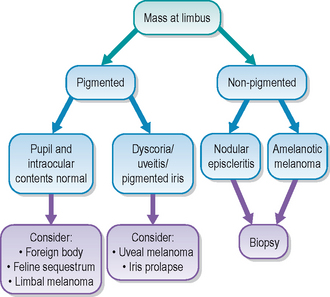
56 Limbal melanoma
PRESENTING SIGNS
The condition can be seen in dogs (particularly German shepherd dogs and Labrador retrievers) and less commonly in cats, and owners present the patient because they have noticed a change in appearance to the eye. Normally only one eye is affected. They have noticed a dark lesion at the junction between the white and clear parts of the eye which is slightly raised and enlarging. Most commonly the lesion is at 12 o’clock but it can be anywhere around the circumference of the cornea. The lesion has usually been noted a few days or even weeks prior to presentation but since the pet shows no signs of discomfort or visual impairment the owners do not tend to present them immediately on noticing the lesion. Indeed, sometimes they will have been aware of it for many months and only point it out to the clinician when the pet is presented for another reason such as vaccination.
CASE HISTORY
The patient is normally clinically well with no relevant current or previous systemic or ocular problems. No treatment has usually been given for the ocular lesion and the owner has been aware of it slowly enlarging.
CLINICAL EXAMINATION
General clinical examination is normal. On ophthalmic examination the patient has normal menace responses and vision is unaffected. Mild localized conjunctival hyperaemia can be present but the eye is certainly not red or inflamed in appearance. No significant ocular discharge is present. A smooth, shiny, raised pigmented mass is present at the limbus. Occasionally it is only poorly or non-pigmented but most are very dark in colour. The lesion covers the limbus and extends into the cornea, with some localized corneal oedema around it. Sometimes an arc of corneal lipid is also present distal to the lesion (lipid keratopathy). It is usually 3–5 mm in diameter on presentation. It is most frequent between the 12 and 3 o’clock position but can be situated anywhere around the limbus – ventral and ventromedial lesions are often much larger before being presented simply because they are more difficult to see. Pupillary light reflexes are normal and no dyscoria is present. The iris is unaffected – it is of normal colour and shape. Viewing the patient from the side with a pen torch will reveal that the lesion is outside the globe and does not include the iris. No uveitis or other intraocular changes are present. Intraocular pressure is normal.
CASE WORK-UP
The main differential for limbal melanoma is extension from a uveal (i.e. iris or ciliary body) neoplasm. This can be achieved by ultrasonography. A limbal melanoma will be seen as a raised mass on the outside of the globe – a stand-off is necessary to allow visualization of such superficial lesions (a surgical glove filled with water or ultrasound gel works very well). A uveal melanoma will show thickening, and usually a discrete mass, within the iris/ciliary body, which then extends outwards towards or even through the sclera. In addition, other ocular signs are more commonly present with uveal tumours (see Table 56.1).
Table 56.1 Differentiation between uveal and limbal melanoma
| Uveal melanoma | Limbal melanoma |
|---|---|
| Dyscoria can be present | Pupil normal |
| Darkening of iris | Iris normal colour |
| Mass visible within iris | Mass on surface of globe |
| Uveal inflammation common | No uveitis |
| Intraocular pressure can be low | Intraocular pressure normal |
| Drainage angle can be affected | Drainage angle normal |
| Difficult to biopsy | Relatively easy to biopsy |
| Relatively common | Uncommon |
| Low risk of metastasis in dogs (4%), higher in cats (60%) | Metastasis not reported |
Gonioscopy is also recommended and referral for this should be considered. With a limbal melanoma there will be no involvement of the drainage angle, while uveal melanomas normally result in pigment deposition and closing of the iridocorneal angle in the affected sector.
Biopsy might be necessary if there is any doubt over the pathology involved, especially if the lesion is poorly or non-pigmented, and thus similar in appearance to nodular episcleritis. Although this can be done with sedation and topical anaesthesia, it is frequently more sensible to anaesthetize the patient.
EPIDEMIOLOGY
Limbal melanomas are also called epibulbar melanomas or melanocytomas. Heavily pigmented breeds such as the German shepherd dog and black Labrador retrievers have a predisposition to the development of melanomas and this certainly applies to limbal melanomas. Some reports suggest that females are at a slightly greater risk than males. However, any breed, and either sex, can be affected and rarely the condition is also observed in cats.
Two distinct age groups are seen with the condition – young dogs aged 2–4 years and an older group aged 8–11 years. The condition is potentially more serious in the younger age range since they tend to grow more rapidly and can be locally invasive. Thus, if left untreated, they can result in intraocular extension and all the consequences that this entails. In older dogs they normally behave in a much more benign manner and can be stationary or only very slowly growing. Metastasis has not been reported.
Histopathologically limbal melanomas consist of a predominance of plump melanocytes. Although the condition is not particularly common, it is very important to recognize and differentiate from uveal melanomas since treatment and prognosis are very much better for limbal melanomas.
TREATMENT OPTIONS – MEDICAL
Although there is no medical management for this condition, in older patients with slowly growing lesions, a ‘wait and see’ approach can be acceptable. Since the lesions tend to be benign in older dogs, and rarely progress to affect vision, patients can be checked at regular intervals (initially every month then reducing to every 3 months). The lesions should be accurately measured with callipers, and diagrams or photographs used to document any changes. Should the lesion start to enlarge, then surgery is appropriate. Surgery is usually advocated in younger dogs and it might be prudent to refer such cases.
TREATMENT OPTIONS – SURGICAL
Surgical removal of limbal melanomas is advised in younger patients and in lesions which are enlarging. If equipped with microsurgical instruments and magnification this can be performed in general practice but referral should be considered. The lesion is removed via superficial keratectomy under general anaesthesia. The corneal portion of the lesion is delineated 2 mm beyond its leading edge with a scalpel blade (Beaver type) and the cornea is grasped with delicate forceps and dissected beneath the pigment towards the limbus. Significant haemorrhage will occur as the limbus is transected and sterile cellulose spears soaked in 10% phenylephrine will help to reduce this. The conjunctival portion of the mass can then be excised. All resected tissue should be submitted for histopathological examination. Normally some pigment will be left around the limbus.
Adjunctive therapy such as photocoagulation (using a diode laser), cryosurgery or β-irradiation has been advocated to destroy any remaining neoplastic cells and most ophthalmologists recommend this. Simply debulking with surgery will not prevent regrowth. The alternate approach is to surgically remove all pigmented tissue. However, this will usually leave a much weakened limbal area (sometimes even removing a full thickness section) and further support in the form of grafts of nictitans cartilage, corneal transplants or adjacent corneal transposition will be required. These are obviously specialist procedures!
Postoperative treatment usually consists of topical antibiotics until the cornea has epithelialized, followed by a few days of topical steroids to reduce any vascular reaction during healing. Patients should be checked every 6 months for signs of regrowth.
Enucleation is not necessary in most cases of limbal melanoma – only in cases which have been neglected or mismanaged such that intraocular extension and subsequent uveitis/glaucoma have developed. It should never be suggested as a first line treatment.
PROGNOSIS
The prognosis for limbal melanomas is good. Older patients can be monitored and many do not require surgery since the lesions tend to be benign. With surgical excision, or extensive debulking followed by laser photoablation, cryosurgery or occasionally local irradiation, younger patients are normally cured of the disease. If left untreated, the more aggressive form in younger dogs will result in intraocular extension and resultant uveitis and secondary glaucoma. These eyes will require enucleation but with early recognition and appropriate management this can be avoided. Metastasis from limbal melanomas has not been reported.
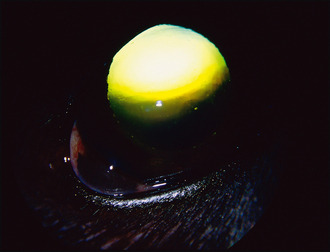
CLINICAL SIGNS
General clinical examination was unremarkable. Vision was good. Abnormalities were confined to the left eye where a black shiny mass was noted at the ven-trolateral limbus, measuring approximately 3 × 4 mm (Figure 56.2).
WORK-UP
No work-up was undertaken initially but the patient was examined again a month later, and the lesion had grown. The patient was referred. Gonioscopy revealed a normal drainage angle and a diagnosis of limbal melanoma was reached.
TREATMENT
Since the dog was young and the lesion was growing, surgery was advised. The mass was removed via superficial keratectomy followed immediately by laser photoablation of the tumour base. Histopathology confirmed a limbal melanoma. Topical chloramphenicol was dispensed four times daily for 5 days along with oral carprofen. After 5 days the cornea was fluorescein negative and dexamethasone drops (Maxidex, Alcon) were supplied twice daily for 10 days.
OUTCOME
The dog did very well. The surgical site healed quickly and although some pigment remained it was flat within the episclera and did not alter in the 12 months of follow-up (Figure 56.3).
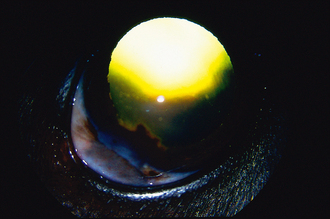
Figure 56.3 Same eye as pictured in Figure 56.2, 12 months following resection and laser ablation. Some pigment scarring is present but there is no evidence of tumour regrowth.
This case illustrates that with accurate diagnosis and appropriate treatment the prognosis for limbal melanoma is very good.