Chapter 7 Movement System Syndromes of the Knee
Introduction
Common knee pain problems seen by physical therapists include overuse injuries, such as patellofemoral pain syndrome (PFPS); traumatic injuries, such as anterior cruciate ligament (ACL) tears; and degenerative conditions, such as osteoarthritis (OA). Treatment directed at the identified source, such as soft tissue injury, may be useful after injury to reduce pain and return to function, however may not address the cause or contributing factors of the condition. One of the proposed contributing factors to injury is abnormal movement patterns or movement impairments. There is growing support that movement impairments may contribute to knee problems such as PFPS,1-3 iliotibial band (ITB) friction syndrome,4-5 ACL tears,6 and OA.7,8 In addition, studies have shown that addressing movement impairments can improve symptoms, enhance patient function after injury,9-12 and prevent future injury.13,14
In this chapter, we will focus on the syndromes and treatment of movement impairments proposed to contribute to mechanical knee pain and injury. The diagnosis of acute, traumatic injuries, such as ligamentous and meniscal tears is described in Chapter 2. The treatment of acute, traumatic injuries is not discussed in detail here because many excellent sources are available to describe the rehabilitation of these conditions.* The syndromes described in this chapter will, however, assist the therapist in identifying possible underlying movement impairments present during the early stages of rehabilitation.
* Suggested Readings:
Movement system syndromes (MSS) are influenced by a variety of factors that are important to consider during examination and treatment. Factors to consider are intrinsic characteristics, such as age, gender, and structural variations, and extrinsic characteristics, such as work or sport activity and work environment. For each patient, the examiner must consider the contribution of individual factors, as well as the possible interaction of these factors. OA provides an example of how multiple factors may contribute to the progression of a musculoskeletal problem. Increased age,15 high body mass,15-17 structural alignment,8,18 knee laxity,19,20 and participation in activities that involve deep knee flexion21 have all been shown to increase the risk of knee OA or the progression of knee OA. The interaction of these factors may further compound the risk. For example, Sharma et al16 found a positive relationship between body mass index (BMI) and the severity of radiographic OA in the varus-aligned knee. How quickly a joint degenerates or an injury occurs is likely determined by the interaction of multiple factors specific to the individual. These factors must be taken into account during the treatment of knee pain problems.
The relationship of the knee to the entire lower quarter should be considered when evaluating individuals with knee pain problems. The knee is the interface between the ankle/foot complex and the hip and is often affected by these neighboring joints. Many muscles crossing the knee joint also cross either the hip or the ankle/foot. Thus alignment faults, structural variations, or movement impairments at the hip or ankle/foot may result in altered stresses at the knee. For example, excessive femoral adduction while performing sit-to-stand may result in increased knee valgus, which is an alignment that has been associated with knee pain and knee injury.3-5
Based on the theory of relative stiffness/flexibility, as described in Chapter 1, the body takes the path of least resistance when completing a task. An illustration of relative stiffness/flexibility between the knee and the hip may be seen in a ballet dancer who has a limitation in hip lateral rotation as the result of structural femoral anteversion. To achieve sufficient turn out for first position, the dancer demonstrates lateral rotation of the tibia to compensate for the lack of hip lateral rotation. The tibiofemoral joint is less stiff than the hip and therefore moves into lateral rotation more easily (Figure 7-1). With continued practice of first position using compensatory rotation of the tibia, the knee undergoes repeated mechanical stresses that accumulate over time, resulting in microtrauma and potentially macrotrauma or injury.
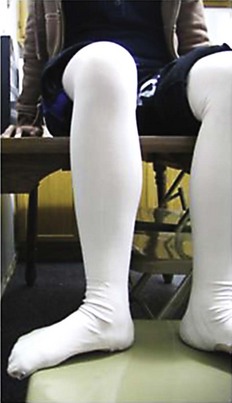
Figure 7-1 Excessive tibial lateral rotation. Ballet dancer in sitting position demonstrating excessive tibial lateral rotation. Excessive tibial lateral rotation may be the consequence of limited hip lateral rotation.
Relative stiffness/flexibility may also occur between a muscle and a joint. The tibiofemoral joint may be relatively less stiff than the tensor fasciae latae-iliotibial band (TFL-ITB). The relative stiffness/flexibility of the TFL-ITB can be observed during the two-joint hip flexor length. If the structures surrounding the tibiofemoral joint do not provide sufficient passive stiffness to stabilize the joint and the TFL-ITB does not easily stretch because of stiffness or shortness, lateral rotation of the tibia may be observed. In a sprinter, this relative stiffness/flexibility could result in repetitive tibial lateral rotation each time the limb initiates swing phase, the position in which the TFL-ITB should be in its most lengthened position. The stresses of repetitive rotation at the tibiofemoral joint may eventually lead to a knee pain problem.
Using the MSS concepts, a standardized examination22 is performed to determine the movement system syndrome and identify the factors contributing to the syndrome. The movement system syndrome is named for the direction of motion that is associated with an increase in the patient’s pain. For example, if the patient reports an increase in symptoms during the primary test of a single-leg squat and demonstrates femoral adduction with knee valgus, then tibiofemoral rotation with valgus (TFRVal) is suspected as the movement impairment. To confirm that TFRVal is associated with the pain complaint, the patient is asked to perform a secondary test by repeating the task while controlling the femoral adduction and knee valgus and keeping the knee aligned properly. If the patient reports a decrease in pain during the secondary test compared to the primary test, the movement system diagnosis of TFRVal is supported. Further substantiation of the diagnosis occurs if the examiner finds that the patient demonstrates the same direction of motion during multiple test items.
Specific to the knee, the movement system syndrome may not be obvious from the standard examination and basic functional activities. This is particularly true in high-level athletes because their impairments and/or symptoms may not be revealed until the knee is physically taxed with higher level activities. Therefore sport-specific or work-specific tasks may need to be assessed. Examples include running, jumping, and landing from a jump. In addition, the specific activity that the patient reports as most problematic should be assessed. Using the concepts of the MSS examination, primary and secondary tests of the higher level activities can be performed to confirm the suspected movement system diagnosis.
Once the movement system syndrome is identified and the stage for rehabilitation is determined, treatment can be provided. Treatment emphasis is on educating the patient in how to restore precise movement during all functional and athletic activities. Therapeutic exercise is also prescribed to address physical impairments, such as poor muscle performance or reduced muscle extensibility, thought to contribute to the movement system syndrome. Traditionally, the focus of rehabilitation of the knee has been placed on strengthening of the thigh musculature in the sagittal plane (quadriceps and hamstrings) with little regard to the influence of transverse or coronal plane motion at the tibiofemoral joint. We have found, however, that many knee pain problems, including PFPS and OA are treated effectively by addressing movement impairments related to excessive rotation or varus/valgus at the tibiofemoral joint. In addition, fitness activities are encouraged; however, modifications may need to be provided during the early stages of rehabilitation.
This chapter describes the normal alignment and movement of the knee and the actions of the surrounding musculature, as well as the structural and acquired faults that affect the knee and must be considered as part of the overall assessment. Finally, the proposed movement system syndrome of the knee and specific treatment recommendations associated with each syndrome are described (Table 7-1). Case examples are used to illustrate the major points.
TABLE 7-1 Movement System Syndromes of the Knee
| Symptom | Source of Pain | Treatment |
|---|---|---|
| TIBIOFEMORAL ROTATION (TFR) WITH VALGUS (TFRVAL) OR TFR WITH VARUS (TFRVAR) SYNDROME | ||
| Impaired motion at the tibiofemoral joint, transverse or frontal plane | ||
| TIBIOFEMORAL HYPOMOBILITY (TFHYPO) SYNDROME | ||
| Physiologic loss of ROM | ||
|
In patients with OA:
Caution should be taken to avoid excessive strengthening of quadriceps and hamstrings in patients with malalignment or laxity in the knee20
|
||
| KNEE EXTENSION (KEXT) SYNDROME AND KEXT SYNDROME WITH PATELLAR SUPERIOR GLIDE (KEXTSG) SYNDROME | ||
| Associated with dominance or shortness/stiffness of quadriceps muscle | ||
| KNEE HYPEREXTENSION (KHEXT) SYNDROME | ||
| Associated with dominance of hamstrings | ||
| PATELLAR LATERAL GLIDE (PLG) SYNDROME | ||
| Impaired alignment or tracking of the patella in the trochlear groove | ||
| TIBIOFEMORAL ACCESSORY HYPERMOBILITY (TFAH) SYNDROME | ||
| Excessive motion at the tibiofemoral joint | ||
| KNEE IMPAIRMENT | ||
| No movement system syndrome identified or unable to perform a movement examination as occurs in cases of acute trauma or post-surgery | ||
| Any structure of the knee associated with trauma or surgery | ||
ACL, Anterior cruciate ligament; ITB, iliotibial band; LR, lateral rotation; MR, medial rotation; NWB, non–weight-bearing; OA, osteoarthritis; PCL, posterior cruciate ligament; ROM, range of motion; TFL, tensor fascia latae; WB, weight-bearing.
Modified from Harris-Hayes M, Sahrmann SA, Norton BJ, et al: Diagnosis and management of a patient with knee pain using the movement system impairment classification system, J Orthop Sports Phys Ther 38(4):203-213, 2008.
Alignment of the Knee
The alignment of the entire lower extremity, including the hip, knee, ankle, and foot must be considered when assessing an individual with knee pain. Alignment of the knee is discussed in detail, and alignment of the hip and the ankle and foot is referred to briefly. Additional information on the ankle and foot can be found in Chapter 8, and additional information on the hip can be found in Sahrmann.22
When assessing alignment, one must consider the possibility of structural impairments and distinguish structural from acquired impairments. Structural impairments are related to bony structure and cannot be corrected with training or exercise. Acquired impairments are often the result of postural habits and can be changed with training. Examples of structural impairments that affect the knee include femoral or acetabular anteversion or retroversion, genu valgus or varus, tibial varum, tibial torsion, and a rigid supinated foot. Although structural impairments cannot be changed or corrected, exercises and activities may need to be modified to accommodate the structural impairment. For example, if an individual’s hip lateral rotation is limited by femoral anteversion, the patient should be encouraged not to force hip lateral rotation during posterior gluteus medius strengthening.22 The patient should also be educated about the problems that can occur if he or she participates in activities that require excessive hip lateral rotation, such as ballet, because compensations often occur at other joints such as the knee. In addition, the patient should be instructed to avoid excessive lateral rotation of the hip during all functional activities such as sitting on the floor in the tailor position or stretching during dance warm-ups.
Normal Alignment
Sagittal Plane
Alignment of the lower extremity in the sagittal plane is viewed from the lateral aspect of the individual. The tibia and femur should be aligned vertically with the knee angle at approximately 0 degrees of flexion/extension (Figure 7-2). The angle of the hip joint, measured by a line bisecting the pelvis and a line bisecting the femur, should be 0 degrees in normal alignment. The ankle should be in a neutral position, with 0 degrees of dorsiflexion in relaxed standing.
Impairments
Genu recurvatum or knee hyperextension, defined as knee extension greater than 5 degrees, is commonly observed in children or young adults (Figure 7-3). Genu recurvatum may lead to many other impairments, including tibial bowing in the frontal or sagittal plane, altered compressive forces at the tibiofemoral joint, functional weakness of the quadriceps and gluteus maximus along with possible overrecruitment of the hamstrings, and posterior capsule stretching with ligamentous laxity.22-24 The knee may appear hyperextended when there is significant posterior bowing of the tibia in the sagittal plane.22 Standing with the knees in flexion is most typically seen in older individuals with end-stage OA or individuals with an acute injury (Figure 7-4).
Alignment of the knee may be related to alignment deviations of the hip and ankle. For example, knee hyperextension is often associated with posterior pelvic tilt, hip extension, and ankle plantarflexion.22,23 Knee flexion is often present with anterior pelvic tilt, hip flexion, and ankle dorsiflexion.
Frontal Plane
Normal Alignment
Frontal plane alignment is viewed from the anterior and posterior aspect. The femoral shaft angles medially as a result of the angle of inclination of the proximal femur. The long axis of the femur diverges about 10 degrees from the long axis of the tibia, therefore knee alignment in the frontal plane is a physiologic valgus angle of 170 to 175 degrees in the adult (Figure 7-5).25,26

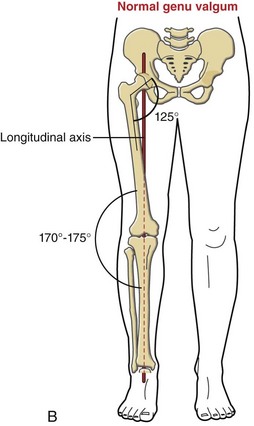
Figure 7-5 A and B, Normal physiologic valgus. The normal 125-degree angle of inclination of the proximal femur and the longitudinal axis of rotation throughout the entire lower extremity are also shown.
(B, From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
The amount of physiologic valgus changes with normal aging in children. Newborns demonstrate genu varum until about 20 months. Then the angle progresses toward valgus and peaks at approximately 168 degrees when the child reaches about 3 years.27 The valgus then gradually decreases and reaches the adult value of approximately 170 to 175 degrees by age 6.25,27,28
Impairments
If the described angle is less than 170 degrees, it is considered genu valgum (Figure 7-6), and if the angle is greater than 180 degrees, it is considered genu varum (Figure 7-7).25 Genu valgum may place excessive tensile stresses or strain on the structures on the medial side of the knee and compressive forces on the lateral compartment of the knee. Genu varum may place excessive tensile stresses or strain on the structures on the lateral side of the knee and compressive forces on the medial compartment of the knee. In the young adult, genu varum appears to be more common in men than women.

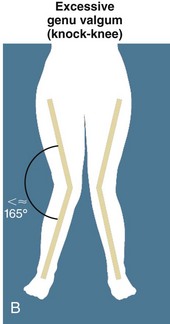
Figure 7-6 A and B, Genu valgum. Excessive frontal plane deviations.
(B, From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)

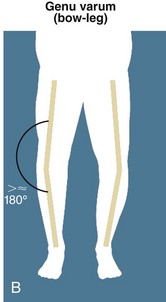
Figure 7-7 A and B, Genu varum. Excessive frontal plane deviations.
(B, From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
Malalignment of the tibiofemoral joint in the frontal plane has been associated with osteoarthritis and functional limitations. People with knee OA and a varus or valgus alignment impairment have an increased risk of progression of tibiofemoral OA8,18,20 and patellofemoral OA.29-31 In addition, an alignment change of 5 degrees in the frontal plane is associated with decreased ability to perform sit-to-stand and increased pain in people with knee OA.18 Alignment impairments may also be associated with compartment-specific OA, such as genu varum with medial compartment OA, and genu valgum with lateral compartment OA, which is discussed in detail in the “Tibiofemoral Rotation Syndrome” section.32
The structure of the tibia and femur should be considered when assessing frontal plane alignment. Tibial varum is present if the distal one third of the tibia deviates medially from a vertical reference line. Tibial varum has more commonly been measured from the posterior view in resting calcaneal stance with average amounts ranging from 4.6 degrees to 8.3 degrees.33,34 Our preference is to observe and measure tibial varum from the anterior view because the tibial shaft is more visible and palpable. Keeping in mind the norms stated above, a reasonable criterion for excessive tibial varum would be a deviation greater than 10 degrees (Figure 7-8). Tibial varum is often associated with subtalar joint pronation,33,34 although we have seen it occur with a supinated foot. Tibial varum is more commonly observed with genu varum than genu valgum.

Figure 7-8 Tibial varum. A line representing the tibial shaft deviates from a vertical reference line greater than 10 degrees.
The structure of the femur may also be associated with genu valgum and varum; however, studies to confirm this have not been reported. Coxa varum, an angle of inclination at the hip that is notably less than 125 degrees,26 may contribute to a genu valgum. Coxa valgum, an angle of inclination at the hip that is notably greater than 125 degrees,26 may contribute to a genu varum through excessive loading on the medial knee compartment that leads to a loss of medial knee joint space.
Transverse Plane
Normal Alignment
Transverse plane alignment is observed from the anterior and posterior aspects. General assessment of the entire lower extremity should be performed, followed by a more specific assessment of each region, such as the hip or knee. Rotation of the femur is assessed from the posterior view, using the vertical creases that represent the border of the hamstrings and comparing the medial crease to the lateral crease. The distance of the vertical creases should be equal from the medial and lateral aspects of the knee, respectively. Another method would be to palpate the medial and lateral epicondyles and assess the direction of the plane that they are facing (e.g., more medially or more laterally compared to the sagittal plane). The anterior view can also be used to assess for consistency; however, an impaired alignment of the patella can be misleading. See Chapter 8 for a discussion of normal alignment of the foot and ankle in the transverse plane.
Impairments
Femoral medial rotation is a common alignment impairment observed in patients with knee pain (Figure 7-9). When femoral medial rotation is noted in standing alignment, the possibility of a structural femoral anteversion should also be considered and determined with further examination.22 The appearance of femoral medial rotation may also suggest poor performance of the hip lateral rotators or reduced extensibility of the TFL-ITB. These muscle properties can be assessed with further testing.

Figure 7-9 Femoral medial rotation. Note the medial and lateral hamstring creases are not an equal distance from the medial and lateral aspects of the knee, respectively. In fact, on the right lower extremity, the lateral hamstring is barely visible.
When the foot is directed laterally during stance, it may be the result of an acquired postural impairment, such as femoral lateral rotation, or a structural impairment, such as femoral retroversion, tibial external torsion, or foot deformity. The location of the impairment should be assessed (e.g., femur or tibia) and to determine if the impairment is acquired or structural so that treatment may be adjusted accordingly.
Tibial torsion is described as a rotation of the tibial shaft. Although we have observed individuals with internal tibial torsion, external tibial torsion is much more common. External tibial torsion is demonstrated when the distal tibia is rotated in the lateral direction greater than 20 to 40 degrees35-37 compared to the proximal tibia (Figure 7-10). External tibial torsion may be a compensation that develops when femoral anteversion is present and the individual attempts to correct a toe-in alignment. When external tibial torsion is determined to be present, the position of the foot should not be corrected. Trying to align the foot straight ahead will compromise the normal alignment of the ankle/foot and affect the ability of the individual to dorsiflex the ankle.22 Attempting this correction could also affect the knee by imposing medial rotation of the tibia on the femur.

Figure 7-10 Tibial torsion on the right. Note position of the foot relative to the knee. The femur appears to be in medial rotation. However, the foot is laterally deviated, which leads the clinician to suspect torsion or tibial lateral rotation. The specific test for tibial torsion should then be performed.
Alignment of the Patellofemoral Joint
Normal Alignment
Patellar alignment may be viewed anteriorly. In the frontal plane, the patella should be centered in the trochlear groove, although imaging has suggested a slight lateral deviation.27 In the sagittal plane, patellar alignment is represented by a Insall-Salvati ratio.38 The Insall-Salvati ratio is the ratio of the patellar tendon length compared to the patellar height with the knee in 60 degrees of flexion. A normal Insall-Salvati ratio is 1±0.2. Although an estimate may be made clinically, measurements are best determined by lateral radiographs.
Impairments
Impaired patellar alignment may lead to abnormal stresses on the patellofemoral joint and surrounding soft tissues that with time may lead to peripatellar pain. The most common alignment impairments of the patella are excessive lateral or excessive superior displacement. Poor performance of the vastus medialis oblique (VMO) muscle and a short, stiff TFL-ITB are thought to contribute to lateral patellar displacement;39 however, there is limited research to demonstrate this correlation.
By definition, lateral patellar tilt is present when the lateral patellar border is posterior to the medial patellar border and the lateral border cannot be elevated in the anterior direction.40 The observation of lateral patellar tilt has been shown to be associated with a lateral patellar tilt angle greater than 10 degrees when measured by magnetic resonance imaging (MRI). Further study is needed, however, to assess the association of lateral patellar tilt and the presence of pain.
Excessive superior patellar displacement, also known as patella alta, is represented by an Insall-Salvati ratio greater than or equal to 1.2. The superior patellar displacement may indicate that the quadriceps are relatively more stiff than the patellar tendon. This relationship is detailed in the “Knee Extension Syndrome” section. Patella baja, or excessive inferior patellar displacement, has an Insall-Salvati ratio less than or equal to 0.8. Patella baja may be observed as a complication after surgical procedures such as ACL reconstruction, which may be related to the scarring down of the patellar tendon after a surgical procedure.
Although patellar malalignment is believed to be a contributing factor to various knee pain problems, the clinical assessment of patellar alignment is unreliable.41 Therefore the entire clinical picture must be considered.
Motions of the Knee Joint
Sagittal Plane
Knee Flexion and Extension
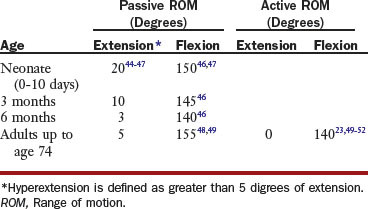
In the sagittal plane, the tibiofemoral joint flexes and extends about a medial-lateral axis passing transversely through the femoral condyles. The axis of rotation does not remain in one location but instead shifts and forms an evolute during the movement. The range of motion (ROM) available varies with age (Table 7-2). Passive ROM (PROM) at the tibiofemoral joint does not change significantly during the adult years42,43; however, reduced extensibility of the rectus femoris and hamstring muscles has been shown to significantly contribute to joint limitations in the older individual.43
Frontal Plane
In the frontal plane, the tibiofemoral joint abducts and adducts around an anterior to posterior axis. Normal values for tibial adduction and abduction relative to femur are highly variable, with reported mean total values ranging from 2 to 14 degrees.53-57 There is less motion available when the knee is extended, with only 2 to 6 degrees of total abduction and adduction,53,54 compared to when the knee is flexed, and motion can increase to 14 degrees.53-57 Abduction and adduction is typically a passive motion that occurs during activities such as gait.
Transverse Plane
In the transverse plane, the tibiofemoral joint rotates around a vertical axis located approximately at the intercondylar eminence.58 An individual is expected to have approximately twice the amount of lateral rotation as medial rotation.59 Reported values for tibiofemoral rotation ROM are highly variable because of the various methods used to assess tibiofemoral rotation. With the knee flexed to 90 degrees, total rotation ROM is between 25 to 57 degrees.53,59-63 With the knee fully extended, there is essentially no rotation available due to the passive tension of the surrounding ligaments.
During either tibial-on-femoral knee extension or femoral-on-tibial knee extension, conjunct rotation occurs; this is termed the screw-home mechanism. This passive rotary-locking mechanism results in approximately 10 degrees of tibial lateral rotation relative to the femur. The major contributing factor to the screw-home mechanism is the shape of the medial femoral condyle that curves approximately 30 degrees laterally, helping to direct the tibia toward its locked position in lateral rotation.26
Motion of the Patellofemoral Joint
In knee extension, the patella is slightly laterally displaced. With flexion from 0 to 30 degrees, it glides inferiorly and medially. As the knee flexes greater than 30 degrees, the patella continues to glide inferiorly, but changes to a lateral glide.64,65 During extension from a flexed position, the patellar motion is the reverse of flexion. These motions are so small that they are hardly noticeable to the observer when motion is normal. Tilting and rotation are also reported to occur in the patella. However, there is no consensus in the amount of patellar motion and the reliability in evaluation of position and movement is limited.
Knee Motion During Gait
Sagittal Plane
At initial contact (heel strike), the knee flexes 5 degrees, then continues to flex to 10 to 15 degrees during the initial 15% of the gait cycle. During this time, the quadriceps are working eccentrically to provide shock absorption as the body weight is transferred to the limb. The knee reaches almost full knee extension just before heel off, and at heel off, it begins to flex again. Approximately 35 degrees of knee flexion should be noted at toe off and about 60 degrees (maximum flexion) is seen at midswing.66 The knee then extends again to almost full knee extension just before initial contact. Children demonstrate a similar pattern; however, they tend to walk with more knee flexion. They do not get as much extension as adults during midstance or before initial contact.67,68
Frontal Plane
Minimal tibial abduction/adduction may be noted during the gait cycle with a maximum of 5 degrees.25,69
Transverse Plane
Generally, during gait, the tibia medially rotates from heel strike until 20 percent of gait cycle (just before midstance). The tibia then laterally rotates until toe off and medially rotates through swing.25,69 Normal rotation between the tibia and femur during the gait cycle should be approximately 8 to 9 degrees.25,69 At initial contact, the tibia is laterally rotated about 2 to 3 degrees relative to the femur. From initial contact through midstance, the tibia is medially rotated more than the femur, approaching 5 degrees of tibial medial rotation compared with the femur. During swing, the tibia is laterally rotated relative to the femur.
Knee Motion During Running
Knee motion during running is similar to walking; however, the knee is relatively more flexed throughout the cycle.66 On heel strike, the stance knee flexes up to 45 degrees as the quadriceps work eccentrically to aid shock absorption. The knee then extends during stance; however, it never reaches full extension. At midstance, the knee remains flexed approximately 25 degrees. Maximum knee flexion of 90 degrees occurs during swing phase. A similar pattern of knee motion occurs with all speeds of running; however, as speed increases, the amount of knee flexion during swing increases as high as 130 degrees.
Muscle Actions of the Knee
Extensors
The quadriceps muscle is the primary extensor of the knee joint and consists of four muscles: vastus intermedius, vastus lateralis, vastus medialis, and rectus femoris (Figure 7-11). The rectus femoris is the only one of these muscles that crosses both the hip and knee, allowing it to also act as a hip flexor.

Figure 7-11 Quadricep muscles. The quadriceps can be seen here including the reflected rectus femoris (the only two joint muscle of the quadriceps), along with the vastus lateralis, vastus intermedius and vastus medialis.
(From Drake RL, Vogl AW, Mitchell AWM: Gray’s anatomy for students, ed 2, Baltimore, 2009, Churchill Livingstone.)
The quadriceps angle, or Q-angle, represents the line of the resultant force of the quadriceps that tends to pull the patella superiorly and laterally relative to the patellar ligament. The Q-angle is represented by the angle between a line connecting the anterior superior iliac spine (ASIS) to the midpoint of the patella and a line connecting the tibial tubercle to the midpoint of the patella (Figure 7-12). The normal values for Q-angle are less than 10 degrees in men25,51,70 and less than 15 degrees in women.25,51,70 A Q-angle larger than normal is proposed to create excessive lateral forces on the patella through a bowstring effect that may predispose the patella to pathological changes. Q-angle can be influenced by excessive femoral anteversion, genu recurvatum, ankle/foot pronation, lateral tibial rotation, genu valgus, patellar alignment, and tibial tubercle anomalies.2,70,71 The Q-angle should not be confused with the physiologic valgus of the knee.
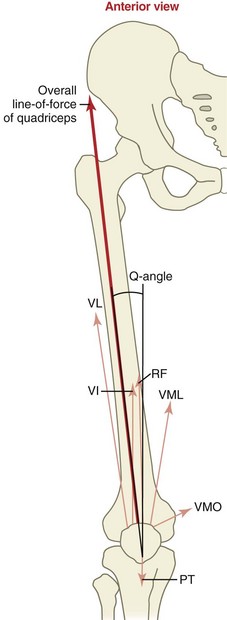
Figure 7-12 Q-angle. The overall line-of-force of the quadriceps is shown as well as the separate line-of-force of the muscles within the quadriceps. The vastus medialis is divided into its two predominant fiber groups: the obliquus and the longus. The net lateral pull exerted on the patella by the quadriceps is indicated by the Q-angle. PT, Patellar tendon; RF, rectus femoris; VI, vastus intermedius; VL, vastus lateralis; VML, vastus medialis (“longus”); VMO, vastus medialis (“obliquus”).
(From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
Quadriceps muscle impairments related to knee pain may include poor performance or overrecruitment. As mentioned previously, the oblique portion of the vastus medialis (VMO) may provide an important restraint to lateral patellar displacement given the angulation of the fibers that attach to the patella. Poor performance of the VMO may contribute to excessive lateral patellar displacement.39
With intensive physical training or loading through weight training or sports, the quadriceps may become relatively too stiff or short and contribute to excessive stress on the patella, patellar ligament, or tibial tubercle. This excessive pull superiorly may be associated with patella alta. In contrast, the quadriceps can become functionally weak when habitual alignment of knee hyperextension is present.
The articularis genus is a small muscle located on the anterior distal femur that inserts into the synovial membrane of the knee joint. As the knee is extended, it assists in drawing the synovial membrane upward and preventing folds of the membrane from becoming compressed within the knee joint.
Flexors
The hamstring muscles are comprised of the semimembranosus and semitendinosus muscles medially and the biceps femoris muscle laterally (see Figure 7-16). Their primary actions include knee flexion and hip extension; however, they also assist with hip medial and lateral rotation and may contribute to tibial medial and lateral rotation. The hamstrings are at risk of overuse when synergists, such as the gluteus maximus, are underused.22 For example, when the foot is fixed on the ground, the hamstrings can extend the knee by pulling the knee back to the body through its action as a hip extensor. Usually, when hamstring dominance such as this occurs, the quadriceps and gluteus maximus are not performing optimally. This movement impairment is commonly seen in individuals with a swayback alignment22 and genu recurvatum.
Movement impairments in the transverse plane may be the result of impaired hamstrings. The medial hamstrings assist in medial rotation of the hip and can become dominant and shorter in length compared to the biceps femoris. This imbalance in synergists is seen when an individual maintains excessive hip medial rotation or participates in sports or activities that tend to position or encourage hip medial rotation such as cycling. The biceps femoris assists in lateral rotation of the femur and lateral rotation of the tibia. When the primary hip lateral rotators are not performing optimally, the biceps femoris may compensate by increasing its action in an attempt to control hip lateral rotation.22 The overuse of the biceps in this way may lead to a muscle strain. The biceps femoris may also contribute to lateral rotation or posterolateral displacement of the lower leg relative to the femur, given its distal attachment to the fibular head. A patient case demonstrating this phenomena is provided by Sahrmann.22
The sartorius muscle flexes, abducts, and laterally rotates the hip and also flexes the knee and rotates it medially. The gracilis acts primarily to adduct the hip and also flexes and medially rotates the knee. Both muscles insert below the medial tibial condyle into the pes anserinus along with the semitendinosus tendon. The pes anserinus insertion may become injured with excessive tibial lateral rotation contributing to medial knee pain.
The gastrocnemius and soleus muscles are powerful ankle plantarflexors; however, the gastrocnemius is also a knee flexor (Figure 7-13). The plantaris also assists with ankle plantarflexion and knee flexion. The gastrocnemius and soleus are described in more detail in Chapter 8. Impairments in length and strength of the gastrocnemius are fairly common. Related to the knee, individuals who stand in knee hyperextension tend to develop shortness of the gastrocnemius as a result of the alignment of relative plantarflexion. In movement impairments of the knee, poor performance of the ankle plantarflexors may be observed as a lack of push-off during gait, a delayed heel rise, or excessive dorsiflexion during foot flat.
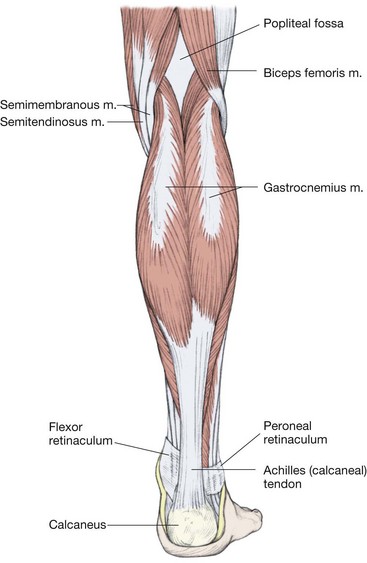
Figure 7-13 Posterior muscles of the lower leg. The gastrocnemius is cut to allow visualization of the soleus muscle.
(From Mathers, et al: Clinical anatomy principles, St Louis, 1996, Mosby.)
The popliteus muscle is a knee flexor and tibial medial rotator (see Figure 7-13). The popliteus is also known as the key to the knee, because it “unlocks” the knee as it moves from the fully extended (locked) position into flexion. The popliteus unlocks the knee either by medially rotating the tibia in a non–weight-bearing activity or laterally rotating the femur in a weight-bearing activity. The popliteus is mostly active during crouching and may help the posterior cruciate ligament (PCL) prevent anterior dislocation of the femur.23,26
Other Important Hip Muscles That Can Affect the Knee
Lateral Rotators of the Hip
The primary hip lateral rotators include the deep (sometimes referred to as short or intrinsic) lateral rotators and the gluteus maximus. The intrinsic or deep lateral rotators of the hip include the piriformis, gemellus superior and inferior, obturator internus and externus, and quadratus femoris muscles (Figure 7-14). The obturator externus, however, is generally considered a secondary lateral rotator of the hip because its line of force is so close to the longitudinal axis of rotation when the hip is in the anatomical position. As primary lateral rotators of the hip, the deep lateral rotators serve to provide precise control of rotation of the femoral head in the acetabulum, thus maintaining the integrity and stability of the hip similar to the way that the rotator cuff muscles provide control of the humeral head in the glenoid. In patients with knee pain syndromes, these muscles often become lengthened and weak, thus losing the precise control of the hip and allowing hip medial rotation to occur.
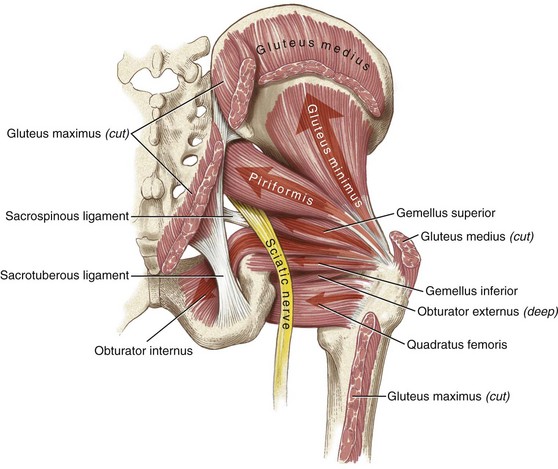
Figure 7-14 Hip lateral rotators. Some of the deep lateral rotators of the hip are depicted here—obturator internus, obturator externus and piriformis. They help to maintain control and stability of the hip joint. When lengthened or weak, they can contribute to femoral medial rotation and knee pain.
(From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
In addition to being a primary lateral rotator, the gluteus maximus muscle is also a primary hip extensor (Figures 7-15 and 7-16). Individuals who stand in a swayback alignment commonly have atrophy of the gluteus maximus because their weight line is posterior to their center of mass.22,23 In these cases, when the gluteus maximus becomes functionally weak, the hamstrings may become the dominant hip extensors instead of the gluteus maximus.

Figure 7-15 Gluteus maximus and tensor fasciae latae–iliotibial band. The TFL-ITB is a major contributor to impairments of the lower extremity. When it is too short or too dominant, it often contributes to femoral medial rotation. Also, the attachment of the TFL-ITB to the patella and the lateral tibial tuberosity may result in impairments of the patella and lateral rotation of the tibia. From this figure, also note the large contribution of the gluteus maximus into the ITB.
(From Mathers LH, Chase RA, Dolph J, et al: Clinical anatomy principles, St Louis, 1996, Mosby.)
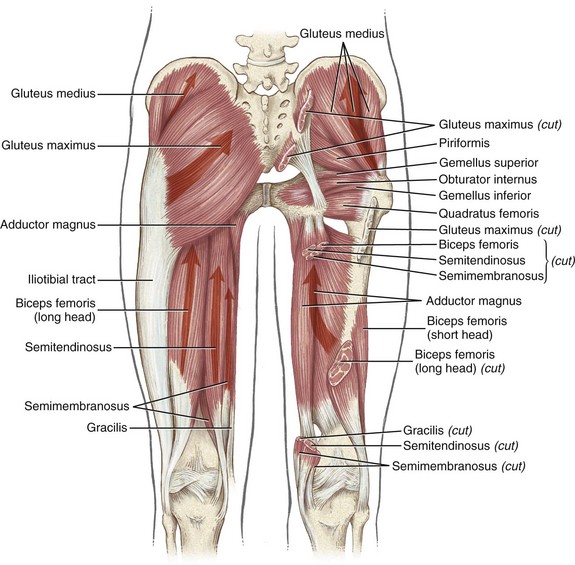
Figure 7-16 The posterior muscles of the hip. The left side highlights the gluteus maximus and hamstring muscles (long head of the biceps femoris, semitendinosus, and semimembranosus). The right side highlights the gluteus medius and five of the six short external rotators, i.e., piriformis, gemellus superior and inferior, obturator internus, and quadratus femoris.
(From Neuman DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
A large portion of the gluteus maximus muscle attaches into the ITB. Therefore shortness or stiffness of the gluteus maximus can contribute to relative stiffness/flexibility issues involving the ITB. Relative stiffness/flexibility as a result of shortness or stiffness of the gluteus maximus through the ITB seems to be more common in males than females and should be suspected if the patient sits in excessive hip abduction.
The secondary lateral rotators of the hip include the sartorius, the biceps femoris, and the posterior fibers of the gluteus minimus and medius (Figure 7-16). The posterior gluteus medius acts to abduct, extend, and laterally rotate the hip. The length and strength of the posterior gluteus medius is often affected by postural changes at the pelvis and hip. If an individual stands with the right iliac crest higher than the left or with the right hip in medial rotation, the posterior gluteus medius on the right may be lengthened and possibly weak, particularly if tested in the shortened position. Poor performance of this muscle is often a key factor in knee pain problems.
Because control of the knee is needed throughout the range of hip flexion to hip extension in activities such as sit to stand and cutting, the muscle performance of the hip lateral rotators should be tested with the hip flexed and with the hip extended. A number of the hip lateral rotators change their action when the hip is flexed. Although they are hip lateral rotators when the hip is in 0 degrees of flexion, the piriformis and portions of the gluteal muscles change to medial rotators of the femur as the hip is flexed to 90 degrees. This switch in action is due to a change in the location of the muscles’ moment arms relative to the axis of rotation.72,73 Once identified, muscle performance deficits can then be targeted with specific exercises, with the hip flexed or hip extended. Given their likely role in providing stability of the hip, specific attention to the deep lateral rotators (hip flexed position) is warranted.
Medial Rotators of the Hip
The TFL-ITB is a two-joint muscle complex that flexes, abducts, and medially rotates the hip and laterally rotates the tibia through its insertion onto the lateral tibial tubercle (see Figure 7-15). The TFL-ITB also assists in stabilizing the knee when the knee is extended, although it does not actively extend the knee.23,26 When the TFL-ITB becomes short or too stiff, it can cause a compensatory motion such as lateral tibial rotation or valgus at the knee. The TFL-ITB can also contribute to patellar lateral glide as a result of its insertion onto the lateral patella.22
The anterior fibers of the gluteus medius abduct, flex, and medially rotate the hip. Because the anterior fibers of the gluteus medius tend to be stronger than the posterior fibers, the imbalance often results in excessive medial rotation. The anterior gluteus minimus also abducts, flexes, and medially rotates the hip, contributing further to the potential for excessive medial rotation of the hip.22 When testing performance of the medial rotators of the hip, it is important to remember that muscle function may be increased when the hip is flexed, compared to when the hip is extended.72,73 When the hip is extended, there are no primary medial rotators of the hip.26
Movement System Syndromes of the Knee
Tibiofemoral Rotation Syndrome
Tibiofemoral rotation (TFR) syndrome is characterized by knee pain associated with impaired rotation of the tibiofemoral joint. Excessive rotation between the tibia and femur can be seen during tests of alignment, tests of movement, and performance of functional activities. There are two subcategories of TFR syndrome: TFR with valgus (TFRVal) syndrome and TFR with varus (TFRVar) syndrome. This text focuses on the most common TFR syndrome, TFRVal, and only briefly discusses TFRVar.
Symptoms and History
Individuals that have the diagnosis of TFR syndrome (with valgus or varus) report pain along the tibiofemoral joint line, the peripatellar regions, or at the insertion of the ITB. Pain is often associated with activities that contribute to rotation between the tibia and femur, including weight-bearing activities, such as walking and stair climbing, or non–weight-bearing activities, such as sitting with the lower leg placed in a rotated position relative to the femur. Individuals that demonstrate this movement fault may include ballet dancers, runners, equestrians, and sedentary workers. Those with OA who report instability74 are also likely to fall into the TFR category.
Tibiofemoral Rotation with Valgus Syndrome
Individuals with TFRVal syndrome demonstrate excessive medial rotation or adduction of the femur relative to the tibia, or excessive lateral rotation or abduction of the tibia relative to the femur resulting in knee valgus. This motion has also been described as medial collapse2,75 or poor dynamic knee stability.6,76 Clinically, it appears that females are more likely to demonstrate TFRVal than men, and this observation appears to be supported in the literature as well.76-78 Although it is more common in women, TFRVal syndrome may be present in males, thus the need to take an individualized approach to examination.
Symptoms and History
Structures that may be injured in an individual with TFRVal syndrome include structures of the tibiofemoral joint, the patellofemoral joint, the ITB, and surrounding musculature. A number of studies have demonstrated an association between the movement impairment associated with TFRVal syndrome and knee injury,1,4,6,79-84 highlighting the importance of assessing the entire lower extremity. In a prospective study, Hewett et al6 reported that during the landing phase of a jump, young women with a knee valgus angle greater than 8 degrees were more likely to suffer a noncontact ACL injury than those with an angle of less than 8 degrees (Figure 7-17). In addition, Hewett’s group demonstrated that the risk of ACL injury is reduced with training to correct the movement impairment.13,85
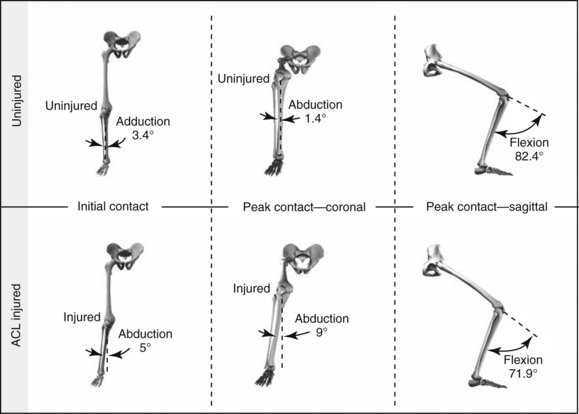
Figure 7-17 Biomechanical model depicting mean knee joint kinematics during the drop vertical jump at initial contact and maximal displacement in the ACL-injured and uninjured groups (n = 9 knees and n = 390 knees, respectively). Left, Coronal plane view of knee abduction angle at initial contact in the ACL-injured and uninjured groups. Center, Coronal plane view of maximum knee abduction angle in the ACL-injured and uninjured groups. Right, Sagittal plane view of maximum knee flexion angle in the ACL-injured and uninjured groups.
(From Hewett TE, Myer GD, Ford KR, et al: Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study, Am J Sports Med 33:492, 2005.)
Overuse syndromes, such as PFPS and ITB friction syndrome, have also been associated with TFRVal. Traditional treatment of PFPS has focused on the movement and alignment of the patella11,86,87; however, numerous studies have demonstrated that the alignment or movement of the tibia and femur may be associated with PFPS.1,3,81-84 Although repetitive knee extension-flexion has been implicated in ITB friction syndrome, a recent study demonstrated that increased hip adduction may contribute to the onset of ITB friction syndrome.4
An examination that includes the assessment of movement quality and tests of muscle length and muscle performance, in addition to tests to identify injured structures, is recommended. Key tests and signs of the movement examination are described in the following sections. Tests to assess specific knee structures, such as the ligaments or meniscus, are not the focus of this text; therefore the reader is encouraged to consult other available sources.*
Key Tests and Signs
Alignment Analysis
While the patient is standing, the examiner assesses the overall posture and specific alignment of the lower extremities. Alignment is often not predictive of the movement impairment; however, alignment may contribute to the movement impairment. From the posterior view, the patient may demonstrate medial rotation of the femur or lateral rotation of the tibia (Figure 7-18). The patient may also demonstrate knee valgus. From the lateral view, posterior pelvic tilt with hip extension and knee hyperextension might indicate poor performance of the gluteals. A lordotic posture might suggest short or stiff hip flexors and poor abdominal control. Excessive pronation or supination of the foot should also be noted.
Movement Impairments
Standing tests
Single-leg stance should be assessed by comparing both lower extremities. During single-leg stance on the involved limb, the patient will demonstrate excessive medial rotation of the involved femur. The patient may also demonstrate excessive ankle pronation. During single-leg stance on the uninvolved limb, tibial lateral rotation may be noted in the involved limb when the knee is flexed to 90 degrees (Figure 7-19). In addition to movement quality, the examiner may observe the patient’s ability to maintain balance when standing on one limb. Poor stability may indicate poor proprioception, which may be a contributor to the patient’s pain problem.


Figure 7-19 Single-leg stance observing the limb being flexed. Note the alignment of the foot. A, The left uninvolved foot is vertical relative to the floor. B, The right foot is angled away from the vertical indicating tibial lateral rotation.
During hip and knee flexion in stance (partial squat), the patient will demonstrate femoral (hip) adduction/medial rotation and knee valgus (Figure 7-20, A). This motion may increase or produce the patient’s symptoms. When the motion is corrected (Figure 7-20, B), the pain typically improves, supporting the diagnosis of TFRVal syndrome.


Figure 7-20 Hip and knee flexion in standing. A, Note the femoral adduction and medial rotation. There is minimal pronation at the foot, which may contribute to excessive stresses at the knee. B, Secondary test of hip and knee flexion in standing. The movement impairment of femoral adduction and medial rotation was corrected.
Supine tests
When performing the two-joint hip flexor length test,88 lateral rotation or abduction of the tibia may be observed when the involved limb is lowered into hip extension (Figure 7-21). If the patient reports pain during the test, the test is repeated with stabilization of the tibia to prevent the observed motion. If the patient’s symptoms are improved, then the movement impairment of TFR is supported. Further tests would be needed to determine if the diagnosis is TFRVal syndrome or TFRVar syndrome.


Figure 7-21 Tibial lateral rotation during two-joint hip flexor length test. A, Starting position of the two-joint hip flexor length test. Note position of the right tibia and foot in the sagittal plane. B, End position of the two-joint hip flexor length test. Note position of the right tibia and foot. Tibia is now more laterally rotated relative to the femur, secondary to the tension of the TFL-ITB as it is being stretched.
Prone tests
Lateral rotation of the tibia during knee flexion in prone may be observed. If this motion is painful, then the secondary test should be performed by repeating the motion while preventing the tibial rotation. If the patient’s symptoms are improved, then the movement impairment of TFR is supported. Further tests would be needed to determine if the diagnosis was TFRVal syndrome or TFRVar syndrome. During the performance of hip medial or lateral rotation, the examiner may observe excessive rotation or gliding of the tibia relative to the femur. If hip rotation ROM is measured in this position, care should be taken to prevent motion of the tibia relative to the femur, which may inflate the value of hip rotation ROM.89
Joint Integrity
In our experience, individuals with TFRVal syndrome often demonstrate an overall laxity in the tibiofemoral joint in the involved and uninvolved joint; however, this laxity has not been quantified. The therapist may suspect ligamentous laxity if there is excessive motion at the tibiofemoral joint while testing hip rotation. In the absence of trauma, tests for ligamentous integrity are often negative with the patient demonstrating equal motion on both limbs.
Muscle Length Impairments
A common muscle impairment includes reduced extensibility of the TFL-ITB,90 which may contribute to a relative lateral rotation of the tibia through its attachment on the lateral tibial tubercle.
Muscle Strength/Performance Impairments
Impairments of muscle strength and performance include poor performance of the hip lateral rotators and hip abductors.91,92 Tibial medial rotators may also be impaired, restricting their ability to control tibial lateral rotation, however these muscles are challenging to assess.
Functional Activities
Gait
During gait, excessive medial rotation or adduction of the femur during stance or tibial lateral rotation during swing may be observed. Excessive pronation of the foot may also be observed.
Step-up and step-down
Most patients with knee pain problems will report an increase in their symptoms with stair ambulation. A step-up and step-down test may be performed to assess the patient’s preferred pattern. Patients with TFRVal syndrome will demonstrate femoral adduction and knee valgus with performance of this activity (Figure 7-22). If the movement is painful, a secondary test is performed by repeating the movement and correcting the movement impairment. Because this activity introduces significant stresses on the structures of the knee, reducing the patient’s pain significantly may be difficult. If symptoms are not reduced with movement impairment modifications of either the tibiofemoral joint or the patellofemoral joint (see patellofemoral lateral glide syndrome), the patient’s pain severity may be too high for the activity being performed.
Tibial lateral rotation may be observed as the patient attempts to clear the toes as they raise the involved foot to the next step (Figure 7-23). This movement impairment may indicate that the medial rotators of the tibia are not sufficiently stabilizing the tibia as the lateral hamstrings contract to flex the knee.
Other Functional Tests
Activities that aggravate the patient’s symptoms should be assessed for movement impairments. Patients with TFRVal syndrome exhibit femoral adduction or knee valgus during the symptomatic activities. Common activities include prolonged sitting, squatting, and sit-to-stand. If the patient is an athlete or has low symptom irritability, higher level activities may need to be assessed to determine the movement impairment. These may include running,1 single-leg squat,1,93 and various forms of jumping or hopping.1,76,94
Summary of Examination Findings
TFRval syndrome presents with the movement impairment of femoral adduction and medial rotation relative to the tibia or tibial abduction/lateral rotation relative to the femur that contributes to a knee valgus. Positions or movements associated with TFRVal syndrome are often painful, and when the movement impairments are corrected, pain is reduced.
Treatment
Corrective Exercise Program
Treatment for this classification includes educating the individual on correcting the postural habits and movements that contribute to the movement impairment and thus the pain problem. The patient is provided with a general description of the impairment: excessive rotation between the tibia and femur. Specific instruction for alignment and functional activities is provided and practiced by the patient. The patient is also instructed in exercises to address the associated muscle impairments.
Alignment
First, the patient is educated in correction of posture and functional activities. To improve alignment between the femur and tibia, the therapist must address impairments in both the sagittal and transverse planes in an effort to achieve a more neutral or ideal alignment. If hyperextension is present, the patient is instructed to unlock the knees. To align the tibia and femur in the transverse plane, the patient is asked to align knees over feet with neutral rotation of hips and tibias by decreasing medial rotation of femur and lateral rotation of tibia. To correct femoral medial rotation, the patient is instructed to contract his or her gluteals and hip lateral rotators to laterally rotate the femur. However, if structural tibial torsion or femoral anteversion is present, normal alignment will not be possible and attempts to “correct” the patient’s alignment may result in abnormal stresses to the adjacent joints. Instruction to the patient should emphasize proper alignment that accommodates for these structural impairments. For example, if the patient has tibial torsion, the appearance of a lateral foot progression angle or “turn out” should be allowed. If the patient demonstrates femoral anteversion, the appearance of medial rotation of the femur should be allowed.
Functional activities
Functional activities that contribute to the movement impairment must also be addressed. The functional activity that is most bothersome to the patient should be addressed first, followed by the activities in which the patient spends the most time such as work or school activities. This chapter covers the activities that are useful for most patients; however, the therapist is encouraged to use the principles of the MSI system to address other functional activities that may not be described here.
Gait
To control femoral adduction and medial rotation during gait, the patient is instructed to contract the “buttock muscles” of the stance limb during weight acceptance; the goal is to recruit the hip abductors and lateral rotators. This is sometimes difficult for the patient to achieve on the first visit, therefore an exercise like weight-shifting with unilateral muscle contraction may be useful to assist the patient who is learning to contract the muscles at the appropriate time. The patient should also be instructed to avoid rotating on a fixed foot when making turns.
If the patient is having significant pain in the knee, an assistive device may be suggested to decrease the forces through the affected knee. The cane should be placed in the hand opposite the involved limb. Using the cane in the opposite hand has been shown to significantly reduce external moments95 across the knee.
Another strategy during gait is to have the patient walk with the feet apart. This change in alignment shifts the adduction moment toward the medial knee and can decrease the pain. As with all recommended alterations in alignment or movement patterns, the change in the symptoms is the guide to the effectiveness and/or appropriateness of the recommendations.
Sit-to-stand; stand-to-sit
The patient should also be instructed to avoid femoral adduction, femoral medial rotation, and knee valgus when transitioning from a sitting position to a standing position. For proper performance of sit-to-stand, the patient is instructed to slide forward in the chair and place the feet hip width apart and aligned behind the knees. On rising, the patient should lean forward to advance the tibias anteriorly over the feet, then use the quadriceps and gluteus maximus muscles to lift the body up and forward out of chair. While performing this, the patient should keep the knee and toes aligned in the transverse plane. Common cues that are useful include “squeeze your seat and keep your knee over your second toe” and “do not let the knees come together.” If the patient has difficulty with the correction, a resistive band may be placed around the distal femurs and the patient instructed to gently push into the band to keep it taut as they rise from the chair. If the band becomes loose during the performance of the activity, the patient is provided feedback for the suboptimal performance.
Stairs
The instructions used in the previous paragraph are also useful for stairs. The patient should avoid femoral adduction, femoral medial rotation, and knee valgus while ascending and descending stairs. During stair ascent, the patient may need to shift the weight anteriorly (lean forward over the stairs) to more functionally engage the gluteals.96
If the patient has significant pain with stairs, there are a number of methods to reduce symptoms during stair ambulation. These suggestions are useful for all patients with knee pain, despite their movement system syndrome. While ascending stairs, the patient is instructed to use a step-to pattern, leading with the uninvolved extremity and then advancing the involved extremity. As the patient improves and begins to use a step-over-step method, he or she may still be challenged in completing the step-up leading with the involved leg. The patient can use the plantarflexors of the uninvolved leg to help push-up from the lower step. The patient should also be encouraged to use the handrail to reduce the weight bearing on the involved limb.
Descending stairs is often painful for someone with knee impairments. While descending stairs, the patient may use a step-to pattern first leading with the involved extremity and then advancing the uninvolved extremity. Patients who are significantly limited may need to descend the stairs backward; however, this should be assessed closely to be sure the patient can perform safely. As the patient improves and begins to use a step-over-step method, a useful method to reduce stress to the involved limb while descending stairs is to use the plantarflexors eccentrically to absorb some of the body weight as the body is lowered onto the lower step.
Other functional activities
Personal activities related to work, school, fitness, and leisure should also be addressed. The patient should be instructed to avoid the TFRVal movement impairment during functional activities. For example, in sitting, the patient may sit with the foot in a relatively lateral position to the knee. The patient should be instructed to modify the position so that the knee and foot are aligned in the transverse plane (Figure 7-24). An impairment may also be demonstrated in the patient’s driving. Some patients change from the gas to brake pedal by keeping their heel in contact with the floorboard and rotating the tibia to move the foot, resulting in repetitive rotation between the tibia and the femur. These patients should be instructed to lift the foot from the floor as they change pedals to avoid the repetitive rotation, or they can rotate at the hip rather than the knee. After specific instruction in the performance of key activities, the patient should understand concepts that can be generalized to other activities.


Figure 7-24 Sitting position. A, Patient with TFRVal syndrome and knee pain bilaterally demonstrates her working position. She is a transcriptionist and uses a foot pedal regularly. Note position of the feet relative to the knees. B, Working position corrected. Patient is instructed in a modified position.
(From Harris-Hayes M, Sahrmann SA, Norton BJ, et al: Diagnosis and management of a patient with knee pain using the movement system impaiment classification system, J Orthop Sports Phys Ther 38(4):203-213, 2008.)
Fitness activities
If the patient does not have a fitness program, then a discussion is warranted to encourage a fitness program as a goal. If the patient participates regularly in fitness, we encourage continued participation in some form of fitness, although the current program may need to be modified. For example, the patient’s aerobic activities may need to be modified by addressing the movement impairment (Figure 7-25) and possibly reducing the intensity. The modified intensity level should be related to the patient’s stage of rehabilitation. For example, if the patient’s injury is in Stage 1 for rehabilitation, then the patient may use one-leg cycling for aerobic conditioning and progress to activities in the water with the body submerged to reduce stresses to the knee. For Stage 2, the person may be instructed to use a bike or to start with a walking program while concentrating on maintaining proper tibiofemoral alignment. The intensity is then gradually increased as the patient’s symptoms improve. Box 7-1 shows an example program to progress an individual back to running after injury.97 The type of fitness equipment also needs to be considered. For example, if the patient has tibial torsion then Nordic Track or even bicycle pedals that require a fixed forward position of the feet can cause injury to the knee.


Figure 7-25 Fitness activity: Cycling. A, Note the valgus alignment of the right knee. B, Position is modified to correct for TFRVal syndrome.
BOX 7-1 How to Encourage and Promote Fitness without Injury
Stage 2 For Rehabilitation
Example: running
Home Exercise Program
In addition to modifying the patient’s functional activities, the patient should be instructed in an exercise program to improve muscle performance and extensibility. Exercise prescription should be based on the results of the physical examination and include only exercises that address limitations specific to the patient. In addition, patients should be instructed in the appropriate response to the exercises. Appropriately, patients may feel some muscle soreness or fatigue with activities that overload the muscle. The pain will be in the muscle regions and not in the joint. However, they should not feel an increase in their symptoms during the performance of their exercises or experience a “pressure sensation” in the knee. This should be made explicit to patients. If either pain or pressure occurs, they should review the instructions to the exercise to be sure that they are performing it correctly and try again. If they still experience pain or pressure, they should discontinue this exercise until they return for their next visit.
Exercises to improve strength and performance of the hip abductors and hip lateral rotators may be prescribed. Many of these exercises are described in detail by Sahrmann.22 Exercises to improve hip abductor and hip lateral rotator strength, listed from easiest to most difficult, include hip lateral rotator isometrics in prone, hip abduction in prone, progressive hip abduction with lateral rotation in side lying, hip lateral rotation against resistance bands in sitting, and lunges in standing while maintaining proper alignment of the knee. During the performance of these exercises, therapists should check to be sure that the patient is recruiting the correct muscles by palpating the lateral rotators and posterior gluteus medius. In addition, it is important that the patient is able to feel the contraction in the buttock region so that he or she can recreate the exercise at home. To specifically target the gluteus maximus, the patient can perform hip extension in prone with the knee flexed and progress to exercises in standing such as hip extension using resistance bands.
An exercise used to improve the motor recruitment or timing of the hip lateral rotators and abductors is weight shifting with gluteal contraction on the stance lower extremity. Once the patient has demonstrated good performance of the weight-shifting exercise, the exercise may be progressed to standing on one leg with correct alignment. Resisted activities of the opposite leg while standing on the affected leg may also be used to challenge the hip lateral rotators and abductors.
Exercises to improve the extensibility of the TFL-ITB should be prescribed. We recommend the following exercises: (1) prone knee flexion (bilateral [Figure 7-26] or unilateral), (2) prone hip lateral rotation without tibiofemoral motion, (3) two-joint hip flexor length test position, and (4) Ober test position. During the performance of these exercises, the tibiofemoral joint must be stabilized to prevent rotation. The patient is instructed to control tibial rotation by stiffening the necessary musculature at the knee. For example, while performing prone knee flexion, the patient points the foot toward the opposite limb, therefore contracting the tibial medial rotators to help stabilize the joint. If the patient is unable to control the tibial rotation, the exercises will need to be modified. Modifications might include either abducting the hip or placing a pillow under the pelvis to put the TFL-ITB on some slack. During all of these stretching exercises, the patient should have good abdominal support to avoid pelvic anterior tilt or transverse rotation.


Figure 7-26 Prone knee flexion. A, Prone bilateral knee flexion to improve the extensibility of the TFL-ITB. B, To prevent tibial lateral rotation during performance of the stretch, the patient is instructed to keep the toes together and the heels in line with the tibias.
Improvement of abdominal performance may be needed. The abdominals assist in keeping the pelvis stable during activities involving the limbs. Some individuals may demonstrate poor performance of the abdominals as evidenced by increased rotation of the pelvis during functional activities such as gait or during performance of exercise (for example, pelvic rotation or tilting while lifting the leg during hip abductor strengthening). If so, he or she should be instructed in exercises to improve strength (lower abdominal progression as described by Sahrmann22) and recruitment (encourage patient to pull in abdominals with functional activities).
Taping
If the patient has difficulty correcting the movement impairment, taping may be helpful. The posterior X taping method, developed by our colleague, Debbie Fleming-McDonnell,* has been used as a method to prevent or reduce rotation at the tibiofemoral joint (Figure 7-27). The strips of tape that move from proximal-lateral thigh around the posterior knee to the distal-medial tibia are proposed to assist in reducing femoral medial rotation and tibial lateral rotation. We often add other strips of tape for symmetry or to assist in preventing knee hyperextension in patients who tend to hyperextend.
Orthotics
Most patients improve by addressing deficits of the hip only; however, some patients may benefit from orthotics to correct pronation at the foot. A number of articles related to the use of orthotics for knee pain problems have been published; however, the findings are equivocal.98-102 We believe the inconclusive findings are related to the lack of foot type classification in studies related to knee pain. We believe that some individuals may benefit from correcting impairments of the foot and others may not (Figures 7-28 and 7-29). For example, if a patient demonstrates pronation that is excessive or occurs at an inappropriate time during gait, abnormal rotation at the tibiofemoral joint may result. If pronation is suspected to contribute to the rotation at the tibiofemoral joint, an orthotic may be appropriate.103 If, however, orthotics do not reduce excessive tibiofemoral rotation or they increase tibiofemoral rotation, they may not be indicated.

Figure 7-28 Decision-making for orthotics. Patient may not benefit from orthotic. Note excessive femoral medial rotation and foot supination. Recommend correcting hip impairment first.


Figure 7-29 Decision-making for orthotics. A, Patient may benefit from orthotic. Note excessive femoral medial rotation and foot pronation. Hip may still be a contributor. Recommend correcting contribution of the hip with the addition of orthotics if needed. B, Patient may benefit from orthotic; however, correcting standing alignment by reducing hip abduction may improve alignment of the knee and foot.
A careful assessment of the foot should be done to determine whether the rotation of the femur results in rotation at the tibiofemoral joint or motion at the foot. If excessive medial rotation of the hip occurs and the foot is stiffer than the tibiofemoral joint, whether by foot structure or by using an orthotic, tibiofemoral rotation will be exaggerated. Therefore the therapist must assess if the rotation at the tibiofemoral joint is increased or decreased if a pronation support is provided. When orthotics are indicated, temporary orthotics may be fabricated to assess the usefulness of the orthotic and allow the patient to test the correction before deciding to purchase a customized pair of orthotics.
Neuromuscular Training
Impairments of the neuromuscular system, such as poor balance or proprioception, may be present with any of the movement impairment syndromes. Treatment should include neuromuscular training to address impairments of proprioception and balance and the ability to accommodate to perturbations. When instructing the patient in neuromuscular training exercises, the patient should avoid motions and positions such as excessive knee valgus or femoral medial rotation. Examples of neuromuscular retraining activities are provided in Box 7-2. At time of the writing of this text, there are a number of laboratories studying this topic in patients with knee disorder.13,14,104,105 The reader is encouraged to review current studies.
BOX 7-2 Neuromuscular Training
When instructing the patient in neuromuscular training exercises, it is important to remind the patient to avoid motions or alignments consistent with his or her specific movement system syndrome.
Proprioception/Balance106
Activities to improve proprioception of the knee should be incorporated as soon as possible. Begin early in treatment using activities such as weight shifting, progressive increases in weight bearing on the involved LE, and then eventually unilateral stance. As the patient can take full weight on the involved knee, activities are progressed to the use of a balance board.
Progression: Activities should be progressed to prepare patient to return to daily activities, fitness routines, and work or sporting activities. As the patient progresses, proprioception can be challenged by asking the patient to stand on unstable surfaces (pillows, trampoline, or BOSU ball); perturbations can be applied by having the patient catch a ball being thrown to him while standing on one leg or by perturbing the surface on which the patient is standing.105 Sliding board activities have also been shown to be beneficial to patients after surgery.107
Sport-Specific Training (If Appropriate)
In preparation to return to sports, sport-specific activities should be added. The initial phases of these activities will include straight plane activities at a slow pace and then a gradual increase in the level of difficulty by increasing the intensity and patterns to include changes of direction, starts, and stops.
Agility Exercises
Emphasis is placed on proper movement.
Hopping timed
Within each level, begin with short bouts of hopping and longer rests between (15 seconds on, 30 seconds off), then increase on time and decrease off time (30 seconds on, 15 seconds off).
Jumping from short surface, 2 inches
Emphasis should be placed on landing on both feet evenly with neutral knees over toes (avoid excessive knee valgus or femoral adduction or medial rotation). The patient should also think about landing softly, using the ankle plantarflexors and allowing the knees to flex to help absorb the landing.13,106
Other plyometrics: ladder drills
note: If plyometrics and resistance training are to be performed during the same visit, plyometrics should be performed before the resistance training activities.106
Running
See Box 7-1 for initial running program. Once the individual is able to run 1 mile without an increase in symptoms or swelling, cutting activities may begin.
note: Care should be taken to evaluate how the patient chooses to cut. Often, particularly in patients who have suffered noncontact injuries, the patient may have adopted an inefficient cutting pattern such as planting the left foot when trying to cut to the left.
Jumping Program
Please refer to article by Hewett et al.13 for description of jumping program. The following are some of the key concepts used in their program.
Drills
Once the patient can complete cutting drills without pain or swelling and demonstrates good control of the LE, variations, such as the following, can be added:
Basketball Specific Training
Please refer to article by Louw et al108 for description of specific training for basketball.
Functional testing
Consider functional tests before the patient’s return to sport. There are many functional tests available. The validity of these tests are controversial; however, each test can offer some insight in how the patient may perform in his or her specific sport. It is recommended that a battery of tests be used to assess the aspects of balance, coordination, agility, and strength. Refer to Fitzgerald et al109 for a proposed system to test patients returning to sports after non-operative treatment of ACL tear. Common test items for the knee include the following:
Tibiofemoral Rotation with Varus Syndrome
Symptoms and History
Individuals with TFRVar syndrome also demonstrate excessive rotation at the tibiofemoral joint; however, it is associated with a knee varus. The patient may demonstrate a varus thrust during gait. A varus thrust has been described in individuals with injury to the posterolateral corner of the knee and recently studied in the osteoarthritic knee.7 Traditionally, varus thrust has been described as motion that is primarily in the frontal plane and thought to be the consequence of structural changes of the medial compartment in the osteoarthritic knee. We have observed, however, an apparent varus thrust in young individuals without radiological evidence of OA or ligamentous injury. This apparent varus thrust seems to be a result of a combination of hip medial rotation and knee hyperextension.
Structures that may be injured in an individual with TFRVar syndrome include the structures of the tibiofemoral joint, the ITB, and the surrounding musculature. The medial compartment of the tibiofemoral joint may be particularly at risk, given that it is responsible for 60% to 80% of the total load across the knee. Recent interest has been placed on the external knee adduction moment and its contributions to the load on the medial knee compartment.110 The external knee adduction moment is defined as the product of the ground reaction force and the perpendicular distance to the knee joint (Figure 7-30). Clinically, the alignment associated with the knee adduction moment is genu varus. The knee adduction moment has been associated with the progression of knee OA.111 An increase in varus alignment of the knee may result in a larger moment arm of the ground reaction force and thus increase the force through the medial compartment.

Figure 7-30 The external knee adduction moment is defined as the product of the ground reaction force and the perpendicular distance to the knee joint. G, Ground reaction force vector; I, momentum of ground reaction force; K, knee joint center.
(Modified from Jenkyn TR, Hunt MA, Jones IC, et al: Toe-out gait in patients with knee osteoarthritis partially transforms external knee adduction moment into flexion moment during early stance phase of gait: a tri-planar kinetic mechanism, J Biomech 41(2):276-83, 2008.)
Several authors have reported that using a “toe-out” gait pattern reduces the knee adduction moment and thus reduces symptoms.112-114 Two mechanisms have been proposed to explain the reduction of symptoms when a toe-out pattern is used. In their study of individuals with knee OA, Jenkyn et al113 demonstrated that a portion of the external knee adduction moment was transformed into a flexion moment during the early phase of stance. Chang et al115 provided another theory based on their interpretation of a study by Wang et al116: A toe-out gait pattern shifts the ground reaction force vector closer to the knee joint center. This shift results in a reduction in the moment arm of the ground reaction force and thus the external knee adduction moment.
Key Tests and Signs
Alignment Analysis
A patient with TFRVar syndrome often presents with femoral medial rotation and knee varus and may demonstrate a supinated or a fixed flat foot. The genu varus may be due to structural problems, such as OA in the medial compartment of the knee, or it may be a postural fault cause by femoral medial rotation along with knee hyperextension (Figure 7-31, A-D). The examiner should be careful not to classify by standing alignment alone. An individual may demonstrate a varus alignment in standing but demonstrate knee valgus with activities (Figure 7-31, E-F). The examiner must consider the entire movement examination and the symptom behavior to determine the appropriate diagnosis.

Figure 7-31 TFRVar Alignment. Patient’s alignment during examination. Anterior view (A) and posterior view (B). Patient demonstrates structural faults of genu varum and tibial varum. Genu varum is increased with postural fault of femoral medial rotation and knee hyperextensions. Patient’s modified alignment (same patient as A and B), anterior view (C), and posterior view (D). Patient has been instructed to correct postural faults by “unlocking his knees” and contracting the hip lateral rotators to reduce femoral medial rotation. Varus alignment in standing (E) might suggest TFRVar; however, patient demonstrates valgus positioning of the knee (F) during a single leg squat indicating that TFRVal is the likely diagnosis.
Movement Impairments
Standing tests
During single-leg stance on the involved limb, the patient will demonstrate excessive medial rotation of the involved femur with minimal to no movement at the foot. Balance may also be a factor in this syndrome, although clinically it is not as common in TFRVar syndrome as it is in TFRVal syndrome.
Supine tests
Similar to TFRVal syndrome, the patient with TFRVar syndrome may demonstrate rotation or abduction of the tibia during the performance of the two-joint hip flexor length test (see Figure 7-21).
Joint Integrity
The patient may demonstrate mild-to-moderate laxity in the fibular collateral ligament (lateral collateral ligament); however, overall laxity in the tibiofemoral joint is not typically observed in the young individual with TFRVar syndrome. Older patients with arthritic changes may demonstrate some general joint laxity.
Muscle Strength/Performance Impairments
Impairments of muscle strength and performance include poor performance of the hip lateral rotators and possibly hip abductors.91,92
Functional Activities
Gait
During gait, excessive femoral medial rotation and knee hyperextension may contribute to the apparent varus thrust during stance. Ankle dorsiflexion and foot pronation are often limited, which may increase stresses to the tibiofemoral joint.
Step-up
During a step-up, the patient does not shift the body weight forward over the foot and demonstrates a faulty movement of pulling the knee back to the body, instead of bringing the body forward over the limb. Because the foot is anchored on the floor during the step-up, hip extension performed by the hamstrings may assist with knee extension, therefore reducing the need to recruit the quadriceps to extend the knee. Gluteal muscles also have a reduced ability to extend the hip when the patient’s body weight is kept in a relative posterior position.
Other Functional Tests
Activities that aggravate the patient’s symptoms should be assessed for a movement impairment. Common activities include prolonged sitting, squatting, and sit-to-stand. If the patient is an athlete or has low irritability of their symptoms, higher level activities, such as single-leg squat and jumping, may need to be assessed to determine the movement impairment.
Summary of Examination Findings
TFRVar syndrome presents with the movement impairment of excessive rotation between the tibia and femur that is associated with a genu varum. Varum of the tibiofemoral joint may be secondary to structural changes in the medial joint surfaces as in OA; however, an apparent varum may be secondary to acquired impairments of femoral medial rotation and knee hyperextension. Positions or movement associated with TFRVar syndrome are often painful, and when corrected, pain is reduced.
Treatment
Corrective Exercise Program
Treatment for TFRVar syndrome is similar to the treatment for TFRVal syndrome with a few subtle differences; only the differences are discussed here.
Alignment
Instructions to correct alignment are similar to those for TFRVal syndrome. To improve alignment between the femur and tibia, the therapist must address impairments in both the sagittal and transverse planes in an effort to achieve a more neutral or ideal alignment. If hyperextension is present, the patient is instructed to unlock the knees. To align the tibia and femur in the transverse plane, the patient is asked to align knees over feet with neutral rotation of hips by decreasing medial rotation of femur. To correct femoral medial rotation, the patient is instructed to contract their gluteals and hip lateral rotators to laterally rotate the femur. As described previously, structural impairments, such as tibial varum must be noted and considered when attempting to correct alignment (see Figure 7-31).
Functional activities
Instructions to maintain proper alignment and movement strategies during functional activities are recommended. Cues to correct femoral medial rotation are the same as those provided for patients with TFRVal syndrome. Genu varum is often challenging to correct; however, cues to reduce impact on the knee joint may be useful in reducing stresses on the knee joint. For example, during gait, patients are encouraged to use a heel-to-toe gait pattern and use the rolling of the foot to provide shock absorption. In severe cases, symptoms may be reduced by instructing the patient to walk with a “toe out” pattern.112-114 If the patient is experiencing medial condyle degenerative changes, the instruction is to walk with the feet closer together and in slight lateral rotation to decrease the stress on the medial condyle.
If the patient could benefit from a cane, typically, the cane is placed in the hand opposite the involved limb. Anecdotally, however, some patients have reported decreased symptoms when the cane is placed in the ipsilateral hand. Using the cane in the ipsilateral hand may decrease the forces on the medial knee. To apply weight onto the cane, the patient shifts the body weight closer to the affected knee, thus reducing the external moment arm of the body weight and possibly the amount of force through the medial compartment of the knee.
Home Exercise Program
Exercises to improve strength and performance of the hip lateral rotators may be prescribed if the patient demonstrates excessive medial rotation. See the “Home Exercise Program” section for “Tibiofemoral Rotation with Valgus Syndrome” for a description of these exercises.
Taping/Bracing
The taping method demonstrated in Figure 7-27 is useful to prevent or reduce rotation and hyperextension at the tibiofemoral joint. In patients with advanced disease, particularly OA, an unloader brace may be useful.117,118
Orthotics
Cushioned shoes and an additional cushioned insert may improve shock absorption of the lower extremity, particularly in patients with a rigid, supinated, or structurally (fixed) pronated foot.
Case Presentation
Tibiofemoral Rotation with Valgus Syndrome
Symptoms and History
A 16-year-old female soccer player is referred to physical therapy for evaluation and treatment of right knee pain. She reports right anteromedial knee pain for 2 months. Her pain began during preseason training and limited her ability to participate in practice. During practice, her pain would increase to 5/10. The pain could be sharp, particularly with cutting and kicking the soccer ball with the involved limb. Her pain improved with rest and ice. Her Knee Outcome Score–Activities of Daily Living (KOS-ADLs)119 is 74%, and her KOS-Sports score is 57%. Radiographs show no abnormalities of the tibiofemoral or patellofemoral joint.
Alignment Analysis
The patient is 5 feet 10 inches and weighs 150 pounds. In stance, the patient demonstrates medial rotation of the femur and greater foot progression angle (toe out) on the right. In sitting, the tibia is rotated laterally relative to the femur. There are no obvious impairments of patellar alignment.
Movement Analysis
During single-leg stance on the right, the patient demonstrates excessive medial rotation of the femur and pronation of the foot. During a partial squat, the patient demonstrates femoral adduction, knee valgus, and foot pronation. The patient reports an increase in her pain during the performance of the squat. The patient is then instructed to keep her knee in line with her toes and avoid allowing the knees to come together. She is able to correct her performance and reports that her symptoms are decreased compared to the uncorrected movement.
During knee flexion in prone, the patient demonstrates lateral rotation of the tibia and reports an increase in her symptoms at the end of the motion. With manual correction to control tibial lateral rotation, the patient reports a decrease in her symptoms compared to the uncorrected movement.
Joint Integrity
Accessory motions of the patellofemoral joint are excessive in the medial and lateral directions but equal to the uninvolved side. Accessory motions of the tibiofemoral joint are also equal bilaterally. The patient reports no change in her symptoms with the accessory motion testing.
Muscle Length Impairments
During the two-joint hip flexor length test, the patient demonstrates a short, stiff TFL on the right. As the hip is extended, the tibia rotates laterally and the patient reports an increase in her symptoms. With manual correction to control the rotation of the tibia, the patient reports a decrease in her symptoms compared to the first performance.
Muscle Strength/Performance Impairments
On the right, the hip lateral rotators are 4−/5 tested in sitting, the gluteus maximus is 4/5, the TFL is 4/5, and the posterior gluteus medius is 3+/5. While testing the posterior gluteus medius, the patient’s hip flexes and medial rotates, indicating that the hip flexors are compensating for performance of the posterior gluteus medius. With cueing, she is able to correct the position but could only maintain the position against minimal pressure to the distal lower extremity.
Stiffness/Extensibility/Flexibility
The TFL-ITB is relatively more stiff than the knee joint causing compensatory lateral tibial rotation during the two-joint hip flexor length test.
Tests for Source
The patient reports tenderness with palpation along the medial and lateral joint lines, as well as the medial patellar facet. McConnell test120 and the patellofemoral grind test52,120 for patellofemoral pain are negative. All ligamentous and meniscal tests are negative.
Functional Activities
During sit-to-stand and stair ambulation, the patient demonstrates femoral adduction and knee valgus. She does not report pain with sit-to-stand; however, she is instructed in correcting her movement to reduce femoral adduction and knee valgus. She is able to correct easily. With cutting activities on the right lower extremity, the patient demonstrates femoral adduction and tibial lateral rotation. The cutting maneuvers increase her symptoms. The patient attempts to correct her movement quality during the cutting maneuver; however, she is unable to correct the fault completely.
Diagnosis and Staging
The diagnosis is TFRval syndrome and the stage for rehabilitation is Stage 2. Her prognosis is good to excellent. Positive moderators include her young age, overall good health, high motivation to return to her activities, and her ability to change the simple movement impairments, such as partial squat and sit-to-stand, with instruction only. Negative moderators include her high activity level.
Treatment
The patient was seen once per week for 4 weeks, then once every other week for 2 weeks for a total of 6 visits over 8 weeks. Treatment included instruction in correct performance of functional activities, including her sporting activities. She was also instructed in a home exercise program to improve performance of the hip abductors and hip lateral rotators and exercises to increase the extensibility of the TFL-ITB. Although she reported pain in the right knee only, she was encouraged to perform the exercises bilaterally.
During the first visit, the patient was instructed in correct performance of sit-to-stand, stair ambulation, and squatting. She was instructed to contract her gluteals to control the femoral adduction and knee valgus during the activities. She was able to make these corrections quite easily.
To improve the recruitment of the hip musculature during functional activity, the patient was instructed in the exercises, weight shifting, and single-leg stance. She was encouraged to contract her hip lateral rotators when weight was shifted onto the ipsilateral lower extremity. She was instructed to perform these exercises frequently throughout the day if possible. Daily activities, such as brushing one’s teeth or speaking on the phone, provide excellent opportunities to work on weight shifting throughout the day.
To improve performance of the hip lateral rotators and hip abductors, side lying hip abduction/lateral rotation was prescribed with the hip and knee extended (level 2 Sahrmann22). The patient was instructed to perform the exercise with her back and leg against the wall. She was instructed to keep the shoulders, hips, and heels on the wall while performing the exercise. The wall provides feedback to remind her to keep her hip in the extended position and avoiding hip flexion.
To more specifically target the hip lateral rotators in hip flexion, she was instructed in lateral rotation in sitting with the feet together.22 An elastic exercise band was placed around the distal end of the femurs to provide resistance to the hip lateral rotators. These exercises were to be performed once a day, in 3 sets, each set to fatigue. The repetitions depend on her ability to perform the exercise correctly.
Knee flexion in prone was prescribed to improve the extensibility of the TFL-ITB. To prevent tibial lateral rotation, the patient was instructed to flex both knees while keeping her feet together during the exercise.
Although the patient could easily correct her movement impairments during functional activities, it was unlikely that she could correct her movement strategies entirely during her soccer practice, so the patient’s knee was taped with the method shown in Figure 7-27. She was instructed to keep the tape in place up to 3 days, as long as she did not develop skin irritation.
At her second visit, 1 week later, the patient reported 50% compliance with the exercises and 70% compliance with the functional activity corrections. She stated that with the tape, she was able to participate in the entire soccer practice. She still had an increase in symptoms, that only increased to a 2/10 maximum. In a subsequent practice after she had removed the tape, she was unable to participate in the entire practice. She demonstrated correct performance of the exercises, therefore the exercises were progressed. Sidelying hip abduction/lateral rotation was progressed to level 3.22 She was also given prone hip extension with the knee flexed. She was instructed to place pillows under her abdomen while performing prone hip extension, to allow for adequate motion, which was restricted by her short TFL-ITB.
Also, at her second visit, some of her soccer drills were addressed. Recommendations were provided in correcting the movement impairments of hip adduction and tibial lateral rotation during her activities. The patient was taped again.
At 1 month, the patient was able to participate in her practices without a significant increase in her pain and the patient was progressed to Stage 3. Taping was discontinued, and exercises were progressed. The strength and recruitment of her hip musculature improved, thus her program was progressed to exercises in weight bearing. She was given resisted shuffles using an elastic band around the distal femurs. Resisted hip extension and hip abduction in standing were given, using an elastic band for resistance.
Sports-specific drills were practiced while encouraging proper alignment of the knees. Neuromuscular training was also incorporated. The patient was encouraged to incorporate these activities into her regular soccer warm-ups.
Outcome
The patient was seen for a total of 6 visits over 8 weeks. At the time of her last visit, 2 months after her initial visit, the patient reported that she was playing soccer pain-free and continued to use the training drills during her soccer practice. Function was also improved as demonstrated by improved scores: KOS-ADLs is 100% and KOS-Sports is 100%.