UPPER LIMB
1. INTRODUCTION
The upper limb is part of the appendicular skeleton and includes the shoulder, arm, forearm, and hand. It is continuous with the lower neck and is suspended from the trunk at the shoulder. It is anatomically and clinically convenient and beneficial to divide the limb into its functional muscle compartments and to review the nerve(s) and vessels supplying these compartments. Thus, for each component of the upper limb, we will focus on organizing the clinical anatomy into functional compartments and understanding how that anatomy is ideally suited for a wide range of motion, thereby allowing us to manipulate our surrounding environment.
To prepare for your study, please review the movements of the upper limb at the shoulder, elbow, wrist, and fingers, which are presented in Chapter 1, “Introduction to the Human Body.”
2. SURFACE ANATOMY
Key Landmarks
Much of the underlying anatomy of the upper limb can be appreciated by a careful inspection of the surface features (Fig. 7-1). The following surface features are of special note:
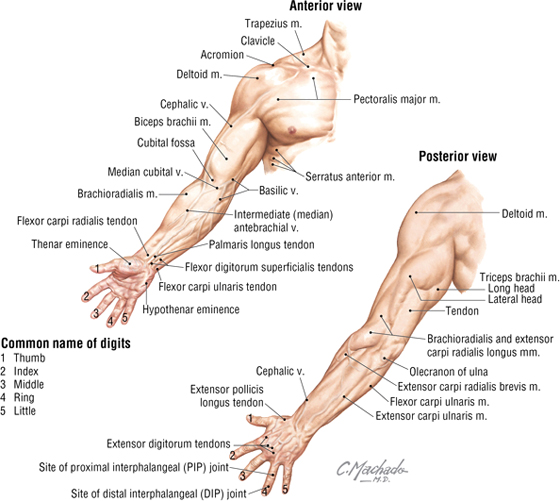
FIGURE 7-1 Key Surface Landmarks of the Upper Limb
- Acromion: attachment site of the trapezius and deltoid muscles; easily palpable
- Clavicle: long bone that lies subcutaneously throughout its length
- Olecranon: elbow and proximal portion of the ulna
- Deltoid muscle: muscle that caps the shoulder
- Flexor tendons: wrist and finger flexors that are visible at the distal anterior forearm
- Extensor tendons: wrist and finger extensors that are visible on the dorsum of the hand
- Thenar eminence: cone of muscles at the base of the thumb
- Hypothenar eminence: cone of muscles at the base of the little finger
- Dorsal venous network: veins seen on the dorsum of the hand
- Cephalic vein: subcutaneous vein that drains the lateral forearm and arm into the axillary vein
- Basilic vein: vein that drains the medial forearm and distal arm into the axillary vein
- Median cubital vein: vein that lies in the cubital fossa (anterior aspect of the elbow); is commonly used for venipuncture
As we've seen elsewhere in the body, a set of superficial and deep veins drain the upper limb. Superficial veins drain blood toward the heart and communicate with deep veins that parallel the major arteries of the upper limb (Fig. 7-2). When vigorous muscle contraction increases the blood flow to the limb and compresses the deep veins, venous blood is shunted into the superficial veins and then returned to the heart. (The veins become more prominent as the limb is being exercised, e.g., when lifting weights.) These veins have valves to assist in venous return. Cutaneous nerves also lie in the superficial fascia and are the terminal sensory branches of the major nerves arising from the brachial plexus (ventral rami of C5-T1 spinal levels) (see Fig. 7-2).
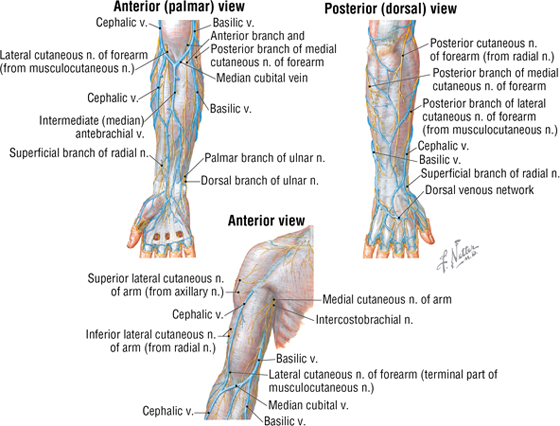
FIGURE 7-2 Superficial Veins and Nerves of the Upper Limb
3. SHOULDER
Bones and Joints of the Pectoral Girdle and Shoulder
The pectoral girdle is composed of the following structures:
- Clavicle (collar bone)
- Scapula (shoulder blade)
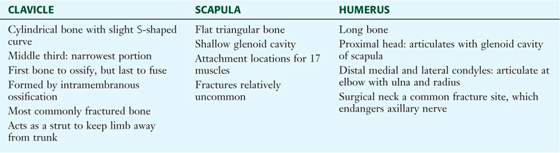
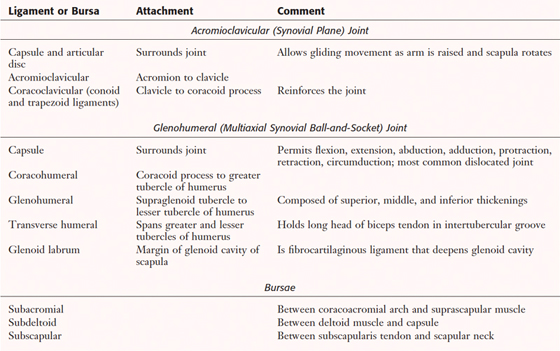
The humerus, or arm bone, articulates with the scapula and forms the shoulder joint. These bones are shown in Figure 7-3 and listed in Table 7-1. The three joints contributing to the pectoral girdle and shoulder are described in Table 7-2 (acromioclavicular and glenohumeral joints) and Table 3-2 (sternoclavicular joint).
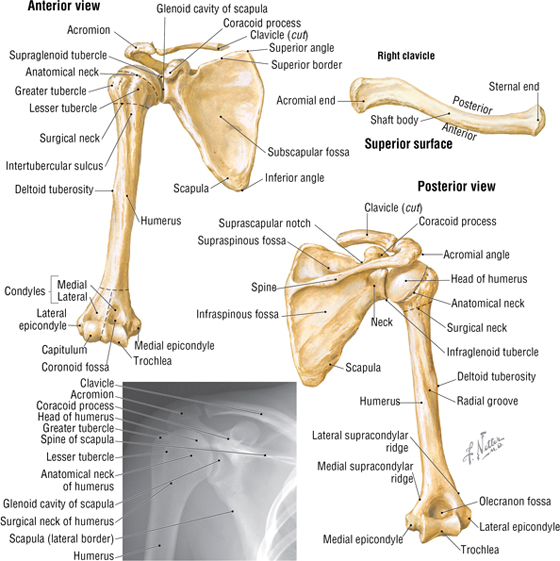
FIGURE 7-3 Bones of the Pectoral Girdle and Shoulder
|
TABLE 7-1 Features of the Clavicle, Scapula, and Humerus
|
 |
|
TABLE 7-2 Acromioclavicular and Glenohumeral Joints
|
 |
C L I N I C A L F O C U S
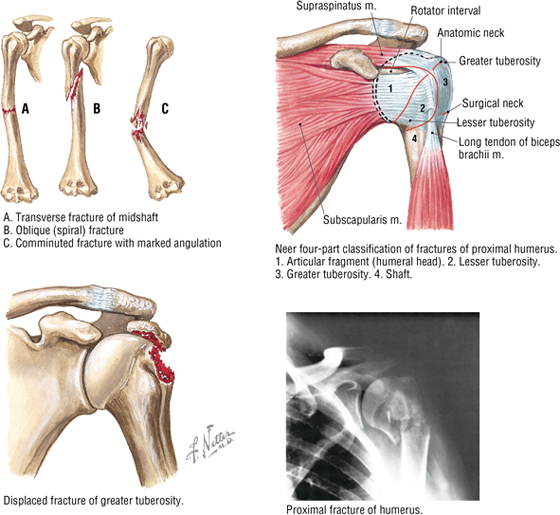
Fracture of the Proximal Humerus
Fractures of the proximal humerus often occur from a fall on an outstretched hand or from direct trauma to the area. They are especially common in the elderly, where osteoporosis is a factor. The most common site is the surgical neck of the humerus, because the bone begins to taper down at this point and is structurally weaker (see Fig. 7-3).
The sternoclavicular and acromioclavicular joints of the pectoral girdle allow for a significant amount of movement of the limb and combined with the shallow ball-and-socket glenohumeral joint permit extension, flexion, abduction, adduction, protraction, retraction, and circumduction movements. This flexibility and range of movement greatly enhance our ability to interact with our environment. The tendons of the four rotator cuff muscles (see the “Muscles” section later in the chapter) also help stabilize this shallow articulation without inhibiting the extensive range of motion at the shoulder (Fig. 7-4).
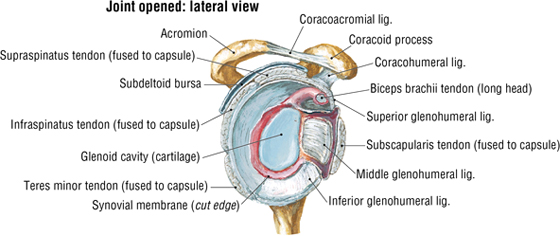
FIGURE 7-4 Shoulder Joint Tendons and Ligaments (Contd.)
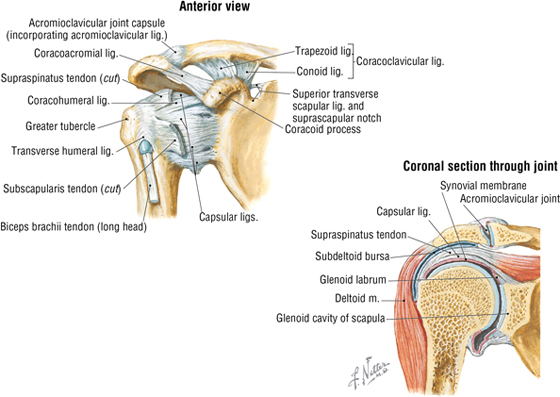
FIGURE 7-4 (Contd.) Shoulder Joint Tendons and Ligaments
C L I N I C A L F O C U S
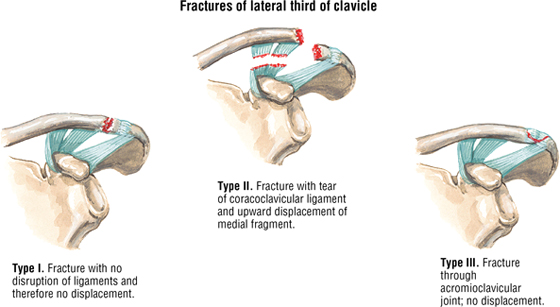
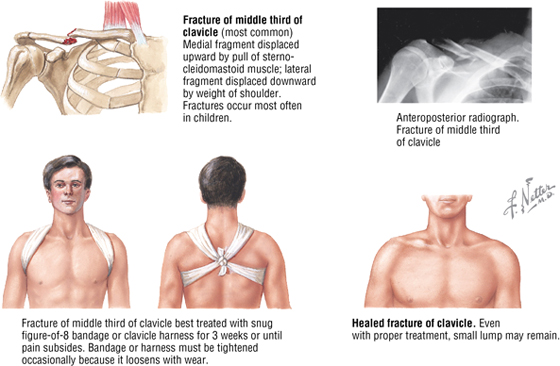
Clavicular Fractures
Fracture of the clavicle is quite common, especially in children. The fracture usually results from a fall on an outstretched hand or from direct trauma to the shoulder. Fractures of the medial third of the clavicle are rare (about 5%), but those of the middle third are common (about 80%). In a complete fracture, the proximal bone fragment is pulled superiorly by the sternocleidomastoid muscle, whereas the distal fragment is pulled inferiorly by the weight of the shoulder. Fractures of the lateral third can involve coracoclavicular ligament tears.
C L I N I C A L F O C U S
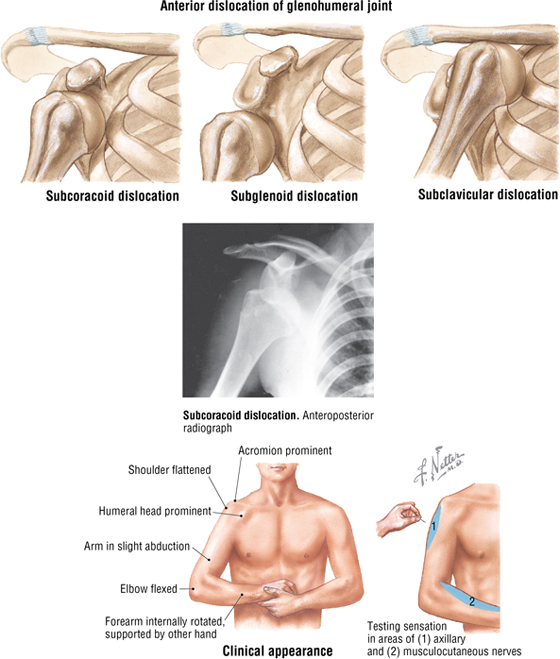
Glenohumeral Dislocations
Almost 95% of shoulder (glenohumeral joint) dislocations occur in an anterior direction. Abduction, extension, and lateral (external) rotation of the arm at the shoulder (e.g., the throwing motion) place stress on the capsule and anterior elements of the rotator cuff (subscapularis tendon). The types of anterior dislocations include the following:
- Subcoracoid (most common)
- Subglenoid
- Subclavicular (rare)
The axillary (most often) and musculocutaneous nerves may be injured during such dislocations.
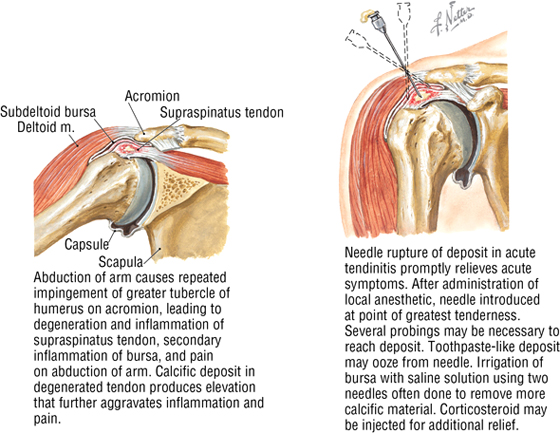
C L I N I C A L F O C U S
Shoulder Tendinitis and Bursitis
Movement at the shoulder joint (or almost any joint) can lead to inflammation of the tendons surrounding that joint and secondary inflammation of the bursa that cushions the joint from the overlying muscle or tendon. A painful joint can result, possibly even with calcification within the degenerated tendon. The supraspinatus muscle tendon is especially vulnerable because it can become pinched by the greater tubercle of the humerus, the acromion, and the coracoacromial ligament.
Muscles
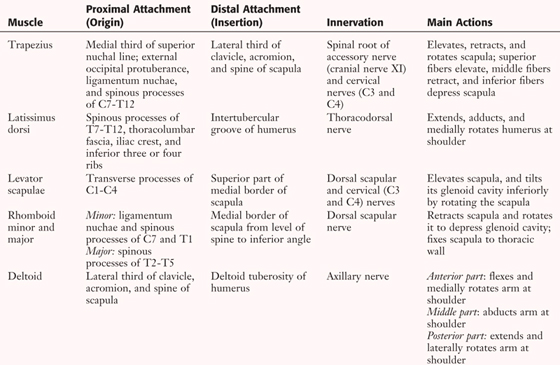
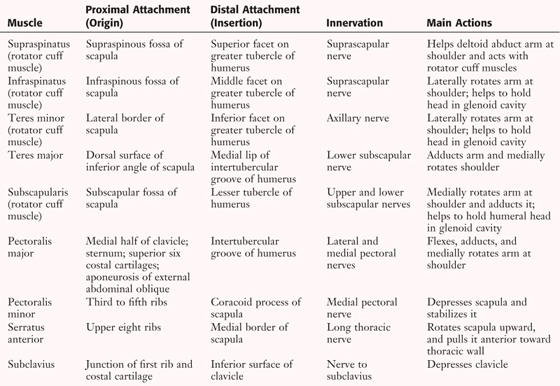
Muscles of the shoulder include the superficial back muscles, the deltoid and teres major muscles, the four rotator cuff muscles, and the superficial muscles of the pectoral region (anterior chest wall) (Fig. 7-5 and Table 7-3). It is important to note that 17 different muscles attach to the scapula (back, limb, and neck muscles) and account for the range of movement of the scapula as the upper limb is abducted (the scapula rotates), adducted, flexed, extended, and rotated.
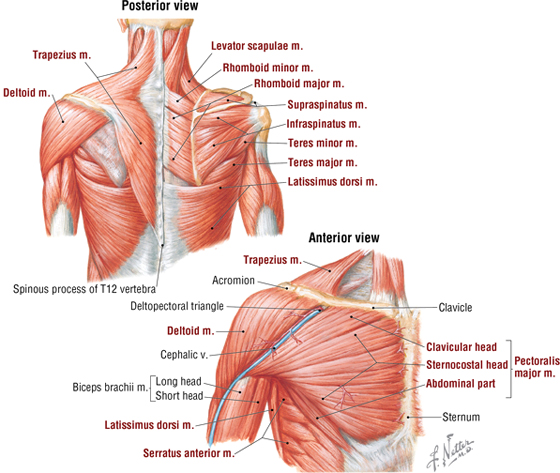
FIGURE 7-5 Muscles Acting on the Shoulder
|
TABLE 7-3 Shoulder Muscles (Contd.)
|
 |
|
TABLE 7-3 (Contd.) Shoulder Muscles
|
 |
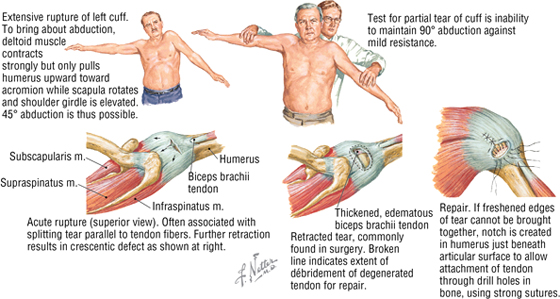
C L I N I C A L F O C U S
Rotator Cuff Injury
The tendons of insertion of the rotator cuff muscles form a musculotendinous cuff about the shoulder joint on its anterior, superior, and posterior aspects. The muscles of the rotator cuff group are as follows:
- Subscapularis
- Infraspinatus
- Supraspinatus
- Teres minor
Repeated abduction and flexion (e.g., a throwing motion) cause wear and tear on the tendons as they rub on the acromion and coracoacromial ligament, which may lead to cuff tears or rupture. The tendon of the supraspinatus is the most vulnerable to injury.
4. AXILLA
The axilla (armpit) is a pyramid-shaped region that contains important neurovascular structures that pass through the shoulder region. These neurovascular elements are enclosed in a fascial sleeve called the axillary sheath, which is a direct continuation of the prevertebral fascia of the neck. The axilla has the following six boundaries (Fig. 7-6):
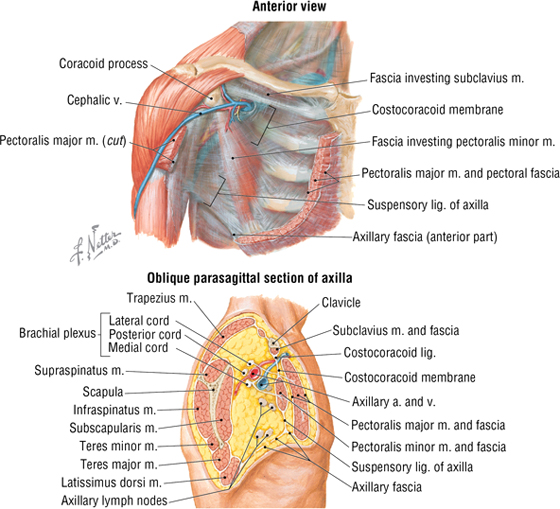
FIGURE 7-6 Boundaries and Features of the Axilla
- Base (floor): axillary fascia and skin of armpit
- Apex (inlet): passageway for structures entering or leaving the shoulder and arm; bounded by first rib, clavicle, and superior part of the scapula
- Anterior wall: pectoralis major and minor muscles, and clavipectoral fascia
- Posterior wall: subscapularis, teres major, latissimus dorsi, and long head of the triceps muscle
- Medial wall: upper rib cage, intercostal and serratus anterior muscles
- Lateral wall: humerus (intertubercular sulcus)
Important structures in the axilla include the following:
- Axillary artery: divided into three parts for descriptive purposes
- Axillary vein(s)
- Axillary lymph nodes: five major collections
- Brachial plexus of nerves: ventral rami of C5-T1
- Biceps and coracobrachialis muscles: portions
- Axillary tail (of Spence) of the female breast
Axillary fasciae are as follows:
- Pectoral fascia: invests the pectoralis major muscle; attaches to the sternum and clavicle
- Clavipectoral fascia: invests the subclavius and pectoralis minor muscles
- Axillary fascia: forms the base of axilla
- Axillary sheath: invests the axillary neurovascular structures
Axillary Vessels
The axillary artery begins at the first rib and is divided into three descriptive parts by the pectoralis minor muscle (Fig. 7-7 and Table 7-4). It continues as the brachial artery distally at the inferior border of the teres major muscle.
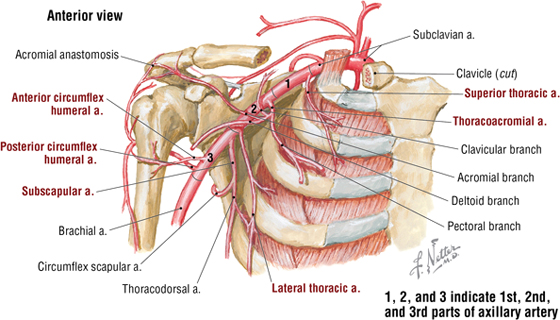
FIGURE 7-7 Branches of the Axillary Artery
|
TABLE 7-4 Branches of the Axillary Artery
|
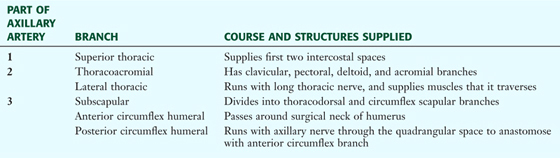 |
Like most joints, the shoulder joint has a rich vascular anastomosis. This anastomosis not only supplies the 17 muscles attaching to the scapula and other shoulder muscles but also provides collateral circulation to the upper limb should the proximal part of the axillary artery become occluded (proximal to the subscapular branch). This anastomosis includes the following important component arteries (Fig. 7-8):
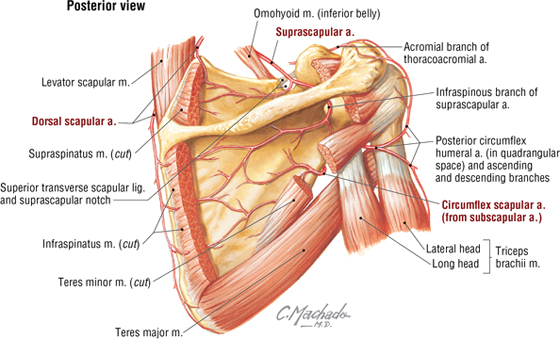
FIGURE 7-8 Arteries of the Scapular Anastomosis
- Dorsal scapular (transverse cervical) branch of the subclavian (thyrocervical artery)
- Suprascapular from the subclavian (thyrocervical trunk)
- Subscapular and its circumflex scapular and thoracodorsal branches
The axillary vein begins at the inferior border of the teres major muscle and is a continuation of the basilic vein (and/or the brachial venae comitantes, which includes several small brachial veins that parallel the brachial artery in the arm). When the axillary vein meets the first rib, it becomes the subclavian vein.
Brachial Plexus
The axillary artery, axillary vein (lies medial to the artery), and cords of the brachial plexus are all bound in the axillary sheath (see Fig. 7-6). In Figure 7-9, the sheath and some parts of the axillary vein have been removed and several muscles have been reflected to better visualize the arrangement of the plexus as it invests the axillary artery. Key nerves and branches of the axillary artery also are shown supplying muscles.
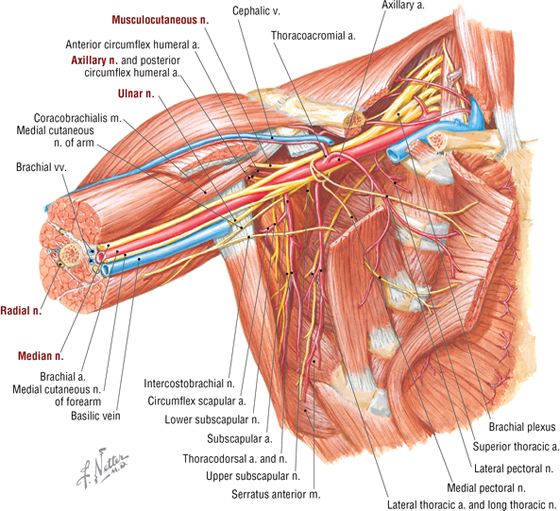
FIGURE 7-9 Brachial Plexus (Terminal Branches Highlighted) and Axillary Artery
Nerves that innervate most of the shoulder muscles and all of the muscles of the upper limb arise from the brachial plexus. The plexus arises from ventral rami of spinal nerves C5-T1 (Fig. 7-10). The plexus is descriptively divided into five roots (ventral rami), three trunks, six divisions (three anterior, three posterior), three cords (named for their relationship to the axillary artery), and five large terminal branches. Important motor branches of the brachial plexus are indicated in Table 7-5.
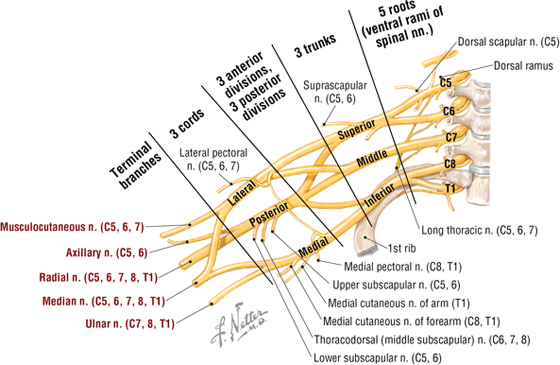
FIGURE 7-10 Schematic of the Brachial Plexus
|
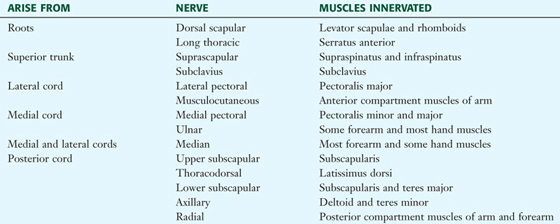
TABLE 7-5 Major Motor Branches of the Brachial Plexus
|
 |
Later in this chapter, we will summarize the specific individual nerve lesions related to the brachial plexus or distal to it.
C L I N I C A L F O C U S
Brachial Plexopathy
Damage (trauma, inflammation, tumor, radiation damage, bleeding) to the brachial plexus may present as pain, loss of sensation, and/or motor weakness. Clinical findings depend on the site of the lesion:
- Upper plexus lesions: usually affect the distribution of C5-C6 nerve roots, with the deltoid and biceps muscles affected, and sensory changes that extend below the elbow to the hand.
- Lower plexus lesions: usually affect the distribution of C8-T1 nerve roots, with median and ulnar innervated muscles affected; hand weakness and sensory changes involve most of the palmar hand and ulnar aspect of the dorsal hand
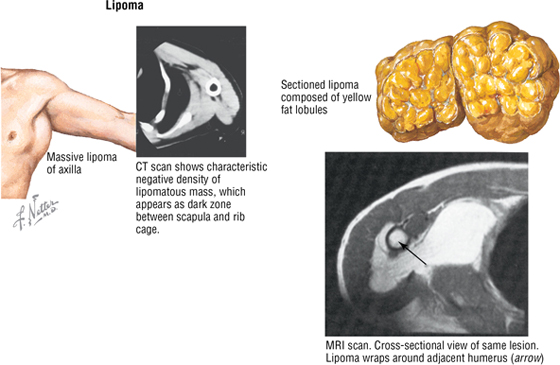
C L I N I C A L F O C U S
Axillary Lipoma
Benign soft tissue tumors occur much more often than do malignant tumors. In adults, the most common type is the lipoma. A lipoma is composed of mature fat. It is usually large and soft, asymptomatic, and more common than all other soft tissue tumors combined. A lipoma presents as a solitary mass. Most are found in the following locations:
- Axilla
- Shoulders
- Proximal region of the limbs
- Abdomen
- Back
Axillary Lymph Nodes
The axillary lymph nodes lie in the fatty connective tissue of the axilla. They are the major collection nodes for all lymph draining from the upper limb and portions of the thoracic wall, especially the breast (about 75% of lymphatic drainage from the breast passes through these nodes). The 20 to 30 nodes are divided into the following five groups (Fig. 7-11):
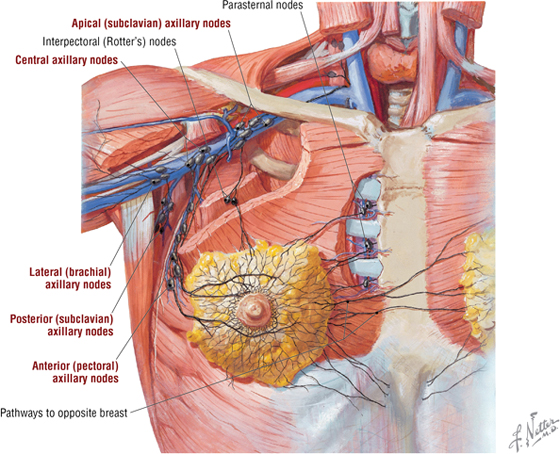
FIGURE 7-11 Axillary Lymph Nodes and the Lymph Drainage of the Breast
- Central nodes: receive lymph from several of the other groups
- Lateral (brachial, humeral) nodes: receive most of the upper limb drainage
- Posterior (subscapular) nodes: drain the upper back
- Anterior (pectoral) nodes: drain the breast and anterior trunk
- Apical (subclavian) nodes: connect with infraclavicular nodes
5. ARM
As you study the anatomical arrangement of the arm and forearm, organize your study around the functional muscular compartments. We have already discussed the humerus, the long bone of the arm (see Fig. 7-3 and Table 7-1).
The arm is divided into an anterior (flexor) compartment and a posterior (extensor) compartment by an intermuscular septum, which is attached medially and laterally to the deep (investing) fascia surrounding the muscles.
Anterior Compartment Muscles, Vessels, and Nerves
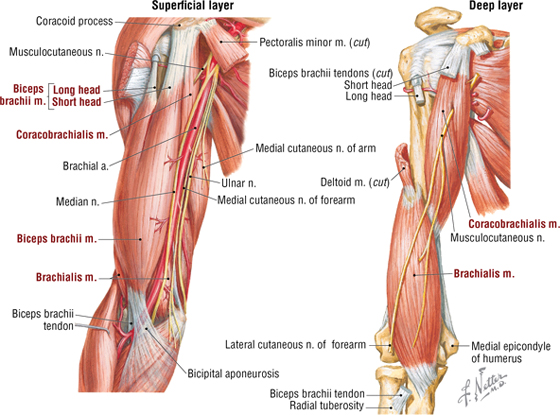
FIGURE 7-12 Anterior Compartment Arm Muscles and Nerves
|
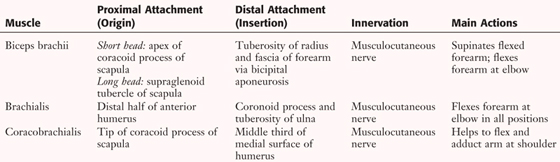
TABLE 7-6 Anterior Compartment Arm Muscles
|
 |
- Are primarily flexors of the forearm at the elbow
- Are secondarily flexors of the arm at the shoulder (biceps and coracobrachialis)
- Can supinate the flexed forearm (biceps only)
- Are innervated by the musculocutaneous nerve
- Are supplied by the brachial artery
Posterior Compartment Muscles, Vessels, and Nerves
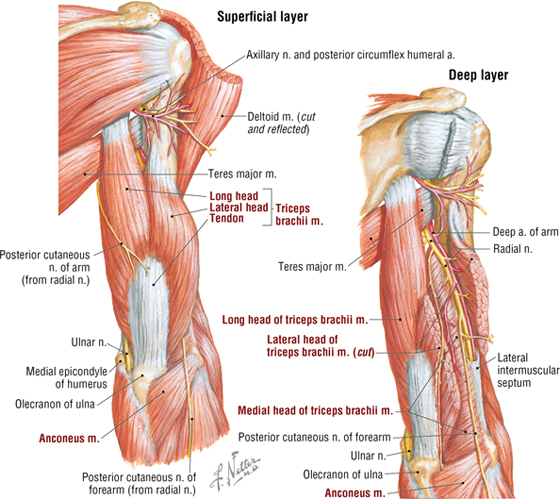
FIGURE 7-13 Posterior Compartment Arm Muscles and Nerves
|
TABLE 7-7 Posterior Compartment Arm Muscles
|
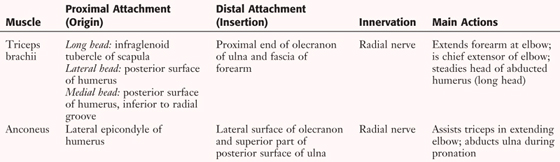 |
- Are primarily extensors of the forearm at the elbow
- Are supplied with blood from the deep artery of the arm (profunda brachii)
- Are innervated by the radial nerve
C L I N I C A L F O C U S
Deep Tendon Reflexes
A brisk tap to a partially stretched muscle tendon near its point of insertion elicits a deep tendon (muscle stretch) reflex that is dependent on the following:
- Intact afferent (sensory) nerve fibers
- Normal functional synapses in the spinal cord at the appropriate level
- Intact efferent (motor) nerve fibers
- Normal functional neuromuscular junctions on the tapped muscle
- Normal muscle fiber functioning (contraction)
Characteristically, the deep tendon reflex only involves several spinal cord segments (and their afferent and efferent nerve fibers). If pathology is involved at the level tested, the reflex may be weak or absent, requiring further testing to determine where along the pathway the lesion occurred. For the arm, you should know the following segmental levels for the deep tendon reflex:
- Biceps brachii reflex C5 and C6
- Triceps brachii reflex C7 and C8
The artery of the arm is the brachial artery and its branches. The brachial artery extends from the inferior border of the teres major muscle to just below the anterior elbow, where it divides into the ulnar and radial arteries (Fig. 7-14 and Table 7-8). A rich anastomosis exists around the elbow joint between branches of the brachial artery and branches of the radial and ulnar arteries. One can feel a brachial pulse by pressing the artery medially at the mid-arm against the underlying humerus.
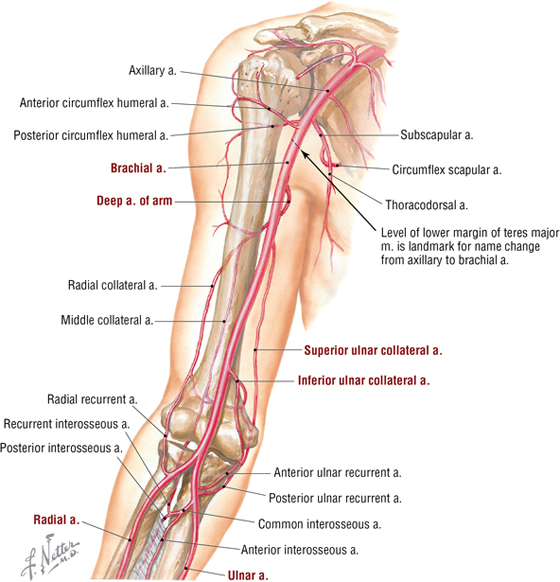
FIGURE 7-14 Brachial Artery and Its Anastomoses
|
TABLE 7-8 Branches of the Brachial Artery
|
 |
As shown in Figure 7-2, the superficial cephalic and basilic veins course in the subcutaneous tissues of the arm. The deep brachial veins usually consist of either paired veins or venae comitantes that surround the brachial artery. These veins drain into the basilic and/or axillary vein.
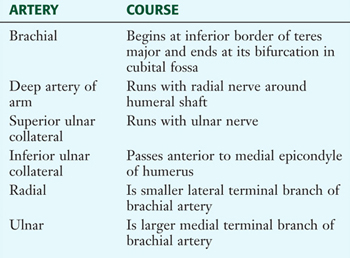
Arm in Cross Section
Cross sections of the arm nicely show the anterior and posterior compartments and their respective flexor and extensor muscles (Fig. 7-15). Note the nerve of each compartment and the medially situated neurovascular bundle containing the brachial artery, median nerve, and ulnar nerve. The median and ulnar nerves do not innervate arm muscles but simply pass through the arm to reach the forearm and hand.
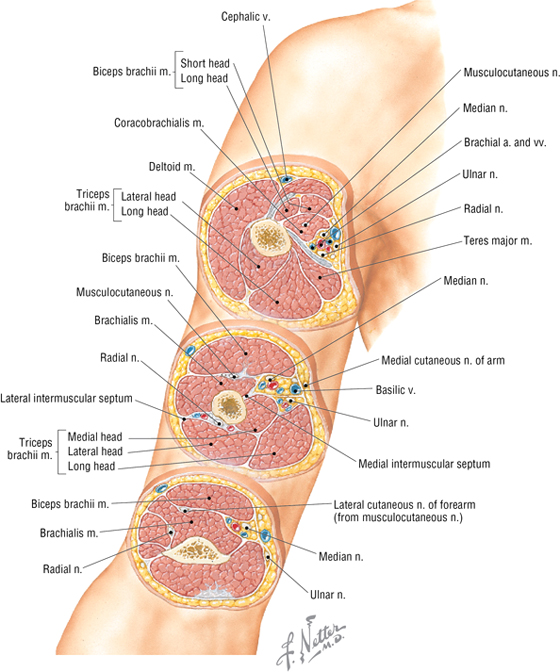
FIGURE 7-15 Serial Cross Sections of the Arm
C L I N I C A L F O C U S
Blood Pressure Measurement
The brachial artery is commonly used to measure blood pressure. The cuff of the sphygmomanometer is centered around the brachial artery on the medial side of the arm, and then the brachial pulse is felt just medial to the biceps brachii tendon. While feeling the pulse, the cuff is inflated to about 30 mm Hg above the level at which the pulsations disappear. The bell of the stethoscope is placed lightly over the site of the brachial pulse, and the cuff is slowly deflated. The point at which blood begins to flow through the previously compressed brachial artery denotes the systolic pressure and is heard through the stethoscope as consecutive beats caused by the turbulent blood flow. The pressure is continually lowered until the sounds become muffled and disappear. Then the cuff is quickly deflated to zero pressure. The point at which the sound disappears is the diastolic pressure. Both systolic and diastolic pressure levels are recorded to the nearest 2 mm Hg; a normal blood pressure is 120/80 mm Hg, although normal can vary and is dependent on a number of contributing factors (e.g., age, medications, or level of excitement).
C L I N I C A L F O C U S
Fractures of the Humerus
Fractures of the humerus may occur proximally (e.g., surgical neck fractures, which are common in older persons from a fall on an outstretched hand); they also may occur along the midshaft, usually from direct trauma, or distally (uncommon in adults). Proximal fractures mainly occur at the following four sites:
- Humeral head (articular fragment)
- Lesser tuberosity
- Greater tuberosity
- Proximal shaft (surgical neck)
Midshaft fractures usually heal well but may involve entrapment of the radial nerve as it spirals around the shaft to reach the arm's posterior muscle compartment (triceps muscle).
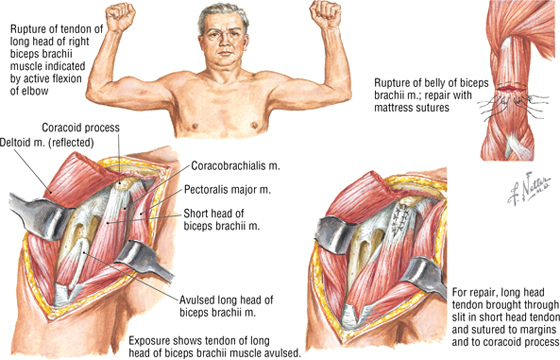
C L I N I C A L F O C U S
Biceps Brachii Rupture
Rupture of the biceps brachii may occur at the tendon or, rarely, the muscle belly. This tendon has the highest rate of spontaneous rupture of any tendon in the body. Rupture is seen most often in patients older than 40 years of age, in association with rotator cuff injuries (as the tendon begins to undergo degenerative changes), and with repetitive lifting (weight lifters). Rupture of the long head tendon is most common and may occur in the following locations:
- Shoulder joint
- Intertubercular (bicipital) sulcus of the humerus
- Musculotendinous junction
6. FOREARM
Bones and Elbow Joint
The bones of the forearm (defined as elbow to wrist) are the laterally placed radius and medial ulna (Fig. 7-16 and Table 7-9). The radioulnar fibrous (syndesmosis) joint unites both bones via an interosseous membrane, which also divides the forearm into anterior and posterior compartments.
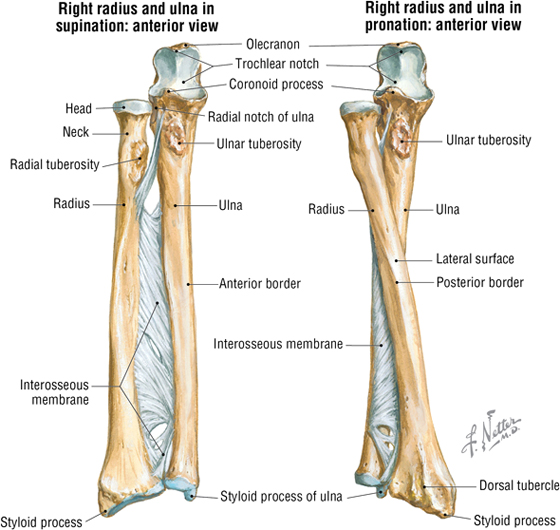
FIGURE 7-16 Radius and Ulna of the Forearm
|
TABLE 7-9 Features of the Radius and Ulna
|
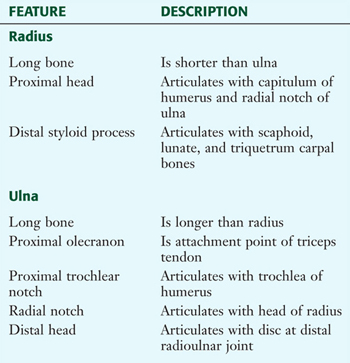 |
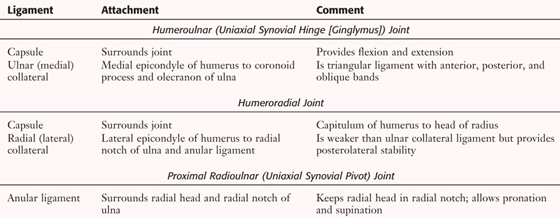
The elbow joint is composed of the humeroulnar and humeroradial joints for flexion and extension, and the proximal radioulnar joint for pronation and supination (Figs. 7-17 and 7-18 and Table 7-10).
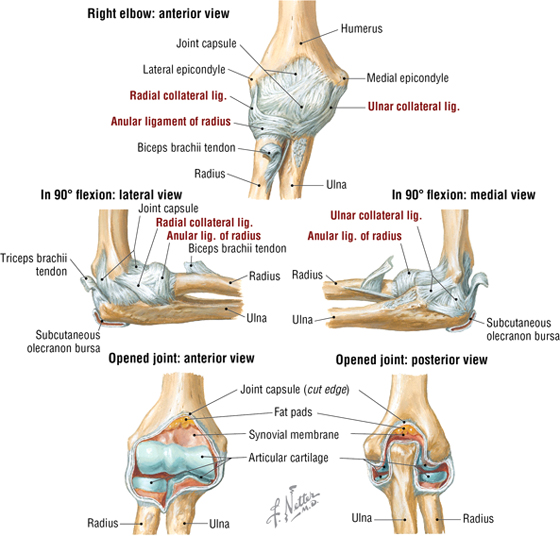
FIGURE 7-17 Elbow Joint and Ligaments
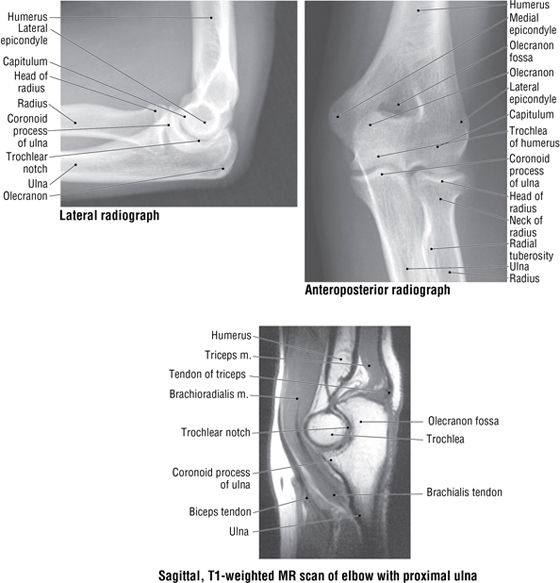
FIGURE 7-18 Imaging of the Elbow. (MR reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Elsevier Mosby, 2007.)
|
TABLE 7-10 Forearm Joints
|
 |
C L I N I C A L F O C U S
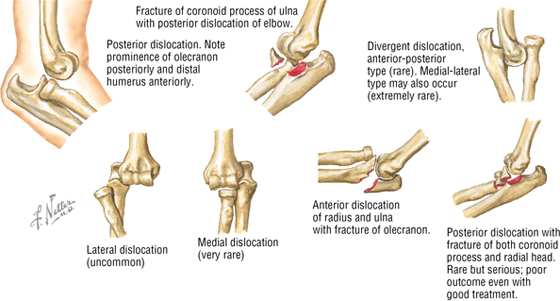
Elbow Dislocation
Elbow dislocations occur third in frequency after shoulder and finger dislocations. Dislocation often results from a fall on an outstretched hand and includes the following types:
- Posterior (most common)
- Anterior (rare; may lacerate brachial artery)
- Lateral (uncommon)
- Medial (rare)
Dislocations may be accompanied by fractures of the humeral medial epicondyle, olecranon (ulna), radial head, or coronoid process of the ulna. Injury to the ulnar (most common) or median nerve may accompany these dislocations.
Anterior Compartment Muscles, Vessels, and Nerves
The muscles of the anterior compartment are arranged in two layers, with the muscles of the superficial layer largely arising from the medial epicondyle of the humerus (Fig. 7-19 and Table 7-11). These muscles exhibit the following features:
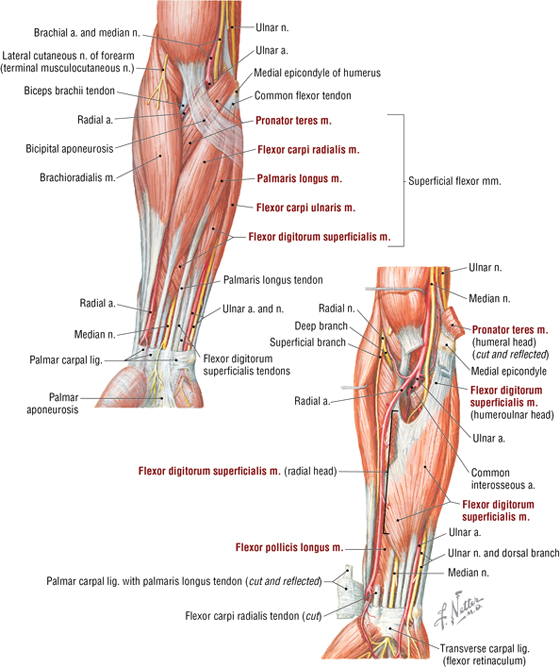
FIGURE 7-19 Anterior Compartment Forearm Muscles and Nerves
|
TABLE 7-11 Anterior Compartment Forearm Muscles
|
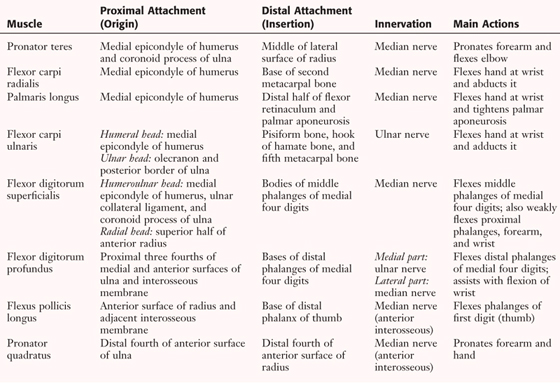 |
- They are primarily flexors of the hand at the wrist and/or are finger flexors
- Two of the muscles are pronators
- Secondarily, several muscles can abduct and adduct the hand at the wrist
- Their muscle bellies reside in the forearm, but their tendons extend to the wrist or into the hand (except for the pronator muscles)
- They are supplied by the ulnar and radial arteries
- All except two muscles are innervated by the median nerve
The cubital fossa is the region anterior to the elbow and is demarcated by the brachioradialis muscle laterally and the pronator teres muscle medially (see Fig. 7-19). The median nerve and brachial artery traverse the cubital fossa and are covered by the bicipital aponeurosis.
Posterior Compartment Muscles, Vessels, and Nerves
The muscles of the posterior compartment also are arranged in a superficial and deep layer, with the superficial layer of muscles largely arising from the lateral epicondyle of the humerus (Fig. 7-20 and Table 7-12). These muscles exhibit the following features:
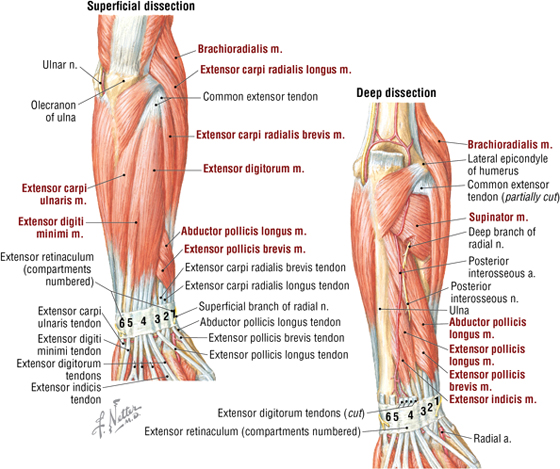
FIGURE 7-20 Posterior Compartment Forearm Muscles and Nerves
|
TABLE 7-12 Posterior Compartment Forearm Muscles and Nerves
|
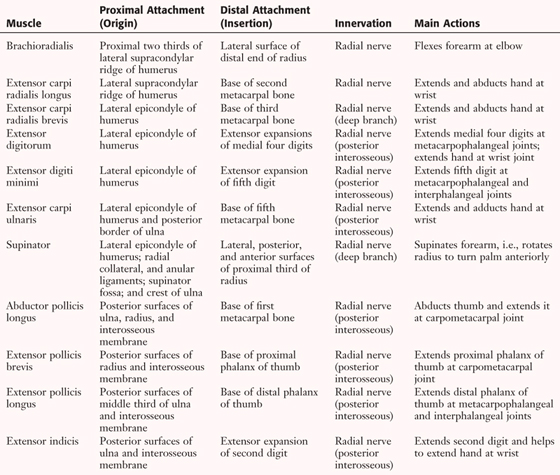 |
- They are primarily extensors of the hand at the wrist and/or are finger extensors; several can adduct or abduct the thumb
- One muscle is a supinator
- Secondarily, several muscles can abduct and adduct the hand at the wrist
- Their muscle bellies reside largely in the forearm, but their tendons extend to the wrist or into the dorsum of the hand
- They are supplied by the radial and ulnar arteries (common interosseous branch)
- All are innervated by the radial nerve
C L I N I C A L F O C U S
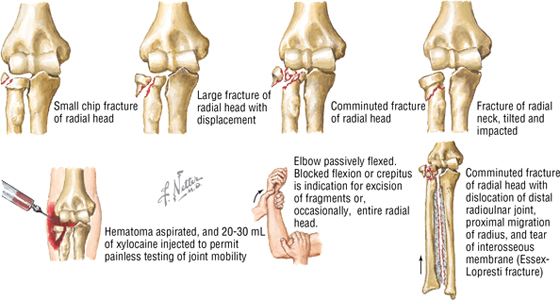
Fracture of the Radial Head and Neck
Fractures to the proximal radius often involve either the head or the neck of the radius. These fractures can result from a fall on an outstretched hand (indirect trauma) or a direct blow to the elbow. Fracture of the radial head is more common in adults, whereas fracture of the neck is more common in children.
C L I N I C A L F O C U S
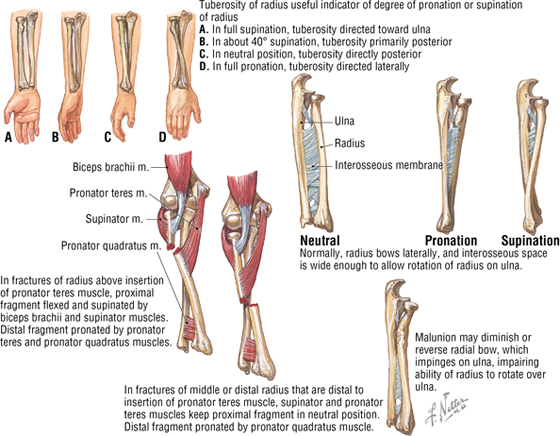
Biomechanics of Forearm Radial Fractures
The ulna is a straight bone with a stable articulation (elbow), but the radius is not uniform in size, proximal to distal. Natural lateral bowing of the radius is essential for optimal pronation and supination. However, when the radius is fractured, the muscles attaching to the bone deform this alignment. Careful reduction of the fracture should attempt to replicate the normal anatomy to maximize pronation and supination, as well as to maintain the integrity of the interosseous membrane.
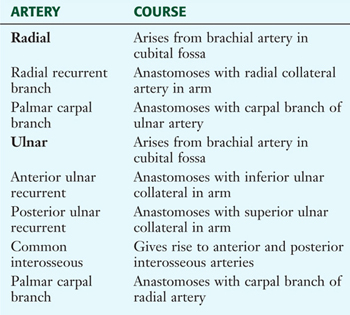
The muscles of the forearm are supplied by the radial and ulnar arteries (see Fig. 7-19; Fig. 7-21; Table 7-13). Deeper muscles also receive blood from the common interosseous branch of the ulnar artery. Deep veins parallel the radial and ulnar arteries and have connections with the superficial veins in the subcutaneous tissue of the forearm.
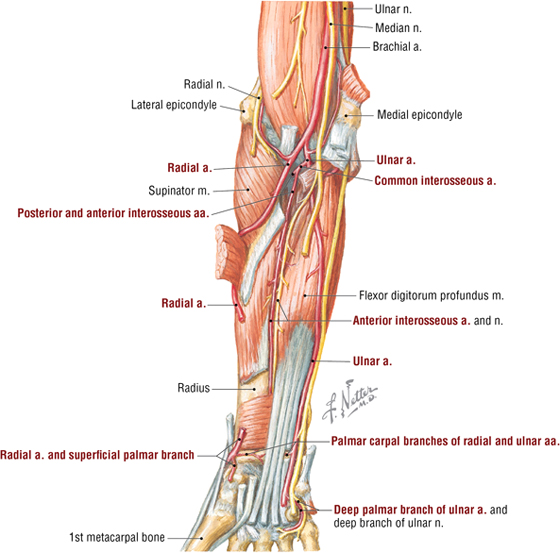
FIGURE 7-21 Forearm Arteries
|
TABLE 7-13 Major Branches of the Radial and
Ulnar Arteries
|
 |
Forearm in Cross Section
Cross sections of the forearm demonstrate the anterior (flexor-pronator) and posterior (extensor-supinator) compartments and their respective neurovascular structures (Fig. 7-22). The median nerve innervates all but the flexor carpi ulnaris and the ulnar half of the flexor digitorum profundus muscles in the anterior compartment. (The ulnar nerve innervates these.) The radial nerve innervates all the posterior compartment muscles.
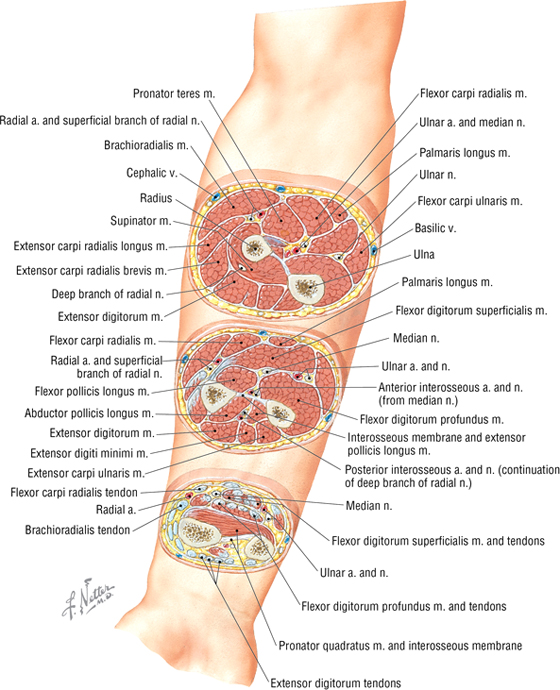
FIGURE 7-22 Serial Cross Sections of the Forearm
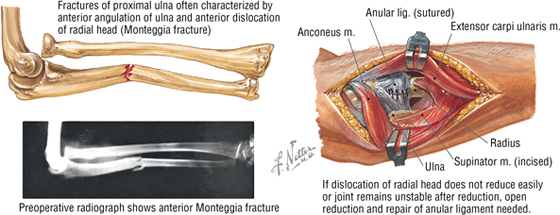
C L I N I C A L F O C U S
Fracture of the Ulna Shaft
Usually, a direct blow to or forced pronation of the forearm is the most common cause of a fracture of the shaft of the ulna. Fracture of the ulna with dislocation of the proximal radioulnar joint is termed a Monteggia fracture. The radial head usually dislocates anteriorly, but posterior, medial, or lateral dislocation also may occur. Such dislocations may put the posterior interosseous nerve (branch of the radial nerve) at risk.
7. WRIST AND HAND
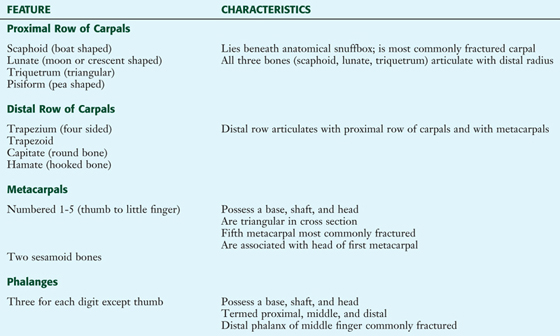
Bones and Joints
The wrist connects the hand to the forearm and is composed of eight carpal bones aligned in a proximal and distal row (four carpals in each row). The hand includes the metacarpus (the palm, with five metacarpal bones) and five digits with their phalanges (Fig. 7-23 and Table 7-14).
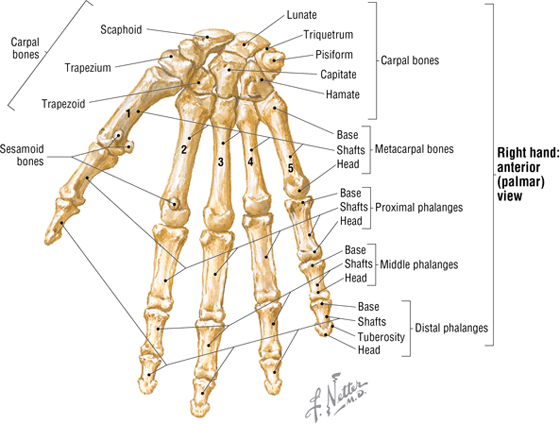
FIGURE 7-23 Wrist and Hand Bones
|
TABLE 7-14 Features of the Wrist and Hand Bones
|
 |
The wrist joint is a radiocarpal synovial joint between the radius and an articular disc covering the distal ulna, and the proximal articular surfaces of the scaphoid, lunate, and triquetrum (radiocarpal and distal radiocarpal [ulnocarpal in some books] joints) (Figs. 7-24 and 7-25; Table 7-15). Although the carpal joints (intercarpal and midcarpal) are within the wrist, they provide for gliding movements and significant wrist extension and flexion (see Table 7-15).
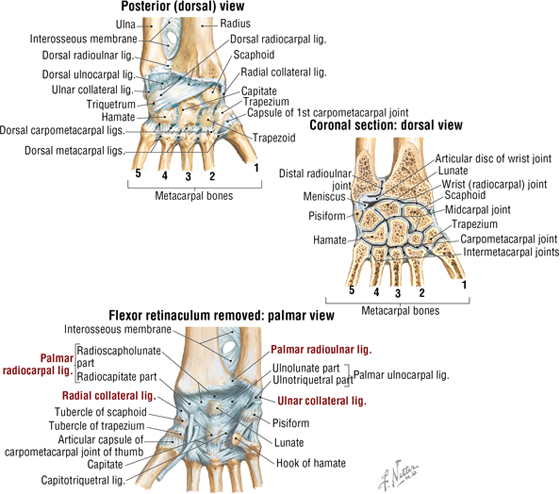
FIGURE 7-24 Wrist Joint Ligaments
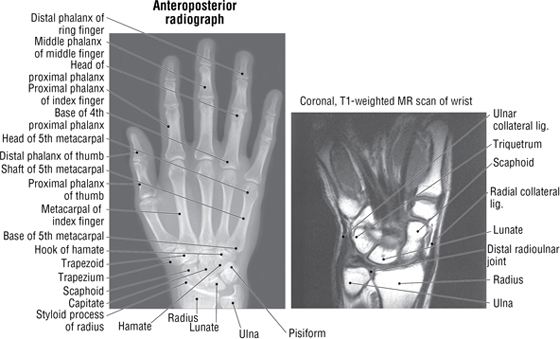
FIGURE 7-25 Radiographic Images of the Wrist and Hand. (MR reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Elsevier Mosby, 2007.)
|
TABLE 7-15 Joints and Ligaments of the Wrist and Hand (Contd.)
|
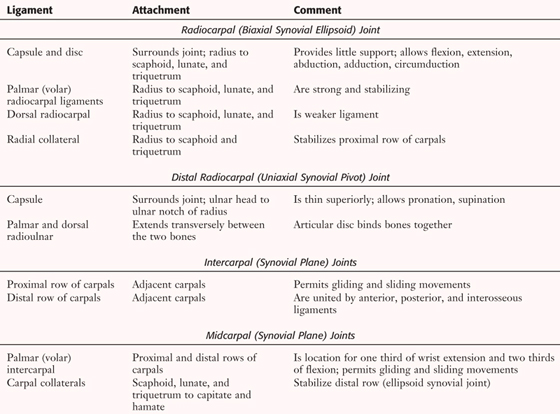 |
|
TABLE 7-15 (Contd.) Joints and Ligaments of the Wrist and Hand
|
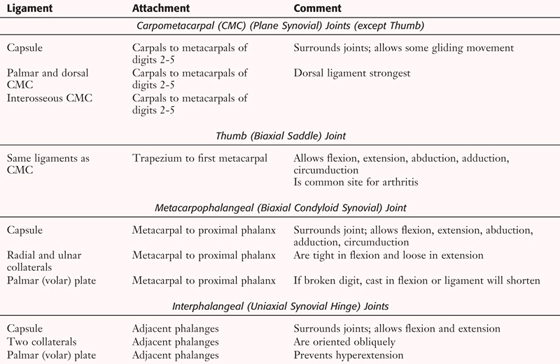 |
Carpometacarpal (CMC, carpals to metacarpals), metacarpophalangeal (MCP), and proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints complete the joints of the hand (Fig. 7-26). Note that the thumb (the first digit) possesses only one interphalangeal joint (see Table 7-15).
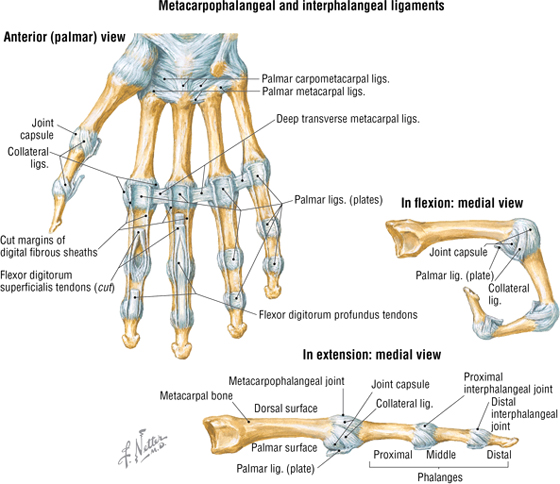
FIGURE 7-26 Finger Joints and Ligaments
C L I N I C A L F O C U S
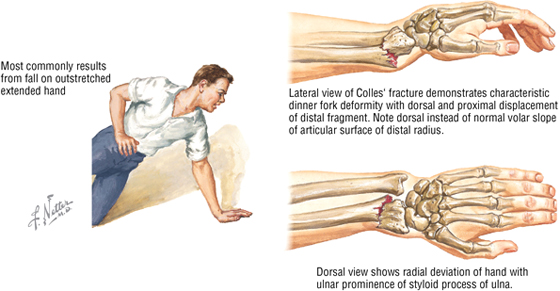
Distal Radial (Colles’) Fracture
Fractures of the distal radius are common (about 80% of forearm fractures) in all age groups and often result from a fall on an outstretched hand. Colles’ fracture is an extension-compression fracture of the distal radius that produces a typical dinner-fork deformity.
C L I N I C A L F O C U S
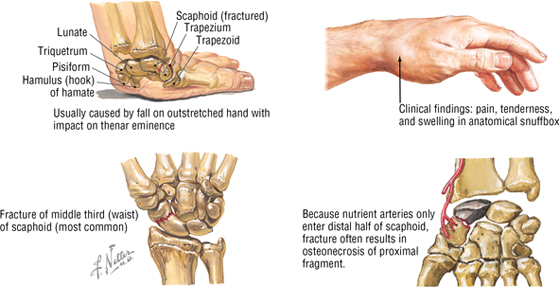
Fracture of the Scaphoid
The scaphoid bone is the most frequently fractured carpal bone and may be injured by falling on an extended wrist. Fracture of the middle third (waist) of the bone is most common. Pain and swelling in the anatomical “snuffbox” often occurs, and optimal healing depends on an adequate blood supply (from the palmar carpal branch of the radial artery). Loss of the blood supply can lead to nonunion or avascular osteonecrosis.
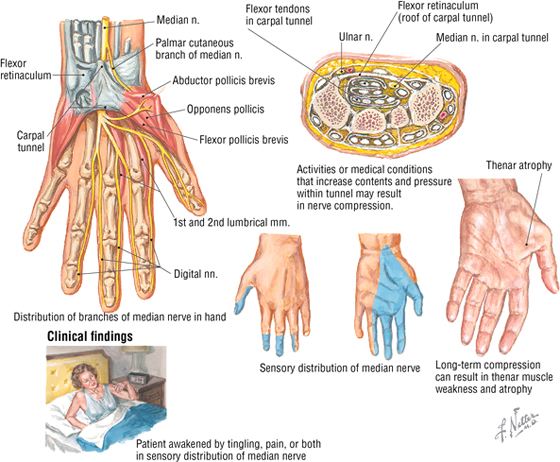
Carpal Tunnel and the Extensor Compartments
The carpal tunnel is formed by the arching alignment of the carpal bones and the thick flexor retinaculum (transverse carpal ligament), which covers the tunnel on its anterior surface (Fig. 7-27). Structures passing through the carpal tunnel include the following:
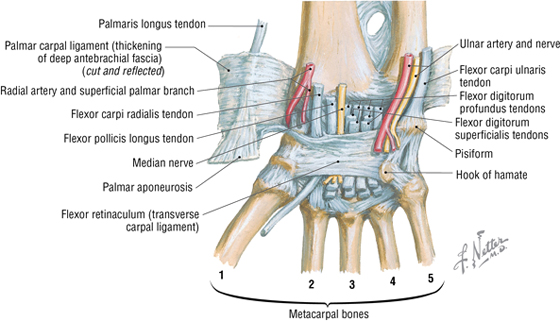
FIGURE 7-27 The Carpal Tunnel: Palmar View
- Four flexor digitorum superficialis tendons
- Four flexor digitorum profundus tendons
- One flexor pollicis longus tendon
- Median nerve
Synovial sheaths surround the muscle tendons and permit sliding movements as the muscles contract and relax.
C L I N I C A L F O C U S
Median Nerve Compression and Carpal Tunnel Syndrome
Median nerve compression in the carpal tunnel, the most common compression neuropathy, is often linked to occupational repetitive movements related to wrist flexion and extension, holding the wrist in an awkward position, or strong gripping of objects. Long-term compression commonly leads to thenar atrophy and weakness of the thumb and index fingers, reflecting the loss of innervation to the muscles distal to the median nerve damage.
The extensor tendons and their synovial sheaths enter the hand by passing on the medial, dorsal, and lateral aspects of the wrist beneath the extensor retinaculum, which segregates the tendons into six compartments (Fig. 7-28).
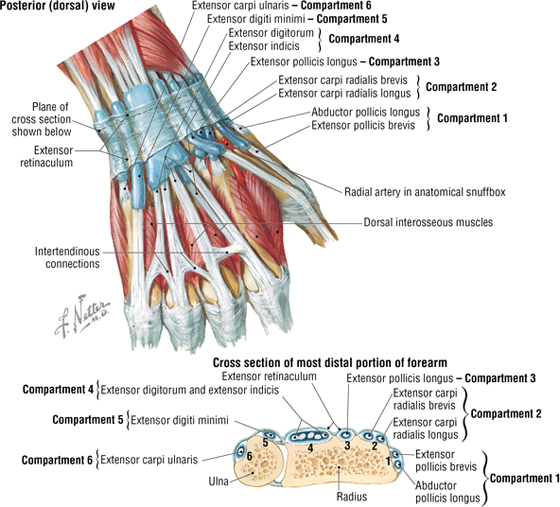
FIGURE 7-28 Extensor Tendons and Sheaths of the Wrist
Intrinsic Hand Muscles
The intrinsic hand muscles originate and insert in the hand and carry out fine precision movements, whereas the forearm muscles and their tendons that pass into the hand are more important for powerful hand movements such as gripping objects (Fig. 7-29 and Table 7-16).
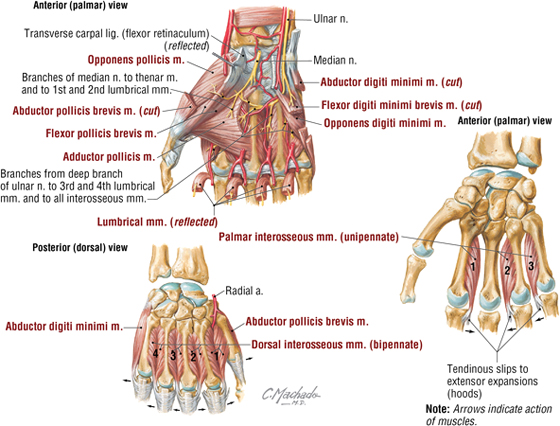
FIGURE 7-29 Intrinsic Hand Muscles
|
TABLE 7-16 Intrinsic Hand Muscles
|
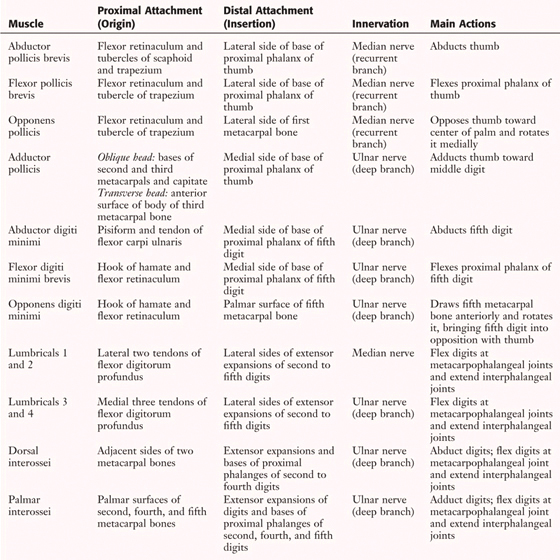 |
The blood supply to the hand is by the radial and ulnar arteries, which anastomose with each other via two palmar arches (superficial and deep) (Fig. 7-30 and Table 7-17). Except for the thumb and lateral index finger, the remainder of the hand is supplied by the ulnar artery. Corresponding veins drain largely to the dorsum of the hand and collect in the cephalic (lateral) and basilic (medial) veins (see Fig. 7-2). Deeper veins parallel the arteries and, throughout their course in the forearm and arm, have connections with the superficial veins. The upper limb veins possess valves to assist in venous return. Most of the intrinsic hand muscles are innervated by the ulnar nerve. (The three thenar muscles and the two lateral lumbricals are innervated by the median nerve.)
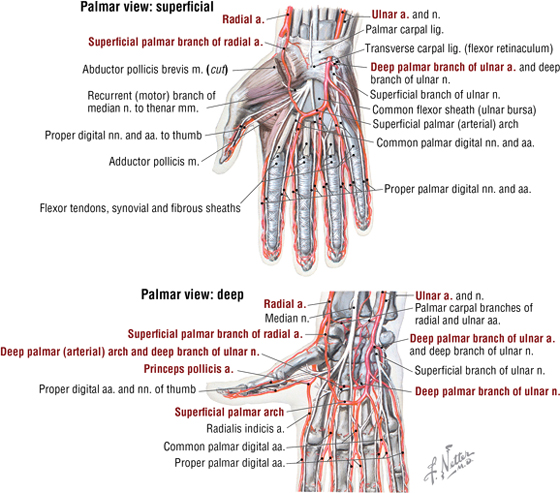
FIGURE 7-30 Arteries and Nerves of the Hand
|
TABLE 7-17 Arteries of the Hand
|
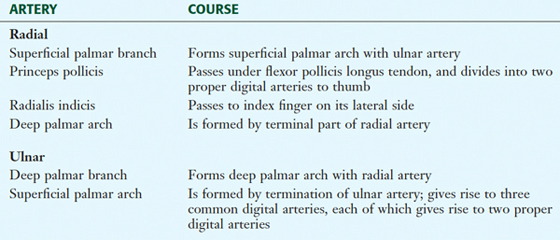 |
C L I N I C A L F O C U S
Allen’s Test
The Allen’s test is used to test the vascular perfusion distal to the wrist. The physician lightly places his or her thumbs on the patient’s ulnar and radial arteries, and the patient makes a tight fist to “blanch” the palmar skin (squeeze the blood into the dorsal venous network). Then, while compressing the radial artery with the thumb, the physician releases the pressure on the ulnar artery and asks the patient to open his or her clenched fist. Normally, the skin will turn pink immediately, indicating normal ulnar artery blood flow through the anastomotic palmar arches. The test is then repeated by occluding the ulnar artery to assess radial artery flow.
Palmar Spaces and Tendon Sheaths
As the long tendons pass through the hand toward the digits, they are surrounded by a synovial sheath and, in the digits, a fibrous digital sheath that binds them to the phalanges (see Fig. 7-30; Fig. 7-31; Table 7-18). In a cross section of the palm, one can see the long flexor tendons segregate out to their respective digits and visualize the potential spaces (thenar and midpalmar) of the hand. The thenar eminence is created by the following muscles (all median nerve innervated):
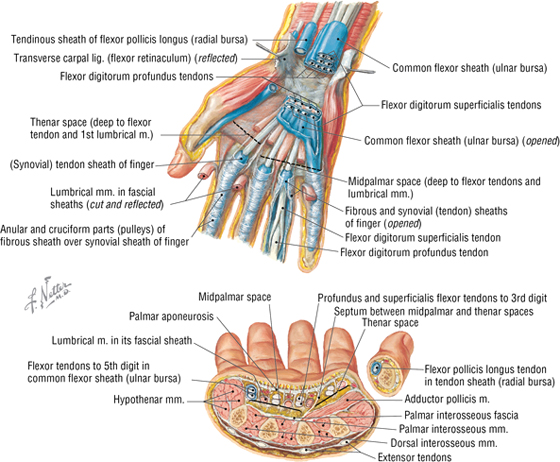
FIGURE 7-31 Bursae, Spaces, and Tendon Sheaths of the Hand
|
TABLE 7-18 Palmar Spaces and Compartments
|
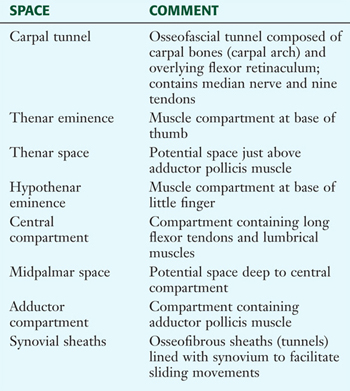 |
- Flexor pollicis brevis
- Abductor pollicis brevis
- Opponens pollicis
The hypothenar eminence is created by the following muscles (all ulnar nerve innervated):
- Flexor digiti minimi brevis
- Abductor digiti minimi
- Opponens digiti minimi
The long flexor tendons (flexor digitorum superficialis and profundus) course on the palmar side of the digits, with the superficialis tendon splitting to allow the profundus tendon to pass to the distal phalanx (Fig. 7-32). On the dorsum of the digits, the extensor expansion (hood) provides for insertion of the long extensor tendons and lumbrical and interosseous muscles. Lumbricals and interossei flex the metacarpophalangeal joint and extend the proximal and distal interphalangeal joints (see Table 7-16).
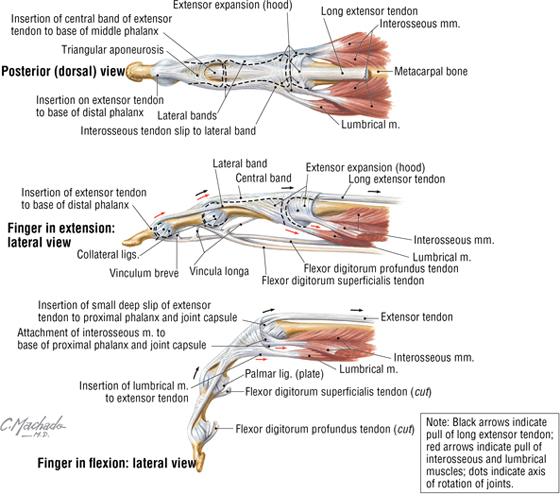
FIGURE 7-32 Long Tendon Sheaths of the Fingers
C L I N I C A L F O C U S
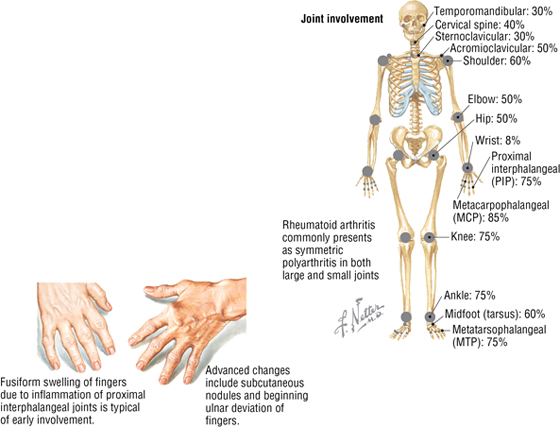
Rheumatoid Arthritis
Rheumatoid arthritis, a multifactorial disease with a clear genetic component, affects about 1% of the population worldwide and is more common in women than in men. The clinical presentation includes the following:
- Onset usually between 40 and 50 years of age
- Morning stiffness
- Warm joints and joint swelling
- Arthritis in three or more joints
- More common in small joints of wrist and hand
- Symmetrical disease
- Rheumatoid nodules
- Serum IgM rheumatoid factor
C L I N I C A L F O C U S
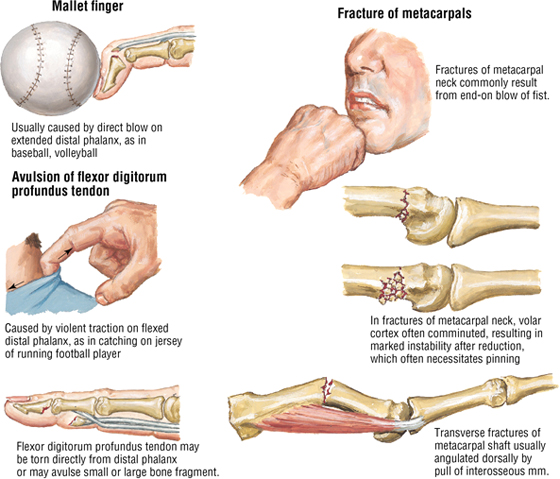
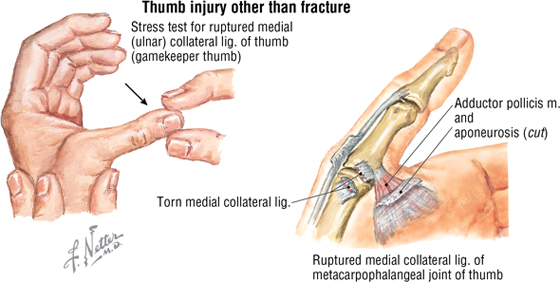
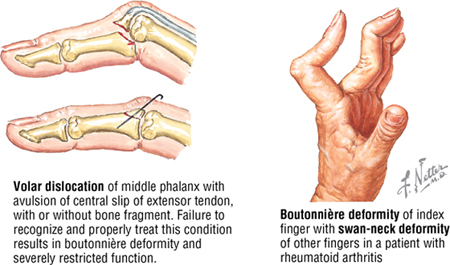
Finger Injuries
Various traumatic finger injuries may occur, causing fractures, disruption of the flexor and extensor tendons, and torn ligaments. Each element must be carefully examined for normal function, including muscle groups, capillary refill (Allen’s test), and two-point sensory discrimination.
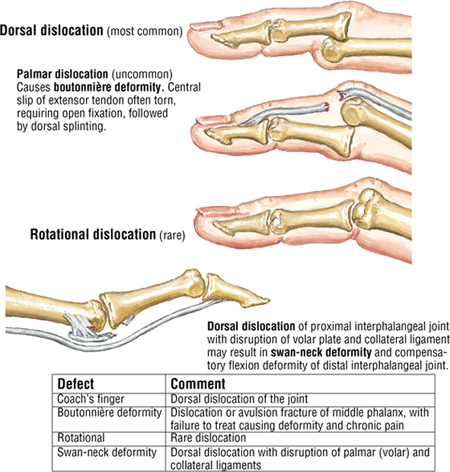
C L I N I C A L F O C U S
Proximal Interphalangeal Joint Dislocations
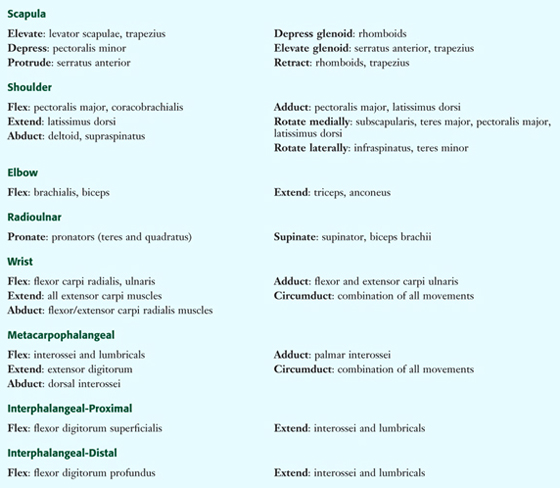
8. UPPER LIMB MUSCLE SUMMARY
Table 7-19 summarizes the actions of major muscles on the joints. The list is not exhaustive and highlights only major muscles responsible for each movement (the separate muscle tables provide more detail); realize that most joints move because of the action of multiple muscles working on that joint, but this list only focuses on the more important of those muscles for each joint.
|
TABLE 7-19 Summary of Actions of Major Upper Limb Muscles
|
 |
9. UPPER LIMB NERVE SUMMARY
Shoulder Region
Shoulder muscles are largely innervated by the suprascapular (C5, C6), musculocutaneous (C5, C6, C7), long thoracic (C5, C6, C7), and axillary nerves (C5, C6); there may be some variability in spinal segment distribution to these nerves (Fig. 7-33 and Table 7-20).
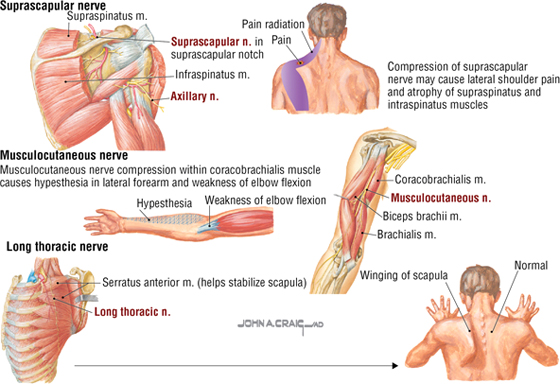
FIGURE 7-33 Shoulder Region Neuropathy
|
TABLE 7-20 Shoulder Region Neuropathy
|
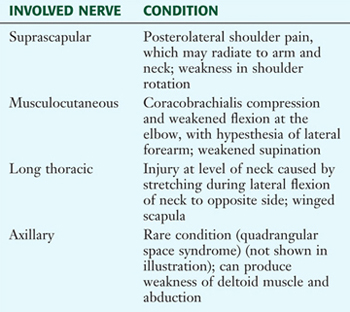 |
Radial Nerve in the Arm and Forearm
The radial nerve (C5, C6, C7, C8, T1) innervates the muscles that extend the forearm at the elbow (posterior compartment arm muscles) and the skin of the posterior arm, via the inferior lateral and posterior cutaneous nerves of the arm (Fig. 7-34).
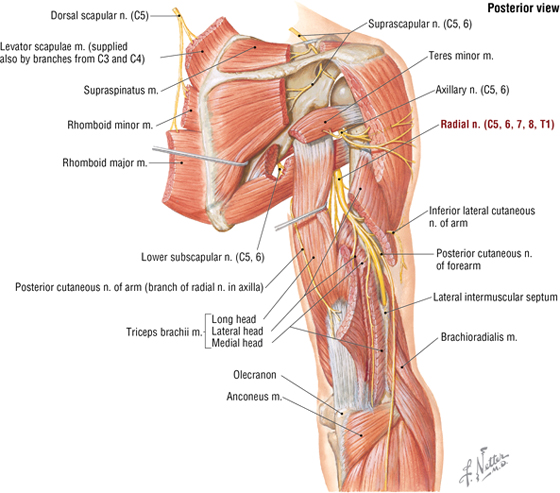
FIGURE 7-34 Radial Nerve Distribution in the Arm
C L I N I C A L F O C U S
Radial Nerve Compression
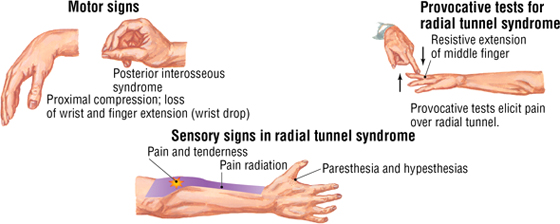
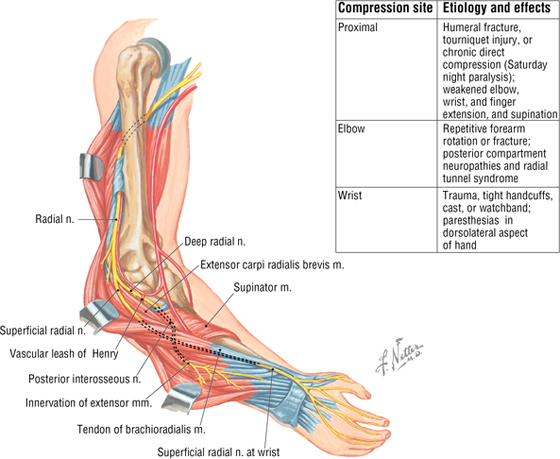
The radial nerve innervates (1) extensor muscles of the wrist and fingers and (2) the supinator (posterior compartment forearm muscles). It also conveys cutaneous sensory information from the posterior forearm and the radial side of the dorsum of the hand. Pure radial nerve sensation (no overlap with other nerves) is tested on the skin overlying the first dorsal interosseous muscle (Fig. 7-35).
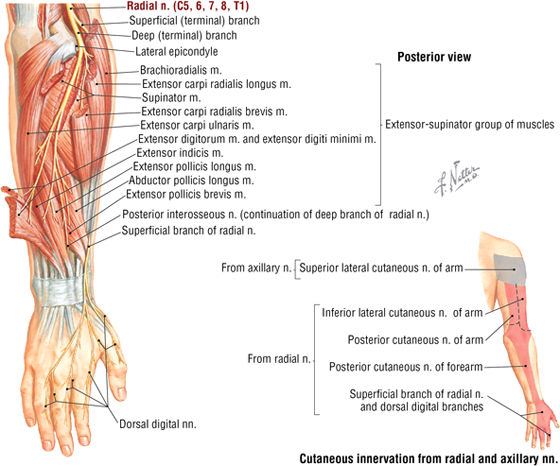
FIGURE 7-35 Radial Nerve Distribution in the Forearm and Dorsal Hand
Median Nerve in the Forearm and Hand
The median nerve (C5 variable, C6, C7, C8, T1) innervates all but the flexor carpi ulnaris and the ulnar half of the flexor digitorum profundus muscles of the anterior compartment of the forearm (wrist and finger flexors and forearm pronators). It also innervates the thenar muscles and first two lumbricals. Pure median nerve sensation is tested on the skin overlying the palmar aspect of the tip of the index finger (Fig. 7-36).
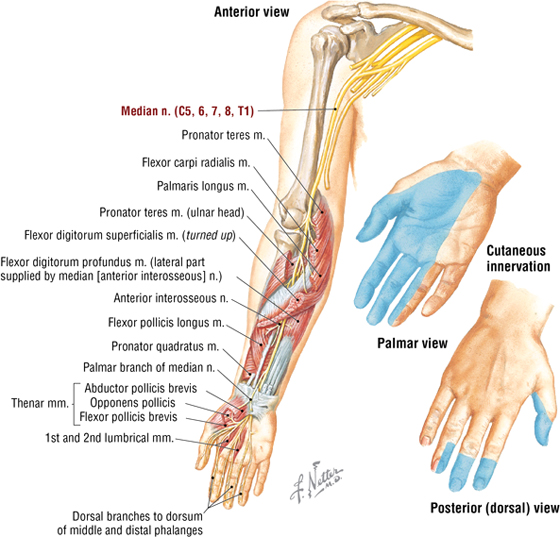
FIGURE 7-36 Median Nerve Distribution in the Forearm and Hand
C L I N I C A L F O C U S
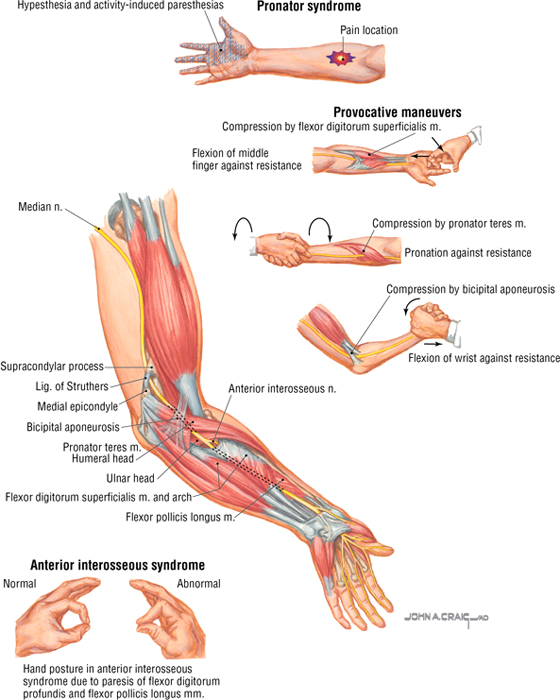
Proximal Median Nerve Compression
Compression at the elbow is the second most common site of median nerve entrapment, after the wrist (carpal tunnel). Repetitive forearm pronation and finger flexion, especially against resistance, can cause muscle hypertrophy and entrap the nerve.
Ulnar Nerve in the Forearm and Hand
The ulnar nerve (C7 variable, C8, T1) innervates the flexor carpi ulnaris muscle and the ulnar half of the flexor digitorum profundus muscle in the anterior forearm and most of the intrinsic hand muscles (hypothenar muscles, two lumbricals, adductor pollicis, and all interossei). Pure ulnar nerve sensation is tested on the skin overlying the palmar aspect of the tip of the little finger (Fig. 7-37).
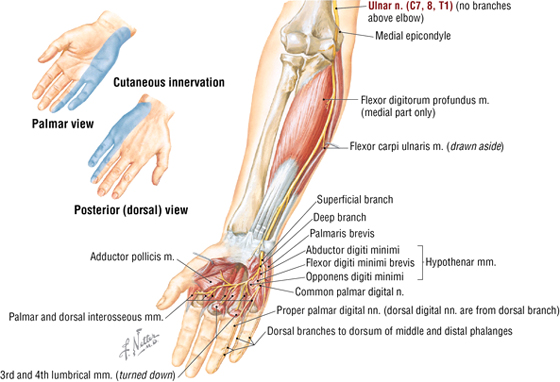
FIGURE 7-37 Ulnar Nerve Distribution in the Forearm and Hand
C L I N I C A L F O C U S
Ulnar Nerve Compression in the Cubital Tunnel
Cubital tunnel syndrome results from compression of the ulnar nerve as it passes beneath the ulnar collateral ligament and between the two heads of the flexor carpi ulnaris muscle. This syndrome is the second most common compression neuropathy after carpal tunnel syndrome. The tunnel space is significantly reduced with elbow flexion, which compresses and stretches the ulnar nerve. The nerve also may be injured by direct trauma to the subcutaneous portion as it passes around the medial epicondyle.
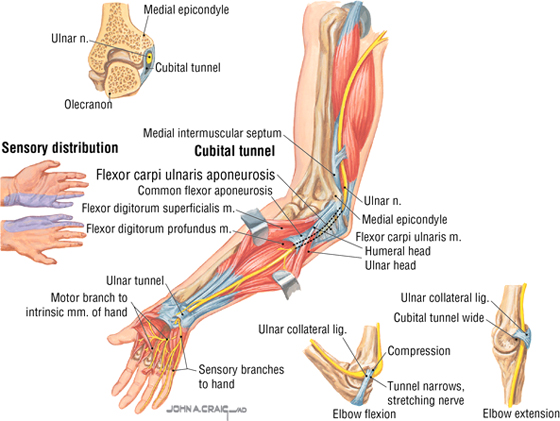
C L I N I C A L F O C U S
Ulnar Tunnel Syndrome
The ulnar tunnel exists at the wrist where the ulnar nerve and artery pass deep to the palmaris brevis muscle and palmar (volar) carpal ligament, just lateral to the pisiform bone. Within the tunnel, the nerve divides into the superficial sensory and deep motor branches. Injury may result from trauma, ulnar artery thrombosis, fractures (hook of the hamate), dislocations (ulnar head, pisiform), arthritis, and repetitive movements. Claw hand may be present if the motor components are injured.
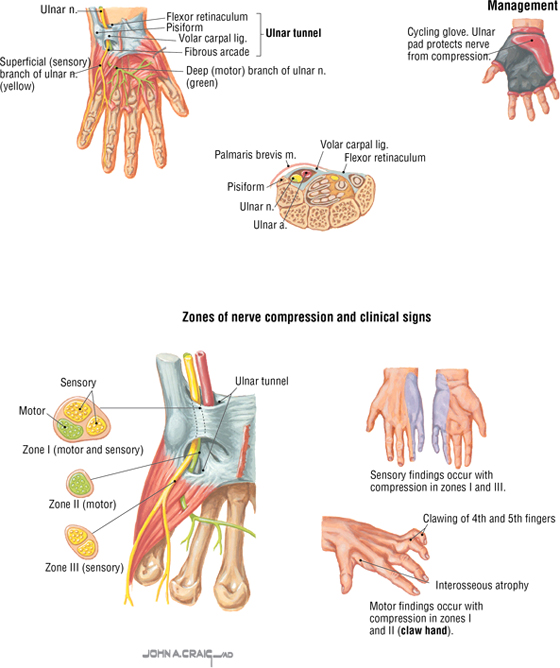
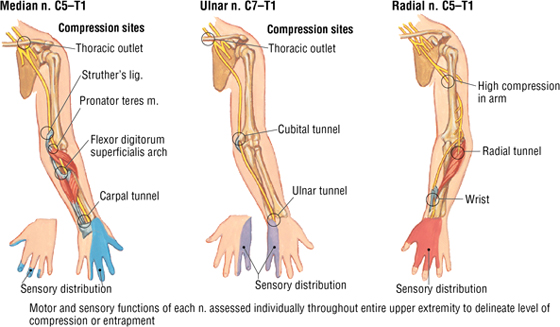
C L I N I C A L F O C U S
Clinical Evaluation of Compression Neuropathy
Compression injury to the radial, median, and ulnar nerves may occur at several sites along each of their courses down the arm and forearm. A review of the applied anatomy and clinical presentation of several common neuropathies is shown in this illustration. Refer to the muscle tables presented in this chapter for a review of the muscle actions and anticipated functional weaknesses.
10. EMBRYOLOGY
Appendicular Skeleton
Along the embryonic axis, mesenchyme derived from sclerotomes forms the xial skeleton and gives rise to the skull and spinal column (see Fig. 2-21). The appendicular skeleton forms from mesenchyme derived from the somatopleure that condenses to form cartilaginous precursors of limb bones. Upper (and lower) limb bones then develop by endochondral ossification from the cartilaginous precursors (except the clavicle, which develops by intramembranous ossification) (Fig. 7-38).
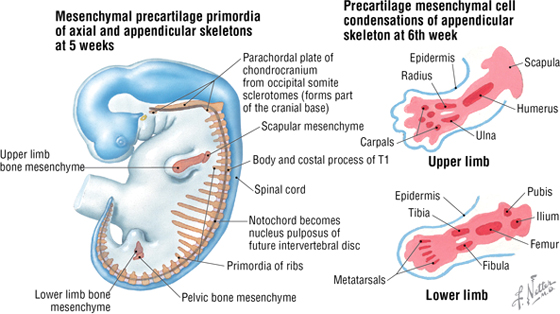
FIGURE 7-38 Development of the Appendicular Skeleton
Neuromuscular Development
Segmental somites give rise to myotomes that form collections of mesoderm dorsally called epimeres (epaxial). These epimeres are innervated by the dorsal rami of the spinal nerves. The epaxial muscles form the intrinsic back muscles. Ventral mesodermal collections form the hypomeres (hypaxial), which are innervated by the ventral rami of spinal nerves. Hypaxial muscles in the limbs divide into ventral (flexor) and dorsal (extensor) muscles (Fig. 7-39). The terminal branches of the brachial plexus (axillary, musculocutaneous, radial, median, and ulnar nerves) then grow into the limb as the mesoderm develops, supplying the muscles of each compartment.
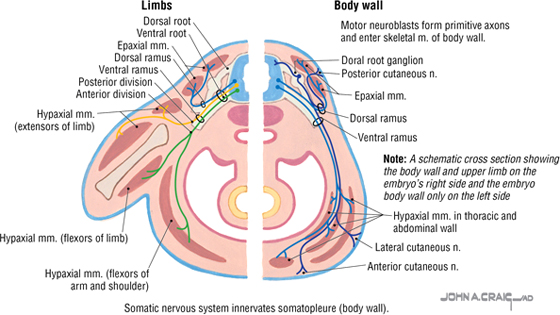
FIGURE 7-39 Neuromuscular Development
Limb Bud Rotation and Dermatomes
Initially, as limb buds grow out from the embryonic trunk, the ventral muscle mass (future flexors) faces medially and the dorsal mass (future extensors) faces laterally (Fig. 7-40). With continued growth and differentiation, the upper limbs rotate 90° laterally, so that in anatomical position the ventral flexor muscle compartment faces anteriorly and the dorsal extensor muscle compartment faces posteriorly. The lower limbs rotate 90° medially and are thus 180° out of phase with the upper limbs. (The elbow faces posteriorly, and the knee faces anteriorly.) Thus, in the upper limbs, the flexors of the shoulder, elbow, and wrist/fingers are positioned anteriorly, and extensor muscles of the same joints are aligned posteriorly.
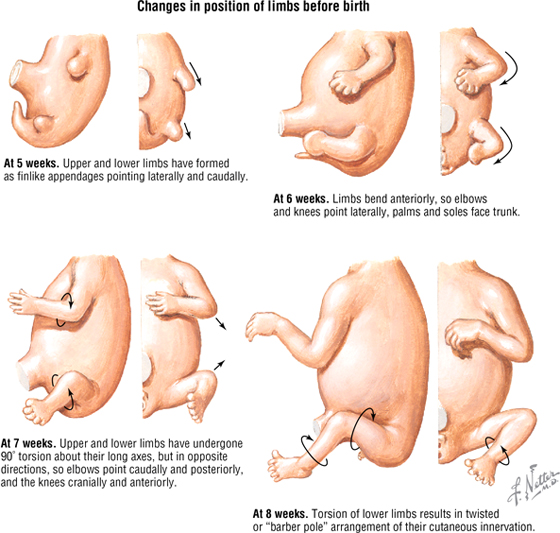
FIGURE 7-40 Limb Bud Rotation
Although the dermatome distribution on the trunk is fairly linear horizontally, on the limbs some spiraling occurs, especially on the lower limb. The upper limb is more uniform, with dermatomes (C4-T2) that closely parallel the myotome innervation from the brachial plexus (C5-T1); a small contributing branch from C4 and T2 to the brachial plexus is normally observed. As noted previously, dermatome maps vary, and overlap of sensory innervation from the dermatome above and below is common (Fig. 7-41).
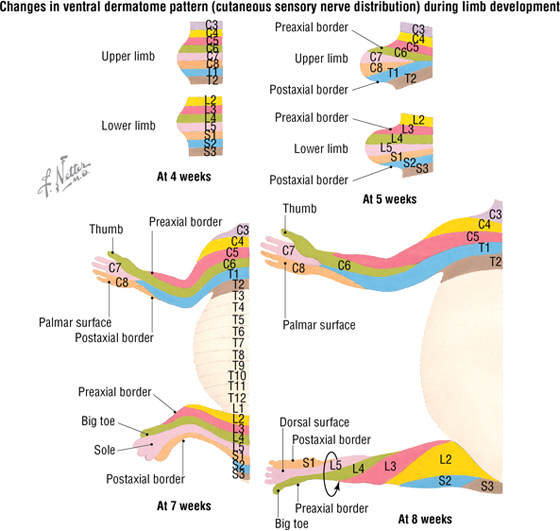
FIGURE 7-41 Limb Bud Rotation and Dermatome Patterns
C L I N I C A L F O C U S
Online Figures
Healing of fracture
Brachial plexopathy
Trigger finger
De Quervain tenosynovitis
Additional figures available online. See Table of Contents for Instructions for online access.
