Chapter 1 Update of Concepts Underlying Movement System Syndromes
Introduction
Since 1980, the members of the physical therapy faculty at Washington University School of Medicine in St. Louis have been attempting to define, describe, and study the body of knowledge of physical therapy. A part of that pursuit has been the development of diagnostic categories or syndromes of conditions that are treated by physical therapists. Our efforts have resulted in the recognition that an important physiological system of the body is the movement system and that dysfunctions of this system can be classified into syndromes. These syndromes provide direction for diagnosis, treatment, and pursuing underlying kinesiopathology. The syndromes for orthopedic conditions causing musculoskeletal pain are (1) based on the movement directions or alignments that cause pain, (2) associated with movement impairments, and (3) improved by correction of the movement impairment that decreases or eliminates the symptoms. The systematic examination used to determine the diagnosis also identifies contributing factors. Based on clinical experience, research and analysis of the literature,1-28 and organization of materials for academic teaching, key concepts of the movement system that contribute to the development of pain syndromes are proposed. Understanding the following key concepts and their application to patients with musculoskeletal pain will enable the practitioner to develop an appropriate movement system (MS) diagnosis and treatment program.
The General Premise: Movement System Impairments Cause Pain Syndromes
Ten years have passed since publication of Diagnosis and Treatment of Movement Impairment Syndromes.29 The purpose of the first book was to describe a generic model for organizing musculoskeletal pain conditions into syndromes that constitute diagnostic categories to direct treatment of the mechanical aspects of the problem. The belief is that correction or modification of factors altering the precision of motion (physiological motion but also as much as possible the accessory/arthrokinematic motion) alleviates or reduces the tissue irritation and thus the painful condition. The model also described the key contributing factors to the various diagnostic groups. A major premise of the model is that pain most often arises from tissues that are stressed by subtle impairments in movement or alignment and that key factors contribute to these particular impairments. One important factor is that the body, following the laws of physics, takes the path of least resistance for movement. The activities an individual performs require movements of multiple joints that are contiguous, in the same kinematic chain (i.e., in serial arrangement), and all of which have different flexibility characteristics. The result is that one joint of those that are anatomically arranged in series moves the most easily and most readily when an individual performs an activity. Our research supports the premise that the ease and rapidity with which a joint moves are more important factors in a movement pattern associated with pain than muscle shortness, soft tissue restrictions, or limited range of motion (ROM) of an adjoining joint.6,8,15,16 These latter factors may have contributed to the initial development of the flexibility of the joint causing the pain, but once established, the offending motion has to be addressed primarily and the tissue adaptations, secondarily. Clearly, stretching muscles or soft tissues will not stop the offending motion. But when the offending motion is stopped or controlled, the appropriate tissues will be stretched.
The motion contributing to the stress occurs during the first few degrees of motion or with initiation of an activity. The primary impairment is believed to be an accessory rather than a physiological motion, which is consistent with the problem arising during the first few degrees of movement. Accessory motion hypermobility is an underlying characteristic of degenerative joint disease.30-32 Lumbopelvic motion with lower extremity motions in patients with low back pain is an example of abnormal early onset joint motion. In the prone position, lumbopelvic rotation occurs earlier and to a greater extent during the first few degrees of knee flexion and hip rotation in patients with low back pain than in control subjects, and the pattern was specific to the MS category.6,8,15,16 The predisposition of these joints to move readily contributes to the frequency of their movement and furthers the tendency for motion. Thus, a specific joint or joints of the lumbar spine, for example, develop a tendency or susceptibility to move readily in a specific direction (directional susceptibility to movement [DSM]) during all activities. In most joints, the accessory motion impairment is not clinically observable, thus the physiological motion associated with the pain is most often designated as the DSM.
Clarification of the meaning of hypermobility is essential. There are three possible meanings of hypermobility; the first is the joint ROM exceeds the ideal. The term can be applied to a physiological (osteokinematic) motion. For example, if the physiological motion of rotation between 2 cervical vertebrae is ideally 4 degrees or less, then 6 degrees of motion is hypermobility. Second, if the amount of accessory motion exceeds the normal. For example, translation between the cervical vertebrae, is 2 mm, then 3 mm of translation is hypermobility. Accessory motion hypermobility can occur even though the joint’s physiological motion is less than normal. Third, the frequency of movement of a specific joint in a specific direction occurs more often than is considered ideal. If an individual has a habit of constantly moving the head and neck when talking, the cervical vertebrae that move the most readily will also be moving the most frequently. Also, excessive frequency of motion can occur in the presence of cervical hypomobility. In the cervical spine with degenerative disc disease and exostosis, motion at some joints may be markedly restricted but limited to a lesser extent at other joints. As the individual attempts to rotate the head and neck, although the ROM of every joint is less than normal, there will still be some joints that move more readily and will move more frequently than optimal. Accessory motion will probably occur the most readily and will be greater than normal, although the physiological motion is less than normal. The attempt to achieve maximum voluntary motion with limited physiological motion will cause tissue stress and pain.
As might be suspected, when a joint moves more readily than other joints in the same kinetic chain, the repeated movements and prolonged postures associated with everyday activities can be the precipitating, as well as the perpetuating, factors of the joint’s DSM. As a result, movement in the offending direction has been associated with pain and is often impaired (deviates from the kinesiological standard). When the movement is corrected, the symptoms decrease or are eliminated. Based on the premise that the diagnosis should direct treatment, the DSM is most often also the diagnosis. Correcting the pattern or stopping the movement in the painful direction is the focus of treatment because the symptoms are decreased or eliminated by this action.
For example, rotation of some cervical vertebrae can occur more readily than other vertebrae. Supporting the shoulders can alleviate the motion restriction of the cervical vertebrae caused by the tautness of the cervicoscapular muscles. When the shoulders are supported during rotation, the motion of those vertebral joints that are usually restricted is increased. Another example is found in some individuals who move more readily at the carpometacarpal (CMC) joint of the thumb than in the metacarpophalangeal (MP) joint because the MP is the stiffest of the two joints, and the neuromuscular recruitment pattern has adapted to this difference in the two joints. When the patient grasps an object, the movement of the thumb will occur more readily and be greater in range at the CMC joint than at the MP joint. As a result, because of the increased frequency of motion, there is a greater likelihood over the years of degenerative changes at the CMC joint.
What cannot be emphasized enough is that in some regions the movement impairments are often very subtle, and detection takes practice and involves tactile, as well as visual, cues. Cervical motion is a good example. One examination method is to have the therapist assess the pattern of cervical rotation by monitoring the movement with the hands. The patient sits in a chair with the forearms on armrests that are elevated enough to alleviate the downward pull on the neck from the weight of the upper extremities. The therapist, while standing behind the patient, lightly places the hands almost all the way around the posterolateral aspects of the cervical spine with the fingers on the jaw and thumbs at the base of the skull (Figure 1-1). The patient actively rotates the head and neck, as the therapist goes “along for the ride” to be able to detect the natural pattern of motion rather than just assessing ROM or controlling the motion. In patients with neck pain, a common pattern is a very rapid upper cervical motion with either slight side-flexion, or extension motion in the lower cervical area rather relatively precise rotation. Precise motion is envisioned as rotation around a rod running through the head and cervical spine. These patients may also complain of popping or clicking during the motion. Most often the therapist also has to correct the starting alignment of the patient’s head and neck before the patient initiates the motion. Then the patient is instructed to very easily turn the head and neck. When the patient exerts a minimal rather than a “natural” effort, the range will be the same, but the clicking and popping will cease or be minimal. The therapist also very easily guides the motion so that its pattern is more precise than the natural pattern. By minimizing the muscle contraction the muscles are not developing as much tension in either the rotational or the stabilizing direction, which decreases interjoint forces and the compression among the cervical vertebrae. The patient established a pattern of recruitment that was necessary to overcome the usual amount of tension required to rotate the head and neck because of the downward pull of the shoulders or some other perceived resistance. Although the load was reduced by supporting the arms, the active tension was not automatically adjusted. Often, once the patient “learns” to use less active tension and to perform the motion precisely, the new pattern can be used even without arm support.
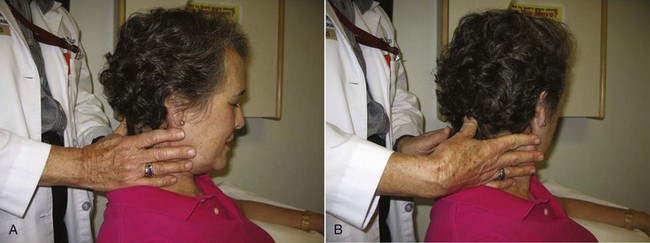
Figure 1-1 Hand position for assessing quality of cervical rotation. A, Initial position. B, Therapist initially follows the motion as the patient actively rotates the head and neck. If there is a movement fault, the therapist gently guides the motion to provide precision as the patient actively rotates the head.
As stated previously, the movement direction or alignment that most consistently causes or increases the patient’s symptoms and that, when corrected, decreases or alleviates the symptoms is considered the diagnosis. Movements of the limbs also impose forces and motions on spinal segments, so the symptoms can also be elicited by limb movements. The complete description of all the impairments evident as signs or causing symptoms that contribute to the offending or principal movement impairment is the syndrome. As with other diagnoses used by medical practitioners, factors contributing to the diagnosis are delineated as part of the description of the syndrome. The formulation of a theory of the underlying mechanisms, as well as the specific syndromes and contributing factors, then becomes a basis for research.
This book attempts to clarify and develop consistency in explaining the concepts and the terminology used to describe MS syndromes. The conditions described in this book are characterized as problems of the MS because the emphasis has been on identifying the offending movement, alignment and role of contiguous joints, and general limb movements in the condition. The movement problem and many of the contributing factors are considered as impairments rather than pathological conditions, at least early in the development of the condition. Impairment is defined as any disorder in structure or function resulting from anatomical, physiological, or psychological abnormalities that interfere with normal activities.33 In this book, impairments at the tissue level are described in stages that guide the progression from tissue protection to progressive and systematic stress. The staging addresses the changes in classification from tissue protection to a MS syndrome that can be determined once the patient’s condition permits the performance of the necessary examination.
The Human Movement System
The human movement system is a physiological system of the body that produces motion of the body or its component parts, or the functional interaction of the structures that contribute to the act of moving.34 As depicted in Figure 1-2, the physiological actions of other body systems combine to compose the movement system, with biomechanics playing an important role as the interface among the skeletal, muscular, and nervous systems.
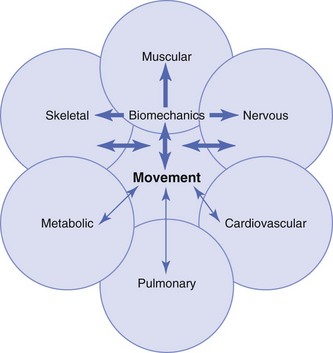
Figure 1-2 Schematic of the physiological systems that comprise the movement system and depiction of biomechanics as an important interface. The relative width of the arrows indicates amount of contribution. The arrows in both directions indicate that not only do these systems produce movement but that they are all also affected by movement.
In an attempt to understand the development of musculoskeletal pain, the original kinesiopathological model has been expanded to provide a more complete although complex description of some of the contributing factors to MS syndromes (Figure 1-3). Kinesiopathological refers to how movement that is excessive, imprecise, or insufficient contributes to the development of pathology. The complexity of the model stems from an attempt to provide a relatively complete description of the major factors and interactions that contribute to movement becoming imprecise, causing pain and pathological problems. In addition to providing theories for research, this model is particularly important for purposes of diagnosis and treatment of musculoskeletal problems. Based on kinesiology, no one segment or region of the system can be affected in isolation. A traditional approach to musculoskeletal conditions is to identify and treat the tissues considered to be the source of the pain or the pathoanatomical structures. Most often, the painful tissues have been progressively subjected to microtrauma because of movement impairments or alterations in the precision of motion, and the end result is macrotrauma. As stated by Adams and Dolan, “Skeletal tissues respond actively to their mechanical environment so that the end result of mechanical loading can vary between adaptive remodeling and biological ‘degeneration,’ depending on the precise circumstances.”35 Importantly, the adjoining body regions are most often a contributing factor to the movement impairment.
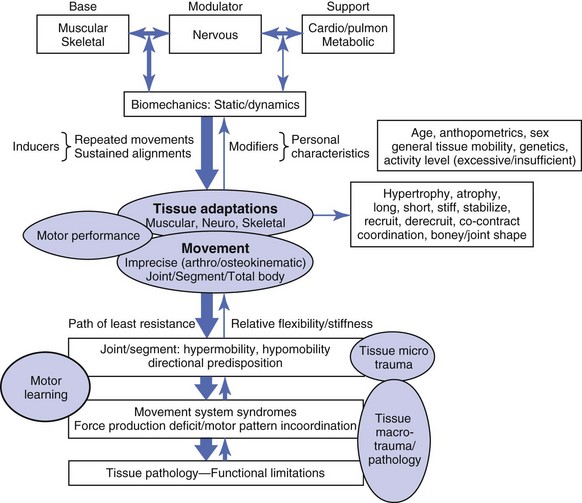
Figure 1-3 The kinesiopathological model of the human movement system depicting factors leading to the development of movement system (MS) syndromes.
Although tissues of the body are known to be subjected to progressive degeneration from aging and microtrauma, the traditional approach to understanding the condition is not based on assessing the interactions of these two factors. Rather, treatment has been more consistent with a condition that (1) arises from an isolated trauma to one specific painful site and (2) can be immediately rectified by treatment focused on that site. The concepts proposed in this book are designed to have the practitioner consider all anatomical, physiological, and biomechanical interactions of the multiple body regions that contribute to the cause and that perpetuate the microtrauma and eventual macrotrauma of one specific region of the body. Research and clinical practice has demonstrated that alterations in motor control and muscle deficiencies underlie many of the biomechanical interaction contributing to the development of MS syndromes. We have subclassified the syndromes as motor pattern incoordination or force produce deficit problems. In some patients, both factors are present. The human movement system consists of highly interactive components, thus diagnosis and treatment must take this into consideration. Simply said, the movement of the hips and even the arms can cause and contribute to low back pain,4,25 just as movements of the arms can contribute to neck pain and movement of the shoulder can contribute to hand problems. The alignment of the trunk contributes to back and neck pain, and the alignment of the pelvis and trunk affects the knee, as well as the foot. A comprehensive appreciation for these relationships and for the multiple tissue adaptations that become contributing factors is essential, and this model is an attempt to share the information that has been developed, with full appreciation that this is only a beginning, and to provide a useful foundation for future studies and clinical analysis.
Elements of the Model
The model, consisting of base, modulator, and support elements, describes the generalized contributions and functions characteristic of a dynamic system and the factors contributing to the development of musculoskeletal pain conditions.
Base Elements
The components of the base elements are the muscular and skeletal systems. These systems are considered the base elements because they consist of the tissues that provide the foundation and the structure of the system.
Modulator Element
The component of the modulator element is the nervous system. The term modulator is used to emphasize the regulator activity of the nervous system. Besides the role of modulating muscular activity, the nervous system also plays a role in the psychosocial aspects of musculoskeletal pain. Although psychosocial aspects are important regulators in the development of the condition, reaction to the condition, and participation in resolution of the condition, these aspects are beyond the intention and scope of this book.
Support Elements
The components of support elements are the cardiovascular, pulmonary, and metabolic systems. These systems do not contribute directly to movement, but as indicated by the term support, they provide the nutrients and substances required for maintaining the viability and health of those systems that do directly produce movement. The lack of physical activity or exercise causes pathological changes in the cardiovascular and metabolic systems and thus compromises the health of the individual. This book does not discuss or describe the type of exercise designed to optimize the components of the support elements, but the importance of the type of training required for optimizing endurance and cardiovascular and metabolic function is recognized. Often, individuals cannot initiate or continue with endurance exercise because of musculoskeletal pain. Therefore material about optimizing movement is considered essential to preventing or minimizing the development of musculoskeletal pain conditions that prevent participation in endurance exercise.
Biomechanics
The model indicates that biomechanics is an interface between muscular and neurological activity. The pattern of muscular recruitment is highly influenced by relationships to gravity, as well as the force required to move the extremity and react to external forces. The design of the movement system also provides a variety of strategies to develop a moment about a joint. Many of those strategies are determined by biomechanics. For example, control of knee flexion in the standing position can be (1) the direct result of eccentric contraction of quadriceps muscle, or (2) an indirect result of contraction of the hamstrings acting as hip extensors as long as the foot is fixed. The demands on the force requirements from these muscles is either increased or decreased, depending on whether the line of gravity is anterior or posterior to the knee joint. If the line of gravity is anterior to the knee joint, the demand on muscle force is decreased. If the line of gravity is posterior to the knee joint, the demand on muscle force is increased. Gravitational forces also influence the shape of weight-bearing bones and joints (discussed in the “Tissue Adaptations of the Skeletal System” section). Specific examples of how the therapist needs to consider biomechanical factors are detailed in subsequent sections.
Tissue Adaptations
The dynamic and biological characteristics of the components of the movement system enable tissues to adapt to the demands placed on them.36 The specific tissue adaptations are normal biological responses to forms of stress but may contribute to deviations from principles of kinesiology. For example, alterations in muscle length, strength, and stiffness can affect the precision in joint motion. In combination, these adaptations can become problematic. The key adaptations of the skeletal, muscular, and nervous systems and how they contribute to the development of musculoskeletal pain are described in some detail in the appropriate section.
Inducers
The repeated movements and sustained alignments associated with everyday activities are the inducers of the tissue adaptations. When an individual undertakes a “training program,” either for increasing muscle strength or improving cardiovascular endurance, there is an expectation that tissues will change. What is not readily appreciated is that every aspect of an individual’s activities, whether passive or active, also induces changes in tissues. Although the physically active person will improve and increase the size of muscles and connective tissues, at the same time, the risk of injury also increases. Musculoskeletal pain problems and injuries of athletes mostly occur from noncontact stress. Golfers develop back, elbow, wrist, shoulder, and knee problems.37 Tennis players also develop shoulder, elbow, and knee problems. Studies have been directed toward identifying the injuries associated with sports activities because of the frequency and costs.38 The repetitive use of specific segments of the body combined with high and rapid force development can exceed tissue tolerance, resulting in microtrauma. Obviously, not all golfers, tennis players, or other athletes use the same movement patterns, and some of those patterns are more optimal than others. At the other extreme, even individuals who are inactive induce changes by the alignment and movements while sitting and during work activities. Alignments maintained for prolonged periods can induce changes in muscle length. Without activity, muscle and connective tissues are not stressed enough to provide optimal tissue health. Similarly, constantly leaning in one direction or rotating frequently to one side can also induce changes in muscles, joint alignment, and the precision of motion. A relatively frequent example is evident in women who have held babies on their hip, usually the left hip if they are right handed. The typical postural adaptation is for the trunk to shift to the right, slightly rotate to the right, and side flex to the left. Needless to say, the more prolonged the activity in hours per day, days per week, weeks per year, and for extended years, the more exaggerated the posture. Most often the patient is totally unaware of this adjustment. Importantly, even though the activity has ceased, the ideal alignment is not restored unless a specific effort is made to correct the posture. If a patient has decreased ROM of the knee joint, the treatment is to perform repeated movements to improve and increase the ROM. Improvement is achieved by changes in the tissues. When everyday activities involve repeated movements in a specific direction, the movement in that direction occurs more readily and easily because of the tissue changes. Also, once a joint develops a tendency to move easily and readily in a direction, that movement will occur with all activities involving that joint and not just the one that induced the joint changes. The therapist must obtain information about the activities (work, fitness, and leisure) that the individual performs on a regular basis. Awareness of how an individual performs an activity is particularly important. After completing the examination and identifying the DSM, that information is used to assess whether the patient’s activity involves the offending motion. For example, if the patient has neck pain that occurs with rotation and the evening activity is watching television, the viewing position often involves maintaining a rotated position because the chair does not face the TV. As explained in Chapter 3, a common factor in neck pain is that the patient is constantly moving the head and neck when communicating as part of body language. The therapist begins to gather pertinent information by observing preferred positions and body language, as well as from the history.
Modifiers
Although repeated movements and sustained alignments are proposed as inducers of tissue adaptations, there are modifiers that affect the adaptations. The modifiers are factors such as age, sex, height, weight, and genetic characteristics that include predisposition to osteoarthritis, benign general joint hypermobility, structural or anthropometric characteristics, and the amount and type of activity. A few generalizations about these modifiers can be useful in assessing their role in the development of movement impairments.
Age
In young individuals, tissues are more extensible and joints more flexible than in older individuals. Thus the offending motions are usually of greater ROM than the motions in an older patient. The health of the tissues is better in the younger individual than in the older individual because some degree of degeneration is already present with aging, although degenerative changes in the spine have been reported in individuals who are only 20 years of age.39 In older individuals or those with a chronic condition, the movement impairments are usually more subtle so that the examination requires careful observation and usually slight corrections. The treatment using movement corrections and stabilizing exercises requires even greater precision in the older individual than in the younger patient. The way everyday activities are performed becomes even more critical in the older than in the younger individual. For example, a younger individual can sit leaning on one arm for prolonged periods without experiencing pain, but a short duration of leaning to one side can cause pain in an older individual. The prolonged alignments that have been used for years have usually induced tissue, bony, and structural changes in the aging such as the reduced height of intervertebral discs and changes in the facet joints. Other structural changes that can contribute to the pain syndrome are loss of the normal cervical curve and an acquired kyphosis or degenerative scoliosis.
Sex
Studies of patients with low back pain have demonstrated a difference in the pain-inducing movements and alignments between men and women.11,17 The broader shoulders, higher center of gravity, and larger and stiffer muscles in men as compared to women also contribute to differences in tissue adaptation and movement patterns. The greater incidence of anterior cruciate ligament (ACL) injuries in women as compared to men is an example of variations in tissue adaptation that can be attributed to sex.40,41 Recent studies demonstrate that women use more quadriceps activity during jumping than men and less hip extensor activity, creating different forces at the knee joint.42,43
Tissue Mobility
Of the genetic factors, benign joint hypermobility syndrome is one of the important problematic characteristics.44 Individuals with hypermobility (Figure 1-4) seem to be more disposed to musculoskeletal pain problems than individuals with tissues that limit joint excursions; this occurs not only with the physiological motion but particularly in the accessory motions. Maintaining good alignment and precise motion is more difficult if the individual is hypermobile as compared to individuals with tissue stiffness. For example, individuals with tissue hypermobility tend to have depressed shoulders and the downward pull on the neck can contribute to the development of neck pain. These problems are particularly evident in women with large breasts whose bra straps exert a downward pull and who have held children in their arms for long periods of time over several years. These tissue adaptations do not reverse after cessation of the activity. Maintaining good alignment of the trunk and the knees is also difficult for the patient with joint hypermobility. In the presence of joint hypermobility, the individual with a supinated foot will tend to have knee hyperextension, whereas another individual without a rigid foot will tend to develop a pronated foot. Therefore one of the important assessments during the examination is obtaining information about the general tissue and joint mobility and the effects on alignment and movement patterns. Treatment programs for these individuals are usually more challenging than for individuals with tissue stiffness because most often, specific exercises are not as useful as constant attention to alignments. The hypermobile individual will usually respond quickly to exercises to correct alignment, but equally as rapidly the original alignment will return, which is why these individuals must correct their alignment frequently during the day.

Figure 1-4 Forward bending with excessive hip flexion indicates generalized joint hypermobility. The lack of passive tension of the hip extensor muscles contributes to the failure to reverse the lumbar curve during forward bending. Low back pain is alleviated because of the unloading of the spine and the distraction of the trunk in this position. This condition makes maintaining good alignment and movement control difficult.
Anthropometrics
Body proportions are also a contributing factor in predisposing an individual to musculoskeletal problems. For example, a long trunk is usually associated with depressed shoulders and often neck pain. The reason is that the armrests on chairs are too low for an individual with a long trunk; therefore the shoulders are allowed to drop to support the forearms. The structure of the thorax is also a factor because the rib cage can be more barrel-shaped with a greater anterior-posterior dimension than a medial-lateral dimension. The barrel shape affects the position of the scapula and can contribute to shoulder joint problems. The carrying angle of the elbow is also related to the width of the pelvis. This aspect of assessment overlaps with the identification of structural variations.
Activity Level
The activity level can range from excessive, which tends to exacerbate the development of musculoskeletal pain problems, to insufficient activity. The consequence of insufficient activity is usually related to metabolic and cardiovascular problems, although musculoskeletal problems can also develop because of muscle weakness and poor support of the trunk. If the individual initiates an exercise program that is not carefully designed, injuries can develop more readily than if they had been previously active. The therapist needs to also factor into the examination whether the pain condition is from excessive activity that can be associated with problems from muscle hypertrophy and associated stiffness, as well as motor pattern incoordination, or from a lack of activity in which a systematic increase in physical activity and exercise to improve the force production deficit is necessary. In the former situation, part of the treatment may be to decrease the demands on specific muscles and increase the extensibility of those muscles.
Excessive activity in a young male
A competitive 36-year-old male cyclist developed neck pain because of the shortness and stiffness of the rectus abdominis muscle combined with the extended position of the cervical spine. The intense activity of the competitive cycling requires the abdominal muscles to contract about 60 times per second during the increased rate and dept of breathing. In addition, the abdominal muscles are stabilizing the pelvis, which is necessary to stabilize the attachments of the proximal hip muscles involved in the pedaling action. These actions of the abdominal muscles are occurring in a position in which the muscles are in a shortened length. This individual also is a stock broker who sits all day working on several computer screens. His head, neck, and thorax will be in the same position working on the computer and riding the bicycle. He also frequently rotates his head and neck to view the multiple computer screens. The hypertrophy of the abdominals in the shortened position depresses the chest and restricts the elevation of the rib cage. The depression and restriction to elevation of the rib cage creates a downward pull on the scaleni muscles that attach to the rib cage. Because these muscles flex and rotate the cervical spine, excessive tension on the attachments of the scaleni muscles would increase the resistance to neck extension and rotation. This patient needs to elongate the abdominal muscles and refrain from performing abdominal muscle exercises.
Excessive activity in a female with structural and genetic modifiers
A competitive 28-year-old female cyclist developed knee pain. She has a wide pelvis with prominent trochanters, femoral anteversion, and genu valgus. The characteristics of her hips are consistent with coxa vara that is associated with genu valgus. During forward bending, she has 100 degrees of hip flexion, which is indicative of general tissue hypermobility. When cycling, her femur is directed medially, while her tibia is laterally rotated. The cycling in the hip flexed position with the tibia in lateral rotation has resulted in shortness of the tensor fascia lata-iliotibial band (TFL-ITB). During the hip flexor length test, her tibia laterally rotates from the passive tension of the TFL-ITB as the hip is lowered to the fully extended position, and knee pain is experienced. The lateral rotation of the tibia is decreased if the hip is allowed to abduct during the length test. During a step up as well as during sit-to-stand and reverse, her knee is directed medially. If she actively contracts the hip lateral rotator muscles during these movements, the knee pain is reduced. The femoral anteversion and genu valgus has predisposed her to tibiofemoral rotation of the knee, which has become exaggerated by the intensity of her cycling. She needs to correct the tibiofemoral rotation during basic activities, and she can also stretch the TFL-ITB by using the 2-joint hip flexor test position and letting the hip abduction during the lowering to neutral from hip flexion. When lowering the leg, she needs to actively medially rotate her leg. Once she is in the neutral or hip extended position, she can adduct her hip but stop the motion if she has pain in the knee. If she sleeps on her side, she needs to sleep with a pillow between her knees and not allow her hip to be flexed and medially rotate while the tibia is laterally rotated.
Activity in an aged female with structural changes
A 68-year-old female who is recently retired decided to undertake a weight training program. She has lost 2 inches in height, and she has a marked thoracic kyphosis and a very prominent abdomen. She is doing lat pull downs on a weight training machine. She is sitting forward on the seat and trying to pull the bar down behind her head. She is also using an abdominal strengthening machine in which she sits and holds onto pads with her arms and rotates from one side to the other. She is beginning to develop thoracic pain and some pain in her legs. Observation indicates that as her shoulders flex to begin the lat pull down her rib cage elevates and her lumbar spine extends. Then, during the pull down phase of the motion, the thoracic spine flexes. When her shoulders are flexing, she is compensating for the thoracic kyphosis by extending her lumbar spine. The pull of the lattisimus dorsi muscle is also extending her lumbar spine. Because of insufficient strength in her latissimus dorsi muscle, she is flexing her thoracic spine instead of isolated shoulder extension. During the abdominal muscle exercises, she rotates at the apex of the thoracic flexion curve and extends her lumbar spine. This woman’s pectoral muscles are stiffer than her abdominal muscles; therefore, when she eccentrically contracts her pectorals, they elevate the rib cage. Her thoracic pain is caused by the elevation of the rib cage during the lat pull down exercise, which is also contributing to the thoracic kyphosis. The abdominal machine is causing rotation of her rib cage at a specific segment that is predisposed to rotation because of the kyphosis. The increase in lumbar extension is causing her to develop symptoms in her legs from the narrowing of the intervertebral space associated with extension. She already has compromised spacing of the vertebrae as indicated by the loss of height. To correct the performance of these exercises, she needs to contract her abdominals as the bar is going up and not try to restrain the motion with her shoulder flexor muscles. She needs to sit against the back of the seat and pull the bar forward, and she needs to avoid both thoracic flexion and lumbar extension. She also needs to contract her abdominal muscles during the pull down phase. She should stop the trunk rotation exercise.
Tissue Adaptations of the Skeletal System
Although skeletal structures seem relatively fixed, bone is a dynamic tissue that is constantly being modified by the forces acting on it. For purposes of this material, the modifications of skeletal structure and alignment can be considered both dynamic and static. Dynamic conditions are correctable and sometimes easily modifiable, whereas the static conditions are relatively permanent or structural. The dynamic conditions are the postural malalignments associated with an acquired thoracic kyphosis, whereas the static or permanent kyphosis is present in individuals with Scheuermann’s disease. The alignment of the thorax is a major factor in patients with neck pain. A thoracic kyphosis requires the individual to extend the head and neck. In younger individuals without changes in the cervical discs or vertebrae, the alignment will not be immediately pain inducing. In the older individual with degenerative joint changes in the cervical spine, the forced cervical extension from a thoracic kyphosis is usually pain inducing. The therapist must determine if the kyphosis is acquired or fixed in order to be able to develop a feasible and effective treatment program. Acquired rotation of the thoracic spine can be the result of sitting postures, throwing or even carrying a backpack, whereas a fixed scoliosis in a younger individual or a degenerative scoliosis in an older individual is permanent. In Chapter 4, the differences in postural and structural scoliosis are discussed. Similarly, as described in Chapter 7, there are acquired postural faults, such as standing with the knees in varus as the result of hip medial rotation and knee hyperextension, that can be corrected (Figure 1-5). In contrast, some individuals have a structural varus that is not correctable but needs to be monitored because of a predisposition to or the presence of degenerative knee joint disease (Figure 1-6).

Figure 1-5 Genu varus and correction. A, Postural genu varus of the left knee from hip medial rotation and knee hyperextension. B, Correction of knee alignment by contracting hip lateral rotator muscles.

Figure 1-6 Structural genus varus of left knee. This degree of varus and the enlargement of the knee is indicative of degenerative joint disease.
Another consideration is the effect of prolonged forces on the shape of bones and joints. The changes that take place in the shape of long bones and in the joint when an individual has stood for many years in knee hyperextension is consistent with Wolff’s Law.45 Wolff (1836-1902) proposed that “changes in the form and function of bones, or changes in function alone, are followed by changes in the internal structure and shape of the bone in accordance with mathematical laws.” During development, the bones will adopt a shape according to the forces imposed on them. In mature bone in which the general shape is established and no changes are made in the distribution of forces, the change is in the mass according to the mechanical demands. Prolonged standing with the knees in hyperextension results in sagittal plane varus (bowing) of the tibia and fibula, changes in the shape of the articular surface of the tibia, and changes in the alignment of the femur and the tibia (Figures 1-7 and 1-8). Changes in the shape and alignment of the joint also affect the characteristics of the ligaments and the distribution of forces on the articular cartilage, as well as alter the precision of joint motion. As noted in Figure 1-7, B, the position of the patella in the individual with hyperextended knees is lower than in the individual with well-aligned knees. Even in the corrected knee position (see Figure 1-7, C), the patella still sits inferiorly. Such positioning is consistent with the reduced use of the quadriceps because of the knee remaining in the locked position as compared to the frequent intermittent use of the quadriceps to prevent knee flexion that occurs in individuals with well-aligned knees (see Figure 1-7, A).

Figure 1-7 A, Normally aligned knee. B, Hyperextended knee. C, Hyperextended knee in the corrected position. The bowing of the tibia and fibula in the knee that has been maintained in hyperextension for years is consistent with the effects on bone expressed in Wolff’s law.
(From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
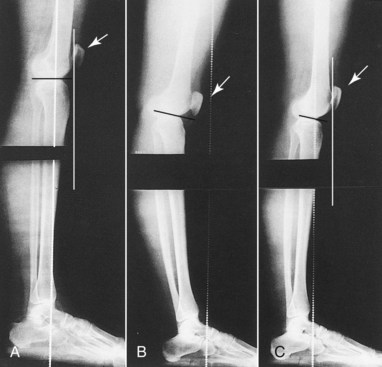
Figure 1-8 A, Normally aligned knee. B, Hyperextended knee. C, Hyperextended knee in the corrected position. In addition to the bowing of the tibia and fibula in the hyperextended knee, a number of other factors could predispose this knee to injury. The articular surface of the tibia is not horizontal, the femur is forward of the tibia, stressing the cruciate ligaments, and the patella sets low, reflecting minimal use of quadriceps.
(From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
A major consideration is how skeletal alignment, both acquired and structural, affects the demands on muscle participation. Individuals with good alignment where the line of gravity is only slightly behind (hip) or in front (knee) of the joint center when standing are constantly altering the participation of the anterior and posterior musculature as the line of gravity oscillates from posterior-to-anterior relationships to the joint (Figure 1-9). The same principle applies to the trunk: If the trunk is swayed forward, the back extensors and hip extensor muscles become active (Figure 1-10, A). If the trunk sways backward, the abdominal and hip flexor muscles become active (Figure 1-10, B). The initial observations of a patient with pain problems should be an assessment of the alignment and the participation of musculature based on the relationship to the line of gravity. Awareness of the structural and muscular consequences of postural faults reinforces the belief that beginning in childhood, all individuals should be monitored on a yearly basis to assess acquired skeletal malalignment and monitor structural variations. Based on the results of the examination, the therapist can recommend corrective postural training and exercise programs.
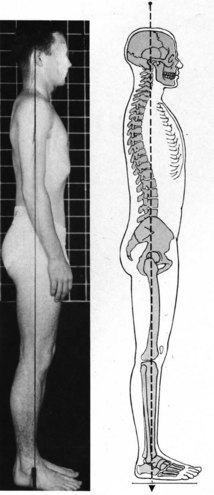
Figure 1-9 Ideal alignment. Optimal distribution of forces on bones and joints and the length and balanced stiffness of muscles and supporting structures. Also, with this type of alignment, when the individual leans forward slightly, the posterior muscles become active. When the individual leans backward, the anterior musculature becomes active. Thus ideal alignment aides the balanced participation of musculature.
(From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
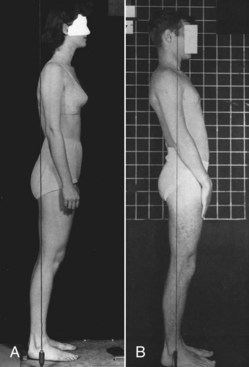
Figure 1-10 Two variations in the relationship of the trunk to the line of gravity. A, In the forward-leaning individual with the line of gravity posterior to the trunk, the back extensor muscles are active. B, In the backward-leaning individual with the line of gravity anterior to the trunk, the abdominal muscles are active.
(From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
Tissue Adaptations of the Nervous System
Obviously, the contributions of the nervous system to movement are essential and have been the subject of many books, but what is only recently becoming widely accepted is that motor control plays a key role in musculoskeletal pain. Currently, there are two general theories about changes in movement in patients with musculoskeletal pain. One theory is that pain causes the change in movement patterns and alters motor control.46 The other theory is that changes in movement patterns cause the problems that result in pain.29 Certainly an acute and intense onset of pain can affect the patient’s alignment and movement patterns. But the major question is, “What precipitated the pain episode?” As suggested by the model, the repeated movements and sustained postures of daily activities induce the changes in tissues and movement patterns that cause the pain problems. Therefore the pathological changes are secondary to the altered movement pattern and motor control and not primary. Both concepts require that treatment emphasize correction of the movement patterns and the altered motor control. If altered movement patterns cause the problem, then guidelines for prevention are possible. If the pain causes the problem, then the precipitating factors may not be easy to identify. Clinical experience with correcting movement patterns and alleviating symptoms supports the belief that the altered movement patterns are the key factor in causing pain and that correcting the movements and the contributing factors is the most effective long-term treatment.
A prevailing characteristic of the human body is to reduce the degrees of freedom when establishing a movement pattern, thereby achieving a degree of efficiency and minimizing energy expenditure. Movement patterns become established as they are repeated, and the pattern is reinforced by changes in both the nervous and muscular systems. Different stages are involved in motor learning.47 The initial stage is motor performance, in which conscious effort is required to learn a new skill. With practice, the skill no longer requires conscious effort but becomes relatively automatic, performed efficiently and with skill. The final state is termed motor learning. Every activity that an individual performs involves this process. A classic example is learning to ride a bicycle: You learn to pedal to propel the bicycle, but at the same time, you learn how to balance and keep your center of gravity appropriately within the base of support provided by the bicycle. Mainly subconsciously, you are learning the relationship between speed and body adjustments to manage the line of gravity. After practice with conscious effort to master the requirements for balance and pedaling, riding the bike then becomes automatic, and even after many years without cycling, the skill is quickly restored. Another aspect to consider is that even though the pedaling seems simple and straightforward, not everyone uses the same strategy. Studies have shown variations in muscle patterns during cycling, depending on skill and other activity.48-50 One can also suspect that there are variations in how much hip extensor muscle versus knee extensor muscle activity is used, whether one lower extremity exerts more force than the other. If there are toe clips, how much force used by the hip and knee flexors versus the extensors can vary. Similarly, even though many studies of normal gait have provided the characteristic movement of the center of gravity, the joint angles, and the muscle recruitment patterns, gait is still highly individual, which is how we are able to recognize someone at a distance by the gait pattern, long before we can see the face.
When considering the factors contributing to musculoskeletal pain problems, the patterns of recruitment and derecruitment are primary. The belief is that the patterns are established by the requirement of the activity, personal characteristics, and intensity of use.
Case example
The patient is a 32-year-old right-handed construction worker with pain in the left scapular area between the vertebral border of the scapula and the thoracic spine (Figure 1-11, A). During left shoulder flexion and the return from flexion, the patient had marked winging and anterior tilt of the scapula, which was markedly abducted and internally rotated in the rest position (Figure 1-11, B and C). Both manual and electrophysiological testing did not indicate any muscle weakness or denervation of the serratus anterior muscle. The abducted position of the scapula is also not consistent with serratus anterior muscle weakness. Typically, with serratus anterior muscle weakness, the scapular rest position is adduction.
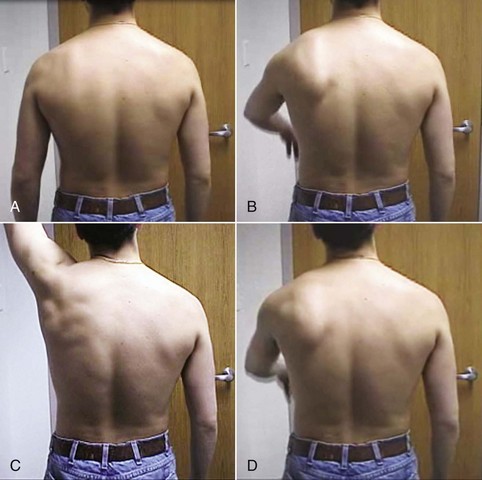
Figure 1-11 A right-handed construction worker with pain for 2 years in the left scapular area. All diagnostic studies were negative. A, Abduction, anterior tilt, and internal rotation of the left scapula. B, Shoulder flexion causes almost immediate scapular anterior tilt, abduction, and internal rotation, causing the scapula to appear to wing. C, The patient has almost full range of motion (ROM) of shoulder flexion without scapular winging, which is inconsistent with severe weakness of the serratus anterior muscle. D, During the return from shoulder flexion, the scapula abducts, tilts anteriorly and internally rotates, the same faults evident during flexion.
Key finding
Careful observation of the shoulder motion indicated that the patient was moving the scapula and humerus in a 1:1 ratio both during active shoulder flexion and the return from flexion.
Treatment
The patient was instructed to face the wall with his elbow flexed and the little finger side of his hand against the wall and to easily slide his hand up the wall to flex his shoulder. On the return, the therapist lightly supported the inferior angle of the scapula and instructed the patient to let his elbow drop to return to the starting position. The purpose of the instruction was to have the patient relax the scapulohumeral muscles more rapidly than he was relaxing the serratus anterior muscle. After approximately 20 repetitions, the patient was able to let his shoulder extend without scapular winging or tilt. The explanation of this motor control–induced problem is that as a right-handed laborer, the primary activity of his left hand was to hold things or objects in place for hammering or sawing. Thus he trained his left upper extremity musculature to maintain a constant long duration co-contraction of the glenohumeral musculature. Finally, his pattern was to lower the arm by allowing the scapula to downwardly rotate, while still maintaining the same glenohumeral alignment, rather than changing the glenohumeral joint position. In other words, he elongated the serratus anterior muscle more rapidly than the scapulohumeral muscles. The pattern became established and was generalized to all other activities involving his left shoulder motion. Undoubtedly, the fact that he was right handed and did not perform a wide repertoire of movements or skills with his left arm contributed to the problem. After training him to change the recruitment and derecruitment patterns, he was able to change the movement patterns affecting his scapula and eliminate his pain problem. When the patient returned for the third time 2 months later, his scapula was no longer winging (Figure 1-12).
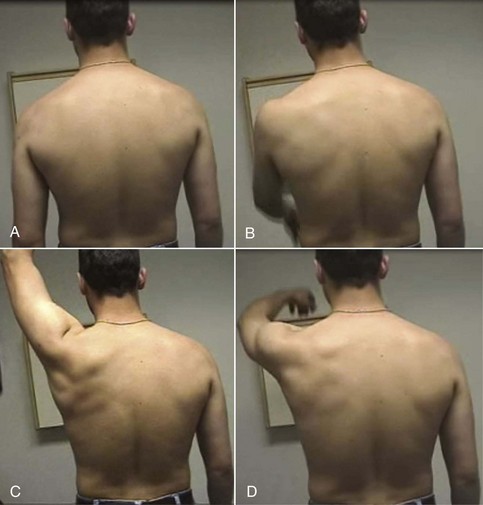
Figure 1-12 A, Two months later, third physical therapy visit. The scapula alignment is still impaired, but the vertebral border is not as prominent and the humerus is not as abducted or internally rotated, suggesting improvement in the scapular alignment. B, During shoulder flexion, the scapula no longer tilts anterior or internally rotates, thus not appearing to wing. C, Shoulder flexion range of motion is increased. D, During the return from shoulder flexion, the scapula is not tilting anteriorly or rotating internally, thus not appearing to wing.
The challenge for the therapist is to identify the movement strategy and if the pattern is painful or inconsistent with the kinesiology of the movement, then to retrain the patient. A prevailing belief is that as long as the body is able to move in a certain way, the movement is acceptable and not necessarily potentially harmful. Such a belief is no more accurate than a belief that an individual can eat any type of food and without limit. Similarly, those of us involved in exercise, learn with experience that developing the appropriate program for an individual is not easy if you are aware of all the things that need to be considered.
Case example
A patient has knee pain related to a learned pattern of lower extremity movement. This example of a learned motor pattern that can affect the knee and foot is one of allowing the knees to come together (adduct and medially rotate) when going from sit-to-stand and reverse (Figure 1-13, A). This type of pattern was considered “lady-like” and used by those with proper training. Also, women were taught to sit and hold their knees together. When performed frequently and for long periods of time, the result was decreased performance of the hip abductor and lateral rotator muscles. Also, the hip adductors became over recruited.

Figure 1-13 Learned movement pattern and correction with instruction. A, During sit-to-stand, the patient demonstrates her learned pattern of putting her knees together by hip adduction and internal rotation, as well as using her hands as an additional support. B, Able to come to standing while keeping her hips and knees in correct alignment and without support from her hands.
Diagnosis
Tibiofemoral rotation: motor pattern incoordination with force production deficit. The consequence at the knee was tibiofemoral rotation and often the foot became pronated.
Treatment
The patient was instructed to practice sit-to-stand and reverse with knees apart (Figure 1-13, B), as well as sidelying hip lateral rotation from hip and knee in a flexed position and hip abduction. Side stepping was also recommended.
Learned gait patterns that are characterized by decreased push-off or knee hyperextension are also examples of normal adaptations using motor control mechanisms that result in imprecise movements and are reinforced by muscular and supporting tissue adaptations. In these instances, pain does not have to initiate the motor control adaptation. but the motor control adaptation can lead to the development of pain.
In summary, motor control can be considered a major contributing factor to the development of movement patterns that cause musculoskeletal pain syndromes. The critical factor is not what you do as much as how you do it. Many of us can downhill snow ski, but only a few of us will ever reach a competitive level, much less the Olympic level. The way the nervous system and the responding musculoskeletal system control the performance is the issue, not the participation in skiing. The same mechanisms apply to movement patterns and musculoskeletal pain conditions.
As depicted in the model (see Figure 1-3), these patterns start as motor performance, which is the first stage in motor learning. With continued practice or repetitions, performance becomes motor learning and thus the pattern is considered relatively permanent. At that point, cognitive effort and retraining is necessary to alter the pattern. The therapist needs to recognize that the patient’s reference for movement is the continuation of basic patterns that have been used for years. There is no internal sensing system that tells us when performance is optimal (we do what is familiar and not what is right). If a patient’s habitual posture is one of a thoracic kyphosis with a forward head, correcting that alignment requires recognition of the fault and conscious practice of the correct alignment. Because the patient does not know what is right but only what is familiar, correction is difficult. In addition, the patient needs to be instructed in the appropriate strategy for correcting the alignment fault and movement pattern. Most individuals correct a kyphosis by increasing lumbar extension. They should decrease the thoracic kyphosis by increasing the use of the thoracic back extensor muscles. The primary indicator of problems with performance is the development of pain. Recognition of the role of motor control and musculoskeletal adaptations in mechanical pain strongly suggests that passive treatment can only be viewed as temporary and palliative, rather than a means of (1) alleviating the contributing factors, (2) delaying recurrence, and (3) slowing the progression of the condition. The patient should be informed that changing motor patterns is at least a 4- to 6-week process, depending on the frequency and constancy of the correction. Inter-estingly, that is about the same time required for muscular hypertrophy. The changes in both systems help achieve and reinforce the eventual correction.
Tissue Adaptations of the Muscular System
The adaptations of muscle are changes in (1) length, both increased and decreased; (2) tension development capacity, hypertrophy, and atrophy; and (3) stiffness, the resistance to passive elongation. Traditionally, physical therapy and athletic communities have been concerned about the development of short muscles that need to be stretched. The manifestations of what is often attributed to muscle shortness is twofold. One example is the decreased ROM of a joint (e.g., lack of 80 degrees of hip flexion with the knee extended during the straight-leg raise). The decreased hip flexion is attributed to shortness of the hamstring muscles. The second manifestation is flexion of the lumbar spine resulting from posterior pelvic tilt when the hamstrings are stretched, either during the straight-leg raise or during knee extension when sitting (Figure 1-14). The effect on the lumbar spine is believed to be caused by the lack of sufficient hamstring muscle length. The standard treatment is to stretch the hamstring muscles to eliminate the effect on the pelvis and lumbar spine. Yet, shortness of the hamstring muscles is not a sufficient explanation for the pelvic tilt and the lumbar flexion. Why is the explanation not sufficient, and what are the implications for treatment? If the complete explanation was that the hamstrings are too short, then how are other findings explained? For example, in other patients, when their hamstring muscles are stretched, the pelvis does not tilt and the lumbar spine does not flex but rather the knee does not fully extend. An explanation lies in the relative stiffness of the tissues affecting the lumbar spine as compared to the stiffness of the hamstring muscles.
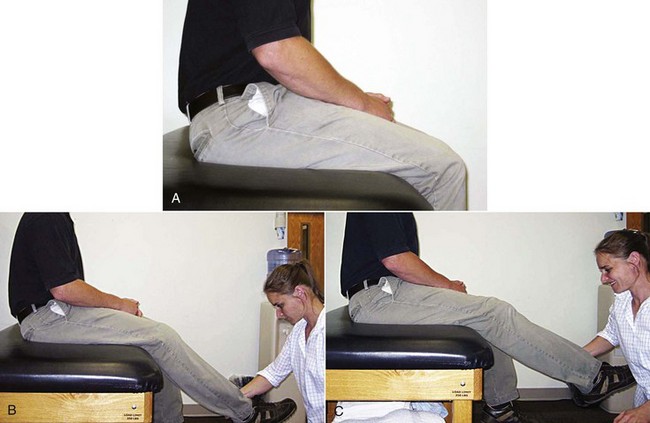
Figure 1-14 A, Patient’s hip joint angle is almost 90 degrees with his knees flexed. B, With passive knee extension to only 45 degrees, his pelvis tilts posteriorly, and his lumbar spine flexes. The position of the pelvis and lumbar spine indicates that the hamstring muscles are stiffer than the supporting tissues of the lumbar spine. The alignment change occurred before the end of the excursion of the hamstring muscles. C, When the hip joint angle is maintained at 90 degrees, the knee cannot be fully extended. The hamstring muscles are short.
Relative Stiffness/Flexibility
Based on clinical testing of the muscle lengths of many patients over the past 50 years, the number of individuals with actual muscle shortness is far fewer than the number of individuals who have a “relative stiffness or flexibility” problem. Muscle stiffness is defined as the change in tension per unit change in length.51 Stiffness refers to the resistance present during the passive elongation of muscle and connective tissue. The stiffness is a normal property of muscle and is the passive tension of a muscle when stretched. The combination of active and passive tension is also referred to as stiffness. But, in the current discussion and incumbent in this theory, the term stiffness is restricted to the passive property of muscle. When a muscle is being elongated and there is movement at the proximal attachment of the muscle, the best explanation is that the tissues stabilizing the joint are not stiff enough relative to the stiffness of the muscle being stretched. Consider the following scenario. Hamstring length is assessed with the patient sitting in a chair with the hip flexed to 80 degree and the knee extended (Figure 1-14). First, when the therapist passively extends the knee, the resistance that is felt is the passive stiffness of the hamstring muscles. If, as the knee is passively extended from 90 degrees of flexion to 45 degrees, the pelvis posteriorly tilts and the lumbar spine flexes, this motion is not an indication of hamstring muscle length. This behavior is an indication of the relative flexibility of the lumbar spine versus the hamstring muscles. If the back extensor muscles attaching to the pelvis and spine are as stiff or stiffer than the hamstring muscles, the pelvis would not tilt and the knee could not be extended (see Figure 1-14, C). The range of knee extension would be determined by the length of the hamstrings. Often, in the individual whose pelvis posteriorly tilts and the lumbar spine flexes as the knee is being passively extended, if the pelvis and the lumbar spine are stabilized at 80 degrees of hip flexion, the knee can be fully extended to 0 degrees of flexion (see Figure 1-15). The concept is that the hamstrings and the tissues (muscles and ligaments) of the lumbar spine are springs in series. When the passive tension of the spring being stretched (hamstrings) is greater than the passive tension of the spring in series (lumbar spine tissues), there will be motion at the intervening joint (Figure 1-16). Reasonably, the earlier the movement at this joint the greater the indication of the lack of “stiffness or stability” of the joint. In other words, if the hamstrings are passively stretched and the knee is within 20 degrees of full extension before the pelvis tilts and the lumbar spine flexes, the spine is fairly stiff or stable. If the pelvis begins to tilt posteriorly and the lumbar spine flexes after only 20 degrees of passive knee extension, the spine is very flexible. What the therapist should note is the resistance that is associated with the passive knee extension, as well as the timing of the associated movement. If the patient is actively contracting the hip flexor muscles preventing posterior pelvic tilt posteriorly the motion of the pelvis and lumbar spine would be prevented.

Figure 1-15 A, The patient’s pelvis is tilted posteriorly, and his lumbar spine is flexed when his knee is passively fully extended. The position of the pelvis and spine can be the result of relative flexibility, which indicates that the hamstrings are stiffer than the supporting tissues of the lumbar spine but not that the hamstring muscles are short. B, The patient’s hip joint angle is 90 degrees, and no motion of the pelvis or lumbar spine occurs when the knee is fully extended passively. The hamstring muscles would not be considered short.
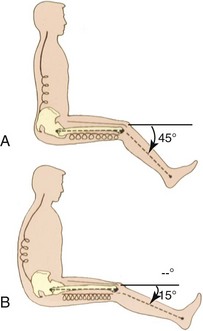
Figure 1-16 Diagrammatic illustration of the effect of relative stiffness of the back extensor muscles and the hamstring muscles. A, The back extensor muscles are stiffer than the hamstring muscles, so the knee does not extend. B, The back extensor muscles are less stiff than the hamstrings, therefore the pelvis posteriorly tilts and the lumbar spine flexes as the knee extends.
The mechanism of the relative stiffness/flexibility problem is multifold. For example, as the intervertebral discs lose their height, the attached ligaments become slack rather than remain taut, which changes the passive tension about the joint. Another factor is the passive tension (stiffness) of the hamstring musculotendinous unit versus the passive tension of the back extensor musculotendinous unit. A major source of the passive tension (stiffness) in muscle fibers is an intracellular contractile protein called titin.52,53 Titin is the largest connective tissue protein in the body and provides the passive tension for both striated and cardiac muscle (Figure 1-17). Titin attaches the myosin filament to the Z-line of the sarcomere and there are 6 titin proteins for every myosin filament. Therefore, muscle hypertrophy that increases the number of sarcomeres in parallel and consequently the amount of myosin will also increase the passive tension or stiffness of the muscle. A study examining the passive stiffness of the elbow flexors demonstrated a very high correlation between muscle volume and passive stiffness54 (Figure 1-18).
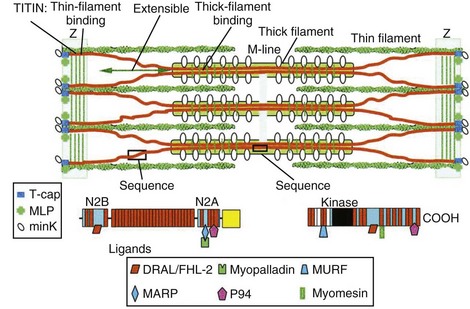
Figure 1-17 Schematic of the sarcomere illustrating the attachments of titin.
(From Granzier HL, Labeit S: The giant protein titin: a major player in myocardial mechanics, signaling, and disease, Circ Res 94:284-295, 2004.)
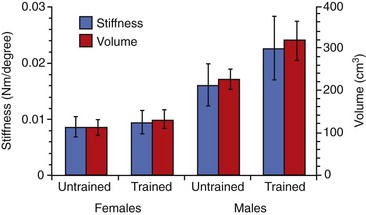
Figure 1-18 Relationship between passive stiffness and muscle volume. There is a high correlation between muscle size and passive stiffness, therefore the greater the hypertrophy of a muscle the greater the resistance to passive elongation.
(From Chleboun GS, Howell JN Conatser RR, et al: The relationship between elbow flexor volume and angular stiffness at the elbow, Clin Biomech 12(6):383-392, 1997.)
A reasonable implication is that one of the important roles of muscle hypertrophy is the effect on passive tension. Realizing that an intrinsic property of the human body is the minimization of energy expenditure when inactive or even when active, the role of passive tension becomes particularly important. Passive tension is a primary contributing factor to alignment, often stability, and even the timing and effectiveness of the mechanical event connected with muscle contraction. Therefore the therapist should note the detected amount of tension as the muscle is passively stretched. This information is indicative of the tension across a joint and can be a source of the stabilizing force across a joint, the compression of the joint, and the resistance to the antagonistic muscle when it contracts. For example, if the patient is sitting and there is marked resistance as the knee is passively extended, then the quadriceps are working against that resistance during active knee extension. Also, if there is a lot of resistance from the hamstrings and that is combined with the tension generated by the quadriceps, then the compressive forces into the joint are going to be greater than if the hamstrings are not stiff. The passive tension provided by muscle plays an important role in joint stability, alignment, and in some situations contributes to pain. Thus an individual’s postural alignment is indicative of the passive tension and the length of trunk and opposing muscles. In Figure 1-19, A, the preferred, most energy-efficient posture is a swayback alignment with a thoracic kyphosis and forward shoulders. The patient also appears to be in a slight anterior pelvic tilt. Clearly, the rectus abdominis is stiffer than the thoracic back extensors as indicated by the kyphosis. The swayback alignment means that the upper body is behind the line of gravity so that the rectus abdominis is the antigravity lumbar muscle and thus is active. By swaying back, the back extensor muscles are not active and therefore not contributing to the anterior pelvic tilt. The anterior pelvic tilt also suggests that the passive tension from the hip flexors is greater than the tension generated by the rectus abdominis and external oblique abdominal muscles to posterior tilting of the pelvis (see Figure 1-19, A). When the subject corrects her alignment, the strong effort required to lift her chest and decrease the thoracic kyphosis is evident (see Figure 1-19, B). This corrected alignment is not energy efficient because of the strong contraction required by the thoracic back extensors, particularly against the stiffness of the rectus abdominis muscle. What an amazing design is incorporated in a system that rewards you when you are at rest for the work you do actively. In other words, performing appropriate abdominal exercises not only “strengthens” the abdominal muscles so that they generate increased active tension, but these muscles also provide control and stability of the trunk when not contracting because of the passive tension or stiffness. But, as illustrated by this example, the stiffness can also contribute to alignment impairments. Consider the alignment of the pelvis. If the hip flexor muscles (e.g., rectus femoris and iliacus muscles) are hypertrophied, the passive tension will pull the pelvis into an anterior tilt (Figure 1-20). To achieve optimal alignment, the rectus abdominis and the external oblique muscles must have a similar, if not a greater, degree of passive tension to maintain the neutral or optimal alignment of pelvic tilt. This situation becomes more complex when considering the contribution of the lumbar back extensor muscles that also anterior tilt the pelvis anteriorly. If the pelvis is tilted anteriorly, the passive tension at the necessary length of the abdominal muscles does not offset the pull of the rectus femoris, the other hip flexors, and the back extensors. But, clearly, such muscle dynamics are not the only possibilities, and further examples are useful.
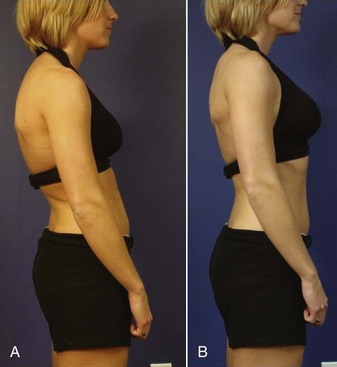
Figure 1-19 Implications of standing alignment and passive stiffness. A, Natural standing alignment with minimum energy expenditure. The swayed back trunk with the thoracic kyphosis indicates the thoracic back extensor muscles are not as stiff as the rectus abdominis muscle. The swayback minimizes the activity of the lumbar back extensor muscles, thereby not contributing to anterior tilt of the pelvis that is associated with action of these muscles. The anterior pelvic tilt indicates that the hip flexors are stiffer than the abdominal muscles that do not generate counterbalancing passive tension at the correct length to maintain ideal pelvic alignment. B, Active contraction of thoracic back extensor muscles improves her thoracic alignment. The emphasis of her treatment program is to improve the participation of the external oblique abdominal muscle more than the rectus abdominis to achieve correct pelvic tilt without increasing the thoracic kyphosis. The permanent correction requires enough change in the passive tension and length of the abdominal and thoracic back extensor muscles to “hold” the correct alignment passively and not actively.
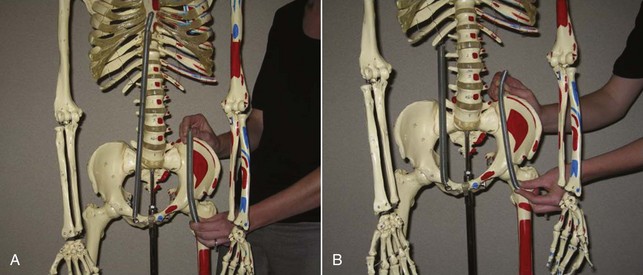
Figure 1-20 Springs depicting the passive tension of the abdominal and hip flexor muscles. The passive tension (stiffness) of muscles exerts an almost constant pull on its attachments. A, When the least stiff spring is the abdominal muscles, the stiffer spring of the hip flexors will pull the pelvis into an anterior pelvic tilt. B, When abdominal muscles are stiffer than the hip flexor muscles, the pelvis will be maintained in the correct alignment.
The alignment of a thoracic kyphosis can develop from a variety of factors. In some cases, the abdominal muscle strength (and associated passive tension) can be contributing to the kyphosis while in other cases, the abdominal muscles are weak because of the kyphosis.
An individual participates in fitness activities, such as cycling, or has performed numerous sit-up exercises, the abdominals will be stiff and/or short (see Figure 1-19). The exercise or activity has resulted in abdominal muscles that are stiffer than the thoracic back extensors. Thus the abdominal muscles are contributing to the kyphosis. Therefore the back extensor muscles may be pulled into the elongated position and have to work against the passive tension of the abdominals. Thus to correct the alignment, the thoracic back extensor muscles in this individual have to become stronger than the abdominals and have to generate enough tension passively at a shorter length than the muscle currently demonstrates.
A variation occurs when the trunk is swayed back so that the abdominals are the antigravity muscle of the trunk. This is a frequent posture of men who have performed many sit-up exercises (Figure 1-21). This individual is swayed back enough that his abdominal muscles are holding the trunk against gravity. The demands on his abdominal muscles are exaggerated because his shoulders are broad and in line with his trunk. The hypertrophy of the abdominal muscles and the associated passive stiffness means that the thoracic back extensor muscles have to generate more tension to correct the kyphosis than if the abdominal muscles were not stiff. In this swayback position, the back extensor muscles are not required to support his trunk and, thus, are usually atrophied. As evident from his posterior pelvic tilt and flat lumbar spine, neither the back extensors, nor the hip flexors are generating sufficient passive tension to counterbalance the tension of the abdominal muscles and correct the alignment of the thoracic and lumbar spine as well as the pelvis and hip joint. This passive tension of a muscle is NOT “inhibited” by any type of nervous system mechanism. This passive tension is a function of the intrinsic connective tissue proteins of muscle. Also noteworthy is that in these situations the antagonist to the thoracic back extension, the rectus abdominis muscle, becomes a source of resistance. This situation is one in which the body is acting as a resistance machine. The stiffness of the abdominal muscles is resistance to the thoracic back extensor muscles. Correction of this situation requires that the patient stands with his back against the wall to correct the sway back alignment. He should try to actively extend his back as he flexes his shoulders. During the day, he should frequently lean forward while trying to keep his back straight to increase the use of his back extensor muscles and the gluteus maximus muscles. He has to be careful when lifting weights, because he will automatically sway back and use his abdominal muscles to stabilize his trunk.
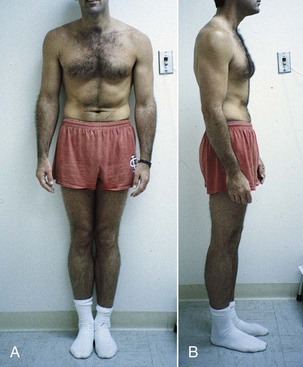
Figure 1-21 Hypertrophy of the abdominal muscles maintained by being the antigravity muscles of the trunk. A, Anterior view indicating the muscle definition of the abdominal muscles. B, The side view demonstrating that the head and shoulders are swayed back so that the line of gravity is anterior to the trunk. The patient also worked with his arms in front of him causing even more posterior sway of the trunk.
A third situation is one in which the individual has allowed the trunk to remain flexed out of habit, and the thoracic back extensors have lengthened and do not have the passive tension at the right length to keep the thoracic spine correctly aligned (Figure 1-22). In this individual, the abdominal muscles are weak without a great deal of passive tension (stiffness). Correction of the kyphosis requires frequent and sustained contraction of the thoracic extensor muscles until the length and the passive tension of the muscles is sufficient to maintain the correct alignment of the thoracic spine.

Figure 1-22 Thoracic kyphosis associated with excessive length of the thoracic paraspinal muscles and with laxity of the abdominal muscles.
A high degree of muscular passive tension can also influence the effectiveness of an active muscle force. Consider the situation of the abdominal muscles in two individuals with very different muscle conditions. In one individual, the abdominal muscles, attaching to the ribcage and the pelvis, are notably hypertrophied so that the individual has a flat abdomen and obvious muscle definition (see Figure 1-21). These abdominal muscles will be exerting tension on the pelvis and the rib cage. The second individual has notable distension of the abdomen and an obvious lack of muscle definition (Figure 1-23). If the first individual elicits a minimal contraction of his abdominal muscles, there is immediate delivery of tension to the rib cage and pelvis and the tension will be effective because of the hypertrophy. In the second individual with the distended abdomen and poor muscle definition, contraction of the abdominal muscles requires a great effort and the development of tension would be relatively slow because of the slack that has to be taken up to have an effect on the rib cage and pelvis. The eventual delivery of tension would be relatively small because of the lack of sarcomeres in parallel in the muscle cells. The timing of electromyographic (EMG) activity might be similar in both individuals, but the rate and the effectiveness of force development would be very different.

Figure 1-23 Prominence of abdomen consistent with diminished abdominal muscle stiffness and a diastasis of the linea alba above the umbilicus. Contraction of abdominal muscles with this condition will have a minimal effect on the alignment of the pelvis and rib cage.
Assessment of the contributing factors to the patient’s condition is essential to develop an effective treatment program. Consider the variations in the three individuals described as having different contributing factors to their thoracic kyphosis (see Figures 1-19, 1-21, and 1-22). These individuals may consider abdominal muscle exercises as an important part of their fitness program, but in some cases, such exercises would not be an impediment, but in other cases, they would be. In the first example (see Figure 1-19), the patient should perform exercises that emphasize the external oblique muscles, particularly the action of a posterior pelvic tilt. The patient should flatten the back against a wall and then try to extend the thoracic spine and try to hold the position for as long as possible. The forward shoulder posture helped minimize the demands on her abdominals to hold her trunk against gravity. Using hand weights, performing shoulder flexion to 90 degrees in the corrected position would also hypertrophy the thoracic back extensor muscles, helping to induce the changes in passive stiffness that is needed to achieve the change in the alignment. When performing shoulder flexion, she has to posteriorly tilt and externally rotate her scapula to correct the alignment. Contraction of the serratus anterior muscle and the trapezius to maintain the scapular position will increase the passive stiffness of the muscle, which is necessary to correct scapular and shoulder girdle position.
In the second individual (see Figure 1-21) with the swayback posture with the abdominal muscles functioning as an antigravity muscle, correcting the swayback is extremely important. As mentioned, this individual should perform exercises that emphasize thoracic and lumbar back extensor muscle activity and even hip flexion exercises to correct the posterior pelvic tilt. The individual should frequently stand with the back against the wall and practice aligning the shoulders and the hips. This individual could also practice external oblique abdominal exercises but should avoid any type of trunk curls. The abdominal muscles would be an even greater source of resistance to the thoracic back extensors than in the first individual. Both of these individuals should practice standing straight and taking deep breaths, particularly after exercising such as riding a bike. Lateral thoracic and not lumbar side flexion would also be beneficial to stretch the abdominal muscles. The final individual (see Figure 1-22) with the assumed thoracic kyphosis needs to practice the correct thoracic alignment but does not have the resistance of the abdominal muscles. Abdominal exercises for the external oblique abdominal muscles in particular could be performed. She should not do any trunk-curls, which would add to the kyphosis, and because she is probably at risk for osteopenia. The program should emphasize frequent performance rather than a lot of repetitions at one time. If the individual has a lumbar lordosis, then abdominal muscle exercises, again particularly for the external oblique muscles, would be important. These exercises emphasize posterior pelvic tilt and not thoracic flexion movements. The patient has to try to elongate her trunk while performing exercises. Two exercises that are useful for elongating the trunk are shown in Figures 1-24 and 1-25.

Figure 1-24 The modified quadruped position can be used to decrease the thoracic kyphosis and help elongate the trunk. The patient is instructed to allow the upper back to relax, letting the chest drop toward the table. The patient can then rock backward, which provides a slight stretch of the trunk.

Figure 1-25 A, Patient sitting slumped with a thoracic kyphosis. B, Pushing up in the chair to elongate the trunk. She is not lifting her buttocks off of the chair, but she is just elongating the trunk by pushing into the seat of the chair and locking her elbows. The patient then tries to contract all of her trunk muscles to maintain the trunk alignment, and then she lifts her hands off the seat of the chair. C, Side view of the trunk elongation exercise.
These may be subtle variations, but such detail adds to the effectiveness and the efficiency of the treatment. Obviously, correction of the thoracic kyphosis requires contraction of the thoracic back extensor muscles sufficiently to achieve the optimal spinal alignment. Then the back extensor muscles have to hypertrophy enough that they can maintain the thoracic spine in the correct alignment with passive and not active tension.
Too often such a patient is given back extension exercises without ensuring that the thoracic spine is extending and instead the patient is extending the lumbar spine. Instead, the most effective exercise would be for the patient to stand with the back against the wall and lift the chest while trying to perform a posterior pelvic tilt with the external oblique abdominal muscles and then perform bilateral shoulder flexion. Once the patient has the correct thoracic alignment, lifting light weights while standing in the optimal alignment can be added to the program. The purpose is to hypertrophy the thoracic back extensors with the goal of the musculature developing enough passive stiffness at the right length so that the posture is maintained without active effort. All three individuals should also do the quadruped exercise that allows the thoracic spine to flatten. In the same position, performing shoulder flexion while maintaining the corrected alignment contracts the thoracic back extensor muscles at the correct length.
In ideal alignment, there is optimal muscle participation that is not present when alignment is impaired as in the previous examples (see Figure 1-9). If an individual has ideal alignment in the standing position, when leaning forward slightly, the back extensors are activated because they are the antigravity muscle. When this individual leans backward slightly, the abdominal muscles are activated because they are the antigravity muscles. This type of oscillation in muscle participation contributes to balanced use of both anterior and posterior trunk muscles rather than almost constant use of one group of muscles.
In summary, muscle stiffness is an extremely valuable property of muscle that enables the body to be supported with minimal energy expenditure. The foregoing examples demonstrated the importance of optimal passive tension of muscles attaching to either side of a joint. Good alignment is indicative of balanced passive tension of muscles attaching to a joint or skeletal segment, such as the thorax or pelvis. The passive tension, which also has a high correlation to active tension, is the key to the alignment and stabilizing properties of the joint. As in all things, stiffness can become excessive or insufficient. The relative stiffness/flexibility properties are often the contributing factor to (1) alignment impairments, (2) one joint moving more readily than an adjoining joint, and (3) inadequate stabilization or inappropriate movement during the passive elongation of a muscle.
Case example
A young woman with right thoracic pain played volleyball and soccer. She illustrated another variation of the role of relative stiffness. For both soccer and volleyball, she had developed a great deal of trunk rotation to the right and very limited rotation to the left. As a right-handed individual, she used her right hand for spiking, which she performed frequently causing hypertrophy of her right pectoral muscles.
Key finding
In the supine position, when her right shoulder was passively or actively flexed, the right side of her ribcage elevated. When her left shoulder was passively or actively flexed, the left side of her ribcage did not elevate. The explanation is that the abdominal muscles attaching to the right side of her ribcage were elongated, allowing the excessive trunk rotation, therefore the passive tension from the pectoral muscles that are stretched with shoulder flexion elevated her ribcage because the passive tension from the abdominals was not sufficient.
Diagnosis
Thoracic rotation motor pattern incoordination. The asymmetrical effect on the ribcage was contributing to the rotation of the thoracic spine and her thoracic pain.
These examples also indicate how excessive or asymmetrical passive tension from muscles, such as the abdominals, can contribute to pain problems. Another example is how passive tension of the abdominal muscles can contribute to neck pain and limited ROM (see Chapter 3). Because the scalene muscles attach to the ribcage, if the rectus abdominis and the external oblique muscles are stiff and/or short, they pull down on the ribcage and the attachment of the scaleni muscles. Passively elevating of the ribcage in these patients, enables them to increase the rotation of the cervical spine, as well as alleviate their neck pain (Figure 1-26). One of the methods used to assess the abdominal muscle extensibility is to measure the change in the circumference of the ribcage between maximum exhalation to maximum inhalation. The ideal change is 3 in or 7 cm. As the individual ages, the excursion decreases, but a change of 2 in or less in a young individual is not optimal. The same assessment of the change in the diameter of the ribcage is made during bilateral shoulder flexion, which stretches the abdominals. If the excursion is markedly limited, again the abdominal muscles are considered too short or stiff. If the infrasternal angle is less than 70 degrees, this could be another indicator of short or excessively stiff abdominals, particularly the external oblique muscles (Figure 1-27).

Figure 1-26 Stiffness of the scaleni muscles limiting rotation of head and cervical spine. Patient with severe headaches and neck pain with short and stiff abdominal muscles. A, Maximum head and neck rotation. B, Increased rotation of head and neck when arms are supported and the rib cage is passively elevated.
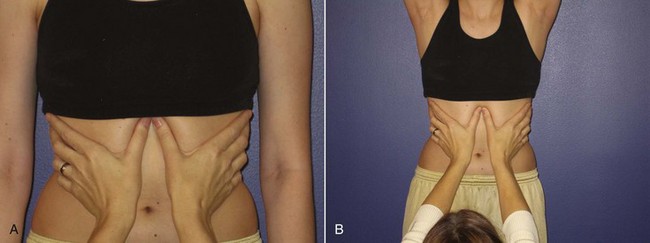
Figure 1-27 Assessing the infrasternal angle as an indication of abdominal muscle resting length. A, Narrow infrasternal angle associated with stiffness and/or shortness of the external oblique abdominal muscles. B, If the external oblique abdominal muscles are short, the change in diameter of the rib cage during maximum inhalation is less than 2 inches.
Muscle Length Adaptations
Increased length
Another muscle adaptation that clinically seems to be more common than loss of muscle length is increased resting muscle length. Possibly, small changes in muscle length are changes in passive resting tension, while greater increases in muscle length are associated with addition of sarcomeres in series in the muscle fibers. Although evidence for increased sarcomeres in series in adult human muscle is very limited,55 such adaptations have been demonstrated in animals as the result of both passive immobilization56 (Table 1-1 and Figure 1-28) and active use in a lengthened position.57 A recent review paper suggests that short-term muscle lengthening is associated with changes in sensation, the subject’s response to the discomfort of muscle stretching.51 The effects from long-term muscle lengthening have not been studied,51 but based on clinical observations, some muscle behaviors are best explained by such muscle length adaptations. The implications are important for both resting alignment and active motions. For example, individuals whose shoulders are depressed not only are increasing the stress on their neck, but they are also changing the resting alignment of their shoulder at the sternoclavicular joint and at the glenohumeral joint. If the shoulders are very depressed, there has to be an associated change in the length of the upper trapezius and the serratus anterior muscles. This change in length of the muscles not only affects the resting alignment of the shoulders but also affects the characteristics of the movement of the shoulder joint because of the shift in the length-tension curve to the right. Thus the development of appropriate tension to upwardly rotate and elevate the scapula will not be possible if the underlying condition is an increase in the number of sarcomeres in series.
TABLE 1-1 Muscle Belly Length, Sarcomere Number, and Sarcomere Length Measurements of Young and Adult Muscles Immobilized in the Lengthened and Shortened Positions*

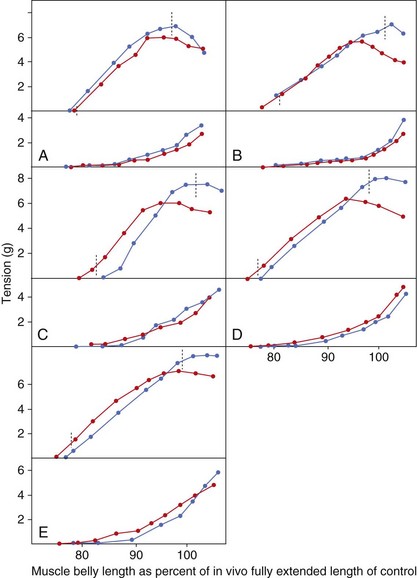
Figure 1-28 Active and passive length-tension curves of mice muscles that have been immobilized in a lengthened position for 3 weeks and compared to control muscles. Note the curves of the lengthened muscles are shifted to the right. Red line, Control muscle; blue line, experimental-lengthened muscle.
(From Williams PE, Goldspink G: Changes in sarcomere length and physiological properties in immobilized muscles, J Anat 127:459-468, 1978.)
Decreased length
As shown by experiments in animals,56 the development of true muscle shortness is associated with loss of sarcomeres in series in muscle fibers. Animal studies have shown that muscles maintained in a shortened position or at a short resting length for as little as 3 weeks will lose sarcomeres in series and prevent the full excursion of the joint to which it is attached56 (Figure 1-29). A typical example is the lack of 80 degrees of hip flexion with the knee extended that is considered an indication of “short” hamstrings. There is a lack of clarity in clinical practice about the various mechanisms involved in muscle shortness and tissues affected by stretch or the need to stretch. Possibly because “muscle stretching” is such a long-standing part of practice that, in spite of the efforts of various investigators to clarify the process,58,59 confusion exists about methods to be used. A reasonable way to consider the appropriate intervention for variations in hamstring length is as follows. For example, if the decreased ROM of hip flexion with the knee extended is only 10 to 15 degrees and can be regained by stretching for a few minutes, the alteration can best be explained by the creep or viscoelastic properties of muscle. Repetitions of the stretch produce a temporary change in the resting length of the muscle, conveying the impression that the muscle is “longer” or “stretched.” But this is a temporary state, and the muscle will return to its original resting length over a period of minutes, partially depending upon the duration of the stretching. In contrast, if the hamstring muscles are limiting the motion of the joint by 30 to 40 degrees, then the most likely explanation is that the muscle fibers have lost sarcomeres in series and the treatment has to be stretching of long duration (for example, 30 minutes or more, several times a day for many days) and as sustained as possible. Stretching should not be forceful because a reasonable explanation for this condition is that the muscle has lost sarcomeres in series and that requires protein synthesis and not just a change in the conformation of the proteins in the muscle cells.
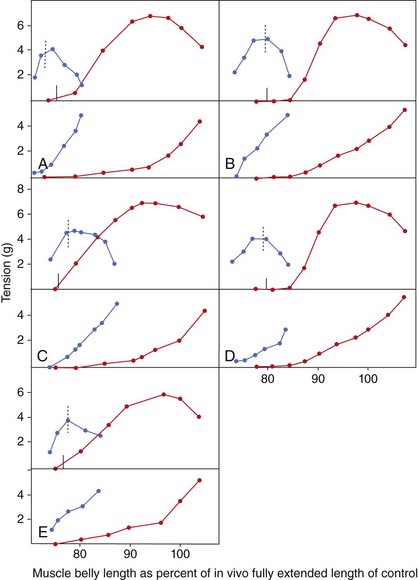
Figure 1-29 Active and passive length-tension curves of mice muscles that have been immobilized in a shortened position for 3 weeks and compared to control muscles. Note the curve of the shortened muscle is shifted to the left. Red line, Control muscle; blue line, experimental-shortened muscle.
(From Williams PE, Goldspink G: Changes in sarcomere length and physiological properties in immobilized muscles, J Anat 127:459-468, 1978.)
Although muscles can become shortened by loss of sarcomeres in series, this is not the most common problem contributing to musculoskeletal pain. The most common problem is the relative stiffness of muscles attaching to the joint. If an individual stands with the pelvis in an anterior pelvic tilt, the therapist should not assume that the hip flexors are short. Rather, a likely explanation is that the passive stiffness of the hip flexors, anteriorly tilting the pelvis, is greater than the passive stiffness of the rectus abdominis and the external oblique muscles, posteriorly tilting the pelvis, at the length necessary to maintain the pelvis in the optimal position. The back extensor muscles could also be contributing to the anterior tilt of the pelvis, further increasing the demands on the passive tension of the abdominal muscles. These concepts are discussed in the section on relative flexibility/stiffness.
Accurate assessment of the contributing factors is important to the development of the treatment program. If the problem is a relative stiffness problem, then stretching the hip flexors is not going to change the pelvic alignment. Rather, the external oblique and rectus abdominis muscles must be able to generate the necessary passive tension at the right length, which requires hypertrophying the abdominal muscles so that the amount of titin increases. But the exercises must be performed in such a way as to optimize the hypertrophy with the abdominal muscles at the right length. The actively performed exercises must produce the desired change in length and passive tension, which means that performing exercises, such as leg raises or leg lowering in the supine position, may be counter productive because they are also a hip flexor muscle exercise and performed with the hip flexors in a shortened position. This would be problematic in individuals with large and heavy thighs or long lower extremities. Thus the stiffness of the hip flexors at a short length may be increasing more rapidly than the desired changes in the abdominal muscles.
Muscle Performance
The term muscle performance is preferred as compared to muscle weakness to place an emphasis on whether all factors influencing the muscle’s participation are performing optimally. Performance includes timing, length, passive tension, and the ability to generate active tension and endurance. Assessment of muscle strength provides information about muscle performance, and the results of the test can provide at least four possible determinations about the muscle. These test results indicate how a muscle is being used, characteristics of the adaptations, and insights into the movement patterns. The inference is that all factors that determine recruitment and use patterns are not optimal. The implication is that strengthening the muscle will not adequately address the problem because the “weakness” is the result not the cause. This rationale, of course, does not apply to conditions in which there is denervation, disease, or direct trauma to the muscle. Manual muscle testing (MMT) can be used to discern whether the muscle is (1) weak because of atrophy and the lack of sarcomeres in parallel and thus unable to develop adequate active tension; (2) strained because of being subjected to forces that have torn or disrupted the Z-lines of the sarcomeres and unable to develop adequate active tension; (3) too long, having added sarcomeres in series, and the muscle does not develop the appropriate tension throughout the ROM (Figure 1-30), or (4) normal.
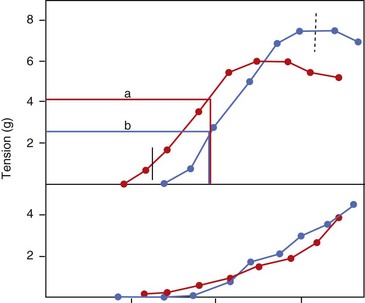
Figure 1-30 Illustration of the effect on the active tension of lengthened muscle. If the control muscle and the lengthened muscle are tested in the same position (line a), the tension is less for the lengthened muscle than for the control (line b).
(Data adapted from Williams PE, Goldspink G: Changes in sarcomere length and physiological properties in immobilized muscles, J Anat 127:459-468, 1978.)
Determination of these four possibilities is based on the following test findings. The MMT methods used are those that apply pressure with the 1-joint muscle at its shortest length, as developed by Kendall et al.60 For example, when testing the lower trapezius muscle, the shoulder is placed in about 145 degrees of abduction with the glenohumeral joint laterally rotated and the scapula upwardly rotated. The therapist applies pressure to the forearm as the patient attempts to hold the position. If the patient is able to hold the test position when the therapist applies maximum pressure, the muscle is graded strong/normal or 5/5. If when the therapist applies pressure, the patient is not able to hold the position and the arm and scapula are unable to tolerate the pressure throughout the range, the muscle is considered weak and the grade can range from 3+ to 4+, depending on the amount of pressure the therapist applies that causes the arm to move. If the therapist applies pressure and the patient is unable to hold at the initial test position, but after a few degrees of motion of the arm and scapula, the patient is able to resist the continued pressure, the muscle is considered long but not weak. The final possible test finding is that if the patient has tenderness in the muscle belly of the muscle to palpation, then strain is suspected. If during testing, when the therapist applies pressure, the patient complains of pain and the muscle tests weak because the shoulder position cannot be held throughout the range as pressure is applied by the therapist, and the muscle is considered weak because of muscle strain. Clearly, these conditions require different interventions. The strained muscle must not be subjected to continued stress so healing can take place. The weak muscle must be strengthened by an appropriately designed progressive resistance exercise program. The long muscle must be used in shortened ranges, and the load decreased enough to allow the part to which it attaches to be moved through its optimal ROM.
The following examples are given to clarify and illustrate these possible muscle performance conditions and relate them to other tissue conditions and adaptations. Although this book does not discuss MS syndromes of the shoulder girdle, for syndromes of the neck, elbow, and the hand, part of the treatment involves optimizing shoulder girdle function. The performance of the serratus anterior muscle is used as the example.
Case example 1
A 40-year-old woman has not been physically active, but her appearance is important to her so she has tried to stand up straight and hold her shoulders back to have good posture. She has developed neck pain and some discomfort on the top of her shoulder that occurs when she performs tasks that involve reaching overhead. She is 5 ft 5 inches tall and weighs 140 lbs.
Physical examination
The examination indicates that the vertebral border of her scapula at the spine of scapula is 2 inches away from her thoracic spine. Therefore, her scapula is in adduction (retraction), which means the resting position of the serratus anterior muscle is longer than the optimal length. When she performs shoulder flexion, her scapula only upwardly rotates 40 degrees, instead of the optimal 50 to 55 degrees, and the inferior angle of the scapula barely reached the side of her thorax rather than reaching the midaxillary line. Her shoulder flexion was 175 degrees. MMT of the serratus anterior demonstrates that she could not hold the test position and that her arm gave through the range as the therapist applied pressure. Based on the pressure the therapist applied, the muscle was determined to be weak and graded 4−/5.
Key findings
The patient’s scapula was not moving correctly because the upward rotation was only 40 degrees, not the appropriate 50 to 55 degrees, but she was flexing her shoulder almost 175 degrees. Therefore, as compensation for the decreased scapular upward rotation and abduction, the glenohumeral flexion was greater than 120 degrees. The serratus anterior muscle tested weak. No resistance was noted during assisted scapular motion. Correction of the scapular motion eliminated the pain in the shoulder.
Treatment
The patient was given two main exercises for this condition. First, she was instructed to perform shoulder flexion by facing the wall, with her elbow flexed and then sliding the little finger side of her hand up the wall as she flexed her shoulder and extended her elbow. When the patient initially performed this exercise, her scapula did not move through the optimal ROM, and she commented on the discomfort at the top of her shoulder. The therapist then assisted the scapular motion as the patient performed the shoulder flexion so that there was optimal scapular upward rotation and abduction. The therapist did not note any resistance as she assisted the scapular motion. The therapist continued to assist the patient with the exercise, providing verbal, as well as manual cues, so that the patient was able to produce the correct scapular motion during the shoulder flexion. The important point is that the patient was not given serratus anterior muscle strengthening exercises, such as the push-up plus, but was given an exercise that required the optimal motion of the scapula. Improving the “strength” of a muscle does not automatically mean or ensure that the scapula will move correctly. To be sure the end result is that the scapula moves correctly, the therapist must see the scapula move correctly as the patient performs the motion. There is no magic in an exercise unless the exercise is producing the desired result at the time of performance. For the second exercise, the patient is in the quadruped position to ensure activity of the serratus anterior muscle, which supports the thorax through its attachment to the scapula as the weight is placed on the upper extremity. The patient’s initial position was one of scapular adduction and slight winging. She was instructed to rock backward, decreasing the loading on her shoulder girdle and allowing her scapulae to abduct and upwardly rotate. The therapist provided some assistance in guiding the scapula into the correct position. The patient then rocked forward to the starting position while maintaining the abducted position of the scapula and controlling the winging. She stopped coming forward at the point she could not control the scapula. Again, the major point is that the serratus anterior muscle is forced to develop tension, but the correct control of the scapular motion is the criterion for being an acceptable exercise. The exercises will progress as the patient is able to demonstrate the proper movement of the scapula and does not have pain. The goal is to improve the support of the scapula by the serratus anterior muscle so that the downward pull from the cervicoscapular muscles is reduced, thus reducing stress on the neck.
Case example 2
The second case is a 28-year-old male who performs a regular program of resistive exercises and plays tennis at least twice a week. He also has neck pain that increases when he plays tennis. He is 5 ft 11 inches tall and weighs 185 lbs. He has a very muscular build with marked hypertrophy of his shoulder girdle muscles.
Physical examination
In the standing position, his shoulders are depressed and his scapula are adducted, with the vertebral border of the spine of the scapula  inches from his thoracic spine. The muscle definition of the rhomboids is particularly obvious. On completion of shoulder flexion, the scapula was upwardly rotated 45 degrees (55 degrees is normal) and the inferior angle reached the posterolateral border of the thorax, not the midaxillary line, yet shoulder flexion was 175 degrees. MMT of the serratus anterior muscle indicated that the patient could not maintain the initial test position when the therapist applied pressure, but after a 15-degree change in the shoulder angle because of scapular downward rotation, he was able to maintain the position against maximum pressure. The test performance indicated that the serratus anterior muscle was long but not weak. When the patient was asked to perform the exercise of shoulder flexion by sliding the little finger side of his hand up the wall, the therapist had to assist the movement of the scapula. The therapist noted that there was marked resistance to the assistance given to the scapula in the direction of upward rotation and abduction.
inches from his thoracic spine. The muscle definition of the rhomboids is particularly obvious. On completion of shoulder flexion, the scapula was upwardly rotated 45 degrees (55 degrees is normal) and the inferior angle reached the posterolateral border of the thorax, not the midaxillary line, yet shoulder flexion was 175 degrees. MMT of the serratus anterior muscle indicated that the patient could not maintain the initial test position when the therapist applied pressure, but after a 15-degree change in the shoulder angle because of scapular downward rotation, he was able to maintain the position against maximum pressure. The test performance indicated that the serratus anterior muscle was long but not weak. When the patient was asked to perform the exercise of shoulder flexion by sliding the little finger side of his hand up the wall, the therapist had to assist the movement of the scapula. The therapist noted that there was marked resistance to the assistance given to the scapula in the direction of upward rotation and abduction.
Key findings
The interpretation is that the serratus anterior was too long to move the scapula through the optimal range and the resistance to the motion was from the stiffness of the hypertrophied rhomboid muscles. The serratus anterior muscle had to generate enough tension to overcome the passive resistance of the rhomboids, as well as shorten enough to move the scapula through the optimal range.
Diagnosis
Scapular downward rotation—motor pattern incoordination. In this situation, the assistance of the therapist in moving the scapula also helped improve the extensibility of the rhomboid muscles.
Treatment
The patient was encouraged to frequently perform shoulder flexion with a major emphasis on abducting and upwardly rotating the scapula. He was also advised to avoid any tendency to “hold” his shoulders back and to cease any type of scapular adduction exercises. The patient also performed the quadruped exercise with the major emphasis on abducting and upwardly rotating the scapula.
Another consideration is how these tissue adaptations contribute to the stress on the cervical spine. First, the hypertrophy of the shoulder girdle musculature increases the weight of the upper extremities and the support by the cervicoscapular muscles adds to the compressive forces on the cervical spine. The passive stiffness of these muscles can also restrict the ease of cervical rotation. Second, when the patient uses his arms, particularly during the overhead motion that requires scapular upward rotation and abduction, the passive stiffness of the levator scapulae muscle could exert a rotational, as well as a compressive, force as it is being stretched during the scapular motion. Also, the passive resistance from the stiffness of the rhomboids requires the upper trapezius to develop greater tension than if there were minimal resistance to scapular upward rotation and elevation. The increased demands on the upper trapezius muscle can further add to the compressive force on the cervical spine. If the patient has neck pain during shoulder flexion, support of the scapula by the therapist during the shoulder motion can decrease or even eliminate the symptoms, which supports the hypothesis about the contributing factors. Improving the participation of the serratus anterior muscle and decreasing the stiffness of the rhomboid muscles would reduce the stress on the cervical spine. These examples illustrate the influences of the intersegmental demands and explain why the therapist needs to consider multiple influences on the painful joint during the examination when developing the treatment program.
In summary, in both patients, the movement impairment of the scapula was similar, but the underlying contributing factors were markedly different, requiring a different emphasis in the treatment program. In both conditions, the primary emphasis has to be on ensuring that the scapula moves correctly. In the first patient, a major contributing factor was the actual weakness, or inability to develop sufficient contractile tension, as well as the increased length of the serratus anterior muscle. In the second patient, the serratus anterior muscle was not weak but was long and had to develop enough tension to overcome the resistance from the rhomboid muscles. In both of these cases, the shoulder flexion was 180 degrees, which means that glenohumeral motion occurred more readily and was a site of compensation for the deficient scapular motion. Because the scapular motion was insufficient to achieve the 180 degrees of shoulder flexion, the glenohumeral motion exceeded the standard of 120 degrees. Improving scapular motion will decrease the stress on the glenohumeral joint structures by stopping the excessive excursion. These scenarios both address movement imprecision and the body’s tendency to the path of least resistance. Additional discussion of tissue adaptations is provided in the first volume of this book, Diagnosis and Treatment of Movement Impairment Syndromes.
Imprecise Movement
The end result of the tissue adaptations, whether skeletal, muscular, and neurological, is that movement is altered and no longer precise. As stated frequently, our hypothesis is that alteration in the accessory or arthrokinematic motion is probably the most common and most important contributing factor. Excessive physiological or osteokinematic motion has to be associated with altered accessory motion. As discussed in the previous case examples, the lack of scapular motion resulted in excessive glenohumeral motion. This also means excessive accessory motion of either or both superior glide or anterior glide. Assessment of accessory motion impairments is indeed difficult, and most often the fault is implied when pain is present during the performance of a physiological motion. Often, gentle assistance by the therapist to control movement precision as the patient performs the motion can confirm that the slight alteration in motion is the cause of the pain. The therapist guiding the pattern of rotation of the head and cervical spine can be used to assess whether the movement fault is the problem (see Chapter 3). Similarly, as discussed in Chapter 7, having the patient correcting the tibiofemoral rotation can alleviate the pain during knee extension in weight bearing. Although the focus is on the painful joint, it is very important to consider the pattern of movement and control evident in all of the other joints of the limb, as well as the alignment of the entire body. The therapist needs to assess the precision of motion of the painful joint, the entire limb segment, and the whole body. An example is a young patient with knee pain who stands in a swayback posture with knees hyperextended, hip extended, and shoulders posterior to the hip joint. There is poor definition of the gluteal muscles (Figure 1-31). During single-leg standing, the painful knee hyperextends and medially rotates. When going up steps, there is tibiofemoral rotation and the patient brings the knee back to meet the body rather than the body up to the knee (Figure 1-32). The patient also leans forward in an exaggerated manner when going up the steps. One reasonable explanation is that the patient is placing an abnormal amount of stress on the anterior knee joint, which may be changing the articular surface of the tibia over time. The cruciate ligaments will be subjected to inappropriate stress.7 The weight line of the body will be anterior to the knee joint, which decreases the demands on the quadriceps. The poor definition of the gluteal muscles suggests that the hamstrings are the dominate muscle (see Figure 1-32). The deep lateral rotator muscles of the hip are also likely to be poorly developed. During the step up, the femur is rotating medially because the lateral rotation is not controlled by the gluteal muscles or the deep lateral rotators. In fact, the medial hamstrings could be contributing to excessive medial rotation. The observation that the patient brings the knee back to meet the body is consistent with use of the hip extensors for knee control rather than the quadriceps. Leaning forward with the trunk can also reduce the demands on the quadriceps. Thus, control of the knee joint is affected not only by the precision of motion at the knee joint itself but also by control of the entire segment and of the entire body. Every tissue adaptation that alters alignment has the potential of affecting the precision of joint motion. As mentioned previously, one of the challenges for the therapist is to differentiate structural variations in alignment from acquired changes in alignment. The therapist must also perform a detailed assessment of muscular and motor control performance. Patients need to understand that their alignment and movement patterns are based on what is familiar and not what is optimal or right. The body does not have an internal referencing system that gives immediate feedback about optimal versus nonoptimal alignment or movement. A major responsibility of the therapist is to identify the impairments in muscle performance and movement patterns and provide the instruction in both exercise and movement correction during activities.

Figure 1-31 Swayback posture with line of gravity posterior to hip joint, decreasing the hip extensor moment. Associated with poor definition of the gluteal muscles.
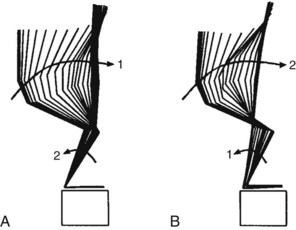
Figure 1-32 Motion analysis display of two strategies controlling the knee motion during stepping up on a footstool. A, Strategy in which the body is moved toward the knee that emphasizes control by the knee extensor muscles. B, Strategy in which the knee is pulled toward the body that emphasizes control by the hip extensor muscles.
(From Sahrmann SA: Diagnosis and treatment of movement impairment syndromes, St Louis, 2002, Mosby; courtesy Amy Bastian, PhD, PT.)
A recent radio program featured a physician who specializes in foot problems, a podiatrist, and a fitness expert who also specializes in running. They all seemed to agree that walking was automatic, all people walked in the same way, and there was not much to change. They did seem to believe that running was different and that some instruction in how to run would be useful. Clearly, they have not made the observation of recognizing someone by how they walked without seeing the face. The variations in gait are many, from lack of push-off to excessive push-off, from excessive hip adduction and lumbopelvic rotation to trunk lateral sway. The wear pattern on shoes is a good indicator of variations in walking and even the impressions in the top of the shoes. Some individuals extend their toes so much that the impression of the toes is very evident in the top of the shoe. One patient has deep gouges on the inside of the heel part of his shoes because his hips adduct so much during the swing phase that he hits the contralateral shoe on swing phase, not a little but a lot. Another indication of variation in muscle strategies during walking is the callous distribution. Some individuals, even long distance runners, do not have any notable callouses, but other individuals have very thick callouses. These individuals push the feet into the supporting surface, creating shear in their shoes, whereas people without callouses generate much of their swing phase with proximal muscles. They do not have to control the movement of their line of gravity with their feet but by the control of their trunk. All of these variations reflect alterations in the precision of motion. The task is to ascertain how alterations are affecting the painful joint and not get lost in the variations merely because they exist.
Path of Least Resistance
The movements of the joints of the body follow the rules of physics and take the path of least resistance. Forced to select the most important and useful observation pertaining to musculoskeletal pain, this concept is the clear choice. The symptoms in the majority of patients, particularly the nonacute patients, are reduced or eliminated when the painful area is stabilized and not allowed to move. Undoubtedly that accounts for the current popularity of “stabilizing” exercises or “core” exercises. The other most common factor that can be present at the same time is compression or loading of the joint. In fact, identifying whether compression is part of the problem is extremely important because abdominal muscle exercises can add to the compression. Because movements involve the participation of multiple joints, many of them in series, the joint that moves the most readily is the one that has the least resistance. One of the key controlling factors of the path of least resistance is the relative stiffness or flexibility of the tissues attaching to a joint. A few examples illustrate how generally this rule applies to a variety of situations. One example is found in individuals that have cardiac bypass surgery in which the thorax is opened. After the surgery, the scar tissue and stiffness of the chest is so great that patients become abdominal breathers. The abdomen becomes distended because they are no longer able to expand the ribcage during inhalation. Another example is the development of changes in the vertebrae above and below after spinal fusion, known as adjacent segment disease.61 One explanation is that the movement of the adjoining vertebral segments is increased because of the lack of motion at the fused joint. Other factors, such as the variations in joint degeneration, also influence the path of least resistance. For example, during cervical rotation, if degenerative changes are greater in the lower cervical joints than the upper cervical joints, then the movement will occur more readily in the upper cervical region than the lower. Because movement occurs along the path of least resistance, which means that the joint that moves the most readily in a specific direction, is subjected to a greater frequency of motion. When the frequency becomes excessive by changing the extensibility of the tissues and there is an associated alteration in the precision of the joint motion, the result is microtrauma. The vicious cycle of the readiness of the joint to move furthering the frequency of motion eventually causes microtrauma that becomes macrotrauma. With increased frequency of motion, there will be associated changes in flexibility and extensibility of the supporting tissues and a resulting change in the precision of the joint motion. The tissue trauma associated with repeated motion has been well documented.39,62,63 A very useful guideline when determining the diagnosis and developing the treatment program is to presume that pain is arising from the site that is moving and the movement is occurring at this site because it is the path of least resistance. In addition, not only does the path of least resistance determine the site but also the direction of the offending motion.
Joint Mobility
The adaptations of the skeletal, nervous, and muscular systems are normal biological responses to repeated movements and sustained alignments. Over time, however, they can combine to cause alterations in the precision of motion. As discussed in the previous sections, the modifiers or variations in individuals explain why not all people develop pain problems or at least not as readily as other people. The primary means of preventing, as well as correcting, the cause of mechanically induced pain is to maintain precise movement of the joint. As depicted in the model, the problematic outcome of the tissue adaptations is the development of a relative stiffness or flexibility condition that becomes exaggerated because the body takes the path of least resistance for movement. The result of this cascade of events is that a joint develops hypermobility. Hypothetically, the hypermobility is an accessory or arthrokinematic motion rather than physiological or orthrokinematic motion. One of the consequences of imprecise movement is the development of points of high contact stress because of inadequate distribution of forces within the joint. For example, disc degeneration can begin as young as 20 years of age and is a process of structural failure.39 The disc damage is attributed to compression, bending, and torsion.35,62 Once the disc undergoes structural change, the loading is altered and the joint begins to become unstable because the length and tension of supporting structures is altered. If motion is imprecise, the trauma to tissue is further increased. The changes in the spine begin with hypermobility that progresses, and the final phase is hypomobility.35 At this stage, the degenerative process has affected the joint to such an extent that motion has become limited and there are numerous tissue changes, including loss of cartilage and the development of exostosis. Although most studies have been of the degenerative process of the spine, a similar process has to apply to all joints. The most effective form of treatment will correct or minimize the hypermobility. This supports the rationale for “stabilization or core” exercises, but generic stabilization exercises are not sufficient. The components necessary for an effective program are identifying the offending movement direction and the contributing factors and retraining the patient to move the affected segment correctly, redistributing the movement, and using the appropriate timing.
This major emphasis on joint hypermobility does not mean that some painful conditions do not involve a form of a sustained malalignment or a stress into a malaligned position. Such conditions can respond to an abrupt and possibly forceful form of treatment. But the questions that remain, even if there is immediate relief of pain, are (1) what caused the condition to develop in the first place, (2) does it mean that the painful tissues are now fully restored to an optimal state, (3) what will prevent the condition from arising again, (4) does the patient understand the condition, and (5) is the patient aware of the contributing factors and how to avoid a repeat episode? Has the patient been given an active strategy to address the condition or is the patient dependent on passive intervention? In our experience, even conditions that respond to a form of manipulation can also be addressed by active treatment during the acute episode, and certainly, active treatment is required for long-term management. Furthermore, as reported in the literature, the resolution of acute pain is not as costly as the resolution or prevention of chronic pain.64 Chronic pain problems are most often the ones associated with forms of tissue degeneration and strategies to prevent, slow, or minimize tissue trauma and degeneration have to be of particular importance. Because there is a discernible pattern to the resulting pain problem, the condition can be classified as a specific syndrome. The syndrome would be named for the movement direction or the sustained alignment that (1) most consistently causes symptoms; (2) is imprecise; and (3) when corrected, decreases or eliminates the symptoms.
Summary
This book describes the MS syndromes of the cervical and thoracic spines, the elbow, hand, knee, and foot. The most complete picture as possible of the contributing factors, the tests used in the examination, and the treatment program is presented. Treatment consists of specific exercises, as well as instruction in changing movement patterns to correct the problems of relative stiffness or flexibility. As noted in the model, a further delineation in the syndromes is undertaken by attempting to identify whether the important contributing factors are from motor control, resulting in motor pattern incoordination, or from muscle weakness or force production deficit. The individual with hypertrophied muscles who uses muscles in patterns causing problems is at one extreme, and the individual who has generalized weakness or marked weakness of key muscles is the other extreme. Many patients fall somewhere on the continuum between these two extremes. The value of sublabeling is to help the practitioner and the patient understand that treatment is not just a function of strengthening muscles but also retraining. In fact, excessive muscle strength can be a contributing factor to movement impairments. One of the most challenging aspects of guiding an individual’s exercise program is designing one that promotes optimal tissue health and prevents tissue injury because improper exercise can also contribute to problems.
In the future, the syndromes described in this book and its predecessor will most likely be modified by research, as well as by careful clinical analysis. As with pathological conditions of other systems of the body, advances in treatment and insights into causes depend on classification or delineations of subclassifications or diagnostic groups. This pattern exists for all pathophysiological and kinesiopathological conditions. The goal is to provide adequate information to enable others to participate in the process of using and clarifying MS syndromes. If the hypothesis on the “causes” of musculoskeletal pain syndromes has merit and preventive examinations are instituted, the impact on costs associated with these conditions should be significantly reduced. If, after an initial episode of pain, the patient seeks or is referred for an examination to identify impaired alignments, movement patterns, and muscle performance, the cost savings could be substantial. Of course, this supposes that patients will follow the recommendations. Clearly, as health care costs continue to escalate, emphasis on prevention and personal responsibility for healthful living is going to increase. As the consequences of insufficient exercise and excessive eating are shown to contribute to disease development, individuals are going to have to assume responsibility for their health. Individuals, as well as practitioners, will learn that these problems are not the inevitable outcome of aging and activity and that the progression of these disorders can be modified. The medical practitioner is now fully aware of how lifestyle is a major contributor to the development of cardiovascular and metabolic disorders. Musculoskeletal pain syndromes are also lifestyle disorders. Research currently underway will provide insights into the accuracy of that belief.
As depicted in the model, the consequence of the cascade of events is the development of a musculoskeletal pain syndrome or more accurately, a MS syndrome. Therapists must develop a specific diagnosis of these conditions. Our hypothesis is that these syndromes describe the cause of the problem as compared to the source, the pathoanatomical structure, that is painful. The source of pain is the consequence of impaired motion.
Clearly, other practitioners and the public will not appreciate the expertise of physical therapists in identifying syndromes unless terminology is used that encapsulates the condition. Terminology to describe the patterns represented by these syndromes needs to be accepted to communicate among ourselves and to the public. Just as other practitioners used diagnostic manuals describing the syndromes of the body system for which they have responsibility, so, too, physical therapists must have diagnostic manuals describing MS syndromes.
In addition to insights gained from ongoing analysis of the model and all of its components, trends in health care that were beginning to emerge 10 years ago are becoming clear. The impact of these trends on physical therapy is also becoming evident. Several factors suggest that physical therapy must undergo a paradigm change. The change is from a practitioner providing episodic care after acute injury to a practitioner providing preventive, as well as restorative, care on a yearly basis throughout life. The content of this book and the first volume provides information that (1) identifies the key factors contributing to the development of musculoskeletal pain and (2) can be used for the yearly examination and a patient-centered program. The factors supporting the importance of having a practitioner with expertise in the movement system are (1) that musculoskeletal pain is part of the degenerative process characteristic of the human biological system and is affected by lifestyle; (2) structural variations that can predispose an individual to pain problems, depending on the sports or fitness activity that they select; (3) the continuing evidence that exercise is the most potent agent for maintaining and restoring health; and (4) the rapidly rising cost of health care.
The monitoring of the movement system should consist of an examination of muscle performance, alignment, movement patterns, general conditioning, and the appropriateness of exercise programs and sports adaptations. As already stated, exercise is critical to the maintenance of health, and optimal exercise requires optimal development of the MS of the human body. The physical therapist’s expertise should be in assessment and program development for prevention and diagnosis of MS dysfunctions when they occur. Individuals should have a yearly (or at the least every 2 years) examination of their movement systems, and such examinations should begin early in life and continue throughout life. The expertise that is required is knowledge of 1) structural variations that affect the appropriateness of specific activities and sports, 2) musculoskeletal development, and 3) the condition of the cardiovascular system. Clearly, all individuals must participate in exercise and activity that will optimize their health. To be able to sustain their activity level injury, prevention is a necessity and the physical therapist is ideally prepared for this role.
This type of practice can be considered analogous to the role of the dentist who monitors, recommends, and treats the dental system from early childhood through old age. This role of the physical therapist in guiding, monitoring, diagnosing, and treating the human movement system is increasingly important as the practice of medicine continues to change. The majority of physicians lack knowledge of the mechanical aspects of musculoskeletal disorders, as well as the examination skills, to detect a wide variety of relatively minor musculoskeletal conditions. Rather, a physician’s expertise is needed primarily to identify severe disorders of other systems, such as the cardiac or nervous system, as well as potential neoplasms. Physicians are relying more and more on chemical and radiological assessments and not just on the physical examination. A practitioner who is skilled in a movement examination can help differentiate between the radiological findings suggesting the site of pain-generating tissue and the clinical examination suggesting a different site. For example, a skilled clinical movement examination can help differentiate whether pain in the shoulder area is coming from the cervical spine or the shoulder joint. Similarly, pain in the hip region can arise from the lumbar spine, the hip joint, or both. Radiological changes in both regions may be present or even misleading, and a thorough movement examination can be the method of identifying not only the actual pain generating site but also the mechanical interaction of these joints that is often contributing to the tissue injury. For example, if the hip joint does not extend easily during walking, then rotation will be imposed on the pelvis and the lumbar spine, contributing to tissue microtrauma and eventually macrotrauma. The pain in the hip region can be from early degenerative hip joint changes or from lumbar spine motion or from both. Radiological assessments to determine the site causing the pain, particularly in an aged population with multiple sites of degeneration can be misleading and a skilled MS examination can be particularly useful.
Tissue impairment diagnoses as they pertain to the different regions of the body are described in some detail in this book and how some of these diagnoses are associated with MS syndromes. The practice pattern used is one in which patients are not typically seen for frequent treatments. Rather, the treatment plan places the emphasis for remediation on the patient. In other words, the therapist completes a standard examination, determines a diagnosis, explains the diagnosis to the patient, and plans and teaches the patient a very specific exercise program, but the patient is given the responsibility of correcting the problem. The exercises address the needed tissue and movement corrections, and the therapist reviews and instructs the patient in the necessary modification of the way basic, sports, and fitness activities are performed. The instruction by the therapist includes several methods by which the patient can alleviate the symptoms. These include changes in movement or alignment or even types of supports such as pillows or armrests when sitting. Our experience is that such methods not only empower the patient but help reduce the anxiety that accompanies pain. This type of practice is compatible with the model of a yearly visit for preventive purposes. Of course, if a problem develops then the therapist is in a good position to offer an efficient and effective program because the patient is already known to the therapist. The contents of this book and its predecessor should serve as a guide to understanding MS syndromes, determining a diagnosis, and developing a treatment program. There will be changes as research and clinical experience provide additional information, but this information should provide a useful basis for current patient care, as well as future analysis.
1 Scholtes SA, Norton BJ, Lang CE, et al. The effect of within-session instruction on lumbopelvic motion during a lower limb movement in people with and people without low back pain. Man Ther. 2010;15:496-501.
2 Harris-Hayes M, Holtzman GW, Earley JA, et al. Development and preliminary reliability testing of an assessment of patient independence in performing a treatment program: standardized scenarios. J Rehabil Med. 2010;42(3):221-227.
3 Harris-Hayes M, Sahrmann SA, Van Dillen LR. Relationship between the hip and low back pain in athletes who participate in rotation-related sports. J Sport Rehabil. 2009;1:60-75.
4 Van Dillen LR, Maluf KS, Sahrmann SA. Further examination of modifying patient-preferred movement and alignment strategies in patients with low back pain during symptomatic tests. Man Ther. 2009;14(1):52-60.
5 Harris-Hayes M, Van Dillen LR. The inter-tester reliability of physical therapists classifying low back pain problems based on the movement system impairment classification system. PMR. 2009;1(2):117-126.
6 Scholtes SA, Gombatto SP, Van Dillen LR. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech. 2009;24(1):7-12. (Bristol, Avon)
7 Andrade GT, Azevedo DC, De Assis Lorentz I, et al. Influence of scapular position on cervical rotation range of motion. J Orthop Sports Phys Ther. 2008;38(11):668-673.
8 Gombatto SP, Norton BJ, Scholtes SA, et al. Differences in symmetry of lumbar region passive tissue characteristics between people with and people without low back pain. Clin Biomech. 2008;23(8):986-995. (Bristol, Avon)
9 Van Dillen LR, Bloom NJ, Gombatto SP, et al. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport. 2008;9(2):72-81.
10 Gombatto SP, Klaesner JW, Norton BJ, et al. Validity and reliability of a system to measure passive tissue characteristics of the lumbar region during trunk lateral bending in people with and people without low back pain. J Rehabil Res Dev. 2008;45(9):1415-1429.
11 Scholtes SA, Van Dillen LR. Gender-related differences in prevalence of lumbopelvic region movement impairments in people with low back pain. J Orthop Sports Phys Ther. 2007;37(12):744-753.
12 Harris-Hayes M, Wendl PM, Sahrmann SA, et al. Does stabilization of the tibiofemoral joint affect passive prone hip rotation range of motion measures in unimpaired individuals? A preliminary report. Physiother Theory Pract. 2007;23(6):315-323.
13 Van Dillen LR, McDonnell MK, Susco TM, et al. The immediate effect of passive scapular elevation on symptoms with active neck rotation in patients with neck pain. Clin J Pain. 2007;23(8):641-647.
14 Caldwell C, Sahrmann S, Van Dillen L. Use of a movement system impairment diagnosis for physical therapy in the management of a patient with shoulder pain. J Orthop Sports Phys Ther. 2007;37(9):551-563.
15 Gombatto SP, Collins DR, Sahrmann SA, et al. Patterns of lumbar region movement during trunk lateral bending in 2 subgroups of people with low back pain. Phys Ther. 2007;87(4):441-454.
16 Van Dillen LR, Gombatto SP, Collins DR, et al. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Arch Phys Med Rehabil. 2007;88(3):351-360.
17 Gombatto SP, Collins DR, Sahrmann SA, et al. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clin Biomech. 2006;21(3):263-271. (Bristol, Avon)
18 Van Dillen LR, Sahrmann SA, Caldwell CA, et al. Trunk rotation-related impairments in people with low back pain who participated in 2 different types of leisure activities: a secondary analysis. J Orthop Sports Phys Ther. 2006;36(2):58-71.
19 Harris-Hayes M, Van Dillen LR, Sahrmann SA. Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiother Theory Pract. 2005;21(3):181-196.
20 Van Dillen LR, Sahrmann SA, Wagner JM. Classification, intervention, and outcomes for a person with lumbar rotation with flexion syndrome. Phys Ther. 2005;85(4):336-351.
21 McDonnell MK, Sahrmann SA, Van Dillen L. A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: a case report. J Orthop Sports Phys Ther. 2005;35(1):3-15.
22 Van Dillen LR, Sahrmann SA, Norton BJ, et al. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys Med Rehabil. 2003;84(3):313-322.
23 Van Dillen LR, Sahrmann SA, Norton BJ, et al. Movement system impairment-based categories for low back pain: stage 1 validation. J Orthop Sports Phys Ther. 2003;33(3):126-142.
24 Hollman JH, Deusinger RH, Van Dillen LR, et al. Knee joint movements in subjects without knee pathology and subjects with injured anterior cruciate ligaments. Phys Ther. 2002;82(10):960-972.
25 Van Dillen LR, Sahrmann SA, Norton BJ, et al. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther. 2001;31(8):402-413. discussion 414-418
26 Maluf KS, Sahrmann SA, Van Dillen LR. Use of a classification system to guide nonsurgical management of a patient with chronic low back pain. Phys Ther. 2000;80(11):1097-1111.
27 Van Dillen LR, McDonnell MK, Fleming DA, et al. Effect of knee and hip position on hip extension range of motion in individuals with and without low back pain. J Orthop Sports Phys Ther. 2000;30(6):307-316.
28 Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. Phys Ther. 1998;78(9):979-988.
29 Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St Louis: Mosby; 2002.
30 Lukoschek M, Boyd RD, Schaffler MB, et al. Comparison of joint degeneration models. Surgical instability and repetitive impulsive loading. Acta Orthop Scand. 1986;57(4):349-353.
31 Guilak F, Fermor B, Keefe FJ, et al. The role of biomechanics and inflammation in cartilage injury and repair. Clin Orthop Relat Res. 2004;423:17-26.
32 Lota JC, Ulrich JA. Innervation, inflammation, and hypermobility may characterize pathologic disc degeneration: review of animal model data. J Bone Joint Surg Am. 2006;88:76-82.
33 Mosby’s medical dictionary, ed 8. St Louis: Mosby. 2009.
34 Stedman’s dictionary, ed 28. Philadelphia: Lippincott Williams & Wilkins. 2005.
35 Adams MA, Dolan P. Recent advances in lumbar spinal mechanics and their clinical significance. Clin Biomech. 1995;10(1):3-19.
36 Mueller MJ, Maluf KS. Tissue adaptation to physical stress: a proposed “physical stress theory” to guide physical therapist practice, education, and research. Phys Ther. 2002;82:383-403.
37 Gosheger G, Liem D, Ludwig K, et al. Injuries and overuse syndromes in golf. Am J Sports Med. 2003;31(3):438-443.
38 Conn JM, Annest JL, Gilchrist J. Sports and recreation related injury episodes in the US population, 1997-99. Inj Prev. 2003;9(2):117-123.
39 Adams M, Bogduk N, Burton K, et al. The biomechanics of back pain, 2 ed. Churchill Livingstone; 2006.
40 Brophy R, Silvers HJ, Gonzales T, et al. Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med. 2010;44:694-697.
41 Prodromos CC, Han Y, Rogowski J, et al. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320-1325.
42 Sigward SM, Powers CM. The influence of gender on knee kinematics, kinetics and muscle activation patterns during side-step cutting. Clin Biomech. 2006;21(1):41-48. (Bristol, Avon)
43 Pollard CD, Sigward SM, Powers CM. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech. 2010;25(2):142-146. (Bristol, Avon)
44 Remvig L, Jensen DV, Ward RC. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: review of the literature. J Rheumatol. 2007;34:804-809.
45 Taylor RT. A discussion of Wolff’s law. J Bone Joint Surg Am. 1902:S1-S15.
46 Sterling M, Jull G, Wright A. The effect of musculoskeletal pain on motor activity and control. J Pain. 2001;2(3):135-145.
47 Halsband U, Lange RK. Motor learning in man: a review of functional and clinical studies. J Physiol. 2006;99:414-424. (Paris)
48 Wakeling JM, Horn T. Neuromechanics of muscle synergies during cycling. J Neurophysiol. 2009;101:843-854.
49 Chapman AR, Vicenzino B, Blanch P, et al. Leg muscle recruitment during cycling is less developed in triathletes than cyclists despite matched cycling training loads. Ex Brain Res. 2007;3:503-518.
50 Chapman A, Vicenzino B, Blanch P, et al. Do differences in muscle recruitment between novice and elite cyclist reflect different movement patterns or less skilled muscle recruitment? J Sci Med Sport. 2009;12(1):31-34.
51 Weppler CH, Magnusson SP. Increasing muscle extensibility: a matter of increasing length or modifying sensation? Phys Ther. 2010;90:438-449.
52 Wang K, McCarter R, Wright J, et al. Regulation of skeletal muscle stiffness and elasticity by titin isoforms: a test of the segmental extension model of resting tension. Biophysics. 1991;88:7101-7105.
53 Labeit S, Kolmerer B. Titins: giant proteins in charge of muscle ultrastructure and elasticity. Science. 1995;270:293-296.
54 Chleboun GS, Howell JN, Conatser RR, et al. The relationship between elbow flexor volume and angular stiffness at the elbow. Clin Biomech. 1997;12(6):383.
55 Boakes JL, Foran J, Ward SR, et al. Case reports: muscle adaptation by serial sarcomere addition 1 year after femoral lengthening. Clin Orthop Rel Res. 2007;456:250-253.
56 Williams P, Goldspink G. Changes in sarcomere length and physiological properties in immobilized muscle. J Anat. 1978;127:459-468.
57 Lynn R, Talbot JA, Morgan DL. Differences in rat skeletal muscles after incline and decline running. J Appl Physiol. 1998;85:98.
58 Gajdosik RL. Passive extensibility of skeletal muscle: review of the literature with clinical implications. Clin Biomech. 2001;16:87.
59 Lieber RL, ed 3. Philadelphia: Lippincott Williams & Wilkins. 2010.
60 Kendall FP, McCreary EK, Provance PG, et al. Muscles testing and function with posture and pain, ed 5. Baltimore: Lippincott Williams & Wilkins; 2005.
61 Kaito T, Hosono N, Mukai Y, et al. Induction of early degeneration of the adjacent segment after posterior lumbar interbody fusion by excessive distraction of lumbar disc space. J Neurosurg Spine. 2010;12(6):671.
62 McGill S, ed 2. Waterloo, Ontario: Wabuno Publishers, Backfitpro Inc. 2004.
63 Marras WS. The case for cumulative trauma in low back disorders. Spine J. 2003;3:177.
64 Becker A. Chronic low back pain associated with high health care costs. Spine. 2010;35(18):1714.