Aseptic Techniques
After completing this chapter, the student should be able to do the following:
 Describe how to limit the spread of disease agents from the hands to environmental surfaces.
Describe how to limit the spread of disease agents from the hands to environmental surfaces.
 Describe how to limit the spread of disease agents from dental aerosols and spatter.
Describe how to limit the spread of disease agents from dental aerosols and spatter.
 Describe the proper use of disposable items.
Describe the proper use of disposable items.
 Describe the importance of the high-volume evacuator in infection control.
Describe the importance of the high-volume evacuator in infection control.
 Describe how to change a high-volume evacuator trap safely.
Describe how to change a high-volume evacuator trap safely.
 Describe the proper use of the saliva ejector.
Describe the proper use of the saliva ejector.
 Describe the use of preprocedure mouth rinses.
Describe the use of preprocedure mouth rinses.
Some infection control techniques do not fall under the major infection control categories discussed in previous chapters. Collectively, they are referred to as aseptic techniques because they prevent or reduce the spread of microorganisms from one site to another, such as from patient to dental team, from patient to operatory surfaces, or from one operatory surface to another.
TOUCHING OF AS FEW SURFACES AS POSSIBLE
Gloves used for patient care are contaminated, and that contamination will be transferred to any surface touched. Thus one should touch as few surfaces as possible with saliva- or blood-coated fingers. Any surfaces that may be touched should be protected with surface covers or precleaned and disinfected (see Chapter 12). One should make every effort to dispense all items needed at chairside before patient care begins. This task reduces the need for leaving chairside with contaminated gloves, mask, and protective clothing, which may spread contamination to other parts of the office. As mentioned in Chapter 10, removal of contaminated gloves or use of an overglove before leaving chairside during patient care is the best practice. One should put on gloves or carefully remove and discard overgloves when returning to chairside. Another alternative is to have an uninvolved person retrieve items needed unexpectedly during patient care, which is particularly important during some types of surgery (e.g., implant surgery).
One should not rub eyes, skin, or nose or touch hair with contaminated, gloved hands.
MINIMIZATION OF DENTAL AEROSOLS AND SPATTER
Dental aerosols and spatter are generated during use of high- and low-speed handpieces, ultrasonic scalers, and the air/water syringe. Dental aerosols are small, invisible particles of saliva that may contain a few microorganisms and may be inhaled or remain airborne for extended periods. Aerosol particles are less than 50 μm in diameter, and the smallest ones of 5 μm in diameter can be inhaled to the depths of the lungs (air sacs or alveoli). One should remember that the average diameter of a bacterial cell is only 1 μm, and viruses are much smaller than that. Spatter consists of particles larger than 50 μm. When these particles are propelled from the patient’s mouth, they settle rapidly or land on nearby operatory surfaces or the face, neck, chest, and arms of the dental team member providing care to the patient. Minimizing the generation of dental aerosols and spatter by use of high-volume evacuation and the rubber dam and by proper positioning of the patient’s head reduces the spread of microbes from the patient’s mouth.
HIGH-VOLUME EVACUATION
High-volume evacuation (HVE) during use of rotary equipment and the air/water syringe greatly reduces the escape of salivary aerosols and spatter from the patient’s mouth, which reduces contamination of the dental team and nearby surfaces. One should clean the HVE system at the end of the day by evacuating a detergent or water-based detergent-disinfectant through the system. One should not use bleach (sodium hypochlorite) because this chemical can destroy metal parts in the system. One should remove and clean the trap in the system periodically. A safer approach, however, is to use a disposable trap. These traps may contain scrap amalgam that should be disposed of properly. The dental team member must wear gloves, masks, protective eyewear, and protective clothing when cleaning or replacing these traps to avoid contact with patient materials in the lines from splashing and direct contact. Disinfection of the trap by evacuating some disinfectant-detergent down the line followed by water is best before one cleans or changes the trap.
SALIVA EJECTOR
Research has shown that in one in five cases, previously suctioned fluids might be retracted into the patient’s mouth when a seal around the saliva ejector is created (i.e., when the patient closes his or her lips around the saliva ejector tip). The seal can cause a type of “suck back” or reverse flow in the vacuum line that might allow the contents of the line to reach the patient’s mouth. Although disease spread if this occurs has not been demonstrated, reverse flow should not be allowed to happen. Thus one should not tell patients to close their lips around the ejector and “spit” into the tip. Alternatively, some disposable saliva ejector tips now have a small hole in the side that relieves the pressure when the tip is closed off preventing reverse flow.
USE OF THE RUBBER DAM
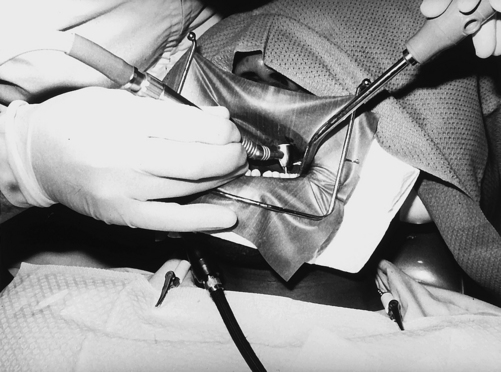
Reduction in microorganisms escaping a patient’s mouth in aerosols or spatter can approach 100% with proper use of the rubber dam, depending on the type and site of the intraoral procedure. Simultaneous use of HVE and the rubber dam provides the best approach to minimize dental aerosols and spatter (Figure 14-1). A sealant is also available for placement at the rubber dam–tooth interface to reduce further the leakage of saliva into the operative site.
Because the rubber dam reduces the amount of saliva present at the operative site, less saliva is available for retraction into water spray handpieces or air/water syringes if antiretraction valves in the dental unit fail.
Even though the rubber dam and HVE greatly reduce the salivary aerosols and spatter, one still must use gloves, mask, protective eyewear, and protective clothing when using these aseptic techniques. The rubber dam may not give a perfect seal, and microorganisms that may be present in biofilms on the inside of the dental unit water lines may be released into the flowing water and aerosolized and sprayed into the face, neck, chest, and arms of the care provider.
PREPROCEDURE MOUTH RINSE
The application of antiseptics to skin or mucous membranes before surgery or injections has been practiced for many years. The goal of such application is to reduce the number of microorganisms on the surface to prevent their entry to underlying tissues, which could cause bacteremia, septicemia, or local harmful infections.
The use of an antimicrobial mouth rinse by the patient before dental procedures is based on a similar principle of reducing the number of oral microorganisms. This reduction also lowers the number of microorganisms that may escape a patient’s mouth during dental care through aerosols, spatter, or direct contact. Thus fewer microorganisms contaminate the dental team and operatory surfaces. Although studies have not yet shown that the aseptic technique of preprocedure mouth rinsing actually prevents diseases in dental team members, studies have shown that a mouth rinse with a long-lasting antimicrobial agent (e.g., chlorhexidine gluconate, essential oils, and iodophor) can reduce the level of oral microorganisms for up to 5 hours. Use of non-antimicrobial mouth rinses allows the oral microorganisms to return to their original levels before most dental procedures are completed, thus having little infection control value.
Although a preprocedure mouth rinse can be used before any dental procedure, it may be most beneficial before a prophylaxis using a prophylaxis cup or ultrasonic scaler. During these procedures, one cannot use a rubber dam to minimize aerosol and spatter generation, and unless a hygienist has an assistant, HVE is not commonly used. The mouth rinsing may be the only approach to minimizing contamination from aerosols and spatter during such procedures.
USE OF DISPOSABLES
A disposable item is manufactured for a single use or for use on only one patient. Such items are manufactured from plastics or less expensive metals that are usually not heat tolerant or are not designed to be cleaned adequately. Thus an item that is labeled as disposable must be disposed of properly after use, and one should not attempt to preclean and sterilize or disinfect it for reuse on another patient.
From an infection control point of view, a single-use (disposable) item has major advantages over a reusable item. The disposable item absolutely prevents the transfer of microorganisms from one patient to another because the contaminated item is discarded and not reused on another patient. Another advantage is that the reusable counterpart may be difficult to clean and sterilize adequately (e.g., the lumen of a needle or the inside of the air/water syringe tip), thus increasing the risk of patient-to-patient cross-contamination. The disposable item eliminates this risk.
Disadvantages of disposables depend on the nature of the individual items but may include less efficient operation than the reusable counterpart, increased expense, and addition of nonbiodegradable materials to the environment on disposal. Determination of cost-effectiveness of disposables or reusables must include the cost of the items and also the labor dollars required to decontaminate the reusable items.
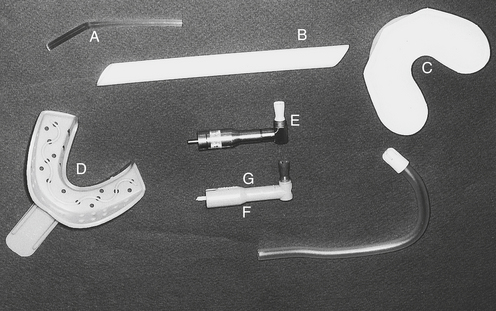
More and more disposable items are becoming available to dentistry and include injection needles, anesthetic carpules, air/water syringe tips, HVE tips, saliva ejector tips, curing light probes, certain hand instruments, prophylaxis angles, prophylaxis cups, high-speed handpieces, light handle attachments, impression trays, scalpel blades, and some burs (Figure 14-2). Other disposable items include patient care gloves, masks, gowns, some face shields, surface covers, patient bibs, sharps containers, biohazard bags, specimen containers, and vacuum line traps.
HOUSEKEEPING AND CLEANING
Dusting of surfaces or sweeping of floors in patient-care areas can distribute microorganism-laden dust particles to other surfaces unless performed with a wet cloth or wet mop. One might consider dust covers for operatory and sterilizing room surfaces over the weekend or during vacation periods. One should clean mops and cloths after use and allow them to dry before reuse, or use single-use, disposable mop heads or cloths. Mop water should contain a low-level disinfectant to keep microorganisms from building up in the water and being painted onto the floor. One should prepare the mop water fresh at least daily. The filters in air vents and furnaces require frequent changing to avoid dust buildup.
Pay particular attention to the waiting room, which offers the first impression about cleanliness of the office. Keep live and artificial plants dusted. Vacuum the carpet frequently. Make sure the chair arms, door knobs, and magazines feel clean and are not sticky. Wipe any sliding glass doors free of fingerprints. Remember that patients can’t see microbes, that but they can see dust.
Flooring, Carpeting, and Upholstery
A smooth-surface floor rather than carpeting is more appropriate for patient-care areas because of its cleanability and lesser likelihood of accumulating dust and dirt. Thus one should avoid using carpeting and cloth-upholstered furnishings in the dental operatory, laboratory, or instrument-processing areas.
OTHER ASEPTIC TECHNIQUES
During high-speed handpiece processing, one sprays a cleaner/lubricant into the drive air line and flushes excess lubricant out by connecting the dental unit air system on an air line installed in the sterilizing room. One must flush the air system so that the aerosol is not released into the air environment by flushing directly into the vacuum system or into a sink with water or a container with absorbent material that will catch the spray. Handpiece cleaning systems may become available that will minimize aerosolization.
Several aseptic techniques relate to instrument processing, as mentioned in Chapter 11. The sterilizing room should be separated into “clean” and “dirty” areas to avoid mingling of sterile and nonsterile instruments. Chemical indicators on instrument packaging also help differentiate between items that have or have not been heat processed. One should also handle and store sterile packages away from sinks in a dry area.
Unit dosing and use of a sterile retrieval system to prevent contamination of supply items were discussed in chapter 12. A key point to remember is that gloves used for patient care are contaminated and that anything touched with those gloves will also be contaminated. Only items needed for the care of a single patient should be on the bracket table, portable unit, or countertops in the operatory. All other items should be stored elsewhere until dispensed for patient care to prevent their contamination.
Barbeau, J., tenBokem, L., Guathier, C., Prevost, A.P. Cross-contamination potential of saliva ejectors used in dentistry. J Hosp Infect. 1998;40:303–311.
Cochran, M.A., Miller, C.H., Sheldrake, M.A. The efficacy of the dental dam as a barrier to the spread of microorganisms during dental treatment. J Am Dent Assoc. 1989;119:141–144.
Council on Dental Materials, Instruments and Equipment, American Dental Association. Dental units and water retraction. J Am Dent Assoc. 1988;116:417–420.
Klyn, S.L., Cummings, D.E., Richardson, B.W., Davis, R.D. Reduction of bacteria-containing spray during ultrasonic scaling. Gen Dent. 2001;49:648–652.
Miller, C.H. Dealing with disposables. Dent Prod Rpt. 2006;39:58.
Miller, C.H. Swishful thinking: Can preprocedural mouthrinsing help prevent cross-contamination? Dent Prod Rpt. 2006;39:154.
Miller, R.L., et al. Studies on dental aerobiology. II. Microbial splatter discharged from the oral cavity of dental patients. J Dent Res. 1971;50:621–625.
Watson, C.M., Whitehouse, R.L. Possibility of cross-contamination between dental patients by means of the saliva ejector. J Am Dent Assoc. 1993;124:77–80.
Review Questions
______1. Particles of oral fluids that can be inhaled into the lung air sacs are called:
______2. What is the key ingredient in a mouth rinse used for preprocedure mouth rinsing?
______3. A disposable air/water syringe tip can be used on how many patients?
______4. Use of the rubber dam will not reduce spattering of what kinds of microbes?
______5. If a patient closes her lips around the ______________, patient-to-patient cross-contamination may occur.
______6. Which of the following may generate dental aerosols or spatter?
______7. What should be done before changing or cleaning a vacuum line trap?