable or fixed appliances can be used to apply traction, but for either technique space is required in the dental arch. For canines in less favourable positions, fixed appliances are essential and as this process can be quite anchorage demanding, reinforcement should be considered. Using fixed appliances, traction can be applied with flexible piggyback archwires, elastomeric chain or string, rigid buccal arms or even magnets. The choice of technique will depend largely upon canine position and preference of the orthodontic operator.
Autotransplantation
Autotransplantation involves the surgical removal of an impacted canine and subsequent implantation into its normal position within the maxillary alveolus. Space will need to be available to accept the transplant and a short period of orthodontic treatment may be needed to generate this, particularly if a deciduous canine has been retained; but this process will generally be less time-consuming than aligning a canine with orthodontic traction (Fig. 10.30). If the position of the ectopic canine prevents any initial orthodontic treatment, the canine can initially be removed and ‘parked’ under the buccal mucosa whilst the necessary orthodontics is undertaken. Once space has been created for the tooth, a secondary surgical procedure can be undertaken to autotransplant the tooth.

Figure 10.30 Autotransplantation of an impacted UL3 in an adult patient. Fixed appliances were used to create some space for this tooth prior to transplantation (upper panels).
A retained URC with a poor long-term prognosis and aesthetics in a 43-year old woman who previously had the impacted UR3 extracted as a teenager (even though the UR2 was congenitally absent) (middle panels). Implant restoration to replace a previously extracted UL3 after orthodontic treatment to create space (Lower panels). Transplant and implant placement carried out by Jerry Kwok.
A disadvantage of autotransplantation is that these teeth can be susceptible to subsequent ankylosis or external root resorption and generally have a reduced long-term prognosis in comparison to canines aligned orthodontically. In addition, the success of this technique is highly dependent upon the skill of the surgical operator.
Extracting the canine or leaving it in situ
If a decision is made not to accommodate the impacted canine, then it can be extracted or left in situ. In either case, if the deciduous canine remains, the patient should be aware of the long-term prognosis and the likely need for eventual replacement of this tooth (see Fig. 10.30, middle panels). Alternatively, if the deciduous canine is not retained, a good contact between the lateral incisor and first premolar should be established (see Fig. 7.14). This may already be present if there is no spacing in the arch and orthodontic treatment may be avoided. However, if there is any residual spacing, either space closure or prosthetic replacement will be necessary and in both cases, some orthodontic treatment may be required (particularly if there is also an underlying malocclusion). A number of factors should be remembered when extracting a permanent canine:
Box 10.5 Putting a first premolar in the canine position
The morphology of the maxillary first premolar differs from that of the canine in several respects:
However, from the buccal aspect the premolar crown does resemble that of the canine and this tooth can make an excellent substitute, which can be enhanced by a few modifications:

Figure 10.31 Marked resorption of the UR1 in association with an impacted canine. The UR1 was extracted, the canine brought down into the arch and then modified with composite to resemble the central incisor.
The option to leave a maxillary canine in situ is usually made on the basis that the patient is happy with their dental appearance and does not wish to have any form of treatment.
Unerupted permanent mandibular canine
The permanent mandibular canine fails to erupt less commonly than the maxillary and when this does occur, it is usually a consequence of crowding. These teeth are often vertically orientated, labially placed and will erupt spontaneously once space is available in the arch. If surgical exposure is required, care should be taken to ensure these teeth erupt through attached gingiva. Occasionally an impacted mandibular canine can fail to erupt and migrate within the mandible, particularly if it is orientated horizontally (Fig. 10.32) (Peck, 1998). These teeth are not generally amenable to orthodontic traction and the options are then extraction or autotransplantation.
Impacted maxillary first permanent molar
Impaction of a maxillary first permanent molar against the second deciduous molar (Fig. 10.33) occurs in around 4% of the population and is usually indicative of crowding in the posterior maxilla (Kurol & Bjerklin, 1982).
Occasionally these teeth will spontaneously erupt but if this does not occur within 6–12 months, some intervention is indicated:
Primary failure of eruption
Primary failure of eruption (PFE) is an isolated condition associated with a localized failure of tooth eruption:
Diagnosis of PFE is usually made when there is an absence of any clear genetic, pathological or environmental factor responsible for preventing the eruption of an affected tooth (Fig. 10.34).
Management
Management of PFE is difficult because active orthodontic extrusion will normally result in ankylosis and a failure to bring an affected tooth into occlusion. Extraction, followed by either orthodontic space closure or prosthetic replacement, is usually indicated. Alternatively, localized bony osteotomy and orthodontic extrusion of the whole segment can be attempted. If some eruption of the tooth has occurred, a localized coronal buildup may be the treatment of choice to improve the vertical position. Cases where multiple teeth are involved are more difficult to manage, the only available method of bringing them into occlusion being a segmental osteotomy.
Transposition
Dental transposition is the complete positional interchange of two adjacent teeth, or the development, or eruption of a tooth in a position normally occupied by a non-adjacent tooth.
Table 10.6 Classification of dental transpositiona
| Maxilla |
| Mandible |
a Peck et al, 1993, 1998.
Several mechanisms to account for the phenomenon of dental transposition have been proposed:
However, many types of transposition are often associated with factors that have a genetic basis:
On this basis it has been suggested that the primary aetiological basis of transposition is genetic, within a model of multifactorial inheritance (Peck et al, 1993, 1998).
Management
Interceptive extraction of an overlying deciduous tooth may be considered if a transposition is identified early enough and this may facilitate correction, particularly if the transposition is not fully established. Definitive treatment of an established transposition will involve either:
These options need to be evaluated as part of the overall treatment plan for each individual malocclusion and will often require fixed appliances (Ngan et al, 2004).
Early loss of first permanent molars
The decennial National Children’s Dental Health Survey has clearly shown a progressive reduction in dentinal caries experience in the permanent dentition of children aged between 8 and 15 years over the past thirty years (Pitts et al, 2006). However, in those children who do experience dental caries, first permanent molars can be susceptible to progressive and rapid decay (Fig. 10.36). In addition, combined first molar–incisor hypomineralization (MIH) is a recognized condition of unknown aetiology seen in around 15% of Caucasian children, which can significantly affect the long-term prognosis of first permanent molars in more severe cases (Koch et al, 1987). The increased use of fixed orthodontic appliances has meant that a good occlusal result can be obtained following the enforced loss of these teeth in a wider range of cases (Sandler et al, 2000). However, those children who require first molar extraction are often the least suitable for subsequent fixed appliance treatment because of high caries susceptibility and low potential compliance.
Ideally, premature loss of first molars should be followed by successful eruption of the second molars to replace them, ultimately followed by third molars to complete the molar dentition (Fig. 10.37). If any space is required within the arches to correct an underlying malocclusion, the first molar extraction sites should provide this. However, extraction of these teeth often results in a large amount of space being created at some distance from those sites where it is required to relieve incisor crowding or reduce an overjet. In these circumstances, fixed appliances will be required to control this.
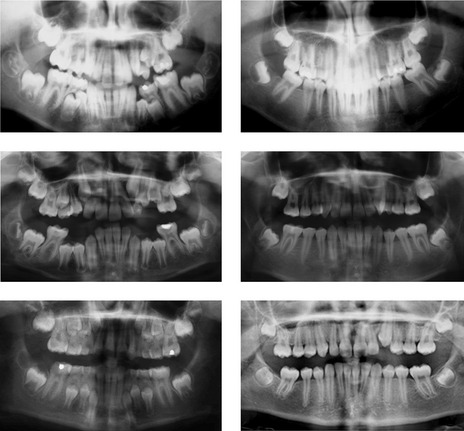
Figure 10.37 Good occlusal results following extraction of the lower first permanent molars (upper panels) and all four first permanent molars (middle and lower panels). The second molars are at a good angulation with minimal spacing and there is evidence of third molar development.
First permanent molars are never the ideal choice of teeth to extract because significant occlusal complications can result, particularly if they are removed before the age of 8 years:
Delayed extraction, during the later stages of second molar eruption, can also result in occlusal problems (Fig. 10.38):

Figure 10.38 A poor occlusal result following extraction of the lower first permanent molars.
The second permanent molars are spaced and mesially angulated after late extraction of the first molars.
However, in many cases the poor prognosis associated with carious, hypoplastic or heavily restored first molars will dictate that extraction is required. Indeed, radiographic evidence of caries into dentine affecting first permanent molars should elicit consideration of their elective extraction. The best spontaneous occlusal results are obtained in the following circumstances:
In most circumstances, not all of the first permanent molars will have a poor prognosis and the need for balancing or compensating extractions will have to be evaluated. Generally, extraction of a mandibular first molar may require compensatory extraction of the opposing maxillary molar to prevent overeruption of this tooth. This decision is more difficult if space is required in the maxillary arch to correct a malocclusion (Box 10.6):
Box 10.6 Treatment planning for the loss of first permanent molars
Class I Malocclusion
Class II Division 1 Malocclusion
Class II Division 2 Malocclusion
Class III Malocclusion
Balancing first molar extractions are rarely required to preserve a centreline. However, these extraction decisions will need to be made as part of the overall treatment plan for the whole occlusion.
Early loss of the maxillary central incisor
Traumatic loss of a maxillary central incisor is seen in around of 3% of children and usually occurs unilaterally, in the mixed dentition and in a child with an increased overjet (Jarvinen, 1978). Reimplantation should always be attempted if possible, because regardless of the long-term prognosis, these teeth will serve as a useful maintainer of both arch space and alveolar bone. If they are subsequently lost, longer term space maintenance can be achieved with a simple upper partial denture. If these teeth are not reimplanted, a decision will need to be made regarding space management. Long-term space maintenance can be achieved with a partial denture; however, this can be associated with a loss of alveolar bone height, which can make subsequent prosthetic replacement more difficult. Alternatively, the space can be allowed to close and reopened in the permanent dentition prior to prosthetic replacement. This allows preservation of alveolar bone, but will require fixed appliance treatment and often space creation in the upper arch.
Management
Unilateral loss of a maxillary central incisor will usually require prosthetic replacement, with either a resin-retained bridge or implant, because a lateral incisor rarely makes a good unilateral substitute for the central incisor. If space is required elsewhere in the maxillary arch, this is usually dealt with on its own merit. Occasionally, if premolar extractions are planned to correct any underlying malocclusion, autotransplantation and subsequent coronal modification of one of these teeth can provide a further option for replacing the maxillary incisor (Fig. 10.39).
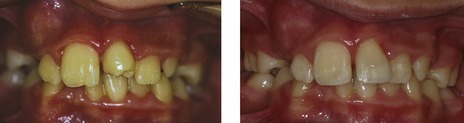
Figure 10.39 Premolar transplanted into the central incisor position and built up with composite
Courtesy of Joanna Johnson.
In cases of bilateral loss, if space is required to reduce an overjet or relieve crowding and the lateral incisors are of a reasonable size and form, consideration can be given to moving them into the position vacated by the centrals (Fig. 10.40), although it can be difficult to obtain good aesthetics without modifying their coronal morphology restoratively.
Maxillary midline diastema
A maxillary midline diastema can be a normal feature of dental development and will often improve following eruption of the permanent canine teeth. However, a number of other causes also exist (Fig. 10.41):
Management
Management of a midline diastema will depend primarily upon the underlying cause. In the absence of any obstruction, pathology or marked reduction in the amount of tooth tissue within the anterior maxilla, active orthodontic treatment to close a diastema is usually carried out in the permanent dentition and unless small, normally requires bodily movement of the incisors with a fixed appliance. The propensity of a closed maxillary diastema to reopen following brace removal means that long-term retention is usually mandatory. For this reason, particularly for a minor diastema, persuading the patient that it is a feature of individuality that does not require closing can be advantageous.
A prominent labial frenum can be suspected in the following circumstances:
The relative contribution of a prominent labial frenum in the aetiology of a diastema is controversial. However, if it is present, removal (or frenectomy) can be prescribed as part of the orthodontic treatment plan to close a diastema. Opinions vary as to the optimal time to carry out a frenectomy:
On balance it would seem sensible to delay any frenectomy until orthodontic closure of the diastema has been completed, which should be carried out in the permanent dentition, following eruption of the maxillary canines.
Digit sucking
A prolonged digit sucking habit can give rise to a number of characteristic features as part of a malocclusion and these often manifest in the late deciduous or early mixed dentitions (see Fig. 1.10):
These features are associated directly with the habitual placement of the digit and indirectly with the reduced tongue position and negative intraoral pressure generated with the habit. The underlying pattern of facial growth will also influence the malocclusion, any tendency toward vertical excess and a posterior mandibular growth rotation will potentially worsen the effects of any habit, or even make a more significant contribution than the habit itself.
Digit sucking occurs quite commonly in children below the age of 10 years and will often cease spontaneously. In most of these cases, the anterior open bite will resolve, although correction of the crossbite may require some maxillary arch expansion. However, in a minority of cases the habit can persist into the teenage years and can be the main contributing factor in the aetiology of a significant malocclusion. These children should be encouraged to stop the habit, ideally without intervention, although a variety of commercial aids are also available. If these fail occasionally a simple removable or fixed orthodontic appliance may be required to finally break the habit.
Crowding
As the permanent incisors are larger than their deciduous predecessors, space must be made available in the dental arches if they are to erupt without crowding. Spacing between the deciduous incisors can provide some of this (see Box 4.5 and Fig. 4.15); but the permanent incisors commonly erupt into crowded positions, particularly in the lower arch. A small improvement in this crowding can sometimes occur prior to eruption of the permanent canines, due largely to incisor proclination during eruption and some transverse expansion into the canine regions (Lundy & Richardson, 1995). However, once the permanent canines have erupted, there will almost certainly be no further improvement in incisor alignment and often an increase in crowding.
A variety of interceptive measures for alleviating incisor crowding during the mixed dentition, including arch expansion, extraction of the deciduous canines and serial extraction, have been described. Expansion across the intercanine width is largely unstable, particularly in the lower arch and is not recommended. Extraction of the deciduous canines will result in some short-term improvement in lower incisor alignment; however, whilst this can be effective for labiolingual displacements, it is less so for rotations. In addition, the incisors may tip lingually, which can reduce arch length and result in greater crowding in the long-term. Despite these limitations the extraction of deciduous canines can be a useful strategy in the following circumstances:
Serial extraction
The use of serial extraction as an interceptive orthodontic procedure was originally popularized by Bjerger Kjellgren at the Eastman Dental Institute in Stockholm (Kjellgren, 1947). Serial extraction aims to produce a well-aligned dentition in cases with a full complement of teeth and no significant sagittal discrepancy, without the need for orthodontic appliances. Essentially, serial extraction involves:
Serial extraction borrows space in the mixed dentition for early alignment of the labial segments and ultimately repays this by extraction of four first premolars. As a complete sequence it is no longer recommended for a number of reasons:
Crossbites
Teeth can erupt into a position of crossbite during the mixed dentition, either individually or within a group. Early correction is indicated, particularly if the crossbite is associated with a mandibular displacement or periodontal damage, and this can be achieved relatively easily during the mixed dentition.
Posterior crossbite
A posterior crossbite in the mixed dentition can be an early manifestation of a skeletal discrepancy, or be related to a persistent digit-sucking habit and can occur unilaterally or bilaterally. There is a weak association between posterior crossbite with displacement and the later development of temporomandibular dysfunction (Mohlin & Thilander, 1984); whilst asymmetric muscular activity associated with an established mandibular displacement can be perpetuated from the primary and mixed into the permanent dentition. For these reasons, it is considered appropriate to correct a posterior crossbite and eliminate the displacement as early as possible (Harrison & Ashby, 2001) and a number of relatively simple methods are available to do this.
Removable appliances
Correction can occasionally be achieved by occlusal grinding in the primary dentition; however, more commonly a removable appliance with a midline expansion screw can be used in the early mixed dentition (see Fig. 8.14).
Anterior crossbites
An anterior crossbite can cause gingival recession associated with the lower incisors if there is a displacement on closing, particularly if these teeth are displaced labially (Fig. 10.42). This is an indication for treatment in the mixed dentition and correction can be achieved with removable or fixed appliances. In the presence of a positive overbite, a corrected anterior crossbite will usually be self-retaining.
Removable appliances
If space is available in the dental arch, a removable appliance can be used to push the upper incisor teeth over the bite using simple palatal springs (see Fig. 8.16). This tipping movement will also usually result in some reduction of the overbite, which is often beneficial. Occlusal interferences usually need to be eliminated before overbite correction can take place, especially with an increased overbite, and posterior occlusal capping can be incorporated into the appliance to achieve this.
Fixed appliances
If space or bodily tooth movement are required to correct an anterior crossbite, removable appliances are inappropriate. In these circumstances, a fixed appliance with four brackets placed on the upper incisors and bands on the first molars (2 × 4 appliance) (Fig. 10.43) can be very effective. The bite can be opened with glass ionomer cement placed on the occlusal surface of the first molars. Simple fixed appliances offer a number of advantages over removable appliances:
Skeletal problems in the mixed dentition
Skeletal discrepancies can also manifest during the mixed dentition and will often respond well to early intervention. However, the potential advantages associated with early correction need to be considered in relation to the disadvantages of long-term treatment, maintaining the stability of correction during subsequent facial growth and the fact that a shorter course of treatment in the late mixed or early permanent dentition will almost certainly achieve the same result.
Class II malocclusion
Class II malocclusions are amenable to early treatment using functional appliances; however, the timing of treatment should be carefully considered. Several large randomized controlled trials have shown little difference in outcome, in terms of both overall growth and the final occlusal result, between patients who underwent an early phase of treatment to reduce an overjet in the mixed dentition and those who received comprehensive treatment in the late mixed and early permanent dentition (see Chapter 8). Whilst overjet correction can be rapid in the mixed dentition, a significant problem is the length of time this correction must be retained whilst waiting for a patient to enter the permanent dentition, prior to a final stage of fixed appliance orthodontic treatment to detail the occlusion. The only significant difference would appear to be the overall treatment time; patients who undergo early correction ultimately spend longer in treatment. As a general rule, the most effective time for undertaking correction of a class II malocclusion is during the adolescent growth spurt, as this will optimize mandibular growth whilst limiting the overall treatment time. However, several exceptions do exist (Box 10.7) and these relate primarily to reducing the risk of trauma and improving self-esteem.
Removable appliances
If the upper labial segment is proclined and spaced, a removable appliance with an active labial bow can be used to reduce an overjet (see Fig. 8.13). This should be worn full-time until the overjet is reduced and then as a retainer at night. In the presence of maxillary excess or a class II buccal segment relationship, headgear may also be needed in conjunction with the removable appliance.
Functional appliances
Functional appliances are very effective at overjet reduction. There can be problems associated with retention of tooth-borne appliances in the mixed dentition, as the first molars are often not fully erupted and can be difficult to crib effectively. The use of an activator-type appliance can help overcome this.
Class III malocclusions
A reduced or reverse overjet in the mixed dentition is usually a sign of an underlying class III skeletal relationship and this will tend to worsen with age. Treatment decisions are often delayed at this stage to monitor further growth and to better determine the extent of the skeletal problem; however, early treatment may be considered in patients with the following features:
A class III malocclusion on a skeletal I base with a significant forward mandibular displacement is sometimes referred to as a ‘pseudo class III malocclusion’, because the incisor relationship does not reflect the underlying skeletal relationship (see Fig. 6.17). This type of class III malocclusion is very amenable to early orthodontic treatment, but creating a positive overbite as well as overjet is crucial for stability following correction. When the overbite is reduced or there is an anterior openbite, it is more sensible to monitor growth into adolescence before final treatment decisions are made.
Functional appliances
Functional appliances are most commonly used to correct class II malocclusion; however, numerous appliances have also been described for the treatment of class III cases. These are only really able to treat the milder class III cases described above. This is largely because their effects are restricted to inducing the following tooth movements:
A class III version of the Fränkel Functional Regulator (FR III) is most commonly used, but this appliance is bulky, prone to breakage and difficult to wear. More recently, a class III twin block, with the blocks reversed in comparison to the class II version, has been described (Fig. 10.44).
Fixed appliances
A 2 × 4 appliance can be used to correct a class III incisor relationship. If proclination of the upper labial segment is required, a compressed loop or pushcoil can be placed in the buccal segments.
Protraction headgear
Extraoral force can be utilized in an attempt to move the maxilla forwards in class III cases, applied by attaching heavy elastics from either a removable or fixed appliance to a facemask, which rests on the patient’s forehead and chin for anchorage (Fig. 10.45). If worn for 12 to 14 hours each day, a significant anterior skeletal displacement of the maxilla is possible, making this approach the most appropriate for patients with maxillary hypoplasia (Fig. 10.46). This technique is theoretically more effective when combined with rapid maxillary expansion, because the expansion will disrupt the maxillary sutures and allows greater anterior displacement of the maxilla by the headgear. Greater skeletal change is seen in pre-adolescent patients, which essentially means those in the early mixed dentition. However, long-term results are dependent on further growth and patients with a vertical growth pattern or mandibular prognathism will often tend to outgrow any early positive effects of treatment. In addition, these appliances are some of the most demanding to wear in terms of patient compliance.
Abnormalities of tooth structure
Defects in the enamel or dentine of the tooth can give rise to varying degrees of discolouration and loss of structure. These anomalies can be caused by local and systemic environmental factors or genetic disease.
Enamel defects
The enamel of deciduous teeth begins to calcify at around 4 months in utero and is complete by the end of the first year of life. In the permanent dentition, this process occurs between 4 months and around 8 years of age (excluding third molars). A range of local and systemic factors can disturb enamel formation, which can lead to chronological hypoplasia and hypocalcification of the tooth crown (Table 10.7).
Table 10.7 Anomalies of enamel and dentine
| Enamel defects |
| Localized factors |
| Systemic factors |
| Dentine defects |
| Localized factors |
| Systemic factors |
Amelogenesis imperfecta (OMIM 104510)
Amelogenesis imperfecta (AI) is a collective term for a group of inherited conditions characterized primarily by abnormal enamel formation in either dentition (Fig. 10.47). AI can be inherited as an autosomal dominant, autosomal recessive or sex-linked trait and has a prevalence that can range from 1 : 1,000 to 1 : 14,000, depending upon the population. The predominant enamel phenotype is either:
The classification of AI is complex, being based historically upon phenotype (Table 10.8). However, as knowledge of the genetic basis underlying this condition has improved, the classification has been adapted (Wright, 2006).
Table 10.8 Classification of amelogenesis imperfectaa
| Type I hypoplastic |
| Type II hypomaturation |
| Type III hypocalcified |
| Type IV hypomaturation–hypoplastic with taurodontism |
Dentine defects
In addition to systemic factors, localized environmental factors such as infection and trauma can interfere with dentinogenesis (Table 10.7).
Inherited conditions affecting dentine
A number of genetic conditions exist that can affect the dentine within teeth, either in isolation or in addition to other structures within the body (MacDougall et al, 2006) (Table 10.9). All of these conditions exhibit an autosomal dominant pattern of inheritance and can be classified as:
Table 10.9 Genetic defects affecting dentine
Dentinogenesis imperfecta (DGI) represents the most common group of inherited dentine disorders (Fig. 10.48) and there are three essential subgroups, types I–III:
Orthodontic management of AI and DGI
Children affected by AI or DGI will require long-term multidisciplinary dental management. The appearance of affected teeth is often poor, with early loss of enamel leading to dentine exposure and subsequent sensitivity, which in turn can result in poor oral hygiene and a significant caries risk. All these factors make orthodontic treatment potentially difficult, this problem being compounded by a known association between AI and the presence of anterior open bite. When considering orthodontic treatment for the more severe cases:
Becker A. The Orthodontic Treatment of Impacted Teeth, 2nd edn. London: Informa Healthcare; 2007.
Burden D, Harper C, Mitchell L, et al. Management of unerupted maxillary incisors. Faculty of Dental Surgery of the Royal College of Surgeons of England. Available at URL http://www.rcseng.ac.uk/fds/clinical_guidelines, 1997.
Hussain J, Burden D, McSherry P. The management of the palatally ectopic maxillary canine. Faculty of Dental Surgery of the Royal College of Surgeons of England. Available at URL http://www.rcseng.ac.uk/fds/clinical_guidelines, 2003.
COBOURNE M, WILLIAMS A, MCMULLEN R. A guideline for the extraction of first permanent molars in children. Faculty of Dental Surgery of the Royal College of Surgeons of England http://www.rcseng.ac.uk/fds/clinical_guidelines, 2009.
Winter GB. Anomalies of tooth formation and eruption. In: Welbury RR, editor. Paediatric Dentistry. Oxford: Oxford University Press, 2001.
Bishara SE. Impacted maxillary canines: a review. Am J Orthod Dentofacial Orthop. 1992;101:159-171.
Bjerklin K, Bennett J. The long-term survival of lower second primary molars in subjects with agenesis of the premolars. Eur J Orthod. 2000;22:245-255.
Brin I, Becker A, Shalhav M. Position of the maxillary permanent canine in relation to anomalous or missing lateral incisors: a population study. Eur J Orthod. 1986;8:12-16.
Brook AH. A unifying aetiological explanation for anomalies of human tooth number and size. Arch Oral Biol. 1984;29:373-378.
Cobourne MT. Familial human hypodontia—is it all in the genes? Br Dent J. 2007;203:203-208.
Ericson S, Kurol J. Radiographic assessment of maxillary canine eruption in children with clinical signs of eruption disturbance. Eur J Orthod. 1986;8:133-140.
Ericson S, Kurol J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod. 1988;10:283-295.
Ferguson JW. Management of the unerupted maxillary canine. Br Dent J. 1990;169:11-17.
HARRISON JE AND ASHBY D (2001). Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev, CD000979.
Jacobs SG. Localization of the unerupted maxillary canine: how to and when to. Am J Orthod Dentofacial Orthop. 1999;115:314-322.
Jarvinen S. Incisal overjet and traumatic injuries to upper permanent incisors. A retrospective study. Acta Odontol Scand. 1978;36:359-362.
Jumlongras D, Bei M, Stimson JM, et al. A nonsense mutation in MSX1 causes Witkop syndrome. Am J Hum Genet. 2001;69:67-74.
Kjellgren B Serial extraction as a corrective procedure in dental orthopaedic therapy Trans Eur Orth Soc 1947 134-160
Koch G, Hallonsten AL, Ludvigsson N, et al. Epidemiologic study of idiopathic enamel hypomineralization in permanent teeth of Swedish children. Comm Dent Oral Epidemiol. 1987;15:279-285.
Kokich VG. Surgical and orthodontic management of impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2004;126:278-283.
Kurol J. Infraocclusion of primary molars: an epidemiologic and familial study. Community Dent Oral Epidemiol. 1981;9:94-102.
Kurol J. Impacted and ankylosed teeth: why, when, and how to intervene. Am J Orthod Dentofacial Orthop. 2006;129:S86-90.
Kurol J, Bjerklin K. Ectopic eruption of maxillary first permanent molars: familial tendencies. ASDC J Dent Child. 1982;49:35-38.
Lammi L, Arte S, Somer M, et al. Mutations in AXIN2 cause familial tooth agenesis and predispose to colorectal cancer. Am J Hum Genet. 2004;74:1043-1050.
Leonardi M, Armi P, Franchi L, et al. Two interceptive approaches to palatally displaced canines: a prospective longitudinal study. Angle Orthod. 2004;74:581-586.
Lundy HJ, Richardson ME. Developmental changes in alignment of the lower labial segment. Br J Orthod. 1995;22:339-345.
MacDougall M, Dong J, Acevedo AC. Molecular basis of human dentin diseases. Am J Med Genet A. 2006;140:2536-2546.
Mohlin B, Thilander B. The importance of the relationship between malocclusion and mandibular dysfunction and some clinical applications in adults. Eur J Orthod. 1984;6:192-204.
Neal JJ, Bowden DE. The diagnostic value of panoramic radiographs in children aged nine to ten years. Br J Orthod. 1988;15:193-197.
Ngan DC, Kharbanda OP, Darendeliler MA. Considerations in the management of transposed teeth. Aust Orthod J. 2004;20:41-50.
Nieminen P, Arte S, Pirinen S, et al. Gene defect in hypodontia: exclusion of MSX1 and MSX2 as candidate genes. Hum Genet. 1995;96:305-308.
PARKIN N, BENSON PE, SHAH A ET AL (2009). Extraction of primary (baby) teeth for unerupted palatally displaced permanent canine teeth in children. Cochrane Database Syst Rev 2: CD004621.
PARKIN N, BENSON PE, THIND B ET AL (2008). Open versus closed surgical exposure of canine teeth that are displaced in the roof of the mouth. Cochrane Database Syst Rev 4: CD006966.
Peck L, Peck S, Attia Y. Maxillary canine-first premolar transposition, associated dental anomalies and genetic basis. Angle Orthod. 1993;63:99-109.
Peck S. On the phenomenon of intraosseous migration of nonerupting teeth. Am J Orthod Dentofacial Orthop. 1998;113:515-517.
Peck S, Peck L, Kataja M. The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod. 1994;64:249-256.
Peck S, Peck L, Kataja M. Mandibular lateral incisor-canine transposition, concomitant dental anomalies, and genetic control. Angle Orthod. 1998;68:455-466.
Pitts NB, Chestnutt IG, Evans D, et al. The dentinal caries experience of children in the United Kingdom, 2003. Br Dent J. 2006;200:313-320.
Power SM, Short MB. An investigation into the response of palatally displaced canines to the removal of deciduous canines and an assessment of factors contributing to favourable eruption. Br J Orthod. 1993;20:215-223.
Sandler PJ, Atkinson R, Murray AM. For four sixes. Am J Orthod Dentofacial Orthop. 2000;117:418-434.
Sarnas KV, Rune B. The facial profile in advanced hypodontia: a mixed longitudinal study of 141 children. Eur J Orthod. 1983;5:133-143.
Simons AL, Stritzel F, Stamatiou J. Anomalies associated with hypodontia of the permanant lateral incisors and second premolar. J Clin Pediatr Dent. 1993;17:109-111.
Sletten DW, Smith BM, Southard KA, et al. Retained deciduous mandibular molars in adults: a radiographic study of long-term changes. Am J Orthod Dentofacial Orthop. 2003;124:625-630.
Stewart DJ. Dilacerated unerupted maxillary central incisors. Br Dent J. 1978;145:229-233.
Tyrologou S, Koch G, Kurol J. Location, complications and treatment of mesiodentes—a retrospective study in children. Swed Dent J. 2005;29:1-9.
van den Boogaard MJ, Dorland M, Beemer FA, van Amstel HK. MSX1 mutation is associated with orofacial clefting and tooth agenesis in humans. Nat Genet. 2000;24:342-343.
Vastardis H, Karimbux N, Guthua SW, Seidman JG, et al. A human MSX1 homeodomain missense mutation causes selective tooth agenesis. Nat Genet. 1996;13:417-421.
Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2006;128:418-423.
Witkop CJJR. Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: problems in classification. J Oral Pathol. 1988;17:547-553.
Wright JT. The molecular etiologies and associated phenotypes of amelogenesis imperfecta. Am J Med Genet A. 2006;140:2547-2555.