CHAPTER 118 Infectious Arthritis
CHAPTER 118 Infectious Arthritis
ETIOLOGY
Infectious arthritis, or suppurative or septic arthritis, is a serious bacterial infection of the joint space that results from hematogenous dissemination of bacteria in children. Infectious arthritis less often results from contiguous spread of infection from surrounding soft tissues or direct inoculation into the joint (penetrating trauma). Spread of osteomyelitis is common and occurs with rupture into the joint space via transphyseal vessels to the epiphysis or rupture of a metaphyseal abscess in the joint where the joint capsule inserts below the epiphysis (see Fig. 117-1A). The bacteria causing infectious arthritis are similar to bacteria causing osteomyelitis (Table 118-1). Lyme disease also may cause arthritis as part of the late disease (see Chapter 122).
TABLE 118-1 Pathogenic Organisms Causing Arthritis in Children
| Common | Uncommon |
|---|---|
| YOUNG INFANTS (<2 MONTHS) | |
| OLDER INFANTS AND CHILDREN (2 MONTHS TO MATURITY) | |
| REACTIVE ARTHRITIS | |
* The incidence of invasive infections caused by H. influenzae type b has diminished greatly with universal childhood Hib vaccination.
The arthritis of disseminated gonococcal infections includes both reactive and suppurative forms of arthritis in early and late gonococcal disease, respectively. With untreated genital infection, gonococcemia may occur with fever and a polyarticular, symmetrical arthritis and rash, known as the arthritis-dermatitis syndrome. Bacterial cultures of the synovium are sterile at this stage despite a relatively high prevalence of bacteremia. Monarticular arthritis of large, weight-bearing joints develops days to weeks later. Cultures of affected synovial fluid at this stage often yield the pathogen.
Reactive arthritis is immune-mediated synovial inflammation that follows a bacterial or viral infection, especially Yersinia and other enteric infections. Reactive arthritis of the hip joints in children 3 to 6 years of age is known as toxic synovitis or transient synovitis of the hip (see Chapter 199).
EPIDEMIOLOGY
Infectious arthritis occurs most commonly in children younger than 5 years of age and adolescents.
CLINICAL MANIFESTATIONS
The typical features of suppurative arthritis include erythema, warmth, swelling, and tenderness over the affected joint with a palpable effusion and decreased range of movement. The onset may be sudden or insidious with symptoms noted only when the joint is moved, such as during a diaper change, or if parents become aware of decreased voluntary movement of a joint or limb. Toddlers may exhibit a limp. In septic arthritis of the hip, the lower limb may be preferentially held in external rotation and flexion to minimize pain from pressure on the joint capsule. Similarly, the knee and elbow joints usually are held in flexion. The joints of the lower extremity are most often involved: the knees (40%), the hips (20%), and the ankles (14%). Small joints, such as those of the hand, usually are involved after penetrating trauma or closed fist injuries.
Minor genital tract symptoms that have been ignored may precede development of the early arthritis-dermatitis syndrome associated with disseminated gonococcal infection. A history of febrile illness antedating the development of monarticular arthritis characterizes late gonococcal arthritis.
Reactive arthritis is typically symmetrical, polyarticular, and usually involves the large joints, especially the hips. Patients may have had a preceding episode of gastroenteritis or urethritis. Urethritis may appear with the arthritis.
LABORATORY AND IMAGING STUDIES
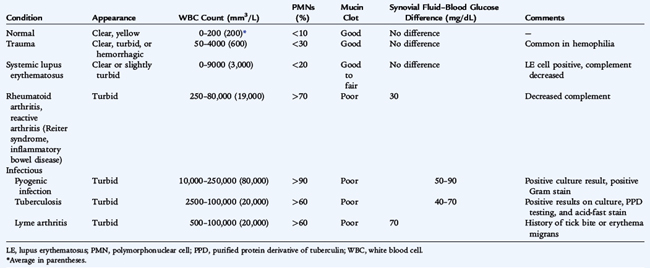
Leukocytosis and an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are common. Arthrocentesis and analysis of the effusion is the test of choice for rapid diagnosis of infectious arthritis (Table 118-2). Adolescents with acute infectious arthritis should have urethral, cervical, rectal, and pharyngeal examination and cultures or nucleic acid amplification tests performed for Neisseria gonorrhoeae.
Blood or joint cultures are positive in 70% to 85% of cases. Joint fluid that exhibits the characteristics of pyogenic infection may not reveal bacterial pathogens in 30% of patients, even in the absence of preceding antibiotic therapy, because of the bacteriostatic effects of synovial fluid. Gram stain, acid-fast stain, and potassium hydroxide (KOH) preparation for fungi should be performed and are often informative even if the cultures are negative.
Plain radiographs typically add little information to the physical findings. Radiographs may show swelling of the joint capsule, a widened joint space, and displacement of adjacent normal fat lines. Radionuclide scans are of limited use, although technetium-99m bone scans may be helpful to exclude concurrent bone infection, either adjacent or distant from the infected joint. Ultrasound is especially useful for identifying joint effusions and is the diagnostic procedure of choice for evaluation of suppurative infections of the hip. Magnetic resonance imaging (MRI) is useful in distinguishing joint infections from cellulitis or deep abscesses.
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of infectious arthritis in infants, children, and adolescents includes other infectious diseases, rheumatoid disorders, rheumatic fever, and trauma. Suppurative arthritis must be distinguished from Lyme disease, osteomyelitis, suppurative bursitis, fasciitis, myositis, cellulitis, and soft tissue abscesses. Psoas muscle abscess often presents with fever and pain on hip flexion and rotation. Juvenile rheumatoid arthritis, Kawasaki syndrome, Schönlein-Henoch purpura, other rheumatoid disorders, and Crohn disease must be differentiated from infectious arthritis. In most of these diseases, the presence of symmetrical or multiple joint involvment often excludes infectious arthritis. Suppurative bursitis with Staphylococcus aureus occurs most often in older boys and men and is usually a consequence of trauma or, less commonly, a complication of bacteremia.
TREATMENT
Initial antibiotic therapy for infectious arthritis is based on the likely organism for the age of the child and the Gram stain of joint fluid. Suppurative arthritis of the hip joint, especially, or shoulder joint necessitates prompt surgical drainage. With insertion of the joint capsule below the epiphysis in these ball-and-socket joints, increased pressure in the joint space can affect adversely the vascular supply to the head of the femur or humerus, leading to ischemic injury and necrosis. Infections of the knee may be treated with repeated arthrocenteses in addition to appropriate parenteral antibiotics.
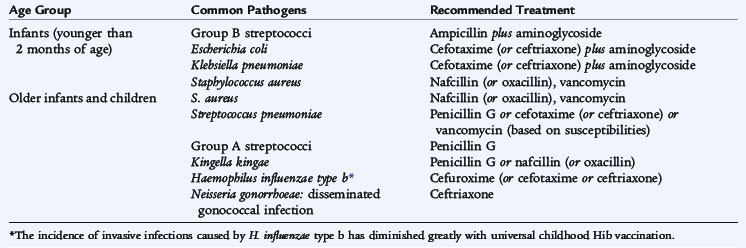
Several antimicrobial agents provide adequate antibiotic levels in joint spaces (Table 118-3). Initial therapy for neonates should include antibiotics, such as nafcillin and cefotaxime, with activity against S. aureus, group B streptococcus, and aerobic gram-negative rods. Initial therapy for children 3 months to 5 years old should include antibiotics with activity against S. aureus. Addition of appropriate antibiotics should be considered if the child is unimmunized against Haemophilus influenzae. Confirmed methicillin-susceptible S. aureus infections are treated with nafcillin or oxacillin, and methicillin-resistant S. aureus infections are treated with vancomycin, or clindamycin if susceptible.
The duration of therapy depends on clinical resolution of fever and pain and decline of the ESR and CRP. Infection with virulent organisms, such as S. aureus, usually necessitates treatment for at least 21 days. Treatment may be changed to oral antibiotics if adherence can be ensured. Oral agents with excellent activity against S. aureus that are often used to complete therapy include cephalexin, amoxicillin-clavulanate, dicloxacillin, clindamycin, and ciprofloxacin (for patients ≥18 years).
COMPLICATIONS AND PROGNOSIS
The major complications of neonatal, childhood, and gonococcal arthritis are loss of joint function resulting from damage to the articular surface. The highest incidence of these complications occurs with hip infections, presumably as a result of ischemic injury to the head of the femur. As a result, prompt open drainage of infected hip joints and often shoulder joints is critical. The high incidence of concurrent suppurative arthritis with adjacent osteomyelitis in neonates places the epiphyseal growth plate at high risk for growth abnormalities.
The prognosis for the common forms of infectious arthritis encountered in infants and children is excellent. The poorest outcome is for infectious arthritis of the hip or shoulder. Neonates with osteomyelitis have an approximately 40% to 50% likelihood of growth disturbances with loss of longitudinal bone growth and ultimate limb shortening.
PREVENTION
There are no effective means to prevent hematogenous S. aureus arthritis. Universal immunization of infants with conjugate Hib (Haemophilus influenzae type b) vaccine has practically eliminated serious bacterial infections from this organism, including bone and joint infections. Because the serotypes of Streptococcus pneumoniae causing joint infections are represented in the conjugate pneumococcal vaccine, the incidence of pneumococcal joint infections should decrease with widespread immunization.