Chapter 8 Movement System Syndromes of the Foot and Ankle
Introduction
Use of the movement system classification in the examination and treatment of musculoskeletal pain problems of the foot and ankle starts with the basic premise that a large component of the stress that causes tissue injury is the result of movement. Movement results in injury and pain because the motion is completed in an imprecise manner (excursion is excessive, insufficient, and/or asynchronous with the functional requirements) and/or the repetitions of the motion or the duration the posture is maintained exceeds the tissue’s capabilities. The physical therapist examines muscle length and performance, structural variations, and the ease and excursion through which the foot, ankle, knee, hip, and spine move. The physical therapist determines the component impairments contributing to injurious motions and/or forces at unsuitable distal or proximal anatomical sites within the foot and entire lower extremity. Daily activities and habits of the patient are also assessed. Additionally, the physical therapist considers the impact of body weight, age, foot size, and disease on the foot and ankle.
The foot and ankle have very complex and often opposing functional responsibilities during weight-bearing activities. The foot and ankle must be flexible to adapt to uneven surfaces, transfer high forces, and allow motion of the body in multiple directions around a planted foot. During weight-bearing activities, the foot must quickly transform into a rigid lever that allows muscular contractions to propel the body forward, upward, sideways, or any combination of these motions. The foot also has an important role in balance; sensing body location and maintaining an upright posture.
The most common movement system syndromes of the foot and ankle injury are related to the inability of the foot to function equally well as a flexible adapter (requiring motion in the direction of pronation) and a rigid lever (requiring motion in the direction of supination). The injured foot often falls toward an extreme of one of these two roles (either a great flexible adapter with poor ability to transform to a rigid lever or a rigid lever with limited flexibility). The movement impairment often presents as excessive or incorrect timing of the normal motions of pronation and/or supination.
This chapter outlines key principles involved in the assessment of alignment, structural variations, movement, and tests of muscle length and strength. The syndromes are described, and suggestions for associated impairments in the hip and knee are mentioned. Additionally, treatment for restoring precise motion through limiting hypermobility, addressing limitations in joint and muscle extensibility, and training for the change in movement in daily activities and habits is provided.
Alignment of the Ankle and Foot
Ankle
The joints of the ankle include the proximal tibiofibular joint, distal tibiofibular joint, and the talocrural joint. The fibula has a limited weight-bearing function but serves as the attachment of the biceps femoris and fibular collateral ligament (lateral collateral ligament). Additionally, the fibula has a role in increasing torsional stiffness (rotational stability) of the lower limb.1 The alignment of the fibula at the proximal and distal tibia is challenging to assess. The determination of normal or impaired alignment is generally by comparison to the other side.
Foot progression angle (toe-out angle) during gait is an important alignment factor to consider in the assessment (Figure 8-1). The normal values for foot progression angle are between 7 to 13 degrees.2 The foot progression angle is the result of rotation at the hip joint, rotation at the tibiofemoral joint, femoral torsion, and/or tibial torsion. The contribution of rotation at the hip or tibiofemoral joints is determined by assessing joint alignment. Femoral and tibial torsion can be more difficult to determine. The assessment of femoral torsion, the twist of the femur in the transverse plane, is discussed in detail in the chapter on the hip in Sahrmann.3
Tibial torsion, the twist of the bones of the tibia and fibula in the transverse plane, is often implicated in the predisposition of the lower extremity to injury. The normative data describe tibial torsion as usually between 20 to 40 degrees of lateral rotation.4-6 The measurement techniques to collect normative data have generally used radiological images or cadaveric analysis. The external landmarks available for use by clinicians in determining torsion are generally poor. Use of femoral landmarks for the proximal alignment of the tibia and fibula compared to the medial and lateral malleoli7 does not allow differentiation of lateral rotation at the tibiofemoral joint from torsion of the bones of the lower leg. Use of the tibial tuberosity and attempts to palpate the tibial condyles to determine proximal alignment is limited by variances in anatomy and difficulty in finding the tibial condyles. Because of the limitations in the nonradiological determination of tibial torsion, the clinically measured value should not be relied on, but general approach should be taken that considers the overall impact of foot progression angle on the function of the foot.
An increase in the foot progression angle rotates the foot away from the sagittal plane, into greater abduction and toward the frontal plane. During walking, the body moves forward in the sagittal plane, and rotation of the foot out of the plane of primary movement can contribute to injury. Body weight is now transferred to the medial side of the foot earlier, increasing the stress on the medial foot structures (talonavicular and first metatarsophalangeal [MTP] joint, as well as posterior tibialis muscle and tendon and the plantar fascia). The primary foot and ankle muscles involved in ambulation (the anterior tibialis and gastrocnemius/soleus muscles) are rotated out of their plane of primary importance. The fibularis (peroneus) longus and brevis become biased to aid in propelling the body forward, and the anterior tibialis has a decreased role in talocrural dorsiflexion or control of plantar flexion and an increase in its function in inversion and control of eversion. Finally, less talocrural dorsiflexion is needed during walking, which can either contribute to a gradual reduction in dorsiflexion or can be a compensation for already reduced dorsiflexion. In summary, foot progression angle with walking can contribute to excessive stress that increases the risk of injury.
Foot
Hindfoot
The hindfoot includes the talus, calcaneus, and the subtalar joint (joint between the talus and calcaneus). Inclusion of the talus in both the ankle and the foot indicates the importance of the talus to the function of the foot, as well as the function of the leg. The talus is responsible for absorbing and transmitting rotatory forces that have come from the hip and/or knee but also transmits rotatory forces up to the knee and hip that originated in the foot. The interconnectedness of the leg to the foot by way of the talus has led many to consider alignment of the hindfoot key in understanding the mechanics of the foot. In assessing alignment of the hindfoot, one can begin by assessing standing calcaneal alignment. The calcaneal alignment is generally classified as valgus, varus, or neutral and generally rests in slight valgus (3.5 degrees).8 The standing alignment of the calcaneus is then compared to the position of the calcaneus in subtalar joint neutral.
Assessment of subtalar joint neutral is the only clinical method available to determine structural variation in the hindfoot. Subtalar joint neutral is difficult to determine and measure in a reliable manner. However, the neutral alignment is a useful tool in interpreting standing alignment and providing a general reference for understanding the function of the foot. The determination of subtalar joint neutral occurs in prone. The examiner grasps the head of the talus with the thumb and index finger of one hand and the fifth metatarsal head with the other hand (Figure 8-2). The examiner uses the grasp on the fifth metatarsal head to move the forefoot and hindfoot into abduction and adduction until the fingers on the head of the talus palpate an equal proportion of the head of the talus on the medial and lateral side (under the thumb and index finger). The foot is held in this position to assess alignment. The alignment of the vertical bisection of the calcaneus is compared to the bisection of the lower leg.
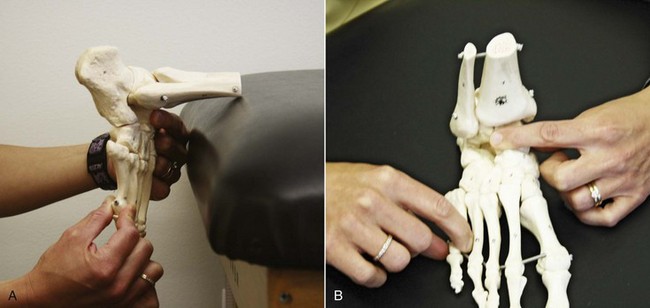
Figure 8-2 Subtalar joint neutral hand placement on skeleton: Outside hand at fifth metatarsal head and inside hand on head and neck of talus in standard position (A) and dorsal view (B).
The hindfoot is determined to be in varus alignment if the calcaneus is inverted relative to the lower leg, in valgus alignment if the calcaneus is everted relative to the lower leg, and neutral if the calcaneus is aligned with the lower leg (Figure 8-3, A). The forefoot alignment is determined to be in subtalar joint neutral by comparing the plane of the hindfoot to the plane of the forefoot. If the forefoot is inverted on the hindfoot, the forefoot is considered to have a varus alignment. If the forefoot is everted on the hindfoot, the forefoot has a valgus alignment, and if the hindfoot and forefoot planes are parallel, the forefoot has a neutral alignment (Figure 8-3, B).
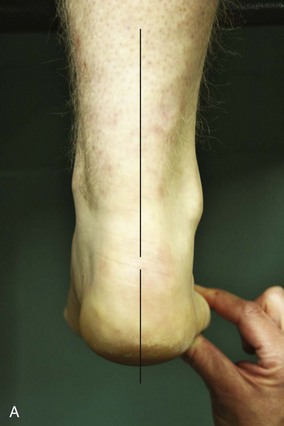

Figure 8-3 A, Neutral hindfoot alignment with vertical bisection of lower leg in line with the vertical bisection of the calcaneus. B, Neutral forefoot to hindfoot alignment with the plane of the hindfoot parallel to the forefoot.
The alignment of the metatarsal heads can also be assessed at this time. The metatarsal heads should be aligned along the same plane. Often the first metatarsal head will be located in a more plantar position than the remaining metatarsal heads. This is called a plantarflexed (dropped) first ray, which is a forefoot compensation for structural variations of varus at the hindfoot or forefoot (Figure 8-4).
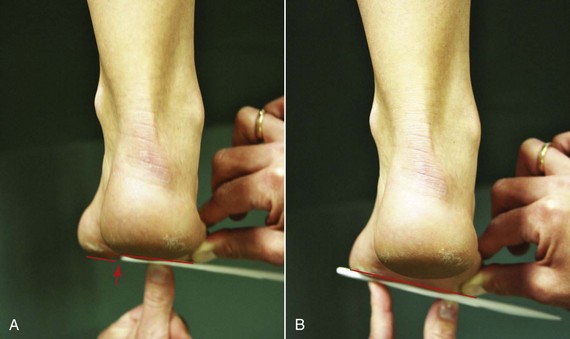
Figure 8-4 A, First metatarsal head is plantarflexed (dropped) below the plane of second to fourth metatarsal heads. B, Correction of the dropped first ray. The forefoot varus alignment relative to the hindfoot is now apparent.
The non–weight-bearing subtalar joint neutral alignment, providing insight into structure variability, is the backdrop for interpreting standing alignment and function. For example, suppose during prone subtalar joint assessment the neutral subtalar joint position was with the calcaneus inverted relative to the lower leg (hindfoot varus). During the standing alignment assessment, the calcaneus is vertical. The hindfoot is assessed as being able to compensate for the varus structural deviation (hindfoot alignment is termed compensated hindfoot varus); however, the standing calcaneal alignment is now understood as potentially harmful as the subtalar joint is being maintained near an end-range position.
Arches
Standing alignment assessment proceeds to the arches of the foot. There is truly only one arch in the foot that is continuous from anterior to posterior and medial to lateral, but the arch is usually described as three arches: the medial longitudinal arch, the lateral longitudinal arch, and the transverse arch. Much of the research on foot type, function, and injury has used the standing alignment of the medial longitudinal arch as the primary method of determining foot type.9-11 The height of the arch is often a key element. Extremes of high arch and low arch are relatively easy to classify. The high arch, a supinated foot type, is often accompanied by calcaneal inversion and an adducted forefoot, and the head of the talus and navicular are more prominent on the dorsal surface of the foot. The low-arch foot, a pronated foot type, is often accompanied by calcaneal eversion and a splayed and abducted forefoot, and the head of the talus and the navicular are more prominent in the middle of the arch (medial bulge).
The lateral longitudinal arch has greater inherent bony stability than the medial longitudinal arch. The joint surfaces of the calcaneus and cuboid are concavoconvex, providing some restriction to movement.12 The lateral longitudinal arch height is much lower, often appearing flat in visual assessment.
The transverse arch is formed in part by the wedge shape of the cuneiforms12 (Figure 8-5). As the transverse arch is assessed more distally on the foot, the height of the arch decreases until all metatarsal heads are in a level plane and capable of bearing weight.
Forefoot
The forefoot includes the metatarsals and phalanges. The normal alignment of the forefoot includes metatarsal and phalanges all aligned straight on one another. The toes should be relatively flat on the ground.
The common alignment impairment at the first MTP joint is hallux valgus. This alignment presents as angulation of the first metatarsal into abduction and the phalanx into adduction. The toes will also present with alignment faults that usually include a component of metatarsal-phalangeal hyperextension with flexion at the all interphalangeal joints (claw toes) or flexion at the proximal interphalangeal joint and extension at the distal interphalangeal joint (hammer toes).
Motions of the Ankle and Foot
Static alignment determined in subtalar joint neutral and standing are only a small part of understanding how the foot functions. Examination of how the joints of the foot and ankle move and function during walking, running, hopping, squatting, and various daily activities provides the bulk of the information that directs the diagnosis and treatment.
Ankle
Proximal and Distal Tibiofibular Joints
The proximal tibiofibular joint has very little motion, and individual variability in the shape of the joint surfaces has resulted in a wide variety of associated fibular motions reported with dorsiflexion and plantarflexion.13 The fibula at the proximal tibiofibular joint has been reported to glide anterior, lateral, and superior with talocrural dorsiflexion and to glide posterior, medial, and inferior with talocrural plantarflexion.13 The distal tibiofibular joint consists of a convex fibula and a concave tibia.12 During talocrural joint motion from neutral to dorsiflexion, the fibula at the distal tibiofibular joint has been found to have motions of internal rotation, lateral displacement (widens), and posterior and superior glide.14 During talocrural motion from dorsiflexion to plantarflexion, the fibula at the distal tibiofibular joint has been found to be medially displaced.15
Talocrural Joint
The axis of motion at the talocrural joint is not uniplanar but triplanar, crossing all three planes of motion. The motions about the axis are termed pronation and supination. Table 8-1 shows component motion description. The axis at the talocrural joint, although it crosses all three planes, lies primarily in the transverse plane in a medial-to-lateral direction. Thus plantarflexion and dorsiflexion are the primary motions.
TABLE 8-1 Motions at the Hindfoot Associated with Open- and Closed-Chain Pronation and Supination
| Open Chain | Closed Chain | |
|---|---|---|
| Pronation | Calcaneal eversion | Calcaneal eversion |
| Calcaneal dorsiflexion | Talar plantarflexion | |
| Calcaneal abduction | Talar adduction | |
| Supination | Calcaneal inversion | Calcaneal inversion |
| Calcaneal plantarflexion | Talar dorsiflexion | |
| Calcaneal adduction | Talar abduction |
Dorsiflexion
Adequate dorsiflexion motion at the talocrural joint is crucial in advancing the tibia over the foot in walking, running, jumping, squatting, and many other weight-bearing activities. A minimum of 10 degrees of dorsiflexion (with the knee extended) is needed for walking and 30 degrees for running.16 Dorsiflexion motion requires adequate length of the gastrocnemius muscle, soleus muscle, and calcaneal (Achilles) tendon, as well as ligaments and joint structures of the talocrural joint. Because the head of the talus is wider anteriorly than posteriorly, a small amount of motion is required at the tibiofibular joint to fully accept the dome of the talus.13 If dorsiflexion is found to be limited, the source of limited talocrural motion can be assessed by measuring talocrural dorsiflexion with the knee extended and flexed and assessing talocrural joint accessory motion. Additionally, dorsiflexion should be isolated to the talocrural joint, and compensations at the foot (e.g., eversion, midtarsal dorsiflexion, and pronation) should not be allowed during dorsiflexion. The following information is gleaned from this test:
Without adequate motion at the talocrural joint, the body can employ a number of strategies for compensating. The patient can increase the foot progression angle, demonstrate an early heel rise, or use a forefoot strike pattern (only the forefoot is in contact with the ground) during walking and running to compensate for the lack of dorsiflexion. Additionally, the failure to dorsiflex at the talocrural joint during stance phase can be compensated for by hyperextending the knee and/or increasing the dorsiflexion that occurs at the more distal joints of the foot: talonavicular, naviculocuneiform, calcaneocuboid, and/or cuboid-metatarsal joints (Figure 8-6).
Plantarflexion
Plantarflexion at the talocrural joint plays an important role in propelling the body during walking, running, and jumping. Normal plantarflexion motion during gait is approximately 30 degrees. Plantarflexion at the talocrural joint alone, however, is relatively ineffective in propelling the body forward. The foot (calcaneus to metatarsal heads) must become a rigid lever to transfer the plantarflexion force through the foot, raising the body over the toes. The foot becomes more rigid in a number of ways. First, the foot becomes rigid through maximizing bony alignment. The contraction of the plantarflexors has a supination component. Supination of the subtalar joint and transtarsal joint helps place the joints in their closed pack, which is a more stable position providing some stability to the foot.
The second way the foot becomes rigid is by the passive tensioning function of the plantar aponeurosis. The plantar aponeurosis is a thick fascial sheath originating at the calcaneal tubercle and inserting into multiple locations but primarily into the flexor tendons of the foot and the base of the fifth metatarsal. As the heel begins to rise at the end of the stance phase, the MTP joints dorsiflex and the plantar aponeurosis becomes taut. The joints of the foot are approximated, the arch rises, and the foot becomes more rigid (windlass mechanism). Third, the foot is rigid because of the muscular forces that directly impact joint stability. The posterior tibialis muscle/tendon is aligned to provide not only a force that produces plantarflexion with supination but also a force directed along the long axis of the foot. The posterior tibialis tendon inserts into all the tarsal bones, except the talus, as well as the bases of second to fourth metatarsals. The posteriorly directed force along the long axis of the foot is critical to the function of the foot. The force provides muscular “cinching” of the foot bones, increasing foot rigidity and the effectiveness of the ankle plantarflexor muscles.17 An extreme example of failure of the mechanisms that provide rigidity to the midfoot allowing plantar flexion at the midfoot is seen in Figure 8-7. (Contraction of the gastrocnemius in subject B of Figure 8-7 would result in isolated plantarflexion of the calcaneus without a forceful transfer of plantarflexion to propel the body.) The intrinsic muscles of the foot also function to support the arch of the foot and provide rigidity to the foot during plantarflexion.

Figure 8-7 A, An individual with diabetes and peripheral neuropathy. Note the normal upward inclination of the calcaneus. B, The foot of an individual with diabetes, peripheral neuropathy, and Charcot’s osteoarthropathy. This individual has lost the necessary rigidity of the foot and the pull of the gastrocnemius/soleus muscle through the calcaneal (Achilles) tendon resulted in calcaneal plantarflexion.
Foot
Subtalar Joint
The axis of motion at the subtalar joint is also triplanar. The axis, although it crosses all planes, lies primarily between the sagittal and transverse plane, allowing more inversion and eversion and abduction and adduction than plantarflexion and dorsiflexion.
Inversion and eversion
Motion at the subtalar joint is fairly limited because of the lack of symmetry in shape of the three talar facets (the posterior talar facet is concave, whereas the middle and anterior talar facets are flat to convex). Subtalar joint range of motion (ROM) is reported to be between 5 to 10 degrees of calcaneal eversion and 20 to 30 degrees of calcaneal inversion.18-20
The triplanar motion of the subtalar joint is difficult to capture during weight-bearing activities using standard kinematic techniques. Passive calcaneal motion of inversion and eversion are easily measured goniometrically and often used to provide some indication of the movement at the subtalar joint. During walking the calcaneus contacts the ground in slight inversion (approximately 2.5 degrees from standing calcaneal position). The calcaneus moves into slight eversion through heel-off and then begins the return to inversion (approximately 6 degrees from the standing calcaneal position) right before toe-off.21
In the weight-bearing foot, the intimate connection of the talus to the lower leg through the talocrural joint links medial rotation of the lower leg to subtalar joint pronation (talar adduction and calcaneal eversion) and vice versa, subtalar joint pronation to lower leg medial rotation. The same is true for the linking of lateral rotation of the lower leg to supination and supination to lateral rotation of the leg. The linking of foot and leg motion through the subtalar joint illuminates why many have worked to assess and understand subtalar alignment, motion, and function.
Transverse Tarsal or Midtarsal Joints
The transverse tarsal joint is comprised of the talonavicular and calcaneocuboid joints. The axes of motion at the transverse tarsal joints are triplanar, allowing pronation and supination. In most feet, motion at the subtalar joint is intimately connected to the motions that occur at the talonavicular and calcaneocuboid joints. As the subtalar joint supinates, it draws the transverse tarsal joint into supination, a more stable joint position of the transverse tarsal joint (locked position), converting the midfoot into a more rigid lever. As the subtalar joint pronates the transverse tarsal joint pronates, which creates a more loose position of the joints and a more flexible midfoot.22,23
The transverse tarsal joints are the intermediate joints between the hindfoot and the forefoot. One of the functions of the transverse tarsal joint is to position the forefoot for ground contact during push-off. In performing this function, the transverse tarsal joint becomes a frequent site of compensation for structural variances and movement impairments of both the hindfoot and forefoot. The transverse tarsal joint can become hyperflexible, limiting the ability of the foot to transform into a rigid lever and decreasing the stability of the longitudinal arches, which contributes to flat-foot deformities.
In the high arched or more rigid foot type, the subtalar joint and the transverse tarsal joints are maintained in the closed pack or locked position. The lack of mobility is thought to contribute to injuries at the foot and lower extremity as a result the inability of the rigid foot to dissipate the high forces occurring during weight-bearing activities.
Tarsometatarsal Joints
The tarsometatarsal joints generally have very little motion and are critical in providing the structure for the transverse arch. Motion that occurs at the tarsometatarsal joints is generally with the focus of positioning the forefoot flat on the ground for push-off. If the motion that has proceeded from the hindfoot to the midfoot during gait has inadequately prepared the forefoot for weightbearing, the tarsometatarsal joints may assist. For example, insufficient pronation of the hindfoot and midfoot from heel strike through midstance might result in the medial side of the forefoot being up off the weight-bearing surface. If there is motion available at the tarsometatarsal joints, a pronatory twist will occur at the tarsometatarsal joints to bring the forefoot flat.23 A supinatory twist will occur in the tarsometatarsal joints if too much pronation has occurred at the hindfoot and midfoot during early stance phase. The site of compensatory motion often becomes the source of symptoms.
Metatarsophalangeal Joints
The MTP joints’ primary direction of function is into dorsiflexion. Adequate MTP dorsiflexion allows the foot to roll over the toes as the plantarflexor muscles propel the body forward. Additionally, MTP dorsiflexion stretches the plantar aponeurosis, elevating the arch and assisting in making the foot rigid during push-off. First MTP joint dorsiflexion needed for walking is reported to be between 30 to 60 degrees.24,25 Lack of first toe extension prevents the normal pattern of roll-over, and weight is transferred either medial or lateral of the first toe. Medial weight transfer increases the abduction force on the proximal phalanx, predisposing the individual to hallux valgus deformity. Lateral transfer of weight increases the force borne by the second and third metatarsal heads, often resulting in pain at the MTP joints.
First MTP joint dorsiflexion can be limited by the length of the flexor hallucis longus, plantar aponeurosis (fascia), or joint restrictions. Theoretically, the contribution of flexor hallucis longus muscle length to limited MTP joint dorsiflexion motion can be determined by comparing MTP dorsiflexion ROM with the talocrural joint dorsiflexed (flexor hallucis longus on stretch) to MTP dorsiflexion ROM with the talocrural joint plantarflexed (flexor hallucis longus on slack). First MTP dorsiflexion in full plantarflexion should measure ≥60 degrees. First MTP dorsiflexion in full talocrural dorsiflexion is rarely measured. Hopson et al25 found on average 85 degrees of MTP dorsiflexion in 0 degrees of talocrural dorsiflexion. Nawoczenski et al24 found 35 to 45 degrees of MTP dorsiflexion in a standing passive and active test. Clinically, MTP dorsiflexion measured in talocrural dorsiflexion is very limited, between 10 to 15 degrees (Figure 8-8). Decreased MTP dorsiflexion in full talocrural dorsiflexion can indicate flexor hallucis muscle length impairment. However, the plantar aponeurosis may also be limiting MTP motion in this position because the position of maximum MTP and ankle dorsiflexion has been found to place maximum stretch on the plantar aponeurosis.26
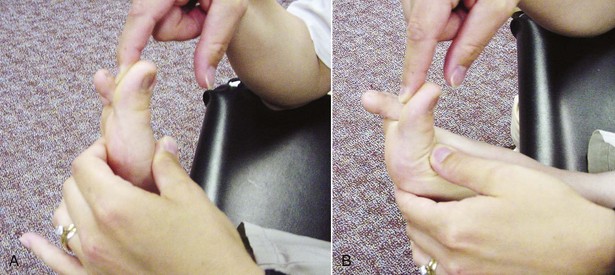
Figure 8-8 First metatarsophalangeal extension. A, In talocrural joint dorsiflexion. B, In talocrural joint plantarflexion.
Functionally, there is rarely an occasion in which maximum MTP dorsiflexion is needed during maximum talocrural dorsiflexion. During gait, 30 to 60 degrees of first MTP dorsiflexion24,25 is needed during push-off when the talocrural joint is in approximately 10 to 25 degrees of talocrural plantarflexion.21,23 Thus the most functional assessment of first MTP dorsiflexion would be to assess MTP dorsiflexion motion in approximately 20 degrees of talocrural plantarflexion. In summary, the following information can be gleaned from the test:
The contribution of MTP dorsiflexion to engage the windlass mechanism of the foot thus increasing foot rigidity during push-off is critical. Stretching into first MTP dorsiflexion should be approached with caution to avoid overlengthening of the foot structures critical for engaging the windlass mechanism of the foot.
Interphalangeal Joints
The interphalangeal joints have a critical role in increasing the area over which the weight-bearing force is distributed during push-off. To increase surface area during push-off, the toes must be flat on the ground. The intrinsic muscles of the foot are critical in stabilizing the MTP joints against excessive dorsiflexion (hyperextension) while extending the interphalangeal joints of the toes to provide a flat surface for force distribution. Without appropriate function of the intrinsic muscles of the foot, claw toe deformities develop as the extrinsic toe flexors and extensors act unopposed.
Muscle Actions
Leg
The four muscular compartments of the leg are the superficial posterior compartment, the deep posterior compartment, the lateral compartment, and the anterior compartment. The compartments are separated by fascial encasements that are continuations from the tensor fascia latae of the thigh.12 The fascial compartments assist the muscle by transferring the contractile force produced by the muscle to the bone (Figure 8-9). The fascial compartments also provide spatial constraints to edema and can compromise nerve and blood vessel function within a compartment when edema increases.
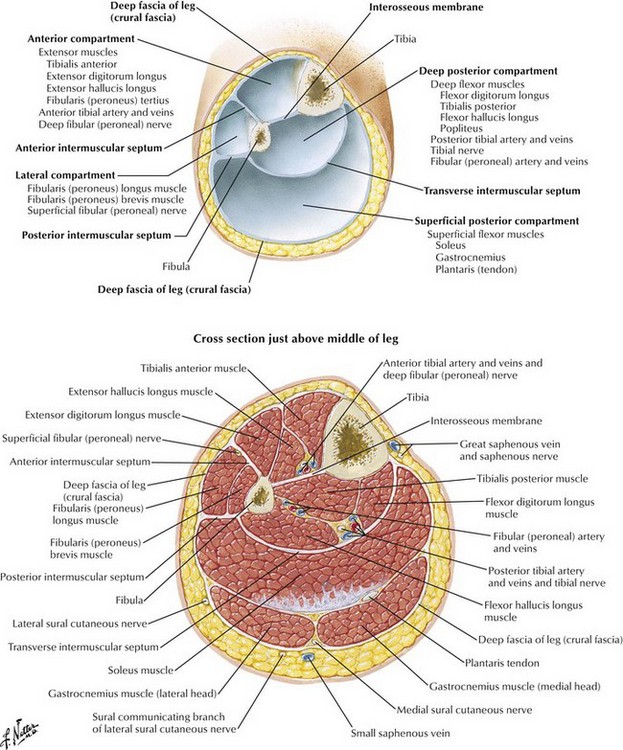
Figure 8-9 Fascial compartments and components.
(From Greene WB: Netter’s orthopaedics, Philadelphia, 2006, Saunders.)
Posterior Compartments
The superficial and deep posterior compartments of the leg contain the primary plantarflexors of the ankle (the gastrocnemius, soleus, tibialis posterior, flexor hallucis longus, and flexor digitorum longus muscles), the posterior tibial artery and veins, tibial nerve, and fibular (peroneal) artery and veins. All posterior compartment muscles insert medial to the midline of the foot and therefore also assist in supination. Strong plantarflexion with supination is important in the muscular component that transforms the foot into the rigid lever for effective push off during gait. The posterior compartment also has a significant eccentric role during walking and running by controlling tibial progression over the foot and pronation of the foot from initial contact until the start of push-off.
The posterior tibialis, flexor hallucis longus, and flexor digitorum muscles and the posterior tibial artery and tibial nerve make a sharp turn around the medial malleolus and travel beneath the flexor retinaculum in the region posterior to the medial malleolus. The area in which this sharp turn occurs is a frequent site for tendon injury, as well as nerve compression.
Lateral Compartment
The lateral compartment contains the fibularis (peroneus) longus and brevis muscles and the superficial fibular (peroneal) nerve. The fibularis muscles are ankle evertors and weak ankle plantarflexors. Additionally, the fibularis longus muscle crosses the plantar surface of the foot and inserts on the base of the first metatarsal and medial cuneiform bone, providing a supportive sling for the foot and muscular control of the forefoot position. The fibularis brevis muscle inserts into the base of the fifth metatarsal, providing rigidity to the lateral column of the foot.
Anterior Compartment
The anterior compartment contains the tibialis anterior, extensor hallucis longus, and the extensor digitorum longus muscles; the anterior tibial artery and veins; and the deep fibular (peroneal) nerve. The muscles, the anterior tibial artery, and the deep fibular nerve pass under the superior and inferior extensor retinaculum. All muscles within the anterior compartment are ankle dorsiflexors. The insertions of the tibialis anterior and extensor hallucis longus are medial to the talocrural joint axis, inverting the foot during dorsiflexion. The insertion of the extensor digitorum longus is lateral to the talocrural joint axis and everts the foot during dorsiflexion. For balanced dorsiflexion that occurs primarily in the sagittal plane, the anterior tibialis and extensor hallucis longus inversion force must be countered by the eversion force produced by the extensor digitorum longus.
The anterior compartment muscles function concentrically during the swing phase of walking and running, dorsiflexing the foot, and clearing the toe. The anterior compartment muscles work eccentrically to control lowering of the foot from heel strike to foot flat in a heel-strike first pattern of walking and running.
Foot
The intrinsic muscles of the foot provide important stabilization of the arches and the MTP and interphalangeal joints of the foot, as well as help regulate tension and direction of force produced by the extrinsic muscles of the foot. The quadratus plantae muscle attaches from the calcaneus to the tendons of the flexor digitorum longus muscle to redirect the diagonal force of the flexor digitorum longus so that the toes flex in the sagittal plane (Figure 8-10). The lumbricals attach from the flexor digitorum longus tendon to the medial proximal phalanx and on to the dorsal expansion of the extensor digitorum longus. When the lumbricals contract, they flex the MTP joint, place the flexor digitorum longus tendons on slack, and pull on the extensor digitorum longus dorsal expansion to extend the interphalangeal joints. The interossei attach to the shafts of the metatarsals and insert onto the base of the proximal phalanx, assisting in flexing the MTP joint, extending the interphalangeal joints, and providing a force to abduct and adduct the toes. Through the function of the interossei and lumbricals, hammer and claw toe deformities are prevented.23
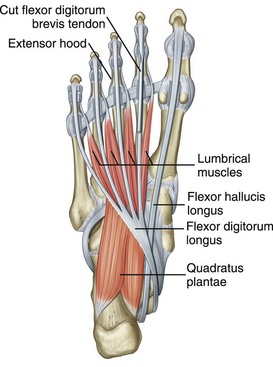
Figure 8-10 Quadratus plantae muscle.
(From Drake R: Gray’s anatomy for students, ed 2, Churchill Livingstone, 2009, London.)
The intrinsic muscles, in general, originate and insert along the longitudinal axis of the foot (they run proximal to distal). Through muscular contraction, the intrinsic muscles provide critical stabilization of the foot, assisting in the transformation of the foot from a flexible adaptor during initial phases of stance to a rigid lever during push off.12
An important function of the interossei and lumbricals is to stabilize the MTP joints during talocrural dorsiflexion. The extensor digitorum assists in producing balanced talocrural dorsiflexion but is also simultaneously acting to dorsiflex the MTP joints. MTP joint dorsiflexion during talocrural dorsiflexion is an unwanted action. First, the extensor digitorum tendon is shortened over both joints (the MTP and talocrural joints), decreasing the talocrural dorsiflexion torque production capability. Second, the plantar fascia is placed on maximum stretch, increasing the risk of injury. Finally, repetitive MTP extension contributes to hammer and claw toe deformities. The lumbricals and interossei muscles act to counter the action of the extensor digitorum longus and stabilize the MTP joints during talocrural dorsiflexion.
Interestingly, there are no intrinsic foot muscles that originate from the talus or calcaneus and attach to the navicular or cuboid. The stability of the transtarsal joint depends on bony shape, taut ligamentous restraints, and extrinsic muscles of the foot that cross this joint. The lack of intrinsic muscle joint restraints may contribute to the transtarsal joint becoming a frequent site of hypermobility.
Understanding the anatomy and kinesiology of the ankle and foot is the fundamental foundation necessary to critically examine functional activities of the foot and to determine the movement system diagnosis. The remainder of the chapter uses this knowledge of anatomy and kinesiology to assess movement and to determine when a movement impairment exists and what factors may be contributing to this movement impairment.
Examination of the Ankle and Foot
History
A standard history should be collected by the physical therapist and should include the history of the injury, pain ratings (symptoms at their worst, best, and average) and frequency and the duration of the pain. The standard history also includes the effect of daily activities and positions on symptoms, and the physical therapist must become familiar with the patient’s daily routine and requirements, as well as any changes in activity level that may have occurred around the onset of the symptoms.
The physical therapist must also ask additional questions regarding the patient’s footwear. Detailed information about the type and age of the footwear and the frequency and duration that each type of footwear is worn should be obtained. The therapist should become familiar with previous inserts, orthoses, or lower extremity braces the patient has been prescribed and/or worn.
The systems review should include the patient’s medical and surgical history and current medications. Musculoskeletal, neurovascular, and systemic sources of signs and symptoms must be examined and may require referral to a physician for additional management.
Potential Conditions Requiring Referral
Stress Fracture
Stress fractures are a common musculoskeletal source of undiagnosed foot and ankle symptoms that must be ruled out before completing a movement system examination and prescribing an intervention. Stress fracture pain generally is local and isolated to the bone, although symptom presentation can be diffuse and confusing. The six locations of stress fractures that are at high risk for serious sequelae if undertreated are anterior lateral tibial diaphysis, medial malleolus, talus, navicular, fifth metatarsal, and sesamoids.27 Local or suspicious signs and symptoms in the high risk areas should be immediately referred to a physician because delayed treatment or undertreatment tends to result in progression to a complete fracture, a nonunion, the need for operative intervention, and/or recurrence or refracture.
Deep Vein Thromboses
Deep vein thromboses (DVT) can be the source of calf pain and edema. The strongest risk factors associated with development of a DVT include a fracture of the pelvis, femur, or tibia; hip or knee replacement; spinal cord injury; major general surgery; or major trauma. The Homans’ sign28-30 (calf squeeze) has been commonly used to assess the presence of DVTs. Unfortunately, Homans’ sign has little diagnostic value.31 The Clinical Decision Rule developed by Wells et al assesses signs and symptoms, assigning a score and a probability of the presence of a DVT and has been found reliable and valid.32,33
Diabetes Mellitus
The lower extremity is at risk for devastating consequences of diabetes mellitus. Peripheral neuropathy and small vessel vascular disease can lead to unperceived injury, deformity, and nonhealing ulcers. Lower extremity amputation is often the outcome. An aggressive and complete screening for sensation and blood flow (see the “Peripheral Vascular Disease” section) should be completed on all patients who have suspicious histories. Sensation should be tested with Semmes-Weinstein monofilaments. For the foot and ankle, individuals are considered to lack protective sensation, which is sensation capable of detecting injury, if they are unable to feel the 5.07/10-gm filament on any location on the foot.
For individuals with diabetes mellitus, the hemoglobin A1c level (HbA1c) measures the percentage of hemoglobin in the blood that has glucose attached, indicating blood glucose control over a 3 month period of time. Normally, this value should be ≤6%. A higher HbA1c value indicates poor glucose control and is correlated with an increase risk of developing complications related to diabetes.34
Peripheral Vascular Disease
Peripheral vascular disease can present as claudicating pain, which is pain in the lower leg that comes on with walking and decreases or resolves with rest. The clinician should look for loss of hair on the feet and legs, decreased capillary refill, nonpalpable pulses at the dorsalis pedis and/or posterior tibial arteries, and poor skin color. The patient may also report results from an ankle-arm index assessment that compares blood pressure in the arms to blood pressure in multiple sites in the lower extremity. Normal ankle-arm index values should be between 0.91 to 1.3.35 There is and increased risk of a cardiovascular event with values <1.0 and ≥1.4.
Rheumatoid Arthritis
Although rare (16%), an initial presentation of rheumatoid arthritis (RA) occurs in the foot and ankle.36 Specifically, individuals complain of forefoot pain. Hindfoot pain is often a later manifestation of RA.
Seronegative Spondyloarthropathies
Foot and ankle pain are also common complaints in ankylosing spondylitis, psoriatic arthritis, Reiter’s syndrome, and inflammatory bowel arthritides. Foot and ankle complaints are generally accompanied by additional signs and symptoms specific to the disease.
Gout
Gout can present in an acute or chronic manner. The pain, redness, and swelling is generally localized to the first MTP.37
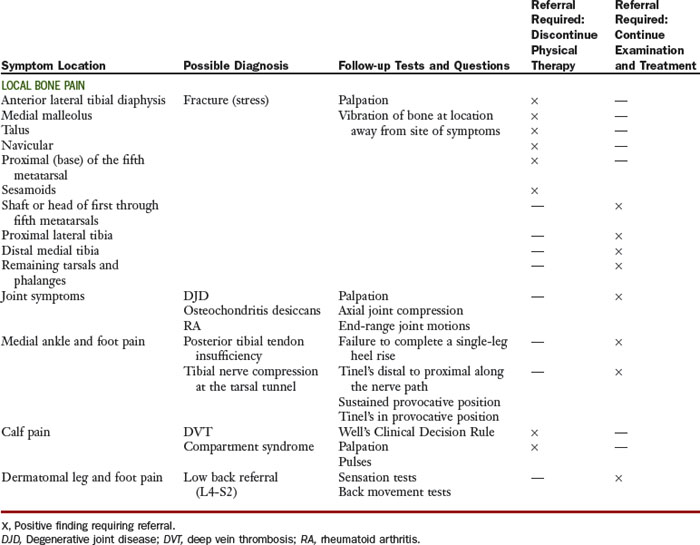
Potential Diagnoses and/or Conditions Requiring Referral
There are a number of undiagnosed conditions that should be suspected from the history and symptoms. If the conditions are not ruled out, they require a referral to a physician in addition to physical therapy or before physical therapy (see the Chapter 8 Appendix).
Movement System Syndromes of the Ankle and Foot
A movement system diagnosis is useful because the treatment plan directly addresses the movement pattern causing excessive stress on a particular tissue and resulting in injury. The body structures that are stressed and injured with a particular movement system syndrome are numerous and those that are listed with each movement system syndrome are not meant to be exhaustive but reflect those most commonly seen by physical therapists (Table 8-2). The source of symptoms (the body structure injured) is not specific to the movement system syndromes and should not be used in determining the movement impairment diagnosis. In the foot and ankle, where almost all muscles cross more than one joint and produce multiplanar motions, a particular body structure can be overstressed and injured by more than one individual movement (Table 8-3).
TABLE 8-2 Foot and Ankle Syndromes
| Syndrome | Key Findings | Source of Symptoms |
|---|---|---|
| Pronation | Incorrect timing or amount of motion of the ankle/foot in the direction of pronation during weight-bearing activities (hindfoot, midfoot, and/or forefoot). | Plantar fascia, posterior and anterior tibialis muscle/tendon, metatarsal heads, interdigital or tibial nerves, medial column joints and ligaments (talocrural, subtalar, talonavicular, naviculocuneiform, tarsometatarsal, and MTP joints) |
| Supination | Incorrect timing or amount of motion of the ankle and foot in the direction of supination during weight-bearing activities (hindfoot, midfoot, and/or forefoot). | Plantar fascia, fibular muscle/tendon, gastrocnemius/soleus muscle, calcaneal tendon, metatarsal heads, lateral column joints and ligaments (talocrural, subtalar, calcaneocuboid, tarsometatarsal, and MTP joints) |
| Insufficient dorsiflexion | Insufficient dorsiflexion during weight-bearing activities that require the tibia to advance over the foot. | Plantar fascia, gastrocnemius/soleus muscle, calcaneal tendon, calcaneal bursa, anterior tibialis muscle/tendon, deep fibular nerve |
| Hypomobility | Limitation in physiological and accessory motion of the ankle/foot joint(s). | Individual ankle and foot joints |
| Foot/ankle impairment | Tissue injury from surgery or trauma that requires protection for repair. | Individual ankle and foot tissues (bone, cartilage, muscle, tendon, ligament, skin, nerve) |
| Proximal tibiofibular glide | Positional fault of the fibula on tibia or hypermobility of the tibiofibular joint during hamstring contraction. | Proximal tibiofibular joint |
MTP, Metatarsophalangeal.
Pronation Syndrome
The principal movement impairment associated with pronation syndrome is pronation at the foot/ankle during weight-bearing activities that is excessive for that individual and/or when there is insufficient movement of the foot in the direction of supination in later stance phase. The pronation impairment can occur in the hindfoot, midfoot, and/or forefoot. A foot with the pronation syndrome is a flexible foot that provides the path of least resistance to motion and the site of compensation for various structural and movement impairments within the foot, ankle, knee, and hip.
Symptoms and Pain
The stress of the pronation movement impairment results in tissue injury. The tissues at greatest risk of injury include those impacted by excessive tensile forces from overstretching or muscular efforts to resist the pronation movement and occasionally those tissues that experience compression as a result of the excessive joint position. The following section of possible structures involved in pronation syndrome is not complete but identifies the most common structures and the symptoms reported during the history component of the examination.
Plantar Aponeurosis (Fascia)
Involvement of the plantar aponeurosis is most often accompanied by patient complaints of heel pain that is worse with the first step out of bed in the morning and after a period of prolonged non–weight-bearing activities.
Posterior Tibialis Muscle and Tendon
The patient complains of pain localized to the muscle at distal one-third of the medial tibia or anywhere along the tendon as it follows its course around the medial malleolus to the primary insertion at the navicular bone. The symptoms are most apparent during the weight-bearing phase of activities as the muscle works eccentrically to control pronation and/or concentrically to supinate and plantarflex the foot and ankle.
Anterior Tibialis Muscle and Tendon
Pain is localized to the muscle at the proximal lateral tibia and/or the tendon as it inserts into the medial cuneiform and first metatarsal. The symptoms are often present at heel strike as the muscle works eccentrically to control plantarflexion. Anterior tibialis muscle pain is often called shin splints and particularly apparent after running or long distance walking.
Tibial Nerve
Pain, tingling, and/or numbness is located on the posterior medial ankle and/or the plantar surface of the foot. Determining whether the tibial nerve is involved is critical but also difficult. Tinel’s tapping test along the nerve pathway and if needed, Tinel’s tapping test in the provocative positions of full dorsiflexion, calcaneal eversion, and toe extension can assist the physical therapist is determining the source of symptoms.38
Gastrocnemius/Soleus Muscles and Calcaneal (Achilles) Tendon
The patient complains of pain in the muscle belly or tendon, particularly during late stance, as the muscle is working eccentrically and the tendon is being placed on stretch to control the tibia’s progression over the foot and during the concentric contraction required during push-off.
Metatarsal Heads
For the movement impairment of pronation, metatarsal pain is localized to the head of the second and third metatarsals and increases during the late stance and the push-off phases of walking and running (Figure 8-11).
Interdigital Nerves
The interdigital nerves can become irritated, producing complaints of pain, tingling, or numbness between the metatarsals and into the corresponding toes. The most common location is between the third and fourth toes. The interdigital nerve often receives branches from both the medial plantar nerve and the lateral plantar nerve, increasing the size of the nerve and the risk of impingement during weight-bearing activities.
Alignment: Structural Variations and Acquired Impairments
Standing foot alignment has been a primary method for determining foot type. The typical description of a pronated foot includes a combination of calcaneal eversion, medial bulge (prominence of the talonavicular joint medially), low medial longitudinal arch, forefoot abduction relative to the hindfoot at the transtarsal joint, and increased width of the forefoot (splayed forefoot) (Figure 8-12). Often, as the remainder of the lower extremity alignment is examined, there will be alignment impairments proximal to the foot that contribute to pronation at the foot. These include medial rotation at the hip, medial rotation at the knee, and structural variations of the femur and/or tibia that result in an increase in medially directed forces through the foot (e.g., femoral anteversion, medial tibial torsion, or genu valgus) (Figure 8-13).

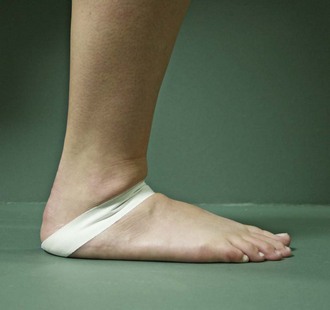
Figure 8-12 Left foot, classic standing alignment for pronation impairment: Calcaneal eversion, medial bulge, low medial longitudinal arch, forefoot abduction, and increased width of the forefoot.
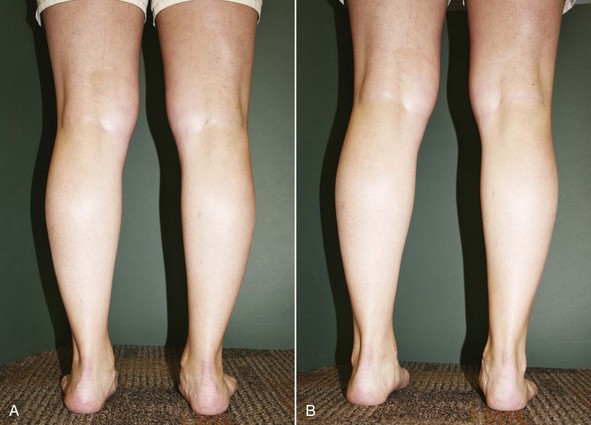
Figure 8-13 A, Individual with calcaneal valgus, dropped medial longitudinal arch, medial bulge, and abducted forefoot bilaterally. B, Same individual, is able to minimize foot pronation through correcting hip medial rotation and knee hyperextension.
There are a number of hindfoot and forefoot alignment variations that can contribute to the pronation syndrome. The most common structural variations are subtalar joint neutral alignment of hindfoot and/or forefoot varus. If adequate subtalar joint eversion motion is available, the calcaneus may evert to compensate for the varus alignment in an attempt to get the foot flat on the weight-bearing surface. If the midfoot and forefoot are flexible, they can also compensate for varus alignment faults contributing to a lowering of the medial longitudinal arch, forefoot abduction, and splaying (widening) of the forefoot (Figure 8-14). Valgus hindfoot and forefoot structural faults that persist with standing can also contribute to the pronated standing alignment.
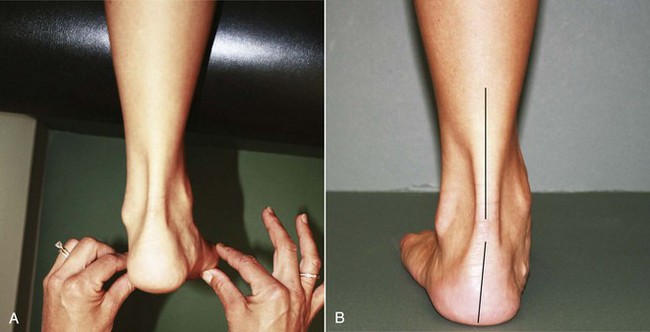
Figure 8-14 A, Left foot subtalar joint alignment in prone: Hindfoot in neutral alignment relative to the leg and a forefoot varus relative to the hindfoot. B, Left foot standing alignment includes slight calcaneal eversion, bulge in the medial longitudinal arch, and forefoot abduction. Calcaneal eversion indicates the ability of the hindfoot to assist in compensating for the forefoot varus structural variation.
Movement Impairments
Walking and Running
During walking and running, the pronation movement impairments can include excessive calcaneal eversion during the early and midstance phases, excessive arch flattening in the midstance phase, and/or insufficient movement of the foot in the direction of supination in the late stance phase (Figure 8-15). Often, there is poor contraction of the gastrocnemius muscle with very little push-off noted. Medial rotation of the hip with an increase in medial foot loading can also be viewed.

Figure 8-15 Instances in stance in an individual with pronation syndrome. A, Heel strike. B, Midstance. C, Heel off. D, Toe off.
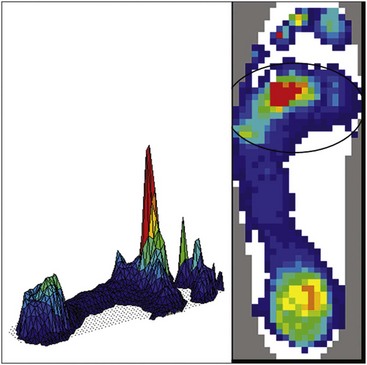
Plantar pressure scans taken during barefoot walking show an increase in force distributed through the medial side of the foot, as well as high pressure through second and third metatarsal heads (Figure 8-16).
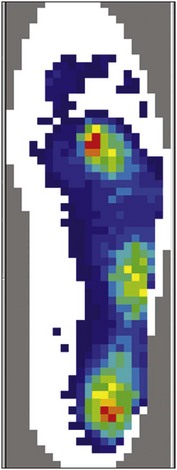
Figure 8-16 High pressure at second and third metatarsal heads in a subject with pronation during walking. Lateral midfoot pressure is related to cuboid subluxation
During running, the pattern used by most people is to contact the ground first with the heel of the foot. A heel-strike pattern of running recruits the anterior compartment muscles to absorb shock and lower the foot down. The posterior compartment muscles are then recruited to control tibial advancement and assist with plantarflexion force. A running pattern that results in the midfoot or forefoot making the initial contact can contribute to pronation movement impairments. With a midfoot or forefoot initial contact, the force of body weight travels through the midtarsal joint and encourages dorsiflexion motion at the midtarsal joints. Additionally, the anterior compartment muscles are not recruited and the posterior compartment muscles remain active throughout stance, placing additional stress on the gastrocnemius and posterior tibialis muscles. The patient should be encouraged to run with a relatively frequent heel-strike–first pattern. In most cases, the patient does not need to make a complete shift to a heel-strike running pattern, but often a moderate decrease in the frequency or severity of the midfoot or forefoot strike pattern can result in a decrease in symptoms.
If symptoms are reproduced during walking and running and the pronation impairment is suspected, the secondary tests would be to provide cues to contract the gastrocnemius and posterior tibialis muscles, lifting from the heel and raising the medial longitudinal arch. If the patient is unable to control pronation during walking and running, external arch support (inserts, scaphoid pads, or arch taping) can be added, and movement and symptom reproduction is reassessed. If hip and knee medial rotation control appears to be an important factor, cues to contract the gluteal muscles and intrinsic hip lateral rotators can be used to assess the impact of the hip and knee movement impairment on foot function and symptom production.
Single-Leg Hopping
The patient is asked to repetitively hop on one leg. Individuals with the pronation syndrome demonstrate calcaneal eversion, dropping of the medial longitudinal arch, forefoot abduction, and/or knee and hip medial rotation. Poor contraction of the gastrocnemius is often very apparent during the single-leg hop test. The patient has a decreased jump height and compensates for the lack of plantarflexion strength with an increased swing of the upper extremities and increased reliance on the quadriceps and/or hip extensors to complete the jump. The contributing movement impairments of medial rotation at the hip and/or knee are also easily assessed during single-leg hop. If symptoms occur during single-leg hop, the secondary tests would be similar to those described for the walking and running test: Encourage gastrocnemius muscle contraction, add external arch support, and correct associated hip and knee movement impairments to assess movement and symptom production.
Step-Down and/or Small Knee Bend
The patient is asked to perform a step-down and/or a small knee bend. The physical therapist assesses the movement and symptom reproduction. Movement impairments consistent with pronation (calcaneal eversion, arch flattening, and weight transferred over the medial side of the foot and knee or hip medial rotation) and symptom reproduction support the movement system diagnosis of pronation. If symptoms are reproduced or the therapist suspects baseline symptoms could be reduced, the patient is cued to correct the movement impairment raising the arch, transferring weight slightly more lateral, and contracting the hip lateral rotators to control femoral medial rotation. A decrease in symptoms with the correction of the movement impairment supports the diagnosis of pronation syndrome.
Joint Integrity and Muscle Length
Muscle Strength/Performance Impairments
Determining the muscle performance impairments in the foot and ankle can be challenging. The forces experienced by the ankle and foot during walking, running, and hopping are often larger than the forces a physical therapist can generate during manual muscle testing (MMT). Additionally, the muscles of the foot and ankle often have an extremely large eccentric role that is not tested with standard MMT. Functional tests should be incorporated to determine true muscle performance.
Gastrocnemius/Posterior Tibialis Muscles
The gastrocnemius muscle is critical in producing powerful plantarflexion during walking and running. Along with the posterior tibialis, flexor digitorum longus, and flexor hallucis longus, the gastrocnemius muscle contributes to supination of the foot during the late stance phase. To assess function, observe the calcaneus during single-leg heel rise. Together, the ankle plantarflexors should contract and result in calcaneal inversion and elevation of the calcaneus through the full available motion. The ability to complete 25 single-leg heel raises is considered normal.39 Dysfunction of the posterior tibialis tendon and muscle is evident during a single-heel rise since the calcaneus does not invert, the individual is unable to complete a full heel raise, and often dorsiflexion is seen at the midfoot (Figure 8-17). During walking and running, a visible and strong contraction of the gastrocnemius muscle is expected. Weakness or poor recruitment of the plantarflexor muscles contributes to pronation that occurs past midstance.
Posterior Gluteus Medius, Gluteus Maximus, and Intrinsic Hip Lateral Rotation Muscles
Performance impairment of the hip lateral rotators results in excessive hip medial rotation. Hip medial rotation can cause pronation motion at the foot.
Intrinsic Muscles of the Foot
The intrinsic muscles of the foot are important in maintaining the arches of the foot during weight-bearing activities. The strength assessment is often indirect, observing the individual’s ability to complete a towel crunch with the toes, lifting the arch, and flexing the MTP joints.
Plantar Callus Findings
Callus formation is an indication of high stress, either friction or force. In the patient with pronation syndrome the location of calluses are generally on the second metatarsal head, third metatarsal head, and/or medial side of the first toe. Callus formation at the second and third metatarsal heads indicates that the location of force during push-off remains in the center of the foot. The normal pattern of force during the final phase of push-off is through the first and second metatarsal heads. The medial toe callus represents late pronation (pronation at push-off).
Footwear Considerations
Heel Counter
The heel counter is the posterior component of the shoe that wraps around the heel and is attached to the sole of the shoe. The purpose of the heel counter is to cup the heel and control hindfoot motion. The heel counter should fit the heel snugly and should be made of firm material. If the material is flexible or absent (e.g., an open-back sandal) there is no external assistance to control the calcaneal motion of eversion that can contribute to pronation syndrome.
Shoe Sole Components
The density (firmness) of the material used in the sole of the shoe impacts the shoe’s “resistance” to a particular motion. Shoes manufactured to control pronation often have a dual or multidensity sole. A material with increased firmness is added to the medial side of the shoe (a less dense or softer material remains lateral), discouraging motion in the direction of pronation (Figure 8-18).

Figure 8-18 Right Asics Gel Foundation 8. Firm density material at the medial heel with less dense material laterally. Gel material is also dual density with firm gel medial and soft gel lateral.
The location of the firm material as it relates to the patient’s specific movement impairment is very important. For a patient with a neutral calcaneus but increased pronation at the midfoot, the firm material should be located only at the medial midfoot (Figure 8-19). For this particular patient, inclusion of firm material at the hindfoot may encourage a new movement impairment of calcaneal inversion and potentially result in new symptoms. If the pronation impairment occurs at the hindfoot and midfoot, the firm material should run from the heel through the midfoot.
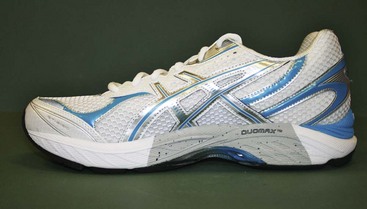
Figure 8-19 Right Asics GT-2150. Note multidensity arch material to increase support for the midfoot.
The general flexibility of the sole should be assessed. The sole of the shoe should bend easily only at the toe break. Where the shoe breaks is in part determined by the location of the grooves in the sole material. The removal of sole material to form the grooves encourages bending at the specific location. The groove on the shoe should match the patient’s MTP joint line from the first to the fifth toes (Figure 8-20). Footwear with little sole rigidity results in bending at the midfoot, which encourages dorsiflexion at the midtarsals and tarsometatarsal joints (Figure 8-21).
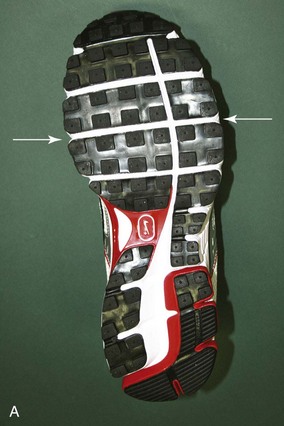

Figure 8-20 A, Left Air Pegasus+ 26. Note the white line of material at the metatarsal break is more distal lateral than medial. B, Left Asics Gel Nimbus 11. The white line of material is more proximal lateral than medial. The pattern of sole material removal at the forefoot should match the outline of the metatarsophalangeal joints where dorsiflexion occurs during walking and running.
Heel-to-Toe Height
Limited dorsiflexion contributes to pronation as discussed previously in this chapter. Limited dorsiflexion can be compensated for by lifting the heel slightly above the toe. This can be accomplished through footwear and is often unnoticed by the individual wearing the shoe (Figure 8-22). The onset of foot symptoms related to a change in footwear may be associated with a change in the heel to forefoot height (the amount of heel lift). Even a small reduction of heel height can increase the stress on the foot and result in injury.
Arch Support
The amount of direct arch support material in the insole of the shoe is generally small and often made of very soft (compressible) materials. The location is also fixed and may fail to support the arch in the appropriate location. External arch pads (scaphoid/navicular pads) can be easily added to most any footwear.
Last Shape
The last of a shoe is the mold used to shape the shoe. The shape of shoes is generally straight, semi-curved, or curved. To assess last shape, bisect the heel into equal amounts of sole material, medial and lateral. Continue the line that bisects the heel up to the forefoot of the shoe. A straight last will have equal amounts of forefoot sole material on the medial and lateral sides of the line that bisects the heel (Figure 8-23). Curved lasts will have more material on the medial side of the forefoot portion of the shoe compared to the lateral side. Individuals with pronation syndrome often have a straighter foot and would fit best into a straight or semi-curved last. The shape of the shoe should not be used to force a change in foot shape.
Summary
Pronation syndrome is characterized by pronation during weight-bearing activities that is excessive for that individual and/or is occurring past midstance during walking or running. The movement impairment will be observed during weight-bearing activities (walking, running, single-leg hop, small knee bends, and/or stepping down). The movement impairment of pronation occurs in the presence of a foot that is flexible and accommodates for limitations. The associated limitation can be limited dorsiflexion motion at the talocrural joint, weakness of the foot and ankle supinators and/or foot intrinsic muscles, and/or hip lateral rotators.
Treatment
Walking and Running
The patient is instructed to work on the specific cues that assisted in symptom reduction during the examination or the cues that the physical therapist believes, with practice, may result in symptom reduction. The following cues are among the possibilities that may assist the patient:
Many of the changes being requested of the patient during walking and running are similar to a strengthening program. As such, encourage the patient to have focused practice time and gradual implementation to avoid injury.
Muscle Performance
Weakness of the supinators (gastrocnemius and posterior tibialis muscles) can be addressed with a progressive strengthening program, which includes elastic band resistance exercise into plantarflexion and plantarflexion/inversion, heel raises, and single-leg hopping. During the exercise, assess the contraction of the gastrocnemius muscle cueing the patient to raise the heel.
Intrinsic muscles of the foot can be strengthened by completing towel crunches using the toes to grab the towel and pull the towel under the foot. The movement must be accomplished by flexing at the MTP joints, raising the arch, and cupping the foot (Figure 8-24, A). The patient should not be allowed to complete the towel crunch with isolated motion of the flexor digitorum longus with flexion occurring only at the proximal and distal interphalangeal joints (Figure 8-24, B). Weight can be added to the towel to increase resistance.
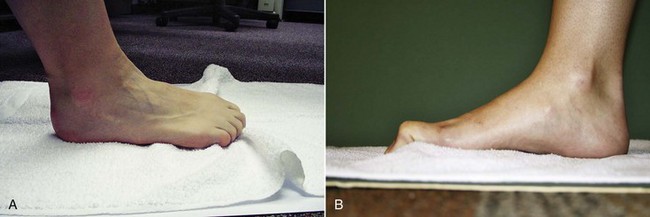
Figure 8-24 A, Towel crunch with toes using intrinsic muscles to flex the metatarsophalangeal joints. B, Toe intrinsic exercise done incorrectly using flexor digitorum longus and flexor hallucis longus to curl toes without flexing the metatarsophalangeal joint and raising the arch.
Posterior hip muscle strengthening is described in detail in Chapter 7, “Corrective Exercises: Purposes and Special Considerations,” in Sahrmann.3 An appropriate strengthening progression activity includes sidelying hip lateral rotation progressing to lateral rotation with abduction and adding weight as appropriate.
Muscle strengthening occurs when the muscle is overloaded. The general recommendations are that the exercise should be completed at 70% of the patient’s maximum voluntary contraction for 10 repetitions, 3 sets, 3 to 5 times/week. In general, exercise or activity is permissible if pain remains ≤2/10 on a 0 to 10 scale.
Muscle Length and Joint Integrity
Decreased length of the gastrocnemius muscle and tendon can be addressed with a small lunge stretch at the wall, dropping the heel off a ledge, or long sitting dorsiflexion towel stretch; all stretches would be done with the knee extended. The soleus muscle and tendon can be stretched by bending the knee during the wall, heel hang, or towel stretch. Unique instructions for patients with pronation syndrome include preventing pronation during the stretch (this could include active patient correction of pronation and wearing good footwear during the stretch) and keeping the foot facing forward or in line with the femur and tibia. The heel should be kept on the ground during the stretch.
To address talocrural joint limitation, a posterior glide or a distraction technique of the talus on the ankle mortise is recommended in addition to the stretches described. Additionally, a prolonged stretch can be provided by a dorsiflexion splint. The splint is a non–weight-bearing brace and is generally recommended for night wear but could be used during the day if the individual could remain non–weight-bearing during splint use. Splint use in the foot and ankle is often reserved for patients whose symptoms do not respond to the traditional treatment plan to improve dorsiflexion. Splint wearing at night can be uncomfortable, disrupting sleep, which often results in poor patient compliance.
Limited talocrural dorsiflexion can be compensated for by adding a heel lift in the shoe. A heel lift used long term can contribute to loss of talocrural dorsiflexion and should be approached with caution.
Limited extensor digitorum longus muscle and tendon extensibility can be addressed by having the patient plantarflex the involved foot with the toes plantarflexed either in a sitting position or while on hands and knees and rocking back. Limited first MTP dorsiflexion related to decreased extensibility of the flexor hallucis longus can be addressed with a prolonged stretch into dorsiflexion with the ankle in dorsiflexion. To address limitations in first MTP joint dorsiflexion, an anterior glide of the proximal phalanx on the metatarsal can be performed.
Stretching should be held for 30 seconds, 2 to 3 repetitions, completed regularly throughout the day (5 to 8 times/day), and completed 5 to 7 days/week.
Activity Modification
Activity level should be modified to decrease forces on the foot. If the symptoms are severe, the therapist should consider the use of an assistive device or a period of immobilization to decrease tissue irritability.
As the tissue heals, a cautious and gradual increase in activity will assist in returning the patient to the previous level of activity. If appropriate for the patient’s goals, activity should progress to dynamic activities such as jumping, hopping, shuttle run, cutting, and so on. A guide for progressing from walking to running begins with a run/walk program. Generally, a 1 : 4 ratio (1 minute run with a 4 minute walk) is a reasonable place to begin. The physical therapist should closely monitor symptoms. The symptoms guidelines used in clinical practice are that symptoms should remain ≤2 out of 10, and symptoms that come on with activity should resolve within a very short time after activity (no longer than 1 hour). As the tissue tolerance to activity improves, the number of run/walk cycles is increased and then duration of running is increased while walking duration is decreased.
The progression to high level agility sport activity includes starting with straight plane jogging and jumping on a smooth flat surface. The most effective strategy is to work on increasing distance before increasing speed because an increase in speed increases the peak forces through the foot and is more likely to result in tissue injury or reinjury. As the patient’s tolerance of weight-bearing activities improves, the terrain should be varied, as well as the addition of hills, cutting, and progressing to unexpected turns. The equipment (balls, cleats, sticks, rackets, and so on) associated with the sport of interest should be introduced, as well as a plan to gradually introduce other players and to address the dynamics of the sport (player contact, single-leg balance activities, speed of the sport, or ball movement).
External Tissue Support
Footwear
The footwear prescription is specific to each individual, but some general guidelines for pronation syndrome can be provided. The last (shape) of the shoe should look like the patient’s foot. Most often a straight or semi-curved last is appropriate. A firm heel counter to control hindfoot motion is advisable for most all individuals. If pronation occurs at the hindfoot, the shoe should include more rigid material at the medial heel and less rigid material at the lateral heel. The medial structure of the shoe should be made of firm materials, and the sole should be rigid from hindfoot through midfoot, bending only at the metatarsal heads. The shoe length, width, and height of the toe box should accommodate the size of the foot and any deformities present.
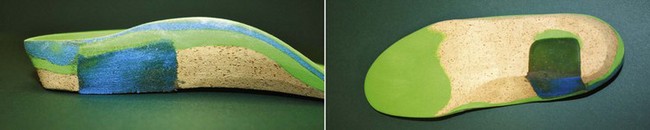
Orthoses
Orthoses are not recommended for all patients. Indications that orthoses may be appropriate include (1) the inability to correct the movement impairment through cueing, (2) significant structural variations, (3) the problem is recurrent, or (4) the foot alignment places the individual at risk for future problems. A temporary orthosis is a cheap and efficient method to assess the usefulness of an orthosis. Components can be easily added and removed to aid in determining what is most helpful for managing the patient’s symptoms. The component most often added is arch support (scaphoid/navicular pad). Medial hindfoot and forefoot posts are additional options that can assist with limiting motion that results in symptoms (Figure 8-25). The goal of the orthosis is not to achieve a subtalar joint neutral position but to prevent excessive or end-range motion so that the symptoms resolve. For local metatarsal pain, a common orthoses component is a metatarsal pad (Figure 8-26). The pad should be located just proximal (0.5 to 1 cm proximal) to the metatarsal head to unload the metatarsal heads and limit MTP hyperextension.40
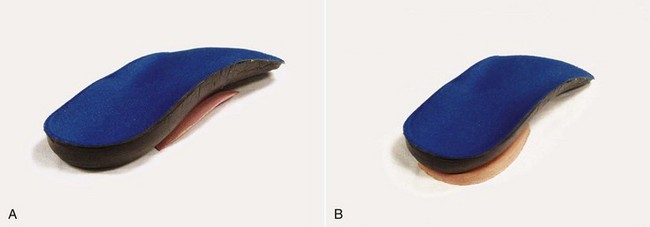
Figure 8-25 An off-the-shelf orthosis with a (A) scaphoid/navicular pad and (B) hindfoot medial post.

Figure 8-26 A, Total contact insert with local metatarsal relief. B, Global (all) metatarsal head relief.
An important orthoses modification for patients with tarsal tunnel nerve (tibial nerve) involvement is to avoid firm materials in the medial heel of the orthosis or sole of the shoe. Firm materials may contribute to nerve compression and irritation (Figure 8-27).
Taping
Taping to support the arch can assist in symptom management while additional treatment options are being implemented. There are a variety of techniques, but most have a common component of restraining longitudinal motion between the calcaneus and the metatarsal heads (Figure 8-28).
Case Presentation
Pronation Syndrome
An internist referred a 42-year-old female for evaluation and treatment of right “heel pain.” Her heel pain began approximately 10 weeks ago when she returned to work full time as a floor salesperson at a local shopping center. The patient has had to decrease her working hours from 40 to 20 because she was unable to tolerate the heel pain. The patient’s pain is located on the plantar surface of the heel. She states the pain occurs only during weight bearing and is much worse in the morning when she first gets out of bed (7/10) than later in the afternoon (4/10). She states her pain is worse when walking barefoot or in her work shoes, which are dress flats. She reports increasing pain with walking more than 15 minutes and has difficulty completing daily activities like grocery shopping and playing games with her children. She is 5 foot 6 inches and weighs 190 lb. Her Foot and Ankle Ability Measure score is 49% (100% indicates normal function).
In standing, the foot alignment shows a vertical calcaneus and a normal-to-low arch bilaterally. The alignment of the hip and knee includes medial rotation of the femur and slight lateral rotation of the tibia bilaterally. Symptoms in standing were 3/10. In prone the assessment of subtalar joint neutral reveals a small hindfoot varus and neutral forefoot alignment.
During walking, the calcaneus hits in inversion, moves into eversion by midstance, and remains in the everted position through late stance (right foot greater than left). Symptoms during barefoot walking increased to 5/10. Secondary tests, including cues to raise her heel earlier in stance and to contract her gastrocnemius, decreased the amount of eversion during midstance to late stance and decrease her symptoms minimally (4/10).
Muscle Length/Joint ROM Analysis
| Right | Left | |
|---|---|---|
| Talocrural dorsiflexion (knee extended) | 0 degrees | 5 degrees |
| Talocrural dorsiflexion (knee flexed) | 5 degrees | 10 degrees |
| Calcaneal eversion | 5 degrees | 5 degrees |
| First MTP joint extension (30 degrees talocrural plantarflexion) | 60 degrees* | 60 degrees |
* Increased symptoms at the calcaneal tubercle and into the arch.
Joint accessory motion assessment found no difference in mobility between the right and left talocrural joints during an anterior-to-posterior glide of the talus on the ankle mortise.
Muscle Performance Impairments
Towel crunch with toes: the toes flexed, the MTP joints extended. The patient was able to correct performance to lift arch and plantarflex the MTP joints, but the foot cramped after five toe crunches.
Pronation occurred past midstance with no motion in the direction of supination during late stance. The primary contributing factors to pronation syndrome were decreased talocrural dorsiflexion ROM from decreased length of the gastrocnemius and soleus muscles and weakness of the gluteus medius/hip lateral rotators and foot plantarflexors/supinators. There was also a slight structural variation (hindfoot varus in the presence of sufficient calcaneal eversion motion) that could contribute to pronation. Additionally, the footwear provided insufficient support and cushion for a job that requires prolonged standing. The stage for rehabilitation is 2. The pain rating was moderate to high, she was mobile but limited in her ability to complete activities that require longer weight bearing, and her Foot and Ankle Ability Measure indicates a moderate amount of disability. Source of the symptoms was the plantar aponeurosis. The patient was seen 1 time/week for 8 weeks to assess and modify the treatment plan.
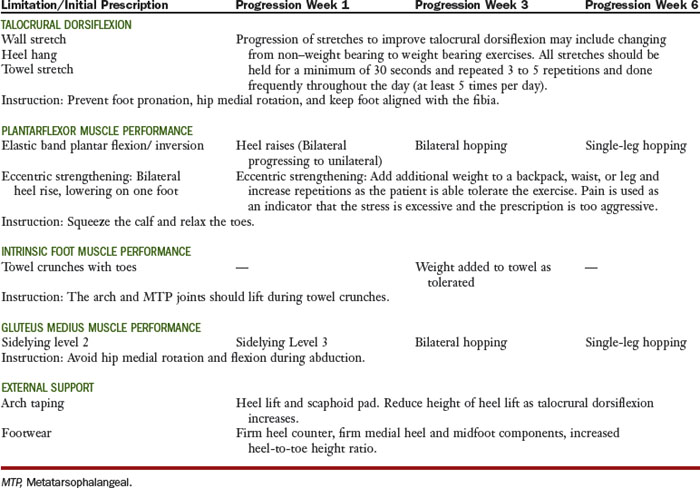
Table 8-4 includes pronation syndrome interventions and outcomes.
Arch taping resulted in an immediate decrease in symptoms with weight bearing to a 2/10. First step morning pain decreased to a 4/10 within the first week after implementation of the suggested changes to her morning routine. The temporary addition of a heel lift and scaphoid pad to the shoe was needed to assist with initial symptom relief. The patient continued the home exercise program to strengthen the hip, ankle, and foot, increase talocrural dorsiflexion motion, and modify the medial femoral rotation and foot and ankle pronation for approximately 8 weeks before symptoms consistently remained at 0/10 with a full 40-hour week of work.
Supination Syndrome
The principal movement impairment associated with supination syndrome is supination of the foot and ankle that occurs at the wrong time (heel strike to midstance in the gait cycle) or that occurs in an amount that is excessive for that individual. The supination impairment can occur in the hindfoot, midfoot, and/or forefoot. The foot with the supination impairment is generally a rigid foot with little or no ability to absorb shock and compensate for structural or movement impairments within the foot and ankle, knee, or hip.
Symptoms and Pain
Plantar Aponeurosis (Fascia)
Involvement of the plantar aponeurosis is most often accompanied by patient complaints of heel pain that is worse with the first step out of bed in the morning and after a period of prolonged non–weight-bearing function.
Fibular (Peroneal) Muscles and Tendon
The patient complains of pain localized to the muscles (posterior to the fibula) or anywhere along the tendon as it follows its course around the lateral malleolus to the insertion at the base of the fifth metatarsal for the fibularis brevis or following the fibularis longus as it runs along the lateral border of the cuboid and to the plantar surface of the foot. The symptoms are most apparent during the weight-bearing phase of activities as the muscle works to eccentrically control supination and dorsiflexion and during push-off as the muscle acts concentrically to assist with plantarflexion.
Gastrocnemius/Soleus Muscles and Calcaneal (Achilles) Tendon
The patient complains of pain in the muscle belly or tendon, particularly during late stance, as the muscle is working eccentrically and the tendon is being placed on stretch to control the tibia’s progression over the foot and during the concentric contraction required during push-off.
Alignment: Structural Variations and Acquired Impairments
The description of a supinated foot type includes a combination of calcaneal inversion, lateral bulge (prominence of the talonavicular joint dorsal and lateral), high medial longitudinal arch, forefoot adduction relative to the hindfoot at the transtarsal joint, and narrow forefoot width (Figure 8-29). Lower extremity alignment impairments that contribute to a supination impairment at the foot include lateral rotation at the hip and/or knee or structural variations of the femur or tibia that seem to be associated with a supinated foot (e.g., femoral retroversion, lateral tibial torsion).
The most common subtalar joint neutral alignment finding in individuals with supination syndrome includes a hindfoot and/or forefoot varus in which the joint mobility is limited and there is no ability to compensate with subtalar or midtarsal joint motion. Valgus hindfoot and forefoot structural variations that are compensated by inversion in standing can also contribute to the supinated standing alignment. In the prone position, an individual with supination syndrome may also have a first metatarsal head that is plantarflexed below the plane of the second to fifth metatarsal heads; this is called a plantarflexed or dropped first ray and is a common compensation for a forefoot varus (see Figure 8-4).
Movement Impairments
Walking and Running
During walking and running, the supination movement impairment usually includes calcaneal inversion at heel strike that remains through push-off. There is generally an absence of pronation during the initial portion of stance. The center of gravity during stance remains lateral on the weight-bearing surface of the foot (Figure 8-30). There is often a very late whip to the medial side of the foot during push-off. The foot is rigid, and there is very little shock absorption during walking and running, which can contribute to symptoms at the knee, hip, and back. The rigid foot can also produce varus motion at the knee that can contribute to knee symptoms.
The barefoot plantar pressure assessment in Figure 8-31 is common in individuals with the supination movement impairment. There is no loading of the midfoot, which reduces the surface area for force distribution (increases localized pressure). The metatarsal head pressure is high, particularly under the first metatarsal. In this individual, there is also very high medial great toe pressure, evidence of the late transfer of weight medially over the first toe.
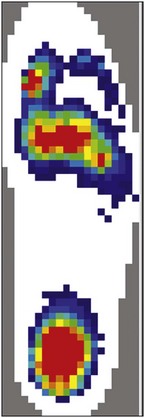
Figure 8-31 Barefoot pressure scan during walking of supinated individual. Note the lack of midfoot loading and the high forefoot pressure under the first metatarsal.
If symptoms are reproduced during walking and running and the movement impairments previously described are noted, the supination impairment is suspected. The secondary tests for supination impairment can be challenging to implement as the foot and the movement pattern are often fixed and unable to be volitionally corrected. Attempts can be made to control the offending motion (calcaneal inversion, late medial motion) with verbal cues to avoid extreme lateral loading through the foot, to soften the landing with knee flexion, and to roll medially sooner. Unfortunately, the rigidity of the foot often prevents the individual from changing the movement pattern. Attempts can be made to post the heel laterally to encourage eversion motion. Additionally, an arch support can be added to footwear to assess the effect of increasing the contact area over which the load is borne.
Single-Leg Hopping
The patient is asked to hop repetitively on one foot. The rigid foot associated with supination syndrome is an excellent lever for the plantarflexors, transferring the plantarflexor force easily and propelling the body up. Often, the patient with supination syndrome is able to jump fairly high and with what seems like little effort. The supination movement impairment at the foot is generally not apparent during the single-leg hop, since only the forefoot is striking the ground. Observation of the single-leg hop provides valuable information about plantarflexor muscle performance, as well as contributing movement impairments at the knee and hip. If symptoms occur during single-leg hop, the secondary test would be cues to address hip and knee movement impairments (lateral rotation or varus motions) and soften the landing with knee flexion. Weakness of the gastrocnemius/soleus complex should also be assessed further through single-leg heel rises. The addition of arch support may not affect the symptoms during the test because the heel and midfoot do not touch the ground during single-leg hopping.
Step-Down and/or Small Knee Bend
During a step-down or small knee bend, the most common impairment noted is limited dorsiflexion. The compensation is often an early heel rise and the rigidity of the foot becomes apparent (no decrease in arch height during the motion). The lateral distribution of force through the foot can also be seen during the small knee bend. Symptom reproduction during low impact activities like step-downs or small knee bends is rare. However, if symptoms are reproduced or the therapist suspects baseline symptoms could be reduced, the patient is cued to correct the movement impairment keeping weight more central (away from the lateral aspect of the foot). A decrease in symptoms with the correction of the movement impairment supports the diagnosis of supination syndrome. Additionally, the physical therapist can assess the role of insufficient dorsiflexion in symptom reproduction by limiting dorsiflexion motion to avoid end-range or adding a small heel lift. If correction of the insufficient dorsiflexion results in symptom reduction, the therapist needs to consider insufficient dorsiflexion syndrome as a possible movement impairment diagnosis (see the following “Insufficient Dorsiflexion Syndrome” section).
Muscle Length/Joint Range of Motion Impairments
Talocrural Dorsiflexion and Passive First Metatarsophalangeal Dorsiflexion
Limitation in motion at the talocrural joint and the first MTP joint are also associated with the supination movement impairment. Decreased talocrural dorsiflexion during late stance results in either an early heel rise or transfer of weight lateral for the tibia to advance over the foot. Limited first MTP motion results in a transfer of force medial at late stance (push-off) or keeps the force lateral. The tests to determine source of limitation are described in the “Metatarsophalangeal Joints” section.
Footwear Considerations
Heel Counter
In patients with supination syndrome the heel counter should have qualities similar to those recommended for pronation syndrome in that the counter should be made of firm material and hold the heel snugly. In the case of supination syndrome the heel counter will help to control inversion of the calcaneus.
Shoe Sole Components
The supinated foot has a decreased ability to absorb shock during early stance and may require additional attention to cushioning. Sole components, such as air and soft materials, are marketed to attenuate shock (Figure 8-32). Footwear manufacturers rarely add firm material components to the lateral side of the shoe to encourage pronation. However, the individual with supination syndrome should not wear a shoe designed for pronation syndrome because the shoe would have firm materials medially and would encourage the supination movement impairment.
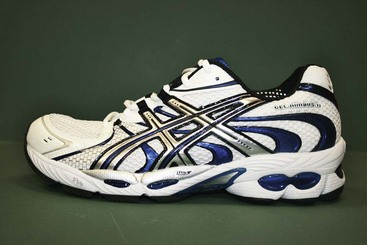
Figure 8-32 Asics GEL-Nimbus 11. Manufactured primarily for cushion and flexibility with the inclusion of gel and sole materials that attenuate shock.
As with pronation syndrome, the sole of the shoe should bend easily only at the MTP joint line. The groove on the forefoot of the shoe should match the patient’s MTP joint line from the first to the fifth toes.
Heel-to-Toe Height
Limited dorsiflexion is also associated with supination syndrome and can be compensated for by lifting the heel slightly above the toe. A reduction in the heel-to-toe height ratio can contribute to symptom onset similar to that described with pronation syndrome.
Arch Support
The lack of contact area of the supinated foot during walking contributes to high pressure. Footwear should be assessed for the ability of the insoles to provide contact, support, and force distribution through the entire foot.
Last Shape
The most common shape of a supinated foot is forefoot adduction relative to the hindfoot. A curved last generally matches the shape of the supinated foot best (Figure 8-33). The shape of the shoe should not be used to force a change in the shape of the foot or to attempt to alter motion of the foot.
Plantar Callus Findings
In the patient with supination syndrome, the location of calluses are generally on the first metatarsal head, fifth metatarsals, and/or medial side of the first toe. Callus formation at the first and fifth metatarsal heads indicates the late lateral loading under the fifth and often a rigid first ray that bears a large load. The medial toe callus is a result of the late pronation that occurs during push-off as a result of the prolonged lateral loading in the supinated foot.
Summary
Supination syndrome is characterized by a rigid, high-arched foot that has little ability to compensate for structural and movement impairments within the foot and ankle or up the leg to the hip. The high arch, calcaneal inversion, and forefoot adduction will be apparent with weight-bearing activities. There is generally poor shock absorption and little loading through the midfoot.
Treatment
Walking and Running
The patient is instructed to work on the tasks that use specific cues that assisted in symptom reduction during the examination or the cues that the physical therapist believes with practice may result in symptom reduction. Often, the cues are related to softening the landing, hitting more centrally on the heel, and concentrating on trying to limit lateral loading through the foot.
Range of Motion
The treatment plan for limited motion is similar to that described for pronation syndrome.
Activity Modification
The general guidelines for activity restriction and progression described in the “Pronation Syndrome” section apply here as well. For supination syndrome, specific suggestions include use of softer surfaces when shock absorption is a concern.
External Tissue Support
Footwear
Footwear for the patient with supination syndrome should include a last that looks like the patient’s foot, most often a semi-curved or curved last. As with pronation syndrome, a firm heel counter to control hindfoot motion and a sole that resists bending from hindfoot to midfoot, bending only at the metatarsal heads, is advisable for most all individuals. Cushioning is important and should be included within the shoe. The cushioning component of the footwear may wear down quickly, and footwear may need to be replaced more frequently. Finally, for all individuals, shoe length and width and height of the toe box should accommodate the size of the foot and any deformities.
Orthoses
As with pronation syndrome, orthoses are not recommended for all patients and the indications for permanent orthoses include significant structural variations, a recurrent problem, or if the foot alignment places the individual at risk for future problems. The temporary orthosis components that may be appropriate for a patient with supination syndrome include arch support to distribute force more evenly but avoid increasing lateral forces and inversion ankle instability.
Taping
Taping to support the arch can be helpful in supination syndrome as well. The indications for taping are that providing support for the arch and assisting with force distribution (arch supports were helpful) decreased symptoms during the examination. Calcaneal (Achilles) tendon irritation can be assisted with a taping technique that provides support to the tissue (Figure 8-34).
Case Presentation
Supination Syndrome
A 35-year-old male, who stands 6 foot tall and weighs 175 lbs, was referred by an internist for evaluation and treatment of right foot pain. His foot pain began approximately 1 month ago during a 10-mile run in new shoes. He reports running approximately 30 miles/week, including 1 long run (10 to 15 miles) on the weekend.
The patient’s pain is located on the plantar surface of the fifth metatarsal head. The patient reports limitation caused by pain during walking (5/10), running (7/10), as well as a very sharp pain (8/10) when he turns on a planted right foot. The pain is reproduced when he manually extends his fifth toe and is generally tender to the touch on the plantar surface. When he is standing, symptoms are minimal (2/10) and absent when sitting. His Foot and Ankle Ability Measure score was 54% (100% indicates normal function) and the Foot and Ankle Ability Measure Sport Scale was 32% (100% indicates normal function).
In standing, the calcaneus is inverted and the arch is high bilaterally. The forefoot is slightly adducted on the hindfoot. There is an increase in lateral tibial torsion. In prone, the assessment of subtalar joint neutral finds hindfoot and forefoot varus alignment.
During walking and running, the calcaneus hits in inversion and remains in an inverted position through late stance. Push-off occurs through the lateral side of the foot, symptoms are 5/10. Symptoms increased to 7/10 during running, and cues to roll through the middle of the foot (not as lateral) during walking and running decreased symptoms to 4/10.
Muscle Length/Joint ROM Impairments
| Right | Left | |
|---|---|---|
| Talocrural dorsiflexion (knee extended) | −5 degrees | 0 degrees |
| Talocrural dorsiflexion (knee flexed) | 0 degrees | 10 degrees |
| First MTP joint extension (30 degrees talocrural plantarflexion) | 25 degrees | 25 degrees |
Joint accessory motion assessment found limited mobility bilaterally during an anterior-to-posterior glide of the talus on the ankle mortise.
Patient is wearing his old running shoes and brought his new running shoes with him. The new running shoes have a curved last, the metatarsal break is distal to the first metatarsal head and proximal to the fifth metatarsal head, and the sole is flexible, bending easily from the middle of the shoe to the toe.
The patient’s movement tests support a movement system syndrome of supination. The patient’s foot is supinated throughout stance with lateral loading of the foot throughout. The likely source of symptoms is the fifth metatarsal head. The stage for rehabilitation is 2. Although the patient’s symptoms are high during weight bearing, symptoms were easily reduced with modification to the walking pattern. The patient is completing daily activities, and the Foot and Ankle Ability Measure indicates moderate disability. The primary contributing factor to the movement impairment is a rigid foot that has little capacity for changing ROM. There is a varus structural variation of the hindfoot and forefoot in the presence of limited calcaneal eversion motion that contributes to supination. Additionally, the new footwear provided little support and encouraged additional lateral loading and hyperextension at the fifth metatarsal joint because the metatarsal head break in his new shoe is proximal to his joint line.
Prognosis is excellent for resolving symptoms with compensations that include modifying footwear with a temporary insert. The patient is relatively young with a short time since onset of symptoms. The severity of symptoms is fairly high but primarily occur with high impact activity. Clinical experience has found very little success in changing talocrural dorsiflexion and first MTP motion in individuals with very rigid and supinated feet.
The primary goal of treatment is to decrease the load borne by the fifth metatarsal head. The patient works to avoid exaggerating the pattern of lateral loading that his foot structure encourages. Cues to heel strike in less inversion and to roll more centrally through his foot do decrease his symptoms and should be implemented as part of the treatment plan. Additionally, a temporary orthosis can be fabricated that will include a metatarsal pad under the fifth metatarsal head to provide unloading of the bone during healing. A lateral post to encourage pronation can be added as well; however, the rigidity of the foot often prevents the lateral post from changing motion and symptoms. A stretching program to address the talocrural and first MTP motion will be implemented. The recommended footwear components for his running shoe include a last that is less curved (semi-curved), a firm heel counter, sole materials and design that allows the primary break in the shoe to occur at the location that matches his metatarsal joints, and an increased heel-to-toe ratio to compensate for limited dorsiflexion.
The patient was seen 1 time/week for 8 weeks. The addition of the temporary orthosis with arch support and a metatarsal pad, change in footwear, stretching program, and cues for changing weight-bearing patterns reduced maximum symptoms to a 2/10 within 2 visits. Complete resolution of symptoms at the fifth metatarsal head required a 3 week rest from running. The patient continued with low-impact aerobic training (bicycling and swimming). As the symptoms improved to 0/10 with walking, running was gradually increased with a walk/run program in which the patient started with running 1 minute and walking 4 minutes for 5 bouts (total weight-bearing time was 20 minutes). Gradually, the amount of time spent running was increased, the amount of time walking was decreased, and the number of bouts were increased until the patient had returned to running 10 miles pain-free.
Insufficient Dorsiflexion Syndrome
The principal movement impairment associated with insufficient dorsiflexion syndrome is insufficient talocrural dorsiflexion. The impairment occurs during midstance to push-off or during swing phase and is not associated with excessive supination or pronation. Limited talocrural dorsiflexion is a common impairment that could be present in all other foot and ankle syndromes. A patient is given the diagnosis of insufficient dorsiflexion only after all other diagnoses have been ruled out (pronation syndrome, supination syndrome, and hypomobility syndrome).
Symptoms and Pain
Plantar Aponeurosis (Fascia)
Involvement of the plantar aponeurosis is most often accompanied by patient complaints of heel pain that are worse with the first step out of bed in the morning and after a period of prolonged non–weight-bearing activities.
Gastrocnemius/Soleus Muscle and Calcaneal (Achilles) Tendon
The patient complains of pain in the muscle belly or tendon, particularly during late stance, as the muscle is working eccentrically and the tendon is being placed on stretch to control the tibia’s progression over the foot and during the concentric contraction required during push-off.
Bursa
Pain is reported at posterior calcaneus, most apparent with direct pressure. The pain provoking pressure can occur during midstance through push off, when squatting or when sitting in a position that applies direct pressure to the bursa.
Anterior Tibialis Muscle and Tendon
The patient complains of pain localized to the muscle at the anterior and lateral proximal fibula or anywhere along the tendon as it follows its course to insert on the medial cuneiform and base of the first metatarsal bone. The symptoms are most apparent from heel strike to foot flat as the anterior tibialis is working eccentrically to lower the foot to the ground or during swing phase as the anterior tibialis is working concentrically to clear the foot.
Deep Fibular Nerve
The patient reports achiness, tingling, and/or numbness on the dorsum of foot and can radiate into toes. Symptoms are most common when shoes are on (tied tightly on the dorsum of the foot) and/or during activities requiring maximum dorsiflexion (running up hills, squatting).
Alignment: Structural Variations and Acquired Impairments
Patients with insufficient dorsiflexion syndrome often stand with knee hyperextension and the ankles in relative plantarflexion. There are no specific clinical tests that can be performed to evaluate the contribution of structural variations to limited talocrural dorsiflexion motion.
Movement Impairments
Walking and Running
During walking and running those with isolated insufficient talocrural dorsiflexion demonstrate a number of gait impairments during stance. The inability of the tibia to easily advance over the foot during late stance can be compensated for in a number of ways: (1) early heel rise, (2) knee hyperextension, and/or (3) increase in the foot progression angle (toe is pointed out). Limited talocrural dorsiflexion during swing phase is also visible, often with overuse of the extensor digitorum and poor stabilization of the metatarsal heads with the intrinsic muscles of the foot (Figure 8-35).
Individuals with insufficient talocrural dorsiflexion often rely on the passive tension of the gastrocnemius and soleus muscles and calcaneal tendon to control the advancement of the tibia over the foot during stance. There is often poor eccentric use of the gastrocnemius muscle in tibial control.
If symptoms are reproduced during stance phase of walking and running, a secondary test is adding a heel lift and assessing symptom reproduction. Cues to contract the gastrocnemius, lifting the heel actively, can be helpful in addressing the use of passive tension. The secondary test for symptoms produced during swing includes cues to relax the toes, avoiding toe hyperextension to see if symptoms are reduced.
Squat
The contribution of limited dorsiflexion to the patient’s pain is often overlooked because active ROM (AROM) in non–weight-bearing activities often appears equal between sides. However, if the patient squats, the therapist will notice that on the involved side, the heel is higher or the tibia is more posterior and this end-range position with loading often reproduces the patient’s complaints (Figure 8-36).

Figure 8-36 Squat test in an individual with limited talocrural dorsiflexion. Note the right heel is higher (less dorsiflexion) than the left.
The secondary test for symptoms produced during end-range squatting is to provide a posterior glide of the talus during squatting.
Step-Down and/or Small Knee Bend
During a step-down or small knee bend, an early heel rise is noted. A secondary test is to add a posterior glide at the talus during the small knee bend or step-down (Figure 8-37).
Footwear Considerations
Recent Decrease in Heel-to-Toe Height
Limited talocrural dorsiflexion can be compensated for by lifting the heel slightly above the toe. A reduction in the heel-to-toe height ratio of the shoe can contribute to symptom onset similar to that described with pronation syndrome. Frequent use of shoes with high heels can contribute to insufficient dorsiflexion syndrome.
Summary
Insufficient dorsiflexion syndrome is characterized by limited talocrural dorsiflexion with the absence of other movement impairments of pronation, supination, or global limitation in motion (hypomobility). The impairment is noted in late stance, during swing, and/or during activities requiring maximum talocrural dorsiflexion (squatting, step-down, lunges, and so on).
Treatment
Walking and/or Running
Walking and running cues focus primarily on encouraging active contraction of the gastrocnemius muscle to reduce the reliance on the passive tension of the gastrocnemius and soleus muscle and calcaneal tendon unit. The specific cues are to have the patient actively lift the heel during late stance.
Decreased Range of Motion
The primary treatment focuses on addressing limited talocrural motion. The treatment options related to length of the gastrocnemius/soleus muscle and tendon are similar to those described for pronation syndrome. Joint mobilizations to increase dorsiflexion are also useful. A unique treatment option to provide a self-mobilization to the talocrural joint includes applying a piece of tape from the talus anterior progressing inferiorly and posteriorly on the medial and lateral side of the talus and attaching the tape to the plantar surface of the calcaneus (Figure 8-38). With the tape in place, the patient performs standing activities requiring tibial advancement over a fixed foot (lunges, squats). The tape can be used during functional activities to assist with providing a stabilizing force for the talus as the tibia advances over the foot during closed chain activities. The tape can be substituted with a towel, and the patient can provide the posterior inferior glide of the talus with the edge of the towel while actively advancing the tibia over the fixed foot (Figure 8-39).
Activity Modification
The general guidelines for activity restriction and progression described in the “Pronation Syndrome” section apply here as well.
External Tissue Support
Footwear
The last of the shoe should match the patient’s foot. Additionally, as with most individuals, a firm heel counter with a sole that bends at the metatarsal head break is generally appropriate. Shoe length and width and height of the toe box should accommodate the size of the foot and any deformities. An increase in the heel-to-toe ratio may be a reasonable compensation, particularly if the treatment to address talocrural dorsiflexion limitation is unsuccessful.
Orthoses
A heel lift may be indicated temporarily or permanently, depending on the ability of the stretching plan to improve talocrural dorsiflexion.
Case Presentation
Insufficient Dorsiflexion Syndrome
Symptoms and History
A 27-year-old male was referred to physical therapy by the orthopedist for treatment of right ankle pain, with an osteochondral defect of the talus and 1 year after microfracture repair.
The patient reports ankle joint pain (5/10) when performing squats during weight lifting. He has had to stop squats. He is also unable to complete some of his taekwondo kicks and positions because of ankle pain. The patient’s pain is located on the anterior talocrural joint, primarily lateral. There is no pain with walking. He has minor pain (3/10) during running. Foot and Ankle Ability Measure score was 95% (100% indicates normal function), and the Foot and Ankle Ability Measure Sport Scale was 68% (100% indicates normal function).
Alignment Analysis
In standing, the calcaneus is vertical and the medial longitudinal arch height is normal. In prone, the assessment of subtalar joint neutral finds hindfoot and forefoot neutral alignment.
Movement Analysis
During walking and running, the calcaneus hits in inversion and moves into eversion through midstance. The calcaneus moves toward inversion during push-off. The same movement pattern is noted during running. Anterior talocrural joint pain is reproduced during late stance phase. Cues to lift heel earlier in stance phase decreased anterior talocrural joint pain. No difference in dorsiflexion ROM is noted during gait assessment.
Small knee bend produced no symptoms, and no movement impairment was noted. A full squat was completed because of the patient’s functional complaint. The heel on the right came off the ground earlier than the left. Symptoms (a pinching feeling) were reproduced at end-range. A posterior glide of the talus during the full squat relieved symptoms.
Muscle Length/Joint ROM Impairments
Talocrural dorsiflexion with the knee extended was 0 degrees on the right and 10 degrees on the left. With the knee flexed, talocrural dorsiflexion was 0 degrees on the right and 15 degrees on the left. Joint accessory mobility was limited with the anterior-to-posterior glide on the right. Subtalar joint motion is normal (10 degrees eversion, 20 degrees inversion), and first MTP motion was normal bilaterally.
| Right | Left | |
|---|---|---|
| Talocrural dorsiflexion (knee extended) | 0 degrees | 10 degrees |
| Talocrural dorsiflexion (knee flexed) | 0 degrees | 15 degrees |
| Subtalar joint inversion | 20 degrees | 20 degrees |
| Subtalar joint eversion | 10 degrees | 10 degrees |
| First MTP joint extension (30 degrees talocrural plantarflexion) | 60 degrees | 60 degrees |
Joint accessory motion assessment found limited mobility during an anterior-to-posterior glide of the talus on the ankle mortise on the right.
Patient is wearing new running shoes. The last was semi-curved, and the heel counter is firm. The sole has gel pockets for cushion in the heel, increased density of the foam under the arch, and bends easily only at the metatarsal head break. The difference between the heel height and toe height of the shoe is 1 inch.
Diagnosis
The patient’s movement tests support a movement system diagnosis of insufficient dorsiflexion. The patient’s foot displays a normal movement pattern of pronation during early stance and supination during push-off. The likely source of symptoms is the anterior talocrural joint. The stage for rehabilitation is 3. Stage 3 is chosen because the patient has pain only with high level activities (pain is not limiting walking and running). The primary contributing factor to the movement impairment is limited talocrural dorsiflexion.
Prognosis
The prognosis for resolving symptoms so that high level activities can be performed with minimal pain is good. The patient is relatively young; however, the duration of limited motion is fairly long and the history of cartilage damage and surgical intervention leaves the status of the anatomy unknown.
Intervention
The patient was seen once/week for 4 weeks and then once every 2 weeks for 8 weeks to assist him in returning to his fitness and sport activities. The primary goal of intervention was to increase talocrural joint dorsiflexion. The home program included prolonged dorsiflexion stretches. The patient was instructed in a self-mobilization with movement using a towel at the talus during dorsiflexion in kneeling. Additionally, physical therapy treatment included anterior-to-posterior glides of the talus on the ankle mortise. The patient also experienced symptom relief with taping the talus to the calcaneus during weight-bearing activities, as well as during stretching. He was taught to tape himself for his daily fitness activities. No footwear changes were recommended, and no heel lift was added.
Outcome
The talus taping technique decreased squatting symptoms to 2/10. The patient progressed over the next 12 weeks to being able to complete all sport activities without symptoms. There were occasional days with ankle symptoms, generally a day or 2 after a vigorous workout. However, the symptoms resolved within 2 to 3 days with rest.
Hypomobility Syndrome
The principal movement impairment in this syndrome is associated with a limitation in the physiological and accessory motions of the foot and ankle. This may result from degenerative changes in the joint or the effects of prolonged immobilization.
Symptoms and Pain
Degenerative Changes
The patient complains of pain with weight bearing (gait, standing, and stairs) that decreases with rest. However, the patient often reports stiffness in the morning or after prolonged periods of rest. The onset of pain is generally gradual, and the location and description of symptoms is often vague and deep within the joint. Osteoarthritis (OA) in the foot and ankle is often associated with a previous history of trauma and joint narrowing and irregular articular surfaces. Rheumatoid arthritis (RA) is associated with joint stiffness, destruction, and deformity.
Alignment: Structural Variations and Acquired Impairments
There are no common structural variations associated with hypomobility. Visually, the calf will appear atrophied. General enlargement of the foot and ankle from edema may be present, as well as localized enlargement from bone and joint changes as a result of the degeneration and/or surgery.
Movement Impairments
Walking and Running
The patient demonstrates a walking pattern that includes a decreased step length on the uninvolved side, decreased stance time on the involved side, an increase in the foot progression angle (toe out), little heel strike, and push-off. The knee may hyperextend to compensate for limited ankle motion. The patient is often dependent on an assistive device and reports limited tolerance of weight-bearing activities. The patient may be unable to run or hop.
Muscle Length/Joint Range-of-Motion Impairments
Hypomobility syndrome includes limitations in physiological and accessory joint motion. Hypomobility syndrome is differentiated from insufficient dorsiflexion syndrome because the limitations in motion are in more directions and include more than the talocrural joint. In most cases, talocrural dorsiflexion is limited in those with hypomobility syndrome, but plantarflexion will also be limited and additional joints can be involved (subtalar, intertarsal, intermetatarsal, and MTP joints). Decreased joint motion related to surgery, trauma, and/or immobilization requires additional research by the physical therapist. A copy of the operative report and/or clarification with the surgeon can assure joints were not purposely fused or that hardware is not traversing a joint. The physical therapist needs a clear understanding as to whether joint motion should be increased or if compensations should be implemented because increasing motion is contraindicated.
During the assessment, if joint limitations are associated with osteoarthritis, repetition of passive motion often improves motion and symptoms. Throughout the examination in an individual suspected of hypomobility, it is likely that the limited joint motion is being compensated for by proximal and distal joints that do not have limited mobility. The hip abduction, knee hyperextension, and midfoot joint dorsiflexion are especially common compensatory motions.
Muscle Strength/Performance Impairments
MMTs of the ankle and foot muscles find weakness throughout. Often the patient is unable to complete even one single-leg heel rise through the full ROM.
Balance and Proprioception Impairment
The ability to maintain single-leg stance on the involved side will be impaired (poor control and decreased duration). Lack of ability to balance on one foot is often evident with the eyes open, and performance will worsen when the patient is instructed to close the eyes, limiting visual input and isolating foot and ankle proprioception.
Summary
Hypomobility syndrome is primarily defined by physiological and accessory joint limitations. Multiple directions of motions and/or joints will be involved in the loss of motion. Associated with the limitation in motion and the history of immobilization is general foot and ankle weakness and impaired balance and proprioception.
Treatment
Decreased Range of Motion
Joint stiffness from injury, surgery, and/or immobilization often requires an aggressive ROM treatment plan. Prolonged stretching with braces, casting, or increasing the duration and frequency of home stretches is often indicated. In therapy, joint mobilization and manipulation are also indicated.
Decreased motion caused by OA and RA is addressed more gently to avoid joint irritation and worsening of symptoms. The limitation to motion often involves changes in bone and joint anatomy, and ROM exercises are often used before activity to improve function and prevent progressive loss of motion not to increase joint motion.
Muscle Performance Impairments
Plantarflexor muscle performance limitations impair function the most. Generally, resistance band strengthening is an appropriate place to start since weight bearing is often painful. Progression to heel raises with a leg-press machine, bilateral heel raises, and single-leg heel raises is important. Completion of heel raises does not always translate into enough strength for push-off with walking and running.
Control of ankle dorsiflexion when landing on the toes during hopping, running, sprinting, and descending stairs is the result of an eccentric contraction of the plantarflexors. Specific eccentric overloading of the plantarflexors is critical for patients with high level activity goals.41-43 Finally, progression to dynamic bilateral and single-leg hopping, cutting, and sport specific exercises is required for full return of plantar flexor strength.
Balance and Proprioception Impairments
Impaired balance and proprioception is often a key contributor to falls and additional injuries. The treatment plan should include progression from eyes open to eyes closed and from solid surfaces to moving/uneven surfaces (mini-trampoline) and should progress to dynamic activities like high marching over objects, kicking balls, and walking backward. When participation in sport activities is a goal, balance and proprioception activities must include progression to quick stops and starts, maintaining balance during player contact, and gradual return to full game participation.
Activity Modification
The general guidelines for activity restriction and progression described in the section on Pronation Syndrome apply here as well. If the patient has OA and RA, continuing with weight bearing, high impact, high-repetition activities (walking or running for fitness) is often contraindicated. The patient often needs to be guided into lower impact activities, such as stationary bicycling, water aerobics, or StairMaster/elliptical, or activities, such as rowing, that involve aerobic fitness through the upper extremities. Weight loss can also significantly impact pain with weight-bearing activities and should be discussed if appropriate for the patient. Use of assistive devices may be temporarily or permanently indicated for patients with arthritis.
External Tissue Support
Footwear
For patients with hypomobility syndrome, shoe size and shape are particularly important. The involved foot and ankle is often larger, and edema fluctuates with weight-bearing activity. A shoe that has extra depth with laces is helpful to accommodate size and edema fluctuation. An increase in the heel-to-toe ratio may be a reasonable compensation, particularly if the treatment to address talocrural dorsiflexion limitation is unsuccessful.
For patients with OA or RA, there are a number of shoe modifications that can be made to assist with foot and ankle symptoms during weight bearing. A steel shank in the sole of the shoe (making the sole of the shoe rigid) with a rocker at the toe break allows the patient to more easily roll over the foot without needing as much talocrural dorsiflexion or MTP dorsiflexion.
Orthoses
For individuals with OA or RA, a total contact insert made of accommodative material is often indicated. Deformities of the foot should be considered in the design and materials chosen for the orthosis. A heel lift may be necessary to manage the loss of dorsiflexion ROM. Temporary orthoses or additional arch support are often indicated to manage foot pain that is often related to the new onset of a pronation impairment that results from the limited foot and ankle mobility.
Case Presentation
Hypomobility Syndrome
Symptoms and History
A 78-year-old male was referred by the orthopedist for evaluation and treatment of the right ankle, status/post (s/p) open reduction, internal fixation (ORIF). The patient states that 6 months ago he fell in his bathroom. His right foot was caught under the cabinet, and he heard a snap. The patient had surgery with pins and plates that provided internal fixation for a fractured tibia and fibula. He was casted for 8 weeks. He had physical therapy 3 times/week at home for the first 4 weeks. No additional physical therapy was ordered by his physician until his 6 month follow-up visit when the physician noted the continued limp and the patient complained of limited ability to complete many activities required by his daily life (taking care of his lawn, walking through the grocery store, and completing his daily walk for fitness). His Foot and Ankle Ability Measure score was 40% (100% indicates normal function).
Alignment Analysis
The ankle, foot, and toes are moderately swollen making assessment of alignment difficult.
Movement Analysis
Muscle Performance Impairments
Patient is unable to tolerate full resistance to any motion. Approximate muscle strength of 2−/5 throughout ankle musculature.
Muscle Length/Joint ROM Impairments
| Right | Left | |
|---|---|---|
| Ankle dorsiflexion (knee extended) | −10 degrees | 6 degrees |
| Plantar flexion | 10-30 degrees | 0-48 degrees |
| Inversion | 0-4 degrees | 0-24 degrees |
| Eversion | 0-2 degrees | 0-8 degrees |
| First MTP dorsiflexion | 0-20 degrees | 0-60 degrees |
Diagnosis
The patient’s movement tests support a movement system syndrome of hypomobility. The patient is 6 months postsurgery, the tissues have healed, but ROM continues to be limited and general foot function is compromised. The stage for rehabilitation is 2. Stage 2 is chosen because the patient is outside of the tissue protection phase and requires progression of activity, strengthening, and ROM. The primary contributing factor to the movement impairment is limited motion at the talocrural, subtalar, and MTP joints. Additionally, ankle and foot muscle performance is limited.
Prognosis
The prognosis for returning the patient to his full function is good. He is older and the duration since onset is long; however, little intervention has been attempted and activity expectations are reasonable.
Treatment
The patient was seen initially 3 times/week for 4 weeks. Treatment frequency decreased to 1 to 2 times/week for 8 additional weeks. The primary goals of intervention were to increase ROM, address muscle performance, and functional limitations. The patient was given a home and in-therapy stretching program to address the talocrural and first MTP motion and a therapist-assisted subtalar joint ROM program. The stretching program began gently, with minimal overpressure, 30-second duration hold, and 3 to 5 times/day frequency. Mobilizations were shy of end–range and were closely monitored for symptom response. Patient progress and tolerance was assessed with the gentle ROM program. The stretching and mobilization treatments were progressed over the first 2 weeks of physical therapy, and prolonged stretching was implemented with the use of a night splint (that can be used during the day) after 3 weeks of physical therapy. Lower extremity strengthening exercises focused on calf, anterior thigh (quadriceps), and hip muscles. Additionally, general fitness was addressed with the stationary bicycling initially, progressing to treadmill and outside walking as patient tolerance increased. Single-limb stance tolerance was addressed initially in the parallel bars, progressing to walking without an assistive device and adding surface variations as tolerated. The canvas shoe provided very little stability for his foot. With the assistance of a trained footwear specialist, he was able to find a shoe that accommodated his edematous foot yet provided support during weight-bearing activities. Edema management included a double thickness of Tubigrip (ConvaTec Inc., Stillman, NJ), extending from the tip of the toes to midcalf.
Outcome
ROM was slow to progress despite the aggressive program. Dorsiflexion at the talocrural joint progressed to 0 degrees, plantar flexion increased to 35 degrees, and first MTP motion increased to 35 degrees by the end of 12 weeks of physical therapy. Despite the lack of full motion, the patient’s strength, balance and proprioception, and weight-bearing tolerance increased so that the patient could walk without a noticeable limp on all flat and uneven surfaces.
Foot and Ankle Impairment
A key criterion for placement into the foot and ankle impairment diagnostic category is the need to protect tissue. Usually, the tissue involved is stressed by a surgical procedure or trauma and may cause significant pain at rest and during movement. The patient is unable to tolerate a typical movement system examination. The limitation in movement is not primarily related to a chronic pain condition. These are general guidelines and not intended to stand alone. Consult the physician for specific precautions, protocols, and progressions. The physical therapist must be familiar with the tissues that were affected in the surgical procedure or injury.
The general diagnosis of foot and ankle impairment is used if the tissue injured and/or impacted by surgery is unknown. The tissue injured and/or impacted by surgery is used in the diagnosis when it is known, through the physician’s referral or the patient’s medical record. For example, the diagnosis might be tibia and fibula fracture s/p ORIF. For additional information regarding the tissue impairment diagnosis, see Chapter 2.
Unique Physiological Factors for the Foot and Ankle
In most cases, the bones, muscles, tendons, cartilage, and ligaments of the foot and ankle respond to stress and follow healing patterns similar to structures elsewhere in the body. There are some unique physiological factors that are specific to the foot/ankle that will help guide the physical therapist in decision making regarding the examination and in planning the treatment program.
Bone
Fractures of the base of the fifth metatarsal have a high probability of nonunion secondary to the pull of the fibularis brevis. Additionally, stress fractures of the anterior lateral tibial diaphysis, medial malleolus, talus, navicular, and sesamoids are high-risk areas that often fail to heal; re-fractures occur and operative intervention is needed.28
Muscle
It is common to loose dorsiflexion ROM and to experience gastrocnemius/soleus muscle atrophy with immobilization.
Tendon
Calcaneal (Achilles) tendon rupture can be treated conservatively with cast immobilization or be surgically repaired with a period of cast immobilization. During the healing process, strong gastrocnemius/soleus contractions and end-range dorsiflexion motions are restricted. After the period of immobilization, the physical therapist needs to cautiously strengthen the gastrocnemius/soleus muscle and tendon.
If severe, a posterior tibial tendon injury or insufficiency may result in significant deformity of the arch (flattening). If treated conservatively, this injury or insufficiency may require long periods of immobilization. Surgical repair with a tendon transfer is often required for resolution of the symptoms. Cast immobilization is typical after posterior tibial tendon repair and tendon transfer. Contraction of the posterior tibial muscle would be contraindicated until adequate healing has occurred.
Ligament
Lateral ankle sprains can be accompanied by fractures. The Ottawa Ankle Rules indicate that indications for additional imaging after ankle sprain include the inability to bear weight or tenderness at the base of the fifth metatarsal, navicular, or the posterior edge or tip of either malleolus.44
Syndesmotic ankle sprain (“high ankle sprain”) is associated with greater discomfort during weight bearing and longer healing time and may require immobilization.45
Skin
Edema has the potential to limit mobility and compromise the space occupied by nerves and arteries. The areas where space is limited and nerves and arteries pass include the compartments within the leg, the extensor retinaculum and the flexor retinaculum.
It is important to inspect the surgical incision. The therapist should note the location, appearance, mobility, sensitivity of the incision, and if the incision appears healed (approximately 10 days). Signs of infection (red, warm, drainage, patient fever, or lymph streaking) should be reported to the physician immediately.
Nerve
The common fibular (peroneal) nerve is superficial and easily injured as it wraps around the head of the fibula. The deep fibular (peroneal) nerve can be compromised as it runs through the anterior compartment of the leg and/or beneath the extensor retinaculum. The tibial nerve can be compressed as it runs through the posterior compartment and/or beneath the flexor retinaculum (tarsal tunnel). The interdigital nerve can be compromised between the metatarsals. The most common site of symptoms is between the third and fourth metatarsals. The interdigital nerve between the third and fourth metatarsals is often enlarged because it can receive nerve fibers from both the medial and lateral plantar nerves.
Unique Assessment and Treatment for the Foot and Ankle
A full and detailed list of items to assess and guidelines for test completion and interpretation are outline in Chapter 2. The items unique to the foot and ankle are highlighted here.
Edema
The foot and ankle are prone to edema after trauma and/or surgery, and this edema warrants close examination, documentation, treatment, and monitoring (Figure 8-40) Treatment often requires the use of compression garments, as well as basic techniques of ice and elevation.
Appearance
Loss of the gastrocnemius/soleus muscle bulk is the most apparent change after a prolonged period of lower extremity immobilization. However, all lower extremity muscles (hip, knee, and foot and ankle) on the involved side will be affected by a period of immobilization.
Proprioception/Balance
When appropriate, given weight-bearing precautions, the ability to maintain single-leg stance with eyes open and with eyes closed should be assessed. Treatment must include activities with the eyes closed to remove visual compensation. Additionally, progression to dynamic activities on variable surfaces is important, including uneven (grass, rocks) and moving (wobble board) surfaces. If interested in returning to sport activities, balance during cutting or rapid changes in direction and sport-specific activities must be assessed.
Functional Mobility
Lower extremity injuries often require the use of an assistive device. The patient’s ability to complete all mobility tasks while maintaining weight-bearing precautions is critical (sit to and from stand, ambulation, stairs, and transfers in and out of a car).
Plantarflexion function during walking and running should be assessed, when allowed. Often, the patient is able to complete single-leg heel raises in standing; however, dynamic plantar flexion function during walking is impaired and the heel fails to rise appropriately during push-off. During running and sprinting the patient will complain of an inability to remain on their toes. Improving gastrocnemius/soleus muscle function can be challenging. A progressive overload program must be established and include the addition of hopping and running.
Summary
Foot and ankle impairment is a classification system that allows the therapist to clarify the tissue involved, as well as the surgery. The examination is guided by the therapist’s assessment of the rehabilitation stage and his or her knowledge of the surgical procedure, precautions, and rehabilitation protocol. This classification is used when there is no apparent and contributing movement impairment, or symptoms are so severe that a full movement system examination cannot be completed.
Case Presentation
Ankle Impairment Stage 1
Symptoms and History
The patient is a 40-year-old female referred by the orthopedist for physical therapy 6 weeks s/p right ankle bimalleolar fracture, ORIF. The patient reports that 6 weeks ago she missed the last step going down to her basement and fractured her right tibia and fibula. The patient reports non–weight-bearing activity in a cast for 2 weeks after surgery and progressed to partial weight bearing in a walking cast for 4 weeks. The physician started her on full weight-bearing activity 3 days ago in a boot. She reports she always has a bit of pain even when sitting or resting (3/10). Pain increases to 5/10 with attempts at full weight bearing activity. Her Foot and Ankle Ability Measure score was 10% (100% indicates normal function).
Alignment Analysis
Patient is obese with visible psoriatic patches noted on bilateral lower and upper extremities. The ankle, foot, and toes are moderately swollen with pitting edema of the right ankle and foot.
Scar: Incision closed, no redness, no warmth, no drainage. Scar is slightly adhered centrally with very mild hypersensitivity to touch.
Movement Analysis
Standing/walking
Assessed in boot only without assistive device. Patient walks with decreased stance time right, no push-off on right, and decreased step length on left.
Muscle Length/Joint ROM Impairments
| Right | Left | |
|---|---|---|
| Ankle dorsiflexion (knee extended) | −16 degrees | −4 degrees |
| Ankle dorsiflexion (knee flexed) | −10 degrees | 2 degrees |
| Plantar flexion | 51 degrees | 54 degrees |
| Inversion | 40 degrees | 43 degrees |
| Eversion | 2 degrees | 8 degrees |
Diagnosis
The patient’s evaluation supports a diagnosis of bimalleolar fracture, s/p open reduction internal fixation, Stage 1. The patient is 6 weeks postsurgery and just beginning to progress toward full weight-bearing activities and is still in an immobilization boot. The patient would likely progress to Stage 2 quickly once weight-bearing tolerance improves. The primary contributing factor to the foot and ankle impairment is the need to protect and gradually load tissue after surgical intervention. Weight-bearing tolerance is limited, talocrural dorsiflexion in decreased, and edema is present.
Prognosis
The prognosis for returning the patient to her full weight-bearing function is good. The patient’s increased weight will likely delay tolerance of full weight-bearing activities.
Treatment
The patient was seen 3 times/week for 4 weeks and then 1 to treatment times/week for 8 additional weeks. The initial goals of treatment were to increase weight-bearing tolerance and wean her from wearing the boot. A home program was implemented to address decreased ROM and as appropriate, strength. The patient received education about edema management and scar mobilization.
Outcome
Initial attempts at weaning from the immobilization boot were met with an increase in irritation of the posterior tibialis tendon from increased pronation during weight bearing. The patient required the addition of a heel lift, scaphoid pad, and arch taping to manage the posterior tibialis tendon symptoms. Two weeks were required for the patient to wean from the boot to regular footwear for ambulation. Talocrural dorsiflexion ROM improved to −5 degrees but remained limited at 6 months after surgery. The patient was instructed to continue with talocrural dorsiflexion stretching, but she continued to need a small heel lift to avoid posterior tibialis tendon irritation.
Proximal Tibiofibular Glide Syndrome
The principal movement impairment is posterior and/or superior motion of the fibula on the tibia during active hamstring contraction (especially during running). The principal positional impairment is the fibula located anterior, posterior, superior, or inferior to the normal position on the tibia after trauma, particularly an ankle sprain.
Symptoms and Pain
Pain in posterolateral or lateral aspect of tibiofibular joint is often associated with running or general tibiofibular pain is associated with a history of lateral ankle sprains. Tingling or numbness can also be reported if the fibular head is compressing the common fibular (peroneal) nerve. The location of the tingling or numbness can be locally at the lateral knee or referred to the lateral distal leg and/or dorsum of the foot.
Alignment: Structural Variations and Acquired Impairments
Palpation of fibula location on tibia, relative to uninvolved side, reveals malalignment (anterior, posterior, and/or superior). A glide in the direction of the positional or movement impairment increases pain. A glide in the opposite direction of the positional or movement impairment will decrease symptoms.
Movement Impairments
Walking/Running
The movement impairment is very small and not visible during motions. Symptoms are localized to the fibular head, or referred to areas innervated by the common fibular (peroneal) nerve or its branches, during walking and running. If the symptoms are reduced or go away with stabilization of the tibiofibular joint the diagnosis of proximal tibiofibular glide syndrome is supported.
Sitting
Resisted hamstring contraction can reproduce symptoms in an individual with proximal tibiofibular glide syndrome, and the symptoms are reduced with joint stabilization.
Talocrural dorsiflexion has associated tibiofibular motions and can reproduce symptoms. If symptoms are related to proximal tibiofibular glide syndrome, stabilization at the proximal tibiofibular joint will reduce symptoms.
Muscle Length/Joint Range-of-Motion Impairments
Hamstring length and talocrural dorsiflexion impairment are common with this diagnosis. Positions when the hamstring are stretched or when the talocrural joint is at end-range of motion can reproduce symptoms. Stabilization of the fibular head during the stretch decreases symptoms.
Summary
Proximal tibiofibular glide syndrome is either a positional fault generally occurring after ankle and foot trauma (ankle sprain) or a movement impairment as a result of hamstring contraction pulling the fibula posteriorly. The positional or movement impairments are difficult to see and palpate, but when correction of a suspected positional impairment or stabilization against a suspected motion decreases symptoms, the diagnosis is supported.
Treatment
Alignment Impairments
Positional impairments of the tibiofibular joint can be addressed by gliding the fibula on the tibia as indicated by evaluation findings.
Decreased Range of Motion
Hamstring and talocrural dorsiflexion limitations should be addressed with a home program.
External Tissue Support
Taping
Taping to immobilize or limit motion between the proximal tibia and fibula can help reduce symptoms (Figure 8-41). Caution should be taken to avoid compression of the common fibular nerve as it passes superficially around the fibular head. Taping of the fibula is a required precursor to hamstring and talocrural stretching exercises that assist in stabilizing the joint during the prescribed exercise. Taping of the fibula is also helpful after mobilization treatments correcting positional impairments.
Conclusions
The foot and ankle are a complex chain of joints that must convert quickly from a flexible adapter and shock attenuator to a rigid lever capable of propelling the body in all different directions. The ability of the foot to perform these diverse and opposing functions and precisely time the function to the intended task is impacted by a number of factors. Joint stability, muscle function, and motor coordination are critical to the foot and ankle. However, function at the foot and ankle is intimately connected to the function and alignment of the knee and hip. The physical therapist is the most highly trained health professional with the ability to evaluate weight-bearing activities, understand the functional requirements of the lower extremity, recognize the movement impairment(s), assess the factors that contribute to the movement impairment, and develop a focused and effective treatment plan.
1 Thambyah A, Pereira BP. Mechanical contribution of the fibula to torsion stiffness in the lower extremity. Clin Anat. 2006;19(7):615-620.
2 Lin CJ, Lai KA, Chou YL, et al. The effect of changing the foot progression angle on the knee adduction moment in normal teenagers. Gait Posture. 2001;14(2):85-91.
3 Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. St Louis: Mosby; 2002.
4 Seber S, Hazer B, Kose N, et al. Rotational profile of the lower extremity and foot progression angle: computerized tomographic examination of 50 male adults. Arch Orthop Trauma Surg. 2000;120(5-6):255-258.
5 Schneider B, Laubenberger J, Jemlich S, et al. Measurement of femoral antetorsion and tibial torsion by magnetic resonance imaging. Brit J Radiol. 1997;70(834):575-579.
6 Yoshioka Y, Siu DW, Scudamore RA, et al. Tibial anatomy and functional axes. J Orthop Res. 1989;7(1):132-137.
7 Piva SR, Fitzgerald K, Irrgang JJ, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskeletal Disord. 7, 2006.
8 McPoil T, Cornwall MW. Relationship between neutral subtalar joint position and pattern of rearfoot motion during walking. Foot Ankle Int. 1994;15(3):141-145.
9 Nigg BM, Cole GK, Nachbauer W. Effects of arch height of the foot on angular motion of the lower-extremities in running. J Biomech. 1993;26(8):909-916.
10 Williams DS, Mcclay IS, Hamill J, et al. Lower extremity kinematic and kinetic differences in runners with high and low arches. J Appl Biomech. 2001;17(2):153-163.
11 Hunt AE, Smith RM. Mechanics and control of the flat versus normal foot during the stance phase of walking. Clin Biomech. 2004;19(4):391-397.
12 Gray’s anatomy: the anatomical basis of medicine and surgery, ed 38. Edinburgh: Churchill Livingstone. 1999.
13 Soavi R, Girolami M, Loreti I, et al. The mobility of the proximal tibio-fibular joint. A roentgen stereophotogrammetric analysis on six cadaver specimens. Foot Ankle Int. 2000;21(4):336-342.
14 Beumer A, Valstar ER, Garling EH, et al. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis. A radio stereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77(3):531-540.
15 Bragonzoni L, Russo A, Girolami M, et al. The distal tibiofibular syndesmosis during passive foot flexion. RSA-based study on intact, ligament injured and screw fixed cadaver specimens. Arch Orthop Trauma Surg. 2006;126(5):304-308.
16 Novacheck TF. The biomechanics of running. Gait Posture. 1998;7(1):77-95.
17 Rattanaprasert U, Smith R, Sullivan M, et al. Three-dimensional kinematics of the forefoot, rearfoot, and leg without the function of tibialis posterior in comparison with normals during stance phase of walking. Clin Biomech. 1999;14(1):14-23.
18 Kaufman KR, Brodine SK, Shaffer RA, et al. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999;5:585-593.
19 Grimston SK, Nigg BM, Hanley DA, et al. Differences in ankle joint complex range of motion as a function of age. Foot Ankle. 1993;14(4):215-222.
20 Astrom M, Arvidson T. Alignment and joint motion in the normal foot. J Orthop Sports Phys Ther. 1995;22(5):216-222.
21 Cornwall MW, McPoil TG. Motion of the calcaneus, navicular, and first metatarsal during the stance phase of walking. J Am Podiatr Med Assoc. 2002;92(2):67-76.
22 Neumann DA. Kinesiology of the musculoskeletal system: foundations for physical rehabilitation. St Louis: Mosby; 2002.
23 Levangie PK, Norkin CC. Joint structure & function: a comprehensive analysis, ed 4. Philadelphia: FA Davis; 2005.
24 Nawoczenski DA, Baumhauer JF, Umberger BR. Relationship between clinical measurements and motion of the first metatarsophalangeal joint during gait. J Bone Joint Surg Am. 1999;81(3):370-376.
25 Hopson MM, McPoil TG, Cornwall MW. Motion of the first metatarsophalangeal joint—reliability and validity of 4 measurement techniques. J Am Podiatr Med Assoc. 1995;85(4):198-204.
26 Flanigan RM, Nawoczenski DA, Chen LL, et al. The influence of foot position on stretching of the plantar fascia. Foot & Ankle Int. 2007;28(7):815-822.
27 Kaeding CC, Yu JR, Wright R, et al. Management and return to play of stress fractures. Clin J Sport Med. 2005;15(6):442-447.
28 Hoppenfeld S. Physical examination of the spine and extremities. Norwalk, CT: Appleton-Century-Crofts; 1976.
29 Evans RC. Lower leg, ankle, and foot. Evans RC, editor. Illustrated orthopedic physical assessment. St Louis: Mosby. 2001.
30 Magee DJ. Orthopedic physical assessment, ed 4. Philadelphia: Saunders; 2002.
31 Goodacre S, Sutton AJ, Sampson FC. Meta-analysis: the value of clinical assessment in the diagnosis of deep venous thrombosis. Ann Intern Med. 2005;143(2):129-139.
32 Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. The Lancet. 1997;350:1795-1798.
33 Riddle DL, Wells PS. Diagnosis of lower-extremity deep vein thrombosis in outpatients. Phys Ther. 2004;84(8):729-735.
34 Kumar V, Cotran RS, Robbins SL. Basic pathology, ed 5. Philadelphia: Saunders; 1992.
35 Sutton-Tyrrell K, Venkitachalam L, Kanaya AM, et al. Relationship of ankle blood pressures to cardiovascular events in older adults. Stroke. 2008;39(3):863-869.
36 Geppert MJ, Mizel MS. Management of heel pain in the inflammatory arthritides. Clin Orthop. 1998;349:93-99.
37 Huether SE, McCance KL. Understanding pathophysiology (with media), ed 4. St Louis: Mosby; 2007.
38 Kinoshita M, Okuda R, Morikawa J, et al. The Dorsiflexion-eversion test for diagnosis of tarsal tunnel syndrome. J Bone Joint Surg Am. 2001;83(12):1835-1839.
39 Lunsford BR, Perry J. The standing heel-rise test for ankle plantar flexion: criterion for normal. Phys Ther. 1995;75(8):694-698.
40 Hastings MK, Mueller MJ, Pilgram TK, et al. Effect of metatarsal pad placement on plantar pressure in people with diabetes and peripheral neuropathy. Ankle Foot Int. 2007;28(1):84-88.
41 Roos EM, Engstrom M, Lagerquist A, et al. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy—a randomized trial with 1-year follow-up. Scand J Med Sci Sport. 2004;14(5):286-295.
42 Alfredson H, Pietila T, Jonsson P, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26(3):360-366.
43 Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport. 2007;10(1):52-58.
44 Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269(9):1127-1132.
45 Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294-298.