11 Management of the permanent dentition
The majority of orthodontic treatment is carried out in the late mixed or permanent dentition. This allows for comprehensive treatment within a finite and realistic timeframe, whilst optimizing adolescent growth and compliance. In this chapter the management of malocclusion in the permanent dentition will be discussed in terms of different occlusal traits. Although separated for clarity, an individual patient will often present with more than one of these. Therefore, treatment planning will routinely incorporate more than one aim. The final section in this chapter will look at the rationale and management of retention following active treatment.
Tooth–arch size problems
A discrepancy between the overall tooth size and arch dimension can lead to either dental arch crowding or spacing, depending upon whether there is too much or too little space for the teeth.
Crowding
Crowding and malalignment of the anterior teeth are some of the commonest problems encountered in the treatment of malocclusion, and patients are often very conscious of them. Crowding is usually recorded in millimetres and treatment will depend upon both the severity and position within the dental arch. In order to align crowded teeth space will need to be created. As a general rule, mild crowding requires up to 4-mm of space to relieve, moderate crowding between 5 and 8-mm and severe crowding 9-mm or more.
Mild crowding
If crowding is mild the removal of teeth can leave excessive space, which if closed with fixed appliances will often result in over-retraction of the labial segments. Therefore, unless this is an aim of treatment, mild crowding can usually be treated without extractions. A number of techniques that can provide space in the dental arches without the need for extraction exist.
Molar distalization
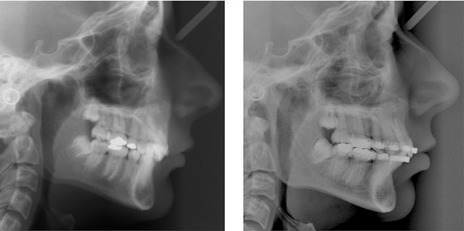
Moving the first permanent molars distally can create space. This is technically difficult in the mandibular arch and rarely attempted, but it is possible in the maxilla and appropriate for mild crowding, where the buccal segment relationship is up to half a unit class II. The most predictable technique, with the least associated anchorage loss, is extraoral traction mediated by the wearing of headgear (Fig. 11.1) (Sfondrini et al, 2002).
The biggest problems with the use of headgear are the dependence upon good compliance and favourable growth for success. In an attempt to overcome problems associated with compliance, numerous appliances have been designed to distalize the maxillary buccal segments without the need for headgear and are accordingly described as ‘non-compliance’ appliances. Most use the palate for anchorage, with a distalizing force applied directly to the maxillary first molars via either palatal springs or compressed coils. Although effective, all will tip the molars to some extent and result in anchorage loss in the form of an increase in overjet. To avoid this, implants can be used to support the anchorage further and these have been shown to be effective (Fig. 11.2) (Sandler et al, 2008).
Maintenance of the leeway space
The greater mesiodistal dimension of the second deciduous molars in comparison to the second premolar teeth can provide some additional space for the relief of crowding (Brennan & Gianelly, 2000). This can be done if the position of the first permanent molars is held just prior to exfoliation of the deciduous molars by fitting a lingual arch (see Figs 9.19 and 10.3). In the mandibular arch this provides approximately 2 to 2.5-mm of space per quadrant and in the maxilla around 1 to 1.5-mm.
Lip bumper
A lip bumper is a mandibular fixed appliance consisting of a 1.0-mm stainless steel wire attached to bands cemented to the first permanent molars. The wire passes along the buccal and labial sulci of the dentition, so that the labial portion sits in front of the lower incisors (Fig. 11.3). The wire can be encased in acrylic to increase its dimensions and is positioned so that the pressure normally applied to the mandibular dentition from the lower lip and cheeks is now applied to the appliance. This results in:
These appliances are most effective before the lower second permanent molars erupt or if they are extracted; however, as they act to allow passive expansion of the lower arch dentition, following removal relapse is common without permanent retention.
Interproximal enamel reduction
The removal of enamel from the interproximal regions can also be used to generate up to 1-mm of space per contact point in the buccal segments and 0.75-mm in the labial segments (Sheridan, 1985). This can be an effective way of gaining a precise amount of space in mildly crowded cases with no apparent long-term damage to the teeth (see Fig. 7.19).
Active arch expansion
The active expansion of teeth is only recommended in the maxillary arch in the presence of a crossbite and in these cases a small amount of space can be generated for the relief of crowding. A variety of appliances for expanding the lower dentition to create space in the arch have been described. However, the instability of these procedures, particularly across the intercanine region, makes this practice unsatisfactory.
Moderate crowding
Unless the labial segments are to be proclined significantly, a moderate space requirement usually dictates the need for extractions. The extraction choice is dependent upon the position of the crowding and the anchorage requirements to achieve the treatment aims, particularly in relation to a need for incisor retraction. If there is an increased overjet to reduce as well as crowding, the space required necessitates the removal of teeth as far forward in the arch as possible, which normally means first premolars. If incisor retraction is undesirable, second premolars should be extracted.
By timing extractions appropriately, significant alignment can result without active orthodontic treatment, especially if first premolars are being extracted to relieve labial segment crowding only. In the maxillary arch the canines often erupt buccally; if first premolars are removed as the canines erupt, they will move distally and erupt into the line of the arch. In the mandibular arch, if the canines are mesially angulated, removal of first premolars will allow some uprighting of the canines into the extraction spaces. This will relieve crowding in the labial segments and allow spontaneous alignment of labiolingually displaced teeth (Stephens, 1989). Rotated teeth are less likely to align without active treatment. All spontaneous alignment will occur in the first six months following extraction and after this, fixed appliances are often required to fully align the teeth. However, well-timed extractions can result in a shorter overall treatment duration and occasionally negate the need for further treatment.
Severe crowding
If the crowding is severe, extraction is almost always necessary and often in combination with anchorage support. This is most important in the maxillary arch where there is a greater tendency for the buccal teeth to move mesially and hence space to be lost. Various techniques for anchorage support are available and these are described in Chapter 5.
If more space is required than can be provided by the loss of premolars, not only does anchorage need to be supported but extra space will need to be created. This can be done by distalization of the buccal segments using extraoral traction or a temporary anchorage device (TAD), or occasionally by the extraction of more than one tooth per quadrant (Fig. 11.4).
Spacing
The main cause of spacing in the dental arches is a discrepancy of tooth size in relation to arch length. This can be the result of localized or generalized microdontia, hypodontia or an increased jaw dimension.
Tooth size–arch length discrepancy
One of the commonest manifestations of a tooth size–arch length discrepancy is a midline diastema in the maxilla, often associated with diminutive lateral incisors. A small midline diastema is often seen during normal dental development prior to eruption of the maxillary canines, but this will usually close on eruption of these teeth. However, a larger diastema can persist into the permanent dentition and can be a cause of concern to the patient. Fixed appliances are usually required to close the space, possibly with some buildup of the adjacent teeth if they are small.
The labial frenum has been considered to be a primary aetiological factor in the persistent midline diastema, due to the insertion of fibrous tissue into alveolar bone between the central incisors, and frenectomy suggested if the diastema is going to be closed (Edwards, 1977). However, this does not result in greater closure or a reduced potential for the diastema to reopen in the longer term following active treatment. Commonly, a frenum will remodel superiorly on closure of the space, and therefore if a frenectomy is performed, it can be carried out after the diastema is closed (Bergstrom et al, 1973; Shashua & Artun, 1999). For those cases where the frenum does not remodel and is unsightly or is causing problems, frenectomy is indicated. The closure of any diastema, irrespective of adjunctive surgical procedures, will be very prone to open up again after treatment and will require permanent retention.
Hypodontia
With the exception of third molars, hypodontia most commonly affects the maxillary lateral incisor and mandibular second premolar teeth in most populations. Localized hypodontia, when only one or two of these teeth are missing, is often encountered and commonly associated with spacing in the dental arches. Generally there are two treatment options:
Maxillary lateral incisors
Whether the space is opened or closed for congenitally absent maxillary lateral incisors depends primarily upon the underlying malocclusion and whether space requirements in the lower arch justify the need for extraction. The size, shape and colour of the adjacent canine is also important, although this can be modified. General guidelines for management of congenitally absent maxillary incisors include:
Space closure
When planning the substitution of a maxillary lateral incisor with a canine, this tooth may need to be adjusted to optimize the aesthetic result (Fig. 11.5) and there are several ways this can be achieved (Table 11.1). The first premolar distal to the canine should also be slightly rotated in a mesiopalatal direction to hide the palatal cusp and increase the amount of labial surface on show anteriorly to more accurately mimic a canine.

Figure 11.5 Maxillary canines substituting for the lateral incisors.
On the left, there has been no modification of the canines. On the right, the crown tips have been built up with composite.
Table 11.1 Optimizing dental aesthetics when a maxillary canine is substituting for a lateral incisor
Space creation
Creating space for a missing maxillary lateral incisor will mean that the patient is reliant upon a prosthesis for the rest of their life and it is important that they understand the implications of this. Generally, the choice of prosthesis will be between an adhesive bridge or implant (Fig. 11.6). In the younger patient a simple denture or retainer incorporating the tooth can provide a useful temporary prosthesis. In patients where implant replacement is being considered, careful planning is required to ensure adequate bone and space are available (Table 11.2). Unless sufficient space already exists in the arch, space will actively need to be created. This usually involves fixed appliances and the use of compressed coil springs.

Figure 11.6 Replacement of the maxillary lateral incisors with adhesive bridges (left panels). Replacement of the UR1 and UR2 with implant restorations (right panels).
Table 11.2 Considerations when creating space for the implant replacement of missing teeth
| Care must be taken that adequate space is created between the roots of adjacent teeth. This invariably requires bodily movement and fixed appliances. In addition, enough bone must be present buccolingually. • Implants cannot be placed until around 18 years of age when vertical alveolar bone growth has ceased; otherwise, the implant and supragingival restoration will appear to submerge.
• If space for the prosthetic tooth is created too early and retained, there will be a reduction in width in the alveolus especially on the labial side, potentially compromising the position of the implant (Beyer et al, 2007).
|
Mandibular second premolars
The aesthetic implications of congenitally absent mandibular second premolars are less important than those associated with the maxillary lateral incisor; however, they also require careful management.
Generalized hypodontia
Where there is more than one missing tooth in each quadrant, treatment becomes more complex and will involve space redistribution with fixed appliances and prosthetic replacement of missing teeth. This treatment needs to be planned and executed within a multidisciplinary specialist team. Depending on how many teeth are missing and their position, anchorage management can be a problem, although recent advances in the use of temporary anchorage devices can help overcome this (Fig. 11.7). There is also an association between hypodontia and microdontia, meaning that existing teeth may require buildup to achieve the aesthetic and occlusal aims of treatment.
Anteroposterior problems
Anteroposterior problems usually manifest as an increased or reverse overjet, where there is a discrepancy between the dental arches. Protrusion of both upper and lower dentitions will result in bimaxillary protrusion or proclination. Conversely, retroclination of the dentition can result in bimaxillary retrusion, development of a class II division 2 incisor relationship and an increased overbite (discussed in vertical problems).
Increased overjet
An increased overjet is associated with a class II malocclusion and there are essentially two options for its reduction:
Which option is chosen will depend on a number of factors, which relate primarily to the skeletal and soft tissue pattern, and patient age:
Mechanotherapy for reducing an overjet
The options for reducing an increased overjet range from simple incisor tipping mediated by a removable appliance, functional appliances that attempt alteration of dental and skeletal relationships, fixed appliances to tip and move teeth bodily or orthognathic surgery to reposition the jaws.
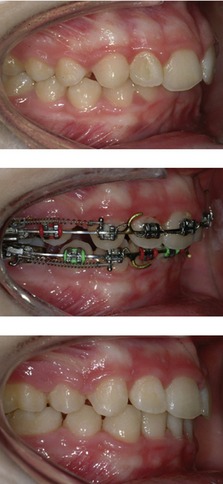
Figure 11.8 Class II division 1 malocclusion with an increased overjet treated by extraction of upper first premolars, lower second premolars and fixed appliances.
Courtesy of Saba Quereshi.

Figure 11.9 Class II division 1 malocclusion treated by extraction of upper first premolars only, treating to a class II buccal segment relationship.
When using an edgewise bracket system the incisors are moved backwards bodily on a heavy rectangular wire. This can be done using space closing loops, although when using a preadjusted system, sliding mechanics are generally used. A stretched elastomeric module or nickel titanium coil spring is connected between the terminal molar and hooks situated on the archwire in the labial segment (Fig. 11.10). This will result in the archwire shortening as it slides through the brackets in the buccal segment and is often facilitated by the use of class II elastics. If anchorage has been correctly planned, bodily retraction of the incisors and a reduction in the overjet will take place. When using the Begg or Tip-Edge appliance the overjet is reduced early in treatment by tipping the teeth with light class II elastics (Fig. 11.10). The teeth are later uprighted using auxiliary springs.
Reduced or reverse overjet
A reduced or reverse overjet is associated with a class III malocclusion and the options for correction include:
Anatomical limitations mean that there is less scope for the retraction of lower incisors and advancement of the uppers using orthodontic mechanics. Therefore, the more severe class III cases are more reliant on surgical intervention. Whether a class III case can be treated by orthodontic tooth movement alone will depend significantly on the degree of existing incisor compensation for the skeletal pattern (Table 11.3). The upper incisors are often already proclined and the lowers retroclined and for orthodontic treatment to be successful it is important that this is minimal; otherwise, it limits the potential for further movement of these teeth aimed at correcting the class III incisor relationship.
Table 11.3 Features of a class III malocclusion that would indicate it is suitable for orthodontic camouflage treatment
The stability of incisor correction will depend in part on whether a positive overbite can be achieved at the end of treatment. Stability will also depend on future adolescent growth because any increase in mandibular prognathism will tend to worsen the class III incisor relationship. If there is any doubt, it is better to monitor growth in patients with a class III malocclusion before final treatment decisions are made, which can be done using serial cephalometric lateral skull radiographs taken a year apart (Table 11.4).
Table 11.4 Skeletal factors contributing to the development of a class III malocclusiona
Mechanotherapy for correcting a class III incisor relationship
Correcting a reduced or reverse overjet with simple upper incisor tipping can be mediated by a removable appliance, whilst bodily tooth movement or lower incisor retraction will require fixed appliances. In more severe cases, orthognathic surgery to reposition the jaws will be required in combination with orthodontic treatment. The adverse nature of facial growth and difficulty in addressing the reduced maxillary or increased mandibular growth seen in many class III cases means the use of growth modification is more problematic in these patients. Functional appliances and protraction headgear, if used, are usually commenced in the mixed dentition. Options in the permanent dentition include:
Orthognathic surgery and class III malocclusion
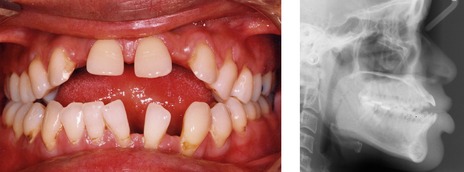
If there is a moderate or severe skeletal III skeletal base relationship, especially if the lower face height is increased and there is a reduced overbite, correction will almost certainly require a combination of orthodontics and surgery. A class III malocclusion is usually not due to a single factor, but a combination of morphological traits; therefore one surgical procedure does not fit all, and the surgical plan will need to be tailored to each individual case (see Table 11.4). There is also the tendency for a class III malocclusion to worsen with age, as mandibular growth persists. Surgery should be delayed until all adolescent growth has ceased, which will be the late teens. This does not mean that a crowded maxillary arch cannot be treated in the interim if this is a concern to the patient or teeth are ectopic (Fig. 11.12), even if it involves extractions. If the upper labial segment is left in the correct position in relation to the dental base it will not compromise any further surgical treatment although the patient will not have an ideal incisor relationship until definitive treatment is carried out. In the mandibular arch, extractions are best avoided in growing patients who look like they may need orthognathic surgery. Any retroclination of the lower labial segment will need to be undone as part of the presurgical orthodontic preparation and this is difficult following mid-arch extractions without reopening the extraction sites.

Figure 11.12 A 14 year-old class III case with impacted maxillary canines (left panel). The canines were aligned with a fixed appliance following the extraction of upper first premolars (right panel). No attempt was made to camouflage the underlying malocclusion and a reverse overjet was created. Once facial growth is complete, fixed appliances will be used to achieve full decompensation and orthognathic surgery carried out to definitively correct the malocclusion
(Courtesy of Poh Then).
Bimaxillary proclination
Bimaxillary proclination or protrusion occurs when both the maxillary and mandibular incisor dentitions are perceived to be forwards in relation to their dental bases and the cranial base. It can occur in relation to an underlying skeletal discrepancy, with an associated increase or reduction in the overjet. If the skeletal base relationship is class I, the overjet is often within a normal range despite the labial segment proclination. As the incisors are proclined there will be a tendency to a reduced overbite and in extreme cases an anterior open bite.
Bimaxillary protrusion is a common finding in patients of African-Caribbean and Chinese descent and should therefore be considered part of the normal clinical spectrum of variation in these patients. However, in extreme cases it can cause unacceptable protrusion and incompetence of the lips, for which treatment is sought. This will usually involve retraction of the anterior teeth, necessitating mid-arch extractions and the use of fixed appliances. Using round wires and allowing the teeth to tip means that even very proclined teeth can be uprighted, which will improve lip competence and profile. However, as the teeth occupy a position of balance between the pressures from the tongue on one side and the lips and cheek on the other, any significant change in the position of the incisors will be unstable. Therefore permanent retention is usually required.
Vertical problems
Vertical problems usually manifest as either an increase or decrease in the incisor overbite. This can range from a small increase or decrease in either direction to an increased and complete overbite, or frank open bite.
Increased overbite
An increased overbite occurs when the incisors have erupted past each other and is often, although not always, associated with reduced vertical facial proportions. An increased overbite is a common feature of class II division 2 malocclusion and its reduction will be necessary to establish a class I incisor relationship.
It is much easier to correct an increased overbite in a growing patient because growth of the mandibular condyles can help compensate for any posterior dental extrusion that may be used to facilitate overbite reduction. In addition, correction of the inter-incisal angle is important for the stability of overbite reduction, as the establishment of an occlusal stop is essential to prevent the incisors from erupting past each other and the overbite increasing again following treatment. This is especially relevant for class II division 1 cases associated with proclined upper incisors because unless maxillary incisor inclination is corrected, an occlusal stop will not be established and the overbite will relapse (Houston, 1989) (Fig. 11.13). Management of deep overbite in cases with a low maxillary–mandibular planes angle is also made easier with a non-extraction approach. If teeth are extracted as space is closed towards the end of the treatment, overbite control becomes difficult as the incisors will tend to upright, which can lead to the overbite deepening again.

Figure 11.13 Creating the correct interincisal relationship to avoid relapse of overbite reduction following treatment.
Simple tipping of the upper incisors to reduce an increased overjet in the presence of an increased overbite is not appropriate treatment because no occlusal stop is created. The upper incisors can retrocline and the lower incisors over-erupt, resulting in a worsening of the overbite (upper panel). The key to stable overbite reduction is moving the upper incisor root into the correct position behind the plane of the lower incisor edge (lower panel).
Mechanotherapy for correcting an increased overbite
There are essentially four ways to reduce a deep overbite associated with an increased curve of Spee in the lower arch using conventional orthodontic mechanics: buccal segment extrusion (relative incisor intrusion in a growing patient), incisor intrusion or incisor proclination (Fig. 11.14).
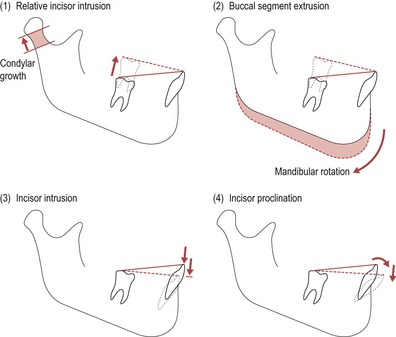
Figure 11.14 Levelling the curve of Spee in the mandible.
(1) Relative incisor intrusion. (2) Buccal segment extrusion. (3) Incisor intrusion. (4) Incisor proclination.
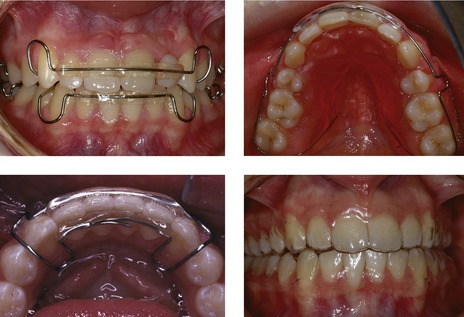
Buccal segment extrusion can be achieved using a removable appliance with a flat anterior bite plane. The appliance opens up the bite and allows eruption of the buccal segments, levelling the curve of Spee and reducing the overbite (Fig. 11.15). Many functional appliances have a similar bite-plane effect if the acrylic of the appliance is removed over the lower premolars and molars to allow eruption of these teeth.
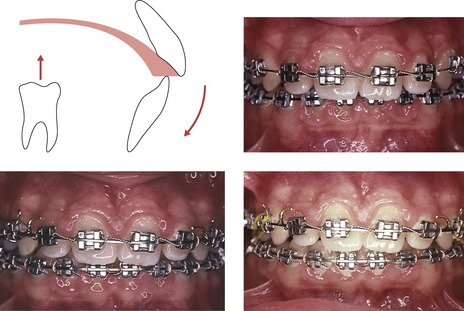
Figure 11.15 Overbite reduction can be achieved with a removable appliance by incorporating a flat anterior bite plane (upper left panel). Fixed appliances can reduce an increased overbite by placing a reverse curve of Spee in the lower archwire (upper right, lower left and lower right panels showing progressive overbite reduction; and see Fig. 9.30).
Using an edgewise-fixed appliance with a continuous archwire can also achieve buccal segment extrusion, although this will also be accompanied by some incisor intrusion. These changes can be accentuated by using a rectangular stainless steel archwire with a reverse curve of Spee (Fig. 11.15). The lower second molars are generally included to increase vertical anchorage and aid these movements. Care must be taken, as there will also be a tendency for the lower incisors to procline, which will assist bite opening, but may not desirable or stable. Therefore it is often necessary to place lingual crown torque in the labial section of the archwire to counter this. The judicial use of class II inter-maxillary elastics will also assist in overbite reduction as the vertical component of force will tend to extrude the mandibular molars. Class II inter-maxillary elastics are integral in the Begg and Tip-Edge appliances which aim to reduce an increased overbite early on in treatment by the use of rigid round steel arches that bypass the premolar teeth to create a long range of action and light forces. An intrusive force is applied to the labial segments from the archwire by tip-back or anchor bends placed into the molar tubes and an extrusive force applied to the molars by the use of light class II elastics. Together this is very effective at reducing an increased overbite (see Fig. 9.29).
Anterior open bite
An anterior open bite is associated with a lack of vertical incisor overlap. It may be localized, affecting only a few teeth; or it may be caused by a divergence of the skeletal planes. Treatment is often required because the patient has trouble incising food due to the lack of an anterior occlusion. Speech may also be a concern, as an anterior open bite can be associated with lisping. While treatment can improve both the occlusion and function, there is no guarantee that speech will improve as speech patterns are established early in life, long before establishment of the permanent dentition.
When planning treatment it is important to establish the aetiology (Table 11.5). In the presence of an anterior open bite, the tongue will come forwards between the incisors to fill the gap and create an anterior seal during swallowing. For many years it was thought that this tongue activity or ‘tongue thrust’ was the primary aetiological factor in the development of anterior open bite. It is now recognized that in the vast majority of cases this is an adaptive behaviour. If the main aetiological factor is a digit-sucking habit, as long as this ceases at an appropriate time, there can be complete and stable resolution of the anterior open bite. The main problems arise with anterior open bites that are skeletal in origin.
Table 11.5 Aetiology of anterior open bite
|
• Secondary to local pathology such as a supernumerary tooth preventing eruption of the maxillary incisors;
|
Mechanotherapy to correct an anterior open bite
There are essentially three ways that a skeletal open bite can be treated:

Figure 11.17 Anterior elastic to close an anterior open bite during the final stages of treatment with a fixed appliance.
Table 11.6 Treatment modalities to correct an anterior open bite
In a growing child, the use of high-pull headgear, especially when there is a skeletal class II base relationship, will control posterior vertical growth of the maxilla. This will theoretically redirect mandibular growth in a more anterior than vertical direction. The headgear can be run directly either to bands on the upper first molars or to a removable appliance with posterior capping (an intrusion splint) (Fig. 11.18). Headgear can also be used in combination with a functional appliance to try and correct an increased overjet when there is a reduced overbite and a vertical growth pattern. The main problem with this approach is that vertical growth continues throughout adolescence and therefore to be truly effective, headgear will have to be worn until adolescent growth has stopped.
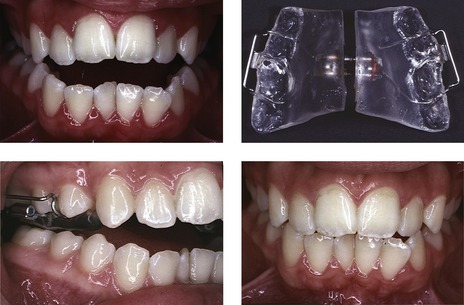
Figure 11.18 Anterior open bite treated with high-pull headgear attached to a buccal intrusion splint.
In adults growth will have essentially ceased. Therefore, treatment of an anterior open bite will necessitate intrusion of the buccal segments. Although implants and microscrews potentially provide an exciting new way of achieving this, at present the most predictable and stable way of correcting an anterior open bite in an adult is by surgical impaction of the maxilla (see Fig. 12.27). This will reduce the posterior dental height, allowing the mandible to auto-rotate and close the anterior open bite.
Transverse problems
The displacement of a tooth palatally in the maxilla or buccally in the mandible may result in a localized crossbite and is usually a reflection of crowding. Although a removable appliance with a palatal spring can be used to tip these teeth buccally, if space is created the tooth will usually need to be bodily moved, necessitating the use of fixed appliances. When there is a transverse discrepancy between the dental arches, a crossbite can affect all the teeth in the quadrant.
Buccal posterior crossbite
Posterior crossbite can be unilateral or bilateral, depending upon whether one or two sides of the dental arch are affected.
The greater the skeletal contribution to a crossbite, the more difficult it is to correct. A skeletal crossbite with no associated displacement of the mandible on closing is often best accepted, especially if it is bilateral. Attempting orthodontic correction in these cases may result in the creation of a unilateral crossbite with a displacement, which is occlusally less acceptable. As it is very difficult to constrict the mandibular arch, any treatment will usually involve expansion of the maxillary arch. Various techniques can be used to achieve this, but all will produce considerable tipping of the maxillary buccal teeth, with the exception of surgical expansion. On expansion, there will be a relative extrusion of these palatal cusps as the teeth are tipped. This can be a problem in patients with a reduced overbite, as this will worsen due to displacement of the mandible downwards and backwards (Fig. 11.19). Therefore caution should be exercised when expanding patients with an increased vertical pattern of growth and the use of techniques to control this, such as high-pull headgear in combination with expansion, should be considered.

Figure 11.19 Increase in the vertical dimension and reduction in overbite following expansion of the maxillary dental arch.
Mechanotherapy to correct a posterior crossbite
The following techniques can be used to produce maxillary expansion:
Irrespective of what type of expansion is undertaken, relapse potential is high. This can be reduced by establishing good intercuspation of the buccal dentition at the end of treatment, but a long period of retention will usually be required. Vacuum-formed retainers, if used, should be reinforced with a wire placed in the palate.
Lingual posterior crossbites
Localized lingual posterior crossbites can also occur, particularly when crowding causes a maxillary premolar to be displaced buccally. Complete lingual posterior crossbites are less common and usually associated with an underlying skeletal class II discrepancy. In a child, a functional appliance can be used to correct this relationship, and by doing so this may help correct the lingual crossbite. In an adult, fixed appliances can be used with cross-elastics and an expanded mandibular archwire. However, orthodontic expansion of the mandibular arch to any significant extent is problematic. If there is a skeletal class II base relationship, mandibular advancement surgery may help correct the lingual crossbite. Surgical techniques using distraction osteogenesis for widening the mandibular arch have also been described.
Relapse and retention
Following active orthodontic treatment the majority of patients will require a period of retention. This is a phase of treatment aimed at stabilization and maintenance of the achieved orthodontic correction, allowing settling of the occlusion and preventing or minimizing subsequent relapse.
Relapse
Relapse is a partial or full return of the pre-treatment features of a malocclusion following active treatment. Numerous longitudinal studies have shown the re-emergence of crowding, especially of the lower incisors following orthodontic treatment (Little et al, 1981, 1988). This is an almost universal finding that can occur many years following treatment, with a large degree of individual variation. It is impossible to gauge susceptibly in individual cases, although greater incisor irregularity may be expected following non-extraction expansion of the lower arch, rather than treatment involving premolar extraction (Little et al, 1990). Other occlusal features especially prone to relapse following treatment include rotations and spacing. Overall, a number of factors can potentially contribute to orthodontic relapse.
Periodontal and gingival tissues
Following orthodontic tooth movement, the tissues of the periodontal ligament and gingivae remodel to the new position of the tooth. Whilst collagen fibres in the periodontal ligament take between three to four months to remodel, those in the gingival tissues take slightly longer, at around six months. The slowest turnaround occurs in the elastic supracrestal fibres, which take up to one year. This has important implications for teeth that were rotated, as this slow remodelling is implicated in the very high relapse rate for rotational correction. The retention regime for these teeth can be supplemented by supracrestal fibrotomy (or pericision), a surgical procedure involving sectioning of the supracrestal fibres. This is carried out under local anaesthetic, once the rotation has been orthodontically corrected. A surgical blade is inserted into the gingival sulcus, severing the supracrestal and transeptal fibres. It has been shown to reduce rotational relapse in the maxillary incisor region with no loss of periodontal attachment (Edwards, 1988). However, this procedure should not be done on the mid-labial portion of any tooth with a narrow zone of attached gingivae or thin plate of alveolar bone, particularly the lower incisors. An alternative technique is simply to divide the interdental papilla. Overcorrection of rotated teeth early in treatment and maintaining them in their new position for a significant period before appliances are removed is also recommended which will allow for some relapse.
Soft tissues
To a large extent the soft tissues define the limitations of orthodontic tooth movement. Any change in the position of the teeth can move them out of the zone of soft tissue balance and increase the chance of relapse. For this reason the arch form, particularly of the lower arch, is not amenable to any significant change. If expanded during treatment, especially across the intercanine width, this will be very prone to relapse. Similarly, labiolingual movement of the lower incisors to any great degree is notoriously prone to relapse.
Vertically, the lower lip position is very important in the stability of overjet reduction. If the lips are competent following treatment and the lower lip rests labially to the upper incisors, there is greater stability. This is in part dependent on growth of the soft tissues, which grow vertically more than the underlying skeletal bases during the preadolescent period. This results in an increase in lip competence, especially in boys whose lips grow later and to a greater extent than girls (Nanda, 1990).
An endogenous tongue thrust is primarily neurological in origin, resulting in anterior position of the tongue and excessive force exerted on swallowing. Although this phenomenon is real, it is very rare and most abnormal tongue activity is adaptive. To create an anterior seal on swallowing with an anterior open bite, the tongue will invariably come forwards to fill the gap. If the anterior open bite is corrected, the tongue activity is normalized and the result will be stable. However, if a true tongue thrust is present, no amount of treatment will guarantee stability, as the primary aetiological factor will remain (Fig. 11.22).
Occlusion
Teeth retained by the occlusion are often stable. Correction of an anterior crossbite with a positive overbite following treatment requires no retention. It is also a widely held belief that a well-interdigitated class I occlusion aids stability at the end of treatment and there is some evidence for this (Kahl-Nieke et al, 1995). This is certainly true for overbite reduction and buccal segment correction but there is little evidence that it will prevent relapse or reappearance of incisor crowding. Occlusal forces themselves act in an anterior direction, and have been postulated to be causative in the development of lower incisor crowding (Southard et al, 1990); however, the short duration of these forces makes this unlikely.
Growth
Facial growth continues throughout life, generally in the same direction as that occurring during adolescence, but to a much smaller degree (Behrents, 1985). Facial growth is not linear but rotational, especially mandibular growth. This can lead to forces being placed on the teeth from either soft tissues or the occlusion as the dentition compensates to maintain the occlusal position. This can manifest most notably as late lower incisor crowding, as the lower labial segment uprights to compensate for mandibular growth. This is thought to be a major factor in late lower incisor crowding seen in both orthodontically treated and untreated individuals.
In class III malocclusion, mandibular growth can result in the reappearance of a reverse overbite following early correction. This is one of the main reasons for monitoring growth in class III cases during adolescence before final treatment decisions are made.
Retention
Planning the retention phase of orthodontic treatment is part of the treatment planning process and allows the patient to make an informed decision about their treatment (Box 11.1). Retention should be discussed prior to the commencement of active treatment. The following factors need to be considered:
Box 11.1 Managing long-term retention
When fitting retainers for patients, often following at least 18 months of treatment, the first question they will ask is ‘How long will I have to wear retainers for?’ The honest answer is for as long as they want to keep their teeth perfectly straight. Not all patients will exhibit relapse or reappearance in crowding, especially in the lower labial segment, but from the evidence available, it is not possible to predict who these patients will be. Many patients have very high expectations of treatment and even some minor deterioration in the alignment of the teeth will be unacceptable. Therefore, long-term retention is recommended for all patients who are concerned about any changes occurring following removal of their appliances.
The next decision is whether to use a removable or fixed retainer (Atack et al, 2007). Even with fixed retainers, some reappearance in crowding can appear in the lower labial segment. Fixed retainers also have a high failure rate and unfortunately the patient will often only notice a breakage when the lower incisors start moving. In some patients they can also cause problems with oral hygiene. Removable retainers, if compliance is good, will provide as effective retention as fixed retainers, and if worn part-time, are generally well tolerated. In addition, any breakages or problems with appliance fit are usually apparent to the patient before relapse has occurred. However, compliance is the unpredictable factor. If we accept that the choice for long-term retention is made in partnership with the patient, this is not necessarily a negative thing. It will give responsibility to the patient for their retention and ultimately how long they maintain it. It will also allow for the patient’s general practitioner to monitor the retention and provide further retainers as required.
Original malocclusion
If the original malocclusion was severe, a small amount of relapse following treatment may be acceptable, as the overall aesthetic improvement will remain good. However, if the patient only presented with a mild malocclusion, any relapse may be unacceptable. This is especially true when mild labial segment crowding is treated. Numerous strategies for improving the stability of lower incisors following alignment have been devised. One of these is interproximal enamel reduction. Removing a small amount of enamel creates broader, flatter contact points between these teeth and theoretically reduces the chance of them slipping past each other and becoming crowded (Boese, 1980a, b). Despite these added precautions, all patients need to be made aware of the relapse potential prior to beginning treatment and the necessity for long-term or even permanent retention.
Growth pattern
Following treatment the original growth pattern will re-impose itself and continue to a greater or lesser degree throughout life. This is true for both sagittal and vertical growth. Thus, a corrected class III incisor relationship will relapse if there is unfavourable mandibular growth and an anterior open bite, which will reappear with continued vertical growth. Retention should therefore be involved in maintaining the skeletal correction. If a functional appliance or headgear was used to control growth during the active treatment phase it should ideally be continued during the retention phase, at least until adolescent growth is complete. This of course is very much compliance-based and provides a good argument against starting treatment too early where there is a skeletal discrepancy.
Type of retainers
Retainers are appliances designed to maintain the position of the teeth following orthodontic treatment. Retainers can be either removable or fixed.
Removable retainers
Removable retainers can be taken out of the mouth by the patient and therefore rely on good compliance. They are generally easy to maintain and do not compromise oral hygiene although like all removable appliances, they can affect speech. Although many different types of retainer have been described, the main types include the following:
Fixed retainers
Fixed retainers usually consist of a wire cemented or bonded to the teeth, which the patient cannot remove. These retainers are used when long-term or permanent retention is required, particularly for the lower incisors, and the wire usually extends from canine to canine. They can also be used for the upper incisors to prevent reopening of a midline diastema, but a higher failure rate can occur in this region, especially with an increased overbite. Early designs were made from plain wires with steel pads at each end bonded to the canines. This design was very good at maintaining the lower intercanine width but less effective at preventing rotational relapse of incisors not bonded to it. Later fixed retainers consisted of flexible multistrand stainless steel wires bonded to the lingual surfaces of the teeth with composite (Zachrisson, 1977) (Fig. 11.24). These are well tolerated, allow some physiological movement of the teeth, do not compromise on aesthetics and can provide excellent retention. They do not interfere with speech and are less reliant upon compliance than removable retainers. Fixed retainers do not seem to produce any long-term periodontal problems, although calculus can build up around them, particularly in the lower incisor region. Their placement is time-consuming and technique-sensitive and a back-up removable retainer should also be supplied to the patient to preserve tooth position if the fixed retainer fails.
Duration of retention
The duration of retention required following orthodontic treatment is variable. However, the only way to permanently guarantee stability of tooth position is to retain it indefinitely.
No retention
This is the exception rather than the rule, and is only applicable in cases where the occlusion will hold the correction or where no active treatment was undertaken:
Medium-term retention
Medium-term retention usually means a period that allows reorganization of the soft tissues and periodontal ligament, and for adolescent growth and dental development to be completed, including eruption of the third molars. In reality this means retention into the late teenage years or early twenties and is usually indicated in most routine cases. Most retention regimes are fairly arbitrary and there is no evidence that there is any great difference in a period of full-time as opposed to part-time or nocturnal wear following removal of the active appliances. A period of full-time wear may result in less chance of the patient forgetting to wear the retainer, but when compliance is not a concern, removable retainers can be worn on a part-time basis from the end of active treatment.
Permanent retention
The only way to prevent any change in tooth alignment following active treatment is by long-term or even permanent retention. Certain occlusal traits are very prone to relapse following correction and these include:
In certain situations as part of the treatment plan, teeth may be purposely moved into areas where they will be prone to relapse:
In such cases, permanent retention will be needed to maintain the position of the teeth usually in the form of a fixed retainer. It is important that this is discussed with the patient before they commence treatment and it should be part of the consent process.
McLaughlin RP, Bennett JC, Trevisi HJ. Systemised Orthodontic Treatment Mechanics. St Louis: Mosby; 2001.
Melrose C, Millett DT. Towards a perspective on orthodontic retention? Am J Orthod Dentofacial Orthop. 1998;113:507-514.
Proffit WR, Fields HW, Sarver DM. Comtemporary Orthodontics, 4th edn. St Louis: Mosby-Elsevier; 2007.
Atack N, Harradine N, Sandy JR, et al. Which way forward? Fixed or removable lower retainers. Angle Orthod. 2007;77:954-959.
Atherton GJ, Glenny AM, O’Brien K. Development and use of a taxonomy to carry out a systematic review of the literature on methods described to effect distal movement of maxillary molars. J Orthod. 2002;29:211-216. discussion 195–196
Behrents RG. The biological basis for understanding craniofacial growth during adulthood. Prog Clin Biol Res. 1985;187:307-319.
Bergstrom K, Jensen R, Martensson B. The effect of superior labial frenectomy in cases with midline diastema. Am J Orthod. 1973;63:633-638.
Beyer A, Tausche E, Boening K, et al. Orthodontic space opening in patients with congenitally missing lateral incisors. Angle Orthod. 2007;77:404-409.
Boese LR. Fiberotomy and reproximation without lower retention 9 years in retrospect: part II. Angle Orthod. 1980;50:169-178.
Boese LR. Fiberotomy and reproximation without lower retention, nine years in retrospect: part I. Angle Orthod. 1980;50:88-97.
Brennan MM, Gianelly AA. The use of the lingual arch in the mixed dentition to resolve incisor crowding. Am J Orthod Dentofacial Orthop. 2000;117:81-85.
Edwards JG. A clinical study: the diastema, the frenum, the frenectomy. Oral Health. 1977;67:51-62.
Edwards JG. A long-term prospective evaluation of the circumferential supracrestal fiberotomy in alleviating orthodontic relapse. Am J Orthod Dentofacial Orthop. 1988;93:380-387.
Guyer EC, Ellis EE3rd, McNamara JAJR, et al. Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56:7-30.
Houston WJ. Incisor edge-centroid relationships and overbite depth. Eur J Orthod. 1989;11:139-143.
Kahl-Nieke B, Fischbach H, Schwarze CW. Post-retention crowding and incisor irregularity: a long-term follow-up evaluation of stability and relapse. Br J Orthod. 1995;22:249-257.
Kim YH. Anterior openbite and its treatment with multiloop edgewise archwire. Angle Orthod. 1987;57:290-321.
Little RM, Riedel RA, Artun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423-428.
Little RM, Riedel RA, Stein A. Mandibular arch length increase during the mixed dentition: postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990;97:393-404.
Little RM, Wallen TR, Riedel RA. Stability and relapse of mandibular anterior alignment-first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981;80:349-365.
McNamara JAJR. Components of class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51:177-202.
Nanda SK. Growth patterns in subjects with long and short faces. Am J Orthod Dentofacial Orthop. 1990;98:247-258.
Ng J, Major PW, Heo G, Flores-Mir C. True incisor intrusion attained during orthodontic treatment: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2005;128:212-219.
Ostler MS, Kokich VG. Alveolar ridge changes in patients congenitally missing mandibular second premolars. J Prosthet Dent. 1994;71:144-149.
Rowland H, Hichens L, Williams A, et al. The effectiveness of Hawley and vacuum-formed retainers: a single-center randomized controlled trial. Am J Orthod Dentofacial Orthop. 2007;132:730-737.
Sandler J, Benson PE, Doyle P, et al. Palatal implants are a good alternative to headgear: a randomized trial. Am J Orthod Dentofacial Orthop. 2008;133:51-57.
Sfondrini MF, Cacciafesta V, Sfondrini G. Upper molar distalization: a critical analysis. Orthod Craniofac Res. 2002;5:114-126.
Shashua D, Artun J. Relapse after orthodontic correction of maxillary median diastema: a follow-up evaluation of consecutive cases. Angle Orthod. 1999;69:257-263.
Sheridan JJ. Air-rotor stripping. J Clin Orthod. 1985;19:43-59.
Southard TE, Behrents RG, Tolley EA. The anterior component of occlusal force. Part 2. Relationship with dental malalignment. Am J Orthod Dentofacial Orthop. 1990;97:41-44.
Stephens CD. The use of natural spontaneous tooth movement in the treatment of malocclusion. Dent Update. 1989;16:337-338.
Zachrisson BU. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod. 1977;71:440-448.