Tibiofemoral Hypomobility Syndrome
The movement impairment of tibiofemoral hypomobility (TFHypo) syndrome is associated with a limitation in the physiologic motion of the knee. The limitation may result from degenerative changes in the joint or from the effects of prolonged immobilization. OA of the knee may contribute to TFHypo syndrome, although not all individuals with OA have TFHypo syndrome. The diagnosis of tibiofemoral rotation should be considered if a patient has radiographic evidence of OA but no limitation in knee ROM.
Symptoms and History
Individuals with the diagnosis of TFHypo syndrome report knee pain located deep in the joint and often describe their pain as vague. Symptoms are typically increased with weight-bearing activities, such as walking, standing, and stair ambulation, and are relieved with rest. Reports of stiffness after prolonged periods of rest are common. The most common diagnoses used by a referring physician include OA and knee contracture.
Key Tests and Signs
Alignment Analysis
During assessment of standing alignment, the patient often demonstrates knee flexion; however, individuals with OA may demonstrate genu varum or genu valgus. The knee joint may also appear to be enlarged or show signs of inflammation/swelling. In addition to assessing knee alignment, alignment of the hip and foot should also be assessed.
Movement Impairments
Standing tests
During single-leg stance on the involved limb, the patient may demonstrate poor hip and trunk control, which is evidenced by pelvic tilt or trunk lateral bending. This is often described as a positive Trendelenburg sign121 or a gluteus medius limp when severe (notable lateral trunk flexion over involved side). The patient may also demonstrate poor balance requiring upper extremity support for performance.
Sitting
During sitting knee extension, the patient may demonstrate decreased knee extension ROM. Careful observation of this movement is recommended. Some patients demonstrate co-contraction of the lower extremity muscles, particularly quadriceps and hamstrings, while attempting to extend the knee. If co-contraction is occurring, the limb moves slowly and the patient appears to be using a great deal of effort. If co-contraction is suspected, a cue to reduce effort of the activity often results in ease of the motion and a reduction in symptoms. Passively extending the patient’s knee while the patient is sitting in a chair with a backrest will provide information about hamstring length and stiffness.
Joint Integrity
Patients with TFHypo syndrome demonstrate a reduction of ROM in flexion and extension. Limitations in knee ROM may be due to impaired arthrokinematics and/or reduced muscle extensibility, therefore assessment of joint flexibility, accessory motions, and muscle extensibility is recommended. Often, end-range of motion is painful. Patients with TFHypo syndrome associated with OA may report a decrease in their end-range pain with repeated passive motion. Patients with osteoarthritic changes of the joint may demonstrate a capsular pattern, defined as a loss in flexion ROM that is greater than the loss of extension.122 Recently, however, the validity of using this pattern to detect individuals with OA has been called into question.123,124
Muscle Length Impairments
Decreased extensibility of the hip flexors, hamstrings, and ankle plantarflexors may also be associated with the TFHypo syndrome.
Muscle Strength/Performance Impairments
Common muscle impairments include poor performance of the gluteal musculature, hip lateral rotators, gastrocnemius, and quadriceps. As described previously, co-contraction of the quadriceps and hamstrings may be visible during exercise or performance of functional activities. Co-contraction has been shown to increase joint contact pressures that may result in increased injury to the joint surfaces.125,126
Functional Activities
Gait
Patients with TFHypo syndrome demonstrate reduced knee ROM throughout their functional activities. During ambulation, there is a reduction of knee excursion in both flexion and extension. Often the knee is maintained in flexion throughout the entire gait cycle. The patient may also demonstrate a decreased stride length and decreased push-off.
Stairs
While descending stairs, the patient may demonstrate reduced knee flexion excursion on the stance limb. This reduced excursion is not solely the result of reduced joint flexibility but may be an impaired movement strategy caused by muscle co-contraction. The patient demonstrates co-contraction of the lower extremity muscles127 that often results in an increase in symptoms and effort. Follow-up instruction to “let go” of the musculature often results in an improvement in symptoms.
Sit-to-stand
Reduced knee flexion is also seen as the patient moves from a sitting position to standing. Sufficient knee flexion is required to move the tibia anteriorly to bring the patient’s center of mass (COM) over their feet. When the anterior movement of the tibia is reduced, the patient compensates with increased hip and trunk flexion to advance their COM anteriorly.
Summary of Examination Findings
Patients with TFHypo syndrome present with a physiologic limitation of knee motion, typically in knee flexion and knee extension. They also demonstrate a limitation of knee joint excursion during functional activities such as gait and stair ambulation. The observed limitation in ROM may be due to limitations in joint flexibility and muscle extensibility or an impaired motor recruitment pattern.
Treatment
Treatment for this syndrome includes first educating the individual on correcting the postural habits and movements that may be contributing to the movement impairment.
Primary Objectives
The primary objectives of a treatment program include the following:
Corrective Exercise Program
The patient is instructed in functional activities and an exercise program to address the associated movement impairments. All patients should be encouraged to participate in regular fitness activities to maintain current weight or reduce weight if the patient is overweight or obese.
Alignment
It is often difficult for patients with TFHypo syndrome to change alignment immediately; however, correct alignment should be encouraged.
Functional activities
In the early stages of rehabilitation, compensatory modifications may be needed to accommodate the lack of ROM or to prevent increased pain. As the patient’s ROM and pain improves, the performance of functional activities should focus on teaching the components of ideal motion. If it is determined that the limitation in ROM is structurally fixed, then compensatory techniques should be provided.
Gait
During gait, the patient is instructed to use a “rolling” heel-to-toe gait pattern. This modification’s intent is to improve the shock absorption contribution of the foot and encourage improved push-off. If the patient is experiencing severe pain or demonstrates a significant malalignment, such as genu varum, an assistive device should be recommended to redistribute the forces on the affected knee. See the information on the use of a cane in the “Functional Activities” section for “Tibiofemoral Rotation with Varus Syndrome.”
Sit-to-stand; stand-to-sit
To rise from a sitting position to standing, the patient should be instructed to slide forward to the edge of the chair. Once at the front of the chair, the patient should position the feet about hip-width apart and slightly posterior to the knees. If knee flexion is significantly limited, the patient may keep the affected knee comfortably extended while placing the unaffected foot appropriately. The patient is instructed to lean forward at the hips to be sure his or her center of mass is moved forward over his or her base of support. The patient is also encouraged to contract the quadriceps and gluteals and avoid femoral adduction when rising from the chair.
When transitioning from standing to a sitting position, the patient is instructed again to contract the gluteals and quadriceps and slowly lower themself into the chair. Individuals with significant limitations or pain may need to begin practicing these movements with a higher seat surface and use their upper extremities on the armrests to assist with pushing up from the seat and lowering into the seat. Performance of sit-to-stand may be progressed by reducing the use of the upper extremities and lowering the height of the seat.
Stairs
Patients with TFHypo syndrome often have a high severity of symptoms with stair ambulation. Please see the “Treatment” section in the “Tibiofemoral Rotation with Valgus Syndrome” section for methods to reduce symptoms with stair ambulation. If the patient demonstrates co-contraction during the stair descent, cues to “let go” or relax their musculature often results in a reduction of symptoms.
Other functional activities
Activities the patient performs throughout the day that may contribute to the patient’s symptoms should be addressed. For example, patients often report increased stiffness and pain after prolonged sitting. They should be instructed to decrease the amount of time that the knee is maintained in one position. They can accomplish this by rising from the chair every 20 to 30 minutes and walking or flexing and extending the knee if the situation will not allow rising from their chair, such as during a business meeting or class.
Fitness activities
Fitness activities should be addressed as soon as possible. The appropriate level of activity demand should be assessed. In the early rehabilitation stages, the patient should begin with non–weight-bearing or reduced weight-bearing activities such as swimming, water exercises, and stationary biking without resistance. As the patient improves, weight bearing should be gradually increased. Using a StairMaster or elliptical cross-trainer can serve as a good transition to walking. While initiating strengthening exercises, it is safer for the patient to begin with high repetitions of relatively low resistance; high levels of resistance are not encouraged because of the high levels of compressive forces through the joint.
Home Exercise Program
The patient should be provided with a home exercise program and instruction on the appropriate response to exercise. Specific exercises should be provided to increase ROM and improve lower extremity muscle strength and muscle extensibility.
Exercises to improve muscle performance, including strengthening and motor recruitment of the hip musculature, are described in detail in the treatment description of TFRVal syndrome. Patients with TFHypo syndrome may also benefit from strengthening of the gastrocnemius muscle, beginning with elastic band resistance and progressing to weight-bearing heel raises. Other muscles that should be considered are the abdominals and the quadriceps, if appropriate.
Historically, quadriceps strengthening has been recommended for patients with knee OA, based on the theory that the quadriceps provide shock absorption at the knee. A recent trial involving patients with knee OA demonstrated that pain can be decreased with the implementation of a strengthening program.128 However, epidemiological studies specific to knee OA have shown that increased quadriceps strength can actually accelerate the progression of OA in knees with malalignment16,18,20 or laxity.20 One must consider the compressive forces that the quadriceps can add to a joint before administering aggressive quadriceps strengthening activities. We recommend that therapeutic exercises to hypertrophy the quadriceps be avoided in patients with malalignment or laxity of the knees. However, the functional performance of the quadriceps may be enhanced through proper performance of functional activities such as sit-to-stand, stand-to-sit, step-up and step-down, and partial wall squats.
Exercises to improve the extensibility of the hip flexors, gastrocnemius, and hamstrings are also prescribed.22 To improve the extensibility of the hip flexors, the following exercises may be provided: hip and knee extension in supine (heel slide) with the opposite hip held passively flexed to the chest, knee flexion in prone, and hip lateral rotation in prone to specifically stretch the TFL-ITB. To improve the extensibility of the gastrocnemius, the patient may be instructed to perform ankle dorsiflexion in sitting with the knee extended or ankle dorsiflexion in standing. Hamstring extensibility may be increased with knee extension in sitting (see Figure 7-40).
Other Interventions
Accessory and physiologic mobilizations may be used to reduce pain and increase ROM. If the patient is having pain at rest, a distraction mobilization can be taught to the patient for independent use at home. A trial of gentle distraction should be performed to determine if this technique will be appropriate. For the home technique, the patient sits with the knees at 90 degrees, with the lower leg dangling. A small pillow or rolled-up towel is used to elevate the thigh so that the foot is off the floor. A small weight or shoe, approximately 1 to 2 pounds, is applied to the distal limb (Figure 7-32). Patient allows the leg to dangle up to 10 minutes to help relieve discomfort. This may be performed as often as needed to relieve pain.
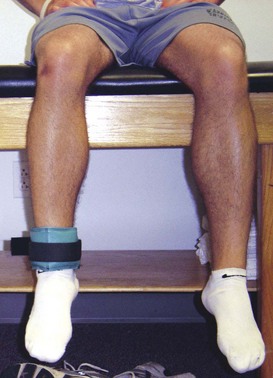
Figure 7-32 Home program for distraction mobilization to reduce pain. Patient is instructed to place light weight or heavy shoe, approximately 1 to 2 pounds, to the distal limb. Patient allows the leg to dangle up to 10 minutes to help relieve discomfort. This may be performed as often as needed to relieve pain.
Bracing may be considered for patients who continue to have symptoms that are limiting their function. Braces range from the simple neoprene sleeve thought to provide warmth and possible improvement in proprioception to customized unloader braces to redistribute forces in the knee. If prescribing a brace, the therapist must consider the patient’s goals and motivation, as well as the anthropomorphic characteristics for adequate fit. We recommend a trial of a relatively inexpensive, easy-to-apply brace first. If symptoms are not affected, then a custom brace might be considered.
Finally, neuromuscular training may also improve function of the lower extremity. Activities in Box 7-2 may need to be modified for the patient’s skill level. A program developed for nonoperative ACL has been modified for use in the older individual and has preliminary evidence indicating success.104
Knee Extension Syndrome
Knee extension (Kext) syndrome is described as knee pain associated with quadriceps dominance or stiffness that results in an excessive pull on the patella, patellar tendon, or tibial tubercle. This movement system syndrome may be associated with poor performance of the hip extensors. The Kext syndrome has a subcategory of patellar superior glide (KextSG). Although both conditions are a result of quadriceps stiffness, the structures that are involved are related to the location of relative stiffness/flexibility. In KextSG syndrome, the patellar tendon and surrounding retinacula are relatively more flexible than the quadriceps, therefore when the quadriceps contracts, the patellar is displaced superiorly in the trochlear groove. Excessive stresses may be placed on the patellofemoral joint or patella tendon as the patella is pulled superiorly. In Kext syndrome, the patella is thought to be relatively stable and therefore the strain may be placed on the structures superior to the patella. Because the movement impairments of the two conditions are similar, they are described concurrently; movement impairment of Kext syndrome is described and information specific to KextSG syndrome is highlighted.
Symptoms and History
Patients with Kext syndrome report symptoms superior to the patella in structures such as the quadriceps or quadriceps tendon. In contrast, patients with KextSG syndrome report symptoms in the peripatellar region or the infrapatellar region and may involve the patellofemoral joint structures or the patellar tendon and the patellar tendon attachment sites, including the patellar inferior pole and tibial tuberosity. In patients with either syndrome, symptoms are aggravated with activities that require repetitive or forceful knee extension such as jumping. Patients are often athletes such as runners, football linemen, and volleyball players. Common diagnoses used by referring physicians include patellar tendinopathy (often called jumper’s knee), quadriceps strain, and Osgood-Schlatter disease.
One impairment that might be associated with KextSG syndrome is patella alta. Researchers have identified a clear association between patella alta and increased lateral displacement and lateral tilt of the patella, particularly with a quadriceps contraction.129-131 Such patellar instability can occur with patella alta because the patella rests superior to the femoral lateral condyle, which typically prevents excessive lateral patellar glide.
In addition, patella alta may also be associated with anterior knee pain or chondromalacia in the absence of patellar instability.132-136 One potential mechanism underlying the anterior knee pain associated with patella alta is a decrease in contact area between the patella and the femur, which has been demonstrated by Ward and his colleagues.137,138 Because physical stress to biological tissue is defined as the force per unit area, any decrease in the size of the contact area at a particular joint would increase the stress on that joint, potentially leading to degenerative changes and pain.
Current evidence for the treatment of patella alta is limited to surgical intervention.131,134,136 In this chapter, we provide a conservative treatment approach for patella alta as related to the diagnosis of knee extension.
Key Tests and Signs
Alignment Analysis
The patient with Kext syndrome or KextSG syndrome may demonstrate a swayback posture with a posterior pelvic tilt. Overdevelopment of the quadriceps musculature may be apparent. In addition, patients with KextSG syndrome often demonstrate patella alta as described by Insall38 (Figure 7-33).
Movement Impairments
Standing tests
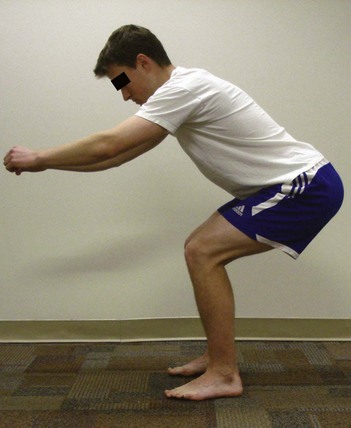
During hip and knee flexion in stance (partial squat), the patient with Kext syndrome often shifts the body weight posteriorly, keeping the tibia perpendicular to the floor (Figure 7-34). The secondary test for this movement is to instruct the patient to shift the body weight anteriorly and allow the tibia to advance forward over the foot (Figure 7-35). If symptoms are reduced, Kext syndrome should be suspected. If KextSG syndrome is suspected (pain located peripatellar or inferior to the patella), the partial squat test may be repeated as the examiner places an inferior glide on the patella. If symptoms are decreased compared to the primary test, KextSG syndrome is supported.
Supine tests
While performing the two-joint hip flexor length test,88 knee extension may be observed when the involved limb is lowered into hip extension. If the knee extension persists when the hip is brought into abduction, rectus femoris stiffness is implicated. If the patient reports pain during the test, the test may be repeated while the examiner places an inferior glide on the patella. If symptoms decrease, then KextSG syndrome is supported. The patient with Kext (without superior glide) will likely report an increase in symptoms if an inferior glide is placed on the patella, which would place additional stress on the structures superior to the patella.
Prone tests
During knee flexion in prone, patients with KextSG or Kext syndrome will demonstrate a short or stiff rectus femoris and may report pain at the end of their motion. For symptoms in the peripatellar or inferior patellar region, an inferior glide is placed on the patella during the test. A decrease in symptoms with this secondary test supports KextSG syndrome as the diagnosis. Similar to the two-joint hip flexor length test, an increase in symptoms with the inferior glide would implicate Kext syndrome (without superior glide) as the diagnosis.
Sitting tests
The McConnell test120 for patellofemoral pain may be modified to confirm KextSG syndrome. In sitting, the patient performs an isometric quadriceps contraction against resistance at 120, 90, 60, 30, and 0 degrees of knee flexion. If the patient’s pain is produced or increased during any of the contractions, the test is performed again with a manual correction by the examiner. To assess for KextSG syndrome, the examiner places an inferior glide on the patella and asks the patient to again perform the isometric contraction. If the pain is decreased, the patellofemoral joint is implicated as the source of symptoms and KextSG syndrome is implicated as the movement system diagnosis.
Joint Integrity
Patients with KextSG syndrome may demonstrate reduced accessory motion for inferior glide of the patella.
Muscle Length Impairments
Patients with KextSG syndrome or Kext syndrome demonstrate a short or stiff quadriceps during prone knee flexion or the two-joint hip flexor length tests.
Muscle Strength/Performance Impairments
Patients with KextSG syndrome or Kext syndrome often demonstrate poor performance of the gluteus maximus and hamstrings. Quadriceps musculature may compensate for the reduced performance of the hip extensors. The imbalance between the quadriceps and the hip extensors may result in an increased demand on the quadriceps to perform activities that involve extension of the lower extremity.
Stiffness, extensibility, or flexibility
The quadriceps may be short or have increased stiffness due to hypertrophy. In patients with KextSG syndrome, the quadriceps are relatively more stiff than the patellar tendon and the surrounding patellar retinacula and therefore the patella is pulled superiorly excessively. This relative stiffness/flexibility may be observed in a number of tests such as the two-joint hip flexor length test and prone knee flexion.
Functional Activities
During assessment of movements, such as walking and running, patients with Kext syndrome and KextSG syndrome demonstrate decreased knee flexion excursion, particularly between heel strike and foot flat. Reduced knee flexion excursion may also be seen while landing from a jump. While landing from a jump, the knees should flex to assist in absorbing the forces associated with the landing. Patients with Kext or KextSG syndrome often lack this knee flexion and land with a stiff knee, which may be the result of the inability of the quadriceps to elongate appropriately during the landing.
Similar to the partial squat test described earlier, the patient keeps the body weight shifted posteriorly during a step-up or squatting activity. This position may reduce the contribution of the hip extensors and increase the need for quadriceps participation. The increased quadriceps participation may result in an increased load on the patellofemoral joint or peripatellar structures.
Summary of Examination Findings
Kext and KextSG syndromes presents with stiffness of the quadriceps musculature often associated with quadriceps hypertrophy and activities that require repetitive knee extension. The two syndromes differ primarily in location of the structures in which the relative stiffness/flexibility is occurring, thus setting up those structures for injury. KextSG syndrome, the more common of the two, occurs because the quadriceps muscles pull the patella superiorly, resulting in injury in the peripatellar or infrapatellar region. Pain can be reduced by stabilizing the patella in an inferior direction during the aggravating activities. Kext syndrome is less common and often presents as a strain to the quadriceps musculature or the quadriceps tendon.
Treatment
Primary Objectives
The primary objectives of a treatment program for Kext syndrome and KextSG syndrome include the following:
Corrective Exercise Program
Treatment for this classification includes educating the patient in correcting the postural habits and movements that may be contributing to the movement impairment and thus the pain problem. The patient is provided with a general description of the impairment, including dominance/stiffness of the quadriceps and reduced performance of the hip extensors. Then, specific instruction for alignment and functional activities is provided and practiced by the patient. The patient is also instructed in exercises that will address the associated muscle impairments. Treatment described is appropriate for both Kext syndrome and KextSG syndrome, unless otherwise noted.
Functional activities
Functional activities that contribute to the movement impairment must be addressed. The functional activity that is most bothersome to the patient should be addressed first, followed by the activities in which the patient spends the most time such as work or school activities. In this chapter, we cover those activities that are useful for most patients; however, the therapist is encouraged to use the principles of the movement system to address functional activities that may not be described in this chapter.
Sitting
If the patient reports increased symptoms during sitting, he or she should be instructed to reduce the amount of knee flexion while sitting. As symptoms improve, the patient may gradually increase the amount of flexion. If superior patellar glide is contributing, the patient may be instructed to perform a manual inferior glide to the patella to decrease symptoms and to decrease quadriceps stiffness.
Gait
During gait, the patient is encouraged to improve push-off. The patient may also benefit from cues to shift their body weight slightly forward.
Sit-to-stand
To rise from a sitting position to standing, the patient should be instructed to slide forward to the edge of the chair. Once at the front of the chair, the patient should position the feet about hip-width apart and slightly posterior to the knees. The patient is instructed to flex forward at the hips to shift the COM over their feet. The patient should then contract his or her gluteals when rising from the chair while making sure the tibia advances forward over the foot.
Stairs
Similar to rising from a chair, the patient should be instructed in flexing at the hip and shifting the tibia anteriorly to bring the center of mass over the foot. As the patient rises up the step, he or she should use the gluteals to lift the body weight up and forward to ascend stairs. If the patient is unable to ascend or descend stairs without an increase in symptoms, compensatory methods may need to be provided. Please see the “Functional Activities” section in the “Tibiofemoral Rotation with Valgus Syndrome” section for methods to reduce symptoms with stair ambulation.
Fitness activities
Patients with Kext syndrome and KextSG syndrome often participate in fitness, weight training, or sporting activities. These activities may need to be modified to reduce symptoms and reduce quadriceps hypertrophy. If the person participates in weight training, quadriceps strengthening activities should be reduced, and activities to target the gluteals and hamstrings should be substituted. It is important to remember that when a muscle hypertrophies through strengthening, the stiffness of the muscles also increases.
The patient’s aerobic activities may be modified by reducing the intensity to a level appropriate for the patient’s stage for rehabilitation. The intensity is then increased gradually as the patient’s symptoms improve.
If the patient participates in jumping activities on a regular basis, jumping activities should be addressed. The patient should be instructed in achieving sufficient knee flexion during landing and to perform a soft landing. The patient should begin to practice the new strategy at low intensity levels, including small jumps and low impact landing. As the patient improves, the technique may be progressed to higher intensity jumps and landings if symptoms are not aggravated.
Home Exercise Program
Exercises to improve the performance of the gluteus maximus include prone hip extension with the knee flexed, weight shifting, standing on one leg, hip extension in standing with resistance, lunges, and squats. Care should be taken not to increase the patient’s knee symptoms with any of these exercises, particularly lunges and squats, which will incorporate quadriceps participation. The appropriate level of exercise depends on the stage for rehabilitation and the gluteus maximus strength.
Exercises to improve the extensibility of the quadriceps should also be prescribed. We recommend prone knee flexion or the two-joint hip flexor length test position. During all stretching exercises, the patient should have good abdominal support to avoid pelvic anterior tilt or transverse rotation. Patients with KextSG syndrome need to stabilize the patella during these stretches to prevent superior glide and isolate the stretch to the quadriceps. Stabilization of the patella may be accomplished by manual assistance of another person or through taping (Figure 7-36).

Figure 7-36 Horseshoe taping technique: To assist stabilization of the patella in patients with knee extension with patellar superior glide (KextSG) syndrome.
If prone knee flexion is prescribed, the patient should flex the knee only as far as he or she can without increased pain. In addition, the therapist needs to be sure the movement of the patella is not restricted by pressure against the supporting surface. In some cases, a folded towel needs to be placed under the thigh so the patella is able to move inferiorly during knee flexion.
Other Interventions
Taping and patellar mobilization may be useful in patients with KextSG syndrome. We have developed a method to reduce the pull of the quadriceps on the patellar tendon and tibial tubercle (see Figure 7-36). Patients who participate in activities that involve repetitive jumping should be taught to reinforce the taping technique, because the taping may loosen with the repetitive jumping stresses. Patellar inferior glides and mobilization with movement may be used to help improve the patellar positioning. Based on the concept proposed by Mulligan,139 a mobilization for KextSG syndrome was developed. While in the sitting position, the patient performs knee extension and flexion. During the eccentric flexion phase, the patient performs a manual inferior glide of the patella.
Case Presentation
Knee Extension with Patellar Superior Glide Syndrome
Symptoms and History
A 28-year-old male triathlete is referred to physical therapy for evaluation and treatment of left knee pain. He reports left knee pain for 5 months that was located immediately posterior to the patella. His pain began after a recent marathon. He stated that he had no pain during or after the race. He took the recommended rest after the marathon, then approximately 3 weeks after the marathon, he began to increase his running mileage in preparation for his next triathlon. After running a set of intervals, he noticed a sharp pain behind the left kneecap. He had used ibuprofen and ice with minimal relief. At the time of the examination, the patient rated his pain as a 2/10 at rest that increased to 6/10 with running. His symptoms do not appear to increase with cycling or swimming. His KOS-ADL119 score is 76%, and KOS-Sports score is 71%. No imaging was performed.
Alignment/Appearance
The patient is 6 feet 3 inches and weighs 210 pounds with a fit appearance. In stance, the patient’s alignment was unremarkable.
Movement Analysis
During a partial squat, the patient reports an increase in knee pain. No movement faults are noted. For the secondary test, the partial squat is repeated while the examiner placed a manual patellar glide in the medial direction. The patient reports an increase in knee pain similar to the previous test. The examiner asks the patient to repeat the test while the examiner placed a manual glide in the inferior direction. The patient reports no pain with the test.
Joint Integrity
Accessory motions of the patellofemoral joint were limited in the inferior direction. The patient reports no change in symptoms with the accessory motions.
Muscle Length Impairments
During the two-joint hip flexor length test, the patient demonstrated a short rectus femoris on the left. As the hip was extended, the knee extended and the patient reports an increase in his symptoms. With a manual glide of the patella in the inferior direction, the patient reports a decrease in his pain compared to the first performance. Hamstrings are short and stiff.
Muscle Strength/Performance Impairments
Using manual muscle testing, the left hip lateral rotators are 4+/5, the gluteus maximus is 4−/5, the iliopsoas is 4/5, and the posterior gluteus medius is 4+/5. Hamstring and quadriceps are strong (5/5); however, the patient reports an increase in his pain when resistance is applied to the quadriceps.
Stiffness/Extensibility/Flexibility
The rectus femoris was relatively more stiff than the patellofemoral joint causing superior glide of the patella during rectus femoris length tests.
Tests for Source
The patient reported tenderness with palpation along the medial and lateral patellar facets. There was no tenderness along the tibiofemoral joint line. The McConnell test120 and the patellofemoral grind test52,120 for patellofemoral pain were positive. During the McConnell test, the patient reported pain when resistance is applied with the knee in 60 degrees of flexion. This pain is alleviated with a manual inferior glide. All ligamentous and meniscal tests were negative.
Functional Activities
The patient reports an increase in his symptoms during a stair ascent. As he pushed off of the step with the involved limb, he kept his trunk vertical and did not flex forward at the hip. Cues to lean forward and use his gluteals to push up to the next step resulted in decreased symptoms with the step. Gait was unremarkable. During landing from a jump, he demonstrates reduced knee flexion excursion, giving a stiff knee appearance.
Diagnosis and Staging
The diagnosis is KextSG syndrome, and the stage for rehabilitation is Stage 2. His prognosis is good to excellent. Positive moderators include his young age, overall good health, high motivation to return to his activities, and his ability to change the movement impairments with instruction only. Negative moderators include his high activity level.
Treatment
The patient was seen once per week for 2 weeks, then once every other week for 2 weeks for a total of 4 visits over 7 weeks. Treatment included instruction in correct performance of functional activities, including his sporting activities. He was also instructed in a home exercise program to improve performance of the hip extensors and hip lateral rotators as well as exercises to increase the extensibility of the rectus femoris and hamstrings.
During the first visit, the patient was instructed in shifting his COM forward over the feet during functional activities such as sit-to-stand and ascending stairs. This was accomplished by leaning forward and dorsiflexing the ankle to advance his tibia anteriorly over the foot. He was then instructed to use his gluteals while extending the lower extremity to raise his body weight up to the next step.
To improve performance of the hip lateral rotators and posterior gluteus medius, sidelying hip abduction/lateral rotation with the hip and knee extended was prescribed. To improve gluteus maximus performance, prone hip extension with the knee flexed was prescribed. To accomodate rectus femoris stiffness, he performed this exercise with pillows under his hips to allow greater hip motion. He was instructed to perform the exercises one time per day. He was instructed to perform 3 sets, each set to fatigue. The repetitions depended on his ability to perform the exercise correctly. He was also instructed to stop all of the exercises that he was using to increase quadriceps strength such as resisted knee extension, lunges and squats. He was encouraged instead to substitute gluteal strengthening activities such as hip extension.
To improve extensibility of the rectus femoris, the two-joint hip flexor test position was used as a stretching technique. He was instructed to extend the hip toward the surface of the mat. Once the hip was in the final position, the patient was instructed to flex the knee. The patient was unable to perform the stretch without an increase in symptoms, so the examiner applied the taping method in Figure 7-36 to assist. With the tape applied, the patient could perform the stretch without discomfort behind the patella. He also reported feeling a good stretch in the quadriceps muscles. An alternative stretch, knee flexion in prone, was provided for the times that he could not be taped. He was instructed to flex the knee through the ROM that did not increase his pain.
Regarding his fitness program, the patient was encouraged to continue with cycling and swimming according to his training schedule. For the running component, he was encouraged to avoid interval training that involved sprints for 2 weeks. During these 2 weeks, the distance he runs should be limited to a distance that does not increase his symptoms by more than 2 points. For example, if he rated his pain at rest as 2/10 and increased to 5/10 after the run, he should reduce his distance during the next run. He was encouraged to continue using ice as needed.
The patient was also instructed in how to apply the tape appropriately. He was instructed to at minimum wear the tape during stretching and during his runs. He was encouraged to wear the tape throughout the day if possible.
At his second visit, 1 week later, the patient reported 80% compliance with the exercises and 70% compliance with the functional activity corrections. He reported that his worst pain in the last week was 2/10 after sitting for a prolonged time at a conference. He stated that the tape was helpful and discovered that he could run longer distances if the tape was in place. He demonstrated correct performance of the exercises, therefore the exercises were progressed. Sidelying hip abduction/lateral rotation and prone hip extension were progressed to standing hip abduction/lateral rotation and standing hip extension using resistance. The patient’s gym had a pulley resistance system, so he was instructed in the proper performance of the exercises using the pulley system.
He demonstrated proper performance of the two-joint hip flexor length stretch; however, he reported that he had some difficulty finding an appropriate place to perform the stretch. He would like to be able to perform the stretch before and after runs outside. He was instructed in a method to perform the stretch in a half-kneeling position (Figure 7-37). He was encouraged to maintain proper trunk alignment during performance of the stretch.
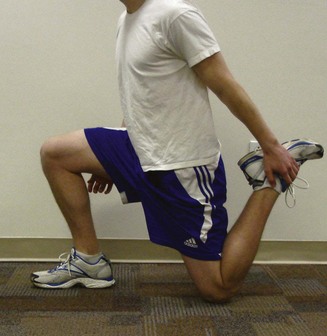
Figure 7-37 The two-joint hip flexor length stretch in half-kneeling position. May be performed in Stage 3 of rehabilitation. The patient is instructed to use the ground to prevent superior glide of the patella while performing the stretch. For patient comfort, this stretch should not be performed on a hard surface. The patient is instructed to maintain proper trunk alignment by using abdominal contraction to prevent lumbar extension and to avoid leaning forward.
On review of functional activities, such as sit-to-stand and stair ambulation, the patient was able to demonstrate the activities independently. He reported that he no longer had pain with stairs, although he was surprised when he had an increase in pain after prolonged sitting. With follow-up questioning, the patient revealed that he did not wear the tape on the day of the conference because he felt it was not needed. To address this relative stiffness/flexibility, the patient was instructed in a self-mobilization using inferior glide of the patella during knee flexion. He was instructed to perform this as often as he could throughout the day, particularly during the days he was sitting for a prolonged period of time.
At 5 weeks, the patient reported that he had no pain at rest or with his training runs. He stated that he had not used tape in the last 2 weeks and felt ready to begin interval training again. He demonstrated independence is his home program and functional activities. He was instructed in how to progress his resistance training for the hip musculature and encouraged to continue performing the stretches on a consistent basis. The strengthening and stretching routine that he typically performed before his injury was reviewed and suggestions were provided. For example, during his hamstring stretch, he demonstrated increased lumbar flexion. He was instructed to avoid lumbar flexion to isolate the stretch to the hamstrings and to avoid unnecessary stress to the lumbar spine.
The examiner agreed that he could initiate his interval training. The patient was encouraged to apply tape during the first few sessions. If he had no increase in symptoms, then he could try a session without tape.
Outcome
At the time of his last visit, 7 weeks later, the patient reported that he had returned to his preinjury training status without tape. Function was also improved as demonstrated by 100% on both KOS-ADL119 and KOS-Sports scores. He continued to perform his stretching and resistance activities. He also reported beginning a yoga class, which he felt was helpful; however, he wanted to be sure if that was appropriate. Given the patient’s inherent stiffness and high activity level, a regular stretching program would be appropriate. The examiner reviewed the poses that the patient was performing and educated him on how to modify particular poses to avoid increased stress to the joints.
Knee Hyperextension Syndrome
Knee hyperextension (Khext) syndrome is described as knee pain associated with an impaired knee extensor mechanism. Dominance of the hamstrings and poor performance of gluteus maximus and quadriceps muscles result in hyperextension of the knee placing excessive stresses on the knee. Differentiating Khext syndrome from TFR syndrome can be a challenge; therefore tests to rule out TFR syndrome should be performed before providing the Khext syndrome diagnosis.
Symptoms and History
Patients report pain located in the peripatellar region or tibiofemoral joint that is aggravated during prolonged standing or with activities that involve rapid knee extension such as swimming or kicking during martial arts. Race walkers also demonstrate Khext syndrome as they repetitively hyperextend their knee to maintain prolonged foot contact during their sport. Common diagnoses used by referring physicians include patellofemoral pain syndrome and fat pad syndrome, also called Hoffa’s disease.140
The articles that are available related to Khext syndrome are limited to describing the effect of knee alignment on structures of the knee. Loudon et al24 provided a thorough review of the relationship of knee hyperextension alignment and tissue injury. Extension of the knee is not limited by bony anatomy, thus the soft tissues of the posterior knee are primarily responsible for the resistance needed to prevent the knee from further extension. Based on the anatomy and principles of biomechanics, a reasonable assumption is that prolonged knee hyperextension during standing or repetitive hyperextension during gait could result in increased tensile stresses on the ACL and the soft tissues of the posterior knee, as well as compressive stresses on the anterior structures such at the fat pad.141
There are a few studies that demonstrate a direct association between knee hyperextension and injury. In a prospective study of female soccer players, Myer et al142 reported that knee hyperextension alignment increases the odds of sustaining an ACL injury by fivefold. In a case-control study, Loudon et al143 used conditional step-wise logistic regression to find a significant correlation between knee hyperextension alignment and ACL injury. There is also evidence that women with hyperextension of the knee may have reduced knee joint position sense that may reduce the individual’s ability to control end-range knee extension movements.144
Although knee hyperextension alignment is implicated in knee injury and pain, an individual with Khext syndrome can demonstrate signs of hyperextension during other tests such as gait and stair ambulation. The diagnosis of Khext syndrome should not be given based on alignment alone.
Key Tests and Signs
Alignment Analysis
Individuals with Khext syndrome often demonstrate knee extension greater than 5 degrees in standing (Figure 7-38). They may also demonstrate a swayback posture with a posterior pelvic tilt and ankle plantarflexion. Correction of the standing alignment may result in a decrease in the patient’s symptoms.
Joint Integrity
Patients in this category may demonstrate a general joint hypermobility as assessed by the Beighton index145; however, this is not a requirement. Some patients appear to have general laxity of the ligaments, yet their Beighton index is relatively low. The patient may demonstrate knee extension PROM that is greater than 10 degrees; however, in acute flare-ups of the condition, the patient may actually demonstrate a reduction in knee extension compared to the uninvolved side. This is thought to be a protective mechanism to reduce stresses to the injured structures.
Muscle Length Impairments
The patient may have a short or stiff gastrocnemius; however, these limitations are not seen in all patients with Khext syndrome. Hamstring shortness is often associated with this syndrome.
Muscle Strength/Performance Impairments
Impairments of muscle strength and performance include poor performance of gluteus maximus and quadriceps. The gluteus maximus often tests weak during manual muscle testing (MMT) and demonstrates delayed recruitment during activities such as prone hip extension with the knee extended. The gluteus maximus should contract early in the motion of limb movement during prone hip extension. A notable delay in gluteus maximus contraction may indicate that the hamstrings are acting as the primary hip extensors for the hip movement. The quadriceps often tests strong during a MMT; however, the patient may display poor functional use of the quadriceps during activities such as a step-up or sit-to-stand as evidenced by the patient pulling his or her knees back to the body.
Functional Activities
Gait
During gait, the patient may demonstrate hyperextension from heel strike through late stance. The patient may also demonstrate a prolonged foot flat, keeping their heel in contact with the floor longer than expected. Noyes et al146 described this gait pattern in patients with posterolateral ligament complex injuries; however, this pattern has been observed in symptomatic patients without documented ligamentous injury.
Step-up
During a step-up, the patient demonstrates a faulty movement of pulling the knee back to the body, instead of shifting the body forward over the limb. This motion is achieved by using the hamstrings more than the quadriceps and gluteus maximus to extend the hip and the knee. Because the foot is anchored on the floor, hip extension performed by the hamstrings results in knee extension and therefore reduces the need to recruit the quadriceps to extend the knee.
Summary of Examination Findings
Khext syndrome presents with the movement impairment of knee hyperextension during alignment, movement tests, and functional activities. A special note related to secondary tests for Khext syndrome is that patients with this syndrome often have a chronic condition that does not always modify immediately with secondary tests. The patient may need to try modifications for a period of time to see the effect. For example, the patient may report no change in symptoms with correction of standing alignment; however, if standing alignment is modified while at work, symptoms may improve dramatically.
Differentiating between Khext syndrome and tibiofemoral rotation syndrome can be challenging. If signs for both Khext syndrome and tibiofemoral rotation syndrome are observed, the therapist should follow treatment guidelines for tibiofemoral rotation syndrome, which provides treatment related to the rotation component and also addresses the hyperextension component. Khext syndrome should be reserved for those displaying the movement impairment in the sagittal plane only.
Treatment
Corrective Exercise Program
Treatment for this syndrome includes educating the individual in correcting the postural habits and movements contributing to the movement impairment and thus the pain problem. The patient is provided with a general description of the impairment and specific instruction for alignment and functional activities. Then the functional activities are practiced by the patient. The patient is also instructed in exercises that will address the associated muscle impairments.
Alignment
First, the patient is educated in correction of posture and functional activities. To improve alignment between the femur and tibia, the patient is instructed to relax or unlock the knees to reduce hyperextension of the knee. If the patient stands in a posterior pelvic tilt, this should also be corrected. A mirror is useful during correction of the alignment. Patients often report that their position of hyperextension feels “normal,” and the correction feels as if their knees are too flexed as in a partial squat. The mirror reinforces the proper alignment of the knee.
Functional activities
Gait
During ambulation, the patient is encouraged to use a proper heel-to-toe gait pattern and to land softly on the heel at heel strike. The patient is also instructed to avoid knee hyperextension and hip hyperextension during the stance phase of gait cycle. Most patients with knee hyperextension have a delayed heel rise at push-off; therefore a helpful cue is to ask the patient to lift the heel a little earlier than usual. Another useful cue, as described by Noyes et al,146 is to walk with the knee slightly flexed.
Sit-to-stand/stairs
During sit-to-stand and stairs, the patient is instructed to use the quadriceps and gluteus maximus to lift the body up and forward and to avoid pulling the knee(s) back to meet the body. The final position of the knee should be a neutral position not hyperextended. If the patient is unable to ascend or descend stairs without an increase in symptoms, compensatory methods may need to be provided. Please see the “Functional Activities” section the “Tibiofemoral Rotation with Valgus Syndrome” section for methods to reduce symptoms with stair ambulation.
Standing
Patients with Khext syndrome often report increased symptoms with prolonged standing. They should be instructed in correcting their alignment during stance and to reduce the amount of time that they stand in one position. They should be encouraged to change their activities as often as possible, including sitting, walking and leaning into a support surface. If they are in a situation that does not allow them to change their activity, weight shifting provides some temporary reduction in stresses on the knee.
Fitness activities
If the patient does not have a fitness program, then a discussion is warranted to encourage a fitness program as a goal. If the person participates regularly in a fitness program, modification may be necessary. The patient’s aerobic activities may need to be modified by addressing the movement impairment and by reducing the intensity. The intensity level of the aerobic activity should be related to the patient’s stage for rehabilitation. For example, if the patient is a speed walker and the injury is Stage 1 for rehabilitation, the patient may be instructed to use a bike, walk in a pool, or start with a slower walking pace or shorter walking distance. The intensity is then gradually increased. As the patient’s symptoms improve, the patient should begin to increase the walking distance and then increase the speed.
Home Exercise Program
Exercises to improve strength and performance of the gluteus maximus and quadriceps may be prescribed. To improve gluteus maximus performance, exercises, such as prone hip extension with the knee flexed, weight shifting, single-leg stance, and resisted hip extension, are prescribed. When performing prone hip extension with the knee flexed, the patient should have at least one pillow under the abdomen so that the exercise is performed from some hip flexion to neutral and not into hip hyperextension. Functional activities that can be used as exercise to improve gluteus maximus and quadriceps performance include sit-to-stand, wall sits, step-up/step-downs, lunges, and squats. Abdominal muscle exercises may also be appropriate if the patient demonstrates poor trunk and/or pelvic control.
Sitting knee extension with ankle dorsiflexion is an exercise that can be performed easily throughout the day to improve the extensibility of the hamstrings and gastrocnemius. The gastrocnemius can be stretched with prolonged passive ankle dorsiflexion in standing, and the hamstrings can be stretched with prolonged knee extension in the sitting position (see Figure 7-40). To properly stretch the hamstrings, be sure that the spine does not flex.
Taping
Taping may be useful in patients with knee hyperextension. The posterior X taping demonstrated in Figure 7-27 to treat TFRVal syndrome will also assist with preventing Khext syndrome. If the fat pad is very irritable, it may be helpful to try the unloading taping technique proposed by McConnell (Figure 7-39).
Neuromuscular Training
Neuromuscular training to improve proprioception, balance, and the ability to accommodate to perturbations is important (see Box 7-2). During neuromuscular training, the patient is instructed to limit the amount of knee hyperextension.
Case Presentation
Knee Hyperextension Syndrome
Symptoms and History
A 35-year-old female is referred to physical therapy for evaluation and treatment of left knee pain. She reports two previous bouts of similar pain that resolved fairly quickly without intervention. However, this episode began approximately 3 weeks ago and has not improved. The pain is located in the posterior aspect of her knee and just inferior to the patella deep in the joint. She has participated in competitive race walking for the past 3 years. Initially, her pain would only occur during races or when training, but the pain progressed to occurring with daily walking and stair ambulation. Her pain forced her to stop race walking approximately  weeks ago, and she is very anxious to return to this activity. Her pain rating at the time of the initial visit was 3/10 with daily activities and increases to 6/10 if attempting to race walk. She describes her pain as a deep aching in the posterior knee that becomes sharper when race walking. Nothing seems to give her relief except taking Ibuprofen. Her KOS-ADL119 score is 51%, and KOS-Sports score is 40%. Radiographs show no abnormalities of the tibiofemoral or patellofemoral joint. She also states that she has a 2-year-old daughter who she tends to carry on her left hip. She was working part-time as a business consultant.
weeks ago, and she is very anxious to return to this activity. Her pain rating at the time of the initial visit was 3/10 with daily activities and increases to 6/10 if attempting to race walk. She describes her pain as a deep aching in the posterior knee that becomes sharper when race walking. Nothing seems to give her relief except taking Ibuprofen. Her KOS-ADL119 score is 51%, and KOS-Sports score is 40%. Radiographs show no abnormalities of the tibiofemoral or patellofemoral joint. She also states that she has a 2-year-old daughter who she tends to carry on her left hip. She was working part-time as a business consultant.
Alignment Analysis
The patient is 5 feet 6 inches and weighs 135 pounds. In stance, the patient demonstrated tibial varum and genu recurvatum bilaterally; however, both faults were greater on the left compared to the right. She had a flat lumbar spine, posterior pelvic tilt, and hip joint hyperextension with a mild swayback alignment.
Movement Analysis
During single-leg stance on the left, the patient demonstrates increased knee hyperextension. The patient did not report an increase in pain, although she does express a feeling of instability compared to standing on the uninvolved limb. The patient also demonstrates a pelvic lateral tilt (Trendelenburg sign) during single-leg stance bilaterally; however, she demonstrated more tilt during single-leg stance on the left than on the right.
During a step-up onto a 12-inch stool, the patient kept her COM posterior to her base of support and snapped her knee back to her body using her hamstrings. She reported a mild increase in symptoms during this test. She was cued to lean forward to bring her COM over her foot, and to think about using her quadriceps and gluteals as she stepped up. She performed the step-up correctly by following the cues provided. She reported that her symptoms did not increase with the corrected method.
Joint Integrity
Knee extension PROM tested in supine is 15 degrees on the left and 10 degrees on the right. The patient’s tibiofemoral joints are mildly lax compared to normal, which was noted particularly during prone hip rotation testing, during which the leg motion was particularly evident.
Muscle Length Impairments
Hamstring length is tested and found to be short bilaterally with 70 degrees passive straight leg raise. Gastrocnemius length was also short bilaterally, measuring 10 degrees ankle dorsiflexion with the knees flexed and 0 degrees with the knees extended.
Muscle Strength/Performance Impairments
On the left side, the gluteus maximus MMT reveals a grade of 4/5 and shows a delayed onset compared to the hamstrings during hip extension with the knee extended. The left quadriceps MMT grade is 5/5, although poor functional performance is suspected. For example, during a wall squat the left quadriceps fatigued more readily than the right, with notable muscle quivering after only 10 seconds. The posterior gluteus medius MMT grade is 4−/5 bilaterally.
Tests for Source
The patient reports tenderness with palpation distal to the inferior pole of the patella in the region of the fat pad on the left. Mild tenderness is also noted on the posterolateral aspect of the knee. All ligamentous and meniscal tests are negative.
Functional Activities
During sit-to-stand and stair ambulation, the patient demonstrates the tendency to pull her knees back to the body using her hamstrings, rather than keep her COM over her feet and use her quadriceps to extend her knees. Increased symptoms are elicited on the left after completing one flight of stairs. The patient is cued to lean forward and to get her shoulders over her feet while concentrating on not hyperextending her knees. Although she has some difficulty performing the stair ambulation correctly with these cues, the patient reports no aggravation of her symptoms. Gait deficits noted are knee hyperextension from heel strike through terminal stance with a delayed heel rise bilaterally. When cued to decrease the knee hyperextension and attempt an earlier heel rise, the patient has trouble trying to change her gait pattern and becomes a little frustrated. A bilateral hip drop is also noted during gait.
Diagnosis and Staging
The diagnosis is Khext syndrome. The stage for rehabilitation is Stage 2. Her prognosis is good to excellent. Positive moderators include her fairly young age, overall good health, and high motivation to return to her activities. Negative moderators include her difficulty making corrections during alignment and functional activities and her anxiety about wanting to return to race walking, a sport that encourages knee hyperextension by demanding that one foot be in contact with the ground at all times.
Treatment
The patient was seen twice per week for 2 weeks secondary to taping needs, then decreased to once per week for 4 weeks for a total of 8 visits over 6 weeks. Treatment included instruction in correct performance of functional activities, including speed walking. She was also instructed in a home exercise program to improve performance of the hip abductors, gluteus maximus, and quadriceps, along with exercises to increase the extensibility of the hamstrings, gastrocnemius, and soleus muscles. Although she reported pain only in the left knee, she was encouraged to perform the exercises bilaterally.
During the first visit, the patient was instructed to correct her standing alignment of knee hyperextension by relaxing her knees. A mirror was needed for visual feedback of her alignment. Her tendency at first was to excessively flex her knees, and she found it very difficult and tiresome to maintain normal alignment. Therefore it was decided to perform the posterior X taping technique to provide an external source of feedback to her when she would start to hyperextend her knees (see Figure 7-27). The patient was instructed to keep the tape on for 1 to 3 days if tolerated and to check her skin carefully when the tape was removed. Assuming there would be no skin reactions, the plan was for her to return at the end of the week to be re-taped.
She was instructed to try alternating the hip she used for carrying her child, instead of always holding her on the left. Holding her child on the left hip resulted in prolonged positioning of hip adduction and pelvic lateral tilt. This prolonged positioning may have contributed to her hip weakness and increased knee hyperextension on the left. The patient was instructed in performance of sit-to-stand, attempting to get her shoulders over her feet and prevent hyperextending her knees when completing the standing maneuver. This task was easier for her to correct than gait or stair climbing during the first session.
To improve the functional performance of the quadriceps, the patient was instructed in a wall squat exercise. She assumed a position of about 45 degrees hip and knee flexion and was instructed to start by maintaining the position for 15 seconds and to perform 5 repetitions. Each day she was to try to add 5 seconds onto her hold time during the first week. She was also cued to avoid hyperextending her knees when returning from the squat position to the hip and knee extended position.
To begin to improve the performance of her gluteus maximus, the patient was instructed to forward bend by hip flexion only with knees flexed and practice returning by contracting her gluteals to lift her upper body. She was also given the exercise of prone hip extension over 3 or 4 pillows to help place her in enough hip flexion so that her knee could stay relaxed in flexion as she extended her hip using her gluteus maximus. She was instructed to perform the exercise one time per day. She was instructed to perform 3 sets, each set to fatigue. The repetitions depended on her ability to perform the exercise correctly.
To improve the recruitment of the posterior gluteus medius, the patient was instructed in weight shifting. She was instructed to avoid pelvic tilting and knee hyperextension as she shifted. The patient had difficulty maintaining the appropriate pelvic position, so she was encouraged to place her hands on her ASIS to monitor the pelvic alignment. She was then able to perform the activity correctly. She was also encouraged to maintain the trunk in a neutral position and avoid sidebending. She was instructed to perform this exercise frequently throughout the day, if possible.
To address her limitations in hamstring extensibility, she was instructed to sit on the edge of a chair with one leg extended and to lean forward from her hips keeping her spine straight until she felt an appropriate stretch to her hamstrings. Because her knee would easily assume a hyperextended position, the patient had to make a conscious effort to keep the knee relaxed in slight flexion during the stretch (Figure 7-40). While stretching her hamstrings, she was also instructed to try to dorsiflex her ankle without toe extension to provide an additional stretch to her gastrocnemius. The patient was instructed in the typical standing wall stretch for the gastrocnemius as well.
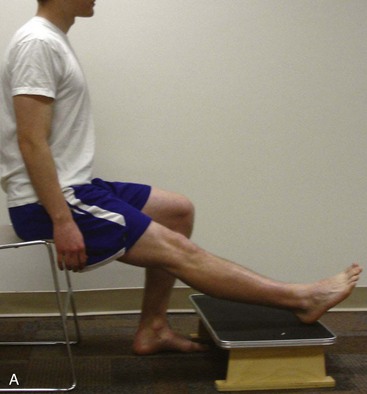
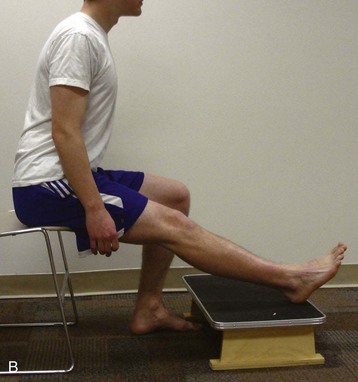
Figure 7-40 Hamstring stretching. Proper performance of hamstring stretch provided to the patient. A, The patient sits on the edge of a chair with one leg extended. B, The patient then leans forward from the hips, keeping the spine straight until an appropriate stretch is felt.
At her second visit, she reported 75% compliance with the exercises and about 50% compliance with the functional activity corrections, which were still hard for her. She stated that the tape behind her knees was definitely helpful in relearning how to stand properly. She was able to wear the tape for 2 days and had no skin reaction, so she requested to have the tape applied again at that visit. Her symptoms had decreased to 2/10, and she reported less pain with stair ambulation.
She demonstrated correct performance of the exercises, therefore the exercises were progressed. With the wall squat, she was now able to sustain the position for 30 seconds before fatiguing. This exercise was progressed by having her place her right foot slightly in front of her left, forcing her to increase the load to her left quadriceps. Her weight shifting was progressed to single-leg stance with light upper extremity support and using all the previous cues. An additional exercise was given to her for the posterior gluteus medius. She was instructed in the side lying hip abduction/lateral rotation exercise. Two to three pillows were placed between her legs and her top leg was aligned in 10 to 20 degrees of hip and knee flexion. When the patient attempted to abduct her hip off the pillows, she reported feeling muscles working in her posterior thigh so it was determined that she was substituting with her hamstrings. With much verbal and manual cueing and specific palpation of her posterior gluteus medius, she was able to perform this exercise correctly. The patient was encouraged to start with five repetitions and progress toward ten, only if she could feel the muscle recruitment in the correct location. Because she was performing her prone hip extension exercise correctly, she was encouraged to add more repetitions.
The patient was re-taped and her gait deviations were addressed with the tape applied. The main cues given to her were to lean forward slightly while walking, take smaller strides and lift her heel earlier at terminal stance. Her attempts at these corrections were better than at her first visit, although she felt very awkward. The patient was instructed to continue with the other exercises, trying to be diligent about her hamstring stretching throughout the day.
At the fifth visit during the third week, taping was discontinued because the patient felt she was now able to control the knee hyperextension on her own. The patient reported 0/10 symptoms at that time with walking and with stair ambulation. She admitted to trying to race walk for a short distance but developed low level symptoms so she decided she was not quite ready. At this visit, she was progressed to level 3 of the posterior gluteus medius progression. She was now able to perform single-leg stance without any upper extremity support, so the activity was progressed by performing single-leg stance on an unstable surface starting with pillows and progressing to foam pads and a BOSU ball. She also began standing lunges and step-ups to strengthen her gluteals and quadriceps more functionally, monitoring her movement pattern to be sure she was not using her hamstrings to pull her knee back to her body.
During her sixth visit in the fourth week, she began to practice walking with increased speed while trying to still work on the specific gait cues she had now been practicing for a few weeks. As long as she did not go too fast, she was able to achieve some corrections and did not experience an increase in symptoms. She was progressed to playing catch with a weighted medicine ball while balancing on one leg on the BOSU ball. Also, she now added 5 pound weights in each hand while performing her lunges and step-ups.
Outcome
The patient was seen for a total of 8 visits over 6 weeks. At her last visit, the patient reported that she could race walk for 1 mile without aggravating her symptoms, although she stated that she was not yet up to her previous speed. She reported that it was impossible to prevent the hyperextension as her speed increased. Since she was determined to continue participation in this sport, she was instructed to work on her gait corrections as much as possible throughout the rest of the day, when not race walking. Function was also improved as demonstrated by a KOS-ADL score of 93% and a KOS-Sports score of 84%. She was instructed to continue her home exercise program daily, if possible, even when she was totally pain-free with all activities and to think of it like “brushing her teeth.” It was explained to her that if she would stop the exercises, her pain would likely return after a period of time. The patient had no problem with this commitment, and she was discharged from physical therapy.
Patellar Lateral Glide Syndrome
Patellar lateral glide (PLG) syndrome is described as knee pain as a result of an impaired patellar relationship within the trochlear groove. Patients with PLG syndrome have an imbalance between the vastus medialis oblique (VMO) and the vastus lateralis (VL) muscles that may place excessive compressive forces in the lateral patellofemoral joint and tensile forces on the medial joint structures. Shortness or stiffness of the TFL-ITB complex may also contribute to a lateral pull on the patella. A similar syndrome has been described by McConnell.87
Symptoms and History
Patients with PLG report peripatellar or retropatellar pain with activities such as stairs, running and squatting. They may also report an increase in symptoms with prolonged knee flexion when sitting, often called movie goers syndrome. PLG rarely occurs in isolation and is often a secondary diagnosis associated with a primary diagnosis of tibiofemoral rotation or knee hyperextension. Common diagnoses used by referring physicians include patellofemoral pain syndrome and patellar chondromalacia.
There is a large body of literature related to the relationship of the VMO and patellofemoral pain; however, the relationship has not been clearly established. A number of authors have reported that patients with patellofemoral pain demonstrate poor performance of the VMO when compared to those without symptoms.147-151 There are, however, others that report there is no difference in VMO performance between those with and without patellofemoral pain.152-155 The inconsistent findings demonstrate a need for classification by movement impairment. Subjects with patellofemoral pain are often included in these studies based on pain location; the movement impairment associated with the pain complaint is not considered. Patients with TFRVal syndrome and patients with PLG syndrome may report a similar pain in the peripatellar region, although they may display dissimilar movement impairments. A relationship between VMO performance and patellofemoral pain may exist in individuals with PLG syndrome but may not exist in individuals with TFRVal syndrome. Classification by movement impairments may assist in clarifying the research findings.
Clinical trials of treatment that incorporate VMO strengthening have demonstrated positive results102; however, the isolated treatment effects of VMO strengthening are not known. Often these clinical trials include additional treatments, such as stretching and taping, therefore it is difficult to determine the effectiveness of VMO strengthening alone. Recently, authors have demonstrated that increasing the VMO force can decrease the pressure on the lateral patellofemoral joint articular cartilage.156
Key Tests and Signs
Alignment Analysis
The patient with PLG syndrome may demonstrate a lateral patellar tilt or lateral patellar glide.
Movement Impairments
Standing tests
During hip and knee flexion in stance (partial squat), the patient may report an increase in their symptoms; however, a movement impairment may not be apparent. A secondary test is performed by asking the patient to repeat the movement while the examiner places a medial glide on the patella. If symptoms are decreased compared to the primary test, PLG is supported.
Supine tests
Patients with PLG syndrome may report an increase in symptoms during the performance of the two-joint hip flexor length test.88 The test is then repeated while the examiner places a medial glide on the patella. If symptoms decrease, then PLG syndrome is supported. Symptoms may also be decreased by abducting the hip, therefore reducing the stretch on the TFL-ITB.
Prone tests
During knee flexion in prone, patients with PLG syndrome may report pain at the end of their motion. Decreased symptoms when a medial glide is placed on the patella supports the diagnosis of PLG syndrome. Similar to the two-joint hip flexor test, placing the hip into abduction reduces the stretch on the TFL-ITB, which may result in a decrease in the patient’s symptoms.
Sitting tests
During knee extension in sitting, the examiner may observe sudden lateral movement of the patella near the end of the knee motion, a motion often referred to as a positive J-sign. This excessive lateral patellar motion may also be seen during an isometric quadriceps contraction.
A McConnell test120 for patellofemoral pain may be performed to assess for PLG syndrome. In sitting, the patient performs an isometric quadriceps contraction against the therapist’s resistance at 120, 90, 60, 30, and 0 degrees of knee flexion. If the patient’s pain is produced or increased during any of the contractions, the test is performed again with a manual correction by the examiner. To prevent patellar lateral glide, the examiner places a medial glide on the patella and the resisted test is repeated. If the pain is decreased, the patellofemoral joint is implicated as the source of symptoms and PLG syndrome is implicated as the movement impairment.
Joint Integrity
Patients with PLG syndrome may demonstrate reduced accessory motion for medial glide of the patella.
Muscle Length Impairments
Patients may demonstrate short and/or stiff TFL-ITB and lateral patellar retinaculum. Though not common, sometimes a short and/or stiff gluteus maximus with attachment to the ITB may contribute to the lateral pull of the patella.
Muscle Strength and Performance Impairments
Although weakness of the VMO may contribute to PLG, clinical testing specific to the VMO is not possible. Other characteristics of muscle performance such as muscle timing or endurance have also been suspected to contribute to PLG. Muscle timing and endurance are also difficult to observe clinically. Laboratory measurements, such as electromyography (EMG), may assist in identifying an imbalance in the timing of contraction between the VMO and VL; however, EMG is often not practical in the clinic.
Functional Activities
During performance of functional activities, observation of the movement impairment of PLG syndrome is often difficult; however, secondary tests can be used to support the diagnosis. For example, during activities such as sit-to-stand or step-up, a medial glide may be placed on the patella. If the patient’s symptoms are reduced compared to the primary test, then PLG syndrome is supported as the diagnosis.
Treatment
Corrective Exercise Program
Treatment for PLG syndrome includes educating the individual in correcting the postural habits and movements that may be contributing to the movement impairment and thus the pain problems. The patient is provided with a general description of the impairment and specific instruction for alignment and functional activities. The activities are then practiced by the patient. The patient is also instructed in exercises that will address the associated muscle impairments.
Functional Activities
Sitting
If a patient reports increased symptoms during sitting, the instruction is to reduce the amount of knee flexion while sitting. If the patient has a stiff or short gluteus maximus contributing to the stiffness of the ITB, resulting in PLG, the thighs should be slightly abducted initially. As symptoms improve, the thighs should be gradually adducted until the sitting position is normal and does not cause symptoms. Patients should be encouraged to get out of their chair and flex/extend their knee every 30 minutes to reduce the amount of time the knee is maintained in a flexed position. Patients should also limit the amount of time spent with their legs crossed.
Sit-to-stand
To rise from a sitting position to standing, the patient should be instructed to slide forward to the edge of the chair. Once at the front of the chair, the patient should position the feet about hip-width apart and slightly posterior to the knees. The patient is instructed to contract the quadriceps when rising from the chair. If this motion is painful, the patient may use the hands to assist by pushing up from the armrests of the chair.
Stair ambulation
Similar to rising from a chair, the patient should be instructed to use the quadriceps and gluteals to ascend the stairs. If the patient is unable to ascend or descend stairs without an increase in symptoms, compensatory methods may need to be provided. Please see the “Functional Activities” section in the “Tibiofemoral Rotation with Valgus Syndrome” section for methods to reduce symptoms with stair ambulation.
Fitness activities
Recommendations related to fitness are provided in the “Functional Activities” section in the “Tibiofemoral Rotation with Valgus Syndrome” section.
Home Exercise Program
The patient should be provided with a home exercise program and instruction on the appropriate response to exercise. Exercises specific to PLG syndrome to improve the performance of the quadriceps may be prescribed. We recommend the use of functional activities to improve quadriceps performance. Those exercises, in the order of difficulty beginning with least aggressive, are sit-to-stand transfers, step-ups, lateral step-ups, squats, lunges, and step-downs. Ekstrom et al157 demonstrated that lunges and lateral step-ups produced greater EMG activity in the VMO compared to other rehabilitation exercises. Biofeedback to improve timing or recruitment of the VMO may be a useful intervention102,158,159; however, more clinical studies are needed. In addition, we recommend avoiding open-chain resisted activities in the range of 0 to 45 degrees of flexion and closed-chain activities in the range of 60 to 90 degrees, since these ranges are thought to result in increased stresses to the patellofemoral joint.160
Exercises to improve the extensibility of the TFL-ITB should also be prescribed. We recommend prone knee flexion (either unilateral or bilateral) or stretching in the two joint-hip flexor length test position. During prone knee flexion, the patient should initially perform with the involved hip in abduction to reduce the pull of the ITB. As symptoms improve, the amount of hip abduction is reduced.
The two-joint hip flexor stretch position may be used as the patient’s symptoms improve. As the involved limb is lowered into extension, the hip should be allowed to abduct. Once the hip is in extension, the hip can then be adducted to add the stretch to the TFL-ITB. Assuming normal anatomy of the femoral lateral condyle, the patella will be secured within the trochlear groove prior to adding the stretch of the TFL-ITB.
Patients must not feel pressure or pain in the location of their symptoms during the stretches. If the symptoms occur, the patella is most likely being mobilized and the stretch will not be effective. Patients with PLG syndrome may need to stabilize the patella during these stretches. Stabilization of the patella may be accomplished by manual assistance of another person or through taping (Figure 7-41). During all stretching exercises, be sure that the patient has good abdominal support to avoid pelvic anterior tilt or rotation. Strengthening the muscles that are antagonists of the TFL-ITB, such as the posterior gluteus medius and gluteus maximus, may also help to improve TFL-ITB extensibility.

Figure 7-41 Taping technique. Taping to reduce patellar lateral glide as proposed by McConnell.87 The patella is pushed medially by the tester and strips of tape are placed along the patella, anchored around the medial hamstring muscle bulk.
Other Interventions
Taping and patellar mobilization may be useful in patients with PLG syndrome. Taping to reduce patellar lateral glide as proposed by McConnell87 has had clinical success (see Figure 7-41). The evidence consistently supports that taping helps to reduce symptoms,87,161-165 although the mechanism behind the symptom reduction has not been determined. Many believe that tape is applied to either change the alignment of the patella or improve the performance of the VMO; however, the literature is mixed.161,166-172 Although the mechanism is not clear, taping is a safe and relatively convenient intervention that has had clinical success.
Patellar mobilizations in the medial direction may be used to help improve the extensibility of the lateral structures such as the patellar retinaculum and ITB. If the patient is in Stage 1 of rehabilitation, gentle mobilizations may be performed to reduce pain and to initiate mobility in the medial direction. As the patient’s symptoms subside, aggressive grades of mobilization should be used to increase extensibility. Patients may be instructed in self-mobilizations to perform along with their home exercise program.
Knee Impairment
Thus far, the focus of this chapter is on the identification and treatment of specific movement system syndromes for the knee. However, patients are commonly referred to physical therapy for rehabilitation of the knee after a surgical procedure or after an acute, traumatic knee injury. When a patient presents to therapy after either a surgical procedure or an acute knee injury, identification of a specific movement system syndrome using a thorough examination may not be possible because of pain, physician-imposed restrictions, or both. In such cases, the physical therapist must recognize the potential pathoanatomical structure(s) involved, perform a limited problem-centered examination to identify specific impairments, and provide treatment that is congruent with the stage for rehabilitation determined according to the guidelines outlined in Chapter 2.
In general, patients for which a movement system syndrome cannot be determined are classified as having a knee impairment, which is a broad term that encompasses a wide array of structural impairments or injuries. An exhaustive discussion of the potential knee injuries a physical therapist might treat and the surgical procedures after which a patient may be referred to physical therapy is beyond the scope of this text. However, to provide optimal care for the patient, the physical therapist must have a thorough understanding of the possible structures of the knee implicated for a particular injury and be familiar with common surgical procedures used by referring physicians. See the Chapter 7 Appendix for additional information regarding specific tissue properties of the structures of the knee, as well as treatment guidelines for each stage of rehabilitation.
Because the knee impairment classification is relatively nonspecific, the physical therapist should provide a source diagnosis, if possible, to guide treatment. Recall from Chapter 2 that if a movement system diagnosis cannot be determined, the diagnosis made by the physical therapist is based on the pathoanatomical structure involved, as identified by the physician; the procedure performed, if any; and the stage for rehabilitation. For example, if a patient presents to physical therapy 3 days after an ACL reconstruction, the diagnosis made by the physical therapist would likely be as follows: ACL tear, status/post ACL reconstruction, Stage 1. If the specific pathoanatomical structure cannot be determined or has not been specified by the physician, the classification of knee impairment should be used to identify the region of the body that is impaired, with an appropriate stage for rehabilitation.
As the patient progresses with physical therapy after an acute injury or surgical procedure, the physical therapist should attend to any underlying movement impairments that either develop or are identified with a more thorough examination. If a movement system syndrome can be determined, the physical therapist should use this diagnosis, with the appropriate stage for rehabilitation, to guide treatment relative to specific movement impairments. If no underlying movement impairment can be determined, the physical therapist should continue to progress treatment as tolerated according to the stage for rehabilitation associated with the source diagnosis provided.173,174
Conclusion
This chapter offers the reader the diagnostic framework to effectively evaluate and treat chronic, acute, and postsurgical knee pain. By specifically identifying movement impairments and considering the tissue characteristics of pathoanatomical structures in the knee, the physical therapist can be more readily prepared to provide optimal treatment and education to patients who present with knee pain than attempting to develop a program without identifying an underlying syndrome.