 CHAPTER 199 Hip
CHAPTER 199 Hip
The hip is a ball (femoral head) and socket (acetabulum) joint that is important for skeletal stability. The femoral head and acetabulum are interdependent for normal growth and development. The femoral neck and head, which contain the capital femoral epiphysis, are intra-articular. The blood supply to this region is unique because the blood vessels are extraosseous and lie on the surface of the femoral neck, entering the epiphysis peripherally. Thus, the blood supply to the femoral head is vulnerable to trauma, infection, and other causes that may increase intra-articular pressure. Damage to the blood supply can lead to avascular necrosis.
DEVELOPMENTAL DYSPLASIA OF THE HIP
In developmental dysplasia of the hip (DDH), the hips at birth are usually not dislocated, but dislocatable, so the term congenital hip dysplasia or dislocation is not appropriate. The femoral head and acetabulum develop from the same mesenchymal cells; by 11 weeks’ gestation, the hip joint is formed. There are two types of DDH: teratologic and typical:
Teratologic dislocations occur early in utero and are usually associated with neuromuscular disorders (spina bifida, arthrogryposis).
Typical dislocations occur in the neurologically normal infant and can occur before or after birth.
The true incidence of DDH is unknown, but it may be as high as 1.5 cases per 1000 infants.
Etiology
Newborn infants have ligamentous laxity and, if significant enough in the hip, there may be spontaneous dislocation and reduction of the femoral head. Persistence of this spontaneous pattern can lead to pathologic changes, such as flattening of the acetabulum, muscle contractures which limit motion, and joint capsule tightening. The left hip is affected three times as often as the right hip, possibly due to in utero positioning.
Physiologic risk factors for DDH include a generalized ligamentous laxity, perhaps from maternal hormones that are associated with pelvic ligament relaxation (estrogen and relaxin). Female infants are at higher risk (9:1); 20% of all patients with DDH have a positive family history.
Other risk factors include breech presentation, first-born child (60%), oligohydramnios, and postnatal infant positioning. In breech presentations, the fetal pelvis is situated in the maternal pelvis, which can increase hip flexion and limit overall fetal hip motion, causing further stretching of the already lax joint capsule and exposing the posterior aspect of the femoral head. This abnormal position then alters the relationship between the acetabulum and femoral head, causing abnormal acetabular development. Postnatal positioning of the hips in a tight swaddle with the hips adducted and extended can displace the hip joint.
Congenital muscular torticollis (15–20% of cases) and metatarsus adductus (1–10%) are associated with DDH. An infant with either of these two conditions necessitates a careful examination of the hips.
Clinical Manifestations
Every newborn requires a screening physical examination for DDH; further evaluation through at least the first 18 months of life is part of the physical examination for toddlers. DDH evolves over time, so the examination may change as the patient ages. The examination starts with inspection for asymmetrical thigh and gluteal folds with the hips and knees flexed. A relative shortening of the femur with asymmetrical skin folds is a positive Galeazzi sign and indicates DDH. Range of motion should be assessed with the pelvis stabilized and the patient supine on the examining table, not in the parent’s lap (Fig. 199-1). Hip abduction should easily reach or exceed 75 degrees and hip adduction should reach 30 degrees. Limitations may indicate contractures associated with DDH especially decreased abduction.
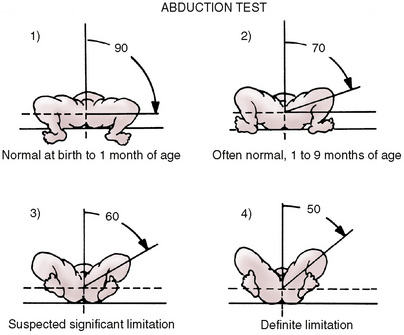
FIGURE 199-1 Hip abduction test. Place the infant supine, flex the hips 90 degrees, and fully abduct the hips. Although the normal abduction range is broad, hip disease should be suspected in any patient who lacks more than 30 to 45 degrees of abduction.
(From Chung SMK: Hip Disorders in Infants and Children. Philadelphia, Lea & Febiger, 1981, p 69.)
The Barlow test attempts to dislocate an unstable hip (Fig. 199-2). The examiner should stabilize the infant’s pelvis with one hand and grasp the abducted and flexed thigh in the other hand. The hip should be flexed to 90 degrees. Next, begin to adduct the hip, while applying a posterior force to the anterior hip. A hip that can be dislocated in this method is readily felt (clunk feeling) and is a positive test. It may reduce spontaneously once the posterior force is removed, or the examiner may need to perform the Ortolani test.
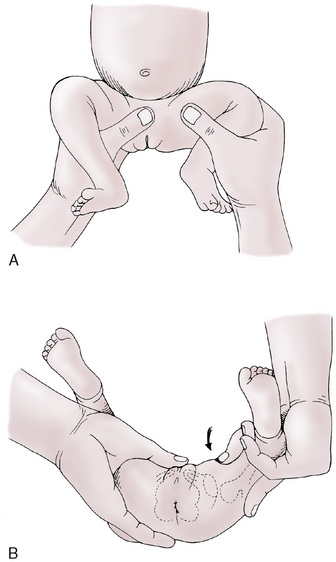
FIGURE 199-2 Barlow (dislocation) test. Reverse of Ortolani test. If the femoral head is in the acetabulum at the time of examination, the Barlow test is performed to discover any hip instability. A, The infant’s thigh is grasped as shown and adducted with gentle downward pressure. B, Dislocation is palpable as the femoral head slips out of the acetabulum. Diagnosis is confirmed with the Ortolani test.
The Ortolani test may reduce a dislocated hip (Fig. 199-3). The examiner should stabilize the pelvis and hold the leg in the same method as for the Barlow test. The infant’s hip should be in 90 degrees of flexion. Abduct the hip while applying anterior pressure to the posterior thigh. A positive test is the palpable reduction of the dislocation, which may be felt (clunk) and heard (audible click). After 2 months of age, the hip may develop muscular contractures, preventing positive Ortolani tests.
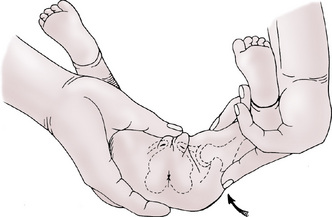
FIGURE 199-3 Ortolani (reduction) test. With the infant relaxed and content on a firm surface, the hips and knees are flexed to 90 degrees. The hips are examined one at a time. The examiner grasps the infant’s thigh with the middle finger over the greater trochanter and lifts the thigh to bring the femoral head from its dislocated posterior position to opposite the acetabulum. Simultaneously the thigh is gently abducted, reducing the femoral head in the acetabulum. In a positive finding, the examiner senses reduction by a palpable, nearly audible clunk.
These tests should be performed with only gentle force and done one hip at a time. The examiner may need to do them multiple times, as they can be difficult to interpret. It can be very difficult to diagnose bilateral DDH because of the symmetry found on examination. With time, it becomes easier to differentiate between normal hip clicks and the abnormal clunks associated with dislocation. A click may occur from breaking the surface tension of the hip joint or snapping gluteal tendons.
Older children with unrecognized DDH may present with limping. A patient with increased lumbar lordosis and a waddling gait may have an unrecognized bilateral DDH.
Radiographic Evaluation
Because the femoral head does not begin to ossify until 4 to 6 months of age, plain radiographs can be misleading until patients are older. Ultrasound is used for initial evaluation of infants with DDH. Ultrasonography is necessary for all infants with a positive family history or breech presentation.
Treatment
The treatment of DDH is individualized and depends on the child’s age at diagnosis. The goal of treatment is a stable reduction that results in normal growth and development of the hip. If DDH is suspected, the child should be sent to a pediatric orthopedist.
The Pavlik harness is an effective treatment up to 6 months of age. It provides hip flexion to just over 90 degrees and limits adduction to no more than neutral. This positioning redirects the femoral head toward the acetabulum. The hip should be reduced within 1 to 2 weeks of beginning the Pavlik harness, although the infant will need more time in the device. If the hips are not reduced during the initial weeks, then the patient will need surgical intervention or casting. The Pavlik harness is successful in treating approximately 95% of dysplastic or subluxated hips, and 80% successful for treatment of true dislocations.
Children over 6 months or those that have failed a Pavlik harness should undergo closed reduction using a hip spica cast, which is usually done under general anesthesia; reduction is confirmed by computed tomography (CT) or magnetic resonance imaging (MRI). If closed reduction fails, open reduction is indicated. Patients over 18 months of age may require a pelvic osteotomy.
Complications
The most important and severe complication of DDH is iatrogenic avascular necrosis of the femoral head. This can occur from excessive flexion or abduction during positioning of the Pavlik harness or hip spica cast. Infants under 6 months of age are at highest risk. Pressure ulcers can occur with prolonged casting. Redislocation or subluxation of the femoral head and residual acetabular dysplasia can occur.
TRANSIENT MONOARTICULAR SYNOVITIS
Transient synovitis, also known as toxic synovitis, is a common cause of limping in children. It is a diagnosis of exclusion, because septic arthritis and osteomyelitis of the hip must be excluded (see Chapters 117 and 118).
Etiology and Epidemiology
The etiology of transient synovitis is uncertain, but possible causes are viral illness and hypersensitivity. Approximately 70% of children diagnosed with transient synovitis have an upper respiratory tract viral infection in the preceding 7 to 14 days. Biopsies have revealed nonspecific synovial hypertrophy. Hip joint aspirations, when necessary, are negative for bacterial culture or signs of bacterial infection.
The mean age at onset is 6 years, with a range of 3 to 8 years. It is twice as common in male children.
Clinical Manifestations and Evaluation
The patient or family will describe an acute onset of pain in the groin/hip, anterior thigh, or knee. Irritation of the obturator nerve can cause referred pain in the thigh and knee when the pathology is at the hip. Patients with transient synovitis are often afebrile, walk with a painful limp, and have normal to minimally elevated white blood cell count and erythrocyte sedimentation rate compared with bacterial diseases of the hip (Table 199-1). Table 197-3 lists the differential diagnosis of a limping child.
TABLE 199-1 Differences Between Bacterial Infection and Transient Synovitis
| Bacterial Infection* | Transient Synovitis |
|---|---|
| Fever—temperature >38.5 ° C | Afebrile |
| Leukocytosis | Normal WBC count |
| ESR >20 mm/hour | Normal ESR and CRP |
| Refusal to walk | Painful limp |
| Hip held in external rotation, abduction, and flexion | Hip held normally |
| Severe pain and tenderness | Moderate pain and mild tenderness |
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; WBC, white blood cell.
* Examples: Septic arthritis, osteomyelitis of hip.
Anteroposterior and frog-leg radiographs of the hip are usually normal. Ultrasonography may reveal a small joint effusion. A bone scan may help differentiate transient synovitis from a septic process.
Treatment
The mainstay of treatment is bed rest and minimal weight bearing until the pain resolves. Nonsteroidal anti-inflammatory medication is usually sufficient to decrease pain. Limiting strenuous activity and exercise for 1 to 2 weeks following recovery is helpful. Follow-up will help ensure that there is no deterioration. Lack of improvement necessitates further evaluation for more serious disorders.
LEGG-CALVE-PERTHES DISEASE
Etiology and Epidemiology
Legg-Calve-Perthes disease (LCPD) is idiopathic avascular necrosis (osteonecrosis) of the capital epiphysis of the femoral head. The etiology is unclear, but it is likely caused by an interruption of the blood supply to the capital femoral epiphysis. There may be an associated hypercoagulability state (factor V Leiden).
LCPD commonly presents in patients 3 to 12 years of age, with a mean age of 7 years. It is four to five times more common in boys. Approximately 20% of patients have bilateral involvement.
Clinical Manifestations
Patients may not present for several weeks because of minimal discomfort; the classic presentation is a child with an atraumatic, painless limp. There may be mild or intermittent hip/groin, anterior thigh, or knee pain. Decreased internal rotation and abduction with some discomfort, thigh muscle spasm, and anterior thigh muscular atrophy may be present. Patients have delayed bone age.
Radiologic Evaluation
Anteroposterior and frog-leg radiographs of both hips are usually adequate for diagnosis and management. It is necessary to document the extent of the disease and follow its progression. MRI and bone scan are helpful to diagnose early LCPD.
Treatment and Prognosis
LCPD is usually a self-limited disorder that should be followed by a pediatric orthopedist. Initial treatment focuses on pain control and restoration of hip range of motion. The goals of treatment are prevention of complications, such as femoral head deformity and secondary osteoarthritis.
Containment is important in treating LCPD; the femoral head is contained inside the acetabulum, which acts like a mold for the capital femoral epiphysis as it reossifies. Nonsurgical containment uses abduction casts and orthoses, while surgical containment is accomplished with osteotomies of the proximal femur and pelvis.
The short-term prognosis is determined by the magnitude of the femoral head deformity after healing has completed. It is improved by early diagnosis, good follow-up, and compliance with the treatment plan. Older children and children with a residual femoral head deformity are more likely to develop osteoarthritis (OA). The incidence of OA in patients who developed LCPD after 10 years of age is close to 100%; it is negligible in children with onset before 5 years of age. Patients between 6 and 9 years of age have a risk of OA of less than 40%.
SLIPPED CAPITAL FEMORAL EPIPHYSIS
Etiology and Epidemiology
Slipped capital femoral epiphysis (SCFE) is a common adolescent hip disorder that is an orthopedic emergency. The incidence is 10.8 per 100,000, and it is slightly higher in males. African-American and Hispanic populations are at higher risk. Approximately 20% of patients with SCFE will have bilateral involvement at presentation, and another 20% to 40% may progress to bilateral involvement. The average age is 10 to 16 years, with a mean of 12 years in boys and 11 years in girls. Additional risk factors for SCFE include obesity, trisomy 21, and endocrine disorders (hypothyroid, pituitary tumor, growth hormone deficiency).
Classification
SCFE is classified as stable or unstable. Unstable patients refuse to ambulate. Stable patients have an antalgic gait. SCFE can also be characterized as acute (symptoms less than 3 weeks) or chronic (symptoms over 3 weeks). Acute-on-chronic SCFE is seen when more than 3 weeks of symptoms are accompanied by an acute exacerbation of pain and difficulty/inability to bear weight.
Clinical Manifestation
The presentation is variable, based on severity and type of slip. Patients will often report hip or knee pain, limp or inability to ambulate, and decreased hip range of motion. There may or may not be a traumatic event. Any knee pain should trigger an examination of the hip, as hip pathology can cause referred pain to the anterior thigh and knee along the obturator nerve. The patient usually holds the affected extremity in external rotation. As the hip is flexed, it will progressively externally rotate. There is usually a limitation of internal rotation, but there may also be a loss of flexion and abduction. If the patient can bear weight, it is typically an antalgic gait with the affected leg in external rotation. It is important to examine both hips to determine bilateral involvement.
Radiologic Evaluation
Anteroposterior and frog-leg radiographs are indicated. Patients with known SCFE or with a high index of suspicion should not undergo frog-leg lateral radiographs. Instead, a cross table lateral radiograph reduces the risk of iatrogenic progression. The earliest sign of SCFE is widening of the physis without slippage (preslip condition). Klein’s line (Fig.199-4) is helpful in assessing the anteroposterior radiograph for SCFE. The slippage can be classified radiographically as type I (0–33% displacement), type II (34–50%), or type III (>50%). The likelihood of complications increases with degree of displacement.


FIGURE 199-4 Slipped capital femoral epiphysis (SCFE). A, Anteroposterior radiograph reveals a widened physis (small arrows) and decreased height of the epiphysis on the left. In addition, there is loss (large arrow) of the Capener triangle (c) (normal double density of the medial metaphysis superimposed on the posterior acetabular rim on right) and an abnormal lateral femoral neck line (normal on right). B, Frog, lateral view confirms the inferomedial position of the SCFE.
(From Blickman H: Pediatric Radiology, The Requisites, 2nd ed. St. Louis, Mosby, 1998, p 244)
Treatment
Patients with SCFE should be immediately made non–weight bearing and referred to a pediatric orthopedist. The goal is to prevent further slippage, enhance physeal closure, and minimize complications, which is usually accomplished with internal fixation in-situ with a single cannulated screw. More severe cases may require osteotomy or bone graft epiphysiodesis to realign the femur. There is controversy surrounding the prophylactic fixation of the nonaffected side. Assessment for endocrine disorders is important, particularly in children outside the range of 10 to 16 years of age.
Complications
The two most serious complications of SCFE are chondrolysis and avascular necrosis. Chondrolysis is destruction of the articular cartilage. It is associated with more severe slips and with intra-articular penetration of operative hardware. This can lead to severe osteoarthritis (OA) and disability. Avascular necrosis occurs when there is a disruption of the blood supply to the capital femoral epiphysis. This usually happens at the time of injury, but may occur during forced manipulation of an unstable slip. Avascular necrosis may occur in up to 50% of unstable SCFEs and may lead to OA.